Leber's plus: patientswith neuropathy
Transcript of Leber's plus: patientswith neuropathy

10ournal ofNeurology, Neurosurgery, and Psychiaty 1995;59:160-164
Leber's "plus": neurological abnormalities inpatients with Leber's hereditary optic neuropathy
E K Nikoskelainen, R J Marttila, K Huoponen, V Juvonen, T Lamminen, P Sonninen,M-L Savontaus
AbstractPrevious studies suggest that Leber'shereditary optic neuropathy (LHON)may be a systemic disorder with manifes-tations in organs other than the opticnerves. To evaluate nervous systeminvolvement 38 men and eight womenwith LHON were re-examined. Thepatients were divided into three groupsaccording to mtDNA analysis-namely,patients with the 11778 or with the 3460mutation and patients without these pri-mary mutations. Fifty nine per cent ofpatients had neurological abnormalitiesbut there was no significant differencebetween the three groups. Movement dis-orders were the most common finding;nine patients had constant posturaltremor, one chronic motor tic disorder,and one parkinsonism with dystonia.Four patients had peripheral neuropathywith no other evident cause. Two patientshad a multiple sclerosis-like syndrome;in both patients MRI showed changes inthe periventricular white matter.Thoracic kyphosis occurred in sevenpatients, five ofwhom had the 3460 muta-tion. In one patient the 3460 mutation wasassociated with involvement of the brainstem. It is suggested that various move-ment disorders, multiple sclerosis-likeillness, and deformities of the vertebralcolumn may associate pathogeneticallywith LHON.
(3 Neurol Neurosurg Psychiatry 1995;59: 160-164)
Keywords: mitochondrial DNA; Leber hereditaryoptic neuropathy
Leber's hereditary optic neuropathy (LHON)is an optic nerve disease that causes blindnessand is associated with maternally inheritedmitochondrial DNA (mtDNA) mutations.Half of the families with LHON have a pointmutation at the nucleotide 11778 in the sub-unit 4 and 15% at the nucleotide position3460 in the subunit 1 of complex 1.1 2 Severalother mutations have also been postulated tobe pathogenic to LHON.-5 There are clini-cally confirmed LHON families with yetundiscovered mtDNA mutation(s).The disease is characterised by acute or
subacute bilateral visual loss usually in youngmen. The acute stage of the disease is recog-nised by typical fundus findings, peripapillarymicroangiopathy, and a swollen retinal nerve
fibre layer. Peripapillary microangiopathyfades from view when optic atrophy develops.The fundus findings in the acute stage can beminimal and easily overlooked. Some authorsconsider that acute LHON can exist withoutany signs of peripapillary microangiopathy.6
Clinical studies suggest that LHON is asystem disorder associated occasionally withneurological, cardiac, and skeletal changes.67Newman, in a recent review, used the termLeber's "plus" to describe patients with theclinical features ofLHON in addition to othersevere neurological or systemic abnormalities.Multiple sclerosis-like illness, spinal cord dis-ease, brain stem and basal ganglia involve-ment, and Charcot-Marie-Tooth disease, aswell as skeletal changes have been consideredto be such abnormalities.8-'7 The purpose ofthis study was to assess the frequency andtype of neurological dysfunctions occurring inFinnish patients with LHON.
Patients and methodsForty six patients with LHON (38 men, eightwomen) from 24 families with the diseasewere neurologically re-examined. The oph-thalmological abnormalities in relation to vari-ous mtDNA mutations are reportedelsewhere.'8 The patients were divided intothree groups according to mtDNA analysis,performed as reported previously.' Therewere 27 patients with the 11778 mutation andnine with the 3460 mutation. The third("other") group comprised 10 patients with-out these primary mutations. This group hadfive patients who did not harbour any of theprimary mutations; however, two brothershad the 12811 and the 13967 mutations inthe ND5 subunit and two brothers the 4732and the 13637 mutation in the subunits ND2and ND5 respectively, and in one patient nocomplex I mutation was detected. All thepatients with unknown mutation had a typicalacute stage of LHON. The patients received afull neurological assessment supplementedwith a review of their previous medicalrecords. Ancillary neuroradiological examina-tions were performed on nine patients.
ResultsTwenty seven patients (59%) had neuro-logical abnormalities in addition to LHON;15 had the 11778 mutation, six had the 3460mutation, and six were from the third group.The single most common abnormality was apostural and action tremor of the hands
Department ofOphthalmologyE K NikoskelainenDepartment ofNeurologyR J MarttilaDepartment ofRadiologyP SonninenDepartment ofMedical Genetics,University ofTurku,Turku, FinlandV JuvonenT LamminenM-L Savontaus
Department ofGenetics andMolecular Medicine,Emory UniversitySchool ofMedicine,Atlanta, USAK HuoponenCorrespondence to:Dr Eeva Nikoskelainen,Department ofOphthalmology, Universityof Turku (TYKS),SF-20520 Turku, Finland.Received 8 November 1994and in revised form23 January 1995Accepted 30 March 1995
160 on N
ovember 22, 2021 by guest. P
rotected by copyright.http://jnnp.bm
j.com/
J Neurol N
eurosurg Psychiatry: first published as 10.1136/jnnp.59.2.160 on 1 A
ugust 1995. Dow
nloaded from

Leber's "plus": neurological abnormalities in patients with Leber's hereditary optic neuropathy
Neurological and skeletal abnormalities
11778 3460 Other Total(n=27) (n 9) (n=10) (n 46)
Migraine 1 3 - 4Epilepsy 1 1 1 3Dementia 1 - - 1Polyneuropathy 8 - 1 9Tremor 5 4 5 14Parkinsonism and dystonia - 1 - 1Chronic motor tic 1 - - 1Multiple sclerosis-like disorder 1 - 1 2Brain stem involvement - 1 - 1Thoracic kyphosis 2 5 - 7Pes cavus - 1 - 1
(table). It occurred in 14 patients belonging toall three mutation groups. In five patients thetremor occurred occasionally in situationsknown to exaggerate physiological tremor,such as muscle fatigue, anxiety, or after exces-
sive alcohol intake. Nine patients had con-
stant hand tremor with an amplitude notlarger than 5 mm for several years; in twocases there was an additional head tremor.Five of these patients had a family history of a
similar tremor. Four patients had severalmaternal relatives with tremor and one malepatient had a daughter with a similar tremor.
Altogether nine patients had clinical evi-dence of a peripheral neuropathy. All thesepatients except one had the 11778 mutation.The patients had sensory complaints in thefeet with decreased or absent ankle jerk anddiminished light touch and vibration sense. Intwo more severely affected patients, nerve
conduction velocities were only slightlydecreased suggesting a predominantly axonalneuropathy. In five patients, alcohol was possi-bly the cause or a contributing factor to neu-
ropathy whereas in the remaining fourpatients no evident cause was found. Migraineoccurred in four patients; none had aura.
Seizures were experienced by three patients.In two of them, the convulsions had occurredduring alcohol withdrawal, and one had com-
plex partial seizures of temporal lobe origin.One woman with the 11778 mutation devel-oped bilateral optic neuropathy at the age of59. The course of her LHON has beendescribed in detail elsewhere.'9 When exam-ined two years later because of gait difficulty,she was profoundly demented and had a mod-erately severe peripheral neuropathy. A heavyuse of alcohol remained as the most probablecause of her neurological ailment. One malepatient had chronic motor tic disorder.
Skeletal abnormalities were noted in seven
patients. In all cases kyphosis or kyphoscoliosisoccurred in the thoracic region. In twopatients with the 11778 mutation, the defor-mity was only of moderate degree whereas inthe other five patients with the 3460 mutation(two from one family and three from another)the kyphosis was pronounced. The case histo-ries of four patients are described in detail.
PATIENT 1
Patient 1 has an extrapyramidal syndromeand carries the 3460 mutation. His LHONwas diagnosed in 1985 when he was 29 years
old. He developed parkinsonism at the age of34. The first symptoms were dragging andtremor of the left leg. Tremor soon appearedin the left hand. When examined two yearsafter the onset, he was hypomimic, had arather severe rest tremor in his left leg andhand with nuchal and left sided rigidity. BrainCT and MRI were normal. He was treatedwith combined levodopa, bromocriptine, andselegiline with a beneficial response initially.One year later he developed serious nuchaldyskinesia with the head turning to the leftand backwards and closely resembling cervicaldystonia. All medications were gradually with-drawn with no improvement of the dyskinesia.Even after a 12 month drug free period thepatient had cervical dystonia in conjunctionwith left sided rest tremor and rigidity.Levodopa treatment was reinstituted withrelief of rigidity and tremor but no change indystonic head movements. Injections of botu-linum toxin A into cervical muscles initiallyrelieved the dystonia but the efficacy was lostafter two treatments. A repeated MRI of thebrain was normal.
PATIENT 2Patient 2 is a woman with the 11778 muta-tion. She was born in 1938 and has a multiplesclerosis-like illness. At the age of 24 shedeveloped temporary double vision. Twoyears later she experienced acute left opticneuropathy associated with hyperaemia anddisc swelling. The visual acuity in this eyedeteriorated during three weeks to permanentfinger counting vision. Three years later theright eye was similarly involved. During theacute stage there was hyperaemia and swellingin the disc and definite peripapillary microan-giopathy. This eye also became blind duringthe subsequent weeks. Simultaneously shedeveloped difficulties with her balance. Herlegs became stiff and her gait was impaired.Neurological examination showed a spasticparaparesis. She was diagnosed as havingmultiple sclerosis. When aged 49, she was re-evaluated. The visual acuity in her right eyewas finger counting at 1 m and in the left eye,hand movements. She had no near vision.The pupils reacted slightly sluggishly to light.Biomicroscopy was normal and intraocularpressure 13 bilaterally. Both visual fields hada large, absolute centrocecal scotoma.Ophthalmoscopy showed severe disc pallorand retinal nerve fibre loss. She has beenexamined neurologically several times and hercondition has steadily deteriorated.Treatment with intravenous methylpred-nisolone has been of no objective benefit. Atthe last neurological examination she wasconfined to a wheelchair. There was a mildweakness in the right arm together with anintention tremor with a final amplitude ofsome millimetres. Her legs were weak andspastic. Both arm and leg reflexes wereincreased with extensor plantar responses.Vibration sense was diminished up to the iliaccrest. She had urgency of micturition andoccasional incontinence. Her CSF contained3 lymphocytes/mm3; there were oligoclonal
161 on N
ovember 22, 2021 by guest. P
rotected by copyright.http://jnnp.bm
j.com/
J Neurol N
eurosurg Psychiatry: first published as 10.1136/jnnp.59.2.160 on 1 A
ugust 1995. Dow
nloaded from

Nikoskelainen, Marttila, Huoponen, Juvonen, Lamminen, Sonninen, Savontaus
Figure 1 T2 weightedbrain MRI showing whitematter changes and smallputaminal necrotic areas.
bands and increased IgG content. Brain MRIdisclosed white matter and putaminal lesionswith increased T2 signal (fig 1).
PATIENT 3
Patient 3 is a man with the 12811 and the13967 mutations at ND 5. He was born in1937 and has a multiple sclerosis-like illness.At the age of 18 his left eye was affected andthree months later his right eye was alsoinvolved. According to his medical chart bothfundi showed neurovascular changes in theacute stage suggestive of LHON. During sub-sequent years he noticed increasing weaknessand stiffness in his legs. In neurological exam-
ination he was found to have a mild spasticparaparesis. An air myelogram was normal.His CSF was otherwise normal, but a goldcolloidal curve was interpreted as slightlyabnormal. Paraparesis steadily worsened andat the age of 50 years he was confined to a
wheelchair. Ten years later the visual acuitieswere finger counting at 1-2 metres. He had
no near vision. Pupils were 7 mm with normallight reactions. Ophthalmoscopy showedsevere disc pallor and retinal nerve fibre lossbilaterally. When examined neurologically atthe age of 55 he was able to walk only a fewmetres with support. Cranial nerve functionsexcept optic nerve involvement were normal.The reflexes were increased in his arms andthere was bilateral slight intention tremor. Hislegs were weak and spastic; reflexes wereincreased with ankle clonus and bilateralextensor plantar responses. There was a sen-sory deficit for light touch and vibration up tothe 10th thoracic dermatome. He had urinaryincontinence and failure to achieve erection.Brain MRI showed periventricular smalllesions with increased T2 signal; additionally,there were widened sulci in the temporalregion bilaterally. Cervical MRI disclosed aspinal stenosis at the level of the 5th to 7thcervical vertebrae. A cervical laminectomy atC5 to C7 was performed without any relief ofparaplegia. His brother also developed typicalLHON with peripapillary microangiopathyprogressing to permanent blindness. Thebrother has postural tremor but a neurologicalexamination was otherwise uninformative.There are no other affected family members.
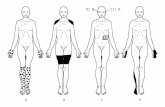
PATIENT 4Patient 4 is a man with the 3460 mutation.He was born in 1946 and has eye movementdisturbance and kyphosis. At the age of 32years he experienced an acute LHON whichdeteriorated rapidly to severe permanentblindness. In 1994 the visual acuity in theright eye was perception of light and in the lefteye, hand movements only. The pupilsreacted somewhat sluggishly to light.Biomicroscopy and intraocular pressures wereuninformative. The optic discs were totallypale and the peripapillary arterioles narrow.There was no visible nerve fibre layer. Hisvisual fields could not be assessed because ofsevere blindness. The left eye was exotropic.The adduction was restricted bilaterally, morein the left eye. He could not converge his eyes.The vertical eye movements were alsorestricted, more upwards than downwards.There was no optokinetic response. He hadincreased reflexes, but the plantar responseswere flexor. The vibration sense was absent atthe ankles. There was no ataxia. He had pescavus and pronounced kyphosis in the tho-racic spine (fig 2). Brain MRI disclosed aslight pontine and cerebellar atrophy, addi-tionally there were widened sulci in the frontaland occipital cortices. No changes in whitematter were seen.
DiscussionLeber20 described minor neurological symp-toms and signs in his patients with LHON.Other authors have reported headaches, emo-tional instability, reflex abnormalities,polyneuropathy, seizures, mental retardation,and other non-specific neurological signs intheir patients.2'22 In the present study fourpatients with migraine and one patient with
162 on N
ovember 22, 2021 by guest. P
rotected by copyright.http://jnnp.bm
j.com/
J Neurol N
eurosurg Psychiatry: first published as 10.1136/jnnp.59.2.160 on 1 A
ugust 1995. Dow
nloaded from

Leber's "plus": neurological abnormalities in patients with Leber's hereditary optic neuropathy
Figure 2 Radiograph ofthoracic spine showing athoracic kyphosis. Thevertebrae show anteriorbody and plate irregularity,disc space narrowing, andsmall Schmorl's nodes(Scheuermann changes).
epilepsy belong to this category. The combi-nation of alcoholism and LHON was rela-tively common as also reported by others.2324Tremor in association with LHON has
been reported by several authors." 17 2629 Inour families tremor was seen in all three sub-groups. The clinical nature of the constanttremor in nine patients was identical to thefeatures of essential tremor. Essential tremoris known to be inherited dominantly in an
autosome; the location of the gene, however,is not known. The pathogenesis of essentialtremor is unknown and no pathologicalchanges have been found in the brain.30 In a
population based epidemiological study theprevalence of essential tremor was 5-5% in a
Finnish population aged over 40.31 Tremoroccurred in 20% (nine of 46) of our patientswith LHON, four of them having maternalrelatives with similar tremor. This may sug-
gest a more specific connection of tremor withLHON. We have not studied the paternal off-spring and thus cannot exclude the possibilityof simultaneous autosomally inherited essen-
tial tremor in these families.One of our patients with the 3460 mutation
had parkinsonism and cervical dystonia. Asimilar case has been reported by Larsson etal."1 They described a patient with the 11778mutation who developed unilateral tremorand rigidity one year after optic nerve involve-ment at the age of 36. Brain MRI showedsharply defined lesions bilaterally in the puta-mina. This type of striatal putaminal necrosiswith prominent dystonic symptoms coseggre-
gating with LHON pedigrees has been
reported by several authors.8 15212932-35Interestingly, Jun et al recently showed thatthe family with LHON and dystonia originallyreported by Novotny et al'5 had a mtDNAmutation at nucleotide pair 14459 of theNADH dehydrogenase subunit 6 gene.36 Thedisorder usually but not necessarily appearsduring childhood.81532 It is noteworthy thatpatients in Leber's "plus" families maydevelop only the movement disorder, whichsuggests that the phenotypes of Leber's "plus"families may vary.
Early medical literature and more recentpapers9 12 16 37-39 have suggested that a multiplesclerosis-like illness may accompany LHON.Harding et a19 showed widespread white matterlesions in five neurologically affected femalepatients and in two female patients withLHON only. All these patients had the 11778mutation. The authors suggested that thistype of neurological disorder occurs only inwomen and that mitochondrial genes maycontribute to the susceptibility to multiplesclerosis. We found multiple sclerosis-like ill-ness in one female and one male patient.These patients with progressing spastic para-paresis closely resemble the cases described inthe medical literature; both of them alsoshowing scattered white matter lesions. Thefemale patient carried the 11778 mutation,and the male patient had the 12811 and the13967 mutation of ND5 indicating that mul-tiple sclerosis like disorder is not restricted towomen or to the 11778 mutation.
In the present study the association of neu-ropathy with LHON still remains only sugges-tive. Johns et al reported that the 15257mutation has a high incidence of spinal cordand peripheral neurological symptoms.'0 Inthe present study we had seven patients from afamily with the 15257 mutation. Two of thesepatients had mild polyneuropathy but in otherpatients the neurological examination wasuninformative. All these patients simultane-ously harboured the 11778 mutation and thusthe relevance of the 15257 mutation in thepathogenesis ofLHON cannot be evaluated.Two patients with a multiple sclerosis-like
syndrome reported by Harding et al hadinternuclear ophthalmoplegia.9 Paulus et alrecently described a patient with the 11778mutation who developed brain stem involve-ment with Parinaud's syndrome and ocu-lopalatal myoclonus.25 In this case MRIshowed a high signal area in the brain stemcorresponding to a hypodense area on CT.Apparently the brain stem may be involved inLHON, at least subclinically. This hypothesisis supported by Mondelli et al who reportedanomalous brain stem auditory evoked poten-tials in seven of their 11 patients withLHON.40 Our patient with restrictions in eyemovement may represent brain stem involve-ment of LHON.
Vertebral column deformities were com-mon in the present study. Seven patients hadthoracic kyphosis, one also with pes cavus.There are previous descriptions of kyphoscol-iosis, arachnodactyly, spondyloepiphysealdysplasia, and short stature associated with
163 on N
ovember 22, 2021 by guest. P
rotected by copyright.http://jnnp.bm
j.com/
J Neurol N
eurosurg Psychiatry: first published as 10.1136/jnnp.59.2.160 on 1 A
ugust 1995. Dow
nloaded from

Nikoskelainen, Marttila, Huoponen, _Juvonen, Lamminen, Sonninen, Savontaus
LHON.26 2932 Kyphosis has also been noted inthe families with LHON that exhibit spasticdystonia syndrome.29 In the present study thehigh incidence of kyphosis in two non-relatedfamilies with the 3460 mutations suggests thatit could represent one phenotypic feature ofthe 3460 mutation. We have, however, not
studied the paternal relatives in these familiesand thus the autosomal inheritance of kyphosiscannot be excluded.
Peripapillary microangiopathy is one of themain findings in LHON. Bruyn et al suggest
that endothelial swelling of the lenticulostri-atal vessels could produce anoxia or ischaemiaand explain the symmetric or even strictly uni-lateral putaminal lesions seen in the spasticdystonia syndrome.8 Also the white matterlesions detected in multiple sclerosis-like dis-ease could be caused by microangiopathy.Abnormal, enlarged mitochondria with com-
plicated cristae in the pericytes of capillaries,endothelial cells, and smooth muscle cells ofthe small arteries in mitochondrial myopathy,encephalopathy, lactic acidosis, and strokelike episodes (MELAS), one of the mitochon-driopathies, has been reported by severalauthors suggesting that abnormalities in smallarteries might be responsible for the strokelike episodes of the disease.41-43 We suggest
that in the enigmatic aetiopathogenesis ofLHON progressive microangiopathy may alsobe an important factor in neurological mani-festations, and warrants fuirther exploration.
This study has been financially supported by grants fromPaulo Foundation, Sigrid Juselius Foundation,The FinnishAcademy, and the NIH(I-RO EY 409040-01).
1 Huoponen K, Lamminen T, Juvonen V, Aula P,Nikoskelainen E, Savontaus M-L. The spectrum ofmitochondrial DNA mutations in families withLeberhereditary optic neuroretinopathy. Hum Genet 1993;92:379-84.
2 Howell N, Kubacka J, Halvorsson S, Mackey D. Leber'shereditary optic neuropathy: the etiological role of a
mutation in the mitochondrial cytochrome b gene.
Genetics 1993;133:133-6.3 Johns DR, NeufeldMJ. Cytochrome b mutations in Leber
hereditary optic neuropathy. Biochem Biophys ResCommun 1991;181:1358-64.
4 Johns DR, NeufeldMJ, Park RD. An ND-6 mitochondrialDNA mutation associated with Leber hereditary opticneuropathy. Biochem Biophys Res Commun 1992;187:1551-7.
5 Mackey D, Howell N. A variant of Leber hereditary opticneuropathy characterized by recovery of vision and by an
unusual mitochondrial genetic etiology. Am.7 HumGenet 1992;51:1218-28.
6 Newman NJ. Leber's hereditary optic neuropathy. Newgenetic considerations. Arch Neurol 1993;50:540-8.
7 Nikoskelainen EK, Savontaus M-L, Wanne OP, KatilaMJ, Nummelin KU. Leber's hereditary optic neuro-retinopathy, a maternally inherited disease. A genealogicstudy in four pedigrees. Arch Ophthalmol 1987;105:665-71.
8 Bruyn GW, Vielvoye GJ, Went LN. Hereditary spasticdystonia: a new mitochondrial encephalopathy?Putaminal necrosis as a diagnostic sign. .7 Neurol Sci1991;103:195-202.
9 Harding AE, Sweeney MG, Miller DH, et al. Occurrenceof a multiple sclerosis-like illness in women who have a
Leber's hereditary optic neuropathy mitochondrial DNAmutation. Brain 1992;115:979--89.-
10 Johns DR, Smith KH, Savino PJ, Miller NR. Leber'shereditary optic neuropathy. Clinical manifestations ofthe 15257 mutation. Ophthalmology 1993;100:981-6.
11 Larsson N-G, Andersen 0, Holme E, Oldfors A,Wahlstrom J. Leber's hereditary optic neuropathy andcomplex I deficiency in muscle. Ann Neural 1991;30:701-8.
12 Lees F, MacDonald A-ME, Turner JWA. Leber's diseasewith symptoms resembling disseminated sclerosis..7 Neurol Neurosurg Psychiatry 1964;27:415-21.
13 McCluskey DAJ, O'Connor PS, Sheehy JT. Leber's opticneuropathy and Charcot-Marie-Tooth disease. Reportof a case. . Clin Neuroophthalmol 1986;6:76-8 1.
14 McLeod JG, Low PA, Morgan JA. Charcot-Marie-Toothdisease with Leber optic atrophy. Neurology 1978;28:179-84.
15 Novotny EJ, Singh G, Wallace DC, et al. Leber's diseaseand dystonia: a mitochondrial disease. Neurology1986;36: 1053-60.
16 Went LN. Leber disease and variants. Handbook of ClinicalNeurology 1972;13:94-1 10.
17 Wilson J. Leber's hereditary optic atrophy. Some clinicaland aetiological considerations. Brain 1963;86:347-62.
18 Nikoskelainen E, Huoponen K, Juvonen V, Lamminen T,Nummelin K, Savontaus ML. Ophthalmological find-ings in Leber hereditary optic neuropathy with specialreference to the int DNA mutations. Ophthalmology1995 (submitted).
19 Nikoskelainen E, Nummelin K, Savontaus M-L. Doessporadic Leber's disease exist? _7 Clin Neuroophthalmol1988;8:225-9.
20 Leber T. Ueber hereditare und congenitalangelegteSehnervenleiden. Graefes Archives of Clinical andExperimental Ophthalmology 1871;2:249-9 1.
21 de Weerdt CJ, Went LN. Neurological studies in familieswith Leber's optic atrophy. Neurologica Scandinavica197 1;47:541-54.
22 Newman NJ, Lott MT, Wallace DC.The clinical charac-teristics of pedigrees of Leber's hereditary optic neu-ropathy with the 11778 mutation. Am . Ophthalmol199 1;111:750-62.
23 Johns DR, Smith KH, Miller NR. Leber's hereditary opticneuropathy. Clinical manifestations of the 3460 muta-tion. Arch Ophthalmol 1992;110:1577-81.
24 Cullom ME, Heher KL, Miller NR, Savino PJ, Johns DR.Leber's hereditary optic neuropathy masquerading astobacco-alcohol amblyopia. Arch Ophthalmol 1993; 111:1482-5.
25 Paulus W, Straube A, Bauer W, Harding AE. Central ner-vous system involvement in Leber's optic neuropathy.J7Neurol 1993;240:251-3.
26 Bereday M, Cobb S. Relation of hereditary optic atrophy(Leber) to other familial degenerative diseases of centralnervous system. AMA Archives of Ophthalmology 1952;48:669-80.
27 Heinonen 0. Beobachtungen bei der LeberschenKrankheit. Acta Ophthalmol 1932;10:20 1- 1.
28 Howell N, Kubacka I, Xu M, McCullough DA. Leberhereditary optic neuropathy: involvement of the mito-chondrial ND 1 Gene and evidence for an intragenicsuppressor mutation. Am _7 Hum Genet 1991;48:935-42.
29 Wallace DC. A new manifestation of Leber's disease and anew explanation for the agency responsible for itsunusual pattern of inheritance. Brain 1970;93:121-32.
30 Rajput AH, Rozdilsky B, Ang L, Rajput A.Clinicopathologic observations in essential tremor:report of six cases. Neurology 1991;41:1422-4.
31 Rautakorpi I, Takala J, Marttila R, Sievers K, Rinne UK.Essential tremor in a Finnish population. Acta NeurolScand 1982;66:58-67.
32 Bruyn GW, Went LN. A sex-linked heredodegenerativeneurological disorder associated with Leber's opticatrophy. . Neurol Sci 1964;1:59-80.
33 Marsden CD, Lang AE, Quinn NP, McDonald WI,Abdallat A, Nimri S. Familial dystonia and visual failurewith striatal CT lucencies. _7 Neurol Neurosurg Psychiatry1986;49:500-9.
34 Leuzzi V, Bertini E, De Negri AM, Gallucci M, GaravagliaB. Bilateral striatal necrosis, dystonia and optic atrophyin two siblings. _7 Neurol Neurosurg Psychiatry 1992;55:16-9.
35 Mackey DA. Three subgroups of patients with Leberhereditary optic neuropathy from the UK. Eye 1995 (inpress).
36 Jun AS, Brown MD, Wallace DC. A mitochondrial DNAmutation at nucleotide pair 14459 of the NADH dehy-drogenase subunit 6 gene associated with maternallyinherited Leber hereditary optic neuropathy and dysto-nia. Proc NatlAcadSci USA 1994;91:6206-10.
37 Nikoskelainen E, Sogg RL, Rosenthal AR, Friberg TR,DorfmanUJ. The early phase in Leber's hereditary opticatrophy. Arch Ophthalmol 1977;1 :565-8.
38 Palan A, Stehouwer A, Went LN. Studies on Leber's opticneuropathy III. Doc Ophthalmol 1989;71:77-87.
39 Flanigan KM, Johns DR. Association of the 11778 mito-chondrial DNA mutation and demyelinating disease.Neurology 1993;43:2720-2.
40 Mondelli M, Rossi A, Scarpini C, Dotti MT, Federico A.BAEP changes in Leber's hereditary optic atrophy: fur-ther confirmation of multisystem involvement. ActaNeurol Scand 1990;81:349-53.
41 Sakuta R, Nonaka I. Vascular involvement in mitochon-drial myopathy. Ann Neurol 1989;25:594-601.
42 Ohama E, Ohara 5, Ikuta F, Tanaka K, Nishizawa M,Miyatake T. Mitochondrial angiopathy in cerebral bloodvessels of mitochondrial encephalomyopathy. ActaNeuropathol (Berl) 1987;74:226-33.
43 Hirano M, Ricci E, Koenigsberger MR, et al. MELAS:an original case and clinical criteria for diagnosis.Neuromuscul Disord 1992;2:125-35.
164 on N
ovember 22, 2021 by guest. P
rotected by copyright.http://jnnp.bm
j.com/
J Neurol N
eurosurg Psychiatry: first published as 10.1136/jnnp.59.2.160 on 1 A
ugust 1995. Dow
nloaded from