OBESITY SURGEONS MÉXICO ADVANCED LAPAROSCOPIC SURGERY FOR OBESITY SLEEVE GASTRECTOMY.
Laparoscopic Sleeve Gastrectomy - University College London
Transcript of Laparoscopic Sleeve Gastrectomy - University College London

University College Hospital
Laparoscopic sleeve gastrectomyCentre for Weight Loss, Metabolic and Endocrine Surgery

2

If you need a large print, audio or translated copy of the document, please contact us on 020 3447 9460. We will try our best to meet your needs.
ContentsPage
1 What is a Sleeve Gastrectomy? 5
2 How does it work? 6
3 How much weight can you expect to lose? 6
4 What are the risks of a Sleeve Gastrectomy? 7
5 What are the available alternatives? 9
6 How should I prepare for the procedure? 9
7 Asking for your consent 9
8 Pre-Assessment 10
9 The day of the operation 10
10 What should I expect after the procedure? 10
11 Discharge 11
12 What to do if you are unwell after surgery 14
13 Follow up appointments 14
14 Useful Links 14
15 Contact details 14
16 How to find us 15
3

4

5
1. What is a Sleeve Gastrectomy?A sleeve gastrectomy is a life changing operation. It is used to help people who are severely obese (BMI 40+ or BMI 35+ with other health conditions) to lose weight and improve their health. Losing weight should help to lower the risk of developing medical problems associated with obesity (e.g. high blood pressure, diabetes, arthritis, breathing problems and asthma).
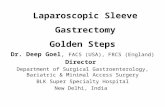
The sleeve gastrectomy makes your stomach smaller and should change the amount you can eat at your meals, which will help you to lose weight. It is not a reversible procedure.
Usually people considering a sleeve gastrectomy will have already tried many non-surgical options available to help them to lose weight.
New Stomach
(the sleeve)
Portion of stomach which is removed

6
2. How does it work?The surgery is usually done laparoscopically, commonly known as keyhole surgery. This means that you will be up and about soon after surgery and should make a speedy recovery. Although you will have some pain after surgery this is usually easily controlled by taking pain killers regularly.
The operation involves removing approximately 75 per cent of your stomach, leaving behind a narrow tube (sleeve) which becomes your new stomach. After the surgery food will follow the normal route into the smaller stomach and then on into the small intestine.
The operation also alters some of the hormone signals from the stomach and intestine to parts of the brain that control body weight. Following this operation, many patients report that they feel less like eating and feel fuller sooner and for longer after a meal.
As the size of your stomach has been reduced, the size of your meals will need to be reduced to be appropriate for your new small stomach. Your reduced portion size combined with low fat, low sugar choices will help you to lose weight.
A sleeve gastrectomy is permanent and is not a reversible procedure.
You may need to take vitamin supplements after the operation; we will tell you if you need to take any supplements.
3. How much weight can you expect to lose?You can expect to lose between 50 and 70 per cent of your excess weight in the fi rst 12 to 18 months following surgery:
A man who weighs 146 kg (22 stone 13lbs) and is 1.85 m (6’ 1’’) tall has a BMI of 42 kg / m2
• The upper limit of the ideal BMI (25 kg / m2) would give him a weight of 85.6 kg (13 stone 6lbs)

7
• 70 per cent excess weight loss = 42.3 kg. Total body weight = 103.7 kg (16 stone 4lbs) (BMI 30 kg / m2)
• A 50 per cent excess weight loss = 30.2 kg, with a weight of 115.8 kg (18 stone 3lbs) (BMI 34 kg / m2)
The amount of weight you are able to lose and keep off after surgery will depend also on the lifestyle changes that you make, such as increasing the amount of exercise you take and eating a healthy diet.
It is important to remember that the operation will not stop from you from craving certain foods or eating what you fancy.
4. What are the risks of a Sleeve Gastrectomy?As with all major surgery, sleeve gastrectomy has some risks. These risks vary according to your age and any other illnesses you may have.
The risk of death at the time of surgery or within the fi rst 30 days after surgery is estimated to occur in less than nought point fi ve per cent (or 1 in every 200 patients) having this operation.
Other complications, listed below, happen in seven per cent to ten per cent of patients (or seven to ten of every 100 patients).
Your surgeon will tell you your individual risk based on your current state of health.
Complications that can occur soon after surgery: • Wound infection: This can be treated with a course of antibiotics.
• Bleeding: You will be monitored carefully for signs of bleeding; a few patients will need a blood transfusion. Usually this will not be a problem but in the worst case scenario the surgeon will take you back to theatre and stop the bleeding (may involve an ‘open’ operation where the stomach has to be opened up with an incision).

• Blood clots in the legs or the lungs: To prevent blood clots from forming you will be given special stockings to wear and an injection to thin your blood. During and immediately after your operation you will also wear special boots; these will squeeze your leg muscles when you are in bed to prevent clots from forming. You should be able to get out of bed and walk around almost straight away. The nurses on the ward will encourage you to do this as it is an important way to prevent blood clots from forming. You will need to wear the stockings for six weeks after the operation. Smoking signifi cantly increases the risk of clotting. If you are a smoker, you must stop smoking before surgery. Your GP will be able to help you with this.
• Leaks from staple lines: This postoperative problem is rare but serious and may require emergency surgery. A leak can be caused by a staple falling out, allowing the contents of the stomach to leak out. If this happens, your hospital stay might be longer. Sometimes this will heal without any further surgery. In the worst case scenario your surgeon may decide to take you back to theatre to fi x the problem and stop the leaking.
Longer term complications after Sleeve GastrectomyLong term problems are uncommon but can include:
• Hernias of the abdominal wall.
• Narrowing of the new stomach which can cause problems with eating and drinking. This will usually settle on its own although sometimes it will need to be stretched under a local anaesthetic.
• Hair loss or thinning in the fi rst six months; this will re-grow.
8

5. What are the available alternatives?It is important for you to know that the procedure recommended is based on your specifi c medical history and dietary history.
Other options we offer include:
• Gastric Band.
• Gastric Bypass.
• Intensive Weight Control Programme (non-surgical pathway).
Please feel free to discuss your options with your surgeon
6. How should I prepare for the procedure?Read information on websites such as BOSPA and Weight Loss info.
• Discuss the operation with your close friends and family.
• Attend a support group at UCLH: ask the Clinical Nurse Specialist for more information.
• We would like you to be as fi t as you can prior to surgery; try to go for a walk every day and to keep up with your usual exercise routine.
• Two weeks before the operation you will be required to follow a low calorie liquid diet. This will help shrink the liver and make the operation easier for the surgeon and safer for you.
7. Asking for your consentBy law we must ask for your consent and will ask you to sign a consent form. This confi rms that you agree to have the operation and understand what it involves. Staff will explain all the risks, benefi ts and alternatives before they ask you to sign a consent form. If you are unsure about any aspect of the treatment proposed, please do not hesitate to speak with a senior member of staff again.
9

8. Pre-AssessmentA few weeks before your operation you will attend a pre-assessment appointment. This appointment is to check everything is in place for your admission. You will be given more information at this appointment about the admission process. You may also be seen by our Consultant Anaesthetist.
9. The day of the operation You will usually be admitted to the hospital on the day of your operation. You must not have anything to eat or drink (this includes chewing gum and calorie free mints) from midnight the night before your surgery, although you may drink plain water up until two hours before.
Please check with the nurse at your pre-assessment appointment which of your usual medication you should take on the day of your operation.
Once your admission is complete you will walk to the operating theatre if you are able. You will be put to sleep by the anaesthetist and you may have a urinary catheter put into the bladder, usually whilst you are asleep. You will also be given an intravenous drip so you can have fl uids during the operation.
10. What should I expect after the procedure?The fi rst few hours after the operation You will wake up in a recovery room where nursing staff will monitor you for any complications.
You will have a drip and may have a urinary catheter and a drain into the wound. You will also be wearing stockings and have a pumping device on your legs to prevent blood clots. As soon as you are fully awake, you will be transferred to either the surgical ward or the intensive care unit (ITU) where your relatives can visit you.
10

You won’t be able to eat or drink to allow your stomach to recover from the operation. To prevent you from becoming dehydrated you will continue to be given fl uids through the drip. You will receive painkillers to control any pain. Your surgeon will instruct you when you may start to drink water, it is important you do not have anything to drink until your surgeon feels it is safe for you to do so.
You will be encouraged to get out of bed as soon as possible after surgery. This helps to reduce the chance of post operative complications such as blood clots in the legs or chest infections.
The day after the operation If you have been looked after in ITU you will be transferred to the ward.
The amount you may drink will be increased every couple of hours until you are able to take 125ml (one glass) of water every hour.
Your drip will be removed when you are drinking enough to keep you hydrated.
If you have a catheter it will be taken out by the nurses and you will be able to get out of bed to go to the toilet.
The following two days after the operationYou should start to feel better very quickly after the operation and will be able to move around on your own.
You need to drink one 125ml glass of smooth fl uid every hour when you are awake. For example you may have tea and coffee, milky drinks and soup with no lumps.
If you have a drain it will be taken out one - two days after your operation. Two to three days after surgery you will be able to go home.
11

11. DischargePain and medicationYou will be given a supply of soluble painkillers to take home with you; these should be taken regularly for the fi rst few days. If you have no pain, gradually reduce the number of tablets you are taking.
Allow soluble tablets to stop fi zzing before you drink them.
Do not take any large tablets whole (in non-soluble form) for six weeks.
Take the soluble lansoprazole tablets for three months.
If you have been taking medication to control your blood pressure or diabetes, these will be reviewed before your discharge. In most cases these can be reduced or sometimes stopped all together. Please make sure you are clear about this before you leave the hospital.
Nutritional supplements If you have been advised to take nutritional supplements please ensure you take the calcium and iron medication two hours apart. If taken together the body is not able to absorb the iron.
WoundsThe small incisions made for your surgery will be more or less healed by the time you leave the hospital. The steri-strips (paper stitches) should be left to come off by themselves. Any stitches will be soluble. You will only need to go home with dressings if one of the wounds is oozing. If this is the case the ward nurse will ask you to visit the nurse at your GP surgery.
Anti-emboli stockingsYou should take these home with you and continue to wear them until you are walking about on a regular basis. We usually recommend wearing them for six weeks after your operation.
12

Eating and DrinkingYou will have been given a diet information sheet at your pre-assessment visit. You should have this with you at all times so you know what to drink and are familiar with the stages of food introduction in the next few weeks.
WashingYou can have a shower but do not soak in the bath for at least a week after surgery.
DrivingYou may drive as soon as you can comfortably wear a seat belt and are able to perform an emergency stop. You should check with your insurance company for their specifi c advice about driving after keyhole (laparoscopic) surgery.
Other ActivitiesYou will be able to walk straight after surgery. Try to go for a walk every day, gradually increasing the distance as you feel able. You will probably need at least two weeks off work but please check with your doctor. It is advisable to avoid heavy lifting for at least two months after abdominal surgery; if you are unsure discuss with your surgeon. You may resume sexual activity as soon as you feel comfortable.
Note: Women of childbearing age must not become pregnant for at least one year following a sleeve gastrectomy. If you do not already have regular contraception it may be worth visiting your local family planning centre for advice. After one year: if you are planning a pregnancy please contact our dieticians for nutritional advice.
13

12. What to do if you are unwell after surgeryMonday to Friday 09:00 till 17:00Contact the Bariatric Nurse Specialists 07943 826 528/07852 221 166Evenings / weekends:Contact your GPIf this does not work or you are very unwell please attend A and E at UCLH or your local A and E who will contact the team here.For conditions unrelated to your bariatric surgery please visit your GP or call NHS direct.
13. Follow up appointmentsYou should receive an appointment to see the clinical nurse specialist fi ve to six weeks after surgery.
14. Useful LinksBritish Obesity Surgery Patient AssociationWebsite: www.bospa.orgWeight Loss Surgery InfoWebsite: www.wlsinfo.org.uk
15. Contact detailsPlease, do not hesitate to ask a member of the Bariatric Team with any further questions you may have. All of us are happy to help you.
Switchboard: 0845 155 5000Secretary Direct Line: 020 3447 9460 Nurse: 07943 826 528Dietician: 07904 912 441Ward: 020 3447 0600Fax: 020 3447 9217Email: [email protected]: www.uclh.nhs.uk
14

16. How to fi nd usWe are based at University College HospitalNo car parking is available at the hospital. Street parking is very limited and restricted to a maximum of two hours.
Please note the University College Hospital lies outside but very close to the Central London Congestion Charging Zone.
15

First published: October 2010Last review date: July 2013Next review date: July 2015Leafl et code: UCLH/S&C/GI/BAR/LAPGB/1© University College London Hospitals NHS Foundation Trust
Created by Medical Illustration RNTNEH 020 3456 5103 Unique Code: 28545