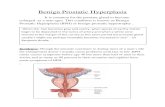
Lumenis Holmium Solutions for Benign Prostatic Hyperplasia ...
Transcript of Lumenis Holmium Solutions for Benign Prostatic Hyperplasia ...
PB-2007973 Rev D
Lumenis Holmium Solutions for Benign Prostatic Hyperplasia (BPH) Bibliography of Published Studies & Peer-Reviewed Papers
The use of Holmium Laser for surgical procedures in Benign Prostate Hyperplasia is clinically based in MOSES innovative technology, versatility for different cases, improved and durable outcomes, feasibility of same-day and catheter free discharge, shorter procedure time, and low complication rate of the procedure. The following list presents selected publications of the last 15 years, pointing out the advantages of using Lumenis high-power Holmium Laser in the surgical treatment of Benign Prostate Hyperplasia in Urology.
1
PB-2007973 Rev D 2
Peer-reviewed publications of using Holmium Laser for Benign Prostatic Hyperplasia (BPH)
Benefits of MOSES™ Technology for HoLEP.....................................................................................3
HoLEP as Gold Standard Treatment................................................................................................4
Benefits of HoLEP in Comparison to Various Technologies.....................................................6
Benefits of HoLEP as a Same-day Procedure..................................................................................8
The Learning Curve of HoLEP..........................................................................................................10
Benefits of Morcellation......................................................................................................................12
Vaporization Techniques Used with Holmium Laser (HoLVP)................................................13
Table of Contents
PB- 2007973 Rev D 2
PB-2007973 Rev D 3
Holmium Laser Enucleation of the Prostate Using Moses 2.0 vs Non-Moses. A Randomized Controlled Trial.
Comparative Study of Holmium Laser Enucleation of the Prostate with MOSES Enabled Pulsed Laser Modulation.
Catheter Removal on the Same Day of Holmium Laser Enucleation of the Prostate: Outcomes of a Pilot Study.
BJU Int. 2020 Oct 7
Urology. 136:196-201.
Urology. 2020 Oct 9;S0090-4295(20)31242-5.
Nevo A, Faraj KS, Cheney SM, Moore JP, Stern KL, Borofsky M, Gnessin E, Humphreys MR.
Large T, Nottingham C, Stoughton C, Williams J Jr, Krambeck AE.
Agarwal DK, Rivera ME, Nottingham CU, Large T, Krambeck AE.
2020
2020
2020
TITLE PUBLICATION AUTHORS YEAR
• Comparison of MOSES 2.0 for Holmium Enucleation of the Prostate (HoLEP) with standard HoLEP in 27 patients and surgeons' evaluation of MOSES 2.0 technology with respect to incision sharpness, fiber control, tissue separation, tissue damage, hemostasis, visibility, and charring.
• When operated by expert surgeon, MOSES 2.0 resulted in shorter enucleation time (21 vs 36.7 min, P = 0.016) and higher enucleation efficiency (1.75 vs 1.05 g/min, P = 0.05). When operated by trainees, MOSES 2.0 resulted in shorter hemostasis time (4.1 vs 9 min, P = 0.035). Additionally, Moses 2.0 had less fiber degradation (3.5 vs 16.8 mm, P < 0.01).
• With higher objective and subjective evaluation scores Moses 2.0 is favored over non-MOSES technology. It allows a smoother, operator-friendly procedure, which may increase the accessibility of HoLEP for surgeons training for HoLEP.
• Comparison of MOSES 2.0 for HoLEP with standard HoLEP in 150 cases using 3 different fiber types.
• MOSES laser enucleation was associated with a 3.9-minutes decrease in time to achieve hemostasis compared with Slimline 550 mm HoLEP (P < 0.001). Patients treated with MOSES presented signifcantly less hemoglobin loss. 91% of patients in the MOSES group were discharged home in less than 24 hours without a catheter.
• Using modulated pulse laser energy (MOSES) for HoLEP is safe, effective, and less affected by increases in prostate gland size. With 15% faster enucleation time and 40% faster hemostasis time, MOSES Technology can potentially help the novice surgeon overcome the learning curve by improving vision clarity.
• Assessment of the feasibility of same day catheter removal after holmium laser enucleation of the prostate (HoLEP) in 30 patients.
• 27 (90%) patients successfully voided on the same day without requiring catheter replacement. All patients were catheter free by Post-op Day 1. For patients who successfully passed their voiding trial, the median times from the end of the procedure to hospital discharge and to catheter removal were 2.6 and 4.9 hours, respectively.
• Same day catheter removal with MOSES 2.0 is a feasible and safe option in a select population of patients undergoing HoLEP making the procedure truly minimally invasive with the potential for transforming the management of BPH, especially in larger glands.
STUDY AIM, RESULTS, & CONCLUSIONS
Lumenis Pulse 120H Moses 2.0
Lumenis Pulse 120H Moses 2.0
Lumenis Pulse 120H Moses 2.0
LASER SYSTEM
Benefits of MOSES™ Technology for HoLEP
PB-2007973 Rev D 4
18 Years of Holmium Laser Enucleation of the Prostate: A Single Center Experience.
Holmium Laser Enucleation of the Prostate (HoLEP): A Review and Update.
HoLEP: The Gold Standard for the Surgical Management of BPH in the 21st Century.
J Urol. 202(4):795-800.
Can J Urol. 26(4 Suppl 1): 13-19.
Am J Clin Exp Urol. 25;3(1):36-42.
Ibrahim A, Alharbi M, Elhilali MM, Aubé M, Carrier S
Das AK, Teplitsky S, Humphreys MR
Michalak J, Tzou D, Funk J.
2019
2019
2015
TITLE PUBLICATION AUTHORS YEAR
• Evaluation of long-term outcomes following Holmium Laser Enucleation of the Prostate (HoLEP) for benign prostatic hyperplasia (BPH) with a median follow-up of 9.1 years of 1476 patients.
• Mean catheter time and hospital stay were 1.2 and 1.3 days, respectively. Functional outcomes, including International Prostate Symptom Score (IPSS), Quality of Life (QoL), Peak flow rate (Qmax), and Post-void Residual (PVR) urine, signifcantly improved in all patients that could be folllowed for more than 10 years (P < 0.001 each); from this cohort only 21 patients (1.4%) required re-treatment.
• Long-term follow-up experience shows that HoLEP is a safe, effective and durable procedure to treat BPH.
• Review of outcomes, safety, and long-term durability of techniques utlized for treating Lower Urinary Tract Symptoms (LUTS) due to BPH.
• HoLEP has a robust body of literature demonstrating its superiority to other techniques like Transurethral Resection of the Prostate (TURP) and Open Prostectomy (OP).
• HoLEP has proven to be an extremely effective and durable treatment recommended by guidelines of global urology associations as a size-independent treatment for patients with moderate to severe LUTS. HoLEP is an excellent option for patients whom may not be good candidates for other procedures due to age, prostate size, or risk of bleeding.
• Review of literature comparing HoLEP to other traditional and alternative laser therapies for BPH including TURP, OP, Photoselective Vaporizarion of the Prostate (PVP), and Thulium Laser Enuceation of the Prostate (ThuLEP).
• HoLEP achieves greater improvements in functional outcomes (IPSS and Qmax) and lower rates of repeat endoscopic procedures at 5-10 year follow-up compared with other therapies (<1% vs. 7.4% and 5.6% for TURP and PVP, respectively). Furthermore, HoLEP results in fewer serious intra- and post-operative complications.
• Numerous large, RCTs demonstrate HoLEP's superiority to other surgical therapies for BPH, in particular HoLEP should be the gold standard therapy in men with large prostates whom are candidates for TURP or OP.
STUDY AIM, RESULTS, & CONCLUSIONS
Lumenis Pulse 100H or 120H
Lumenis Pulse 100H or 120H
Not applicable
LASER SYSTEM
HoLEP as Gold Standard Treatment
PB-2007973 Rev D 5
Holmium Laser Enucleation of the Prostate: Long-term Durability of Clinical Outcomes and Complication Rates During 10 Years of Followup.
Holmium Laser Enucleation of the Prostate--Outcomes Independent of Prostate Size?
Efficacy of Holmium Laser Enucleation of the Prostate in Patients with a Small Prostate (≤30 mL).
Holmium Laser Enucleation of the Prostate: Results at 6 Years.
J Urol. 186(5):1972-6.
J Urol. 180(6):2431-5
World J Mens Health ;35(3):163-169.
Eur Urol. 53(4):744-749.
Elmansy HM, Kotb A, Elhilali MM.
Humphreys MR, Miller NL, Handa SE, Terry C, Munch LC, Lingeman JE.
Park S, Kwon T, Park S, Moon KH
Gilling PJ, Aho TF, Frampton CM, King CJ, Fraundorfer MR.
2011
2008
2017
2008
TITLE PUBLICATION AUTHORS YEAR
• Assessment of HoLEP long-term durability in 949 patients with up to 10-year follow-up.
• Reoperation rate due to residual adenoma was 0.7% over a 10-year period. Postoperative mean PVR volume, mean Qmax, mean IPSS and QoL were 52 ml, 23.4 ml per second, 3.8, and 0.7 at 10 years, respectively.
• HoLEP represents an effective treatment for BPH with low comlication rate and is durable in the long-term.
• Examination of HoLEP outcomes based on prostate size in 507 pts stratified into 3 groups by prostare weight (<75 g, 75-125- g, >125 g).
• Hospitalization, catheterization, preoperative and postoperative outcomes were similar among the groups. Postoperative urinary function was similar among all pts after HoLEP independent of prostate size.
• HoLEP is a safe and effective treatment adavantageous to treat all prostates regardless of size with favorable and equivalent outcomes.
• Comparison of the effects of HoLEP on a small prostate in 132 patients who failed medical treatment. Patients were stratfied into 2 groups based on prostate size — group 1: ≤30 mL (n=30) and group 2: >30 mL (n=102).
• Regardless of prostate size, IPSS, QoL, and PVR significantly decreased and peak urinary flow significantly increased 3 months after surgery. The voiding subscore also significantly decreased 3 months after surgery (P< 0.001).
• When other medical treatments are ineffective, HoLEP is an effective intervention for patients with a small prostate.
• Assessment of satisfaction level and durability of HoLEP of 71 patients in a 6-year follow-up.
• Of the 38 patients that answered the survey 35 (92%) were either satisfied or extremely satisfied with their outcome.
• HoLEP is a durable procedure with high rate of satisfied patients in a long-term follow-up.
STUDY AIM, RESULTS, & CONCLUSIONS
Lumenis Pulse 100H
Lumenis system 80W or 100W
Lumenis Pulse 100H
Lumenis Pulse 100H
LASER SYSTEM
HoLEP as Gold Standard Treatment Modality
PB-2007973 Rev D 6
Superiority of HoLEP over TURP in a Matched-pair Analysis of Bleeding Complications under Various Antithrombotic Regimens.
Holmium Laser Enucleation of the Prostate Versus Bipolar Resection of the Prostate: A Prospective Randomized Study. "Pros and Cons".
Randomised Trial of Bipolar Resection vs Holmium Laser Enucleation vs Greenlight Laser Vapo-enucleation of the Prostate for Treatment of Large Benign Prostate Obstruction: 3-years Outcomes.
J Endourol. 2020 Sep 17.
Urology, 86(5):1037-41.
BJU Int. 2020 Jul 6.
Westhofen T, Schott M, Keller P, Tamalunas A, Stief C, Magistro G.
Fayad AS, Elsheikh MG, Zakaria T, Elfottoh HA, Alsergany R, Elshenoufy A, Elghamarawy H.
Elshal AM, Soltan M, El-Tabey NA, Laymon M, Nabeeh A.
2020
2015
2020
TITLE PUBLICATION AUTHORS YEAR
• Comparison of Holmium Enucleation of the Prostate (HoLEP) with TURP in 221 patients under continuous antithrombotic (AT) therapy in regard to bleeding complications.
• Compared with TURP, HoLEP resulted in a significantly higher percentage of resected tissue (median 71.43% vs 45.45%, P < 0.001) with a significantly lower drop in perioperative haemoglobin levels (median 0.7 vs 2.20 g/dl, P < 0.001) for all subgroups of AT regimens. Also, adverse events were significantly less frequent after HoLEP (5.4% vs 16.4%, P < 0.05).
• HoLEP is an efficient and safe procedure for patients under diverse continuous antithrombotic regimens. It provides a superior perioperative hemostatic control and causes less bleeding complications in this high-risk population.
• Comparison of safety, efficacy, and applicability of HoLEP and Transurethral Resection of the Prostate (TURP) in a 12-month follow-up of 120 patients with Benign Prostatic Hyperplasia (BPH).
• At Month 12 the International Prostate Symptom Score (IPSS) and peak urinary flow (Qmax) were significantly improved in the HoLEP group compared with TURP. While operative time was longer in the HoLEP group, a larger proprtion of HoLEP treated patients had their catheter removed within 24 hours and hemoglobin loss was more significant in the TURP group.
• HoLEP has proven to be effective in treating large prostates with minimal morbidity, better hemostasis, less blood loss, and better voiding pattern than TURP after a 12-month follow-up.
• Comaprison of HoLEP with Transurethral Resection in Saline (TURis) and Greenlight Laser Vapo-Enucleation of the Prostate (GL-PVEP) for treating large sized prostates (80-150 ml) in 182 procedures in 3 groups with 3-years follow-up.
• HoLEP resulted in significantly shorter opearative time (73 ± 30, 92 ± 32, 83 ± 28 min, compared with TURis and TURP, P = 0.005) and higher operative efficiency (1.7 ± 0.7, 1.2 ± 0.4, 1.4 ± 0.6 g/min, P < 0.001). Also, HoLEP resulted in significantly lower re-treatment rate (0%, 9.7%, 6.7%, P = 0.04).
• HoLEP was superior or just as good as TURis and GL-PVEP for treatment of large sized prostate achieving siginificantly better 3-years retreatment rate compared with both techniques.
STUDY AIM, RESULTS, & CONCLUSIONS
Lumenis Pulse 100H
Lumenis Pulse 100H
Lumenis Pulse 100H
LASER SYSTEM
Benefits of HoLEP in Comparison to Various Technologies
PB-2007973 Rev D 7
Long-term Outcomes of Laser Prostatectomy for Storage Symptoms: Comparison of Serial 5-Year Follow-up Data Between 120 W High Performance System Photoselective Vaporization of the Prostate and Holmium Laser Enucleation of the Prostate.
Post-operative Lower Urinary Tract Storage Symptoms: Does Prostate Enucleation Differ from Prostate Vaporization for Treatment of Symptomatic. Benign Prostatic Hyperplasia?
J Urol. 199(6):1591-1599.
J Endourol. 29(10):1159-65.
Cho MC, Song WH, Park J, Cho SY, Jeong H, Oh SJ, Paick JS, Son H.
Elkoushy MA, Elshal AM, Elhilali MM.
2018
2015
TITLE PUBLICATION AUTHORS YEAR
• 60-month follow-up comparison in 266 patients of storage symptom outcomes between HoLEP and Photoselective Vaporizarion of the Prostate (PVP) in 2 groups.
• HoLEP appeared to show a superior degree of improvement in voiding symptoms, QoL, peak urine flow rate, Prostate Serum Antigen (PSA) reduction, and re-treatment rate. While there was no difference in operative time, HoLEP used significanlty less laser energy.
• Follow-up data suggest that improvement in storage symptoms is maintained throughout the long-term postoperative period, with a better improvement in voiding symptoms and quality of life after HoLEP procedure.
• Assessment of post-operative storage symptoms following HoLEP and the PVP with up to 12 months follow-up in 1100 procedures.
• The HoLEP group postoperative IPSS was significantly better than in the PVP group at all follow-up points (P < 0.05), with storage symptoms not improving in the PVP group untill Month 6 postoperatively. Proportion of pts with moderate or severe storage symptoms was signifcantly higher in the PVP group at 1- and 3-months follow-up (P < 0.001 and P = 0.004, respectively).
• Storage urinary symptoms relief is immediate and significantly improved after HoLEP compared to PVP; patients undergoing Green Light PVP may have to wait at least for 3 months postoperatively to have their storage symptoms relieved.
STUDY AIM, RESULTS, & CONCLUSIONS
N/A
Lumenis Pulse 100H
LASER SYSTEM
Benefits of HoLEP in Comparison to Various Technologies
PB-2007973 Rev D 8
Evolution of Day-case HoLEP Success Rate Over Time.
Holmium Laser Enucleation of the Prostate is Safe and Feasible as a Same Day Surgery.
Feasibility of Holmium Laser Enucleation of the Prostate as a 1-day Surgery.
J Endourol. 2020 Sep 16.
Urology. 138:119-124.
World J Urol. 38(4):1017-1025.
Klein C, Marquette T, Comat V, Alezra E, Capon G, Bladou F, Ferriere JM, Bensadoun H, Bernhard JC, Robert G.
Lwin AA, Zeng J, Evans P, Phung MC, Hynes KA5 Price ET, Twiss CO, Tzou DT, Funk JT.
Abdul-Muhsin H, Critchlow W, Navaratnam A, Gnecco J, Tay K, Girardo M, Andrews P, Cheney S, Humphreys M.
2020
2020
2019
TITLE PUBLICATION AUTHORS YEAR
• Examination of the evolution of HoLEP success rate as a same-day surgery (SDS) over a 6-year period (2013-2019) in 266 patients and identfication of predictive factors for prolonged hospitalization or readmissions.
• The overall success rate was 80.5% (214/266) significantly improving over time (P = 0.014) with a significant decrease in operating time (P < 0.001) and total energy delivered (P = 0.041). Risk factors for SDS failure were prostate volume (P = 0.030), particularly if over 90 mL (P < 0.01) and prolonged operative time (P = 0.039).
• SDS HoLEP is a reliable and safe procedure with a high success rate improving over time. The surgeon's experience seems to be crucial in improving perioperative outcomes, but prostate volume over 90 mL remains associated with higher failure rates.
• Assessment of the feasibility and safety of HoLEP as a same-day surgery (SDS HoLEP) in 377 patietns compared with regular admission time.
• SDS rate was 52% (199/377); length of stay was significantly shorter in the SDS group compared to the non-SDS group (3.9 ± 1.8 vs. 30.5 ± 15.8 hr, P < 0.01). There was no difference in complication rate, readmission rate, and long term fucntional outcomes; while the SDS group had a significant shorter operative time and reduced catheterization time (P < 0.05 each).
• Same-day outpatient surgery for HoLEP is both safe and feasible and should be considered regardless of prostate size, comorbidities, age, or anticoagulation status.
• Assessment of the safety and feasibility of HoLEP as a same-day surgery in 179 patients.
• Of the 47 patients suitable for same-day surgery 28 (59.5%) patients were successfully discharged on the same day. Most common cause for admission was degree of hematuria without continuous bladder irrigation. Post-operative time in recovery unit was 339.7±105 min for same-day discharged patients versus 269.6 ± 58 min for admitted pateints (P = 0.0004).
• HoLEP has proven successful as a same-day procedure with good safety profile in selected patients.
STUDY AIM, RESULTS, & CONCLUSIONS
Lumenis Pulse 100H
Lumenis Pulse 120H
Lumenis Pulse 120H
LASER SYSTEM
Benefits of HoLEP as a Same-day Procedure
PB-2007973 Rev D 9
Day-case Holmium Laser Enucleation of the Prostate: Feasibility, Safety and Predictive Factors.
Day-Case Holmium Laser Enucleation of the Prostate: Prospective Evaluation of 90 Consecutive Cases.
Ann R Coll Surg Engl. 100(6):475-479.
J Endourol 31(10):1056-1061.
Lee SM, Gordon K, McMillan R, Crystal F, Acher P.
Comat V, Marquette T, Sutter W, Bernhard JC, Pasticier G, Capon G, Bensadoun H, Ferrière JM, Robert G.
2018
2017
TITLE PUBLICATION AUTHORS YEAR
• Assessment of the feasibility and safety of day-case HoLEP and predictive factors for increased length of hospital stay in 210 patients.
• 74 (35.3%) patients were discharged as true day-cases and a further 84 (40.0%) were discharged within 24 hours. Readmission rate was 5.5%, with all complications Clavien– Dindo grade I or II.
• Same-day HoLEP is both feasible and safe, with low readmission rates.
• Assessment of the feasibility and safety of same-day HoLEP and predictive factors for prolonged hospitalization in 90 procedures with a 3-months follow up.
• Same-day surgery rate was 43.5% (90/211 consecuteive patients); 16.7% of patients (15/90) required prolonoged hospitalization mainly due to gross hematuria. Same-day surgery success rate was over 80.0%; overall complication rate was 36.7%.
• Same-day HoLEP has proven successful regardless of prostate volume, and may be performed by a trained surgeon with an appropriate patient selection.
STUDY AIM, RESULTS, & CONCLUSIONS
N/A
Lumenis Pulse 100H and 120H
LASER SYSTEM
Benefits of HoLEP as a Same-day Procedure
PB-2007973 Rev D 10
Does Surgeon Experience Affect Operative Time, Adverse Events and Continence Outcomes in Holmium Laser Enucleation of the Prostate? A Review of More Than 1,000 Cases.
Learning Curves and Perioperative Outcomes after Endoscopic Enucleation of the Prostate: A Comparison Between GreenLight 532-nm and Holmium Lasers.
Multicentre Prospectie Evaluation of the Learning Curve of Holmium Laser Enucleation of the Prostate (HoLEP).
J Urol 198(3):663-670
World J Urol 35(6):973-983.
BJU Int 117(3):495-9.
Shigemura K, Yamamichi F, Kitagawa K, Yamashita M, Oka Y, Tanaka H, Fujisawa M
Peyronnet B, Robert G, Comat V, Rouprêt M, Gomez-Sancha F, Cornu JN5, Misrai V.
Robert G, Cornu JN, Fourmarier M, Saussine C, Descazeaud A, Azzouzi AR, Vicaut E, Lukacs B.
2017
2017
2016
TITLE PUBLICATION AUTHORS YEAR
• The effects of HoLEP learning curve on surgical outcomes of more than 1000 patients in a Multi-Center review.
• Operative and enucleation times and incidence of urinary incontinence (UI) improved with surgeon's experience (P < 0.05 each); significant improvements were obsereved after 20 cases. Surgeon's experience did not affect surgery-related complications and urination-related outcomes.
• Surgical experience contributes to shorter operation and enucleation times and post-HoLEP UI, but does not affect morcellation time, prostate volume, resected prostate weight, complication rate, and urinary-related outcomes.
• Comparison of HoLEP and GreenLight Enucleation of the Prostate (GreenLEP) for learning curve, perioperative and early functional outcomes in a 6-month follow-up of 100 consecutive patients in each group.
• Operative time reached a plateau after about 30 procedures in both groups. Length of catheterization time and hospital stay were significantly shorter in the HoLEP group (P < 0.0001), while opeative time was shorter with GreenLEP. A greater decrease in International Prostate Symptom Score (IPSS) and Post-void Residual (PVR) urine test was observed with HoLEP at a 6-month time.
• Learning curves of GreenLEP and HoLEP procedures were similar, with a shorter hospital stay and improved post-operative scores noted in the HoLEP group.
• Analysis of the HoLEP learning curve as measured by 4 consecutive successful procedures out of 20 consecutive procedures with procedure time under 90 min.
• 43.6% of cases were reported as successful by the study criteria. Primary reason for unsuccessful procedures was operative time >90 min followed by conversion to TURP. 8 centers were included in the study analysis, 4 of 5 centers successfully competed the learning curve, while 3 other centers resigned mid-study due to un-acceptable complications.
• HoLEP has a steep learning curve, exceeding 20 cases. Operating time and total enucleation efficacy seem the most important difficulties for a beginner. A more intensely mentored and structured mentorship programme might allow for a better adoption of this procedure.
STUDY AIM, RESULTS, & CONCLUSIONS
Lumenis Pulse 100H
Lumenis Pulse 100H
Lumenis Pulse 100H
LASER SYSTEM
The Learning Curve of HoLEP
PB-2007973 Rev D 11
Evaluation of the Learning Curve for Holmium Laser Enucleation of the Prostate Using Multiple Outcome Measures.
Enucleation Ratio Efficacy Might be a Better Predictor to Assess Learning Curve of Holmium Laser Enucleation of the Prostate.
Holmium Laser Enucleation of the Prostate: The Safety, Efficacy, and Learning Experience in China.
Urology 86(4): 824-9.
Int Braz J Urol 38(3):362-71.
J Endourol 22(5):1031-6.
Brunckhorst O, Ahmed K, Nehikhare O, Marra G, Challacombe B, Popert R.
Jeong CW, Oh JK, Cho MC, Bae JB, Oh SJ.
Du C, Jin X, Bai F, Qiu Y.
2015
2012
2008
TITLE PUBLICATION AUTHORS YEAR
• Assessment of the surgical learning curve of HoLEP in over 253 consecutive patients.
• Enucleation ratio efficiency was significantly different between cohorts of 20 pts (P = 0.02) reaching a plateau after 50-60 cases. Complication rate decreased through the caseload but did not show a statistical difference (P = 0.62) or plateauing.
• Learning curve for HoLEP is 40-60 cases depending on outcome used to measure competence. Adjuncts to training such as simulation-based training may be of use for the new surgeon in shortening the initial phase of learning.
• Evaluation of the learning curve of surgeons during Holmium Enucleation of the Prostate (HoLEP) for Benign Prostatic Hypeplasia (BPH) in 6-month follow-up of 140 patients.
• Increasing enucleation efficiency correlated with prostate size (P < 0.001) in the first 50 cases. Mean enucleation and morcellation times were 49.9 ± 23.8 min and 11.0 ± 9.7 min, respectively. Surgery-related complication rate was 19.3%, all complications were mild and transient.
• The learning curve for a novice surgeon performing HoLEP is about 25 cases, even without mentorship.
• Assessment of HoLEP efficacy and safety with learning curve progression in 3 groups of 190 consecutive patients during a 12-month follow-up.
• Procedure time and complication rate decreased significantly after 50 procedures. The surgeon became more confident with HoLEP after about 15 cases in moderate-sized prostates.
• HoLEP is a safe and effective treatment option for BPH, even when performed by inexperienced surgeons, with a decrease in procedure time and complication rate during the learning curve.
STUDY AIM, RESULTS, & CONCLUSIONS
N/A
Lumenis Pulse 100H
Lumenis Pulse 100H
LASER SYSTEM
The Learning Curve of HoLEP
PB-2007973 Rev D 12
DrillCut™ vs VersaCut™ Prostate Tissue Morcellation Devices after Holmium Laser Enucleation: A Prospective, Randomized Controlled Trial.
Wolf Piranha Versus Lumenis VersaCut Prostate Morcellation Devices: A Prospective Randomized Trial.
Ex-Vivo Comparison of Available Morcellation Devices During Holmium Laser Enucleation of the Prostate Through Objective Parameters.
An Improved Morcellation Procedure for Holmium Laser Enucleation of the Prostate.
Can Urol Assoc J. 13(8):266-270.
J Urol, 195(2):413-7.
J Endourol 28(10):1237-40.
J Endourol, 26(12):1625-8.
Ibrahim A, Elhilali MM, Elkoushy MA, Andonian S, Carrier S.
El Tayeb MM, Borofsky MS, Paonessa JE, Lingeman JE.
Cornu JN, Terrasa JB, Lukacs B.
Chen Q, Chen YB, Wang Z, Peng YB, Zheng DC, Cai ZK, Li WJ, Zhou J
2018
2016
2014
2012
TITLE PUBLICATION AUTHORS YEAR
• Comparing safety, efficacy and cost-effectiveness of the Lumenis VersaCut™ morcellator and DrillCut™ morcellator (Karl Storz) during Holmium Enucleation of the Prostate (HoLEP) in 82 patients ranodmized into 2 groups.
• The VersaCut was significantly more efficient in morcellation ( 4.9% vs. 3.6% g/min, P = 0.03). There was no significant difference in terms of complication rates (7.3 vs. 2.4%, P = 0.1). The cost of disposable instruments of the VersaCut was also lower compared to the DrillCut (247.5 vs. 160.9 CAD $, P < 0.01).
• The Lumenis VersaCut Morcellator was associated with significantly higher morcellation efficiency and lower cost of disposables when compared with the DrillCut morcellator.
• Comparing Wolf Piranha™ and Lumenis VersaCut™ prostate morcellation devices for patients with Benign Prostatic Hyperplasia (BPH) undergoing HoLEP in 74 patients in two groups.
• Cost analysis favored the VersaCut significantly, despite the fact that the Piranha achieved a slightly non significant higher morcellation rate at 5.6 gm per minute compared to the VersaCut at 4.8 gm per minute.
• Morcellation rates for the two devices are comparable, with the Piranha having a statistically significant increased cost, more complicated design and less user-friendly.
• In-vitro evaluation of two morcellators (Lumenis VersaCut and Wolf Piranha) and two nephroscopes during HoLEP.
• For the Wolf and Lumenis morcellators, aspiration power parameters were 20.4 mL/s and 22.2 mL/s, and morcellating power parameters were 2.5 g and 6 g of tissue per minute, respectively.
• The Lumenis morcellator is faster than the Wolf morcellator.
• Assessment of modification of the conventional morcellation procedure for HoLEP at 395 patients in two groups.
• Morcellation rate improved with the new modification, with no difference in complications.
• The improved VersaCut morcellation procedure can be used in various situations of suction and can be performed in a more fluent manner and with better efficacy.
STUDY AIM, RESULTS, & CONCLUSIONS
Lumenis VersaCut
Lumenis VersaCut
Lumenis VersaCut
Lumenis VersaCut
LASER SYSTEM
Benefits of Morcellation
PB-2007973 Rev D 13
Initial Experience with New High Powered 120W Holmium for Vaporization of the Prostate.
Holmium Laser for the Surgical Treatment of Benign Prostatic Hyperplasia.
Photoselective Laser Ablation of the Prostate: A Review of the Current 2015 Tissue Ablation Options.
Holmium Laser Ablation of the Prostate (HoLAP): Intermediate-term Results of 144 Patients.
Urol Nephrol Open Access J 4(2):00119.
Can J Urol ,23(4):8356-62.
Can J Urol, 22 Suppl 1:45-52.
World J Urol. 31(5):1253-9.
Beaghler M, Leo M, Gass J, March J, Sandoval S, Wonnaparhown A.
Thurmond P, Bose S, Lerner LB.
Tholomier C, Valdivieso R, Hueber PA, Zorn KC.
Barski D, Richter M, Winter C, Arsov C, de Geeter P, Rabenalt R, Albers P.
2017
2016
2015
2013
TITLE PUBLICATION AUTHORS YEAR
• Examination of using a high-powered Holmium laser system for vaporization of prostate (HolVAP) in 100 patients with Benign Prsotatic Hyperplasia (BPH).
• Post-operatively, the American Urology Association (AUA) score, Post-void Residual (PVR) urine test, and Peak Flow rate (Qmax) improved significantly (9.4 versus 24.1, 33 versus 175, and 15.3 versus 8.2, respectively). Intraoperative visualization and surgeon satisfaction were excellent. Patients required no hospital admission unless other comorbidities were present.
• Experience with HolVAP using 120 W Holmium laser system has demonstrated significant improvements in both subjective and objective parameters. The increase in overall power and advancements in the laser fiber technology provide greater hemostasis and a shorter operative time.
• Comparing the outcomes of HolVAP with HoLEP in 198 patients in two groups.
• Patients in the HolVAP group had a significantly shorter operative time (77 versus 119 minutes). No significant differences were found in flow rate outcomes between groups.
• Both HoLEP and HolVAP are appropriate surgical procedures for the management of BPH. When performed correctly, HolVAP technique produces similar results to HoLEP, and may present a shorter operative time.
• Review the physics and the basics behind laser prostatectomies, as well as to present the most current literature on vaporization procedure.
• HoLVAP is an alternative to Transurethral Resection of Prostate (TURP) for small to medium-sized prostates, and recommended in severely anti-coagulated patients.
• Laser vaporization using Holmium laser is a safe and effective alternative to TURP in the treatment of BPH for carefully selected patients.
• Analyse the intermediate-term outcome of HolVAP of up to 4 years postoperatively in 144 patients with BPH.
• IPSS, Quality of Life (QOL), Qmax, and PVR significantly improved after 3 months (P < 0.0001 each). Re-operation rate was lower in patients with prostate volume <40 ml.
• HolVAP is a safe and effective procedure for the treatment of prostates <40 ml. Patients benefit from HoLVAP because of a low bleeding rate and short hospital stay.
STUDY AIM, RESULTS, & CONCLUSIONS
Lumenis Pulse 120H
N/A
Lumenis Pulse 120H
Lumenis Pulse 100H
LASER SYSTEM
Vaporization Techniques Used with Holmium Laser (HoLVP)
PB-2007973 Rev D 14
Risk information: use of the Lumenis Holmium laser systems, accessories, their delivery devices and Lumenis morcellator in urology is contraindicated for patients who are unable to receive endoscopic treatments or are intolerant to prolonged anesthesia, as well as for resection or excision of large vascularized organs. Lumenis Holmium laser systems and accessories are solely intended for use by physicians trained in the use of the Ho:YAG (2.1 μm) wavelength. Incorrect treatment settings can cause serious tissue damage. The laser should be used only on tissues that are fully observable. See the system user manual for a complete list of contraindications and risks. The use of the Lumenis VersaCut morcellator and accessories is contraindicated for morcellation of bone and for use in liposuction procedures, Gynecologic surgery in which the tissue to be morcellated is known or suspected to contain malignancy and removal of uterine tissue containing suspected fibroids in patients who are peri- or post-menopausal, or candidates for en bloc tissue removal, for example, through the vagina or via a mini-laparotomy incision. Lumenis VersaCut is intended solely for use by physicians trained in the use of the VersaCut morcellator. The Lumenis VersaCut and accessories should only be used under direct or endoscopic visualization in a fluid environment. See the system user manual for a complete list of contraindications and risks.
Lumenis Inc.
San Jose, CA, USAT +1 408 764 3000 +1 877 586 3647F +1 408 764 3999
EMEA
Dreieich Dreieichenhain, GermanyT +49 6103 8335 0 F +49 6103 8335 300
Roma (RM), ItalyT +39 06 90 75 230 F +39 06 90 75 269
Hertfordshire, UKT +44 20 8736 4110 F +44 20 8736 4119
ASIA / PACIFIC
Beijing, ChinaT +86 10 5737 6677
Gurgaon, IndiaT +91 124 422 07 95
Kowloon, Hong KongT +852 217 428 00 F +852 272 251 51
JAPAN
Tokyo, JapanT +81 3 4431 8300F +81 3 4431 8301
Lumenis Ltd.
Yokneam Industrial Park6 Hakidma Street P.O.B. 240Yokneam 2069204, IsraelT +972-4-959-9000
Lumenis (Germany) GmbH
Heinrich-Hertz-Str 3 D-63303Dreieich-Dreieichenhain GERMANYT +49 0 6103 8335 0
www.lumenis.com/Surgical PB- 2007973 Rev D© 2020 Lumenis Ltd., All Rights Reserved