Laparoscopic Adhesiolysis
-
Upload
george-s-ferzli -
Category
Health & Medicine
-
view
3.138 -
download
2
Transcript of Laparoscopic Adhesiolysis

Laparoscopic adhesiolysis

Results after laparoscopic lysis of adhesions and placement ofSeprafilm for intractable abdominal pain
L. Khaitan, S. Scholz, H. L. Houston, W. O. RichardsSurg Endosc (2003) 17: 247–253
• Abnormal attachments between tissues and organs.
• Adhesions have been reported after 93% of abdominal operations [12] and after 55% to 100% of pelvic operations [4].

Intraabdominal and PostoperativePeritoneal Adhesions
Harold Ellis, CBE, FACS (Hon), FRCS2005 by the American College of Surgeons
• Deaver, in the 1923 article, reviews the concept that it is peritoneal inflammation and trauma that are the important etiologic factors in the formation of these structures.

Intraabdominal and PostoperativePeritoneal Adhesions
Harold Ellis, CBE, FACS (Hon), FRCS2005 by the American College of Surgeons
• Until the introduction of anesthesia and then antiseptic surgery allowed laparotomy to become a comparatively common and comparatively safe procedure in the 1880s, intraabdominal adhesions were an uncommon phenomenon and of little, if any, interest to surgeons.
• With the advent of the era of abdominal surgery, deaths from postoperative adhesive obstruction began to be reported.
• The first fatal case of small bowel obstruction from a band (formed after removal of an ovarian cyst ) was by Thomas Bryant, of Guy’s Hospital, London, in 1872
• The first account of a laparotomy for adhesive obstruction was reported in the Lancet in 1883 by William Battle, then a surgical registrar at St Thomas’sHospital, London.
• The patient, a 43-year-old woman, had bilateral ovarian tumors removed 4 years earlier She was admitted with intestinal obstruction, was found at laparotomy to have matted adhesions of terminal ileum to the region of the cecum, and had a terminal ileostomy performed. Sadly, she died 3 weeks later.

Fewer adhesions induced by laparoscopic surgery?C. N. Gutt, T. Oniu, P. Schemmer, A. Mehrabi, M. W. Bu¨ chler
Surg Endosc (2004) 18: 898–906
Pathophysiology of adhesions• Both adhesion formation and adhesion-free epithelialization are pathways of peritoneal wound
healing. • The injury of the peritoneum may be inflammatory or surgical and may include exposure to
infection or to intestinal contents; ischemia; irritation from foreign materials such as sutures, gauze particles, or glove dusting powder; abrasion; desiccation; overheating by lamps or irrigation fluid; and many others.
• The healing attempt begins with the formation, through coagulation, of a fibrin gel matrix, which is the ‘‘ground’’ through which mesothelial cells can migrate and accomplish reepithelialization.
• When two injured peritoneal surfaces covered with this sticky fibrin matrix come into apposition, sticky bands and bridges of fibrin form between them.
• It is then the role of the fibrinolytic system to dissolve this fibrinous strands within a few days. However, this task cannot be always fulfilled because surgery dramatically reduces fibrinolytic activity, both by increasing the levels of plasminogen activator inhibitors and by decreasing the levels of tissue plasminogen activator (tPA) .
• If the fibrinous matrix persists, it will be infiltrated by proliferating fibroblasts which subsequently depose collagen. Mesothelial cells also migrate and form an uninterrupted layer on the surface of the already constituted adhesion.
• As the tissue underlying the adhesion is usually relatively hypoxic, signals initiating angiogenesis will be elaborated, resulting in a vascularized adhesion.

Intraabdominal and PostoperativePeritoneal Adhesions
Harold Ellis, CBE, FACS (Hon), FRCS2005 by the American College of Surgeons
• Up to the 1930s, strangulated hernias accounted for the majority of small bowel obstructions.
• In more modern times, as elective repair of hernias becomes standard treatment, and abdominal surgery so common, adhesive obstruction accounts for about three-quarters of all cases of small bowel occlusion.
• Interestingly, in the Third World, where abdominal surgery is fairly uncommon and patients usually do not report their groin hernias until they strangulate, the situation is reversed; strangulated hernias are common, and adhesive obstruction is rare.

Intraabdominal and PostoperativePeritoneal Adhesions
Harold Ellis, CBE, FACS (Hon), FRCS2005 by the American College of Surgeons
• Since the beginning of the 20th century, truly enormous attempts have been made to prevent the formation of postoperative adhesions.
• Attempts to prevent postoperative adhesions can be classified into:
A. Prevention of fibrin deposition, using citrate, heparin (both topically and systemically).
B. Removal of fibrin exudates between damaged surfaces. Attempts have been made to wash away or dilute the
fibrin using saline, hypertonic dextrose, and other solutions, or to digest or remove it with pepsin, trypsin, streptokinase, and tissue plasminogen activator .

Intraabdominal and PostoperativePeritoneal Adhesions
Harold Ellis, CBE, FACS (Hon), FRCS2005 by the American College of Surgeons
C. Separation of surfaces. Materials used in the past included saline, Ringer’s solution,
dextran, gelatine, olive oil, paraffin, silicones, plasma, lanoline, polyvinyl pyrrolidine, and an amazing variety of membranes—amnion, fish bladder, carp peritoneum, calf peritoneum, oiled silk, silver or gold foil, and free grafts of omentum.
• Only a membrane composed of hyaluronic acid and carboxymethylcellulose was shown to reduce adhesion formation in a clinical prospective randomized trial.
• More recently, a solution of icodextrin has reduced adhesion formation after laparoscopic gynecologic operations in a pilot study.
D. Inhibition of fibroblastic proliferation. Attempts to prevent the conversion of fibrinous adhesions into
established fibrous tissue have included studies of antihistamines and steroids given topically and systemically .

An evaluation of low molecular weight heparin and hyperbaric oxygentreatment in the prevention of intra-abdominal adhesions and wound healing
Soykan Arikan, M.D.a,*, Gokhan Adas, M.D.a, Gul Barut, M.D.b, Akin Savas Toklu, M.D.c,The American Journal of Surgery 189 (2005) 155–160
• Ellis [6] has classified these preventive measures into 5 groups: (1) installation of lubricants or distention with gas, (2) enhancement of peristaltic movements, (3) covering of raw surfaces, (4) enzymatic digestion, and (5) agents to inhibit fibrin deposition.
• It was reported that anticoagulants, especially heparin, were effective in decreasing the incidence of intra-abdominal adhesions [2,7–10].
• Hyperbaric oxygen (HBO) treatment has begun to be used with increasing incidence for many occasions and goals in the recent years. Basically, its effect in removing ischemia defines the main indications for its use [14].
• We concluded that enoxaparine Na decreased abdominal adhesions and HBO therapy had no beneficial effect on the formation of abdominal adhesions. We also showed that enoxaparine Na had no harmful effect on wound healing and HBO therapy increased the process of wound healing.

An evaluation of low molecular weight heparin and hyperbaric oxygentreatment in the prevention of intra-abdominal adhesions and wound healing
Soykan Arikan, M.D.a,*, Gokhan Adas, M.D.a, Gul Barut, M.D.b, Akin Savas Toklu, M.D.c,The American Journal of Surgery 189 (2005) 155–160
• The most common cause of intra-abdominal adhesions is a history of previous abdominal surgery [1].
• The formation of intra-abdominal adhesions may result from mechanical peritoneal damage, intra-abdominal tissue ischemia, or the presence of foreign materials [19,20].
• In the classic pathway of adhesion formation, peritoneal injury from trauma, infection, or ischemia results in an immediate type of inflammatory reaction followed by an increase in vascular permeability and the release of fibrin-rich exudate [15,21].
• In the absence of the lysis of this fibrin through the plasminogen-plasmin cascade, fibrous adhesions may form through collagen deposition [22]. Lysis of the fibrin depends on the activation of the peritoneal mesothelial plasminogen activator. Normal mesothelial cells possess plasminogen-activating activity [23].
• This physiologic property of normal mesothelial cells is decreased in the presence of surgical trauma, ischemia, or inflammation [22].
• Injury results in the rapid release of plasminogen-activator inhibitor-1 and -2 by mesothelial,endothelial, and inflammatory cells. This causes a loss of plasminogen-activating activity [11,24].
• For many decades, many materials and methods have been used to solve the adhesion problem.

Abdominal Adhesiolysis: Inpatient Care and Expenditures inthe United States in 1994
Nancy Fox Ray, MS,*William G. Denton, RN, MBA,†1998 by the American College of Surgeons
• Abdominal adhesions, which can begin forming within a few hours after an operation, represent one of the most common causes of intestinal obstruction.
• Complications of adhesions include chronic pelvic pain (20–50% incidence), small bowel obstruction (49–74% incidence), intestinal obstruction in ovarian cancer patients (22% incidence), and infertility due to complications in the fallopian tube, ovary, and uterus (15–20% incidence).
• Incidence rates for abdominal adhesions have been estimated to be as high as 90% after major gynecologic operations.

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
• Adhesions from prior surgery are the most common cause of small bowel obstruction in the Western world .
• The incidence of an adhesive small bowel obstruction after open abdominal surgery is between 12% and 17% .
• The socioeconomic impact of adhesive small bowel obstructions is significant. In 1996, Medicare paid $3.22 billion for adhesion related complications .
• Historically, laparotomy and open adhesiolysis have been the treatment for patients requiring surgery for small bowel obstruction.
• Unfortunately, this often leads to further formation of intraabdominal adhesions with approximately 10% to 30% of patients requiring another laparotomy for recurrent bowel obstruction .

Adhesion formation is reduced after laparoscopic surgeryC. L. Garrard,1 R. H. Clements,1 L. Nanney,2,3 J. M. Davidson,4 W. O. Richards1,5
Surg Endosc (1999) 13: 10–13
• Adhesions form as the end result of an inflammatory response to injury within the peritoneal cavity.
• Fibrin clot accumulating at the site of injury is usually lysed by the endogenous fibrinolytic systems.
• In more severe injury, fibroblasts migrate into the fibrin clot and produce collagen, which forms scars or adhesions.
• With a greater inflammatory response, there is less fibrinolysis and more fibroblast activity, resulting in more adhesion formation [1].
• The severity of inflammation is related to the degree of local tissue trauma, ischemia, and the presence of a foreign body [6].

Adhesion formation is reduced after laparoscopic surgeryC. L. Garrard,1 R. H. Clements,1 L. Nanney,2,3 J. M. Davidson,4 W. O. Richards1,5
Surg Endosc (1999) 13: 10–13
• We postulate that the tissue trauma of the incision increases the total inflammatory response, thereby inhibiting fibrinolysis and promoting fibroblast migration and collagen formation.
• The trauma of a midline incision contributes to the formation of intra-abdominal adhesions, even when the incision does not transect the peritoneum.
• These results strongly suggest that laparoscopic surgical techniques lead to fewer intra-abdominal adhesions by reducing tissue trauma, which in turn reduces circulating inflammatory mediators.

Abdominal Adhesiolysis: Inpatient Care and Expenditures inthe United States in 1994
Nancy Fox Ray, MS,*William G. Denton, RN, MBA,†1998 by the American College of Surgeons
• According to a previous study by Ray and associates,(11) 281,982 hospitalizations and $1.2 billion in hospital and surgeon expenditures were attributed to lower abdominal adhesiolysis in 1988.
• Since this earlier study was conducted, surgical practice has shifted dramatically from open abdominal procedures, which can lead to recurrent adhesions, to less invasive techniques such as laparoscopy.12–14
• Minimal-access laparoscopic techniques to identify and lyse adhesions increasingly have become the preferred surgical approach because of the advantages of more precise incision, less bleeding, and minimal damage to the surrounding tissue.3

Abdominal Adhesiolysis: Inpatient Care and Expenditures inthe United States in 1994
Nancy Fox Ray, MS,*William G. Denton, RN, MBA,†1998 by the American College of Surgeons
• The total cost in 1988 for adhesiolysis hospitalizations (adjusted to 1994 dollars) was $1.44 billion, which is $111.3 million more than the total cost in 1994. The decreased cost of adhesiolysis hospitalizations in 1994 is attributable to a decreased average length of stay.

Natural history of adhesional small bowel obstruction: counting the costBritish Journal of Surgery 1998, 85, 1294–1298
• Postoperative adhesions have become a major source of morbidity following laparotomy and are the most common cause of small bowel obstruction in the Western world.
• Similarly, pelvic adhesions are a frequent problem in patients suffering from subfertility.
• A recent survey of 750 German hospitals demonstrated that 2·6 per cent of laparotomies were for adhesional bowel obstruction1
• Ray et al.2 estimated that in 1988 the cost of treatment for lower abdominal– pelvic adhesionolysis in the USA was in excess of $1000 million.
• A prospective study by Menzies and Ellis3 indicated that approximately 1 per cent of patients will suffer obstruction within a year of abdominal surgery and that over a third of people who develop adhesional obstruction will do so within a year of surgery, with the remainder presenting with an initial episode of obstruction at a steady rate up to 10 years after surgery. This suggests an overall rate of adhesion-related morbidity of 3 per cent.

Natural history of adhesional small bowel obstruction: counting the costBritish Journal of Surgery 1998, 85, 1294–1298
• Menzies and Ellis’ prospective study3 indicated that while most adhesional obstruction occurs within 10 years (59 per cent by 5 years and 79 per cent by 10 years) there is no time limit as to when a patient may suffer an episode of obstruction.
• The mean time to presentation was 8·9 years with 26 per cent presenting within 1 year and 48 per cent presenting within 5·5 years.
• However, one patient presented with adhesional obstruction 35 years after an appendicectomy.

Fewer adhesions induced by laparoscopic surgery?C. N. Gutt, T. Oniu, P. Schemmer, A. Mehrabi, M. W. Bu¨ chler
Surg Endosc (2004) 18: 898–906
Clinical impact of adhesions• The major consequences of adhesions are infertility, pelvic or
abdominal chronic pain, and intestinal obstruction In addition to this increased morbidity, adhesions waste surgical time and resources by increasing the difficulty and risk of surgical reentry.
Infertility• In a recent study adhesions were found in 271 (37%) of 733 infertile
patients; in 41 (15%) of these 271 cases adhesions were the sole factor for infertility and in the rest of the cases, their presence was associated with tubal occlusion, endometriosis, or other infertility factors [29].
• Other authors also consider that moderate to severe pelvic adhesions may be responsible for 40% of infertility [45].

Fewer adhesions induced by laparoscopic surgery?C. N. Gutt, T. Oniu, P. Schemmer, A. Mehrabi, M. W. Bu¨ chler
Surg Endosc (2004) 18: 898–906
Pelvic and abdominal chronic pain• A prospective study revealed that 200 (82%) of 224 patients suffering of chronic abdominal pain
had only adhesions and no other disease; they underwent primary laparoscopic adhesiolysis and 3 months after adhesiolysis, 74% of patients were pain-free or had less pain, thus demonstrating that adhesions were the only cause of their suffering [40].
Intestinal obstruction• Worldwide statistics indicate adhesions to be one of the leading causes of intestinal obstruction,
accounting for30 to 60% of cases [7, 10, 21, 28, 30, 41, 46]. • An analysis based on data from the Scottish National Service revealed 280 readmissions (0.67%)
necessitating operative treatment for adhesive small-bowel obstruction in a cohort of 41,841 patients who underwent initial abdominal surgery 10 years before [12].
• A review of 18,912 patients with open surgery found that 2.6% required surgery for adhesive intestinal obstruction within the following 2 years [3].
• Another study followed 2,708 laparotomies for an average of 14.5 months and counted 26 cases (1%) that developed intestinal obstruction due to postoperative adhesions within 1 year of surgery [28].
• Although this percent situated between 0.5 and 2.6% may seem low, considering its application to all laparotomies worldwide it results in a considerable number of patients readmitted and re-operated as emergencies.

Fewer adhesions induced by laparoscopic surgery?C. N. Gutt, T. Oniu, P. Schemmer, A. Mehrabi, M. W. Bu¨ chler
Surg Endosc (2004) 18: 898–906
Other consequences• Adhesions to the abdominal incisions may prolong and complicate reentry
into the abdominal cavity at the time of a subsequent medical or surgical procedure.
• Intraperitoneal therapies, peritoneal dialysis, and chemotherapy are hindered [18].
• The complications related to laparoscopic access are mainly due to adhesions to the abdominal wall and frequently lead to conversion to open surgery [26].
• The presence of adhesions from previous surgeries can add at least 15 minutes to the operative time for reoperations, both because of the cautiousness needed when re-entering the abdomen and because of the adhesiolysis required to identify the anatomical structures at the operative site [5].
• Furthermore, adhesiolysis itself can be dangerous, because of accidental injuries to the bowel which, if not recognized, can lead to life-threatening peritonitis [43].

Fewer adhesions induced by laparoscopic surgery?C. N. Gutt, T. Oniu, P. Schemmer, A. Mehrabi, M. W. Bu¨ chler
Surg Endosc (2004) 18: 898–906
Laparoscopic aspects of adhesion formation• Type and amplitude of peritoneal trauma seems to play an important role in
pathophysiology of adhesion formation.• Since laparoscopic procedures are thought to considerably reduce the
overall degree of trauma to the abdominal wall, intraabdominal operative site, and distant intraabdominal organs, they potentially have an advantage of reducing the formation of postoperative adhesions.
Potential advantagesReduced incision of the parietal peritoneum. • The total area of injured peritoneum liable to establish adhesions to
underlying omentum or small bowel is much reduced after laparoscopy. Early return of bowel motility. • Laparoscopy speeds patients’ recovery from surgery. Earlier return of bowel
motility and early ambulation could also diminish postoperative adhesion formation by mechanically separating the coalescent peritoneal surfaces.

Fewer adhesions induced by laparoscopic surgery?C. N. Gutt, T. Oniu, P. Schemmer, A. Mehrabi, M. W. Bu¨ chler
Surg Endosc (2004) 18: 898–906
Reformation of adhesions after adhesiolysis
• There are only a few reports in the literature dealing with the subject of laparoscopic adhesiolysis, and they all conclude that laparoscopic adhesiolysis leads to significantly reduced adhesion reformation relative to open surgery.

Fewer adhesions induced by laparoscopic surgery?C. N. Gutt, T. Oniu, P. Schemmer, A. Mehrabi, M. W. Bu¨ chler
Surg Endosc (2004) 18: 898–906
• Development of acquired adhesions is a biological phenomenon in response to trauma to the peritoneum.
• Whatever this trauma is—mechanical and ischemic in surgery, inflammatory in endometriosis or septic–in- flammatory in peritonitis—the pathogenesis of adhesion formation follows several steps, the pivotal event being the apposition of the damaged peritoneal surfaces and the insufficient fibrinolysis [16].
• Adhesions are an important cause of morbidity and expense. The incidence of adhesion formation after a single abdominal operation is high, with an incidence over a lifetime of 47% after appendectomy and up to 91% after pelvic surgery [34].
• Adhesions are responsible for up to 40% of infertilities [29, 45], 80% of chronic postoperative abdominal pain [40], and 60% of intestinal obstructions [7, 10, 21] and they increase the technical difficulty of subsequent intraabdominal surgical procedures [5, 18].

Fewer adhesions induced by laparoscopic surgery?C. N. Gutt, T. Oniu, P. Schemmer, A. Mehrabi, M. W. Bu¨ chler
Surg Endosc (2004) 18: 898–906
• There are substantial theoretical reasons to claim fewer postoperative adhesions after laparoscopic surgery compared to conventional surgery:
• less tissue damage at the abdominal wall incision(s), decreased possibility of blind dissection of adhesions during abdominal exploration, lack of retractor and pack usage, maintenance of a closed abdomen with presumed reduction in peritoneal drying, less likelihood of introduction of foreign bodies, less tissue trauma and hemorrhage at the operative site.
• The general conclusion based on all materials presented in this article is that laparoscopy is associated with a reduction in the formation and reformation of adhesions.
• This conclusion, although not evidence based, constitutes a serious trend, having a great chance to be confirmed by subsequent randomized trials.

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
• Laparoscopic adhesiolysis was first described by gynecologists for the treatment of chronic pelvic pain and infertility.
• Laparoscopic adhesiolysis for small bowel obstruction was first reported by Bastug et al in 1991 in 1 patient with a single adhesive band.
• In addition, laparoscopy has been shown to decrease the incidence, extent, and severity of intraabdominal adhesions when compared with open surgery, thus potentially decreasing the recurrence rate for adhesive small bowel obstruction [8].

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
• Laparoscopic adhesiolysis for small bowel obstruction has a number of potential advantages:
(1) Less postoperative pain
(2) Quicker return of intestinal function (3) Shorter hospital stay (4) Reduced recovery time(5) Earlier return to full activity (6) Fewer wound complications(7) Decreased postoperative adhesion formation

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470.*
• The most important aspect to a successful outcome is proper patient selection and surgical judgment.
• There are no clear guidelines that state which patients are best suited for laparoscopic adhesiolysis; however, there are several factors that have been shown to predict a successful outcome.

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
• Chosidow et al [15] reported laparoscopic adhesiolysis on an emergent basis in 39 patients; the conversion rate was 36% compared with 7% in elective cases.
• Suter et al [13] found that a bowel diameter exceeding 4 cm was associated with an increased rate of conversion: 55% versus 32% (P 0.02).
• Patients with a distal and complete small bowel obstruction have an increased incidence of intraoperative complications and increased risk of conversion.

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
• Leo´n et al [19] state that a documented history of severe or extensive dense adhesions is a contraindication to laparoscopy.
• Navez et al [21] found that patients who had only a previous appendectomy were most likely to be successfully managed with laparoscopy.
• In contrast, Suter et al [13] found no correlation between the number and or type of previous surgeries and the chance of a successful laparoscopic surgery.

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
• The conversion rates range from 6.7% to 43% [10,13].
• The reported hospital length of stay in most series is 4 to 6 days for the laparoscopic group and around 12 days for the converted group.
• The incidence of intraoperative enterotomies ranges from 3% to 17.6%, with most authors reporting an incidence of about 10% [12,15].
• Suter et al [13] reported an intraoperative enterotomy incidence of 15.6%, of which 62% were repaired laparoscopically.

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
• One of the most dreaded complications of surgery is missed enterotomy.
• Although a missed enterotomy can occur after laparotomy, the incidence is higher after laparoscopic surgery.
• Suter et al [13] reported 4 of 47 cases (8.5%) of missed enterotomies that required reoperation.
• Others have also reported cases that required early reoperation for missed bowel perforations.
• Strickland et al [16] found that the duration of surgery longer than 120 minutes, bowel necrosis, intraoperative perforation, and conversion were significant predictors of postoperative morbidity.
• The reported mortality ranges from 0% to 3%. This rate is lower than the reported mortality after open surgery of adhesiolysis, which most likely represents patient selection.

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
• Navez et al [21] reported that 85% (29 of 34) of the patients treated laparoscopically were asymptomatic with a mean follow-up of 46 months.
• The series with the longest follow-up (mean 61.7 months) reported 87.5% (14 of 16) of the patients treated laparoscopically were asymptomatic [12].
• The question regarding decreased recurrence after laparoscopy compared with laparotomy remains to be answered.
• Interestingly, Khaitan et al [28] have described a new technique of applying Seprafilm laparoscopically, which could further decrease the recurrence of adhesive bowel obstruction.

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
Conclusions• Laparoscopic adhesiolysis has been shown to
be safe and feasible in experienced hands. • In selected patients, laparoscopic adhesiolysis
offers the advantages of decreased length of stay, faster return to full activity, and decreased morbidity.
• Patient selection and surgical judgment appear to be the most important factors for a successful outcome.



Is laparoscopy safe and effective for treatment of acutesmall-bowel obstruction?
P. Strickland, D. J. Lourie, E. A. Suddleson, J. B. Blitz, S. C. Stain
• In these cases, laparoscopy has been contraindicated due to the risk of enteric injury and the possibility of bowel distention, which would prevent the visualization of the point of obstruction.
• The laparoscopic treatment of acute small bowel obstruction is now possible and undoubtedly will become more common.

Is laparoscopy safe and effective for treatment of acutesmall-bowel obstruction?
P. Strickland, D. J. Lourie, E. A. Suddleson, J. B. Blitz, S. C. Stain
• Several reports have described the use of laparoscopy for the lysis of adhesions in patients with chronic abdominal pain or recurrent bowel obstruction [4, 5, 7].
• These studies found symptomatic improvement in 67– 87% of patients after laparoscopic adhesiolysis and a conversion rate of 5–7%.

Is laparoscopy safe and effective for treatment of acutesmall-bowel obstruction?
P. Strickland, D. J. Lourie, E. A. Suddleson, J. B. Blitz, S. C. Stain
Franklin et al. treated 23 patients with acute small bowel obstruction laparoscopically in 1994 [6]. Laparoscopic treatment was possible in 20 of 23 (87%). Their technique utilized a Veress needle, and adhesions were lysed with either scissors or a laser. Three cases were converted to open laparotomy because of severe adhesions, an inability to examine the bowel completely, and a suspected necrotic bowel, respectively.
• In a later series, Ibrahim et al. reviewed 33 consecutive cases of acute small bowel obstruction treated with laparoscopy [9]. Open initial trocar insertion was performed in all cases. Conversion to formal laparotomy was necessary in only five patients—two for small bowel resection, two for malignant adhesions, and one due to intolerance of pneumoperitoneum. Six additional patients underwent minilaparotomy— two for repair of enterotomy, one for gangrenous bowel, one for Meckel’s diverticulum, and one to confirm complete lysis. Overall, 18 patients (55%) underwent successful laparoscopic adhesiolysis, and 22 patients (67%) were spared laparotomy.
• In our series, 40 patients with acute small bowel obstruction were treated with laparoscopy. Open initial trocar insertion was performed in all cases. The point of obstruction was relieved entirely laparoscopically in 24 patients (60%), and only 13 patients required formal laparotomy (32.5%).

Is laparoscopy safe and effective for treatment of acutesmall-bowel obstruction?
P. Strickland, D. J. Lourie, E. A. Suddleson, J. B. Blitz, S. C. Stain
• In our series, enterotomies occurred in four of 40 patients (10%) during laparoscopic exploration and adhesiolysis.
• this figure is comparable to the reported incidence after open laparotomy for acute bowel obstruction. An even higher proportion of the patients had enterotomies after conversion (23%).
• Maintaining a low threshold for conversion to laparotomy in the face of extensive adhesions will further decrease the risk of bowel injury.

Laparoscopic approach to postoperative adhesive obstructionG. Borzellino, S. Tasselli, G. Zerman, C. Pedrazzani, G. Manzoni
Surg Endosc (2004) 18: 686–690
• Landercasper et al. reported a recurrence rate of 53 % after the first obstructive episode and 85% after the second [14],and a 50% recurrence rate within two years was reported by Barkan et al. [3].
• In our study recurrence rate in patients operated on after resolution of the acute phase was 13.5%.

Laparoscopic approach to postoperative adhesive obstructionG. Borzellino, S. Tasselli, G. Zerman, C. Pedrazzani, G. Manzoni
Surg Endosc (2004) 18: 686–690
• A review of literature showed a correlation between selection criteria and conversion rate (range 17–63.4%) [1, 5, 15, 23].
• The highest conversion rates are reported when no selection of patients is adopted [21], while the best results are reached with most severe exclusion criteria [1].
• A significant correlation was found between conversion and presence of peritonism by both Benoist et al.[5] and Suter et al. [23].
• Suter et al. evaluated the diameter of the dilated bowel establishing a limit of 4 cm beyond which the conversion rate increases significantly, while Benoist et al. did not find any correlation between radiological findings and conversion rate.
• Nonetheless, the author reports a conversion rate of 48.4 %, and in 80% of cases the conversion was due to the inability to identify or remove the site of obstruction.

Laparoscopic approach to postoperative adhesive obstructionG. Borzellino, S. Tasselli, G. Zerman, C. Pedrazzani, G. Manzoni
Surg Endosc (2004) 18: 686–690
• The number of previous operations was used as a selection criterion by various authors [1, 5, 23].
• No statistical correlation was found between the number of previous operations and the percentage of recurrence, complication, or need for conversion.
• Some authors included the experience of surgeon in the exclusion criteria [1, 2, 5, 23].
• Literature data reported a rate of intraoperative complications of 0–16.5%; the rate of postoperative complications was 4.5–31% [1, 2, 4, 5, 10, 13, 15, 17, 22, 23].
• The most severe intraoperative complication is small bowel perforation, which may occur at the time of first trocar placement, during manipulation of the bowel, or during lysis of the adhesions.

Laparoscopic approach to postoperative adhesive obstructionG. Borzellino, S. Tasselli, G. Zerman, C. Pedrazzani, G. Manzoni
Surg Endosc (2004) 18: 686–690
• In this study, no intestinal lesion occurred as a result of the insertion of the first trocar.
• This result was obtained with the help of ultrasonographic mapping of abdominal wall adhesions enabling creation of the pneumoperitoneum and insertion of the first trocar in areas free of adhesions in all cases.

Laparoscopic approach to postoperative adhesive obstructionG. Borzellino, S. Tasselli, G. Zerman, C. Pedrazzani, G. Manzoni
Surg Endosc (2004) 18: 686–690
• Only two authors reported follow-up data for the assessment of recurrences after laparoscopic adhesiolysis, with an observational period of 22 and 24 months.
• The percentage of recurrences reported by these authors was 5% and 10% [10, 22].
• The follow-up period of this study was longer, with an average length of 48 months. This may explain the higher percentage of symptomatic recurrences found in our study (15.4%), while surgical recurrences (4.6%) were similar to that reported by other authors.
• The laparoscopic approach could be effective also in patients with recurrent transit disturbances without signs of acute obstruction. In these patients adhesiolysis is associated with resolution of symptoms in 88% of cases with conversion and morbidity rates of 12 % and 8%, respectively.

Laparoscopic approach to postoperative adhesive obstructionG. Borzellino, S. Tasselli, G. Zerman, C. Pedrazzani, G. Manzoni
Surg Endosc (2004) 18: 686–690
• Preoperative ultrasonographic mapping of abdominal wall adhesions has an important role to play in the selection of patients and for first trocar placement.
• In our experience, this evaluation eliminates the risk of visceral injuries and enables the best location for successive trocars.

Laparoscopic adhesiolysis in patients with chronic abdominal pain: a blinded randomised controlled multi-centre trial D J Swank, S C G Swank-Bordewijk, W C J Hop, W F M van Erp, I M C Janssen,
HBonjer, J Jeekel THE LANCET • Vol 361 • April 12, 2003
• In 35–56% of patients with chronic abdominal pain, adhesions will be the only explanation, which suggests that laparoscopy is the best primary intervention in patients with such pain.1,2
• The reported rates of chronic pain relief after this procedure vary from 38% to 87%.8,9

Laparoscopic adhesiolysis in patients with chronic abdominal pain: a blinded randomised controlled multi-centre trial D J Swank, S C G Swank-Bordewijk, W C J Hop, W F M van Erp, I M C Janssen,
HBonjer, J Jeekel THE LANCET • Vol 361 • April 12, 2003
Discussion• We have shown significant relief of chronic pain after
laparoscopic adhesiolysis. However, this reduction in pain did not differ from that in controls with the same symptoms, pain scores, and frequency and severity ofadhesions who underwent diagnostic laparoscopy only.
• On the other hand, results from several studies have shown chronic pain relief after laparoscopic adhesiolysis, with improvement rates of 45–84%.8,9,20–22
• However, there is a 10% morbidity rate associated with laparoscopic adhesiolysis. Other investigators have reported bowel injury rates of between 10% and 25% during laparoscopic adhesiolysis for pain.15,23

Laparoscopic adhesiolysis in patients with chronic abdominal pain: a blinded randomised controlled multi-centre trial D J Swank, S C G Swank-Bordewijk, W C J Hop, W F M van Erp, I M C Janssen,
HBonjer, J Jeekel THE LANCET • Vol 361 • April 12, 2003
• Although laparoscopic adhesiolysis is done throughout the world, this procedure is not evidence based.

Laparoscopic compared with conventional treatment of acuteadhesive small bowel obstruction
C. Wullstein and E. GrossBritish Journal of Surgery 2003; 90: 1147–1151
• Laparoscopy is known to cause fewer intra-abdominal adhesions than open surgery, including adhesiolysis8–11, and results in quicker recovery of postoperative intestinal motility12,13.
• Acute obstruction may be associated with a higher risk of bowel injury and limited exposure due to severe abdominal distension than elective adhesiolysis7.

Laparoscopic compared with conventional treatment of acuteadhesive small bowel obstruction
C. Wullstein and E. GrossBritish Journal of Surgery 2003; 90: 1147–1151
• The number of previous laparotomies was identified as a risk factor for intraoperative complications.
• Major intraoperative complications occurred in 11 of 26 patients with two or more previous laparotomies compared with four of 26 patients with fewer laparotomies (P = 0·066).
• The duration of symptoms had no influence on the complication rate.

Laparoscopic compared with conventional treatment of acuteadhesive small bowel obstruction
C. Wullstein and E. GrossBritish Journal of Surgery 2003; 90: 1147–1151

Laparoscopic compared with conventional treatment of acuteadhesive small bowel obstruction
C. Wullstein and E. GrossBritish Journal of Surgery 2003; 90: 1147–1151
Postoperative results
• Patients in the LAP group experienced a quicker recovery of bowel movements (P < 0·001), a shorter length of hospital stay (P < 0·001) and had fewer postoperative complications (19·2 versus 40·4 per cent; P = 0·032) than those who had a conventional procedure (Tables 4 and 5).

Laparoscopic compared with conventional treatment of acuteadhesive small bowel obstruction
C. Wullstein and E. GrossBritish Journal of Surgery 2003; 90: 1147–1151
• A reduced field of vision together with the vulnerability of the bowel limits the use of laparoscopy and may explain why laparoscopy for acute SBO has the highest rate of conversion in laparoscopic surgery27.
• There is evidence that laparoscopic treatment of acute SBO leads to a higher rate of bowel injury than conventional surgery25.
• The rate of bowel perforation in this series was 26·9 per cent in the LAP group and 13·5 per cent in the CONV group.

Laparoscopic compared with conventional treatment of acuteadhesive small bowel obstruction
C. Wullstein and E. GrossBritish Journal of Surgery 2003; 90: 1147–1151
• Laparoscopic treatment of acute adhesive SBO was feasible in half of these patients, who benefited from a low postoperative complication rate, a quicker recovery of bowel function and a shorter hospital stay.
• An attempt at laparoscopic management of acute SBO seems justified in patients with fewer than two previous laparotomies but should not be offered to other patients because of the unacceptably high risk of intraoperative bowel perforation.

Results after laparoscopic lysis of adhesions and placement ofSeprafilm for intractable abdominal pain
L. Khaitan, S. Scholz, H. L. Houston, W. O. RichardsSurg Endosc (2003) 17: 247–253
• Overall, the outcomes were very good. Of the 19 patients in this study, 14 (74%) are very pleased with their procedure at this writing, and have completely discontinued all analgesics.

Results after laparoscopic lysis of adhesions and placement ofSeprafilm for intractable abdominal pain
L. Khaitan, S. Scholz, H. L. Houston, W. O. RichardsSurg Endosc (2003) 17: 247–253

Results after laparoscopic lysis of adhesions and placement ofSeprafilm for intractable abdominal pain
L. Khaitan, S. Scholz, H. L. Houston, W. O. RichardsSurg Endosc (2003) 17: 247–253
• In conclusion, laparoscopic lysis of adhesions combined with placement of Seprafilm is a relatively novel approach for patients with chronic abdominal pain secondary to adhesions.
• Meanwhile, patients can undergo this procedure with the expectation that their symptoms will improve.

Subjective evaluation of the therapeutic value oflaparoscopic adhesiolysisA retrospective analysis
E. Malik,1 C. Berg,1 A. Meyho¨fer-Malik,1 S. Haider,2 W. G. Rossmanith2Surg Endosc (2000) 14: 79–81
• Our results demonstrate that patients with intermittent pain, such as pain at defecation or micturition, enjoyed marked relief following adhesiolysis if other causes of chronic pain were excluded.
• The majority of patients with dyspareunia were relieved by adhesiolysis.
• Thus, patients who present with dyspareunia should be operated on laparoscopically to establish the existence of adhesions as a possible cause of their discomfort and perform adhesiolysis.
• Chan and Wood emphasized the great benefit of adhesiolysis in eliminating dyspareunia and indicated that amelioration or elimination of the symptoms was achieved in 70% of their patients [1].

Subjective evaluation of the therapeutic value oflaparoscopic adhesiolysisA retrospective analysis
E. Malik,1 C. Berg,1 A. Meyho¨fer-Malik,1 S. Haider,2 W. G. Rossmanith2Surg Endosc (2000) 14: 79–81
• The number of patients with laparoscopically confirmed adhesions without prior laparotomy or laparoscopy was 11 of 101 patients (11%).
• Kolmorgen and Schulz reported a rate of 25% of affected patients without prior surgery [4].
• For Mecke et al., the rate was 30% [9]; for Tavmergen et al., it was 27% [11].

Subjective evaluation of the therapeutic value oflaparoscopic adhesiolysisA retrospective analysis
E. Malik,1 C. Berg,1 A. Meyho¨fer-Malik,1 S. Haider,2 W. G. Rossmanith2Surg Endosc (2000) 14: 79–81
• Adhesiolysis is also beneficial in cases of dysmenorrhea or continuous lower abdominal pain.
• Since adhesions can be causally related to chronic pelvic pain, it is mandatory to achieve complete lysis of adhesions.

Adhesion prophylaxis in gynecological operationsMatthias Korell*, Eduard Elek
International Congress Series 1271 (2004) 278– 280
• Many attempts have been made to solve the problem of postoperative adhesions, but only the barrier methods could reduce its incidence and severity. Currently, we use two products available for adhesion prophylaxis—SprayGel (methylene blue coloured polyethylenglycol) and Adept (4% icodextrin solution) [11].
• SprayGel is as a two-component system with air pump and spray applicator and consists of blue coloured polyethylene glycol (PEG) designed to cover the serosal defects.
• After rapid reaction within seconds, it becomes a gel which sticks to the tissue very well. Rinsing is possible immediately following the application. SprayGel has shown efficacy in both animal and clinical studies [5,6,10,12].
• Adept, which is a 4% icodextrin solution— well-known for years in peritoneal dialysis [7]—has been shown to be effective and safe [2,3,13,16].

An evaluation of low molecular weight heparin and hyperbaric oxygentreatment in the prevention of intra-abdominal adhesions and wound healing
Soykan Arikan, M.D.a,*, Gokhan Adas, M.D.a, Gul Barut, M.D.b, Akin Savas Toklu, M.D.c,The American Journal of Surgery 189 (2005) 155–160
• Menzies and Ellis [1] found that 93% of the patients who had undergone 1 or more previous surgeries had intra-abdominal adhesions.
• These are abnormal attachments, and a significant cause of morbidity and mortality.
• Bowel obstruction, female infertility, abdominal pain, and technical difficulties are among the well-known problems caused by abdominal adhesions [1–3].
• It was reported that 5.7% of the hospital readmissions after any kind of previous abdominal or pelvic surgery were directly related to adhesions and 3.8% of these admissions were treated by laparotomy [4].
• Intra-abdominal adhesions cause a high financial burden for social budgets.Total costs related to adhesions have been estimated to be1.2 billion U.S. dollars per year [5].

Laparoscopic adhesiolysis for chronicabdominal pain is not indicated
D. Swank*International Congress Series 1279 (2005) 85– 89
• Diagnostic laparoscopy can reveal an incidence of adhesions as high as 95% [1–3].
• The presence of adhesions does not mean that these adhesions cause patients pain.
• Many surgeons performed laparoscopic adhesiolysis for chronic abdominal pain, and reported pain relief, but the successes were accompanied with 5% serious complications, and even 1% mortality [2–6].
• Moreover, adhesions reform after laparoscopic adhesiolysis, although to a lesser extent [7], and probably the success of laparoscopic adhesiolysis must be ascribed to placebo surgery [8].
2. Incidence• About 3–5% of all patients with adhesions will suffer from bowel obstruction,
strangulation, acute or chronic pain or infertility [9]. • Readmissions due to adhesion related disorders occurred in 35% of
patients following open gynaecological surgery, with an average of two readmissions per involved patient [10].
• Five percent of patients will be readmitted in the hospital for adhesion-related disorders during the 10 years following surgery [11].

Laparoscopic adhesiolysis for chronicabdominal pain is not indicated
D. Swank*International Congress Series 1279 (2005) 85– 89
4. Laparoscopic adhesiolysis• In the pre-laparoscopic era, conventional adhesiolysis for
chronic pain was rarely performed, because of its complications and the high recurrence rate of adhesions. After 1990, the laparoscope became a new tool, and many patients were laparoscopically treated for chronic abdominal pain, their indication mainly based on the drive of many surgeons to use their skills in laparoscopic surgery.
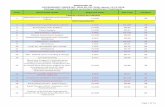
4.1. Laparoscopic adhesiolysis pro• A review of 16 studies, published in the last 10 years,
most of them retrospective and none randomised, reported success rates varying from 46% to 87% (Table 1).

Laparoscopic adhesiolysis for chronicabdominal pain is not indicated
D. Swank*International Congress Series 1279 (2005) 85– 89

Laparoscopic adhesiolysis for chronicabdominal pain is not indicated
D. Swank*International Congress Series 1279 (2005) 85– 89
5. Complications and its prevention• The incidence of serious complications (vascular lesions and visceral perforations) due to laparoscopic
adhesiolysis varies between 5% and 25% [3,8,17,18]. • Patients with greater age and a higher number of previous laparotomies are more prone to complications [18].• Critical in the procedure is the needle insertion, trocar placement and the adhesiolysis itself. • Bonjer et al. [19] reviewed the risks of Veress introduction and noticed 0.05–0.2%risk of visceral perforation. In
patients having had previous laparotomies insertion of the Veress needle in the left ninth intercostal space seems safer than the sub-umbilical route [17,20].
• Tan et al. [21] recommended ultrasonic mapping before trocar insertion in children. • The risk of visceral perforations was halved if an optic trocar (Optiview, Ethicon, Sommerville, NJ, USA) was used
for access, and an ultrasonic device (Ultracision, Ethicon, Cincinatti, OH) was applied for adhesiolysis [17]. • Almost half of all iatrogenous bowel perforations were not recognised, causing general peritonitis and even death
[18].6. Reformation of adhesions• Second-look procedures after laparoscopic adhesiolysis showed a permanent reduction of those adhesions
connecting organs and the abdominal wall, but not of those between organs themselves [7].• However, Mettler [22] found more often an increased adhesion score than a reduced one in patients at second-
look laparoscopy. • The severity of adhesion formation is influenced by 8.iso prostaglandin F2a, which is increased by elevation of the
intra-abdominal pressure induced by carbon dioxide [23]. • Adhesion reformation is a frequent occurrence after laparoscopic surgery, although de novo adhesions appear to
occur much less frequently than with open surgery [24].

Laparoscopic adhesiolysis for recurrent small bowelobstruction: long-term follow-up
Yoshiaki Sato, MD,Endoscopy 0016-5107/2001/
• In these studies, the success rate for laparoscopic adhesiolysis for acute small bowel obstruction has ranged from 46% to 87%.2-4,6

Laparoscopic adhesiolysis for recurrent small bowelobstruction: long-term follow-up
Yoshiaki Sato, MD,Endoscopy 0016-5107/2001/
• Francois et al.1 reported that 32 of 50 patients (64%) treated by laparoscopic adhesiolysis for small bowel obstruction or chronic abdominal pain were asymptomatic at a mean follow-up of 24 months.
• Strickland et al.3 studied 34 patients who underwent laparoscopic or open laparotomy for acute small bowel obstruction and found one recurrent small bowel obstruction requiring surgery in each group during a mean follow-up of 88 weeks.
• However, there have been no reports of laparoscopic adhesiolysis in which the follow-up period was more than 5 years.
• In the present study, the mean follow-up was 61.7 months. Although 14 patients (87.5%) remained asymptomatic, 2 had recurrent small bowel obstruction develop after laparoscopic adhesiolysis, 1 of whom required surgery.
• Laparoscopic adhesiolysis is safe and effective for the management of recurrent small bowel obstruction.
• This operation is associated with a short hospitalization and a low frequency of recurrence of• obstruction. • Because of the risk of formation of adhesions after conventional laparotomy, it is our belief that
laparoscopic adhesiolysis should be the first choice of operation for recurrent small bowel obstruction.
• However, conversion to laparotomy should be considered when it is difficult or dangerous to separate loops of bowel by using laparoscopic techniques.

Laparoscopic adhesiolysis for recurrent small bowelobstruction: long-term follow-up
Yoshiaki Sato, MD,Endoscopy 0016-5107/2001/
1. A, Laparoscopic view of single band adhesion. B,Laparoscopic view of convoluted mass of adherent bowel.

Laparoscopic management of mechanical small bowel obstructionAre there predictors of success or failure?
M. Suter, P. Zermatten, N. Halkic, O. Martinet, V. BettschartSurg Endosc (2000) 14: 478–483
• Conversion rates as low as 6% to 13% [13, 15] have been reported, sometimes with a significant reoperation rate resulting from incomplete exploration, adhesiolysis, or both [13]. In most studies, however, the conversion rate is higher, between 26% and 54% [1, 3, 5, 18, 21, 22, 23, 29].
• Reasons for conversion are mainly inability to identify the origin of the obstruction (usually in relation to a reduced working space because of intestinal distension), inability to relieve obstruction completely because of special anatomic features or adhesions that are too extensive, accidental bowel perforation, bowel necrosis, or causes not amenable to laparoscopic treatment (tumor, incarcerated hernia).

Laparoscopic management of mechanical small bowel obstructionAre there predictors of success or failure?
M. Suter, P. Zermatten, N. Halkic, O. Martinet, V. BettschartSurg Endosc (2000) 14: 478–483
• Neither the number or type of previous operations nor the location of the previous incisions influenced the location and type of adhesions or the need for conversion.
• Evidence of bowel necrosis obviously could be considered as an indicator for immediate laparotomy.

Tips &Tricks in Laparoscopic Adhesiolysis

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
Operative techniquePeritoneal access• Peritoneal access and trocar injury to the
distended bowel are major concerns regarding the feasibility of laparoscopic adhesiolysis.
• The initial trocar should be placed away (alternative site technique) from the scars in an attempt to avoid adhesions (Fig. 1).

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
• Although alternative site entry can be performed with either an open (Hasson) or blind-access (Veress needle) technique, the open approach is more prudent in cases of laparoscopy for small bowel obstruction.
• Sato et al [12] reported using the Veress needle in 16 patients without a single complication. The importance of confirming the position of the needle with the saline drop test and monitoring the pressure during insertion of the Veress needle was emphasized.
• In contrast, Levard et al [11] reported a 3.7% incidence of intestinal perforation using a blind-access technique in cases of bowel obstruction.

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
• Most authors advocate the use of the open technique because of concerns about intraabdominal adhesions fixing segments of bowel to the undersurface of the abdominal wall [13,19,21,23].
• The open technique is performed similar to a muscle-sparing incision for an appendectomy.
• Careful dissection is required to avoid injury to the underlying adherent bowel. Blind cutting or spreading must be avoided.
• The open technique allows the identification of adherent bowel and dissection of the bowel away from the abdominal wall.
• Although the open technique does not completely eliminate the risk of bowel injury, it does allow the surgeon to promptly identify and repair any injury that may occur.
• Finally, there have been no reports of vascular injuries with the open technique, as have been described with the blind access technique.
• The disadvantage of the open technique is the increase in operative time, particularly in obese patients.

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
• Another technique that has gained favor is the use of optical access trocars.
• In experienced hands, optical access trocars are safe and facilitate rapid entry into the peritoneal cavity.
• String et al [9] reported their use in 650 patients, with a mean entry time of 77 seconds and a complication rate of 0.3%.
• With this technique a 0-degree laparoscope is inserted through the transparent cannula as the trocar is advanced through the abdominal wall, thereby visualizing each tissue layer of the abdominal wall.
• The advantage of this technique is that it allows you to identify the bowel wall before inserting the trocar into the bowel.
• Furthermore, if an injury does occur, it is recognized at that time and managed appropriately.

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
• Once safe access is obtained, the next goal is to provide adequate visualization in order to insert the remaining trocars.
• This often requires some degree of adhesiolysis along the anterior abdominal wall. Numerous techniques are available, including finger dissection through the initial trocar site and using the camera to bluntly dissect the adhesions.
• Sometimes, gentle retraction on the adhesions will separate the tissue planes. • Most often sharp adhesiolysis is required. The best technique is to follow the line of
tissue adherence, if possible, which results in less bleeding and less risk for bowel injury. A traction-countertraction technique as used for open adhesiolysis is effective.
• The use of cautery and ultrasound dissection should be limited in order to avoid thermal tissue damage.
• A particularly difficult situation involves dense adhesions between the bowel and anterior abdominal wall. In this case, the plane between the bowel and the peritoneum is often obliterated, and it is necessary to dissect in the preperitoneal fat.
• In most cases, at least two additional trocars will be needed in order to achieve adequate adhesiolysis.
• If possible, the trocars should be placed to operate along the sights of the camera and not against the camera.
• Surgeons should be flexible about trocar placement, and additional trocars should be placed as needed to accomplish the necessary adhesiolysis.

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
Technique for adhesiolysis• After trocar placement, the initial goal is to expose the collapsed
distal bowel. • This is facilitated with the use of angled telescopes and maximal
tilting/rotating of the surgical table. It may also be necessary to move the laparoscope to different trocars to improve visualization.
• Manipulation of thin-walled, friable, dilated small bowel should be avoided.
• Even with atraumatic graspers, injury to the bowel wall can occur. • If necessary, the small bowel mesentery (instead of the bowel wall)
should be grasped in order to manipulate the bowel. • Once the collapsed distal bowel is exposed, atraumatic graspers
should be used to run the decompressed small bowel proximally until the site of obstruction (transition point) is found.

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
• Sharp dissection with the laparoscopic scissors should be used to cut the adhesions. • Cautery should be avoided in order to prevent potential thermal injury to adjacent bowel.• The use of cautery also causes tissue ischemia (a very potent adhesion promoter), which leads
to the formation of more intraabdominal adhesions. • Only pathologic adhesions should be lysed. • Additional adhesiolysis only adds to the operative time and to the risks of surgery without benefit. • If the point of obstruction is not clearly identified, adhesiolysis should continue until all suspicious
adhesion or bands are transected. • If all adhesions cannot be lysed then conversion to an open procedure should be strongly
considered. • Once adequate adhesiolysis is complete, the area lysed should be thoroughly inspected for
possible bleeding and bowel injury.• If found, these complications should be treated appropriately.• Small bleeding points may be controlled with clips, suture, or careful cautery. • Serosal tears and enterotomies can be repaired laparoscopically; however, there should be a low
threshold to convert. • If there is any concern about the integrity of the bowel, we recommend a minilaparotomy in order
to examine the bowel under direct visualization.

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
Intraoperative findings
• Perforated or gangrenous bowel is best managed with conversion to either a minilaparotomy or a formal laparotomy.

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
• Matted small bowel loops and dense adhesions are also best managed with a formal laparotomy.
• Navez et al [21] reported that only 10% of obstructions caused by dense adhesions could be treated successfully with laparoscopy.
• On the other hand, when the cause of obstruction was a single band, laparoscopic adhesiolysis was successful 100% of the time [21].
• Unfortunately, it is difficult to predict the degree of intraabdominal adhesions prior to surgery.

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
• Conversion to a laparotomy should not be considered a failure or complication, but rather a recognition of limitations posed by technology, the surgical expertise, or factors unique to a particular patient or disease process.

Laparoscopic adhesiolysis for small bowel obstructionAlexander Nagle, M.D., Michael Ujiki, M.D., Woody Denham, M.D.,
Kenric Murayama, M.D.*The American Journal of Surgery 187 (2004) 464–470
• Patients who require an emergent operation are not good candidates for laparoscopic adhesiolysis.
• Patients with bowel dilatation less than 4 cm and a partial obstruction can be considered for laparoscopic adhesiolysis.
• Patients who have a chronic or recurrent partial obstruction documented on a contrast study are also good candidates for laparoscopic adhesiolysis.
• Technically, peritoneal access should be achieved with the open (Hasson) technique in order to avoid bowel injury.
• Grasping the dilated, thin-walled bowel and the use of cautery should be avoided. • The most common reasons for conversion include dense adhesions, unable to
visualize the site of obstruction, iatrogenic intestinal perforation, bowel necrosis and colonic cancer.
• There should be a low threshold to convert to a minilaparotomy or to a formal laparotomy.
• Conversion should not be considered a failure, but rather good surgical judgment. • Further studies need to examine the open versus the laparoscopic procedure in a
prospective randomized fashion and evaluate the cost effectiveness of this approach.

Is laparoscopy safe and effective for treatment of acutesmall-bowel obstruction?
P. Strickland, D. J. Lourie, E. A. Suddleson, J. B. Blitz, S. C. Stain
Surgical technique• All patients had nasogastric suction and Foley catheter drainage prior to
operation. • The initial trocar placement at the umbilicus and pneumoperitoneum was
established using a blunt-tip Hasson trocar. • Additional ports (usually two) were placed under direct vision. The entire
abdomen was inspected laparoscopically.• If the point of obstruction was readily identified, it was relieved via sharp
dissection or electrocautery. • More recently, the harmonic scalpel has occasionally been utilized (two
cases). • The bowel was then run from the cecum proximally with two atraumatic
graspers. In those cases in which the point of obstruction was clearly identified (with collapsed bowel distally and dilated loops proximally), the obstruction was relieved without further examination of the bowel. In all other cases, inspection was continued to the ligament of Treitz.

Safe laparoscopic adhesiolysis with optical access trocar and ultrasonic dissectionA prospective study
D. J. Swank,1 H. J. Bonjer,2 J. JeekelSurg Endosc (2002) 16: 1796–1801
• Several safety measures for laparoscopic surgery have been proposed, such as subcostal insertion of the Veress needle [17], use of an optical trocar [10], radially dilating trocars [2], and open introduction of the initial trocar [3, 5, 18].
• The optical trocar (Optiview, Ethicon,Endosurgery, Cincinnati, OH) is a blunt optical trocar, which is guided through the abdominal wall with the camera inside and controlled by the monitor. This device might combine the advantages of a safe and a fast penetration of the abdominal cavity.

Safe laparoscopic adhesiolysis with optical access trocar and ultrasonic dissectionA prospective study
D. J. Swank,1 H. J. Bonjer,2 J. JeekelSurg Endosc (2002) 16: 1796–1801
• Laparoscopic adhesiolysis with scissors is inconvenient because of bleeding.
• Electrodissection causes charring of tissue and delayed perforations because of its excessive heat production [7, 12, 20, 23].
• Bipolar electrosurgery has the advantage of reducing the electrosurgical complications but still has delayed thermal lesions [23].
• The ultrasonically activated scalpel causes less heat production compared with electrocautery dissection,thereby theoretically lowering the risk of delayed perforations.

Safe laparoscopic adhesiolysis with optical access trocar and ultrasonic dissectionA prospective study
D. J. Swank,1 H. J. Bonjer,2 J. JeekelSurg Endosc (2002) 16: 1796–1801
• For pneumoperitoneum a Veress needle was induced preferably caudally to the umbilicus.
• In case of a midline scar, the entry site was chosen left subcostally. In case of a traverse incision in the upper abdomen the Veress needle was introduced in the intercostal space just above the eighth rib in the midclavicular line on the left side.

Safe laparoscopic adhesiolysis with optical access trocar and ultrasonic dissectionA prospective study
D. J. Swank,1 H. J. Bonjer,2 J. JeekelSurg Endosc (2002) 16: 1796–1801
• Optical trocar
• The distal fold of the umbilicus was preferred as introduction site of the initial trocar (Optiview) in patients without a midline incision.
• Otherwise the introduction took place at least 5 cm lateral of the scar away from the expected location of adhesions.

Safe laparoscopic adhesiolysis with optical access trocar and ultrasonic dissectionA prospective study
D. J. Swank,1 H. J. Bonjer,2 J. JeekelSurg Endosc (2002) 16: 1796–1801
• Sufficient tension on the organs is necessary to maximize the effect of ultrasonic adhesiolysis.
• If bowel loops were very adherent with the parietal peritoneum, the latter was released from the abdominal muscles and not lysed from the bowel.
• The lysis of different organs should be done slowly to allow sufficient time to seal small vessels. Small bleedings were dealt with by the UD; if not successful, monopolar electrocautery was used.

Safe laparoscopic adhesiolysis with optical access trocar and ultrasonic dissectionA prospective study
D. J. Swank,1 H. J. Bonjer,2 J. JeekelSurg Endosc (2002) 16: 1796–1801
Optical trocar• The traditional approach of the abdominal cavity for laparoscopic surgery is a closed trocar
penetration after the establishment of a pneumoperitoneum with a Veress needle. • Visceral lesions in closed introduction have been reported between 0.06 and 0.4 % [11]. • Half of these visceral lesions are caused by the trocar and consist of damage to the small bowel
ranging from superficial serosal damage to perforation. However, all other intraabdominal organs may also be involved and these have a high mortality rate of 5% up to 15% [16].
• The rate of major vascular injuries with the closed technique varies from 0.02% to 0.24% [11]. • Vascular lesions are mostly caused by the Veress needle and in a minority of cases Caused as a
consequence of trocar introduction [16]. • The eighth intercostal space as the site for the Veress needle has been chosen three times to
avoidad hesions after a previous traverse incision in the upper abdomen. We found an easy introduction due to the short passage and adherent parietal peritoneum. This site is at least 5 cm away from the diaphragm.
• Childers has chosen the left ninth intercostal space after median laparotomies and has recommended this as a safe site in patients with high-risk subumbilical adhesions [6].

Safe laparoscopic adhesiolysis with optical access trocar and ultrasonic dissectionA prospective study
D. J. Swank,1 H. J. Bonjer,2 J. JeekelSurg Endosc (2002) 16: 1796–1801
• Very large randomized studies might show differences in safety of a specific trocar. • Catarci et al., after evaluation of nearly 13,000 laparoscopic procedures, found the open
approach to be the safest way with minimal risk of visceral and vascular injury (0.09%) versus 0.27% complications with an optical trocar.
• Hashizume emphasizes that with the open Hasson technique only the vascular and visceral risks of the Veress needle and of the initial trocar introduction are diminished and that some visceral lesions are made by the second and following trocars even if introduced under direct vision (0.02%) [11].
• Radially expanding trocars have peritoneal access by dilatation rather than by dissection. • For adhesiolysis we prefer disposable second and third trocar s because the glide of a
disposable trocar is more convenient for multiple very accurate movements.• Even when a pneumoperitoneum cannot be achieved, the optical trocar access is safe. • String et al. used this trocar without a pneumoperitoneum in 650 different laparoscopic
procedures with two small-bowel and gallbladder perforations (0.3%) [25]. This technique avoids the complication risk of the Veress needle puncture, but misses the black hole as indication of distance between abdominal wall and abdominal organs and one has to rely on the movements of the bowel to differentiate the parietal from the visceral peritoneal layer.
• Lifting the abdominal wall does not change the position of the peritoneum in relation to the intraabdominal organs [4].

Safe laparoscopic adhesiolysis with optical access trocar and ultrasonic dissectionA prospective study
D. J. Swank,1 H. J. Bonjer,2 J. JeekelSurg Endosc (2002) 16: 1796–1801
• The great advantage of UD is the simultaneous dissection andhemost asis and therefore minimal need for exchange of instruments during the procedure with decreased operating time as a result [8].
• Although coagulation with ultrasonic dissection seems slower than with electrosurgery, its result in hemostasis is equal [14].
• In 98% of our patients a complete or almost complete adhesiolysis could be achieved• This 3.8% (4/105) incidence of perforations is low compared to the literature in which
visceral perforations during laparoscopic adhesiolysis have been reported in up to 25% of patients [22]. In these reports 40% of bowel perforations were not recognizedd uring the operation. These late perforations might have been causedby thermal lesions due to high temperature (570F) of the electrodissection device.
• In this series no late perforations were diagnosed, probably because of the lower temperature of the tip (180F) and the minimal lateral energy spread of the UD.
• Ultrasonic dissection has some concomitant advantages. In patients with a pacemaker the ultrasonic device can be used without additional security measures [24], it produces no smoke, and the lower temperature of the tip of ultrasonic dissection causes less charring and less tissue necrosis.
• A 5-mm UD will have an advantage in separating closely fixed organs and more precise dissection might be expected.

Safe laparoscopic adhesiolysis with optical access trocar and ultrasonic dissectionA prospective study
D. J. Swank,1 H. J. Bonjer,2 J. JeekelSurg Endosc (2002) 16: 1796–1801
• In conclusion, besides a carefully chosen entry site, the optical trocar identifies all layers of the abdominal wall and adherent organs and contrib utes to safe abdominal access in patients after multiple previous laparotomies.
• Ultrasonic dissection is a very feasible technique for laparoscopic adhesiolysis and might reduce the risk of bowel perforations by preventing the incidence of late (thermal) perforations.

Small bowel obstructionLaparoscopic approachF. Agresta,1 A. Piazza,
Surg Endosc (2000) 14: 154–156
• Surgical technique and instruments. The patient should be placed on a OR table which offers the full range of tilt, as extreme positions may be necessary. Their arms must be by their side to allow the surgical team ample room, and at least two movable video monitors are also required to provide a better view of the operative theatre.
• We have provided these general rules from our experience with the laparoscopic approach to SBO in 63 of 136 patients. Our overall success with laparoscopic treatments has been 82.5%, with a diagnostic accuracy of 92%. If we take into consideration only the cases of chronic SBO, the diagnostic accuracy is 100% and the treatment capacity reaches 97.2%. Therefore, in patients with partial and intermittent small bowel obstruction, the causes of SBO are mostly simple bands that can be easily lysed, and the possibility of facing a compromized bowel is almost absent.

Laparoscopic adhesiolysis for recurrent small bowelobstruction: long-term follow-up
Yoshiaki Sato, MD,Endoscopy 0016-5107/2001/
• Elective laparoscopy was performed with the patient in the supine position under general anesthesia.7-11 The surgeon stood on the left side of the patient. Videomonitors were placed at the head of the table if the previous operation was in the upper abdomen or at the foot if in the lower abdomen.
• The abdomen was punctured away from all scars with a Veres needle, and the syringe test was performed to confirm that the tip of the needle was not located in a vessel or intestines as follows: normal saline solution (5 mL) was injected through the Veres needle. If the saline solution entered the peritoneal cavity, it could not be reaspirated. If the saline solution was reaspirated, it signified that the tip of the Veres needle was in a closed cavity or newly formed space.
• A pneumoperitoneum was established by insufflation of carbon dioxide. The intra-abdominal pressure was monitored. The first trocar was inserted in an area without adhesions as determined by blind exploration with a 23-gauge needle. The remaining trocars were inserted under direct vision in areas devoid of adhesions.
• The pathogenic adhesions were identified and lysed with scissors or forceps. To minimize the risk of intestinal injury, electrosurgical current was not used for dissection.12
• In patients with dense adhesions, especially when there was a convoluted mass of adherent bowel, the operation was converted to a laparotomy.

Laparoscopic adhesiolysis for recurrent small bowelobstruction: long-term follow-up
Yoshiaki Sato, MD,Endoscopy 0016-5107/2001/
• Conversion to laparotomy was performed for intestinal perforation or the presence of dense adhesions, the latter being the most common cause of conversion to laparotomy.2-4
• Adhesions between the small intestines and the abdominal wall were lysed with scissors and forceps close to the abdominal wall.
• Electrosurgical current was used only for hematostatis. • Use of the Veres needle and blind insertion of the first trocar in patients with
an acute small bowel obstruction and bowel distention are associated with an increased risk of bowel injury.2-4
• Although the initial trocar was blindly inserted after the establishment of pneumoperitoneum with a Veres needle, there were no instances of bowel injury. It is our belief that it is safe to use the blind technique if the bowel is adequately decompressed before surgery.
• However, it is important to confirm the position of the needle using the syringe test and to monitor the intra-abdominal pressure during insertion of the first trocar.

Laparoscopic management of acute small bowel obstructionB. Kirshtein1 , A. Roy-Shapira1, L. Lantsberg1, E. Avinoach1 and S. Mizrahi1
Surgical Endoscopy© Springer-Verlag 2005
• The patient was placed on an electrically controlled table with both arms along the body. One monitor was placed at the caudal end of the table and the second on the patients right side.
• Either the Hasson technique or a Veress needle was used to establish the pneumoperitoneum depending on the individual surgeons preference. In either case, the initial port was placed as far away as possible from previous scars. If a Veress needle was used, it was usually inserted in the left upper quadrant. A periumbilical location was chosen in cases of virgin abdomen.
• Pressures were kept between 10 and 15 mmHg; lower pressures were used with sicker patients. A 45? side-view 10-mm telescope was preferred. After thorough examination of the peritoneal cavity, additional 5- or 10-mm ports were inserted under direct vision. The location of the additional ports depended on the operative findings. As required, the camera was repositioned to enable the viewpoint to be changed for the release of adhesions.
• Using a pair of atraumatic laparoscopic forceps, the surgeon followed the distended loops of bowel, in an attempt to identify the zone of transition from dilated to collapsed loops. This maneuver requires patience and the use of both hands.
• If the zone of transition could not be clearly identified, laparoscopy was aborted and the operation converted to a midline laparotomy.
• Adhesions were usually lysed with scissors; occasionally, bipolar coagulation was used for strands of omentum. We only lysed the band causing the obstruction or adhesions that obstructed the view. No attempt was made to lyse all adhesions present.
• If there were signs of strangulation, we observed the released loop of bowel for 5 min for return of color and peristalsis. When there was doubt about the viability, a second-look laparoscopy was scheduled in 24-36 h.
• Whenever it was necessary to resect a loop of bowel, a small, transverse target incision was made, and the resection and anastomosis were performed outside the abdomen.

Laparoscopic management of acute small bowel obstructionB. Kirshtein1 , A. Roy-Shapira1, L. Lantsberg1, E. Avinoach1 and S. Mizrahi1
Surgical Endoscopy© Springer-Verlag 2005
• As we have demonstrated in this series, the single band can often be lysed using minimally invasive methods. Multiple dense adhesions, which are difficult to release laparoscopically, are present after pelvic surgery. Due to the reduced posterior view and the small closed pelvic cavity, adhesiolysis by laparoscopy may be difficult and conversion may be necessary.
• A potential problem in operating on patients with adhesions is that the new operation causes even more adhesions. Indeed, every surgeon has encountered patients who have been operated on a number of times for SBO caused by adhesions. Each additional operation is more difficult and more dangerous than the previous one. Laparoscopy is thought to induce fewer postoperative adhesions than laparotomy [7, 16] and therefore appears to be an attractive alternative to laparotomy for the treatment of this type of patient.
• In most cases, the Veress needle was inserted in the left hypochondrium to initiate the pneumoperitoneum. The first trocar was placed as far as possible from the site of the previous operation. Franklin et al. [6] have routinely used this technique without complications. Caprini et al. have used ultrasound mapping of the adhesions as a way of avoiding the complications of Veress needle puncture [4]. Most authors recommend mandatory open insertion of the initial trocar [2, 8, 9, 15] as a means of preventing small bowel injury.

Laparoscopic management of acute small bowel obstructionB. Kirshtein1 , A. Roy-Shapira1, L. Lantsberg1, E. Avinoach1 and S. Mizrahi1
Surgical Endoscopy© Springer-Verlag 2005
• One of the problems with emergency laparoscopy for SBO is that it is difficult to find the site of the obstruction in the presence of distended bowel loops. Tilting the operating table and changing the scope port enables visualization from different angles, especially in the pelvis or right lower quadrant. If the transitional point is not found, conversion should be performed for formal bowel exploration.
• Safety has been a primary concern for surgeons performing laparoscopy in cases of acute SBO. Patients with bowel distension associated with obstruction are prone to perforation.
• We recommend beginning the bowel exploration from the collapsed are loops, as described by Bailey et al. [2], as a way of preventing incidental bowel injury.
• The need for enterotomy can be reduced if meticulous care is taken in the use of atraumatic graspers only and if the manipulation of friable, distended bowel is minimized by handling the mesentery whenever possible.
• The ability to work with a different instrument in each hand - a grasper for bowel traction and a pair of scissors for the division of adhesions, or two graspers for bowel exploration - is an important skill for the operating surgeon.
• Maintaining a low threshold for conversion in cases of severe dense, extensive adhesions or when pelvic adhesions are found will further decrease the risk of bowel injury. It is our policy not to persevere in this venture for hours but rather to convert readily to laparotomy.
• In cases of iatrogenic perforation and minor contamination with bowel contents in the presence of minimally dilated loops, laparoscopic closure can be performed.

Laparoscopic management of acute small bowel obstructionExperience from a Saudi teaching hospital
A. A. Al-MulhimSurg Endosc (2000) 14: 157–160
• What then are the possible safeguards? • We believe that positioning the patient on an electrically
controlled table with arms on the side is crucial because this spares extra space for the surgeon and assistants.
• In case of previous abdominal surgery, the choice of left hypochondrium for Veress needle insertion is preferable because adhesions usually are distant from this area, although alternative sites may be used as indicated.
• The use of 10-mm rather than the 5-mm instruments makes handling the distended bowel safer, and the use of active electrode monitoring to avert thermal injury to the bowel from monopolar electrosurgery may eliminate the risk of perforation [19].

Laparoscopic management of acute small-bowel obstructionI. M. Ibrahim, F. Wolodiger, B. Sussman, M. Kahn, F. Silvestri, A. Sabar
Surg Endosc (1996) 10: 1012–1015
1. Although Franklin et al. [3] used a Veress needle successfully to initiate pneumoperitoneum, we feel that open peritoneoscopy (initial trocar insertion) is mandatory.
• The pattern of intraabdominal adhesions is unpredictable. Blind insertion of a Veress needle or trocar into the abdomen is in our opinion dangerous, especially in the presence of distended bowel.
• Identifying the peritoneum before inserting a trocar is crucial to avoid smallbowel injury. All subsequent trocars should be inserted under direct vision. Obstructed bowel is distended, rigid, and easily traumatized.
2. Bimanual manipulation of the bowel is important. Running the bowel (especially when distended) can be taxing and frustrating. The surgeon must be comfortable.
• Therefore, the patient’s arms are tucked in to give the surgeon and assistant ample room. Furthermore, two movable video monitors should be used so that the surgeon, the scope, and the monitor are in a straight line for optimal intraabdominal manipulation.
• In addition the OR table should have the full range of tilt as extreme positions may be necessary.

Laparoscopic management of acute small-bowel obstructionI. M. Ibrahim, F. Wolodiger, B. Sussman, M. Kahn, F. Silvestri, A. Sabar
Surg Endosc (1996) 10: 1012–1015
3. Edematous and dilated bowel is prone to perforation from small blunt instruments. It should not be grasped by small instruments. Larger 10-mm instruments are preferable.
• Grasping the mesentery in order to manipulate the bowel decreases the likelihood of direct trauma.
4. The site of obstruction may be obscured by dilated loops of small bowel. In addition to tilting the OR table, changing the scope port is crucial at times. This allows visualization from different angles, especially in the pelvis or right lower quadrant.
5. In the virgin abdomen it is not enough to lyse bands, adhesive or otherwise. The cause of adhesions should be sought.
• In one of our cases, not satisfied with simple lysis, we followed the band to its insertion into the small bowel and a Meckel’s diverticulum was discovered.
6. Malignant adhesions are difficult to handle laparoscopically. The transition zone is not clear and the bowel is studded with metastases, dilated and edematous in multiple areas. Therefore, our recommendation is that the presence of malignant adhesions mandates immediate conversion to laparotomy.

Laparoscopic management of mechanical small bowel obstructionAre there predictors of success or failure?
M. Suter, P. Zermatten, N. Halkic, O. Martinet, V. BettschartSurg Endosc (2000) 14: 478–483
• In any case, the first trocar or the Veress needle always was placed in an area without former surgical incision, and very often in the left upper quadrant.
• Additional trocars (5 or 10 mm) then were placed according to intra-abdominal status and location of adhesions, to provide for a good triangulation between the instruments and to allow for an optimal placement of the optic.
• The small bowel was followed proximally starting from the ileocecal junction whenever possible. • Care was taken to manipulate the bowel gently and to avoid holding the bowel itself, but rather to grasp the
mesentery. • If a band was found that clearly was responsible for the obstruction, it was cut with scissors, sometimes after
bipolar coagulation. We did not systematically look for a second band, especially if relief of the obstacle and progression of bowel content could be demonstrated clearly.
• When multiple adhesions were found, they were freed as completely as possible. The small bowel then was examined on its entire length until the operating surgeon was convinced that the obstruction was relieved.
• If the cause of the obstruction could not be demonstrated clearly, or if division of adhesions was deemed too risky, especially when the bowel was very distended, the procedure was converted to laparotomy.
• Conversion was the rule also if accidental bowel perforation occurred with gross peritoneal contamination, in case of bowel necrosis, or if a tumor was found.
• However, small perforations with only minor leakage of intestinal content or seromuscular tears were sutured laparoscopically. The nasogastric tube was left in place at the end of the procedure, and removed according to clinical evolution.
• When the Veress needle was used, the site planned for trocar placement always was checked with needle punctures before the trocar was inserted.
• In these cases, the first trocar always was a so-called “security-trocar” (Surgiport®, USSC), which somehow prevents accidental puncture of intra-abdominal organs once the peritoneum is entered, but does not completely rule out iatrogenic perforation.

Laparoscopic management of mechanical small bowel obstructionAre there predictors of success or failure?
M. Suter, P. Zermatten, N. Halkic, O. Martinet, V. BettschartSurg Endosc (2000) 14: 478–483
• For the laparoscopic approach of SBO, proper installation of the patient and the equipment are important. Both arms must be placed along the patient and, ideally, two monitors should be available. In this way, the surgical team can move around the patient according to the operative findings. Tilting of the operating table can be useful for adequate exposure.
• An open technique must be used to create the pneumoperitoneum. The trocars must be placed in rela- tion to previous incisions, and according to the position of the adhesions to be divided.
• Manipulation of the distended bowel with atraumatic forceps must be very cautious and limited.• A small bowel diameter exceeding 4 cm, as seen on the preoperative plain abdominal film,
predicted an increased risk of conversion in this study. This is not surprising, because the working space in the abdominal cavity is considerably reduced as dilation of the intestinal loops increases.
• Additionally, intestinal fragility increases with distension and makes accidental perforation more likely.
• Others consider only patients with moderate intestinal distension as candidates for laparoscopy [6, 8, 12, 20].
• In the current study, 24 patients with a small bowel diameter exceeding 4 cm, including 11 with a diameter exceeding 5 cm, have been successfully treated without conversion.
• On the basis of these results, we still consider laparoscopy in patients with important dilation, but set a lower threshold for conversion.

Laparoscopic Management of Small BowelObstruction: Indications and Outcome
Enrique Luque-de Ledn, M.D., Altjandro Metzger, M.D., Gregory G. Tsotos, M.D.,J GASTROINTEST SURG 1998;2:132-140.)
• Patients were placed in the supine position with abducted arms and supports mounted to allow safe tilting and lateral rotation of the operating table.
• Two video monitors were used; the video monitor to the patient’s right was positioned inferiorly at the level of the hip and the monitor to the left positioned superiorly at the level of the shoulder (Fig. 2).
• This positioning forms a plane parallel to the root of the small bowel mesentery and allows the operating surgeon to look and work in the same direction as the camera orientation.
• The configuration of the operating room arrangement was flexible to permit modifications during the operation.
• Patients were prepared and draped in a way that allowed conversion to an open procedure when necessary.
• All interventions were performed under general endotracheal anesthesia with a nasogastric tube and urinary catheter in place.
• Because nitrous oxide as an anesthetic gas has been found to produce bowel dilatation, its use was specifically avoided in most patients.

Laparoscopic Management of Small BowelObstruction: Indications and Outcome
Enrique Luque-de Ledn, M.D., Altjandro Metzger, M.D., Gregory G. Tsotos, M.D.,J GASTROINTEST SURG 1998;2:132-140.)
• A pneumoperitoneum (15 cm HzO) was established using an open technique with a modified Hasson-type4 balloon cannula (Origin Medsystems Inc., Menlo Park, Calif.) inserted via a 1.5 cm periumbilical vertical incision. A 30-degree angled-view laparoscope was used, and twoadditional 5 mm trocars, introduced under direct vision, were usually placed in the right upper and left lower quadrants (see Fig. 2). A fourth or rarely a fifth trocar was required to allow better retraction, improve visualization, or facilitate intraperitoneal adhesiolysis
• in a few cases. Adhesions to the anterior abdominal wall were dissected using scissors, electrocautery hook, or blunt avulsion and the operation proceeded until complete visualization of the small bowel could be obtained.
• Evaluation of the entire jejunoileum was attempted in a systematic fashion starting at the ileocecal junction, looking at the right (lower) monitor, with the patient in a Trendelenburg position. The bowel was carefully inspected and systematically “run” in a retrograde fashion with a “hand-to-hand” technique, which involved grasping the bowel by its antimesenteric border alternately between two large, atraumatic graspers. Extreme care was necessary while “running” the acutely obstructed bowel because traumatic iatrogenie enterotomies can occur (see below).
• Inspection was facilitated by tilting and rotating the operating table. As the proximal jejunum was approached, the patient was placed in a reverse Trendelenburg position, and visualization shifted to the left-sided (upper) monitor.
• We considered this systematic exploration of the entire jejtmoileum an essential part of the procedure such that when complete inspection of the small bowel was not feasible, conversion to an open procedure was strongly considered.
• Use of a 5 mm laparoscope placed through one of the lateral 5 mm trocars was often necessary to obtain a better view of certain regions.
• When adhesions or obstructing bands were encountered, they were usually lysed with scissors, thereby avoiding potential thermal injury to adjacent bowel.

Laparoscopic Management of Small BowelObstruction: Indications and Outcome
Enrique Luque-de Ledn, M.D., Altjandro Metzger, M.D., Gregory G. Tsotos, M.D.,J GASTROINTEST SURG 1998;2:132-140.)

Laparoscopic Management of Small BowelObstruction: Indications and Outcome
Enrique Luque-de Ledn, M.D., Altjandro Metzger, M.D., Gregory G. Tsotos, M.D.,J GASTROINTEST SURG 1998;2:132-140.)
• As with the open operative approach for SBO, when a point of obstruction was not clearly identified, lysis continued until all suspicious adhesions or bands responsible for the symptomatology were dissected.
• Similarly, we evaluated the entire jejunoileum, even if a convincing obstruction was found in the ileum.
• Abnormalities requiring bowel resection or stricturoplasty prompted performance of laparoscopicassisted procedures. These were carried out by removing the 10 mm laparoscope and placing a 5 mm laparoscope in another port. The abnormal bowel was then grabbed with a Babcock clamp placed through the 10 mm periumbilical port and pulled through the umbilical incision; the incision was enlarged just enough (usually 2 to 3 cm) to allow exteriorization and extracorporeal repair of the bowel (Fig. 3).
• The bowel was then returned to the abdominal cavity, the fascial defect closed or occluded with the balloon trocar, and the pneumoperitoneum reestablished so that a final inspection could be performed. In patients in whom conversion to laparotomy was deemed necessary, a midline incision was usually performed.

Laparoscopic Management of Small BowelObstruction: Indications and Outcome
Enrique Luque-de Ledn, M.D., Altjandro Metzger, M.D., Gregory G. Tsotos, M.D.,J GASTROINTEST SURG 1998;2:132-140.)
• Because of dilated and fragile thin-walled bowel, the risk of traumatic iatrogenic enterotomies is increased during both trocar insertion and bowel manipulation.
• For these reasons and because of fear of intraperitoneal adhesions fixing segments of bowel to the undersurface of the abdominal wall, we strongly believe that access into the peritoneal cavity to establish the pneumoperitoneum should be obtained by an open, Hasson-type approach.4 We prefer a vertical periumbilical incision because this location is optimal both for intraperitoneal inspection during evaluation of the bowel and for potential laparoscopic-assiste exteriorization of bowel for extracorporeal resection, lysis of difficult adhesions between bowel loops, or stricturoplasty. In addition, if conversion to open celiotomy is necessary, a midline extension of the original periumbilical incision generally provides the best operative exposure. If appropriate access cannot be obtained because of adhesions from a previous midline incision, one can attempt to gain access laterally, but again an open approach with full visualization seems prudent.

Laparoscopic Management of Small BowelObstruction: Indications and Outcome
Enrique Luque-de Ledn, M.D., Altjandro Metzger, M.D., Gregory G. Tsotos, M.D.,J GASTROINTEST SURG 1998;2:132-140.)
• Overzealous retraction of thin-walled small bowel fixed intraperitoneally during manipulation may also lead to iatrogenic enterotomies as occurred in three of our patients. The incidence of iatrogenic enterotomies in other reported series has ranged from 3 % to 2 1% .10J2J5,17,18,20
• Nontraumatic bowel clamps rather than the “dissecting” graspers commonly used during laparoscopic cholecystectomy are suggested.
• In addition, when “running” the bowel between the two manipulating bowel clamps, both clamps should remain in view at all times. When one clamp leaves the visual field, it is difficult to appreciate the amount of traction being applied; also, if an enterotomy should occur, it may not be appreciated. One of our patients was readmitted several weeks postoperatively with an intraperitoneal abscess. He had undergone an extensive laparoscopic adhesiolysis, and presumably a small enterotomy was made that we did not recognize.
• Repair of an iatrogenic enterotomy does not necessarily require conversion to open celiotomy and can be accomplished either by intracorporeal suturing’* or by extracorporeal repair by exteriorizing the involved bowel.