Joel Marion -...
Transcript of Joel Marion -...
3
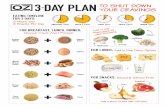
11 Flat Belly Foods That Crush Cravings
It’s no secret that overweight and obesity levels have been on the rise over the last several decades. In the United States alone, approximately 29% of 20- to 39-year olds, 37% of 40- to 59-year olds, and 31% of those aged 60+ years are obese.1 In a study jointly conducted in 2010, the International Association for the Study of Obesity (IASO) and the International Obesity Task Force (IOTF) estimated that approximately 1.5 BILLION people across the globe are overweight, with over 475 million obese adults.2
According to the World Health Organization (WHO), the prevalence of overweight and obesity has further increased since the IASO/IOTF report was published just a few short years ago. In fact, WHO reports that, in 2014, over 1.9 BILLION folks across the world were overweight, with over 600 million of those folks being classified as obese.3 That’s more than a 25% increase in obesity in less than 5 years. According to data from the National Health and Nutrition Examination Survey (NHANES), 2 out of every 3 adults in the United States are overweight or obese, and over one-third of the adult population is obese.4
Simply put, overweight and obesity are no secret, and yet the scientific community offers a simple explanation of their cause: Overweight and obesity are the result of an energy imbalance (i.e., calories in vs. calories out).5 Along that line of thinking, in order to lose weight, one must eat fewer calories than what s/he burns (i.e., negative energy balance) on a regular, consistent basis—a fundamental principle of metabolism and thermodynamics.6
As simple as that concept is, anyone who’s attempted to lose weight through a reduced-calorie diet can tell you that it’s not easy, and for the overwhelming majority of folks, not sustainable. In fact, researchers estimate that fewer than 25% of folks who lose weight are successfully able to keep it off for at least a year.7
4
The Role of SnackingA variety of dietary factors, including intake of energy drinks, sugar-sweetened beverages, and sports drinks, away-from-home eating, portion sizes, and snacking have been related to increases in calorie intake and the prevalence of obesity at various stages of life.8–15
While it’s often thought—perhaps mistakenly so—that lower meal frequencies are to blame for the increase in the population’s collective waist girth, it’s becoming readily apparent that increases in eating opportunities may be in part responsible for the rise in obesity. In fact, snacking, which is broadly defined as eating occasions different from main meals (e.g., breakfast, lunch, dinner/supper), has been commonly regarded as contributing to excess weight.16,17
Along these lines, multiple studies examining the eating behaviors and food choices of young adults and children have reported large increases in snacking frequency and higher contribution of snacking to total calorie intake.18,19 However, snacking is not just for kids.
As a matter of fact, research suggests that increases in eating opportunities are in large part responsible for increases in total calorie consumption among adults. That’s right, snacking—not portion size—is largely the driving factor behind overeating, overweight, and obesity.
Along these lines, researchers from the University of North Carolina set out to examine overall patterns of snacking, shifts in calorie intake from snacking, snacking occasions, and energy intake per snacking event over the course of the last 30 years. In addition, they also investigated shifts in snack foods and beverage sources, as well as the overall trends of the energy density of snacks and meals.20
What the researchers found was quite interesting:
• The number of snacking occasions increased;
5
• The contribution of snacks to total calorie intake increased; • The energy density of snacks also increased; and • Desserts contribute the highest percentage of calories to total energy intake,
and the researchers noted increases in the consumption of salty snacks (e.g., crackers, chips, popcorn, pretzels) and sugar-sweetened (e.g., soda, juice, sports drinks) beverages with subsequent decreases in fruit and dairy.
In another study conducted at the University of North Carolina, researchers found that, over the last 30 years, average daily total calorie intake has increased from 1,803 calories in 1977–78 to 2,374 calories in 2003–06, an increase of 570 calories. In the last decade alone, the average daily energy intake increased by 229 calories. As you likely already know, there has not been an increase in physical activity and energy expenditure to offset this 31.6% increase in calorie intake. In fact, as a population, people are moving less!
Although the energy density of food and drink, portion size, and the number of meals and snacks per day have all contributed to the increases in total calorie consumption, increases in the number of eating occasions (e.g., snacking) and in portion size have accounted for most of the change. In fact, in the last 10 years alone, increases in eating opportunities have accounted for 39 times the increase in calories compared to portion sizes.21
Snacking by the Numbers• 98% of children and 97% of adults snacked daily in 2006, compared to 74% and
71%, respectively, in 1977.• 579 calories adults consumed daily from snacks, 222 calories more than 1977.• 27% of a child’s total calories come from snacks.• 3 hours (children) and 3.5 hours (adults) between eating occasions, 1 hour less
than 1977.• 74% of Americans snack in the evening, 57% in the afternoon, and 45% in the
morning. • $63.7 billion was the revenue of the U.S. snack industry in 2010.
6
• Global snack sales totaled $374 billion annually ending March 2014, an increase of 2% year-over-year.
• Women consume more snacks than men. Nearly one in four women surveyed said they snack three to four times a day. A little less than one in five men do. Women are also more likely to snack while using the phone or tablets during their down time.
• Both men and women reported satisfying hunger and cravings as their top reason for snacking, but a greater share of women report snacking for stress relief, because of boredom, or as an indulgence.
• About 17% of people said they are snacking more than they were just one year ago.
• 25% of people who snack daily do so three to five times a day and 3% report that they are “always snacking.” About 8% say they “always” binge snack, and another 31% do so occasionally.
The Role of CravingsOf course, there are many factors that influence calorie intake and energy expenditure, and food intake is driven by much more than just physical energy needs. In other words, despite the fact that overweight and obese folks carry more than enough energy on them (in the form of stored body fat), they frequently still experience insatiable hunger and voracious appetite, as well as increased feelings of pleasure (though fleeting) when snacking or eating “junk foods.”22
Cravings are considered to be a component of the brain’s pleasure and reward response to food, and research has shown that reduced-calorie dieting generally increases the likelihood of food cravings.23 Having said that, it’s readily apparent that hunger and food reward centers in your brain play a substantial role in weight gain and weight regain. Along those lines, evidence suggests that some folks may be more predisposed than others to struggle with uncontrollable cravings and appetite.24–26
That said, you are not entirely to blame for excessive hunger, compulsive overeating,
7
and insatiable sugar cravings. Your body and physiology are working against you, and this will probably come as no surprise, food manufacturers are too. Yep, they have “cracked the code” of engineering food and beverages. They understand that a combination of certain ingredients in precise amounts can literally make food highly addictive and override the body’s ability to stop eating when full.
Hunger HormonesLeptin and ghrelin are two hormones that play a major role on food intake, hunger, and body weight. Leptin, a hormone produced by fat cells, is responsible for long-term regulation of calorie balance by suppressing hunger.27 In overweight and obese populations, we see a decrease in leptin sensitivity (i.e., leptin resistance). This decrease in leptin sensitivity leads to the inability to feel full even when calories are plentiful and fat stores are high.28
As an “energy-sensing” hormone, leptin levels plummet with decreasing caloric intake. In fact, research shows that leptin levels can drop, on average, by 43% after just one week of calorie restriction.29 What’s more, because fat cells are responsible for the secretion of leptin, when you lose fat, leptin levels also drop, as you have less of the very tissue that produces this hormone.30 What does this drop in leptin mean? It means an increase in appetite, hunger, and activity of food reward centers. In other words, you’re more hungry, rarely feel full, and food (especially “junk food”) is tastier than ever.
You may be starting to see the conundrum and how the body’s physiology is set up to work against weight loss efforts, but that’s just the beginning. Ghrelin is leptin’s counter hormone, and it is often referred to as the “hunger hormone.” Ghrelin is produced in the GI tract and functions as a signaling compound in the Central Nervous System (CNS).31 Ghrelin is released when the stomach is empty, and levels go down after eating (particularly after eating proteins and carbohydrates, highlighting a potential association between insulin and ghrelin).32 In addition to stimulating hunger,
8
ghrelin also “turns on” reward centers in the brain, increasing the pleasure and reward response to eating and reinforcing the consumption of rewarding, tasty food.33–35
Not surprisingly, studies also show that levels of ghrelin steadily increase with weight loss, a change that corresponds with the simultaneous drop in leptin levels. In that sense, these two hunger hormones work in tandem to combat starvation and weight loss. Simply put, your body is programmed to work against you and your quest of a leaner, sexier body.
In addition to leptin and ghrelin, there is a number of other hormonal regulators of appetite.36 For instance, in addition to ghrelin, neuropeptide Y (NPY) and agouti-related peptide (AgRP) stimulate food intake and weight gain. On the other hand, in addition to leptin, cholecystokinin (CCK), peptide YY (PYY, PP), oxyntomodulin, glucagon-like peptide-1 (GLP-1), gastric inhibitory peptide (GIP), insulin, and adiponectin (and possibly others) inhibit feeding and stimulate satiety, which is the set of biological processes that inhibits you from eating until your next meal. Satiety is also described as feeling full and satisfied, and along these lines, it’s a tremendously important variable to consider.
Serotonin Regulates Appetite and SatietySerotonin is a “feel-good” neurotransmitter that soothes, calms, and reduces anxiety, and it is heavily involved with food intake, including carbohydrate cravings. For instance, refined sugars and starches result in a rush of serotonin.37
Serotonin plays a crucial role in the regulation of appetite and satiety, as it acts in both the brain and the gut to induce feelings of fullness and satisfaction.38,39 In fact, serotonin works opposite of the hunger hormone ghrelin. That’s right, while high levels of ghrelin stimulate appetite, high levels of serotonin induce satiety and reduce appetite.
Along these lines, researchers conclude that there’s adequate evidence to suggest that eating to excess or for reasons other than to meet energy needs may be in part brought
9
on by a “serotonin hunger” in the brain.
“Serotonin hunger” seems to be most effectively satisfied by consuming carbohydrate-rich foods, which help (via insulin) increase brain levels of a compound called tryptophan—which converts to serotonin, leading to an increase in this “feel-good” neurotransmitter that signals satiety.40 Thus, folks tend to overeat high-carbohydrate foods not just to meet energy needs but rather to promote feelings of wellbeing. (Along these lines, it’s most likely NOT the turkey per se that’s making you drowsy after indulging in a Thanksgiving feast.)
Normal, healthy levels of serotonin lead to feelings of satisfaction and wellbeing, and as one might expect, low levels of serotonin are related to negative mood and reduced feelings of wellbeing. Thus, it should come as no surprise that when one is feeling sad or blue, the innate response is often to overeat sugary, carbohydrate-dense foods.41
Emotional Eating“Emotional eating” is defined as eating to relieve negative emotions or affect (e.g., unhappiness, anxiety, or anger), and stress has been well documented as a key driver of emotional eating.42 Emotional eaters typically consume more calories, they eat more frequently, and they opt for greater amounts of highly palatable, high-calorie, sweet, high-fat foods in response to emotional stress.43–46
It’s no secret that stress can be a “trigger” for overeating. In fact, research shows that around 70% of individuals increase their food intake during periods of stress.47,48 Females, overweight individuals, and folks who think about food or body weight obsessively are more likely to eat when stressed.49
As one might expect, research also shows that stress-induced eating typically involves a predisposition for high-sugar and high-fat foods, which are “comfort foods” known to provide strong rewarding effects and reinforce snacking.50
10
Studies have shown that emotional eaters may try to regulate the negative emotions caused by everyday life through eating behavior, and while their chosen “comfort foods” may provide short-term protection against stress, they also drive appetite for these unhealthy foods at the same time, which ups the risk of weight gain. The benefits on mood may be fleeting, but for most people, the short-lived feelings of wellbeing may be sufficient to promote repeated attempts to boost mood through stress eating patterns.51
This pattern of stress-induced, emotional eating creates a negative, vicious, perpetuating cycle of overeating and weight gain, followed by restriction, which again leads to overeating and weight gain.49,52,53
Previously, it was mentioned that serotonin plays an intricate role of feelings of wellbeing. Would it surprise you that serotonin is also closely linked to stress and emotional states like anxiety and arousal?54 Yep, serotonin attenuates stress, making the connection between emotional eating and serotonin levels even stronger.
Clearly, the odds are stacked against you—thanks both to our unchangeable biology and the purposeful engineering of addictive foods by big corporations. The good news is that there’s a solution. That’s right, you can manage your appetite. You can kick your sugar cravings to the curb. You can say goodbye to emotional and stress-induced eating. You can take control over your bad snacking habits.
And you can start by focusing on several key dietary factors that positively influence satiety, or feelings of fullness and satisfaction.
Protein. It has been well-established that among all three of the major macronutrients (e.g., protein, carbohydrate, fat), protein consistently exhibits the most pronounced effect on satiety and appetite control.55,56 High-protein meals boost satiety,57 and high-protein diets improve appetite control, as well as reduce daily food intake.58 In a recent
11
study published in the Nutrition Journal, researchers from the University of Missouri found that consuming higher protein, dairy-based snacks (e.g., yogurt) improved satiety, appetite control, and limited subsequent food intake when compared to higher fat and higher carbohydrate-based snacks.59
Fiber. Besides protein, dietary fiber is another food ingredient that has been shown to have a powerful effect on satiety. Fiber is thought to increase satiety in a number of ways, depending on the type of fiber, and relative to its ability to bulk foods, increase viscosity, gel in the stomach, increase gastric distention, slow the rate of gastric emptying, impact satiety hormones, and ferment in the gut (more on this later). What’s more, a diet rich in fiber is thought to promote satiety and weight management because it tends to contain foods that are low in energy density, which when eaten in the same volume (or more) as foods high in energy density are equally satiating despite providing fewer calories.60 Speaking of which…
Energy Density and Food Volume. Rather than the calorie content of food, the volume of food that is consumed at a meal appears to be an important factor that makes people feel full and stop eating.61 In fact, research strongly suggests that how much you eat daily is regulated by the weight of the food consumed rather than by a certain number of calories. Researchers from Penn State have posited that “energy density is a key determinant of energy intake in that cognitive, behavioral, and sensory cues related to the volume or weight of food consumed can interact with or override physiological cues associated with food intake.”62
Energy density is defined as the ratio of calories to the weight of food (i.e., calories per gram). Foods like oils, bacon, butter, cookies, crackers, junk food, fast food, etc., are generally considered “high-energy-dense” foods (i.e., 4 – 9 calories per gram by weight); on the contrary, nearly all fresh vegetables, many fruits, and broth-based soups are considered “low-energy-dense” foods (i.e., 0.0 – 1.5 calories per gram, by weight), as they tend to have a high water content and contain dietary fiber, two important factors reducing energy density.
12
Along those lines, researchers have found that when folks consume more low-energy-dense foods, they feel satisfied earlier and those feelings of fullness persist for relatively longer periods of time—despite reductions in calorie intake. In other words, diets rich in low-energy-dense foods like vegetables and moderate amounts of fruit allow folks to eat more total food, leading to greater feelings of satiety, all while reducing calorie intake.63
By definition, that’s eating more (overall food) and less (calories). Bingo!
A number of studies have demonstrated that diets rich in low-energy-dense foods promote satiety (i.e., feelings of fullness and satisfaction), reduce hunger, and decrease overall calorie intake.62–66 What’s more, long-term studies have shown that low-energy-dense diets also promote weight loss. In fact, studies lasting longer than 6 months show that folks who eat more low-energy-dense foods experience THREE TIMES greater weight loss than people who simply opt to reduce calories.67
Smart Carbs. As trendy as it is to go low- or no-carb (which can certainly work well for some folks), including some slow-digesting, high-fiber smart carbs—in appropriate amounts relative to your goals, activity levels, and body type—can help keep you feeling full and satisfied and even help you stick to your nutrition plan better. Eating some carbs may help reduce levels of the stress hormone cortisol, which when in excess or out of rhythm can negatively impact health, body composition, sleep, and more. As mentioned, carbs also promote the release of the “feel-good” molecule serotonin, which promotes satiety, feelings of wellbeing, and restful night’s sleep.
That may seem counterintuitive considering that you’ve probably been told to avoid carbs at nighttime. However, in a recent study published in the journal Obesity, researchers found that overweight folks who ate a larger percentage of their daily carbohydrates at dinner lost more weight, body fat, and inches from their waistlines compared to a group that ate the same number of daily calories in a more traditional way (e.g., more carbs at breakfast and lunch). Not only that, this strategy of eating more carbs later in the day helped shift hunger hormones, resulting in less hunger throughout the day.68,69
13
Mindfulness. Lastly, arguably more important than what you eat is how you eat. Here’s the simplest, arguably most effective piece of nutrition advice ever: SLOW DOWN.
Although incredibly simple, it’s not easy. After all, most people rush through the day with little time to spare for anything, and when you do have time to eat, you likely gobble it down—probably while you’re trying to multi-task on something else. When it comes to late-night eating, it’s typically accompanied by myriad distractions (e.g., TV, Internet) that influence what, how much, and how quickly food is consumed.
That said, slow eating has a number of advantages:
• Slow eating helps you “check in,” be present, and pay attention to what (and how much) you’re eating and why. Eating when distracted, on the other hand, leads to overeating both acutely and at subsequent meals.
• Slow eating allows you to sense into your body’s internal hunger and fullness cues.
• Slow eating helps you enjoy your food (e.g., textures, tastes, and smells).• Slow eating enhances digestion.• Slow eating doesn’t depend on controlling what you eat—it can be done any
time, anywhere, no matter what’s on your plate.• Slow eating makes you and your body the boss—no external rules (e.g., calorie
counting).
Not only that, eating slowly can help you lose weight. A number of studies have shown that simply by eating more slowly, folks consume fewer calories—in fact, enough to drop 10 pounds in a year without doing anything differently!70
One reason is that it takes about 20 minutes for your brain and stomach to register fullness, and by eating slowly, you have time to recognize when you’re satisfied—not stuffed—and stop on time.
In a recent research article that appeared in the American Journal of Clinical Nutrition,
14
researchers from the University of Birmingham (United Kingdom) reviewed 24 different studies that examined the effect that manipulating memory, distraction, awareness, or attention has on food intake.71
The researchers found that eating when distracted not only causes folks to eat more at that meal or snack, but get this, it also causes people to eat an even greater amount later on in subsequent meals. On the other hand, the researchers found that being more attentive to meals and using “food memories” (e.g., using visual reminders of meals, keeping food wrappers) led to decreased food intake both acutely and at later meals.
This research provides clear evidence that the practice of “mindful eating” is increasingly important when trying to lose fat. As a matter of fact, the authors concluded:
“Evidence indicates that attentive eating is likely to influence food intake, and incorporation of attentive-eating principles into interventions provides a novel approach to aid weight loss and maintenance without the need for conscious calorie counting.”
This piece of advice is useful at any time of day, but it may come in particularly handy at night when most folks have a tendency to snack “mindlessly” while sitting around watching TV. Cornell University researcher and food psychologist Dr. Brian Wansink has written a book on what he refers to as “mindless eating” and the significance that one’s food environment has what and how much s/he eats.72,73
Along these same lines, researchers from North Carolina conducted an entire study to promote research on the question, “Do hunger and satiety still affect eating or has recreational (or mindless) eating taken over?” Like Dr. Wansink’s research, they found that food intake is influenced by a multitude of biological and social signals, which have led to significant increases in overall calorie consumption and the frequency that people eat/snack over the course of a day.74
15
With all of that in mind, slow down when you eat; take smaller bites; and chew each bite slower, longer, and more completely. Also, take time to consider the food choices you tend to make at night and the type of environmental cues (e.g., TV, others eating) that influence your eating behaviors.
Finally, before getting into a list of foods, it’s important to remind you that, in the grand scheme of things, your health, fitness, performance, and body composition are contingent on your entire body of “nutrition work”—not an individual food or single meal. In other words, there’s no one “magical” food. Instead of viewing foods in isolation as “good” or “bad,” think about weight management and “deep health” as the product of practicing healthy eating habits, creating a positive food environment, and choosing high-quality, nutritious foods in appropriate amounts relative to your goals and activity levels regularly and consistently over time. Good nutrition takes practice, and just like getting better and mastering anything in life, it’s about progress—not perfection.
With all of that in mind, let’s get to those craving-crushing, flat-belly foods!
POTATOESFor one reason or another, potatoes seem to get a bad rap. Before delving into why they shouldn’t, it is critical to distinguish whole, unprocessed potatoes from potato-based “foods,” like potato chips, French fries, and restaurant preparations of mashed potatoes and loaded baked potatoes, which are typically a far cry from the humble spud. Potatoes are a nutrient-dense food, containing a variety of different phytonutrients that have antioxidant activity, as well as 10 different vitamins and minerals, including the following:
• Vitamin B6• Copper• Potassium• Vitamin C
16
• Manganese• Phosphorus• Niacin• Pantothenic acid
In addition to their nutrient density, potatoes are an excellent source of resistant starch, which is a special type of carbohydrate that is not digested by the human body, when cooked then cooled.75 Resistant starch is considered both a dietary fiber and a “functional fiber,” depending on whether or not it is consumed naturally from foods or as a supplement.76
Multiple studies have shown resistant starch increases satiety and reduces food intake both acutely and in subsequent feedings.77,78 Research has also shown that consumption of resistant starch increases fat burning, decreases fat storage, and improves insulin sensitivity.79,80
That’s not all; researchers speculate that resistant starch may also increase the thermic effect of feeding, which means that it boosts the metabolism, as well as promote weight loss and preserve calorie-burning muscle.81
One of the very intriguing aspects of resistant starch is that it serves as a prebiotic for the beneficial bacteria that compose the gut microflora. In other words, while it goes undigested by us, resistant starch is fermented by gut bacteria, and as a result, has the potential to positively impact human health in the myriad ways previously described.82
For example, when gut bacteria ferment resistant starch, a byproduct is short-chain fatty acids (e.g., butyrate), which serve to fuel the immune cells that line the gut. These short-chain fatty acids can also help regulate appetite by promoting the release of key hunger suppressing hormones (e.g., GLP-1, PYY).83
Understanding the importance of feeling full, Dr. Susanna Holt and her team of researchers at the University of Sydney set out to establish a satiety index of common
17
foods.61 In the study, the researchers fed participants fixed-calorie portions of thirty-eight different foods and subsequently recorded their perceived hunger following each feeding.
The results of the study, like many similar studies, indicate that satiety is most strongly related to the weight of the food consumed (i.e., energy density), and Dr. Holt and her colleagues also found that higher amounts of protein, dietary fiber, and water content also correlated positively with satiety scores—lending more credence to building a nutrition plan around high-fiber, low-energy-dense and protein-rich foods. Of all the foods tested by Dr. Holt and her team of researchers, boiled potatoes scored highest on the satiety index, over 40% higher than any other food tested.
In addition to potatoes, other root vegetables (e.g., carrots, beets, rutabaga, turnips, parsnips) and tubers (e.g., sweet potatoes, yams, cassava) are also great options, although it is important to note that nutrient content may vary significantly across individual vegetables.
APPLESIf you only look at the nutrition facts of an apple, you may be underwhelmed. While apples are a very good source of fiber (including both soluble and insoluble pectin) and vitamin C, they do not contain significant amounts of other vitamins and minerals. However, what apples lack in those micronutrients, they more than makes up for in their fat-fighting polyphenol content, including the following:
• Flavonols, including quercetin • Catechins, including epicatechin• Anthocyanins (in red-skinned apples)• Chlorogenic acid
18
• Phloridizin and more
Research on the polyphenols in apples has demonstrated some significant benefits in terms of carbohydrate metabolism:
• Quercetin has been shown to inhibit digestive enzymes like alpha-amylase and alpha-glucosidase, which are responsible for breaking down carbohydrates into absorbable sugars. Quercetin has been shown to be effective at reducing blood sugar after a meal.84
• The polyphenols, phenolic acids, and tannins in apples have been shown to reduce the absorption of carbohydrates in the small intestine.85
• Apple polyphenols have also been shown to enhance insulin sensitivity and efficiency, promoting the uptake of carbohydrates into muscle cells to be stored as energy.86
In addition to potential improvements in insulin sensitivity and carbohydrate metabolism, the polyphenols in apples appear to confer significant gut health benefits.87 In lab animals, researchers have found that consumption of polyphenol-rich apples resulted in positive changes in the gut microbiota and improvements in immune system function.88
In Dr. Holt’s satiety study mentioned in the section above, the team of researchers from the University of Sydney also included apples, which ranked among the top five foods tested.
According to the Environmental Working Group, conventional apples top the list of the most pesticide-contaminated produce. With all of that in mind, apples can indeed be a healthy component of a satiating nutrition plan, but because many of the health-promoting nutrients are located in the skin of the apple, it may be wise to opt for organic when possible.
19
OATMEALMany people know that processed flours and the foods made from them (e.g., bread, ready-to-eat breakfast cereals, bagels, donuts, pastries etc.) are not the best options for looking, feeling, and performing their best. These fast-digesting, processed carbohydrates can negatively impact carbohydrate management, insulin sensitivity, body composition, and a variety of other metabolic parameters (e.g., cholesterol, triglycerides).
In a recent study published in the journal Appetite, researchers from the Fred Hutchinson Cancer Research Center in Seattle, Washington, examined how carbohydrate choices affect mood and energy levels.82 Healthy weight and overweight/obese but otherwise healthy adults consumed both a “high glycemic load” (HGL) diet (including refined grains like breakfast cereals, bagels, crackers, cookies, and cakes as well as refined sugars and other processed carbohydrates like instant mashed potatoes and instant soups) and a “low glycemic load” (LGL) diet (including whole grains, legumes, nuts, and fresh fruits and vegetables) in randomized crossover design study for 4 weeks each. At the end of the trial, the researchers found that the LGL diet led to significantly better scores for mood, energy, and fatigue; on the other hand, the participants reported lower energy levels, more fatigue, and depressed mood following the HGL diet, which is representative of the typical Western diet.89
Furthermore, foods made with refined carbohydrates are typically void of fiber, and researchers have linked low fiber intakes to increased risk for diabetes and obesity.90–93 Overall, it’s no secret that heavily processed carbohydrates like these are some of the most fattening ingredients around and closely linked to obesity.94
With all of that in mind, when it comes to choosing carbohydrates, the emphasis should be placed on whole, minimally-processed “smart carbs” that are slow-digesting and
20
high in fiber, which is a nutrition all-star. Dietary fiber promotes a healthy digestive tract, regularity, improves carbohydrate management (e.g., slowed gastric emptying), promotes satiety, reduces calorie intake, and enhances weight loss.95,96
Unfortunately, most people don’t consume nearly enough dietary fiber. According to American Dietetic Association, the average American consumes a paltry 15 grams of dietary fiber per day, only about HALF of the recommended daily intake.97 As you might have imagined, researchers have linked low fiber intakes to increased risk for diabetes and obesity.94,98
In a review of the body of research, researchers at the Human Nutrition Research Center on Aging at Tufts University found that simply increasing fiber intake by 14 grams per day for at least two days can result in an 18% decrease in calorie intake, and over the course of 4 months, that simple dietary intervention was associated with an average weight loss of more than 5 pounds.95
One of our favorite “smart carbs” is oatmeal, which ranked as the third most satiating food in Dr. Holt’s satiety study.61 In particular, we prefer whole rolled oats and steel-cut oats, which are both good sources of fiber, as well as several other nutrients:
• Manganese• Molybdenum• Phosphorus• Copper• Biotin• Vitamin B1• Magnesium• Chromium• Zinc
On the other hand, much of the commercially-available oatmeal (e.g., pre-packaged oatmeal) is heavily processed and contains added refined sugars. With that in mind,
21
when it comes to oatmeal, take the extra time to prepare the old-fashioned, minimally-processed versions. In fact, you can even prepare an awesome oatmeal breakfast the night before. Here’s what you’ll need for our delicious Brownie Batter Overnight Oats:
• 1 cup oats• 1 scoop BioTrust Low Carb Café Mocha• 1 scoop BioTrust Low Carb Milk Chocolate• ¾ cup plain Greek yogurt• 1 cup unsweetened almond milk• 1 tbsp cocoa powder• 1 tsp chia seeds
Making your Brownie Batter Overnight Oats is as simple as 1-2-3:
1. Mix all ingredients in a bowl.2. Transfer into a sealed container (e.g., Mason jar)3. Refrigerate overnight for 8 – 12 hours.
BEANSBeans are an excellent plant-based source of protein, and depending on the type, they provide upwards of 12 grams of fiber per 1-cup serving. Remember, dietary fiber and protein are two nutrients that researchers have found to be positively associated with satiety, or feelings of fullness.61
Not surprisingly, researchers found that, when study participants added garbanzo beans daily to their normal diet, they reported significant improvements in satiety, appetite, meal satisfaction, and bowel function. What’s more, participants decreased their consumption of snack foods as well as their overall calorie intake.99 Additionally, researchers from Purdue University found that subjects who added beans to a reduced-
22
calorie diet lost over three times as much weight as the control group, which consumed the same number of calories, over the course of 6 weeks.100
What’s more, an increase in the hormone CCK, which helps to slow gastric emptying and increase satiety, has been reported following bean consumption. Thus, in addition to their high protein and fiber content, beans may positively influence appetite by stimulating satiety centers in the brain. Legumes, including certain beans and lentils, are also a good source of resistant starch, which as discussed previously can beneficially impact appetite, satiety, metabolism, insulin sensitivity, and even body composition.
Overall, the research is quite clear that adding 3 – 5 cups (per week) of beans to your diet may have some significant beneficial effects on your body composition as well as your cardiovascular health. There are many options from which to choose, including black beans, dried peas, garbanzo beans, kidney beans, lentils, lima beans, navy beans, pinto beans, and more.
WHEY PROTEINAs was previously mentioned, one of the numerous benefits associated with a higher protein intake is increased satiety. However, a number of studies have provided further evidence that all proteins are not created equally, and whey protein may be a particularly superior protein source for appetite control.
In a study published in the journal Physiology & Behavior, a team of researchers from the Netherlands found that when healthy participants received a breakfast with soy protein they experienced significantly greater hunger compared to the same breakfast with whey protein.101 What’s more, when the folks ate the breakfast with whey protein, they demonstrated much stronger responses in the hormone GLP-1, which suppresses appetite, promotes satiety, and contributes to controlling food intake.102
23
In a randomized, double-blind, placebo-controlled study published in the journal Nutrition Research, a team of researchers from Iran found that participants who consumed a whey protein supplement 30 minutes prior to their largest meal experienced significantly greater reductions in appetite and calorie intake compared to participants who consumed a soy protein supplement.103 What’s more, after 12 weeks, the folks who supplemented with whey protein experienced greater reductions in body fat and waist circumference, as well as superior improvements body composition (i.e., less fat, more muscle) compared to the soy protein group.
In another randomized, double-blind, placebo-controlled study published in the Journal of Nutrition, researchers representing the United States Department of Agriculture (at the Beltsville Human Nutrition Research Center) instructed overweight participants to consume either a whey protein supplement, soy protein supplement, or carbohydrate supplement (all equal calories) along with their normal eating habits for 23 weeks. At the end of the study, only the whey protein group lost a significant amount of weight and body fat. What’s more, only the folks supplementing with whey protein experienced significant reductions in waist circumference and decreases in levels of the “hunger hormone” ghrelin.104
In a recent study conducted by Dr. Daniela Jakubowicz, professor of medicine at Tel Aviv University, and colleagues, study participants who consumed 49 grams of whey protein first thing in the morning lost 145% more weight than a group consuming a normal amount of protein at breakfast—despite consuming the exact same number of calories! Only the group consuming the whey protein at breakfast experienced significant reductions in the hunger hormone ghrelin.105
As previously noted, ghrelin stimulates the appetite, promotes food intake, and may facilitate weight gain.106 Previous studies have shown the greatest (and most sustained) reductions in ghrelin after eating protein-rich meals (compared to carbohydrates and fats).107,108 Additional studies have shown that supplementation with whey protein leads to weight loss, reductions in ghrelin and appetite, and improvements in other appetite-related hormones (e.g., GLP-1, which suppresses appetite).102–104
24
GREEK YOGURTGreek yogurt contains more than double the protein of regular yogurt and only about one-third the amount of sugar. Even more, authentic strained Greek yogurt is rich in multiple sources of probiotics. Research indicates that the gut flora (i.e., the bacterial ecosystem) of obese folks differs significantly from that of thin people.109 Along these lines, research published in the British Journal of Nutrition suggests that certain probiotics from the Lactobacillus family of bacteria, which are prominent in Greek yogurt, may help you lose weight and keep it off.110
When choosing a Greek yogurt, it’s best to opt for plain versions, as fruit-flavored varieties have over three times as much sugar. Instead, add some low-energy-dense fresh fruits (e.g., berries), which will provide a nutrient-dense source of fiber, vitamins, and antioxidant phytochemicals.
When choosing Greek yogurt (and other dairy), it’s a good idea to opt for organic. In a recent systemic review and meta-analysis published in the British Journal of Nutrition, researchers reviewed the results of 170 published studies comparing the nutrient composition of organic (i.e., grass-fed, pasture-raised) to conventional (i.e., grain/commodity-fed) dairy.111 Compared to conventional dairy, the researchers found that dairy from pasture-raised cows was 56% higher in omega-3 fats (EPA, DHA, DPA), which help promote a healthy inflammatory response and support thyroid health and function. What’s more, organic dairy contained 69% more conjugated linoleic acid, which, as previously mentioned, has been shown preferentially modulate body composition, enhance immunity, and promote a healthy inflammatory response.112
25
LEAN MEATS, FISH & EGGSWhen it comes to improving body composition, appetite control, and satiety, there is arguably not a single more effective, well-established dietary factor than optimizing one’s protein intake. Research has shown that consuming diets higher in protein are not only safe for otherwise healthy individuals, they may provide a host of benefits. Higher protein diets may:
• Accelerate fat loss and spare lean body mass while following a reduced-calorie diet.113–115
• Attenuate weight regain and contribute to long-term weight maintenance.116,117
• Optimize 24-hour muscle protein synthesis and facilitate the maintenance or building of muscle mass.118,119
• Boost metabolic rate.120,121
• Preserve metabolic rate after weight loss.122,123
• Increase satiety and improve appetite control.57–59
• Improve carbohydrate metabolism and glycemic regulation.124–127
• Increase calcium absorption.128,129
Quite the laundry list of benefits! Here are some of our favorite options:
• Lean meats, poultry, fish, seafood, and wild game (preferably grass-fed, pasture-raised, organic, etc., when appropriate)
• Eggs (preferably pasture-raised)• Dairy, particularly Greek yogurt and cottage cheese (preferably grass-fed,
pasture-raised)
26
BROTH-BASED SOUPSBroth-based soups may arguably be the most appetite satiating food of all. When properly prepared, broth-based soups are low-energy-dense, and they contain a ton of fiber (from veggies and beans) and protein (from one or more of the sources mentioned above). Here’s one of our favorite recipes, which is a Shredded Chicken Chili.
Ingredients:
• 2 tbsp extra virgin olive oil• 1 sweet onion, diced• 1 red bell pepper, diced• 1 jalapeño, diced• 3 cloves garlic, minced• 3 – 4 boneless, skinless chicken breasts• 1 – 28-ounce can diced tomatoes• 1 – 4-ounce can diced green chiles• 4 cups chicken broth• 2 tsp chili powder• 1 tsp ground cumin• black pepper, to taste• guacamole, for garnish
Directions:
1. Preheat olive oil in a large skillet over medium-high heat. Sauté onion, bell pepper, jalapeño, and garlic until onions are translucent. Transfer the cooked vegetables into the slow cooker and add the remaining ingredients (excluding the
27
guacamole). Cook everything for 4 hours on high, or 8 hours on low.2. Once everything is cooked, use a pair of tongs to remove the chicken to a cutting
board or plate. Using two forks, or a knife, shred the chicken into bite-sized pieces. Transfer the chicken back into the slow cooker and stir to mix.
3. Spoon the soup into serving bowls and top with guacamole. Enjoy!
SPINACH Popeye’s super strength came from eating spinach, and the creators of that famous cartoon really did know what they were talking about. Spinach is arguably one of the most nutrient-dense foods you can find, as it is loaded with essential vitamins and minerals, as well as copious phytochemicals. As a matter of fact, spinach is an excellent source of:
• Vitamin K• Vitamin A• Manganese• Folate• Magnesium• Iron• Copper • Vitamin B2• Vitamin B6• Vitamin E• Calcium• Potassium• Vitamin C• Fiber• Phosphorus
28
• Vitamin B1• Zinc• Choline
With that laundry list of essential nutrients, it’s easy to see why this “superfood” would be at the top of anyone’s list trying to lose fat and promote a healthy lifestyle. What’s more, all of these nutrients come at a very low price, calorically speaking. As a matter of fact, a single cup of spinach contains only 7 calories. In addition to these micronutrients, spinach is also a rich source of phytonutrients and antioxidants, like the carotenoids lutein, zeaxanthin, neoxanthin, and violaxanthin.
In a study published in the journal Appetite, Swedish researchers gave overweight women either a beverage containing a greens extract (made from baby spinach leaves) or a placebo prior to breakfast each day. At the end of the 3-month study, the women consuming the beverage with the spinach extract lost, on average, 11 pounds—43% more weight than the placebo group, which was provided the same nutrition and exercise advice.131
The researchers credited the enhanced weight loss to slowed digestion time, improved appetite control, and reductions in hunger. In fact, the women consuming the spinach extract benefited from a 95% decrease in the urge to eat highly palatable foods like sweets, junk food, and fast food.
The researchers found that after the women consumed the spinach extract, they demonstrated a 2.6-fold greater increase (compared to the placebo group) in the hormone GLP-1, which promotes satiety (i.e., feelings of fullness), regulates reward-induced food consumption (i.e., hedonic compensation), and plays an important role in the urge to eat sweet, salt, and fat (i.e., junk food).
In a follow-up study published in the Journal of the American College of Nutrition, the same group of researchers confirmed these findings, as they found that folks who consumed the spinach extract demonstrated increased satiety for several hours
29
after consumption. What was particularly interesting about this study was that the researchers found that spinach extract seemed to positively impact the “food reward system,” often referred to as hedonic compensation.132
Essentially, an eating episode (i.e., the choice to eat food) can be sparked by metabolic need, hedonic drive, or a combination of the two. In other words, in today’s world, we no longer eat only when we’re “metabolically hungry.” Instead, we are driven to eat even when we’re not truly hungry and despite having vast energy reserves (i.e., body fat).
More and more, obesity researchers are investigating the impact of hedonic drive and eating factors, which involves cognitive, reward, and emotional factors and may include choosing to eat based on food environment, food addiction, stress relief, boredom, and mood elevation.133 By suppressing food cravings via acting on the reward system (through various hormones), certain foods like spinach may possess a novel way to reduce calorie consumption and positively address energy balance.
GRAPEFRUITWhile the media has publicized grapefruit as an effective —yet largely unsubstantiated—strategy for weight loss for decades, there’s actually a fair amount of science to support the notion. Like oranges, which ranked fourth on Dr. Holt’s satiety index, grapefruits are an excellent source of vitamin C. In fact, when comparing whole fruits, grapefruits contain about 26% more of this key micronutrient.
In addition to its vitamin C content, grapefruits are also a good source of fiber, which you already know is one of the key drivers of satiety. What’s more, grapefruits have a very high water content (~91%), and subsequently, they are considered a low-energy-dense food. As you already know, these are important factors that play a significant role in appetite control and weight management.
30
In one study published in the journal Nutrition & Metabolism, researchers from Vanderbilt found that when folks added half of a grapefruit (before breakfast, lunch, and dinner) to a reduced-calorie diet they ended up consuming up to 500 fewer calories per day—without any increase in hunger—which had a tremendous impact on weight loss. With the addition of grapefruit, the participants’ rate of weight loss increased by over 13% compared to when they were following a reduced-calorie diet without the fruit.137
In a study published in the Journal of Medicinal Food, researchers from the Scripps Clinic in California found that overweight folks consuming fresh grapefruit three times daily before meals lost 5 TIMES more weight than the placebo group (i.e., no grapefruit) over the course of 12 weeks. Not only that, the researchers also found that the addition of grapefruit significantly improved insulin sensitivity, which is intimately tied to carbohydrate metabolism and weight management.138,139
COCONUT OILWhile once shunned because of its saturated fat content (more on that below), coconut oil is now lauded as a “miracle” food; some may even go so far as to call it a “cure” for [insert health concern here]. While it may not be the “magic bullet” that some would lead you to believe, there may be something to the “coconut craze.”146 Combined with an overall healthy diet, there are a number of health benefits that may be conferred by regularly consuming virgin coconut oil.
Coconut oil is principally made up of saturated fat (about 92%), with as much as 70% of that being a special type of fat called medium chain fatty acids (MCFAs), or medium chain triglycerides (MCTs), making coconut oil unique among dietary fats. You see, unlike long chain fatty acids (LCFA), which are the more common fats found in foods, MCTs are easily burned for energy and are far less likely to be stored as fat.147
31
Furthermore, in the scientific community, MCTs are viewed as “functional” fats that provide a host of health benefits, as they have been shown to lower body weight, improve markers of metabolic health, reduce belly fat (i.e., visceral fat), and improve insulin sensitivity.148 In other words, all fats are not created equally, and coconut oil is a very rich source of this unique, health-promoting saturated fat.
Research suggests that the MCTs found in coconut oil have a significant metabolism-boosting effect. In one study, researchers found that consuming MCTs increased metabolism more than eating LCFAs from other foods. As a matter of fact, the participants who consumed MCTs lost significantly more weight and burned more fat than the group consuming LCTs.149
Researchers have also found that consuming just 1 – 2 tablespoons daily of MCTs can elevate the metabolism by as much as 5%, which may mean burning an additional 150 calories or more per day.150 In addition to short-term feeding studies showing an acute rise in calorie burning with MCTs, research has shown that this elevation in metabolism continues even over prolonged periods of time.151 What’s particularly interesting is that this increase in energy expenditure appears to be met by a subsequent increase in fat burning.
The MCTs in coconut oil may also suppress appetite, which may be related to their conversion in the liver to ketone bodies (more on that in a moment). In one crossover trial, researchers assessed whether increasing the amount of MCTs in the diet influenced food intake under free living conditions. They found that when men at the most MCTs, they consumed, on average, over 250 fewer calories per day.152
In a crossover trial published in The American Journal of Clinical Nutrition, researchers from France found that when they added MCTs to a standardized breakfast, men ate significantly fewer calories at lunch compared to when they ate the same breakfast with LCFAs.153 Numerous other studies have shown that the addition of MCTs promotes satiety, resulting in an involuntary reduction in food intake.154,155
Furthermore, numerous randomized controlled trials have shown that supplementing
32
the diet with MCTs (like those found in coconut oil) leads to greater weight loss and reductions in belly fat than other fats (e.g., LCFAs, including olive oil, soybean oil, canola oil, and corn oil), effects likely due to MCTs’ ability to increase metabolic rate (i.e., calorie expenditure) and fat burning and suppress appetite.154,155,158–160
As mentioned, MCTs are easily burned for fuel, providing immediate and lasting energy. You see, MCTs are easily absorbed and metabolized by the liver, where they are readily converted to ketone bodies, which serve as an important energy source for the brain. Ketone bodies are the most energy-efficient fuel, and they are particularly useful for the brain and muscles in times of stress.
For instance, ketones can replace glucose (i.e., sugar) as the major energy source for the brain. Traditionally, ketogenic diets (i.e., very high fat up to 80%, low carbohydrate < 30 – 50g/day, moderate protein ≤ 20%), which lead to a state of ketosis where the body relies heavily on ketones for fuel, have been used for drug-resistant epilepsy, and more recently, for neurodegenerative diseases (e.g., Parkinson’s).161,162
Speaking of the ketogenic diet (KD), numerous studies have shown significant weight loss on a high fat, low carbohydrate diet without significant elevations of serum cholesterol, including a 56-week randomized controlled trial where participants exhibited significant weight loss, reduction of blood glucose, and improvement of lipid markers after eating a well-formulated KD.164,165
While there is indeed debate as to what’s the “best” diet, the evidence is clear that the KD is a viable, effective tool for weight management. In a meta-analysis published in The Lancet, researchers set out to summarize the large body of evidence from randomized controlled trials examining the effects of different diets on weight loss outcomes. The authors concluded, “In weight loss trials, higher-fat weight loss interventions led to significantly greater weight loss than low-fat interventions.”166 In a study published in the journal Endocrine, researchers from Spain found that participants following a KD lost 183% more weight (13.6 vs. 4.8kg) than those following a standard low-calorie diet (LCD) after 2 months. After 12 months, participants in the KD group had
33
lost nearly 3 times more weight than the LCD (19.9 vs. 7kg).167
There is no doubt that there is strong supportive evidence that the use of ketogenic diets in weight-loss therapy is effective; however, there are contrasting theories regarding the mechanisms through which they work. Per Paoli et al., “A simpler, perhaps more likely, explanation for improved weight loss is a possible appetite-suppressant action of ketosis.” The weight-loss effects of KD may be caused by several factors, with the most viable likely being a reduction in appetite due to higher satiety effect of proteins, effects on appetite control hormones, and possibly direct appetite-suppressant action of ketone bodies.165
Clearly, there’s no shortage of evidence that coconut oil has the potential increase satiety, improve appetite control, boost metabolism, and promote a healthy body weight. Plus, there are a ton of tasty ways you can incorporate coconut oil in your diet:
• Smoothies• Coffee & hot drinks• Salad dressing• Mayonnaise• Sautéing & frying • Roasting• Baking• Energy balls & bars• Candy• Popcorn
In fact, we cover each of these along with examples of delicious recipes in the following report, which is yours FREE today:
10 Ways to Add Coconut Oil to Your Diet
34
References:1. Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM.
Prevalence of Overweight and Obesity in the United States, 1999-2004. JAMA. 2006;295(13):1549. doi:10.1001/jama.295.13.1549.
2. International Association for the Study of Obesity. Working Together to Tackle Obesity: An Advocacy Tookit for IASO Members.; 2013. http://www.worldobesity.org/site_media/uploads/IASO-Advocacy-toolkit-Oct13.pdf.
3. World Health Organization. Obesity and Overweight. Fact Sheet 311. World Health Organization; 2015. http://www.who.int/mediacentre/factsheets/fs311/en/.
4. Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of Obesity and Trends in the Distribution of Body Mass Index Among US Adults, 1999-2010. JAMA. 2012;307(5):491. doi:10.1001/jama.2012.39.
5. Nammi S, Koka S, Chinnala KM, Boini KM. Obesity: an overview on its current perspectives and treatment options. Nutr J. 2004;3:3. doi:10.1186/1475-2891-3-3.
6. Hall KD, Heymsfield SB, Kemnitz JW, Klein S, Schoeller DA, Speakman JR. Energy balance and its components: implications for body weight regulation. Am J Clin Nutr. 2012;95(4):989-994. doi:10.3945/ajcn.112.036350.
7. Wing RR, Hill JO. Successful weight loss maintenance. Annu Rev Nutr. 2001;21:323-341. doi:10.1146/annurev.nutr.21.1.323.
8. Bellisle F, McDevitt R, Prentice AM. Meal frequency and energy balance. Br J Nutr. 1997;77 Suppl 1:S57-70.
9. Kant AK, Schatzkin A, Ballard-Barbash R. Evening eating and subsequent long-term weight change in a national cohort. Int J Obes Relat Metab Disord J Int Assoc Study Obes. 1997;21(5):407-412.
10. Roberts SB, Williamson DF. Causes of adult weight gain. J Nutr. 2002;132(12):3824S-3825S.
11. Hays NP, Bathalon GP, McCrory MA, Roubenoff R, Lipman R, Roberts SB. Eating behavior correlates of adult weight gain and obesity in healthy women aged 55-65 y. Am J Clin Nutr. 2002;75(3):476-483.
12. Ma Y, Bertone ER, Stanek EJ, et al. Association between eating patterns and
35
obesity in a free-living US adult population. Am J Epidemiol. 2003;158(1):85-92.13. Guthrie JF, Lin B-H, Frazao E. Role of food prepared away from home in the
American diet, 1977-78 versus 1994-96: changes and consequences. J Nutr Educ Behav. 2002;34(3):140-150.
14. Nielsen SJ, Popkin BM. Patterns and trends in food portion sizes, 1977-1998. JAMA. 2003;289(4):450-453.
15. Popkin BM. The World Is Fat: The Fads, Trends, Policies, and Products That Are Fattening the Human Race. New York: Avery; 2010.
16. Bertéus Forslund H, Torgerson JS, Sjöström L, Lindroos AK. Snacking frequency in relation to energy intake and food choices in obese men and women compared to a reference population. Int J Obes 2005. 2005;29(6):711-719. doi:10.1038/sj.ijo.0802950.
17. Drummond S, Crombie N, Kirk T. A critique of the effects of snacking on body weight status. Eur J Clin Nutr. 1996;50(12):779-783.
18. Jahns L, Siega-Riz AM, Popkin BM. The increasing prevalence of snacking among US children from 1977 to 1996. J Pediatr. 2001;138(4):493-498. doi:10.1067/mpd.2001.112162.
19. Zizza C, Siega-Riz AM, Popkin BM. Significant increase in young adults’ snacking between 1977-1978 and 1994-1996 represents a cause for concern! Prev Med. 2001;32(4):303-310. doi:10.1006/pmed.2000.0817.
20. Piernas C, Popkin BM. Snacking increased among U.S. adults between 1977 and 2006. J Nutr. 2010;140(2):325-332. doi:10.3945/jn.109.112763.
21. Duffey KJ, Popkin BM. Energy Density, Portion Size, and Eating Occasions: Contributions to Increased Energy Intake in the United States, 1977–2006. Ludwig D, ed. PLoS Med. 2011;8(6):e1001050. doi:10.1371/journal.pmed.1001050.
22. Greenway FL. Physiological adaptations to weight loss and factors favouring weight regain. Int J Obes. 2015;39(8):1188-1196. doi:10.1038/ijo.2015.59.
23. Hill AJ. The psychology of food craving. Proc Nutr Soc. 2007;66(2):277-285. doi:10.1017/S0029665107005502.
24. Wang GJ, Volkow ND, Logan J, et al. Brain dopamine and obesity. Lancet Lond Engl. 2001;357(9253):354-357.
25. Volkow ND, Wang G-J, Telang F, et al. Low dopamine striatal D2 receptors
36
are associated with prefrontal metabolism in obese subjects: Possible contributing factors. NeuroImage. 2008;42(4):1537-1543. doi:10.1016/j.neuroimage.2008.06.002.
26. Volkow ND, Wang G-J, Baler RD. Reward, dopamine and the control of food intake: implications for obesity. Trends Cogn Sci. 2011;15(1):37-46. doi:10.1016/j.tics.2010.11.001.
27. Brennan AM, Mantzoros CS. Drug Insight: the role of leptin in human physiology and pathophysiology--emerging clinical applications. Nat Clin Pract Endocrinol Metab. 2006;2(6):318-327. doi:10.1038/ncpendmet0196.
28. Pan H, Guo J, Su Z. Advances in understanding the interrelations between leptin resistance and obesity. Physiol Behav. 2014;130:157-169. doi:10.1016/j.physbeh.2014.04.003.
29. Dubuc GR, Phinney SD, Stern JS, Havel PJ. Changes of serum leptin and endocrine and metabolic parameters after 7 days of energy restriction in men and women. Metabolism. 1998;47(4):429-434.
30. Weigle DS, Cummings DE, Newby PD, et al. Roles of leptin and ghrelin in the loss of body weight caused by a low fat, high carbohydrate diet. J Clin Endocrinol Metab. 2003;88(4):1577-1586. doi:10.1210/jc.2002-021262.
31. Inui A, Asakawa A, Bowers CY, et al. Ghrelin, appetite, and gastric motility: the emerging role of the stomach as an endocrine organ. FASEB J Off Publ Fed Am Soc Exp Biol. 2004;18(3):439-456. doi:10.1096/fj.03-0641rev.
32. Schwartz MW, Woods SC, Porte D, Seeley RJ, Baskin DG. Central nervous system control of food intake. Nature. 2000;404(6778):661-671. doi:10.1038/35007534.
33. Dickson SL, Egecioglu E, Landgren S, Skibicka KP, Engel JA, Jerlhag E. The role of the central ghrelin system in reward from food and chemical drugs. Mol Cell Endocrinol. 2011;340(1):80-87. doi:10.1016/j.mce.2011.02.017.
34. Egecioglu E, Jerlhag E, Salomé N, et al. Ghrelin increases intake of rewarding food in rodents. Addict Biol. 2010;15(3):304-311. doi:10.1111/j.1369-1600.2010.00216.x.
35. Skibicka KP, Hansson C, Egecioglu E, Dickson SL. Role of ghrelin in food reward: impact of ghrelin on sucrose self-administration and mesolimbic dopamine and acetylcholine receptor gene expression. Addict Biol. 2012;17(1):95-107.
37
doi:10.1111/j.1369-1600.2010.00294.x.36. Austin J, Marks D. Hormonal Regulators of Appetite. Int J Pediatr Endocrinol.
2009;2009. doi:10.1155/2009/141753.37. Ross J. The Mood Cure. New York: Penguin; 2002.38. Voigt J-P, Fink H. Serotonin controlling feeding and satiety. Behav Brain Res.
2015;277:14-31. doi:10.1016/j.bbr.2014.08.065.39. Schellekens H, De Francesco PN, Kandil D, et al. Ghrelin’s Orexigenic Effect
Is Modulated via a Serotonin 2C Receptor Interaction. ACS Chem Neurosci. 2015;6(7):1186-1197. doi:10.1021/cn500318q.
40. Wurtman RJ, Wurtman JJ. Brain serotonin, carbohydrate-craving, obesity and depression. Obes Res. 1995;3 Suppl 4:477S-480S.
41. Wurtman JJ. Carbohydrate craving, mood changes, and obesity. J Clin Psychiatry. 1988;49 Suppl:37-39.
42. Walfish S. Self-assessed emotional factors contributing to increased weight gain in pre-surgical bariatric patients. Obes Surg. 2004;14(10):1402-1405. doi:10.1381/0960892042583897.
43. Oliver G, Wardle J, Gibson EL. Stress and food choice: a laboratory study. Psychosom Med. 2000;62(6):853-865.
44. Vicennati V, Pasqui F, Cavazza C, et al. Cortisol, energy intake, and food frequency in overweight/obese women. Nutr Burbank Los Angel Cty Calif. 2011;27(6):677-680. doi:10.1016/j.nut.2010.07.016.
45. Kim Y, Yang HY, Kim A-J, Lim Y. Academic stress levels were positively associated with sweet food consumption among Korean high-school students. Nutrition. 2013;29(1):213-218. doi:10.1016/j.nut.2012.08.005.
46. Macedo DM, Diez-Garcia RW. Sweet craving and ghrelin and leptin levels in women during stress. Appetite. 2014;80:264-270. doi:10.1016/j.appet.2014.05.031.
47. Stone AA, Brownell KD. The stress-eating paradox: Multiple daily measurements in adult males and females. Psychol Health. 1994;9(6):425-436. doi:10.1080/08870449408407469.
48. Epel E, Jimenez S, Brownell K, Stroud L, Stoney C, Niaura R. Are stress eaters at risk for the metabolic syndrome? Ann N Y Acad Sci. 2004;1032:208-210. doi:10.1196/annals.1314.022.
38
49. Greeno CG, Wing RR. Stress-induced eating. Psychol Bull. 1994;115(3):444-464.50. Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav.
2007;91(4):449-458. doi:10.1016/j.physbeh.2007.04.011.51. Gibson EL. The psychobiology of comfort eating: implications for
neuropharmacological interventions. Behav Pharmacol. 2012;23(5-6):442-460. doi:10.1097/FBP.0b013e328357bd4e.
52. Laitinen J, Ek E, Sovio U. Stress-related eating and drinking behavior and body mass index and predictors of this behavior. Prev Med. 2002;34(1):29-39. doi:10.1006/pmed.2001.0948.
53. Polivy J, Herman CP. Distress and eating: why do dieters overeat? Int J Eat Disord. 1999;26(2):153-164.
54. Graeff FG, Guimarães FS, De Andrade TG, Deakin JF. Role of 5-HT in stress, anxiety, and depression. Pharmacol Biochem Behav. 1996;54(1):129-141.
55. Paddon-Jones D, Westman E, Mattes RD, Wolfe RR, Astrup A, Westerterp-Plantenga M. Protein, weight management, and satiety. Am J Clin Nutr. 2008;87(5):1558S-1561S.
56. Veldhorst M, Smeets A, Soenen S, et al. Protein-induced satiety: Effects and mechanisms of different proteins. Physiol Behav. 2008;94(2):300-307. doi:10.1016/j.physbeh.2008.01.003.
57. Halton TL, Hu FB. The effects of high protein diets on thermogenesis, satiety and weight loss: a critical review. J Am Coll Nutr. 2004;23(5):373-385.
58. Leidy HJ. Increased dietary protein as a dietary strategy to prevent and/or treat obesity. Mo Med. 2014;111(1):54-58.
59. Ortinau LC, Hoertel HA, Douglas SM, Leidy HJ. Effects of high-protein vs. high- fat snacks on appetite control, satiety, and eating initiation in healthy women. Nutr J. 2014;13:97. doi:10.1186/1475-2891-13-97.
60. Chambers L, McCrickerd K, Yeomans MR. Optimising foods for satiety. Trends Food Sci Technol. 2015;41(2):149-160. doi:10.1016/j.tifs.2014.10.007.
61. Holt SH, Miller JC, Petocz P, Farmakalidis E. A satiety index of common foods. Eur J Clin Nutr. 1995;49(9):675-690.
62. Rolls BJ, Bell EA. Intake of fat and carbohydrate: role of energy density. Eur J Clin
39
Nutr. 1999;53 Suppl 1:S166-173.63. Ledikwe JH, Blanck HM, Kettel Khan L, et al. Dietary energy density is
associated with energy intake and weight status in US adults. Am J Clin Nutr. 2006;83(6):1362-1368.
64. Duncan KH, Bacon JA, Weinsier RL. The effects of high and low energy density diets on satiety, energy intake, and eating time of obese and nonobese subjects. Am J Clin Nutr. 1983;37(5):763-767.
65. Ello-Martin JA, Roe LS, Ledikwe JH, Beach AM, Rolls BJ. Dietary energy density in the treatment of obesity: a year-long trial comparing 2 weight-loss diets. Am J Clin Nutr. 2007;85(6):1465-1477.
66. Tohill BC, Seymour J, Serdula M, Kettel-Khan L, Rolls BJ. What epidemiologic studies tell us about the relationship between fruit and vegetable consumption and body weight. Nutr Rev. 2004;62(10):365-374.
67. Yao M, Roberts SB. Dietary energy density and weight regulation. Nutr Rev. 2001;59(8 Pt 1):247-258.
68. Sofer S, Eliraz A, Kaplan S, et al. Greater weight loss and hormonal changes after 6 months diet with carbohydrates eaten mostly at dinner. Obes Silver Spring Md. 2011;19(10):2006-2014. doi:10.1038/oby.2011.48.
69. Sofer S, Eliraz A, Kaplan S, et al. Changes in daily leptin, ghrelin and adiponectin profiles following a diet with carbohydrates eaten at dinner in obese subjects. Nutr Metab Cardiovasc Dis NMCD. 2013;23(8):744-750. doi:10.1016/j.numecd.2012.04.008.
70. Shah M, Copeland J, Dart L, Adams-Huet B, James A, Rhea D. Slower eating speed lowers energy intake in normal-weight but not overweight/obese subjects. J Acad Nutr Diet. 2014;114(3):393-402. doi:10.1016/j.jand.2013.11.002.
71. Robinson E, Aveyard P, Daley A, et al. Eating attentively: a systematic review and meta-analysis of the effect of food intake memory and awareness on eating. Am J Clin Nutr. 2013;97(4):728-742. doi:10.3945/ajcn.112.045245.
72. Wansink B. What really determines what we eat. The hidden truth. Diabetes Self Manag. 2006;23(6):44, 47-48, 51.
73. Wansink B. Mindless Eating: Why We Eat More than We Think. New York: Bantam Books; 2007.
40
74. Popkin BM, Duffey KJ. Does hunger and satiety drive eating anymore? Increasing eating occasions and decreasing time between eating occasions in the United States. Am J Clin Nutr. 2010;91(5):1342-1347. doi:10.3945/ajcn.2009.28962.
75. Murphy MM, Douglass JS, Birkett A. Resistant starch intakes in the United States. J Am Diet Assoc. 2008;108(1):67-78. doi:10.1016/j.jada.2007.10.012.
76. Slavin J. Fiber and Prebiotics: Mechanisms and Health Benefits. Nutrients. 2013;5(4):1417-1435. doi:10.3390/nu5041417.
77. Bodinham CL, Frost GS, Robertson MD. Acute ingestion of resistant starch reduces food intake in healthy adults. Br J Nutr. 2010;103(6):917-922. doi:10.1017/S0007114509992534.
78. Nilsson AC, Ostman EM, Holst JJ, Björck IME. Including indigestible carbohydrates in the evening meal of healthy subjects improves glucose tolerance, lowers inflammatory markers, and increases satiety after a subsequent standardized breakfast. J Nutr. 2008;138(4):732-739.
79. Higgins JA, Higbee DR, Donahoo WT, Brown IL, Bell ML, Bessesen DH. Resistant starch consumption promotes lipid oxidation. Nutr Metab. 2004;1(1):8. doi:10.1186/1743-7075-1-8.
80. Robertson MD, Wright JW, Loizon E, et al. Insulin-sensitizing effects on muscle and adipose tissue after dietary fiber intake in men and women with metabolic syndrome. J Clin Endocrinol Metab. 2012;97(9):3326-3332. doi:10.1210/jc.2012-1513.
81. Higgins JA. Resistant starch and energy balance: impact on weight loss and maintenance. Crit Rev Food Sci Nutr. 2014;54(9):1158-1166. doi:10.1080/10408398.2011.629352.
82. Birt DF, Boylston T, Hendrich S, et al. Resistant Starch: Promise for Improving Human Health. Adv Nutr Int Rev J. 2013;4(6):587-601. doi:10.3945/an.113.004325.
83. Byrne CS, Chambers ES, Morrison DJ, Frost G. The role of short chain fatty acids in appetite regulation and energy homeostasis. Int J Obes. 2015;39(9):1331-1338. doi:10.1038/ijo.2015.84.
84. S. A. H, A. A, T. O. M, T. A. A. Quercetin Dampens Postprandial Hyperglycemia in Type 2 Diabetic Patients Challenged with Carbohydrates Load. Int J Diabetes Res. 2012;1(3):32-35. doi:10.5923/j.diabetes.20120103.01.
41
85. Manzano S, Williamson G. Polyphenols and phenolic acids from strawberry and apple decrease glucose uptake and transport by human intestinal Caco-2 cells. Mol Nutr Food Res. 2010;54(12):1773-1780. doi:10.1002/mnfr.201000019.
86. Hanhineva K, Törrönen R, Bondia-Pons I, et al. Impact of dietary polyphenols on carbohydrate metabolism. Int J Mol Sci. 2010;11(4):1365-1402. doi:10.3390/ijms11041365.
87. Cardona F, Andrés-Lacueva C, Tulipani S, Tinahones FJ, Queipo-Ortuño MI. Benefits of polyphenols on gut microbiota and implications in human health. J Nutr Biochem. 2013;24(8):1415-1422. doi:10.1016/j.jnutbio.2013.05.001.
88. Espley RV, Butts CA, Laing WA, et al. Dietary flavonoids from modified apple reduce inflammation markers and modulate gut microbiota in mice. J Nutr. 2014;144(2):146-154. doi:10.3945/jn.113.182659.
89. Breymeyer KL, Lampe JW, McGregor BA, Neuhouser ML. Subjective mood and energy levels of healthy weight and overweight/obese healthy adults on high-and low-glycemic load experimental diets. Appetite. 2016;107:253-259. doi:10.1016/j.appet.2016.08.008.
90. Roberts SB. High-glycemic index foods, hunger, and obesity: is there a connection? Nutr Rev. 2000;58(6):163-169.
91. Pi-Sunyer FX. Glycemic index and disease. Am J Clin Nutr. 2002;76(1):290S-8S.92. Nuttall FQ, Gannon MC. Plasma glucose and insulin response to macronutrients in
nondiabetic and NIDDM subjects. Diabetes Care. 1991;14(9):824-838.93. Moghaddam E, Vogt JA, Wolever TMS. The effects of fat and protein on glycemic
responses in nondiabetic humans vary with waist circumference, fasting plasma insulin, and dietary fiber intake. J Nutr. 2006;136(10):2506-2511.
94. Salmerón J, Manson JE, Stampfer MJ, Colditz GA, Wing AL, Willett WC. Dietary fiber, glycemic load, and risk of non-insulin-dependent diabetes mellitus in women. JAMA. 1997;277(6):472-477.
95. Howarth NC, Saltzman E, Roberts SB. Dietary fiber and weight regulation. Nutr Rev. 2001;59(5):129-139.
96. Slavin JL. Dietary fiber and body weight. Nutr Burbank Los Angel Cty Calif. 2005;21(3):411-418. doi:10.1016/j.nut.2004.08.018.
97. Slavin JL. Position of the American Dietetic Association: health implications of
42
dietary fiber. J Am Diet Assoc. 2008;108(10):1716-1731.98. Salmerón J, Ascherio A, Rimm EB, et al. Dietary fiber, glycemic load, and risk of
NIDDM in men. Diabetes Care. 1997;20(4):545-550.99. Murty CM, Pittaway JK, Ball MJ. Chickpea supplementation in an Australian diet
affects food choice, satiety and bowel health. Appetite. 2010;54(2):282-288. doi:10.1016/j.appet.2009.11.012.
100. McCrory M, Lovejoy J, Palmer P, et al. Effectiveness of legume consumption for facilitating weight loss: a randomized trial (abstract). FASEB J. 2008;22:1084.9.
101. Veldhorst MAB, Nieuwenhuizen AG, Hochstenbach-Waelen A, et al. Dose-dependent satiating effect of whey relative to casein or soy. Physiol Behav. 2009;96(4-5):675-682.
102. Dailey MJ, Moran TH. Glucagon-like peptide 1 and appetite. Trends Endocrinol Metab TEM. 2013;24(2):85-91. doi:10.1016/j.tem.2012.11.008.
103. Tahavorgar A, Vafa M, Shidfar F, Gohari M, Heydari I. Whey protein preloads are more beneficial than soy protein preloads in regulating appetite, calorie intake, anthropometry, and body composition of overweight and obese men. Nutr Res N Y N. 2014;34(10):856-861. doi:10.1016/j.nutres.2014.08.015.
104. Baer DJ, Stote KS, Paul DR, Harris GK, Rumpler WV, Clevidence BA. Whey protein but not soy protein supplementation alters body weight and composition in free-living overweight and obese adults. J Nutr. 2011;141(8):1489-1494. doi:10.3945/jn.111.139840.
105. Jakubowicz D, Landau Z, Wainstein J, Bar-Dayan Y, Froy O. Whey Protein Induces Greater Reduction of Postprandial Glycemia and HbA1c, Weight Loss and Satiety Compared to Other Protein Sources in Type 2 Diabetes. April 2016.
106. Hall WL, Millward DJ, Long SJ, Morgan LM. Casein and whey exert different effects on plasma amino acid profiles, gastrointestinal hormone secretion and appetite. Br J Nutr. 2003;89(2):239-248. doi:10.1079/BJN2002760.
107. Wang Z, Heshka S, Gallagher D, Boozer CN, Kotler DP, Heymsfield SB. Resting energy expenditure-fat-free mass relationship: new insights provided by body composition modeling. Am J Physiol Endocrinol Metab. 2000;279(3):E539-545.
108. Lomenick JP, Melguizo MS, Mitchell SL, Summar ML, Anderson JW. Effects of meals high in carbohydrate, protein, and fat on ghrelin and peptide YY secretion
43
in prepubertal children. J Clin Endocrinol Metab. 2009;94(11):4463-4471. doi:10.1210/jc.2009-0949.
109. Shen J, Obin MS, Zhao L. The gut microbiota, obesity and insulin resistance. Mol Aspects Med. 2013;34(1):39-58. doi:10.1016/j.mam.2012.11.001.
110. Sanchez M, Darimont C, Drapeau V, et al. Effect of Lactobacillus rhamnosus CGMCC1.3724 supplementation on weight loss and maintenance in obese men and women. Br J Nutr. 2014;111(8):1507-1519. doi:10.1017/S0007114513003875.
111. Średnicka-Tober D, Barański M, Seal CJ, et al. Higher PUFA and n-3 PUFA, conjugated linoleic acid, α-tocopherol and iron, but lower iodine and selenium concentrations in organic milk: a systematic literature review and meta- and redundancy analyses. Br J Nutr. 2016;115(6):1043-1060. doi:10.1017/S0007114516000349.
112. Pariza MW. Perspective on the safety and effectiveness of conjugated linoleic acid. Am J Clin Nutr. 2004;79(6 Suppl):1132S-1136S.
113. Layman DK, Boileau RA, Erickson DJ, et al. A reduced ratio of dietary carbohydrate to protein improves body composition and blood lipid profiles during weight loss in adult women. J Nutr. 2003;133(2):411-417.
114. Tang M, Armstrong CLH, Leidy HJ, Campbell WW. Normal vs. high-protein weight loss diets in men: effects on body composition and indices of metabolic syndrome. Obes Silver Spring Md. 2013;21(3):E204-210. doi:10.1002/oby.20078.
115. Wycherley TP, Moran LJ, Clifton PM, Noakes M, Brinkworth GD. Effects of energy-restricted high-protein, low-fat compared with standard-protein, low-fat diets: a meta-analysis of randomized controlled trials. Am J Clin Nutr. 2012;96(6):1281-1298. doi:10.3945/ajcn.112.044321.
116. Layman DK, Evans EM, Erickson D, et al. A Moderate-Protein Diet Produces Sustained Weight Loss and Long-Term Changes in Body Composition and Blood Lipids in Obese Adults. J Nutr. 2009;139(3):514-521. doi:10.3945/jn.108.099440.
117. Larsen TM, Dalskov S-M, van Baak M, et al. Diets with High or Low Protein Content and Glycemic Index for Weight-Loss Maintenance. N Engl J Med. 2010;363(22):2102-2113. doi:10.1056/NEJMoa1007137.
118. Mamerow MM, Mettler JA, English KL, et al. Dietary Protein Distribution Positively Influences 24-h Muscle Protein Synthesis in Healthy Adults. J Nutr.
44
2014;144(6):876-880. doi:10.3945/jn.113.185280.119. Rodriguez NR. Protein-Centric Meals for Optimal Protein Utilization: Can It Be That
Simple? J Nutr. 2014;144(6):797-798. doi:10.3945/jn.114.193615.120. Westerterp-Plantenga MS, Rolland V, Wilson SA, Westerterp KR. Satiety related to
24 h diet-induced thermogenesis during high protein/carbohydrate vs high fat diets measured in a respiration chamber. Eur J Clin Nutr. 1999;53(6):495-502.
121. Westerterp KR. Diet induced thermogenesis. Nutr Metab. 2004;1(1):5. doi:10.1186/1743-7075-1-5.
122. Soenen S, Martens EAP, Hochstenbach-Waelen A, Lemmens SGT, Westerterp-Plantenga MS. Normal protein intake is required for body weight loss and weight maintenance, and elevated protein intake for additional preservation of resting energy expenditure and fat free mass. J Nutr. 2013;143(5):591-596. doi:10.3945/jn.112.167593.
123. Ebbeling CB, Swain JF, Feldman HA, et al. Effects of dietary composition on energy expenditure during weight-loss maintenance. JAMA. 2012;307(24):2627-2634. doi:10.1001/jama.2012.6607.
124. Layman DK, Baum JI. Dietary protein impact on glycemic control during weight loss. J Nutr. 2004;134(4):968S-73S.
125. Farnsworth E, Luscombe ND, Noakes M, Wittert G, Argyiou E, Clifton PM. Effect of a high-protein, energy-restricted diet on body composition, glycemic control, and lipid concentrations in overweight and obese hyperinsulinemic men and women. Am J Clin Nutr. 2003;78(1):31-39.
126. Gannon MC, Nuttall FQ, Saeed A, Jordan K, Hoover H. An increase in dietary protein improves the blood glucose response in persons with type 2 diabetes. Am J Clin Nutr. 2003;78(4):734-741.
127. Gannon MC, Nuttall FQ. Effect of a high-protein, low-carbohydrate diet on blood glucose control in people with type 2 diabetes. Diabetes. 2004;53(9):2375-2382.
128. Mangano KM, Sahni S, Kerstetter JE. Dietary protein is beneficial to bone health under conditions of adequate calcium intake: an update on clinical research. Curr Opin Clin Nutr Metab Care. 2014;17(1):69-74. doi:10.1097/MCO.0000000000000013.
129. Tang M, O’Connor LE, Campbell WW. Diet-induced weight loss: the effect of
45
dietary protein on bone. J Acad Nutr Diet. 2014;114(1):72-85. doi:10.1016/j.jand.2013.08.021.
130. Gregor MF, Hotamisligil GS. Inflammatory mechanisms in obesity. Annu Rev Immunol. 2011;29:415-445. doi:10.1146/annurev-immunol-031210-101322.
131. Montelius C, Erlandsson D, Vitija E, Stenblom E-L, Egecioglu E, Erlanson-Albertsson C. Body weight loss, reduced urge for palatable food and increased release of GLP-1 through daily supplementation with green-plant membranes for three months in overweight women. Appetite. 2014;81:295-304. doi:10.1016/j.appet.2014.06.101.
132. Rebello CJ, Chu J, Beyl R, Edwall D, Erlanson-Albertsson C, Greenway FL. Acute Effects of a Spinach Extract Rich in Thylakoids on Satiety: A Randomized Controlled Crossover Trial. J Am Coll Nutr. June 2015:1-8. doi:10.1080/07315724.2014.1003999.
133. Berthoud H-R. Metabolic and hedonic drives in the neural control of appetite: who is the boss? Curr Opin Neurobiol. 2011;21(6):888-896. doi:10.1016/j.conb.2011.09.004.
134. Brody S, Preut R, Schommer K, Schürmeyer TH. A randomized controlled trial of high dose ascorbic acid for reduction of blood pressure, cortisol, and subjective responses to psychological stress. Psychopharmacology (Berl). 2002;159(3):319-324. doi:10.1007/s00213-001-0929-6.
135. Epel ES, McEwen B, Seeman T, et al. Stress and body shape: stress-induced cortisol secretion is consistently greater among women with central fat. Psychosom Med. 2000;62(5):623-632.
136. Despres J-P. Body Fat Distribution and Risk of Cardiovascular Disease: An Update. Circulation. 2012;126(10):1301-1313. doi:10.1161/CIRCULATIONAHA.111.067264.
137. Silver HJ, Dietrich MS, Niswender KD. Effects of grapefruit, grapefruit juice and water preloads on energy balance, weight loss, body composition, and cardiometabolic risk in free-living obese adults. Nutr Metab. 2011;8(1):8. doi:10.1186/1743-7075-8-8.
138. Fujioka K, Greenway F, Sheard J, Ying Y. The effects of grapefruit on weight and insulin resistance: relationship to the metabolic syndrome. J Med Food. 2006;9(1):49-54. doi:10.1089/jmf.2006.9.49.
46
139. Kahn BB, Flier JS. Obesity and insulin resistance. J Clin Invest. 2000;106(4):473-481. doi:10.1172/JCI10842.
140. Jung UJ, Kim HJ, Lee JS, et al. Naringin supplementation lowers plasma lipids and enhances erythrocyte antioxidant enzyme activities in hypercholesterolemic subjects. Clin Nutr Edinb Scotl. 2003;22(6):561-568.
141. Zygmunt K, Faubert B, MacNeil J, Tsiani E. Naringenin, a citrus flavonoid, increases muscle cell glucose uptake via AMPK. Biochem Biophys Res Commun. 2010;398(2):178-183. doi:10.1016/j.bbrc.2010.06.048.
142. Kurth-Kraczek EJ, Hirshman MF, Goodyear LJ, Winder WW. 5’ AMP-activated protein kinase activation causes GLUT4 translocation in skeletal muscle. Diabetes. 1999;48(8):1667-1671.
143. O’Neill HM, Holloway GP, Steinberg GR. AMPK regulation of fatty acid metabolism and mitochondrial biogenesis: implications for obesity. Mol Cell Endocrinol. 2013;366(2):135-151. doi:10.1016/j.mce.2012.06.019.
144. Richard AJ, Amini-Vaughan Z, Ribnicky DM, Stephens JM. Naringenin Inhibits Adipogenesis and Reduces Insulin Sensitivity and Adiponectin Expression in Adipocytes. Evid Based Complement Alternat Med. 2013;2013:1-10. doi:10.1155/2013/549750.
145. Yoshida H, Watanabe W, Oomagari H, Tsuruta E, Shida M, Kurokawa M. Citrus flavonoid naringenin inhibits TLR2 expression in adipocytes. J Nutr Biochem. 2013;24(7):1276-1284. doi:10.1016/j.jnutbio.2012.10.003.
146. Kormos W. On call. The coconut craze. I have seen many products promoting the health benefits of coconut oil or coconut water. Is there any proof of those benefits? Harv Mens Health Watch. 2014;18(11):2.
147. St-Onge M-P. Dietary fats, teas, dairy, and nuts: potential functional foods for weight control? Am J Clin Nutr. 2005;81(1):7-15.
148. Nagao K, Yanagita T. Medium-chain fatty acids: Functional lipids for the prevention and treatment of the metabolic syndrome. Pharmacol Res. 2010;61(3):208-212. doi:10.1016/j.phrs.2009.11.007.
149. St-Onge M-P, Jones PJH. Greater rise in fat oxidation with medium-chain triglyceride consumption relative to long-chain triglyceride is associated with lower initial body weight and greater loss of subcutaneous adipose tissue. Int J Obes
47
Relat Metab Disord J Int Assoc Study Obes. 2003;27(12):1565-1571. doi:10.1038/sj.ijo.0802467.
150. Dulloo AG, Fathi M, Mensi N, Girardier L. Twenty-four-hour energy expenditure and urinary catecholamines of humans consuming low-to-moderate amounts of medium-chain triglycerides: a dose-response study in a human respiratory chamber. Eur J Clin Nutr. 1996;50(3):152-158.
151. St-Onge M-P, Bourque C, Jones PJH, Ross R, Parsons WE. Medium- versus long-chain triglycerides for 27 days increases fat oxidation and energy expenditure without resulting in changes in body composition in overweight women. Int J Obes Relat Metab Disord J Int Assoc Study Obes. 2003;27(1):95-102. doi:10.1038/sj.ijo.0802169.
152. Stubbs RJ, Harbron CG. Covert manipulation of the ratio of medium- to long-chain triglycerides in isoenergetically dense diets: effect on food intake in ad libitum feeding men. Int J Obes Relat Metab Disord J Int Assoc Study Obes. 1996;20(5):435-444.
153. Van Wymelbeke V, Himaya A, Louis-Sylvestre J, Fantino M. Influence of medium-chain and long-chain triacylglycerols on the control of food intake in men. Am J Clin Nutr. 1998;68(2):226-234.
154. Han JR, Deng B, Sun J, et al. Effects of dietary medium-chain triglyceride on weight loss and insulin sensitivity in a group of moderately overweight free-living type 2 diabetic Chinese subjects. Metabolism. 2007;56(7):985-991. doi:10.1016/j.metabol.2007.03.005.
155. St-Onge M-P, Ross R, Parsons WD, Jones PJH. Medium-chain triglycerides increase energy expenditure and decrease adiposity in overweight men. Obes Res. 2003;11(3):395-402. doi:10.1038/oby.2003.53.
156. Assunção ML, Ferreira HS, dos Santos AF, Cabral CR, Florêncio TMMT. Effects of dietary coconut oil on the biochemical and anthropometric profiles of women presenting abdominal obesity. Lipids. 2009;44(7):593-601. doi:10.1007/s11745-009-3306-6.
157. Liau KM, Lee YY, Chen CK, Rasool AHG. An open-label pilot study to assess the efficacy and safety of virgin coconut oil in reducing visceral adiposity. ISRN Pharmacol. 2011;2011:949686. doi:10.5402/2011/949686.
48
158. St-Onge M-P, Bosarge A. Weight-loss diet that includes consumption of medium-chain triacylglycerol oil leads to a greater rate of weight and fat mass loss than does olive oil. Am J Clin Nutr. 2008;87(3):621-626.
159. Nosaka N, Maki H, Suzuki Y, et al. Effects of margarine containing medium-chain triacylglycerols on body fat reduction in humans. J Atheroscler Thromb. 2003;10(5):290-298.
160. Kasai M, Nosaka N, Maki H, et al. Effect of dietary medium- and long-chain triacylglycerols (MLCT) on accumulation of body fat in healthy humans. Asia Pac J Clin Nutr. 2003;12(2):151-160.
161. Fernando WM a. DB, Martins IJ, Goozee KG, Brennan CS, Jayasena V, Martins RN. The role of dietary coconut for the prevention and treatment of Alzheimer’s disease: potential mechanisms of action. Br J Nutr. 2015;114(1):1-14. doi:10.1017/S0007114515001452.
162. Murray AJ, Knight NS, Cole MA, et al. Novel ketone diet enhances physical and cognitive performance. FASEB J Off Publ Fed Am Soc Exp Biol. August 2016. doi:10.1096/fj.201600773R.
163. Reger MA, Henderson ST, Hale C, et al. Effects of beta-hydroxybutyrate on cognition in memory-impaired adults. Neurobiol Aging. 2004;25(3):311-314. doi:10.1016/S0197-4580(03)00087-3.
164. Dashti HM, Al-Zaid NS, Mathew TC, et al. Long term effects of ketogenic diet in obese subjects with high cholesterol level. Mol Cell Biochem. 2006;286(1-2):1-9. doi:10.1007/s11010-005-9001-x.
165. Paoli A, Rubini A, Volek JS, Grimaldi KA. Beyond weight loss: a review of the therapeutic uses of very-low-carbohydrate (ketogenic) diets. Eur J Clin Nutr. 2013;67(8):789-796. doi:10.1038/ejcn.2013.116.
166. Tobias DK, Chen M, Manson JE, Ludwig DS, Willett W, Hu FB. Effect of low-fat diet interventions versus other diet interventions on long-term weight change in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2015;3(12):968-979. doi:10.1016/S2213-8587(15)00367-8.
167. Moreno B, Bellido D, Sajoux I, et al. Comparison of a very low-calorie-ketogenic diet with a standard low-calorie diet in the treatment of obesity. Endocrine. 2014;47(3):793-805. doi:10.1007/s12020-014-0192-3.
49
168. Arunima S, Rajamohan T. Effect of virgin coconut oil enriched diet on the antioxidant status and paraoxonase 1 activity in ameliorating the oxidative stress in rats - a comparative study. Food Funct. 2013;4(9):1402-1409. doi:10.1039/c3fo60085h.
169. Yeap S, Beh B, Ali N, et al. Antistress and antioxidant effects of virgin coconut oil in�vivo. Exp Ther Med. November 2014. doi:10.3892/etm.2014.2045.
170. Law KS, Azman N, Omar EA, et al. The effects of virgin coconut oil (VCO) as supplementation on quality of life (QOL) among breast cancer patients. Lipids Health Dis. 2014;13:139. doi:10.1186/1476-511X-13-139.