Kidney and Male GU 2010.3
description
Transcript of Kidney and Male GU 2010.3

Kidney and Male GU 2010.3
Renal Vasculitis
Prostatic carcinoma

Vasculitis
Inflammation and necrosis of blood vessels
Capillaries -> Aorta

Examples of Vasculitis
• Large blood vessels – Giant cell (Temporal) Arteritis
• Medium sized vessels – Polyarteritis Nodosa
• Small vessel vasculitis– Capillaries, venules, arterioles +/- small arteries– Systemic or one site only (skin, renal glomeruli)

Vasculitis

Vasculitis - artery in Polyarteritis Nodosa
Lumen
Inflammation of artery wall

Glomerulus in vasculitis: crescents, necrosis
• Crescent around glomerulus
• Necrosis and small crescent
GlomCRESCENT
Nec
Cres

Typical of small vessel vasculitis in kidney
• Crescent: proliferation of cells inside Bowman’s capsule - blocks urinary space
• Necrosis and crescent
NCr
Cr

Vasculitis: Clinical, Serology
• Acute renal failure, haematuria, proteinuria• Systemic signs: include rash, arthralgias,
respiratory, neuromuscular symptoms• Duration of illness variable• ANCA (MPO, PR3) • (ANA, anti-GBM antibodies)

Anti-neutrophil cytoplasmic antibodies (ANCA)
• Serum antibodies to enzymes in neutrophil granules, monocyte lysosomes
• Immunofluorescence: Cytoplasmic or Perinuclear
• P-ANCA (anti-myeloperoxidase) in 80% of micro polyangiitis; more often indolent, renal limited
• C-ANCA (anti-proteinase 3) in 90% of Wegener’s
• Very useful in diagnosis; follow up of disease activity in Wegener’s with C-ANCA

Crescentic GN, vasculitis: Immunofluorescence findings
65% “pauci-immune” – pauci = few or no IC
• 20% immune complex
• 15% anti-GBM
. .. ,.

Immunofluorescence, EM
• Pauci-immune– (little / no immunofluorescent staining)– 90% of ANCA-assoc GN
• Electron microscopy– GBM breaks, fibrin (indicate structural damage)– Crescent cells (epithelial > macrophages/lymphocytes)– No EM deposits
. .. ,.

ANCA-Mediated Glomerulonephritis
• ANCA mediated, Pauci-immune Crescentic GN – Wegener’ granulomatosis – Microscopic polyangiitis– Churg-Strauss syndrome– Glomerular Pathology identical in all 3– Pathology at other sites? Respiratory tract? – MPA may have different stage lesions, more chronic– ANCA Type PR3 or MPO– Specific diagnosis needs careful correlation– If prompt treatment: 75% 5year survival

**
Scar (healing) after necrosis
Scar
Chronic, partly healed lesions in vasculitis
**Fibrocellular crescent

Necrosis and/or Crescents in GN • PAUCI-IMMUNE (90% are ANCA-positive)
– Microscopic polyangiitis, Wegener’s, Churg-Strauss, (drugs)
• IMMUNE COMPLEX (also Electron dense deposits)– Henoch-Schlonlein purpura– Cryoglobulinemia– Lupus nephritis– Bacterial endocarditis– Drug reaction– other
• ANTI-GBM DISEASE– Goodpasture’s syndrome and anti-GBM nephritis

R D
• 28 year old male• Acute renal failure• Pulmonary
haemorrhage
• N = Necrotic segment of glomerulus
N

R D
• Crescent, necrosis, fibrin
• Linear staining for IgG
• (EM: GBM breaks, fibrin)
Cres

And Your Diagnosis is: ANCA-mediated?
Immune complex?
Anti-GBM disease?


Prostate
• Surrounds bladder neck and urethra
• Normal weight = 20gm• Enlarged prostate
palpable on rectal examination
• CZ = Central zone• PZ = Peripheral zone

Benign prostatic hyperplasia
• Nodules around prostatic urethra
• 70% men over 60 yrs
• Growth requires dihydrotestosterone (Leydig cells), its metabolite 3-alpha-androstanediol & estrogens, which increase DHT receptor expression in prostatic tissue– DHT converted from testosterone by 5-alpha-reductase
• BPH not precancerous
• Clinical: – (None in most)
– Obstruction - compression of urethra -> frequency, nocturia, etc
– Dysuria because of UTI; acute retention

Benign prostatic hyperplasia
• Prostate = 40 - 200 gm• Nodules vary in size,
colour and texture• Nodules consist of
glands and / or fibromuscular stroma
NODULE

Benign prostatic hyperplasia
• Treatment– None
– Transurethral resection (TURP)
– (Open prostatectomy for very enlarged prostates)
– Medical treatment
• 5 alpha-reductase inhibitor, or
• Alpha adrenergic blockade

Carcinoma of the prostate• Commonest cancer in males
– Second leading cause of cancer deaths in men >50
– Incidence increases with age 70 >60 >50 yrs
– Afro-Americans at earlier age >US whites >Asians
• Endocrine, genetic & environmental factors– Androgens
– Susceptibility loci on chromosomes 1 and 10 (near PTEN)
– Incidence in Scandinavians > Japanese
– Animal fat in diet?
• Prostatic Intraepithelial Neoplasia (PIN) – in situ precursor of prostatic carcinoma

Clinical presentation
• Latent carcinoma - asymptomatic. Screening - PSA, PR +/- Transrectal Ultrasound, prostatic biopsies – PSA is a serine protease secreted by prostatic acinar cells, that liquifies the
ejaculate. A single serum PSA test is not fully sensitive or specific.
• Advanced carcinoma - obstruction or symptoms due to local extension or metastases e.g. bone pain.

PSA in prostatic acini

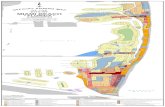
Preferential sites for prostatic lesions
• Transverse section
• BPH around prostatic
urethra *
• 70% of carcinomas are peripheral, and often posterior
*

Pathology• Peripheral in 70%, mostly posterior, palpable on PR
• Often not easily recognised on gross examination
• Invasion outside capsule; seminal vesicles, bladder
• Lymphatics; bloodstream, osteoblastic mets late
• Micro: Adenocarcinoma (different patterns = diff grades)– Grading: Gleason grade 1 ( virtually normal glands -> Gleason grade 5
(poorly differentiated).
– Gleason score: add two predominant grades
– Score = 6 predicts a good prognosis; 8-10 a poor prognosis
– Immunostaining: PSA+, loss of HMW keratin staining

Prostatic carcinoma - microscopic
Gleason Grade 3
Gleason G 5

Capsular & perineural invasion (L) and bone metastasis (R)
Nerve

Prostatic carcinoma stage, prognosis• Staging: clinical, PR, U/S, CT/MRI, bone scan,
pathological stage in prostatectomy– T1, T2 - both treated by radical prostatectomy or radiotherapy– T3 locally invasive - radiotherapy– T4 metastatic - hormonal therapy
• Prognosis: – Slow growing cancers– Stage and Gleason score– 90% 10 yr survival for T1, T2 – 10-40% for T4


![4- GU Onc351[1] Semester/Surgery/22- Common...Adrenal Tumors. Renal Tumors. Renal Tumors Benign tumours of the kidney are rare All renal neoplasms should be regarded as potentially](https://static.fdocuments.in/doc/165x107/5f0983b17e708231d4273048/4-gu-onc3511-semestersurgery22-common-adrenal-tumors-renal-tumors-renal.jpg)




![Ëf gu/kflnsfsf] aflif{s gu/ ljsf; of]hgfresungamun.gov.np/sites/resungamun.gov.np/files/final book7677.pdf · /];'Ëf gu/kflnsfsf] aflif{s gu/ ljsf; of]hgf -cf=j=@)&^÷ && sf nflu](https://static.fdocuments.in/doc/165x107/6080ec786385b40b254b254c/f-gukflnsfsf-aflifs-gu-ljsf-of-book7677pdf-f-gukflnsfsf-aflifs.jpg)