Malformed vertebrae: a clinical and imaging review · 2018-06-07 · Thisreviewarticle...
Transcript of Malformed vertebrae: a clinical and imaging review · 2018-06-07 · Thisreviewarticle...

PICTORIAL REVIEW
Malformed vertebrae: a clinical and imaging review
Apeksha Chaturvedi1 & Nina B. Klionsky1 & Umakanthan Nadarajah2& Abhishek Chaturvedi1 & Steven P. Meyers1
Received: 13 April 2017 /Revised: 21 December 2017 /Accepted: 10 January 2018 /Published online: 3 April 2018# The Author(s) 2018
AbstractAvariety of structural developmental anomalies affect the vertebral column.Malformed vertebrae can arise secondary to errors ofvertebral formation, fusion and/or segmentation and developmental variation. Malformations can be simple with little or noclinical consequence, or complex with serious structural and neurologic implications. These anomalies can occasionally mimicacute trauma (bipartite atlas versus Jefferson fracture, butterfly vertebra versus burst fracture), or predispose the affected indi-vidual to myelopathy. Accurate imaging interpretation of vertebral malformations requires knowledge of ageappropriate normal,variant and abnormal vertebral morphology and the clinical implications of each entity. This knowledge will improve diagnosticconfidence in acute situations and confounding clinical scenarios.This review article seeks to familiarize the reader with the embryology, normal and variant anatomy of the vertebral column andthe imaging appearance and clinical impact of the spectrum of vertebral malformations arising as a consequence of disorderedembryological development.Teaching points• Some vertebral malformations predispose the affected individual to trauma or myelopathy.• On imaging, malformed vertebrae can be indistinguishable from acute trauma.• Abnormalities in spinal cord development may be associated and must be searched for.• Accurate interpretation requires knowledge of normal, variant and abnormal vertebral morphology.
Keywords Vertebral malformations . Children . Spine .Magnetic resonance imaging . Developmental
The vertebral column and spinal cord develop early ingestation in a fine-tuned, sequential manner [1]. Anydisruption of this normal sequence of events can leadto variations in the structural anatomy of the spine andspinal cord [2]. Structural malformations of the spineare often simple and may either go undetected or bediscovered fortuitously. Occasionally, these may becomplex with serious structural or neurological implica-tions [2, 3]. These may occur sporadically, in isolation
or as an accompaniment to multiorgan developmentalmalformations [4]. When symptomatic, these abnormal-ities can predispose the affected individual to biome-chanical instability, spinal canal narrowing and myelop-athy and can even be life-threatening. Developmentaldefects of cardiovascular, neurological, urinary and re-productive systems may be associated [5].
This article overviews the embryology of the verte-bral column and imaging appearance and clinical impactof the spectrum of abnormalities arising as a conse-quence of disordered development. It is difficult to sep-arate discussion of the spine from that of the enclosedspinal cord, so associated spinal cord/brain anomalieswill be mentioned where applicable but will not beelaborated.
Embryology
Development of the spine and spinal cord occurs side byside, intimately intertwined. The vertebral column develops
Electronic supplementary material The online version of this article(https://doi.org/10.1007/s13244-018-0598-1) contains supplementarymaterial, which is available to authorized users.
* Apeksha [email protected]
1 Department of Pediatric Radiology, Golisano Children’s Hospital,University of Rochester Medical Center, 601, Elmwood Avenue,Rochester, NY 14642, USA
2 Sri Jayewardenepura General Hospital, Colombo, Sri Lanka
Insights into Imaging (2018) 9:343–355https://doi.org/10.1007/s13244-018-0598-1

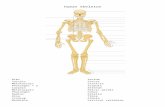
in distinct phases, as illustrated below (Fig. 1a) [5]. Spinalcord development occurs in four basic embryologicalstages including gastrulation (weeks 2 to 3), primaryneurulation (weeks 3 to 4) and secondary neurulation(weeks 5 to 6). Simply put, gastrulation is the process bywhich a bilaminar embryonic disk is converted into atrilaminar structure by migration of epiblastic cells throughthe Hensen’s node (knoblike termination of the primitivestreak containing totipotential cells) to the epiblast/hypoblast interface—a process that ultimately results information of the intervening mesoderm/notochord. The no-tochord plays an important role in somitic differentiation,vertebral chondrogenesis and segmentation [6].
Since the notochord is created during gastrulation, multi-system abnormalities typically coexist with notochordal de-velopmental anomalies [7]. After the notochord interacts with
the overlying ectoderm to form the neuroectoderm, neuraltube closure occurs to complete the process of primary neuru-lation. The sacrum and coccyx develop last at about 31 days ofgestation [5] from a large aggregate of undifferentiated cells(caudal cell mass) representing remnants of the primitivestreak. Underlying embryological processes includecanalisation (secondary neurulation) and retrogressivedifferentiation.
The craniovertebral junction (CVJ) is embryologicallyunique and complex. Four occipital sclerotomes contributeto formation of the occipital bone, clivus and occipital con-dyles, anterior arch of the atlas and the apical, cruciate andalar ligaments. The posterior arch of the atlas is derivedfrom both the first occipital and first cervical sclerotomes.The axis is derived from both the fourth occipital and firstand second cervical sclerotomes. The ventral portion of the
Fig. 1 a-d: Embryology of vertebral bodies and intervertebral discs:Illustration (1–6) demonstrating the steps in development of vertebralbodies from sclerotomes. The sclerotomes migrate around the neuraltube and the notochord forming the vertebral bodies, arches, transverseand spinous processes. Chondrification centres appear during the 6thweek of development within a mesenchymal template, which enclosethe notochord and developing neural tube. The notochord expands anddevelops into the nucleus pulposus of intervertebral disks. The six stagesof vertebral development include: (1) gastrulation and formation of thesomitic mesoderm and notochord, (2) condensation of the somitic meso-derm into somites, (3) formation of dermomyotomes and sclerotomes, (4)formation of membranous somites and re-segmentation with definitivevertebral formation, (5) vertebral chondrification and (6) vertebralossification. b : Ossification of subaxial cervical, thoracic and lumbar
vertebrae: This follows chondrification and typically occurs after 9 weeksof gestation. One dorsal and one ventral primary ossification centre formsfor each vertebral body; these unite to create a centrum, which developsinto three primary loci at the conclusion of embryonic development. Oneof these loci eventually develops into the vertebral body while the othertwo develop into one half of the eventual vertebral arch. c: Developmentof C1 (atlas): The atlas develops from three centres of ossification sepa-rated by cartilaginous synchondroses—one for body and two for lateralmasses. The sequence of appearance and fusion of the ossification centresas noted in the illustration. d: Development of the C2 (axis): Six centres ofossification separated by four cartilaginous synchondroses. Sequence ofappearance and fusion of the ossification centres as noted in theillustration
344 Insights Imaging (2018) 9:343–355

first cervical sclerotome forms most of the odontoid process[3, 5].
The final steps in vertebral formation, chondrification andossification occur after 6 and 9 weeks respectively.Chondrification of the CVJ begins at 45 days andchondrification of the C1 anterior arch begins at 50 to 55 daysof gestation [5, 8].
The subaxial cervical, thoracic and lumbar vertebralbodies each have two ossification centres, which merge,and single ossification centres on each side of the vertebralarch (Fig. 1b). Ossification centres of the first and secondcervical vertebrae follow a predictable sequence and timingof appearance and fusion [9, 10] (Figs. 1c,d and 2). Theatlas should be completely visible on cervical spine radio-graphs by 6–7 years of age [10]. The body of C2 usuallyfuses to the neural arches and dens between 3 and 6 years ofage, and the dens fuses to the ossiculum terminale at12 years [10].
At the sacrococcygeal levels, the first three sacral elementscontain an additional pair of ossification centres. Fusion ofsacral vertebrae begins early in puberty and is complete inthe middle part of the 3rd decade. Ossification of the firstcoccygeal segment begins between 1 to 4 years of age; re-maining coccygeal segments ossify craniocaudally between5 to 20 years of age [11].
Vertebral malformations have been classified based on theunderlying embryopathy [5, 12] (ESM_1). Developmentalvariances leading to transitional vertebrae at the thoracolumbarand lumbosacral junctions and developmentally short/absentpedicles have been identified as a separate category. The sub-sequent paragraphs outline the embryology, clinical and radio-logical manifestations of commonly encountered vertebralmalformations (ESM_1).
Abnormal gastrulation
The embryological processes underlying this spectrum ofmalformations involve disorders resulting from abnormaldevelopment of the notochord during gastrulation. Thesetypically manifest with malformation of the neuraxis andaxial skeleton involving tissues derived from all three pri-mary germ cell layers [13]. Broadly, these include disordersof midline integration of the notochord (split notochordsyndrome, split cord) and disorders of notochordal forma-tion (caudal agenesis and segmental spinal dysgenesis)(ESM_2).
Split notochord syndrome This results from splitting of thenotochord leading to a persistent connection between the ven-tral endoderm and the dorsal ectoderm. The most severe man-ifestation is a dorsal enteric fistula through which the intesti-nal cavity communicates with a dorsal skin surface to themidline, traversing all the intervening structures [11].Variants on this theme include a dorsal bowel hernia anddiverticuli, duplications, cysts or sinuses along this anomaloustract [11].
Split cord/diastematomyelia (Fig. 3a,b) This refers to sagittaldivision of the spinal cord into two symmetric/asymmetrichemicords, each containing a central canal, one dorsal and oneventral horn and each invested by its own leptomeninges [11].
Erroneous specification of the rostrocaudal positionalencoding of prospective notochordal cells can result in in-advertent apoptosis of notochordal precursors and subse-quent interference with primary and secondary neurulation,leading to disordered formation of the notochord; these canmanifest as caudal/sacral agenesis or segmental spinaldysgenesis.
Caudal/sacral agenesis (Fig. 4a-e) This represents a group ofrare structural vertebral anomalies affecting the formation ofthe distal spinal segments and the spinal cord [14]. Theseabnormalities are characterised by varying degrees of devel-opmental failure involving the lower extremities,sacrococcygeal and occasionally distal thoracolumbar verte-brae and the corresponding spinal cord segments [15]. Basedon the underlying embryopathy, there are two broad variants.Type I involve disorders of both primary and secondary neu-rulation, thereby resulting in pronounced agenesis of the distalvertebrae with coexistent aplasia of the caudal metameres ofthe spinal cord, whereas type II involve disorders of onlysecondary neurulation, resulting in less severe vertebral dys-genesis, absence of only the tip of the conus medullaris andassociation with tethered cord syndrome [16]. Associatedmyelomeningoceles, diastematomyelia, tethered spinal cord,thickened filum terminale and lipomas of the cord may bepresent.
Fig. 2 Normal lateral radiograph of the cervical spine in a 13 month oldreveals the ossification centre of the body of the atlas. The posteriorarches have not yet appeared
Insights Imaging (2018) 9:343–355 345

Caudalagenesismaybeacomponent in syndromiccomplexesincluding OEIS (concurrent omphalocele, cloacal extrophy, im-perforate anus and spinal deformities) [17], Currarino’s triad [sa-cral dysgenesis, a pre-sacral mass and anorectal malformation](Fig. 5a-d) and VACTERL anomalies (vertebral anomalies, im-perforate anus, cardiacmalformations, tracheoesophageal fistula,renal anomalies and limb deformities) [7].
A discussion of sacral dysgenesis is incomplete withouta mention of sirenomelia/mermaid sequence (Fig. 6a-b).This rare, lethal congenital anomaly is characterised by anabsent sacrum, rectum and bladder, fused lower extremitiesand bilateral renal agenesis [18]. The underlying aetiologyis believed to be related to vascular disruption to the caudalportion of the embryo [18].
Fig. 4 a-b: Caudal/sacral agene-sis: Lateral radiograph of thespine (a) in one infant reveals ab-sence of the distalscacrococcygeal segments.Accompanying sagittal T2-weighted MR image (b) of thelumbar spine reveals abnormaltruncation of the conus medullaris(arrow). c-e: Caudal agenesis(another neonate): Frontal radio-graph of the abdomen (c) in a ne-onate reveals absence of the entirelumbar and sacrococcygeal spine;the iliac bones are dysmorphicand abnormally close, thoughseparate. Accompanying sagittal(d) and coronal (e) MR images ofthe spine reveal absence of thelumbar-sacrococcygeal segmentsof the spine. Abnormal high ter-mination and truncation of thespinal cord is noted (arrow on d)
Fig. 3 a-b: Split cord/diastematomyelia in 15 year old:Axial (a) and sagittal T2-weighted (b) MR images of thelumbar spine reveals an osseousseptum (thin arrow on a) dividingthe spinal cord into symmet-ric halves (thick, block arrowson a ). Notice that the cord is low-lying and posteriorly positionedwithin the spinal canal (thinarrow on b) and contains a syrinx(block arrow on b ). Associateddural ectasia (star on b) is alsoseen
346 Insights Imaging (2018) 9:343–355

Segmental spinal dysgenesis (Fig. 7a-e) This is a complexspinal dysraphism. Thoracic, lumbosacral segments ofthe spine may be affected. The clinical/radiological def-inition includes: (1) segmental agenesis or dysgenesis ofthe lumbar or thoracolumbar spine; (2) segmental abnor-mality of the underlying spinal cord and nerve roots; (3)congenital paraplegia or paraparesis; (4) congenital low-er limb deformities [16]. The most extreme cases mani-fest with absence of the spinal cord at the affected leveland focal aplasia of the vertebral body, resulting in acutekyphosis [7]. The lower spinal cord is thick and abnor-mally low [7]. Associated lipomas, dermal sinuses orhydromyelia may be present. Horseshoe kidney is com-monly associated [7].
Abnormal alignment of sclerotomal rests
Hemivertebrae These result from complete failure of for-mation of one of the two paired cartilaginous centres ofthe developing vertebra, secondary to tardy developmentof a somite on one side resulting in a caudal metamericsegmental shift of one somatic column relative to anoth-er, leading to an unpaired sclerotome and resultant
hemivertebra [5]. The contralateral vertebral centrumand corresponding dorsal vertebral arch are characteris-tically absent. The ipsilateral posterior arch, though pres-ent, is incorporated into the vertebral arch above orbelow.
Hemivertebrae can occur sporadically or in associationwith spinal dysraphisms, skeletal, cardiac, genitourinaryand gastrointestinal anomalies; the latter category of in-fants is predisposed to increased perinatal mortality [19].
Based on their growth pattern, hemivertebrae can beclassified into the fully segmented (nonincarceratedand incarcerated variants) (Fig. 8a-b), semisegmented(Fig. 8c-e) and nonsegmented. The fully segmented,nonincarcerated hemivertebra has a normal disk spaceabove and below and causes the most disruption of nor-mal spinal curvature; the incarcerated variant is setinto defects in the vertebra above and below and leadsto less pronounced disruption of spinal curvature [20].A semisegmented hemivertebra only has one diskspace adjacent to it. A nonsegmented hemivertebralacks disk spaces on either side, being attached to bothits neighbours; this variant is least likely to result inscoliosis [19].
Fig. 5 a-d: Dysmorphic sacrumwith imperforate anus andpresacral cystic mass: Frontalabdominal radiograph of anewborn demonstrates absence ofbowel gas in the pelvis (a) with ahistory of no passage ofmeconium; the patient had ano-rectal atresia. Pelvic radiograph(b) demonstrates an abnormal sa-crum. Retrograde cystogram (c)demonstrates an elongated uri-nary bladder with extrinsic in-dentations along its posterior as-pect, suggesting a pelvic mass.Pelvic ultrasound (d) demon-strates a lobulated cystic pelvicmass; pathology was consistentwith teratoma
Insights Imaging (2018) 9:343–355 347

Disordered vertebral formation from sclerotomalprecursors
Embryologically, these occur as a consequence of disruptionof the somitic mesoderm during gastrulation, somites duringsegmentation or sclerotomal precursors during the membra-nous phase. Examples include wedge vertebrae and less than10% of hemivertebrae.
Wedge vertebrae These arise as a result of diminished cellcontribution from the ventral sclerotome and thereby dimin-ished centrum height (Fig. 9a-b). As a more severe manifes-tation of this spectrum, the posterior vertebral arches may bedeficient and hypoplastic posterior segments of the adjacentvertebrae may fuse to form a dorsolateral unsegmented barwith associated rib anomalies at the thoracic location. In yetmore severe forms, irregular hemivertebraemay result. These
Fig. 6 a-b: Sirenomelia(Bmermaid sequence^): Post-mortem AP (a) and lateral (b) ra-diographs of the lower body of aprematurely terminated foetusdemonstrates absent sacrum andfused bilateral lower extremities.This anomaly is incompatiblewith life
a c
d
b e
Fig. 7 a-d: Segmental spinaldysgenesis in a neonate: SagittalCT reconstruction (a) and sagittalT2 MR (b) images of the spine inthe neonate with congenitalparaplegia show absence of L1and posterior dislocation of ahypoplastic L2 vertebra into thespinal canal (arrows on a and b).The spinal cord (star on b) isabsent over the affected segmentsof the spine, but is thick andabnormally low further distally(block arrows on c and d). The 3Dbony reformats fromconcomitantly performed CT (e)redemonstrate absence of L1 andhypoplasia of the posteriorlydislocated L2
348 Insights Imaging (2018) 9:343–355

are distinct from hemivertebrae arising secondary tohemimetameric shifts, cross the midline to a variable degreeand comprise less than 10% of all hemivertebrae [5].
Defective vertebral segmentation
These abnormalities occur as a result of failed segmentation ofsomites. These include block vertebrae, unsegmented barsand congenital cervical spine fusions as seen with Klippel-Feil syndrome [21].
Block vertebrae are congenitally fused vertebrae and maybe ventral (affecting only the vertebral body) (Fig. 10),dorsal (affecting the vertebral arch) or both. Unilateralunsegmented bars represent a common cause of congenitalscoliosis. These lack growth plates but the unaffected sideof the spine continues to grow leading to spinal deformities[20]. These may coexist with hemivertebrae. Spinal curva-ture deteriorates at an average rate of 5° or greater annually[20].
Klippel Feil syndrome This represents congenital partial orcomplete fusion of two or more adjacent cervical vertebrae
Fig. 8 a-b: Segmentedhemivertebra in two patients: The3D reconstruction from a non-contrast CT of the spine (a) andcoronal T1-weighted MR imageof different levels of the thoracicspine (b) demonstrate a laterallylocated wedge of bone composedof half a vertebral body (markedby asterisks). Note that there isassociated scoliotic deformity,more pronounced on a. This va-riety of hemivertebra, beingclearly separate from its neigh-bour above and below, has themost potential for impacting spi-nal curvature. c-e:Semisegmented hemivertebra in16 year old: 3D reconstruction(c) and coronal and oblique sagit-tal reconstructions from a non-contrast CT of the spine (d and e)demonstrate a laterally locatedwedge of bone composed of half avertebral body (marked by aster-isks). Note that this variant is at-tached to its neighbouring inferiorvertebra and has only the superiordisc space adjacent to it
a bFig. 9 a-b: Wedge vertebra at T12: Sagittal CT (a) and volumetric CTreconstruction of the spine (b) demonstrate a small, wedge-shaped T12(stars on a and b) with associated focal kyphosis; there was associat-ed scoliosis (not depicted)
Insights Imaging (2018) 9:343–355 349

[22] (Fig. 11a-c). The classic triad including short neck, lim-ited neck motion and low posterior hairline is present in 50%of these patients [23]. According to one retrospective review,the most common lesion is an isolated fusion of C2 and C3[24]. Intraspinal abnormalities such as Arnold-Chiari malfor-mation type I, syringomyelia, diastematomyelia or tetheredcord may be associated. These abnormalities increase the vul-nerability of the cord to traumawith evenminor injury [22, 25,26]. Reduced neck mobility in these patients makes emergen-cy endotracheal intubation challenging [22].
On radiographs, vertebral bodies typically have narrow, tallconfigurations and decreased anteroposterior dimensions withabsent or small intervening disks. Associated fusion of poste-rior elements, occipitalisation of the atlas, congenital scoliosis,kyphosis and Sprengel deformity (see below) may be present.Flexion and extension radiographs should be routinely per-formed in these patients to assess for potential instability[27]. Patients should be counselled to protect themselvesagainst injury.
Sprengel deformityThis refers to a dysmorphic, high-positionedscapula at birth that results from lack of normal caudal migrationof the scapula during embryogenesis. The scapula often has aconvex medial margin, concave lateral margin, decreased heightto width ratio and associated hypoplasia of the scapular muscle[28]. CT can identify associated congenital scoliosis andomovertebral bars and help in surgical planning [28].
Disordered vertebral alignment
This entity results from simple mechanical buckling of theembryo between the 4th and 6th embryonic weeks, after neu-rulation but before chondrification [29]. This commonly oc-curs at or near the thoracolumbar junction and manifests ascongenital vertebral dislocation. The spinal canal at the af-fected level is typically widened, pedicles of the more ceph-alad vertebra are elongated, and the dorsal vertebral arches aredysraphic. The spinal cord is frequently low-lying, althoughintact across the lesion. Usually, patients are neurologicallyintact or present with subtle neurological deficits. Associatedtracheoesophageal fistula and unilateral renal agenesis may bepresent.
Disordered fusion of the sclerotome, chondrificationor ossification centres
Vertebral malformations attributed to disordered assimilationor fusion include butterfly vertebra and dysplasticspondylolysis [30].
Butterfly vertebra (Fig. 12) These manifest as a sagittal cleftbetween the unfused sclerotomal pairs. Moulding of adjacentvertebral bodies towards the midsagittal constriction may ormay not be present. Although usually asymptomatic, this canbe mistaken for compression, burst or wedge fractures onimaging [30].
Localised failure of fusion of ventral and dorsal ossificationcentres can result in malformed vertebral pedicles or facets(dysplastic spondylolysis). When this process occurs dorsally,spina bifida occulta can result.
Disordered ossification
Failure of development of the vertebral centrum duringlate stages of gestation manifests as isolated hypoplasiaor aplasia of the vertebral centrum, without correspond-ing alterations in the dorsal vertebral arch. On imaging,part or all of the vertebral centrum may be absent withintact pedicles and posterior body up to the neurocentralsynchondrosis. Also included in the spectrum are dorsalhemivertebra with isolated absence or wedging of theventral portion of the centrum [5].
Fig. 10 Ventral block vertebra in 8 month old: Lateral radiograph of thespine demonstrates fused L2 and L3 vertebral bodies (arrow). The T12and L1 vertebral bodies were also partially fused
350 Insights Imaging (2018) 9:343–355

Craniovertebral junction (CVJ) malformations
The unique embryology of the craniovertebral junction pre-disposes this region to some unique developmental errors(ESM_3). Abnormalities of the CVJ can impact the cervical
spinal cord, brainstem, cerebellum, cervical nerve roots, lowercranial nerves and vascular supply to these structures.Atlanto-occipital assimilation is the most common congenitalanomaly of the craniovertebral junction (Fig. 13a-b). Osodontoideum (Fig. 14a-c) refers to a circumferentially
Fig. 11 a-c: Klippel-Feil abnor-mality with Sprengel shoulder:Frontal radiograph of the neckand upper chest in an 11 year olddemonstrates marked elevation ofthe left scapula. Also seen aresegmentation anomalies of thecervical spine (demarcated bycircle on a). Sagittal (b) and axial(c) T2-weighted MR imagesdemonstrate a large bonyomovertebral bar (marked byasterisks on both images) extend-ing between the medial border ofelevated scapula and spinousprocess of a lower cervicalvertebra
Fig. 12 Butterfly vertebra in twopatients: Coronal reformattedimage from a non-contrast CT ofthe spine (a) and coronal T1-weighted MR image of the upperthoracic spine (b) both demon-strate separate ossification centreson each side of the vertebral body(marked by asterisks). Note thatthere is moulding of the adjacentvertebral bodies towards the mid-sagittal constriction, especiallypronounced on a
Insights Imaging (2018) 9:343–355 351

corticated ossific fragment separated from a hypoplastic orforeshortened base of the dens [31, 32]. The two subtypesinclude orthotopic and dystopic [31]. This can be stable orunstable [31]; the latter, if symptomatic, should be surgicallyaddressed [33]. Klippel-Feil anomaly, spondyloepiphysealdysplasia, Down syndrome and Morquio syndrome may beassociated.
Persistent ossiculum terminale (Fig. 15a-b) This condition ex-ists when the ossiculum terminale (secondary ossification cen-tre located at the superior margin of dens) fails to fuse with thedens, a process that normally occurs early in the 2nd decade oflife. Usually incidental, this may mimic a type I dens fracture;both are typically stable [31]. Smooth, corticated margins
characterise a persistent ossiculum terminale, whereas irregu-lar, lucent margins are seen with acute type I fractures of thedens, enabling differentiation [31].
Other abnormalities of this region include congenitally ab-sent anterior/posterior atlas arches (Fig. 16a-b), odontoid tip/entire odontoid, bifid odontoid, fused odontoid tip with infe-rior clivus, with basilar invagination and hypoplastic occipitalcondyles [3] (ESM_3).
Developmental variance
This category includes vertebral malformations that do notstrictly fall under any of the above categories but arise second-ary to variances in development. Entities discussed under this
Fig. 14 Dystopic os odontoideumin a 19 year old: Sagittal (a),coronal (b) and axial (c) imagesfrom a non-contrast CT in a 19year old demonstrate a well-corticated ossific density alongthe superior margin of the dens(marked by asterisks on images a,b and c). The dens itself is rela-tively small with a foreshortenedbase (block arrow on b). Note thatthe os odontoideum is locatedsomewhat posterior to the C2body and is therefore not in itsexpected anatomic location
Fig. 13 Atlanto-occipitalassimilation in a 19-year-old fe-male: Coronal (a) and sagittal (b)reformats from a cervical spineCT reveal abnormal fusion of theright-sided arch of atlas with thecorresponding occipital condyle(arrows). The structures areclearly separate on the left
352 Insights Imaging (2018) 9:343–355

category include transitional vertebrae [34] and congenitallyshort/absent vertebral pedicles.
Thoracolumbar and lumbosacral junctional variancesThoracolumbar junctional variances manifest either as anincrease or decrease in the number of rib-bearing thoracicvertebrae or altered appearances of the costal processes ofthe most caudal thoracic or the uppermost lumbar vertebra.Lumbosacral transitional vertebrae have been described aseither sacralisation of the lowest lumbar segment orlumbarisation of the most superior sacral segment of the spine[35]. On imaging, these are best seen with CT. Clinically,these can be associated with back pain/BBertolotti syndrome^[36] and can lead to nomenclature and/or surgical errors [37].Castellvi et al. proposed a radiographic classification systembased on the morphological characteristics of these vertebrae[38]. Treatment may be conservative or surgical.
Congenital/developmental spinal stenosis secondary to shortpedicles (Fig. 17a–b) This developmental variant manifestsas narrowing of the anteroposterior dimension of the spi-nal canal to less than 10 mm or thecal sac cross-sectionalarea less than 77 ± 13 mm² [39]. This occurs most com-monly at the level of the lumbar spine, where it maypresent with neurogenic intermittent claudication andradiculopathy [40]. The spinal cord is vulnerable to trau-ma or disk herniation. In one prospective cohort study[39], the measured pedicle lengths among congenitallystenotic patients approximated 6 mm whereas the controlgroup had pedicle lengths closer to 9 mm.
Pedicular agenesis [41] This unusual disorder manifestswith isolated agenesis of a vertebral pedicle, most com-monly C5 or C6. Imaging findings include misleading ap-pearance of enlarged ipsilateral neural foramen, dysplasticdorsally displaced ipsilateral lamina and a dysplastic
Fig. 15 Persistent ossiculum terminale: Sagittal (a) and axial (b) imagesfrom a non-contrast CTof the cervical spine in a 32 year old demonstratea small, well-corticated ossific density along the superior margin of thedens (arrows on images a and b). This likely represents the persistentossiculum terminale, which arises as a result of failure of fusion of thesecondary ossification centre with the superior aspect of the dens. Thisentity can be mistaken for a remote type I fracture of the dens
Fig. 16 Hypoplasia/aplasia of the posterior arch of C1. Axial CT imagesat the level of the atlas on two patients reveal cervical vertebral cleft(posterior rachischisis) in a and absent posterior arches in b. Also noteanterior vertebral body clefts on both images
Insights Imaging (2018) 9:343–355 353

ipsilateral transverse process. Although a stable congenitalanomaly, this can be mistaken for acute trauma [42].
Conclusion
Structural abnormalities of the spine can occur at multiplelevels and have a variety of imaging and clinical manifesta-tions. The radiologist plays an important role in assessingthese abnormalities and can alert the clinician to the likelihoodof a serious complication arising secondary to such abnormal-ities and assist in the pre-operative workup and postoperativefollow-up.
Acknowledgments The authors are grateful to Margaret Kowaluk,Nadezhda Kiriyak and Gwen Mack from the Graphics section,Department of Imaging Sciences, University of Rochester MedicalCenter, Rochester, New York, for help with radiographic images andoriginal artwork in this article.
Open Access This article is distributed under the terms of the CreativeCommons At t r ibut ion 4 .0 In te rna t ional License (h t tp : / /creativecommons.org/licenses/by/4.0/), which permits unrestricted use,distribution, and reproduction in any medium, provided you giveappropriate credit to the original author(s) and the source, provide a linkto the Creative Commons license, and indicate if changes were made.
References
1. Meyers SP. Differential Diagnosis in Neuroimaging-Spine:Thieme; December, 2016
2. Trenga AP, Singla A, Feger MA, Abel MF (2016) Patterns of con-genital bony spinal deformity and associated neural anomalies onX-ray and magnetic resonance imaging. J Child Orthop 10(4):343–352
3. Klimo P Jr, Rao G, Brockmeyer D (2007) Congenital anomalies ofthe cervical spine. Neurosurg Clin N Am 18(3):463–478
4. Passias PG, Poorman GW, Jalai CM et al (2017) Incidence of con-genital spinal abnormalities among pediatric patients and their as-sociation with scoliosis and systemic anomalies. J Pediatr Orthop
5. Dias MS (2007) Normal and abnormal development of the spine.Neurosurg Clin N Am 18(3):415–429
6. Fleming A, Keynes RJ, Tannahill D (2001) The role of thenotochord in vertebral column formation. J Anat 199(Pt 1–2):177–180
7. Schwartz ES, Rossi A (2015) Congenital spine anomalies: theclosed spinal dysraphisms. Pediatr Radiol 45(Suppl 3):S413–S419
8. David KM, McLachlan JC, Aiton JF et al (1998) Cartilaginousdevelopment of the human craniovertebral junction as visualisedby a new three-dimensional computer reconstruction technique. JAnat 192(Pt 2):269–277
9. Copley LA, Dormans JP (1998) Cervical spine disorders in infantsand children. J Am Acad Orthop Surg 6(4):204–214
10. Kim HJ (2013) Cervical spine anomalies in children and adoles-cents. Curr Opin Pediatr 25(1):72–77
11. Barkovich JARJ (2012) Pediatric Neuroimaging. 5th Ed. ed.Lippincott Williams and Wilkins, Philadelphia, PA
12. Tsou PM, Yau A, Hodgson AR (1980) Embryogenesis and prenataldevelopment of congenital vertebral anomalies and their classifica-tion. Clin Orthop Relat Res 152:211–231
13. Dias MS, Walker ML (1992) The embryogenesis of complexdysraphic malformations: a disorder of gastrulation? PediatrNeurosurg 18(5–6):229–253
14. Singh SK, Singh RD, Sharma A (2005) Caudal regression syn-drome—case report and review of literature. Pediatr Surg Int21(7):578–581
15. Boulas MM (2009) Recognition of caudal regression syndrome.Adv Neonatal Care 9(2):61–69 quiz 70-1
16. Rossi A, Biancheri R, Cama A, Piatelli G, Ravegnani M, Tortori-Donati P (2004) Imaging in spine and spinal cord malformations.Eur J Radiol 50(2):177–200
17. Pang D (1993) Sacral agenesis and caudal spinal cordmalformations. Neurosurgery 32(5):755–778 discussion 78-9
18. Sikandar R, Munim S (2009) Sirenomelia, the mermaid syndrome:case report and a brief review of literature. J PakMed Assoc 59(10):721–723
19. Johal J, LoukasM, Fisahn C, Chapman JR, Oskouian RJ, Tubbs RS(2016) Hemivertebrae: a comprehensive review of embryology,imaging, classification, and management. Childs Nerv Syst32(11):2105–2109
Fig. 17 Congenital stenosis of thespinal canal: Sagittal (a) and axial(b) T1-weighted MR images ofthe lumbar spine reveal narrowedanteroposterior diameter of thespinal canal (< 10 mm)
354 Insights Imaging (2018) 9:343–355

20. Oskouian RJ Jr, Sansur CA, Shaffrey CI (2007) Congenital abnor-malities of the thoracic and lumbar spine. Neurosurg Clin N Am18(3):479–498
21. Tracy MR, Dormans JP, Kusumi K (2004) Klippel-Feil syndrome:clinical features and current understanding of etiology. Clin OrthopRelat Res 424:183–190
22. Xue X, Shen J, Zhang J et al (2014) Klippel-Feil syndrome incongenital scoliosis. Spine (Phila Pa 1976) 39(23):E1353–E1358
23. Hensinger RN, Lang JE, MacEwen GD (1974) Klippel-Feil syn-drome; a constellation of associated anomalies. J Bone Joint SurgAm 56(6):1246–1253
24. Winter RB, Moe JH, Lonstein JE (1984) The incidence of Klippel-Feil syndrome in patients with congenital scoliosis and kyphosis.Spine (Phila Pa 1976) 9(4):363–366
25. Samartzis D, Lubicky JP, Herman J, Shen FH (2006) Faces of spinecare: from advanced imaging. Severe thoracic kyphoscoliosis in aKlippel-Feil patient with complete cervical spine fusion and defor-mity—primum non nocere. Spine J 6(6):723–724
26. Vaidyanathan S, Hughes PL, Soni BM, Singh G, Sett P (2002)Klippel-Feil syndrome—the risk of cervical spinal cord injury: acase report. BMC Fam Pract 3:6
27. O’Donnel DP, Seupaul RA (2008) Klippel-Feil syndrome. Am JEmerg Med 26(2):252 e1–252 e2
28. Harvey EJ, Bernstein M, Desy NM, Saran N, Ouellet JA (2012)Sprengel deformity: pathogenesis and management. J Am AcadOrthop Surg 20(3):177–186
29. Dias MS, Li V, Landi M, Schwend R, Grabb P (1998) The embryo-genesis of congenital vertebral dislocation: early embryonic buck-ling? Pediatr Neurosurg 29(6):281–289
30. Satpathy A, Sloan R, Bhoora IG (2004) Compression fracture orbutterfly vertebra: diagnostic importance in a trauma setting. Ann RColl Surg Engl 86(6):W41–W43
31. O’Brien WT Sr, Shen P, Lee P (2015) The dens: normal develop-ment, developmental variants and anomalies, and traumatic inju-ries. J Clin Imaging Sci 5:38
32. Nguyen JC, Pollock AN (2015) Os odontoideum. Pediatr EmergCare 31(3):225–227
33. Arvin B, Fournier-Gosselin MP, Fehlings MG (2010) Osodontoideum: etiology and surgical management. Neurosurgery66(suppl_3):A22–A31
34. Wigh RE (1980) The thoracolumbar and lumbosacral transitionaljunctions. Spine (Phila Pa 1976) 5(3):215–222
35. Konin GP, Walz DM (2010) Lumbosacral transitional vertebrae:classification, imaging findings, and clinical relevance. AJNR AmJ Neuroradiol 31(10):1778–1786
36. Elster AD (1989) Bertolotti’s syndrome revisited. Transitional ver-tebrae of the lumbar spine. Spine (Phila Pa 1976) 14(12):1373–1377
37. Hughes RJ, Saifuddin A (2004) Imaging of lumbosacral transitionalvertebrae. Clin Radiol 59(11):984–991
38. Castellvi AE, Goldstein LA, Chan DP (1984) Lumbosacral transi-tional vertebrae and their relationship with lumbar extradural de-fects. Spine (Phila Pa 1976) 9(5):493–495
39. Singh K, Samartzis D, Vaccaro AR et al (2005) Congenital lumbarspinal stenosis: a prospective, control-matched, cohort radiographicanalysis. Spine J : Off J N Am Spine Soc 5(6):615–622
40. Cowley P (2016) Neuroimaging of spinal canal stenosis. MagnReson Imaging Clin N Am 24(3):523–539
41. Abduljabbar FH, Rossel F, Nooh A, Jarzem P (2015)Misdiagnosing absent pedicle of cervical spine in the acute traumasetting. Orthop Rev (Pavia) 7(3):5889
42. Ferracci FX, Dudoit T, Gilard V, Perez A, Lucas F (2017) Cervicalpedicular agenesis: case report and a review of the literature.Neurochirurgie 63(4):323–326
Insights Imaging (2018) 9:343–355 355