Lasmiditan for the treatment of migraine...migraine is characterized by headache occurrence at least...
Transcript of Lasmiditan for the treatment of migraine...migraine is characterized by headache occurrence at least...

Full Terms & Conditions of access and use can be found athttp://www.tandfonline.com/action/journalInformation?journalCode=ieid20
Download by: [Universita Studi la Sapienza] Date: 24 January 2017, At: 00:36
Expert Opinion on Investigational Drugs
ISSN: 1354-3784 (Print) 1744-7658 (Online) Journal homepage: http://www.tandfonline.com/loi/ieid20
Lasmiditan for the treatment of migraine
Matilde Capi, Fernando de Andrés, Luana Lionetto, Giovanna Gentile,Fabiola Cipolla, Andrea Negro, Marina Borro, Paolo Martelletti & MartinaCurto
To cite this article: Matilde Capi, Fernando de Andrés, Luana Lionetto, Giovanna Gentile,Fabiola Cipolla, Andrea Negro, Marina Borro, Paolo Martelletti & Martina Curto (2017)Lasmiditan for the treatment of migraine, Expert Opinion on Investigational Drugs, 26:2,227-234, DOI: 10.1080/13543784.2017.1280457
To link to this article: http://dx.doi.org/10.1080/13543784.2017.1280457
Accepted author version posted online: 11Jan 2017.Published online: 23 Jan 2017.
Submit your article to this journal
Article views: 31
View related articles
View Crossmark data

DRUG EVALUATION
Lasmiditan for the treatment of migraineMatilde Capia, Fernando de Andrés b,c, Luana Lionettod, Giovanna Gentilee, Fabiola Cipollae, Andrea Negrof,g,Marina Borroe, Paolo Martelletti f,g and Martina Curtof,g,h,i
aExperimental Immunology Laboratory, Fondazione Luigi Maria Monti, IDI-IRCCS, Rome, Italy; bCICAB Clinical Research Centre, ExtremaduraUniversity Hospital and Medical School, Badajoz, Spain; cDepartment of Analytical Chemistry and Food Technology, Faculty of Pharmacy, Universityof Castilla-La Mancha, Albacete, Spain; dAdvanced Molecular Diagnostic Unit, Fondazione Luigi Maria Monti, IDI-IRCCS, Rome, Italy; eNESMOSDepartment, Sapienza University of Rome, Rome, Italy; fDepartment of Clinical and Molecular Medicine, Sapienza University, Rome, Italy; gRegionalReferral Headache Centre, Sant’Andrea Hospital, Rome, Italy; hDepartment of Neurology and Psychiatry, Sapienza University of Rome, Rome, Italy;iBipolar & Psychotic Disorders Program, McLean Hospital, Belmont, MA, USA
ABSTRACTIntroduction: Migraine is one of the most common diseases in the world, with high economical andsubjective burden. Migraine acute therapy is nowadays based on specific and non-specific drugs but upto 40% of episodic migraineurs still have unmet treatment needs and over 35% do not benefit fromtriptans administration. Serotonin-1F receptors have been identified in trigeminal system and becamean ideal target for anti-migraine drug development as potential trigeminal neural inhibitors. Lasmiditan,a novel serotonin1F receptor agonist, showed specific affinity in vitro for the receptor without anyvasoconstrictive action and inhibited markers associated with electrical stimulation of trigeminal gang-lion in migraine animal models.Areas covered: This article reviews both preclinical and clinical studies on lasmiditan as a potentialacute therapy for migraine, as well as pharmacokinetic and pharmacodynamic features. It also sum-marizes safety and tolerability data gathered in the various human studies.Expert opinion: The absence of vasoconstrictive effects makes lasmiditan a promising novel migraineacute therapy. Although preclinical and Phase I and II studies established a significant efficacy, thelimited knowledge about pharmacokinetics and metabolism, the high rate of non-serious centralnervous system side effects and the lack of larger studies remain still a matter of concern that shouldbe addressed in future studies.
ARTICLE HISTORYReceived 6 September 2016Accepted 16 December 2016
KEYWORDSMigraine; acute; lasmiditan;5-HT1F receptor; clinical trials
1. Introduction
Migraine is one of the most common primary headache dis-order, ranked as one of the most prevalent (3rd) and debilitat-ing diseases worldwide as stated by the World HealthOrganization (WHO) [1–3]. Specifically, migraine affects over14% of adults worldwide [4] with an estimated progression tothe chronic form in about 1–4% of the population [5], espe-cially between the age of 50 and 60 years [6]. Chronicmigraine is characterized by headache occurrence at least15 days per month for more than 3 months, and with thefeatures of migraine headache on at least 8 days per month[7–9]. The total economic burden of migraine is estimatedaround €27 billion per year in Europe, and it is likely to besimilar in USA [9].
Migraine is characterized by moderate–severe, unilateral,throbbing headache attacks lasting from 4 to 72 h, accompa-nied by additional symptoms such as nausea, vomiting, pho-nophobia, and/or photophobia. According to the ICHD-3betaclassification [7], two major subtypes are indicated formigraine: migraine without aura, which is characterized byheadache with specific features and associated symptoms;and migraine with aura, primarily characterized by the
transient focal neurological symptoms that usually precedeor sometimes accompany the headache. A premonitoryphase (from hours to days before the headache attack) and aresolution phase can additionally occur in some patients. Bothphases include hyperactivity, hypoactivity, depression, crav-ings for foods, repetitive yawning, fatigue, and neck stiffnessand/or pain [7]. In about one-third of the cases migraine head-ache is preceded by the aforementioned aura (i.e. short-last-ing, fully reversible visual, sensory, or speech symptoms),which is less prevalent in women [10,11]. The cornerstonesof migraine pharmacological treatment are represented by theacute therapy, aimed to abort attacks and provide a promptrelief from pain, and the preventive treatment, aimed to lowerattacks frequency and severity [12]. Migraine acute therapy isnowadays based on specific (triptans and ergot derivatives)and nonspecific drugs (analgesics and nonsteroidal anti-inflammatory drugs – NSAIDs) that have shown efficacy intreating attacks. The choice between these two main classesmight be based on a stratified care approach, i.e. dependingon migraine severity and other clinical factors, or on the stepcare management, meaning that patients are primarily treatedwith analgesics but might receive specific drugs in case ofpoor response [12,13]. Both the ineffectiveness and the
CONTACT Paolo Martelletti [email protected] Department of Clinical and Molecular Medicine, Regional Referral Headache Centre, Via diGrottarossa, 1035, Rome 00189 Italy.
EXPERT OPINION ON INVESTIGATIONAL DRUGS, 2017VOL. 26, NO. 2, 227–234http://dx.doi.org/10.1080/13543784.2017.1280457
© 2017 Informa UK Limited, trading as Taylor & Francis Group

overuse of acute drugs are two of the major risk factors formigraine chronification. Moreover, medication overuse isthought to be associated with a less-effective acute treatmentthat might lead the patient to increase drug intake and/or thedosages, which in turn leads to headache progression [9].Acute treatment of migraine attacks has been greatlyimproved for the last two decades, although treatmentrequirements of 40% of episodic migraineurs are not currentlymet, and headache-related disability (19%) and dissatisfactionwith current drugs (15%) were stated in the AmericanMigraine Prevalence and Prevention as the most frequentcomplaints from patients [14]. Likewise, over 35% of partici-pants in clinical trials do not benefit from oral triptans admin-istration [15,16]. Therefore, novel and more effective acutetherapies are under active investigation and would hopefullyimprove migraine disability and clinical course. The pathophy-siology of migraine remains still not completely understood,and most of the acute agents have been developed when apivotal role in migraine headache was attributed to the abnor-mal vasodilation of intracranial vessels [17]. This hypothesiswas reinforced by the effectiveness of triptans in migraine, agroup of serotonin1B/1D (5-HT1B/1D) receptor agonists withvasoconstrictive effects. However, although the role of trige-minovascular system dysfunction has been widely described[10], it is still uncertain if it represents the primary nociceptive
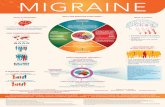
stimulus for migraine headache [18] and the neurogenichypothesis has been proposed. According to this model, cra-nial vasodilation is a secondary event in migraine pathophy-siology, and the primary cause is supposed to be the neuronalsensitization of the trigeminal system, i.e. the increased trans-mission of pain sensory information through the pathway [18].This hypothesis implies the possibility of an alternative non-vascular antimigraine mechanism represented by the neuralinhibition of trigeminal system [18,19]. In this view, serotonin-1F (5-HT1F) receptors, expressed by trigeminal neurons, tri-geminal ganglion (TG), and trigeminal nucleus caudalis (TNC)with no vasoconstrictive effects (Figure 1), became an idealtarget for antimigraine drug development. Lasmiditan, a novel5-HT1F receptor agonist, showed in vitro specific binding affi-nity for the receptor without any vasoconstrictive action andinhibited markers associated with electrical stimulation of theTG in animal models of migraine [20]. Moreover, human clin-ical trials showed significant effectiveness with a favorablesafety profile of lasmiditan oral administration as migraineacute treatment (Box 1).
2. Overview of the market
Currently, the so-called triptans family represents the mainstayof acute moderate-to-severe migraine therapy. Other first-linedrugs for mild-to-moderate migraine include nonspecificagents such as NSAIDs, acetaminophen, caffeine [21,22].Fixed combination of aspirin (250 mg), acetaminophen(200 mg), and caffeine (50 mg) showed a superior effective-ness than the same drugs administered alone [23–25].
Sumatriptan was the first triptan introduced in clinical use in1991, followed by other six molecules belonging to this family(naratriptan, rizatriptan, zolmitriptan, almotriptan, eletriptan,and frovatriptan) that largely replaced ergot derivatives usefor migraine acute treatment [26]. Collectively, they possesshigh affinity to three serotonin (5-HT) receptor subtypes (i.e.5-HT1B, 5-HT1D, and 5-HT1F) and their efficacy was demonstratedin large, randomized, placebo-controlled clinical trials. However,the vascular distribution of 5-HT1B receptors within the smoothmuscle and in cerebral blood vessels endothelium mediates thevasoconstrictive properties of triptans, and, consequently, the
Figure 1. Localization of 5-HT1F receptors within the migraine-related anatomical structures.
Box 1. Lasmiditan summary.
Drug name LasmiditanPhase IIIIndication Acute migrainePharmacology description/mechanism ofaction
5-HT1F agonist
Route of administration Oral, intravenousChemical structure
Pivotal trial(s) [17,18,32,33,42,43,44]
228 M. CAPI ET AL.

risk of coronary vasoconstriction [27]. For this reason, patientswith cardio- and/or cerebrovascular disease, uncontrolledhypertension, and/or with particular forms of migraine-likehemiplegic migraine cannot use triptans [27,28]. Furthermore,other triptans-related side effects such as chest tightness, throatdiscomfort, muscle pain, and paraesthesia could lead somepatients to avoid them [27]. Therefore, effective novel antimi-graine treatments without a relevant vasoconstrictor activityremain a considerable area of unmet clinical need. In thisview, lasmiditan represents a desirable option for the abortivetherapy of migraine attacks. Calcitonin gene-related peptide(CGRP) receptor antagonists (gepants) and monoclonal antibo-dies against CGRP and CGRP receptors constitute promisingalternatives [29,30], and different glutamate receptors antago-nists as well [31].
3. Introduction to lasmiditan
3.1. Chemistry
Lasmiditan, also known as COL-144 and LY573144, is a novel5-HT receptor agonist with high-affinity and selectivity for the5-HT1F receptor. Its chemical IUPAC name is 2,4,6-trifluoro-N-[6-[(1-methylpiperidin-4-yl)-carbonyl]pyridin-2yl]benzamide.
The chemical structure of lasmiditan, as well as the phar-macological profile, is clearly different from triptans. In fact,the indole structure of triptans, identical to the neurotransmit-ter 5-HT, is replaced by a pyridinoyl-piperidine scaffold, whichis not found in any other antimigraine classes. In addition,lasmiditan antimigraine efficacy is mediated through a non-vascular, primarily neural, mechanism, with a loss of the vaso-constrictor activity owned by triptans.
3.2. Pharmacodynamics
5-HT1F receptor agonists represent a potential alternative treat-ment in patients not responding to triptans and/or with cardio-vascular disorders. Selective 5-HT1F receptor agonists do notinvolve blood vessel diameter or contractility, while 5-HT1B/1Dreceptor agonists (such as triptans) do [32]. The first compoundtested as selective for 5-HT1F receptor has been LY334370 [17].This compound, while preserving the indole-based chemicalstructure, showed a relatively high selectivity for 5-HT1F (100-fold selective compared to 5HT1B and 5HT1D) and also for 5HT1Areceptors [20]. However, its development had to be discontinuedbecause of long-term safety concerns in animals [18].
Therefore, a new selective 5-HT1F receptor agonist, lasmidi-tan, has been developed changing the chemical structure ofLY334370 by deleting the indole moiety and is currently underclinical assessment. This new molecule showed a better recep-tor selectivity profile for 5-HT1F and a reduced affinity for 5-HT1A/1B/1D compared to LY334370.
Lasmiditan selectivity has been evaluated using radioli-gand-binding techniques on a panel of over 50 ion channels,transporters, and receptors. It showed high selectivity for 5-HT1F (450-fold higher affinity for 5-HT1F than for 5-HT1A/1B/1Dreceptors) and a significant low cross-reactivity with othermembers of the 5-HT1 receptor family, even if all of thesereceptors are structurally homologous. Moreover, lasmiditan
showed no significant affinity with a group of receptors thatregulate the vascular tone, the monoaminergic subtypes [20].
Lasmiditan chemical structure and activity profile are differentfrom those of triptans and LY334370 and account for its inclusionin a novel drug class called ‘ditans’ [33]. 5-HT1F receptors arepresent in different locations in the trigeminovascular system: inthe peripheral TG and in the central TNC (Figure 1). Sited atperipheral and central ends of sensory trigeminal neurons, theirfunction seems to be related to the hyperpolarization of nerveterminals and to the inhibition of trigeminal impulses [34]. Sinceit has been hypothesized that cranial vasodilation is not theprimary nociceptive stimulus for migraine, the inhibition of tri-geminal pathways could be a nonvascular antimigraine mechan-ism [19]. 5-HT1F receptors are not expressed by endothelial orsmooth-muscle cells of cerebral vessels; therefore, they are notimplicated in the vascular tone regulation of the human brain.
Moreover, after electrical stimulation of the TG in rats, theadministration of lasmiditan inhibited dural plasma proteinextravasation and decreased c-Fos expression in the TNC [10,35].
Furthermore, unlike sumatriptan, lasmiditan also penetratesthe blood–brain barrier (BBB) and could therefore trigger 5-HT1Freceptors centrally located on trigeminal neurons and reducethe c-Fos expression. Its effects could also be mediated by theaction of 5-HT1F receptors located outside the central nervoussystem (CNS), on primary trigeminal afferents or on cell bodieswithin the TG. Therefore, lasmiditan appears to be involved inthe reduction of second-order trigeminal neurons activationthat is considered an essential mechanism in the pathophysiol-ogy of acute migraine [30]. Moreover, 5-HT1F receptors havebeen found in humans also in cortical layers 4 and 5 and inthe granule cells of cerebellum [36] and lasmiditan activelypenetrates the BBB (brain/plasma ratios of 1.08, 1.57, 1.30, and1.33 at 0.5, 2, 4, and 6 h post-dosing, respectively) [37] withoutbeing a substrate of the efflux pump multidrug-resistance pro-tein 1. Therefore, other central effects might be linked to 5-HT1Fagonism by lasmiditan, but we could find no data available onthis topic. Furthermore, at the same concentrations, triptanscaused a 50% vessel diameter constriction whereas lasmiditanhad no vasoconstrictive effects. Moreover, lasmiditan low affinityfor 5-HT1B receptors produces no contractions of rabbit saphe-nous vein in doses up to 100 μM [33].
The interaction with 5-HT1F receptors and the absence ofvasoconstrictive effects make lasmiditan the first molecule of anew drug category, the neurally acting antimigraine agents(NAAMAs) [33].
3.3. Pharmacokinetics and metabolism
Data on the pharmacokintetics of lasmiditan are scarce. Wewere able to find only information about lasmiditan oral bioa-vailability from a poster presentation [38], reported around40%, and the time at which the maximum serum concentra-tion of lasmiditan is attained (Tmax), which ranges between 1.5and 2.5 h after oral administration of 50–400 mg [33,35,39]. Nodata about the possible influence of age and gender on theseparameters are available.
The results of a randomized, open-label study aimed toestimate lasmiditan relative bioavailability have been recentlyreported. The primary outcomes were the maximum serum
EXPERT OPINION ON INVESTIGATIONAL DRUGS 229

concentration (Cmax), Tmax, and the area under the curve (AUC)of lasmiditan 200 mg under fed and fasted conditions in 30healthy subjects. Cmax was, respectively, 394.7 ± 167.8(mean ± standard deviation) and 322.8 ± 122.0 ng/mL; Tmax
resulted, respectively, 2.5 ± 1.0 (mean ± standard deviation)and 1.5 ± 1.0 h and AUC0–t was 2244 ± 926.2 (mean ± standarddeviation) and 1892 ± 746.0 ng h/mL [40]. No data are availableon lasmiditan half-life (t1/2) and metabolism; therefore, the exis-tence of active and/or inactive metabolites is not known.
4. Clinical efficacy
So far, two selective 5-HT1F agonists have been tested inhuman trials for migraine: LY334370 [9] and lasmiditan(LY573144; COL-144) [32]. LY334370 was effective in an earlyproof-of-concept, placebo-controlled, double-blind, parallel-group study on moderate-to-severe acute migraineurs [41].Unfortunately, further clinical studies have been haltedbecause of long-term-associated animal toxicity [18].
4.1. Preclinical data
The hypothesis of an antimigraine effect of 5-HT1F receptorsagonists arose from the observation that sumatriptan was ableto inhibit CGRP release by the activation of 5-HT trigeminalneurons presynaptic receptors [42]. Given the sumatriptanmodest affinity for 5-HT1F receptors and their distribution ontrigeminal neurons, it was hypothesized that selective 5-HT1Fagonists might be useful in migraine [43,44]. Therefore, differ-ent 5-HT agonists were initially tested in the guinea pig duralplasma protein extravasation model and a strong correlationwas found between the 5-HT1F receptors affinity and theability to inhibit plasma protein extravasation, without vaso-constrictive effects [44,45]. The first 5-HT1F agonist developed,LY334370, showed promising efficacy with the inhibition ofdural extravasation in guinea pig migraine models [46] withany vasoconstrictive effects, but it was not developed after thehuman proof-of-concept trials because of its significant affinityfor 5-HT1A receptors and its possibility to activate 5-HT1B
receptors at certain plasma levels [20]. Therefore, researchhas focused on the elaboration of a 5-HT1F agonist with asubstantially different structure from triptans, and lasmiditanwas generated. It was then tested for binding affinity to the 5-HT1F receptors in vitro, and in two rodent models of migraine[20]. Specifically, lasmiditan oral administration strongly inhib-ited TNC c-Fos induction and protein dural extravasation asso-ciated with the electrical stimulation of TG [20]. It is able tocross the BBB and its action might be both central on trigem-inal neurons and peripheral on primary trigeminal afferentsand cell bodies within the TG. The vasocontrictive propertieswere also assessed in vitro using rabbit saphenous vein rings,and lasmiditan up to 100 μM concentrations showed no visi-ble contractions [20]. Anyway, there are no data demonstrat-ing the inhibition of CGRP release by lasmiditan and little isknown also about its binding sites in human brain potentiallylinked to adverse effects [10].
4.2. Phase I clinical trials
Four Phase I studies have been conducted for lasmiditan oralformulations and one for the intravenous (Table 1) [47]. Wewere not able to find published data from the first Phase Istudy on intravenous administration of lasmiditan in 2003,where 40 subjects were challenged with lasmiditan with theaim of evaluate safety, tolerability, and pharmacokinetics.Nonetheless, a larger Phase II study was carried out in 2007to assess intravenous lasmiditan efficacy and doses range inmigraine patients (see next paragraph). Two Phase I trials wereperformed in 2008 (COL MIG-102, COL MIG-103; Table 1) andaimed to evaluate bioavailability, safety, tolerability, and otherpharmacokinetic parameters of different oral formulations(oral solution, oral tablet, and sublingual). Although we werenot able to find extensive published data from these studies,oral formulations were demonstrated to reach plasma levelspreviously associated with efficacy of the intravenous admin-istration [38] without severe adverse effects associated.Reported side effects with the maximum dose of 400 mgwere drowsiness, dizziness, and paraesthesia. The oral solution
Table 1. Lasmiditan clinical trials.
Study Formulation PhasePatients onlasmiditan Objectives Results Date
COL-MIG 102 Oral solution andsublingual
I 44 Safety, tolerability, andpharmacokinetics
– 2008
COL-MIG 103 Oral solution and oraltablet
I 44 Bioavailability and pharmacokinetics – 2008
COL-MIG 104 Oral tablet I 30 Bioavailability under fed/fastedconditions
Ref [35] 2015
COL-MIG 105 Oral tablet I 55 Thorough QT study – 2011No Name (intravenousinfusion)
Intravenous I 40 Safety, tolerability, andpharmacokinetics
– 2003
COL-MIG 201 Intravenous II 88 Efficacy and dose–response relationship Ref [17] 2007COL-MIG 202 Oral tablet IIb 305 Efficacy and safety of a range of oral
dosesRef [32] 2009
COL-MIG 301 (SAMURAI) Oral tablet III 1.483 Efficacy Closed 2016COL-MIG 303(SPARTAN)
Oral tablet III 1.483 Efficacy Ongoing 2016
COL-MIG 305(GLADIATOR)
Oral tablet Long-term,open-label
2.200 Efficacy and long-term safety Ongoing 2016
Data from CoLucid Pharmaceuticals, Inc. Securities and Exchange Commission on 30 April 2015. http://investor.colucid.com/phoenix.zhtml?c=232283&p=irol-SECText&TEXT=aHR0cDovL2FwaS50ZW5rd2l6YXJkLmNvbS9maWxpbmcueG1sP2lwYWdlPTEwMjM2NTAwJkRTRVE9MCZTRVE9MCZTUURFU0M9U0VDVElPTl9FTlRJUkUmc3Vic2lkPTU3, last accessed 28 August 2016.
230 M. CAPI ET AL.

dose range at least effective as sumatriptan in acute migrainetreatment was calculated with a population pharmacokinetic–pharmacodynamic model and resulted of 170 mg and above[48]. In 2011, the Phase I study COL MIG-105 [A Randomized,Double-blind, Placebo-controlled, 4-way Crossover Study toCompare the Effects on the Cardiac de- and Re-polarizationDuration as well as other Cardiac Safety Parameters of TwoDoses of Oral Lasmiditan (100 mg and 400 mg) with those ofMoxifloxacin (400 mg) and Placebo in Healthy Subjects] deeplyexamined the QT/QTc changes in 55 subjects treated withlasmiditan and found no significant QT prolongation at either100 or 400 mg, compared to moxifloxacin that showed its QTprolonging effect similar to that seen in other published stu-dies [33,49]. Although we could not find extensive publisheddata, CoLucid reported no pro-arrhythmic effect of lasmiditanin the cardiologist assessments of ECGs, with safety and toler-ability similar to that observed in previous studies. The lastPhase I study evaluated the effect of the fed and fasted stateon pharmacokinetic parameters (Cmax, Tmax, AUC) and adverseeffects. The fed state was associated with an increased Cmax,Tmax, and AUC and a lower rate of mild adverse effect (19 vs.23) [40]. No serious adverse effects occurred and the mostcommon side effect was somnolence.
4.3. Phase II clinical trials
Two Phase II trials were performed in 2007 and 2009 (Table 1).The first study aimed to test the efficacy of intravenous lasmi-ditan for acute migraine treatment and to get informationabout the effective dose range [18]. It was a proof-of-concept,randomized, multicenter, double-blind, placebo-controlledtrial with a group-sequential, adaptive-treatment design. Onehundred and thirty patients with moderate-to-severe head-ache were allocated to a dose level of lasmiditan or placeboin small cohorts (five or six patients) and the dose used in thesubsequent cohort was adjusted depending on the headacheresponse and safety of the preceding group. Headacheresponse was defined as improvement from moderate orsevere headache to mild or no headache after 2 h fromlasmiditan administration. The first intravenous dose was2.5 mg and the highest was 45 mg. Lasmiditan was adminis-tered to 88 patients, whereas 42 received a placebo. Betterresponse (ranging from 54.2% to 75%) was observed in thegroups of patients receiving 10, 20, 30, and 45 mg of lasmidi-tan when compared to the placebo group (45.2%).Furthermore, a significant linear association between doselevels and response rates was identified [18]. The dose of20 mg showed a headache response rate of 64%, with atherapeutic gain of 19% with respect to placebo [19]. Thistrial was not powered to demonstrate superiority of singledoses of lasmiditan to placebo but gave the first largerhuman validation to the hypothesis that 5-HT1F agonism iseffective in migraine acute treatment.
The second Phase II trial aimed to assess efficacy and safetyof lasmiditan oral formulation [35] for acute migraine treat-ment. This was a dose-ranging, double-blind, parallel-group,and multicenter study. Five hundred and twenty-one patientswith migraine with or without aura who were not using
prophylactic treatments were randomly assigned to treat amigraine attack with oral lasmiditan 50, 100, 200, 400 mg orplacebo in a 1:1:1:1:1 ratio. Totally, 391 patients receivedlasmiditan and 86 were treated with placebo. The primaryend point was the headache response, defined as a moder-ate-to-severe attack becoming mild or disappearing at 2 h.Every lasmiditan dose was superior to placebo at 2 h and asignificant linear dose–response association was found. After1 h, all the doses but the 50 mg were superior to placebo, andthe 400 mg significantly reduced headache severity starting asearly as 30 min with respect to placebo. For oral lasmiditan400 mg, the therapeutic gain (38%) was higher than that ofthe intravenous 20 mg [19], probably because of the dosedifference (oral 400 mg corresponds to the intravenous doseof about 160 mg) [19]. The headache responses in the 100-and 400-mg groups were similar (Figure 2), and 100 mg wassuperior to 200 mg in terms of headache relief. It remains tobe clarified in larger clinical trials if it is related to the smallsample sizes and random variation in migraine attacks severityand response. Safety and tolerability issues reported in thesetrials will be discussed in the appropriate section (see below).
4.4. Ongoing trials
Two Phase III clinical trials and one long-term, open-labelstudy are ongoing (Table 1). The first Phase III trial (COL MIG-301 or SAMURAI, Id number NCT02439320) has been com-pleted with the enrollment of the last patient in June 2016[50]. Detailed results are expected to be available in the thirdquarter of 2016. It is a prospective randomized, double-blind,placebo-controlled, parallel-group study of two doses of las-miditan (100 and 200 mg) for the outpatient treatment of onemigraine attack. Only patients with episodic disablingmigraine (migraine disability assessment score ≥11) havebeen included. Primary outcome measure was the proportionof headache-free subjects 2 h post-dose (defined as moderateor severe headache becoming none); secondary outcome wasfreedom from the most bothersome symptom associated withmigraine, as identified by the subject, among nausea,
Figure 2. Headache response 2 h after the administration of placebo and orallasmiditan at different doses. Data taken from [35].
EXPERT OPINION ON INVESTIGATIONAL DRUGS 231

sensitivity to sound, and sensitivity to light. Other outcomemeasures were headache relief and use of rescue medication2 h post-dose, headache recurrence within 48 h from dose,proportion of patients nausea free, photophobia and phono-phobia free 2 h post-dose, safety up to 11 weeks (adverseevents [AEs]), and health-care resource utilization 6 monthsprior to enter in the study compared with its use during thetime of the study. The use of a second dose within 24 h wasallowed for rescue or recurrence of migraine. The presence ofcardiovascular risk factors did not exclude patients from thestudy whereas the initiation or change in concomitant pre-ventive medication within 3 months was an exclusion criter-ion. Patients were randomized with a 1:1:1 ratio to lasmiditan200 mg, lasmiditan 100 mg, or placebo.
The second Phase III trial (COL MIG-302 or SPARTAN, Idnumber NCT02605174) started in April 2016 and had a designsimilar to SAMURAI study. It evaluated with similar primary,secondary, and other outcomes three doses of lasmiditancompared to placebo (50, 100, 200 mg). It is expected toclose the recruitment in June 2017 [51].
The long-term open-label trial of lasmiditan (COL MIG-305 or GLADIATOR, Id number NCT02565186) is a safety/efficacy study started in October 2015 and estimated toend in May 2018. The subjects who have completed COLMIG-301 and 302 will be eligible to participate in thestudy. Subjects will be randomly assigned with a 1:1 ratioto receive lasmiditan 100 mg or lasmiditan 200 mg for thefirst and the second dose, if needed for rescue or recur-rence of migraine. All migraine attacks of the includedsubjects are treated with lasmiditan on an outpatientbasis for up to 12 months. Two end points are established:first, the proportion of patients and the proportion ofattacks associated with any AE and with specific AEs; and,second, the proportion of attacks treated with lasmiditanthat respond 2 h after receiving a dose. The 12-monthhealth-care resource utilization is additionally analyzed.
5. Safety and tolerability
The larger human safety and tolerability data were reportedfrom the oral lasmiditan Phase II study [35]. Lasmiditan waswell tolerated, as no triptan-like events (e.g. chest symp-toms) were reported. No clinically significant abnormalitiesof any safety parameters, i.e. heart rate, blood pressure, 12-lead ECG, hematology, biochemistry, and urine analysis fol-lowing the administration of lasmiditan, were observed, andnone of the subjects was excluded from the study due tothe occurrence of side effects. However, this selective 5-HT1Freceptor agonist showed a high incidence of adverse CNS-related events, such as dizziness, fatigue, vertigo, somno-lence, and paraesthesia. AEs rate increased when increasinglasmiditan dose. Specifically, treatment-emergent adverseevents (TEAEs) were reported by 65%, 72%, 86%, and 84%of subjects in the lasmiditan 50, 100, 200, and 400 mggroups, respectively [33]. In the placebo group, the 22% ofsubjects reported a TEAE. In lasmiditan 200 mg group,dizziness was reported by 38% of subjects, even if it hasbeen rated as severe by 17% of subjects treated with400 mg (compared to 15% in the 200-mg group).
Lasmiditan 400 mg induced fatigue in 23% of subjectswhereas the highest degree of severity (15%) was foundwith 200 mg (compared to 10% in the 400-mg group).Lasmiditan 400 mg was associated with vertigo in 23% ofpatients and scored as severe by 10% of them. Lasmiditan100 mg produced somnolence in 12% of subjects, even ifthe 50-mg dose was related to the major severity of this AE(4% vs. 2% in 100-mg group). 20% of patients treated withlasmiditan 400 mg reported paraesthesia and scored assevere by 7%. Lasmiditan 100 mg caused nausea in 10%of the subjects, and was reported as severe in a higherpercentage of patients treated with 50 mg (2% vs. 0%).Lasmiditan 200 mg induced sensation of heaviness in 10%of patients, although the 50- and the 400-mg groupsreported the highest percentage of severe intensity (4%vs. 3%) [35].
Several CNS symptoms were observed, probably because ofthe CNS permeability to lasmiditan. 5-HT1F receptors aremainly located in the cerebellum and the lateral vestibularnucleus, where they can be activated when lasmiditan isadministered, thus contributing to these aforementionedunwanted effects.
Although it was proven to be effective, little is knownregarding the binding sites of lasmiditan in human brain.This could predict a potential wide range of central sideevents that may delay lasmiditan further development [39].The high incidence of moderate or severe AEs after oral lasmi-ditan 100 and 400 mg could, if confirmed in a Phase III trial,limit the clinical use [19].
6. Conclusions
Lasmiditan has much higher affinity for 5-HT1F receptors thanfor vasoconstrictor 5-HT1B receptors [20] and seems to be safeand effective in the acute treatment of migraine when orallyadministered. Both preclinical and clinical studies showed pro-mising efficacy data with no severe AEs. Although these dataremain to be confirmed in Phase III clinical trials, it might offeran alternative to treat acute migraine with no cardiovascularrisk associated.
7. Expert opinion
Acute migraine pharmacological treatments aim to abort theattacks effectively in order to improve patients’ burden andfunctioning. Moreover, an effective acute therapy might pre-vent migraine chronification and drug abuse. Although effec-tive, currently specific and unspecific acute drugs are not ableto satisfy patients’ needs in a substantial percentage of sub-jects. In particular, triptans administration is limited in patientswith cardio- and/or cerebrovascular disease, uncontrolledhypertension, and with particular forms of migraine like hemi-plegic migraine due to their vasoconstrictive effects.Therefore, a novel, nonvascular, and effective acute antimi-graine drug would probably improve quality of life, socialand role functioning, and disease course in a significant num-ber of patients. Lasmiditan, a novel 5-HT1F agonist with novasoconstrictive action demonstrated in vitro and in vivo, has
232 M. CAPI ET AL.

been developed with these aims and showed a significantefficacy both in animal models of migraine and in humanPhase I and II trials. The absence of cardiovascular side effectsmight offer a new and effective therapeutic alternative inpatients affected by both episodic and chronic migraine withcontraindications or nonresponsive to triptans. Although it hasnot been compared yet to triptans in clinical studies, it hasbeen demonstrated effective with respect to placebo in twoPhase II clinical trials and other three Phase III trials areongoing. Nevertheless, lasmiditan ability to cross the BBBmight be the pharmacological substrate not only of its efficacybut also of the high rate of CNS side effects described in PhaseII clinical trials. In fact, dizziness, drowsiness, vertigo, somno-lence, and paraesthesia were reported from a substantialnumber of participants, across all the different oral lasmiditandoses groups. Although no serious AEs occurred, CNS sideeffects might affect both quality of life and functioning andshould be balanced, in future clinical use, with the benefitsgiven by headache relief in migraine patients. Moreover, phar-macokinetic data are still limited in literature, with only oralbioavailability, Cmax, Tmax, and AUC reported. Therefore, furtherstudies are needed to clarify additional pharmacokinetic data(t1/2) and metabolism parameters of lasmiditan before its clin-ical use could be suggested.
The absence of vasoconstrictive effects make lasmiditan thefirst molecule of a new drug category, the NAAMAs, with apromising future in acute migraine treatment. Moreover, las-miditan efficacy demonstrated in migraineurs strengthens theneural hypothesis of migraine that places vasodilation as asecondary event to the central sensitization of trigeminal sys-tem. Therefore, lasmiditan 5-HT1F agonist activity, both cen-trally on trigeminal neurons and peripherally on trigeminalafferents and cell bodies within the TG, might represent aconsiderable advancement in migraine acute therapy.Although preclinical and human data are promising andestablished a significant efficacy for acute migraine treatment,the limited knowledge about pharmacokinetics and metabo-lism, the high rate of nonserious CNS side effects, and the lackof large studies remain still a matter of concern that should beaddressed in future studies.
Funding
This paper received an unconditioned support by “Fondazione Italiana perlo Studio delle Cefalee” (FISC-ONLUS).
Declaration of interest
F de Andres was supported by Instituto de Salud Carlos III-Sara Borrellprogram (CD13/00348). The authors have no other relevant affiliations orfinancial involvement with any organization or entity with a financialinterest in or financial conflict with the subject matter or materials dis-cussed in the manuscript apart from those disclosed.
ORCID
Fernando de Andrés http://orcid.org/0000-0003-1076-0743Paolo Martelletti http://orcid.org/0000-0002-6556-4128
References
Papers of special note have been highlighted as either of interest (•) or ofconsiderable interest (••) to readers.
1. WHO. The world health report 2001 - mental health: new under-standing. Geneva: New Hope; 2001.
2. Steiner TJ, Stovner LJ, Birbeck GL. Migraine: the seventh disabler.Headache. 2013;53:227–229.
3. Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability(YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: asystematic analysis for the global burden of disease study 2010.Lancet. 2012;380:2163–2196.
4. Stovner LJ, Hagen K, Jensen R, et al. The global burden of head-ache: A documentation of headache prevalence and disabilityworldwide. Cephalalgia. 2007;27:193–210.
5. Martelletti P. The therapeutic armamentarium in migraine is quiteelderly. Expert Opin Drug Metab Toxicol. 2015;11:175–177.
•• The most important global study on disability related diseases,including for the first time medication overuse headachealongside migraine and tension-type headache.
6. Stovner LJ, Al Jumah M, Birbeck GL, et al. The methodology ofpopulation surveys of headache prevalence, burden and cost: prin-ciples and recommendations from the global campaign againstheadache. J Headache Pain. 2014;15:5.
7. Headache Classification Committee of the InternationalHeadache Society. The international classification of headachedisorders, 3rd edition (beta version). Cephalalgia. 2013;33:629–808.
8. Bigal ME, Serrano D, Reed M, et al. Chronic migraine in the popula-tion: burden, diagnosis, and satisfaction with treatment. Neurology.2008;71:559–566.
9. May A, Schulte LH. Chronic migraine: risk factors, mechanisms andtreatment. Nat Rev Neuro. 2016;12:455–464.
10. Mitsikostas DD, Tfelt-Hansen P. Targeting to 5-HT1F receptor sub-type for migraine treatment: lessons from the past, implications forthe future. Cent Nerv Syst Agents Med Chem. 2012;12:241–249.
11. Goadsby P, Lipton R, Ferrari M. Migraine- current understandingand treatment. N Engl J Med. 2002;346:257–270.
• An updated picture on harmful chronic migraine.12. Antonaci F, Ghiotto N, Wu S, et al. Recent advances in migraine
therapy. SpringerPlus. 2016;5:637.13. Becker WJ. Acute migraine treatment in adults. Headache.
2015;55:778–793.14. Lipton RB, Buse DC, Serrano D, et al. Examination of unmet treat-
ment needs among persons with episodic migraine: results of theAmerican Migraine Prevalence and Prevention (AMPP) study.Headache J Head Face Pain. 2013;53:1300–1311.
15. Ferrari MDM, Goadsby PJ, Roon KI, et al. Triptans (serotonin, 5-HT1B/1D agonists) in migraine: detailed results and methods of ameta-analysis of 53 trials. Cephalalgia. 2002;22:633–658.
16. Lionetto L, Borro M, Curto M, et al. Choosing the safest acutetherapy during chronic migraine prophylactic treatment: pharma-cokinetic and pharmacodynamic considerations. Expert Opin DrugMetab Toxicol. 2016;12:399–406.
17. Mitsikostas DD, Paemeleire K. Pharmacological management ofheadaches. Berlin: SpringerNature; 2015.
18. Ferrari MD, Färkkilä M, Reuter U, et al. Acute treatment of migrainewith the selective 5-HT1F receptor agonist lasmiditan–a rando-mised proof-of-concept trial. Cephalalgia. 2010;30:1170–1178.
19. Tfelt-Hansen PC, Olesen J. The 5-HT1F receptor agonist lasmiditan as apotential treatment of migraine attacks: a review of two placebo-controlled phase II trials. J Headache Pain. 2012;13:271–275.
20. Nelson DL, Phebus LA, Johnson KW, et al. Preclinical pharmacolo-gical profile of the selective 5-HT1F receptor agonist lasmiditan.Cephalalgia. 2010;30:1159–1169.
21. Giamberardino MA, Martelletti P. Emerging drugs for migrainetreatment. Expert Opin Emerg Drugs. 2015;20:137–147.
22. Evers S, Afra J, Frese A, et al. EFNS guideline on the drug treatmentof migraine–revised report of an EFNS task force. Eur J Neurol.2009;16:968–981.
EXPERT OPINION ON INVESTIGATIONAL DRUGS 233

23. Goldstein J, Hagen M, Gold M. Results of a multicenter, double-blind, randomized, parallel-group, placebo-controlled, single-dosestudy comparing the fixed combination of acetaminophen, acet-ylsalicylic acid, and caffeine with ibuprofen for acute treatment ofpatients with severe migraine. Cephalalgia. 2014;34:1070–1078.
24. Diener HC, Peil H, Aicher B. The efficacy and tolerability of a fixedcombination of acetylsalicylic acid, paracetamol, and caffeine inpatients with severe headache: a post-hoc subgroup analysis from amulticentre, randomized, double-blind, single-dose, placebo-con-trolled parallel group study. Cephalalgia. 2009;31:1466–1476.
25. Tajti J, Majláth Z, Szok D, et al. Drug safety in acute migrainetreatment. Expert Opin Drug Saf. 2015;14:891–909.
26. McCrory DC, Gray RN. Oral sumatriptan for acute migraine.Cochrane Database Syst Rev. 2003;3:CD002915.
27. MaassenVanDenBrink A, Reekers M, Bax WA, et al. Coronary side-effect potential of current and prospective antimigraine drugs.Circulation. 1998;98:25–30.
28. Tepper SJ, Millson D. Safety profile of the triptans. Expert OpinDrug Saf. 2003;2:123–132.
29. Negro A, Lionetto L, Simmaco M, et al. CGRP receptor antagonists:an expanding drug class for acute migraine? Expert Opin InvestigDrugs. 2012;21:807–818.
30. Giamberardino MA, Affaitati G, Curto M, et al. Anti-CGRP mono-clonal antibodies in migraine: current perspectives. Intern EmergMed. 2016;11:1045–1057.
•• An unprecedented vision on safety in acute therapy combinedwith prophylaxis in headache.
31. Sabato D, Lionetto L, Martelletti P. The therapeutic potential ofnovel anti-migraine acute therapies. Expert Opin Investig Drugs.2015;24:141–144.
32. Neeb L, Meents J, Reuter U. 5-HT(1F) receptor agonists: a newtreatment option for migraine attacks? Neurotherapeutics.2010;7:176–182.
33. Reuter U, Israel H, Neeb L. The pharmacological profile and clinicalprospects of the oral 5-HT1F receptor agonist lasmiditan in theacute treatment of migraine. Ther Adv Neurol Disord. 2015;8:46–54.
• An interesting paper on the pharmacology of lasmiditan.34. Rizzoli PB. Emerging therapeutic options for acute migraine: focus on
the potential of lasmiditan. Neuropsychiatr Dis Treat. 2014;10:547–552.35. Färkkilä M, Diener H-C, Géraud G, et al. Efficacy and tolerability of
lasmiditan, an oral 5-HT 1F receptor agonist, for the acute treat-ment of migraine: A phase 2 randomised, placebo-controlled, par-allel-group, dose-ranging study. Lancet Neurol. 2012;11:405–413.
36. Lucaites VL, Krushinski JH, Schaus JM, et al. [3H]LY334370, a novelradioligand for the 5-HT1F receptor. II. Autoradiographic localiza-tion in rat, guinea pig, monkey and human brain. NaunynSchmiedebergs Arch Pharmacol. 2005;371:178–184.
37. Kovalchin J, Ghiglieri A, Zanelli E, et al. Lasmiditan acts specificallyon the 5-HT1F receptors in the central nervous system. Glasgow:5th European Headache and Migraine Trust International Congress;2016 Sep 15th–18th. Available from: http://bit.ly/2jeutMs
38. Pilgrim A, Dussault B, Rupniak N, et al. COL-144, an orally bioavail-able selective 5-HT1F receptor agonist for acute migraine therapy.Cephalalgia. 2009;29:24–25.
39. Tajti J, Csáti A, Vécsei L. Novel strategies for the treatment ofmigraine attacks via the CGRP, serotonin, dopamine, PAC1, andNMDA receptors. Expert Opin Drug Metab Toxicol. 2014;10:1509–1520.
40. ClinicalTrials. Avaliable from: www.clinicaltrials.gov/ct2/show/NCT02233296?term=NCT02233296&rank=1
41. Goldstein DJ, Roon KI, Offen WW, et al. Selective seratonin 1F (5-HT(1F)) receptor agonist LY334370 for acute migraine: a randomisedcontrolled trial. Lancet. 2001;358:1230–1234.
42. Durham PL, Russo AF. Regulation of calcitonin gene-related pep-tide secretion by a serotonergic antimigraine drug. J Neurosci.1999;19:3423–3429.
43. Ramadan NM, Skljarevski V, Phebus LA, et al. 5-HT1F receptoragonists in acute migraine treatment: a hypothesis. Cephalalgia.2003;23:776–785.
44. Adham N, Bard JA, Zgombick JM, et al. Cloning and characteriza-tion of the guinea pig 5-HT1F receptor subtype: a comparison ofthe pharmacological profile to the human species homolog.Neuropharmacology. 1997;36:569–576.
45. Johnson KW, Schaus JM, Durkin MM, et al. 5-HT1F receptor agonistsinhibit neurogenic dural inflammation in guinea pigs. Neuroreport.1997;8:2237–2240.
46. Shepheard S, Edvinsson L, Cumberbatch M, et al. Possible antimi-graine mechanisms of action of the 5HT1F receptor agonistLY334370. Cephalalgia. 1999;19:851–858.
47. CoLucid Pharmaceuticals, Inc. Securities and exchange commission.[cited 2015 Apr 30]. Avaliable from: www.getfilings.com/sec-filings/150430/CoLucid-Pharmaceuticals-Inc_S-1.A/
48. Liefaard L, Drenth HJ, Pilgrim AJ, et al. Prediction of therapeuticallyeff ective dose of COL-144 based on relationship between plasmaconcentrations and headache response (poster). Cephalalgia.2009;29:24.
49. CoLucid. 2012. Available from: http://www.colucid.com/colucid-pharmaceuticals-details-phase-3-development-strategy-for-lasmiditan-to-address-major-unmet-needs-in-acute-migraine-therapy/
50. Colucid. Available from: www.colucid.com/colucid-pharmaceuticals-announces-last-patient-randomized-samurai-phase-3-pivotal-trial-lasmiditan-migraine-2/
51. ClinicalTrials.gov Available from: www.clinicaltrials.gov/ct2/show/record/NCT02605174?term=lasmiditan&rank=1
234 M. CAPI ET AL.