Magnetic Resonance Imaging and Troponin Elevation Following Percutaneous Coronary Intervention: New...
-
Upload
paul-schoenhagen -
Category
Documents
-
view
217 -
download
0
Transcript of Magnetic Resonance Imaging and Troponin Elevation Following Percutaneous Coronary Intervention: New...

E
MaFCNa
P
C
Sf2mdmbhembi“bd
dIcome
bicPh
dfaapss(o(e�iiAptegtF(ctaba
iavmCgpwiT4bat1Cmc
*at
IStSPAM
J A C C : C A R D I O V A S C U L A R I N T E R V E N T I O N S V O L . 3 , N O . 9 , 2 0 1 0
© 2 0 1 0 B Y T H E A M E R I C A N C O L L E G E O F C A R D I O L O G Y F O U N D A T I O N I S S N 1 9 3 6 - 8 7 9 8 / $ 3 6 . 0 0
P U B L I S H E D B Y E L S E V I E R I N C . D O I : 1 0 . 1 0 1 6 / j . j c i n . 2 0 1 0 . 0 6 . 0 1 1
DITORIAL VIEWPOINT
agnetic Resonance Imagingnd Troponin Elevationollowing Percutaneousoronary Intervention
ew Insights Into Myocyte Necrosisnd Scar Formation*
aul Schoenhagen, MD,† Harvey D. White, DSC‡
leveland, Ohio; and Auckland, New Zealand
erum biomarker evidence of myocyte necrosis is frequentlyound after percutaneous coronary intervention (PCI). About0% of patients develop elevated levels of creatine kinase-yocardial band (CK-MB) (1,2) and up to 48% of patients
evelop elevated troponin levels following PCI (2–9). Severalechanisms related to procedural complications such as side
ranch occlusion, dissection, and disruption of collateral flowave been proposed for these elevations. The concept of plaquembolization at the time of balloon inflation or stent deploy-ent leading to myocardial necrosis and scar formation has
een supported by observations with magnetic resonancemaging (MRI) and late gadolinium enhancement (LGE)scar” imaging after PCI (10). These data show an associationetween post-PCI elevations of troponin I with MRI-etectable scar formation.
See page 950
Following stenting, LGE may occur at the site of stenteployment and distally in the treated coronary artery (11).ntravascular ultrasound has shown a correlation betweenhanges in plaque volume before and after PCI and the massf distal hyperenhancement, but not with hyperenhance-ent at the site of stenting. Thus providing indirect
vidence that plaque embolization has occurred.
Editorials published in JACC: Cardiovascular Interventions reflect the views of theuthors and do not necessarily represent the views of JACC: Cardiovascular Interven-ions or the American College of Cardiology.
From the †Imaging Institute and Heart and Vascular Institute, Cardiovascularmaging, Cleveland Clinic, Cleveland, Ohio; and the ‡Green Lane Cardiovascularervice, Auckland City Hospital, Auckland, New Zealand. Dr. Schoenhagen reportshat he has no relationships to disclose. Dr. White has received research grants fromanofi-Aventis, Eli Lilly, The Medicines Company, National Institutes of Health,fizer, Roche, Johnson and Johnson, Schering-Plough, Merck Sharpe and Dohme,
estraZeneca, GlaxoSmithKline, Daiichi Sankyo Pharma Development, and Bristol-yers Squibb. He has also received a consultancy fee from Regado Biosciences.
Furthermore, post-PCI elevation of troponin I levels haveeen shown to be related to abnormal tissue perfusion (12)ndependent of the presence of thrombus, epicardial flow, orharacteristics of the coronary artery stenosis undergoingCI. Elevated biomarker levels are also associated withigher atheromatous plaque burden (13).The universal definition of myocardial infarction (MI)
esignates biomarker increase (with troponin preferred)rom a normal baseline to a level 3 times the 99th percentiles PCI-related MI (Type 4a) (14). The importance of thessociation between elevated biomarker levels after PCI andrognosis continues to be debated. Several studies havehown that the elevation of troponin levels after PCI istrongly associated with the composite of death and MI2,5). However, the associations have usually been with earlyutcomes (hospital or 90 days) and not with later follow-up4). A further important consideration is the level of thelevation with 1 study (6) showing that only troponin levels5 times the upper limit of normal were prognostically
mportant. In some studies (7), prognosis did not seem to benfluenced if baseline pre-PCI levels were not elevated (15).
recent meta-analysis (9) of 15 studies showed thatatients with normal baseline and any elevation of post-PCIroponin levels had increased risk of major adverse cardiacvents (death, MI, repeat PCI, and coronary artery bypassraft [CABG]) when compared with those patients withoutroponin elevation at an average follow-up of 17.7 months.or patients fulfilling the universal definition of type 4a MI
14), there was a further increased risk: odds ratio: 2.5 (95%onfidence interval 1.26 to 4.00). Patients with elevation ofroponin �3 times the upper limit of normal did not have
worse prognosis during follow-up. In general, serumiomarkers do not allow the characterization of localizationnd distribution of the underlying pathological process.
This limitation can be overcome by correlation withmaging modalities, as exemplified by the study of Locca etl. (16) in the current issue of JACC: Cardiovascular Inter-entions, which compared elevation of troponin I levelseasured by (Beckman Access 2 [Beckman Coulter, Brea,alifornia]) analyzer, which is clinically useful but not
uideline compliant (17) to MRI and LGE after PCI in 45atients. New LGE occurred in 33.3% of patients. The scarsere mostly small including �1.5% of left ventricular mass
n 14 of 15 patients and had no effect on ejection fraction.he site of the infarction was distal in 53% and proximal in7% of patients. Interestingly, post–stent dilation, probablyy causing more plaque embolization, was the only factorssociated with LGE. Elevation of biomarkers beyond 3imes the upper limit of normal occurred with CK-MB in1% of patients and with troponin I in 47% of patients.orrelation of LGE with elevation of biomarkers wasoderate, occurring in 40% of patients with elevation of
reatine kinase-myocardial band and 43% of patients with
levation of troponin I.
estwDismopsMp
Lpcr8vmmf0ems((iddiit
cmbim
dwewlesewms
icLsieyddieoaolrmfind
baeiHurhc
J A C C : C A R D I O V A S C U L A R I N T E R V E N T I O N S , V O L . 3 , N O . 9 , 2 0 1 0
S E P T E M B E R 2 0 1 0 : 9 5 9 – 6 2
Schoenhagen and White
Editorial Viewpoint
960
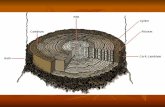
The underlying mechanism of MRI myocardial tissuenhancement with nonspecific extracellular contrast agentsuch as gadolinium is the increased distribution volume forhese molecules within the infarct region with delayedashout in comparison to the normal myocardium (18).elayed contrast-enhanced MRI is well validated in the
dentification of chronic myocardial scar (19,20). It hasufficient spatial resolution to differentiate patterns of trans-ural or subendocardial necrosis in the distribution of
bstructed vessels (20,21), and more diffuse, patchyatterns of necrosis related to distal embolization (22). Ineveral single-center trials, the prognostic impact of
RI-detected scar has been demonstrated in differentatient populations (23–25).It is important to consider issues related to scar size with
GE imaging. The minimal detectable scar volume de-ends on the spatial resolution of the MRI sequence. In theurrent study (16), similar to most other studies, spatialesolution was 1.4 � 1.7 mm in plane with slice thickness ofmm and a 2-mm gap. Therefore, the minimal resolvable
olume from a theoretical standpoint would be about 0.02l. However, practically, a bigger volume (a few times theinimal resolvable volume) is necessary to differentiate scar
rom noise. In the current study (16), the mean scar size was.83 g (about 40 times the minimal resolvable volume),quivalent to 0.53% of the size of the normal left ventricularyocardium. This is relatively small in comparison to other
tudies after intervention (2 g) (22), PCI and CABG (5 g)26), CABG (4.4 g) (27), and reperfused acute MI (20.6 g)28). The timing between myocardial injury and LGEmaging is important, because serial MRI studies performeduring the acute phase of MI have shown that the size ofelayed gadolinium enhancement may significantly change
mmediately after reperfusion, secondary to resolution ofnterstitial edema in reversibly injured myocardium withinhe peri-infarction zone (28–31).
Previous studies describe LGE imaging for the identifi-ation, characterization and quantification of periproceduralyocardial necrosis after PCI (22,26,30) and coronary
ypass surgery (CABG) (27). In these studies, the mass ofnfarcted tissue correlated with elevation of biochemical
arkers of myocardial damage (32). In contrast, the current
Table 1. Comparison of Troponins With MRI for Detecting Myocyte Necros
Contemporary Troponin Assays
Cutoff: normal vs. pathologic Well-defined
Sensitivity/spatial resolution Very sensitive, no localization
Time pattern of rise and fall Well known but limitations, e.g., delayed responsefrom nonreperfused myocardium
Method standardization High
Relation with prognosis Controversial (2,4,5–8,15)
Fulfills universal definition of MI Few
MI � myocardial infarction; MRI � magnetic resonance imaging.
ata by Locca et al. (16) demonstrate that in many patientsith elevated troponin I, LGE imaging could not identify
vidence of scar. The investigators raise the question as tohether current cutoff levels of biomarkers are too sensitive,
eading to overdiagnosis of post-PCI MI. An alternativexplanation in the context of uncomplicated PCI would bemall and patchy myocardial necrosis related to distalmbolization of plaque (11,22,33). False negative resultsith LGE imaging would be expected in patients withultiple small areas of necrosis, if individual scar area were
maller than the spatial limitation of the MRI sequence.Animal and post-mortem studies may provide further
nsights. However, more important will be clinical trialsomparing quantitative extent of biomarker elevation andGE scar with clinically meaningful outcome. Small studies
how an independent predictive value of delayed LGEmaging in patients undergoing coronary revascularization,ither PCI or CABG, during a median follow-up of 2.9ears (26). However, long-term outcome data from well-esigned, prospective, multicenter trials are lacking. In theesign of such trials, it will be critical to consider thenability of differentiating procedure-related versus pre-xisting infarction, therefore requiring pre- and post-perative MRI acquisitions. Strict standardization of imagecquisition and analysis, including contrast dose and thresh-ld definition for identification of scar is vital (34–36). Aimitation of MRI is the contraindication in patients witheduced kidney function (glomerular filtration rate �30l/min) because of concerns about nephrogenic systemic
brosis (37). Table 1 compares troponins, including theewer higher sensitivity troponins (38), with MRI foretecting myocyte necrosis. Much of the data are evolving.Future clinical trials, correlating clinical outcome with
oth biomarkers and comprehensive MRI imaging (LGEnd T2-weighted), characterizing scar and the at-risk areaarly after infarction, respectively (31,39,40), will providemportant further insight into periprocedural necrosis.
owever, even if such data will eventually be available, it isnrealistic to propose pre-and post-procedural LGE foroutine PCI. In the context of the current debate aboutealth care costs, it appears more realistic that such data willalibrate levels of biomarker elevation to corresponding scar
her Sensitivity Troponin Assays MRI
lving (38) Evolving
remely sensitive, no localization Localization, but limited spatial resolution
lving Decrease of scar area during the first week (28)
h Evolving
lving Evolving
No
is
Hig
Evo
Ext
Evo
Hig
Evo
Yes

mc
RGPZ
R
1
1
1
1
1
1
1
1
1
1
2
2
2
2
2
2
2
2
2
2
3
3
3
3
J A C C : C A R D I O V A S C U L A R I N T E R V E N T I O N S , V O L . 3 , N O . 9 , 2 0 1 0 Schoenhagen and White
S E P T E M B E R 2 0 1 0 : 9 5 9 – 6 2 Editorial Viewpoint
961
ass and distribution and help define clinical biomarkerriteria for defining post-PCI MI.
eprint requests and correspondence: Prof. Harvey D. White,reen Lane Cardiovascular Service, Auckland City Hospital,rivate Bag 92024, Victoria Street West, Auckland 1142, Newealand. E-mail: [email protected].
EFERENCES
1. Califf RM, Abdelmeguid AE, Kuntz RE, et al. Myonecrosis afterrevascularization procedures. J Am Coll Cardiol 1998;31:241–51.
2. Cantor WJ, Newby LK, Christenson RH, et al., on behalf ofSYMPHONY and 2nd SYMPHONY Cardiac Markers SubstudyInvestigators. Prognostic significance of elevated troponin I afterpercutaneous coronary intervention. J Am Coll Cardiol 2002;39:1738 – 44.
3. Adams JE 3rd, Sicard GA, Allen BT, et al. Diagnosis of perioperativemyocardial infarction with measurement of cardiac troponin I. N EnglJ Med 1994;330:670–4.
4. Cavallini C, Savonitto S, Violini R, et al., on behalf of Italian“Atherosclerosis, Thrombosis, and Vascular Biology” and “Society forInvasive Cardiology–GISE” Investigators. Impact of the elevation ofbiochemical markers of myocardial damage on long-term mortalityafter percutaneous coronary intervention: results of the CK-MB andPCI study. Eur Heart J 2005;26:1494–8.
5. Fuchs S, Kornowski R, Mehran R, et al. Prognostic value of cardiactroponin I levels following catheter-based coronary intervention. Am JCardiol 2000;85:1077–82.
6. Kizer JR, Muttrej MR, Matthai WH, et al. Role of cardiac troponin Tin the long-term risk stratification of patients undergoing percutaneouscoronary intervention. Eur Heart J 2003;24:1314–22.
7. Miller WL, Garratt KN, Burritt MF, Lennon RJ, Reeder GS, Jaffe AS.Baseline troponin level: key to understanding the importance ofpost-PCI troponin elevations. Eur Heart J 2006;27:1061–9.
8. Okmen E, Cam N, Sanli A, Unal S, Tartan Z, Vural M. Cardiactroponin I increase after successful percutaneous coronary angioplasty:predictors and long-term prognostic value. Angiology 2006;57:161–9.
9. Testa L, Van Gaal WJ, Biondi Zoccai GG, et al. Myocardialinfarction after percutaneous coronary intervention: a meta-analysisof troponin elevation applying the new universal definition. QJM2009;102:369 –78.
0. Selvanayagam JB, Porto I, Channon K, et al. Troponin elevation afterpercutaneous coronary intervention directly represents the extent ofirreversible myocardial injury: insights from cardiovascular magneticresonance imaging. Circulation 2005;111:1027–32.
1. Porto I, Selvanayagam JB, Van Gaal WJ, et al. Plaque volume andoccurrence and location of periprocedural myocardial necrosis afterpercutaneous coronary intervention: insights from delayed-enhancement magnetic resonance imaging, thrombolysis in myocardialinfarction myocardial perfusion grade analysis, and intravascular ultra-sound. Circulation 2006;114:662–9.
2. Bolognese L, Ducci K, Angioli P, et al. Elevations in troponin I afterpercutaneous coronary interventions are associated with abnormaltissue-level perfusion in high-risk patients with non-ST-segment-elevation acute coronary syndromes. Circulation 2004;110:1592–7.
3. Mehran R, Dangas G, Mintz GS, et al. Atherosclerotic plaque burdenand CK-MB enzyme elevation after coronary interventions: intravas-cular ultrasound study of 2,256 patients. Circulation 2000;101:604–10.
4. Thygesen K, Alpert JS, White HD, et al., on behalf of JointESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocar-dial Infarction. Universal definition of myocardial infarction. Circula-tion 2007;116:2634–53.
5. Prasad A, Gersh BJ, Bertrand ME, et al. Prognostic significance ofperiprocedural versus spontaneously occurring myocardial infarction
after percutaneous coronary intervention in patients with acute coro-nary syndromes: an analysis from the ACUITY (Acute Catheterization3
and Urgent Intervention Triage Strategy) trial. J Am Coll Cardiol2009;54:477–86.
6. Locca D, Bucciarelli-Ducci C, Ferrante G, et al. New universaldefinition of myocardial infarction following complex percutaneouscoronary interventions: a cardiovascular magnetic resonance study.J Am Coll Cardiol Intv 2010;3:950–8.
7. Apple FS, Pearce LA, Smith SW, Kaczmarek JM, Murakami MM.Role of monitoring changes in sensitive cardiac troponin I assay resultsfor early diagnosis of myocardial infarction and prediction of risk ofadverse events. Clin Chem 2009;55:930–7.
8. Judd RM, Lugo-Olivieri CH, Arai M, et al. Physiological basis ofmyocardial contrast enhancement in fast magnetic resonance images of2-day-old reperfused canine infarcts. Circulation 1995;92:1902–10.
9. Kim RJ, Fieno DS, Parrish TB, et al. Relationship of MRI delayedcontrast enhancement to irreversible injury, infarct age, and contractilefunction. Circulation 1999;100:1992–2002.
0. Wagner A, Mahrholdt H, Holly TA, et al. Contrast-enhanced MRIand routine single photon emission computed tomography (SPECT)perfusion imaging for detection of subendocardial myocardial infarcts:an imaging study. Lancet 2003;361:374–9.
1. Wu E, Judd RM, Vargas JD, Klocke FJ, Bonow RO, Kim RJ.Visualisation of presence, location, and transmural extent of healedQ-wave and non–Q-wave myocardial infarction. Lancet 2001;357:21–8.
2. Ricciardi MJ, Wu E, Davidson CJ, et al. Visualization of discretemicroinfarction after percutaneous coronary intervention associatedwith mild creatine kinase-MB elevation. Circulation 2001;103:2780–3.
3. Cheong BY, Muthupillai R, Wilson JM, et al. Prognostic significanceof delayed-enhancement magnetic resonance imaging: survival of 857patients with and without left ventricular dysfunction. Circulation2009;120:2069–76.
4. Kwon DH, Halley CM, Carrigan TP, et al. Extent of left ventric-ular scar predicts outcomes in ischemic cardiomyopathy patientswith significantly reduced systolic function: a delayed hyperen-hancement cardiac magnetic resonance study. J Am Coll CardiolImg 2009;2:34 – 44.
5. Kwong RY, Chan AK, Brown KA, et al. Impact of unrecognizedmyocardial scar detected by cardiac magnetic resonance imaging onevent-free survival in patients presenting with signs or symptoms ofcoronary artery disease. Circulation 2006;113:2733–43.
6. Rahimi K, Banning AP, Cheng AS, et al. Prognostic value of coronaryrevascularisation-related myocardial injury: a cardiac magnetic reso-nance imaging study. Heart 2009;95:1937–43.
7. Steuer J, Bjerner T, Duvernoy O, et al. Visualisation and quantificationof peri-operative myocardial infarction after coronary artery bypasssurgery with contrast-enhanced magnetic resonance imaging. EurHeart J 2004;25:1293–9.
8. Ibrahim T, Hackl T, Nekolla SG, et al. Acute myocardial infarction:serial cardiac MR imaging shows a decrease in delayed enhancement ofthe myocardium during the 1st week after reperfusion. Radiology2010;254:88–97.
9. van Dijkman PR, van der Wall EE, de Roos A, et al. Acute, subacute,and chronic myocardial infarction: quantitative analysis of gadolinium-enhanced MR images. Radiology 1991;180:147–51.
0. Baks T, van Geuns RJ, Biagini E, et al. Effects of primary angioplastyfor acute myocardial infarction on early and late infarct size and leftventricular wall characteristics. J Am Coll Cardiol 2006;47:40–4.
1. Yan AT, Shayne AJ, Brown KA, et al. Characterization of theperi-infarct zone by contrast-enhanced cardiac magnetic resonanceimaging is a powerful predictor of post-myocardial infarction mortality.Circulation 2006;114:32–9.
2. Ingkanisorn WP, Rhoads KL, Aletras AH, Kellman P, Arai AE.Gadolinium delayed enhancement cardiovascular magnetic resonancecorrelates with clinical measures of myocardial infarction. J Am CollCardiol 2004;43:2253–9.
3. Prati F, Pawlowski T, Gil R, et al. Stenting of culprit lesions inunstable angina leads to a marked reduction in plaque burden: a majorrole of plaque embolization? A serial intravascular ultrasound study.Circulation 2003;107:2320–5.
4. Amado LC, Gerber BL, Gupta SN, et al. Accurate and objectiveinfarct sizing by contrast-enhanced magnetic resonance imaging in a

3
3
3
3
3
4
Kei
J A C C : C A R D I O V A S C U L A R I N T E R V E N T I O N S , V O L . 3 , N O . 9 , 2 0 1 0
S E P T E M B E R 2 0 1 0 : 9 5 9 – 6 2
Schoenhagen and White
Editorial Viewpoint
962
canine myocardial infarction model. J Am Coll Cardiol 2004;44:2383–9.
5. Schuijf JD, Kaandorp TA, Lamb HJ, et al. Quantification of myocar-dial infarct size and transmurality by contrast-enhanced magneticresonance imaging in men. Am J Cardiol 2004;94:284–8.
6. Setser RM, Bexell DG, O’Donnell TP, et al. Quantitative assessmentof myocardial scar in delayed enhancement magnetic resonance imag-ing. J Magn Reson Imaging 2003;18:434–41.
7. Leiner T, Kucharczyk W. NSF prevention in clinical practice: sum-mary of recommendations and guidelines in the United States, Canada,and Europe. J Magn Reson Imaging 2009;30:1357–63.
8. White HD. Higher sensitivity troponin levels in the community: Whatdo they mean and how will the diagnosis of myocardial infarction bemade? Am Heart J 2010;159:933–6.
9. Aletras AH, Tilak GS, Natanzon A, et al. Retrospective determination
of the area at risk for reperfused acute myocardial infarction with iT2-weighted cardiac magnetic resonance imaging: histopathologicaland displacement encoding with stimulated echoes (DENSE)functional validations. Circulation 2006;113:1865–70.
0. Friedrich MG, Abdel-Aty H, Taylor A, Schulz-Menger J, MessroghliD, Dietz R. The salvaged area at risk in reperfused acute myocardialinfarction as visualized by cardiovascular magnetic resonance. J AmColl Cardiol 2008;51:1581–7.
ey Words: coronary artery bypass graft � late gadoliniumnhancement � magnetic resonance imaging � myocardialnfarction � myocyte necrosis � percutaneous coronary
ntervention � scar � serum biomarker � troponin.