Kidney anatomy, physiology and disorders
-
Upload
university-of-mauritius -
Category
Health & Medicine
-
view
19.494 -
download
2
Transcript of Kidney anatomy, physiology and disorders

ANATOMY & PHYSIOLOGY OF KIDNEY & KIDNEY
DISORDERS

Presented by:
o Sameerah Firdaus BAUHADOOR
o Housna Nazifah KORUMTOLLEE
o Dr Shanoo SUROOWAN

The kidneys:An Excretory organ or a
Regulatory organ?!!!

The Kidneys- function
• The main purpose of the kidney is to separate urea, mineral salts, toxins, and other waste products from the blood.
• They also do the job of conserving water, salts, and electrolytes.
• At least one kidney must function properly for life to be maintained.

The Human Kidney
bean shaped, reddish brown organs.
about the size of your fist.
It measures 10-12 cm long.
covered by a tough
capsule of fibrous connective tissue- renal capsule
Adhering to the surface of each kidney-two layers of fat to help cushion them.

The Human Kidneys concaved side having a
depression where a renal artery enters, and a renal vein and a ureter exit the kidney.
located in the upper rear region of the abdominal cavity just above the waistline.
protected by the ribcage.
The renal cortex, the renal medulla and the renal pelvis - major regions of the kidney.
The left kidney lies slightly above the right kidney.

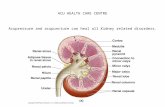
The Kidney Diagram

Kidneys and their structures
The Renal Arteries• transport oxygenated
blood from the heart and aorta to kidneys for filtration
The Renal Veins• Transport the filtered,
deoxygenated blood from kidneys to the posterior vena cava and finally the heart

Kidneys and their structures
Renal Capsule (inferior/superior)
• Outer membrane which encloses and protects kidneys against infections and trauma.
The Renal Cortex• Outer layer
(granulated) of the kidney that contains most of the nephrons.

Kidneys and their structures
Nephron• Most basic microscopic
structures of the kidneys
• Inside each kidney, there are about 1 million nephrons
• Physiological unit of the kidney used for filtration of blood, and reabsorption and secretion of materials

Kidneys and their structures
The Renal Medulla• Inner layer (radially striated) of the
kidney
• contains renal pyramids, renal papillae, renal columns, renal calyces (minor/major),renal pelvis and part of nephron, not located in the cortex
• Site for salt, water and urea absorption

Kidneys and their structures
The Renal Pyramid• Triangular shaped unit
in the medulla
• houses the loop of Henle and collecting duct of the nephron
The Renal Column• Area between the
pyramids, located in the medulla
• Used as a space for blood vessels

Kidneys and their structures
The Renal Papillae• The tips of the renal
pyramids • release urine into the
calyces
The Renal Calyces• Collecting sacs that
surround the renal papillae
• Transport urine from renal papillae to renal pelvis

Kidneys and their structure
The Renal Pelvis• Cavity which lies in
the centre of the kidney and which extends into the ureter
• Collects urine from all of the calyces in the kidney

Kidneys and their structures
The Ureters (right/left)• Tubes that transports
urine from the renal pelvis to the bladder
The Urinary Bladder• Hollow, expandable,
muscular organ located in the pelvic girdle
• Functions as a temporary reservoir for urine

The Kidney Nephron Diagram

The two types of Nephrons
Cortical•The loop of Henle does not extend past the cortex of the kidney.
Juxtamedullary•Loop of Henle extends past the cortex and into the medulla of the kidney.

Nephron structures and functions
Afferent Arteriole• Transport arterial
blood to glomerulus for filtration
Efferent Arteriole• Transports filtered
blood from glomerulus through the peritubular capillaries and the vasa recta, and to the kidney venous system

Nephron structures and functions Glomerulus• The site for blood
filtration
• operates as a nonspecific filter - removes both useful and non-useful material
• the product of the glomerulus – filtrate
Bowman’s Capsule• A sac that encloses
glomerulus • transfers filtrate from
the glomerulus to the Proximal Convoluted Tubule (PCT)

Nephron structures and functions
Proximal Convoluted Tubule (PCT)• A thick, constantly active segment of the
nephron
• that reabsorbs most of the useful substances of the filtrate: sodium (65%), water (65%), bicarbonate (90%), chloride (50%), glucose (nearly 100%)
• The primary site for secretion (elimination) of drugs, waste and hydrogen ions.

Nephron structures and functions
The loop of Henle• U-shaped tube that consists
of a descending limb and an ascending limb.
• begins in the cortex, receiving filtrate from the PCT, extends into the medulla, and then returns to the cortex to empty into the distal convoluted tubule(DCT).
• Its primary role is to concentrate the salt in the interstitium, the tissue surrounding the loop.

Nephron structures and functions
Decending Limb of the Loop of Henle• A part of the counter current multiplier
• fully permeable to water and completely impermeable to solutes (salt particles)
• receives filtrate from the PCT, allows water to be absorbed and passes “salty” filtrate to the next segment.
“Saves water and passes the salt”

Nephron structures and functions
Ascending Limb of the loop of Henle• a part of the counter current multiplier
• impermeable to water and actively transports (reabsorbs) salt (NaCl) to the interstitial fluid of the pyramids in the medulla.
“Saves salt and passes the water.”
• the passing filtrate becomes dilute and the interstitium becomes hyperosmotic

Nephron structures and functions
Distal Convoluted Tubule (DCT)
• Variably active portion of the nephron
• receives dilute fluid from the ascending limb of the loop of Henle

Nephron structures and functions
Collecting Duct• variably active
portion of the Nephron
• receives fluid from the DCT
• The last segment to save water for the body

Nephron structures and functions
Peritubular Capillaries• transport reabsorbed
materials from the PCT and DCT into kidney veins and eventually back into the general circulation
• help complete the conservation process (reabsorption) that takes place in the kidney

PHYSIOLOGY

Kidney nephronThe nephrons are the functional units of thekidney and are the site of:
1. Filtration of blood 2. Maintainance of Renal blood pressure3. Formation of urine4. Counter current mechanism5. Acid-base balance6. Regulation of electrolytes7. Reabsorption of materials8. Secretion of materials( production of hormones)9. Excretion of wastes

1. Filtration of BloodThe glomerulus is the site of filtration of blood.

The Bowman’s capsule (basement membrane + podocytes)
• filters blood,
• hold back large molecules such as proteins,
• passes through small molecules such as water, salts, and sugar
• Aids in the formation of urine


PODOCYTES:• Also known as visceral epithelial cells
• Cells in the Bowman's capsule in the kidneys that wrap around the capillaries of the glomerulus leaving slits between them.
• They are involved in regulation of glomerular filtration rate (GFR). When podocytes contract, they cause closure of filtration slits. This decreases the GFR by reducing the surface area available for filtration.

2. 2. Maintainance of Renal Blood Pressure
• This process is achieved by the Juxtaglomerular apparatus.

The three cellular components of the apparatusare the
1. juxtaglomerular cells2. macula densa,3. extraglomerular mesangial cells, and

The Juxtaglomerular Apparatus

Function of the JC cells
1. Release of ReninStimulus : Low blood pressureAction : Release of ReninAngiotensin Angiotensin I Angiotensin II
Angiotensin II It acts as a vasoconstrictor to raise blood pressure.
It stimulates the release of aldosterone hormone from the adrenal cortex.

22. Release of Aldosterone hormone
It stimulates the DCT to reabsorb salt.

3. 3. Reabsorption of salt (NaCl)
• Salt reabsorbtion induces the movement of water to the blood by osmosis thereby raising the blood volume and hence increasing the blood pressure.

Function of the Macula Densa Cells
• It monitors the salt content of the blood.
• If concentration of salt is raised, the macula densa cells inhibit the release of renin from the JC cells.
• No release of renin No angiotensin II , No aldosterone . Blood pressure decreases until it is sent back to normal.

Function of the extra glomerular mesangial cells
• It secretes erythropoietin
• Erythropoietin is a glycoprotein hormone which controls erythropoiesis or red blood cell production.


OSMOLARITY:Osmolarity is the measure of soluteconcentration, defined as the number ofosmoles(Osm) of solute per liter (L) of solution(osmol/L or Osm/L).
NOTE: Molarity measures the number of moles of solute per unit volume of solution,

3.Formation of urine
• Takes place in 3 main steps;1. Ultrafiltration– seeping of fluid from glomerular capillaries to
the Bowman’s capsule along with useful substances (e.g. glucose, vitamins ,amino acids)
2. Reabsorption along the nephron – PCT; selective reabsorption of useful substances – LOH, DCT and CD Reabsorption of water and salts
3. Secretion from blood to tubule

4.Counter Current Multiplier
• A system of limbs running in opposite directions• Consists of;
Descending limb andAscending limb of theLoop of Henle.
• Helps in the absorption of water from fluid found in the LOH

Counter current MultiplierInterstitial fluid should be hypertonic for water to be
reabsorbed

Counter current multiplierNa+ is actively pumped out of the ascending limb into the interstitial fluid.• Cl- follows Na+ passively• Increases the Na+ and Cl- of interstitial fluid by about 4 times.• Water seeps out of the of the descending limb into the interstitial fluid by osmosis

Counter current multipier
• Down the descending limb of the LOH, fluid becomes more concentrated due to loss of water.
• Na+ and Cl- concentration increase as fluid turns and heads on towards the ascending limb.
• All the way up osmotic pressure of fluid in LOH is almost equal to the osmotic pressure in interstitial fluid.
• The fluid again passes through hypertonic interstitial fluid loosing water again until into the collecting duct.
• The final product in the CD is urine!!!!

5. Regulation of electrolytes
Electrolytes are substances that become ions insolution and acquire the capacity to conductelectricity.
The primary ions of electrolytes are sodium (Na+),potassium(K+), calcium (Ca2+), magnesium (Mg2+),chloride (Cl−), hydrogen phosphate (HPO4
2−), and
hydrogen carbonate (HCO3−).

Maintainance of an electrolyte balance occursso that the osmolarity of both the body fluids and theurine is the same.
Maximum electrolyte balance is maintained by
the release of hormones which are going to
trigger the reabsorption of certain ions thereby
preventing electrolyte disbalances.

ADH• Also known as vasopressin• Released by hypothalamusStimulus: Low blood level
• Prevents the production of dilute urine • Helps in reabsorption of water in kidneys• Maintains osmolarity of plasma levels normal

6. Acid-base balance
• Forms part of human homeostasis• Is important to maintain cellular stability• Alterations in the acid-base balance are resisted by
extracellular and intracellular chemical buffers and by respiratory and renal regulation.
In acid-base balance, the kidney is responsiblefor 2 major activities:• Reabsorption of filtered bicarbonate: 4,000 to 5,000
mmol/day • Excretion of the fixed acids (acid anion and
associated H+): about 1 mmol/kg/day.


Formation of H+ Secretion from the organic acid and base secretory
system (uric acid, antibiotics and diuretics). H2CO3 H+ + HCO3
-
In case of high H+
H+ is bound to ammonia, phosphate and bicarbonate to form NH4
+, H2PO4-, CO2 and H2O.

7. Reabsorption of materials
Nutrients such as glucose, amino acidsand other metabolites are reabsorbed in the medulla such that the body does notlose important nutrients.
Location: convoluted proximal tubulesituated in the cortex of the kidney

8. Secretion of substances
Release of several substances occur inorder to aid in the functions of the kidney:
1. Calcitriol (activated form of vitamin D promotes intestinal absorption of calcium and the renal reabsorption of phosphate)
2. renin,
3. Erythropoietin

4. ADH
5. Prostaglandins
6. Kinins
7. 1,25-dihydroxyvitamin D3

9. Excretion of wastes
The kidney is also involved in theexcretion of wastes such as:1. Urea( from protein metabolism)
2. Uric acid
( from nucleic acid metabolism)

3. Creatinine (from metabolic breakdown of creatine phosphate)
4. End-products of Hb metabolism
5. Metabolites of hormones
6. Foreign substances: drugs, pesticides, other chemicals ingested in food

Finding the amount of a substance excreted per unit time
Given • Amount filtered in gNaCl/day• Amount reasorbed in gNaCl/day• Amount excreted in gNaCl/day
Amount excreted = Amount filtered – Amount reabsorbed

Plasma clearance rate
It is defined of the amount of blood cleaned of asubstance per unit time.
Clearance is a function of glomerular filtration,secretion from the peritubular capillaries to thenephron, and reabsorption from the nephron backto the peritubular capillaries.

Finding plasma clearance rate
C = V x U/P
C= plasma clearance rate in ml/minV=urine production rate in ml/minU=concentration of a substance in urine in mg/mlP=concentration of a substance in plasma in mg/ml
Units of plasma clearance rate: ml/min

Question
Assume urine production rate (V) is 2 ml/min.
If after a dose of inulin, a man’s urine has 30mg/ml and his plasma has 0.5 mg/ml of thissubstance, what is the inulin clearance rate?

Answer
Inulin clearance rate = 120ml/min.

RENAL PATHOLOGY

Kidney disorders• Are diseases that affect the kidney.
• Usually affects both kidneys.
• The kidneys ability to remove waste products and control water balance is severely affected.
• This causes an accumulation of waste products and fluids causing severe uremia.
• Uremia=kidney failure

Causes
Renal pathologies
Hereditary disorders;
inflammatory &non-inflammatory
Other causes
Congenital disease
Kidney stones
Renal tumours

Signs of kidney problems!!!
• proteins, blood or glucose in urine
• The GFR is usually assessed to confirm kidney disease; determine amount of inulin excreted.
• A fall in GFR= kidney disease is obvious

Pathology
Polycystic kidney disease(PKD):
• Hereditary disease
• Caused by a mutation in the PKD(PKD1/PKD2) gene causing defects in the uptake of ca++, leads to formation of cysts.
• Kidney enlarges due to the presence of hundreds /thousands of renal cysts that can be up to 20 cm in diameter
• Causes uremia ,i.e. kidney failure

kidneys with cysts

Pathology
Kidney stones( renal calculi)• Urine becomes saturated with salts of
calcium, phosphate, oxalate, urate and other salts so its pH changes
• change in pH favors precipitation of the salts and hence formation of stones.
• Blood may be seen in urine=hematuria

Kidney tumors-dissection
tumour

Pathology
Urinary tract cancer
• Invades fats that surround the kidney.
• Symptoms: hematuria, pain.
• Surgical removal of kidney as treatment

Pathology
Nephrotic syndrome(Non-inflammatory)
• Loss of podocyte structure
• Large proteins can enter the renal corpuscle
• Increase in urinary protein secretion=proteinuria


Pathology
Alport’s syndrome(inflammatory)• Inflammation of glomerular
capillaries=glomerulonephritis
• Basement membrane becomes irregular in thickness and fails to serve as an effective filtration barrier to blood cells and proteins.

Pathology
Incontinence• caused by inability to control voluntary micturition
(releasing urine from the bladder).
• Causes: age, emotional disorders pregnancy, damage to the nervous system, stress, excessive laughing and coughing
• leads to wetting of clothing, discomfort and embarrassment

Treatment
Treatment
Drug therapy
Change in lifestyle;
exercise, diet, water intake
Dialysis therapy

Drug treatment
• Drug treatment very effective to relieve pain in difficult conditions such as renal calculi
• ROWATINEX, a common drug found in the pharmacy relaxes urinary tract spasm and allows the easy passage of kidney stones into urine

Dialysis therapy
• Dialysis is a process that artificially removes metabolic wastes from the blood in order to compensate for kidney (renal) failure.
• Most common type is homodialysis

Dialysis therapy

Purpose of homodialysis
• Allows patient to survive even though his 2 kidneys cannot filter blood
• Used to treat patient with ESRD(end stage renal disease), poisoning and overdose

REFERENCES• Grays anatomy
• Wikipedia
• http://www.cliffsnotes.com/study_guide/Anatomy-of-the-Kidneys
• http://www.comprehensive-kidney-facts.com/kidney-anatomy.htm
• http://www.biologymad.com/resources/kidney.swf

I am happy that now you know
more about me!!!

Questions?