IUCD: Uterine perforation
-
Upload
aboubakr-mohamed-elnashar -
Category
Health & Medicine
-
view
346 -
download
1
Transcript of IUCD: Uterine perforation
IUCD CONTRAINDICATIONS
ABSOLUTE 1. Pregnancy 2. PID or STI 3. Puerperal sepsis 4. Immediate post-septic abortion 5. Severely distorted uterine cavity 6. Unexplained vaginal bleeding 7. Cervical or endometrial cancer 8. Malignant trophoblastic disease 9. Copper allergy (for copper IUDs) 10.Breast cancer (for LNG-IUS)
ABOUBAKR ELNASHAR
RELATIVE
1. Risk factor for STIs or human HIV
2. Impaired response to infection
- in HIV-positive women
- in women undergoing corticosteroid therapy
from 48 h to 4 w postpartum
3. Ovarian cancer
4. Benign gestational trophoblastic disease
ABOUBAKR ELNASHAR
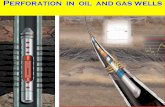
UTERINE PERFORATION
Rare
0.6 to 1.6/1000 insertions.
All uterine perforations, either partial or complete, occur or are initiated at the time of IUD insertion.
ABOUBAKR ELNASHAR
Risk factors
1. Postpartum insertion,
2. An inexperienced operator
3. A uterus that is immobile,
4. Extremely anteverted
5. Extremely retroverted
ABOUBAKR ELNASHAR
Counseling prior to IUD
Benefits and risks
Efficacy
Bleeding Pattern
Perforation 1 in 1000
Ectopic Rate
Expulsion 3-15/100 women
PID: IUD does not protect against STIs or HIV.
Informed consent:
risks, benefits, alternative methods
ABOUBAKR ELNASHAR
Preparation for Fitting
Practical training strongly advised from FFP
of RCOG1
Use of assistant recommended
Consider analgesics or local anaesthesia -
pre-counselling and during fitting
Insert within 7 days of onset of menstruation1
References :
1. Mirena SPC September 1999
ABOUBAKR ELNASHAR
Pain relief prior to, and during, IUD insertion
should be discussed with women
1. Topical anaesthesia: Lignocaine Gel 2% –
Instillagel/Instillaquill
2. Intra-Cervical-- warm 1% lignocaine 3mls at 12,
4, 8 o’clock
3. Para-cervical: 5mls at 3 and 9 o’clock
4. Oral Valium
ABOUBAKR ELNASHAR
Timing of insertion
• At any time during the menstrual cycle once
pregnancy or the possibility of pregnancy can
be excluded.
During or shortly after menses {ruling out
pregnancy and the masking of insertion-
related bleeding} no evidence to support the
common practice of inserting the IUD only
during menses.
Infection and expulsion rates may be higher
when inserted during menses.
ABOUBAKR ELNASHAR
Postpartum
immediate insertion (within 10–15 minutes after
delivery of the placenta): higher risk of expulsion
and uterine perforation.
6 weeks postpartum.
until the uterus is completely involuted
immediately after a first trimester pregnancy
termination.
ABOUBAKR ELNASHAR
Cochrane Collaboration review:
neither doxycycline nor azithromycin before IUD
insertion conferred benefit.
American Health Association:
For prevention of bacterial endocarditis (SBE),
antibiotic prophylaxis is not necessary prior to IUD
insertion if there is no obvious infection.
ANTIBIOTIC PROPHYLAXIS
ABOUBAKR ELNASHAR
FOLLOW UP
1. Exclusion of infection
2. Assessment of bleeding patterns,
3. Assessment of patient and partner satisfaction
4. Reinforce the issue of condom use for protection against STIs and HIV.
After this visit, an IUD user should continue annual well-woman care as for any sexually active woman.
ABOUBAKR ELNASHAR
An IUD user should be instructed to contact her
healthcare provider if any of the following occur:
1. She cannot feel the IUD’s threads
2. She or her partner can feel the lower end of the IUD
3. She thinks she is pregnant
4. She experiences persistent abdominal pain, fever, or
unusual vaginal discharge
5. She or her partner feel pain or discomfort during
intercourse
6. She experiences a sudden change in her menstrual
periods
7. She wishes to have the device removed or wishes to
conceive
ABOUBAKR ELNASHAR
TROUBLE SHOOTING
1. Lost strings
2. Pregnancy with an iud in place
3. Amenorrhea or delayed menses
4. Pain and abnormal bleeding
5. Difficulty removing the iud
6. Sti identified with iud in place
7. Actinomycosis on pap smear
ABOUBAKR ELNASHAR
LOST STRINGS
Speculum exam
If the strings are not seen
1. expelled,
2. perforated the uterine wall, or
3. The strings may have been drawn up into
the cervical canal.
ABOUBAKR ELNASHAR
Pregnancy should be excluded.
Once pregnancy is excluded, the cervical canal
should be explored (with a cotton swab, forceps, or
similar instrument) to see if the strings can be found.
If the strings cannot be found: ultrasound
If the device is seen within the uterus, it can be left in
situ.
If the device is not identified within the uterus or the
pelvis, a plain x-ray of the abdomen
Both the LNG-IUS and the copper IUD are radio-
opaque.
ABOUBAKR ELNASHAR
PAIN AND ABNORMAL BLEEDING
Increased menstrual bleeding with or without an
increase in menstrual cramping may occur in IUD
users.
In the event of partial expulsion or perforation, the
device should be removed and consideration
given to inserting another IUD.
In the first few months after insertion, pain and
spotting can also occur between menses.
ABOUBAKR ELNASHAR
Once partial expulsion, perforation, pregnancy,
and infection are ruled out, treatment with NSAIDs
may be helpful in treating these symptoms.
The number of days of bleeding or spotting usually
decreases over time.
If pain or bleeding persists or worsens, removing
the IUD must be considered.
ABOUBAKR ELNASHAR
Suspected perforation
Procedure should be stopped
vital signs and level of discomfort
monitored until stable.
Follow up should be arranged to include
ultrasound scan and/or plain abdominal x-
ray to locate the device if it has been left
in situ.
ABOUBAKR ELNASHAR





























![RestorationofFertilityafterRemovalofExtrauterine ...downloads.hindawi.com/journals/criog/2011/189565.pdf · A previous case report [14]showedfindingofanextra-uterine IUCD in a women](https://static.fdocuments.in/doc/165x107/5fd903248c72c343d15a6c50/restorationoffertilityafterremovalofextrauterine-a-previous-case-report-14showedindingofanextra-uterine.jpg)









