Jems201205 dl
-
Upload
santiago-clei-wandeson-ferreira -
Category
Health & Medicine
-
view
1.911 -
download
2
Transcript of Jems201205 dl

Choose 13 at www.jems.com/rs
FP-Spread.indd 5 4/23/2012 10:35:52 AM

JOURNAL OF EMERGENCY MEDICAL SERVICES
TheConscience
of EMS
Contents
Premier media Partner of the iafC, the iafC emS SeCtion & fire-reSCue med www.jems.com maY 2012 JEMS 7
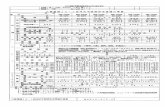
Departments & columns 9 i Load & go i now on JemS.com 14 i EMS in action i Scene of the month 16 i FroM thE Editor i on the front Lines By a.J. heightman, mPa, emt-P 18 i LEttErS i in Your Words 20 i Priority traFFic i news You Can use 24 i LEadErShiP SEctor i Crisis management By Gary Ludwig, mS, emt-P 27 i ManagEMEnt FocuS i extra Set of hands By richard huff, nremt-B 30 i trickS oF thE tradE i numbers �By thom dick 32 i caSE oF thE Month i miracle in the desert �By Jeff Westin, md; Pat Songer, nremt-P, aSm; Kelly Buchanan,
md; Loren Gorosh, md; ryan hodnick, do; & Bryan e. Bledsoe, do, faCeP, faaem
36 i rESEarch rEviEw i What Current Studies mean to emS �By david Page, mS, nremt-P 74 i ad indEx 75 i EMPLoyMEnt & cLaSSiFiEd adS 78 i thE LightEr SidE i Zombie emS �By Steve Berry 82 i LaSt word i the ups & downs of emS
46 i PrEParEd For thE worSt i tactical training offers many benefits to emS�� By�William�Justice,�NREMT-P;�Lt.�Kerry�Massie,�NREMT-I;�&�Jeffrey�M.�Goodloe,�
MD,�NREMT-P,�FACEP
52 i PartnErS in criME i emS provides a training program for local law enforcement� By�Capt.�Mario�Ramirez,�MD,�MPP;�Andrew�N.�Pfeffer,�MD;�Greg�Lee;�&�Corey�M.�
Slovis,�MD,�FACEP
56 i what’S buggin’ EMS i how to rid your rigs of a bedbug infestation�� � By�Wayne�M.�Zygowicz,�BA,�EFO,�EMT-P
62 i brEaking barriErS i Practice cultural sensitivity to provide care to immigrant
communities�By�Keith�Widmeier,�NREMT-P,�CCEMT-P,�EMS-I,�BA;�&�Emily�Coffey,�BA,�NREMT-P
68 i MuLtiPLE airwayS i rapid assessment is key for managing numerous patients�� � By�Paul�E.�Phrampus,�MD
About the CoverA Pima County (Ariz.) Sheriff’s Department deputy demonstrates the value of early law enforcement officer delivery of EMS treatment, particularly at an active-shooter incident or situations where it’s unsafe for EMS to enter. Find out how training and equipping first-arriving police officers, sheriff’s deputies and highway patrol officers can help save patients (and other officers) in “On the Front Lines,” p 16; “Beyond the Tape,” pp 38–45; “Prepared for the Worst,” pp. 46–51; and “Partners in Crime,” pp. 52–55. Photo Matthew StrauSS
MAy 2012 VOL. 37 NO. 5
i bEyond thE taPE i Law enforcement officers make major impact
as initial care providers By�David�Kleinman,�NREMT-P,�&�Tammy�Kastre,�MD
38
i 62
i 68
007_TOCMay.indd 7 4/20/2012 11:56:54 AM

www.jems.com mAY 2012 JEMS 9
The EMS 10: Innovators in EMS award winners pose at the dinner where they were honored for their achieve-ments. Pictured from top left are Tom Bouthillet, Michael Millin, Seth Hawkins, Will Smith, Pat Songer, Rob Lawrence, Stephanie Haley-Andrews and David Reinis. Not pictured are Mary Meyers, Paul Paris, E. Reed Smith and Todd Stout. In case you’ve missed the past winners of this annual award, make sure to check them out at jems.com/ems10
To vote, do a keyword search on JEMS.com for “polls.”s jems.com/poll2012/
The mobile version
s http://m.jems.com/poll/
may poll quesTion How do you celebrate EMS Week?
like usfacebook.com/jemsfans
follow us twitter.com/jemsconnect
geT connecTedlinkedin.com/groups?about=&gid=113182
ems news alerTsjems.com/enews
besT bloggersFireEMSBlogs.com
check iT ouTjems.com/ems-products
JEMS.com offers youoriginal content, jobs,products and resources.But we’re much morethan that; we keepyou in touch withyour colleaguesthrough our:
> Facebook fan page;> JEMS Connect site;> Twitter account;> LinkedIn profile;> Product Connect site; and> Fire EMS Blogs site.
follow us on
load & go log in for EXClUSiVE ConTEnT
A BETTEr WAy To LEArn
JEMSCE.CoM onLInE ConTInuIng
EduCATIon ProgrAM
april poll resulTsWhich is a more dangerous location for EMS providers driving an ambulance?
34% Interstate or rural highway
27% rural streets
39% Suburban streets.
Innovators dine
Sponsored Product FocusspeechmikeWith more than 50 years of experience in the voice technology market, Philips Speech Processing provides innovative, practical dictation and transcription solutions that allow professionals to increase productivity and efficiency. As the leading dictation device on the market, the SpeechMike is specifically designed to enhance productivity for optimal speech recognition results. Its ergonomic, intuitive design boasts dictation control, play-back speakers, and PC navigation in a single device, and it allows users to send sound files for transcription at the press of a button.
s Check out their ad on JEMS.com!
p My agency hosts an event.p I recognize it with coworkers.p I don’t even know when it is!p other
Pho
To g
ary
JaC
kSo
n
009_Load.indd 9 4/17/2012 10:10:11 AM

Editor-in-ChiEf I A.J. heightman, MPA, EMt-P I [email protected] Editor I Jennifer Berry I [email protected]
AssoCiAtE Editor I Lauren hardcastle I [email protected] Editor I Allison Moen I [email protected]
AssistAnt Editor I Kindra sclar I [email protected] nEws/BLoG MAnAGEr I Bill Carey I [email protected]
MEdiCAL Editor I Edward t. dickinson, Md, nrEMt-P, fACEP tEChniCAL Editors
travis Kusman, MPh, nrEMt-P; fred w. wurster iii, nrEMt-P, AAsContriButinG Editors I Bryan Bledsoe, do, fACEP, fAAEM; Ann-Marie Lindstrom
EditoriAL dEPArtMEnt I 800/266-5367 I [email protected]
Art dirECtor I Liliana Estep I [email protected] iLLustrAtors
steve Berry, nrEMt-P; Paul Combs, nrEMt-BContriButinG PhotoGrAPhErs
Mark C. ide, Craig Jackson, ray Kemp, Kevin Link, Julie Macie, Jeffrey Mayes, Courtney McCain, rick McClure, tom Page, rick roach,
steve silverman, Chris swabb, Grant therrien, raul torres
dirECtor of eProduCts/ProduCtion I tim francis I [email protected] CoordinAtor I Matt Leatherman I [email protected]
AdvErtisinG dirECtor I Judi Leidiger I 619/795-9040 I [email protected] ACCount rEPrEsEntAtivE I Cindi richardson I 661-297-4027 I
[email protected] sALEs CoordinAtor I Elizabeth Zook I [email protected]
sALEs & AdMinistrAtivE CoordinAtor I Liz Coyle I [email protected] eMEdiA CAMPAiGn MAnAGEr I Lisa Bell I [email protected]
AdvErtisinG dEPArtMEnt I 800/266-5367 I fax 619/699-6722
MArKEtinG dirECtor I debbie Murray I [email protected] MAnAGEr I Melanie dowd I [email protected]
dirECtor, AudiEnCE dEvELoPMEnt & sALEs suPPort I Mike shear I [email protected] dEvELoPMEnt CoordinAtor I Marisa Collier I [email protected]
suBsCriPtion dEPArtMEnt I 888/456-5367
rEPrints, ePrints & LiCEnsinG I wright’s Media I 877/652-5295 I [email protected]
eMedia Strategy I 410/872-9303 I MAnAGinG dirECtor I dave J. iannone I [email protected]
dirECtor of eMEdiA sALEs I Paul Andrews I [email protected] dirECtor of eMEdiA ContEnt I Chris hebert I [email protected]
eMS today ConferenCe & expoSitionrEEd ExhiBitions I Christine ford I 203/840-5391 I [email protected]
EMs todAy ExhiBit sALEs I 203/840-5611Jeff stasko I [email protected]
elSevier publiC SafetyviCE PrEsidEnt/PuBLishEr I Jeff Berend I [email protected]
foundinG Editor I Keith Griffiths
foundinG PuBLishErJames o. Page
(1936–2004)
JOURNAL OF EMERGENCY MEDICAL SERVICES
TheConscience
of EMS
JOURNAL OF EMERGENCY MEDICAL SERVICES
TheConscience
of EMS
Choose 16 at www.jems.com/rs
010_012_STAFFBOXES.indd 10 4/17/2012 10:12:46 AM

Choose 17 at www.jems.com/rs
4C J
EM
S_1
1
FP_RT.indd 1 4/16/2012 11:06:24 AM

JOURNAL OF EMERGENCY MEDICAL SERVICES
TheConscience
of EMS
JOURNAL OF EMERGENCY MEDICAL SERVICES
TheConscience
of EMS
EDITORIAL bOARDWILLIAm K. ATKInsOn II, PHD, mPH, mPA, EmT-PPresident & Chief Executive Officer
WakeMed Health & Hospitals
JAmEs J. AugusTInE, mDMedical Advisor, Washington Township (OH) Fire Department Director of Clinical Operations, EMP ManagementClinical Associate Professor, Department of
Emergency Medicine, Wright State University
sTEvE bERRy, nREmT-PParamedic & EMS Cartoonist, Woodland Park, Colo.
bRyAn E. bLEDsOE, DO, FACEP, FAAEmProfessor of Emergency Medicine, Director, EMS Fellowship
University of Nevada School of MedicineMedical Director, MedicWest Ambulance
CRIss bRAInARD, EmT-PDeputy Chief of Operations, San Diego Fire-Rescue
CHAD bROCATO, DHs, REmT-PAssistant Chief of Operations, Deerfield Beach Fire-Rescue Adjunct Professor of Anatomy & Physiology, Kaplan University
J. RObERT (ROb) bROWn JR., EFOFire Chief, Stafford County, Va., Fire and Rescue Department Executive Board, EMS Section,
International Association of Fire Chiefs
CAROL A. CunnIngHAm, mD, FACEP, FAAEmState Medical Director
Ohio Department of Public Safety, Division of EMS
THOm DICK, EmT-PQuality Care Coordinator
Platte Valley Ambulance
mARC ECKsTEIn, mD, mPH, FACEPDirector of Prehospital Care, Los Angeles County/
USC Medical CenterMedical Director, Los Angeles Fire DepartmentProfessor, Emergency Medicine,
University of Southern California
CHARLIE EIsELE, bs, nREmT-PFlight Paramedic, State Trooper, EMS Instructor
bRuCE EvAns, mPA, EmT-P Deputy Chief, Upper Pine River Bayfield Fire Protection, Colorado District
JAy FITCH, PHDPresident & Founding Partner, Fitch & Associates
RAy FOWLER, mD, FACEPAssociate Professor, University of Texas Southwestern SOMChief of EMS, University of Texas Southwestern Medical Center Chief of Medical Operations,
Dallas Metropolitan Area BioTel (EMS) System
ADAm D. FOx, DPm, DOAssistant Professor of Surgery,
Division of Trauma Surgery & Critical Care, University of Medicine & Dentistry of New Jersey
Former Advanced EMT-3 (AEMT-3)
gREgORy R. FRAILEy, DO, FACOEP, EmT-PMedical Director, Prehospital Services, Susquehanna HealthTactical Physician, Williamsport Bureau of
Police Special Response Team
JEFFREy m. gOODLOE, mD, FACEP, nREmT-PAssociate Professor & EMS Division Director,
Emergency Medicine, University of Oklahoma School of Community Medicine
Medical Director, EMS System for Metropolitan Oklahoma City & Tulsa
KEITH gRIFFITHsPresident, RedFlash GroupFounding Editor, JEMS
DAvE KEsEg, mD, FACEPMedical Director, Columbus Fire Department Clinical Instructor, Ohio State University
W. Ann mAggIORE, JD, nREmT-PAssociate Attorney, Butt, Thornton & Baehr PCClinical Instructor, University of New Mexico,
School of Medicine
COnnIE J. mATTERA, ms, Rn, EmT-PEMS Administrative Director & EMS System Coordinator,
Northwest (Illinois) Community Hospital
RObERT J. mcCAugHAnChief, City of Pittsburgh EMS Chair, IAEMSC Metro Chief’s Section
RObIn b. mcFEE, DO, mPH, FACPm, FAACTMedical Director, Threat Science Toxicologist & Professional Education Coordinator,
Long Island Regional Poison Information Center
mARK mEREDITH, mDAssistant Professor, Emergency Medicine and Pediatrics,
Vanderbilt Medical Center Assistant EMS Medical Director for Pediatric Care,
Nashville Fire Department
gEOFFREy T. mILLER, EmT-PDirector of Simulation Eastern Virginia Medical School,
Office of Professional Development
bREnT myERs, mD, mPH, FACEPMedical Director, Wake County EMS SystemEmergency Physician, Wake Emergency Physicians PAMedical Director, WakeMed Health & Hospitals Emergency
Services Institute
mARy m. nEWmAnPresident, Sudden Cardiac Arrest Foundation
JOsEPH P. ORnATO, mD, FACP, FACC, FACEPProfessor & Chairman, Department of Emergency Medicine,
Virginia Commonwealth University Medical CenterOperational Medical Director, Richmond Ambulance Authority
JERRy OvERTOn, mPAChair, International Academies of Emergency Dispatch
DAvID PAgE, ms, nREmT-PParamedic Instructor, Inver Hills (Minn.) Community CollegeParamedic, Allina Medical TransportationMember of the Board of Advisors,
Prehospital Care Research Forum
PAuL E. PEPE, mD, mPH, mACP, FACEP, FCCmProfessor, Surgery, University of Texas
Southwestern Medical CenterHead, Emergency Services, Parkland Health & Hospital SystemHead, EMS Medical Direction Team,
Dallas Area Biotel (EMS) System
DAvID E. PERssE, mD, FACEPPhysician Director, City of Houston Emergency Medical Services Public Health Authority, City of Houston Department. of Health
& Human ServicesAssociate Professor, Emergency Medicine, University of Texas
Health Science Center—Houston
JOHn J. PERuggIA JR., bsHus, EFO, EmT-P Assistant Chief, Logistics, FDNY Operations
EDWARD m. RACHT, mDChief Medical Officer, American Medical Response
JEFFREy P. sALOmOnE, mD, FACs, nREmT-PAssociate Professor of Surgery,
Emory University School of MedicineDeputy Chief of Surgery, Grady Memorial HospitalAssistant Medical Director, Grady EMS
KATHLEEn s. sCHRAnK, mDProfessor of Medicine and Chief,
Division of Emergency Medicine, University of Miami School of Medicine
Medical Director, City of Miami Fire RescueMedical Director, Village of Key Biscayne Fire Rescue
JOHn sInCLAIR, EmT-PInternational Director, IAFC EMS SectionFire Chief & Emergency Manager, Kittitas Valley Fire & Rescue
COREy m. sLOvIs, mD, FACP, FACEP, FAAEmProfessor & Chair, Emergency Medicine,
Vanderbilt University Medical CenterProfessor, Medicine, Vanderbilt University Medical CenterMedical Director, Metro Nashville Fire DepartmentMedical Director, Nashville International Airport
bARRy smITH, EmT-PCQI Coordinator, Regional EMS Authority (REMSA), Reno, Nev.
WALT A. sTOy, PHD, EmT-P, CCEmTPProfessor & Director, Emergency Medicine,
University of PittsburghDirector, Office of Education,
Center for Emergency Medicine
RICHARD vAnCE, EmT-PCaptain, Carlsbad Fire Department
JOnATHAn D. WAsHKO, bs-EmsA, nREmT-P, AEmDAssistant Vice President, North Shore-LIJ Center for EMSCo-Chairman, Professional Standards Committee,
American Ambulance AssociationAd-Hoc Finance Committee Member, NEMSAC
KEITH WEsLEy, mD, FACEPMedical Director, HealthEast Medical Transportation
KATHERInE H. WEsT, bsn, mED, CICInfection Control Consultant,
Infection Control/Emerging Concepts Inc.
sTEPHEn R. WIRTH, Esq.Attorney, Page, Wolfberg & Wirth LLC.Legal Commissioner & Chair, Panel of Commissioners,
Commission on Accreditation of Ambulance Services (CAAS)
DOugLAs m. WOLFbERg, Esq.Attorney, Page, Wolfberg & Wirth LLC
WAynE m. ZygOWICZ, bA, EFO, EmT-PEMS Division Chief, Littleton Fire Rescue
12 JEMS MAY 2012
010_012_STAFFBOXES.indd 12 4/17/2012 10:12:53 AM

>> Photos AssociAted PressEMS IN ACTIONscene of the month
14 JEMS MAY 2012
Providers from Southwest Ambulance prepare to initiate the transfer of U.S. Rep. Gabrielle Giffords (D-Ariz.) to
TIRR Memorial Hermann Rehabilitation Hospital in Houston on Jan. 26, 2011. Providers use extreme caution to provide follow-up treatment for Giffords’ critical head injury after she was shot at a Congress On Your Corner event at a Safeway shopping center outside of Tucson, Ariz. This high-profile case serves as a reminder to EMS providers that they’re never able to predict what patients they may have the opportunity to treat or trans-fer. Thanks to the excellent care delivered to Giffords and the team effort between law enforcement and EMS, Giffords was transported in a safe and coordinated manner and has made outstanding progress in her recovery.
HIgH-PROfIlE cAre
014_015_EMSinAction.indd 14 4/17/2012 10:13:38 AM

To truly understand the importance of the content in the May 2012 issue of JEMS, which focuses on updating the
training and equipment carried by law enforce-ment officers in your EMS system, I’d like you to watch a gut-wrenching clip from the 1988 movie, In the Line of Duty. The clip is only eight minutes long, but I think those eight minutes will be some of the most stressful, and emo-tionally-charged of your career.
The clip shows a firefight that occurred on the streets of Miami on April 11, 1986, between eight FBI agents and two known murderers/bank robbers: Michael Platt and William Matix. Before the fight was over, multiple FBI agents were killed by .223 gunshots from a Ruger mini-14 in the hands of Michael Platt.
The brave FBI agents who were engaged in this street battle were not armed with weapons or ammunition that could make the most pro-nounced impact on their targets. Platt himself had sustained 12 gunshot wounds (9 mm, .38 and 00 shot) but continued to fight.
This firefight and the resulting aftermath resulted in dramatic changes in the way we equip law enforcement officers. It was the gen-esis of the 10 mm and .40 S&W rounds and use of more advanced weaponry by law officers.
When I watched this powerful docudrama in 1988, it dramatically affected me as an edu-cator and EMS system planner. It also sig-nificantly changed the way I thought about the EMS/law enforcement interface and the need for better frontline care by (and for) police officers and other members of the emergency response family.
At this year’s National Association of EMS Physician Conference in Tucson, Ariz., in January, I heard a hidden message during a keynote lecture by Brad Bradley, EMT-P, of the Northwest Fire Rescue District, and Joshua B. Gaither, MD, of the University of Arizona Medical Center, on the mass shoot-
ing near Tucson involving Congresswoman Gabrielle Giffords (D-Ariz.)
Gaither pointed out that the Pima County Sheriff’s Department deputies who were in the initial hot zone arresting the would-be assassin and ensuring scene safety, used the recently updated EMS training and small specialized law enforcement Individual First Aid Kits (IFAKs) to treat 14 of the 19 surviving victims.
In the early stages of this incident, the depu-ties retrieved their IFAKs, carried conveniently behind the front headrest of their police cruis-ers, and used tourniquets and hemostatic clot-ting agents to control significant bleeding and prevent the onset of shock. They also used chest seals to seal open wounds and combat tension pneumothorax.
It was a subtle statement that begged for more explanation. So I contacted David Kleinman, a detective with the Arizona Department of Public Safety and a tactical
paramedic with Pima Regional SWAT. I learned that Kleinman had developed a spe-cialized training program, called The First Five Minutes, which was adopted by the Pima County Sheriff’s Department.
That training, plus the up-to-date medical supplies they carried in each patrol vehicle, allowed the Pima County deputies to have a major effect on the survival of many of the victims at the Safeway shooting scene. The content involved the most up-to-date treat-ment and supplies for hemorrhage control and shock abatement.
Military research on the care rendered to crit-ically injured soldiers in Iraq and Afghanistan
has shown that if you combat and control hemorrhage before the onset of shock, mortality decreases significantly.1 So this training for law enforcement officers was not just up-to-date, but it was also timely.
I asked David to write an article for this month’s JEMS that detailed the training and how it was used effectively to keep many of the critically injured victims alive on Jan. 8, 2011. We found that several other innovative law enforcement initiatives were implemented in 2011 to train and equip officers to save themselves when injured, save their colleagues and save citizens during natural or man-made disasters and mass casualty incidents. It was clear to us that this new wave of updated train-ing was significant and worthy of our atten-tion, and yours.
The strong message for fire and EMS agen-cies is that law officers are often on the front lines long before fire and EMS units arrive. Please follow this educational trend, work to have updated training provided to the law offi-cers in your service area, and “arm” each officer with the essential equipment they need to save their lives and others.
The contents I believe each patrol officer should carry in a compact gear pouch include: >> 4"compressiondressing; >> Hemostaticclottingagentdressing; >> Tacticaltourniquet; >> Chestseal; >> 3x3x2(gauzesponges); >> 4-1/2"Kerlixsterilerollbandages; >> 1"Transporesurgicaltape; >> Traumashears; >> Ventilationmask; >> ThreepairofNitrilegloves;and >> SAMSplint
The cost per kit is less than $100—but it’s a small investment to save an officer or civilian when time is critical. JEMS
RefeRences1. KraghJ,LittrellM,JonesJ,etal.Battlecasualtysurvival
withemergencytourniquetusetostoplimbbleeding.JEmergMed.2011;41(6):590–597.
fRom the editoRputting issues into perspective
>> by A.J. HeigHtMAn, MpA, eMt-p
16JEMS MAY 2012
Go to www.youtube.com/watch?v=lBGfKtuo2Am
Contents of the Pima County Sheriff’s Dept IFAK.
On the FrOnt LIneS Updatingthetraining&carecapabilitiesoflawofficers
pHo
to M
Att
Hew
str
Au
ss
016_Editor.indd 16 4/20/2012 11:57:48 AM

LETTERSin your words
18 JEMS MAY 2012
SELf DEfEnSEI definitely think we should be prepared for any harmful situation. I was involved in a situation that went bad fast. I was assaulted by a patient who was on numerous illegal drugs. Initially, he presented with hypoglycemic symptoms, but after loading him into the unit, he began to exhibit signs of paranoia and hallucinations. Luckily, the police department was on scene, but unfortunately he had a chance to grab me.
It took the fast thinking of the officer to physically make him release his hold on me, and for my partner to administer Versed, which did absolutely nothing, to get me freed. It happened so fast, so I agree that it would have been helpful if I’d known some self defense. That way, I would have known how to break the death grip he had on me when he wrapped his legs around me, with-out injuring him. He not only physically harmed me, but he also made me lose the trust I had prior to that day.
Misty BortzVia Facebook
Like I was taught, I don’t plan to fight; I plan to end it. And I’m not referring to irrational, overdose or dementia patients. I’m referring to the rational patients who might turn on us one day. Everyone is always happy to see EMS. Cops are always immediately on hand and helpful, and happy endings are guaranteed, right? The truth is, you never know when something might happen. I believe in doing no harm first and foremost. I also believe in com-ing home safe and in one piece after every shift.
Heather Gaff MewisVia Facebook
While I was responding to a code orange (a suicidal psych patient), who had just been struck by a vehicle in an attempt to take his life after assaulting his mother in her home, police and sheriff were on scene as my unit arrived. I’ve done mixed martial arts for a few years, and when three law enforcement officers and one of my two partners couldn’t restrain the patient, I fell back on
my own training to ensure scene safety by doing what the rest on scene couldn’t.
I wrapped the patient up in a Brazilian Ju Jitsu hold. Once I had him fully restrained, the officers assisted in putting restraints on the man while they systematically strapped both me and the patient to the backboard. After we were both strapped in and he was much better restrained, they loosened one strap at a time, so I could slip my limbs out and prepare the patient for transport. If a patient’s aggression causes this kind of situation, knowing how to defend yourself is literally a lifesaver.
Joe LeeVia Facebook
AmiSh PERSPEcTivEAs a former EMT with Lancaster EMS as well as Strasburg EMS, I’ve worked with several of the Amish EMTs, and I must say they’re very dedicated and caring for the entire community—not just their own people. The area that they cover is a large tourist area, and they work well
with people from all over the country and from all walks of life.
However, treating the Amish themselves can be a real challenge. I ran on a call for a child with a trau-matic injury after being kicked by a horse. My partner and I wanted to fly the child to a nearby hospital, but the family said ‘no helicopter; just take the patient to the hospital and let God decide the outcome.’ As a healthcare provider, sometimes they do tie your hands as far as treatment and transport go.
James AdamsVia Facebook
I work in northeast Indiana, and we have a large Amish population. We have a very good relationship with them, perform occasional safety days for them and have several medics who travel to Amish schools with an ambulance to interact with the kids. We have several EMTs and medics who grew up Amish, which is helpful for speaking with the young kids who don’t speak English. As mentioned, there are sometimes differences in opinions, as far as flying patients (they strongly prefer not to use the helicopter), and they definitely don’t call unless things are very serious. The one thing you can always count on, with the Amish, though, is that they’re very grateful for our help and are supportive of what we do. JEMS
Julie ShoemakerVia Facebook
Do you have questions, comments or concerns about recent JEMS or JEMS.com articles? We’d love to hear from you. E-mail your letters to editor.jems@
elsevier.com or send to 525 B St. Suite 1800, San Diego, CA 92101, Attn: Allison Moen.
This month, Facebook users chime in on “EMS Providers Should Train like Fighters,” a JEMS.com article by fitness col-umnist John Amtmann, EdD, on why it’s important for EMS pro-viders to train for the worst-case scenario. Would you be prepared to defend yourself? Also, users share feedback on a March JEMS article by Bryan Bledsoe, DO,
FACEP, FAAEM, on EMS in the Pennsylvania Amish community (“Simple Way of Life: EMS in Amish country”).
Pho
to is
toc
kPh
oto
.co
m
illu
stra
tio
n s
tev
e be
rry
Due to graphic content,rubbernecking
discretion is advised.
018_Letters.indd 18 4/20/2012 11:58:45 AM

Speaker: Rob Lawrence
Sponsored by:
With content from writers who are EMS professionals in the field, JEMS provides the information you need on clinical issues, products and trends.
Available in print or digital editions!
Giving you the detailed product information you need, when you need it. We collect all the information from manufacturers and put it in one place, so it’s easy for you to find and easy for you to read. Go to www.jems.com/ems-products
Your online connection to the EMS world, jems.com gives you information on:
• Products• Jobs• Patient Care• Training• Technology
Sign up now for the weekly JEMS.com eNewsletter. Get breaking news, articles and product information sent right to your computer. Read it on your time and stay ahead of the latest news!
jems.com eNewsletter Product Connect
jems.com Websitejems, journal of emergency medical services
Watch live or in the
archives!
Go to www.jems.com
Comprehensive, Credible, Educational...
JEMS Products Help You Save Lives.
n ems strategies for Improving Cardiac Arrest survival may 21 2012, at 1 p.m. eT/10 a.m. PT n Drug shortage Action Plans for emsn Are You Bagging the Life Out of Your Patients?n statewide Trauma system enables multi-Agency Coordination with Trauma Centers to Improve Patient Outcomes
4 NeW WeBCAsTs! Register at jems.com/webcasts.
Sponsored by:
Sponsored by:
Sponsored by:
JEMS FOP May2012 FP.indd 1 4/16/2012 1:42:43 PM

L ook out, Washington, here comes EMS. Paramedics and EMTs from across the coun-
try went to the hill for the third time to talk to members of Congress about what’s important to the EMS community and its patients.
There’s only so much that can be done on the local and state lev-els. Federal funding and guidance is needed in some areas. And that’s why we saw the third EMS on the Hill Day, hosted by the National Association of Emergency Medical Technicians (NAEMT).
Legislators have to hear from their constituents if there’s any chance of them understand-ing what’s going on outside of Washington. EMS providers go to talk to their representatives and sen-ators about what they see as a non-partisan issue: providing quality care to their patients.
NAEMT President Connie Meyer, EMT-P, EMS captain for Johnson County Med-Act in Olathe, Kan., was excited about this year’s EMS on the Hill Day. She says they expected 190–200 EMS personnel to attend—up from 145 in 2011. Something new this year was a partnership with the American Ambulance Association (AAA). AAA participation replaced their regular lobby day.
EMS on the Hill Day attendees were invited to participate in AAA’s Reimbursement Task Force meeting on Tuesday afternoon, March 20, for discussions on reimbursement issues, healthcare reform, Medicare ambulance relief and other emergent topics.
Tuesday evening included a pre-visit brief-ing with the opportunity for attendees to mingle and see old friends or network with new contacts.
Wednesday morning, the visits to Congressional offices began. Armed with their talking points (more on that below), EMS professionals met with their representa-
tives and senators or staffs. The meetings not only gave EMS personnel the chance to speak of legislature issues that touch them profes-sionally and personally, but they also allowed the legislators the opportunity to learn more about EMS. During a previous visit, one staffer asked, “So you’re not a fire man?”
And the knowledge exchange has already led to an event that Meyer characterized as “huge.” What she’s referring to is a request from a federal legislator for NAEMT input on a bill being written. An elected official in Washington came to NAEMT for advice.
While visiting the Congressional offices, attendees have talking points, supplied by NAEMT. This year’s issues include the fol-lowing talking points:
>> The Medicare Ambulance Access Preservation Act of 2011 to provide for a more permanent solution to below-cost Medicare ambulance reimbursement;
>> The extension of death and other ben-efits under the Public Safety Officers’ Benefits (PSOB) program to non-profit, nongovernmental paramedics and EMTs who die or are severely injured in
the line of duty; and>> The legislation to establish new
EMS grant programs; enhance research initiatives; and promote high-quality, innovative and cost-effective field EMS.
To assist active members in attend-ing EMS on the Hill Day, NAEMT awarded grants of up to $1,200 each to four active members.
One of the grant recipients was Jason Scheiderer, EMT-P, of Indianapolis, Ind. He’s employed by Indianapolis EMS and teaches paramedic courses at Indiana University-Purdue University Indianapolis. Scheiderer has advo-cated for local issues, walking the fine line between concerned taxpayer and public employee. NAEMT’s state advocacy coordinator for Indiana, Scheiderer appreciates NAEMT’s focus
on improving EMS on a grand scale. “Not getting into local issues like fire department vs. private EMS providers,” he says.
W. Mike McMichael III, EMT-B, and 2011 NAEMT grant recipient from Delaware, returns to Washington for the 2012 event. McMichael says, “I’m tickled to death to be involved” in this endeavor that “will help everyone in the country.” Although he personally knows his representative and Delaware’s two senators, he liked the oppor-tunity to see them working.
On May 4, 2011, in Washington, D.C., 145 EMS professionals from 39 states and the District of Columbia and Puerto Rico met with more than 217 U.S. Senators, House Representatives and their congressional staff at the second annual EMS on the Hill Day.
The fourth EMS on the Hill Day is tenta-tively scheduled for the first week in March 2013. That would coincide with 2013 EMS Today, so you could attend both on one plane ticket.
Mark your calendar and watch the NAEMT site for more details in the months to come.
—Ann-Marie Lindstrom
PRIORITY TRAFFICNEWS YOU CAN USE
20 JEMS MAY 2012
NAEMT hosts third-annual event EMS on the HILL
For more of the latest EMS news, visit jems.com/news
phO
tO d
rEA
mSt
imE.
CO
m
020_022_Ptraffic.indd 20 4/17/2012 10:15:26 AM

www.jems.com mAY 2012 JEMS 21
Mardi Gras No Party for EMs
New Orleans EMS responded to more than 2,000 calls during a 10-day
period in February. That’s 67 more than
their normal activity. Despite
all the strange weather across the
country this winter, the increased call volume in New Orleans wasn’t because of hurricanes or other natural disasters.
It was Mardi Gras—definitely a man-made, and perhaps unnatu-ral, event. Weeks of reveling take their toll on the thousands of residents and tourists who show up for the 60 Krewe parades and other celebrations.
Deputy Chief of EMS Ken Bouvier says, “Obviously, there’s a lot of alcohol poisoning.” Perhaps, not unrelated, there are also falls from ladders and balconies in the French Quarter.
Bouvier says their transportation fleet included 25 ambulances, six Fast Cars, an ASAP mini-ambulance, two bicycles and an 18-stretcher mobile ambulance bus.
The parade route is approximately 60 city blocks, according to Bouvier. “We try not to cross parades, so we have staff on both sides of the streets.”
The Red Cross saw about 1,000 patients in its four first aid tents. The tents were staffed with six to eight volunteers ready to treat such minor complaints as sprains, foreign objects in the eye or requests for a Band-Aid. Red Cross first responders also wandered through the crowds keeping an eye open for anyone in need of medical assistance. Armed with radios, the first responders called EMS as needed.
Bouvier characterized this year’s Mardi Gras as “well attended” without violence along the parade route—evidently that’s notewor-thy when you talk about Mardi Gras.
PlaNNiNGPlanning is paramount for a city-wide, three-week celebration. Bouvier says they start planning for the next year about a week after Mardi Gras ends. They look at the statistics and reports to see what worked and what could be improved. For example, the city made more use of the Red Cross this year, “because it works,” says Bouvier. The mini ambulance and bike teams are new additions, too.
As Mardi Gras draws near, New Orleans EMS has to make sure it has enough medications on hand, enough staff ready to work—for-get about ever getting time off to enjoy the festivities with your family or friends—and enough ambulances ready to roll.
Next year’s Mardi Gras will be an enhanced challenge, says Bouvier. New Orleans hosts Super Bowl XLVII on February 3, 2013, so the city has decided to split up the Mardi Gras events to bookend the Super Bowl. That is, there will be a week of Mardi Gras celebra-tion, a week devoted to Super Bowl activities and then another week of Mardi Gras.
Bouvier says they will be ready. And they’ll all probably be ready for a long vacation in March. —Ann-Marie Lindstrom
pho
to d
rea
mst
ime.
co
m
Choose 20 at www.jems.com/rs
020_022_Ptraffic.indd 21 4/17/2012 10:17:58 AM

22 JEMS MAY 2012
>> continued from page 21
Check out all the upcoming free webcasts JEMS has to offer: www.jems.com/webcasts
2012 NatioNal EMS MEMorial BikE ridEThe National EMS Memorial Bike Ride (NEMSMBR) is gearing up for the 2012 Ride, with routes beginning in Boston, Mass., or Paintsville, Ky., on May 19—both finishing in Alexandria, Va., on May 25.
During the ride, participants will travel through the states of Massachusetts, Kentucky, Rhode Island, Connecticut, New York, New Jersey, Pennsylvania, Maryland and Virginia.
“To see these parts of the United States on a bicycle is such a unique perspective,” says Tim Perkins, NEMSMBR public information officer.
“It’s also great to interact with the pro-viders and agencies along the route, not to mention the reason for the ride: honoring over 30 individuals who have given the ultimate sac-rifice providing EMS care,” says Perkins.
Additional rides are scheduled for Colorado in June and Louisiana in September.
QUiCk taKe
For more information about the bike ride,
visit www.muddyangels.com.
T he healthcare industry has come a long way since Health Insurance Portability and Accountability Act (HIPAA) went into effect almost a decade ago. For the most part, EMS providers now have a much bet-
ter understanding of how HIPAA applies to their day-to-day operations. Nevertheless, many “HIPAA myths” still exist. Here are some of the top myths in the EMS industry today.
>> MyTh: hIPAA prevents EMS agencies and facilities from sharing patient information.
All healthcare providers should know that HIPAA permits them to freely share patient information for treatment-related purposes. That means that facilities can give EMS providers medical records about patients, and crews can look at those records for treatment purposes. It doesn’t matter that another provider created the medical record.
Ambulance services may also provide a copy of their trip reports to facilities because such practice would also fall under the “treatment” umbrella. Under HIPAA, “treatment” includes the provision, coordination and management of healthcare between providers.
>> MyTh: Law enforcement offi-cers are automatically enti-tled to patient information.
Many EMS providers believe that if a law enforcement official asks for information about a patient, they’re automatically entitled to it. Although there are circumstances under which ambulance services may release patient informa-tion to law enforcement, there’s no general provi-sion in HIPAA that broadly permits providers to release patient information to law enforcement. To the contrary, providers can only give patient information to law enforcement officials under specific circumstances.
If an ambulance service receives a request for healthcare information from law enforcement, the service must check to see whether HIPAA contains a specific exception that permits the release of the information. Some of the more common exceptions include reporting a crime in an emergency or disclosures that are required by state law (e.g., gunshot wounds and dog bites). Check with your HIPAA privacy officer before you release information to law enforcement. If you improperly disclose information, you risk violating HIPAA, and that information might not be allowed to be introduced as evidence because it was improperly obtained.
>> MyTh: It’s OK to post as long as the patient isn’t identified.EMS providers have a legal and ethical duty to refrain from posting any “protected health information”
(PHI) on the Internet. Most of us know that PHI is anything that could directly identify a patient. However, what many fail to consider is that some information might reasonably identify a patient, even though it doesn’t mention a patient by name. The bottom line is that if someone reading the post might be able to figure out who the patient is, the information might be PHI, and posting it could violate HIPAA.
For example, a post stating, “Was on a pretty crazy trauma on I-95 tonight … that guy had no shot,” might convey enough information to enable friends or family members of the deceased patient to identify him because they undoubtedly know about the incident.
Because others can determine the identity of the patient from the limited information provided, this post improperly divulges PHI. Generally, no legitimate reasons justify posting any information about a patient on the Internet. Moreover, it’s unethical—and unprofessional—to refer to a patient, in any manner, on the Internet.
DEbunKIng HIPAA MytHs
Pro Bono is written by attorneys Doug Wolfberg, Ryan Stark and Steve Wirth of Page, Wolfberg & Wirth LLC, a national EMS-industry law firm. Visit the firm’s website at www.pwwemslaw.com for more EMS law information.
pho
to d
rea
mst
ime.
co
mEMS providers travel across the country for the national EMS Memorial bike Ride.
pho
to c
ou
rtes
y n
emsm
Br
020_022_Ptraffic.indd 22 4/20/2012 11:59:37 AM

LEADERSHIP SECTORpresented by the iafc ems section
>> by gary ludwig, ms, emt-p
24 JEMS may 2012
We’re familiar with the usual type of leadership that a manager at IBM, Bank of America or the cor-
ner grocery store shows when managing their operation and people. Usually these manag-ers mistakenly try to manage people when they should be leading people. The impor-tant thing to remember is that we manage things and we lead people. We manage budgets, inventory and fleets.
It’s rare that the manager working at IBM, Bank of America or the corner grocery store need to lead people in a crisis. That isn’t true for the EMS manager. Not only do they have to lead people under normal everyday con-ditions, but they also may be asked to show their leadership during high-intensity events, such as tornadoes or mass-casualty incidents. EMS managers may be thrust into a leader-ship role during an active shooter attack.
The leadership skills that an EMS manager must exhibit during a crisis are much differ-ent from the leadership skills that they use in their day-to-day operations. In their day-to-day office operations, they have the abil-ity to sit back and use discretionary time to make a decision. If someone comes into their office with a problem, the EMS manager has the luxury of requesting more information, maybe making some phone calls, sitting on it overnight or even checking with their boss before they make a decision.
Unfortunately, that isn’t the case on the scene of an active shooter or a bus crash. Sometimes split-second decisions must to be made. Sometimes decisions have to be made with limited information. And sometimes the EMS manager may have to make some tough decisions that have a direct affect on someone’s life. The leadership skills that an EMS manager must show during these criti-cal times are crucial.
LEADERSHIP TIPSIn my opinion, one of the finest examples of leadership was former New York City Mayor Rudolph Giuliani’s management of
9/11. Don’t forget, the U.S. president was sheltered away until late in the evening to protect the head of our federal government. President Bush wasn’t seen on television; it was Giuliani who became the face of reassur-ance on television for the American people. But 9/11 wasn’t the only time Giuliani was thrust into a crisis. He routinely showed up at emergency scenes in New York City.
Giuliani describes four steps for crisis lead-ership in his book Leadership. “It is in times of crisis that good leaders emerge,” he says.
He says the first step is to be visible. Giuliani says, “While mayor, I made it my policy to see with my own eyes the scene of every crisis so I could evaluate it firsthand.”1
Who can forget those scenes of Mayor Giuliani walking on the streets of New York with his contingent of staff and department heads while being interviewed by the news media? EMS managers must respond to scenes and take charge of their operation. Many times, they fall into the incident man-agement structure. Although they may not have overall command of an event, EMS managers are still responsible for the medical operations branch.
Giuliani’s second step is to be com-posed. He writes in his book, “Leaders have to control their emotions under
pressure. Much of your ability to get people to do what they have to do is going to depend on what they perceive when they look at you and listen to you. They need to see someone who is stronger than they are, but human, too.”
Many times in my career I’ve seen an inci-dent commander yell or even scream into a radio. Yelling on the radio or at employees on a scene, or giving an appearance of being out of control, is a prescription for crisis—the situation EMS managers are trying to control.
Giuliani’s third step is to be vocal. He writes, “I had to communicate with the public to do whatever I could to calm people down and contribute to an orderly and safe evacua-tion [of lower Manhattan].”
EMS managers must demonstrate the same trait during a high-intensity event. You need to be able to give people firm directions and instructions. You need to give your employees or others clear and concise instructions or action steps.
Giuliani’s fourth step to crisis leadership is to be resilient. Giuliani describes himself as an optimist. With his words during some of his press conferences about 9/11, he gave Americans hope that they would meet this challenge and overcome it.
EMS managers must also show the same resiliency. They demonstrate through actions and words that whatever the challenge that the EMS organization and its employees are facing, they’ll be able to deal with it.
And, most importantly, always remember there are times to demonstrate everyday lead-ership and times during emergencies that you have to demonstrate true leadership skills. JEMS
REfEREnCES1. Giuliani R: Leadership. Hyperion: New York, 2002.
Gary Ludwig, MS, EMT-P, is a deputy fire chief
with the Memphis (Tenn.) Fire Department.
He has 34 years of fire and rescue experi-
ence. He’s chair of the EMS Section for the
International Association of Fire Chiefs and
can be reached at www.garyludwig.com.
Crisis ManaGeMentRudy Giuliani advocates for managing things, not people
‘It is in times of crisis that good leaders emerge.’
024_Leadership.indd 24 4/17/2012 10:18:35 AM

Choose 22 at www.jems.com/rs
FP_RT.indd 1 4/16/2012 4:07:25 PM

FP_LFT.indd 1 4/16/2012 11:39:07 AM

If a call for a mass casualty incident (MCI) goes out in northern New Jersey, there’s
a good chance James Pruden, MD, the med-ical director for emergency preparedness at St. Joseph’s Regional Medical Center, is going for a ride.
Pruden is part of a breed of physicians who are just as comfortable working outside of the confines of an emergency department (ED) as they are in the field—where they can be more helpful controlling a scene.
“There’s a subset of physicians, wild and crazy guys, who get that surge and pleasure being out there in the environment,” says Pruden, who heads up St. Joseph’s Emer-gency Physician Response Vehicle pro-gram, MD-2.
The St. Joseph’s program, which is part of the New Jersey EMS Task Force system, is used to respond to everything from school bus rollovers, to fires and planned events throughout the region.
The parameters for the units being dis-patched are wide open, but the common thread is that the doctors responding are dif-ferent from their hospital-bound brethren.
“It’s not just about having an emer-gency physician,” says Scott Matin, vice president of Mobile Health Services at the Monmouth Ocean Hospital Services Cor-poration (MONOC), which also launched mobile physician unit MD-1 in January.
MONOC’s MD-1 unit is headed by Mark Merlin, MD, a new member of MONOC’s Medical Advisory Board, chair of the EMS/Disaster Medicine Fellowship at Newark Beth Israel Medical Center and medical director of the New Jersey EMS Task Force. MD-1 is stationed with Merlin or a member of his team.
“It’s about having someone with emer-gency experience. It is different doing something in the emergency room than it is having to do it in the field. You’re not on
a table, but in the back of [a] crashed upside down vehicle,” says Matin.
And that’s where the mobile physicians’ units come into play, especially at times when there may be an MCI or some other incident in which the scene could use a physician on hand.
In some ways, the MD units are a “force multiplier,” says Robert J. Bertollo, MICP, LRCP, MBA, the program man-ager of Life Support Education and Emer-gency Response Operations for St. Joseph’s Regional Medical Center.
St. Joseph’s Regional Medical Center has operated an MD unit for two years that was funded through the Urban Areas Security Initiative. Pruden recalls a scenario a few years ago—before MD-2 existed—during which employees at a local factory were overcome by a chemical odor that trav-eled through the building. There were hun-dreds of potential patients involved, and 50
www.jems.com mAY 2012 JEMS 27
EmErgEncy physicians assist thEir prEhospital countErparts >> By RichaRd huff, NREMT-B
ManageMent Focus
The medical director units that arrive on-scene with a physician are especially beneficial during mass casualty incidents.
pho
to is
toc
kph
oto
.co
m
027_029_ManagementFocus.indd 27 4/17/2012 10:19:09 AM

28 JEMS MAY 2012
ended up being transported to local EDs. “What you can do is send the physician to the site, where you then
have the ability to express people on the scene,” Pruden says. Triage and treatment protocols could have been decided on the
scene of the factory incident, he says, altering the volume of patients sent to local hospitals.
MD Units UseThere has been an increase in the use of MD units in the field around the country in recent years. For example, besides the units in New Jersey and Erie County, New York, has a Specialized Medical Assis-tance Response Team, which is a volunteer public health emergency response organization that makes physician response available around the clock.
For the most part, the MD units are similar. They’re staffed by physicians like Pruden, who enjoy the challenge of working at an emergency scene. Typically, the medical teams operate out of non-transport-type sports utility vehicles that mimic paramedic vehi-cles—although without the required depth of supplies. Some units include equipment for on-scene surgical procedures.
The initial concept for MD vehicles in EMS responses was for the more serious patient scenarios in which extrication may severely cut into the golden hour and reduce survivability. It’s safe to say,
however, the parameters for use are evolving. Although relatively new in New Jersey, the greatest use so far has been for MCIs and pre-planned events, such as major festival concerts for which a high range of injury is likely.
“Its real worth is when there’s a physician on scene and in a med-ical control capability,” says Bertollo. In those cases, the specially trained doctors can increase the volume of patients handled on scene by taking medical control.
“When it gets to the point where you need that, a doctor can make multiple decisions,” Bertollo says.
“If you are at the scene, you can identify and quickly establish symptom protocols,” Pruden adds.
The Monmouth Ocean Hospital Service Corporation unit wouldn’t respond to the typical EMS call, but rather come into play for cases in which someone is trapped for an extended amount of time, or when there might be a need for an emergency amputation to free the patient.
“These are going to be ones where a half-hour response time still means you’re going to make it to the scene,” Matin says.
ProtocolAt St. Joseph’s, the response parameters for the MD unit have been pretty broad, Bertollo says, and often left to an on-scene agency to request the team. When the program was launched, he explains, the folks at St. Joseph’s visited regional EMS providers to familiarize them with the operation.
extra set of HanDs >> continued from page 27
In some ways, the MD units are a ‘force multiplier.’
choose 23 at www.jems.com/rs
027_029_ManagementFocus.indd 28 4/20/2012 3:03:59 PM

www.jems.com mAY 2012 JEMS 29
“You need a physician because you’ve transcended the ability of the EMTs or paramedics on scene,” he says. “We’ve had multiple patients at fire scenes, industrial accidents ... and we’ve certainly dis-patched during floods,” he adds. “Also, if there are specialty things, like a shooting or multiple-patient pediatric calls.”
There will be more use of the unit in mass casualty situations than a physician strapping on a surgical kit to do an on-scene ampu-tation or blood transfusion, says Bertollo. The dispatch operation serving St. Joseph’s has put a system into place: When something on scene seems unusual, a call goes out to the five physicians on the MD-2 team.
“Basically, what we’ve said is if you get into a circumstance where you find something unique or strange looking and the medics say, ‘we wish we had a doc out here,’ give us a call,” Pruden says.
Doing so, of course, gives the physicians in the program real-time exposure with the frontline emergency responders they normally wouldn’t see with any regularity, making everyone more comfort-able in future scenarios. Likewise, it also gives the physicians experi-ence in situations that are dissimilar from routine ED settings.
And it also expands the program beyond simply preparing EMS providers to respond to “the big one,” adds Pruden.
There are benefits to the mobile physician teams beyond responses, too. The folks at MONOC expect to use Merlin and his team in educational situations and drills.
“What’s nice about this program is, we hope in the end there is not a lot a huge need for it,” Matin says. “There are added benefits being involved with this program. We do a tremendous amount of educa-tion. Having that number of physicians at hand is a fantastic thing.”
EMS IntEractIonHaving a higher medical authority on the scene of an EMS call does raise the potential for conflicts between providers. Matin says he understands there could be concerns about how EMS provid-ers react in the field to the arrival of a physician on the scene, but it shouldn’t be a problem in this case.
“These doctors are going to be coming out on special scenes,” he says. “I can tell you the medics will be glad they’re there.”
Bertollo agrees, “They’ve integrated well. The physicians that have staffed those responses have known from the outset they’ve wanted to be an integrated player. We’re here to augment and lend support.”
Pruden goes a step further, noting the goals of the MD-2 unit are similar to why he loves disaster responses.
“It’s the unity of purpose,” he says. “In an event, when you’re responding to some critical event, you and other human beings have the same goal, to help people, to get a response, to turn this thing into the most positive outcome you can make. Frequently, those events suppressed ulterior motives. It’s amazing to work in an envi-ronment where everybody has the same goal. It’s an incredible rush to be engaged with that kind of mindset where people are working together.” JEMS
Richard Huff, NREMT-B, is an active member and the former chief of the Atlantic
Highlands (N.J.) First Aid & Safety Squad. He’s a CPR, CEVO and first aid instructor and
multi-dimensional EMS educator. He’s also an award-winning journalist and author.
choose 24 at www.jems.com/rs
027_029_ManagementFocus.indd 29 4/17/2012 10:28:19 AM

TRICKS OF THE TRADEcaring for our patients & ourselves
>> by thom Dick, emt-p
30 JEMS MAY 2012
I don’t think you can quantify everything that’s important in life. But in all of the science on which emergency medicine
has come to depend, we never seem to give up trying.
Think for a moment. We use a numeric score to rate people’s pain. (I don’t think it tells us a dang thing.) We use endless scales to measure the concentration of ions in their body fluids, the physical pressure of the blood in their vascular systems, the color of their urine, and their heart and respira-tory rates. We use scales to assess the sizes of their pupils and describe the shapes of their upper airways. We use a trauma score to predict their survival after they get hurt, and another scale to describe the severity of their burns. We imprint depth scales on the tubes we insert in their orifices. We even use numeric gradients during our runs to express the urgency of our responses to their emergencies.
We frame our lives in the same way, Life-Saver. A while back, my hometown’s pro football team (the Broncos) braced itself to take on the New England Patriots in a divi-sional championship game. The Broncos were no better than mediocre this year, but they had supposedly earned a shot at the Pats by beating the Steelers a week earlier, in the first few seconds of overtime. The media and the Bronco fans celebrated the win; although, few would have blamed the Steeler fans for believing they were robbed. The final score was 29–23.
In reality, there was only the barest margin of difference between the play of those two teams, and an objective observer would probably have awarded the win to Pittsburgh. In addition, the NFL’s history won’t reflect the fact that Pittsburgh’s great quarterback, Ben Roethlisberger, played the whole game on a painful, unstable ankle.
We seem obsessed with the numbers in our lives. We’ve developed maps to tell us the depths of the ocean, as well as its salin-ity, its temperature and how much water it
contains. We assess the effects of the wastes we pour into it by guessing how many living organisms disappear afterward. (No doubt some of us believe there are acceptable num-bers of those, too, even if we can’t possibly count them all.)
We’ve developed systems to help us enu-merate the stars, assess their color, bright-ness, size and mass, and measure how far they are from us (almost as though we still believe they revolve around us). We think we know the volume of the vast space they inhabit (even if it’s so great, we can’t compre-hend it). We’ve envisioned ourselves at the tippy-top of the hierarchy of all life, based on the complexity of our cognitive thought processes. Scholars have attempted since the fifth century to describe the value of nothing. (What a surprise: We’ve assigned a number to that, too.)
We even rate human intelligence using a numerical value. We call it IQ, for intel-ligence quotient. We discuss people in terms of their IQs, as well as their age, height, weight, body-mass index, annual income, and belt and neck sizes (as though their dimensions actually help us to understand anything about them).
The business of helping people in crisis is a lot bigger than the stuff we can measure. Measurements are simple routines, each of which typi-cally reveals no more than a single answer to a simple question. What’s the blood pressure? What’s the blood glu-
cose? What’s the pH?It’s important to respect what those
numbers tell us, but only as puzzle pieces. Whatever we do, we need to be much more focused instead on a prime number we call “one.”
Serving people is all about individuals. Taking care of them requires a willingness to admit that we don’t know much about them. But we have a persistent commitment to observe, question, examine and think. In emergency situations, we sometimes need to do all of those things at warp speed. (If anybody ever told you this EMS stuff would be easy, they altered the truth.)
Next time you kneel in front of somebody you don’t know or sit beside someone in that ambulance of yours, look them straight in the eye. No matter how ordinary they seem, how ugly or even unpleasant, ask for their name. And use it. And make sure there’s no doubt in their mind about one thing: While they’re with you, they’re important. What they say matters. And how they feel is essential. Not just any old person has the talent or the desire to do that. Those who do are called caregivers.
Are you one of those? If so, you really are special. JEMS
Thom Dick has been involved in EMS for
42 years, 23 of them as a full-time EMT and
paramedic in San Diego County. He’s currently
the quality care coordinator for Platte Valley
Ambulance, a hospital-based 9-1-1 system in
Brighton, Colo. Contact him at [email protected].
Numbers Reflections on the value of one
Our patients are much more than the numbers of their blood pressure reading or their pH level; they’re individuals.
pho
to is
toc
kph
oto
.co
m
030_Tricks.indd 30 4/17/2012 10:28:46 AM

Choose 26 at www.jems.com/rs
Choose 25 at www.jems.com/rs
pg31_RT.indd 1 4/20/2012 3:11:28 PM

CASE OF THE MONTHDILEMMAS IN DAY-TO-DAY CARE
>> BY JEff WESTIN, MD; PAT SONgER, NREMT-P, ASM; KELLY BuChANAN, MD; LOREN gOROSh, MD; RYAN hODNICK, DO; & BRYAN E. BLEDSOE, DO, fACEP, fAAEM
32 JEMS MAY 2012
Burning Man is a massive event held around every Labor Day in the Black Rock desert in northwestern Nevada.
The encampment is an official city called Black Rock City, and although it exists for only a week or so each year, it becomes the third-largest city in Nevada. The event attracts in excess of 50,000 attendees.
The purpose of Burning Man is radical self-expression in various art forms. It’s truly a one-of-a-kind event. Black Rock City operates as a functional geopolitical entity with fire, police and EMS systems. Each is dispatched from a manned com-munications center that’s constructed and deconstructed annually.
In 2011, Humboldt General Hospital EMS in Winnemucca was contracted to provide medical care for Burning Man. Medical care included a fully staffed and operational EMS system, as well as a field hospital called Rampart General and two BLS aid centers.
A total of 2,307 patients were treated. Three-hundred and eighty-two requests for ambulances were made, with 185 patients being transported to Rampart General. Only 33 patients were transported out of the desert for care. The following high-lights one of those cases that took place during the event.
REMOTE CAREOn the final day of the Burning Man event, EMS is summoned to a chest pain call in a trailer within the encampment. On arrival, paramedics find a 60-year-old male in acute distress.
He’s pale and diaphoretic and in extremis. The patient describes the pain as “tearing”
and can’t get into a comfortable position. The EMS crew extricates him from his trailer and moves him to the awaiting ambulance for a more detailed assessment.
He becomes unresponsive shortly after they place him in the ambulance. Paramedics check his pulse, take a quick look at the monitor, and note the patient is in a non-perfusing v tach. On a hunch, they administer a precordial thump, and it works. The patient converts to a sinus rhythm. He’s transported to Rampart General in Black Rock City.
Once the patient arrives at the field hos-pital, the emergency staff rapidly assesses him. He’s alert and oriented, but his blood pressure is undetectable. He’s writhing in pain on the stretcher. IV fluids are given, and his blood pressure is finally detectable at a systolic pressure of 72 mmHg and then
up to 76 mmHg. He remains mildly tachy-cardic. He receives IV fentanyl for pain. Rampart General has X-ray capabilities and a stat chest X-ray is obtained. The emer-gency physician notes that the mediasti-num is wide at 10.5 cm—consistent with a thoracic aortic aneurysm and dissection. A medical helicopter is summoned and the patient is closely monitored and stabilized by the emergency staff.
As soon as the helicopter arrives, the patient is moved to the aircraft and transported to a major medical center about 150 miles away. Once he arrives, he undergoes a computed tomography angio-gram (CTA) that confirms the suspected aortic dissection.
The patient is emergently taken to sur-gery where the aneurysm is repaired. The operation is successful, and the patient is
Miracle in the DesertCardiac case at remote Burning Man event presents challenges
>> a case froM university MeDical center in las veGas
PhO
TO C
Ou
RTES
Y B
RYA
N B
LED
SOE
Burning Man, an elaborate weeklong festival in the nevada desert, presents unique challenges to eMs providers.
032_035_Case.indd 32 4/17/2012 10:29:16 AM

www.jems.com mAY 2012 JEMS 33
moved to the intensive care unit (ICU).Following surgery, the patient suffers a second cardiac arrest
and is taken to the cardiac catheterization lab for evaluation and subsequent stenting of a coronary artery lesion. He’s returned to the ICU and remains stable. He’s discharged home with appropri-ate provisions for follow-up. Despite his ordeal, he’s already plan-ning his next trip to Burning Man.
DiscussionFirst, this is not a true “case from University Medical Center” because it didn’t happen at UMC. However, emergency physi-cians, emergency medicine residents and medical students from the University of Nevada School of Medicine provided much of the medical care at Burning Man. As you can tell, this patient had all the cards stacked against him. He had a critical thoracic aortic dissection, and he was in the middle of a Nevada desert more than 150 miles from a medical facility with cardiothoracic surgery capa-bilities. Furthermore, he suffered a cardiac arrest. Yet despite all of this, he survived.
Thoracic aortic aneurysms and dissections are life-threatening conditions that affect the thoracic portions of the aorta. An aneurysm is a dilation of an artery greater than 50% of its nor-mal diameter. They’re classified based on the region of the aorta affected (e.g., ascending aortic, aortic arch, descending aortic and thoracoabdominal), and are at risk for rupture.
A dissection results from a tear in the interior lining of the aorta (the tunica intima). This tear, referred to as an intimal tear, causes the layers of the aortic wall to separate thus forming a false lumen. The pressure from the blood within the aorta causes the false lumen to expand, or dissect.
As the dissection progresses, blood flow to various blood ves-sels is affected, causing ischemia to the tissues they supply (e.g., the coronary arteries and spinal cord). Thoracic aneurysms most commonly occur in persons older than age 65. Death from a rup-tured aneurysm is typically one of the top 10–20 causes of death annually. The incidence of thoracic aneurysmal rupture is approxi-mately 3.5 per 100,000 persons.1
Patients who develop cardiac arrest from a thoracic aneurys-mal dissection rarely survive. Furthermore, resuscitation with a precordial thump is even less common.2 Hypotension is common, and hypertension should be avoided. This patient received enough fluids to restore perfusion as determined by monitoring his men-tal status and a maintaining a systolic blood pressure between 76–78 mmHg.
Consideration was given to adding vasopressors, but because dissection was suspected, they weren’t administered. A thoracic aortic dissection is characterized by widening of the mediastinum on chest X-ray. Fortunately, limited X-ray capabilities were avail-able at Rampart General. The diagnosis was later confirmed by a CTA at the receiving hospital.
Teaching PoinTsIt’s often difficult to diagnosis aortic dissection, either thoracic or abdominal, in the prehospital setting. Because of this, EMS provid-ers must have a high index of suspicion when patients present with signs and symptoms consistent with thoracic aortic dissection. The most common presenting sign is pain—either in the chest or
choose 27 at www.jems.com/rs
032_035_Case.indd 33 4/17/2012 10:33:45 AM

www.jems.com mAY 2012 JEMS 35
between the scapulae in the upper back. With large aneurysms, the superior vena cava can be compressed, causing distended neck veins. A murmur may be heard. Sometimes hoarseness, cough and wheezing may be present. In other instances, such as this one, shock and cardiac arrest may be present.
So much of quality EMS is identifying injuries and illness in the field, recognizing the potential severity and ensuring the patient is rapidly transported to an appropriate medical facility.
The concerns of EMS crews and a presumptive field diagno-sis can also aid emergency department personnel in directing appropriate resources to critically ill or injured patients. Quality emergency physicians will listen to the concerns of field crews and react accordingly.
SummaryThis was a miraculous case that illustrates the importance of seam-less interaction between field EMS crews and physicians. First, this case occurred in one of the most austere and hostile environ-ments imaginable. Next, it included a patient who was resuscitated from pulseless v tach with a precordial thump performed by a paramedic crew. The patient was subsequently evaluated and diagnosed with a thoracic aorta dissection by medical staff in a tent (with a diagnosis made by plain chest X-ray) and emergently transported 150 miles to a hospital where successful surgery was carried out.
It truly was a “perfect storm,” or perhaps, it was the general goodwill and spirit of Burning Man. Or maybe those crystals that were everywhere actually worked. JEMS
Jeff Westin, MD, was a third-year emergency medicine resident at the University
of Nevada School of Medicine. He’s an attending emergency physician for Kaiser-
Permanente in Portland, Ore. He can be contacted at [email protected].
Pat Songer, NREMT-P, ASM, is director of EMS at Humboldt General Hospital
EMS. He can be contacted at [email protected].
Kelly Buchanan, MD, is an EMS fellow at the University of Nevada School of
Medicine. She can be contacted at [email protected].
Loren Gorosh, MD, is a third-year emergency medicine resident
at the University of Nevada School of Medicine. He can be contacted at
Ryan Hodnick, DO, is a second-year emergency medicine resident
at the University of Nevada School of Medicine. He can be contacted at
Bryan Bledsoe, DO, FACEP, FAAEM, is professor of emergency medicine at
the University of Nevada School of Medicine and director of the EMS Fellowship
Program. He is also the medical director for Burning Man. He can be contacted at
referenceS1. Rogers RL, McCormack R. Aortic disasters. Emerg Med Clin North Am.
2004;22(4):887–908.2. Haman L, Parizek P, Vojacek J. Precordial thump efficacy in termination of
inducedventriculararrhythmias.Resuscitation.2009;80(1):14–16.
>> continued from page 33
caSe Of THe mOnTH
choose 29 at www.jems.com/rs
032_035_Case.indd 35 4/17/2012 10:34:00 AM

Aguilar SA, Patel M, Castillo E, et al. Gender differences
in scene time, transport time, and total scene to hospi-
tal arrival time determined by the use of a prehospital
electrocardiogram in patients with complaint of chest
pain. J Emerg Med. 2012; Feb 15. [Epub ahead of print].
These authors retrospectively analyzed San Diego EMS charts, measuring the
effect of prehospital 12-lead ECGs on scene times. Out of 21,742 chest pain calls, no sig-nificant scene time increases or differences were found between patients with and without ST-elevation myocardial infarction (STEMI). This is nothing new; this has been studied many times. The researchers did, however, find that in STEMI cases, male patients had an average of 17-minute scene times vs. females, who had 20-minute scene times. This delay is then projected to a pos-sible increase of 0.25–1.6% greater mortality.
This study adds to a growing body of literature showing that women experiencing acute coronary syndromes receive delayed diagnosis and care. Possible explanations could include atypical presentations, delayed symptoms or comorbidities. I’ll add my own observation that performing prehospital 12-leads on women involves a certain need for tact and social privacy that may cause a delay. In any case, now that we are aware of it … let’s all try to speed up identification and care for women having STEMIs.
Waldron R, Finalle C, Tsang J, et al. Effect of gender on prehospital refusal of medical aid. J Emerg Med. 2012; Feb 9. [Epub ahead of print].
It shouldn’t be any news that patient refusals often end in adverse outcomes and con-
tinue to be a problem for EMS. I applaud these authors for discovering a new angle to this issue. This New York City project retrospectively reviewed one year’s worth of patient-care reports for a single hospital-based ambulance service. The staff at this service is made up of 82 EMTs and paramed-ics, with 67 men (82%) and 15 women (18%).
Out of 19,455 total patient encounters, 238 refusals were documented. (If this is accurate, congratulations are due on a 1.2% refusal rate. This is one of the lowest ever reported in recent literature).
Although most of the refusals came dur-ing the evening tour, no correlation was found to it being in the beginning or near the end of the crew’s shift. The authors did, however, discover that crews composed of two male providers were four times more likely to have an encounter end in a refusal when compared to a crew that had one or both female crew members.
In the discussion, the authors note that differences in communication styles between genders may lead to perceptions of behaviors demonstrating greater care by female healthcare providers.
I TreaTmenT of seIzures ISilbergleit R, Durkalski V, Lowenstein D, et al.
Intramuscular versus intravenous therapy for prehospi-
tal status epilepticus. N Engl J Med. 2012;366(7):591–600.
The much anticipated results from the Rapid Anticonvulsant Medication Prior
to Arrival Trial (RAMPART) study were published in February in the New England Journal of Medicine. The study’s main objective was to show that prehospital intramuscular (IM) midazolam (10 mg) was just as good as the in-hospital standard of care: IV loraz-epam (4 mg) for status epilepticus.
Because lorazepam has a short shelf life when it’s stored un-refrigerated, most EMS systems find it costly and impractical to
carry. Midazolam is widely used, but it hasn’t been studied well in the prehospital environment. This landmark prehospital study will likely be remembered more for its rigorous scientific methods rather than for the actual results. It’s a great example of the “gold standard” of research: double-blinded, prospective, randomized studies with great follow through to hospital discharge. The authors used some innovative and ground-breaking strategies to overcome the usual hurdles that make prehospital research so difficult.
First, the details: RAMPART involved 4,314 paramedics from 33 EMS agencies and 79 receiving hospitals across the U.S. They enrolled 893 patients and randomly assigned them to either the midazolam or the lorazepam group. Neither the patient, the paramedic nor the receiving hospital were aware of what medication was admin-istered. The results: IM midazolam stopped the seizure before hospital arrival 73.4% of the time while IV lorazepam was 63.4% effective. They conclude that midazolam is safe and effective.
Although IV lorazepam had a more rapid onset, establishing an IV in a seizing patient was widely variable. Thanks to accurate time stamps, this study clearly proves that auto-injectors allow for rapid administra-tion of medications and faster seizure ces-sation—even if the IM medication is slower to take effect. Patients who received mid-azolam were also hospitalized less often and required fewer intubations.
Now for the unique components that make this a landmark study. The authors used a special box that contained both an auto-injector and the IV medication. The paramedics were blinded to which treat-ment they were administering by having them give all patients an IM shot first, then starting an IV and giving everyone an IV bolus. All the auto-injectors and syringes looked the same, so it was impossible to tell which had active medication.
36 JEMS MAY 2012
researCH reVIeWWhat current studies mean to ems
>> by david Page, ms, nremt-P
Gender MaTTersStudy compares cardiac care for male vs. female patients
study evaluated IM vs. IV treatment.
Pho
to is
toc
kPh
oto
.co
m
036_037_ResearchReview.indd 36 4/17/2012 10:34:43 AM

www.jems.com mAY 2012 JEMS 37
David Page, MS, NREMT-P, is an educator at Inver Hills Community College and a paramedic at Allina EMS in Minneapolis/St. Paul. He’s a member of the Board of Advisors of the Prehospital Care Research
Forum. Send him feedback at [email protected].
Visit www.pcrfpodcast.org for audio commentary.
If the box contained “active” midazolam auto-injectors, then the IV bolus was a pla-cebo and vice versa. If the box had “active” lorazepam IV bolus, then the auto-injec-tor was a placebo. This is clever because many studies have shown that providers will go to great lengths (even tasting the two medications) to uncover which is the “active” medication. This often destroys the randomization process that is so critical to research.
Another interesting technique was the inclusion of an automatic, time-stamped voice recorder that was activated as soon as the box was opened. Most studies try to use the notoriously inaccurate times on the patient-care report or have providers fill out an extra piece of paper with study information—or sometimes they even have to be interviewed by telephone after the fact. The paramedics in this study could simply say what was happening, such as the “IM shot has been given” and “the seizure has stopped.” The recordings were later analyzed and the accurate time stamp extracted.
Note that Seattle’s Medic One program has measured improvements objectively for decades with voice recordings for cardiac arrest patients. This system pro-vides valuable feedback, which the crews look forward to hearing to help measure improvements objectively. The technique, however, is dependent on a cumbersome ECG monitor add-on, and it unfortunately hasn’t caught on with the rest of us. It’s too bad we appear to be more afraid of recording our errors than we are motivated to learn from them, and eventually save more lives. Congratulations to RAMPART for incorporating state-of-the-art recording boxes to get accurate data. JEMS
I glossary IPlacebo: Simulated but ineffective or inert medication replacement, such as giving injecting saline instead giving an actual medication.
VISIT OGSI at Booth 600at Disaster Relief &
Recovery Expo
Oxygen Generating Systems Intl. / www.ogsi.com / Toll Free 800-414-6474814 Wurlitzer Drive, North Tonawanda, NY 14120 / [email protected] / Phone 716-564-5165
Choose 30 at www.jems.com/rs
Choose 31 at www.jems.com/rs
036_037_ResearchReview.indd 37 4/17/2012 10:40:14 AM

38 JEMS MAY 2012
038_044_Tuscon.indd 38 4/17/2012 10:40:52 AM

Pho
to M
att
hew
Str
au
SS
www.jems.com mAY 2012 JEMS 39
>> By DaviD Kleinman, nRemT-P & Tammy KasTRe, mD
Law enforcement officers make major impact as initiaL care providers
It was an otherwise quiet morning in Pima County, Ariz., when, at 10:11 a.m. on Jan. 8, 2011, the Pima
County Sheriff’s Department received a 9-1-1 call advising of a shooting in progress at a local shopping center. During the next 20 minutes, details of a horrific and historic scene unfolded, despite the lone shooter being taken into custody within five minutes of the original 9-1-1 call.
Before it was all over, that isolated shooter had fired 30 rounds into a crowd gathered for the Congress on Your Corner event with Congress-woman Gabrielle Giffords (D-Ariz.) outside a busy Safeway grocery store
Officers who are prepared to provide care during active shooter and hostage situations can be an asset to ems.
038_044_Tuscon.indd 39 4/17/2012 10:41:07 AM

40 JEMS MAY 2012
Beyond the tape >> continued from page 39
pho
to a
SSo
cia
ted
pre
SS/
ma
tt Y
ork
on the outskirts of Tucson. Facing the arriv-ing deputies were 19 injured and/or dying people all in close proximity. Luckily, they had trained for such situations. Is your department prepared to receive a 9-1-1 call like this?
The Northwest Fire Rescue District (NWFRD) serves the suburban area of Tuc-son where the mass shooting occurred. A NWFRD paramedic rescue ambulance and three ground ambulances from South-west Ambulance were dispatched based on the initial information received by dis-patch from the initial 9-1-1 call. Three ALS engines, a ladder company and EMS Cap-tain and Battalion Chief (BC) Lane Spalla also responded on the first-alarm MCI response. Three medical helicopters were also placed on standby based on the scope of the incident.
Although the first EMS/fire units arrived on scene in just five minutes, they were held off in a safe staging area by law enforce-ment until 10:23 a.m., when the scene was declared safe for entry.
This scene was also different from many other active-shooter mass casualty incidents (MCIs) because the arriving deputies were all trained in MCI and advanced care proce-dures that enabled them to play a major role in the treatment and survival of the multiple critically wounded patients who were inside the incident hot zone prior to the secured arrival of fire and EMS responders.
In the critical minutes of an incident involving gunfire and the need to secure the scene, where patients had the potential to exsanguinate, the deputies arriving on scene were armed with special emergency care packs that were strategically positioned behind the headrest of each patrol vehicle for easy access and deployment.
During the 47 minutes that deputies were with the injured at the scene, they treated 10 of the 19 injured patients. They controlled bleeding, provided rescue breathing and chest compressions, deployed hemostatic agents, bandaged numerous wounds, and assisted citizens and congressional staffers in the care of the injured.
The first seven patients were triaged, treated and transported from the scene by 10:35 a.m. All were transported by 11:01 a.m.
The early combat and control of hem-orrhage before the onset of shock has been proven by the military in the Iraq and
Afghanistan war zones to be the key factor in preventing death from severe hemorrhage.
Emergency department (ED) physicians and trauma surgeons from Tucson’s level one trauma center University Medical Cen-ter acknowledge that the quick actions of the Pima County Sheriff Department depu-ties and their specialized training and EMS equipment resulted in decreased hemor-rhage, improved vital signs and less need for shock resuscitation for multiple victims.
InItIal FIrst respondersIt’s essential that treatment begin immedi-ately and patients be transported expedi-tiously in accordance to the severity of their injuries. And even in an urban environment,
the time it takes for EMS to arrive on scene can mean the difference between life and death for the wounded. Too often the first responder is a law enforcement officer faced with a tactical situation of providing a law enforcement function that must quickly transition into providing first care to civil-ians or a fellow officer.
The Safeway shooting happened in a geo-graphic location in Pima County that’s read-ily served by multiple paramedic units from three large fire departments. But it’s con-ceivable that this same scenario could occur with one or more of the following situa-tional complications:
>> Extended EMS unit response to a rural or remote setting;
First responders work together on Jan. 8, 2011, at the Safeway where the active shooter event happened.
Emergency personnel work together at the scene where Rep. Gabrielle Giffords, D-Ariz., and others were shot.
pho
to a
SSo
cia
ted
pre
SS/
Jam
eS p
alk
a
038_044_Tuscon.indd 40 4/17/2012 10:42:04 AM

Choose 32 at www.jems.com/rs
Choose 33 at www.jems.com/rs
pg41_RT.indd 1 4/16/2012 4:06:00 PM

42 JEMS MAY 2012
>> EMS resources committed on other high-priority calls and delayed in response or arrival;
>> Traffic congestion that delays or pro-hibits EMS access to a scene;
>> An unsafe scene that doesn’t allow fire and EMS providers to approach immediately.
Any of these complications can
significantly affect the well-being of the wounded, because the EMS provider would be markedly delayed in arrival and their ability to provide essential emergency care.
Early InvolvEmEntIn a 2007 study published in Prehospital and Disaster Medicine, the authors noted, “No widely accepted, specialized medical train-ing exists for police officers confronted with medical emergencies while under condi-tions of active threat.”1
Given the knowledge’ acquired from historical and modern battle, culminat-ing in the trauma combat casualty care (TCCC) guidelines, we know the follow-ing are causes of preventable death on the battlefield:
>> Hemorrhage from extremity wounds;>> Tension pneumothorax; and>> Airway compromise.Each of these conditions can be man-
aged early and effectively using relatively simple techniques and minimal equip-ment. Unfortunately these techniques and equipment are rarely taught to law enforce-ment officers.
Even in an urban environment, the time it takes for EMS to arrive on scene can mean the difference between life and death for the wounded. Law enforcement personnel rou-tinely are the first arriving responders to arrive at tactical situations. They are also
often the first to arrive at such mass casualty situations as major traffic collisions involv-ing multiple patients.
At tactical incidents, officers are often faced with the challenge of initiating law enforcement functions and almost simulta-neously ensuring that needed care is started on critically injured fellow officers and civilians.
Special weapons and tactics (SWAT) teams have long understood how impor-tant it is to have paramedics imbedded in their teams, immediately available for any medical need and tactically trained and aware of how to react and respond in a hos-tile or active shooter environment. Tactical EMS (TEMS) providers can readily address airway, breathing and circulation problems that create an urgency that transcends the response times of most staged civilian med-ical assistance units.
Although it’s not always practical for law enforcement agencies to employ para-medics to work in the field with officers, much can be done to train police officers to care for themselves, their colleagues and other patients.
tactIcal ParamEdIc traInIngIn the spring of 2009, the leadership of the Pima County Sheriff’s Department recog-nizing the need for global training for all staff with “feet on the street.” They took
BEyond thE taPE>> continued from page 40
pho
to c
ou
rtes
y d
av
id K
lein
ma
n
First Five Minutes trainingThe concept of training law enforcement offi-cers in initial care and providing them with special medical kits isn’t new. This is a concept that has been used by the U.S. Secret Service for decades, with special kits immediately available to each agent and all agents familiar with the items in the kit. However, the First Five Minutes program is one of the first in which the care provided by officers before EMS arrival has been lauded as having saved several patients. The four-hour First Five Minutes train-ing includes the following elements:
>> Scene safety and orientation components, including familiarity with area fire and EMS agencies and services.
>> The capabilities of local hospitals and the availability of helicopter rescue.
>> Body substance isolation (BSI) and real-world applications.
>> Assessment of circulation, airway and breathing. This includes methods to estab-lish and maintain an open airway, as well as how to provide rescue breathing and con-tinuous compression resuscitation (CCR).
>> How to contact an injured officer.>> When and how to remove body armor.They also learn a 90-second assessment of the
situation and patient medical conditions with primary focus on hemorrhage control maneu-vers and identification of shock. At the end of each assessment, deputies are encouraged to make transport decisions: Do they stay at the scene and wait for EMS, or do they transport the wounded rapidly via police or private vehicles?
For hands-on training, the deputies partici-pated in a skills lab that includes the use of the emergency compression bandages, hemostatic combat gauze, chest seals and tourniquets.
A Pima County Sheriff’s Department deputy uses trauma shears during the First Five Minutes training program.
038_044_Tuscon.indd 42 4/17/2012 10:42:38 AM

www.jems.com mAY 2012 JEMS 43
Pho
to C
ou
rtes
y D
av
iD K
lein
ma
nPh
oto
ma
tth
ew s
tra
uss
elements of TCCC and results from the research done by Valor Project and created the First Five Minutes, a tactical emergency medical training program that was rolled out to all deputies during annual advanced officer training. This specialized EMS and law enforcement training program was developed with assistance from Richard Carmona, MD, MPH, the 17th U.S. surgeon general and former Pima County Sheriff’s Department SWAT team leader and medi-cal director.
Although the First Five Minutes program isn’t the first medical training course taught to Pima County sheriff’s deputies, it’s dif-ferent from their normal medical training because the primary goal is to give police officers the training necessary to sustain themselves or others in situations with life-threatening medical emergencies.
Along with the training, a special emer-gency response equipment kit was devel-oped and issued to all deputies after they completed the training. The law enforce-ment individual first aid kit (IFAK) was assembled to include essential supplies and devices necessary to combat the three most common causes of preventable traumatic death, namely 1) hemorrhage in accessible and controllable regions; 2) hemorrhage in inaccessible or uncontrollable areas and 3) airway/respiratory management.
Officer safety and tactical considerations are incorporated into every aspect of the First Five Minutes lesson plan. Officers are reminded that they’re police officers first and medical providers second. The pro-gram introduction relates the importance of providing immediate medical care to the downed officer. The Fort Hood (Texas) Police Department shooting and the mur-der of Phoenix Police Department Officer Travis Murphy illustrate this issue.
At numerous points during the class, instructors emphasize that this pro-gram isn’t designed to be a first aid class, but rather a survival class for police offi-cers. A law enforcement IFAK is issued to each student at the beginning of the class
so become familiar with its contents to ensure rapid retrieval of essential items when necessary.
Although the IFAK is designed primarily for law enforcement professionals to treat fellow officers, deputies are told to use their discretion at emergency scenes. They’re encouraged to use their IFAKs, once the scene is secure, to stabilize civilians when they feel it can be life-saving in advance of EMS arrival. Such was the case at the Safe-way/Giffords MCI scene.
Because the assisting officer is often the first person to contact the injured person, the training stresses the idea that the officer’s observations and findings are the most sig-nificant issues in long-term care and recovery
An officer responding to a scene that’s unsafe for EMS can use a compact kit equipped with the essentials of hemorrhage control and airway management.
A tourniquet could mean the difference between life and death for an officer pinned down by fire.
Pho
to m
att
hew
str
au
ss
038_044_Tuscon.indd 43 4/17/2012 10:44:41 AM

44 JEMS MAY 2012
of the wounded person. Officers are told to report the following to EMS providers:
>> The nature of the injury;>> Patient’s mental status, including any
changes in mental status;>> Airway control necessary, rates of
breathing and circulation;>> Injuries they saw, who they treated,
and how they treated those injuries; and
>> Any unusual findings or concerns. At the conclusion of the training, the
officers’ skills are evaluated through par-ticipation in multiple scenarios. Two eval-uators are used for each scenario: one evaluates officer safety, use of cover and concealment, tactical movement and other skills related to police work; the second (an EMT or paramedic) evaluates the medical triage and care provided to the patient.
Other PrOgrams Similar emergency medical training pro-grams address this need. This includes the specialized tactics for operational rescue and medicine program (STORM), devel-oped by the Georgia Health Sciences Uni-versity in conjunction with the National Tactical Officers Association.
The STORM course provides clearly defined medical strategies, procedures and
rescue techniques to enhance the safety of law enforcement personnel and the popula-tions they serve. STORM is tailored to five unique tactical audiences: self aid-buddy care, operator, paramedic, medical direc-tor and commander. Each course consists of didactics, hands-on skills stations and tacti-cal scenario-based training.
The Nashville Police Department recently implemented a modern-day “first aid” program, which was taught once a week for five months to their entire roster of 1,400 active-duty officers. The training featured lecture and practical skill sessions training kits, which were issued to each offi-cer as they completed the training program (see “Partners in Crime,” p. 52–55).
COnClusiOnNot all law enforcement agencies consider emergency care to be part of a police offi-cer’s job. With the ever-increasing call load and requirements placed on officers, it’s easy to see how agencies can lessen liabil-ity and workload by eliminating a job that’s already served by fire departments and EMS agencies.
However, a wounded officer, or an offi-cer responding to a mass casualty incident well in advance of EMS, presents an oppor-tunity for lives to be saved by law enforce-ment personnel.
Every officer should have the neces-sary training and equipment to provide
on-scene emergency medical self care. They also should be able to assist other officers and civilians injured during a law enforcement operation.
Key aspects of implementing a successful law enforcement emergency care program are simplicity and ease of use in an emer-gency. Without those two factors, officers are limited in what they can effectively do at a scene.
The training and equipment used by law enforcement personnel prior to EMS gaining access to the scene of the Safeway shooting incident proving it to be worth-while in a time of crisis, resulting in saved lives. The First Five Minutes program is easy to teach, simple to understand and effective in treating the injured before EMS arrival. JEMS
David Kleinman, NREMT-P, is a detective with the
Arizona Department of Public Safety and a tactical para-
medic with Pima Regional SWAT. com. He can be reached
Tammy Kastre, MD, is the medical director for the
Pima County Sheriff’s Department SWAT team and a
board-certified ED physician.
referenCes1. Sztajnkrycer MD, Callaway DW, Benz AA. Police
officer response to the injured officer: A survey-based analysis of medical care decisions. Prehosp Disaster Med. 2007;22(4):335–341.
BeyOnd the taPe>> continued from page 43
pho
to m
att
hew
Str
au
SS
The IFAKThe contents of the IFAK are chosen specifically for law enforcement officers who would need to provide care to trauma patients before EMS arrives on scene. The IFAK’ includes the follow-ing items:
>> A zippered bag with interior elastic straps for holding contents in place. The exte-rior of the bag has multiple attachments points—allowing it to be mounted in the vehicle, on a backpack or even on a duty belt.
>> A pair of trauma shears.>> Two emergency compression bandages.>> One package of hemostatic combat gauze.>> One chest seal.>> One tourniquet.
The individual first aid kit includes supplies and devices necessary to combat the most common causes of preventable traumatic death.
038_044_Tuscon.indd 44 4/17/2012 10:44:45 AM

46 JEMS MAY 2012
TacTical Training offers many benefiTs To ems
>> By William Justice, NRemt-P;lt. KeRRy massie, NRemt-i; &
JeffRey m. Goodloe, md, NRemt-P, faceP
046_050_TacticalEMS.indd 46 4/17/2012 10:46:54 AM

www.jems.com mAY 2012 JEMS 47
EMS providers should be prepared to handle any situation because you never know when a call could go awry.
Pho
tos
Co
urt
esy
oKl
ah
om
a h
igh
wa
y P
atr
ol
>> Tac Team Alpha: I’ve got visual on barricaded subject with hostages.
>> Command: Acknowledge Alpha. Maintain visual and advise of any change in behavior or position.
>> Tac Team Alpha: Subject appears increasingly disoriented.
Sounds of multiple shots are heard fired from the subject’s location.
>> Tac Team Alpha: I’ve got visual on wounded hostage.
>> Command: Copy Alpha on wounded hostage.
>> Command to Tac Team Delta: Go for entry; go for entry.
>> Tac Team Delta: Going entry.
>> Tac Team Delta: Subject secured. Repeat, subject secured. But offi-cer down! Officer down! Operator care initiated.
>> Command: Medics up.
046_050_TacticalEMS.indd 47 4/17/2012 10:47:06 AM

48 JEMS MAY 2012
Paramedic Tango reaches the downed officer, finding blood on the ground
next to a large, mid-thigh gunshot wound in his right leg. The bleeding is already con-trolled by a tourniquet applied by another tactical operator involved in the initial team entry that occurred 65 seconds before Tango made patient contact. The patient is awake, alert and complains of thigh pain. He denies any other injury, and none is found on a quick but thorough physical exam.
Paramedic Ocean reaches the wounded hostage at the same time Tango reaches the downed officer. Ocean finds three gunshot wounds in the hostage’s chest and abdo-men. This patient is awake, talking, anxious and diaphoretic, and he has an increasingly rapid radial pulse. Ocean applies an occlu-sive seal over the largest wound, which is to the right of the sternum. He finds no exit wounds during the remainder of his exam, and he calls for rapid extrication.
A physician and paramedic await the patients at the tactical command post. They have vascular access supplies ready and aeromedical helicopter resources responding with an estimated arrival time of five minutes. The wounded law enforce-ment officer and the wounded hostage arrive for tactical field care within six min-utes of sustaining their wounds.
TacTical TrainingOn the day the events described above occurred, they happened only in training. But the Oklahoma Highway Patrol (OHP) EMS Unit state troopers are well aware that events such as these can occur on any day at any time.
This knowledge, coupled with a com-mitment to safety for all Oklahomans, including their fellow troopers, has guided OHP leaders in developing an increasingly sophisticated cadre of all-hazard medi-cal teams for tactical, special event, mass casualty and natural disaster response throughout the state. In addition to OHP’s progressive leadership, many strategically placed building blocks exist that allow for law enforcement-related medical emer-gency success.
Within OHP and other states’ police organizations, specialized law enforce-ment teams meet the extraordinary operational challenges in tactical, riot, explosive ordinance and disaster situa-
tions. These officers may be dedicated to full-time service on such teams or accept these additional roles beyond their daily police duties. The presence of specialized operational teams, with specific training, tasks and capabilities, creates a strong infrastructure in which to introduce and advance medical emergency capabilities, not only within existing teams, but also for specialized EMS response teams.
above & beyondJust like their EMS and fire colleagues, law enforcement officers are hard-wired for public service. Within an agency the size of the OHP, a call for troopers inter-ested in new medical duties will typically result in a competitive process, yielding top-flight EMT and paramedic candidates and graduates.
EMS professionals willing to think out-side their usual environments and roles are often conduits for exciting changes. Leaders within the University of Okla-homa Department of Emergency Medicine (OUDEM) were approached by OHP with hopes of gaining medical oversight sup-port for troopers trained and in training as EMTs and paramedics.
Select OUDEM physicians and para-medics who expressed interest in partici-pating in the program were screened for their medical knowledge, law enforce-ment duty awareness, physical abilities
and teamwork attributes. They were also required to complete extensive security background checks. Next came an exten-sive process that included exhaustive data-base queries and character references for each candidate.
After the OHP special team orienta-tion, the selected physicians and para-medics received special “boots on the ground” training and emergency response experiences statewide before being approved to serve on OUDEM’s Special Operations Medical Oversight and Sup-port (SOMOS) group.
Each physician and paramedic has a for-mal affiliation with OHP, which provides them with protection from claims while they’re on duty in special assignments and allows for medical liability protection and worker’s compensation for injuries through OUDEM.
The physicians and paramedics work together to ensure coverage is available for statewide response around the clock, using response vehicle assets secured under the Department of Homeland Security fund-ing or responding with a state trooper in a patrol vehicle.
Specialized equipmenT“High speed/low drag” is the catch-phrase for expedient, effective operations. Equip-ment carried on each person and in team support vehicles is evaluated and imple-
prepared for The WorST >> continued from page 47
Troopers practice chest decompressions on a manikin during a training session.
046_050_TacticalEMS.indd 48 4/17/2012 10:49:00 AM

www.jems.com mAY 2012 JEMS 49
mented with this mantra. Medical equip-ment primarily designed for emergency department (ED) and/or daily EMS use often fails this specialized operations requirement. Anything bulky can become an unintentional “target,” and heavyweight items impede rapid movements often needed in access and egress maneuvers.
All team members, law enforcement officers and medical support specialists carry individual first aid kits, for more about IFAKs, see “Beyond the Tape,” pp. 38–40. In general, active operational area equipment is kept to necessary, but effec-tive, “minimums.”
In addition to the IFAKs each officer carries, space- and weight-efficient extrac-tion devices are also available during all operations. These devices are specifically designed to allow for rapid patient move-ment by a minimum number of law officers and paramedics. This often includes devices capable of being used by a single-operator, such as drag straps/pulls and sleds.
Tactical field care—the next echelon of
care—is planned and carried out at stra-tegic locations using larger medical kits containing additional hemorrhage control agents, hemostatic dressings and gauze, as well as more advanced airway and phar-maceutical supplies. IV and intraosseous fluids are carried with a constant balancing of physical weight of fluid against antici-pated clinical needs based on probable patient conditions and times to definitive trauma destinations.
SuStained OperatiOnS & CareSOMOS members are also equipped with 72-hour go bags to allow faster deploy-ment to large events that may advance to extended operations. The “go bags” have prepacked personal items, such as uni-forms, safety glasses, additional protective equipment, multiple flashlights with extra batteries, foul weather gear, safety gloves and self-heating meals. The special bags also include members’ personal medica-tions, back up contact lens/glasses and other specific daily required products.
Disaster-specific equipment, designed to address a multitude of casualties, is car-ried in a dedicated trailer assigned to OHP in the state’s regional EMS system disaster plan. Typical mass casualty supplies for tri-age, treatment area set-up, basic medical care and extrication devices and patient removal equipment are efficiently orga-nized throughout the trailer. Although the trailer is designated for primary use in one of Oklahoma’s eight health regions, it can be mobilized throughout the state as con-ditions may warrant.
depth Of training Putting the right equipment in the hands of motivated professionals is a good place to start, but it’s a poor destination. Routine training for the “non-routine” response is integral to nearly any special operations team’s success when it matters most.
Training exercises and didactics that sup-port effective operations primarily address the following three major medical missions:
>> Injured law enforcement care and
Choose 34 at www.jems.com/rs
Trainees are educated about and practice suturing in the lab setting.
046_050_TacticalEMS.indd 49 4/17/2012 10:51:14 AM

50 JEMS MAY 2012
medical advice on how to minimize the risk of these injuries;
>> Civilian care in special law enforce-ment operations settings with coordination and support for local EMS agencies; and
>> Civilian care in statewide disaster settings while working alongside local EMS agencies.
The training schedule consists of two mandatory days per month, a yearly one-week exercise, and additional train-ing as it becomes available from local, state and federal organizations, such as Basic Disaster Life Support and Homeland Security exercises.
All medical specialists are trained and certified as EMT-Tacticals or equivalent, with a strong basis in tactical combat casu-alty care (TCCC) philosophy and meth-odology. Many members are instructors certified in trauma specific disciplines (Pre-hospital Trauma Life Support, International Trauma Life Support and Advanced Trauma Life Support), which serve as good funda-mental trauma support courses; although modifications in application are necessary in the tactical environment.
The axiom, “Good medicine can get you or someone else killed” is often applied to training drills. For instance, definitive air-way management could be desirable, but intubating in the line of sight of an active shooter isn’t going to end well for either the intubator or the intubatee.
All team members, including primary law enforcement operators, are trained to proficiencies in performing basic medical/trauma assessment, controlling bleeding, using tourniquets and hemostatic agents, sealing open chest wounds, and perform-ing simple airway management techniques and patient evacuation.
Advanced certification medical spe-cialists (e.g., paramedics and physicians) are additionally proficient in airway management, including surgical crico-thyrotomy, vascular access and tension pneumothorax decompression.
Bomb technicians at OHP are invaluable instructors in explosive ordinance aware-ness level training and bomb suit access training. Trauma shears are useless in the access, assessment and care of an explosive ordinance technician, and operators and medical support specialists must know the proper methods for bomb suit removal and
blast-related injury care. As it is for any special operations team,
the training is rigorous, in-depth and designed to push members to mental and physical extremes. Just as special opera-tions medicine was new to the troopers, working in the hot/warm zones of law enforcement special operations was eye-opening to the physicians and paramed-ics. The mutual respect is immeasurable, with everyone remaining engaged, sup-portive and enthusiastic for new informa-tion and skills.
Although textbooks and medical lit-erature is being absorbed by everyone involved, the medical director has found benefit in dedicated weight room “learn-ing” as well.
FrontLine trainingA specialized tactical casualty care course was designed and delivered to the tacti-cal team operators. The operators are instructed to “get off the X,” which means getting to a place of increased safety before implementing any detailed medical care. After the operators are in an area of conceal-ment, and preferably cover, their training in bleeding control, chest seal application and basic airway control with nasal or oralpha-ryngeal airways is designed to save lives and minimize injuries.
The training and teamwork ensures that the tactical law enforcement operators rapidly incorporate medical support for their peers in tactical operations drills and actual situations.
taking it to the StreetBecause of the praise from the law enforcement officer tactical operators, the training has also been extended by the medical team to road patrol troopers and additional staff at the OHP training cen-ter. The same approach to simple, non-invasive assessment and aid that makes lifesaving differences was a success in the pilot course that now serves as the tem-plate for ongoing courses.
Practical scenarios making the didac-tics come to life play an important role in this training curriculum’s effects. With more than 400 state troopers interested in training, the schedule looks filled for an exciting future.
Everyone is feeling the crunch of budget
limitations at best and cutbacks at worst. To mitigate this issue, all avenues of financ-ing are actively considered. Examples of successful funding to date include U.S. Department of Homeland Security grants, criminal activity forfeiture money, and corporate and private donations, in addi-tion to line-item OHP budgeted items.
the SuStainabLe FutureEarly intervention for controlling bleeding, minimizing chest trauma, and improv-ing oxygenation and ventilation can make the difference in life or death in the special operations environment. Applying the concepts from law enforcement to addi-tional areas managed by law enforcement officers and medical support specialists can offer many benefits, namely reducing civilian casualties and treating patients injured in disaster situations.
A realistic training program design and remarkable enthusiasm will enable the OHP to offer new and expanded medical capabilities throughout the state that will benefit officers and citizens alike.
The benefits of a tactical program are simple, yet profound. Law enforcement officers assigned special operations tasks know onsite medical specialists “have their back” when they need it most.
Civilians exposed to the dangers of law enforcement special operations similarly benefit from immediately available aid with expertise. The state’s disaster plan is additionally strengthened by an additional cadre of medical professionals equipped to respond for effective medical aid and scene control. JEMS
William Justice, NREMT-P, is the coordinator of
OUDEM’s Special Operations Medical Oversight and
Support group. He can be reached at via e-mail at
Lt. Kerry Massie, NREMT-I, is the coordinator of
OHP’s medical emergency teams and an experienced
law enforcement tactical operator and trainer. He can be
reached via e-mail at [email protected].
Jeffrey M. Goodloe, MD, NREMT-P, FACEP, is the
medical director of OUDEM’s Special Operations
Medical Oversight & Support group and the OHP’s
medical emergency teams. He’s also a JEMS Edito-
rial Board Member. He can be reached via e-mail at
PrePared For the WorSt >> continued from page 49
046_050_TacticalEMS.indd 50 4/17/2012 10:51:24 AM

52 JEMS MAY 2012
Pho
to Jo
shu
a K
ecKl
ey
052_055_InjuredOfficer.indd 52 4/17/2012 10:52:36 AM

www.jems.com mAY 2012 JEMS 53
EMS providES a training prograM
for local law EnforcEMEnt
>> By Capt. Mario raMirez, MD, Mpp; anDrew n. pfeffer,
MD; GreG Lee, & Corey M. SLoviS, MD, faCep
Today, all U.S. military soldiers entering combat do so with standardized individual first aid kits (IFAKs) that have proven successful in improving survival after injury on the battlefield.
One of our core responsibil-ities as prehospital medi-cal providers is to offer care and assistance to not only the general public, but
also to those who assist and protect us in the field: law enforcement officers. Despite the risk of injury that most police officers face in their daily line-of-duty work, they don’t often receive good medical instruction on self care and buddy aid. As a result, they too represent a medically underserved popula-tion that EMS providers are in an excellent position to assist.
Although most police officers receive some medical instruction during their train-ing at a law enforcement academy, no federal or state standard governs the level of train-ing required or the frequency with which refresher courses must be offered.1
Without such standards, there’s a wide variety in the medical skill sets of officers within and between law enforcement agen-cies. Some officers may have a deep under-standing of medical care, while others may know very little. With all they do to provide scene safety for us to do our work, it simply makes sense that we should return the favor.
052_055_InjuredOfficer.indd 53 4/17/2012 10:52:48 AM

54 JEMS MAY 2012
The ProblemAlthough tactical emergency medical ser-vices (TEMS) is defined as medical support for police and law enforcement officers, it has traditionally focused on high-risk spe-cial weapons and tactics (SWAT) units. By concentrating resources on only these rela-tively small units, however, we’re making a strategic mistake: The majority of injuries in law enforcement are borne by the street level officer, not the tactical operator.
The Department of Justice/Federal Bureau of Investigation’s Law Enforcement Officers Killed and Assaulted database reported that 57,268 police officers were assaulted in 2009, with more than 95% of those assaults occurring against officers in non-SWAT assignments.2
These assaults resulted in more than 15,000 injuries and 48 deaths. Of those offi-cers who sustained fatal injuries, only five were involved in tactical/SWAT scenar-ios. Therefore, although focused “SWAT medicine” offers an exciting opportunity to provide direct care in the high-risk tac-tical setting for officers and perpetrators, targeting medical instruction toward the larger population of non-SWAT officers who sustain a greater number of injuries may be the smarter move.
law enforcemenTs needsThe inherent danger of law enforcement work puts officers at risk for motor vehicle accidents, ballistic injuries, stab wounds and orthopedic injuries. It follows then, that the street level officer needs training in the basics of first aid, including hemorrhage control, airway and pneumothorax management, and sprain/fracture treatment. And with police officers often representing the first persons on the scene of an emergency, it also makes sense to instruct them on the use of automated external defibrillators.
Unfortunately, like other public agencies, most law enforcement groups are currently operating on tight budgets. As a result, the knowledge and supplies to provide immedi-ate casualty care should be easily obtainable at low cost and provide as much “bang for the buck” as possible.
Care items should be readily portable so they can be carried on, or easily reached by, the police officer at work. These items should be both durable and survivable to minimize expiration and turnover of
supplies. As EMS providers, it’s important that we take the time to teach each officer how to use these materials, taking care to provide enough depth to make the con-cepts understandable without making things too technical.
Today, all U.S. military soldiers entering combat do so with standardized individual first aid kits (IFAKs) that have proven suc-cess in improving survival after injury on the battlefield. Our department felt that similar success could be achieved in the civilian sector by issuing kits to our street level police officers.
The nashville exPerienceIn Nashville, every police officer is required to undergo annual in-service training on a topic of the leadership’s choosing. At the request of our local law enforcement agency, we built a modern day “first aid” program and taught that program once a week for five months to the entire roster of approximately 1,400 active duty officers.
In each weekly course, we taught the same lecture and practical skill session using a PowerPoint presentation and train-ing kits that modeled the IFAKs that we then issued to each officer. We covered the
ParTners in crime >> continued from page 53
pho
to Jo
shu
a K
ecKl
eyph
oto
co
urt
esy
na
shv
ille
po
lic
e d
epa
rtm
ent
At the conclusion of the course, each officer is issued an IFAK with all contents stored neatly in a single modular lightweight load-carrying equipment pouch.
The purpose of this pilot project was to primarily train the officers in specialty techniques to care for themselves and their partners. The program has been well received by Nashville police officers.
052_055_InjuredOfficer.indd 54 4/17/2012 10:52:56 AM

www.jems.com mAY 2012 JEMS 55
following topics:The airway, breathing, circulation, dis-
ability and exposure assessment of first aid; >> Basic airway opening, including
jaw thrust and head tilt/chin lift; >> CPR; >> Lacerations and bleeding; >> Dressing application; >> Tourniquet use; >> Ballistic injuries and wound
considerations; >> Blunt-force injuries; >> Burn injuries; >> Management of impaled objects;
and >> Extraction and evacuation
techniques.To practice their skills with real-time
feedback, we gave the officers an oppor-tunity to apply bandages and tourniquets and treat mock sucking chest wounds. At the conclusion of the course, each officer was issued an IFAK with all contents stored neatly in a single modular lightweight load-carrying equipment pouch.
It contains 6" Israeli battle dressing, a tour-niquet, a triangular bandage, stretch and ster-ile gauze, petrolatum gauze, medical shears, medical tape, personal protective gear (e.g., shield, gloves) and a Mylar rescue blanket.
Cost was a key consideration for us. We were able to obtain the materials above and supply each of the 1,400 officers with a complete kit at an individual unit cost of $56.80. The funds used to pay for the purchase of these materials came from a Department of Homeland Security Metro-politan Medical Response System grant.
OutcOmesIt’s important to note that we didn’t cer-tify the officers as first responders after the course was completed. The purpose of our pilot project was to primarily train the offi-cers in specialty techniques to care only for themselves and their partners.
The course was also not long enough to certify the officers to the first responder standard and wasn’t designed to teach them to provide care to the general popu-lation. That’s what their original academy training is designed to do. What we were able to achieve, however, was the instruc-tion of a large population of public safety officers who are at high risk for frequent injury in a very short period of time.
There’s no doubt that in the care of the critically injured trauma patient, two con-cepts hold true: 1) every second counts and 2) care at a Level I trauma center is associ-ated with improved patient outcomes. We believe our program will allow officers to provide earlier care, which will lead to improved outcomes when injuries occur.
cOnclusiOnAs the experts in prehospital emergency care, EMS has a duty to improve flaws that can be fixed easily in our systems. This low-cost, high-impact program for law officers presents us with a real opportunity to improve patient outcomes by designing some direct lectures on specific topics and interspersing hands-on skill sessions.
EMTs, paramedics and EMS physicians can and should teach their jurisdiction’s law enforcement officers how to deal with the immediate health threats of such inju-ries as sucking chest wounds, exsanguinat-ing hemorrhages and airway obstructions.
With the use of public, private or gov-ernment funds, officers can be equipped with life-saving emergency supplies for very little money per officer. By prepar-ing a standardized lecture and practical skills series that can be taught by EMTs, paramedics or physicians, there’s a real opportunity to improve outcomes for an
underserved population that does so much to make our own jobs as safe as possible.
Author’s Note: The previous statements rep-resent the views of the authors and not necessar-ily the view of the Department of Defense or its respective components. JEMS
Capt.MarioRamirez, MD, MPP, was formerly a tactical
and EMS fellow at Vanderbilt University Medical Center.
He’s now an emergency medicine physician serving with
the United States Air Force.
AndrewN.Pfeffer, MD, is currently a resident in emer-
gency medicine at Vanderbilt University Medical Center.
GregLee, is currently an armorer and firearms instruc-
tor for the Metropolitan Nashville Police Training Academy
with 31 years of law enforcement service. He’s also a retired
Master Sergeant from the Tennessee Air National Guard.
Corey M. Slovis, MD, FACEP, is chairman of emer-
gency medicine at the Vanderbilt Medical Center in
Nashville, Tenn. He also serves as medical director for
the Metro Nashville Fire Department and the Nashville
International Airport.
RefeRences1. Sztajnkrycer MD, Callaway DW, Baez AA. Police officer
response to the injured officer: A survey-based analy-sis of medical care decisions. Prehosp Disaster Med. 2007;22(4):335–341.
2. Department of Justice Federal Bureau of Investigation. 2009. Law Enforcement Officers Killed and Assaulted. In Federal Bureau of Investigation. Retrieved March 8, 2011, from www2.fbi.gov/ucr/killed/2009.
The Department of Justice/Federal Bureau of Investigation’s Law Enforcement Officers Killed & Assaulted database reported that 57,268 police officers were assaulted in 2009, with more than 95% of those occurring against officers in non-SWAT assignments.
052_055_InjuredOfficer.indd 55 4/17/2012 10:53:01 AM

56 JEMS MAY 2012
How to rid your rigs of a bedbug infestation >> By Wayne M. ZygoWicZ, Ba, eFo, eMT-P
It was one of the creepiest calls para-medic/firefighter Darwin Mace had ever been involved with during his 14 years with Littleton (Colo.) Fire Rescue. What started out as a routine
call for abdominal pain turned into some-thing right out of the Twilight Zone.
The tones went off for the address of an office building next to the firehouse. On arrival, his crew found a well-dressed female in her 60s sitting in her cubical complaining of abdominal pain. She was being attended to by coworkers. Mace ordered two sets of vitals, took a 4-lead ECG and obtained her oxygen saturation levels. He reviewed her medical history and performed a focused abdominal exam.
As he concentrated on her treatment plan, he decided to move her to his ambulance to avoid any further embarrassment in front of her coworkers. She was pleasant and talk-ative as the crew headed to the ambulance for further assessment and pain control.
“At first, I noticed this small bug on her shirt so I grabbed it and squashed it. I thought it had fallen on her as we moved her to our rig,” he remembers. As he began moving her clothing to attach 12-lead ECG cables, he saw something scurry under the cot sheet. Bugs! Lots of them. At least 20 bugs had fallen out of her left pocket and were looking for hid-ing places. “This is bizarre,” thought Mace as he examined her other pocket. He found more bugs. Then it dawned on him as he
composed himself. They were bedbugs.He quickly covered her tightly with a
blanket, attempting to isolate the pests. He notified the receiving hospital and contin-ued his medical treatment as the bugs wig-gled under the covers.
It wasn’t long before other bedbug inci-dents started popping up. The next time was a working fire incident—a smoky mat-tress fire in a basement. Firefighters arrived quickly, knocked the fire down and removed the half-burnt, smoldering mattress from the structure. Embarrassed by the situa-tion, the home owner admitted trying to kill a bedbug infestation using alcohol and a lighter.
Next was the notice from the housing
056_060_Bedbugs.indd 56 4/17/2012 10:54:15 AM

Pho
to Ja
nic
e h
an
ey c
arr
www.jems.com mAY 2012 JEMS 57
authority that 10 days earlier, the fire depart-ment had transported a patient from an apartment so infested with bedbugs that the unit was posted as unfit for human habitation. The tenant was vacated imme-diately, and their belongings were treated or destroyed.
What are these pests; where did they come from; and what risks do they pose to first responders? Better yet, how do we stop them from taking up residence in our sta-tions, ambulances, city halls and homes?
Bedbug infestations are on the rise across the nation, and first responders will encoun-ter patients and buildings infested with these creatures. Be aware, be prepared and have a game plan for dealing with bedbugs.
BedBug ApocAlypseBedbugs have made resurgence in the U.S., Canada, Australia and the United Kingdom. These blood-sucking pests were nearly erad-icated by the end of World War II by strong pesticides, such as Malathion and Dichlo-rodiphenyltrichloroethane, known as DDT. The most effective pesticides used to kill and control bedbugs were later banned in the U.S. during the ’70s due to their toxic-ity, environmental hazards and human risk. Bedbugs are back, and the war against them is being fought in cities around the U.S.
Experts have been tracking the rapid spread of bedbugs for years. The cause of their exploding population is still somewhat of a mystery, but pest-control specialists
believe it’s related to their resistance to weaker modern-day pesticides. Another cause is increased domestic and interna-tional travel.
Staying overnight in a bedbug-infested environment can provide a one-way ticket for a hitchhiking bedbug to be transported to another location. Bedbug infestations have been dis-covered in expensive hotels, apartment buildings, homes, cruise ships, airliners, office buildings, schools, libraries, movie theaters, transpor-tation hubs and fire stations. City leaders are teaming up with bedbug experts to develop effective strategies to combat these pests and
This digitally-colorized scanning electron micrograph (SEM) revealed some of the ultrastructural morphology displayed on the ventral surface of a bedbug.
056_060_Bedbugs.indd 57 4/17/2012 10:54:00 AM

58 JEMS MAY 2012
stop their rapid spread.Lack of knowledge of common preven-
tion techniques also aids bedbug tourism. Most people aren’t aware of their comeback or don’t believe they have a bedbug problem. Nobody likes creepy bugs, and people whose homes are infested avoid the topic to escape the scorn and embarrassment associated with having “bugs.”
Creepy CrawlersThe common bedbug (Cimex lectularius) can be found worldwide. They feed exclusively on blood and are usually found close to their blood hosts. They’re nocturnal, becoming active at night. They leave their covert hiding places to feed on blood. Bedbugs are resil-ient, have a life span of about 10 months and can live up 90 days without a meal.
Under ideal environmental conditions (70–90° F), bedbugs go through five devel-opment stages, reaching maturity within a few months. Females lay between one and five eggs a day, usually producing 200–500 offspring during their lifetimes. Their eggs, which are commonly found near their host’s bed, are about 1 mm in length and pearly white. They hatch within three
weeks. Newly hatched bedbugs, called nymphs, are translucent
and no bigger than the head of a pin. After feeding on
blood, they may appear reddish in color. Adult bedbugs are gener-
ally brown, a quarter of an inch long and oval with no wings. They don’t
fly, but they can move swiftly on hor-izontal and vertical surfaces. They’re good hitchhikers and can easily latch onto a blan-ket, sock, shoe lace or bunker coat.
These blood suckers activate when they sense an increase in heat and carbon dioxide (CO
2) in the room as their human prey com-fortably drifts off to sleep. They inject their victims with an aesthetic and anticoagulant, usually making their bites painless. Bed-bug bites frequently appear in rows of three to four bites with red welts, and their effect on people will vary from individual to indi-vidual. Itching after a bite can cause redness and skin irritation, and constant scratching may cause open sores, which can lead to skin dermatitis and infection. It’s hard to tell the number of bugs in the environment by the amount of bites on one person. One bug may move around multiple times as they feed or
just feed once while others move in for a snack. Although numer-ous disease pathogens have been discovered in bedbugs, they haven’t shown the ability to transmit and spread disease as other insects do.
Hide & seekBedbug infestations aren’t caused by poor sanitary con-ditions and aren’t a reflection of a person’s social status or hygiene. These bugs have been found in various setting from upscale mansions to homeless shelters. Infestation begins by bringing an item that has bed-bugs or eggs attached to it into an un-infested environment. But poor sanitation and clutter make it more difficult to locate, control and eliminate an infestation after it starts.
Bedbugs play hide and seek well. Most infestations are only discovered after their bites appear on their victims. Human dwell-ings are a perfect environment for bedbugs to thrive in and provide a reliable and con-venient food source—your blood. Their assault isn’t typically limited to the bed or bedroom because they generally disperse throughout the structure via wall cracks, door frames, plumbing areas and electri-cal outlets. They live and breed in the tini-est cracks and crevices and are often hard to detect with the naked eye. Bedbugs can hide or lay their eggs virtually anywhere. They like cool, secluded spots, such as mat-tresses, box springs, wooden head boards, picture frames, furniture, carpeting, luggage and clothing. They fasten their rice-like eggs to rough surfaces, which make the eggs diffi-cult to dislodge.
Most people don’t notice the first signs of the presence of bedbugs. Tiny brown or black fecal spots and dots of dried dark blood are common in their habitat area. Cast skins—hollowed out bedbug skins shed during the nymph stage—are another sign your living space has been invaded. In size-able infestations, a sweet, foul odor may be given off by an oily liquid they emit.
deteCtionBedbugs lead a secretive life, and detecting them in the early stages of an infestation,
when few bugs are first present, can be chal-lenging. It can also be crucial to preventing a full-scale invasion. Although bedbug detec-tion and monitoring tools have certainly improved over the past 70 years, no detec-tion tool is 100% reliable. Sometimes captur-ing the bugs or locating their eggs is the only way to be certain of their presence.
Visual inspection can be time consum-ing and labor intensive, but it’s still the most commonly used and least reliable method of detecting bedbugs. No special equipment is required besides a bright flashlight, a good set of eyes and a strong magnifying lens to help identify eggs or small, freshly hatched nymphs. These cryptic insects like to hide and avoid being seen. Detection devices can be placed under the legs of bed frames and
wHat’s Buggin’ eMs >> continued from page 57
Table 1: Top 10 U.S. Cities for Bedbug Infestations
CincinnatiColumbusChicago,DenverDetroit
Washington, D.C.New YorkPhiladelphiaDaytonBaltimore
Source: America’s top 10 infested cities. (Aug. 24, 2010). In The Daily Beast. Retrieved Feb. 2, 2012, from www.thedailybeast.com/articles/2010/08/24/bedbug-outbreak-which-cities-are-most-infested.html
pho
tos
Wa
yn
e Zy
go
Wic
Z/Ja
nic
e h
an
ey c
arr
Bedbug infestations have been discovered in residences, public places and even EMS stations.
056_060_Bedbugs.indd 58 4/17/2012 10:59:41 AM

www.jems.com mAY 2012 JEMS 59
furniture to intercept the bugs as they migrate to their food source. Inexpensive “pitfall” traps capture the bugs after they fall into the trap and they can’t climb out. The traps work 24 hours a day with little maintenance required, other than occasionally emptying out trapped bugs and lubricating the traps with talcum powder. Other active trap-ping devices use CO2, heat or chemicals to lure the bugs into traps.
K-9 scent detection has become a popular and effective option for detecting low-level infestations. Man’s best friend has been trained to sniff out drugs, explosives, cadavers, mold, termites and cancer—why not bedbugs? Specially trained bedbug dogs can inspect places where humans can’t get too easily or where visual inspection is too tedious and time consuming. A well-trained bedbug detection dog will detect low levels of bugs, even as few as one. Good canines can differentiate active bugs and viable eggs from old infestations with dead bug and empty egg shells. The National Entomology Scent Detection Canine Association supports this emerging science and is working to estab-lish standards for all entomology scent detection canines, handlers and trainers through an accreditation program.
Although bedbug canines are an effective detection tool, they aren’t always 100% accurate. Dogs rely on a “scent picture” to locate the bugs and that may be affected by air movement, wind direction, humidity and temperature. Their effectiveness is directly related to what they can smell. It’s important that a verification system is used to confirm the validity of a dog’s positive “alert” to bedbugs. One method is to have the handler produce physical evidence of the infes-tation (bugs or eggs) after a positive alert. Another confirmation approach is to use a second canine inspector to positively confirm the first dog’s work before spending money on extermination, which can be complicated and expensive.
BedBugs: Now what?They may be small and resilient, but don’t panic. Some feel that if you’re able to see them, they can be killed with a direct spray of 91% alcohol or simply vacuumed up. That may work in some cases, but repeated inspections should be conducted in the following weeks to make sure the dead critter was alone. And you have to carefully secure and dispose of all vacuum bag contents because survivors can escape.
Most experts will tell you that finding and eradicating an infes-tation isn’t a simple job. Chances of conquering a large number of bugs yourself are slim and using the wrong pesticides may drive the creepy-crawlies deeper into the structure. So the best thing to do is call in a licensed professional who’s trained in bedbug biology and behavior to give you sound advice.
The three most common methods used to kill bedbugs are cool-ing, heating and chemicals. The Environmental Protection Agency recommends cold treatments below 0° F (-19° C) for at least four days but using cooling treatments in a large ambulance may be impractical.
Superheating is an effective method to kill bedbugs in all stages of their lives but requires specialized propane or electric heating equip-ment. Rooms are superheated and monitored until the bug’s thermal death point is reached (near 122° F) and maintained for a minimum of one hour while strong fans circulate the heat. Heating and encap-sulating an ambulance, for example, can cost as much as $1,500 per occurrence. More than 300 consumer products currently on the market are registered by the EPA to fight bedbugs. But buyers beware: Before you apply any pesticides, read the label first and follow the
Choose 36 at www.jems.com/rs
Choose 35 at www.jems.com/rs
056_060_Bedbugs.indd 59 4/17/2012 11:03:22 AM

directions closely. Using incorrect chemi-cals in the wrong locations may make you or your patients sick and not fix the problem.
The key to eliminating and preventing bedbugs is to develop an integrated pest management strategy that includes aware-ness, prevention and education. Many states have formed bedbug task forces, and pub-lic safety officials (i.e., police, fire and EMS) should join their collaborative efforts to understand the magnitude of the bug prob-lem in their community and help reduce the risk of exposure for first responders.
An Ounce Of PreventiOnPublic safety leaders must take proactive steps to keep these bugs out of first respond-er’s vehicles and station facilities. The con-sequences of taking these small bugs lightly can have enormous operational implica-tions. Fire stations around the country have been closed for months due to bedbug infes-tations, which can directly affect service lev-els and disrupt personnel.
First responders (and their families) rely on their managers to wage a proactive battle against bedbugs before they end up in first responder’s homes.
Have a strategy and follow the following simple prevention techniques:
>> Develop SOPs. These should address transporting patients with bedbugs or from properties with known infestations;
>> Flag all addresses with known infestations. This will give responders early warning of the problem. Don disposable shoe and head covers, gloves and gowns before entering, and avoid pants with cuffs;
>> Develop a bedbug resources list. Include numbers for immediate inspection, treat-ment and long-term prevention. Most
agencies don’t have the assets to allow an ambu-lance to sit idle
while it waits for bedbug inspection;
>> Quarantine units, equipment and clothing after exposure. This can
prevent transporting the bugs into your station;
>> Bag and seal uniforms and linens after exposures. Laun-
dering most clothing with hot water and detergent, followed by
dry cleaning or drying for at least
20 minutes, should kill all bedbugs;
>> Watch where you place your bags. Leave kits outside a residence known to have bedbugs. Avoid placing med-ical bags on uphol-stered furniture, bedding or car-peted floors on all calls, or consider replacing soft med-ical cases with hard plastic cases;
>> Launder bed-ding weekly. Clean blankets and bed-spreads in sleeping quarters with heat;
>> Provide bedding encasements. Mattress and box springs encasements aid in early detection and can prevent infestations in beds when bedbugs are introduced in the environment;
>> Vacuum and clean surfaces. Vacuums and surface cleaning play a major role in bedbug management. (Remember eggs may not vac-uum up easily.) Tightly bag up and dispose of vacuum’s contents immediately after use;
>> Seal personal gear. Keep clothing and gear in tightly sealed plastic containers to avoid transporting the bugs to your home;
>> Eliminate clutter. Cluttered areas can cause a bedbug control program to fail; and
>> Be on alert. Be on bedbug patrol on every call, and have a bedbug code word.
SleeP tightOf all the things first responders have faced over the years, including infectious diseases, flu and terrorism, these small pests pale in comparison. Although they may not make you sick, they will ruin your day. They spread quickly, and killing them can be expensive and time consuming. So start working on an integrated pest management strategy for your organization so that when you lay your head down tonight, you sleep tight. JEMS
Wayne M. Zygowicz, BA, EFO, EMT-P, is the EMS chief
for Littleton (Colo.) Fire Rescue. He has been involved in
EMS and the fire service for 30 years. He also serves as
a member of the JEMS Editorial Board. Contact him at
reSOurceS>> CentersforDiseaseControlandPrevention.(n.d.).
BedbugFAQs.InCentersforDiseaseControlandPrevention.RetrievedFeb.2,2012,fromhttp://www.cdc.gov/parasites/bedbugs/faqs.html.
>> CooperR.(n.d.).Bedbug101:Avoidinginfestations.InBedBugCentral.RetrievedFeb.2,2012,fromwww.bedbugcentral.com/bedbugs101/topic.cfm/avoiding-infestations.
>> Cooper,R.(n.d.).Bedbug101:Caninescentdetec-tion.InBedBugCentral.RetrievedFeb.2,2012,fromwww.bedbugcentral.com/bedbugs101/topic.cfm/canine-scent-detection.
>> Cooper,R.(n.d.).Bedbug101:Identification.InBedBugCentral.RetrievedFeb.1,2012,fromwww.bedbugcentral.com/bedbugs101/topic.cfm/identification.
>> MillerDM.(n.d.).Non-chemicalbedbugmanage-ment.InVirginiaDepartmentofAgricultureandConsumerServices.RetrievedFeb.1,2012,fromwww.vdacs.virginia.gov/pesticides/pdffiles/bb-non-chemical1.pdf.
>> PorterMF.(n.d.).Bedbugs.InUniversityofKentucky,CollegeofAgriculture.RetrievedFeb.1,2012,fromwww.ca.uky.edu/entomology/entfacts/ef636.asp.
>> U.S.EnvironmentalProtectionAgency.(n.d.).Bed-buginformation.InEnvironmentalProtectionAgency.RetrievedFeb.1,2012,fromwww.epa.gov/pesticides/bedbugs/#ipm.
>> Whatyouneedtoknowaboutbedbugs.(n.d.).InMSNBC.RetrievedFeb.1,2012,fromwww.msnbc.msn.com/id/11915026/ns/date-line_nbc-dont_let_the_bed_bugs_bite/t/what-you-need-know-about-bed-bugs/
WhAt’S Buggin’ eMS >> continued from page 59
A verification method to confirm a bedbug canine’s positive alert to bedbugs is to have a handler produce physical evidence of the infestation afterward.
pho
to W
ay
ne
Zyg
oW
icZ
60 JEMS MAY 2012
056_060_Bedbugs.indd 60 4/17/2012 11:02:53 AM

Watch Steve Berry and JEMS Editor-in-Chief AJ Heightman tell you why this book is a must-read!
SteveBerryBook_fp_05-12.indd 1 4/20/2012 3:36:32 PM

62 JEMS MAY 2012
Practice cultural sensitivity to Provide care to immigrant communities >> By Keith Widmeier, Nremt-P, CCemt-P, emS-i, BA, & emily Coffey, BA, Nremt-P
our unit is dispatched to a motor vehicle collision (MVC) that’s 10 miles north of your station on the major high-
way going through the county. Bystanders report one female patient in the driver’s seat who’s trapped in an
upside-down vehicle. Bystanders advise that she’s in dis-tress but are unsure whether she’s hurt because she doesn’t
speak English. As you responded to the MVC, you started contemplat-
ing what language your patient speaks. The county you serve has a large agricultural community with many immigrants who
live there on work visas for eight to 10 months of the year. The immigrants tend to be from Latin America, with many individu-
als from Mexico, Guatemala, Honduras and El Salvador. This leads you to believe that the patient likely speaks Spanish. En route, you
started evaluating the resources you have available to assist you with communicating with your patient.
On arrival, you note a four-door red sedan on its top. There’s a Mexican flag sticker on the window. The patient is unrestrained, attempting to open the door without success. The doors only open about an inch. The windows are busted out, but the opening is not big enough to extricate the patient.
062_067_Cultural.indd 62 4/17/2012 11:14:35 AM

www.jems.com mAY 2012 JEMS 63
Pho
to G
len
ell
ma
n
062_067_Cultural.indd 63 4/17/2012 11:18:12 AM

64 JEMS MAY 2012
Your patient is clearly scared. You iden-tify fear in her body language and tone; however, your Spanish is limited to the Spanish I class you had your freshman year. You ask, “Do you speak English?” in Span-ish. Your patient responds “no.”
Given the low volume of your service, funding is rather limited. You contact dis-patch in accordance with your local stan-dard operating procedure. They have one dispatcher who speaks fluent Spanish; how-ever, she’s unavailable. A nun from a local Catholic church speaks fluent Spanish and often volunteers her services, but she’s cur-rently assisting another church in a contigu-ous county and is also unavailable.
Dispatch contacts the local county hospital to request assistance. They pro-vide you with access to their outsourced telephone translator service. Using a cell phone to contact dispatch, they conference you into the translator.
You advise the translator of your name and your perception of the situation. You ask that the translator explain the process of extrication and spinal immobilization. The translator writes down everything you said, and you pass the cell phone to the patient. She begins to respond to the translator. She hands the phone back to you. As you con-tinue to evaluate the patient, you notice a deformity of her right lower extremity.
Based on your assessment, you recom-mend the patient be transported to the regional hospital in a contiguous county that has orthopedic capabilities. You explain this to the translator. The translator advises that the patient doesn’t want to go outside the county. Her family has only one vehicle, which is no longer usable. She fears that her husband won’t be able to visit her.
You explain to the translator the likeli-hood of the patient being transferred due to the orthopedic injury, but the patient is adamant about being close to her family. Ultimately, you compromise and transport her to the local county hospital. She’s con-cerned about going to the hospital at all, but she’s willing to accept this agreement.
IntroductIonEMS providers focus on doing everything they can to provide quality patient care. As patient advocates, we focus on scene man-agement, clinical prowess and skill perfor-mance. If we’re able to achieve excellence in
these areas, we often feel that we’re doing everything we can for our patients. How-ever, that clinical knowledge and skill per-formance is only part of the job. If you don’t have good bedside manner, you won’t be treating your patient to your full-est potential.
Research demonstrates that good bed-side manner greatly reduces the risk for mal-practice litigation.1 Without understanding the various cultures that exist in your ser-vice area, your bedside manner can only go so far. True patient advocacy requires both an understanding of the cultures and groups most prevalent in your service area and a general cultural skill set that will enable you to interact with groups with which you’re unfamiliar. It’s important that you’re able to empathize with the patient and their cul-tural context. Although it isn’t imperative to experience the situation firsthand, good patient advocates are able to understand the cultural point of view of the patient.
the LeArn ModeLThe LEARN model is an effective tool for working with your patient to develop a cul-turally sensitive solution.2
L: Listene: explainA: Acknowledger: recommendn: negotiate
The first step is to listen to your patient’s perception of the problem. Although this is a universal principle during patient assess-ment, it’s imperative to evaluate from a cultural perspective when the patient’s experiences are profoundly different from your own. The use of active listening skills can reveal valuable information about the patient’s concerns of the perceived emer-gency, as well as religious, moral, ethical or cultural issues that may arise.
The next phase is to explain your per-ception of the problem at hand. It’s impor-tant not to discuss your personal beliefs on religion, politics or morality. You should only share the information you interpret to be medically relevant. Remember, it’s not our job to preach, witness or lobby for a particular viewpoint; our focus should be on providing medical care and making the
patient feel at ease.The provider should acknowledge and
discuss the differences and similarities in the perceived issues at hand. Remember, your foremost goal as a patient advocate should be the resolution of the medical emergency or traumatic injury. But the patient’s cultural concerns may inhibit standard treatment and may require the provider to think outside of the box.
The provider will then need to rec-ommend a course of action. This can be complicated if the course of action you recommend contradicts the patient’s cul-tural beliefs, which can be so strong that the patient may see the risk of betray-ing their values as greater than the risk of physical harm.
After evaluating the situation, both per-spectives and the recommended course of treatment, the provider should attempt to negotiate a treatment plan that will be acceptable to the patient and maxi-mize the ability to provide the physical care required. Remember we can’t force patients to choose the treatment plan that we feel is in their best interest.
Every patient has the right to choose if and to what degree they’d like to consent to care. If we refuse to budge on our recom-mendations, the patient may refuse care. If that decision is made due to our own stub-bornness, then we aren’t looking out for the patient’s best interest.
IMMIgrAnt PAtIents & FAMILIesThe U.S. immigrant community varies widely. Depending on your location, you may regularly interact with a variety of immi-grant communities. EMS providers should know how important it is for people to hold onto their culture, which may interfere with what’s generally accepted as the best course of action from a clinical perspective.
When considering implied consent, we generally maintain that treatment should be performed in accordance with the assumed desires of a reasonable per-son of sound mind. However, some cul-tural beliefs prohibit specific practices that would be of no concern within American culture at large. For example, most Ameri-cans aren’t opposed to porcine insulin, but Jewish and Muslim patients might choose to accept the risks of hyperglycemia rather than receive this particular medication.
BreAkIng BArrIers >> continued from page 63
062_067_Cultural.indd 64 4/17/2012 11:18:14 AM

www.jems.com mAY 2012 JEMS 65
Although many Americans aren’t con-cerned about the origins of medication or the gender of the EMS provider, such con-cerns may arise. Other cultures may object to care that’s provided by members of the opposite sex, or they may have certain requirements that must be met to ensure modesty while care is provided. In those cases, we should use the LEARN model and make the appropriate accommodations.
ImmIgrant CommunItIesWhen people move to the U.S., some are more likely to move to places in which family members or acquaintances also live, or to areas with well-established ethnic or racial neighborhoods. Communities based on cultural identity often develop from an influx of people from a specific region. These communities can vary in size and diversity. In larger metropolitan areas, you may notice distinct divisions between communities: Puerto Rican, Mexican, Honduran and El Salvadoran, for example.
In areas with smaller populations, though, you may notice a Latin American community that comprises individuals from various countries throughout Cen-tral and South America. Generally, as the population of the service area grows larger, so do the opportunities for differentiation.
Communities with strong racial or eth-nic identities may have their own grocery stores, recreation centers, restaurants and places of worship. This isn’t to say if you aren’t a member of the community, you can’t enter, but these facilities tend to be tailored to the communities they serve. This may mean that the written informa-tion and verbal communication within the facility (other than state and federally man-dated information) may not be in English.
Generational differences also exist among immigrants to the U.S. First-gener-ation immigrants, or those who were born abroad, will generally relocate to com-munities that resemble the country from which they moved. Geographic mobility is often limited among these individuals, because they may be less comfortable with American culture and more at ease with the culturally delineated areas to which they first move.
These communities have accommo-dations that ease the process of assim-ilation and reduce cultural tensions.
First-generation immigrants may also be hesitant to summon assistance or to trust public safety workers, particularly when they move from areas in which govern-mental corruption is high.
Second and subsequent generations tend to demonstrate their culture along with the American culture. The language barrier in these generations may be non-existent, because these individuals tend to grow up speaking English and the language of their parents. Second-generation Amer-icans are often educated in U.S. schools and are socialized into mainstream Ameri-can culture. Because of this socialization to the broader norms of the U.S., individuals from second and later generations may be more comfortable with public safety work-ers and less adherent to specific cultural practices that might impede patient care.
Many major metropolitan areas across the country have created some type of immigrant community liaison program from public safety.3 Most of these endeav-ors have been led by law enforcement and
public health agencies, but as a profession, EMS is fully capable and well-placed to take an active role in community outreach for the immigrant community.
CommunIty outreaChAs a profession, one of the things we truly lack is community outreach. When we per-form community outreach, we don’t spe-cifically exclude the various immigrant communities within our service district from coming. However, a variety of rea-sons often prohibit those populations from attending the outreach activities.
One reason may be a lack of knowledge about the available courses. Large metro-politans may have a local newspaper or other media source that’s specifically tar-geted toward an immigrant community. Regardless of language ability, many immi-grants may choose this avenue of media for their local news. Therefore, if EMS provid-ers aren’t making their community out-reach presence known within these media sources, they may not be doing their best
Purchase today at JEMS.com/shop
The AED is charged and you’re ready to bring your patient back to life as you round the board in this special Emergency Medical Services edition of MONOPOLY, presented by JEMS.
You’ll need to muster all of your protocols, skills and EMS know-how to outwit your colleagues to take command of all the EMS Stations and Hospitals you can afford. Get ready to enjoy this special EMS Edition of the world’s most popular board game, MONOPOLY. Get your limited edition game today!
Save Some Lives and Be the Top Responder!
062_067_Cultural.indd 65 4/20/2012 2:42:28 PM

66 JEMS MAY 2012
to incorporate all the citizens within their service district.
Another issue may be immigrant popu-lations fearing the unfamiliarity outside of their community. It’s common for immi-grants to remain among their own people. However, this doesn’t mean they’re choos-ing not to receive the education that your service is providing—just the location where it’s held.
The solution is to hold some classes on their turf. Discuss the idea with a commu-nity center or organization that serves the population you’re trying to help. Bringing this education to their location will help spread the message of safety and emer-gency preparedness.
Language barriers can be an issue for community outreach as well. Although many of the educational materials (e.g., American Heart Association.) are available in a variety of languages, it may be difficult to teach without speaking the language yourself. Fortunately, a variety of study-at-home material is available in languages other than English.
It may also be beneficial to partner with other healthcare providers in the com-munity to ensure your service’s message spreads. An added benefit of working with others in the community is that your agen-cy’s exposure is increased, and you may learn some additional phrases within the language. Also, the community will be familiar with you and your service.
Language BarrierLanguage barriers are a multifaceted issue. An inability to communicate with the patient, patient’s family and other individu-als on the scene can cause a variety of hard-ships, misunderstandings and accidents. Furthermore, the risk of complications from language barriers is elevated when providers have a false sense of the effective-ness of communication.
Scene safety can be difficult to ascertain if you’re unable to understand the verbal information on scene. On-scene conversa-tions in another language might not reveal the normal clues about potential violence against providers, drug use, family vio-lence or environmental hazards. EMS pro-viders lose the ability to understand and control the scene in which they’re working. Body language is extremely important in
these situations, particularly when consid-ering scene safety.
Ultimately, provider safety is para-mount, and if you feel that the scene may be deteriorating, you should attempt to retreat to a safe distance in accordance with local policies and procedures. Although an overestimation of the hazards at hand might be embarrassing, it’s always best to take the safest course of action regarding your own welfare.
When communicating with patients whose predominant language isn’t Eng-lish, it may be difficult to obtain a full and accurate account of the present event or the patient’s past medical history. In times of stress, individuals who are fluent in Eng-lish may use their primary language instead, simply because it requires less active man-agement and thought on their behalf.
Calls in immigrant communities aren’t exempt from hysterical family and friends on scene, just as they aren’t in “normal” American families. Unfortunately, with-out the ability to communicate with these individuals, the de-escalation skills that many EMS providers have either learned or developed over time may become inef-fective. Although some tools exist to assist
with language barriers, such as translation by phone, many of them are costly, burden-some or time consuming.
One relatively inexpensive and common solution to a language barrier is to attempt to use a translator on scene. However, this may cause a variety of ethical dilemmas. One example is when a younger, second-generation American needs to translate for first-generation Americans. The second-generation immigrant may be a child.
So EMS providers need to consider whether it’s appropriate to share the infor-mation. Will the child be able to accurately reflect the message that you’re attempting to transmit in the necessary tone? Beyond inflection and communication issues, you may need to expose the child to potentially scarring situations to use them as a trans-lator. Consider the thought of request-ing a 10-year-old child to ask his mother whether she’s sexually active, uses any ille-gal drugs or abuses any prescription drugs.
In some cases, the family may travel for the husband’s employment. Because the husband is interacting with other English and non-English speaking people, he may become acclimated quicker than his wife. The husband may be an ideal translator, but some problems could arise from his transla-tion. In cases of suspected family violence, the suspected abuser wouldn’t necessarily translate their victim’s answers correctly.
Another option for translation is using a bystander. EMS providers should exercise caution with using bystander translation. You may be forcing the patient to share med-ical information with someone else who isn’t a medical professional. Although that person may be a coworker or friend, you truly have no way of obtaining informed consent to include this person into the case without speaking the language.
Other options for addressing language barriers include telephone services, trans-lation apps and flip guides or “cheat sheets.” Many hospitals and EMS systems, such as the ones in our case, use telephone-based translator services. Although this can be extremely effective and beneficial, rates for these services may be $4 per minute or more, meaning they aren’t financially fea-sible for many services.
One thing to note with translator apps on smartphones and tablets is that most require you have a basic knowledge of the
Breaking Barriers >> continued from page 65
Most Americans aren’t opposed to porcine insulin, but Jewish and Muslim patients might choose to accept the risks of hyperglycemia rather than receive this particular medication.
pho
to c
raig
Jac
kso
n
062_067_Cultural.indd 66 4/17/2012 11:19:45 AM

www.jems.com mAY 2012 JEMS 67
language. A patient speaking a regional-ized dialect of a common language may not translate in the app.
Many flip guides printed in the U.S. include common medical phrases in Span-ish. Some pocket charts are laminated and have pictures identifying specific medical and traumatic problems. These products may be useful and tend to be fairly cost effective. When you use them, try to focus on short, literal statements and use yes-or-no questions, so you aren’t faced with the translation of a lengthy answer.
When communicating across a lan-guage barrier, remember to speak slowly and steadily. Many individuals who don’t speak English may understand spoken Eng-lish quite well, so you may be able to com-municate more than you originally thought.
The key is to be patient and not to make assumptions. The U.S. doesn’t have a national language, so you should never think of individuals who don’t speak Eng-lish as stubborn or assume that they’re refusing to fit into mainstream culture.
ConClusionPatient advocacy is important whether you’re caring for someone who’s similar to you or someone who comes from a vastly different cultural background. Cultural sen-sitivity and an overall concern for the physi-cal and emotional well-being of all patients will establish a good framework from which you can become a patient advocate.
Remember that the individuals who belong to the groups we’ve discussed often face discrimination and prejudice daily; you may be one of the few people outside of their community who seems to truly care about their feelings or concerns.
When you’re able to provide quality care that incorporates the patient’s values, beliefs and cultural practices—and allows the patient to feel that their culture is impor-tant—you’ll know that you’re well on the way to being a culturally competent pro-vider. JEMS
Keith Widmeier, NREMT-P, CCEMT-P, EMS-I, BA, is the
training officer for Wayne County EMS in Monticello, Ky.
He’s responsible for all initial, continuing and community
education for Wayne County.
Emily Coffey, BA, NREMT-P,is a paramedic at Wayne
County EMS and an instructor and graduate student of
sociology at Western Kentucky University. She received
her bachelor’s degree in sociology and sexuality studies
from Western Kentucky University in 2010.
RefeRenCes 1. BuccoA.AFriendlyApproachtoReduc-
ingMedicalMalpracticeLitigation.Berkeley:2006.
2. BerlinEA,FowkesWC.Ateachingframe-workforcross-culturalhealthcare:Appli-cationinfamilypractice.WestJMed.1983;139(6)934–938.
3. NationalLeagueofCities.(n.d.).PublicSafetyProgramsfortheImmigrantCommu-nity.InNationalLeagueofCities.RetrievedApr.1,2012,fromwww.nlc.org.
To get the JEMS CE Learning Pack, please contact:[email protected] or (877) 435-9309
• Access to the JEMS CE catalog of more than 40 courses. The JEMS Course of the Month features a topic of particular interest. All courses are CECBEMS-approved and include real-time testing for CE certi� cates
• One-year digital subscription to JEMS for all members• Discount of $50 toward registration for the EMS Today Conference• Monthly JEMS CE eNewsletter, including news, links and resources
Total value is $139 for each user, but the cost is only $25 per user; it’s easy to calculate your savings.
NEW FOR ORGANIZATIONS: Round out your training arsenal with the JEMS CE Learning Pack available exclusively through CentreLearn.The JEMS CE Learning Pack lets you give each of your personnel:
The JEMS CE Learning Pack – Available exclusively through CentreLearn.
PLUS, your organization will also receive a one-year digital subscription to EMS Insider, the monthly newsletter for EMS supervisors, administrators and executives.
For more about practicing culutural sensitivity, visit
jems.com/training.
062_067_Cultural.indd 67 4/17/2012 11:22:52 AM

68 jems MAY 2012
Lt. Stacie Farmer, Douglas County Fire Department, demonstrates how to insert a King LT-D.
Apply a water soluble lubricant and apply a tongue jaw lift. Begin insertion by introducing the King LT-D to the corner of the mouth.
Prior to insertion, EMS providers should check the cuffs for proper infla-tion and deflation.
Without using excessive force, advance the King LT-D until the base connector aligns with the teeth or gums.
Pho
tos
Do
ug
las
Co
un
ty (g
a.)
Fire
DeP
art
men
t
068_073_CEairway.indd 68 4/17/2012 11:23:58 AM

www.jems.com mAY 2012 JEMS 69
Rapid assessment is key foR managing numeRous patients>> By Paul E. PhramPus, mD
You’re one of the first-arriving units at the scene of a multi-story nursing home fire. A significant fire is being
battled by firefighters, and there’s smoke pouring from the building. Patients are arriv-ing at the triage intake area, and it’s obvious numerous patients are in respiratory dis-tress ranging from mild to severe. You’re the senior paramedic and will need to begin the treatment decision making.
IntroductIonThe ability to rapidly assess the need to provide airway management to a patient is a critical component of the EMS provider’s skill set. Not many decisions in EMS are both time sensitive and critically important. Airway management is a combination of skills that includes the ability to properly assess the patient, followed by the formula-tion of a plan and then the ability to carry out the psychomotor skills associated with devices and procedures.
When encountering a situation during which multiple patients require active man-agement, our assessment skills won’t change dramatically; however, our decision-making and plan formulation will vary depending on a number of factors, such as expertise, human resource and equipment availabil-ity. A discussion of airway management for the individual patient will help to segue into some of the different thought processes, decision making and plans associated with managing a scene that has multiple patients requiring airway management.
AIrwAy MAnAgeMentAirway management spans a wide vari-ety of potential treatments ranging from the basics of inserting an oropharyngeal
airway, providing oxygen and observing, through advanced procedures, such as endotracheal intubation (ETI) and surgical cricothyrotomies. It’s important to remem-ber there’s no “one size fits all” approach to airway management. Avoid a thought pro-cess of “airway management equals ETI.” For example, ETI has to be recognized as a time- and equipment-intensive procedure when considered from beginning to end in a mass casualty incident (MCI).
Patients may require airway management for a variety of reasons, including medi-cal, trauma and environmental conditions. Essentially, the need for airway management falls into three broad categories: mechani-cally opening the airway to facilitate the pas-sage of air/oxygen, facilitating the delivery of positive-pressure ventilation and finally, protecting the airway against potential aspi-ration and other major contamination of the
multiple Patients
head tilt chin lift
salivation/bleedingDepressed lOC/tongue only
suction/place onside if possible
BVm
subglottic device or crich
Place supraglottic device
Glottic opening compromise?
Need to open airway only? Need positive pressure and/or aspiration protection
Need for airway management
Figure 1: airway assessment Diagram
Advance the tip of the King Airway between the tongue and soft palette, rotating the tube midline.
068_073_CEairway.indd 69 4/20/2012 12:00:42 PM

70 JEMS MAY 2012
Multiple AirwAys>> continued from page 69
lower airways.The need for mechanically opening the
airway arises from conditions that prevent the patient from doing so on their own. The most common airway compromise results from depressed mental status leading to a relaxation of the tongue, which falls poste-riorly and occludes the airway of the supine patient. Other examples include swelling of the airway, blood and foreign body obstruc-tions, as well as direct and indirect trauma to the airway. Indirect causes include inha-lation and ingestion of toxic substances, as well as thermal injuries—all of which can cause significant swelling.
The need to deliver positive-pressure ventilation can arise in any condition dur-ing which the patient is suffering from hypoxia and has an impairment of respi-ratory function. Depressed mental status, pulmonary edema or bronchospasm from asthma, chronic obstructive pulmonary disease or toxic inhalation are common causes of situations that may require pos-itive-pressure ventilation.
Protection against aspiration is needed for patients who are unable to mount pro-tective reflexes that assist in clearing the airway. Often, this patient population has a depressed mental status or unconsciousness. Risk of aspiration may include blood in the airway, as often occurs after traumatic injury, conditions causing excessive salivation and the vomiting of gastric content. In some situ-ations, the entire airway management plan for the patient may revolve around the need for suctioning and mechanically assisting the patient to reduce the aspiration risk.
AnAtoMy Pertinent airway anatomy to consider begins with the upper airway structures, including the oral pharynx, tongue and epiglottis. The glottic opening is the opening between the
vocal cords, or larynx, which serves as the dividing point between the upper and lower airway structures.
Anterior to the larynx is the thyroid car-tilage and the cricoid ring. The latter two prominent structures serve to protect the glottic opening and also provide the palpable landmarks to perform a surgical cricothy-roidotomy or transtracheal jet ventilation through the cricithyroid membrane. The lower airway includes the trachea, bronchi and distal to the lungs.
AssessMentThe assessment of a patient with a poten-tial need for airway management generally focuses on the patient’s respiratory, neuro-logic and cardiovascular systems. In gen-eral, the assessment begins the moment you see the patient.
A simple assessment of the neurologic exam is important to determine whether the patient has the mental status capacity to maintain airway protective mechanisms. In the unconscious patient, this is assessed by noting the presence or absence of a gag reflex. In the case of patients exhibiting delirium and other forms of altered mental status in which they may be speaking, yelling or screaming during the initial assessment while they have serious underlying injury, it’s likely they won’t require immediate airway assistance other than supplemental oxygen.
Special attention to the respiratory rate and pulse are important when assess-ing a patient’s vital signs. Oxygen satura-tions should be measured. You should also observe for additional signs of respiratory distress, such as tachypnea and accessory muscle use. It’s important to remember that in a patient with depressed mental sta-tus, the signs of respiratory distress may be blunted or absent—even in the presence of significant hypoxia.
Skin color, temperature and moisture can provide such information as the level of sympathetic nervous system activation. Oxygenation may be important informa-tion to consider as well. Pale skin can indi-cate shock, while cyanotic skin is a critical indicator of severe, systemic hypoxemia.
Auscultation of the lungs can provide valuable information when assessing the patient’s need for airway management. The most important assessment from ausculta-tion is to determine the presence or absence of airflow into the lower airways. Having none, or diminished sounds of air move-ment, suggests obstruction or lack of respi-ratory effort on the part of the patient. Once the presence of air movement is established, noting the quantity of air movement, along with sounds indicating obstruction, is the next logical step.
Snoring or sonorous sounds are indica-tive of a partial obstruction most often caused from the tongue. Stridor is a high-pitched inspiratory sound associated with the obstruction of the upper airway, such as that associated with swelling of the glot-tis opening.
Wheezing is generally an expiratory sound associated with bronchospasm of the lower airways, but in more severe cases, it may involve an inspiratory component. As bronchospasm worsens, there’s an increase in the overall obstruction of the lower air-ways and may begin to also include inspira-
Key termsEpiglottis: Leaf-shaped structure located posterior to the base of the tongue.Hypopharynx: The laryngeal part of the pharynx extending from the hyoid bone to the lower margin of the cricoid cartilage.Larynx: The portion of the airway connecting the throat with the trachea.Nasopharyngeal Airway: A basic airway that is inserted via the nose into the posterior oropharynx, behind the tongue.Oropharyngeal airway: A basic airway that is inserted via the mouth into the posterior pharynx, behind the tongue.
leArning objectives>> Compare and contrast the practice of prehospital airway management between routine
single-patient encounters and those situations involving multiple patients.>> Describe ways to engage laypersons or minimally trained providers in the care of airway
management at the scene of a mass casualty incident involving multiple patients requiring airway management.
>> Describe the indications, contraindications and limitations of supraglottic airway management techniques.
>> Describe the indications, contraindications and limitations of subglottic airway management techniques.
068_073_CEairway.indd 70 4/20/2012 12:05:57 PM

www.jems.com mAY 2012 JEMS 71
tory wheezing and progress to not hearing any air movement at all in the worst cases.
As a rapid assessment process is being carried out, it’s worth thinking about the categorization described above: 1) Does the patient need their airway mechani-cally opened; 2) Does the patient require positive-pressure ventilation; and 3) Does the patient need protection for aspiration or some combination of the three situations?
The proper assessment of the patient will assist you in forming an airway manage-ment plan. However, formulating airway plans will change when dealing with a MCI during which multiple patients require air-way attention.
TreaTmenT OpTiOnsTreatment and treatment options will vary significantly based on the resources avail-able in the case of a multi-patient airway encounter. In this context, resources include the availability of personnel, as well as their abilities, and the specialty equipment that may be needed in such a situation. Another consideration in overwhelming multiple patient encounters is the engagement of untrained medical providers and layper-sons in realistic tasks that can assist until the situation is stabilized.
After rapid assessment and determina-tion of the need for airway support using the categories suggested, the provider(s) can then begin to implement treatment plans being mindful of the fact that MCI situa-tions may require deviations from typical standard treatment options. One of the big-gest differences for MCIs is that we do not use ETI routinely for airway management. In multi-patient airway encounters, this method of securing the airway often isn’t practical due to the extensive amount of needed equipment, setup time, and the skill and expertise level.
In MCI situations, EMS providers should immediately try to determine which patients will need only supplemental oxygen. In the setting of constrained resources, the appli-cation of oxygen should be limited to those exhibiting signs of respiratory distress with alterations of their oxygen saturations.
A category of patients who may be treated fairly quickly involve those who require only minor mechanical assistance that can be accomplished by opening their airway. This includes patients with altered mental status
or those who are exhibiting excessive saliva-tion or vomiting but are otherwise able to maintain their own airway. These patients can be simply placed on their side in a lateral recumbent position to assist them in clearing their airway. Depending on the availability of resources, a lesser-trained provider—or per-haps even a layperson—can be assigned to the patient with a suction apparatus to assist.
In situations that involve only a single patient, this can be remedied by a number of things: a head tilt chin-lift maneuver, the insertion of an oral or nasal pharyngeal airway or the application jaw thrust with bag-valve mask (BVM) assistance. In situa-tions involving multiple patients for which resources are strained, other forms of treat-ment may be necessary.
In the formulation of the plan, it’s impor-tant to remember that the most common cause of airway obstruction in the uncon-scious patient is the tongue falling backward to occlude the hypopharynx. In such circum-stances, removing an article of clothing from the patient, such as a shoe, may serve as an appropriate prop to place behind the patient’s C-spine to maintain the head in a head tilt-chin lift position that will serve to elevate the tongue from the posterior hypo-pharynx, thereby creating a patent airway.
Patients who aren’t responding to a mechanical opening of the airway may require more advanced intervention, which may include positive-pressure ventilation to deliver oxygen to avoid hypoxia. In such cir-cumstances, the next logical choice is BVM ventilation as a temporizing measure.
BVM ventilation can be accomplished by one skilled rescuer but many times will require two. In cases for which it’s difficult to
maintain a seal with the mask, or for which the patient requires simultaneous applica-tion of a jaw-thrust maneuver to maintain a patent airway, a two-person BVM ventilation technique is essential.
When performing two-person BVM, the more experienced person should be main-taining the seal of the mask, and the lesser experienced or even a layperson can perform the part of squeezing the bag.
When BVM ventilation is necessary, it’s often enhanced by an adjunct, such as a naso-pharyngeal or oropharyngeal airway. Adjunctive basic airway devices are designed to creative patent passage posterior to the tongue to allow effective exchange of gases for the patient requiring this level of support. It’s important to remember the patients that have an intact gag reflex won’t tolerate an oropharyngeal airway. A nasopharyngeal airway should be avoided with patients who have severe facial trauma and the potential for skull fractures.
Simply opening the airway of the patient who needs positive-pressure ventilation assistance or protection from airway aspira-tion gastric contents isn’t enough. In these circumstances, more advanced measures of airway care are necessary. In such situa-tions, several options exist.
Advanced airway treatment options can be divided into two broad categories: supra-glottic and subglottic—depending on how the device or procedure is designed to func-tion. The decision of which method to use will often be determined by the clinical cause necessitating airway management, along
Illustrated above are the key components of the LMA airway. Note the integrated bite block and fixation tab that helps maintain proper cuff depth.
illu
stra
tio
n c
ou
rtes
y l
ma
no
rth
am
eric
a
068_073_CEairway.indd 71 4/17/2012 11:24:02 AM

72 JEMS MAY 2012
Multiple AirwAys>> continued from page 71
with the presence or absence of a gag reflex and whether local protocols support the use of sedative and paralytic medications to facilitate airway management.
suprAglottic AirwAysSupraglottic airways are designed to be used above the vocal cords, or glottis open-ing. They’re placed using a blind technique and create a seal around the glottic open-ing but don’t actually cross the vocal cords. Supraglottic devices are contraindicated in situations for which the glottic opening is compromised, threatening the patency of the airway. Examples include laryngeal swelling from thermal burns, anaphylaxis and direct trauma to the neck with an expanding hematoma.
Similar to oropharyngeal airways, supra-glottic devices aren’t tolerated in patients with intact gag reflexes. ALS providers should consider use of sedative medications for patients with an intact gag reflex requir-ing a supraglottic device..
Common supraglottic devices include laryngeal mask airways (LMAs), as well as King airway devices. Advantages of both the LMA and the King tubes include overall ease-of-use, requiring little extra equipment and set up, as well as a rapid insertion time.
When properly inserted, these devices afford some level of airway protection from aspiration. In general, supraglottic devices require only the device itself and a syringe to inflate either the cuff or the bal-loon of the device.
lMALMAs have had a long history of use in air-way management in the hospital setting. They have a long track record of being safe and relatively easy to use. During the past several years, they’ve been introduced into the prehospital care setting. The LMA is designed to create a seal around the entire glottic opening by leveraging itself against the posterior pharyngeal wall. An inflatable cuff that surrounds the laryngeal opening creates a seal that facilitates the ability to use positive-pressure ventilation and provide some protection against aspiration.
The size of the LMA is selected on the basis of the patient’s weight. Once the proper size LMA is identified, the device is initially prepared by checking the seal of the mask. Once complete, the air is completely evacu-
ated from the cuff prior to placing the device into the patient. The placement of the LMA is a blind technique assisted by elevating the tongue, often with the blade of a laryngo-scope or gloved thumb. The device is placed in and guided into the posterior pharynx anatomically. Once placed, the cuff is inflated with a syringe with the proper amount of air indicated on the packaging of the LMA.
Once the LMA cuff is inflated, a BVM should be connected and ventilation attempted. Observation of chest rise, auscul-tation of the lung sounds and the presence of end-tidal carbon dioxide (EtCO
2) indicate a properly placed device that’s functioning. Assess for the possibility of an air leak by lis-tening during the positive pressure created by the squeezing of the BVM.
If a leak is encountered, place additional air into the cuff and reassess ventilation and seal quality. In some cases, the LMA will need to be removed and replaced to be able to obtain an adequate seal that allows for positive-pressure ventilation and protection. A common cause of an irresolvable leak dur-ing the placement of an LMA is the folding of the distal tip of the LMA cuff back onto itself.
King AirwAy The King airway has rapidly become a pop-ular device for airway management in the prehospital care setting. Its ease of use, quick setup and insertion are ideal features for this supraglottic device. Newer versions of the tube also facilitate gastric emptying through a suction port that allows a gastric tube to be placed in the stomach through the tube. This is an important consideration for reducing the risk of aspiration during the definitive management of the patient when the King tube will need to be removed.
The device features a high-volume, low-pressure balloon system that creates a seal in the hypopharynx and distally in the esophagus. This effectively isolates the glottic opening and allows for the use of positive-pressure ventilation and provides some protection against aspiration. Unlike its predecessor, the combitube, King tubes are designed to be placed into the esophagus every time. The decision making surround-ing the use of the device is also much simpler.
The selection of a properly sized King tube is based on the height of the patient. Once the proper tube is selected, the tongue is lifted, and the device is placed in the patient until reaching the guide marks on the tube, which is similar to the place-ment of an LMA. Once placed, the balloon is inflated with proper amount of air that’s indicated on the package for the device with a syringe. An assessment of effective venti-lation is conducted similar to that described for the LMA.
If a leak is detected, additional air can be placed into the balloon. If an air leak persists after adding additional air to the balloon, the device should be gently pulled back approximately 1–2 cm; that will often create a seal. Studies have shown that the King tube is so easy to use that laypeople were able to successfully place it with instructions given over the phone.
subglottic AirwAy MAnAgeMentSubglottic airway management techniques involve devices or procedures that either cross the vocal cords or are performed below the vocal cords. Most commonly, subglottic airway management is accomplished by ETI. Other forms of subglottic emergent airway treatment include surgical cricothyrotomy and trans-tracheal jet ventilation.
ETI has long been the mainstay of airway
Inflate the cuffs per the manufacturer’s recom-mendations until a seal is obtained. Connect the King Airway to a BVM, ventilate, and slowly withdraw the King Airway until ventilations become easy and free flowing.
Listen to epigastric region and lung sounds to confirm proper tube placement.
068_073_CEairway.indd 72 4/17/2012 11:24:11 AM

www.jems.com mAY 2012 JEMS 73
1. Themostcommoncauseof theobstructedair-wayintheunconsciouspatientis
a. aswellingoftheglotticopening. b. aforeignbody. c. relaxationofthetonguecausinganocclu-
sionofthehypopharynx. d. aresultofvomitingandexcessivesalvation.
2. Whenconductingarapidassessmentofapatientfor the purposes of considering airway manage-ment,youhearstridor.Thisisanindicationof
a. occlusionoftheupperairwaybythetonguethatmayrequireanoropharyngealairway.
1. C; 2. B; 3. B; 4. D; 5. B
Test your comprehension with this post-article quiz. Answers are provided at the end. Photocopying is permitted for nonprofit training purposes only. For readers in need of continuing education credits, please visit JEMSCE.com to choose from courses that are CECBEMS approved and meet NREMT refresher requirements.
REVIEW QUESTIONS
b. upper airway swelling that may require asubglotticairwaytreatmentplan.
c. bronchospasm of the lower airways thatmayrequireabronchodilator.
d. bleeding or excessive salivation that isoccludingtheupperairway.
3. An airway management task that can be easilyassigned to a layperson during a mass-casualtyincidentis
a. theplacementofanlaryngealmaskairway. b. squeezingthebagduringtwo-personBVM
ventilation. c. holdingamasksealduringtwo-personBVM
ventilation. d. noneoftheabove.
4. Which of the following is a contraindication totheuseoftheoropharyngealairway?
a. Bleeding b. Facialtrauma c. Potentialskullfractures d. Intactgagreflex
5. ThedisadvantagestoETIduringmultiplepatientencountersinclude
a. noprotectionagainstaspiration. b. the amount of time and equipment
required. c. theinabilitytousepositive-pressureventi-
lation. d. theinabilitytomeasureEtCO
2.
management in patients requiring airway opening, positive-pressure ventilation and protection from gastric aspiration. ETI may have a role in multi-patient encounters, but such factors as the amount of equipment required, the setup time and the skill and expertise of the provider must be considered.
Although the intubation is usually accomplished quickly, the amount of setup and equipment required will limit its usefulness in multi-patient encounters. Additionally, ETI requires more aseptic precautions and that the laryngoscope be cleaned between each patient encounter. This becomes another complicating logistic in the setting of multi-patient encounters.
Advantages of ETI include positive control of the airway, affording maximal amount of airway protection against gastric aspiration (although it can still occur) and minimizing problems associated with air leaks that can commonly occur with the use of the supraglottic devices.
During ETI, the tongue is moved in a way that allows access to the vocal cords with a laryngoscope or similar device. Once the view of the vocal cords is obtained, an endotracheal tube is passed across the vocal cords into the trachea. Once inside the tra-chea, a low-pressure balloon is inflated to create a seal that facilitates being able to use positive-pressure ventilation and protec-tion from aspiration.
Surgical cricothyrotomy may be indi-cated in the setting of a patient who requires advanced airway management and has a
contraindication, or where there’s ineffective use of a supraglottic device and an inability to perform ETI. A cricothyrotomy can be accomplished fairly quickly with a mini-mum amount of required equipment.
A cricothyrotomy is accomplished by identifying the cricothyroid membrane and making an incision through the skin. Then, through the membrane itself, a tracheal tube, such as a 6.0, is placed directly into the tra-chea. Once the tube is placed, the cuff of the tube is inflated and an assessment of ade-quate ventilation is performed.
Potential complications of surgical crico-thyrotomy include bleeding, placement of the tube into a false passage in the neck but outside of the trachea, as well as dislodgment of the tube after it’s placed—because they’re notoriously difficult to secure.
In dire emergencies when a patient is suf-fering from persistent hypoxia in the set-ting of being unable to otherwise oxygenate them, transtracheal jet ventilation may be considered. This involves performing a nee-dle cricothyrotomy through the cricothyroid membrane and providing oxygen through a catheter via a high-pressure oxygen source.
SummaryEncountering a situation that necessitates the assessment and management of patients requiring airway management can present a significant challenge. It will require a dif-ferent thought process and set of decision-making skills that vary from the routine practice of airway management during a
single patient encounter. Rapid triaging of the need for airway
management is important. Creating a cat-egorization of those patients who simply need supplemental oxygen from those who require assistance with the mechani-cal opening of the airway, a need for pos-itive-pressure ventilation and those who require protection from aspiration can be a useful starting place for the creation of a treatment plan.
Treatment decisions will depend on the amount of equipment and personnel resources that are available. Non-tradi-tional decision procedures and positioning may need to be implemented, such as plac-ing patients in a lateral recumbent position to use gravity to assist in keeping the air-way patent.
In the setting of multiple patient encoun-ters requiring airway management, it’s important to consider the length of time each procedure will take and the amount of equip-ment that will be required. A rapid securing of the airway by a supraglottic device in suit-able patients may be favored over traditional approaches of ETI secondary to the relative complexity of the procedure. JEMS
Paul E. Phrampus, MD, is an associate professor in the
departments of emergency medicine and anesthesiol-
ogy at the University of Pittsburgh School of Medicine.
He’s the director of the Winter Institute for Simulation,
Education and Research (WISER). He’s also a former para-
medic and remains an EMS educator. He can be reached
068_073_CEairway.indd 73 4/17/2012 11:24:13 AM

Airon Corporation 24 29
American Heart Association 27 33
Bound Tree Medical 11 2
Columbia Southern University 36 59
Disaster Response Solutions 33 41
ECCU 51
Ecolab 25 31
Elsevier Books 45
Emergency Medical Products/L.A. Rescue 34 49
EMST TODAY 2013 79-81
Ferno-Washington Inc. 12 3
Firehouse Furniture 31 37
Hartwell Medical 26 31
I-TEC Mfg Emergency Medical Products 18 13
JEMS 19, 45, 61, 65, 67
JEMS Monopoly 65
Junkin Safety Appliance Co. 35 59
Laerdal Medical Corporation 38 84
LMA North America 17 11
Mercedes 13 4-5
Mercury Medical 21 23
Meridian Medical Technologies Inc. 22 25-26
Moore Medical LLC 29 35
O-Two Systems International Inc. 19 17
Oxygen Generating Systems Intl. 30 37
Philips Healthcare 14 6
Pinnacle 28 34
Pulmodyne 16 10
Siena Heights University 32 41
Skedco Inc. 20 21
Stryker EMS 37 83
UCLA Center for Prehospital Care/Prehospital Care Research Forum 51
Ziamatic Corp. 23 28
Zoll Medical Corporation 15 8
ad directYour source for immediate information on advertisers’ products and services
Advertiser RS# Page Advertiser RS# Page
FREE advertiser and product informationwww.jems.com/rs
IT’SFAST,EASYANDJUSTACLICKAWAY!74 JEMS MAY 2012
Ad_Direct_05_12.indd 74 4/20/2012 4:08:58 PM

www.jems.com mAY 2012 JEMS 75
Equipment
Equipment Employment
Are you ready to join a clinically progressive teamwith a tradition of excellence?
Sussex County EMSCaring People, Quality Service
Immediate openings for Nationally Registered ParamedicsContact us at: (302) 854-5050 / www.sussexcountyems.com
Are you up to the challenge?
Classifieds_May12JEMS.indd 75 4/16/2012 4:08:44 PM

76 JEMS MAY 2012
Equipment
LIFE SUPPORT EQUIPMENT CERTIFICATION AND DEPOT
REPAIR
CALL 1.800.383.8962www.advancedbiomedical.com
Save 25% - All Services
ADVANCED BIO-MEDICAL HAVE OPEN POSITIONS?
Get them filled with a JEMS recruitment classified.
Reach our audience with your message!
Email: [email protected]
JEMS helps instructors
JEMS, The Journal of EmergencyMedical Services, provides instructors and students with the critical EMS information they need to provide excellent patient care and achieve success in their careers.
Each monthly issue includes:
� Inspiring Advice on Leadership, Professionalism & Higher Learning
� Breakthrough Clinical Concepts & Fundamental Assessment Tips
� Compelling Case Studies
� Cutting-Edge Gear & Technology
help their students
If you’re an instructor, call to enroll in our Student Subscription Program.
(800) 266-5367 ext. 6832 or JEMS.com
Classifieds_May12JEMS.indd 76 4/16/2012 2:52:42 PM

Exclusively for EMS Management
POWERFUL SOLUTIONSFROM SMART THINKERS
EMS Insider provides you with the “inside information” on EMS. It’s a monthly publication
from Elsevier Public Safety and affiliated with JEMS (Journal of Emergency Medical Services)
so it has the best network of sources in EMS. That means you get only the highest quality
reporting . . . insightful, timely, authoritative. . . not available elsewhere. EMS Insider pays for
itself. Every issue contains articles to help you, by bringing you money-saving and revenue-
generating ideas. Don’t miss out, order your subscription today!
*All Newsletter Subscriptions include access to content and archives from the past 15 years at www.JEMS.com.
Subscribe to EMS Insiderwww.JEMS.com or call 1.888.456.5367
avoid pending lawsuits
researchgrant
funding
EMS TrendAnalysis
EMS Research & Technology
revenuegenerating
ideasAVOIDCOSTLY FINES
Classifieds_May12JEMS.indd 77 4/19/2012 10:59:45 AM

the LIGhteR SIDewhat they didn’t tell you in medic school
>> by steve berry
78 JEMS MAY 2012
Paramedic: That’s a nasty bite you got there, big fella. How’d you get it? Not talking, are we? Suit yourself, but your insistent moan-
ing and yowling is starting to get on my nerves. And stop looking at me like I’m someone you could sink your teeth into. I’m not the one who tased you—not that it phased you a bit.
I gotta admit, I’ve never seen anyone with such stamina and total disregard toward painful stim-uli— especially when the police officers took you down with that subtle shotgun blast. Oh, arggh, yourself. There’s no use at fighting the restraints with your rudimentary attempts of biting and clawing, Big Guy. I used to work in a rodeo after all. Ha ha! Hey, you look familiar. Have I transported you to detox before? Your clueless wandering and poorly coordinated ataxic gait looked familiar.
I can’t smell alcohol on your breath, but holy latrines, your breath reminds me of death warmed over. Not that you’re warm by any means. You’re chilled to the bone, including the various ones stick-ing out from your decomposing, skin-sloughing limbs, which explains why I’ve encased myself in protective MRSA (monster repellant safety attire).
What I can’t understand is how you can keep bleeding with a pulse rate of zero, but ah hell, what do I know? I’m just a brainless ambulance driver. Hmmm. That last comment seemed to have calmed you down quite a bit.
What is it with all this zombie mania over the past several years? How else do you explain the plethora of zombie films, zombie websites, Facebook and high gas prices? Our brains are as infatuated with zombies just as much as zombies are infatuated with ours. From a psychological perspective, zombies may symbolize fears we’re inescapably drawn to: death, mayhem, mindless conformity, the collapse of social order and the need to floss.
Maybe zombies amplify our trepidation of an incurable disease, or perhaps they profess an innate aggressive need to shoot people in the cerebrum. For me, it’s finding any excuse not to pay taxes.
Whatever the reason is for this social escapism into the realm of reanimated pulse-less people, it’s time EMS takes advantage of this basic brain stem functioning craze and inaugurate zombieism into our training and public emergency preparedness programs—not that it hasn’t already happened.
More than one million copies of the Zombie Survival Guide—a comprehensive book about surviving and adapting to a world of flesh eaters—have been sold in the U.S. Taking note of this zombie infatuation, the Center for Disease Control and Prevention, aka CDCP (creeping decomposed crowd pestilence), put this same premise into an educational hand-book on how to prepare for a real emergency.
Capitalizing on the undead faddism, com-munities are taught to prepare for a blitz-krieg of famished cannibals the way they would a hurricane, pandemic or presidential election year. This includes finding the cause of the illness (e.g., virus, bacteria, toxin, radia-tion or high-dose epinephrine IV), source of infection (zombie), how it’s transmitted (e.g., bite, unless zombie is toothless sans dentures—sad to watch really), how readily it’s spread (surprisingly fast seeing as zom-bies move at the speed of a sloth on valium), aggressive quarantine strategies (i.e., shoot anyone in the head who comes to your door, even if they say “trick or treat”) and how to be self-sufficient for a long siege.
Usually it takes some effort to gather
volunteers to act as patients when putting together a disaster drill, but officials from the Department of Emergency Manage-ment in Delaware and Ohio managed to get 10 times that number for their simulated hazmat scenarios.
I began to incorporate zombie didactics into a few of my EMS lectures to prevent my students from going into a zombie state of consciousness from cerebral overload. The living dead have served as narrative themes of the central nervous system while explor-ing the science of the brain. I’d use a clip from a zombie film. Based on the zombie’s behavior, students would use the science of their neurological function to identify which
part or parts of the zombie’s brain were interacting with the real world and which weren’t.
The 2009 movie Zombieland cleverly integrated a list of rules to enhance your chance of survival should you find yourself alone in a world of brain-sludged humanoids. I’ve taken the liberty to incorporate most of those same rules teaching scene safety … except the No. 2 rule of using a “double tap.” That’s considered to be bad form as an EMS responder.
EMS is no stranger to zombies. Just work a 48-hour shift, and you can experience it firsthand. And yes, many of you have resus-citated the dead only to see them become alive and dead at the same time. The differ-ence in zombie resuscitation is that zombies can resuscitate themselves by the very nature of the wound, thus freeing you to do more important things like run away, with your arms flailing, screaming like a girl.
Until next time, Scott Adams once said, “One way to compensate for a tiny brain is to pretend to be dead.” JEMS
Zombie emSProviding care to the undead
Steve berry is an active paramedic with Southwest Teller County EMS in Colorado. He’s the author of the cartoon book series I’m Not An Ambulance Driver. Visit his website at www.iamnotanambulancedriver.com to purchase his books or CDs.
078_LighterSide.indd 78 4/17/2012 11:24:42 AM

February 28-March 3, 2012Baltimore, MD
International Conferenceon Disaster
& Terrorism
Preparedness
Presented in partnership with
EMS TODAY 2012 WRAP-UPThank you to everyone who attended!
EMST 2012 wrap up ad 3P.indd 1 4/19/2012 10:38:22 AM

Next Year: March 5-9, 2013, Washington, D.C.
EMS TODaY 2012 ...
JEMS GAMES
Cumberland County (N.C.) took the gold!
Educational sessions from dynamic speakers, hundreds of products on display, networking with thousands of professionals from around the world ... all part of the “EMS Today experience”
SPECIAL GUESTS
Appearances by Randolph
Mantooth and Steve Berry
kept the exhibit hall buzzing
with excitement.
SCHOLARSHIP wInnERS
Thanks to our sponsorsing exhibitors,
24 scholarship winners received free
registrations to the conference.
HAndS-On wORkSHOPS
Lots of skill-building opportunities!
EMST 2012 wrap up ad 3P.indd 2 4/19/2012 10:38:31 AM

the best in emsEducational sessions from dynamic speakers, hundreds of products on display, networking with
thousands of professionals from around the world ... all part of the “EMS Today experience”
Go to emstoday.com for the exciting details!
COOKING CONTESTOnce again, there were some SERIOUS chefs at work ... and “The Long Fellows” from Longwood (Penn.) Fire Com-pany took the gold! Scan the code and watch them!
A PACKEd ExhIbIT hAllEveryone crowded the hall to view all the products on display, see new product launches and attend free CEH sessions in the Learning Center.
TwO POwErful KEyNOTESRandolph Mantooth and Clint Van Zandt: thought-provoking presentations.
EMST 2012 wrap up ad 3P.indd 3 4/19/2012 10:38:43 AM

“There’s a disconnect that exists in EMS today,” she says. “They say, ‘I’m all scared I’m going to get these diseases.’ But do I do what I’m supposed to?’”
We applaud these agencies for having a relatively low rate of infectious diseases detected, but we also urge EMS as a whole to focus more on this issue to eliminate any unsanitary conditions for both patients and providers.
Training TEchniquEsThe Gilbert (Ariz.) Police
Department recently updated its training and added specialized kits to patrol vehi-cles. They adopted the “First Five Minutes” program, which updates officers on cur-rent best practices in tactical EMS and focuses on such topics as scene security, intelligence gathering, and the dissemina-tion of information to responding medical personnel.
Every supervisor is issued a large kit to be carried in their vehicle, which includes bandages with a clotting agent, trauma and occlusive dressings.
However, the Gilbert Police Department went one step further by placing key items, such as tourniquets and hemostatic dress-ings in special holders that each officer car-ries with them while on duty on their belt or external vest carrier, so they are imme-diately available if needed by an officer for self treatment or the treatment of others.
We commend Gilbert PD for taking such an innovative approach to its officer care capabilities. For more, see “Beyond the Tape,” pp. 38–44. JEMS
infEcTion WaTchA new study of Chicago-
area ambulances found that only 6% showed signs of a dangerous type of bac-teria. That’s good news for those providers working in those ambulances who may fear being surrounded by infectious diseases in their workplaces.
Katherine West, RN, BSN, MSEd, a principal at Infection Control/Emerging Concepts, Inc., and JEMS Editorial Board member, wasn’t shocked by the results, although she says there needs to be more training on how to prevent the spread of diseases.
“If people are cleaning their vehicles the way they are supposed to, the findings would be favorable,” West says.
Researchers from Lewis University in Romeoville, Ill., sampled 26 areas inside
71 ambulances from 34 different Chicago-area municipalities, according to the report that was published in the April issue of the American Journal of Infection Control. They found that approximately 6% of those sites sampled tested positive for Staphyloccocus aureus, a bacterium that can cause serious infections.
Also, they found that five of the 71 ambulances tested positive for Methicillin-resistant Staphylococcus aureus in at least one location.
“These results indicate that first respond-ers are doing a good job of protecting their patients,” James Rago, PhD, the lead author of the study, said in a statement.
Although the findings of the survey are good, West believes more needs to be done to educate EMS providers on the impor-tance of cleaning ambulances after every call.
82 JEMS MAY 2012
LasT WorDThe Ups & downs of eMs
JEMs (Journal of Emergency Medical Services), ISSN 0197-2510, is pub lished monthly by Elsevier Public Safety, 525 B Street, Suite 1800, San Diego, CA 92101-4495; 800/266-5367 (fed. ID #13-1958712). subscripTions: Send $44 for one year (12 issues) or $74 for two years (24 issues) to P.O. Box 17049, North Hollywood, CA 91615-9247, or call 888/456-5367. Canada: Please add $25 per year for postage. All other foreign subscriptions: Please add $35 per year for surface and $75 per year for airmail postage. Send $32 for one year (12 issues) or $62 for two years (24 issues) of digital edition. Single copy: $10.00. posTMasTEr: Send address changes to JEMS (Journal of Emergency Medical Services), P.O. Box 17049, North Hollywood, CA 91615-9248. Claims of nonreceipt or damaged issues must be filed within three months of cover date. Periodicals postage paid at San Diego, Calif., and at additional mailing offices. Canada Post International Publications Mail Product (CanadianDistribution) Sales Agreement No. 1247948. aDvErTising inforMaTion: Rates are available at www.jems.com/jems/advertise/or by request from JEMS Advertising Department at 525 B Street, Suite 1800, San Diego, CA 92101-4495; 800/266-5367. copyrighT © 2012 Elsevier Inc. No material may be reproduced or uploaded on computer network services without the expressed permission of the publisher. JEMS is indexed in the Cumulative Index to Nursing & Allied Health Literature and included in the Medline/PubMed database. JEMS is printed in the United States.
LighTEn ThE LoaDBariatric patients in Memphis, Tenn., may
now be transported to local hospitals with a bit more comfort thanks to a new bariatric ambulance put into service by the Memphis Fire Department.
The unit was created for $5,000 by retrofitting a fleet ambulance in with ramps, a winch and a large cot, according to Deputy Fire Chief Gary Ludwig.
Ludwig says the ambulance has served two impor-tant purposes. “It’s done one to prevent injuries to firefighters and their backs,” says Ludwig, “and two to provide some dignity to the patients.”
There was clearly a need for this type of vehicle, Ludwig says. The Memphis Fire Department had been transporting an average of at least one bariat-ric patient, weighing 600–800 lbs. a month during recent months.
In the past, like most EMS operations without specialty bariatric units, members of the Memphis Fire Department would have had to improvise when facing heavy patients.
“We’ve moved patients any way possible,” Ludwig says.
The heavier patients typically wouldn’t fit on stan-dard ambulance cots, leaving some to be transported on the floor of the vehicles. The new unit can accom-modate patients up to 1,600 lbs. Because of the early high-volume of use for the unit and the size of the area covered by the department, Ludwig says there’s already talk of adding a second bariatric unit.
“We’re going to reevaluate after about four or five months,” he says. “The first week in service we had three [calls]. The first week we also had an 800-lb. patient.”
pho
To C
oU
rTes
y M
eMph
is f
ire
dep
arT
Men
T
pho
To C
oU
rTes
y G
ilbe
rT f
ire
dep
arT
Men
T
082_Lastword.indd 82 4/17/2012 11:25:47 AM