Making Best Use of Speech-Language Therapy: When to Refer and What to Expect
-
Upload
bilinguistics -
Category
Health & Medicine
-
view
2.342 -
download
1
Transcript of Making Best Use of Speech-Language Therapy: When to Refer and What to Expect
Making the Best Use of Speech-Language Therapy
Celia Neavel, MD, FSAHMLee Anne Holmberg M.A., CCC-SLP
Ellen S. Kester, Ph.DJon Yates, AAC Specialist
2012, Dell Children’s Hospital, Austin, TX
OBJECTIVES
1. Discuss speech and language in school-age youth.
2. Identify when referral for Speech-Language Evaluation and Therapy would benefit the patient.
3. Explain utilization of Alternative and Augmentative Communication (AAC).
4. Describe community resources for youth with speech and language delay and their families.
ALL OF THE DOCUMENTS AND CHARTS IN THISPRESENTATION CAN BE DOWNLOADED FROM OURFREE RESOURCE LIBRARY.
Click here to visit the Resource Library
LANGUAGE DISORDERS Language
Shared system for communicating Involves sounds, signs, gestures, and/or spoken or
written words Specific Language Impairment
Absence other developmental problems Other language disorders assoc. with
Hearing impairment Autism Mental retardation Congenital or acquired disorders of brain
development Head injury, brain tumors.
NORMAL LANGUAGE DEVELOPMENT IN CHILDREN AND ADOLESCENTS
Verbal AND non-verbal; follows predictable course
4-5 y.o. 200-300 words; can describe, define, answer why; tell
simple story; understandable to all 5-6 y.o.
Understands > 2000 words, sequencing, rhyming; creates stories; carries out series 3 directions
School Years; Huge demand on skills for school and social
acceptance; emerging figurative language
WARNING SIGNS SCHOOL-AGED CHILD
Phonological awareness problems
New inattentive or not well-controlled ADHD
Problems reading, writing, understanding social
interactions
Feelings hurt or gets angry/frustrated
Trouble learning second language
Parents with language/literacy problems
LANGUAGE AND COGNITIVE DEVELOPMENT INADOLESCENTS
Core language skills established. Semantics, syntax, language concepts and basic pragmatic skills Early adolescents more concrete
Adult pragmatic and social language skills being refined, including ability to: Interact with adults and peers in classroom and social
activities Maintain or shift topic of the conversation; participate
appropriately in conversation Take another person’s point of view to know what information
is needed during a communication event Incorporate subtle variations in tone, word usage, rhythm
depending on situation
IMPLICATIONS OF VOICE, SPEECH, AND LANGUAGE DISORDERS
Need to communicate to function in our society
Affect emotional and social life, education and job
Substantial cost in life quality and human
potential
Number will likely increase Improved survival for medically fragile infants and
individuals who sustained injury or acquired disease
GOALS FOR INTERVENTIONS Help with developmental trajectory Maintain or improve self-esteem Maximize function Decrease anxiety Educate other important adults so can:
Understand youth’s weaknesses Make appropriate modifications and contribute
further to interventions
IDENTIFYING VOICE, SPEECH, AND LANGUAGE DISORDERS Suspected by family, physician, or educator
Consider delayed versus disordered ASK FUNCTIONING AGE
Speech-language pathologists evaluate & diagnose History, exam, comparison to standardized norms
Voice assessment Speech assessment
Motor speech disorders and/or stuttering Language assessment
Formalized questionnaires; direct observation; testing vocabulary, understanding, word and sentence production, language in social situations
Must take into account the native language of the speaker
BILINGUAL CHILDREN
Ellen S. Kester, Ph.DPresident, Bilinguistics Speech and Language Services5766 Balcones Drive, Suite 205Austin, TX 78731(512) 480-9573 Phone (512) 458-9573 Faxwww.bilinguistics.com
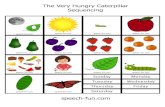
EXAMPLES FROM BILINGUISTICS
4-year-old Spanish-speaking child with a total of approximately 20 words, who could follow one-step commands with gestures but not without gestures. Intelligibility of 30-40%.
3-year-old bilingual child who has difficulty following simple directions with gestures. He uses single words and two-word utterances. Intelligibility is 40-50%.
Neither of these children had been referred for a speech-language evaluation previously.
WHY DO WE GET REFERRALS LIKETHIS? Misconceptions about bilingual development Mobility of population Parents don’t understand “no cost” options Parents not comfortable expressing concerns Parents not aware of developmental differences Parents may be aware of differences, but not
know value of early intervention Language barriers may impede referral process
Children code switch between languages because they don't know either language well.
Raising children with two languages will confuse them.
Children with language impairment should not learn more than one language at a time.
Children who use the sentence structure of one language when speaking the other likely have language impairment.
We should expect bilingual children to be delayed in developing communication skills
Bilingual children develop early vocabulary at the same rate as monolingual children (Pearson, 1993).
Early language milestones are similar (single words, lexical spurt, 2-word phrases, following directions) (Pearson and
Fernandez, 2001).
Conceptual scores are similar (Pearson, 1998).
DETERMINING SPEECH-LANGUAGEIMPAIRMENT IN BILINGUALS
EnglishEnglishSpanish
OKSpanish
OK NormalNormal
EnglishOK
EnglishOK
Spanish Spanish NormalNormal
EnglishEnglish SpanishSpanishImpaired*Impaired*
Difficulty learning both languages, even with adult assistance
Family history of language/learning disabilities Slower development than siblings Difficulty interacting with peers Inappropriate pragmatic/social language skills (i.e.,
turn-taking, topic maintenance, considering listener needs, non-verbal communication)
Difficulty with language in many routines Idiosyncratic error patterns Language performance unlike others with similar
cultural/linguistic experiences
Click here to visit the Resource Library
SPEECH-LANGUAGE PATHOLOGY YOUSHOULD KNOW
• Language Disorders:– Receptive Language Disorder– Expressive Language Disorder– Pragmatic Language Disorder
• Articulation Disorders:– Oral Apraxia– Stuttering-– Voice Disorder
• Feeding Disorder:– Dysphasia
A FEW DIAGNOSIS THAT WARRANT REFERRAL TO SPEECH-LANGUAGE PATHOLOGIST Children with ADD or ADHD
Hearing Loss or Chronic Ear Infections
Cleft Palate or other Craniofacial Anomalies
Difficulty Feeding and Swallowing
Autism Spectrum Disorders
Variety of Syndromes including- Down Syndrome, Fragile X
Syndrome, Turner’s Syndrome, etc.
Children with Cerebral Palsy
OTHER SITUATIONS THAT WARRANT REFERRAL TO SPEECH-LANGUAGE PATHOLOGIST Children that schools discharged from speech therapy Learning disabilities or children struggling in school School-aged and cannot identify significant details in story or
situation and then sequence them in understandable way 2 – 5 y.o. with very small vocabulary and having difficulty
stringing words together in phrases and sentences When parent of a 2 y.o. or older says, “My child is not talking and
using words, and does not seem to understand me.” When parent says, “I do not understand what my child says.”
Please do not tell a parent who is concerned to wait until child is 4 or 5 y.o. A lot of speech-language development goes on before then!!!!
TESTS MOST COMMONLY USED FOR EVALUATIONS Language Tests:
Preschool Language Scale 4 (PLS4) Clinical Evaluation of Language Functioning (CELF) Clinical Evaluation of Language Functioning-Primary (CELF-
P) Test of Language Disorders (TOLD)
Articulation Tests: Goldman Fristoe Test of Articulation
WHAT TO LOOK FOR IN SPEECH-LANGUAGE REPORT
Speech-language diagnosis accompanies medical diagnosis, if applicable
Chronological age of child included
Standard scores from formal testing (average range 85-
115)
Language age levels in all subtests of formal testing
Narrative discusses child’s strengths and weaknesses
Specific recommendations
Stated goals to be addressed in therapy
WHAT A SPEECH-LANGUAGEPATHOLOGIST CAN OFFER
• Speech and language Screenings, evaluations, and treatment.
• Recommendations for referrals to other therapies i.e. OT, PT
• Collaboration with other service providers (doctors, psychologists, other therapists, and schools).
• Education on the child's communication issues for parents, and other providers
• Parent training on communication and the child’s needs and goals
WORKING WITH THE SCHOOLS:WHAT SPEECH-LANGUAGE PATHOLOGIST FOCUSES ON
Collaboration with teachers, school speech-language pathologists, and counselors
Education and training on specific techniques that are working well in the child’s therapy
Opening a dialogue to share progress and difficulties the child is experiencing
QUESTIONS TO SCREEN FOR POSSIBLE SPEECH-LANGUAGE DELAYS
Young Children:How much is your child talking?How many words is your child using?How many words is your child stringing
together? Is your child able to follow directions (Go
get your shoes.)?Does your child understand what your are
telling him/her?How much are you able to understand
your child?
QUESTIONS TO SCREEN FOR POSSIBLE SPEECH-LANGUAGE DELAYSAdolescents: How is your child functioning in school? How much of what your child tells you are you
able to understand? Is your child able to use logical sentence? Is their spoken grammar correct? Is your child able to identify the main details in a
story? Then is your child able to sequence these main
details to retell the story? Can your child follow multi-step directions? Does your child have pronunciation difficulties?
WHAT IS AUGMENTATIVE ALTERNATIVECOMMUNICATION (AAC)?
Augmentative and alternative communication (AAC) includes all forms of communication (other than oral speech) that are used to express thoughts, needs, wants, and ideas.
asha.org
TYPES OF AACUnaided AAC: Using body to communicate with
others. Includes, gestures, body language, and/or sign language.
Aided AAC: Using tools along with the body to communicate with others. Tools can include: Pencil and paper. Communication boards or communication books. Electronic Voice Output Devices (VOD).
www.asha.org
TOTAL COMMUNICATION APPROACH TOAAC Includes use of combination of speech, gestures, sign,
and AAC.
Important because it gives person variety of methods to use for successful communicate with others.
TYPES OF CLIENTS WITH AN AAC DEVICESEEN AT EASTERS SEALS
Clients with Down Syndrome
Clients with profound oral apraxia
Autistic clients
Clients with severe Cerebral Palsy
ASSESSMENT
AAC Devices recognized as treatment by:
American Medical Association
American Academy of Neurology
American Academy of Physical Medicine & Rehabilitation
American Speech-Language Hearing Association
CONDITION SETS THAT BENEFIT FROM THE USE OF A COMMUNICATION DEVICE
•Cerebral Palsy•Down Syndrome•Mental Retardation•Autism•Muscular Dystrophy
Congenital/Develop‐mental
Acquired
Child Adult
•Traumatic Brain Injury (TBI)
•Spinal Cord Injury (SCI)
•TBI •Stroke•SCI
•Amyotrophic Lateral Sclerosis (ALS)
• Parkinson’s Disease•Huntington’s Disease•Multiple Sclerosis (MS)
Degenerative
Acute
•Cerebral Palsy•Down Syndrome•Mental Retardation•Autism•Muscular Dystrophy
SOME INTERESTING FACTS8 out of 1000 people worldwide cannot use speech to communicate.
2‐3 million in U.S. could benefit from speech generating devices.
Only 5% of these people have a speech device.
Funding is available.
Source: Univ of NebraskaLincoln Website
WHAT BENEFITS DOES AAC PROVIDE TO YOUR PATIENTS?WHAT BENEFITS DOES AAC PROVIDE TO YOUR PATIENTS? Improves overall quality of life Supports meaningful personal relationships Develops functional communication skills
Improves Functional Communication Measures Reinforces traditional rehabilitation activities
Schedules (appointments and daily activities) Reminders (medication and appointments) Videos (physical therapy examples)
Helps patients communicate important medical and personal information to healthcare teams
FUNDING: SHOW ME THE MONEY
Medical Model Medicare Medicaid Private Insurance STAP Other Organizations
ALS VA
School IEP
Third Party Billing Other
Fund Raising
FUNDING: MEDICAL MODEL
Private Insurance Many insurers follow Medicare guidelines.
Call insurance company and ask questions about benefits. Confirm whether coverage available for Durable Medical Equipment/Speech Generating Devices.
Payment varies by policy. Ask if met deductible and Out of Pocket Maximum for
calendar year.
Any co-payments or deductibles need to be collected before device is shipped. Go through STAP for this!!
FUNDING: MEDICAL MODEL
Texas Medicaid Assistance 100%
Covers approved equipment with no out pocket cost to client
Does require 30-DAY trial period
Process takes about 2 months with trial
FUNDING: STAP
STAP stands for:
Specialized Telecommunications Assistance Program
Falls under umbrella of DARS Department of Assistive and Rehabilitative ServicesThis is a TAX that we pay for on our phone bills every month
FUNDING: STAP
Process
Fill out STAP application and provide small report. Application must be accompanied by proof of TX residency.
Everyone in Texas with a dual diagnosis qualifies for STAP.
FUNDING: STAP
With this funding there is no reason why anyone in Texas should be without a voice.
This is also a great alternative for schools! STAP timeline is about 4 weeks. Times do
fluctuate!! Follow up with STAP!!
RESOURCES 0-3 y.o. Early Childhood Intervention =/ >3 y.o. Child Find through School/School District or
youth’s school if already enrolled Non-Profit Therapy Organization Private Therapy Organization Consider:
Hours Location – home or center-based; family’s transportation Type Insurance Accepted If Youth-focused Waiting List Areas of Specialization
THANK-YOU DCMCCT speech therapists for sharing list!
REFERENCES
http://www.nidcd.nih.gov/health/voice/ National Institute on Deafness and Other Communication Disorders, National Institutes of Health
asha.org American Speech-Language-Hearing Association
Crossed Wires: Identification, Impact, Management and Outcomes of Language Disorders presentation by Lynn Wegner, MD at Texas Scottish Rite March 6, 2010
CODING 784.3 Aphasia 784.40 Voice and
resonance disorder, unspecified
784.42 Dysphonia 784.43 Hypernasality 784.44 Hyponasality 784.49 Other voice
and resonance disorders
784.59 Other speech disturbance,NOS
784.61 Alexia and dyslexia
783.42 Delayed Milestones
CODING 315.31 Expressive
language disorder 315.32 Mixed
expressive-receptive language disorder
315.34 Speech and language delay due to hearing loss
315.39 Other language disorder (phonologic, articulation)
315.5 Mixed developmental disorder
315.8 Other specified delays in development
315.9 Unspecified delays in development/ learning disorders NOS
Rapidly identify speech-language patterns related to second language acquisition to distinguish difference fromdisorder.
DIFFERENCE OR DISORDER: UNDERSTANDINGSPEECH AND LANGUAGE DEVELOPMENT INCULTURALLY AND LINGUISTICALLY DIVERSESTUDENTS