ISSN 2518-6507 Volume 2 (2017) Issue 3 World Federation of ... · PDF file†...
-
Upload
nguyendang -
Category
Documents
-
view
224 -
download
1
Transcript of ISSN 2518-6507 Volume 2 (2017) Issue 3 World Federation of ... · PDF file†...

Volume 2 (2017) Issue 3ISSN 2518-6507
World Federation of Neuro-Oncology Societies
magazineNeurology bull Neurosurgery bull Medical Oncology bull Radiotherapy bull Paediatric Neuro-Oncology bull Neuropathology bull Neuroradiology bull Neuroimaging bull Nursing bull Patient Issues
EditorialsW Wick EA (Nino) Chiocca
Brain Tumor Epigenetics From Research to Clinical PracticeSilvia Marino
The Value of Surgical Resection for Malignant Gliomas in the ModernEra Beyond Extent of ResectionStephen G Bowden Seunggu Jude Han
Update on Radiation Combinations in the Treatment of Patients withMalignant Brain Tumors From Radiosensitizers to ImmunotherapyDebra Nana Yeboa Erik P Sulman
British Neuro Oncology Society Conference 2017Maryanne Roach
Indian Society of Neuro-Oncology Annual Conference Report 2017Tejpal Gupta
Supporting Family Caregivers as Part of Neuro-Oncology Patient CareCristina Cruz Margaretta S Page
REPORT FROM ASCO 2017Manmeet Ahluwalia
InterviewsHoward Colman John de Groot Patrick Y Wen
Hotspots in Neuro-Oncology 2017Riccardo Soffi etti
Hotspots in Neuro-Oncology Practice 2017Susan Marina Chang
The EANO Youngster Initiative What Does Mentoring Meanto YouAnna Sophie Berghoff
World Federation of Neuro-Oncology Societies
Editors Wolfgang Wick President EANO E Antonio Chiocca President SNO
Managing Editor EANO Roberta Rudagrave Torino Italy
SNO Editor Nicholas Butowski San Francisco USA
Editorial Board
Khaled Abdel Karim Cairo Egypt Egyptian Group of Neuro Oncology (EGNO) Sebastian Brandner London United Kingdom British Neuro-Oncology Society (BNOS)
Oumlz Buumlge Istanbul Turkey Noroonkiloji Dernegi (Neurooncology Society) (TNOD)
Chas Haynes Houston USA Society of Neuro-Oncology (SNO)
Filip de Vos Utrecht Netherlands Landelijke Werkgroep Neuro-Oncologie (LWNO)
Francois Ducray Lyon France Association des Neuro-Oncologues drsquoExpression Francaise (ANOCEF)
Anca Grosu Freiburg Germany German Neuro-Oncological Working Group (NOA)
Andreas Hottinger Lausanne Switzerland Swiss Group for Clinical Cancer Research Working Group Central Nervous System Tumors (SAKK)
Chae-Yong Kim Seoul Korea Korean Society for Neuro-Oncology (KSNO)
Zarnie Lwin Brisbaine Australia Asian Society of Neuro-Oncology (ASNO)
Marcos Maldaun Sao Paulo Brazil Society of Neuro-Oncology Latin America (SNOLA)
Christine Marosi Vienna Austria Austrian Society for Neuro-Oncology (SANO)
Mariacutea Martiacutenez Barcelona Spain Grupo Espanol de Investigacion en Neurooncologia (GEINO)
Motoo Nagane Tokyo Japan Japan Society for Neuro-Oncology (JSNO)
Roberta Rudagrave Torino Italy Associazione Italiana di Neuro-Oncologia (AINO
Gupta Tejpal Mumbai India Indian Society of Neuro-Oncology (ISNO)
Nicolas Whenham Brussels Belgium Belgian Association for Neuro-Oncology (BANO)
Yun-fei Xia Guangzhou China Chinese Society of Neuro-oncology (CSNO)
magazine
copy 2017 Published by The World Federation of Neuro-Oncology Societies This is an Open Access publication distributed under the terms of the Creative Commons Attribution License (httpcreativecommonsorglicensesby40) which permits unrestricted reuse distribution and reproduction in any medium provided the original work is properly cited
Editorial
First of all on behalf of EANO I wouldlike to congratulate the SNO leader-ship for an amazing conference inSan Francisco In addition to theinsights from invited lectures and ed-ucational activities in part supportedby the US Moonshot program theEANO highlight for sure was theaward-winning clinical abstract onthe CeTeG-trial in which UlrichHerrlinger from Bonn presented theNOA-09 trial demonstrating an over-all survival benefit in a small but con-trolled randomized study for thecombination of cyclic CCNU andtemozolomide in patients withnewly diagnosed glioblastoma har-boring a hypermethylated MGMTpromoter
In this issue of the magazine we willhave opinion papers on the value ofbrain tumor epigenetics as well as onthe role of radiation therapy in com-bined modality therapies with a focusnot only on the classical approachesbut also radiosensitization and immu-notherapies In addition to the largebody of literature on precision medi-cine approaches three colleaguesfrom the US share their vision on thepresent but more important also onthe potential future use of next-gener-ation sequencing and other high-throughput technologies in neuro-oncology We have the periodicupdates on Nurses Activities featuredarticles from Neuro Oncology andNeuro Oncology Practice as well as a
view from the EANO youngsters onmentoring
Two of our national organizations(the British and the Indiansocieties) present their views on theWFNOS and the national IndianNeuro Oncology conferencerespectively
On behalf of my colleagues from theEANO board I would like to wish allreaders a successful completion of2017 and a great start into the year2018 with one highlight our EANOconference in Stockholm in Octoberalready determined
W Wick
President EANO
99
Volume 2 Issue 3 Editorial
Editorial
This year from November 15 to 19SNO held its 22nd annual meeting inSan Francisco Each meeting has atheme and this yearrsquos overall themefocused on the ldquoCancer Moonshotrdquoprogram that was proposed byformer president Obama in 2016 andwas initially led by former vice-president Biden whose son perishedfrom a GBM The meeting wasattended by over 2500 participantsfrom all over the world with a recordnumber of submitted abstracts (over1800) The meeting was preceded bytwo successful former meetings theNeuro-oncology Review Course andthe SNOSCIDOT course on intersti-tial CNS delivery both held on Nov15 Our Education Day was held onNov 16 it focused on the subject ofGBM resistance and was organizedby Sue Bell Robert Cavaliere KhalidShah and Albert Kim The mainmeeting was organized by ManishAghi Vinay Puduvalli and FrankFurnari and was highlighted by key-note talks by Jennifer Doudna on
CrispRCas9 and Carlo Croce onmicroRNAs There were multipleSNO educational events from a sun-rise session to lunchtime tutorialsand dinner events such as very wellattended poster and e-talk sessionsThere were also multiple events dedi-cated to stress relief as well includ-ing opening receptions gala dinnersand burnout relief events We are
looking forward to the 23rd meetingin New Orleans which will be led byour new officers (President PatrickWen Vice-President Gelared Zadehand SecretaryTreasurer TracyBatchelor)
EA (Nino) Chiocca
President SNO
100
Volume 2 Issue 3 Editorial
Brain TumorEpigeneticsFrom Researchto ClinicalPractice
Silvia MarinoBlizard Institute Barts and The London School ofMedicine and Dentistry Queen Mary University ofLondon 4 Newark Street E12AT London UK
101
IntroductionEpigenetics is defined as the study of heritable changesin gene expression that are not caused by alterations inDNA sequences1 The phenotypic difference between acaterpillar and a butterfly for example is due to epige-netic regulation of gene expression in the same animalwith the same DNA I particularly like this example to ex-plain the meaning of the term epigenetics as it impres-sively demonstrates how powerful these mechanisms arein controlling phenotypic changes Epigenetic changesare reversible and include the key processes of DNAmethylation histone modifications and noncoding RNA-associated gene silencing (recently reviewed2) known toplay an essential role during the embryonic and postnataldevelopment of an organism and in tissue homeostasis2
Disruptions of epigenetic processes can induce changesin gene function which together with genetic changescan lead to the neoplastic transformation of a normal cell(recently reviewed)3
Recent technological advances have significantly con-tributed to the tremendous progress in understandinghow these epigenetic modifications are regulated in nor-mal cells and deregulated in cancer cells For examplethis knowledge has enabled the translation into better di-agnostic algorithms for tumor classification prognostica-tion and risk assessment Importantly we are nowentering a time when novel therapies targeting thesederegulated epigenetic mechanisms are being devel-oped with some of them showing very promising effectsin preclinical models
It is beyond the scope of this article to comprehensivelyreview mechanisms of epigenetic regulation of gene ex-pression and their deregulation in brain tumors excellentrecent reviews are available to the readers on thesesubjects2ndash5 Here I will discuss a few examples of recentepigenetic discoveries which have informed the develop-ment of novel diagnostic and prognostic tools or led tosuccessful preclinical testing of new epigenetic drugs inexperimental models
Epigenetic Profiles inthe MolecularClassification of BrainTumorsGlioma One of the first examples of an epigenetic changeinforming the design of an assay for diagnostic screeningto corroborate a therapeutic decision is the assessmentof methylation of the MGMT promoter in malignantgliomas6 MGMT (O6-methylguanine DNA methyltransfer-ase) is a key enzyme in the DNA repair network which
removes the mutagenic and cytotoxic adducts from O6
guanine in DNA the preferred point of attack of alkylatingchemotherapeutic agents (ie BCNU temozolomide etc)Hypermethylation of cytosine-phosphate-guanine (CpG)islands located in the promoter region of MGMT is pri-marily responsible for the loss of MGMT function in manytumor types hence leading to an increased sensitivity tothe killing effects of alkylating drugs used in chemo-therapy6 This test is widely used in clinical practice topredict response to temozolomide the alkylating drug ofchoice in high-grade gliomas although it should bestressed that there is still no consensus as to which testmethod to use which CpG sites to assess and what themethylation cutoff should be
Ependymoma Until very recently these tumors havebeen subclassified and graded on the basis of histologi-cal features into low and high grade In 2015 a molecularclassification based on DNA methylation profiling hasbeen proposed which defines 9 molecular subgroups 3for each anatomical location of these tumors (supratento-rial posterior fossa and spinal cord)7 In the supratento-rial location ependymomas with the fusion geneC11ORF95RELA (ST-EPN-RELA) have a poor prognosisand in the posterior fossa it is the ependymoma groupEPN-A that is characterized by a poor prognosis7 Allother ependymomas show a comparatively goodprognosis7 Although not yet included in the World HealthOrganization (WHO) 2016 classification a recent consen-sus paper has recommended that this classification beused for enrollment in prospective clinical trials8 and it isexpected to contribute to informing decisions onmolecular-based treatments as they become available
Medulloblastoma (MB) International consensusrecognizes 4 medulloblastoma molecular subgroupsWNT (MBWNT) SHH (MBSHH) Group 3 (MBGrp3) andGroup 4 (MBGrp4) each defined by their characteristicDNA methylation and genome-wide transcriptomicprofiles9 Recently the heterogeneity within these sub-groups has been reduced by 2 independent studieswhich have defined additional subtypes Schwalbe andcolleagues10 have suggested to split MBSHH into 2 age-dependent subtypes corresponding to ldquoinfantrdquo (lt43 y)and ldquochildhoodrdquo patients (43 y) and MBGrp3 andMBGrp4 into further high-risk and low-risk subtypes whilethe MBWNT group remains unchanged10 Interestingly thelow-risk subtypes were defined primarily by hypermethy-lation in comparison to normal cerebellum whereas thehigh-risk subtypes were defined by relativehypomethylation10 Cavalli and coauthors11 used integra-tive clustering of DNA methylation and gene expressiondatasets from 763 patients to split the original 4 sub-groups into 12 subtypes MBSHH is split into 4 subtypes(abc d) MBWNT into 2 subtypes (ab) MBGrp3 andMBGrp4into 3 subtypes each (abc)11 The subtypes iden-tified in these 2 studies overlap considerably and themain differences seem to be related to the inclusion ofadult MB patients in the Cavalli study Importantly MBsubgroups and their subtypes identified by their
Brain Tumor Epigenetics From Research to Clinical Practice Volume 2 Issue 3
102
epigenetic and related transcriptional profiles1011 havedistinct genetic and clinicopathological features1011 andtheir implementation for patient stratification for betterprognostication and enrollment into subgroupsubtype-directed therapies in the context of clinical trials will be astep change in the treatment of MB patients
All CNS tumors A classification tool for brain tumorsbased on genome-wide DNA methylation patterns and arandom forest-based machine learning approach hasbeen developed and extensively tested by the GermanCancer Research Center (wwwmolecularneuropathologyorg) This resource is available online and has provento be a valuable tool to improve brain tumor diagnosticsThis approach has facilitated the identification of com-mon druggable molecular pathway alterations across var-ious histological tumor entities thus allowing patients toenter the most appropriate clinical trials and in somecases be offered molecularly matched therapies As anexample DNA methylation profiles allow precise identifi-cation of cases with mitogen-activated protein kinase(MAPK) activation which is a feature of tumors withBRAF V600E mutation1213 which can span various tradi-tional histological entities such as pilocytic astrocytomaspleomorphic xanthoastrocytomas ganglioglioma andsubependymal giant cell astrocytomas to predict re-sponse to specific inhibitors interrupting the BRAFMEKcomponent of the MAP kinase pathway14
Novel TherapeuticApproaches TargetingEpigeneticDeregulationDiffuse intrinsic pontine glioma (DIPG) is a highlyaggressive pediatric tumor located in the brainstem andcharacterized by a rapid and diffusely infiltrative patternof growth These tumors cannot be treated surgicallybecause of their location and infiltrative nature15
Radiation therapy is the standard treatment although itprovides only temporary symptom relief with no overallsurvival benefits and conventional chemotherapy drugsare ineffective15
Mutations in histone H3 variants occur in more than 80of DIPG and result in a lysine-to-methionine substitution(H3K27M)16 17 H3K27M has been shown to inhibitpolycomb repressive complex 2 (PRC2) by binding to itscatalytic subunit EZH2 and reducing the methylation ofH3 at lysine 27 (H3K27me) at selected target loci18 Theresidual PRC2 activity is required to maintain DIPGproliferative potential by repressing neuronaldifferentiation in patient-derived cell lines and in agenetically engineered mouse model1920 Importantlysmall-molecule EZH2 inhibitors abolish tumor cell growth
in these models raising the possibility that inhibitionof EZH2 could be a novel therapeutic strategy for thesetumors19
An independent study showed that H3K27M associateswith increased H3K27 acetylation (H3K27ac) and that themajority of the heterotypic H3K27M-K27ac nucleosomesco-localize with bromodomain proteins at the loci of ac-tively transcribed genes20 The authors have shown thatblocking the recruitment of bromodomain proteins by het-erotypic H3K27M-K27ac nucleosomes in DIPG with bro-modomain and extraterminal domain family inhibitorsefficiently inhibited tumor progression thus identifying thisclass of compounds as potential therapeutics in DIPG20
These important advances in understanding the underly-ing biology of DIPG have led to the identification of novelepigenetic therapeutic approaches which are very effec-tive at the preclinical level and if confirmed in transla-tional studies could change the way we treat thesetumors in the near future
Conclusion and outlookThese are exciting and challenging times for theneuro-oncology community Exciting because there isgrowing expectation in the field that new discoveriessuch as those discussed in this article can soon translateinto new and more effective therapeutic approachesChallenging because it is clear that new skill sets are re-quired to effectively apply them to benefit patients
The clinical training in many neuro-oncology specialtieswill have to take into account the additional knowledgeand skills needed in the field and offer education incomplementary disciplines such as next-generationsequencing technologies integrated with interpretativedata analysis as well as molecular biology for the designof biologically informed assays and tools The require-ment for these new highly specialized skills also needs tobe reflected in the composition of the clinical teamswhere bioinformatics expertise will play an increasinglyimportant role for the integration of multimodal data inpatient care
References
1 Waddington CH Canalization of development and the inheritance ofacquired characters Nature 1942150563ndash565
2 Allis CD Jenuwein T The molecular hallmarks of epigenetic controlNat Rev Genet 201617487ndash500
3 Flavahan WA Gaskell E Bernstein BE Epigenetic plasticity and thehallmarks of cancer Science (New York NY 2017357
4 Edwards JR Yarychkivska O Boulard M Bestor TH DNA methyla-tion and DNA methyltransferases Epigenetics amp chromatin20171023
5 Filbin MG Suva ML Gliomas genomics and epigenomics arriving atthe start and knowing it for the first time Annual Rev Pathol201611497ndash521
6 Hegi ME et al MGMT gene silencing and benefit from temozolomidein glioblastoma N Engl J Med 2005352997ndash1003
Volume 2 Issue 3 Brain Tumor Epigenetics From Research to Clinical Practice
103
7 Pajtler KW et al Molecular Classification of Ependymal Tumorsacross All CNS Compartments Histopathological Grades and AgeGroups Cancer Cell 201527728ndash743
8 Pajtler KW et al The current consensus on the clinical managementof intracranial ependymoma and its distinct molecular variants ActaNeuropathol 20171335ndash12
9 Taylor MD et al Molecular subgroups of medulloblastoma the cur-rent consensus Acta Neuropathol 2012123465ndash472
10 Schwalbe EC et al Novel molecular subgroups for clinical classifi-cation and outcome prediction in childhood medulloblastoma a co-hort study Lancet Oncol 201718958ndash971
11 Cavalli FMG et al Intertumoral Heterogeneity withinMedulloblastoma Subgroups Cancer Cell 201731737ndash754 e736
12 Schindler G et al Analysis of BRAF V600E mutation in 1320 nervoussystem tumors reveals high mutation frequencies in pleomorphicxanthoastrocytoma ganglioglioma and extra-cerebellar pilocytic as-trocytoma Acta Neuropathol 2011121397ndash405
13 Tanaka S et al Epithelioid glioblastoma arising from pleomorphicxanthoastrocytoma with the BRAF V600E mutation Brain TumorPathol 201431172ndash176
14 Banerjee A et al A phase I trial of the MEK inhibitor selumetinib(AZD6244) in pediatric patients with recurrent or refractory low-grade glioma a Pediatric Brain Tumor Consortium (PBTC) studyNeuro Oncol 2017191135ndash1144
15 Hargrave D Bartels U Bouffet E Diffuse brainstem glioma in chil-dren critical review of clinical trials Lancet Oncol 20067241ndash248
16 Schwartzentruber J et al Driver mutations in histone H33 and chro-matin remodelling genes in paediatric glioblastoma Nature2012482226ndash231
17 Wu G et al Somatic histone H3 alterations in pediatric diffuse in-trinsic pontine gliomas and non-brainstem glioblastomas Naturegenetics 201244251ndash253
18 Lewis PW et al Inhibition of PRC2 activity by a gain-of-function H3mutation found in pediatric glioblastoma Science (New York NY2013340857ndash861
19 Mohammad F et al EZH2 is a potential therapeutic target forH3K27M-mutant pediatric gliomas Nature Med 201723483ndash492
20 Piunti A et al Therapeutic targeting of polycomb and BET bromodo-main proteins in diffuse intrinsic pontine gliomas Nature Med201723493ndash500
Brain Tumor Epigenetics From Research to Clinical Practice Volume 2 Issue 3
104
The Value of SurgicalResection for MalignantGliomas in the ModernEra Beyond Extent ofResection
Stephen G Bowden MDSeunggu Jude Han MDDepartment of Neurological Surgery OregonHealth and Sciences University 3303 SW BondAve Center for Health and Healing CH8NPortland OR 97239 Telephone 503-494-4314Fax 503-346-6810 hanseohsuedu
105
Malignant gliomas are among the most difficult oncologi-cal entities to treat Despite aggressive treatment prog-nosis remains poor and recurrence and treatmentfailures seem inevitable The current standard-of-caretherapy includes maximal safe surgical resection fol-lowed by concurrent and adjuvant chemoradiotherapyHistorically surgical resection has conferred greater sur-vival benefit to these patients than adjuvant therapiespresumably through the cornerstone principle of cytore-duction However the extent of surgical resection is fre-quently limited by nearby eloquent tissue and risks to keyneurological functions In addition the value of such ag-gressive approaches has been questioned in light of thewidespread infiltration of glioma cells Meanwhile our un-derstanding of glioma biology continues to advance rap-idly fueled in large part by the acquisition of tumor tissueduring surgery Thus the exact role and value of surgeryparticularly in comparing the clinical benefits of maximalextent of resection (EOR) with the biomedical benefits oftissue provision has been a topic of great interest anddebate in both the neuro-oncological and neurosurgicalcommunities
EOR patient age tumor histology performance statusand molecular markers have been widely accepted assignificant predictors of patient outcomes in malignantglioma9 In the past 2 decades many large retrospectivecohort studies have demonstrated improvements in sur-vival with increasing EOR5917 Due to ethical considera-tions evidence from a randomized prospective studysupporting the clinical benefit of aggressive resectionsdoes not exist and likely never will Instead the closestthing to such evidence in malignant glioma comes fromthe randomized phase III trial comparing surgical resec-tions with or without the use of 5-aminolevulinic acid(5-ALA) The use of 5-ALA serving as a means to and aproxy for greater EOR resulted in extended overall sur-vival for patients with newly diagnosed glioblastoma19 Arecent meta-analysis of 41 117 unique patients by Brownet al adherent to the guidelines of PRISMA (PreferredReporting Items for Systematic Reviews and Meta-Analyses) also demonstrated a clear survival benefit forgross total resection over subtotal resection or biopsy atupfront surgery for glioblastoma1 The body of literatureas a whole clearly favored aggressive resections andthere seemed to be little disagreement for a strategytoward maximal resection when clinically feasibleHowever the challenge still remains when such strategiescome at the risk of neurological morbidity A recent reportby Rahman et al illustrates that the survival benefits fromaggressive resection are lost if the patient develops anew postoperative neurologic deficit as a result15
All the while our understanding of glioma genetics mo-lecular biology and mechanisms of resistance has con-tinued to deepen and evolve borne of thoughtful andsystematic studies using patient-acquired tumor sam-ples Molecular profiles and tumor genetics have proventhemselves to be the best predictors of clinical behaviorand now represent crucial components of the diagnostic
classification scheme of infiltrating gliomas12 With tumortissue at the molecular and genetic level being able to ro-bustly predict patient outcomes accurate tissue diagno-sis has become paramount in the management ofgliomas The role and value of open surgical resection to-ward this end have become clearer as concerns of sam-pling error with biopsy alone led to a number of studiesevaluating the ldquoaccuracyrdquo of stereotactic biopsy proce-dures Jackson et al reported a series of 81 patients whounderwent stereotactic biopsy followed by open surgicalresection The tissue diagnosis was concordant betweenbiopsy and open resection samples in only 51 ofpatients6 Other studies have also demonstrated diagnos-tic concordance between stereotactic biopsy and surgi-cal resection samples in only 57 to 79 ofcases131428 The major limitation of stereotactic biopsyfor infiltrating gliomas likely stems from the significantintratumoral heterogeneity and collectively these studieshighlight the value of open surgical resection in providinga more global representation and understanding of thetumor tissue
The value of extensive resection is perhaps even moreprofound when considering the therapeutic implicationsof such heterogeneity Multiple-site and serial-samplinganalyses have revealed a high degree of both spatial andtemporal heterogeneity within these tumors a conse-quence of serial evolutionary events during tumor growthand progression23 These studies have also led to theconcept of therapy-driven clonal selection and preferen-tial regrowth of resistant cell populations as a potentialmechanism of treatment failure Efforts to expand our un-derstanding of the tremendously complex network ofmutations and biological consequences of chronologicalhierarchy would be greatly facilitated by carefullyplanned thoughtful acquisition of tumor samples duringsurgery
Despite the recent paradigm shift in glioma diagnosticclassification little gains have been made in improvingthe overall prognosis for patients with malignant gliomassince the introduction of concurrent and adjuvant temo-zolomide in 200521 The strategies more recently tested inlarge randomized phase III trials by and large have yieldeddisappointing results while the reasons and mechanismsof treatment failures remain unclear Even so encourag-ing responses have occasionally been seen in varioussubsets of patients and studies exploring the presenceof potential biomarkers have generated intriguing andpromising results in these populations The developmentof the antindashvascular endothelial growth factor monoclonalantibody bevacizumab is one such example Two initialphase II trials showed prolonged progression-free sur-vival in recurrent glioblastoma relative to historical con-trols prompting the US Food and Drug Administration togrant accelerated approval to bevacizumab for recurrentglioblastoma in 2009825 However 2 large randomized tri-als evaluating the addition of bevacizumab to radiationand temozolomide in the newly diagnosed setting failedto show a benefit in overall survival24 and its utility in the
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
106
recurrent setting is now a topic of debate in light of sub-sequent phase III trial results However a post hoc analy-sis of patients enrolled in the AVAglio trial recentlydemonstrated that bevacizumab improved overall sur-vival for those with a proneural subtype tumor18 Just asO6-methylguanine-DNA-methyltransferase (MGMT) pro-moter methylation does for temozolomide the geneticprofile of the tumor could serve as a potential biomarkerof clinical response for bevacizumab as well and valida-tion studies are currently ongoing Such analyses al-though performed post hoc require targeted prospectivecollection of tumor tissue at initial surgery In addition ge-netic profiling of newly diagnosed malignant gliomas willneed to become routine if this approach is to be utilizedwidely Similarly cilengitide an inhibitor of aVb3 andaVb5 integrins with anti-angiogenic properties showedinitial promise in recurrent glioblastoma studies but failedto show any additional benefit in the newly diagnosedsetting20 A subsequent post hoc analysis of the phase IItrial revealed improved progression-free and overall sur-vival in patients with high aVb3 levels in the tumor cells26
However tumor tissues were not systematically collectedand less than half of the patientsrsquo tumor tissues wereavailable for analysis from the phase III trialUnfortunately this drug will most likely not undergo fur-ther development and one cannot help wonder if the out-come would have been different if the enrollment in thephase III trial had been enriched for or restricted to tumorswith high expression of the aVb3 integrin The only trueldquosuccess storyrdquo since the adaptation of radiation andtemozolomide has come from the novel approach of tu-mor treating fields (TTFields) a transcutaneous deliveryof low-intensity intermediate frequency alternating elec-tric fields The multicenter phase III trial EF-14 random-ized patients with supratentorial glioblastoma withoutevidence of tumor progression following standard che-moradiation to receive maintenance treatment withTTFields plus temozolomide or temozolomide alone22
The study was terminated early based on results of aplanned interim analysis demonstrating benefit inprogression-free survival overall survival a secondaryendpoint was also significantly enhanced at this timeDespite the trialrsquos success TTFields has not been univer-sally adopted by the neuro-oncology community andenthusiasm among clinicians and patients remains low27
Experts have raised concerns regarding the study designsuch as its open-label design lacking a sham-treatmentcontrol arm as well as the generalizability of the resultsbased on the unique randomization point occurring afterconcurrent chemoradiation16 Perhaps most significantlya lack of widely understood mechanism of action hasalso been raised as a factor with comparison to othertreatments the preclinical data for TTFields is relativelylacking particularly when applied in conjunction with che-moradiation27 Even during the early phase stages theuse of robust tissue-based analyses exploring the mech-anism of action such as dose response modeling andmultisite tissue biopsies may have mitigated some of
these concerns and led to wider acceptance by the com-munity Bevacizumab and cilengitide clearly benefitedfrom retrospective analyses of human tumor tissue toidentify susceptible treatment populations while the en-thusiasm for TTFields is perhaps in part tempered by thelack thereof Collectively the evolution of these treat-ments underscores the value of extensive targeted tissuesampling in furthering development of new adjunctivetherapies
Open surgical resection of tumors with such targeted tis-sue acquisition for analysis will continue to play a key rolein prospective clinical trial designs Comparison ofpretreatment and posttreatment tissue profiles representsa valuable line of investigation by delving into mecha-nisms of therapeutic action as well as mechanisms oftreatment failures1011 It also provides an opportunity toinvestigate a number of key fundamental steps along anagentrsquos path to clinical success such as does the agentsuccessfully traffic to the tumor if so how much anddoes the agent then actually have its hypothesizedeffects at the biochemical or cellular level Thusearly-phase trials can and should include posttreatmentmolecular endpoints when possible in addition to safetyendpoints Immunotherapy and immune checkpoint inhi-bition represent exciting novel therapeutic approachesfor neuro-oncology particularly based on their success inmetastatic cancers Large phase III trials studying block-ade of the programmed cell death protein (PD)1PDligand 1 axis with monoclonal antibodies for newlydiagnosed and recurrent glioblastoma are under way butinitial reports have been concerning for negative resultsAs in the development of many previous novel agentstissue-based mechanism studies have been largely lack-ing in the preclinical phases However an Alliance-supported trial currently enrolling focuses on a biomarkeras a primary endpoint patients with recurrent glioblas-toma indicated for surgery are randomized to receivepembrolizumab a PD1 inhibitor either before or aftersurgery (NCT02852655) The resected tumor tissue willthen be analyzed for the profile of tumor-infiltratingT cells and comparison will be made between the 2groups This study represents a tremendously valuableopportunity to explore the impact and the potential chal-lenges of checkpoint inhibition for malignant gliomas inthe clinical setting and should the large phase III trialsend up negative this pilot study will be very informative
Advances in imaging biomarkers and molecular charac-terization of gliomas in conjunction with new targetedtherapies will continue to improve and transform themanagement of these tumors Multimodality imaging cannow more accurately reflect ongoing biological processeswithin these tumors such as the presence of oncogenicmutations or cells undergoing malignant transformationNovel biomarkers such as circulating tumor DNA showpromise in detecting early recurrence or monitoring treat-ment response3724 Lastly the new classification schemerevolving around molecular characterization will provide a
Volume 2 Issue 3 The Value of Surgical Resection for Malignant Gliomas in the Modern Era
107
necessary corollary to these novel diagnostic tools Itremains indisputable however that clinical validation ofthese novel diagnostic tools will also require systematiccorrelation with human tumor tissue obtained throughsurgery These samples ideally gathered prospectivelywill provide a pivot upon which we can expand our under-standing of the complex network of oncological pro-cesses driving these tumors
Malignant gliomas are incredibly challenging disease en-tities in many ways due to the inter- and intratumoral het-erogeneity that is a hallmark of them Experience to datehints that future successes in malignant gliomas rest inneuro-oncology entering the era of precision medicinewhere validated biomarkers and targeted personalizedtherapies are seamlessly integrated into the managementparadigm Accordingly systems supporting surgical re-section and patient-specific tumor tissue analysis mustbe built and organized to guide the decision making fortherapy As our overall approach to the management ofmalignant gliomas evolves so should the framework ofsurgical management The clinical benefits of maximalsafe resection are well founded and well reportedHowever the oncological neurosurgeon must now lookbeyond maximal cytoreduction itself and recognize thevalue of thoughtful acquisition and analysis of tumor tis-sue Modern neurosurgeons must consider themselvessurgical neuro-oncologists and engagement and partici-pation of surgeons into clinical trials particularly early-phase trials should be encouraged and valued In turnwe should provide our surgical trainees with the trainingand tools in neuro-oncology to help them participate andcontribute in multidisciplinary collaborative efforts aimingto advance the understanding of brain tumor biology andultimately improve the outlook of our patients
References
1 Lacroix M Abi-Said D Fourney DR Gokaslan ZL et al A multivariateanalysis of 416 patients with glioblastoma multiforme prognosisextent of resection and survival J Neurosurg 2001 95190ndash198
2 Hervey-Jumper SL Berger MS Maximizing safe resection of low-and high-grade glioma J Neurooncol 2016 130269ndash282
3 Sanai N Polley MY McDermott MW Parsa AT Berger MS An ex-tent of resection threshold for newly diagnosed glioblastomas JNeurosurg 2011 1153ndash8
4 Stummer W Pichlmeier U Meinel T et al Fluorescence-guided sur-gery with 5-aminolevulinic acid for resection of malignant glioma arandomised controlled multicentre phase III trial Lancet Oncol2006 7392ndash401
5 Brown TJ Brennan MC Li M et al Association of the extent ofresection with survival in glioblastoma a systematic review andmeta-analysis JAMA Oncol 2016 21460ndash1469
6 Rahman M Abbatematteo J De Leo EK et al The effects of new orworsened postoperative neurological deficits on survival of patientswith glioblastoma J Neurosurg 2017 127123ndash131
7 Louis DN Perry A Reifenberger G et al The 2016 World HealthOrganization Classification of Tumors of the Central NervousSystem a summary Acta Neuropathol 2016 131803ndash820
8 McGirt MJ Bulsara KR Cummings TJ et al Prognostic value ofmagnetic resonance imaging-guided stereotactic biopsy in the
evaluation of recurrent malignant astrocytoma compared with a le-sion due to radiation effect J Neurosurg 2003 9814ndash20
9 Muragaki Y Chernov M Maruyama T et al Low-grade glioma onstereotactic biopsy how often is the diagnosis accurate MinimInvasive Neurosurg 2008 51275ndash279
10 Woodworth G McGirt MJ Samdani A Garonzik I Olivi AWeingart JD Accuracy of frameless and frame-based image-guided stereotactic brain biopsy in the diagnosis of glioma com-parison of biopsy and open resection specimen Neurol Res 200527358ndash362
11 Suzuki H Aoki K Chiba K et al Mutational landscape and clonal ar-chitecture in grade II and III gliomas Nat Genet 2015 47458ndash468
12 Stupp R Mason WP van den Bent MJ et al Radiotherapy plus con-comitant and adjuvant temozolomide for glioblastoma N Engl JMed 2005 352987ndash996
13 Kreisl TN Kim L Moore K et al Phase II trial of single-agent bevaci-zumab followed by bevacizumab plus irinotecan at tumor progres-sion in recurrent glioblastoma J Clin Oncol 2009 27740ndash745
14 Vredenburgh JJ Desjardins A Herndon 2nd JE et al Phase II trial ofbevacizumab and irinotecan in recurrent malignant glioma ClinCancer Res 2007 131253ndash1259
15 Chinot OL Wick W Mason W et al Bevacizumab plusradiotherapy-temozolomide for newly diagnosed glioblastomaN Engl J Med 2014 370709ndash722
16 Gilbert MR Dignam JJ Armstrong TS et al A randomized trial ofbevacizumab for newly diagnosed glioblastoma N Engl J Med2014 370699ndash708
17 Sandmann T Bourgon R Garcia J et al Patients with proneural glio-blastoma may derive overall survival benefit from the addition of bev-acizumab to first-line radiotherapy and temozolomide retrospectiveanalysis of the AVAglio trial J Clin Oncol 2015 332735ndash2744
18 Jackson RJ Fuller GN Abi-Said D et al Limitations of stereotacticbiopsy in the initial management of gliomas Neuro Oncol 20013193ndash200
19 Stupp R Hegi ME Gorlia T et al Cilengitide combined with stan-dard treatment for patients with newly diagnosed glioblastoma withmethylated MGMT promoter (CENTRIC EORTC 26071-22072study) a multicentre randomised open-label phase 3 trial LancetOncol 2014 151100ndash1108
20 Weller M Nabors LB Gorlia T et al Cilengitide in newly diagnosedglioblastoma biomarker expression and outcome Oncotarget2016 715018ndash15032
21 Stupp R Taillibert S Kanner AA et al Maintenance therapy withtumor-treating fields plus temozolomide vs temozolomide alone forglioblastoma a randomized clinical trial JAMA 20153142535ndash2543
22 Wick W TTFields where does all the skepticism come from NeuroOncol 2016 18303ndash305
23 Sampson JH Alternating electric fields for the treatment of glioblas-toma JAMA 2015 3142511ndash2513
24 Lang FF Asher A Prospective clinical trials of brain tumor therapy thecritical role of neurosurgeons J Neurooncol 2004 69151ndash167
25 Lang FF Gilbert MR Puduvalli VK et al Toward better early-phasebrain tumor clinical trials a reappraisal of current methods and pro-posals for future strategies Neuro Oncol 2002 4268ndash277
26 Elkhaled A Jalbert L Constantin A et al Characterization of metab-olites in infiltrating gliomas using ex vivo (1)H high-resolution magicangle spinning spectroscopy NMR Biomed 2014 27578ndash593
27 Jalbert LE Neill E Phillips JJ et al Magnetic resonance analysis ofmalignant transformation in recurrent glioma Neuro Oncol 2016181169ndash1179
28 Touat M Duran-Pena A Alentorn A Lacroix L Massard C Idbaih AEmerging circulating biomarkers in glioblastoma promises andchallenges Expert Rev Mol Diagn 2015 151311ndash1323
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
108
Update on RadiationCombinations in theTreatment of Patientswith Malignant BrainTumors FromRadiosensitizers toImmunotherapy
Debra Nana Yeboa MD1
Erik P Sulman MD PhD123
Departments of 1Radiation Oncology2Translational Molecular Pathology and3Genomic Medicine The University of Texas MDAnderson Cancer Center 1515 Holcombe BlvdUnit 97 Houston Texas USA Tel 713-563-2300dnyeboamdandersonorg andepsulmanmdandersonorg
109
AbstractAdvances in radiosensitizers and immunotherapyhave ushered in a new frontier in brain tumortreatment The brain has often been viewed as asanctuary site due to the bloodndashbrain barrier andthus the 2 primary modalities of therapy includedsurgery and radiation therapy (RT) More recentlysystemic therapies have played a greater role aseither combination therapy radiosensitizers or im-munotherapy Two novel radiosensitizers are beingdeveloped for the treatment of brain metastasesRRx-001 for example is a small molecule thataccelerates the NO2 to NO conversion of deoxyhe-moglobin and the agent 2-dexoyglucose (2-DG) is anonmetabolized glucose analogue that interfereswith ATP formation Poly(ADP-ribose) DNA polymer-ase inhibitors are promising due to their distinctradiobiological effects Veliparib and olaparib areamong the most studied with randomized trialsexploring their use in gliomas and brain metastasesImmunotherapy including immune checkpoint inhib-itors may play a role for both primary gliomas andbrain metastases RT has been shown to enhancethe function of cytotoxic T lymphocytes induce infil-tration of cytotoxic T lymphocytes and enhancefunction Trials are presently exploring use of bothprogrammed cell death protein (PD)1 and PD ligand1 blockade in glioblastoma patients with radiationSimilarly several immunotherapies are being investi-gated with either stereotactic radiosurgery or wholebrain radiation therapy for brain metastases In thisreview the use of radiosensitizers and immunother-apy agents with RT will be discussed broadly
Keywords brain metastases brain tumors gliomasimmunotherapy radiation therapy radiosensitizers
Radiosensitizers andImmunotherapy inBrain TumorsAdvances in radiosensitizers and immunotherapy haveushered in a new frontier to brain tumor treatment Braintumors however are a diverse class sharing only similaranatomic location Both primary brain malignancies andbrain metastasis have widely diverse histologies and mo-lecular phenotypes With the bloodndashbrain barrier thebrain has often been viewed as a sanctuary site and thusthe 2 primary modalities of therapy included surgery andradiation with decreased benefit from systemic agentsdue to lack of brain penetration However more recentlysystemic therapies have played a greater role as eithercombination therapy radiosensitizers or immunother-apy While temozolomide (TMZ) has played a pivotal rolefor glioblastoma (GBM) only a subset of patients benefitfrom the treatment1 The use of alternative systemicagents that may potentiate the effects of radiation ther-apy (RT) is becoming increasingly appealing Similarly forbrain metastases a variety of systemic agents are beingexplored primarily based on histology and immune pro-file In this review the use of radiosensitizers and immu-notherapy agents currently under investigation with RTwill be discussed
RadiosensitizersThe guiding concept of radiation sensitization is to in-crease the biologic effect of radiation such as increasedDNA damage decreased DNA repair decreased hypoxiaor increased G2M cell cycle blockade leading to im-proved tumor control and increased patient survival2
Poly(adenosine diphosphate-ribose) DNA polymerase(PARP) inhibitors are promising radiosensitizers due totheir roles in DNA repair3 PARP inhibitors work againstPARP1 a nuclear enzyme involved in the recruitment ofrepair proteins used in base excision repair and single-strand break repair PARP1 may also play a role in nonho-mologous end-joining4 The primary investigation ofPARP inhibitors has been in potentiating radiation andchemotherapy effects the latter in the context of homolo-gous repair deficient tumors For radiation the primarymechanism of action is inducing damage to nucleotidesleading to single-strand and double-strand breaks ThusPARP inhibitors in combination with radiation have an ap-pealing mechanism to inhibit or delay DNA repair andlikely convert more single-strand breaks to double-strandbreaks4
While several PARP inhibitors are currently being evalu-ated in a variety of tumors including talazoparib and nira-parib veliparib and olaparib are among the most studiedand there are randomized trials exploring their use in
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
110
gliomas The US National Cancer Institute (NCI)ndashfundedAlliance for Clinical Trials in Oncology (Alliance) A071102is a randomized phase IIIII trial evaluating the use ofveliparib in combination with TMZ in the adjuvant settingin patients with GBM tumors exhibiting hypermethylationof the O6 methylguanine DNA methyltransferase (MGMT)gene promoter Preclinical data supporting this trial sug-gested that only patients with MGMT methylated tumorswould benefit from the combination a group of patientsfor whom TMZ concurrent with radiation might be mostbeneficial5 A phase I trial performed by the NCI-fundedAmerican Brain Tumor Consortium attempted to combineveliparib with radiation and TMZ but failed to identify asuitable recommended phase II dose due to significanthemotoxicity6 Thus attempts to combine radiation withveliparib have focused on patients least likely to benefitfrom TMZ namely with MGMT unmethylated tumors forwhom TMZ could be withheld The Australian VeliparibRT and TMZ trial in newly diagnosed unmethylatedMGMT glioblastoma (VERTU) is a single-arm study inwhich patients receive RT with veliparib followed by adju-vant TMZ and veliparib4
An ongoing novel approach to radiosensitize gliomasinvolves a combination with an agent that interferes withan essential metabolic process 2-Dexoyglucose (2-DG)is a nonmetabolized glucose analogue that acts as acompetitive inhibitor of glycolysis It is transported acrossthe bloodndashbrain barrier by the glucose transporter GLUT-1 and thus has good penetration into the CNSIntracellularly it is trapped and accumulates in cells simi-lar to the mechanism of 18-fluorodeoxyglucose 2-DG isphosphorylated by glycolytic enzymes and the
phosphorylated 2-DG (2-deoxyglucose-P) is trapped in-tracellularly Inhibition of hexokinase activity by 2-DGinterferes with ATP formation and results in tumor celldeath7 While it has positive attributes by selectively tar-geting metabolically active tumor cells 2-DG has alsobeen associated with Q-T prolongation The currentphase III trial in gliomas is assessing the toxicity and tol-erability of 2-DG with hypofractionated radiation of 5 Gyas a radiosensitizer7
Two novel radiosensitizers are being developed for thetreatment of brain metastases First RRx-001 is a smallmolecule initially designed by the aerospace industry Itworks in part as a radiosensitizer by increasing blood flowand thus oxygenation of tumors through nitric oxideRRx-001 which binds to hemoglobin accelerates theNO2 to NO conversion of deoxyhemoglobin It workslocally under hypoxic conditions and subsequentlythe radiosensitive effects through nitric oxide are invasodilation and inhibiting DNA repair enzymes8 Nitricoxide is relatively benign The higher levels of oxidativestress with H2O2 and superoxide in tumors in comparisonto normal tissues result in the preferential generation ofreactive peroxynitrite in the presence of higher nitric oxidelevels7 This accounts for the increased specificity anddecreased toxicity with RRx-001 The dose limiting toxic-ity in a phase I trial of 25 patients treated with eitherweekly or biweekly infusions was infusional pain relatedto the release of NO at the site of injection7 Outside ofpreclinical models 2 clinical reports examining wholebrain radiation therapy (WBRT) with RRx-001 reported anintracranial response A patient with melanoma and 2hemorrhagic edematous lesions of 26 cm and 33 cm
Table 1 Clinical trials involving immunotherapy and radiation therapy1213
Clinical Trials Number Phase Disease Type Treatment Groups
NCT02667587 II Newly diagnosed GBMMGMT-methylated
Nivolumabthorn TMZthorn RT vs placebothornTMZ thorn RT
NCT02617589 III Newly diagnosed GBM Nivolumabthorn RT vs TMZthorn RTNCT02336165 II Newly diagnosed unmethylated
MGMT recurrent glioblastomaMEDI4736thorn standard RT vs MEDI4736 thorn
bevacizumabNCT02530502 III Newly diagnosed GBM RTthorn TMZthorn pembrolizumab TMZthorn
pembrolizumabNCT02313272 I Recurrent glioma Hypofractionated stereotactic radiationthorn
pembrolizumab thorn bevacizumabNCT02696993 III Brain metastases Nivolumabthorn SRS nivolumabthornWBRT
nivolumabthorn ipilimumab thorn SRS nivolu-mabthorn ipilimumab thornWBRT
NCT02115139 II Melanoma brain metastases Ipilimumab thornWBRTNCT02097732 II Melanoma brain metastases Ipilimumab SRS ipilimumab vs SRS
ipilimumabNCT01703507 I Melanoma brain metastases Ipilimumab thornWBRT vs ipilimumab thorn SRSNCT02107755 II Melanoma brain metastases Ipilimumab thorn SRSNCT02858869 pilot Melanoma and NSCLC Pembrolizumabthorn SRSNCT01950195 I Melanoma brain metastases Ipilimumab thorn SRSNCT02662725 II Melanoma brain metastases Ipilimumab thorn SRS
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
111
after a single intravenous dose of RRx-001 of 5 mgm2 4days before WBRT resulted in symptomatic improvementwithin 48 hours By 4 months after radiation there was areduction in size in the largest dimension down to 10 cmand 23 cm of the respective lesions A second report of amelanoma patient with at least 18 lesions after receivingRRx-001 of 5 mgm2 4 days before WBRT as well astwice weekly doses during the 2 weeks of radiation alsoshowed response The patient at 4 months had disap-pearance of 13 of 18 lesions with shrinkage of theremaining 5 lesions8 Presently BRAINSTORM is a phaseIII dose escalation trial of RRx-001 designed to be ad-ministered twice weekly for 2 weeks with WBRT (30 Gy in10 fractions) with the option for weekly maintenance8
Veliparib has also been evaluated in the setting of brainmetastases It was tested in a global randomized con-trolled trial with WBRT Veliparib is orally bioavailable andcrosses the bloodndashbrain barrier It was first examined in amultihistology phase I trial in patients with nonndashsmall celllung cancer (NSCLC) breast cancer melanoma and re-nal and colorectal cancers among others The study of81 patients tested dose tolerance of veliparib from 10 to300 mg orally twice a day with WBRT to 30 Gy in 10 frac-tions or 375 Gy in 15 fractions9 The phase I trial dose es-calation portion did not reach the predefined criteria forthe maximum tolerated dose but there was amplificationof the adverse effects of nausea and vomiting among thehighest dose cohort of 300 mg bid9 The adverse eventprofile at 200 mg bid was similar to that of WBRT aloneDoses of veliparib from 20 to 200 mg bid demonstratesimilar antitumor activity and other studies in preclinicalmodels found that 50 mg daily demonstrated significantreduction in poly(ADP-ribose) in peripheral blood mono-nuclear cells and tumor tissue while also effectivelycrossing the bloodndashbrain barrier Thus the subsequentphase II trial examined 50 mg with WBRT9 In order to as-sess a more homogeneous cohort the phase III globalrandomized trial studied only NSCLC at the 2 doses of50 mg and 200 mg twice daily versus placebo twice a daywith WBRT10 The primary endpoint was overall survivalIn 307 patients in a 111 randomization of 50 mg bid200 mg bid or placebo twice daily the study found nosignificant differences in overall survival among the differ-ent groups10 The majority of patients across the treat-ment groups had a graded prognostic assessment (GPA)score of25 and a Karnofsky performance status ofgt80 The median overall survival was 185 days forpatients receiving placebo and 209 days for those receiv-ing veliparib without any statistically significant differ-ence These results were similar to the disease-specificestimate of median survival for the disease-specific GPAof NSCLC patients with brain metastases10
Several other radiosensitizers have failed to improve overradiation alone in a number of trials These have includedtrials with WBRT including motexafin gadolinium efap-roxyn bortozemib thalidomide teniposide topotecanpaclitaxel and cisplatin7 Of note other PARP inhibitorsalso being assessed include talazoparib and niraparib4
which may yield positive results The use of valproic acid(VPA) as a histone deacetylase inhibitor has also beenconsidered to have radiosensitizing potential in additionto its anti-epileptic drug properties11 While studies havereported that patients with GBM receiving an anti-epilep-tic agent may have higher overall survival than those re-ceiving standard chemoradiation therapy alone thebenefit remains controversial Retrospective analysissuggested that patients taking VPA specifically had bettersurvival in comparison to other anti-epileptic drugs Alsoa recent prospective phase II trial was performed in 37patients with GBM receiving VPA 25 mgkg concurrentlywith TMZ chemoradiation and reported a median survivalof 296 months While controversial further data andinvestigation are needed into this and other agents thatmay potentiate RT
Immunotherapy and radiationImmune checkpoint inhibitors lead to activation of T cellswhich may traffic across the bloodndashbrain barrier to inter-act with tumor Primary brain tumors may evade the im-mune system through upregulation of immunecheckpoints and possible immunosuppression12
Monoclonal antibodies promote immune-mediated anti-tumor activity by inhibiting the immune functionndashmediated cytotoxic T-lymphocyte associated protein 4(CTLA-4) and programmed cell death protein 1 (PD-1)receptors PD protein ligand (PD-L1) is upregulated inGBM through oncogenic signaling possibly throughphosphatase and tensin homolog loss and interleukin-10signaling1314 RT has also been shown to enhance thefunction of cytotoxic T lymphocytes RT may induce aninfiltration of cytotoxic T lymphocytes and enhance theirfunction It may also induce antindashCTLA-4 agents inhibitingT-cell function and increasing the CD8thorn T cellregulatoryT cell ratio in cases of melanoma15 Thus PD-1 and PD-L1 blockers may have a further role in CNS managementwith the use of radiation
In preclinical models radiation has been examined withimmunotherapy that included among other mechanismsvaccination PD-1 blockade and CTLA-4 blockade Inmice radiation plus a vaccination of irradiated gliomacells was associated with increased survival of 40 to80 compared with 0 to 10 for other groups stud-ied16 A benefit of PD-1 blockade with stereotactic radio-surgery (SRS) specifically has also been shown in amouse model In comparison to mice treated with radia-tion antindashPD-1 therapy or a combination only those re-ceiving combination therapy had a higher percentagesurvival alive beyond 180 days after treatment17 Othermouse carcinoma models have identified response withanti-CTLA antibody and fractionated radiation therapy18
CD137 activation CTLA-4 blockade and focal radiationtherapy have been examined in an immunocompetent in-tracranial GBM model Mice treated with triple combina-tion therapy had 50 greater survival19 In other murine
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
112
models the use of antindashPD-1 and antindashCTLA-4 agentsshowed improved survival and increased tumor infiltratingleukocyte populations compared with single modalitywith concurrent radiation16 There are conflicting data re-garding timing or sequencing of therapy with some ani-mal models showing no difference in tumor response inrelation to timing of RT and delivery of immunotherapy18
For instance in one animal model CTLA-4 blockade de-livered simultaneously with radiation or delivered a coupleof days after showed no difference in survival among themice19
Increased PD-1 expression in circulating monocytes hasbeen identified as a biomarker for tumor-induced immu-nosuppression and may serve as a prognostic factor forpotentially worse survival outcomes in clinic13 In onestudy GBM patients with lower PD-L1 expression hadhigher median overall survival than those with higher PD-L1 expression suggesting that lower expression may beassociated with less immunosuppression and more im-mune activity against the tumor glioma20 RT with immunecheckpoint blockade is being investigated to assess if theaddition of PD-1 and PD-L1 inhibitors may improve theoutcomes or toxicity profile of standard therapy For in-stance a multi-institutional trial opened as a phase III willevaluate outcomes in GBM receiving radiation and pem-brolizumab with TMZ (NCT02530502) Next durvalumabor MEDI4736 a PD-L1 inhibitor is being examined forunmethylated MGMT GBMs with standard radiotherapy(NCT02336165)12 The impact of checkpoint inhibitorsduring adjuvant treatment of GBM is currently beingevaluated in the NCI-funded NRG-BN002 trial(NCT02311920) which will evaluate the antindashCTLA-4antibody ipilimumab alone or in combination with theantindashPD-1 antibody nivolumab for patients with newlydiagnosed GBM
Brain metastases have clonal populations of cells differ-ent from the rest of the brain and a unique microenviron-ment that may influence immunotherapy There may bemore immune infiltrates in metastases than in primarybrain tumors21 PD-L1 expression in brain metastasesvaries by histology In a series evaluating PD-L1 expres-sion in various tumors including melanoma NSCLCbreast renal colorectal and small cell less than 10showed significant expression22 There was greatest ex-pression among NSCLC and melanoma with a correla-tion between PD-L1 expression and tumor infiltratinglymphocytes22 Institutional series have examined thecombination of radiation and immune checkpoint block-ade In another study specific to melanoma brain metas-tases PD-L1 expression was found in over 50 of thecases and among those cases over 40 expressedPD-L1 in more than 5 of tumor cells23 The largest bodyof data for use of PD-L1 with radiation is for melanomaand NSCLC
Ipilimumab is a human monoclonal antibody that blocksCTLA-4 and allows for T-cell activation and proliferationto enhance the immune response to cancer In a
retrospective review of 70 patients with brain metastasestreated with SRS or WBRT the 33 patients receiving im-munotherapy had a median survival of 183 months incomparison to the 37 patients who did not receive ipili-mumab with a median survival of 53 months While therewere limited data among the cohort to evaluate sequenc-ing of therapy among 10 evaluable patients 40 whoreceived ipilimumab prior to RT had a partial response incomparison to only 10 among the cohort of 22 evalu-able patients who did not receive ipilimumab therapy atall with radiation24 Another retrospective institutionalstudy of 77 patients in which 37 received ipilimumabfound that patients treated with SRS and ipilimumab hada median survival of 213 months versus 49 months forthose not receiving ipilimumab Most interestingly theyidentified that the correlation remained significant evenafter adjusting for additional factors such as performancestatus Secondly there was not an increased need for useof salvage WBRT25
The sequencing of radiotherapy and immune checkpointinhibitors is of interest In a study of patients with brainmetastases the one-year survival for patients receivingSRS before ipilimumab was greater at 65 in contrast to56 for those receiving it concurrently and 40 for thosereceiving it after SRS26 Similarly another study of 75patients with 566 brain metastases showed greater tu-mor lesion response at 6 months from SRS for patientsreceiving ipilimumab nivolumab or pembrolizumabwithin 4 weeks of their SRS27 Those receiving concurrenttherapy had by 6 months a decrease of 949 in compar-ison to 662 for those not receiving checkpoint inhibi-tors within 4 weeks Prospective clinical trials areinvestigating different combinations of RT with immunecheckpoint blockers in this setting For instance new tri-als are currently evaluating intracranial tumor control at 6months and the timing of immune therapy or immunecheckpoint inhibitors in relation to SRS28
Vaccines are also being developed for primary braintumors showing some evidence for their use Vaccinesdeveloped from dendritic cells and tumor lysate with tu-mor antigens such as the epidermal growth factor recep-tor variant III vaccine have shown promise29 Forinstance in a placebo controlled phase II trial of ICT-107a vaccine composed on autologous dendritic cells andtumor antigens progression-free survival was increasedby 2 months for those receiving the vaccine30 Radiationmay assist in serving as a primer for the immunogeniceffects by facilitating tumor antigen uptake by dendriticcells and cross presentation on major histocompatibilitycomplex I Thus RT may assist in the tumor-specific cy-totoxic T lymphocytes associated with the immunemechanism
In conclusion although there may be challenges to com-bining and sequencing brain tumors radiosensitizersand immunotherapy the opportunities and potential fornovel applications are promising For brain tumors brainmetastases are typically underrepresented in trials
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
113
despite being among the most common intracraniallesions Despite their large population patients with brainmetastases are often excluded from clinical trials withnovel agents due to concerns regarding confounding out-comes and tolerability12 Primary gliomas also offer anovel frontier for the use of immunotherapy to standardadjuvant chemotherapy and radiation particularly forpatients with GBM less likely to respond to TMZ such aswith unmethylated MGMT As studies work to define therole of RT and radiosensitizers and immunotherapy fur-ther analysis is needed to assess the timing of RT andthese treatments
References
1 Stupp R Hegi ME Mason WP et al Effects of radiotherapy withconcomitant and adjuvant temozolomide versus radiotherapy aloneon survival in glioblastoma in a randomised phase III study 5-yearanalysis of the EORTC-NCIC trial Lancet Oncol 2009 10459ndash466
2 Lawrence TS Blackstock AW McGinn C The mechanism of actionof radiosensitization of conventional chemotherapeutic agentsSemin Radiat Oncol 2003 1313ndash21
3 Lesueur P Chevalier F Austry JB et al Poly-(ADP-ribose)-polymer-ase inhibitors as radiosensitizers a systematic review of pre-clinicaland clinical human studies Oncotarget 2017 8(40)69105ndash69124
4 Lester A Rapkins R Nixdorf S Khasraw M McDonald KCombining PARP inhibitors with radiation therapy for the treatmentof glioblastoma is PTEN predictive of response Clin Transl Oncol2017 19273ndash278
5 Gupta SK Kizilbash SH Carlson BL et al Delineation of MGMT hyper-methylation as a biomarker for veliparib-mediated temozolomide-sensi-tizing therapy of glioblastoma J Natl Cancer Inst 2016 108
6 Kleinberg LR Blakeley J Mikkelsen T et al An American BrainTumor Consortium (ABTC) phase 1 trial of veliparib (ABT-888)temozolomide (TMZ) and concurrent radiation therapy (RT) fornewly diagnosed glioblastoma multiforme (GBM) need for modifica-tion to approach for combining these therapies InternationalJ Radiat Oncol Biol Phys 2012 84S7ndashS8
7 Oronsky BT A Review of two promising radiosensitizers in brainmetastases Rrx-001 and 2-deoxyglucose In NC Oronsky edJ Cancer Sci Ther 2015 pp 137ndash141
8 Kim MM Parmar H Cao Y et al Concurrent whole brain radiother-apy and RRx-001 for melanoma brain metastases Neuro Onc2016 18455ndash456
9 Mehta MP Wang D Wang F et al Veliparib in combination withwhole brain radiation therapy in patients with brain metastasesresults of a phase 1 study J Neurooncol 2015 122409ndash417
10 Chabot P Hsia TC Ryu JS et al Veliparib in combination withwhole-brain radiation therapy for patients with brain metastasesfrom non-small cell lung cancer results of a randomized globalplacebo-controlled study J Neurooncol 2017 131105ndash115
11 Ochiai S Nomoto Y Yamashita Y et al Roles of valproic acid inimproving radiation therapy for glioblastoma a review of literaturefocusing on clinical evidence Asian Pac J Cancer Prev 201617463ndash466
12 Tan AC Heimberger AB Menzies AM Pavlakis N Khasraw MImmune checkpoint inhibitors for brain metastases Curr Oncol Rep2017 1938
13 DrsquoSouza NM Fang P Logan J Yang J Jiang W Li JCombining radiation therapy with immune checkpoint blockade
for central nervous system malignancies Frontiers Oncol 20166212
14 Parsa AT Waldron JS Panner A et al Loss of tumor suppressorPTEN function increases B7-H1 expression and immunoresistancein glioma Nat Med 2007 1384ndash88
15 Binder DC Davis AA Wainwright DA Immunotherapy for cancer inthe central nervous system current and future directionsOncoimmunology 2016 5e1082027
16 Newcomb EW Demaria S Lukyanov Y et al The combination ofionizing radiation and peripheral vaccination produces long-termsurvival of mice bearing established invasive GL261 gliomas ClinCancer Res 2006 124730ndash4737
17 Zeng J See AP Phallen J et al Anti-PD-1 blockade and stereotac-tic radiation produce long-term survival in mice with intracranial glio-mas Int J Radiat Oncol Biol Phys 2013 86343ndash349
18 Chow KK Hara W Lim M Li G Combining immunotherapy withradiation for the treatment of glioblastoma J Neurooncol2015123459ndash464
19 Belcaid Z Phallen JA Zeng J et al Focal radiation therapy com-bined with 4-1BB activation and CTLA-4 blockade yields long-termsurvival and a protective antigen-specific memory response in amurine glioma model PLoS One 2014 9e101764
20 Topalian SL Hodi FS Brahmer JR et al Safety activity and im-mune correlates of anti-PD-1 antibody in cancer N Engl J Med2012 3662443ndash2454
21 Bienkowski M Preusser M Prognostic role of tumour-infiltrating in-flammatory cells in brain tumours literature review Curr OpinNeurol 2015 28647ndash658
22 Harter PN Bernatz S Scholz A et al Distribution and prognostic rel-evance of tumor-infiltrating lymphocytes (TILs) and PD-1PD-L1 im-mune checkpoints in human brain metastases Oncotarget 2015640836ndash40849
23 Berghoff AS Ricken G Widhalm G et al Tumour-infiltrating lym-phocytes and expression of programmed death ligand 1 (PD-L1) inmelanoma brain metastases Histopathology 2015 66289ndash299
24 Silk AW Bassetti MF West BT Tsien CI Lao CD Ipilimumab and ra-diation therapy for melanoma brain metastases Cancer Med 20132899ndash906
25 Knisely JP Yu JB Flanigan J Sznol M Kluger HM Chiang VLRadiosurgery for melanoma brain metastases in the ipilimumab eraand the possibility of longer survival J Neurosurg 2012117227ndash233
26 Kiess AP Wolchok JD Barker CA et al Stereotactic radiosurgeryfor melanoma brain metastases in patients receiving ipilimumabsafety profile and efficacy of combined treatment Int J Radiat OncolBiol Phys 2015 92368ndash375
27 Qian JM Yu JB Kluger HM Chiang VL Timing and type of immunecheckpoint therapy affect the early radiographic response of mela-noma brain metastases to stereotactic radiosurgery Cancer 20161223051ndash3058
28 Silk AW Cao Y Gomez-Hassan D et al A randomized phase IIstudy of ipilimumab induction in patients with melanoma brain me-tastases receiving stereotactic radiosurgery J Clin Oncol 2015 33TPS9079ndashTPS9079
29 Neagu MR Reardon DA An Update on the role of immunotherapyand vaccine strategies for primary brain tumors Curr TreatOptions Oncol 2015 1654
30 Wen PY Reardon DA Phuphanich S et al A randomized double-blind placebo-controlled phase 2 trial of dendritic cell (DC) vaccina-tion with ICT-107 in newly diagnosed glioblastoma (GBM) patientsJ Clin Oncol 2014 322005ndash2005
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
114
British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

World Federation of Neuro-Oncology Societies
Editors Wolfgang Wick President EANO E Antonio Chiocca President SNO
Managing Editor EANO Roberta Rudagrave Torino Italy
SNO Editor Nicholas Butowski San Francisco USA
Editorial Board
Khaled Abdel Karim Cairo Egypt Egyptian Group of Neuro Oncology (EGNO) Sebastian Brandner London United Kingdom British Neuro-Oncology Society (BNOS)
Oumlz Buumlge Istanbul Turkey Noroonkiloji Dernegi (Neurooncology Society) (TNOD)
Chas Haynes Houston USA Society of Neuro-Oncology (SNO)
Filip de Vos Utrecht Netherlands Landelijke Werkgroep Neuro-Oncologie (LWNO)
Francois Ducray Lyon France Association des Neuro-Oncologues drsquoExpression Francaise (ANOCEF)
Anca Grosu Freiburg Germany German Neuro-Oncological Working Group (NOA)
Andreas Hottinger Lausanne Switzerland Swiss Group for Clinical Cancer Research Working Group Central Nervous System Tumors (SAKK)
Chae-Yong Kim Seoul Korea Korean Society for Neuro-Oncology (KSNO)
Zarnie Lwin Brisbaine Australia Asian Society of Neuro-Oncology (ASNO)
Marcos Maldaun Sao Paulo Brazil Society of Neuro-Oncology Latin America (SNOLA)
Christine Marosi Vienna Austria Austrian Society for Neuro-Oncology (SANO)
Mariacutea Martiacutenez Barcelona Spain Grupo Espanol de Investigacion en Neurooncologia (GEINO)
Motoo Nagane Tokyo Japan Japan Society for Neuro-Oncology (JSNO)
Roberta Rudagrave Torino Italy Associazione Italiana di Neuro-Oncologia (AINO
Gupta Tejpal Mumbai India Indian Society of Neuro-Oncology (ISNO)
Nicolas Whenham Brussels Belgium Belgian Association for Neuro-Oncology (BANO)
Yun-fei Xia Guangzhou China Chinese Society of Neuro-oncology (CSNO)
magazine
copy 2017 Published by The World Federation of Neuro-Oncology Societies This is an Open Access publication distributed under the terms of the Creative Commons Attribution License (httpcreativecommonsorglicensesby40) which permits unrestricted reuse distribution and reproduction in any medium provided the original work is properly cited
Editorial
First of all on behalf of EANO I wouldlike to congratulate the SNO leader-ship for an amazing conference inSan Francisco In addition to theinsights from invited lectures and ed-ucational activities in part supportedby the US Moonshot program theEANO highlight for sure was theaward-winning clinical abstract onthe CeTeG-trial in which UlrichHerrlinger from Bonn presented theNOA-09 trial demonstrating an over-all survival benefit in a small but con-trolled randomized study for thecombination of cyclic CCNU andtemozolomide in patients withnewly diagnosed glioblastoma har-boring a hypermethylated MGMTpromoter
In this issue of the magazine we willhave opinion papers on the value ofbrain tumor epigenetics as well as onthe role of radiation therapy in com-bined modality therapies with a focusnot only on the classical approachesbut also radiosensitization and immu-notherapies In addition to the largebody of literature on precision medi-cine approaches three colleaguesfrom the US share their vision on thepresent but more important also onthe potential future use of next-gener-ation sequencing and other high-throughput technologies in neuro-oncology We have the periodicupdates on Nurses Activities featuredarticles from Neuro Oncology andNeuro Oncology Practice as well as a
view from the EANO youngsters onmentoring
Two of our national organizations(the British and the Indiansocieties) present their views on theWFNOS and the national IndianNeuro Oncology conferencerespectively
On behalf of my colleagues from theEANO board I would like to wish allreaders a successful completion of2017 and a great start into the year2018 with one highlight our EANOconference in Stockholm in Octoberalready determined
W Wick
President EANO
99
Volume 2 Issue 3 Editorial
Editorial
This year from November 15 to 19SNO held its 22nd annual meeting inSan Francisco Each meeting has atheme and this yearrsquos overall themefocused on the ldquoCancer Moonshotrdquoprogram that was proposed byformer president Obama in 2016 andwas initially led by former vice-president Biden whose son perishedfrom a GBM The meeting wasattended by over 2500 participantsfrom all over the world with a recordnumber of submitted abstracts (over1800) The meeting was preceded bytwo successful former meetings theNeuro-oncology Review Course andthe SNOSCIDOT course on intersti-tial CNS delivery both held on Nov15 Our Education Day was held onNov 16 it focused on the subject ofGBM resistance and was organizedby Sue Bell Robert Cavaliere KhalidShah and Albert Kim The mainmeeting was organized by ManishAghi Vinay Puduvalli and FrankFurnari and was highlighted by key-note talks by Jennifer Doudna on
CrispRCas9 and Carlo Croce onmicroRNAs There were multipleSNO educational events from a sun-rise session to lunchtime tutorialsand dinner events such as very wellattended poster and e-talk sessionsThere were also multiple events dedi-cated to stress relief as well includ-ing opening receptions gala dinnersand burnout relief events We are
looking forward to the 23rd meetingin New Orleans which will be led byour new officers (President PatrickWen Vice-President Gelared Zadehand SecretaryTreasurer TracyBatchelor)
EA (Nino) Chiocca
President SNO
100
Volume 2 Issue 3 Editorial
Brain TumorEpigeneticsFrom Researchto ClinicalPractice
Silvia MarinoBlizard Institute Barts and The London School ofMedicine and Dentistry Queen Mary University ofLondon 4 Newark Street E12AT London UK
101
IntroductionEpigenetics is defined as the study of heritable changesin gene expression that are not caused by alterations inDNA sequences1 The phenotypic difference between acaterpillar and a butterfly for example is due to epige-netic regulation of gene expression in the same animalwith the same DNA I particularly like this example to ex-plain the meaning of the term epigenetics as it impres-sively demonstrates how powerful these mechanisms arein controlling phenotypic changes Epigenetic changesare reversible and include the key processes of DNAmethylation histone modifications and noncoding RNA-associated gene silencing (recently reviewed2) known toplay an essential role during the embryonic and postnataldevelopment of an organism and in tissue homeostasis2
Disruptions of epigenetic processes can induce changesin gene function which together with genetic changescan lead to the neoplastic transformation of a normal cell(recently reviewed)3
Recent technological advances have significantly con-tributed to the tremendous progress in understandinghow these epigenetic modifications are regulated in nor-mal cells and deregulated in cancer cells For examplethis knowledge has enabled the translation into better di-agnostic algorithms for tumor classification prognostica-tion and risk assessment Importantly we are nowentering a time when novel therapies targeting thesederegulated epigenetic mechanisms are being devel-oped with some of them showing very promising effectsin preclinical models
It is beyond the scope of this article to comprehensivelyreview mechanisms of epigenetic regulation of gene ex-pression and their deregulation in brain tumors excellentrecent reviews are available to the readers on thesesubjects2ndash5 Here I will discuss a few examples of recentepigenetic discoveries which have informed the develop-ment of novel diagnostic and prognostic tools or led tosuccessful preclinical testing of new epigenetic drugs inexperimental models
Epigenetic Profiles inthe MolecularClassification of BrainTumorsGlioma One of the first examples of an epigenetic changeinforming the design of an assay for diagnostic screeningto corroborate a therapeutic decision is the assessmentof methylation of the MGMT promoter in malignantgliomas6 MGMT (O6-methylguanine DNA methyltransfer-ase) is a key enzyme in the DNA repair network which
removes the mutagenic and cytotoxic adducts from O6
guanine in DNA the preferred point of attack of alkylatingchemotherapeutic agents (ie BCNU temozolomide etc)Hypermethylation of cytosine-phosphate-guanine (CpG)islands located in the promoter region of MGMT is pri-marily responsible for the loss of MGMT function in manytumor types hence leading to an increased sensitivity tothe killing effects of alkylating drugs used in chemo-therapy6 This test is widely used in clinical practice topredict response to temozolomide the alkylating drug ofchoice in high-grade gliomas although it should bestressed that there is still no consensus as to which testmethod to use which CpG sites to assess and what themethylation cutoff should be
Ependymoma Until very recently these tumors havebeen subclassified and graded on the basis of histologi-cal features into low and high grade In 2015 a molecularclassification based on DNA methylation profiling hasbeen proposed which defines 9 molecular subgroups 3for each anatomical location of these tumors (supratento-rial posterior fossa and spinal cord)7 In the supratento-rial location ependymomas with the fusion geneC11ORF95RELA (ST-EPN-RELA) have a poor prognosisand in the posterior fossa it is the ependymoma groupEPN-A that is characterized by a poor prognosis7 Allother ependymomas show a comparatively goodprognosis7 Although not yet included in the World HealthOrganization (WHO) 2016 classification a recent consen-sus paper has recommended that this classification beused for enrollment in prospective clinical trials8 and it isexpected to contribute to informing decisions onmolecular-based treatments as they become available
Medulloblastoma (MB) International consensusrecognizes 4 medulloblastoma molecular subgroupsWNT (MBWNT) SHH (MBSHH) Group 3 (MBGrp3) andGroup 4 (MBGrp4) each defined by their characteristicDNA methylation and genome-wide transcriptomicprofiles9 Recently the heterogeneity within these sub-groups has been reduced by 2 independent studieswhich have defined additional subtypes Schwalbe andcolleagues10 have suggested to split MBSHH into 2 age-dependent subtypes corresponding to ldquoinfantrdquo (lt43 y)and ldquochildhoodrdquo patients (43 y) and MBGrp3 andMBGrp4 into further high-risk and low-risk subtypes whilethe MBWNT group remains unchanged10 Interestingly thelow-risk subtypes were defined primarily by hypermethy-lation in comparison to normal cerebellum whereas thehigh-risk subtypes were defined by relativehypomethylation10 Cavalli and coauthors11 used integra-tive clustering of DNA methylation and gene expressiondatasets from 763 patients to split the original 4 sub-groups into 12 subtypes MBSHH is split into 4 subtypes(abc d) MBWNT into 2 subtypes (ab) MBGrp3 andMBGrp4into 3 subtypes each (abc)11 The subtypes iden-tified in these 2 studies overlap considerably and themain differences seem to be related to the inclusion ofadult MB patients in the Cavalli study Importantly MBsubgroups and their subtypes identified by their
Brain Tumor Epigenetics From Research to Clinical Practice Volume 2 Issue 3
102
epigenetic and related transcriptional profiles1011 havedistinct genetic and clinicopathological features1011 andtheir implementation for patient stratification for betterprognostication and enrollment into subgroupsubtype-directed therapies in the context of clinical trials will be astep change in the treatment of MB patients
All CNS tumors A classification tool for brain tumorsbased on genome-wide DNA methylation patterns and arandom forest-based machine learning approach hasbeen developed and extensively tested by the GermanCancer Research Center (wwwmolecularneuropathologyorg) This resource is available online and has provento be a valuable tool to improve brain tumor diagnosticsThis approach has facilitated the identification of com-mon druggable molecular pathway alterations across var-ious histological tumor entities thus allowing patients toenter the most appropriate clinical trials and in somecases be offered molecularly matched therapies As anexample DNA methylation profiles allow precise identifi-cation of cases with mitogen-activated protein kinase(MAPK) activation which is a feature of tumors withBRAF V600E mutation1213 which can span various tradi-tional histological entities such as pilocytic astrocytomaspleomorphic xanthoastrocytomas ganglioglioma andsubependymal giant cell astrocytomas to predict re-sponse to specific inhibitors interrupting the BRAFMEKcomponent of the MAP kinase pathway14
Novel TherapeuticApproaches TargetingEpigeneticDeregulationDiffuse intrinsic pontine glioma (DIPG) is a highlyaggressive pediatric tumor located in the brainstem andcharacterized by a rapid and diffusely infiltrative patternof growth These tumors cannot be treated surgicallybecause of their location and infiltrative nature15
Radiation therapy is the standard treatment although itprovides only temporary symptom relief with no overallsurvival benefits and conventional chemotherapy drugsare ineffective15
Mutations in histone H3 variants occur in more than 80of DIPG and result in a lysine-to-methionine substitution(H3K27M)16 17 H3K27M has been shown to inhibitpolycomb repressive complex 2 (PRC2) by binding to itscatalytic subunit EZH2 and reducing the methylation ofH3 at lysine 27 (H3K27me) at selected target loci18 Theresidual PRC2 activity is required to maintain DIPGproliferative potential by repressing neuronaldifferentiation in patient-derived cell lines and in agenetically engineered mouse model1920 Importantlysmall-molecule EZH2 inhibitors abolish tumor cell growth
in these models raising the possibility that inhibitionof EZH2 could be a novel therapeutic strategy for thesetumors19
An independent study showed that H3K27M associateswith increased H3K27 acetylation (H3K27ac) and that themajority of the heterotypic H3K27M-K27ac nucleosomesco-localize with bromodomain proteins at the loci of ac-tively transcribed genes20 The authors have shown thatblocking the recruitment of bromodomain proteins by het-erotypic H3K27M-K27ac nucleosomes in DIPG with bro-modomain and extraterminal domain family inhibitorsefficiently inhibited tumor progression thus identifying thisclass of compounds as potential therapeutics in DIPG20
These important advances in understanding the underly-ing biology of DIPG have led to the identification of novelepigenetic therapeutic approaches which are very effec-tive at the preclinical level and if confirmed in transla-tional studies could change the way we treat thesetumors in the near future
Conclusion and outlookThese are exciting and challenging times for theneuro-oncology community Exciting because there isgrowing expectation in the field that new discoveriessuch as those discussed in this article can soon translateinto new and more effective therapeutic approachesChallenging because it is clear that new skill sets are re-quired to effectively apply them to benefit patients
The clinical training in many neuro-oncology specialtieswill have to take into account the additional knowledgeand skills needed in the field and offer education incomplementary disciplines such as next-generationsequencing technologies integrated with interpretativedata analysis as well as molecular biology for the designof biologically informed assays and tools The require-ment for these new highly specialized skills also needs tobe reflected in the composition of the clinical teamswhere bioinformatics expertise will play an increasinglyimportant role for the integration of multimodal data inpatient care
References
1 Waddington CH Canalization of development and the inheritance ofacquired characters Nature 1942150563ndash565
2 Allis CD Jenuwein T The molecular hallmarks of epigenetic controlNat Rev Genet 201617487ndash500
3 Flavahan WA Gaskell E Bernstein BE Epigenetic plasticity and thehallmarks of cancer Science (New York NY 2017357
4 Edwards JR Yarychkivska O Boulard M Bestor TH DNA methyla-tion and DNA methyltransferases Epigenetics amp chromatin20171023
5 Filbin MG Suva ML Gliomas genomics and epigenomics arriving atthe start and knowing it for the first time Annual Rev Pathol201611497ndash521
6 Hegi ME et al MGMT gene silencing and benefit from temozolomidein glioblastoma N Engl J Med 2005352997ndash1003
Volume 2 Issue 3 Brain Tumor Epigenetics From Research to Clinical Practice
103
7 Pajtler KW et al Molecular Classification of Ependymal Tumorsacross All CNS Compartments Histopathological Grades and AgeGroups Cancer Cell 201527728ndash743
8 Pajtler KW et al The current consensus on the clinical managementof intracranial ependymoma and its distinct molecular variants ActaNeuropathol 20171335ndash12
9 Taylor MD et al Molecular subgroups of medulloblastoma the cur-rent consensus Acta Neuropathol 2012123465ndash472
10 Schwalbe EC et al Novel molecular subgroups for clinical classifi-cation and outcome prediction in childhood medulloblastoma a co-hort study Lancet Oncol 201718958ndash971
11 Cavalli FMG et al Intertumoral Heterogeneity withinMedulloblastoma Subgroups Cancer Cell 201731737ndash754 e736
12 Schindler G et al Analysis of BRAF V600E mutation in 1320 nervoussystem tumors reveals high mutation frequencies in pleomorphicxanthoastrocytoma ganglioglioma and extra-cerebellar pilocytic as-trocytoma Acta Neuropathol 2011121397ndash405
13 Tanaka S et al Epithelioid glioblastoma arising from pleomorphicxanthoastrocytoma with the BRAF V600E mutation Brain TumorPathol 201431172ndash176
14 Banerjee A et al A phase I trial of the MEK inhibitor selumetinib(AZD6244) in pediatric patients with recurrent or refractory low-grade glioma a Pediatric Brain Tumor Consortium (PBTC) studyNeuro Oncol 2017191135ndash1144
15 Hargrave D Bartels U Bouffet E Diffuse brainstem glioma in chil-dren critical review of clinical trials Lancet Oncol 20067241ndash248
16 Schwartzentruber J et al Driver mutations in histone H33 and chro-matin remodelling genes in paediatric glioblastoma Nature2012482226ndash231
17 Wu G et al Somatic histone H3 alterations in pediatric diffuse in-trinsic pontine gliomas and non-brainstem glioblastomas Naturegenetics 201244251ndash253
18 Lewis PW et al Inhibition of PRC2 activity by a gain-of-function H3mutation found in pediatric glioblastoma Science (New York NY2013340857ndash861
19 Mohammad F et al EZH2 is a potential therapeutic target forH3K27M-mutant pediatric gliomas Nature Med 201723483ndash492
20 Piunti A et al Therapeutic targeting of polycomb and BET bromodo-main proteins in diffuse intrinsic pontine gliomas Nature Med201723493ndash500
Brain Tumor Epigenetics From Research to Clinical Practice Volume 2 Issue 3
104
The Value of SurgicalResection for MalignantGliomas in the ModernEra Beyond Extent ofResection
Stephen G Bowden MDSeunggu Jude Han MDDepartment of Neurological Surgery OregonHealth and Sciences University 3303 SW BondAve Center for Health and Healing CH8NPortland OR 97239 Telephone 503-494-4314Fax 503-346-6810 hanseohsuedu
105
Malignant gliomas are among the most difficult oncologi-cal entities to treat Despite aggressive treatment prog-nosis remains poor and recurrence and treatmentfailures seem inevitable The current standard-of-caretherapy includes maximal safe surgical resection fol-lowed by concurrent and adjuvant chemoradiotherapyHistorically surgical resection has conferred greater sur-vival benefit to these patients than adjuvant therapiespresumably through the cornerstone principle of cytore-duction However the extent of surgical resection is fre-quently limited by nearby eloquent tissue and risks to keyneurological functions In addition the value of such ag-gressive approaches has been questioned in light of thewidespread infiltration of glioma cells Meanwhile our un-derstanding of glioma biology continues to advance rap-idly fueled in large part by the acquisition of tumor tissueduring surgery Thus the exact role and value of surgeryparticularly in comparing the clinical benefits of maximalextent of resection (EOR) with the biomedical benefits oftissue provision has been a topic of great interest anddebate in both the neuro-oncological and neurosurgicalcommunities
EOR patient age tumor histology performance statusand molecular markers have been widely accepted assignificant predictors of patient outcomes in malignantglioma9 In the past 2 decades many large retrospectivecohort studies have demonstrated improvements in sur-vival with increasing EOR5917 Due to ethical considera-tions evidence from a randomized prospective studysupporting the clinical benefit of aggressive resectionsdoes not exist and likely never will Instead the closestthing to such evidence in malignant glioma comes fromthe randomized phase III trial comparing surgical resec-tions with or without the use of 5-aminolevulinic acid(5-ALA) The use of 5-ALA serving as a means to and aproxy for greater EOR resulted in extended overall sur-vival for patients with newly diagnosed glioblastoma19 Arecent meta-analysis of 41 117 unique patients by Brownet al adherent to the guidelines of PRISMA (PreferredReporting Items for Systematic Reviews and Meta-Analyses) also demonstrated a clear survival benefit forgross total resection over subtotal resection or biopsy atupfront surgery for glioblastoma1 The body of literatureas a whole clearly favored aggressive resections andthere seemed to be little disagreement for a strategytoward maximal resection when clinically feasibleHowever the challenge still remains when such strategiescome at the risk of neurological morbidity A recent reportby Rahman et al illustrates that the survival benefits fromaggressive resection are lost if the patient develops anew postoperative neurologic deficit as a result15
All the while our understanding of glioma genetics mo-lecular biology and mechanisms of resistance has con-tinued to deepen and evolve borne of thoughtful andsystematic studies using patient-acquired tumor sam-ples Molecular profiles and tumor genetics have proventhemselves to be the best predictors of clinical behaviorand now represent crucial components of the diagnostic
classification scheme of infiltrating gliomas12 With tumortissue at the molecular and genetic level being able to ro-bustly predict patient outcomes accurate tissue diagno-sis has become paramount in the management ofgliomas The role and value of open surgical resection to-ward this end have become clearer as concerns of sam-pling error with biopsy alone led to a number of studiesevaluating the ldquoaccuracyrdquo of stereotactic biopsy proce-dures Jackson et al reported a series of 81 patients whounderwent stereotactic biopsy followed by open surgicalresection The tissue diagnosis was concordant betweenbiopsy and open resection samples in only 51 ofpatients6 Other studies have also demonstrated diagnos-tic concordance between stereotactic biopsy and surgi-cal resection samples in only 57 to 79 ofcases131428 The major limitation of stereotactic biopsyfor infiltrating gliomas likely stems from the significantintratumoral heterogeneity and collectively these studieshighlight the value of open surgical resection in providinga more global representation and understanding of thetumor tissue
The value of extensive resection is perhaps even moreprofound when considering the therapeutic implicationsof such heterogeneity Multiple-site and serial-samplinganalyses have revealed a high degree of both spatial andtemporal heterogeneity within these tumors a conse-quence of serial evolutionary events during tumor growthand progression23 These studies have also led to theconcept of therapy-driven clonal selection and preferen-tial regrowth of resistant cell populations as a potentialmechanism of treatment failure Efforts to expand our un-derstanding of the tremendously complex network ofmutations and biological consequences of chronologicalhierarchy would be greatly facilitated by carefullyplanned thoughtful acquisition of tumor samples duringsurgery
Despite the recent paradigm shift in glioma diagnosticclassification little gains have been made in improvingthe overall prognosis for patients with malignant gliomassince the introduction of concurrent and adjuvant temo-zolomide in 200521 The strategies more recently tested inlarge randomized phase III trials by and large have yieldeddisappointing results while the reasons and mechanismsof treatment failures remain unclear Even so encourag-ing responses have occasionally been seen in varioussubsets of patients and studies exploring the presenceof potential biomarkers have generated intriguing andpromising results in these populations The developmentof the antindashvascular endothelial growth factor monoclonalantibody bevacizumab is one such example Two initialphase II trials showed prolonged progression-free sur-vival in recurrent glioblastoma relative to historical con-trols prompting the US Food and Drug Administration togrant accelerated approval to bevacizumab for recurrentglioblastoma in 2009825 However 2 large randomized tri-als evaluating the addition of bevacizumab to radiationand temozolomide in the newly diagnosed setting failedto show a benefit in overall survival24 and its utility in the
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
106
recurrent setting is now a topic of debate in light of sub-sequent phase III trial results However a post hoc analy-sis of patients enrolled in the AVAglio trial recentlydemonstrated that bevacizumab improved overall sur-vival for those with a proneural subtype tumor18 Just asO6-methylguanine-DNA-methyltransferase (MGMT) pro-moter methylation does for temozolomide the geneticprofile of the tumor could serve as a potential biomarkerof clinical response for bevacizumab as well and valida-tion studies are currently ongoing Such analyses al-though performed post hoc require targeted prospectivecollection of tumor tissue at initial surgery In addition ge-netic profiling of newly diagnosed malignant gliomas willneed to become routine if this approach is to be utilizedwidely Similarly cilengitide an inhibitor of aVb3 andaVb5 integrins with anti-angiogenic properties showedinitial promise in recurrent glioblastoma studies but failedto show any additional benefit in the newly diagnosedsetting20 A subsequent post hoc analysis of the phase IItrial revealed improved progression-free and overall sur-vival in patients with high aVb3 levels in the tumor cells26
However tumor tissues were not systematically collectedand less than half of the patientsrsquo tumor tissues wereavailable for analysis from the phase III trialUnfortunately this drug will most likely not undergo fur-ther development and one cannot help wonder if the out-come would have been different if the enrollment in thephase III trial had been enriched for or restricted to tumorswith high expression of the aVb3 integrin The only trueldquosuccess storyrdquo since the adaptation of radiation andtemozolomide has come from the novel approach of tu-mor treating fields (TTFields) a transcutaneous deliveryof low-intensity intermediate frequency alternating elec-tric fields The multicenter phase III trial EF-14 random-ized patients with supratentorial glioblastoma withoutevidence of tumor progression following standard che-moradiation to receive maintenance treatment withTTFields plus temozolomide or temozolomide alone22
The study was terminated early based on results of aplanned interim analysis demonstrating benefit inprogression-free survival overall survival a secondaryendpoint was also significantly enhanced at this timeDespite the trialrsquos success TTFields has not been univer-sally adopted by the neuro-oncology community andenthusiasm among clinicians and patients remains low27
Experts have raised concerns regarding the study designsuch as its open-label design lacking a sham-treatmentcontrol arm as well as the generalizability of the resultsbased on the unique randomization point occurring afterconcurrent chemoradiation16 Perhaps most significantlya lack of widely understood mechanism of action hasalso been raised as a factor with comparison to othertreatments the preclinical data for TTFields is relativelylacking particularly when applied in conjunction with che-moradiation27 Even during the early phase stages theuse of robust tissue-based analyses exploring the mech-anism of action such as dose response modeling andmultisite tissue biopsies may have mitigated some of
these concerns and led to wider acceptance by the com-munity Bevacizumab and cilengitide clearly benefitedfrom retrospective analyses of human tumor tissue toidentify susceptible treatment populations while the en-thusiasm for TTFields is perhaps in part tempered by thelack thereof Collectively the evolution of these treat-ments underscores the value of extensive targeted tissuesampling in furthering development of new adjunctivetherapies
Open surgical resection of tumors with such targeted tis-sue acquisition for analysis will continue to play a key rolein prospective clinical trial designs Comparison ofpretreatment and posttreatment tissue profiles representsa valuable line of investigation by delving into mecha-nisms of therapeutic action as well as mechanisms oftreatment failures1011 It also provides an opportunity toinvestigate a number of key fundamental steps along anagentrsquos path to clinical success such as does the agentsuccessfully traffic to the tumor if so how much anddoes the agent then actually have its hypothesizedeffects at the biochemical or cellular level Thusearly-phase trials can and should include posttreatmentmolecular endpoints when possible in addition to safetyendpoints Immunotherapy and immune checkpoint inhi-bition represent exciting novel therapeutic approachesfor neuro-oncology particularly based on their success inmetastatic cancers Large phase III trials studying block-ade of the programmed cell death protein (PD)1PDligand 1 axis with monoclonal antibodies for newlydiagnosed and recurrent glioblastoma are under way butinitial reports have been concerning for negative resultsAs in the development of many previous novel agentstissue-based mechanism studies have been largely lack-ing in the preclinical phases However an Alliance-supported trial currently enrolling focuses on a biomarkeras a primary endpoint patients with recurrent glioblas-toma indicated for surgery are randomized to receivepembrolizumab a PD1 inhibitor either before or aftersurgery (NCT02852655) The resected tumor tissue willthen be analyzed for the profile of tumor-infiltratingT cells and comparison will be made between the 2groups This study represents a tremendously valuableopportunity to explore the impact and the potential chal-lenges of checkpoint inhibition for malignant gliomas inthe clinical setting and should the large phase III trialsend up negative this pilot study will be very informative
Advances in imaging biomarkers and molecular charac-terization of gliomas in conjunction with new targetedtherapies will continue to improve and transform themanagement of these tumors Multimodality imaging cannow more accurately reflect ongoing biological processeswithin these tumors such as the presence of oncogenicmutations or cells undergoing malignant transformationNovel biomarkers such as circulating tumor DNA showpromise in detecting early recurrence or monitoring treat-ment response3724 Lastly the new classification schemerevolving around molecular characterization will provide a
Volume 2 Issue 3 The Value of Surgical Resection for Malignant Gliomas in the Modern Era
107
necessary corollary to these novel diagnostic tools Itremains indisputable however that clinical validation ofthese novel diagnostic tools will also require systematiccorrelation with human tumor tissue obtained throughsurgery These samples ideally gathered prospectivelywill provide a pivot upon which we can expand our under-standing of the complex network of oncological pro-cesses driving these tumors
Malignant gliomas are incredibly challenging disease en-tities in many ways due to the inter- and intratumoral het-erogeneity that is a hallmark of them Experience to datehints that future successes in malignant gliomas rest inneuro-oncology entering the era of precision medicinewhere validated biomarkers and targeted personalizedtherapies are seamlessly integrated into the managementparadigm Accordingly systems supporting surgical re-section and patient-specific tumor tissue analysis mustbe built and organized to guide the decision making fortherapy As our overall approach to the management ofmalignant gliomas evolves so should the framework ofsurgical management The clinical benefits of maximalsafe resection are well founded and well reportedHowever the oncological neurosurgeon must now lookbeyond maximal cytoreduction itself and recognize thevalue of thoughtful acquisition and analysis of tumor tis-sue Modern neurosurgeons must consider themselvessurgical neuro-oncologists and engagement and partici-pation of surgeons into clinical trials particularly early-phase trials should be encouraged and valued In turnwe should provide our surgical trainees with the trainingand tools in neuro-oncology to help them participate andcontribute in multidisciplinary collaborative efforts aimingto advance the understanding of brain tumor biology andultimately improve the outlook of our patients
References
1 Lacroix M Abi-Said D Fourney DR Gokaslan ZL et al A multivariateanalysis of 416 patients with glioblastoma multiforme prognosisextent of resection and survival J Neurosurg 2001 95190ndash198
2 Hervey-Jumper SL Berger MS Maximizing safe resection of low-and high-grade glioma J Neurooncol 2016 130269ndash282
3 Sanai N Polley MY McDermott MW Parsa AT Berger MS An ex-tent of resection threshold for newly diagnosed glioblastomas JNeurosurg 2011 1153ndash8
4 Stummer W Pichlmeier U Meinel T et al Fluorescence-guided sur-gery with 5-aminolevulinic acid for resection of malignant glioma arandomised controlled multicentre phase III trial Lancet Oncol2006 7392ndash401
5 Brown TJ Brennan MC Li M et al Association of the extent ofresection with survival in glioblastoma a systematic review andmeta-analysis JAMA Oncol 2016 21460ndash1469
6 Rahman M Abbatematteo J De Leo EK et al The effects of new orworsened postoperative neurological deficits on survival of patientswith glioblastoma J Neurosurg 2017 127123ndash131
7 Louis DN Perry A Reifenberger G et al The 2016 World HealthOrganization Classification of Tumors of the Central NervousSystem a summary Acta Neuropathol 2016 131803ndash820
8 McGirt MJ Bulsara KR Cummings TJ et al Prognostic value ofmagnetic resonance imaging-guided stereotactic biopsy in the
evaluation of recurrent malignant astrocytoma compared with a le-sion due to radiation effect J Neurosurg 2003 9814ndash20
9 Muragaki Y Chernov M Maruyama T et al Low-grade glioma onstereotactic biopsy how often is the diagnosis accurate MinimInvasive Neurosurg 2008 51275ndash279
10 Woodworth G McGirt MJ Samdani A Garonzik I Olivi AWeingart JD Accuracy of frameless and frame-based image-guided stereotactic brain biopsy in the diagnosis of glioma com-parison of biopsy and open resection specimen Neurol Res 200527358ndash362
11 Suzuki H Aoki K Chiba K et al Mutational landscape and clonal ar-chitecture in grade II and III gliomas Nat Genet 2015 47458ndash468
12 Stupp R Mason WP van den Bent MJ et al Radiotherapy plus con-comitant and adjuvant temozolomide for glioblastoma N Engl JMed 2005 352987ndash996
13 Kreisl TN Kim L Moore K et al Phase II trial of single-agent bevaci-zumab followed by bevacizumab plus irinotecan at tumor progres-sion in recurrent glioblastoma J Clin Oncol 2009 27740ndash745
14 Vredenburgh JJ Desjardins A Herndon 2nd JE et al Phase II trial ofbevacizumab and irinotecan in recurrent malignant glioma ClinCancer Res 2007 131253ndash1259
15 Chinot OL Wick W Mason W et al Bevacizumab plusradiotherapy-temozolomide for newly diagnosed glioblastomaN Engl J Med 2014 370709ndash722
16 Gilbert MR Dignam JJ Armstrong TS et al A randomized trial ofbevacizumab for newly diagnosed glioblastoma N Engl J Med2014 370699ndash708
17 Sandmann T Bourgon R Garcia J et al Patients with proneural glio-blastoma may derive overall survival benefit from the addition of bev-acizumab to first-line radiotherapy and temozolomide retrospectiveanalysis of the AVAglio trial J Clin Oncol 2015 332735ndash2744
18 Jackson RJ Fuller GN Abi-Said D et al Limitations of stereotacticbiopsy in the initial management of gliomas Neuro Oncol 20013193ndash200
19 Stupp R Hegi ME Gorlia T et al Cilengitide combined with stan-dard treatment for patients with newly diagnosed glioblastoma withmethylated MGMT promoter (CENTRIC EORTC 26071-22072study) a multicentre randomised open-label phase 3 trial LancetOncol 2014 151100ndash1108
20 Weller M Nabors LB Gorlia T et al Cilengitide in newly diagnosedglioblastoma biomarker expression and outcome Oncotarget2016 715018ndash15032
21 Stupp R Taillibert S Kanner AA et al Maintenance therapy withtumor-treating fields plus temozolomide vs temozolomide alone forglioblastoma a randomized clinical trial JAMA 20153142535ndash2543
22 Wick W TTFields where does all the skepticism come from NeuroOncol 2016 18303ndash305
23 Sampson JH Alternating electric fields for the treatment of glioblas-toma JAMA 2015 3142511ndash2513
24 Lang FF Asher A Prospective clinical trials of brain tumor therapy thecritical role of neurosurgeons J Neurooncol 2004 69151ndash167
25 Lang FF Gilbert MR Puduvalli VK et al Toward better early-phasebrain tumor clinical trials a reappraisal of current methods and pro-posals for future strategies Neuro Oncol 2002 4268ndash277
26 Elkhaled A Jalbert L Constantin A et al Characterization of metab-olites in infiltrating gliomas using ex vivo (1)H high-resolution magicangle spinning spectroscopy NMR Biomed 2014 27578ndash593
27 Jalbert LE Neill E Phillips JJ et al Magnetic resonance analysis ofmalignant transformation in recurrent glioma Neuro Oncol 2016181169ndash1179
28 Touat M Duran-Pena A Alentorn A Lacroix L Massard C Idbaih AEmerging circulating biomarkers in glioblastoma promises andchallenges Expert Rev Mol Diagn 2015 151311ndash1323
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
108
Update on RadiationCombinations in theTreatment of Patientswith Malignant BrainTumors FromRadiosensitizers toImmunotherapy
Debra Nana Yeboa MD1
Erik P Sulman MD PhD123
Departments of 1Radiation Oncology2Translational Molecular Pathology and3Genomic Medicine The University of Texas MDAnderson Cancer Center 1515 Holcombe BlvdUnit 97 Houston Texas USA Tel 713-563-2300dnyeboamdandersonorg andepsulmanmdandersonorg
109
AbstractAdvances in radiosensitizers and immunotherapyhave ushered in a new frontier in brain tumortreatment The brain has often been viewed as asanctuary site due to the bloodndashbrain barrier andthus the 2 primary modalities of therapy includedsurgery and radiation therapy (RT) More recentlysystemic therapies have played a greater role aseither combination therapy radiosensitizers or im-munotherapy Two novel radiosensitizers are beingdeveloped for the treatment of brain metastasesRRx-001 for example is a small molecule thataccelerates the NO2 to NO conversion of deoxyhe-moglobin and the agent 2-dexoyglucose (2-DG) is anonmetabolized glucose analogue that interfereswith ATP formation Poly(ADP-ribose) DNA polymer-ase inhibitors are promising due to their distinctradiobiological effects Veliparib and olaparib areamong the most studied with randomized trialsexploring their use in gliomas and brain metastasesImmunotherapy including immune checkpoint inhib-itors may play a role for both primary gliomas andbrain metastases RT has been shown to enhancethe function of cytotoxic T lymphocytes induce infil-tration of cytotoxic T lymphocytes and enhancefunction Trials are presently exploring use of bothprogrammed cell death protein (PD)1 and PD ligand1 blockade in glioblastoma patients with radiationSimilarly several immunotherapies are being investi-gated with either stereotactic radiosurgery or wholebrain radiation therapy for brain metastases In thisreview the use of radiosensitizers and immunother-apy agents with RT will be discussed broadly
Keywords brain metastases brain tumors gliomasimmunotherapy radiation therapy radiosensitizers
Radiosensitizers andImmunotherapy inBrain TumorsAdvances in radiosensitizers and immunotherapy haveushered in a new frontier to brain tumor treatment Braintumors however are a diverse class sharing only similaranatomic location Both primary brain malignancies andbrain metastasis have widely diverse histologies and mo-lecular phenotypes With the bloodndashbrain barrier thebrain has often been viewed as a sanctuary site and thusthe 2 primary modalities of therapy included surgery andradiation with decreased benefit from systemic agentsdue to lack of brain penetration However more recentlysystemic therapies have played a greater role as eithercombination therapy radiosensitizers or immunother-apy While temozolomide (TMZ) has played a pivotal rolefor glioblastoma (GBM) only a subset of patients benefitfrom the treatment1 The use of alternative systemicagents that may potentiate the effects of radiation ther-apy (RT) is becoming increasingly appealing Similarly forbrain metastases a variety of systemic agents are beingexplored primarily based on histology and immune pro-file In this review the use of radiosensitizers and immu-notherapy agents currently under investigation with RTwill be discussed
RadiosensitizersThe guiding concept of radiation sensitization is to in-crease the biologic effect of radiation such as increasedDNA damage decreased DNA repair decreased hypoxiaor increased G2M cell cycle blockade leading to im-proved tumor control and increased patient survival2
Poly(adenosine diphosphate-ribose) DNA polymerase(PARP) inhibitors are promising radiosensitizers due totheir roles in DNA repair3 PARP inhibitors work againstPARP1 a nuclear enzyme involved in the recruitment ofrepair proteins used in base excision repair and single-strand break repair PARP1 may also play a role in nonho-mologous end-joining4 The primary investigation ofPARP inhibitors has been in potentiating radiation andchemotherapy effects the latter in the context of homolo-gous repair deficient tumors For radiation the primarymechanism of action is inducing damage to nucleotidesleading to single-strand and double-strand breaks ThusPARP inhibitors in combination with radiation have an ap-pealing mechanism to inhibit or delay DNA repair andlikely convert more single-strand breaks to double-strandbreaks4
While several PARP inhibitors are currently being evalu-ated in a variety of tumors including talazoparib and nira-parib veliparib and olaparib are among the most studiedand there are randomized trials exploring their use in
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
110
gliomas The US National Cancer Institute (NCI)ndashfundedAlliance for Clinical Trials in Oncology (Alliance) A071102is a randomized phase IIIII trial evaluating the use ofveliparib in combination with TMZ in the adjuvant settingin patients with GBM tumors exhibiting hypermethylationof the O6 methylguanine DNA methyltransferase (MGMT)gene promoter Preclinical data supporting this trial sug-gested that only patients with MGMT methylated tumorswould benefit from the combination a group of patientsfor whom TMZ concurrent with radiation might be mostbeneficial5 A phase I trial performed by the NCI-fundedAmerican Brain Tumor Consortium attempted to combineveliparib with radiation and TMZ but failed to identify asuitable recommended phase II dose due to significanthemotoxicity6 Thus attempts to combine radiation withveliparib have focused on patients least likely to benefitfrom TMZ namely with MGMT unmethylated tumors forwhom TMZ could be withheld The Australian VeliparibRT and TMZ trial in newly diagnosed unmethylatedMGMT glioblastoma (VERTU) is a single-arm study inwhich patients receive RT with veliparib followed by adju-vant TMZ and veliparib4
An ongoing novel approach to radiosensitize gliomasinvolves a combination with an agent that interferes withan essential metabolic process 2-Dexoyglucose (2-DG)is a nonmetabolized glucose analogue that acts as acompetitive inhibitor of glycolysis It is transported acrossthe bloodndashbrain barrier by the glucose transporter GLUT-1 and thus has good penetration into the CNSIntracellularly it is trapped and accumulates in cells simi-lar to the mechanism of 18-fluorodeoxyglucose 2-DG isphosphorylated by glycolytic enzymes and the
phosphorylated 2-DG (2-deoxyglucose-P) is trapped in-tracellularly Inhibition of hexokinase activity by 2-DGinterferes with ATP formation and results in tumor celldeath7 While it has positive attributes by selectively tar-geting metabolically active tumor cells 2-DG has alsobeen associated with Q-T prolongation The currentphase III trial in gliomas is assessing the toxicity and tol-erability of 2-DG with hypofractionated radiation of 5 Gyas a radiosensitizer7
Two novel radiosensitizers are being developed for thetreatment of brain metastases First RRx-001 is a smallmolecule initially designed by the aerospace industry Itworks in part as a radiosensitizer by increasing blood flowand thus oxygenation of tumors through nitric oxideRRx-001 which binds to hemoglobin accelerates theNO2 to NO conversion of deoxyhemoglobin It workslocally under hypoxic conditions and subsequentlythe radiosensitive effects through nitric oxide are invasodilation and inhibiting DNA repair enzymes8 Nitricoxide is relatively benign The higher levels of oxidativestress with H2O2 and superoxide in tumors in comparisonto normal tissues result in the preferential generation ofreactive peroxynitrite in the presence of higher nitric oxidelevels7 This accounts for the increased specificity anddecreased toxicity with RRx-001 The dose limiting toxic-ity in a phase I trial of 25 patients treated with eitherweekly or biweekly infusions was infusional pain relatedto the release of NO at the site of injection7 Outside ofpreclinical models 2 clinical reports examining wholebrain radiation therapy (WBRT) with RRx-001 reported anintracranial response A patient with melanoma and 2hemorrhagic edematous lesions of 26 cm and 33 cm
Table 1 Clinical trials involving immunotherapy and radiation therapy1213
Clinical Trials Number Phase Disease Type Treatment Groups
NCT02667587 II Newly diagnosed GBMMGMT-methylated
Nivolumabthorn TMZthorn RT vs placebothornTMZ thorn RT
NCT02617589 III Newly diagnosed GBM Nivolumabthorn RT vs TMZthorn RTNCT02336165 II Newly diagnosed unmethylated
MGMT recurrent glioblastomaMEDI4736thorn standard RT vs MEDI4736 thorn
bevacizumabNCT02530502 III Newly diagnosed GBM RTthorn TMZthorn pembrolizumab TMZthorn
pembrolizumabNCT02313272 I Recurrent glioma Hypofractionated stereotactic radiationthorn
pembrolizumab thorn bevacizumabNCT02696993 III Brain metastases Nivolumabthorn SRS nivolumabthornWBRT
nivolumabthorn ipilimumab thorn SRS nivolu-mabthorn ipilimumab thornWBRT
NCT02115139 II Melanoma brain metastases Ipilimumab thornWBRTNCT02097732 II Melanoma brain metastases Ipilimumab SRS ipilimumab vs SRS
ipilimumabNCT01703507 I Melanoma brain metastases Ipilimumab thornWBRT vs ipilimumab thorn SRSNCT02107755 II Melanoma brain metastases Ipilimumab thorn SRSNCT02858869 pilot Melanoma and NSCLC Pembrolizumabthorn SRSNCT01950195 I Melanoma brain metastases Ipilimumab thorn SRSNCT02662725 II Melanoma brain metastases Ipilimumab thorn SRS
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
111
after a single intravenous dose of RRx-001 of 5 mgm2 4days before WBRT resulted in symptomatic improvementwithin 48 hours By 4 months after radiation there was areduction in size in the largest dimension down to 10 cmand 23 cm of the respective lesions A second report of amelanoma patient with at least 18 lesions after receivingRRx-001 of 5 mgm2 4 days before WBRT as well astwice weekly doses during the 2 weeks of radiation alsoshowed response The patient at 4 months had disap-pearance of 13 of 18 lesions with shrinkage of theremaining 5 lesions8 Presently BRAINSTORM is a phaseIII dose escalation trial of RRx-001 designed to be ad-ministered twice weekly for 2 weeks with WBRT (30 Gy in10 fractions) with the option for weekly maintenance8
Veliparib has also been evaluated in the setting of brainmetastases It was tested in a global randomized con-trolled trial with WBRT Veliparib is orally bioavailable andcrosses the bloodndashbrain barrier It was first examined in amultihistology phase I trial in patients with nonndashsmall celllung cancer (NSCLC) breast cancer melanoma and re-nal and colorectal cancers among others The study of81 patients tested dose tolerance of veliparib from 10 to300 mg orally twice a day with WBRT to 30 Gy in 10 frac-tions or 375 Gy in 15 fractions9 The phase I trial dose es-calation portion did not reach the predefined criteria forthe maximum tolerated dose but there was amplificationof the adverse effects of nausea and vomiting among thehighest dose cohort of 300 mg bid9 The adverse eventprofile at 200 mg bid was similar to that of WBRT aloneDoses of veliparib from 20 to 200 mg bid demonstratesimilar antitumor activity and other studies in preclinicalmodels found that 50 mg daily demonstrated significantreduction in poly(ADP-ribose) in peripheral blood mono-nuclear cells and tumor tissue while also effectivelycrossing the bloodndashbrain barrier Thus the subsequentphase II trial examined 50 mg with WBRT9 In order to as-sess a more homogeneous cohort the phase III globalrandomized trial studied only NSCLC at the 2 doses of50 mg and 200 mg twice daily versus placebo twice a daywith WBRT10 The primary endpoint was overall survivalIn 307 patients in a 111 randomization of 50 mg bid200 mg bid or placebo twice daily the study found nosignificant differences in overall survival among the differ-ent groups10 The majority of patients across the treat-ment groups had a graded prognostic assessment (GPA)score of25 and a Karnofsky performance status ofgt80 The median overall survival was 185 days forpatients receiving placebo and 209 days for those receiv-ing veliparib without any statistically significant differ-ence These results were similar to the disease-specificestimate of median survival for the disease-specific GPAof NSCLC patients with brain metastases10
Several other radiosensitizers have failed to improve overradiation alone in a number of trials These have includedtrials with WBRT including motexafin gadolinium efap-roxyn bortozemib thalidomide teniposide topotecanpaclitaxel and cisplatin7 Of note other PARP inhibitorsalso being assessed include talazoparib and niraparib4
which may yield positive results The use of valproic acid(VPA) as a histone deacetylase inhibitor has also beenconsidered to have radiosensitizing potential in additionto its anti-epileptic drug properties11 While studies havereported that patients with GBM receiving an anti-epilep-tic agent may have higher overall survival than those re-ceiving standard chemoradiation therapy alone thebenefit remains controversial Retrospective analysissuggested that patients taking VPA specifically had bettersurvival in comparison to other anti-epileptic drugs Alsoa recent prospective phase II trial was performed in 37patients with GBM receiving VPA 25 mgkg concurrentlywith TMZ chemoradiation and reported a median survivalof 296 months While controversial further data andinvestigation are needed into this and other agents thatmay potentiate RT
Immunotherapy and radiationImmune checkpoint inhibitors lead to activation of T cellswhich may traffic across the bloodndashbrain barrier to inter-act with tumor Primary brain tumors may evade the im-mune system through upregulation of immunecheckpoints and possible immunosuppression12
Monoclonal antibodies promote immune-mediated anti-tumor activity by inhibiting the immune functionndashmediated cytotoxic T-lymphocyte associated protein 4(CTLA-4) and programmed cell death protein 1 (PD-1)receptors PD protein ligand (PD-L1) is upregulated inGBM through oncogenic signaling possibly throughphosphatase and tensin homolog loss and interleukin-10signaling1314 RT has also been shown to enhance thefunction of cytotoxic T lymphocytes RT may induce aninfiltration of cytotoxic T lymphocytes and enhance theirfunction It may also induce antindashCTLA-4 agents inhibitingT-cell function and increasing the CD8thorn T cellregulatoryT cell ratio in cases of melanoma15 Thus PD-1 and PD-L1 blockers may have a further role in CNS managementwith the use of radiation
In preclinical models radiation has been examined withimmunotherapy that included among other mechanismsvaccination PD-1 blockade and CTLA-4 blockade Inmice radiation plus a vaccination of irradiated gliomacells was associated with increased survival of 40 to80 compared with 0 to 10 for other groups stud-ied16 A benefit of PD-1 blockade with stereotactic radio-surgery (SRS) specifically has also been shown in amouse model In comparison to mice treated with radia-tion antindashPD-1 therapy or a combination only those re-ceiving combination therapy had a higher percentagesurvival alive beyond 180 days after treatment17 Othermouse carcinoma models have identified response withanti-CTLA antibody and fractionated radiation therapy18
CD137 activation CTLA-4 blockade and focal radiationtherapy have been examined in an immunocompetent in-tracranial GBM model Mice treated with triple combina-tion therapy had 50 greater survival19 In other murine
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
112
models the use of antindashPD-1 and antindashCTLA-4 agentsshowed improved survival and increased tumor infiltratingleukocyte populations compared with single modalitywith concurrent radiation16 There are conflicting data re-garding timing or sequencing of therapy with some ani-mal models showing no difference in tumor response inrelation to timing of RT and delivery of immunotherapy18
For instance in one animal model CTLA-4 blockade de-livered simultaneously with radiation or delivered a coupleof days after showed no difference in survival among themice19
Increased PD-1 expression in circulating monocytes hasbeen identified as a biomarker for tumor-induced immu-nosuppression and may serve as a prognostic factor forpotentially worse survival outcomes in clinic13 In onestudy GBM patients with lower PD-L1 expression hadhigher median overall survival than those with higher PD-L1 expression suggesting that lower expression may beassociated with less immunosuppression and more im-mune activity against the tumor glioma20 RT with immunecheckpoint blockade is being investigated to assess if theaddition of PD-1 and PD-L1 inhibitors may improve theoutcomes or toxicity profile of standard therapy For in-stance a multi-institutional trial opened as a phase III willevaluate outcomes in GBM receiving radiation and pem-brolizumab with TMZ (NCT02530502) Next durvalumabor MEDI4736 a PD-L1 inhibitor is being examined forunmethylated MGMT GBMs with standard radiotherapy(NCT02336165)12 The impact of checkpoint inhibitorsduring adjuvant treatment of GBM is currently beingevaluated in the NCI-funded NRG-BN002 trial(NCT02311920) which will evaluate the antindashCTLA-4antibody ipilimumab alone or in combination with theantindashPD-1 antibody nivolumab for patients with newlydiagnosed GBM
Brain metastases have clonal populations of cells differ-ent from the rest of the brain and a unique microenviron-ment that may influence immunotherapy There may bemore immune infiltrates in metastases than in primarybrain tumors21 PD-L1 expression in brain metastasesvaries by histology In a series evaluating PD-L1 expres-sion in various tumors including melanoma NSCLCbreast renal colorectal and small cell less than 10showed significant expression22 There was greatest ex-pression among NSCLC and melanoma with a correla-tion between PD-L1 expression and tumor infiltratinglymphocytes22 Institutional series have examined thecombination of radiation and immune checkpoint block-ade In another study specific to melanoma brain metas-tases PD-L1 expression was found in over 50 of thecases and among those cases over 40 expressedPD-L1 in more than 5 of tumor cells23 The largest bodyof data for use of PD-L1 with radiation is for melanomaand NSCLC
Ipilimumab is a human monoclonal antibody that blocksCTLA-4 and allows for T-cell activation and proliferationto enhance the immune response to cancer In a
retrospective review of 70 patients with brain metastasestreated with SRS or WBRT the 33 patients receiving im-munotherapy had a median survival of 183 months incomparison to the 37 patients who did not receive ipili-mumab with a median survival of 53 months While therewere limited data among the cohort to evaluate sequenc-ing of therapy among 10 evaluable patients 40 whoreceived ipilimumab prior to RT had a partial response incomparison to only 10 among the cohort of 22 evalu-able patients who did not receive ipilimumab therapy atall with radiation24 Another retrospective institutionalstudy of 77 patients in which 37 received ipilimumabfound that patients treated with SRS and ipilimumab hada median survival of 213 months versus 49 months forthose not receiving ipilimumab Most interestingly theyidentified that the correlation remained significant evenafter adjusting for additional factors such as performancestatus Secondly there was not an increased need for useof salvage WBRT25
The sequencing of radiotherapy and immune checkpointinhibitors is of interest In a study of patients with brainmetastases the one-year survival for patients receivingSRS before ipilimumab was greater at 65 in contrast to56 for those receiving it concurrently and 40 for thosereceiving it after SRS26 Similarly another study of 75patients with 566 brain metastases showed greater tu-mor lesion response at 6 months from SRS for patientsreceiving ipilimumab nivolumab or pembrolizumabwithin 4 weeks of their SRS27 Those receiving concurrenttherapy had by 6 months a decrease of 949 in compar-ison to 662 for those not receiving checkpoint inhibi-tors within 4 weeks Prospective clinical trials areinvestigating different combinations of RT with immunecheckpoint blockers in this setting For instance new tri-als are currently evaluating intracranial tumor control at 6months and the timing of immune therapy or immunecheckpoint inhibitors in relation to SRS28
Vaccines are also being developed for primary braintumors showing some evidence for their use Vaccinesdeveloped from dendritic cells and tumor lysate with tu-mor antigens such as the epidermal growth factor recep-tor variant III vaccine have shown promise29 Forinstance in a placebo controlled phase II trial of ICT-107a vaccine composed on autologous dendritic cells andtumor antigens progression-free survival was increasedby 2 months for those receiving the vaccine30 Radiationmay assist in serving as a primer for the immunogeniceffects by facilitating tumor antigen uptake by dendriticcells and cross presentation on major histocompatibilitycomplex I Thus RT may assist in the tumor-specific cy-totoxic T lymphocytes associated with the immunemechanism
In conclusion although there may be challenges to com-bining and sequencing brain tumors radiosensitizersand immunotherapy the opportunities and potential fornovel applications are promising For brain tumors brainmetastases are typically underrepresented in trials
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
113
despite being among the most common intracraniallesions Despite their large population patients with brainmetastases are often excluded from clinical trials withnovel agents due to concerns regarding confounding out-comes and tolerability12 Primary gliomas also offer anovel frontier for the use of immunotherapy to standardadjuvant chemotherapy and radiation particularly forpatients with GBM less likely to respond to TMZ such aswith unmethylated MGMT As studies work to define therole of RT and radiosensitizers and immunotherapy fur-ther analysis is needed to assess the timing of RT andthese treatments
References
1 Stupp R Hegi ME Mason WP et al Effects of radiotherapy withconcomitant and adjuvant temozolomide versus radiotherapy aloneon survival in glioblastoma in a randomised phase III study 5-yearanalysis of the EORTC-NCIC trial Lancet Oncol 2009 10459ndash466
2 Lawrence TS Blackstock AW McGinn C The mechanism of actionof radiosensitization of conventional chemotherapeutic agentsSemin Radiat Oncol 2003 1313ndash21
3 Lesueur P Chevalier F Austry JB et al Poly-(ADP-ribose)-polymer-ase inhibitors as radiosensitizers a systematic review of pre-clinicaland clinical human studies Oncotarget 2017 8(40)69105ndash69124
4 Lester A Rapkins R Nixdorf S Khasraw M McDonald KCombining PARP inhibitors with radiation therapy for the treatmentof glioblastoma is PTEN predictive of response Clin Transl Oncol2017 19273ndash278
5 Gupta SK Kizilbash SH Carlson BL et al Delineation of MGMT hyper-methylation as a biomarker for veliparib-mediated temozolomide-sensi-tizing therapy of glioblastoma J Natl Cancer Inst 2016 108
6 Kleinberg LR Blakeley J Mikkelsen T et al An American BrainTumor Consortium (ABTC) phase 1 trial of veliparib (ABT-888)temozolomide (TMZ) and concurrent radiation therapy (RT) fornewly diagnosed glioblastoma multiforme (GBM) need for modifica-tion to approach for combining these therapies InternationalJ Radiat Oncol Biol Phys 2012 84S7ndashS8
7 Oronsky BT A Review of two promising radiosensitizers in brainmetastases Rrx-001 and 2-deoxyglucose In NC Oronsky edJ Cancer Sci Ther 2015 pp 137ndash141
8 Kim MM Parmar H Cao Y et al Concurrent whole brain radiother-apy and RRx-001 for melanoma brain metastases Neuro Onc2016 18455ndash456
9 Mehta MP Wang D Wang F et al Veliparib in combination withwhole brain radiation therapy in patients with brain metastasesresults of a phase 1 study J Neurooncol 2015 122409ndash417
10 Chabot P Hsia TC Ryu JS et al Veliparib in combination withwhole-brain radiation therapy for patients with brain metastasesfrom non-small cell lung cancer results of a randomized globalplacebo-controlled study J Neurooncol 2017 131105ndash115
11 Ochiai S Nomoto Y Yamashita Y et al Roles of valproic acid inimproving radiation therapy for glioblastoma a review of literaturefocusing on clinical evidence Asian Pac J Cancer Prev 201617463ndash466
12 Tan AC Heimberger AB Menzies AM Pavlakis N Khasraw MImmune checkpoint inhibitors for brain metastases Curr Oncol Rep2017 1938
13 DrsquoSouza NM Fang P Logan J Yang J Jiang W Li JCombining radiation therapy with immune checkpoint blockade
for central nervous system malignancies Frontiers Oncol 20166212
14 Parsa AT Waldron JS Panner A et al Loss of tumor suppressorPTEN function increases B7-H1 expression and immunoresistancein glioma Nat Med 2007 1384ndash88
15 Binder DC Davis AA Wainwright DA Immunotherapy for cancer inthe central nervous system current and future directionsOncoimmunology 2016 5e1082027
16 Newcomb EW Demaria S Lukyanov Y et al The combination ofionizing radiation and peripheral vaccination produces long-termsurvival of mice bearing established invasive GL261 gliomas ClinCancer Res 2006 124730ndash4737
17 Zeng J See AP Phallen J et al Anti-PD-1 blockade and stereotac-tic radiation produce long-term survival in mice with intracranial glio-mas Int J Radiat Oncol Biol Phys 2013 86343ndash349
18 Chow KK Hara W Lim M Li G Combining immunotherapy withradiation for the treatment of glioblastoma J Neurooncol2015123459ndash464
19 Belcaid Z Phallen JA Zeng J et al Focal radiation therapy com-bined with 4-1BB activation and CTLA-4 blockade yields long-termsurvival and a protective antigen-specific memory response in amurine glioma model PLoS One 2014 9e101764
20 Topalian SL Hodi FS Brahmer JR et al Safety activity and im-mune correlates of anti-PD-1 antibody in cancer N Engl J Med2012 3662443ndash2454
21 Bienkowski M Preusser M Prognostic role of tumour-infiltrating in-flammatory cells in brain tumours literature review Curr OpinNeurol 2015 28647ndash658
22 Harter PN Bernatz S Scholz A et al Distribution and prognostic rel-evance of tumor-infiltrating lymphocytes (TILs) and PD-1PD-L1 im-mune checkpoints in human brain metastases Oncotarget 2015640836ndash40849
23 Berghoff AS Ricken G Widhalm G et al Tumour-infiltrating lym-phocytes and expression of programmed death ligand 1 (PD-L1) inmelanoma brain metastases Histopathology 2015 66289ndash299
24 Silk AW Bassetti MF West BT Tsien CI Lao CD Ipilimumab and ra-diation therapy for melanoma brain metastases Cancer Med 20132899ndash906
25 Knisely JP Yu JB Flanigan J Sznol M Kluger HM Chiang VLRadiosurgery for melanoma brain metastases in the ipilimumab eraand the possibility of longer survival J Neurosurg 2012117227ndash233
26 Kiess AP Wolchok JD Barker CA et al Stereotactic radiosurgeryfor melanoma brain metastases in patients receiving ipilimumabsafety profile and efficacy of combined treatment Int J Radiat OncolBiol Phys 2015 92368ndash375
27 Qian JM Yu JB Kluger HM Chiang VL Timing and type of immunecheckpoint therapy affect the early radiographic response of mela-noma brain metastases to stereotactic radiosurgery Cancer 20161223051ndash3058
28 Silk AW Cao Y Gomez-Hassan D et al A randomized phase IIstudy of ipilimumab induction in patients with melanoma brain me-tastases receiving stereotactic radiosurgery J Clin Oncol 2015 33TPS9079ndashTPS9079
29 Neagu MR Reardon DA An Update on the role of immunotherapyand vaccine strategies for primary brain tumors Curr TreatOptions Oncol 2015 1654
30 Wen PY Reardon DA Phuphanich S et al A randomized double-blind placebo-controlled phase 2 trial of dendritic cell (DC) vaccina-tion with ICT-107 in newly diagnosed glioblastoma (GBM) patientsJ Clin Oncol 2014 322005ndash2005
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
114
British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

Editorial
First of all on behalf of EANO I wouldlike to congratulate the SNO leader-ship for an amazing conference inSan Francisco In addition to theinsights from invited lectures and ed-ucational activities in part supportedby the US Moonshot program theEANO highlight for sure was theaward-winning clinical abstract onthe CeTeG-trial in which UlrichHerrlinger from Bonn presented theNOA-09 trial demonstrating an over-all survival benefit in a small but con-trolled randomized study for thecombination of cyclic CCNU andtemozolomide in patients withnewly diagnosed glioblastoma har-boring a hypermethylated MGMTpromoter
In this issue of the magazine we willhave opinion papers on the value ofbrain tumor epigenetics as well as onthe role of radiation therapy in com-bined modality therapies with a focusnot only on the classical approachesbut also radiosensitization and immu-notherapies In addition to the largebody of literature on precision medi-cine approaches three colleaguesfrom the US share their vision on thepresent but more important also onthe potential future use of next-gener-ation sequencing and other high-throughput technologies in neuro-oncology We have the periodicupdates on Nurses Activities featuredarticles from Neuro Oncology andNeuro Oncology Practice as well as a
view from the EANO youngsters onmentoring
Two of our national organizations(the British and the Indiansocieties) present their views on theWFNOS and the national IndianNeuro Oncology conferencerespectively
On behalf of my colleagues from theEANO board I would like to wish allreaders a successful completion of2017 and a great start into the year2018 with one highlight our EANOconference in Stockholm in Octoberalready determined
W Wick
President EANO
99
Volume 2 Issue 3 Editorial
Editorial
This year from November 15 to 19SNO held its 22nd annual meeting inSan Francisco Each meeting has atheme and this yearrsquos overall themefocused on the ldquoCancer Moonshotrdquoprogram that was proposed byformer president Obama in 2016 andwas initially led by former vice-president Biden whose son perishedfrom a GBM The meeting wasattended by over 2500 participantsfrom all over the world with a recordnumber of submitted abstracts (over1800) The meeting was preceded bytwo successful former meetings theNeuro-oncology Review Course andthe SNOSCIDOT course on intersti-tial CNS delivery both held on Nov15 Our Education Day was held onNov 16 it focused on the subject ofGBM resistance and was organizedby Sue Bell Robert Cavaliere KhalidShah and Albert Kim The mainmeeting was organized by ManishAghi Vinay Puduvalli and FrankFurnari and was highlighted by key-note talks by Jennifer Doudna on
CrispRCas9 and Carlo Croce onmicroRNAs There were multipleSNO educational events from a sun-rise session to lunchtime tutorialsand dinner events such as very wellattended poster and e-talk sessionsThere were also multiple events dedi-cated to stress relief as well includ-ing opening receptions gala dinnersand burnout relief events We are
looking forward to the 23rd meetingin New Orleans which will be led byour new officers (President PatrickWen Vice-President Gelared Zadehand SecretaryTreasurer TracyBatchelor)
EA (Nino) Chiocca
President SNO
100
Volume 2 Issue 3 Editorial
Brain TumorEpigeneticsFrom Researchto ClinicalPractice
Silvia MarinoBlizard Institute Barts and The London School ofMedicine and Dentistry Queen Mary University ofLondon 4 Newark Street E12AT London UK
101
IntroductionEpigenetics is defined as the study of heritable changesin gene expression that are not caused by alterations inDNA sequences1 The phenotypic difference between acaterpillar and a butterfly for example is due to epige-netic regulation of gene expression in the same animalwith the same DNA I particularly like this example to ex-plain the meaning of the term epigenetics as it impres-sively demonstrates how powerful these mechanisms arein controlling phenotypic changes Epigenetic changesare reversible and include the key processes of DNAmethylation histone modifications and noncoding RNA-associated gene silencing (recently reviewed2) known toplay an essential role during the embryonic and postnataldevelopment of an organism and in tissue homeostasis2
Disruptions of epigenetic processes can induce changesin gene function which together with genetic changescan lead to the neoplastic transformation of a normal cell(recently reviewed)3
Recent technological advances have significantly con-tributed to the tremendous progress in understandinghow these epigenetic modifications are regulated in nor-mal cells and deregulated in cancer cells For examplethis knowledge has enabled the translation into better di-agnostic algorithms for tumor classification prognostica-tion and risk assessment Importantly we are nowentering a time when novel therapies targeting thesederegulated epigenetic mechanisms are being devel-oped with some of them showing very promising effectsin preclinical models
It is beyond the scope of this article to comprehensivelyreview mechanisms of epigenetic regulation of gene ex-pression and their deregulation in brain tumors excellentrecent reviews are available to the readers on thesesubjects2ndash5 Here I will discuss a few examples of recentepigenetic discoveries which have informed the develop-ment of novel diagnostic and prognostic tools or led tosuccessful preclinical testing of new epigenetic drugs inexperimental models
Epigenetic Profiles inthe MolecularClassification of BrainTumorsGlioma One of the first examples of an epigenetic changeinforming the design of an assay for diagnostic screeningto corroborate a therapeutic decision is the assessmentof methylation of the MGMT promoter in malignantgliomas6 MGMT (O6-methylguanine DNA methyltransfer-ase) is a key enzyme in the DNA repair network which
removes the mutagenic and cytotoxic adducts from O6
guanine in DNA the preferred point of attack of alkylatingchemotherapeutic agents (ie BCNU temozolomide etc)Hypermethylation of cytosine-phosphate-guanine (CpG)islands located in the promoter region of MGMT is pri-marily responsible for the loss of MGMT function in manytumor types hence leading to an increased sensitivity tothe killing effects of alkylating drugs used in chemo-therapy6 This test is widely used in clinical practice topredict response to temozolomide the alkylating drug ofchoice in high-grade gliomas although it should bestressed that there is still no consensus as to which testmethod to use which CpG sites to assess and what themethylation cutoff should be
Ependymoma Until very recently these tumors havebeen subclassified and graded on the basis of histologi-cal features into low and high grade In 2015 a molecularclassification based on DNA methylation profiling hasbeen proposed which defines 9 molecular subgroups 3for each anatomical location of these tumors (supratento-rial posterior fossa and spinal cord)7 In the supratento-rial location ependymomas with the fusion geneC11ORF95RELA (ST-EPN-RELA) have a poor prognosisand in the posterior fossa it is the ependymoma groupEPN-A that is characterized by a poor prognosis7 Allother ependymomas show a comparatively goodprognosis7 Although not yet included in the World HealthOrganization (WHO) 2016 classification a recent consen-sus paper has recommended that this classification beused for enrollment in prospective clinical trials8 and it isexpected to contribute to informing decisions onmolecular-based treatments as they become available
Medulloblastoma (MB) International consensusrecognizes 4 medulloblastoma molecular subgroupsWNT (MBWNT) SHH (MBSHH) Group 3 (MBGrp3) andGroup 4 (MBGrp4) each defined by their characteristicDNA methylation and genome-wide transcriptomicprofiles9 Recently the heterogeneity within these sub-groups has been reduced by 2 independent studieswhich have defined additional subtypes Schwalbe andcolleagues10 have suggested to split MBSHH into 2 age-dependent subtypes corresponding to ldquoinfantrdquo (lt43 y)and ldquochildhoodrdquo patients (43 y) and MBGrp3 andMBGrp4 into further high-risk and low-risk subtypes whilethe MBWNT group remains unchanged10 Interestingly thelow-risk subtypes were defined primarily by hypermethy-lation in comparison to normal cerebellum whereas thehigh-risk subtypes were defined by relativehypomethylation10 Cavalli and coauthors11 used integra-tive clustering of DNA methylation and gene expressiondatasets from 763 patients to split the original 4 sub-groups into 12 subtypes MBSHH is split into 4 subtypes(abc d) MBWNT into 2 subtypes (ab) MBGrp3 andMBGrp4into 3 subtypes each (abc)11 The subtypes iden-tified in these 2 studies overlap considerably and themain differences seem to be related to the inclusion ofadult MB patients in the Cavalli study Importantly MBsubgroups and their subtypes identified by their
Brain Tumor Epigenetics From Research to Clinical Practice Volume 2 Issue 3
102
epigenetic and related transcriptional profiles1011 havedistinct genetic and clinicopathological features1011 andtheir implementation for patient stratification for betterprognostication and enrollment into subgroupsubtype-directed therapies in the context of clinical trials will be astep change in the treatment of MB patients
All CNS tumors A classification tool for brain tumorsbased on genome-wide DNA methylation patterns and arandom forest-based machine learning approach hasbeen developed and extensively tested by the GermanCancer Research Center (wwwmolecularneuropathologyorg) This resource is available online and has provento be a valuable tool to improve brain tumor diagnosticsThis approach has facilitated the identification of com-mon druggable molecular pathway alterations across var-ious histological tumor entities thus allowing patients toenter the most appropriate clinical trials and in somecases be offered molecularly matched therapies As anexample DNA methylation profiles allow precise identifi-cation of cases with mitogen-activated protein kinase(MAPK) activation which is a feature of tumors withBRAF V600E mutation1213 which can span various tradi-tional histological entities such as pilocytic astrocytomaspleomorphic xanthoastrocytomas ganglioglioma andsubependymal giant cell astrocytomas to predict re-sponse to specific inhibitors interrupting the BRAFMEKcomponent of the MAP kinase pathway14
Novel TherapeuticApproaches TargetingEpigeneticDeregulationDiffuse intrinsic pontine glioma (DIPG) is a highlyaggressive pediatric tumor located in the brainstem andcharacterized by a rapid and diffusely infiltrative patternof growth These tumors cannot be treated surgicallybecause of their location and infiltrative nature15
Radiation therapy is the standard treatment although itprovides only temporary symptom relief with no overallsurvival benefits and conventional chemotherapy drugsare ineffective15
Mutations in histone H3 variants occur in more than 80of DIPG and result in a lysine-to-methionine substitution(H3K27M)16 17 H3K27M has been shown to inhibitpolycomb repressive complex 2 (PRC2) by binding to itscatalytic subunit EZH2 and reducing the methylation ofH3 at lysine 27 (H3K27me) at selected target loci18 Theresidual PRC2 activity is required to maintain DIPGproliferative potential by repressing neuronaldifferentiation in patient-derived cell lines and in agenetically engineered mouse model1920 Importantlysmall-molecule EZH2 inhibitors abolish tumor cell growth
in these models raising the possibility that inhibitionof EZH2 could be a novel therapeutic strategy for thesetumors19
An independent study showed that H3K27M associateswith increased H3K27 acetylation (H3K27ac) and that themajority of the heterotypic H3K27M-K27ac nucleosomesco-localize with bromodomain proteins at the loci of ac-tively transcribed genes20 The authors have shown thatblocking the recruitment of bromodomain proteins by het-erotypic H3K27M-K27ac nucleosomes in DIPG with bro-modomain and extraterminal domain family inhibitorsefficiently inhibited tumor progression thus identifying thisclass of compounds as potential therapeutics in DIPG20
These important advances in understanding the underly-ing biology of DIPG have led to the identification of novelepigenetic therapeutic approaches which are very effec-tive at the preclinical level and if confirmed in transla-tional studies could change the way we treat thesetumors in the near future
Conclusion and outlookThese are exciting and challenging times for theneuro-oncology community Exciting because there isgrowing expectation in the field that new discoveriessuch as those discussed in this article can soon translateinto new and more effective therapeutic approachesChallenging because it is clear that new skill sets are re-quired to effectively apply them to benefit patients
The clinical training in many neuro-oncology specialtieswill have to take into account the additional knowledgeand skills needed in the field and offer education incomplementary disciplines such as next-generationsequencing technologies integrated with interpretativedata analysis as well as molecular biology for the designof biologically informed assays and tools The require-ment for these new highly specialized skills also needs tobe reflected in the composition of the clinical teamswhere bioinformatics expertise will play an increasinglyimportant role for the integration of multimodal data inpatient care
References
1 Waddington CH Canalization of development and the inheritance ofacquired characters Nature 1942150563ndash565
2 Allis CD Jenuwein T The molecular hallmarks of epigenetic controlNat Rev Genet 201617487ndash500
3 Flavahan WA Gaskell E Bernstein BE Epigenetic plasticity and thehallmarks of cancer Science (New York NY 2017357
4 Edwards JR Yarychkivska O Boulard M Bestor TH DNA methyla-tion and DNA methyltransferases Epigenetics amp chromatin20171023
5 Filbin MG Suva ML Gliomas genomics and epigenomics arriving atthe start and knowing it for the first time Annual Rev Pathol201611497ndash521
6 Hegi ME et al MGMT gene silencing and benefit from temozolomidein glioblastoma N Engl J Med 2005352997ndash1003
Volume 2 Issue 3 Brain Tumor Epigenetics From Research to Clinical Practice
103
7 Pajtler KW et al Molecular Classification of Ependymal Tumorsacross All CNS Compartments Histopathological Grades and AgeGroups Cancer Cell 201527728ndash743
8 Pajtler KW et al The current consensus on the clinical managementof intracranial ependymoma and its distinct molecular variants ActaNeuropathol 20171335ndash12
9 Taylor MD et al Molecular subgroups of medulloblastoma the cur-rent consensus Acta Neuropathol 2012123465ndash472
10 Schwalbe EC et al Novel molecular subgroups for clinical classifi-cation and outcome prediction in childhood medulloblastoma a co-hort study Lancet Oncol 201718958ndash971
11 Cavalli FMG et al Intertumoral Heterogeneity withinMedulloblastoma Subgroups Cancer Cell 201731737ndash754 e736
12 Schindler G et al Analysis of BRAF V600E mutation in 1320 nervoussystem tumors reveals high mutation frequencies in pleomorphicxanthoastrocytoma ganglioglioma and extra-cerebellar pilocytic as-trocytoma Acta Neuropathol 2011121397ndash405
13 Tanaka S et al Epithelioid glioblastoma arising from pleomorphicxanthoastrocytoma with the BRAF V600E mutation Brain TumorPathol 201431172ndash176
14 Banerjee A et al A phase I trial of the MEK inhibitor selumetinib(AZD6244) in pediatric patients with recurrent or refractory low-grade glioma a Pediatric Brain Tumor Consortium (PBTC) studyNeuro Oncol 2017191135ndash1144
15 Hargrave D Bartels U Bouffet E Diffuse brainstem glioma in chil-dren critical review of clinical trials Lancet Oncol 20067241ndash248
16 Schwartzentruber J et al Driver mutations in histone H33 and chro-matin remodelling genes in paediatric glioblastoma Nature2012482226ndash231
17 Wu G et al Somatic histone H3 alterations in pediatric diffuse in-trinsic pontine gliomas and non-brainstem glioblastomas Naturegenetics 201244251ndash253
18 Lewis PW et al Inhibition of PRC2 activity by a gain-of-function H3mutation found in pediatric glioblastoma Science (New York NY2013340857ndash861
19 Mohammad F et al EZH2 is a potential therapeutic target forH3K27M-mutant pediatric gliomas Nature Med 201723483ndash492
20 Piunti A et al Therapeutic targeting of polycomb and BET bromodo-main proteins in diffuse intrinsic pontine gliomas Nature Med201723493ndash500
Brain Tumor Epigenetics From Research to Clinical Practice Volume 2 Issue 3
104
The Value of SurgicalResection for MalignantGliomas in the ModernEra Beyond Extent ofResection
Stephen G Bowden MDSeunggu Jude Han MDDepartment of Neurological Surgery OregonHealth and Sciences University 3303 SW BondAve Center for Health and Healing CH8NPortland OR 97239 Telephone 503-494-4314Fax 503-346-6810 hanseohsuedu
105
Malignant gliomas are among the most difficult oncologi-cal entities to treat Despite aggressive treatment prog-nosis remains poor and recurrence and treatmentfailures seem inevitable The current standard-of-caretherapy includes maximal safe surgical resection fol-lowed by concurrent and adjuvant chemoradiotherapyHistorically surgical resection has conferred greater sur-vival benefit to these patients than adjuvant therapiespresumably through the cornerstone principle of cytore-duction However the extent of surgical resection is fre-quently limited by nearby eloquent tissue and risks to keyneurological functions In addition the value of such ag-gressive approaches has been questioned in light of thewidespread infiltration of glioma cells Meanwhile our un-derstanding of glioma biology continues to advance rap-idly fueled in large part by the acquisition of tumor tissueduring surgery Thus the exact role and value of surgeryparticularly in comparing the clinical benefits of maximalextent of resection (EOR) with the biomedical benefits oftissue provision has been a topic of great interest anddebate in both the neuro-oncological and neurosurgicalcommunities
EOR patient age tumor histology performance statusand molecular markers have been widely accepted assignificant predictors of patient outcomes in malignantglioma9 In the past 2 decades many large retrospectivecohort studies have demonstrated improvements in sur-vival with increasing EOR5917 Due to ethical considera-tions evidence from a randomized prospective studysupporting the clinical benefit of aggressive resectionsdoes not exist and likely never will Instead the closestthing to such evidence in malignant glioma comes fromthe randomized phase III trial comparing surgical resec-tions with or without the use of 5-aminolevulinic acid(5-ALA) The use of 5-ALA serving as a means to and aproxy for greater EOR resulted in extended overall sur-vival for patients with newly diagnosed glioblastoma19 Arecent meta-analysis of 41 117 unique patients by Brownet al adherent to the guidelines of PRISMA (PreferredReporting Items for Systematic Reviews and Meta-Analyses) also demonstrated a clear survival benefit forgross total resection over subtotal resection or biopsy atupfront surgery for glioblastoma1 The body of literatureas a whole clearly favored aggressive resections andthere seemed to be little disagreement for a strategytoward maximal resection when clinically feasibleHowever the challenge still remains when such strategiescome at the risk of neurological morbidity A recent reportby Rahman et al illustrates that the survival benefits fromaggressive resection are lost if the patient develops anew postoperative neurologic deficit as a result15
All the while our understanding of glioma genetics mo-lecular biology and mechanisms of resistance has con-tinued to deepen and evolve borne of thoughtful andsystematic studies using patient-acquired tumor sam-ples Molecular profiles and tumor genetics have proventhemselves to be the best predictors of clinical behaviorand now represent crucial components of the diagnostic
classification scheme of infiltrating gliomas12 With tumortissue at the molecular and genetic level being able to ro-bustly predict patient outcomes accurate tissue diagno-sis has become paramount in the management ofgliomas The role and value of open surgical resection to-ward this end have become clearer as concerns of sam-pling error with biopsy alone led to a number of studiesevaluating the ldquoaccuracyrdquo of stereotactic biopsy proce-dures Jackson et al reported a series of 81 patients whounderwent stereotactic biopsy followed by open surgicalresection The tissue diagnosis was concordant betweenbiopsy and open resection samples in only 51 ofpatients6 Other studies have also demonstrated diagnos-tic concordance between stereotactic biopsy and surgi-cal resection samples in only 57 to 79 ofcases131428 The major limitation of stereotactic biopsyfor infiltrating gliomas likely stems from the significantintratumoral heterogeneity and collectively these studieshighlight the value of open surgical resection in providinga more global representation and understanding of thetumor tissue
The value of extensive resection is perhaps even moreprofound when considering the therapeutic implicationsof such heterogeneity Multiple-site and serial-samplinganalyses have revealed a high degree of both spatial andtemporal heterogeneity within these tumors a conse-quence of serial evolutionary events during tumor growthand progression23 These studies have also led to theconcept of therapy-driven clonal selection and preferen-tial regrowth of resistant cell populations as a potentialmechanism of treatment failure Efforts to expand our un-derstanding of the tremendously complex network ofmutations and biological consequences of chronologicalhierarchy would be greatly facilitated by carefullyplanned thoughtful acquisition of tumor samples duringsurgery
Despite the recent paradigm shift in glioma diagnosticclassification little gains have been made in improvingthe overall prognosis for patients with malignant gliomassince the introduction of concurrent and adjuvant temo-zolomide in 200521 The strategies more recently tested inlarge randomized phase III trials by and large have yieldeddisappointing results while the reasons and mechanismsof treatment failures remain unclear Even so encourag-ing responses have occasionally been seen in varioussubsets of patients and studies exploring the presenceof potential biomarkers have generated intriguing andpromising results in these populations The developmentof the antindashvascular endothelial growth factor monoclonalantibody bevacizumab is one such example Two initialphase II trials showed prolonged progression-free sur-vival in recurrent glioblastoma relative to historical con-trols prompting the US Food and Drug Administration togrant accelerated approval to bevacizumab for recurrentglioblastoma in 2009825 However 2 large randomized tri-als evaluating the addition of bevacizumab to radiationand temozolomide in the newly diagnosed setting failedto show a benefit in overall survival24 and its utility in the
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
106
recurrent setting is now a topic of debate in light of sub-sequent phase III trial results However a post hoc analy-sis of patients enrolled in the AVAglio trial recentlydemonstrated that bevacizumab improved overall sur-vival for those with a proneural subtype tumor18 Just asO6-methylguanine-DNA-methyltransferase (MGMT) pro-moter methylation does for temozolomide the geneticprofile of the tumor could serve as a potential biomarkerof clinical response for bevacizumab as well and valida-tion studies are currently ongoing Such analyses al-though performed post hoc require targeted prospectivecollection of tumor tissue at initial surgery In addition ge-netic profiling of newly diagnosed malignant gliomas willneed to become routine if this approach is to be utilizedwidely Similarly cilengitide an inhibitor of aVb3 andaVb5 integrins with anti-angiogenic properties showedinitial promise in recurrent glioblastoma studies but failedto show any additional benefit in the newly diagnosedsetting20 A subsequent post hoc analysis of the phase IItrial revealed improved progression-free and overall sur-vival in patients with high aVb3 levels in the tumor cells26
However tumor tissues were not systematically collectedand less than half of the patientsrsquo tumor tissues wereavailable for analysis from the phase III trialUnfortunately this drug will most likely not undergo fur-ther development and one cannot help wonder if the out-come would have been different if the enrollment in thephase III trial had been enriched for or restricted to tumorswith high expression of the aVb3 integrin The only trueldquosuccess storyrdquo since the adaptation of radiation andtemozolomide has come from the novel approach of tu-mor treating fields (TTFields) a transcutaneous deliveryof low-intensity intermediate frequency alternating elec-tric fields The multicenter phase III trial EF-14 random-ized patients with supratentorial glioblastoma withoutevidence of tumor progression following standard che-moradiation to receive maintenance treatment withTTFields plus temozolomide or temozolomide alone22
The study was terminated early based on results of aplanned interim analysis demonstrating benefit inprogression-free survival overall survival a secondaryendpoint was also significantly enhanced at this timeDespite the trialrsquos success TTFields has not been univer-sally adopted by the neuro-oncology community andenthusiasm among clinicians and patients remains low27
Experts have raised concerns regarding the study designsuch as its open-label design lacking a sham-treatmentcontrol arm as well as the generalizability of the resultsbased on the unique randomization point occurring afterconcurrent chemoradiation16 Perhaps most significantlya lack of widely understood mechanism of action hasalso been raised as a factor with comparison to othertreatments the preclinical data for TTFields is relativelylacking particularly when applied in conjunction with che-moradiation27 Even during the early phase stages theuse of robust tissue-based analyses exploring the mech-anism of action such as dose response modeling andmultisite tissue biopsies may have mitigated some of
these concerns and led to wider acceptance by the com-munity Bevacizumab and cilengitide clearly benefitedfrom retrospective analyses of human tumor tissue toidentify susceptible treatment populations while the en-thusiasm for TTFields is perhaps in part tempered by thelack thereof Collectively the evolution of these treat-ments underscores the value of extensive targeted tissuesampling in furthering development of new adjunctivetherapies
Open surgical resection of tumors with such targeted tis-sue acquisition for analysis will continue to play a key rolein prospective clinical trial designs Comparison ofpretreatment and posttreatment tissue profiles representsa valuable line of investigation by delving into mecha-nisms of therapeutic action as well as mechanisms oftreatment failures1011 It also provides an opportunity toinvestigate a number of key fundamental steps along anagentrsquos path to clinical success such as does the agentsuccessfully traffic to the tumor if so how much anddoes the agent then actually have its hypothesizedeffects at the biochemical or cellular level Thusearly-phase trials can and should include posttreatmentmolecular endpoints when possible in addition to safetyendpoints Immunotherapy and immune checkpoint inhi-bition represent exciting novel therapeutic approachesfor neuro-oncology particularly based on their success inmetastatic cancers Large phase III trials studying block-ade of the programmed cell death protein (PD)1PDligand 1 axis with monoclonal antibodies for newlydiagnosed and recurrent glioblastoma are under way butinitial reports have been concerning for negative resultsAs in the development of many previous novel agentstissue-based mechanism studies have been largely lack-ing in the preclinical phases However an Alliance-supported trial currently enrolling focuses on a biomarkeras a primary endpoint patients with recurrent glioblas-toma indicated for surgery are randomized to receivepembrolizumab a PD1 inhibitor either before or aftersurgery (NCT02852655) The resected tumor tissue willthen be analyzed for the profile of tumor-infiltratingT cells and comparison will be made between the 2groups This study represents a tremendously valuableopportunity to explore the impact and the potential chal-lenges of checkpoint inhibition for malignant gliomas inthe clinical setting and should the large phase III trialsend up negative this pilot study will be very informative
Advances in imaging biomarkers and molecular charac-terization of gliomas in conjunction with new targetedtherapies will continue to improve and transform themanagement of these tumors Multimodality imaging cannow more accurately reflect ongoing biological processeswithin these tumors such as the presence of oncogenicmutations or cells undergoing malignant transformationNovel biomarkers such as circulating tumor DNA showpromise in detecting early recurrence or monitoring treat-ment response3724 Lastly the new classification schemerevolving around molecular characterization will provide a
Volume 2 Issue 3 The Value of Surgical Resection for Malignant Gliomas in the Modern Era
107
necessary corollary to these novel diagnostic tools Itremains indisputable however that clinical validation ofthese novel diagnostic tools will also require systematiccorrelation with human tumor tissue obtained throughsurgery These samples ideally gathered prospectivelywill provide a pivot upon which we can expand our under-standing of the complex network of oncological pro-cesses driving these tumors
Malignant gliomas are incredibly challenging disease en-tities in many ways due to the inter- and intratumoral het-erogeneity that is a hallmark of them Experience to datehints that future successes in malignant gliomas rest inneuro-oncology entering the era of precision medicinewhere validated biomarkers and targeted personalizedtherapies are seamlessly integrated into the managementparadigm Accordingly systems supporting surgical re-section and patient-specific tumor tissue analysis mustbe built and organized to guide the decision making fortherapy As our overall approach to the management ofmalignant gliomas evolves so should the framework ofsurgical management The clinical benefits of maximalsafe resection are well founded and well reportedHowever the oncological neurosurgeon must now lookbeyond maximal cytoreduction itself and recognize thevalue of thoughtful acquisition and analysis of tumor tis-sue Modern neurosurgeons must consider themselvessurgical neuro-oncologists and engagement and partici-pation of surgeons into clinical trials particularly early-phase trials should be encouraged and valued In turnwe should provide our surgical trainees with the trainingand tools in neuro-oncology to help them participate andcontribute in multidisciplinary collaborative efforts aimingto advance the understanding of brain tumor biology andultimately improve the outlook of our patients
References
1 Lacroix M Abi-Said D Fourney DR Gokaslan ZL et al A multivariateanalysis of 416 patients with glioblastoma multiforme prognosisextent of resection and survival J Neurosurg 2001 95190ndash198
2 Hervey-Jumper SL Berger MS Maximizing safe resection of low-and high-grade glioma J Neurooncol 2016 130269ndash282
3 Sanai N Polley MY McDermott MW Parsa AT Berger MS An ex-tent of resection threshold for newly diagnosed glioblastomas JNeurosurg 2011 1153ndash8
4 Stummer W Pichlmeier U Meinel T et al Fluorescence-guided sur-gery with 5-aminolevulinic acid for resection of malignant glioma arandomised controlled multicentre phase III trial Lancet Oncol2006 7392ndash401
5 Brown TJ Brennan MC Li M et al Association of the extent ofresection with survival in glioblastoma a systematic review andmeta-analysis JAMA Oncol 2016 21460ndash1469
6 Rahman M Abbatematteo J De Leo EK et al The effects of new orworsened postoperative neurological deficits on survival of patientswith glioblastoma J Neurosurg 2017 127123ndash131
7 Louis DN Perry A Reifenberger G et al The 2016 World HealthOrganization Classification of Tumors of the Central NervousSystem a summary Acta Neuropathol 2016 131803ndash820
8 McGirt MJ Bulsara KR Cummings TJ et al Prognostic value ofmagnetic resonance imaging-guided stereotactic biopsy in the
evaluation of recurrent malignant astrocytoma compared with a le-sion due to radiation effect J Neurosurg 2003 9814ndash20
9 Muragaki Y Chernov M Maruyama T et al Low-grade glioma onstereotactic biopsy how often is the diagnosis accurate MinimInvasive Neurosurg 2008 51275ndash279
10 Woodworth G McGirt MJ Samdani A Garonzik I Olivi AWeingart JD Accuracy of frameless and frame-based image-guided stereotactic brain biopsy in the diagnosis of glioma com-parison of biopsy and open resection specimen Neurol Res 200527358ndash362
11 Suzuki H Aoki K Chiba K et al Mutational landscape and clonal ar-chitecture in grade II and III gliomas Nat Genet 2015 47458ndash468
12 Stupp R Mason WP van den Bent MJ et al Radiotherapy plus con-comitant and adjuvant temozolomide for glioblastoma N Engl JMed 2005 352987ndash996
13 Kreisl TN Kim L Moore K et al Phase II trial of single-agent bevaci-zumab followed by bevacizumab plus irinotecan at tumor progres-sion in recurrent glioblastoma J Clin Oncol 2009 27740ndash745
14 Vredenburgh JJ Desjardins A Herndon 2nd JE et al Phase II trial ofbevacizumab and irinotecan in recurrent malignant glioma ClinCancer Res 2007 131253ndash1259
15 Chinot OL Wick W Mason W et al Bevacizumab plusradiotherapy-temozolomide for newly diagnosed glioblastomaN Engl J Med 2014 370709ndash722
16 Gilbert MR Dignam JJ Armstrong TS et al A randomized trial ofbevacizumab for newly diagnosed glioblastoma N Engl J Med2014 370699ndash708
17 Sandmann T Bourgon R Garcia J et al Patients with proneural glio-blastoma may derive overall survival benefit from the addition of bev-acizumab to first-line radiotherapy and temozolomide retrospectiveanalysis of the AVAglio trial J Clin Oncol 2015 332735ndash2744
18 Jackson RJ Fuller GN Abi-Said D et al Limitations of stereotacticbiopsy in the initial management of gliomas Neuro Oncol 20013193ndash200
19 Stupp R Hegi ME Gorlia T et al Cilengitide combined with stan-dard treatment for patients with newly diagnosed glioblastoma withmethylated MGMT promoter (CENTRIC EORTC 26071-22072study) a multicentre randomised open-label phase 3 trial LancetOncol 2014 151100ndash1108
20 Weller M Nabors LB Gorlia T et al Cilengitide in newly diagnosedglioblastoma biomarker expression and outcome Oncotarget2016 715018ndash15032
21 Stupp R Taillibert S Kanner AA et al Maintenance therapy withtumor-treating fields plus temozolomide vs temozolomide alone forglioblastoma a randomized clinical trial JAMA 20153142535ndash2543
22 Wick W TTFields where does all the skepticism come from NeuroOncol 2016 18303ndash305
23 Sampson JH Alternating electric fields for the treatment of glioblas-toma JAMA 2015 3142511ndash2513
24 Lang FF Asher A Prospective clinical trials of brain tumor therapy thecritical role of neurosurgeons J Neurooncol 2004 69151ndash167
25 Lang FF Gilbert MR Puduvalli VK et al Toward better early-phasebrain tumor clinical trials a reappraisal of current methods and pro-posals for future strategies Neuro Oncol 2002 4268ndash277
26 Elkhaled A Jalbert L Constantin A et al Characterization of metab-olites in infiltrating gliomas using ex vivo (1)H high-resolution magicangle spinning spectroscopy NMR Biomed 2014 27578ndash593
27 Jalbert LE Neill E Phillips JJ et al Magnetic resonance analysis ofmalignant transformation in recurrent glioma Neuro Oncol 2016181169ndash1179
28 Touat M Duran-Pena A Alentorn A Lacroix L Massard C Idbaih AEmerging circulating biomarkers in glioblastoma promises andchallenges Expert Rev Mol Diagn 2015 151311ndash1323
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
108
Update on RadiationCombinations in theTreatment of Patientswith Malignant BrainTumors FromRadiosensitizers toImmunotherapy
Debra Nana Yeboa MD1
Erik P Sulman MD PhD123
Departments of 1Radiation Oncology2Translational Molecular Pathology and3Genomic Medicine The University of Texas MDAnderson Cancer Center 1515 Holcombe BlvdUnit 97 Houston Texas USA Tel 713-563-2300dnyeboamdandersonorg andepsulmanmdandersonorg
109
AbstractAdvances in radiosensitizers and immunotherapyhave ushered in a new frontier in brain tumortreatment The brain has often been viewed as asanctuary site due to the bloodndashbrain barrier andthus the 2 primary modalities of therapy includedsurgery and radiation therapy (RT) More recentlysystemic therapies have played a greater role aseither combination therapy radiosensitizers or im-munotherapy Two novel radiosensitizers are beingdeveloped for the treatment of brain metastasesRRx-001 for example is a small molecule thataccelerates the NO2 to NO conversion of deoxyhe-moglobin and the agent 2-dexoyglucose (2-DG) is anonmetabolized glucose analogue that interfereswith ATP formation Poly(ADP-ribose) DNA polymer-ase inhibitors are promising due to their distinctradiobiological effects Veliparib and olaparib areamong the most studied with randomized trialsexploring their use in gliomas and brain metastasesImmunotherapy including immune checkpoint inhib-itors may play a role for both primary gliomas andbrain metastases RT has been shown to enhancethe function of cytotoxic T lymphocytes induce infil-tration of cytotoxic T lymphocytes and enhancefunction Trials are presently exploring use of bothprogrammed cell death protein (PD)1 and PD ligand1 blockade in glioblastoma patients with radiationSimilarly several immunotherapies are being investi-gated with either stereotactic radiosurgery or wholebrain radiation therapy for brain metastases In thisreview the use of radiosensitizers and immunother-apy agents with RT will be discussed broadly
Keywords brain metastases brain tumors gliomasimmunotherapy radiation therapy radiosensitizers
Radiosensitizers andImmunotherapy inBrain TumorsAdvances in radiosensitizers and immunotherapy haveushered in a new frontier to brain tumor treatment Braintumors however are a diverse class sharing only similaranatomic location Both primary brain malignancies andbrain metastasis have widely diverse histologies and mo-lecular phenotypes With the bloodndashbrain barrier thebrain has often been viewed as a sanctuary site and thusthe 2 primary modalities of therapy included surgery andradiation with decreased benefit from systemic agentsdue to lack of brain penetration However more recentlysystemic therapies have played a greater role as eithercombination therapy radiosensitizers or immunother-apy While temozolomide (TMZ) has played a pivotal rolefor glioblastoma (GBM) only a subset of patients benefitfrom the treatment1 The use of alternative systemicagents that may potentiate the effects of radiation ther-apy (RT) is becoming increasingly appealing Similarly forbrain metastases a variety of systemic agents are beingexplored primarily based on histology and immune pro-file In this review the use of radiosensitizers and immu-notherapy agents currently under investigation with RTwill be discussed
RadiosensitizersThe guiding concept of radiation sensitization is to in-crease the biologic effect of radiation such as increasedDNA damage decreased DNA repair decreased hypoxiaor increased G2M cell cycle blockade leading to im-proved tumor control and increased patient survival2
Poly(adenosine diphosphate-ribose) DNA polymerase(PARP) inhibitors are promising radiosensitizers due totheir roles in DNA repair3 PARP inhibitors work againstPARP1 a nuclear enzyme involved in the recruitment ofrepair proteins used in base excision repair and single-strand break repair PARP1 may also play a role in nonho-mologous end-joining4 The primary investigation ofPARP inhibitors has been in potentiating radiation andchemotherapy effects the latter in the context of homolo-gous repair deficient tumors For radiation the primarymechanism of action is inducing damage to nucleotidesleading to single-strand and double-strand breaks ThusPARP inhibitors in combination with radiation have an ap-pealing mechanism to inhibit or delay DNA repair andlikely convert more single-strand breaks to double-strandbreaks4
While several PARP inhibitors are currently being evalu-ated in a variety of tumors including talazoparib and nira-parib veliparib and olaparib are among the most studiedand there are randomized trials exploring their use in
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
110
gliomas The US National Cancer Institute (NCI)ndashfundedAlliance for Clinical Trials in Oncology (Alliance) A071102is a randomized phase IIIII trial evaluating the use ofveliparib in combination with TMZ in the adjuvant settingin patients with GBM tumors exhibiting hypermethylationof the O6 methylguanine DNA methyltransferase (MGMT)gene promoter Preclinical data supporting this trial sug-gested that only patients with MGMT methylated tumorswould benefit from the combination a group of patientsfor whom TMZ concurrent with radiation might be mostbeneficial5 A phase I trial performed by the NCI-fundedAmerican Brain Tumor Consortium attempted to combineveliparib with radiation and TMZ but failed to identify asuitable recommended phase II dose due to significanthemotoxicity6 Thus attempts to combine radiation withveliparib have focused on patients least likely to benefitfrom TMZ namely with MGMT unmethylated tumors forwhom TMZ could be withheld The Australian VeliparibRT and TMZ trial in newly diagnosed unmethylatedMGMT glioblastoma (VERTU) is a single-arm study inwhich patients receive RT with veliparib followed by adju-vant TMZ and veliparib4
An ongoing novel approach to radiosensitize gliomasinvolves a combination with an agent that interferes withan essential metabolic process 2-Dexoyglucose (2-DG)is a nonmetabolized glucose analogue that acts as acompetitive inhibitor of glycolysis It is transported acrossthe bloodndashbrain barrier by the glucose transporter GLUT-1 and thus has good penetration into the CNSIntracellularly it is trapped and accumulates in cells simi-lar to the mechanism of 18-fluorodeoxyglucose 2-DG isphosphorylated by glycolytic enzymes and the
phosphorylated 2-DG (2-deoxyglucose-P) is trapped in-tracellularly Inhibition of hexokinase activity by 2-DGinterferes with ATP formation and results in tumor celldeath7 While it has positive attributes by selectively tar-geting metabolically active tumor cells 2-DG has alsobeen associated with Q-T prolongation The currentphase III trial in gliomas is assessing the toxicity and tol-erability of 2-DG with hypofractionated radiation of 5 Gyas a radiosensitizer7
Two novel radiosensitizers are being developed for thetreatment of brain metastases First RRx-001 is a smallmolecule initially designed by the aerospace industry Itworks in part as a radiosensitizer by increasing blood flowand thus oxygenation of tumors through nitric oxideRRx-001 which binds to hemoglobin accelerates theNO2 to NO conversion of deoxyhemoglobin It workslocally under hypoxic conditions and subsequentlythe radiosensitive effects through nitric oxide are invasodilation and inhibiting DNA repair enzymes8 Nitricoxide is relatively benign The higher levels of oxidativestress with H2O2 and superoxide in tumors in comparisonto normal tissues result in the preferential generation ofreactive peroxynitrite in the presence of higher nitric oxidelevels7 This accounts for the increased specificity anddecreased toxicity with RRx-001 The dose limiting toxic-ity in a phase I trial of 25 patients treated with eitherweekly or biweekly infusions was infusional pain relatedto the release of NO at the site of injection7 Outside ofpreclinical models 2 clinical reports examining wholebrain radiation therapy (WBRT) with RRx-001 reported anintracranial response A patient with melanoma and 2hemorrhagic edematous lesions of 26 cm and 33 cm
Table 1 Clinical trials involving immunotherapy and radiation therapy1213
Clinical Trials Number Phase Disease Type Treatment Groups
NCT02667587 II Newly diagnosed GBMMGMT-methylated
Nivolumabthorn TMZthorn RT vs placebothornTMZ thorn RT
NCT02617589 III Newly diagnosed GBM Nivolumabthorn RT vs TMZthorn RTNCT02336165 II Newly diagnosed unmethylated
MGMT recurrent glioblastomaMEDI4736thorn standard RT vs MEDI4736 thorn
bevacizumabNCT02530502 III Newly diagnosed GBM RTthorn TMZthorn pembrolizumab TMZthorn
pembrolizumabNCT02313272 I Recurrent glioma Hypofractionated stereotactic radiationthorn
pembrolizumab thorn bevacizumabNCT02696993 III Brain metastases Nivolumabthorn SRS nivolumabthornWBRT
nivolumabthorn ipilimumab thorn SRS nivolu-mabthorn ipilimumab thornWBRT
NCT02115139 II Melanoma brain metastases Ipilimumab thornWBRTNCT02097732 II Melanoma brain metastases Ipilimumab SRS ipilimumab vs SRS
ipilimumabNCT01703507 I Melanoma brain metastases Ipilimumab thornWBRT vs ipilimumab thorn SRSNCT02107755 II Melanoma brain metastases Ipilimumab thorn SRSNCT02858869 pilot Melanoma and NSCLC Pembrolizumabthorn SRSNCT01950195 I Melanoma brain metastases Ipilimumab thorn SRSNCT02662725 II Melanoma brain metastases Ipilimumab thorn SRS
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
111
after a single intravenous dose of RRx-001 of 5 mgm2 4days before WBRT resulted in symptomatic improvementwithin 48 hours By 4 months after radiation there was areduction in size in the largest dimension down to 10 cmand 23 cm of the respective lesions A second report of amelanoma patient with at least 18 lesions after receivingRRx-001 of 5 mgm2 4 days before WBRT as well astwice weekly doses during the 2 weeks of radiation alsoshowed response The patient at 4 months had disap-pearance of 13 of 18 lesions with shrinkage of theremaining 5 lesions8 Presently BRAINSTORM is a phaseIII dose escalation trial of RRx-001 designed to be ad-ministered twice weekly for 2 weeks with WBRT (30 Gy in10 fractions) with the option for weekly maintenance8
Veliparib has also been evaluated in the setting of brainmetastases It was tested in a global randomized con-trolled trial with WBRT Veliparib is orally bioavailable andcrosses the bloodndashbrain barrier It was first examined in amultihistology phase I trial in patients with nonndashsmall celllung cancer (NSCLC) breast cancer melanoma and re-nal and colorectal cancers among others The study of81 patients tested dose tolerance of veliparib from 10 to300 mg orally twice a day with WBRT to 30 Gy in 10 frac-tions or 375 Gy in 15 fractions9 The phase I trial dose es-calation portion did not reach the predefined criteria forthe maximum tolerated dose but there was amplificationof the adverse effects of nausea and vomiting among thehighest dose cohort of 300 mg bid9 The adverse eventprofile at 200 mg bid was similar to that of WBRT aloneDoses of veliparib from 20 to 200 mg bid demonstratesimilar antitumor activity and other studies in preclinicalmodels found that 50 mg daily demonstrated significantreduction in poly(ADP-ribose) in peripheral blood mono-nuclear cells and tumor tissue while also effectivelycrossing the bloodndashbrain barrier Thus the subsequentphase II trial examined 50 mg with WBRT9 In order to as-sess a more homogeneous cohort the phase III globalrandomized trial studied only NSCLC at the 2 doses of50 mg and 200 mg twice daily versus placebo twice a daywith WBRT10 The primary endpoint was overall survivalIn 307 patients in a 111 randomization of 50 mg bid200 mg bid or placebo twice daily the study found nosignificant differences in overall survival among the differ-ent groups10 The majority of patients across the treat-ment groups had a graded prognostic assessment (GPA)score of25 and a Karnofsky performance status ofgt80 The median overall survival was 185 days forpatients receiving placebo and 209 days for those receiv-ing veliparib without any statistically significant differ-ence These results were similar to the disease-specificestimate of median survival for the disease-specific GPAof NSCLC patients with brain metastases10
Several other radiosensitizers have failed to improve overradiation alone in a number of trials These have includedtrials with WBRT including motexafin gadolinium efap-roxyn bortozemib thalidomide teniposide topotecanpaclitaxel and cisplatin7 Of note other PARP inhibitorsalso being assessed include talazoparib and niraparib4
which may yield positive results The use of valproic acid(VPA) as a histone deacetylase inhibitor has also beenconsidered to have radiosensitizing potential in additionto its anti-epileptic drug properties11 While studies havereported that patients with GBM receiving an anti-epilep-tic agent may have higher overall survival than those re-ceiving standard chemoradiation therapy alone thebenefit remains controversial Retrospective analysissuggested that patients taking VPA specifically had bettersurvival in comparison to other anti-epileptic drugs Alsoa recent prospective phase II trial was performed in 37patients with GBM receiving VPA 25 mgkg concurrentlywith TMZ chemoradiation and reported a median survivalof 296 months While controversial further data andinvestigation are needed into this and other agents thatmay potentiate RT
Immunotherapy and radiationImmune checkpoint inhibitors lead to activation of T cellswhich may traffic across the bloodndashbrain barrier to inter-act with tumor Primary brain tumors may evade the im-mune system through upregulation of immunecheckpoints and possible immunosuppression12
Monoclonal antibodies promote immune-mediated anti-tumor activity by inhibiting the immune functionndashmediated cytotoxic T-lymphocyte associated protein 4(CTLA-4) and programmed cell death protein 1 (PD-1)receptors PD protein ligand (PD-L1) is upregulated inGBM through oncogenic signaling possibly throughphosphatase and tensin homolog loss and interleukin-10signaling1314 RT has also been shown to enhance thefunction of cytotoxic T lymphocytes RT may induce aninfiltration of cytotoxic T lymphocytes and enhance theirfunction It may also induce antindashCTLA-4 agents inhibitingT-cell function and increasing the CD8thorn T cellregulatoryT cell ratio in cases of melanoma15 Thus PD-1 and PD-L1 blockers may have a further role in CNS managementwith the use of radiation
In preclinical models radiation has been examined withimmunotherapy that included among other mechanismsvaccination PD-1 blockade and CTLA-4 blockade Inmice radiation plus a vaccination of irradiated gliomacells was associated with increased survival of 40 to80 compared with 0 to 10 for other groups stud-ied16 A benefit of PD-1 blockade with stereotactic radio-surgery (SRS) specifically has also been shown in amouse model In comparison to mice treated with radia-tion antindashPD-1 therapy or a combination only those re-ceiving combination therapy had a higher percentagesurvival alive beyond 180 days after treatment17 Othermouse carcinoma models have identified response withanti-CTLA antibody and fractionated radiation therapy18
CD137 activation CTLA-4 blockade and focal radiationtherapy have been examined in an immunocompetent in-tracranial GBM model Mice treated with triple combina-tion therapy had 50 greater survival19 In other murine
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
112
models the use of antindashPD-1 and antindashCTLA-4 agentsshowed improved survival and increased tumor infiltratingleukocyte populations compared with single modalitywith concurrent radiation16 There are conflicting data re-garding timing or sequencing of therapy with some ani-mal models showing no difference in tumor response inrelation to timing of RT and delivery of immunotherapy18
For instance in one animal model CTLA-4 blockade de-livered simultaneously with radiation or delivered a coupleof days after showed no difference in survival among themice19
Increased PD-1 expression in circulating monocytes hasbeen identified as a biomarker for tumor-induced immu-nosuppression and may serve as a prognostic factor forpotentially worse survival outcomes in clinic13 In onestudy GBM patients with lower PD-L1 expression hadhigher median overall survival than those with higher PD-L1 expression suggesting that lower expression may beassociated with less immunosuppression and more im-mune activity against the tumor glioma20 RT with immunecheckpoint blockade is being investigated to assess if theaddition of PD-1 and PD-L1 inhibitors may improve theoutcomes or toxicity profile of standard therapy For in-stance a multi-institutional trial opened as a phase III willevaluate outcomes in GBM receiving radiation and pem-brolizumab with TMZ (NCT02530502) Next durvalumabor MEDI4736 a PD-L1 inhibitor is being examined forunmethylated MGMT GBMs with standard radiotherapy(NCT02336165)12 The impact of checkpoint inhibitorsduring adjuvant treatment of GBM is currently beingevaluated in the NCI-funded NRG-BN002 trial(NCT02311920) which will evaluate the antindashCTLA-4antibody ipilimumab alone or in combination with theantindashPD-1 antibody nivolumab for patients with newlydiagnosed GBM
Brain metastases have clonal populations of cells differ-ent from the rest of the brain and a unique microenviron-ment that may influence immunotherapy There may bemore immune infiltrates in metastases than in primarybrain tumors21 PD-L1 expression in brain metastasesvaries by histology In a series evaluating PD-L1 expres-sion in various tumors including melanoma NSCLCbreast renal colorectal and small cell less than 10showed significant expression22 There was greatest ex-pression among NSCLC and melanoma with a correla-tion between PD-L1 expression and tumor infiltratinglymphocytes22 Institutional series have examined thecombination of radiation and immune checkpoint block-ade In another study specific to melanoma brain metas-tases PD-L1 expression was found in over 50 of thecases and among those cases over 40 expressedPD-L1 in more than 5 of tumor cells23 The largest bodyof data for use of PD-L1 with radiation is for melanomaand NSCLC
Ipilimumab is a human monoclonal antibody that blocksCTLA-4 and allows for T-cell activation and proliferationto enhance the immune response to cancer In a
retrospective review of 70 patients with brain metastasestreated with SRS or WBRT the 33 patients receiving im-munotherapy had a median survival of 183 months incomparison to the 37 patients who did not receive ipili-mumab with a median survival of 53 months While therewere limited data among the cohort to evaluate sequenc-ing of therapy among 10 evaluable patients 40 whoreceived ipilimumab prior to RT had a partial response incomparison to only 10 among the cohort of 22 evalu-able patients who did not receive ipilimumab therapy atall with radiation24 Another retrospective institutionalstudy of 77 patients in which 37 received ipilimumabfound that patients treated with SRS and ipilimumab hada median survival of 213 months versus 49 months forthose not receiving ipilimumab Most interestingly theyidentified that the correlation remained significant evenafter adjusting for additional factors such as performancestatus Secondly there was not an increased need for useof salvage WBRT25
The sequencing of radiotherapy and immune checkpointinhibitors is of interest In a study of patients with brainmetastases the one-year survival for patients receivingSRS before ipilimumab was greater at 65 in contrast to56 for those receiving it concurrently and 40 for thosereceiving it after SRS26 Similarly another study of 75patients with 566 brain metastases showed greater tu-mor lesion response at 6 months from SRS for patientsreceiving ipilimumab nivolumab or pembrolizumabwithin 4 weeks of their SRS27 Those receiving concurrenttherapy had by 6 months a decrease of 949 in compar-ison to 662 for those not receiving checkpoint inhibi-tors within 4 weeks Prospective clinical trials areinvestigating different combinations of RT with immunecheckpoint blockers in this setting For instance new tri-als are currently evaluating intracranial tumor control at 6months and the timing of immune therapy or immunecheckpoint inhibitors in relation to SRS28
Vaccines are also being developed for primary braintumors showing some evidence for their use Vaccinesdeveloped from dendritic cells and tumor lysate with tu-mor antigens such as the epidermal growth factor recep-tor variant III vaccine have shown promise29 Forinstance in a placebo controlled phase II trial of ICT-107a vaccine composed on autologous dendritic cells andtumor antigens progression-free survival was increasedby 2 months for those receiving the vaccine30 Radiationmay assist in serving as a primer for the immunogeniceffects by facilitating tumor antigen uptake by dendriticcells and cross presentation on major histocompatibilitycomplex I Thus RT may assist in the tumor-specific cy-totoxic T lymphocytes associated with the immunemechanism
In conclusion although there may be challenges to com-bining and sequencing brain tumors radiosensitizersand immunotherapy the opportunities and potential fornovel applications are promising For brain tumors brainmetastases are typically underrepresented in trials
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
113
despite being among the most common intracraniallesions Despite their large population patients with brainmetastases are often excluded from clinical trials withnovel agents due to concerns regarding confounding out-comes and tolerability12 Primary gliomas also offer anovel frontier for the use of immunotherapy to standardadjuvant chemotherapy and radiation particularly forpatients with GBM less likely to respond to TMZ such aswith unmethylated MGMT As studies work to define therole of RT and radiosensitizers and immunotherapy fur-ther analysis is needed to assess the timing of RT andthese treatments
References
1 Stupp R Hegi ME Mason WP et al Effects of radiotherapy withconcomitant and adjuvant temozolomide versus radiotherapy aloneon survival in glioblastoma in a randomised phase III study 5-yearanalysis of the EORTC-NCIC trial Lancet Oncol 2009 10459ndash466
2 Lawrence TS Blackstock AW McGinn C The mechanism of actionof radiosensitization of conventional chemotherapeutic agentsSemin Radiat Oncol 2003 1313ndash21
3 Lesueur P Chevalier F Austry JB et al Poly-(ADP-ribose)-polymer-ase inhibitors as radiosensitizers a systematic review of pre-clinicaland clinical human studies Oncotarget 2017 8(40)69105ndash69124
4 Lester A Rapkins R Nixdorf S Khasraw M McDonald KCombining PARP inhibitors with radiation therapy for the treatmentof glioblastoma is PTEN predictive of response Clin Transl Oncol2017 19273ndash278
5 Gupta SK Kizilbash SH Carlson BL et al Delineation of MGMT hyper-methylation as a biomarker for veliparib-mediated temozolomide-sensi-tizing therapy of glioblastoma J Natl Cancer Inst 2016 108
6 Kleinberg LR Blakeley J Mikkelsen T et al An American BrainTumor Consortium (ABTC) phase 1 trial of veliparib (ABT-888)temozolomide (TMZ) and concurrent radiation therapy (RT) fornewly diagnosed glioblastoma multiforme (GBM) need for modifica-tion to approach for combining these therapies InternationalJ Radiat Oncol Biol Phys 2012 84S7ndashS8
7 Oronsky BT A Review of two promising radiosensitizers in brainmetastases Rrx-001 and 2-deoxyglucose In NC Oronsky edJ Cancer Sci Ther 2015 pp 137ndash141
8 Kim MM Parmar H Cao Y et al Concurrent whole brain radiother-apy and RRx-001 for melanoma brain metastases Neuro Onc2016 18455ndash456
9 Mehta MP Wang D Wang F et al Veliparib in combination withwhole brain radiation therapy in patients with brain metastasesresults of a phase 1 study J Neurooncol 2015 122409ndash417
10 Chabot P Hsia TC Ryu JS et al Veliparib in combination withwhole-brain radiation therapy for patients with brain metastasesfrom non-small cell lung cancer results of a randomized globalplacebo-controlled study J Neurooncol 2017 131105ndash115
11 Ochiai S Nomoto Y Yamashita Y et al Roles of valproic acid inimproving radiation therapy for glioblastoma a review of literaturefocusing on clinical evidence Asian Pac J Cancer Prev 201617463ndash466
12 Tan AC Heimberger AB Menzies AM Pavlakis N Khasraw MImmune checkpoint inhibitors for brain metastases Curr Oncol Rep2017 1938
13 DrsquoSouza NM Fang P Logan J Yang J Jiang W Li JCombining radiation therapy with immune checkpoint blockade
for central nervous system malignancies Frontiers Oncol 20166212
14 Parsa AT Waldron JS Panner A et al Loss of tumor suppressorPTEN function increases B7-H1 expression and immunoresistancein glioma Nat Med 2007 1384ndash88
15 Binder DC Davis AA Wainwright DA Immunotherapy for cancer inthe central nervous system current and future directionsOncoimmunology 2016 5e1082027
16 Newcomb EW Demaria S Lukyanov Y et al The combination ofionizing radiation and peripheral vaccination produces long-termsurvival of mice bearing established invasive GL261 gliomas ClinCancer Res 2006 124730ndash4737
17 Zeng J See AP Phallen J et al Anti-PD-1 blockade and stereotac-tic radiation produce long-term survival in mice with intracranial glio-mas Int J Radiat Oncol Biol Phys 2013 86343ndash349
18 Chow KK Hara W Lim M Li G Combining immunotherapy withradiation for the treatment of glioblastoma J Neurooncol2015123459ndash464
19 Belcaid Z Phallen JA Zeng J et al Focal radiation therapy com-bined with 4-1BB activation and CTLA-4 blockade yields long-termsurvival and a protective antigen-specific memory response in amurine glioma model PLoS One 2014 9e101764
20 Topalian SL Hodi FS Brahmer JR et al Safety activity and im-mune correlates of anti-PD-1 antibody in cancer N Engl J Med2012 3662443ndash2454
21 Bienkowski M Preusser M Prognostic role of tumour-infiltrating in-flammatory cells in brain tumours literature review Curr OpinNeurol 2015 28647ndash658
22 Harter PN Bernatz S Scholz A et al Distribution and prognostic rel-evance of tumor-infiltrating lymphocytes (TILs) and PD-1PD-L1 im-mune checkpoints in human brain metastases Oncotarget 2015640836ndash40849
23 Berghoff AS Ricken G Widhalm G et al Tumour-infiltrating lym-phocytes and expression of programmed death ligand 1 (PD-L1) inmelanoma brain metastases Histopathology 2015 66289ndash299
24 Silk AW Bassetti MF West BT Tsien CI Lao CD Ipilimumab and ra-diation therapy for melanoma brain metastases Cancer Med 20132899ndash906
25 Knisely JP Yu JB Flanigan J Sznol M Kluger HM Chiang VLRadiosurgery for melanoma brain metastases in the ipilimumab eraand the possibility of longer survival J Neurosurg 2012117227ndash233
26 Kiess AP Wolchok JD Barker CA et al Stereotactic radiosurgeryfor melanoma brain metastases in patients receiving ipilimumabsafety profile and efficacy of combined treatment Int J Radiat OncolBiol Phys 2015 92368ndash375
27 Qian JM Yu JB Kluger HM Chiang VL Timing and type of immunecheckpoint therapy affect the early radiographic response of mela-noma brain metastases to stereotactic radiosurgery Cancer 20161223051ndash3058
28 Silk AW Cao Y Gomez-Hassan D et al A randomized phase IIstudy of ipilimumab induction in patients with melanoma brain me-tastases receiving stereotactic radiosurgery J Clin Oncol 2015 33TPS9079ndashTPS9079
29 Neagu MR Reardon DA An Update on the role of immunotherapyand vaccine strategies for primary brain tumors Curr TreatOptions Oncol 2015 1654
30 Wen PY Reardon DA Phuphanich S et al A randomized double-blind placebo-controlled phase 2 trial of dendritic cell (DC) vaccina-tion with ICT-107 in newly diagnosed glioblastoma (GBM) patientsJ Clin Oncol 2014 322005ndash2005
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
114
British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

Editorial
This year from November 15 to 19SNO held its 22nd annual meeting inSan Francisco Each meeting has atheme and this yearrsquos overall themefocused on the ldquoCancer Moonshotrdquoprogram that was proposed byformer president Obama in 2016 andwas initially led by former vice-president Biden whose son perishedfrom a GBM The meeting wasattended by over 2500 participantsfrom all over the world with a recordnumber of submitted abstracts (over1800) The meeting was preceded bytwo successful former meetings theNeuro-oncology Review Course andthe SNOSCIDOT course on intersti-tial CNS delivery both held on Nov15 Our Education Day was held onNov 16 it focused on the subject ofGBM resistance and was organizedby Sue Bell Robert Cavaliere KhalidShah and Albert Kim The mainmeeting was organized by ManishAghi Vinay Puduvalli and FrankFurnari and was highlighted by key-note talks by Jennifer Doudna on
CrispRCas9 and Carlo Croce onmicroRNAs There were multipleSNO educational events from a sun-rise session to lunchtime tutorialsand dinner events such as very wellattended poster and e-talk sessionsThere were also multiple events dedi-cated to stress relief as well includ-ing opening receptions gala dinnersand burnout relief events We are
looking forward to the 23rd meetingin New Orleans which will be led byour new officers (President PatrickWen Vice-President Gelared Zadehand SecretaryTreasurer TracyBatchelor)
EA (Nino) Chiocca
President SNO
100
Volume 2 Issue 3 Editorial
Brain TumorEpigeneticsFrom Researchto ClinicalPractice
Silvia MarinoBlizard Institute Barts and The London School ofMedicine and Dentistry Queen Mary University ofLondon 4 Newark Street E12AT London UK
101
IntroductionEpigenetics is defined as the study of heritable changesin gene expression that are not caused by alterations inDNA sequences1 The phenotypic difference between acaterpillar and a butterfly for example is due to epige-netic regulation of gene expression in the same animalwith the same DNA I particularly like this example to ex-plain the meaning of the term epigenetics as it impres-sively demonstrates how powerful these mechanisms arein controlling phenotypic changes Epigenetic changesare reversible and include the key processes of DNAmethylation histone modifications and noncoding RNA-associated gene silencing (recently reviewed2) known toplay an essential role during the embryonic and postnataldevelopment of an organism and in tissue homeostasis2
Disruptions of epigenetic processes can induce changesin gene function which together with genetic changescan lead to the neoplastic transformation of a normal cell(recently reviewed)3
Recent technological advances have significantly con-tributed to the tremendous progress in understandinghow these epigenetic modifications are regulated in nor-mal cells and deregulated in cancer cells For examplethis knowledge has enabled the translation into better di-agnostic algorithms for tumor classification prognostica-tion and risk assessment Importantly we are nowentering a time when novel therapies targeting thesederegulated epigenetic mechanisms are being devel-oped with some of them showing very promising effectsin preclinical models
It is beyond the scope of this article to comprehensivelyreview mechanisms of epigenetic regulation of gene ex-pression and their deregulation in brain tumors excellentrecent reviews are available to the readers on thesesubjects2ndash5 Here I will discuss a few examples of recentepigenetic discoveries which have informed the develop-ment of novel diagnostic and prognostic tools or led tosuccessful preclinical testing of new epigenetic drugs inexperimental models
Epigenetic Profiles inthe MolecularClassification of BrainTumorsGlioma One of the first examples of an epigenetic changeinforming the design of an assay for diagnostic screeningto corroborate a therapeutic decision is the assessmentof methylation of the MGMT promoter in malignantgliomas6 MGMT (O6-methylguanine DNA methyltransfer-ase) is a key enzyme in the DNA repair network which
removes the mutagenic and cytotoxic adducts from O6
guanine in DNA the preferred point of attack of alkylatingchemotherapeutic agents (ie BCNU temozolomide etc)Hypermethylation of cytosine-phosphate-guanine (CpG)islands located in the promoter region of MGMT is pri-marily responsible for the loss of MGMT function in manytumor types hence leading to an increased sensitivity tothe killing effects of alkylating drugs used in chemo-therapy6 This test is widely used in clinical practice topredict response to temozolomide the alkylating drug ofchoice in high-grade gliomas although it should bestressed that there is still no consensus as to which testmethod to use which CpG sites to assess and what themethylation cutoff should be
Ependymoma Until very recently these tumors havebeen subclassified and graded on the basis of histologi-cal features into low and high grade In 2015 a molecularclassification based on DNA methylation profiling hasbeen proposed which defines 9 molecular subgroups 3for each anatomical location of these tumors (supratento-rial posterior fossa and spinal cord)7 In the supratento-rial location ependymomas with the fusion geneC11ORF95RELA (ST-EPN-RELA) have a poor prognosisand in the posterior fossa it is the ependymoma groupEPN-A that is characterized by a poor prognosis7 Allother ependymomas show a comparatively goodprognosis7 Although not yet included in the World HealthOrganization (WHO) 2016 classification a recent consen-sus paper has recommended that this classification beused for enrollment in prospective clinical trials8 and it isexpected to contribute to informing decisions onmolecular-based treatments as they become available
Medulloblastoma (MB) International consensusrecognizes 4 medulloblastoma molecular subgroupsWNT (MBWNT) SHH (MBSHH) Group 3 (MBGrp3) andGroup 4 (MBGrp4) each defined by their characteristicDNA methylation and genome-wide transcriptomicprofiles9 Recently the heterogeneity within these sub-groups has been reduced by 2 independent studieswhich have defined additional subtypes Schwalbe andcolleagues10 have suggested to split MBSHH into 2 age-dependent subtypes corresponding to ldquoinfantrdquo (lt43 y)and ldquochildhoodrdquo patients (43 y) and MBGrp3 andMBGrp4 into further high-risk and low-risk subtypes whilethe MBWNT group remains unchanged10 Interestingly thelow-risk subtypes were defined primarily by hypermethy-lation in comparison to normal cerebellum whereas thehigh-risk subtypes were defined by relativehypomethylation10 Cavalli and coauthors11 used integra-tive clustering of DNA methylation and gene expressiondatasets from 763 patients to split the original 4 sub-groups into 12 subtypes MBSHH is split into 4 subtypes(abc d) MBWNT into 2 subtypes (ab) MBGrp3 andMBGrp4into 3 subtypes each (abc)11 The subtypes iden-tified in these 2 studies overlap considerably and themain differences seem to be related to the inclusion ofadult MB patients in the Cavalli study Importantly MBsubgroups and their subtypes identified by their
Brain Tumor Epigenetics From Research to Clinical Practice Volume 2 Issue 3
102
epigenetic and related transcriptional profiles1011 havedistinct genetic and clinicopathological features1011 andtheir implementation for patient stratification for betterprognostication and enrollment into subgroupsubtype-directed therapies in the context of clinical trials will be astep change in the treatment of MB patients
All CNS tumors A classification tool for brain tumorsbased on genome-wide DNA methylation patterns and arandom forest-based machine learning approach hasbeen developed and extensively tested by the GermanCancer Research Center (wwwmolecularneuropathologyorg) This resource is available online and has provento be a valuable tool to improve brain tumor diagnosticsThis approach has facilitated the identification of com-mon druggable molecular pathway alterations across var-ious histological tumor entities thus allowing patients toenter the most appropriate clinical trials and in somecases be offered molecularly matched therapies As anexample DNA methylation profiles allow precise identifi-cation of cases with mitogen-activated protein kinase(MAPK) activation which is a feature of tumors withBRAF V600E mutation1213 which can span various tradi-tional histological entities such as pilocytic astrocytomaspleomorphic xanthoastrocytomas ganglioglioma andsubependymal giant cell astrocytomas to predict re-sponse to specific inhibitors interrupting the BRAFMEKcomponent of the MAP kinase pathway14
Novel TherapeuticApproaches TargetingEpigeneticDeregulationDiffuse intrinsic pontine glioma (DIPG) is a highlyaggressive pediatric tumor located in the brainstem andcharacterized by a rapid and diffusely infiltrative patternof growth These tumors cannot be treated surgicallybecause of their location and infiltrative nature15
Radiation therapy is the standard treatment although itprovides only temporary symptom relief with no overallsurvival benefits and conventional chemotherapy drugsare ineffective15
Mutations in histone H3 variants occur in more than 80of DIPG and result in a lysine-to-methionine substitution(H3K27M)16 17 H3K27M has been shown to inhibitpolycomb repressive complex 2 (PRC2) by binding to itscatalytic subunit EZH2 and reducing the methylation ofH3 at lysine 27 (H3K27me) at selected target loci18 Theresidual PRC2 activity is required to maintain DIPGproliferative potential by repressing neuronaldifferentiation in patient-derived cell lines and in agenetically engineered mouse model1920 Importantlysmall-molecule EZH2 inhibitors abolish tumor cell growth
in these models raising the possibility that inhibitionof EZH2 could be a novel therapeutic strategy for thesetumors19
An independent study showed that H3K27M associateswith increased H3K27 acetylation (H3K27ac) and that themajority of the heterotypic H3K27M-K27ac nucleosomesco-localize with bromodomain proteins at the loci of ac-tively transcribed genes20 The authors have shown thatblocking the recruitment of bromodomain proteins by het-erotypic H3K27M-K27ac nucleosomes in DIPG with bro-modomain and extraterminal domain family inhibitorsefficiently inhibited tumor progression thus identifying thisclass of compounds as potential therapeutics in DIPG20
These important advances in understanding the underly-ing biology of DIPG have led to the identification of novelepigenetic therapeutic approaches which are very effec-tive at the preclinical level and if confirmed in transla-tional studies could change the way we treat thesetumors in the near future
Conclusion and outlookThese are exciting and challenging times for theneuro-oncology community Exciting because there isgrowing expectation in the field that new discoveriessuch as those discussed in this article can soon translateinto new and more effective therapeutic approachesChallenging because it is clear that new skill sets are re-quired to effectively apply them to benefit patients
The clinical training in many neuro-oncology specialtieswill have to take into account the additional knowledgeand skills needed in the field and offer education incomplementary disciplines such as next-generationsequencing technologies integrated with interpretativedata analysis as well as molecular biology for the designof biologically informed assays and tools The require-ment for these new highly specialized skills also needs tobe reflected in the composition of the clinical teamswhere bioinformatics expertise will play an increasinglyimportant role for the integration of multimodal data inpatient care
References
1 Waddington CH Canalization of development and the inheritance ofacquired characters Nature 1942150563ndash565
2 Allis CD Jenuwein T The molecular hallmarks of epigenetic controlNat Rev Genet 201617487ndash500
3 Flavahan WA Gaskell E Bernstein BE Epigenetic plasticity and thehallmarks of cancer Science (New York NY 2017357
4 Edwards JR Yarychkivska O Boulard M Bestor TH DNA methyla-tion and DNA methyltransferases Epigenetics amp chromatin20171023
5 Filbin MG Suva ML Gliomas genomics and epigenomics arriving atthe start and knowing it for the first time Annual Rev Pathol201611497ndash521
6 Hegi ME et al MGMT gene silencing and benefit from temozolomidein glioblastoma N Engl J Med 2005352997ndash1003
Volume 2 Issue 3 Brain Tumor Epigenetics From Research to Clinical Practice
103
7 Pajtler KW et al Molecular Classification of Ependymal Tumorsacross All CNS Compartments Histopathological Grades and AgeGroups Cancer Cell 201527728ndash743
8 Pajtler KW et al The current consensus on the clinical managementof intracranial ependymoma and its distinct molecular variants ActaNeuropathol 20171335ndash12
9 Taylor MD et al Molecular subgroups of medulloblastoma the cur-rent consensus Acta Neuropathol 2012123465ndash472
10 Schwalbe EC et al Novel molecular subgroups for clinical classifi-cation and outcome prediction in childhood medulloblastoma a co-hort study Lancet Oncol 201718958ndash971
11 Cavalli FMG et al Intertumoral Heterogeneity withinMedulloblastoma Subgroups Cancer Cell 201731737ndash754 e736
12 Schindler G et al Analysis of BRAF V600E mutation in 1320 nervoussystem tumors reveals high mutation frequencies in pleomorphicxanthoastrocytoma ganglioglioma and extra-cerebellar pilocytic as-trocytoma Acta Neuropathol 2011121397ndash405
13 Tanaka S et al Epithelioid glioblastoma arising from pleomorphicxanthoastrocytoma with the BRAF V600E mutation Brain TumorPathol 201431172ndash176
14 Banerjee A et al A phase I trial of the MEK inhibitor selumetinib(AZD6244) in pediatric patients with recurrent or refractory low-grade glioma a Pediatric Brain Tumor Consortium (PBTC) studyNeuro Oncol 2017191135ndash1144
15 Hargrave D Bartels U Bouffet E Diffuse brainstem glioma in chil-dren critical review of clinical trials Lancet Oncol 20067241ndash248
16 Schwartzentruber J et al Driver mutations in histone H33 and chro-matin remodelling genes in paediatric glioblastoma Nature2012482226ndash231
17 Wu G et al Somatic histone H3 alterations in pediatric diffuse in-trinsic pontine gliomas and non-brainstem glioblastomas Naturegenetics 201244251ndash253
18 Lewis PW et al Inhibition of PRC2 activity by a gain-of-function H3mutation found in pediatric glioblastoma Science (New York NY2013340857ndash861
19 Mohammad F et al EZH2 is a potential therapeutic target forH3K27M-mutant pediatric gliomas Nature Med 201723483ndash492
20 Piunti A et al Therapeutic targeting of polycomb and BET bromodo-main proteins in diffuse intrinsic pontine gliomas Nature Med201723493ndash500
Brain Tumor Epigenetics From Research to Clinical Practice Volume 2 Issue 3
104
The Value of SurgicalResection for MalignantGliomas in the ModernEra Beyond Extent ofResection
Stephen G Bowden MDSeunggu Jude Han MDDepartment of Neurological Surgery OregonHealth and Sciences University 3303 SW BondAve Center for Health and Healing CH8NPortland OR 97239 Telephone 503-494-4314Fax 503-346-6810 hanseohsuedu
105
Malignant gliomas are among the most difficult oncologi-cal entities to treat Despite aggressive treatment prog-nosis remains poor and recurrence and treatmentfailures seem inevitable The current standard-of-caretherapy includes maximal safe surgical resection fol-lowed by concurrent and adjuvant chemoradiotherapyHistorically surgical resection has conferred greater sur-vival benefit to these patients than adjuvant therapiespresumably through the cornerstone principle of cytore-duction However the extent of surgical resection is fre-quently limited by nearby eloquent tissue and risks to keyneurological functions In addition the value of such ag-gressive approaches has been questioned in light of thewidespread infiltration of glioma cells Meanwhile our un-derstanding of glioma biology continues to advance rap-idly fueled in large part by the acquisition of tumor tissueduring surgery Thus the exact role and value of surgeryparticularly in comparing the clinical benefits of maximalextent of resection (EOR) with the biomedical benefits oftissue provision has been a topic of great interest anddebate in both the neuro-oncological and neurosurgicalcommunities
EOR patient age tumor histology performance statusand molecular markers have been widely accepted assignificant predictors of patient outcomes in malignantglioma9 In the past 2 decades many large retrospectivecohort studies have demonstrated improvements in sur-vival with increasing EOR5917 Due to ethical considera-tions evidence from a randomized prospective studysupporting the clinical benefit of aggressive resectionsdoes not exist and likely never will Instead the closestthing to such evidence in malignant glioma comes fromthe randomized phase III trial comparing surgical resec-tions with or without the use of 5-aminolevulinic acid(5-ALA) The use of 5-ALA serving as a means to and aproxy for greater EOR resulted in extended overall sur-vival for patients with newly diagnosed glioblastoma19 Arecent meta-analysis of 41 117 unique patients by Brownet al adherent to the guidelines of PRISMA (PreferredReporting Items for Systematic Reviews and Meta-Analyses) also demonstrated a clear survival benefit forgross total resection over subtotal resection or biopsy atupfront surgery for glioblastoma1 The body of literatureas a whole clearly favored aggressive resections andthere seemed to be little disagreement for a strategytoward maximal resection when clinically feasibleHowever the challenge still remains when such strategiescome at the risk of neurological morbidity A recent reportby Rahman et al illustrates that the survival benefits fromaggressive resection are lost if the patient develops anew postoperative neurologic deficit as a result15
All the while our understanding of glioma genetics mo-lecular biology and mechanisms of resistance has con-tinued to deepen and evolve borne of thoughtful andsystematic studies using patient-acquired tumor sam-ples Molecular profiles and tumor genetics have proventhemselves to be the best predictors of clinical behaviorand now represent crucial components of the diagnostic
classification scheme of infiltrating gliomas12 With tumortissue at the molecular and genetic level being able to ro-bustly predict patient outcomes accurate tissue diagno-sis has become paramount in the management ofgliomas The role and value of open surgical resection to-ward this end have become clearer as concerns of sam-pling error with biopsy alone led to a number of studiesevaluating the ldquoaccuracyrdquo of stereotactic biopsy proce-dures Jackson et al reported a series of 81 patients whounderwent stereotactic biopsy followed by open surgicalresection The tissue diagnosis was concordant betweenbiopsy and open resection samples in only 51 ofpatients6 Other studies have also demonstrated diagnos-tic concordance between stereotactic biopsy and surgi-cal resection samples in only 57 to 79 ofcases131428 The major limitation of stereotactic biopsyfor infiltrating gliomas likely stems from the significantintratumoral heterogeneity and collectively these studieshighlight the value of open surgical resection in providinga more global representation and understanding of thetumor tissue
The value of extensive resection is perhaps even moreprofound when considering the therapeutic implicationsof such heterogeneity Multiple-site and serial-samplinganalyses have revealed a high degree of both spatial andtemporal heterogeneity within these tumors a conse-quence of serial evolutionary events during tumor growthand progression23 These studies have also led to theconcept of therapy-driven clonal selection and preferen-tial regrowth of resistant cell populations as a potentialmechanism of treatment failure Efforts to expand our un-derstanding of the tremendously complex network ofmutations and biological consequences of chronologicalhierarchy would be greatly facilitated by carefullyplanned thoughtful acquisition of tumor samples duringsurgery
Despite the recent paradigm shift in glioma diagnosticclassification little gains have been made in improvingthe overall prognosis for patients with malignant gliomassince the introduction of concurrent and adjuvant temo-zolomide in 200521 The strategies more recently tested inlarge randomized phase III trials by and large have yieldeddisappointing results while the reasons and mechanismsof treatment failures remain unclear Even so encourag-ing responses have occasionally been seen in varioussubsets of patients and studies exploring the presenceof potential biomarkers have generated intriguing andpromising results in these populations The developmentof the antindashvascular endothelial growth factor monoclonalantibody bevacizumab is one such example Two initialphase II trials showed prolonged progression-free sur-vival in recurrent glioblastoma relative to historical con-trols prompting the US Food and Drug Administration togrant accelerated approval to bevacizumab for recurrentglioblastoma in 2009825 However 2 large randomized tri-als evaluating the addition of bevacizumab to radiationand temozolomide in the newly diagnosed setting failedto show a benefit in overall survival24 and its utility in the
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
106
recurrent setting is now a topic of debate in light of sub-sequent phase III trial results However a post hoc analy-sis of patients enrolled in the AVAglio trial recentlydemonstrated that bevacizumab improved overall sur-vival for those with a proneural subtype tumor18 Just asO6-methylguanine-DNA-methyltransferase (MGMT) pro-moter methylation does for temozolomide the geneticprofile of the tumor could serve as a potential biomarkerof clinical response for bevacizumab as well and valida-tion studies are currently ongoing Such analyses al-though performed post hoc require targeted prospectivecollection of tumor tissue at initial surgery In addition ge-netic profiling of newly diagnosed malignant gliomas willneed to become routine if this approach is to be utilizedwidely Similarly cilengitide an inhibitor of aVb3 andaVb5 integrins with anti-angiogenic properties showedinitial promise in recurrent glioblastoma studies but failedto show any additional benefit in the newly diagnosedsetting20 A subsequent post hoc analysis of the phase IItrial revealed improved progression-free and overall sur-vival in patients with high aVb3 levels in the tumor cells26
However tumor tissues were not systematically collectedand less than half of the patientsrsquo tumor tissues wereavailable for analysis from the phase III trialUnfortunately this drug will most likely not undergo fur-ther development and one cannot help wonder if the out-come would have been different if the enrollment in thephase III trial had been enriched for or restricted to tumorswith high expression of the aVb3 integrin The only trueldquosuccess storyrdquo since the adaptation of radiation andtemozolomide has come from the novel approach of tu-mor treating fields (TTFields) a transcutaneous deliveryof low-intensity intermediate frequency alternating elec-tric fields The multicenter phase III trial EF-14 random-ized patients with supratentorial glioblastoma withoutevidence of tumor progression following standard che-moradiation to receive maintenance treatment withTTFields plus temozolomide or temozolomide alone22
The study was terminated early based on results of aplanned interim analysis demonstrating benefit inprogression-free survival overall survival a secondaryendpoint was also significantly enhanced at this timeDespite the trialrsquos success TTFields has not been univer-sally adopted by the neuro-oncology community andenthusiasm among clinicians and patients remains low27
Experts have raised concerns regarding the study designsuch as its open-label design lacking a sham-treatmentcontrol arm as well as the generalizability of the resultsbased on the unique randomization point occurring afterconcurrent chemoradiation16 Perhaps most significantlya lack of widely understood mechanism of action hasalso been raised as a factor with comparison to othertreatments the preclinical data for TTFields is relativelylacking particularly when applied in conjunction with che-moradiation27 Even during the early phase stages theuse of robust tissue-based analyses exploring the mech-anism of action such as dose response modeling andmultisite tissue biopsies may have mitigated some of
these concerns and led to wider acceptance by the com-munity Bevacizumab and cilengitide clearly benefitedfrom retrospective analyses of human tumor tissue toidentify susceptible treatment populations while the en-thusiasm for TTFields is perhaps in part tempered by thelack thereof Collectively the evolution of these treat-ments underscores the value of extensive targeted tissuesampling in furthering development of new adjunctivetherapies
Open surgical resection of tumors with such targeted tis-sue acquisition for analysis will continue to play a key rolein prospective clinical trial designs Comparison ofpretreatment and posttreatment tissue profiles representsa valuable line of investigation by delving into mecha-nisms of therapeutic action as well as mechanisms oftreatment failures1011 It also provides an opportunity toinvestigate a number of key fundamental steps along anagentrsquos path to clinical success such as does the agentsuccessfully traffic to the tumor if so how much anddoes the agent then actually have its hypothesizedeffects at the biochemical or cellular level Thusearly-phase trials can and should include posttreatmentmolecular endpoints when possible in addition to safetyendpoints Immunotherapy and immune checkpoint inhi-bition represent exciting novel therapeutic approachesfor neuro-oncology particularly based on their success inmetastatic cancers Large phase III trials studying block-ade of the programmed cell death protein (PD)1PDligand 1 axis with monoclonal antibodies for newlydiagnosed and recurrent glioblastoma are under way butinitial reports have been concerning for negative resultsAs in the development of many previous novel agentstissue-based mechanism studies have been largely lack-ing in the preclinical phases However an Alliance-supported trial currently enrolling focuses on a biomarkeras a primary endpoint patients with recurrent glioblas-toma indicated for surgery are randomized to receivepembrolizumab a PD1 inhibitor either before or aftersurgery (NCT02852655) The resected tumor tissue willthen be analyzed for the profile of tumor-infiltratingT cells and comparison will be made between the 2groups This study represents a tremendously valuableopportunity to explore the impact and the potential chal-lenges of checkpoint inhibition for malignant gliomas inthe clinical setting and should the large phase III trialsend up negative this pilot study will be very informative
Advances in imaging biomarkers and molecular charac-terization of gliomas in conjunction with new targetedtherapies will continue to improve and transform themanagement of these tumors Multimodality imaging cannow more accurately reflect ongoing biological processeswithin these tumors such as the presence of oncogenicmutations or cells undergoing malignant transformationNovel biomarkers such as circulating tumor DNA showpromise in detecting early recurrence or monitoring treat-ment response3724 Lastly the new classification schemerevolving around molecular characterization will provide a
Volume 2 Issue 3 The Value of Surgical Resection for Malignant Gliomas in the Modern Era
107
necessary corollary to these novel diagnostic tools Itremains indisputable however that clinical validation ofthese novel diagnostic tools will also require systematiccorrelation with human tumor tissue obtained throughsurgery These samples ideally gathered prospectivelywill provide a pivot upon which we can expand our under-standing of the complex network of oncological pro-cesses driving these tumors
Malignant gliomas are incredibly challenging disease en-tities in many ways due to the inter- and intratumoral het-erogeneity that is a hallmark of them Experience to datehints that future successes in malignant gliomas rest inneuro-oncology entering the era of precision medicinewhere validated biomarkers and targeted personalizedtherapies are seamlessly integrated into the managementparadigm Accordingly systems supporting surgical re-section and patient-specific tumor tissue analysis mustbe built and organized to guide the decision making fortherapy As our overall approach to the management ofmalignant gliomas evolves so should the framework ofsurgical management The clinical benefits of maximalsafe resection are well founded and well reportedHowever the oncological neurosurgeon must now lookbeyond maximal cytoreduction itself and recognize thevalue of thoughtful acquisition and analysis of tumor tis-sue Modern neurosurgeons must consider themselvessurgical neuro-oncologists and engagement and partici-pation of surgeons into clinical trials particularly early-phase trials should be encouraged and valued In turnwe should provide our surgical trainees with the trainingand tools in neuro-oncology to help them participate andcontribute in multidisciplinary collaborative efforts aimingto advance the understanding of brain tumor biology andultimately improve the outlook of our patients
References
1 Lacroix M Abi-Said D Fourney DR Gokaslan ZL et al A multivariateanalysis of 416 patients with glioblastoma multiforme prognosisextent of resection and survival J Neurosurg 2001 95190ndash198
2 Hervey-Jumper SL Berger MS Maximizing safe resection of low-and high-grade glioma J Neurooncol 2016 130269ndash282
3 Sanai N Polley MY McDermott MW Parsa AT Berger MS An ex-tent of resection threshold for newly diagnosed glioblastomas JNeurosurg 2011 1153ndash8
4 Stummer W Pichlmeier U Meinel T et al Fluorescence-guided sur-gery with 5-aminolevulinic acid for resection of malignant glioma arandomised controlled multicentre phase III trial Lancet Oncol2006 7392ndash401
5 Brown TJ Brennan MC Li M et al Association of the extent ofresection with survival in glioblastoma a systematic review andmeta-analysis JAMA Oncol 2016 21460ndash1469
6 Rahman M Abbatematteo J De Leo EK et al The effects of new orworsened postoperative neurological deficits on survival of patientswith glioblastoma J Neurosurg 2017 127123ndash131
7 Louis DN Perry A Reifenberger G et al The 2016 World HealthOrganization Classification of Tumors of the Central NervousSystem a summary Acta Neuropathol 2016 131803ndash820
8 McGirt MJ Bulsara KR Cummings TJ et al Prognostic value ofmagnetic resonance imaging-guided stereotactic biopsy in the
evaluation of recurrent malignant astrocytoma compared with a le-sion due to radiation effect J Neurosurg 2003 9814ndash20
9 Muragaki Y Chernov M Maruyama T et al Low-grade glioma onstereotactic biopsy how often is the diagnosis accurate MinimInvasive Neurosurg 2008 51275ndash279
10 Woodworth G McGirt MJ Samdani A Garonzik I Olivi AWeingart JD Accuracy of frameless and frame-based image-guided stereotactic brain biopsy in the diagnosis of glioma com-parison of biopsy and open resection specimen Neurol Res 200527358ndash362
11 Suzuki H Aoki K Chiba K et al Mutational landscape and clonal ar-chitecture in grade II and III gliomas Nat Genet 2015 47458ndash468
12 Stupp R Mason WP van den Bent MJ et al Radiotherapy plus con-comitant and adjuvant temozolomide for glioblastoma N Engl JMed 2005 352987ndash996
13 Kreisl TN Kim L Moore K et al Phase II trial of single-agent bevaci-zumab followed by bevacizumab plus irinotecan at tumor progres-sion in recurrent glioblastoma J Clin Oncol 2009 27740ndash745
14 Vredenburgh JJ Desjardins A Herndon 2nd JE et al Phase II trial ofbevacizumab and irinotecan in recurrent malignant glioma ClinCancer Res 2007 131253ndash1259
15 Chinot OL Wick W Mason W et al Bevacizumab plusradiotherapy-temozolomide for newly diagnosed glioblastomaN Engl J Med 2014 370709ndash722
16 Gilbert MR Dignam JJ Armstrong TS et al A randomized trial ofbevacizumab for newly diagnosed glioblastoma N Engl J Med2014 370699ndash708
17 Sandmann T Bourgon R Garcia J et al Patients with proneural glio-blastoma may derive overall survival benefit from the addition of bev-acizumab to first-line radiotherapy and temozolomide retrospectiveanalysis of the AVAglio trial J Clin Oncol 2015 332735ndash2744
18 Jackson RJ Fuller GN Abi-Said D et al Limitations of stereotacticbiopsy in the initial management of gliomas Neuro Oncol 20013193ndash200
19 Stupp R Hegi ME Gorlia T et al Cilengitide combined with stan-dard treatment for patients with newly diagnosed glioblastoma withmethylated MGMT promoter (CENTRIC EORTC 26071-22072study) a multicentre randomised open-label phase 3 trial LancetOncol 2014 151100ndash1108
20 Weller M Nabors LB Gorlia T et al Cilengitide in newly diagnosedglioblastoma biomarker expression and outcome Oncotarget2016 715018ndash15032
21 Stupp R Taillibert S Kanner AA et al Maintenance therapy withtumor-treating fields plus temozolomide vs temozolomide alone forglioblastoma a randomized clinical trial JAMA 20153142535ndash2543
22 Wick W TTFields where does all the skepticism come from NeuroOncol 2016 18303ndash305
23 Sampson JH Alternating electric fields for the treatment of glioblas-toma JAMA 2015 3142511ndash2513
24 Lang FF Asher A Prospective clinical trials of brain tumor therapy thecritical role of neurosurgeons J Neurooncol 2004 69151ndash167
25 Lang FF Gilbert MR Puduvalli VK et al Toward better early-phasebrain tumor clinical trials a reappraisal of current methods and pro-posals for future strategies Neuro Oncol 2002 4268ndash277
26 Elkhaled A Jalbert L Constantin A et al Characterization of metab-olites in infiltrating gliomas using ex vivo (1)H high-resolution magicangle spinning spectroscopy NMR Biomed 2014 27578ndash593
27 Jalbert LE Neill E Phillips JJ et al Magnetic resonance analysis ofmalignant transformation in recurrent glioma Neuro Oncol 2016181169ndash1179
28 Touat M Duran-Pena A Alentorn A Lacroix L Massard C Idbaih AEmerging circulating biomarkers in glioblastoma promises andchallenges Expert Rev Mol Diagn 2015 151311ndash1323
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
108
Update on RadiationCombinations in theTreatment of Patientswith Malignant BrainTumors FromRadiosensitizers toImmunotherapy
Debra Nana Yeboa MD1
Erik P Sulman MD PhD123
Departments of 1Radiation Oncology2Translational Molecular Pathology and3Genomic Medicine The University of Texas MDAnderson Cancer Center 1515 Holcombe BlvdUnit 97 Houston Texas USA Tel 713-563-2300dnyeboamdandersonorg andepsulmanmdandersonorg
109
AbstractAdvances in radiosensitizers and immunotherapyhave ushered in a new frontier in brain tumortreatment The brain has often been viewed as asanctuary site due to the bloodndashbrain barrier andthus the 2 primary modalities of therapy includedsurgery and radiation therapy (RT) More recentlysystemic therapies have played a greater role aseither combination therapy radiosensitizers or im-munotherapy Two novel radiosensitizers are beingdeveloped for the treatment of brain metastasesRRx-001 for example is a small molecule thataccelerates the NO2 to NO conversion of deoxyhe-moglobin and the agent 2-dexoyglucose (2-DG) is anonmetabolized glucose analogue that interfereswith ATP formation Poly(ADP-ribose) DNA polymer-ase inhibitors are promising due to their distinctradiobiological effects Veliparib and olaparib areamong the most studied with randomized trialsexploring their use in gliomas and brain metastasesImmunotherapy including immune checkpoint inhib-itors may play a role for both primary gliomas andbrain metastases RT has been shown to enhancethe function of cytotoxic T lymphocytes induce infil-tration of cytotoxic T lymphocytes and enhancefunction Trials are presently exploring use of bothprogrammed cell death protein (PD)1 and PD ligand1 blockade in glioblastoma patients with radiationSimilarly several immunotherapies are being investi-gated with either stereotactic radiosurgery or wholebrain radiation therapy for brain metastases In thisreview the use of radiosensitizers and immunother-apy agents with RT will be discussed broadly
Keywords brain metastases brain tumors gliomasimmunotherapy radiation therapy radiosensitizers
Radiosensitizers andImmunotherapy inBrain TumorsAdvances in radiosensitizers and immunotherapy haveushered in a new frontier to brain tumor treatment Braintumors however are a diverse class sharing only similaranatomic location Both primary brain malignancies andbrain metastasis have widely diverse histologies and mo-lecular phenotypes With the bloodndashbrain barrier thebrain has often been viewed as a sanctuary site and thusthe 2 primary modalities of therapy included surgery andradiation with decreased benefit from systemic agentsdue to lack of brain penetration However more recentlysystemic therapies have played a greater role as eithercombination therapy radiosensitizers or immunother-apy While temozolomide (TMZ) has played a pivotal rolefor glioblastoma (GBM) only a subset of patients benefitfrom the treatment1 The use of alternative systemicagents that may potentiate the effects of radiation ther-apy (RT) is becoming increasingly appealing Similarly forbrain metastases a variety of systemic agents are beingexplored primarily based on histology and immune pro-file In this review the use of radiosensitizers and immu-notherapy agents currently under investigation with RTwill be discussed
RadiosensitizersThe guiding concept of radiation sensitization is to in-crease the biologic effect of radiation such as increasedDNA damage decreased DNA repair decreased hypoxiaor increased G2M cell cycle blockade leading to im-proved tumor control and increased patient survival2
Poly(adenosine diphosphate-ribose) DNA polymerase(PARP) inhibitors are promising radiosensitizers due totheir roles in DNA repair3 PARP inhibitors work againstPARP1 a nuclear enzyme involved in the recruitment ofrepair proteins used in base excision repair and single-strand break repair PARP1 may also play a role in nonho-mologous end-joining4 The primary investigation ofPARP inhibitors has been in potentiating radiation andchemotherapy effects the latter in the context of homolo-gous repair deficient tumors For radiation the primarymechanism of action is inducing damage to nucleotidesleading to single-strand and double-strand breaks ThusPARP inhibitors in combination with radiation have an ap-pealing mechanism to inhibit or delay DNA repair andlikely convert more single-strand breaks to double-strandbreaks4
While several PARP inhibitors are currently being evalu-ated in a variety of tumors including talazoparib and nira-parib veliparib and olaparib are among the most studiedand there are randomized trials exploring their use in
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
110
gliomas The US National Cancer Institute (NCI)ndashfundedAlliance for Clinical Trials in Oncology (Alliance) A071102is a randomized phase IIIII trial evaluating the use ofveliparib in combination with TMZ in the adjuvant settingin patients with GBM tumors exhibiting hypermethylationof the O6 methylguanine DNA methyltransferase (MGMT)gene promoter Preclinical data supporting this trial sug-gested that only patients with MGMT methylated tumorswould benefit from the combination a group of patientsfor whom TMZ concurrent with radiation might be mostbeneficial5 A phase I trial performed by the NCI-fundedAmerican Brain Tumor Consortium attempted to combineveliparib with radiation and TMZ but failed to identify asuitable recommended phase II dose due to significanthemotoxicity6 Thus attempts to combine radiation withveliparib have focused on patients least likely to benefitfrom TMZ namely with MGMT unmethylated tumors forwhom TMZ could be withheld The Australian VeliparibRT and TMZ trial in newly diagnosed unmethylatedMGMT glioblastoma (VERTU) is a single-arm study inwhich patients receive RT with veliparib followed by adju-vant TMZ and veliparib4
An ongoing novel approach to radiosensitize gliomasinvolves a combination with an agent that interferes withan essential metabolic process 2-Dexoyglucose (2-DG)is a nonmetabolized glucose analogue that acts as acompetitive inhibitor of glycolysis It is transported acrossthe bloodndashbrain barrier by the glucose transporter GLUT-1 and thus has good penetration into the CNSIntracellularly it is trapped and accumulates in cells simi-lar to the mechanism of 18-fluorodeoxyglucose 2-DG isphosphorylated by glycolytic enzymes and the
phosphorylated 2-DG (2-deoxyglucose-P) is trapped in-tracellularly Inhibition of hexokinase activity by 2-DGinterferes with ATP formation and results in tumor celldeath7 While it has positive attributes by selectively tar-geting metabolically active tumor cells 2-DG has alsobeen associated with Q-T prolongation The currentphase III trial in gliomas is assessing the toxicity and tol-erability of 2-DG with hypofractionated radiation of 5 Gyas a radiosensitizer7
Two novel radiosensitizers are being developed for thetreatment of brain metastases First RRx-001 is a smallmolecule initially designed by the aerospace industry Itworks in part as a radiosensitizer by increasing blood flowand thus oxygenation of tumors through nitric oxideRRx-001 which binds to hemoglobin accelerates theNO2 to NO conversion of deoxyhemoglobin It workslocally under hypoxic conditions and subsequentlythe radiosensitive effects through nitric oxide are invasodilation and inhibiting DNA repair enzymes8 Nitricoxide is relatively benign The higher levels of oxidativestress with H2O2 and superoxide in tumors in comparisonto normal tissues result in the preferential generation ofreactive peroxynitrite in the presence of higher nitric oxidelevels7 This accounts for the increased specificity anddecreased toxicity with RRx-001 The dose limiting toxic-ity in a phase I trial of 25 patients treated with eitherweekly or biweekly infusions was infusional pain relatedto the release of NO at the site of injection7 Outside ofpreclinical models 2 clinical reports examining wholebrain radiation therapy (WBRT) with RRx-001 reported anintracranial response A patient with melanoma and 2hemorrhagic edematous lesions of 26 cm and 33 cm
Table 1 Clinical trials involving immunotherapy and radiation therapy1213
Clinical Trials Number Phase Disease Type Treatment Groups
NCT02667587 II Newly diagnosed GBMMGMT-methylated
Nivolumabthorn TMZthorn RT vs placebothornTMZ thorn RT
NCT02617589 III Newly diagnosed GBM Nivolumabthorn RT vs TMZthorn RTNCT02336165 II Newly diagnosed unmethylated
MGMT recurrent glioblastomaMEDI4736thorn standard RT vs MEDI4736 thorn
bevacizumabNCT02530502 III Newly diagnosed GBM RTthorn TMZthorn pembrolizumab TMZthorn
pembrolizumabNCT02313272 I Recurrent glioma Hypofractionated stereotactic radiationthorn
pembrolizumab thorn bevacizumabNCT02696993 III Brain metastases Nivolumabthorn SRS nivolumabthornWBRT
nivolumabthorn ipilimumab thorn SRS nivolu-mabthorn ipilimumab thornWBRT
NCT02115139 II Melanoma brain metastases Ipilimumab thornWBRTNCT02097732 II Melanoma brain metastases Ipilimumab SRS ipilimumab vs SRS
ipilimumabNCT01703507 I Melanoma brain metastases Ipilimumab thornWBRT vs ipilimumab thorn SRSNCT02107755 II Melanoma brain metastases Ipilimumab thorn SRSNCT02858869 pilot Melanoma and NSCLC Pembrolizumabthorn SRSNCT01950195 I Melanoma brain metastases Ipilimumab thorn SRSNCT02662725 II Melanoma brain metastases Ipilimumab thorn SRS
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
111
after a single intravenous dose of RRx-001 of 5 mgm2 4days before WBRT resulted in symptomatic improvementwithin 48 hours By 4 months after radiation there was areduction in size in the largest dimension down to 10 cmand 23 cm of the respective lesions A second report of amelanoma patient with at least 18 lesions after receivingRRx-001 of 5 mgm2 4 days before WBRT as well astwice weekly doses during the 2 weeks of radiation alsoshowed response The patient at 4 months had disap-pearance of 13 of 18 lesions with shrinkage of theremaining 5 lesions8 Presently BRAINSTORM is a phaseIII dose escalation trial of RRx-001 designed to be ad-ministered twice weekly for 2 weeks with WBRT (30 Gy in10 fractions) with the option for weekly maintenance8
Veliparib has also been evaluated in the setting of brainmetastases It was tested in a global randomized con-trolled trial with WBRT Veliparib is orally bioavailable andcrosses the bloodndashbrain barrier It was first examined in amultihistology phase I trial in patients with nonndashsmall celllung cancer (NSCLC) breast cancer melanoma and re-nal and colorectal cancers among others The study of81 patients tested dose tolerance of veliparib from 10 to300 mg orally twice a day with WBRT to 30 Gy in 10 frac-tions or 375 Gy in 15 fractions9 The phase I trial dose es-calation portion did not reach the predefined criteria forthe maximum tolerated dose but there was amplificationof the adverse effects of nausea and vomiting among thehighest dose cohort of 300 mg bid9 The adverse eventprofile at 200 mg bid was similar to that of WBRT aloneDoses of veliparib from 20 to 200 mg bid demonstratesimilar antitumor activity and other studies in preclinicalmodels found that 50 mg daily demonstrated significantreduction in poly(ADP-ribose) in peripheral blood mono-nuclear cells and tumor tissue while also effectivelycrossing the bloodndashbrain barrier Thus the subsequentphase II trial examined 50 mg with WBRT9 In order to as-sess a more homogeneous cohort the phase III globalrandomized trial studied only NSCLC at the 2 doses of50 mg and 200 mg twice daily versus placebo twice a daywith WBRT10 The primary endpoint was overall survivalIn 307 patients in a 111 randomization of 50 mg bid200 mg bid or placebo twice daily the study found nosignificant differences in overall survival among the differ-ent groups10 The majority of patients across the treat-ment groups had a graded prognostic assessment (GPA)score of25 and a Karnofsky performance status ofgt80 The median overall survival was 185 days forpatients receiving placebo and 209 days for those receiv-ing veliparib without any statistically significant differ-ence These results were similar to the disease-specificestimate of median survival for the disease-specific GPAof NSCLC patients with brain metastases10
Several other radiosensitizers have failed to improve overradiation alone in a number of trials These have includedtrials with WBRT including motexafin gadolinium efap-roxyn bortozemib thalidomide teniposide topotecanpaclitaxel and cisplatin7 Of note other PARP inhibitorsalso being assessed include talazoparib and niraparib4
which may yield positive results The use of valproic acid(VPA) as a histone deacetylase inhibitor has also beenconsidered to have radiosensitizing potential in additionto its anti-epileptic drug properties11 While studies havereported that patients with GBM receiving an anti-epilep-tic agent may have higher overall survival than those re-ceiving standard chemoradiation therapy alone thebenefit remains controversial Retrospective analysissuggested that patients taking VPA specifically had bettersurvival in comparison to other anti-epileptic drugs Alsoa recent prospective phase II trial was performed in 37patients with GBM receiving VPA 25 mgkg concurrentlywith TMZ chemoradiation and reported a median survivalof 296 months While controversial further data andinvestigation are needed into this and other agents thatmay potentiate RT
Immunotherapy and radiationImmune checkpoint inhibitors lead to activation of T cellswhich may traffic across the bloodndashbrain barrier to inter-act with tumor Primary brain tumors may evade the im-mune system through upregulation of immunecheckpoints and possible immunosuppression12
Monoclonal antibodies promote immune-mediated anti-tumor activity by inhibiting the immune functionndashmediated cytotoxic T-lymphocyte associated protein 4(CTLA-4) and programmed cell death protein 1 (PD-1)receptors PD protein ligand (PD-L1) is upregulated inGBM through oncogenic signaling possibly throughphosphatase and tensin homolog loss and interleukin-10signaling1314 RT has also been shown to enhance thefunction of cytotoxic T lymphocytes RT may induce aninfiltration of cytotoxic T lymphocytes and enhance theirfunction It may also induce antindashCTLA-4 agents inhibitingT-cell function and increasing the CD8thorn T cellregulatoryT cell ratio in cases of melanoma15 Thus PD-1 and PD-L1 blockers may have a further role in CNS managementwith the use of radiation
In preclinical models radiation has been examined withimmunotherapy that included among other mechanismsvaccination PD-1 blockade and CTLA-4 blockade Inmice radiation plus a vaccination of irradiated gliomacells was associated with increased survival of 40 to80 compared with 0 to 10 for other groups stud-ied16 A benefit of PD-1 blockade with stereotactic radio-surgery (SRS) specifically has also been shown in amouse model In comparison to mice treated with radia-tion antindashPD-1 therapy or a combination only those re-ceiving combination therapy had a higher percentagesurvival alive beyond 180 days after treatment17 Othermouse carcinoma models have identified response withanti-CTLA antibody and fractionated radiation therapy18
CD137 activation CTLA-4 blockade and focal radiationtherapy have been examined in an immunocompetent in-tracranial GBM model Mice treated with triple combina-tion therapy had 50 greater survival19 In other murine
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
112
models the use of antindashPD-1 and antindashCTLA-4 agentsshowed improved survival and increased tumor infiltratingleukocyte populations compared with single modalitywith concurrent radiation16 There are conflicting data re-garding timing or sequencing of therapy with some ani-mal models showing no difference in tumor response inrelation to timing of RT and delivery of immunotherapy18
For instance in one animal model CTLA-4 blockade de-livered simultaneously with radiation or delivered a coupleof days after showed no difference in survival among themice19
Increased PD-1 expression in circulating monocytes hasbeen identified as a biomarker for tumor-induced immu-nosuppression and may serve as a prognostic factor forpotentially worse survival outcomes in clinic13 In onestudy GBM patients with lower PD-L1 expression hadhigher median overall survival than those with higher PD-L1 expression suggesting that lower expression may beassociated with less immunosuppression and more im-mune activity against the tumor glioma20 RT with immunecheckpoint blockade is being investigated to assess if theaddition of PD-1 and PD-L1 inhibitors may improve theoutcomes or toxicity profile of standard therapy For in-stance a multi-institutional trial opened as a phase III willevaluate outcomes in GBM receiving radiation and pem-brolizumab with TMZ (NCT02530502) Next durvalumabor MEDI4736 a PD-L1 inhibitor is being examined forunmethylated MGMT GBMs with standard radiotherapy(NCT02336165)12 The impact of checkpoint inhibitorsduring adjuvant treatment of GBM is currently beingevaluated in the NCI-funded NRG-BN002 trial(NCT02311920) which will evaluate the antindashCTLA-4antibody ipilimumab alone or in combination with theantindashPD-1 antibody nivolumab for patients with newlydiagnosed GBM
Brain metastases have clonal populations of cells differ-ent from the rest of the brain and a unique microenviron-ment that may influence immunotherapy There may bemore immune infiltrates in metastases than in primarybrain tumors21 PD-L1 expression in brain metastasesvaries by histology In a series evaluating PD-L1 expres-sion in various tumors including melanoma NSCLCbreast renal colorectal and small cell less than 10showed significant expression22 There was greatest ex-pression among NSCLC and melanoma with a correla-tion between PD-L1 expression and tumor infiltratinglymphocytes22 Institutional series have examined thecombination of radiation and immune checkpoint block-ade In another study specific to melanoma brain metas-tases PD-L1 expression was found in over 50 of thecases and among those cases over 40 expressedPD-L1 in more than 5 of tumor cells23 The largest bodyof data for use of PD-L1 with radiation is for melanomaand NSCLC
Ipilimumab is a human monoclonal antibody that blocksCTLA-4 and allows for T-cell activation and proliferationto enhance the immune response to cancer In a
retrospective review of 70 patients with brain metastasestreated with SRS or WBRT the 33 patients receiving im-munotherapy had a median survival of 183 months incomparison to the 37 patients who did not receive ipili-mumab with a median survival of 53 months While therewere limited data among the cohort to evaluate sequenc-ing of therapy among 10 evaluable patients 40 whoreceived ipilimumab prior to RT had a partial response incomparison to only 10 among the cohort of 22 evalu-able patients who did not receive ipilimumab therapy atall with radiation24 Another retrospective institutionalstudy of 77 patients in which 37 received ipilimumabfound that patients treated with SRS and ipilimumab hada median survival of 213 months versus 49 months forthose not receiving ipilimumab Most interestingly theyidentified that the correlation remained significant evenafter adjusting for additional factors such as performancestatus Secondly there was not an increased need for useof salvage WBRT25
The sequencing of radiotherapy and immune checkpointinhibitors is of interest In a study of patients with brainmetastases the one-year survival for patients receivingSRS before ipilimumab was greater at 65 in contrast to56 for those receiving it concurrently and 40 for thosereceiving it after SRS26 Similarly another study of 75patients with 566 brain metastases showed greater tu-mor lesion response at 6 months from SRS for patientsreceiving ipilimumab nivolumab or pembrolizumabwithin 4 weeks of their SRS27 Those receiving concurrenttherapy had by 6 months a decrease of 949 in compar-ison to 662 for those not receiving checkpoint inhibi-tors within 4 weeks Prospective clinical trials areinvestigating different combinations of RT with immunecheckpoint blockers in this setting For instance new tri-als are currently evaluating intracranial tumor control at 6months and the timing of immune therapy or immunecheckpoint inhibitors in relation to SRS28
Vaccines are also being developed for primary braintumors showing some evidence for their use Vaccinesdeveloped from dendritic cells and tumor lysate with tu-mor antigens such as the epidermal growth factor recep-tor variant III vaccine have shown promise29 Forinstance in a placebo controlled phase II trial of ICT-107a vaccine composed on autologous dendritic cells andtumor antigens progression-free survival was increasedby 2 months for those receiving the vaccine30 Radiationmay assist in serving as a primer for the immunogeniceffects by facilitating tumor antigen uptake by dendriticcells and cross presentation on major histocompatibilitycomplex I Thus RT may assist in the tumor-specific cy-totoxic T lymphocytes associated with the immunemechanism
In conclusion although there may be challenges to com-bining and sequencing brain tumors radiosensitizersand immunotherapy the opportunities and potential fornovel applications are promising For brain tumors brainmetastases are typically underrepresented in trials
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
113
despite being among the most common intracraniallesions Despite their large population patients with brainmetastases are often excluded from clinical trials withnovel agents due to concerns regarding confounding out-comes and tolerability12 Primary gliomas also offer anovel frontier for the use of immunotherapy to standardadjuvant chemotherapy and radiation particularly forpatients with GBM less likely to respond to TMZ such aswith unmethylated MGMT As studies work to define therole of RT and radiosensitizers and immunotherapy fur-ther analysis is needed to assess the timing of RT andthese treatments
References
1 Stupp R Hegi ME Mason WP et al Effects of radiotherapy withconcomitant and adjuvant temozolomide versus radiotherapy aloneon survival in glioblastoma in a randomised phase III study 5-yearanalysis of the EORTC-NCIC trial Lancet Oncol 2009 10459ndash466
2 Lawrence TS Blackstock AW McGinn C The mechanism of actionof radiosensitization of conventional chemotherapeutic agentsSemin Radiat Oncol 2003 1313ndash21
3 Lesueur P Chevalier F Austry JB et al Poly-(ADP-ribose)-polymer-ase inhibitors as radiosensitizers a systematic review of pre-clinicaland clinical human studies Oncotarget 2017 8(40)69105ndash69124
4 Lester A Rapkins R Nixdorf S Khasraw M McDonald KCombining PARP inhibitors with radiation therapy for the treatmentof glioblastoma is PTEN predictive of response Clin Transl Oncol2017 19273ndash278
5 Gupta SK Kizilbash SH Carlson BL et al Delineation of MGMT hyper-methylation as a biomarker for veliparib-mediated temozolomide-sensi-tizing therapy of glioblastoma J Natl Cancer Inst 2016 108
6 Kleinberg LR Blakeley J Mikkelsen T et al An American BrainTumor Consortium (ABTC) phase 1 trial of veliparib (ABT-888)temozolomide (TMZ) and concurrent radiation therapy (RT) fornewly diagnosed glioblastoma multiforme (GBM) need for modifica-tion to approach for combining these therapies InternationalJ Radiat Oncol Biol Phys 2012 84S7ndashS8
7 Oronsky BT A Review of two promising radiosensitizers in brainmetastases Rrx-001 and 2-deoxyglucose In NC Oronsky edJ Cancer Sci Ther 2015 pp 137ndash141
8 Kim MM Parmar H Cao Y et al Concurrent whole brain radiother-apy and RRx-001 for melanoma brain metastases Neuro Onc2016 18455ndash456
9 Mehta MP Wang D Wang F et al Veliparib in combination withwhole brain radiation therapy in patients with brain metastasesresults of a phase 1 study J Neurooncol 2015 122409ndash417
10 Chabot P Hsia TC Ryu JS et al Veliparib in combination withwhole-brain radiation therapy for patients with brain metastasesfrom non-small cell lung cancer results of a randomized globalplacebo-controlled study J Neurooncol 2017 131105ndash115
11 Ochiai S Nomoto Y Yamashita Y et al Roles of valproic acid inimproving radiation therapy for glioblastoma a review of literaturefocusing on clinical evidence Asian Pac J Cancer Prev 201617463ndash466
12 Tan AC Heimberger AB Menzies AM Pavlakis N Khasraw MImmune checkpoint inhibitors for brain metastases Curr Oncol Rep2017 1938
13 DrsquoSouza NM Fang P Logan J Yang J Jiang W Li JCombining radiation therapy with immune checkpoint blockade
for central nervous system malignancies Frontiers Oncol 20166212
14 Parsa AT Waldron JS Panner A et al Loss of tumor suppressorPTEN function increases B7-H1 expression and immunoresistancein glioma Nat Med 2007 1384ndash88
15 Binder DC Davis AA Wainwright DA Immunotherapy for cancer inthe central nervous system current and future directionsOncoimmunology 2016 5e1082027
16 Newcomb EW Demaria S Lukyanov Y et al The combination ofionizing radiation and peripheral vaccination produces long-termsurvival of mice bearing established invasive GL261 gliomas ClinCancer Res 2006 124730ndash4737
17 Zeng J See AP Phallen J et al Anti-PD-1 blockade and stereotac-tic radiation produce long-term survival in mice with intracranial glio-mas Int J Radiat Oncol Biol Phys 2013 86343ndash349
18 Chow KK Hara W Lim M Li G Combining immunotherapy withradiation for the treatment of glioblastoma J Neurooncol2015123459ndash464
19 Belcaid Z Phallen JA Zeng J et al Focal radiation therapy com-bined with 4-1BB activation and CTLA-4 blockade yields long-termsurvival and a protective antigen-specific memory response in amurine glioma model PLoS One 2014 9e101764
20 Topalian SL Hodi FS Brahmer JR et al Safety activity and im-mune correlates of anti-PD-1 antibody in cancer N Engl J Med2012 3662443ndash2454
21 Bienkowski M Preusser M Prognostic role of tumour-infiltrating in-flammatory cells in brain tumours literature review Curr OpinNeurol 2015 28647ndash658
22 Harter PN Bernatz S Scholz A et al Distribution and prognostic rel-evance of tumor-infiltrating lymphocytes (TILs) and PD-1PD-L1 im-mune checkpoints in human brain metastases Oncotarget 2015640836ndash40849
23 Berghoff AS Ricken G Widhalm G et al Tumour-infiltrating lym-phocytes and expression of programmed death ligand 1 (PD-L1) inmelanoma brain metastases Histopathology 2015 66289ndash299
24 Silk AW Bassetti MF West BT Tsien CI Lao CD Ipilimumab and ra-diation therapy for melanoma brain metastases Cancer Med 20132899ndash906
25 Knisely JP Yu JB Flanigan J Sznol M Kluger HM Chiang VLRadiosurgery for melanoma brain metastases in the ipilimumab eraand the possibility of longer survival J Neurosurg 2012117227ndash233
26 Kiess AP Wolchok JD Barker CA et al Stereotactic radiosurgeryfor melanoma brain metastases in patients receiving ipilimumabsafety profile and efficacy of combined treatment Int J Radiat OncolBiol Phys 2015 92368ndash375
27 Qian JM Yu JB Kluger HM Chiang VL Timing and type of immunecheckpoint therapy affect the early radiographic response of mela-noma brain metastases to stereotactic radiosurgery Cancer 20161223051ndash3058
28 Silk AW Cao Y Gomez-Hassan D et al A randomized phase IIstudy of ipilimumab induction in patients with melanoma brain me-tastases receiving stereotactic radiosurgery J Clin Oncol 2015 33TPS9079ndashTPS9079
29 Neagu MR Reardon DA An Update on the role of immunotherapyand vaccine strategies for primary brain tumors Curr TreatOptions Oncol 2015 1654
30 Wen PY Reardon DA Phuphanich S et al A randomized double-blind placebo-controlled phase 2 trial of dendritic cell (DC) vaccina-tion with ICT-107 in newly diagnosed glioblastoma (GBM) patientsJ Clin Oncol 2014 322005ndash2005
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
114
British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

Brain TumorEpigeneticsFrom Researchto ClinicalPractice
Silvia MarinoBlizard Institute Barts and The London School ofMedicine and Dentistry Queen Mary University ofLondon 4 Newark Street E12AT London UK
101
IntroductionEpigenetics is defined as the study of heritable changesin gene expression that are not caused by alterations inDNA sequences1 The phenotypic difference between acaterpillar and a butterfly for example is due to epige-netic regulation of gene expression in the same animalwith the same DNA I particularly like this example to ex-plain the meaning of the term epigenetics as it impres-sively demonstrates how powerful these mechanisms arein controlling phenotypic changes Epigenetic changesare reversible and include the key processes of DNAmethylation histone modifications and noncoding RNA-associated gene silencing (recently reviewed2) known toplay an essential role during the embryonic and postnataldevelopment of an organism and in tissue homeostasis2
Disruptions of epigenetic processes can induce changesin gene function which together with genetic changescan lead to the neoplastic transformation of a normal cell(recently reviewed)3
Recent technological advances have significantly con-tributed to the tremendous progress in understandinghow these epigenetic modifications are regulated in nor-mal cells and deregulated in cancer cells For examplethis knowledge has enabled the translation into better di-agnostic algorithms for tumor classification prognostica-tion and risk assessment Importantly we are nowentering a time when novel therapies targeting thesederegulated epigenetic mechanisms are being devel-oped with some of them showing very promising effectsin preclinical models
It is beyond the scope of this article to comprehensivelyreview mechanisms of epigenetic regulation of gene ex-pression and their deregulation in brain tumors excellentrecent reviews are available to the readers on thesesubjects2ndash5 Here I will discuss a few examples of recentepigenetic discoveries which have informed the develop-ment of novel diagnostic and prognostic tools or led tosuccessful preclinical testing of new epigenetic drugs inexperimental models
Epigenetic Profiles inthe MolecularClassification of BrainTumorsGlioma One of the first examples of an epigenetic changeinforming the design of an assay for diagnostic screeningto corroborate a therapeutic decision is the assessmentof methylation of the MGMT promoter in malignantgliomas6 MGMT (O6-methylguanine DNA methyltransfer-ase) is a key enzyme in the DNA repair network which
removes the mutagenic and cytotoxic adducts from O6
guanine in DNA the preferred point of attack of alkylatingchemotherapeutic agents (ie BCNU temozolomide etc)Hypermethylation of cytosine-phosphate-guanine (CpG)islands located in the promoter region of MGMT is pri-marily responsible for the loss of MGMT function in manytumor types hence leading to an increased sensitivity tothe killing effects of alkylating drugs used in chemo-therapy6 This test is widely used in clinical practice topredict response to temozolomide the alkylating drug ofchoice in high-grade gliomas although it should bestressed that there is still no consensus as to which testmethod to use which CpG sites to assess and what themethylation cutoff should be
Ependymoma Until very recently these tumors havebeen subclassified and graded on the basis of histologi-cal features into low and high grade In 2015 a molecularclassification based on DNA methylation profiling hasbeen proposed which defines 9 molecular subgroups 3for each anatomical location of these tumors (supratento-rial posterior fossa and spinal cord)7 In the supratento-rial location ependymomas with the fusion geneC11ORF95RELA (ST-EPN-RELA) have a poor prognosisand in the posterior fossa it is the ependymoma groupEPN-A that is characterized by a poor prognosis7 Allother ependymomas show a comparatively goodprognosis7 Although not yet included in the World HealthOrganization (WHO) 2016 classification a recent consen-sus paper has recommended that this classification beused for enrollment in prospective clinical trials8 and it isexpected to contribute to informing decisions onmolecular-based treatments as they become available
Medulloblastoma (MB) International consensusrecognizes 4 medulloblastoma molecular subgroupsWNT (MBWNT) SHH (MBSHH) Group 3 (MBGrp3) andGroup 4 (MBGrp4) each defined by their characteristicDNA methylation and genome-wide transcriptomicprofiles9 Recently the heterogeneity within these sub-groups has been reduced by 2 independent studieswhich have defined additional subtypes Schwalbe andcolleagues10 have suggested to split MBSHH into 2 age-dependent subtypes corresponding to ldquoinfantrdquo (lt43 y)and ldquochildhoodrdquo patients (43 y) and MBGrp3 andMBGrp4 into further high-risk and low-risk subtypes whilethe MBWNT group remains unchanged10 Interestingly thelow-risk subtypes were defined primarily by hypermethy-lation in comparison to normal cerebellum whereas thehigh-risk subtypes were defined by relativehypomethylation10 Cavalli and coauthors11 used integra-tive clustering of DNA methylation and gene expressiondatasets from 763 patients to split the original 4 sub-groups into 12 subtypes MBSHH is split into 4 subtypes(abc d) MBWNT into 2 subtypes (ab) MBGrp3 andMBGrp4into 3 subtypes each (abc)11 The subtypes iden-tified in these 2 studies overlap considerably and themain differences seem to be related to the inclusion ofadult MB patients in the Cavalli study Importantly MBsubgroups and their subtypes identified by their
Brain Tumor Epigenetics From Research to Clinical Practice Volume 2 Issue 3
102
epigenetic and related transcriptional profiles1011 havedistinct genetic and clinicopathological features1011 andtheir implementation for patient stratification for betterprognostication and enrollment into subgroupsubtype-directed therapies in the context of clinical trials will be astep change in the treatment of MB patients
All CNS tumors A classification tool for brain tumorsbased on genome-wide DNA methylation patterns and arandom forest-based machine learning approach hasbeen developed and extensively tested by the GermanCancer Research Center (wwwmolecularneuropathologyorg) This resource is available online and has provento be a valuable tool to improve brain tumor diagnosticsThis approach has facilitated the identification of com-mon druggable molecular pathway alterations across var-ious histological tumor entities thus allowing patients toenter the most appropriate clinical trials and in somecases be offered molecularly matched therapies As anexample DNA methylation profiles allow precise identifi-cation of cases with mitogen-activated protein kinase(MAPK) activation which is a feature of tumors withBRAF V600E mutation1213 which can span various tradi-tional histological entities such as pilocytic astrocytomaspleomorphic xanthoastrocytomas ganglioglioma andsubependymal giant cell astrocytomas to predict re-sponse to specific inhibitors interrupting the BRAFMEKcomponent of the MAP kinase pathway14
Novel TherapeuticApproaches TargetingEpigeneticDeregulationDiffuse intrinsic pontine glioma (DIPG) is a highlyaggressive pediatric tumor located in the brainstem andcharacterized by a rapid and diffusely infiltrative patternof growth These tumors cannot be treated surgicallybecause of their location and infiltrative nature15
Radiation therapy is the standard treatment although itprovides only temporary symptom relief with no overallsurvival benefits and conventional chemotherapy drugsare ineffective15
Mutations in histone H3 variants occur in more than 80of DIPG and result in a lysine-to-methionine substitution(H3K27M)16 17 H3K27M has been shown to inhibitpolycomb repressive complex 2 (PRC2) by binding to itscatalytic subunit EZH2 and reducing the methylation ofH3 at lysine 27 (H3K27me) at selected target loci18 Theresidual PRC2 activity is required to maintain DIPGproliferative potential by repressing neuronaldifferentiation in patient-derived cell lines and in agenetically engineered mouse model1920 Importantlysmall-molecule EZH2 inhibitors abolish tumor cell growth
in these models raising the possibility that inhibitionof EZH2 could be a novel therapeutic strategy for thesetumors19
An independent study showed that H3K27M associateswith increased H3K27 acetylation (H3K27ac) and that themajority of the heterotypic H3K27M-K27ac nucleosomesco-localize with bromodomain proteins at the loci of ac-tively transcribed genes20 The authors have shown thatblocking the recruitment of bromodomain proteins by het-erotypic H3K27M-K27ac nucleosomes in DIPG with bro-modomain and extraterminal domain family inhibitorsefficiently inhibited tumor progression thus identifying thisclass of compounds as potential therapeutics in DIPG20
These important advances in understanding the underly-ing biology of DIPG have led to the identification of novelepigenetic therapeutic approaches which are very effec-tive at the preclinical level and if confirmed in transla-tional studies could change the way we treat thesetumors in the near future
Conclusion and outlookThese are exciting and challenging times for theneuro-oncology community Exciting because there isgrowing expectation in the field that new discoveriessuch as those discussed in this article can soon translateinto new and more effective therapeutic approachesChallenging because it is clear that new skill sets are re-quired to effectively apply them to benefit patients
The clinical training in many neuro-oncology specialtieswill have to take into account the additional knowledgeand skills needed in the field and offer education incomplementary disciplines such as next-generationsequencing technologies integrated with interpretativedata analysis as well as molecular biology for the designof biologically informed assays and tools The require-ment for these new highly specialized skills also needs tobe reflected in the composition of the clinical teamswhere bioinformatics expertise will play an increasinglyimportant role for the integration of multimodal data inpatient care
References
1 Waddington CH Canalization of development and the inheritance ofacquired characters Nature 1942150563ndash565
2 Allis CD Jenuwein T The molecular hallmarks of epigenetic controlNat Rev Genet 201617487ndash500
3 Flavahan WA Gaskell E Bernstein BE Epigenetic plasticity and thehallmarks of cancer Science (New York NY 2017357
4 Edwards JR Yarychkivska O Boulard M Bestor TH DNA methyla-tion and DNA methyltransferases Epigenetics amp chromatin20171023
5 Filbin MG Suva ML Gliomas genomics and epigenomics arriving atthe start and knowing it for the first time Annual Rev Pathol201611497ndash521
6 Hegi ME et al MGMT gene silencing and benefit from temozolomidein glioblastoma N Engl J Med 2005352997ndash1003
Volume 2 Issue 3 Brain Tumor Epigenetics From Research to Clinical Practice
103
7 Pajtler KW et al Molecular Classification of Ependymal Tumorsacross All CNS Compartments Histopathological Grades and AgeGroups Cancer Cell 201527728ndash743
8 Pajtler KW et al The current consensus on the clinical managementof intracranial ependymoma and its distinct molecular variants ActaNeuropathol 20171335ndash12
9 Taylor MD et al Molecular subgroups of medulloblastoma the cur-rent consensus Acta Neuropathol 2012123465ndash472
10 Schwalbe EC et al Novel molecular subgroups for clinical classifi-cation and outcome prediction in childhood medulloblastoma a co-hort study Lancet Oncol 201718958ndash971
11 Cavalli FMG et al Intertumoral Heterogeneity withinMedulloblastoma Subgroups Cancer Cell 201731737ndash754 e736
12 Schindler G et al Analysis of BRAF V600E mutation in 1320 nervoussystem tumors reveals high mutation frequencies in pleomorphicxanthoastrocytoma ganglioglioma and extra-cerebellar pilocytic as-trocytoma Acta Neuropathol 2011121397ndash405
13 Tanaka S et al Epithelioid glioblastoma arising from pleomorphicxanthoastrocytoma with the BRAF V600E mutation Brain TumorPathol 201431172ndash176
14 Banerjee A et al A phase I trial of the MEK inhibitor selumetinib(AZD6244) in pediatric patients with recurrent or refractory low-grade glioma a Pediatric Brain Tumor Consortium (PBTC) studyNeuro Oncol 2017191135ndash1144
15 Hargrave D Bartels U Bouffet E Diffuse brainstem glioma in chil-dren critical review of clinical trials Lancet Oncol 20067241ndash248
16 Schwartzentruber J et al Driver mutations in histone H33 and chro-matin remodelling genes in paediatric glioblastoma Nature2012482226ndash231
17 Wu G et al Somatic histone H3 alterations in pediatric diffuse in-trinsic pontine gliomas and non-brainstem glioblastomas Naturegenetics 201244251ndash253
18 Lewis PW et al Inhibition of PRC2 activity by a gain-of-function H3mutation found in pediatric glioblastoma Science (New York NY2013340857ndash861
19 Mohammad F et al EZH2 is a potential therapeutic target forH3K27M-mutant pediatric gliomas Nature Med 201723483ndash492
20 Piunti A et al Therapeutic targeting of polycomb and BET bromodo-main proteins in diffuse intrinsic pontine gliomas Nature Med201723493ndash500
Brain Tumor Epigenetics From Research to Clinical Practice Volume 2 Issue 3
104
The Value of SurgicalResection for MalignantGliomas in the ModernEra Beyond Extent ofResection
Stephen G Bowden MDSeunggu Jude Han MDDepartment of Neurological Surgery OregonHealth and Sciences University 3303 SW BondAve Center for Health and Healing CH8NPortland OR 97239 Telephone 503-494-4314Fax 503-346-6810 hanseohsuedu
105
Malignant gliomas are among the most difficult oncologi-cal entities to treat Despite aggressive treatment prog-nosis remains poor and recurrence and treatmentfailures seem inevitable The current standard-of-caretherapy includes maximal safe surgical resection fol-lowed by concurrent and adjuvant chemoradiotherapyHistorically surgical resection has conferred greater sur-vival benefit to these patients than adjuvant therapiespresumably through the cornerstone principle of cytore-duction However the extent of surgical resection is fre-quently limited by nearby eloquent tissue and risks to keyneurological functions In addition the value of such ag-gressive approaches has been questioned in light of thewidespread infiltration of glioma cells Meanwhile our un-derstanding of glioma biology continues to advance rap-idly fueled in large part by the acquisition of tumor tissueduring surgery Thus the exact role and value of surgeryparticularly in comparing the clinical benefits of maximalextent of resection (EOR) with the biomedical benefits oftissue provision has been a topic of great interest anddebate in both the neuro-oncological and neurosurgicalcommunities
EOR patient age tumor histology performance statusand molecular markers have been widely accepted assignificant predictors of patient outcomes in malignantglioma9 In the past 2 decades many large retrospectivecohort studies have demonstrated improvements in sur-vival with increasing EOR5917 Due to ethical considera-tions evidence from a randomized prospective studysupporting the clinical benefit of aggressive resectionsdoes not exist and likely never will Instead the closestthing to such evidence in malignant glioma comes fromthe randomized phase III trial comparing surgical resec-tions with or without the use of 5-aminolevulinic acid(5-ALA) The use of 5-ALA serving as a means to and aproxy for greater EOR resulted in extended overall sur-vival for patients with newly diagnosed glioblastoma19 Arecent meta-analysis of 41 117 unique patients by Brownet al adherent to the guidelines of PRISMA (PreferredReporting Items for Systematic Reviews and Meta-Analyses) also demonstrated a clear survival benefit forgross total resection over subtotal resection or biopsy atupfront surgery for glioblastoma1 The body of literatureas a whole clearly favored aggressive resections andthere seemed to be little disagreement for a strategytoward maximal resection when clinically feasibleHowever the challenge still remains when such strategiescome at the risk of neurological morbidity A recent reportby Rahman et al illustrates that the survival benefits fromaggressive resection are lost if the patient develops anew postoperative neurologic deficit as a result15
All the while our understanding of glioma genetics mo-lecular biology and mechanisms of resistance has con-tinued to deepen and evolve borne of thoughtful andsystematic studies using patient-acquired tumor sam-ples Molecular profiles and tumor genetics have proventhemselves to be the best predictors of clinical behaviorand now represent crucial components of the diagnostic
classification scheme of infiltrating gliomas12 With tumortissue at the molecular and genetic level being able to ro-bustly predict patient outcomes accurate tissue diagno-sis has become paramount in the management ofgliomas The role and value of open surgical resection to-ward this end have become clearer as concerns of sam-pling error with biopsy alone led to a number of studiesevaluating the ldquoaccuracyrdquo of stereotactic biopsy proce-dures Jackson et al reported a series of 81 patients whounderwent stereotactic biopsy followed by open surgicalresection The tissue diagnosis was concordant betweenbiopsy and open resection samples in only 51 ofpatients6 Other studies have also demonstrated diagnos-tic concordance between stereotactic biopsy and surgi-cal resection samples in only 57 to 79 ofcases131428 The major limitation of stereotactic biopsyfor infiltrating gliomas likely stems from the significantintratumoral heterogeneity and collectively these studieshighlight the value of open surgical resection in providinga more global representation and understanding of thetumor tissue
The value of extensive resection is perhaps even moreprofound when considering the therapeutic implicationsof such heterogeneity Multiple-site and serial-samplinganalyses have revealed a high degree of both spatial andtemporal heterogeneity within these tumors a conse-quence of serial evolutionary events during tumor growthand progression23 These studies have also led to theconcept of therapy-driven clonal selection and preferen-tial regrowth of resistant cell populations as a potentialmechanism of treatment failure Efforts to expand our un-derstanding of the tremendously complex network ofmutations and biological consequences of chronologicalhierarchy would be greatly facilitated by carefullyplanned thoughtful acquisition of tumor samples duringsurgery
Despite the recent paradigm shift in glioma diagnosticclassification little gains have been made in improvingthe overall prognosis for patients with malignant gliomassince the introduction of concurrent and adjuvant temo-zolomide in 200521 The strategies more recently tested inlarge randomized phase III trials by and large have yieldeddisappointing results while the reasons and mechanismsof treatment failures remain unclear Even so encourag-ing responses have occasionally been seen in varioussubsets of patients and studies exploring the presenceof potential biomarkers have generated intriguing andpromising results in these populations The developmentof the antindashvascular endothelial growth factor monoclonalantibody bevacizumab is one such example Two initialphase II trials showed prolonged progression-free sur-vival in recurrent glioblastoma relative to historical con-trols prompting the US Food and Drug Administration togrant accelerated approval to bevacizumab for recurrentglioblastoma in 2009825 However 2 large randomized tri-als evaluating the addition of bevacizumab to radiationand temozolomide in the newly diagnosed setting failedto show a benefit in overall survival24 and its utility in the
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
106
recurrent setting is now a topic of debate in light of sub-sequent phase III trial results However a post hoc analy-sis of patients enrolled in the AVAglio trial recentlydemonstrated that bevacizumab improved overall sur-vival for those with a proneural subtype tumor18 Just asO6-methylguanine-DNA-methyltransferase (MGMT) pro-moter methylation does for temozolomide the geneticprofile of the tumor could serve as a potential biomarkerof clinical response for bevacizumab as well and valida-tion studies are currently ongoing Such analyses al-though performed post hoc require targeted prospectivecollection of tumor tissue at initial surgery In addition ge-netic profiling of newly diagnosed malignant gliomas willneed to become routine if this approach is to be utilizedwidely Similarly cilengitide an inhibitor of aVb3 andaVb5 integrins with anti-angiogenic properties showedinitial promise in recurrent glioblastoma studies but failedto show any additional benefit in the newly diagnosedsetting20 A subsequent post hoc analysis of the phase IItrial revealed improved progression-free and overall sur-vival in patients with high aVb3 levels in the tumor cells26
However tumor tissues were not systematically collectedand less than half of the patientsrsquo tumor tissues wereavailable for analysis from the phase III trialUnfortunately this drug will most likely not undergo fur-ther development and one cannot help wonder if the out-come would have been different if the enrollment in thephase III trial had been enriched for or restricted to tumorswith high expression of the aVb3 integrin The only trueldquosuccess storyrdquo since the adaptation of radiation andtemozolomide has come from the novel approach of tu-mor treating fields (TTFields) a transcutaneous deliveryof low-intensity intermediate frequency alternating elec-tric fields The multicenter phase III trial EF-14 random-ized patients with supratentorial glioblastoma withoutevidence of tumor progression following standard che-moradiation to receive maintenance treatment withTTFields plus temozolomide or temozolomide alone22
The study was terminated early based on results of aplanned interim analysis demonstrating benefit inprogression-free survival overall survival a secondaryendpoint was also significantly enhanced at this timeDespite the trialrsquos success TTFields has not been univer-sally adopted by the neuro-oncology community andenthusiasm among clinicians and patients remains low27
Experts have raised concerns regarding the study designsuch as its open-label design lacking a sham-treatmentcontrol arm as well as the generalizability of the resultsbased on the unique randomization point occurring afterconcurrent chemoradiation16 Perhaps most significantlya lack of widely understood mechanism of action hasalso been raised as a factor with comparison to othertreatments the preclinical data for TTFields is relativelylacking particularly when applied in conjunction with che-moradiation27 Even during the early phase stages theuse of robust tissue-based analyses exploring the mech-anism of action such as dose response modeling andmultisite tissue biopsies may have mitigated some of
these concerns and led to wider acceptance by the com-munity Bevacizumab and cilengitide clearly benefitedfrom retrospective analyses of human tumor tissue toidentify susceptible treatment populations while the en-thusiasm for TTFields is perhaps in part tempered by thelack thereof Collectively the evolution of these treat-ments underscores the value of extensive targeted tissuesampling in furthering development of new adjunctivetherapies
Open surgical resection of tumors with such targeted tis-sue acquisition for analysis will continue to play a key rolein prospective clinical trial designs Comparison ofpretreatment and posttreatment tissue profiles representsa valuable line of investigation by delving into mecha-nisms of therapeutic action as well as mechanisms oftreatment failures1011 It also provides an opportunity toinvestigate a number of key fundamental steps along anagentrsquos path to clinical success such as does the agentsuccessfully traffic to the tumor if so how much anddoes the agent then actually have its hypothesizedeffects at the biochemical or cellular level Thusearly-phase trials can and should include posttreatmentmolecular endpoints when possible in addition to safetyendpoints Immunotherapy and immune checkpoint inhi-bition represent exciting novel therapeutic approachesfor neuro-oncology particularly based on their success inmetastatic cancers Large phase III trials studying block-ade of the programmed cell death protein (PD)1PDligand 1 axis with monoclonal antibodies for newlydiagnosed and recurrent glioblastoma are under way butinitial reports have been concerning for negative resultsAs in the development of many previous novel agentstissue-based mechanism studies have been largely lack-ing in the preclinical phases However an Alliance-supported trial currently enrolling focuses on a biomarkeras a primary endpoint patients with recurrent glioblas-toma indicated for surgery are randomized to receivepembrolizumab a PD1 inhibitor either before or aftersurgery (NCT02852655) The resected tumor tissue willthen be analyzed for the profile of tumor-infiltratingT cells and comparison will be made between the 2groups This study represents a tremendously valuableopportunity to explore the impact and the potential chal-lenges of checkpoint inhibition for malignant gliomas inthe clinical setting and should the large phase III trialsend up negative this pilot study will be very informative
Advances in imaging biomarkers and molecular charac-terization of gliomas in conjunction with new targetedtherapies will continue to improve and transform themanagement of these tumors Multimodality imaging cannow more accurately reflect ongoing biological processeswithin these tumors such as the presence of oncogenicmutations or cells undergoing malignant transformationNovel biomarkers such as circulating tumor DNA showpromise in detecting early recurrence or monitoring treat-ment response3724 Lastly the new classification schemerevolving around molecular characterization will provide a
Volume 2 Issue 3 The Value of Surgical Resection for Malignant Gliomas in the Modern Era
107
necessary corollary to these novel diagnostic tools Itremains indisputable however that clinical validation ofthese novel diagnostic tools will also require systematiccorrelation with human tumor tissue obtained throughsurgery These samples ideally gathered prospectivelywill provide a pivot upon which we can expand our under-standing of the complex network of oncological pro-cesses driving these tumors
Malignant gliomas are incredibly challenging disease en-tities in many ways due to the inter- and intratumoral het-erogeneity that is a hallmark of them Experience to datehints that future successes in malignant gliomas rest inneuro-oncology entering the era of precision medicinewhere validated biomarkers and targeted personalizedtherapies are seamlessly integrated into the managementparadigm Accordingly systems supporting surgical re-section and patient-specific tumor tissue analysis mustbe built and organized to guide the decision making fortherapy As our overall approach to the management ofmalignant gliomas evolves so should the framework ofsurgical management The clinical benefits of maximalsafe resection are well founded and well reportedHowever the oncological neurosurgeon must now lookbeyond maximal cytoreduction itself and recognize thevalue of thoughtful acquisition and analysis of tumor tis-sue Modern neurosurgeons must consider themselvessurgical neuro-oncologists and engagement and partici-pation of surgeons into clinical trials particularly early-phase trials should be encouraged and valued In turnwe should provide our surgical trainees with the trainingand tools in neuro-oncology to help them participate andcontribute in multidisciplinary collaborative efforts aimingto advance the understanding of brain tumor biology andultimately improve the outlook of our patients
References
1 Lacroix M Abi-Said D Fourney DR Gokaslan ZL et al A multivariateanalysis of 416 patients with glioblastoma multiforme prognosisextent of resection and survival J Neurosurg 2001 95190ndash198
2 Hervey-Jumper SL Berger MS Maximizing safe resection of low-and high-grade glioma J Neurooncol 2016 130269ndash282
3 Sanai N Polley MY McDermott MW Parsa AT Berger MS An ex-tent of resection threshold for newly diagnosed glioblastomas JNeurosurg 2011 1153ndash8
4 Stummer W Pichlmeier U Meinel T et al Fluorescence-guided sur-gery with 5-aminolevulinic acid for resection of malignant glioma arandomised controlled multicentre phase III trial Lancet Oncol2006 7392ndash401
5 Brown TJ Brennan MC Li M et al Association of the extent ofresection with survival in glioblastoma a systematic review andmeta-analysis JAMA Oncol 2016 21460ndash1469
6 Rahman M Abbatematteo J De Leo EK et al The effects of new orworsened postoperative neurological deficits on survival of patientswith glioblastoma J Neurosurg 2017 127123ndash131
7 Louis DN Perry A Reifenberger G et al The 2016 World HealthOrganization Classification of Tumors of the Central NervousSystem a summary Acta Neuropathol 2016 131803ndash820
8 McGirt MJ Bulsara KR Cummings TJ et al Prognostic value ofmagnetic resonance imaging-guided stereotactic biopsy in the
evaluation of recurrent malignant astrocytoma compared with a le-sion due to radiation effect J Neurosurg 2003 9814ndash20
9 Muragaki Y Chernov M Maruyama T et al Low-grade glioma onstereotactic biopsy how often is the diagnosis accurate MinimInvasive Neurosurg 2008 51275ndash279
10 Woodworth G McGirt MJ Samdani A Garonzik I Olivi AWeingart JD Accuracy of frameless and frame-based image-guided stereotactic brain biopsy in the diagnosis of glioma com-parison of biopsy and open resection specimen Neurol Res 200527358ndash362
11 Suzuki H Aoki K Chiba K et al Mutational landscape and clonal ar-chitecture in grade II and III gliomas Nat Genet 2015 47458ndash468
12 Stupp R Mason WP van den Bent MJ et al Radiotherapy plus con-comitant and adjuvant temozolomide for glioblastoma N Engl JMed 2005 352987ndash996
13 Kreisl TN Kim L Moore K et al Phase II trial of single-agent bevaci-zumab followed by bevacizumab plus irinotecan at tumor progres-sion in recurrent glioblastoma J Clin Oncol 2009 27740ndash745
14 Vredenburgh JJ Desjardins A Herndon 2nd JE et al Phase II trial ofbevacizumab and irinotecan in recurrent malignant glioma ClinCancer Res 2007 131253ndash1259
15 Chinot OL Wick W Mason W et al Bevacizumab plusradiotherapy-temozolomide for newly diagnosed glioblastomaN Engl J Med 2014 370709ndash722
16 Gilbert MR Dignam JJ Armstrong TS et al A randomized trial ofbevacizumab for newly diagnosed glioblastoma N Engl J Med2014 370699ndash708
17 Sandmann T Bourgon R Garcia J et al Patients with proneural glio-blastoma may derive overall survival benefit from the addition of bev-acizumab to first-line radiotherapy and temozolomide retrospectiveanalysis of the AVAglio trial J Clin Oncol 2015 332735ndash2744
18 Jackson RJ Fuller GN Abi-Said D et al Limitations of stereotacticbiopsy in the initial management of gliomas Neuro Oncol 20013193ndash200
19 Stupp R Hegi ME Gorlia T et al Cilengitide combined with stan-dard treatment for patients with newly diagnosed glioblastoma withmethylated MGMT promoter (CENTRIC EORTC 26071-22072study) a multicentre randomised open-label phase 3 trial LancetOncol 2014 151100ndash1108
20 Weller M Nabors LB Gorlia T et al Cilengitide in newly diagnosedglioblastoma biomarker expression and outcome Oncotarget2016 715018ndash15032
21 Stupp R Taillibert S Kanner AA et al Maintenance therapy withtumor-treating fields plus temozolomide vs temozolomide alone forglioblastoma a randomized clinical trial JAMA 20153142535ndash2543
22 Wick W TTFields where does all the skepticism come from NeuroOncol 2016 18303ndash305
23 Sampson JH Alternating electric fields for the treatment of glioblas-toma JAMA 2015 3142511ndash2513
24 Lang FF Asher A Prospective clinical trials of brain tumor therapy thecritical role of neurosurgeons J Neurooncol 2004 69151ndash167
25 Lang FF Gilbert MR Puduvalli VK et al Toward better early-phasebrain tumor clinical trials a reappraisal of current methods and pro-posals for future strategies Neuro Oncol 2002 4268ndash277
26 Elkhaled A Jalbert L Constantin A et al Characterization of metab-olites in infiltrating gliomas using ex vivo (1)H high-resolution magicangle spinning spectroscopy NMR Biomed 2014 27578ndash593
27 Jalbert LE Neill E Phillips JJ et al Magnetic resonance analysis ofmalignant transformation in recurrent glioma Neuro Oncol 2016181169ndash1179
28 Touat M Duran-Pena A Alentorn A Lacroix L Massard C Idbaih AEmerging circulating biomarkers in glioblastoma promises andchallenges Expert Rev Mol Diagn 2015 151311ndash1323
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
108
Update on RadiationCombinations in theTreatment of Patientswith Malignant BrainTumors FromRadiosensitizers toImmunotherapy
Debra Nana Yeboa MD1
Erik P Sulman MD PhD123
Departments of 1Radiation Oncology2Translational Molecular Pathology and3Genomic Medicine The University of Texas MDAnderson Cancer Center 1515 Holcombe BlvdUnit 97 Houston Texas USA Tel 713-563-2300dnyeboamdandersonorg andepsulmanmdandersonorg
109
AbstractAdvances in radiosensitizers and immunotherapyhave ushered in a new frontier in brain tumortreatment The brain has often been viewed as asanctuary site due to the bloodndashbrain barrier andthus the 2 primary modalities of therapy includedsurgery and radiation therapy (RT) More recentlysystemic therapies have played a greater role aseither combination therapy radiosensitizers or im-munotherapy Two novel radiosensitizers are beingdeveloped for the treatment of brain metastasesRRx-001 for example is a small molecule thataccelerates the NO2 to NO conversion of deoxyhe-moglobin and the agent 2-dexoyglucose (2-DG) is anonmetabolized glucose analogue that interfereswith ATP formation Poly(ADP-ribose) DNA polymer-ase inhibitors are promising due to their distinctradiobiological effects Veliparib and olaparib areamong the most studied with randomized trialsexploring their use in gliomas and brain metastasesImmunotherapy including immune checkpoint inhib-itors may play a role for both primary gliomas andbrain metastases RT has been shown to enhancethe function of cytotoxic T lymphocytes induce infil-tration of cytotoxic T lymphocytes and enhancefunction Trials are presently exploring use of bothprogrammed cell death protein (PD)1 and PD ligand1 blockade in glioblastoma patients with radiationSimilarly several immunotherapies are being investi-gated with either stereotactic radiosurgery or wholebrain radiation therapy for brain metastases In thisreview the use of radiosensitizers and immunother-apy agents with RT will be discussed broadly
Keywords brain metastases brain tumors gliomasimmunotherapy radiation therapy radiosensitizers
Radiosensitizers andImmunotherapy inBrain TumorsAdvances in radiosensitizers and immunotherapy haveushered in a new frontier to brain tumor treatment Braintumors however are a diverse class sharing only similaranatomic location Both primary brain malignancies andbrain metastasis have widely diverse histologies and mo-lecular phenotypes With the bloodndashbrain barrier thebrain has often been viewed as a sanctuary site and thusthe 2 primary modalities of therapy included surgery andradiation with decreased benefit from systemic agentsdue to lack of brain penetration However more recentlysystemic therapies have played a greater role as eithercombination therapy radiosensitizers or immunother-apy While temozolomide (TMZ) has played a pivotal rolefor glioblastoma (GBM) only a subset of patients benefitfrom the treatment1 The use of alternative systemicagents that may potentiate the effects of radiation ther-apy (RT) is becoming increasingly appealing Similarly forbrain metastases a variety of systemic agents are beingexplored primarily based on histology and immune pro-file In this review the use of radiosensitizers and immu-notherapy agents currently under investigation with RTwill be discussed
RadiosensitizersThe guiding concept of radiation sensitization is to in-crease the biologic effect of radiation such as increasedDNA damage decreased DNA repair decreased hypoxiaor increased G2M cell cycle blockade leading to im-proved tumor control and increased patient survival2
Poly(adenosine diphosphate-ribose) DNA polymerase(PARP) inhibitors are promising radiosensitizers due totheir roles in DNA repair3 PARP inhibitors work againstPARP1 a nuclear enzyme involved in the recruitment ofrepair proteins used in base excision repair and single-strand break repair PARP1 may also play a role in nonho-mologous end-joining4 The primary investigation ofPARP inhibitors has been in potentiating radiation andchemotherapy effects the latter in the context of homolo-gous repair deficient tumors For radiation the primarymechanism of action is inducing damage to nucleotidesleading to single-strand and double-strand breaks ThusPARP inhibitors in combination with radiation have an ap-pealing mechanism to inhibit or delay DNA repair andlikely convert more single-strand breaks to double-strandbreaks4
While several PARP inhibitors are currently being evalu-ated in a variety of tumors including talazoparib and nira-parib veliparib and olaparib are among the most studiedand there are randomized trials exploring their use in
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
110
gliomas The US National Cancer Institute (NCI)ndashfundedAlliance for Clinical Trials in Oncology (Alliance) A071102is a randomized phase IIIII trial evaluating the use ofveliparib in combination with TMZ in the adjuvant settingin patients with GBM tumors exhibiting hypermethylationof the O6 methylguanine DNA methyltransferase (MGMT)gene promoter Preclinical data supporting this trial sug-gested that only patients with MGMT methylated tumorswould benefit from the combination a group of patientsfor whom TMZ concurrent with radiation might be mostbeneficial5 A phase I trial performed by the NCI-fundedAmerican Brain Tumor Consortium attempted to combineveliparib with radiation and TMZ but failed to identify asuitable recommended phase II dose due to significanthemotoxicity6 Thus attempts to combine radiation withveliparib have focused on patients least likely to benefitfrom TMZ namely with MGMT unmethylated tumors forwhom TMZ could be withheld The Australian VeliparibRT and TMZ trial in newly diagnosed unmethylatedMGMT glioblastoma (VERTU) is a single-arm study inwhich patients receive RT with veliparib followed by adju-vant TMZ and veliparib4
An ongoing novel approach to radiosensitize gliomasinvolves a combination with an agent that interferes withan essential metabolic process 2-Dexoyglucose (2-DG)is a nonmetabolized glucose analogue that acts as acompetitive inhibitor of glycolysis It is transported acrossthe bloodndashbrain barrier by the glucose transporter GLUT-1 and thus has good penetration into the CNSIntracellularly it is trapped and accumulates in cells simi-lar to the mechanism of 18-fluorodeoxyglucose 2-DG isphosphorylated by glycolytic enzymes and the
phosphorylated 2-DG (2-deoxyglucose-P) is trapped in-tracellularly Inhibition of hexokinase activity by 2-DGinterferes with ATP formation and results in tumor celldeath7 While it has positive attributes by selectively tar-geting metabolically active tumor cells 2-DG has alsobeen associated with Q-T prolongation The currentphase III trial in gliomas is assessing the toxicity and tol-erability of 2-DG with hypofractionated radiation of 5 Gyas a radiosensitizer7
Two novel radiosensitizers are being developed for thetreatment of brain metastases First RRx-001 is a smallmolecule initially designed by the aerospace industry Itworks in part as a radiosensitizer by increasing blood flowand thus oxygenation of tumors through nitric oxideRRx-001 which binds to hemoglobin accelerates theNO2 to NO conversion of deoxyhemoglobin It workslocally under hypoxic conditions and subsequentlythe radiosensitive effects through nitric oxide are invasodilation and inhibiting DNA repair enzymes8 Nitricoxide is relatively benign The higher levels of oxidativestress with H2O2 and superoxide in tumors in comparisonto normal tissues result in the preferential generation ofreactive peroxynitrite in the presence of higher nitric oxidelevels7 This accounts for the increased specificity anddecreased toxicity with RRx-001 The dose limiting toxic-ity in a phase I trial of 25 patients treated with eitherweekly or biweekly infusions was infusional pain relatedto the release of NO at the site of injection7 Outside ofpreclinical models 2 clinical reports examining wholebrain radiation therapy (WBRT) with RRx-001 reported anintracranial response A patient with melanoma and 2hemorrhagic edematous lesions of 26 cm and 33 cm
Table 1 Clinical trials involving immunotherapy and radiation therapy1213
Clinical Trials Number Phase Disease Type Treatment Groups
NCT02667587 II Newly diagnosed GBMMGMT-methylated
Nivolumabthorn TMZthorn RT vs placebothornTMZ thorn RT
NCT02617589 III Newly diagnosed GBM Nivolumabthorn RT vs TMZthorn RTNCT02336165 II Newly diagnosed unmethylated
MGMT recurrent glioblastomaMEDI4736thorn standard RT vs MEDI4736 thorn
bevacizumabNCT02530502 III Newly diagnosed GBM RTthorn TMZthorn pembrolizumab TMZthorn
pembrolizumabNCT02313272 I Recurrent glioma Hypofractionated stereotactic radiationthorn
pembrolizumab thorn bevacizumabNCT02696993 III Brain metastases Nivolumabthorn SRS nivolumabthornWBRT
nivolumabthorn ipilimumab thorn SRS nivolu-mabthorn ipilimumab thornWBRT
NCT02115139 II Melanoma brain metastases Ipilimumab thornWBRTNCT02097732 II Melanoma brain metastases Ipilimumab SRS ipilimumab vs SRS
ipilimumabNCT01703507 I Melanoma brain metastases Ipilimumab thornWBRT vs ipilimumab thorn SRSNCT02107755 II Melanoma brain metastases Ipilimumab thorn SRSNCT02858869 pilot Melanoma and NSCLC Pembrolizumabthorn SRSNCT01950195 I Melanoma brain metastases Ipilimumab thorn SRSNCT02662725 II Melanoma brain metastases Ipilimumab thorn SRS
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
111
after a single intravenous dose of RRx-001 of 5 mgm2 4days before WBRT resulted in symptomatic improvementwithin 48 hours By 4 months after radiation there was areduction in size in the largest dimension down to 10 cmand 23 cm of the respective lesions A second report of amelanoma patient with at least 18 lesions after receivingRRx-001 of 5 mgm2 4 days before WBRT as well astwice weekly doses during the 2 weeks of radiation alsoshowed response The patient at 4 months had disap-pearance of 13 of 18 lesions with shrinkage of theremaining 5 lesions8 Presently BRAINSTORM is a phaseIII dose escalation trial of RRx-001 designed to be ad-ministered twice weekly for 2 weeks with WBRT (30 Gy in10 fractions) with the option for weekly maintenance8
Veliparib has also been evaluated in the setting of brainmetastases It was tested in a global randomized con-trolled trial with WBRT Veliparib is orally bioavailable andcrosses the bloodndashbrain barrier It was first examined in amultihistology phase I trial in patients with nonndashsmall celllung cancer (NSCLC) breast cancer melanoma and re-nal and colorectal cancers among others The study of81 patients tested dose tolerance of veliparib from 10 to300 mg orally twice a day with WBRT to 30 Gy in 10 frac-tions or 375 Gy in 15 fractions9 The phase I trial dose es-calation portion did not reach the predefined criteria forthe maximum tolerated dose but there was amplificationof the adverse effects of nausea and vomiting among thehighest dose cohort of 300 mg bid9 The adverse eventprofile at 200 mg bid was similar to that of WBRT aloneDoses of veliparib from 20 to 200 mg bid demonstratesimilar antitumor activity and other studies in preclinicalmodels found that 50 mg daily demonstrated significantreduction in poly(ADP-ribose) in peripheral blood mono-nuclear cells and tumor tissue while also effectivelycrossing the bloodndashbrain barrier Thus the subsequentphase II trial examined 50 mg with WBRT9 In order to as-sess a more homogeneous cohort the phase III globalrandomized trial studied only NSCLC at the 2 doses of50 mg and 200 mg twice daily versus placebo twice a daywith WBRT10 The primary endpoint was overall survivalIn 307 patients in a 111 randomization of 50 mg bid200 mg bid or placebo twice daily the study found nosignificant differences in overall survival among the differ-ent groups10 The majority of patients across the treat-ment groups had a graded prognostic assessment (GPA)score of25 and a Karnofsky performance status ofgt80 The median overall survival was 185 days forpatients receiving placebo and 209 days for those receiv-ing veliparib without any statistically significant differ-ence These results were similar to the disease-specificestimate of median survival for the disease-specific GPAof NSCLC patients with brain metastases10
Several other radiosensitizers have failed to improve overradiation alone in a number of trials These have includedtrials with WBRT including motexafin gadolinium efap-roxyn bortozemib thalidomide teniposide topotecanpaclitaxel and cisplatin7 Of note other PARP inhibitorsalso being assessed include talazoparib and niraparib4
which may yield positive results The use of valproic acid(VPA) as a histone deacetylase inhibitor has also beenconsidered to have radiosensitizing potential in additionto its anti-epileptic drug properties11 While studies havereported that patients with GBM receiving an anti-epilep-tic agent may have higher overall survival than those re-ceiving standard chemoradiation therapy alone thebenefit remains controversial Retrospective analysissuggested that patients taking VPA specifically had bettersurvival in comparison to other anti-epileptic drugs Alsoa recent prospective phase II trial was performed in 37patients with GBM receiving VPA 25 mgkg concurrentlywith TMZ chemoradiation and reported a median survivalof 296 months While controversial further data andinvestigation are needed into this and other agents thatmay potentiate RT
Immunotherapy and radiationImmune checkpoint inhibitors lead to activation of T cellswhich may traffic across the bloodndashbrain barrier to inter-act with tumor Primary brain tumors may evade the im-mune system through upregulation of immunecheckpoints and possible immunosuppression12
Monoclonal antibodies promote immune-mediated anti-tumor activity by inhibiting the immune functionndashmediated cytotoxic T-lymphocyte associated protein 4(CTLA-4) and programmed cell death protein 1 (PD-1)receptors PD protein ligand (PD-L1) is upregulated inGBM through oncogenic signaling possibly throughphosphatase and tensin homolog loss and interleukin-10signaling1314 RT has also been shown to enhance thefunction of cytotoxic T lymphocytes RT may induce aninfiltration of cytotoxic T lymphocytes and enhance theirfunction It may also induce antindashCTLA-4 agents inhibitingT-cell function and increasing the CD8thorn T cellregulatoryT cell ratio in cases of melanoma15 Thus PD-1 and PD-L1 blockers may have a further role in CNS managementwith the use of radiation
In preclinical models radiation has been examined withimmunotherapy that included among other mechanismsvaccination PD-1 blockade and CTLA-4 blockade Inmice radiation plus a vaccination of irradiated gliomacells was associated with increased survival of 40 to80 compared with 0 to 10 for other groups stud-ied16 A benefit of PD-1 blockade with stereotactic radio-surgery (SRS) specifically has also been shown in amouse model In comparison to mice treated with radia-tion antindashPD-1 therapy or a combination only those re-ceiving combination therapy had a higher percentagesurvival alive beyond 180 days after treatment17 Othermouse carcinoma models have identified response withanti-CTLA antibody and fractionated radiation therapy18
CD137 activation CTLA-4 blockade and focal radiationtherapy have been examined in an immunocompetent in-tracranial GBM model Mice treated with triple combina-tion therapy had 50 greater survival19 In other murine
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
112
models the use of antindashPD-1 and antindashCTLA-4 agentsshowed improved survival and increased tumor infiltratingleukocyte populations compared with single modalitywith concurrent radiation16 There are conflicting data re-garding timing or sequencing of therapy with some ani-mal models showing no difference in tumor response inrelation to timing of RT and delivery of immunotherapy18
For instance in one animal model CTLA-4 blockade de-livered simultaneously with radiation or delivered a coupleof days after showed no difference in survival among themice19
Increased PD-1 expression in circulating monocytes hasbeen identified as a biomarker for tumor-induced immu-nosuppression and may serve as a prognostic factor forpotentially worse survival outcomes in clinic13 In onestudy GBM patients with lower PD-L1 expression hadhigher median overall survival than those with higher PD-L1 expression suggesting that lower expression may beassociated with less immunosuppression and more im-mune activity against the tumor glioma20 RT with immunecheckpoint blockade is being investigated to assess if theaddition of PD-1 and PD-L1 inhibitors may improve theoutcomes or toxicity profile of standard therapy For in-stance a multi-institutional trial opened as a phase III willevaluate outcomes in GBM receiving radiation and pem-brolizumab with TMZ (NCT02530502) Next durvalumabor MEDI4736 a PD-L1 inhibitor is being examined forunmethylated MGMT GBMs with standard radiotherapy(NCT02336165)12 The impact of checkpoint inhibitorsduring adjuvant treatment of GBM is currently beingevaluated in the NCI-funded NRG-BN002 trial(NCT02311920) which will evaluate the antindashCTLA-4antibody ipilimumab alone or in combination with theantindashPD-1 antibody nivolumab for patients with newlydiagnosed GBM
Brain metastases have clonal populations of cells differ-ent from the rest of the brain and a unique microenviron-ment that may influence immunotherapy There may bemore immune infiltrates in metastases than in primarybrain tumors21 PD-L1 expression in brain metastasesvaries by histology In a series evaluating PD-L1 expres-sion in various tumors including melanoma NSCLCbreast renal colorectal and small cell less than 10showed significant expression22 There was greatest ex-pression among NSCLC and melanoma with a correla-tion between PD-L1 expression and tumor infiltratinglymphocytes22 Institutional series have examined thecombination of radiation and immune checkpoint block-ade In another study specific to melanoma brain metas-tases PD-L1 expression was found in over 50 of thecases and among those cases over 40 expressedPD-L1 in more than 5 of tumor cells23 The largest bodyof data for use of PD-L1 with radiation is for melanomaand NSCLC
Ipilimumab is a human monoclonal antibody that blocksCTLA-4 and allows for T-cell activation and proliferationto enhance the immune response to cancer In a
retrospective review of 70 patients with brain metastasestreated with SRS or WBRT the 33 patients receiving im-munotherapy had a median survival of 183 months incomparison to the 37 patients who did not receive ipili-mumab with a median survival of 53 months While therewere limited data among the cohort to evaluate sequenc-ing of therapy among 10 evaluable patients 40 whoreceived ipilimumab prior to RT had a partial response incomparison to only 10 among the cohort of 22 evalu-able patients who did not receive ipilimumab therapy atall with radiation24 Another retrospective institutionalstudy of 77 patients in which 37 received ipilimumabfound that patients treated with SRS and ipilimumab hada median survival of 213 months versus 49 months forthose not receiving ipilimumab Most interestingly theyidentified that the correlation remained significant evenafter adjusting for additional factors such as performancestatus Secondly there was not an increased need for useof salvage WBRT25
The sequencing of radiotherapy and immune checkpointinhibitors is of interest In a study of patients with brainmetastases the one-year survival for patients receivingSRS before ipilimumab was greater at 65 in contrast to56 for those receiving it concurrently and 40 for thosereceiving it after SRS26 Similarly another study of 75patients with 566 brain metastases showed greater tu-mor lesion response at 6 months from SRS for patientsreceiving ipilimumab nivolumab or pembrolizumabwithin 4 weeks of their SRS27 Those receiving concurrenttherapy had by 6 months a decrease of 949 in compar-ison to 662 for those not receiving checkpoint inhibi-tors within 4 weeks Prospective clinical trials areinvestigating different combinations of RT with immunecheckpoint blockers in this setting For instance new tri-als are currently evaluating intracranial tumor control at 6months and the timing of immune therapy or immunecheckpoint inhibitors in relation to SRS28
Vaccines are also being developed for primary braintumors showing some evidence for their use Vaccinesdeveloped from dendritic cells and tumor lysate with tu-mor antigens such as the epidermal growth factor recep-tor variant III vaccine have shown promise29 Forinstance in a placebo controlled phase II trial of ICT-107a vaccine composed on autologous dendritic cells andtumor antigens progression-free survival was increasedby 2 months for those receiving the vaccine30 Radiationmay assist in serving as a primer for the immunogeniceffects by facilitating tumor antigen uptake by dendriticcells and cross presentation on major histocompatibilitycomplex I Thus RT may assist in the tumor-specific cy-totoxic T lymphocytes associated with the immunemechanism
In conclusion although there may be challenges to com-bining and sequencing brain tumors radiosensitizersand immunotherapy the opportunities and potential fornovel applications are promising For brain tumors brainmetastases are typically underrepresented in trials
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
113
despite being among the most common intracraniallesions Despite their large population patients with brainmetastases are often excluded from clinical trials withnovel agents due to concerns regarding confounding out-comes and tolerability12 Primary gliomas also offer anovel frontier for the use of immunotherapy to standardadjuvant chemotherapy and radiation particularly forpatients with GBM less likely to respond to TMZ such aswith unmethylated MGMT As studies work to define therole of RT and radiosensitizers and immunotherapy fur-ther analysis is needed to assess the timing of RT andthese treatments
References
1 Stupp R Hegi ME Mason WP et al Effects of radiotherapy withconcomitant and adjuvant temozolomide versus radiotherapy aloneon survival in glioblastoma in a randomised phase III study 5-yearanalysis of the EORTC-NCIC trial Lancet Oncol 2009 10459ndash466
2 Lawrence TS Blackstock AW McGinn C The mechanism of actionof radiosensitization of conventional chemotherapeutic agentsSemin Radiat Oncol 2003 1313ndash21
3 Lesueur P Chevalier F Austry JB et al Poly-(ADP-ribose)-polymer-ase inhibitors as radiosensitizers a systematic review of pre-clinicaland clinical human studies Oncotarget 2017 8(40)69105ndash69124
4 Lester A Rapkins R Nixdorf S Khasraw M McDonald KCombining PARP inhibitors with radiation therapy for the treatmentof glioblastoma is PTEN predictive of response Clin Transl Oncol2017 19273ndash278
5 Gupta SK Kizilbash SH Carlson BL et al Delineation of MGMT hyper-methylation as a biomarker for veliparib-mediated temozolomide-sensi-tizing therapy of glioblastoma J Natl Cancer Inst 2016 108
6 Kleinberg LR Blakeley J Mikkelsen T et al An American BrainTumor Consortium (ABTC) phase 1 trial of veliparib (ABT-888)temozolomide (TMZ) and concurrent radiation therapy (RT) fornewly diagnosed glioblastoma multiforme (GBM) need for modifica-tion to approach for combining these therapies InternationalJ Radiat Oncol Biol Phys 2012 84S7ndashS8
7 Oronsky BT A Review of two promising radiosensitizers in brainmetastases Rrx-001 and 2-deoxyglucose In NC Oronsky edJ Cancer Sci Ther 2015 pp 137ndash141
8 Kim MM Parmar H Cao Y et al Concurrent whole brain radiother-apy and RRx-001 for melanoma brain metastases Neuro Onc2016 18455ndash456
9 Mehta MP Wang D Wang F et al Veliparib in combination withwhole brain radiation therapy in patients with brain metastasesresults of a phase 1 study J Neurooncol 2015 122409ndash417
10 Chabot P Hsia TC Ryu JS et al Veliparib in combination withwhole-brain radiation therapy for patients with brain metastasesfrom non-small cell lung cancer results of a randomized globalplacebo-controlled study J Neurooncol 2017 131105ndash115
11 Ochiai S Nomoto Y Yamashita Y et al Roles of valproic acid inimproving radiation therapy for glioblastoma a review of literaturefocusing on clinical evidence Asian Pac J Cancer Prev 201617463ndash466
12 Tan AC Heimberger AB Menzies AM Pavlakis N Khasraw MImmune checkpoint inhibitors for brain metastases Curr Oncol Rep2017 1938
13 DrsquoSouza NM Fang P Logan J Yang J Jiang W Li JCombining radiation therapy with immune checkpoint blockade
for central nervous system malignancies Frontiers Oncol 20166212
14 Parsa AT Waldron JS Panner A et al Loss of tumor suppressorPTEN function increases B7-H1 expression and immunoresistancein glioma Nat Med 2007 1384ndash88
15 Binder DC Davis AA Wainwright DA Immunotherapy for cancer inthe central nervous system current and future directionsOncoimmunology 2016 5e1082027
16 Newcomb EW Demaria S Lukyanov Y et al The combination ofionizing radiation and peripheral vaccination produces long-termsurvival of mice bearing established invasive GL261 gliomas ClinCancer Res 2006 124730ndash4737
17 Zeng J See AP Phallen J et al Anti-PD-1 blockade and stereotac-tic radiation produce long-term survival in mice with intracranial glio-mas Int J Radiat Oncol Biol Phys 2013 86343ndash349
18 Chow KK Hara W Lim M Li G Combining immunotherapy withradiation for the treatment of glioblastoma J Neurooncol2015123459ndash464
19 Belcaid Z Phallen JA Zeng J et al Focal radiation therapy com-bined with 4-1BB activation and CTLA-4 blockade yields long-termsurvival and a protective antigen-specific memory response in amurine glioma model PLoS One 2014 9e101764
20 Topalian SL Hodi FS Brahmer JR et al Safety activity and im-mune correlates of anti-PD-1 antibody in cancer N Engl J Med2012 3662443ndash2454
21 Bienkowski M Preusser M Prognostic role of tumour-infiltrating in-flammatory cells in brain tumours literature review Curr OpinNeurol 2015 28647ndash658
22 Harter PN Bernatz S Scholz A et al Distribution and prognostic rel-evance of tumor-infiltrating lymphocytes (TILs) and PD-1PD-L1 im-mune checkpoints in human brain metastases Oncotarget 2015640836ndash40849
23 Berghoff AS Ricken G Widhalm G et al Tumour-infiltrating lym-phocytes and expression of programmed death ligand 1 (PD-L1) inmelanoma brain metastases Histopathology 2015 66289ndash299
24 Silk AW Bassetti MF West BT Tsien CI Lao CD Ipilimumab and ra-diation therapy for melanoma brain metastases Cancer Med 20132899ndash906
25 Knisely JP Yu JB Flanigan J Sznol M Kluger HM Chiang VLRadiosurgery for melanoma brain metastases in the ipilimumab eraand the possibility of longer survival J Neurosurg 2012117227ndash233
26 Kiess AP Wolchok JD Barker CA et al Stereotactic radiosurgeryfor melanoma brain metastases in patients receiving ipilimumabsafety profile and efficacy of combined treatment Int J Radiat OncolBiol Phys 2015 92368ndash375
27 Qian JM Yu JB Kluger HM Chiang VL Timing and type of immunecheckpoint therapy affect the early radiographic response of mela-noma brain metastases to stereotactic radiosurgery Cancer 20161223051ndash3058
28 Silk AW Cao Y Gomez-Hassan D et al A randomized phase IIstudy of ipilimumab induction in patients with melanoma brain me-tastases receiving stereotactic radiosurgery J Clin Oncol 2015 33TPS9079ndashTPS9079
29 Neagu MR Reardon DA An Update on the role of immunotherapyand vaccine strategies for primary brain tumors Curr TreatOptions Oncol 2015 1654
30 Wen PY Reardon DA Phuphanich S et al A randomized double-blind placebo-controlled phase 2 trial of dendritic cell (DC) vaccina-tion with ICT-107 in newly diagnosed glioblastoma (GBM) patientsJ Clin Oncol 2014 322005ndash2005
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
114
British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

IntroductionEpigenetics is defined as the study of heritable changesin gene expression that are not caused by alterations inDNA sequences1 The phenotypic difference between acaterpillar and a butterfly for example is due to epige-netic regulation of gene expression in the same animalwith the same DNA I particularly like this example to ex-plain the meaning of the term epigenetics as it impres-sively demonstrates how powerful these mechanisms arein controlling phenotypic changes Epigenetic changesare reversible and include the key processes of DNAmethylation histone modifications and noncoding RNA-associated gene silencing (recently reviewed2) known toplay an essential role during the embryonic and postnataldevelopment of an organism and in tissue homeostasis2
Disruptions of epigenetic processes can induce changesin gene function which together with genetic changescan lead to the neoplastic transformation of a normal cell(recently reviewed)3
Recent technological advances have significantly con-tributed to the tremendous progress in understandinghow these epigenetic modifications are regulated in nor-mal cells and deregulated in cancer cells For examplethis knowledge has enabled the translation into better di-agnostic algorithms for tumor classification prognostica-tion and risk assessment Importantly we are nowentering a time when novel therapies targeting thesederegulated epigenetic mechanisms are being devel-oped with some of them showing very promising effectsin preclinical models
It is beyond the scope of this article to comprehensivelyreview mechanisms of epigenetic regulation of gene ex-pression and their deregulation in brain tumors excellentrecent reviews are available to the readers on thesesubjects2ndash5 Here I will discuss a few examples of recentepigenetic discoveries which have informed the develop-ment of novel diagnostic and prognostic tools or led tosuccessful preclinical testing of new epigenetic drugs inexperimental models
Epigenetic Profiles inthe MolecularClassification of BrainTumorsGlioma One of the first examples of an epigenetic changeinforming the design of an assay for diagnostic screeningto corroborate a therapeutic decision is the assessmentof methylation of the MGMT promoter in malignantgliomas6 MGMT (O6-methylguanine DNA methyltransfer-ase) is a key enzyme in the DNA repair network which
removes the mutagenic and cytotoxic adducts from O6
guanine in DNA the preferred point of attack of alkylatingchemotherapeutic agents (ie BCNU temozolomide etc)Hypermethylation of cytosine-phosphate-guanine (CpG)islands located in the promoter region of MGMT is pri-marily responsible for the loss of MGMT function in manytumor types hence leading to an increased sensitivity tothe killing effects of alkylating drugs used in chemo-therapy6 This test is widely used in clinical practice topredict response to temozolomide the alkylating drug ofchoice in high-grade gliomas although it should bestressed that there is still no consensus as to which testmethod to use which CpG sites to assess and what themethylation cutoff should be
Ependymoma Until very recently these tumors havebeen subclassified and graded on the basis of histologi-cal features into low and high grade In 2015 a molecularclassification based on DNA methylation profiling hasbeen proposed which defines 9 molecular subgroups 3for each anatomical location of these tumors (supratento-rial posterior fossa and spinal cord)7 In the supratento-rial location ependymomas with the fusion geneC11ORF95RELA (ST-EPN-RELA) have a poor prognosisand in the posterior fossa it is the ependymoma groupEPN-A that is characterized by a poor prognosis7 Allother ependymomas show a comparatively goodprognosis7 Although not yet included in the World HealthOrganization (WHO) 2016 classification a recent consen-sus paper has recommended that this classification beused for enrollment in prospective clinical trials8 and it isexpected to contribute to informing decisions onmolecular-based treatments as they become available
Medulloblastoma (MB) International consensusrecognizes 4 medulloblastoma molecular subgroupsWNT (MBWNT) SHH (MBSHH) Group 3 (MBGrp3) andGroup 4 (MBGrp4) each defined by their characteristicDNA methylation and genome-wide transcriptomicprofiles9 Recently the heterogeneity within these sub-groups has been reduced by 2 independent studieswhich have defined additional subtypes Schwalbe andcolleagues10 have suggested to split MBSHH into 2 age-dependent subtypes corresponding to ldquoinfantrdquo (lt43 y)and ldquochildhoodrdquo patients (43 y) and MBGrp3 andMBGrp4 into further high-risk and low-risk subtypes whilethe MBWNT group remains unchanged10 Interestingly thelow-risk subtypes were defined primarily by hypermethy-lation in comparison to normal cerebellum whereas thehigh-risk subtypes were defined by relativehypomethylation10 Cavalli and coauthors11 used integra-tive clustering of DNA methylation and gene expressiondatasets from 763 patients to split the original 4 sub-groups into 12 subtypes MBSHH is split into 4 subtypes(abc d) MBWNT into 2 subtypes (ab) MBGrp3 andMBGrp4into 3 subtypes each (abc)11 The subtypes iden-tified in these 2 studies overlap considerably and themain differences seem to be related to the inclusion ofadult MB patients in the Cavalli study Importantly MBsubgroups and their subtypes identified by their
Brain Tumor Epigenetics From Research to Clinical Practice Volume 2 Issue 3
102
epigenetic and related transcriptional profiles1011 havedistinct genetic and clinicopathological features1011 andtheir implementation for patient stratification for betterprognostication and enrollment into subgroupsubtype-directed therapies in the context of clinical trials will be astep change in the treatment of MB patients
All CNS tumors A classification tool for brain tumorsbased on genome-wide DNA methylation patterns and arandom forest-based machine learning approach hasbeen developed and extensively tested by the GermanCancer Research Center (wwwmolecularneuropathologyorg) This resource is available online and has provento be a valuable tool to improve brain tumor diagnosticsThis approach has facilitated the identification of com-mon druggable molecular pathway alterations across var-ious histological tumor entities thus allowing patients toenter the most appropriate clinical trials and in somecases be offered molecularly matched therapies As anexample DNA methylation profiles allow precise identifi-cation of cases with mitogen-activated protein kinase(MAPK) activation which is a feature of tumors withBRAF V600E mutation1213 which can span various tradi-tional histological entities such as pilocytic astrocytomaspleomorphic xanthoastrocytomas ganglioglioma andsubependymal giant cell astrocytomas to predict re-sponse to specific inhibitors interrupting the BRAFMEKcomponent of the MAP kinase pathway14
Novel TherapeuticApproaches TargetingEpigeneticDeregulationDiffuse intrinsic pontine glioma (DIPG) is a highlyaggressive pediatric tumor located in the brainstem andcharacterized by a rapid and diffusely infiltrative patternof growth These tumors cannot be treated surgicallybecause of their location and infiltrative nature15
Radiation therapy is the standard treatment although itprovides only temporary symptom relief with no overallsurvival benefits and conventional chemotherapy drugsare ineffective15
Mutations in histone H3 variants occur in more than 80of DIPG and result in a lysine-to-methionine substitution(H3K27M)16 17 H3K27M has been shown to inhibitpolycomb repressive complex 2 (PRC2) by binding to itscatalytic subunit EZH2 and reducing the methylation ofH3 at lysine 27 (H3K27me) at selected target loci18 Theresidual PRC2 activity is required to maintain DIPGproliferative potential by repressing neuronaldifferentiation in patient-derived cell lines and in agenetically engineered mouse model1920 Importantlysmall-molecule EZH2 inhibitors abolish tumor cell growth
in these models raising the possibility that inhibitionof EZH2 could be a novel therapeutic strategy for thesetumors19
An independent study showed that H3K27M associateswith increased H3K27 acetylation (H3K27ac) and that themajority of the heterotypic H3K27M-K27ac nucleosomesco-localize with bromodomain proteins at the loci of ac-tively transcribed genes20 The authors have shown thatblocking the recruitment of bromodomain proteins by het-erotypic H3K27M-K27ac nucleosomes in DIPG with bro-modomain and extraterminal domain family inhibitorsefficiently inhibited tumor progression thus identifying thisclass of compounds as potential therapeutics in DIPG20
These important advances in understanding the underly-ing biology of DIPG have led to the identification of novelepigenetic therapeutic approaches which are very effec-tive at the preclinical level and if confirmed in transla-tional studies could change the way we treat thesetumors in the near future
Conclusion and outlookThese are exciting and challenging times for theneuro-oncology community Exciting because there isgrowing expectation in the field that new discoveriessuch as those discussed in this article can soon translateinto new and more effective therapeutic approachesChallenging because it is clear that new skill sets are re-quired to effectively apply them to benefit patients
The clinical training in many neuro-oncology specialtieswill have to take into account the additional knowledgeand skills needed in the field and offer education incomplementary disciplines such as next-generationsequencing technologies integrated with interpretativedata analysis as well as molecular biology for the designof biologically informed assays and tools The require-ment for these new highly specialized skills also needs tobe reflected in the composition of the clinical teamswhere bioinformatics expertise will play an increasinglyimportant role for the integration of multimodal data inpatient care
References
1 Waddington CH Canalization of development and the inheritance ofacquired characters Nature 1942150563ndash565
2 Allis CD Jenuwein T The molecular hallmarks of epigenetic controlNat Rev Genet 201617487ndash500
3 Flavahan WA Gaskell E Bernstein BE Epigenetic plasticity and thehallmarks of cancer Science (New York NY 2017357
4 Edwards JR Yarychkivska O Boulard M Bestor TH DNA methyla-tion and DNA methyltransferases Epigenetics amp chromatin20171023
5 Filbin MG Suva ML Gliomas genomics and epigenomics arriving atthe start and knowing it for the first time Annual Rev Pathol201611497ndash521
6 Hegi ME et al MGMT gene silencing and benefit from temozolomidein glioblastoma N Engl J Med 2005352997ndash1003
Volume 2 Issue 3 Brain Tumor Epigenetics From Research to Clinical Practice
103
7 Pajtler KW et al Molecular Classification of Ependymal Tumorsacross All CNS Compartments Histopathological Grades and AgeGroups Cancer Cell 201527728ndash743
8 Pajtler KW et al The current consensus on the clinical managementof intracranial ependymoma and its distinct molecular variants ActaNeuropathol 20171335ndash12
9 Taylor MD et al Molecular subgroups of medulloblastoma the cur-rent consensus Acta Neuropathol 2012123465ndash472
10 Schwalbe EC et al Novel molecular subgroups for clinical classifi-cation and outcome prediction in childhood medulloblastoma a co-hort study Lancet Oncol 201718958ndash971
11 Cavalli FMG et al Intertumoral Heterogeneity withinMedulloblastoma Subgroups Cancer Cell 201731737ndash754 e736
12 Schindler G et al Analysis of BRAF V600E mutation in 1320 nervoussystem tumors reveals high mutation frequencies in pleomorphicxanthoastrocytoma ganglioglioma and extra-cerebellar pilocytic as-trocytoma Acta Neuropathol 2011121397ndash405
13 Tanaka S et al Epithelioid glioblastoma arising from pleomorphicxanthoastrocytoma with the BRAF V600E mutation Brain TumorPathol 201431172ndash176
14 Banerjee A et al A phase I trial of the MEK inhibitor selumetinib(AZD6244) in pediatric patients with recurrent or refractory low-grade glioma a Pediatric Brain Tumor Consortium (PBTC) studyNeuro Oncol 2017191135ndash1144
15 Hargrave D Bartels U Bouffet E Diffuse brainstem glioma in chil-dren critical review of clinical trials Lancet Oncol 20067241ndash248
16 Schwartzentruber J et al Driver mutations in histone H33 and chro-matin remodelling genes in paediatric glioblastoma Nature2012482226ndash231
17 Wu G et al Somatic histone H3 alterations in pediatric diffuse in-trinsic pontine gliomas and non-brainstem glioblastomas Naturegenetics 201244251ndash253
18 Lewis PW et al Inhibition of PRC2 activity by a gain-of-function H3mutation found in pediatric glioblastoma Science (New York NY2013340857ndash861
19 Mohammad F et al EZH2 is a potential therapeutic target forH3K27M-mutant pediatric gliomas Nature Med 201723483ndash492
20 Piunti A et al Therapeutic targeting of polycomb and BET bromodo-main proteins in diffuse intrinsic pontine gliomas Nature Med201723493ndash500
Brain Tumor Epigenetics From Research to Clinical Practice Volume 2 Issue 3
104
The Value of SurgicalResection for MalignantGliomas in the ModernEra Beyond Extent ofResection
Stephen G Bowden MDSeunggu Jude Han MDDepartment of Neurological Surgery OregonHealth and Sciences University 3303 SW BondAve Center for Health and Healing CH8NPortland OR 97239 Telephone 503-494-4314Fax 503-346-6810 hanseohsuedu
105
Malignant gliomas are among the most difficult oncologi-cal entities to treat Despite aggressive treatment prog-nosis remains poor and recurrence and treatmentfailures seem inevitable The current standard-of-caretherapy includes maximal safe surgical resection fol-lowed by concurrent and adjuvant chemoradiotherapyHistorically surgical resection has conferred greater sur-vival benefit to these patients than adjuvant therapiespresumably through the cornerstone principle of cytore-duction However the extent of surgical resection is fre-quently limited by nearby eloquent tissue and risks to keyneurological functions In addition the value of such ag-gressive approaches has been questioned in light of thewidespread infiltration of glioma cells Meanwhile our un-derstanding of glioma biology continues to advance rap-idly fueled in large part by the acquisition of tumor tissueduring surgery Thus the exact role and value of surgeryparticularly in comparing the clinical benefits of maximalextent of resection (EOR) with the biomedical benefits oftissue provision has been a topic of great interest anddebate in both the neuro-oncological and neurosurgicalcommunities
EOR patient age tumor histology performance statusand molecular markers have been widely accepted assignificant predictors of patient outcomes in malignantglioma9 In the past 2 decades many large retrospectivecohort studies have demonstrated improvements in sur-vival with increasing EOR5917 Due to ethical considera-tions evidence from a randomized prospective studysupporting the clinical benefit of aggressive resectionsdoes not exist and likely never will Instead the closestthing to such evidence in malignant glioma comes fromthe randomized phase III trial comparing surgical resec-tions with or without the use of 5-aminolevulinic acid(5-ALA) The use of 5-ALA serving as a means to and aproxy for greater EOR resulted in extended overall sur-vival for patients with newly diagnosed glioblastoma19 Arecent meta-analysis of 41 117 unique patients by Brownet al adherent to the guidelines of PRISMA (PreferredReporting Items for Systematic Reviews and Meta-Analyses) also demonstrated a clear survival benefit forgross total resection over subtotal resection or biopsy atupfront surgery for glioblastoma1 The body of literatureas a whole clearly favored aggressive resections andthere seemed to be little disagreement for a strategytoward maximal resection when clinically feasibleHowever the challenge still remains when such strategiescome at the risk of neurological morbidity A recent reportby Rahman et al illustrates that the survival benefits fromaggressive resection are lost if the patient develops anew postoperative neurologic deficit as a result15
All the while our understanding of glioma genetics mo-lecular biology and mechanisms of resistance has con-tinued to deepen and evolve borne of thoughtful andsystematic studies using patient-acquired tumor sam-ples Molecular profiles and tumor genetics have proventhemselves to be the best predictors of clinical behaviorand now represent crucial components of the diagnostic
classification scheme of infiltrating gliomas12 With tumortissue at the molecular and genetic level being able to ro-bustly predict patient outcomes accurate tissue diagno-sis has become paramount in the management ofgliomas The role and value of open surgical resection to-ward this end have become clearer as concerns of sam-pling error with biopsy alone led to a number of studiesevaluating the ldquoaccuracyrdquo of stereotactic biopsy proce-dures Jackson et al reported a series of 81 patients whounderwent stereotactic biopsy followed by open surgicalresection The tissue diagnosis was concordant betweenbiopsy and open resection samples in only 51 ofpatients6 Other studies have also demonstrated diagnos-tic concordance between stereotactic biopsy and surgi-cal resection samples in only 57 to 79 ofcases131428 The major limitation of stereotactic biopsyfor infiltrating gliomas likely stems from the significantintratumoral heterogeneity and collectively these studieshighlight the value of open surgical resection in providinga more global representation and understanding of thetumor tissue
The value of extensive resection is perhaps even moreprofound when considering the therapeutic implicationsof such heterogeneity Multiple-site and serial-samplinganalyses have revealed a high degree of both spatial andtemporal heterogeneity within these tumors a conse-quence of serial evolutionary events during tumor growthand progression23 These studies have also led to theconcept of therapy-driven clonal selection and preferen-tial regrowth of resistant cell populations as a potentialmechanism of treatment failure Efforts to expand our un-derstanding of the tremendously complex network ofmutations and biological consequences of chronologicalhierarchy would be greatly facilitated by carefullyplanned thoughtful acquisition of tumor samples duringsurgery
Despite the recent paradigm shift in glioma diagnosticclassification little gains have been made in improvingthe overall prognosis for patients with malignant gliomassince the introduction of concurrent and adjuvant temo-zolomide in 200521 The strategies more recently tested inlarge randomized phase III trials by and large have yieldeddisappointing results while the reasons and mechanismsof treatment failures remain unclear Even so encourag-ing responses have occasionally been seen in varioussubsets of patients and studies exploring the presenceof potential biomarkers have generated intriguing andpromising results in these populations The developmentof the antindashvascular endothelial growth factor monoclonalantibody bevacizumab is one such example Two initialphase II trials showed prolonged progression-free sur-vival in recurrent glioblastoma relative to historical con-trols prompting the US Food and Drug Administration togrant accelerated approval to bevacizumab for recurrentglioblastoma in 2009825 However 2 large randomized tri-als evaluating the addition of bevacizumab to radiationand temozolomide in the newly diagnosed setting failedto show a benefit in overall survival24 and its utility in the
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
106
recurrent setting is now a topic of debate in light of sub-sequent phase III trial results However a post hoc analy-sis of patients enrolled in the AVAglio trial recentlydemonstrated that bevacizumab improved overall sur-vival for those with a proneural subtype tumor18 Just asO6-methylguanine-DNA-methyltransferase (MGMT) pro-moter methylation does for temozolomide the geneticprofile of the tumor could serve as a potential biomarkerof clinical response for bevacizumab as well and valida-tion studies are currently ongoing Such analyses al-though performed post hoc require targeted prospectivecollection of tumor tissue at initial surgery In addition ge-netic profiling of newly diagnosed malignant gliomas willneed to become routine if this approach is to be utilizedwidely Similarly cilengitide an inhibitor of aVb3 andaVb5 integrins with anti-angiogenic properties showedinitial promise in recurrent glioblastoma studies but failedto show any additional benefit in the newly diagnosedsetting20 A subsequent post hoc analysis of the phase IItrial revealed improved progression-free and overall sur-vival in patients with high aVb3 levels in the tumor cells26
However tumor tissues were not systematically collectedand less than half of the patientsrsquo tumor tissues wereavailable for analysis from the phase III trialUnfortunately this drug will most likely not undergo fur-ther development and one cannot help wonder if the out-come would have been different if the enrollment in thephase III trial had been enriched for or restricted to tumorswith high expression of the aVb3 integrin The only trueldquosuccess storyrdquo since the adaptation of radiation andtemozolomide has come from the novel approach of tu-mor treating fields (TTFields) a transcutaneous deliveryof low-intensity intermediate frequency alternating elec-tric fields The multicenter phase III trial EF-14 random-ized patients with supratentorial glioblastoma withoutevidence of tumor progression following standard che-moradiation to receive maintenance treatment withTTFields plus temozolomide or temozolomide alone22
The study was terminated early based on results of aplanned interim analysis demonstrating benefit inprogression-free survival overall survival a secondaryendpoint was also significantly enhanced at this timeDespite the trialrsquos success TTFields has not been univer-sally adopted by the neuro-oncology community andenthusiasm among clinicians and patients remains low27
Experts have raised concerns regarding the study designsuch as its open-label design lacking a sham-treatmentcontrol arm as well as the generalizability of the resultsbased on the unique randomization point occurring afterconcurrent chemoradiation16 Perhaps most significantlya lack of widely understood mechanism of action hasalso been raised as a factor with comparison to othertreatments the preclinical data for TTFields is relativelylacking particularly when applied in conjunction with che-moradiation27 Even during the early phase stages theuse of robust tissue-based analyses exploring the mech-anism of action such as dose response modeling andmultisite tissue biopsies may have mitigated some of
these concerns and led to wider acceptance by the com-munity Bevacizumab and cilengitide clearly benefitedfrom retrospective analyses of human tumor tissue toidentify susceptible treatment populations while the en-thusiasm for TTFields is perhaps in part tempered by thelack thereof Collectively the evolution of these treat-ments underscores the value of extensive targeted tissuesampling in furthering development of new adjunctivetherapies
Open surgical resection of tumors with such targeted tis-sue acquisition for analysis will continue to play a key rolein prospective clinical trial designs Comparison ofpretreatment and posttreatment tissue profiles representsa valuable line of investigation by delving into mecha-nisms of therapeutic action as well as mechanisms oftreatment failures1011 It also provides an opportunity toinvestigate a number of key fundamental steps along anagentrsquos path to clinical success such as does the agentsuccessfully traffic to the tumor if so how much anddoes the agent then actually have its hypothesizedeffects at the biochemical or cellular level Thusearly-phase trials can and should include posttreatmentmolecular endpoints when possible in addition to safetyendpoints Immunotherapy and immune checkpoint inhi-bition represent exciting novel therapeutic approachesfor neuro-oncology particularly based on their success inmetastatic cancers Large phase III trials studying block-ade of the programmed cell death protein (PD)1PDligand 1 axis with monoclonal antibodies for newlydiagnosed and recurrent glioblastoma are under way butinitial reports have been concerning for negative resultsAs in the development of many previous novel agentstissue-based mechanism studies have been largely lack-ing in the preclinical phases However an Alliance-supported trial currently enrolling focuses on a biomarkeras a primary endpoint patients with recurrent glioblas-toma indicated for surgery are randomized to receivepembrolizumab a PD1 inhibitor either before or aftersurgery (NCT02852655) The resected tumor tissue willthen be analyzed for the profile of tumor-infiltratingT cells and comparison will be made between the 2groups This study represents a tremendously valuableopportunity to explore the impact and the potential chal-lenges of checkpoint inhibition for malignant gliomas inthe clinical setting and should the large phase III trialsend up negative this pilot study will be very informative
Advances in imaging biomarkers and molecular charac-terization of gliomas in conjunction with new targetedtherapies will continue to improve and transform themanagement of these tumors Multimodality imaging cannow more accurately reflect ongoing biological processeswithin these tumors such as the presence of oncogenicmutations or cells undergoing malignant transformationNovel biomarkers such as circulating tumor DNA showpromise in detecting early recurrence or monitoring treat-ment response3724 Lastly the new classification schemerevolving around molecular characterization will provide a
Volume 2 Issue 3 The Value of Surgical Resection for Malignant Gliomas in the Modern Era
107
necessary corollary to these novel diagnostic tools Itremains indisputable however that clinical validation ofthese novel diagnostic tools will also require systematiccorrelation with human tumor tissue obtained throughsurgery These samples ideally gathered prospectivelywill provide a pivot upon which we can expand our under-standing of the complex network of oncological pro-cesses driving these tumors
Malignant gliomas are incredibly challenging disease en-tities in many ways due to the inter- and intratumoral het-erogeneity that is a hallmark of them Experience to datehints that future successes in malignant gliomas rest inneuro-oncology entering the era of precision medicinewhere validated biomarkers and targeted personalizedtherapies are seamlessly integrated into the managementparadigm Accordingly systems supporting surgical re-section and patient-specific tumor tissue analysis mustbe built and organized to guide the decision making fortherapy As our overall approach to the management ofmalignant gliomas evolves so should the framework ofsurgical management The clinical benefits of maximalsafe resection are well founded and well reportedHowever the oncological neurosurgeon must now lookbeyond maximal cytoreduction itself and recognize thevalue of thoughtful acquisition and analysis of tumor tis-sue Modern neurosurgeons must consider themselvessurgical neuro-oncologists and engagement and partici-pation of surgeons into clinical trials particularly early-phase trials should be encouraged and valued In turnwe should provide our surgical trainees with the trainingand tools in neuro-oncology to help them participate andcontribute in multidisciplinary collaborative efforts aimingto advance the understanding of brain tumor biology andultimately improve the outlook of our patients
References
1 Lacroix M Abi-Said D Fourney DR Gokaslan ZL et al A multivariateanalysis of 416 patients with glioblastoma multiforme prognosisextent of resection and survival J Neurosurg 2001 95190ndash198
2 Hervey-Jumper SL Berger MS Maximizing safe resection of low-and high-grade glioma J Neurooncol 2016 130269ndash282
3 Sanai N Polley MY McDermott MW Parsa AT Berger MS An ex-tent of resection threshold for newly diagnosed glioblastomas JNeurosurg 2011 1153ndash8
4 Stummer W Pichlmeier U Meinel T et al Fluorescence-guided sur-gery with 5-aminolevulinic acid for resection of malignant glioma arandomised controlled multicentre phase III trial Lancet Oncol2006 7392ndash401
5 Brown TJ Brennan MC Li M et al Association of the extent ofresection with survival in glioblastoma a systematic review andmeta-analysis JAMA Oncol 2016 21460ndash1469
6 Rahman M Abbatematteo J De Leo EK et al The effects of new orworsened postoperative neurological deficits on survival of patientswith glioblastoma J Neurosurg 2017 127123ndash131
7 Louis DN Perry A Reifenberger G et al The 2016 World HealthOrganization Classification of Tumors of the Central NervousSystem a summary Acta Neuropathol 2016 131803ndash820
8 McGirt MJ Bulsara KR Cummings TJ et al Prognostic value ofmagnetic resonance imaging-guided stereotactic biopsy in the
evaluation of recurrent malignant astrocytoma compared with a le-sion due to radiation effect J Neurosurg 2003 9814ndash20
9 Muragaki Y Chernov M Maruyama T et al Low-grade glioma onstereotactic biopsy how often is the diagnosis accurate MinimInvasive Neurosurg 2008 51275ndash279
10 Woodworth G McGirt MJ Samdani A Garonzik I Olivi AWeingart JD Accuracy of frameless and frame-based image-guided stereotactic brain biopsy in the diagnosis of glioma com-parison of biopsy and open resection specimen Neurol Res 200527358ndash362
11 Suzuki H Aoki K Chiba K et al Mutational landscape and clonal ar-chitecture in grade II and III gliomas Nat Genet 2015 47458ndash468
12 Stupp R Mason WP van den Bent MJ et al Radiotherapy plus con-comitant and adjuvant temozolomide for glioblastoma N Engl JMed 2005 352987ndash996
13 Kreisl TN Kim L Moore K et al Phase II trial of single-agent bevaci-zumab followed by bevacizumab plus irinotecan at tumor progres-sion in recurrent glioblastoma J Clin Oncol 2009 27740ndash745
14 Vredenburgh JJ Desjardins A Herndon 2nd JE et al Phase II trial ofbevacizumab and irinotecan in recurrent malignant glioma ClinCancer Res 2007 131253ndash1259
15 Chinot OL Wick W Mason W et al Bevacizumab plusradiotherapy-temozolomide for newly diagnosed glioblastomaN Engl J Med 2014 370709ndash722
16 Gilbert MR Dignam JJ Armstrong TS et al A randomized trial ofbevacizumab for newly diagnosed glioblastoma N Engl J Med2014 370699ndash708
17 Sandmann T Bourgon R Garcia J et al Patients with proneural glio-blastoma may derive overall survival benefit from the addition of bev-acizumab to first-line radiotherapy and temozolomide retrospectiveanalysis of the AVAglio trial J Clin Oncol 2015 332735ndash2744
18 Jackson RJ Fuller GN Abi-Said D et al Limitations of stereotacticbiopsy in the initial management of gliomas Neuro Oncol 20013193ndash200
19 Stupp R Hegi ME Gorlia T et al Cilengitide combined with stan-dard treatment for patients with newly diagnosed glioblastoma withmethylated MGMT promoter (CENTRIC EORTC 26071-22072study) a multicentre randomised open-label phase 3 trial LancetOncol 2014 151100ndash1108
20 Weller M Nabors LB Gorlia T et al Cilengitide in newly diagnosedglioblastoma biomarker expression and outcome Oncotarget2016 715018ndash15032
21 Stupp R Taillibert S Kanner AA et al Maintenance therapy withtumor-treating fields plus temozolomide vs temozolomide alone forglioblastoma a randomized clinical trial JAMA 20153142535ndash2543
22 Wick W TTFields where does all the skepticism come from NeuroOncol 2016 18303ndash305
23 Sampson JH Alternating electric fields for the treatment of glioblas-toma JAMA 2015 3142511ndash2513
24 Lang FF Asher A Prospective clinical trials of brain tumor therapy thecritical role of neurosurgeons J Neurooncol 2004 69151ndash167
25 Lang FF Gilbert MR Puduvalli VK et al Toward better early-phasebrain tumor clinical trials a reappraisal of current methods and pro-posals for future strategies Neuro Oncol 2002 4268ndash277
26 Elkhaled A Jalbert L Constantin A et al Characterization of metab-olites in infiltrating gliomas using ex vivo (1)H high-resolution magicangle spinning spectroscopy NMR Biomed 2014 27578ndash593
27 Jalbert LE Neill E Phillips JJ et al Magnetic resonance analysis ofmalignant transformation in recurrent glioma Neuro Oncol 2016181169ndash1179
28 Touat M Duran-Pena A Alentorn A Lacroix L Massard C Idbaih AEmerging circulating biomarkers in glioblastoma promises andchallenges Expert Rev Mol Diagn 2015 151311ndash1323
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
108
Update on RadiationCombinations in theTreatment of Patientswith Malignant BrainTumors FromRadiosensitizers toImmunotherapy
Debra Nana Yeboa MD1
Erik P Sulman MD PhD123
Departments of 1Radiation Oncology2Translational Molecular Pathology and3Genomic Medicine The University of Texas MDAnderson Cancer Center 1515 Holcombe BlvdUnit 97 Houston Texas USA Tel 713-563-2300dnyeboamdandersonorg andepsulmanmdandersonorg
109
AbstractAdvances in radiosensitizers and immunotherapyhave ushered in a new frontier in brain tumortreatment The brain has often been viewed as asanctuary site due to the bloodndashbrain barrier andthus the 2 primary modalities of therapy includedsurgery and radiation therapy (RT) More recentlysystemic therapies have played a greater role aseither combination therapy radiosensitizers or im-munotherapy Two novel radiosensitizers are beingdeveloped for the treatment of brain metastasesRRx-001 for example is a small molecule thataccelerates the NO2 to NO conversion of deoxyhe-moglobin and the agent 2-dexoyglucose (2-DG) is anonmetabolized glucose analogue that interfereswith ATP formation Poly(ADP-ribose) DNA polymer-ase inhibitors are promising due to their distinctradiobiological effects Veliparib and olaparib areamong the most studied with randomized trialsexploring their use in gliomas and brain metastasesImmunotherapy including immune checkpoint inhib-itors may play a role for both primary gliomas andbrain metastases RT has been shown to enhancethe function of cytotoxic T lymphocytes induce infil-tration of cytotoxic T lymphocytes and enhancefunction Trials are presently exploring use of bothprogrammed cell death protein (PD)1 and PD ligand1 blockade in glioblastoma patients with radiationSimilarly several immunotherapies are being investi-gated with either stereotactic radiosurgery or wholebrain radiation therapy for brain metastases In thisreview the use of radiosensitizers and immunother-apy agents with RT will be discussed broadly
Keywords brain metastases brain tumors gliomasimmunotherapy radiation therapy radiosensitizers
Radiosensitizers andImmunotherapy inBrain TumorsAdvances in radiosensitizers and immunotherapy haveushered in a new frontier to brain tumor treatment Braintumors however are a diverse class sharing only similaranatomic location Both primary brain malignancies andbrain metastasis have widely diverse histologies and mo-lecular phenotypes With the bloodndashbrain barrier thebrain has often been viewed as a sanctuary site and thusthe 2 primary modalities of therapy included surgery andradiation with decreased benefit from systemic agentsdue to lack of brain penetration However more recentlysystemic therapies have played a greater role as eithercombination therapy radiosensitizers or immunother-apy While temozolomide (TMZ) has played a pivotal rolefor glioblastoma (GBM) only a subset of patients benefitfrom the treatment1 The use of alternative systemicagents that may potentiate the effects of radiation ther-apy (RT) is becoming increasingly appealing Similarly forbrain metastases a variety of systemic agents are beingexplored primarily based on histology and immune pro-file In this review the use of radiosensitizers and immu-notherapy agents currently under investigation with RTwill be discussed
RadiosensitizersThe guiding concept of radiation sensitization is to in-crease the biologic effect of radiation such as increasedDNA damage decreased DNA repair decreased hypoxiaor increased G2M cell cycle blockade leading to im-proved tumor control and increased patient survival2
Poly(adenosine diphosphate-ribose) DNA polymerase(PARP) inhibitors are promising radiosensitizers due totheir roles in DNA repair3 PARP inhibitors work againstPARP1 a nuclear enzyme involved in the recruitment ofrepair proteins used in base excision repair and single-strand break repair PARP1 may also play a role in nonho-mologous end-joining4 The primary investigation ofPARP inhibitors has been in potentiating radiation andchemotherapy effects the latter in the context of homolo-gous repair deficient tumors For radiation the primarymechanism of action is inducing damage to nucleotidesleading to single-strand and double-strand breaks ThusPARP inhibitors in combination with radiation have an ap-pealing mechanism to inhibit or delay DNA repair andlikely convert more single-strand breaks to double-strandbreaks4
While several PARP inhibitors are currently being evalu-ated in a variety of tumors including talazoparib and nira-parib veliparib and olaparib are among the most studiedand there are randomized trials exploring their use in
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
110
gliomas The US National Cancer Institute (NCI)ndashfundedAlliance for Clinical Trials in Oncology (Alliance) A071102is a randomized phase IIIII trial evaluating the use ofveliparib in combination with TMZ in the adjuvant settingin patients with GBM tumors exhibiting hypermethylationof the O6 methylguanine DNA methyltransferase (MGMT)gene promoter Preclinical data supporting this trial sug-gested that only patients with MGMT methylated tumorswould benefit from the combination a group of patientsfor whom TMZ concurrent with radiation might be mostbeneficial5 A phase I trial performed by the NCI-fundedAmerican Brain Tumor Consortium attempted to combineveliparib with radiation and TMZ but failed to identify asuitable recommended phase II dose due to significanthemotoxicity6 Thus attempts to combine radiation withveliparib have focused on patients least likely to benefitfrom TMZ namely with MGMT unmethylated tumors forwhom TMZ could be withheld The Australian VeliparibRT and TMZ trial in newly diagnosed unmethylatedMGMT glioblastoma (VERTU) is a single-arm study inwhich patients receive RT with veliparib followed by adju-vant TMZ and veliparib4
An ongoing novel approach to radiosensitize gliomasinvolves a combination with an agent that interferes withan essential metabolic process 2-Dexoyglucose (2-DG)is a nonmetabolized glucose analogue that acts as acompetitive inhibitor of glycolysis It is transported acrossthe bloodndashbrain barrier by the glucose transporter GLUT-1 and thus has good penetration into the CNSIntracellularly it is trapped and accumulates in cells simi-lar to the mechanism of 18-fluorodeoxyglucose 2-DG isphosphorylated by glycolytic enzymes and the
phosphorylated 2-DG (2-deoxyglucose-P) is trapped in-tracellularly Inhibition of hexokinase activity by 2-DGinterferes with ATP formation and results in tumor celldeath7 While it has positive attributes by selectively tar-geting metabolically active tumor cells 2-DG has alsobeen associated with Q-T prolongation The currentphase III trial in gliomas is assessing the toxicity and tol-erability of 2-DG with hypofractionated radiation of 5 Gyas a radiosensitizer7
Two novel radiosensitizers are being developed for thetreatment of brain metastases First RRx-001 is a smallmolecule initially designed by the aerospace industry Itworks in part as a radiosensitizer by increasing blood flowand thus oxygenation of tumors through nitric oxideRRx-001 which binds to hemoglobin accelerates theNO2 to NO conversion of deoxyhemoglobin It workslocally under hypoxic conditions and subsequentlythe radiosensitive effects through nitric oxide are invasodilation and inhibiting DNA repair enzymes8 Nitricoxide is relatively benign The higher levels of oxidativestress with H2O2 and superoxide in tumors in comparisonto normal tissues result in the preferential generation ofreactive peroxynitrite in the presence of higher nitric oxidelevels7 This accounts for the increased specificity anddecreased toxicity with RRx-001 The dose limiting toxic-ity in a phase I trial of 25 patients treated with eitherweekly or biweekly infusions was infusional pain relatedto the release of NO at the site of injection7 Outside ofpreclinical models 2 clinical reports examining wholebrain radiation therapy (WBRT) with RRx-001 reported anintracranial response A patient with melanoma and 2hemorrhagic edematous lesions of 26 cm and 33 cm
Table 1 Clinical trials involving immunotherapy and radiation therapy1213
Clinical Trials Number Phase Disease Type Treatment Groups
NCT02667587 II Newly diagnosed GBMMGMT-methylated
Nivolumabthorn TMZthorn RT vs placebothornTMZ thorn RT
NCT02617589 III Newly diagnosed GBM Nivolumabthorn RT vs TMZthorn RTNCT02336165 II Newly diagnosed unmethylated
MGMT recurrent glioblastomaMEDI4736thorn standard RT vs MEDI4736 thorn
bevacizumabNCT02530502 III Newly diagnosed GBM RTthorn TMZthorn pembrolizumab TMZthorn
pembrolizumabNCT02313272 I Recurrent glioma Hypofractionated stereotactic radiationthorn
pembrolizumab thorn bevacizumabNCT02696993 III Brain metastases Nivolumabthorn SRS nivolumabthornWBRT
nivolumabthorn ipilimumab thorn SRS nivolu-mabthorn ipilimumab thornWBRT
NCT02115139 II Melanoma brain metastases Ipilimumab thornWBRTNCT02097732 II Melanoma brain metastases Ipilimumab SRS ipilimumab vs SRS
ipilimumabNCT01703507 I Melanoma brain metastases Ipilimumab thornWBRT vs ipilimumab thorn SRSNCT02107755 II Melanoma brain metastases Ipilimumab thorn SRSNCT02858869 pilot Melanoma and NSCLC Pembrolizumabthorn SRSNCT01950195 I Melanoma brain metastases Ipilimumab thorn SRSNCT02662725 II Melanoma brain metastases Ipilimumab thorn SRS
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
111
after a single intravenous dose of RRx-001 of 5 mgm2 4days before WBRT resulted in symptomatic improvementwithin 48 hours By 4 months after radiation there was areduction in size in the largest dimension down to 10 cmand 23 cm of the respective lesions A second report of amelanoma patient with at least 18 lesions after receivingRRx-001 of 5 mgm2 4 days before WBRT as well astwice weekly doses during the 2 weeks of radiation alsoshowed response The patient at 4 months had disap-pearance of 13 of 18 lesions with shrinkage of theremaining 5 lesions8 Presently BRAINSTORM is a phaseIII dose escalation trial of RRx-001 designed to be ad-ministered twice weekly for 2 weeks with WBRT (30 Gy in10 fractions) with the option for weekly maintenance8
Veliparib has also been evaluated in the setting of brainmetastases It was tested in a global randomized con-trolled trial with WBRT Veliparib is orally bioavailable andcrosses the bloodndashbrain barrier It was first examined in amultihistology phase I trial in patients with nonndashsmall celllung cancer (NSCLC) breast cancer melanoma and re-nal and colorectal cancers among others The study of81 patients tested dose tolerance of veliparib from 10 to300 mg orally twice a day with WBRT to 30 Gy in 10 frac-tions or 375 Gy in 15 fractions9 The phase I trial dose es-calation portion did not reach the predefined criteria forthe maximum tolerated dose but there was amplificationof the adverse effects of nausea and vomiting among thehighest dose cohort of 300 mg bid9 The adverse eventprofile at 200 mg bid was similar to that of WBRT aloneDoses of veliparib from 20 to 200 mg bid demonstratesimilar antitumor activity and other studies in preclinicalmodels found that 50 mg daily demonstrated significantreduction in poly(ADP-ribose) in peripheral blood mono-nuclear cells and tumor tissue while also effectivelycrossing the bloodndashbrain barrier Thus the subsequentphase II trial examined 50 mg with WBRT9 In order to as-sess a more homogeneous cohort the phase III globalrandomized trial studied only NSCLC at the 2 doses of50 mg and 200 mg twice daily versus placebo twice a daywith WBRT10 The primary endpoint was overall survivalIn 307 patients in a 111 randomization of 50 mg bid200 mg bid or placebo twice daily the study found nosignificant differences in overall survival among the differ-ent groups10 The majority of patients across the treat-ment groups had a graded prognostic assessment (GPA)score of25 and a Karnofsky performance status ofgt80 The median overall survival was 185 days forpatients receiving placebo and 209 days for those receiv-ing veliparib without any statistically significant differ-ence These results were similar to the disease-specificestimate of median survival for the disease-specific GPAof NSCLC patients with brain metastases10
Several other radiosensitizers have failed to improve overradiation alone in a number of trials These have includedtrials with WBRT including motexafin gadolinium efap-roxyn bortozemib thalidomide teniposide topotecanpaclitaxel and cisplatin7 Of note other PARP inhibitorsalso being assessed include talazoparib and niraparib4
which may yield positive results The use of valproic acid(VPA) as a histone deacetylase inhibitor has also beenconsidered to have radiosensitizing potential in additionto its anti-epileptic drug properties11 While studies havereported that patients with GBM receiving an anti-epilep-tic agent may have higher overall survival than those re-ceiving standard chemoradiation therapy alone thebenefit remains controversial Retrospective analysissuggested that patients taking VPA specifically had bettersurvival in comparison to other anti-epileptic drugs Alsoa recent prospective phase II trial was performed in 37patients with GBM receiving VPA 25 mgkg concurrentlywith TMZ chemoradiation and reported a median survivalof 296 months While controversial further data andinvestigation are needed into this and other agents thatmay potentiate RT
Immunotherapy and radiationImmune checkpoint inhibitors lead to activation of T cellswhich may traffic across the bloodndashbrain barrier to inter-act with tumor Primary brain tumors may evade the im-mune system through upregulation of immunecheckpoints and possible immunosuppression12
Monoclonal antibodies promote immune-mediated anti-tumor activity by inhibiting the immune functionndashmediated cytotoxic T-lymphocyte associated protein 4(CTLA-4) and programmed cell death protein 1 (PD-1)receptors PD protein ligand (PD-L1) is upregulated inGBM through oncogenic signaling possibly throughphosphatase and tensin homolog loss and interleukin-10signaling1314 RT has also been shown to enhance thefunction of cytotoxic T lymphocytes RT may induce aninfiltration of cytotoxic T lymphocytes and enhance theirfunction It may also induce antindashCTLA-4 agents inhibitingT-cell function and increasing the CD8thorn T cellregulatoryT cell ratio in cases of melanoma15 Thus PD-1 and PD-L1 blockers may have a further role in CNS managementwith the use of radiation
In preclinical models radiation has been examined withimmunotherapy that included among other mechanismsvaccination PD-1 blockade and CTLA-4 blockade Inmice radiation plus a vaccination of irradiated gliomacells was associated with increased survival of 40 to80 compared with 0 to 10 for other groups stud-ied16 A benefit of PD-1 blockade with stereotactic radio-surgery (SRS) specifically has also been shown in amouse model In comparison to mice treated with radia-tion antindashPD-1 therapy or a combination only those re-ceiving combination therapy had a higher percentagesurvival alive beyond 180 days after treatment17 Othermouse carcinoma models have identified response withanti-CTLA antibody and fractionated radiation therapy18
CD137 activation CTLA-4 blockade and focal radiationtherapy have been examined in an immunocompetent in-tracranial GBM model Mice treated with triple combina-tion therapy had 50 greater survival19 In other murine
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
112
models the use of antindashPD-1 and antindashCTLA-4 agentsshowed improved survival and increased tumor infiltratingleukocyte populations compared with single modalitywith concurrent radiation16 There are conflicting data re-garding timing or sequencing of therapy with some ani-mal models showing no difference in tumor response inrelation to timing of RT and delivery of immunotherapy18
For instance in one animal model CTLA-4 blockade de-livered simultaneously with radiation or delivered a coupleof days after showed no difference in survival among themice19
Increased PD-1 expression in circulating monocytes hasbeen identified as a biomarker for tumor-induced immu-nosuppression and may serve as a prognostic factor forpotentially worse survival outcomes in clinic13 In onestudy GBM patients with lower PD-L1 expression hadhigher median overall survival than those with higher PD-L1 expression suggesting that lower expression may beassociated with less immunosuppression and more im-mune activity against the tumor glioma20 RT with immunecheckpoint blockade is being investigated to assess if theaddition of PD-1 and PD-L1 inhibitors may improve theoutcomes or toxicity profile of standard therapy For in-stance a multi-institutional trial opened as a phase III willevaluate outcomes in GBM receiving radiation and pem-brolizumab with TMZ (NCT02530502) Next durvalumabor MEDI4736 a PD-L1 inhibitor is being examined forunmethylated MGMT GBMs with standard radiotherapy(NCT02336165)12 The impact of checkpoint inhibitorsduring adjuvant treatment of GBM is currently beingevaluated in the NCI-funded NRG-BN002 trial(NCT02311920) which will evaluate the antindashCTLA-4antibody ipilimumab alone or in combination with theantindashPD-1 antibody nivolumab for patients with newlydiagnosed GBM
Brain metastases have clonal populations of cells differ-ent from the rest of the brain and a unique microenviron-ment that may influence immunotherapy There may bemore immune infiltrates in metastases than in primarybrain tumors21 PD-L1 expression in brain metastasesvaries by histology In a series evaluating PD-L1 expres-sion in various tumors including melanoma NSCLCbreast renal colorectal and small cell less than 10showed significant expression22 There was greatest ex-pression among NSCLC and melanoma with a correla-tion between PD-L1 expression and tumor infiltratinglymphocytes22 Institutional series have examined thecombination of radiation and immune checkpoint block-ade In another study specific to melanoma brain metas-tases PD-L1 expression was found in over 50 of thecases and among those cases over 40 expressedPD-L1 in more than 5 of tumor cells23 The largest bodyof data for use of PD-L1 with radiation is for melanomaand NSCLC
Ipilimumab is a human monoclonal antibody that blocksCTLA-4 and allows for T-cell activation and proliferationto enhance the immune response to cancer In a
retrospective review of 70 patients with brain metastasestreated with SRS or WBRT the 33 patients receiving im-munotherapy had a median survival of 183 months incomparison to the 37 patients who did not receive ipili-mumab with a median survival of 53 months While therewere limited data among the cohort to evaluate sequenc-ing of therapy among 10 evaluable patients 40 whoreceived ipilimumab prior to RT had a partial response incomparison to only 10 among the cohort of 22 evalu-able patients who did not receive ipilimumab therapy atall with radiation24 Another retrospective institutionalstudy of 77 patients in which 37 received ipilimumabfound that patients treated with SRS and ipilimumab hada median survival of 213 months versus 49 months forthose not receiving ipilimumab Most interestingly theyidentified that the correlation remained significant evenafter adjusting for additional factors such as performancestatus Secondly there was not an increased need for useof salvage WBRT25
The sequencing of radiotherapy and immune checkpointinhibitors is of interest In a study of patients with brainmetastases the one-year survival for patients receivingSRS before ipilimumab was greater at 65 in contrast to56 for those receiving it concurrently and 40 for thosereceiving it after SRS26 Similarly another study of 75patients with 566 brain metastases showed greater tu-mor lesion response at 6 months from SRS for patientsreceiving ipilimumab nivolumab or pembrolizumabwithin 4 weeks of their SRS27 Those receiving concurrenttherapy had by 6 months a decrease of 949 in compar-ison to 662 for those not receiving checkpoint inhibi-tors within 4 weeks Prospective clinical trials areinvestigating different combinations of RT with immunecheckpoint blockers in this setting For instance new tri-als are currently evaluating intracranial tumor control at 6months and the timing of immune therapy or immunecheckpoint inhibitors in relation to SRS28
Vaccines are also being developed for primary braintumors showing some evidence for their use Vaccinesdeveloped from dendritic cells and tumor lysate with tu-mor antigens such as the epidermal growth factor recep-tor variant III vaccine have shown promise29 Forinstance in a placebo controlled phase II trial of ICT-107a vaccine composed on autologous dendritic cells andtumor antigens progression-free survival was increasedby 2 months for those receiving the vaccine30 Radiationmay assist in serving as a primer for the immunogeniceffects by facilitating tumor antigen uptake by dendriticcells and cross presentation on major histocompatibilitycomplex I Thus RT may assist in the tumor-specific cy-totoxic T lymphocytes associated with the immunemechanism
In conclusion although there may be challenges to com-bining and sequencing brain tumors radiosensitizersand immunotherapy the opportunities and potential fornovel applications are promising For brain tumors brainmetastases are typically underrepresented in trials
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
113
despite being among the most common intracraniallesions Despite their large population patients with brainmetastases are often excluded from clinical trials withnovel agents due to concerns regarding confounding out-comes and tolerability12 Primary gliomas also offer anovel frontier for the use of immunotherapy to standardadjuvant chemotherapy and radiation particularly forpatients with GBM less likely to respond to TMZ such aswith unmethylated MGMT As studies work to define therole of RT and radiosensitizers and immunotherapy fur-ther analysis is needed to assess the timing of RT andthese treatments
References
1 Stupp R Hegi ME Mason WP et al Effects of radiotherapy withconcomitant and adjuvant temozolomide versus radiotherapy aloneon survival in glioblastoma in a randomised phase III study 5-yearanalysis of the EORTC-NCIC trial Lancet Oncol 2009 10459ndash466
2 Lawrence TS Blackstock AW McGinn C The mechanism of actionof radiosensitization of conventional chemotherapeutic agentsSemin Radiat Oncol 2003 1313ndash21
3 Lesueur P Chevalier F Austry JB et al Poly-(ADP-ribose)-polymer-ase inhibitors as radiosensitizers a systematic review of pre-clinicaland clinical human studies Oncotarget 2017 8(40)69105ndash69124
4 Lester A Rapkins R Nixdorf S Khasraw M McDonald KCombining PARP inhibitors with radiation therapy for the treatmentof glioblastoma is PTEN predictive of response Clin Transl Oncol2017 19273ndash278
5 Gupta SK Kizilbash SH Carlson BL et al Delineation of MGMT hyper-methylation as a biomarker for veliparib-mediated temozolomide-sensi-tizing therapy of glioblastoma J Natl Cancer Inst 2016 108
6 Kleinberg LR Blakeley J Mikkelsen T et al An American BrainTumor Consortium (ABTC) phase 1 trial of veliparib (ABT-888)temozolomide (TMZ) and concurrent radiation therapy (RT) fornewly diagnosed glioblastoma multiforme (GBM) need for modifica-tion to approach for combining these therapies InternationalJ Radiat Oncol Biol Phys 2012 84S7ndashS8
7 Oronsky BT A Review of two promising radiosensitizers in brainmetastases Rrx-001 and 2-deoxyglucose In NC Oronsky edJ Cancer Sci Ther 2015 pp 137ndash141
8 Kim MM Parmar H Cao Y et al Concurrent whole brain radiother-apy and RRx-001 for melanoma brain metastases Neuro Onc2016 18455ndash456
9 Mehta MP Wang D Wang F et al Veliparib in combination withwhole brain radiation therapy in patients with brain metastasesresults of a phase 1 study J Neurooncol 2015 122409ndash417
10 Chabot P Hsia TC Ryu JS et al Veliparib in combination withwhole-brain radiation therapy for patients with brain metastasesfrom non-small cell lung cancer results of a randomized globalplacebo-controlled study J Neurooncol 2017 131105ndash115
11 Ochiai S Nomoto Y Yamashita Y et al Roles of valproic acid inimproving radiation therapy for glioblastoma a review of literaturefocusing on clinical evidence Asian Pac J Cancer Prev 201617463ndash466
12 Tan AC Heimberger AB Menzies AM Pavlakis N Khasraw MImmune checkpoint inhibitors for brain metastases Curr Oncol Rep2017 1938
13 DrsquoSouza NM Fang P Logan J Yang J Jiang W Li JCombining radiation therapy with immune checkpoint blockade
for central nervous system malignancies Frontiers Oncol 20166212
14 Parsa AT Waldron JS Panner A et al Loss of tumor suppressorPTEN function increases B7-H1 expression and immunoresistancein glioma Nat Med 2007 1384ndash88
15 Binder DC Davis AA Wainwright DA Immunotherapy for cancer inthe central nervous system current and future directionsOncoimmunology 2016 5e1082027
16 Newcomb EW Demaria S Lukyanov Y et al The combination ofionizing radiation and peripheral vaccination produces long-termsurvival of mice bearing established invasive GL261 gliomas ClinCancer Res 2006 124730ndash4737
17 Zeng J See AP Phallen J et al Anti-PD-1 blockade and stereotac-tic radiation produce long-term survival in mice with intracranial glio-mas Int J Radiat Oncol Biol Phys 2013 86343ndash349
18 Chow KK Hara W Lim M Li G Combining immunotherapy withradiation for the treatment of glioblastoma J Neurooncol2015123459ndash464
19 Belcaid Z Phallen JA Zeng J et al Focal radiation therapy com-bined with 4-1BB activation and CTLA-4 blockade yields long-termsurvival and a protective antigen-specific memory response in amurine glioma model PLoS One 2014 9e101764
20 Topalian SL Hodi FS Brahmer JR et al Safety activity and im-mune correlates of anti-PD-1 antibody in cancer N Engl J Med2012 3662443ndash2454
21 Bienkowski M Preusser M Prognostic role of tumour-infiltrating in-flammatory cells in brain tumours literature review Curr OpinNeurol 2015 28647ndash658
22 Harter PN Bernatz S Scholz A et al Distribution and prognostic rel-evance of tumor-infiltrating lymphocytes (TILs) and PD-1PD-L1 im-mune checkpoints in human brain metastases Oncotarget 2015640836ndash40849
23 Berghoff AS Ricken G Widhalm G et al Tumour-infiltrating lym-phocytes and expression of programmed death ligand 1 (PD-L1) inmelanoma brain metastases Histopathology 2015 66289ndash299
24 Silk AW Bassetti MF West BT Tsien CI Lao CD Ipilimumab and ra-diation therapy for melanoma brain metastases Cancer Med 20132899ndash906
25 Knisely JP Yu JB Flanigan J Sznol M Kluger HM Chiang VLRadiosurgery for melanoma brain metastases in the ipilimumab eraand the possibility of longer survival J Neurosurg 2012117227ndash233
26 Kiess AP Wolchok JD Barker CA et al Stereotactic radiosurgeryfor melanoma brain metastases in patients receiving ipilimumabsafety profile and efficacy of combined treatment Int J Radiat OncolBiol Phys 2015 92368ndash375
27 Qian JM Yu JB Kluger HM Chiang VL Timing and type of immunecheckpoint therapy affect the early radiographic response of mela-noma brain metastases to stereotactic radiosurgery Cancer 20161223051ndash3058
28 Silk AW Cao Y Gomez-Hassan D et al A randomized phase IIstudy of ipilimumab induction in patients with melanoma brain me-tastases receiving stereotactic radiosurgery J Clin Oncol 2015 33TPS9079ndashTPS9079
29 Neagu MR Reardon DA An Update on the role of immunotherapyand vaccine strategies for primary brain tumors Curr TreatOptions Oncol 2015 1654
30 Wen PY Reardon DA Phuphanich S et al A randomized double-blind placebo-controlled phase 2 trial of dendritic cell (DC) vaccina-tion with ICT-107 in newly diagnosed glioblastoma (GBM) patientsJ Clin Oncol 2014 322005ndash2005
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
114
British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

epigenetic and related transcriptional profiles1011 havedistinct genetic and clinicopathological features1011 andtheir implementation for patient stratification for betterprognostication and enrollment into subgroupsubtype-directed therapies in the context of clinical trials will be astep change in the treatment of MB patients
All CNS tumors A classification tool for brain tumorsbased on genome-wide DNA methylation patterns and arandom forest-based machine learning approach hasbeen developed and extensively tested by the GermanCancer Research Center (wwwmolecularneuropathologyorg) This resource is available online and has provento be a valuable tool to improve brain tumor diagnosticsThis approach has facilitated the identification of com-mon druggable molecular pathway alterations across var-ious histological tumor entities thus allowing patients toenter the most appropriate clinical trials and in somecases be offered molecularly matched therapies As anexample DNA methylation profiles allow precise identifi-cation of cases with mitogen-activated protein kinase(MAPK) activation which is a feature of tumors withBRAF V600E mutation1213 which can span various tradi-tional histological entities such as pilocytic astrocytomaspleomorphic xanthoastrocytomas ganglioglioma andsubependymal giant cell astrocytomas to predict re-sponse to specific inhibitors interrupting the BRAFMEKcomponent of the MAP kinase pathway14
Novel TherapeuticApproaches TargetingEpigeneticDeregulationDiffuse intrinsic pontine glioma (DIPG) is a highlyaggressive pediatric tumor located in the brainstem andcharacterized by a rapid and diffusely infiltrative patternof growth These tumors cannot be treated surgicallybecause of their location and infiltrative nature15
Radiation therapy is the standard treatment although itprovides only temporary symptom relief with no overallsurvival benefits and conventional chemotherapy drugsare ineffective15
Mutations in histone H3 variants occur in more than 80of DIPG and result in a lysine-to-methionine substitution(H3K27M)16 17 H3K27M has been shown to inhibitpolycomb repressive complex 2 (PRC2) by binding to itscatalytic subunit EZH2 and reducing the methylation ofH3 at lysine 27 (H3K27me) at selected target loci18 Theresidual PRC2 activity is required to maintain DIPGproliferative potential by repressing neuronaldifferentiation in patient-derived cell lines and in agenetically engineered mouse model1920 Importantlysmall-molecule EZH2 inhibitors abolish tumor cell growth
in these models raising the possibility that inhibitionof EZH2 could be a novel therapeutic strategy for thesetumors19
An independent study showed that H3K27M associateswith increased H3K27 acetylation (H3K27ac) and that themajority of the heterotypic H3K27M-K27ac nucleosomesco-localize with bromodomain proteins at the loci of ac-tively transcribed genes20 The authors have shown thatblocking the recruitment of bromodomain proteins by het-erotypic H3K27M-K27ac nucleosomes in DIPG with bro-modomain and extraterminal domain family inhibitorsefficiently inhibited tumor progression thus identifying thisclass of compounds as potential therapeutics in DIPG20
These important advances in understanding the underly-ing biology of DIPG have led to the identification of novelepigenetic therapeutic approaches which are very effec-tive at the preclinical level and if confirmed in transla-tional studies could change the way we treat thesetumors in the near future
Conclusion and outlookThese are exciting and challenging times for theneuro-oncology community Exciting because there isgrowing expectation in the field that new discoveriessuch as those discussed in this article can soon translateinto new and more effective therapeutic approachesChallenging because it is clear that new skill sets are re-quired to effectively apply them to benefit patients
The clinical training in many neuro-oncology specialtieswill have to take into account the additional knowledgeand skills needed in the field and offer education incomplementary disciplines such as next-generationsequencing technologies integrated with interpretativedata analysis as well as molecular biology for the designof biologically informed assays and tools The require-ment for these new highly specialized skills also needs tobe reflected in the composition of the clinical teamswhere bioinformatics expertise will play an increasinglyimportant role for the integration of multimodal data inpatient care
References
1 Waddington CH Canalization of development and the inheritance ofacquired characters Nature 1942150563ndash565
2 Allis CD Jenuwein T The molecular hallmarks of epigenetic controlNat Rev Genet 201617487ndash500
3 Flavahan WA Gaskell E Bernstein BE Epigenetic plasticity and thehallmarks of cancer Science (New York NY 2017357
4 Edwards JR Yarychkivska O Boulard M Bestor TH DNA methyla-tion and DNA methyltransferases Epigenetics amp chromatin20171023
5 Filbin MG Suva ML Gliomas genomics and epigenomics arriving atthe start and knowing it for the first time Annual Rev Pathol201611497ndash521
6 Hegi ME et al MGMT gene silencing and benefit from temozolomidein glioblastoma N Engl J Med 2005352997ndash1003
Volume 2 Issue 3 Brain Tumor Epigenetics From Research to Clinical Practice
103
7 Pajtler KW et al Molecular Classification of Ependymal Tumorsacross All CNS Compartments Histopathological Grades and AgeGroups Cancer Cell 201527728ndash743
8 Pajtler KW et al The current consensus on the clinical managementof intracranial ependymoma and its distinct molecular variants ActaNeuropathol 20171335ndash12
9 Taylor MD et al Molecular subgroups of medulloblastoma the cur-rent consensus Acta Neuropathol 2012123465ndash472
10 Schwalbe EC et al Novel molecular subgroups for clinical classifi-cation and outcome prediction in childhood medulloblastoma a co-hort study Lancet Oncol 201718958ndash971
11 Cavalli FMG et al Intertumoral Heterogeneity withinMedulloblastoma Subgroups Cancer Cell 201731737ndash754 e736
12 Schindler G et al Analysis of BRAF V600E mutation in 1320 nervoussystem tumors reveals high mutation frequencies in pleomorphicxanthoastrocytoma ganglioglioma and extra-cerebellar pilocytic as-trocytoma Acta Neuropathol 2011121397ndash405
13 Tanaka S et al Epithelioid glioblastoma arising from pleomorphicxanthoastrocytoma with the BRAF V600E mutation Brain TumorPathol 201431172ndash176
14 Banerjee A et al A phase I trial of the MEK inhibitor selumetinib(AZD6244) in pediatric patients with recurrent or refractory low-grade glioma a Pediatric Brain Tumor Consortium (PBTC) studyNeuro Oncol 2017191135ndash1144
15 Hargrave D Bartels U Bouffet E Diffuse brainstem glioma in chil-dren critical review of clinical trials Lancet Oncol 20067241ndash248
16 Schwartzentruber J et al Driver mutations in histone H33 and chro-matin remodelling genes in paediatric glioblastoma Nature2012482226ndash231
17 Wu G et al Somatic histone H3 alterations in pediatric diffuse in-trinsic pontine gliomas and non-brainstem glioblastomas Naturegenetics 201244251ndash253
18 Lewis PW et al Inhibition of PRC2 activity by a gain-of-function H3mutation found in pediatric glioblastoma Science (New York NY2013340857ndash861
19 Mohammad F et al EZH2 is a potential therapeutic target forH3K27M-mutant pediatric gliomas Nature Med 201723483ndash492
20 Piunti A et al Therapeutic targeting of polycomb and BET bromodo-main proteins in diffuse intrinsic pontine gliomas Nature Med201723493ndash500
Brain Tumor Epigenetics From Research to Clinical Practice Volume 2 Issue 3
104
The Value of SurgicalResection for MalignantGliomas in the ModernEra Beyond Extent ofResection
Stephen G Bowden MDSeunggu Jude Han MDDepartment of Neurological Surgery OregonHealth and Sciences University 3303 SW BondAve Center for Health and Healing CH8NPortland OR 97239 Telephone 503-494-4314Fax 503-346-6810 hanseohsuedu
105
Malignant gliomas are among the most difficult oncologi-cal entities to treat Despite aggressive treatment prog-nosis remains poor and recurrence and treatmentfailures seem inevitable The current standard-of-caretherapy includes maximal safe surgical resection fol-lowed by concurrent and adjuvant chemoradiotherapyHistorically surgical resection has conferred greater sur-vival benefit to these patients than adjuvant therapiespresumably through the cornerstone principle of cytore-duction However the extent of surgical resection is fre-quently limited by nearby eloquent tissue and risks to keyneurological functions In addition the value of such ag-gressive approaches has been questioned in light of thewidespread infiltration of glioma cells Meanwhile our un-derstanding of glioma biology continues to advance rap-idly fueled in large part by the acquisition of tumor tissueduring surgery Thus the exact role and value of surgeryparticularly in comparing the clinical benefits of maximalextent of resection (EOR) with the biomedical benefits oftissue provision has been a topic of great interest anddebate in both the neuro-oncological and neurosurgicalcommunities
EOR patient age tumor histology performance statusand molecular markers have been widely accepted assignificant predictors of patient outcomes in malignantglioma9 In the past 2 decades many large retrospectivecohort studies have demonstrated improvements in sur-vival with increasing EOR5917 Due to ethical considera-tions evidence from a randomized prospective studysupporting the clinical benefit of aggressive resectionsdoes not exist and likely never will Instead the closestthing to such evidence in malignant glioma comes fromthe randomized phase III trial comparing surgical resec-tions with or without the use of 5-aminolevulinic acid(5-ALA) The use of 5-ALA serving as a means to and aproxy for greater EOR resulted in extended overall sur-vival for patients with newly diagnosed glioblastoma19 Arecent meta-analysis of 41 117 unique patients by Brownet al adherent to the guidelines of PRISMA (PreferredReporting Items for Systematic Reviews and Meta-Analyses) also demonstrated a clear survival benefit forgross total resection over subtotal resection or biopsy atupfront surgery for glioblastoma1 The body of literatureas a whole clearly favored aggressive resections andthere seemed to be little disagreement for a strategytoward maximal resection when clinically feasibleHowever the challenge still remains when such strategiescome at the risk of neurological morbidity A recent reportby Rahman et al illustrates that the survival benefits fromaggressive resection are lost if the patient develops anew postoperative neurologic deficit as a result15
All the while our understanding of glioma genetics mo-lecular biology and mechanisms of resistance has con-tinued to deepen and evolve borne of thoughtful andsystematic studies using patient-acquired tumor sam-ples Molecular profiles and tumor genetics have proventhemselves to be the best predictors of clinical behaviorand now represent crucial components of the diagnostic
classification scheme of infiltrating gliomas12 With tumortissue at the molecular and genetic level being able to ro-bustly predict patient outcomes accurate tissue diagno-sis has become paramount in the management ofgliomas The role and value of open surgical resection to-ward this end have become clearer as concerns of sam-pling error with biopsy alone led to a number of studiesevaluating the ldquoaccuracyrdquo of stereotactic biopsy proce-dures Jackson et al reported a series of 81 patients whounderwent stereotactic biopsy followed by open surgicalresection The tissue diagnosis was concordant betweenbiopsy and open resection samples in only 51 ofpatients6 Other studies have also demonstrated diagnos-tic concordance between stereotactic biopsy and surgi-cal resection samples in only 57 to 79 ofcases131428 The major limitation of stereotactic biopsyfor infiltrating gliomas likely stems from the significantintratumoral heterogeneity and collectively these studieshighlight the value of open surgical resection in providinga more global representation and understanding of thetumor tissue
The value of extensive resection is perhaps even moreprofound when considering the therapeutic implicationsof such heterogeneity Multiple-site and serial-samplinganalyses have revealed a high degree of both spatial andtemporal heterogeneity within these tumors a conse-quence of serial evolutionary events during tumor growthand progression23 These studies have also led to theconcept of therapy-driven clonal selection and preferen-tial regrowth of resistant cell populations as a potentialmechanism of treatment failure Efforts to expand our un-derstanding of the tremendously complex network ofmutations and biological consequences of chronologicalhierarchy would be greatly facilitated by carefullyplanned thoughtful acquisition of tumor samples duringsurgery
Despite the recent paradigm shift in glioma diagnosticclassification little gains have been made in improvingthe overall prognosis for patients with malignant gliomassince the introduction of concurrent and adjuvant temo-zolomide in 200521 The strategies more recently tested inlarge randomized phase III trials by and large have yieldeddisappointing results while the reasons and mechanismsof treatment failures remain unclear Even so encourag-ing responses have occasionally been seen in varioussubsets of patients and studies exploring the presenceof potential biomarkers have generated intriguing andpromising results in these populations The developmentof the antindashvascular endothelial growth factor monoclonalantibody bevacizumab is one such example Two initialphase II trials showed prolonged progression-free sur-vival in recurrent glioblastoma relative to historical con-trols prompting the US Food and Drug Administration togrant accelerated approval to bevacizumab for recurrentglioblastoma in 2009825 However 2 large randomized tri-als evaluating the addition of bevacizumab to radiationand temozolomide in the newly diagnosed setting failedto show a benefit in overall survival24 and its utility in the
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
106
recurrent setting is now a topic of debate in light of sub-sequent phase III trial results However a post hoc analy-sis of patients enrolled in the AVAglio trial recentlydemonstrated that bevacizumab improved overall sur-vival for those with a proneural subtype tumor18 Just asO6-methylguanine-DNA-methyltransferase (MGMT) pro-moter methylation does for temozolomide the geneticprofile of the tumor could serve as a potential biomarkerof clinical response for bevacizumab as well and valida-tion studies are currently ongoing Such analyses al-though performed post hoc require targeted prospectivecollection of tumor tissue at initial surgery In addition ge-netic profiling of newly diagnosed malignant gliomas willneed to become routine if this approach is to be utilizedwidely Similarly cilengitide an inhibitor of aVb3 andaVb5 integrins with anti-angiogenic properties showedinitial promise in recurrent glioblastoma studies but failedto show any additional benefit in the newly diagnosedsetting20 A subsequent post hoc analysis of the phase IItrial revealed improved progression-free and overall sur-vival in patients with high aVb3 levels in the tumor cells26
However tumor tissues were not systematically collectedand less than half of the patientsrsquo tumor tissues wereavailable for analysis from the phase III trialUnfortunately this drug will most likely not undergo fur-ther development and one cannot help wonder if the out-come would have been different if the enrollment in thephase III trial had been enriched for or restricted to tumorswith high expression of the aVb3 integrin The only trueldquosuccess storyrdquo since the adaptation of radiation andtemozolomide has come from the novel approach of tu-mor treating fields (TTFields) a transcutaneous deliveryof low-intensity intermediate frequency alternating elec-tric fields The multicenter phase III trial EF-14 random-ized patients with supratentorial glioblastoma withoutevidence of tumor progression following standard che-moradiation to receive maintenance treatment withTTFields plus temozolomide or temozolomide alone22
The study was terminated early based on results of aplanned interim analysis demonstrating benefit inprogression-free survival overall survival a secondaryendpoint was also significantly enhanced at this timeDespite the trialrsquos success TTFields has not been univer-sally adopted by the neuro-oncology community andenthusiasm among clinicians and patients remains low27
Experts have raised concerns regarding the study designsuch as its open-label design lacking a sham-treatmentcontrol arm as well as the generalizability of the resultsbased on the unique randomization point occurring afterconcurrent chemoradiation16 Perhaps most significantlya lack of widely understood mechanism of action hasalso been raised as a factor with comparison to othertreatments the preclinical data for TTFields is relativelylacking particularly when applied in conjunction with che-moradiation27 Even during the early phase stages theuse of robust tissue-based analyses exploring the mech-anism of action such as dose response modeling andmultisite tissue biopsies may have mitigated some of
these concerns and led to wider acceptance by the com-munity Bevacizumab and cilengitide clearly benefitedfrom retrospective analyses of human tumor tissue toidentify susceptible treatment populations while the en-thusiasm for TTFields is perhaps in part tempered by thelack thereof Collectively the evolution of these treat-ments underscores the value of extensive targeted tissuesampling in furthering development of new adjunctivetherapies
Open surgical resection of tumors with such targeted tis-sue acquisition for analysis will continue to play a key rolein prospective clinical trial designs Comparison ofpretreatment and posttreatment tissue profiles representsa valuable line of investigation by delving into mecha-nisms of therapeutic action as well as mechanisms oftreatment failures1011 It also provides an opportunity toinvestigate a number of key fundamental steps along anagentrsquos path to clinical success such as does the agentsuccessfully traffic to the tumor if so how much anddoes the agent then actually have its hypothesizedeffects at the biochemical or cellular level Thusearly-phase trials can and should include posttreatmentmolecular endpoints when possible in addition to safetyendpoints Immunotherapy and immune checkpoint inhi-bition represent exciting novel therapeutic approachesfor neuro-oncology particularly based on their success inmetastatic cancers Large phase III trials studying block-ade of the programmed cell death protein (PD)1PDligand 1 axis with monoclonal antibodies for newlydiagnosed and recurrent glioblastoma are under way butinitial reports have been concerning for negative resultsAs in the development of many previous novel agentstissue-based mechanism studies have been largely lack-ing in the preclinical phases However an Alliance-supported trial currently enrolling focuses on a biomarkeras a primary endpoint patients with recurrent glioblas-toma indicated for surgery are randomized to receivepembrolizumab a PD1 inhibitor either before or aftersurgery (NCT02852655) The resected tumor tissue willthen be analyzed for the profile of tumor-infiltratingT cells and comparison will be made between the 2groups This study represents a tremendously valuableopportunity to explore the impact and the potential chal-lenges of checkpoint inhibition for malignant gliomas inthe clinical setting and should the large phase III trialsend up negative this pilot study will be very informative
Advances in imaging biomarkers and molecular charac-terization of gliomas in conjunction with new targetedtherapies will continue to improve and transform themanagement of these tumors Multimodality imaging cannow more accurately reflect ongoing biological processeswithin these tumors such as the presence of oncogenicmutations or cells undergoing malignant transformationNovel biomarkers such as circulating tumor DNA showpromise in detecting early recurrence or monitoring treat-ment response3724 Lastly the new classification schemerevolving around molecular characterization will provide a
Volume 2 Issue 3 The Value of Surgical Resection for Malignant Gliomas in the Modern Era
107
necessary corollary to these novel diagnostic tools Itremains indisputable however that clinical validation ofthese novel diagnostic tools will also require systematiccorrelation with human tumor tissue obtained throughsurgery These samples ideally gathered prospectivelywill provide a pivot upon which we can expand our under-standing of the complex network of oncological pro-cesses driving these tumors
Malignant gliomas are incredibly challenging disease en-tities in many ways due to the inter- and intratumoral het-erogeneity that is a hallmark of them Experience to datehints that future successes in malignant gliomas rest inneuro-oncology entering the era of precision medicinewhere validated biomarkers and targeted personalizedtherapies are seamlessly integrated into the managementparadigm Accordingly systems supporting surgical re-section and patient-specific tumor tissue analysis mustbe built and organized to guide the decision making fortherapy As our overall approach to the management ofmalignant gliomas evolves so should the framework ofsurgical management The clinical benefits of maximalsafe resection are well founded and well reportedHowever the oncological neurosurgeon must now lookbeyond maximal cytoreduction itself and recognize thevalue of thoughtful acquisition and analysis of tumor tis-sue Modern neurosurgeons must consider themselvessurgical neuro-oncologists and engagement and partici-pation of surgeons into clinical trials particularly early-phase trials should be encouraged and valued In turnwe should provide our surgical trainees with the trainingand tools in neuro-oncology to help them participate andcontribute in multidisciplinary collaborative efforts aimingto advance the understanding of brain tumor biology andultimately improve the outlook of our patients
References
1 Lacroix M Abi-Said D Fourney DR Gokaslan ZL et al A multivariateanalysis of 416 patients with glioblastoma multiforme prognosisextent of resection and survival J Neurosurg 2001 95190ndash198
2 Hervey-Jumper SL Berger MS Maximizing safe resection of low-and high-grade glioma J Neurooncol 2016 130269ndash282
3 Sanai N Polley MY McDermott MW Parsa AT Berger MS An ex-tent of resection threshold for newly diagnosed glioblastomas JNeurosurg 2011 1153ndash8
4 Stummer W Pichlmeier U Meinel T et al Fluorescence-guided sur-gery with 5-aminolevulinic acid for resection of malignant glioma arandomised controlled multicentre phase III trial Lancet Oncol2006 7392ndash401
5 Brown TJ Brennan MC Li M et al Association of the extent ofresection with survival in glioblastoma a systematic review andmeta-analysis JAMA Oncol 2016 21460ndash1469
6 Rahman M Abbatematteo J De Leo EK et al The effects of new orworsened postoperative neurological deficits on survival of patientswith glioblastoma J Neurosurg 2017 127123ndash131
7 Louis DN Perry A Reifenberger G et al The 2016 World HealthOrganization Classification of Tumors of the Central NervousSystem a summary Acta Neuropathol 2016 131803ndash820
8 McGirt MJ Bulsara KR Cummings TJ et al Prognostic value ofmagnetic resonance imaging-guided stereotactic biopsy in the
evaluation of recurrent malignant astrocytoma compared with a le-sion due to radiation effect J Neurosurg 2003 9814ndash20
9 Muragaki Y Chernov M Maruyama T et al Low-grade glioma onstereotactic biopsy how often is the diagnosis accurate MinimInvasive Neurosurg 2008 51275ndash279
10 Woodworth G McGirt MJ Samdani A Garonzik I Olivi AWeingart JD Accuracy of frameless and frame-based image-guided stereotactic brain biopsy in the diagnosis of glioma com-parison of biopsy and open resection specimen Neurol Res 200527358ndash362
11 Suzuki H Aoki K Chiba K et al Mutational landscape and clonal ar-chitecture in grade II and III gliomas Nat Genet 2015 47458ndash468
12 Stupp R Mason WP van den Bent MJ et al Radiotherapy plus con-comitant and adjuvant temozolomide for glioblastoma N Engl JMed 2005 352987ndash996
13 Kreisl TN Kim L Moore K et al Phase II trial of single-agent bevaci-zumab followed by bevacizumab plus irinotecan at tumor progres-sion in recurrent glioblastoma J Clin Oncol 2009 27740ndash745
14 Vredenburgh JJ Desjardins A Herndon 2nd JE et al Phase II trial ofbevacizumab and irinotecan in recurrent malignant glioma ClinCancer Res 2007 131253ndash1259
15 Chinot OL Wick W Mason W et al Bevacizumab plusradiotherapy-temozolomide for newly diagnosed glioblastomaN Engl J Med 2014 370709ndash722
16 Gilbert MR Dignam JJ Armstrong TS et al A randomized trial ofbevacizumab for newly diagnosed glioblastoma N Engl J Med2014 370699ndash708
17 Sandmann T Bourgon R Garcia J et al Patients with proneural glio-blastoma may derive overall survival benefit from the addition of bev-acizumab to first-line radiotherapy and temozolomide retrospectiveanalysis of the AVAglio trial J Clin Oncol 2015 332735ndash2744
18 Jackson RJ Fuller GN Abi-Said D et al Limitations of stereotacticbiopsy in the initial management of gliomas Neuro Oncol 20013193ndash200
19 Stupp R Hegi ME Gorlia T et al Cilengitide combined with stan-dard treatment for patients with newly diagnosed glioblastoma withmethylated MGMT promoter (CENTRIC EORTC 26071-22072study) a multicentre randomised open-label phase 3 trial LancetOncol 2014 151100ndash1108
20 Weller M Nabors LB Gorlia T et al Cilengitide in newly diagnosedglioblastoma biomarker expression and outcome Oncotarget2016 715018ndash15032
21 Stupp R Taillibert S Kanner AA et al Maintenance therapy withtumor-treating fields plus temozolomide vs temozolomide alone forglioblastoma a randomized clinical trial JAMA 20153142535ndash2543
22 Wick W TTFields where does all the skepticism come from NeuroOncol 2016 18303ndash305
23 Sampson JH Alternating electric fields for the treatment of glioblas-toma JAMA 2015 3142511ndash2513
24 Lang FF Asher A Prospective clinical trials of brain tumor therapy thecritical role of neurosurgeons J Neurooncol 2004 69151ndash167
25 Lang FF Gilbert MR Puduvalli VK et al Toward better early-phasebrain tumor clinical trials a reappraisal of current methods and pro-posals for future strategies Neuro Oncol 2002 4268ndash277
26 Elkhaled A Jalbert L Constantin A et al Characterization of metab-olites in infiltrating gliomas using ex vivo (1)H high-resolution magicangle spinning spectroscopy NMR Biomed 2014 27578ndash593
27 Jalbert LE Neill E Phillips JJ et al Magnetic resonance analysis ofmalignant transformation in recurrent glioma Neuro Oncol 2016181169ndash1179
28 Touat M Duran-Pena A Alentorn A Lacroix L Massard C Idbaih AEmerging circulating biomarkers in glioblastoma promises andchallenges Expert Rev Mol Diagn 2015 151311ndash1323
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
108
Update on RadiationCombinations in theTreatment of Patientswith Malignant BrainTumors FromRadiosensitizers toImmunotherapy
Debra Nana Yeboa MD1
Erik P Sulman MD PhD123
Departments of 1Radiation Oncology2Translational Molecular Pathology and3Genomic Medicine The University of Texas MDAnderson Cancer Center 1515 Holcombe BlvdUnit 97 Houston Texas USA Tel 713-563-2300dnyeboamdandersonorg andepsulmanmdandersonorg
109
AbstractAdvances in radiosensitizers and immunotherapyhave ushered in a new frontier in brain tumortreatment The brain has often been viewed as asanctuary site due to the bloodndashbrain barrier andthus the 2 primary modalities of therapy includedsurgery and radiation therapy (RT) More recentlysystemic therapies have played a greater role aseither combination therapy radiosensitizers or im-munotherapy Two novel radiosensitizers are beingdeveloped for the treatment of brain metastasesRRx-001 for example is a small molecule thataccelerates the NO2 to NO conversion of deoxyhe-moglobin and the agent 2-dexoyglucose (2-DG) is anonmetabolized glucose analogue that interfereswith ATP formation Poly(ADP-ribose) DNA polymer-ase inhibitors are promising due to their distinctradiobiological effects Veliparib and olaparib areamong the most studied with randomized trialsexploring their use in gliomas and brain metastasesImmunotherapy including immune checkpoint inhib-itors may play a role for both primary gliomas andbrain metastases RT has been shown to enhancethe function of cytotoxic T lymphocytes induce infil-tration of cytotoxic T lymphocytes and enhancefunction Trials are presently exploring use of bothprogrammed cell death protein (PD)1 and PD ligand1 blockade in glioblastoma patients with radiationSimilarly several immunotherapies are being investi-gated with either stereotactic radiosurgery or wholebrain radiation therapy for brain metastases In thisreview the use of radiosensitizers and immunother-apy agents with RT will be discussed broadly
Keywords brain metastases brain tumors gliomasimmunotherapy radiation therapy radiosensitizers
Radiosensitizers andImmunotherapy inBrain TumorsAdvances in radiosensitizers and immunotherapy haveushered in a new frontier to brain tumor treatment Braintumors however are a diverse class sharing only similaranatomic location Both primary brain malignancies andbrain metastasis have widely diverse histologies and mo-lecular phenotypes With the bloodndashbrain barrier thebrain has often been viewed as a sanctuary site and thusthe 2 primary modalities of therapy included surgery andradiation with decreased benefit from systemic agentsdue to lack of brain penetration However more recentlysystemic therapies have played a greater role as eithercombination therapy radiosensitizers or immunother-apy While temozolomide (TMZ) has played a pivotal rolefor glioblastoma (GBM) only a subset of patients benefitfrom the treatment1 The use of alternative systemicagents that may potentiate the effects of radiation ther-apy (RT) is becoming increasingly appealing Similarly forbrain metastases a variety of systemic agents are beingexplored primarily based on histology and immune pro-file In this review the use of radiosensitizers and immu-notherapy agents currently under investigation with RTwill be discussed
RadiosensitizersThe guiding concept of radiation sensitization is to in-crease the biologic effect of radiation such as increasedDNA damage decreased DNA repair decreased hypoxiaor increased G2M cell cycle blockade leading to im-proved tumor control and increased patient survival2
Poly(adenosine diphosphate-ribose) DNA polymerase(PARP) inhibitors are promising radiosensitizers due totheir roles in DNA repair3 PARP inhibitors work againstPARP1 a nuclear enzyme involved in the recruitment ofrepair proteins used in base excision repair and single-strand break repair PARP1 may also play a role in nonho-mologous end-joining4 The primary investigation ofPARP inhibitors has been in potentiating radiation andchemotherapy effects the latter in the context of homolo-gous repair deficient tumors For radiation the primarymechanism of action is inducing damage to nucleotidesleading to single-strand and double-strand breaks ThusPARP inhibitors in combination with radiation have an ap-pealing mechanism to inhibit or delay DNA repair andlikely convert more single-strand breaks to double-strandbreaks4
While several PARP inhibitors are currently being evalu-ated in a variety of tumors including talazoparib and nira-parib veliparib and olaparib are among the most studiedand there are randomized trials exploring their use in
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
110
gliomas The US National Cancer Institute (NCI)ndashfundedAlliance for Clinical Trials in Oncology (Alliance) A071102is a randomized phase IIIII trial evaluating the use ofveliparib in combination with TMZ in the adjuvant settingin patients with GBM tumors exhibiting hypermethylationof the O6 methylguanine DNA methyltransferase (MGMT)gene promoter Preclinical data supporting this trial sug-gested that only patients with MGMT methylated tumorswould benefit from the combination a group of patientsfor whom TMZ concurrent with radiation might be mostbeneficial5 A phase I trial performed by the NCI-fundedAmerican Brain Tumor Consortium attempted to combineveliparib with radiation and TMZ but failed to identify asuitable recommended phase II dose due to significanthemotoxicity6 Thus attempts to combine radiation withveliparib have focused on patients least likely to benefitfrom TMZ namely with MGMT unmethylated tumors forwhom TMZ could be withheld The Australian VeliparibRT and TMZ trial in newly diagnosed unmethylatedMGMT glioblastoma (VERTU) is a single-arm study inwhich patients receive RT with veliparib followed by adju-vant TMZ and veliparib4
An ongoing novel approach to radiosensitize gliomasinvolves a combination with an agent that interferes withan essential metabolic process 2-Dexoyglucose (2-DG)is a nonmetabolized glucose analogue that acts as acompetitive inhibitor of glycolysis It is transported acrossthe bloodndashbrain barrier by the glucose transporter GLUT-1 and thus has good penetration into the CNSIntracellularly it is trapped and accumulates in cells simi-lar to the mechanism of 18-fluorodeoxyglucose 2-DG isphosphorylated by glycolytic enzymes and the
phosphorylated 2-DG (2-deoxyglucose-P) is trapped in-tracellularly Inhibition of hexokinase activity by 2-DGinterferes with ATP formation and results in tumor celldeath7 While it has positive attributes by selectively tar-geting metabolically active tumor cells 2-DG has alsobeen associated with Q-T prolongation The currentphase III trial in gliomas is assessing the toxicity and tol-erability of 2-DG with hypofractionated radiation of 5 Gyas a radiosensitizer7
Two novel radiosensitizers are being developed for thetreatment of brain metastases First RRx-001 is a smallmolecule initially designed by the aerospace industry Itworks in part as a radiosensitizer by increasing blood flowand thus oxygenation of tumors through nitric oxideRRx-001 which binds to hemoglobin accelerates theNO2 to NO conversion of deoxyhemoglobin It workslocally under hypoxic conditions and subsequentlythe radiosensitive effects through nitric oxide are invasodilation and inhibiting DNA repair enzymes8 Nitricoxide is relatively benign The higher levels of oxidativestress with H2O2 and superoxide in tumors in comparisonto normal tissues result in the preferential generation ofreactive peroxynitrite in the presence of higher nitric oxidelevels7 This accounts for the increased specificity anddecreased toxicity with RRx-001 The dose limiting toxic-ity in a phase I trial of 25 patients treated with eitherweekly or biweekly infusions was infusional pain relatedto the release of NO at the site of injection7 Outside ofpreclinical models 2 clinical reports examining wholebrain radiation therapy (WBRT) with RRx-001 reported anintracranial response A patient with melanoma and 2hemorrhagic edematous lesions of 26 cm and 33 cm
Table 1 Clinical trials involving immunotherapy and radiation therapy1213
Clinical Trials Number Phase Disease Type Treatment Groups
NCT02667587 II Newly diagnosed GBMMGMT-methylated
Nivolumabthorn TMZthorn RT vs placebothornTMZ thorn RT
NCT02617589 III Newly diagnosed GBM Nivolumabthorn RT vs TMZthorn RTNCT02336165 II Newly diagnosed unmethylated
MGMT recurrent glioblastomaMEDI4736thorn standard RT vs MEDI4736 thorn
bevacizumabNCT02530502 III Newly diagnosed GBM RTthorn TMZthorn pembrolizumab TMZthorn
pembrolizumabNCT02313272 I Recurrent glioma Hypofractionated stereotactic radiationthorn
pembrolizumab thorn bevacizumabNCT02696993 III Brain metastases Nivolumabthorn SRS nivolumabthornWBRT
nivolumabthorn ipilimumab thorn SRS nivolu-mabthorn ipilimumab thornWBRT
NCT02115139 II Melanoma brain metastases Ipilimumab thornWBRTNCT02097732 II Melanoma brain metastases Ipilimumab SRS ipilimumab vs SRS
ipilimumabNCT01703507 I Melanoma brain metastases Ipilimumab thornWBRT vs ipilimumab thorn SRSNCT02107755 II Melanoma brain metastases Ipilimumab thorn SRSNCT02858869 pilot Melanoma and NSCLC Pembrolizumabthorn SRSNCT01950195 I Melanoma brain metastases Ipilimumab thorn SRSNCT02662725 II Melanoma brain metastases Ipilimumab thorn SRS
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
111
after a single intravenous dose of RRx-001 of 5 mgm2 4days before WBRT resulted in symptomatic improvementwithin 48 hours By 4 months after radiation there was areduction in size in the largest dimension down to 10 cmand 23 cm of the respective lesions A second report of amelanoma patient with at least 18 lesions after receivingRRx-001 of 5 mgm2 4 days before WBRT as well astwice weekly doses during the 2 weeks of radiation alsoshowed response The patient at 4 months had disap-pearance of 13 of 18 lesions with shrinkage of theremaining 5 lesions8 Presently BRAINSTORM is a phaseIII dose escalation trial of RRx-001 designed to be ad-ministered twice weekly for 2 weeks with WBRT (30 Gy in10 fractions) with the option for weekly maintenance8
Veliparib has also been evaluated in the setting of brainmetastases It was tested in a global randomized con-trolled trial with WBRT Veliparib is orally bioavailable andcrosses the bloodndashbrain barrier It was first examined in amultihistology phase I trial in patients with nonndashsmall celllung cancer (NSCLC) breast cancer melanoma and re-nal and colorectal cancers among others The study of81 patients tested dose tolerance of veliparib from 10 to300 mg orally twice a day with WBRT to 30 Gy in 10 frac-tions or 375 Gy in 15 fractions9 The phase I trial dose es-calation portion did not reach the predefined criteria forthe maximum tolerated dose but there was amplificationof the adverse effects of nausea and vomiting among thehighest dose cohort of 300 mg bid9 The adverse eventprofile at 200 mg bid was similar to that of WBRT aloneDoses of veliparib from 20 to 200 mg bid demonstratesimilar antitumor activity and other studies in preclinicalmodels found that 50 mg daily demonstrated significantreduction in poly(ADP-ribose) in peripheral blood mono-nuclear cells and tumor tissue while also effectivelycrossing the bloodndashbrain barrier Thus the subsequentphase II trial examined 50 mg with WBRT9 In order to as-sess a more homogeneous cohort the phase III globalrandomized trial studied only NSCLC at the 2 doses of50 mg and 200 mg twice daily versus placebo twice a daywith WBRT10 The primary endpoint was overall survivalIn 307 patients in a 111 randomization of 50 mg bid200 mg bid or placebo twice daily the study found nosignificant differences in overall survival among the differ-ent groups10 The majority of patients across the treat-ment groups had a graded prognostic assessment (GPA)score of25 and a Karnofsky performance status ofgt80 The median overall survival was 185 days forpatients receiving placebo and 209 days for those receiv-ing veliparib without any statistically significant differ-ence These results were similar to the disease-specificestimate of median survival for the disease-specific GPAof NSCLC patients with brain metastases10
Several other radiosensitizers have failed to improve overradiation alone in a number of trials These have includedtrials with WBRT including motexafin gadolinium efap-roxyn bortozemib thalidomide teniposide topotecanpaclitaxel and cisplatin7 Of note other PARP inhibitorsalso being assessed include talazoparib and niraparib4
which may yield positive results The use of valproic acid(VPA) as a histone deacetylase inhibitor has also beenconsidered to have radiosensitizing potential in additionto its anti-epileptic drug properties11 While studies havereported that patients with GBM receiving an anti-epilep-tic agent may have higher overall survival than those re-ceiving standard chemoradiation therapy alone thebenefit remains controversial Retrospective analysissuggested that patients taking VPA specifically had bettersurvival in comparison to other anti-epileptic drugs Alsoa recent prospective phase II trial was performed in 37patients with GBM receiving VPA 25 mgkg concurrentlywith TMZ chemoradiation and reported a median survivalof 296 months While controversial further data andinvestigation are needed into this and other agents thatmay potentiate RT
Immunotherapy and radiationImmune checkpoint inhibitors lead to activation of T cellswhich may traffic across the bloodndashbrain barrier to inter-act with tumor Primary brain tumors may evade the im-mune system through upregulation of immunecheckpoints and possible immunosuppression12
Monoclonal antibodies promote immune-mediated anti-tumor activity by inhibiting the immune functionndashmediated cytotoxic T-lymphocyte associated protein 4(CTLA-4) and programmed cell death protein 1 (PD-1)receptors PD protein ligand (PD-L1) is upregulated inGBM through oncogenic signaling possibly throughphosphatase and tensin homolog loss and interleukin-10signaling1314 RT has also been shown to enhance thefunction of cytotoxic T lymphocytes RT may induce aninfiltration of cytotoxic T lymphocytes and enhance theirfunction It may also induce antindashCTLA-4 agents inhibitingT-cell function and increasing the CD8thorn T cellregulatoryT cell ratio in cases of melanoma15 Thus PD-1 and PD-L1 blockers may have a further role in CNS managementwith the use of radiation
In preclinical models radiation has been examined withimmunotherapy that included among other mechanismsvaccination PD-1 blockade and CTLA-4 blockade Inmice radiation plus a vaccination of irradiated gliomacells was associated with increased survival of 40 to80 compared with 0 to 10 for other groups stud-ied16 A benefit of PD-1 blockade with stereotactic radio-surgery (SRS) specifically has also been shown in amouse model In comparison to mice treated with radia-tion antindashPD-1 therapy or a combination only those re-ceiving combination therapy had a higher percentagesurvival alive beyond 180 days after treatment17 Othermouse carcinoma models have identified response withanti-CTLA antibody and fractionated radiation therapy18
CD137 activation CTLA-4 blockade and focal radiationtherapy have been examined in an immunocompetent in-tracranial GBM model Mice treated with triple combina-tion therapy had 50 greater survival19 In other murine
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
112
models the use of antindashPD-1 and antindashCTLA-4 agentsshowed improved survival and increased tumor infiltratingleukocyte populations compared with single modalitywith concurrent radiation16 There are conflicting data re-garding timing or sequencing of therapy with some ani-mal models showing no difference in tumor response inrelation to timing of RT and delivery of immunotherapy18
For instance in one animal model CTLA-4 blockade de-livered simultaneously with radiation or delivered a coupleof days after showed no difference in survival among themice19
Increased PD-1 expression in circulating monocytes hasbeen identified as a biomarker for tumor-induced immu-nosuppression and may serve as a prognostic factor forpotentially worse survival outcomes in clinic13 In onestudy GBM patients with lower PD-L1 expression hadhigher median overall survival than those with higher PD-L1 expression suggesting that lower expression may beassociated with less immunosuppression and more im-mune activity against the tumor glioma20 RT with immunecheckpoint blockade is being investigated to assess if theaddition of PD-1 and PD-L1 inhibitors may improve theoutcomes or toxicity profile of standard therapy For in-stance a multi-institutional trial opened as a phase III willevaluate outcomes in GBM receiving radiation and pem-brolizumab with TMZ (NCT02530502) Next durvalumabor MEDI4736 a PD-L1 inhibitor is being examined forunmethylated MGMT GBMs with standard radiotherapy(NCT02336165)12 The impact of checkpoint inhibitorsduring adjuvant treatment of GBM is currently beingevaluated in the NCI-funded NRG-BN002 trial(NCT02311920) which will evaluate the antindashCTLA-4antibody ipilimumab alone or in combination with theantindashPD-1 antibody nivolumab for patients with newlydiagnosed GBM
Brain metastases have clonal populations of cells differ-ent from the rest of the brain and a unique microenviron-ment that may influence immunotherapy There may bemore immune infiltrates in metastases than in primarybrain tumors21 PD-L1 expression in brain metastasesvaries by histology In a series evaluating PD-L1 expres-sion in various tumors including melanoma NSCLCbreast renal colorectal and small cell less than 10showed significant expression22 There was greatest ex-pression among NSCLC and melanoma with a correla-tion between PD-L1 expression and tumor infiltratinglymphocytes22 Institutional series have examined thecombination of radiation and immune checkpoint block-ade In another study specific to melanoma brain metas-tases PD-L1 expression was found in over 50 of thecases and among those cases over 40 expressedPD-L1 in more than 5 of tumor cells23 The largest bodyof data for use of PD-L1 with radiation is for melanomaand NSCLC
Ipilimumab is a human monoclonal antibody that blocksCTLA-4 and allows for T-cell activation and proliferationto enhance the immune response to cancer In a
retrospective review of 70 patients with brain metastasestreated with SRS or WBRT the 33 patients receiving im-munotherapy had a median survival of 183 months incomparison to the 37 patients who did not receive ipili-mumab with a median survival of 53 months While therewere limited data among the cohort to evaluate sequenc-ing of therapy among 10 evaluable patients 40 whoreceived ipilimumab prior to RT had a partial response incomparison to only 10 among the cohort of 22 evalu-able patients who did not receive ipilimumab therapy atall with radiation24 Another retrospective institutionalstudy of 77 patients in which 37 received ipilimumabfound that patients treated with SRS and ipilimumab hada median survival of 213 months versus 49 months forthose not receiving ipilimumab Most interestingly theyidentified that the correlation remained significant evenafter adjusting for additional factors such as performancestatus Secondly there was not an increased need for useof salvage WBRT25
The sequencing of radiotherapy and immune checkpointinhibitors is of interest In a study of patients with brainmetastases the one-year survival for patients receivingSRS before ipilimumab was greater at 65 in contrast to56 for those receiving it concurrently and 40 for thosereceiving it after SRS26 Similarly another study of 75patients with 566 brain metastases showed greater tu-mor lesion response at 6 months from SRS for patientsreceiving ipilimumab nivolumab or pembrolizumabwithin 4 weeks of their SRS27 Those receiving concurrenttherapy had by 6 months a decrease of 949 in compar-ison to 662 for those not receiving checkpoint inhibi-tors within 4 weeks Prospective clinical trials areinvestigating different combinations of RT with immunecheckpoint blockers in this setting For instance new tri-als are currently evaluating intracranial tumor control at 6months and the timing of immune therapy or immunecheckpoint inhibitors in relation to SRS28
Vaccines are also being developed for primary braintumors showing some evidence for their use Vaccinesdeveloped from dendritic cells and tumor lysate with tu-mor antigens such as the epidermal growth factor recep-tor variant III vaccine have shown promise29 Forinstance in a placebo controlled phase II trial of ICT-107a vaccine composed on autologous dendritic cells andtumor antigens progression-free survival was increasedby 2 months for those receiving the vaccine30 Radiationmay assist in serving as a primer for the immunogeniceffects by facilitating tumor antigen uptake by dendriticcells and cross presentation on major histocompatibilitycomplex I Thus RT may assist in the tumor-specific cy-totoxic T lymphocytes associated with the immunemechanism
In conclusion although there may be challenges to com-bining and sequencing brain tumors radiosensitizersand immunotherapy the opportunities and potential fornovel applications are promising For brain tumors brainmetastases are typically underrepresented in trials
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
113
despite being among the most common intracraniallesions Despite their large population patients with brainmetastases are often excluded from clinical trials withnovel agents due to concerns regarding confounding out-comes and tolerability12 Primary gliomas also offer anovel frontier for the use of immunotherapy to standardadjuvant chemotherapy and radiation particularly forpatients with GBM less likely to respond to TMZ such aswith unmethylated MGMT As studies work to define therole of RT and radiosensitizers and immunotherapy fur-ther analysis is needed to assess the timing of RT andthese treatments
References
1 Stupp R Hegi ME Mason WP et al Effects of radiotherapy withconcomitant and adjuvant temozolomide versus radiotherapy aloneon survival in glioblastoma in a randomised phase III study 5-yearanalysis of the EORTC-NCIC trial Lancet Oncol 2009 10459ndash466
2 Lawrence TS Blackstock AW McGinn C The mechanism of actionof radiosensitization of conventional chemotherapeutic agentsSemin Radiat Oncol 2003 1313ndash21
3 Lesueur P Chevalier F Austry JB et al Poly-(ADP-ribose)-polymer-ase inhibitors as radiosensitizers a systematic review of pre-clinicaland clinical human studies Oncotarget 2017 8(40)69105ndash69124
4 Lester A Rapkins R Nixdorf S Khasraw M McDonald KCombining PARP inhibitors with radiation therapy for the treatmentof glioblastoma is PTEN predictive of response Clin Transl Oncol2017 19273ndash278
5 Gupta SK Kizilbash SH Carlson BL et al Delineation of MGMT hyper-methylation as a biomarker for veliparib-mediated temozolomide-sensi-tizing therapy of glioblastoma J Natl Cancer Inst 2016 108
6 Kleinberg LR Blakeley J Mikkelsen T et al An American BrainTumor Consortium (ABTC) phase 1 trial of veliparib (ABT-888)temozolomide (TMZ) and concurrent radiation therapy (RT) fornewly diagnosed glioblastoma multiforme (GBM) need for modifica-tion to approach for combining these therapies InternationalJ Radiat Oncol Biol Phys 2012 84S7ndashS8
7 Oronsky BT A Review of two promising radiosensitizers in brainmetastases Rrx-001 and 2-deoxyglucose In NC Oronsky edJ Cancer Sci Ther 2015 pp 137ndash141
8 Kim MM Parmar H Cao Y et al Concurrent whole brain radiother-apy and RRx-001 for melanoma brain metastases Neuro Onc2016 18455ndash456
9 Mehta MP Wang D Wang F et al Veliparib in combination withwhole brain radiation therapy in patients with brain metastasesresults of a phase 1 study J Neurooncol 2015 122409ndash417
10 Chabot P Hsia TC Ryu JS et al Veliparib in combination withwhole-brain radiation therapy for patients with brain metastasesfrom non-small cell lung cancer results of a randomized globalplacebo-controlled study J Neurooncol 2017 131105ndash115
11 Ochiai S Nomoto Y Yamashita Y et al Roles of valproic acid inimproving radiation therapy for glioblastoma a review of literaturefocusing on clinical evidence Asian Pac J Cancer Prev 201617463ndash466
12 Tan AC Heimberger AB Menzies AM Pavlakis N Khasraw MImmune checkpoint inhibitors for brain metastases Curr Oncol Rep2017 1938
13 DrsquoSouza NM Fang P Logan J Yang J Jiang W Li JCombining radiation therapy with immune checkpoint blockade
for central nervous system malignancies Frontiers Oncol 20166212
14 Parsa AT Waldron JS Panner A et al Loss of tumor suppressorPTEN function increases B7-H1 expression and immunoresistancein glioma Nat Med 2007 1384ndash88
15 Binder DC Davis AA Wainwright DA Immunotherapy for cancer inthe central nervous system current and future directionsOncoimmunology 2016 5e1082027
16 Newcomb EW Demaria S Lukyanov Y et al The combination ofionizing radiation and peripheral vaccination produces long-termsurvival of mice bearing established invasive GL261 gliomas ClinCancer Res 2006 124730ndash4737
17 Zeng J See AP Phallen J et al Anti-PD-1 blockade and stereotac-tic radiation produce long-term survival in mice with intracranial glio-mas Int J Radiat Oncol Biol Phys 2013 86343ndash349
18 Chow KK Hara W Lim M Li G Combining immunotherapy withradiation for the treatment of glioblastoma J Neurooncol2015123459ndash464
19 Belcaid Z Phallen JA Zeng J et al Focal radiation therapy com-bined with 4-1BB activation and CTLA-4 blockade yields long-termsurvival and a protective antigen-specific memory response in amurine glioma model PLoS One 2014 9e101764
20 Topalian SL Hodi FS Brahmer JR et al Safety activity and im-mune correlates of anti-PD-1 antibody in cancer N Engl J Med2012 3662443ndash2454
21 Bienkowski M Preusser M Prognostic role of tumour-infiltrating in-flammatory cells in brain tumours literature review Curr OpinNeurol 2015 28647ndash658
22 Harter PN Bernatz S Scholz A et al Distribution and prognostic rel-evance of tumor-infiltrating lymphocytes (TILs) and PD-1PD-L1 im-mune checkpoints in human brain metastases Oncotarget 2015640836ndash40849
23 Berghoff AS Ricken G Widhalm G et al Tumour-infiltrating lym-phocytes and expression of programmed death ligand 1 (PD-L1) inmelanoma brain metastases Histopathology 2015 66289ndash299
24 Silk AW Bassetti MF West BT Tsien CI Lao CD Ipilimumab and ra-diation therapy for melanoma brain metastases Cancer Med 20132899ndash906
25 Knisely JP Yu JB Flanigan J Sznol M Kluger HM Chiang VLRadiosurgery for melanoma brain metastases in the ipilimumab eraand the possibility of longer survival J Neurosurg 2012117227ndash233
26 Kiess AP Wolchok JD Barker CA et al Stereotactic radiosurgeryfor melanoma brain metastases in patients receiving ipilimumabsafety profile and efficacy of combined treatment Int J Radiat OncolBiol Phys 2015 92368ndash375
27 Qian JM Yu JB Kluger HM Chiang VL Timing and type of immunecheckpoint therapy affect the early radiographic response of mela-noma brain metastases to stereotactic radiosurgery Cancer 20161223051ndash3058
28 Silk AW Cao Y Gomez-Hassan D et al A randomized phase IIstudy of ipilimumab induction in patients with melanoma brain me-tastases receiving stereotactic radiosurgery J Clin Oncol 2015 33TPS9079ndashTPS9079
29 Neagu MR Reardon DA An Update on the role of immunotherapyand vaccine strategies for primary brain tumors Curr TreatOptions Oncol 2015 1654
30 Wen PY Reardon DA Phuphanich S et al A randomized double-blind placebo-controlled phase 2 trial of dendritic cell (DC) vaccina-tion with ICT-107 in newly diagnosed glioblastoma (GBM) patientsJ Clin Oncol 2014 322005ndash2005
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
114
British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

7 Pajtler KW et al Molecular Classification of Ependymal Tumorsacross All CNS Compartments Histopathological Grades and AgeGroups Cancer Cell 201527728ndash743
8 Pajtler KW et al The current consensus on the clinical managementof intracranial ependymoma and its distinct molecular variants ActaNeuropathol 20171335ndash12
9 Taylor MD et al Molecular subgroups of medulloblastoma the cur-rent consensus Acta Neuropathol 2012123465ndash472
10 Schwalbe EC et al Novel molecular subgroups for clinical classifi-cation and outcome prediction in childhood medulloblastoma a co-hort study Lancet Oncol 201718958ndash971
11 Cavalli FMG et al Intertumoral Heterogeneity withinMedulloblastoma Subgroups Cancer Cell 201731737ndash754 e736
12 Schindler G et al Analysis of BRAF V600E mutation in 1320 nervoussystem tumors reveals high mutation frequencies in pleomorphicxanthoastrocytoma ganglioglioma and extra-cerebellar pilocytic as-trocytoma Acta Neuropathol 2011121397ndash405
13 Tanaka S et al Epithelioid glioblastoma arising from pleomorphicxanthoastrocytoma with the BRAF V600E mutation Brain TumorPathol 201431172ndash176
14 Banerjee A et al A phase I trial of the MEK inhibitor selumetinib(AZD6244) in pediatric patients with recurrent or refractory low-grade glioma a Pediatric Brain Tumor Consortium (PBTC) studyNeuro Oncol 2017191135ndash1144
15 Hargrave D Bartels U Bouffet E Diffuse brainstem glioma in chil-dren critical review of clinical trials Lancet Oncol 20067241ndash248
16 Schwartzentruber J et al Driver mutations in histone H33 and chro-matin remodelling genes in paediatric glioblastoma Nature2012482226ndash231
17 Wu G et al Somatic histone H3 alterations in pediatric diffuse in-trinsic pontine gliomas and non-brainstem glioblastomas Naturegenetics 201244251ndash253
18 Lewis PW et al Inhibition of PRC2 activity by a gain-of-function H3mutation found in pediatric glioblastoma Science (New York NY2013340857ndash861
19 Mohammad F et al EZH2 is a potential therapeutic target forH3K27M-mutant pediatric gliomas Nature Med 201723483ndash492
20 Piunti A et al Therapeutic targeting of polycomb and BET bromodo-main proteins in diffuse intrinsic pontine gliomas Nature Med201723493ndash500
Brain Tumor Epigenetics From Research to Clinical Practice Volume 2 Issue 3
104
The Value of SurgicalResection for MalignantGliomas in the ModernEra Beyond Extent ofResection
Stephen G Bowden MDSeunggu Jude Han MDDepartment of Neurological Surgery OregonHealth and Sciences University 3303 SW BondAve Center for Health and Healing CH8NPortland OR 97239 Telephone 503-494-4314Fax 503-346-6810 hanseohsuedu
105
Malignant gliomas are among the most difficult oncologi-cal entities to treat Despite aggressive treatment prog-nosis remains poor and recurrence and treatmentfailures seem inevitable The current standard-of-caretherapy includes maximal safe surgical resection fol-lowed by concurrent and adjuvant chemoradiotherapyHistorically surgical resection has conferred greater sur-vival benefit to these patients than adjuvant therapiespresumably through the cornerstone principle of cytore-duction However the extent of surgical resection is fre-quently limited by nearby eloquent tissue and risks to keyneurological functions In addition the value of such ag-gressive approaches has been questioned in light of thewidespread infiltration of glioma cells Meanwhile our un-derstanding of glioma biology continues to advance rap-idly fueled in large part by the acquisition of tumor tissueduring surgery Thus the exact role and value of surgeryparticularly in comparing the clinical benefits of maximalextent of resection (EOR) with the biomedical benefits oftissue provision has been a topic of great interest anddebate in both the neuro-oncological and neurosurgicalcommunities
EOR patient age tumor histology performance statusand molecular markers have been widely accepted assignificant predictors of patient outcomes in malignantglioma9 In the past 2 decades many large retrospectivecohort studies have demonstrated improvements in sur-vival with increasing EOR5917 Due to ethical considera-tions evidence from a randomized prospective studysupporting the clinical benefit of aggressive resectionsdoes not exist and likely never will Instead the closestthing to such evidence in malignant glioma comes fromthe randomized phase III trial comparing surgical resec-tions with or without the use of 5-aminolevulinic acid(5-ALA) The use of 5-ALA serving as a means to and aproxy for greater EOR resulted in extended overall sur-vival for patients with newly diagnosed glioblastoma19 Arecent meta-analysis of 41 117 unique patients by Brownet al adherent to the guidelines of PRISMA (PreferredReporting Items for Systematic Reviews and Meta-Analyses) also demonstrated a clear survival benefit forgross total resection over subtotal resection or biopsy atupfront surgery for glioblastoma1 The body of literatureas a whole clearly favored aggressive resections andthere seemed to be little disagreement for a strategytoward maximal resection when clinically feasibleHowever the challenge still remains when such strategiescome at the risk of neurological morbidity A recent reportby Rahman et al illustrates that the survival benefits fromaggressive resection are lost if the patient develops anew postoperative neurologic deficit as a result15
All the while our understanding of glioma genetics mo-lecular biology and mechanisms of resistance has con-tinued to deepen and evolve borne of thoughtful andsystematic studies using patient-acquired tumor sam-ples Molecular profiles and tumor genetics have proventhemselves to be the best predictors of clinical behaviorand now represent crucial components of the diagnostic
classification scheme of infiltrating gliomas12 With tumortissue at the molecular and genetic level being able to ro-bustly predict patient outcomes accurate tissue diagno-sis has become paramount in the management ofgliomas The role and value of open surgical resection to-ward this end have become clearer as concerns of sam-pling error with biopsy alone led to a number of studiesevaluating the ldquoaccuracyrdquo of stereotactic biopsy proce-dures Jackson et al reported a series of 81 patients whounderwent stereotactic biopsy followed by open surgicalresection The tissue diagnosis was concordant betweenbiopsy and open resection samples in only 51 ofpatients6 Other studies have also demonstrated diagnos-tic concordance between stereotactic biopsy and surgi-cal resection samples in only 57 to 79 ofcases131428 The major limitation of stereotactic biopsyfor infiltrating gliomas likely stems from the significantintratumoral heterogeneity and collectively these studieshighlight the value of open surgical resection in providinga more global representation and understanding of thetumor tissue
The value of extensive resection is perhaps even moreprofound when considering the therapeutic implicationsof such heterogeneity Multiple-site and serial-samplinganalyses have revealed a high degree of both spatial andtemporal heterogeneity within these tumors a conse-quence of serial evolutionary events during tumor growthand progression23 These studies have also led to theconcept of therapy-driven clonal selection and preferen-tial regrowth of resistant cell populations as a potentialmechanism of treatment failure Efforts to expand our un-derstanding of the tremendously complex network ofmutations and biological consequences of chronologicalhierarchy would be greatly facilitated by carefullyplanned thoughtful acquisition of tumor samples duringsurgery
Despite the recent paradigm shift in glioma diagnosticclassification little gains have been made in improvingthe overall prognosis for patients with malignant gliomassince the introduction of concurrent and adjuvant temo-zolomide in 200521 The strategies more recently tested inlarge randomized phase III trials by and large have yieldeddisappointing results while the reasons and mechanismsof treatment failures remain unclear Even so encourag-ing responses have occasionally been seen in varioussubsets of patients and studies exploring the presenceof potential biomarkers have generated intriguing andpromising results in these populations The developmentof the antindashvascular endothelial growth factor monoclonalantibody bevacizumab is one such example Two initialphase II trials showed prolonged progression-free sur-vival in recurrent glioblastoma relative to historical con-trols prompting the US Food and Drug Administration togrant accelerated approval to bevacizumab for recurrentglioblastoma in 2009825 However 2 large randomized tri-als evaluating the addition of bevacizumab to radiationand temozolomide in the newly diagnosed setting failedto show a benefit in overall survival24 and its utility in the
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
106
recurrent setting is now a topic of debate in light of sub-sequent phase III trial results However a post hoc analy-sis of patients enrolled in the AVAglio trial recentlydemonstrated that bevacizumab improved overall sur-vival for those with a proneural subtype tumor18 Just asO6-methylguanine-DNA-methyltransferase (MGMT) pro-moter methylation does for temozolomide the geneticprofile of the tumor could serve as a potential biomarkerof clinical response for bevacizumab as well and valida-tion studies are currently ongoing Such analyses al-though performed post hoc require targeted prospectivecollection of tumor tissue at initial surgery In addition ge-netic profiling of newly diagnosed malignant gliomas willneed to become routine if this approach is to be utilizedwidely Similarly cilengitide an inhibitor of aVb3 andaVb5 integrins with anti-angiogenic properties showedinitial promise in recurrent glioblastoma studies but failedto show any additional benefit in the newly diagnosedsetting20 A subsequent post hoc analysis of the phase IItrial revealed improved progression-free and overall sur-vival in patients with high aVb3 levels in the tumor cells26
However tumor tissues were not systematically collectedand less than half of the patientsrsquo tumor tissues wereavailable for analysis from the phase III trialUnfortunately this drug will most likely not undergo fur-ther development and one cannot help wonder if the out-come would have been different if the enrollment in thephase III trial had been enriched for or restricted to tumorswith high expression of the aVb3 integrin The only trueldquosuccess storyrdquo since the adaptation of radiation andtemozolomide has come from the novel approach of tu-mor treating fields (TTFields) a transcutaneous deliveryof low-intensity intermediate frequency alternating elec-tric fields The multicenter phase III trial EF-14 random-ized patients with supratentorial glioblastoma withoutevidence of tumor progression following standard che-moradiation to receive maintenance treatment withTTFields plus temozolomide or temozolomide alone22
The study was terminated early based on results of aplanned interim analysis demonstrating benefit inprogression-free survival overall survival a secondaryendpoint was also significantly enhanced at this timeDespite the trialrsquos success TTFields has not been univer-sally adopted by the neuro-oncology community andenthusiasm among clinicians and patients remains low27
Experts have raised concerns regarding the study designsuch as its open-label design lacking a sham-treatmentcontrol arm as well as the generalizability of the resultsbased on the unique randomization point occurring afterconcurrent chemoradiation16 Perhaps most significantlya lack of widely understood mechanism of action hasalso been raised as a factor with comparison to othertreatments the preclinical data for TTFields is relativelylacking particularly when applied in conjunction with che-moradiation27 Even during the early phase stages theuse of robust tissue-based analyses exploring the mech-anism of action such as dose response modeling andmultisite tissue biopsies may have mitigated some of
these concerns and led to wider acceptance by the com-munity Bevacizumab and cilengitide clearly benefitedfrom retrospective analyses of human tumor tissue toidentify susceptible treatment populations while the en-thusiasm for TTFields is perhaps in part tempered by thelack thereof Collectively the evolution of these treat-ments underscores the value of extensive targeted tissuesampling in furthering development of new adjunctivetherapies
Open surgical resection of tumors with such targeted tis-sue acquisition for analysis will continue to play a key rolein prospective clinical trial designs Comparison ofpretreatment and posttreatment tissue profiles representsa valuable line of investigation by delving into mecha-nisms of therapeutic action as well as mechanisms oftreatment failures1011 It also provides an opportunity toinvestigate a number of key fundamental steps along anagentrsquos path to clinical success such as does the agentsuccessfully traffic to the tumor if so how much anddoes the agent then actually have its hypothesizedeffects at the biochemical or cellular level Thusearly-phase trials can and should include posttreatmentmolecular endpoints when possible in addition to safetyendpoints Immunotherapy and immune checkpoint inhi-bition represent exciting novel therapeutic approachesfor neuro-oncology particularly based on their success inmetastatic cancers Large phase III trials studying block-ade of the programmed cell death protein (PD)1PDligand 1 axis with monoclonal antibodies for newlydiagnosed and recurrent glioblastoma are under way butinitial reports have been concerning for negative resultsAs in the development of many previous novel agentstissue-based mechanism studies have been largely lack-ing in the preclinical phases However an Alliance-supported trial currently enrolling focuses on a biomarkeras a primary endpoint patients with recurrent glioblas-toma indicated for surgery are randomized to receivepembrolizumab a PD1 inhibitor either before or aftersurgery (NCT02852655) The resected tumor tissue willthen be analyzed for the profile of tumor-infiltratingT cells and comparison will be made between the 2groups This study represents a tremendously valuableopportunity to explore the impact and the potential chal-lenges of checkpoint inhibition for malignant gliomas inthe clinical setting and should the large phase III trialsend up negative this pilot study will be very informative
Advances in imaging biomarkers and molecular charac-terization of gliomas in conjunction with new targetedtherapies will continue to improve and transform themanagement of these tumors Multimodality imaging cannow more accurately reflect ongoing biological processeswithin these tumors such as the presence of oncogenicmutations or cells undergoing malignant transformationNovel biomarkers such as circulating tumor DNA showpromise in detecting early recurrence or monitoring treat-ment response3724 Lastly the new classification schemerevolving around molecular characterization will provide a
Volume 2 Issue 3 The Value of Surgical Resection for Malignant Gliomas in the Modern Era
107
necessary corollary to these novel diagnostic tools Itremains indisputable however that clinical validation ofthese novel diagnostic tools will also require systematiccorrelation with human tumor tissue obtained throughsurgery These samples ideally gathered prospectivelywill provide a pivot upon which we can expand our under-standing of the complex network of oncological pro-cesses driving these tumors
Malignant gliomas are incredibly challenging disease en-tities in many ways due to the inter- and intratumoral het-erogeneity that is a hallmark of them Experience to datehints that future successes in malignant gliomas rest inneuro-oncology entering the era of precision medicinewhere validated biomarkers and targeted personalizedtherapies are seamlessly integrated into the managementparadigm Accordingly systems supporting surgical re-section and patient-specific tumor tissue analysis mustbe built and organized to guide the decision making fortherapy As our overall approach to the management ofmalignant gliomas evolves so should the framework ofsurgical management The clinical benefits of maximalsafe resection are well founded and well reportedHowever the oncological neurosurgeon must now lookbeyond maximal cytoreduction itself and recognize thevalue of thoughtful acquisition and analysis of tumor tis-sue Modern neurosurgeons must consider themselvessurgical neuro-oncologists and engagement and partici-pation of surgeons into clinical trials particularly early-phase trials should be encouraged and valued In turnwe should provide our surgical trainees with the trainingand tools in neuro-oncology to help them participate andcontribute in multidisciplinary collaborative efforts aimingto advance the understanding of brain tumor biology andultimately improve the outlook of our patients
References
1 Lacroix M Abi-Said D Fourney DR Gokaslan ZL et al A multivariateanalysis of 416 patients with glioblastoma multiforme prognosisextent of resection and survival J Neurosurg 2001 95190ndash198
2 Hervey-Jumper SL Berger MS Maximizing safe resection of low-and high-grade glioma J Neurooncol 2016 130269ndash282
3 Sanai N Polley MY McDermott MW Parsa AT Berger MS An ex-tent of resection threshold for newly diagnosed glioblastomas JNeurosurg 2011 1153ndash8
4 Stummer W Pichlmeier U Meinel T et al Fluorescence-guided sur-gery with 5-aminolevulinic acid for resection of malignant glioma arandomised controlled multicentre phase III trial Lancet Oncol2006 7392ndash401
5 Brown TJ Brennan MC Li M et al Association of the extent ofresection with survival in glioblastoma a systematic review andmeta-analysis JAMA Oncol 2016 21460ndash1469
6 Rahman M Abbatematteo J De Leo EK et al The effects of new orworsened postoperative neurological deficits on survival of patientswith glioblastoma J Neurosurg 2017 127123ndash131
7 Louis DN Perry A Reifenberger G et al The 2016 World HealthOrganization Classification of Tumors of the Central NervousSystem a summary Acta Neuropathol 2016 131803ndash820
8 McGirt MJ Bulsara KR Cummings TJ et al Prognostic value ofmagnetic resonance imaging-guided stereotactic biopsy in the
evaluation of recurrent malignant astrocytoma compared with a le-sion due to radiation effect J Neurosurg 2003 9814ndash20
9 Muragaki Y Chernov M Maruyama T et al Low-grade glioma onstereotactic biopsy how often is the diagnosis accurate MinimInvasive Neurosurg 2008 51275ndash279
10 Woodworth G McGirt MJ Samdani A Garonzik I Olivi AWeingart JD Accuracy of frameless and frame-based image-guided stereotactic brain biopsy in the diagnosis of glioma com-parison of biopsy and open resection specimen Neurol Res 200527358ndash362
11 Suzuki H Aoki K Chiba K et al Mutational landscape and clonal ar-chitecture in grade II and III gliomas Nat Genet 2015 47458ndash468
12 Stupp R Mason WP van den Bent MJ et al Radiotherapy plus con-comitant and adjuvant temozolomide for glioblastoma N Engl JMed 2005 352987ndash996
13 Kreisl TN Kim L Moore K et al Phase II trial of single-agent bevaci-zumab followed by bevacizumab plus irinotecan at tumor progres-sion in recurrent glioblastoma J Clin Oncol 2009 27740ndash745
14 Vredenburgh JJ Desjardins A Herndon 2nd JE et al Phase II trial ofbevacizumab and irinotecan in recurrent malignant glioma ClinCancer Res 2007 131253ndash1259
15 Chinot OL Wick W Mason W et al Bevacizumab plusradiotherapy-temozolomide for newly diagnosed glioblastomaN Engl J Med 2014 370709ndash722
16 Gilbert MR Dignam JJ Armstrong TS et al A randomized trial ofbevacizumab for newly diagnosed glioblastoma N Engl J Med2014 370699ndash708
17 Sandmann T Bourgon R Garcia J et al Patients with proneural glio-blastoma may derive overall survival benefit from the addition of bev-acizumab to first-line radiotherapy and temozolomide retrospectiveanalysis of the AVAglio trial J Clin Oncol 2015 332735ndash2744
18 Jackson RJ Fuller GN Abi-Said D et al Limitations of stereotacticbiopsy in the initial management of gliomas Neuro Oncol 20013193ndash200
19 Stupp R Hegi ME Gorlia T et al Cilengitide combined with stan-dard treatment for patients with newly diagnosed glioblastoma withmethylated MGMT promoter (CENTRIC EORTC 26071-22072study) a multicentre randomised open-label phase 3 trial LancetOncol 2014 151100ndash1108
20 Weller M Nabors LB Gorlia T et al Cilengitide in newly diagnosedglioblastoma biomarker expression and outcome Oncotarget2016 715018ndash15032
21 Stupp R Taillibert S Kanner AA et al Maintenance therapy withtumor-treating fields plus temozolomide vs temozolomide alone forglioblastoma a randomized clinical trial JAMA 20153142535ndash2543
22 Wick W TTFields where does all the skepticism come from NeuroOncol 2016 18303ndash305
23 Sampson JH Alternating electric fields for the treatment of glioblas-toma JAMA 2015 3142511ndash2513
24 Lang FF Asher A Prospective clinical trials of brain tumor therapy thecritical role of neurosurgeons J Neurooncol 2004 69151ndash167
25 Lang FF Gilbert MR Puduvalli VK et al Toward better early-phasebrain tumor clinical trials a reappraisal of current methods and pro-posals for future strategies Neuro Oncol 2002 4268ndash277
26 Elkhaled A Jalbert L Constantin A et al Characterization of metab-olites in infiltrating gliomas using ex vivo (1)H high-resolution magicangle spinning spectroscopy NMR Biomed 2014 27578ndash593
27 Jalbert LE Neill E Phillips JJ et al Magnetic resonance analysis ofmalignant transformation in recurrent glioma Neuro Oncol 2016181169ndash1179
28 Touat M Duran-Pena A Alentorn A Lacroix L Massard C Idbaih AEmerging circulating biomarkers in glioblastoma promises andchallenges Expert Rev Mol Diagn 2015 151311ndash1323
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
108
Update on RadiationCombinations in theTreatment of Patientswith Malignant BrainTumors FromRadiosensitizers toImmunotherapy
Debra Nana Yeboa MD1
Erik P Sulman MD PhD123
Departments of 1Radiation Oncology2Translational Molecular Pathology and3Genomic Medicine The University of Texas MDAnderson Cancer Center 1515 Holcombe BlvdUnit 97 Houston Texas USA Tel 713-563-2300dnyeboamdandersonorg andepsulmanmdandersonorg
109
AbstractAdvances in radiosensitizers and immunotherapyhave ushered in a new frontier in brain tumortreatment The brain has often been viewed as asanctuary site due to the bloodndashbrain barrier andthus the 2 primary modalities of therapy includedsurgery and radiation therapy (RT) More recentlysystemic therapies have played a greater role aseither combination therapy radiosensitizers or im-munotherapy Two novel radiosensitizers are beingdeveloped for the treatment of brain metastasesRRx-001 for example is a small molecule thataccelerates the NO2 to NO conversion of deoxyhe-moglobin and the agent 2-dexoyglucose (2-DG) is anonmetabolized glucose analogue that interfereswith ATP formation Poly(ADP-ribose) DNA polymer-ase inhibitors are promising due to their distinctradiobiological effects Veliparib and olaparib areamong the most studied with randomized trialsexploring their use in gliomas and brain metastasesImmunotherapy including immune checkpoint inhib-itors may play a role for both primary gliomas andbrain metastases RT has been shown to enhancethe function of cytotoxic T lymphocytes induce infil-tration of cytotoxic T lymphocytes and enhancefunction Trials are presently exploring use of bothprogrammed cell death protein (PD)1 and PD ligand1 blockade in glioblastoma patients with radiationSimilarly several immunotherapies are being investi-gated with either stereotactic radiosurgery or wholebrain radiation therapy for brain metastases In thisreview the use of radiosensitizers and immunother-apy agents with RT will be discussed broadly
Keywords brain metastases brain tumors gliomasimmunotherapy radiation therapy radiosensitizers
Radiosensitizers andImmunotherapy inBrain TumorsAdvances in radiosensitizers and immunotherapy haveushered in a new frontier to brain tumor treatment Braintumors however are a diverse class sharing only similaranatomic location Both primary brain malignancies andbrain metastasis have widely diverse histologies and mo-lecular phenotypes With the bloodndashbrain barrier thebrain has often been viewed as a sanctuary site and thusthe 2 primary modalities of therapy included surgery andradiation with decreased benefit from systemic agentsdue to lack of brain penetration However more recentlysystemic therapies have played a greater role as eithercombination therapy radiosensitizers or immunother-apy While temozolomide (TMZ) has played a pivotal rolefor glioblastoma (GBM) only a subset of patients benefitfrom the treatment1 The use of alternative systemicagents that may potentiate the effects of radiation ther-apy (RT) is becoming increasingly appealing Similarly forbrain metastases a variety of systemic agents are beingexplored primarily based on histology and immune pro-file In this review the use of radiosensitizers and immu-notherapy agents currently under investigation with RTwill be discussed
RadiosensitizersThe guiding concept of radiation sensitization is to in-crease the biologic effect of radiation such as increasedDNA damage decreased DNA repair decreased hypoxiaor increased G2M cell cycle blockade leading to im-proved tumor control and increased patient survival2
Poly(adenosine diphosphate-ribose) DNA polymerase(PARP) inhibitors are promising radiosensitizers due totheir roles in DNA repair3 PARP inhibitors work againstPARP1 a nuclear enzyme involved in the recruitment ofrepair proteins used in base excision repair and single-strand break repair PARP1 may also play a role in nonho-mologous end-joining4 The primary investigation ofPARP inhibitors has been in potentiating radiation andchemotherapy effects the latter in the context of homolo-gous repair deficient tumors For radiation the primarymechanism of action is inducing damage to nucleotidesleading to single-strand and double-strand breaks ThusPARP inhibitors in combination with radiation have an ap-pealing mechanism to inhibit or delay DNA repair andlikely convert more single-strand breaks to double-strandbreaks4
While several PARP inhibitors are currently being evalu-ated in a variety of tumors including talazoparib and nira-parib veliparib and olaparib are among the most studiedand there are randomized trials exploring their use in
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
110
gliomas The US National Cancer Institute (NCI)ndashfundedAlliance for Clinical Trials in Oncology (Alliance) A071102is a randomized phase IIIII trial evaluating the use ofveliparib in combination with TMZ in the adjuvant settingin patients with GBM tumors exhibiting hypermethylationof the O6 methylguanine DNA methyltransferase (MGMT)gene promoter Preclinical data supporting this trial sug-gested that only patients with MGMT methylated tumorswould benefit from the combination a group of patientsfor whom TMZ concurrent with radiation might be mostbeneficial5 A phase I trial performed by the NCI-fundedAmerican Brain Tumor Consortium attempted to combineveliparib with radiation and TMZ but failed to identify asuitable recommended phase II dose due to significanthemotoxicity6 Thus attempts to combine radiation withveliparib have focused on patients least likely to benefitfrom TMZ namely with MGMT unmethylated tumors forwhom TMZ could be withheld The Australian VeliparibRT and TMZ trial in newly diagnosed unmethylatedMGMT glioblastoma (VERTU) is a single-arm study inwhich patients receive RT with veliparib followed by adju-vant TMZ and veliparib4
An ongoing novel approach to radiosensitize gliomasinvolves a combination with an agent that interferes withan essential metabolic process 2-Dexoyglucose (2-DG)is a nonmetabolized glucose analogue that acts as acompetitive inhibitor of glycolysis It is transported acrossthe bloodndashbrain barrier by the glucose transporter GLUT-1 and thus has good penetration into the CNSIntracellularly it is trapped and accumulates in cells simi-lar to the mechanism of 18-fluorodeoxyglucose 2-DG isphosphorylated by glycolytic enzymes and the
phosphorylated 2-DG (2-deoxyglucose-P) is trapped in-tracellularly Inhibition of hexokinase activity by 2-DGinterferes with ATP formation and results in tumor celldeath7 While it has positive attributes by selectively tar-geting metabolically active tumor cells 2-DG has alsobeen associated with Q-T prolongation The currentphase III trial in gliomas is assessing the toxicity and tol-erability of 2-DG with hypofractionated radiation of 5 Gyas a radiosensitizer7
Two novel radiosensitizers are being developed for thetreatment of brain metastases First RRx-001 is a smallmolecule initially designed by the aerospace industry Itworks in part as a radiosensitizer by increasing blood flowand thus oxygenation of tumors through nitric oxideRRx-001 which binds to hemoglobin accelerates theNO2 to NO conversion of deoxyhemoglobin It workslocally under hypoxic conditions and subsequentlythe radiosensitive effects through nitric oxide are invasodilation and inhibiting DNA repair enzymes8 Nitricoxide is relatively benign The higher levels of oxidativestress with H2O2 and superoxide in tumors in comparisonto normal tissues result in the preferential generation ofreactive peroxynitrite in the presence of higher nitric oxidelevels7 This accounts for the increased specificity anddecreased toxicity with RRx-001 The dose limiting toxic-ity in a phase I trial of 25 patients treated with eitherweekly or biweekly infusions was infusional pain relatedto the release of NO at the site of injection7 Outside ofpreclinical models 2 clinical reports examining wholebrain radiation therapy (WBRT) with RRx-001 reported anintracranial response A patient with melanoma and 2hemorrhagic edematous lesions of 26 cm and 33 cm
Table 1 Clinical trials involving immunotherapy and radiation therapy1213
Clinical Trials Number Phase Disease Type Treatment Groups
NCT02667587 II Newly diagnosed GBMMGMT-methylated
Nivolumabthorn TMZthorn RT vs placebothornTMZ thorn RT
NCT02617589 III Newly diagnosed GBM Nivolumabthorn RT vs TMZthorn RTNCT02336165 II Newly diagnosed unmethylated
MGMT recurrent glioblastomaMEDI4736thorn standard RT vs MEDI4736 thorn
bevacizumabNCT02530502 III Newly diagnosed GBM RTthorn TMZthorn pembrolizumab TMZthorn
pembrolizumabNCT02313272 I Recurrent glioma Hypofractionated stereotactic radiationthorn
pembrolizumab thorn bevacizumabNCT02696993 III Brain metastases Nivolumabthorn SRS nivolumabthornWBRT
nivolumabthorn ipilimumab thorn SRS nivolu-mabthorn ipilimumab thornWBRT
NCT02115139 II Melanoma brain metastases Ipilimumab thornWBRTNCT02097732 II Melanoma brain metastases Ipilimumab SRS ipilimumab vs SRS
ipilimumabNCT01703507 I Melanoma brain metastases Ipilimumab thornWBRT vs ipilimumab thorn SRSNCT02107755 II Melanoma brain metastases Ipilimumab thorn SRSNCT02858869 pilot Melanoma and NSCLC Pembrolizumabthorn SRSNCT01950195 I Melanoma brain metastases Ipilimumab thorn SRSNCT02662725 II Melanoma brain metastases Ipilimumab thorn SRS
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
111
after a single intravenous dose of RRx-001 of 5 mgm2 4days before WBRT resulted in symptomatic improvementwithin 48 hours By 4 months after radiation there was areduction in size in the largest dimension down to 10 cmand 23 cm of the respective lesions A second report of amelanoma patient with at least 18 lesions after receivingRRx-001 of 5 mgm2 4 days before WBRT as well astwice weekly doses during the 2 weeks of radiation alsoshowed response The patient at 4 months had disap-pearance of 13 of 18 lesions with shrinkage of theremaining 5 lesions8 Presently BRAINSTORM is a phaseIII dose escalation trial of RRx-001 designed to be ad-ministered twice weekly for 2 weeks with WBRT (30 Gy in10 fractions) with the option for weekly maintenance8
Veliparib has also been evaluated in the setting of brainmetastases It was tested in a global randomized con-trolled trial with WBRT Veliparib is orally bioavailable andcrosses the bloodndashbrain barrier It was first examined in amultihistology phase I trial in patients with nonndashsmall celllung cancer (NSCLC) breast cancer melanoma and re-nal and colorectal cancers among others The study of81 patients tested dose tolerance of veliparib from 10 to300 mg orally twice a day with WBRT to 30 Gy in 10 frac-tions or 375 Gy in 15 fractions9 The phase I trial dose es-calation portion did not reach the predefined criteria forthe maximum tolerated dose but there was amplificationof the adverse effects of nausea and vomiting among thehighest dose cohort of 300 mg bid9 The adverse eventprofile at 200 mg bid was similar to that of WBRT aloneDoses of veliparib from 20 to 200 mg bid demonstratesimilar antitumor activity and other studies in preclinicalmodels found that 50 mg daily demonstrated significantreduction in poly(ADP-ribose) in peripheral blood mono-nuclear cells and tumor tissue while also effectivelycrossing the bloodndashbrain barrier Thus the subsequentphase II trial examined 50 mg with WBRT9 In order to as-sess a more homogeneous cohort the phase III globalrandomized trial studied only NSCLC at the 2 doses of50 mg and 200 mg twice daily versus placebo twice a daywith WBRT10 The primary endpoint was overall survivalIn 307 patients in a 111 randomization of 50 mg bid200 mg bid or placebo twice daily the study found nosignificant differences in overall survival among the differ-ent groups10 The majority of patients across the treat-ment groups had a graded prognostic assessment (GPA)score of25 and a Karnofsky performance status ofgt80 The median overall survival was 185 days forpatients receiving placebo and 209 days for those receiv-ing veliparib without any statistically significant differ-ence These results were similar to the disease-specificestimate of median survival for the disease-specific GPAof NSCLC patients with brain metastases10
Several other radiosensitizers have failed to improve overradiation alone in a number of trials These have includedtrials with WBRT including motexafin gadolinium efap-roxyn bortozemib thalidomide teniposide topotecanpaclitaxel and cisplatin7 Of note other PARP inhibitorsalso being assessed include talazoparib and niraparib4
which may yield positive results The use of valproic acid(VPA) as a histone deacetylase inhibitor has also beenconsidered to have radiosensitizing potential in additionto its anti-epileptic drug properties11 While studies havereported that patients with GBM receiving an anti-epilep-tic agent may have higher overall survival than those re-ceiving standard chemoradiation therapy alone thebenefit remains controversial Retrospective analysissuggested that patients taking VPA specifically had bettersurvival in comparison to other anti-epileptic drugs Alsoa recent prospective phase II trial was performed in 37patients with GBM receiving VPA 25 mgkg concurrentlywith TMZ chemoradiation and reported a median survivalof 296 months While controversial further data andinvestigation are needed into this and other agents thatmay potentiate RT
Immunotherapy and radiationImmune checkpoint inhibitors lead to activation of T cellswhich may traffic across the bloodndashbrain barrier to inter-act with tumor Primary brain tumors may evade the im-mune system through upregulation of immunecheckpoints and possible immunosuppression12
Monoclonal antibodies promote immune-mediated anti-tumor activity by inhibiting the immune functionndashmediated cytotoxic T-lymphocyte associated protein 4(CTLA-4) and programmed cell death protein 1 (PD-1)receptors PD protein ligand (PD-L1) is upregulated inGBM through oncogenic signaling possibly throughphosphatase and tensin homolog loss and interleukin-10signaling1314 RT has also been shown to enhance thefunction of cytotoxic T lymphocytes RT may induce aninfiltration of cytotoxic T lymphocytes and enhance theirfunction It may also induce antindashCTLA-4 agents inhibitingT-cell function and increasing the CD8thorn T cellregulatoryT cell ratio in cases of melanoma15 Thus PD-1 and PD-L1 blockers may have a further role in CNS managementwith the use of radiation
In preclinical models radiation has been examined withimmunotherapy that included among other mechanismsvaccination PD-1 blockade and CTLA-4 blockade Inmice radiation plus a vaccination of irradiated gliomacells was associated with increased survival of 40 to80 compared with 0 to 10 for other groups stud-ied16 A benefit of PD-1 blockade with stereotactic radio-surgery (SRS) specifically has also been shown in amouse model In comparison to mice treated with radia-tion antindashPD-1 therapy or a combination only those re-ceiving combination therapy had a higher percentagesurvival alive beyond 180 days after treatment17 Othermouse carcinoma models have identified response withanti-CTLA antibody and fractionated radiation therapy18
CD137 activation CTLA-4 blockade and focal radiationtherapy have been examined in an immunocompetent in-tracranial GBM model Mice treated with triple combina-tion therapy had 50 greater survival19 In other murine
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
112
models the use of antindashPD-1 and antindashCTLA-4 agentsshowed improved survival and increased tumor infiltratingleukocyte populations compared with single modalitywith concurrent radiation16 There are conflicting data re-garding timing or sequencing of therapy with some ani-mal models showing no difference in tumor response inrelation to timing of RT and delivery of immunotherapy18
For instance in one animal model CTLA-4 blockade de-livered simultaneously with radiation or delivered a coupleof days after showed no difference in survival among themice19
Increased PD-1 expression in circulating monocytes hasbeen identified as a biomarker for tumor-induced immu-nosuppression and may serve as a prognostic factor forpotentially worse survival outcomes in clinic13 In onestudy GBM patients with lower PD-L1 expression hadhigher median overall survival than those with higher PD-L1 expression suggesting that lower expression may beassociated with less immunosuppression and more im-mune activity against the tumor glioma20 RT with immunecheckpoint blockade is being investigated to assess if theaddition of PD-1 and PD-L1 inhibitors may improve theoutcomes or toxicity profile of standard therapy For in-stance a multi-institutional trial opened as a phase III willevaluate outcomes in GBM receiving radiation and pem-brolizumab with TMZ (NCT02530502) Next durvalumabor MEDI4736 a PD-L1 inhibitor is being examined forunmethylated MGMT GBMs with standard radiotherapy(NCT02336165)12 The impact of checkpoint inhibitorsduring adjuvant treatment of GBM is currently beingevaluated in the NCI-funded NRG-BN002 trial(NCT02311920) which will evaluate the antindashCTLA-4antibody ipilimumab alone or in combination with theantindashPD-1 antibody nivolumab for patients with newlydiagnosed GBM
Brain metastases have clonal populations of cells differ-ent from the rest of the brain and a unique microenviron-ment that may influence immunotherapy There may bemore immune infiltrates in metastases than in primarybrain tumors21 PD-L1 expression in brain metastasesvaries by histology In a series evaluating PD-L1 expres-sion in various tumors including melanoma NSCLCbreast renal colorectal and small cell less than 10showed significant expression22 There was greatest ex-pression among NSCLC and melanoma with a correla-tion between PD-L1 expression and tumor infiltratinglymphocytes22 Institutional series have examined thecombination of radiation and immune checkpoint block-ade In another study specific to melanoma brain metas-tases PD-L1 expression was found in over 50 of thecases and among those cases over 40 expressedPD-L1 in more than 5 of tumor cells23 The largest bodyof data for use of PD-L1 with radiation is for melanomaand NSCLC
Ipilimumab is a human monoclonal antibody that blocksCTLA-4 and allows for T-cell activation and proliferationto enhance the immune response to cancer In a
retrospective review of 70 patients with brain metastasestreated with SRS or WBRT the 33 patients receiving im-munotherapy had a median survival of 183 months incomparison to the 37 patients who did not receive ipili-mumab with a median survival of 53 months While therewere limited data among the cohort to evaluate sequenc-ing of therapy among 10 evaluable patients 40 whoreceived ipilimumab prior to RT had a partial response incomparison to only 10 among the cohort of 22 evalu-able patients who did not receive ipilimumab therapy atall with radiation24 Another retrospective institutionalstudy of 77 patients in which 37 received ipilimumabfound that patients treated with SRS and ipilimumab hada median survival of 213 months versus 49 months forthose not receiving ipilimumab Most interestingly theyidentified that the correlation remained significant evenafter adjusting for additional factors such as performancestatus Secondly there was not an increased need for useof salvage WBRT25
The sequencing of radiotherapy and immune checkpointinhibitors is of interest In a study of patients with brainmetastases the one-year survival for patients receivingSRS before ipilimumab was greater at 65 in contrast to56 for those receiving it concurrently and 40 for thosereceiving it after SRS26 Similarly another study of 75patients with 566 brain metastases showed greater tu-mor lesion response at 6 months from SRS for patientsreceiving ipilimumab nivolumab or pembrolizumabwithin 4 weeks of their SRS27 Those receiving concurrenttherapy had by 6 months a decrease of 949 in compar-ison to 662 for those not receiving checkpoint inhibi-tors within 4 weeks Prospective clinical trials areinvestigating different combinations of RT with immunecheckpoint blockers in this setting For instance new tri-als are currently evaluating intracranial tumor control at 6months and the timing of immune therapy or immunecheckpoint inhibitors in relation to SRS28
Vaccines are also being developed for primary braintumors showing some evidence for their use Vaccinesdeveloped from dendritic cells and tumor lysate with tu-mor antigens such as the epidermal growth factor recep-tor variant III vaccine have shown promise29 Forinstance in a placebo controlled phase II trial of ICT-107a vaccine composed on autologous dendritic cells andtumor antigens progression-free survival was increasedby 2 months for those receiving the vaccine30 Radiationmay assist in serving as a primer for the immunogeniceffects by facilitating tumor antigen uptake by dendriticcells and cross presentation on major histocompatibilitycomplex I Thus RT may assist in the tumor-specific cy-totoxic T lymphocytes associated with the immunemechanism
In conclusion although there may be challenges to com-bining and sequencing brain tumors radiosensitizersand immunotherapy the opportunities and potential fornovel applications are promising For brain tumors brainmetastases are typically underrepresented in trials
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
113
despite being among the most common intracraniallesions Despite their large population patients with brainmetastases are often excluded from clinical trials withnovel agents due to concerns regarding confounding out-comes and tolerability12 Primary gliomas also offer anovel frontier for the use of immunotherapy to standardadjuvant chemotherapy and radiation particularly forpatients with GBM less likely to respond to TMZ such aswith unmethylated MGMT As studies work to define therole of RT and radiosensitizers and immunotherapy fur-ther analysis is needed to assess the timing of RT andthese treatments
References
1 Stupp R Hegi ME Mason WP et al Effects of radiotherapy withconcomitant and adjuvant temozolomide versus radiotherapy aloneon survival in glioblastoma in a randomised phase III study 5-yearanalysis of the EORTC-NCIC trial Lancet Oncol 2009 10459ndash466
2 Lawrence TS Blackstock AW McGinn C The mechanism of actionof radiosensitization of conventional chemotherapeutic agentsSemin Radiat Oncol 2003 1313ndash21
3 Lesueur P Chevalier F Austry JB et al Poly-(ADP-ribose)-polymer-ase inhibitors as radiosensitizers a systematic review of pre-clinicaland clinical human studies Oncotarget 2017 8(40)69105ndash69124
4 Lester A Rapkins R Nixdorf S Khasraw M McDonald KCombining PARP inhibitors with radiation therapy for the treatmentof glioblastoma is PTEN predictive of response Clin Transl Oncol2017 19273ndash278
5 Gupta SK Kizilbash SH Carlson BL et al Delineation of MGMT hyper-methylation as a biomarker for veliparib-mediated temozolomide-sensi-tizing therapy of glioblastoma J Natl Cancer Inst 2016 108
6 Kleinberg LR Blakeley J Mikkelsen T et al An American BrainTumor Consortium (ABTC) phase 1 trial of veliparib (ABT-888)temozolomide (TMZ) and concurrent radiation therapy (RT) fornewly diagnosed glioblastoma multiforme (GBM) need for modifica-tion to approach for combining these therapies InternationalJ Radiat Oncol Biol Phys 2012 84S7ndashS8
7 Oronsky BT A Review of two promising radiosensitizers in brainmetastases Rrx-001 and 2-deoxyglucose In NC Oronsky edJ Cancer Sci Ther 2015 pp 137ndash141
8 Kim MM Parmar H Cao Y et al Concurrent whole brain radiother-apy and RRx-001 for melanoma brain metastases Neuro Onc2016 18455ndash456
9 Mehta MP Wang D Wang F et al Veliparib in combination withwhole brain radiation therapy in patients with brain metastasesresults of a phase 1 study J Neurooncol 2015 122409ndash417
10 Chabot P Hsia TC Ryu JS et al Veliparib in combination withwhole-brain radiation therapy for patients with brain metastasesfrom non-small cell lung cancer results of a randomized globalplacebo-controlled study J Neurooncol 2017 131105ndash115
11 Ochiai S Nomoto Y Yamashita Y et al Roles of valproic acid inimproving radiation therapy for glioblastoma a review of literaturefocusing on clinical evidence Asian Pac J Cancer Prev 201617463ndash466
12 Tan AC Heimberger AB Menzies AM Pavlakis N Khasraw MImmune checkpoint inhibitors for brain metastases Curr Oncol Rep2017 1938
13 DrsquoSouza NM Fang P Logan J Yang J Jiang W Li JCombining radiation therapy with immune checkpoint blockade
for central nervous system malignancies Frontiers Oncol 20166212
14 Parsa AT Waldron JS Panner A et al Loss of tumor suppressorPTEN function increases B7-H1 expression and immunoresistancein glioma Nat Med 2007 1384ndash88
15 Binder DC Davis AA Wainwright DA Immunotherapy for cancer inthe central nervous system current and future directionsOncoimmunology 2016 5e1082027
16 Newcomb EW Demaria S Lukyanov Y et al The combination ofionizing radiation and peripheral vaccination produces long-termsurvival of mice bearing established invasive GL261 gliomas ClinCancer Res 2006 124730ndash4737
17 Zeng J See AP Phallen J et al Anti-PD-1 blockade and stereotac-tic radiation produce long-term survival in mice with intracranial glio-mas Int J Radiat Oncol Biol Phys 2013 86343ndash349
18 Chow KK Hara W Lim M Li G Combining immunotherapy withradiation for the treatment of glioblastoma J Neurooncol2015123459ndash464
19 Belcaid Z Phallen JA Zeng J et al Focal radiation therapy com-bined with 4-1BB activation and CTLA-4 blockade yields long-termsurvival and a protective antigen-specific memory response in amurine glioma model PLoS One 2014 9e101764
20 Topalian SL Hodi FS Brahmer JR et al Safety activity and im-mune correlates of anti-PD-1 antibody in cancer N Engl J Med2012 3662443ndash2454
21 Bienkowski M Preusser M Prognostic role of tumour-infiltrating in-flammatory cells in brain tumours literature review Curr OpinNeurol 2015 28647ndash658
22 Harter PN Bernatz S Scholz A et al Distribution and prognostic rel-evance of tumor-infiltrating lymphocytes (TILs) and PD-1PD-L1 im-mune checkpoints in human brain metastases Oncotarget 2015640836ndash40849
23 Berghoff AS Ricken G Widhalm G et al Tumour-infiltrating lym-phocytes and expression of programmed death ligand 1 (PD-L1) inmelanoma brain metastases Histopathology 2015 66289ndash299
24 Silk AW Bassetti MF West BT Tsien CI Lao CD Ipilimumab and ra-diation therapy for melanoma brain metastases Cancer Med 20132899ndash906
25 Knisely JP Yu JB Flanigan J Sznol M Kluger HM Chiang VLRadiosurgery for melanoma brain metastases in the ipilimumab eraand the possibility of longer survival J Neurosurg 2012117227ndash233
26 Kiess AP Wolchok JD Barker CA et al Stereotactic radiosurgeryfor melanoma brain metastases in patients receiving ipilimumabsafety profile and efficacy of combined treatment Int J Radiat OncolBiol Phys 2015 92368ndash375
27 Qian JM Yu JB Kluger HM Chiang VL Timing and type of immunecheckpoint therapy affect the early radiographic response of mela-noma brain metastases to stereotactic radiosurgery Cancer 20161223051ndash3058
28 Silk AW Cao Y Gomez-Hassan D et al A randomized phase IIstudy of ipilimumab induction in patients with melanoma brain me-tastases receiving stereotactic radiosurgery J Clin Oncol 2015 33TPS9079ndashTPS9079
29 Neagu MR Reardon DA An Update on the role of immunotherapyand vaccine strategies for primary brain tumors Curr TreatOptions Oncol 2015 1654
30 Wen PY Reardon DA Phuphanich S et al A randomized double-blind placebo-controlled phase 2 trial of dendritic cell (DC) vaccina-tion with ICT-107 in newly diagnosed glioblastoma (GBM) patientsJ Clin Oncol 2014 322005ndash2005
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
114
British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

The Value of SurgicalResection for MalignantGliomas in the ModernEra Beyond Extent ofResection
Stephen G Bowden MDSeunggu Jude Han MDDepartment of Neurological Surgery OregonHealth and Sciences University 3303 SW BondAve Center for Health and Healing CH8NPortland OR 97239 Telephone 503-494-4314Fax 503-346-6810 hanseohsuedu
105
Malignant gliomas are among the most difficult oncologi-cal entities to treat Despite aggressive treatment prog-nosis remains poor and recurrence and treatmentfailures seem inevitable The current standard-of-caretherapy includes maximal safe surgical resection fol-lowed by concurrent and adjuvant chemoradiotherapyHistorically surgical resection has conferred greater sur-vival benefit to these patients than adjuvant therapiespresumably through the cornerstone principle of cytore-duction However the extent of surgical resection is fre-quently limited by nearby eloquent tissue and risks to keyneurological functions In addition the value of such ag-gressive approaches has been questioned in light of thewidespread infiltration of glioma cells Meanwhile our un-derstanding of glioma biology continues to advance rap-idly fueled in large part by the acquisition of tumor tissueduring surgery Thus the exact role and value of surgeryparticularly in comparing the clinical benefits of maximalextent of resection (EOR) with the biomedical benefits oftissue provision has been a topic of great interest anddebate in both the neuro-oncological and neurosurgicalcommunities
EOR patient age tumor histology performance statusand molecular markers have been widely accepted assignificant predictors of patient outcomes in malignantglioma9 In the past 2 decades many large retrospectivecohort studies have demonstrated improvements in sur-vival with increasing EOR5917 Due to ethical considera-tions evidence from a randomized prospective studysupporting the clinical benefit of aggressive resectionsdoes not exist and likely never will Instead the closestthing to such evidence in malignant glioma comes fromthe randomized phase III trial comparing surgical resec-tions with or without the use of 5-aminolevulinic acid(5-ALA) The use of 5-ALA serving as a means to and aproxy for greater EOR resulted in extended overall sur-vival for patients with newly diagnosed glioblastoma19 Arecent meta-analysis of 41 117 unique patients by Brownet al adherent to the guidelines of PRISMA (PreferredReporting Items for Systematic Reviews and Meta-Analyses) also demonstrated a clear survival benefit forgross total resection over subtotal resection or biopsy atupfront surgery for glioblastoma1 The body of literatureas a whole clearly favored aggressive resections andthere seemed to be little disagreement for a strategytoward maximal resection when clinically feasibleHowever the challenge still remains when such strategiescome at the risk of neurological morbidity A recent reportby Rahman et al illustrates that the survival benefits fromaggressive resection are lost if the patient develops anew postoperative neurologic deficit as a result15
All the while our understanding of glioma genetics mo-lecular biology and mechanisms of resistance has con-tinued to deepen and evolve borne of thoughtful andsystematic studies using patient-acquired tumor sam-ples Molecular profiles and tumor genetics have proventhemselves to be the best predictors of clinical behaviorand now represent crucial components of the diagnostic
classification scheme of infiltrating gliomas12 With tumortissue at the molecular and genetic level being able to ro-bustly predict patient outcomes accurate tissue diagno-sis has become paramount in the management ofgliomas The role and value of open surgical resection to-ward this end have become clearer as concerns of sam-pling error with biopsy alone led to a number of studiesevaluating the ldquoaccuracyrdquo of stereotactic biopsy proce-dures Jackson et al reported a series of 81 patients whounderwent stereotactic biopsy followed by open surgicalresection The tissue diagnosis was concordant betweenbiopsy and open resection samples in only 51 ofpatients6 Other studies have also demonstrated diagnos-tic concordance between stereotactic biopsy and surgi-cal resection samples in only 57 to 79 ofcases131428 The major limitation of stereotactic biopsyfor infiltrating gliomas likely stems from the significantintratumoral heterogeneity and collectively these studieshighlight the value of open surgical resection in providinga more global representation and understanding of thetumor tissue
The value of extensive resection is perhaps even moreprofound when considering the therapeutic implicationsof such heterogeneity Multiple-site and serial-samplinganalyses have revealed a high degree of both spatial andtemporal heterogeneity within these tumors a conse-quence of serial evolutionary events during tumor growthand progression23 These studies have also led to theconcept of therapy-driven clonal selection and preferen-tial regrowth of resistant cell populations as a potentialmechanism of treatment failure Efforts to expand our un-derstanding of the tremendously complex network ofmutations and biological consequences of chronologicalhierarchy would be greatly facilitated by carefullyplanned thoughtful acquisition of tumor samples duringsurgery
Despite the recent paradigm shift in glioma diagnosticclassification little gains have been made in improvingthe overall prognosis for patients with malignant gliomassince the introduction of concurrent and adjuvant temo-zolomide in 200521 The strategies more recently tested inlarge randomized phase III trials by and large have yieldeddisappointing results while the reasons and mechanismsof treatment failures remain unclear Even so encourag-ing responses have occasionally been seen in varioussubsets of patients and studies exploring the presenceof potential biomarkers have generated intriguing andpromising results in these populations The developmentof the antindashvascular endothelial growth factor monoclonalantibody bevacizumab is one such example Two initialphase II trials showed prolonged progression-free sur-vival in recurrent glioblastoma relative to historical con-trols prompting the US Food and Drug Administration togrant accelerated approval to bevacizumab for recurrentglioblastoma in 2009825 However 2 large randomized tri-als evaluating the addition of bevacizumab to radiationand temozolomide in the newly diagnosed setting failedto show a benefit in overall survival24 and its utility in the
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
106
recurrent setting is now a topic of debate in light of sub-sequent phase III trial results However a post hoc analy-sis of patients enrolled in the AVAglio trial recentlydemonstrated that bevacizumab improved overall sur-vival for those with a proneural subtype tumor18 Just asO6-methylguanine-DNA-methyltransferase (MGMT) pro-moter methylation does for temozolomide the geneticprofile of the tumor could serve as a potential biomarkerof clinical response for bevacizumab as well and valida-tion studies are currently ongoing Such analyses al-though performed post hoc require targeted prospectivecollection of tumor tissue at initial surgery In addition ge-netic profiling of newly diagnosed malignant gliomas willneed to become routine if this approach is to be utilizedwidely Similarly cilengitide an inhibitor of aVb3 andaVb5 integrins with anti-angiogenic properties showedinitial promise in recurrent glioblastoma studies but failedto show any additional benefit in the newly diagnosedsetting20 A subsequent post hoc analysis of the phase IItrial revealed improved progression-free and overall sur-vival in patients with high aVb3 levels in the tumor cells26
However tumor tissues were not systematically collectedand less than half of the patientsrsquo tumor tissues wereavailable for analysis from the phase III trialUnfortunately this drug will most likely not undergo fur-ther development and one cannot help wonder if the out-come would have been different if the enrollment in thephase III trial had been enriched for or restricted to tumorswith high expression of the aVb3 integrin The only trueldquosuccess storyrdquo since the adaptation of radiation andtemozolomide has come from the novel approach of tu-mor treating fields (TTFields) a transcutaneous deliveryof low-intensity intermediate frequency alternating elec-tric fields The multicenter phase III trial EF-14 random-ized patients with supratentorial glioblastoma withoutevidence of tumor progression following standard che-moradiation to receive maintenance treatment withTTFields plus temozolomide or temozolomide alone22
The study was terminated early based on results of aplanned interim analysis demonstrating benefit inprogression-free survival overall survival a secondaryendpoint was also significantly enhanced at this timeDespite the trialrsquos success TTFields has not been univer-sally adopted by the neuro-oncology community andenthusiasm among clinicians and patients remains low27
Experts have raised concerns regarding the study designsuch as its open-label design lacking a sham-treatmentcontrol arm as well as the generalizability of the resultsbased on the unique randomization point occurring afterconcurrent chemoradiation16 Perhaps most significantlya lack of widely understood mechanism of action hasalso been raised as a factor with comparison to othertreatments the preclinical data for TTFields is relativelylacking particularly when applied in conjunction with che-moradiation27 Even during the early phase stages theuse of robust tissue-based analyses exploring the mech-anism of action such as dose response modeling andmultisite tissue biopsies may have mitigated some of
these concerns and led to wider acceptance by the com-munity Bevacizumab and cilengitide clearly benefitedfrom retrospective analyses of human tumor tissue toidentify susceptible treatment populations while the en-thusiasm for TTFields is perhaps in part tempered by thelack thereof Collectively the evolution of these treat-ments underscores the value of extensive targeted tissuesampling in furthering development of new adjunctivetherapies
Open surgical resection of tumors with such targeted tis-sue acquisition for analysis will continue to play a key rolein prospective clinical trial designs Comparison ofpretreatment and posttreatment tissue profiles representsa valuable line of investigation by delving into mecha-nisms of therapeutic action as well as mechanisms oftreatment failures1011 It also provides an opportunity toinvestigate a number of key fundamental steps along anagentrsquos path to clinical success such as does the agentsuccessfully traffic to the tumor if so how much anddoes the agent then actually have its hypothesizedeffects at the biochemical or cellular level Thusearly-phase trials can and should include posttreatmentmolecular endpoints when possible in addition to safetyendpoints Immunotherapy and immune checkpoint inhi-bition represent exciting novel therapeutic approachesfor neuro-oncology particularly based on their success inmetastatic cancers Large phase III trials studying block-ade of the programmed cell death protein (PD)1PDligand 1 axis with monoclonal antibodies for newlydiagnosed and recurrent glioblastoma are under way butinitial reports have been concerning for negative resultsAs in the development of many previous novel agentstissue-based mechanism studies have been largely lack-ing in the preclinical phases However an Alliance-supported trial currently enrolling focuses on a biomarkeras a primary endpoint patients with recurrent glioblas-toma indicated for surgery are randomized to receivepembrolizumab a PD1 inhibitor either before or aftersurgery (NCT02852655) The resected tumor tissue willthen be analyzed for the profile of tumor-infiltratingT cells and comparison will be made between the 2groups This study represents a tremendously valuableopportunity to explore the impact and the potential chal-lenges of checkpoint inhibition for malignant gliomas inthe clinical setting and should the large phase III trialsend up negative this pilot study will be very informative
Advances in imaging biomarkers and molecular charac-terization of gliomas in conjunction with new targetedtherapies will continue to improve and transform themanagement of these tumors Multimodality imaging cannow more accurately reflect ongoing biological processeswithin these tumors such as the presence of oncogenicmutations or cells undergoing malignant transformationNovel biomarkers such as circulating tumor DNA showpromise in detecting early recurrence or monitoring treat-ment response3724 Lastly the new classification schemerevolving around molecular characterization will provide a
Volume 2 Issue 3 The Value of Surgical Resection for Malignant Gliomas in the Modern Era
107
necessary corollary to these novel diagnostic tools Itremains indisputable however that clinical validation ofthese novel diagnostic tools will also require systematiccorrelation with human tumor tissue obtained throughsurgery These samples ideally gathered prospectivelywill provide a pivot upon which we can expand our under-standing of the complex network of oncological pro-cesses driving these tumors
Malignant gliomas are incredibly challenging disease en-tities in many ways due to the inter- and intratumoral het-erogeneity that is a hallmark of them Experience to datehints that future successes in malignant gliomas rest inneuro-oncology entering the era of precision medicinewhere validated biomarkers and targeted personalizedtherapies are seamlessly integrated into the managementparadigm Accordingly systems supporting surgical re-section and patient-specific tumor tissue analysis mustbe built and organized to guide the decision making fortherapy As our overall approach to the management ofmalignant gliomas evolves so should the framework ofsurgical management The clinical benefits of maximalsafe resection are well founded and well reportedHowever the oncological neurosurgeon must now lookbeyond maximal cytoreduction itself and recognize thevalue of thoughtful acquisition and analysis of tumor tis-sue Modern neurosurgeons must consider themselvessurgical neuro-oncologists and engagement and partici-pation of surgeons into clinical trials particularly early-phase trials should be encouraged and valued In turnwe should provide our surgical trainees with the trainingand tools in neuro-oncology to help them participate andcontribute in multidisciplinary collaborative efforts aimingto advance the understanding of brain tumor biology andultimately improve the outlook of our patients
References
1 Lacroix M Abi-Said D Fourney DR Gokaslan ZL et al A multivariateanalysis of 416 patients with glioblastoma multiforme prognosisextent of resection and survival J Neurosurg 2001 95190ndash198
2 Hervey-Jumper SL Berger MS Maximizing safe resection of low-and high-grade glioma J Neurooncol 2016 130269ndash282
3 Sanai N Polley MY McDermott MW Parsa AT Berger MS An ex-tent of resection threshold for newly diagnosed glioblastomas JNeurosurg 2011 1153ndash8
4 Stummer W Pichlmeier U Meinel T et al Fluorescence-guided sur-gery with 5-aminolevulinic acid for resection of malignant glioma arandomised controlled multicentre phase III trial Lancet Oncol2006 7392ndash401
5 Brown TJ Brennan MC Li M et al Association of the extent ofresection with survival in glioblastoma a systematic review andmeta-analysis JAMA Oncol 2016 21460ndash1469
6 Rahman M Abbatematteo J De Leo EK et al The effects of new orworsened postoperative neurological deficits on survival of patientswith glioblastoma J Neurosurg 2017 127123ndash131
7 Louis DN Perry A Reifenberger G et al The 2016 World HealthOrganization Classification of Tumors of the Central NervousSystem a summary Acta Neuropathol 2016 131803ndash820
8 McGirt MJ Bulsara KR Cummings TJ et al Prognostic value ofmagnetic resonance imaging-guided stereotactic biopsy in the
evaluation of recurrent malignant astrocytoma compared with a le-sion due to radiation effect J Neurosurg 2003 9814ndash20
9 Muragaki Y Chernov M Maruyama T et al Low-grade glioma onstereotactic biopsy how often is the diagnosis accurate MinimInvasive Neurosurg 2008 51275ndash279
10 Woodworth G McGirt MJ Samdani A Garonzik I Olivi AWeingart JD Accuracy of frameless and frame-based image-guided stereotactic brain biopsy in the diagnosis of glioma com-parison of biopsy and open resection specimen Neurol Res 200527358ndash362
11 Suzuki H Aoki K Chiba K et al Mutational landscape and clonal ar-chitecture in grade II and III gliomas Nat Genet 2015 47458ndash468
12 Stupp R Mason WP van den Bent MJ et al Radiotherapy plus con-comitant and adjuvant temozolomide for glioblastoma N Engl JMed 2005 352987ndash996
13 Kreisl TN Kim L Moore K et al Phase II trial of single-agent bevaci-zumab followed by bevacizumab plus irinotecan at tumor progres-sion in recurrent glioblastoma J Clin Oncol 2009 27740ndash745
14 Vredenburgh JJ Desjardins A Herndon 2nd JE et al Phase II trial ofbevacizumab and irinotecan in recurrent malignant glioma ClinCancer Res 2007 131253ndash1259
15 Chinot OL Wick W Mason W et al Bevacizumab plusradiotherapy-temozolomide for newly diagnosed glioblastomaN Engl J Med 2014 370709ndash722
16 Gilbert MR Dignam JJ Armstrong TS et al A randomized trial ofbevacizumab for newly diagnosed glioblastoma N Engl J Med2014 370699ndash708
17 Sandmann T Bourgon R Garcia J et al Patients with proneural glio-blastoma may derive overall survival benefit from the addition of bev-acizumab to first-line radiotherapy and temozolomide retrospectiveanalysis of the AVAglio trial J Clin Oncol 2015 332735ndash2744
18 Jackson RJ Fuller GN Abi-Said D et al Limitations of stereotacticbiopsy in the initial management of gliomas Neuro Oncol 20013193ndash200
19 Stupp R Hegi ME Gorlia T et al Cilengitide combined with stan-dard treatment for patients with newly diagnosed glioblastoma withmethylated MGMT promoter (CENTRIC EORTC 26071-22072study) a multicentre randomised open-label phase 3 trial LancetOncol 2014 151100ndash1108
20 Weller M Nabors LB Gorlia T et al Cilengitide in newly diagnosedglioblastoma biomarker expression and outcome Oncotarget2016 715018ndash15032
21 Stupp R Taillibert S Kanner AA et al Maintenance therapy withtumor-treating fields plus temozolomide vs temozolomide alone forglioblastoma a randomized clinical trial JAMA 20153142535ndash2543
22 Wick W TTFields where does all the skepticism come from NeuroOncol 2016 18303ndash305
23 Sampson JH Alternating electric fields for the treatment of glioblas-toma JAMA 2015 3142511ndash2513
24 Lang FF Asher A Prospective clinical trials of brain tumor therapy thecritical role of neurosurgeons J Neurooncol 2004 69151ndash167
25 Lang FF Gilbert MR Puduvalli VK et al Toward better early-phasebrain tumor clinical trials a reappraisal of current methods and pro-posals for future strategies Neuro Oncol 2002 4268ndash277
26 Elkhaled A Jalbert L Constantin A et al Characterization of metab-olites in infiltrating gliomas using ex vivo (1)H high-resolution magicangle spinning spectroscopy NMR Biomed 2014 27578ndash593
27 Jalbert LE Neill E Phillips JJ et al Magnetic resonance analysis ofmalignant transformation in recurrent glioma Neuro Oncol 2016181169ndash1179
28 Touat M Duran-Pena A Alentorn A Lacroix L Massard C Idbaih AEmerging circulating biomarkers in glioblastoma promises andchallenges Expert Rev Mol Diagn 2015 151311ndash1323
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
108
Update on RadiationCombinations in theTreatment of Patientswith Malignant BrainTumors FromRadiosensitizers toImmunotherapy
Debra Nana Yeboa MD1
Erik P Sulman MD PhD123
Departments of 1Radiation Oncology2Translational Molecular Pathology and3Genomic Medicine The University of Texas MDAnderson Cancer Center 1515 Holcombe BlvdUnit 97 Houston Texas USA Tel 713-563-2300dnyeboamdandersonorg andepsulmanmdandersonorg
109
AbstractAdvances in radiosensitizers and immunotherapyhave ushered in a new frontier in brain tumortreatment The brain has often been viewed as asanctuary site due to the bloodndashbrain barrier andthus the 2 primary modalities of therapy includedsurgery and radiation therapy (RT) More recentlysystemic therapies have played a greater role aseither combination therapy radiosensitizers or im-munotherapy Two novel radiosensitizers are beingdeveloped for the treatment of brain metastasesRRx-001 for example is a small molecule thataccelerates the NO2 to NO conversion of deoxyhe-moglobin and the agent 2-dexoyglucose (2-DG) is anonmetabolized glucose analogue that interfereswith ATP formation Poly(ADP-ribose) DNA polymer-ase inhibitors are promising due to their distinctradiobiological effects Veliparib and olaparib areamong the most studied with randomized trialsexploring their use in gliomas and brain metastasesImmunotherapy including immune checkpoint inhib-itors may play a role for both primary gliomas andbrain metastases RT has been shown to enhancethe function of cytotoxic T lymphocytes induce infil-tration of cytotoxic T lymphocytes and enhancefunction Trials are presently exploring use of bothprogrammed cell death protein (PD)1 and PD ligand1 blockade in glioblastoma patients with radiationSimilarly several immunotherapies are being investi-gated with either stereotactic radiosurgery or wholebrain radiation therapy for brain metastases In thisreview the use of radiosensitizers and immunother-apy agents with RT will be discussed broadly
Keywords brain metastases brain tumors gliomasimmunotherapy radiation therapy radiosensitizers
Radiosensitizers andImmunotherapy inBrain TumorsAdvances in radiosensitizers and immunotherapy haveushered in a new frontier to brain tumor treatment Braintumors however are a diverse class sharing only similaranatomic location Both primary brain malignancies andbrain metastasis have widely diverse histologies and mo-lecular phenotypes With the bloodndashbrain barrier thebrain has often been viewed as a sanctuary site and thusthe 2 primary modalities of therapy included surgery andradiation with decreased benefit from systemic agentsdue to lack of brain penetration However more recentlysystemic therapies have played a greater role as eithercombination therapy radiosensitizers or immunother-apy While temozolomide (TMZ) has played a pivotal rolefor glioblastoma (GBM) only a subset of patients benefitfrom the treatment1 The use of alternative systemicagents that may potentiate the effects of radiation ther-apy (RT) is becoming increasingly appealing Similarly forbrain metastases a variety of systemic agents are beingexplored primarily based on histology and immune pro-file In this review the use of radiosensitizers and immu-notherapy agents currently under investigation with RTwill be discussed
RadiosensitizersThe guiding concept of radiation sensitization is to in-crease the biologic effect of radiation such as increasedDNA damage decreased DNA repair decreased hypoxiaor increased G2M cell cycle blockade leading to im-proved tumor control and increased patient survival2
Poly(adenosine diphosphate-ribose) DNA polymerase(PARP) inhibitors are promising radiosensitizers due totheir roles in DNA repair3 PARP inhibitors work againstPARP1 a nuclear enzyme involved in the recruitment ofrepair proteins used in base excision repair and single-strand break repair PARP1 may also play a role in nonho-mologous end-joining4 The primary investigation ofPARP inhibitors has been in potentiating radiation andchemotherapy effects the latter in the context of homolo-gous repair deficient tumors For radiation the primarymechanism of action is inducing damage to nucleotidesleading to single-strand and double-strand breaks ThusPARP inhibitors in combination with radiation have an ap-pealing mechanism to inhibit or delay DNA repair andlikely convert more single-strand breaks to double-strandbreaks4
While several PARP inhibitors are currently being evalu-ated in a variety of tumors including talazoparib and nira-parib veliparib and olaparib are among the most studiedand there are randomized trials exploring their use in
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
110
gliomas The US National Cancer Institute (NCI)ndashfundedAlliance for Clinical Trials in Oncology (Alliance) A071102is a randomized phase IIIII trial evaluating the use ofveliparib in combination with TMZ in the adjuvant settingin patients with GBM tumors exhibiting hypermethylationof the O6 methylguanine DNA methyltransferase (MGMT)gene promoter Preclinical data supporting this trial sug-gested that only patients with MGMT methylated tumorswould benefit from the combination a group of patientsfor whom TMZ concurrent with radiation might be mostbeneficial5 A phase I trial performed by the NCI-fundedAmerican Brain Tumor Consortium attempted to combineveliparib with radiation and TMZ but failed to identify asuitable recommended phase II dose due to significanthemotoxicity6 Thus attempts to combine radiation withveliparib have focused on patients least likely to benefitfrom TMZ namely with MGMT unmethylated tumors forwhom TMZ could be withheld The Australian VeliparibRT and TMZ trial in newly diagnosed unmethylatedMGMT glioblastoma (VERTU) is a single-arm study inwhich patients receive RT with veliparib followed by adju-vant TMZ and veliparib4
An ongoing novel approach to radiosensitize gliomasinvolves a combination with an agent that interferes withan essential metabolic process 2-Dexoyglucose (2-DG)is a nonmetabolized glucose analogue that acts as acompetitive inhibitor of glycolysis It is transported acrossthe bloodndashbrain barrier by the glucose transporter GLUT-1 and thus has good penetration into the CNSIntracellularly it is trapped and accumulates in cells simi-lar to the mechanism of 18-fluorodeoxyglucose 2-DG isphosphorylated by glycolytic enzymes and the
phosphorylated 2-DG (2-deoxyglucose-P) is trapped in-tracellularly Inhibition of hexokinase activity by 2-DGinterferes with ATP formation and results in tumor celldeath7 While it has positive attributes by selectively tar-geting metabolically active tumor cells 2-DG has alsobeen associated with Q-T prolongation The currentphase III trial in gliomas is assessing the toxicity and tol-erability of 2-DG with hypofractionated radiation of 5 Gyas a radiosensitizer7
Two novel radiosensitizers are being developed for thetreatment of brain metastases First RRx-001 is a smallmolecule initially designed by the aerospace industry Itworks in part as a radiosensitizer by increasing blood flowand thus oxygenation of tumors through nitric oxideRRx-001 which binds to hemoglobin accelerates theNO2 to NO conversion of deoxyhemoglobin It workslocally under hypoxic conditions and subsequentlythe radiosensitive effects through nitric oxide are invasodilation and inhibiting DNA repair enzymes8 Nitricoxide is relatively benign The higher levels of oxidativestress with H2O2 and superoxide in tumors in comparisonto normal tissues result in the preferential generation ofreactive peroxynitrite in the presence of higher nitric oxidelevels7 This accounts for the increased specificity anddecreased toxicity with RRx-001 The dose limiting toxic-ity in a phase I trial of 25 patients treated with eitherweekly or biweekly infusions was infusional pain relatedto the release of NO at the site of injection7 Outside ofpreclinical models 2 clinical reports examining wholebrain radiation therapy (WBRT) with RRx-001 reported anintracranial response A patient with melanoma and 2hemorrhagic edematous lesions of 26 cm and 33 cm
Table 1 Clinical trials involving immunotherapy and radiation therapy1213
Clinical Trials Number Phase Disease Type Treatment Groups
NCT02667587 II Newly diagnosed GBMMGMT-methylated
Nivolumabthorn TMZthorn RT vs placebothornTMZ thorn RT
NCT02617589 III Newly diagnosed GBM Nivolumabthorn RT vs TMZthorn RTNCT02336165 II Newly diagnosed unmethylated
MGMT recurrent glioblastomaMEDI4736thorn standard RT vs MEDI4736 thorn
bevacizumabNCT02530502 III Newly diagnosed GBM RTthorn TMZthorn pembrolizumab TMZthorn
pembrolizumabNCT02313272 I Recurrent glioma Hypofractionated stereotactic radiationthorn
pembrolizumab thorn bevacizumabNCT02696993 III Brain metastases Nivolumabthorn SRS nivolumabthornWBRT
nivolumabthorn ipilimumab thorn SRS nivolu-mabthorn ipilimumab thornWBRT
NCT02115139 II Melanoma brain metastases Ipilimumab thornWBRTNCT02097732 II Melanoma brain metastases Ipilimumab SRS ipilimumab vs SRS
ipilimumabNCT01703507 I Melanoma brain metastases Ipilimumab thornWBRT vs ipilimumab thorn SRSNCT02107755 II Melanoma brain metastases Ipilimumab thorn SRSNCT02858869 pilot Melanoma and NSCLC Pembrolizumabthorn SRSNCT01950195 I Melanoma brain metastases Ipilimumab thorn SRSNCT02662725 II Melanoma brain metastases Ipilimumab thorn SRS
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
111
after a single intravenous dose of RRx-001 of 5 mgm2 4days before WBRT resulted in symptomatic improvementwithin 48 hours By 4 months after radiation there was areduction in size in the largest dimension down to 10 cmand 23 cm of the respective lesions A second report of amelanoma patient with at least 18 lesions after receivingRRx-001 of 5 mgm2 4 days before WBRT as well astwice weekly doses during the 2 weeks of radiation alsoshowed response The patient at 4 months had disap-pearance of 13 of 18 lesions with shrinkage of theremaining 5 lesions8 Presently BRAINSTORM is a phaseIII dose escalation trial of RRx-001 designed to be ad-ministered twice weekly for 2 weeks with WBRT (30 Gy in10 fractions) with the option for weekly maintenance8
Veliparib has also been evaluated in the setting of brainmetastases It was tested in a global randomized con-trolled trial with WBRT Veliparib is orally bioavailable andcrosses the bloodndashbrain barrier It was first examined in amultihistology phase I trial in patients with nonndashsmall celllung cancer (NSCLC) breast cancer melanoma and re-nal and colorectal cancers among others The study of81 patients tested dose tolerance of veliparib from 10 to300 mg orally twice a day with WBRT to 30 Gy in 10 frac-tions or 375 Gy in 15 fractions9 The phase I trial dose es-calation portion did not reach the predefined criteria forthe maximum tolerated dose but there was amplificationof the adverse effects of nausea and vomiting among thehighest dose cohort of 300 mg bid9 The adverse eventprofile at 200 mg bid was similar to that of WBRT aloneDoses of veliparib from 20 to 200 mg bid demonstratesimilar antitumor activity and other studies in preclinicalmodels found that 50 mg daily demonstrated significantreduction in poly(ADP-ribose) in peripheral blood mono-nuclear cells and tumor tissue while also effectivelycrossing the bloodndashbrain barrier Thus the subsequentphase II trial examined 50 mg with WBRT9 In order to as-sess a more homogeneous cohort the phase III globalrandomized trial studied only NSCLC at the 2 doses of50 mg and 200 mg twice daily versus placebo twice a daywith WBRT10 The primary endpoint was overall survivalIn 307 patients in a 111 randomization of 50 mg bid200 mg bid or placebo twice daily the study found nosignificant differences in overall survival among the differ-ent groups10 The majority of patients across the treat-ment groups had a graded prognostic assessment (GPA)score of25 and a Karnofsky performance status ofgt80 The median overall survival was 185 days forpatients receiving placebo and 209 days for those receiv-ing veliparib without any statistically significant differ-ence These results were similar to the disease-specificestimate of median survival for the disease-specific GPAof NSCLC patients with brain metastases10
Several other radiosensitizers have failed to improve overradiation alone in a number of trials These have includedtrials with WBRT including motexafin gadolinium efap-roxyn bortozemib thalidomide teniposide topotecanpaclitaxel and cisplatin7 Of note other PARP inhibitorsalso being assessed include talazoparib and niraparib4
which may yield positive results The use of valproic acid(VPA) as a histone deacetylase inhibitor has also beenconsidered to have radiosensitizing potential in additionto its anti-epileptic drug properties11 While studies havereported that patients with GBM receiving an anti-epilep-tic agent may have higher overall survival than those re-ceiving standard chemoradiation therapy alone thebenefit remains controversial Retrospective analysissuggested that patients taking VPA specifically had bettersurvival in comparison to other anti-epileptic drugs Alsoa recent prospective phase II trial was performed in 37patients with GBM receiving VPA 25 mgkg concurrentlywith TMZ chemoradiation and reported a median survivalof 296 months While controversial further data andinvestigation are needed into this and other agents thatmay potentiate RT
Immunotherapy and radiationImmune checkpoint inhibitors lead to activation of T cellswhich may traffic across the bloodndashbrain barrier to inter-act with tumor Primary brain tumors may evade the im-mune system through upregulation of immunecheckpoints and possible immunosuppression12
Monoclonal antibodies promote immune-mediated anti-tumor activity by inhibiting the immune functionndashmediated cytotoxic T-lymphocyte associated protein 4(CTLA-4) and programmed cell death protein 1 (PD-1)receptors PD protein ligand (PD-L1) is upregulated inGBM through oncogenic signaling possibly throughphosphatase and tensin homolog loss and interleukin-10signaling1314 RT has also been shown to enhance thefunction of cytotoxic T lymphocytes RT may induce aninfiltration of cytotoxic T lymphocytes and enhance theirfunction It may also induce antindashCTLA-4 agents inhibitingT-cell function and increasing the CD8thorn T cellregulatoryT cell ratio in cases of melanoma15 Thus PD-1 and PD-L1 blockers may have a further role in CNS managementwith the use of radiation
In preclinical models radiation has been examined withimmunotherapy that included among other mechanismsvaccination PD-1 blockade and CTLA-4 blockade Inmice radiation plus a vaccination of irradiated gliomacells was associated with increased survival of 40 to80 compared with 0 to 10 for other groups stud-ied16 A benefit of PD-1 blockade with stereotactic radio-surgery (SRS) specifically has also been shown in amouse model In comparison to mice treated with radia-tion antindashPD-1 therapy or a combination only those re-ceiving combination therapy had a higher percentagesurvival alive beyond 180 days after treatment17 Othermouse carcinoma models have identified response withanti-CTLA antibody and fractionated radiation therapy18
CD137 activation CTLA-4 blockade and focal radiationtherapy have been examined in an immunocompetent in-tracranial GBM model Mice treated with triple combina-tion therapy had 50 greater survival19 In other murine
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
112
models the use of antindashPD-1 and antindashCTLA-4 agentsshowed improved survival and increased tumor infiltratingleukocyte populations compared with single modalitywith concurrent radiation16 There are conflicting data re-garding timing or sequencing of therapy with some ani-mal models showing no difference in tumor response inrelation to timing of RT and delivery of immunotherapy18
For instance in one animal model CTLA-4 blockade de-livered simultaneously with radiation or delivered a coupleof days after showed no difference in survival among themice19
Increased PD-1 expression in circulating monocytes hasbeen identified as a biomarker for tumor-induced immu-nosuppression and may serve as a prognostic factor forpotentially worse survival outcomes in clinic13 In onestudy GBM patients with lower PD-L1 expression hadhigher median overall survival than those with higher PD-L1 expression suggesting that lower expression may beassociated with less immunosuppression and more im-mune activity against the tumor glioma20 RT with immunecheckpoint blockade is being investigated to assess if theaddition of PD-1 and PD-L1 inhibitors may improve theoutcomes or toxicity profile of standard therapy For in-stance a multi-institutional trial opened as a phase III willevaluate outcomes in GBM receiving radiation and pem-brolizumab with TMZ (NCT02530502) Next durvalumabor MEDI4736 a PD-L1 inhibitor is being examined forunmethylated MGMT GBMs with standard radiotherapy(NCT02336165)12 The impact of checkpoint inhibitorsduring adjuvant treatment of GBM is currently beingevaluated in the NCI-funded NRG-BN002 trial(NCT02311920) which will evaluate the antindashCTLA-4antibody ipilimumab alone or in combination with theantindashPD-1 antibody nivolumab for patients with newlydiagnosed GBM
Brain metastases have clonal populations of cells differ-ent from the rest of the brain and a unique microenviron-ment that may influence immunotherapy There may bemore immune infiltrates in metastases than in primarybrain tumors21 PD-L1 expression in brain metastasesvaries by histology In a series evaluating PD-L1 expres-sion in various tumors including melanoma NSCLCbreast renal colorectal and small cell less than 10showed significant expression22 There was greatest ex-pression among NSCLC and melanoma with a correla-tion between PD-L1 expression and tumor infiltratinglymphocytes22 Institutional series have examined thecombination of radiation and immune checkpoint block-ade In another study specific to melanoma brain metas-tases PD-L1 expression was found in over 50 of thecases and among those cases over 40 expressedPD-L1 in more than 5 of tumor cells23 The largest bodyof data for use of PD-L1 with radiation is for melanomaand NSCLC
Ipilimumab is a human monoclonal antibody that blocksCTLA-4 and allows for T-cell activation and proliferationto enhance the immune response to cancer In a
retrospective review of 70 patients with brain metastasestreated with SRS or WBRT the 33 patients receiving im-munotherapy had a median survival of 183 months incomparison to the 37 patients who did not receive ipili-mumab with a median survival of 53 months While therewere limited data among the cohort to evaluate sequenc-ing of therapy among 10 evaluable patients 40 whoreceived ipilimumab prior to RT had a partial response incomparison to only 10 among the cohort of 22 evalu-able patients who did not receive ipilimumab therapy atall with radiation24 Another retrospective institutionalstudy of 77 patients in which 37 received ipilimumabfound that patients treated with SRS and ipilimumab hada median survival of 213 months versus 49 months forthose not receiving ipilimumab Most interestingly theyidentified that the correlation remained significant evenafter adjusting for additional factors such as performancestatus Secondly there was not an increased need for useof salvage WBRT25
The sequencing of radiotherapy and immune checkpointinhibitors is of interest In a study of patients with brainmetastases the one-year survival for patients receivingSRS before ipilimumab was greater at 65 in contrast to56 for those receiving it concurrently and 40 for thosereceiving it after SRS26 Similarly another study of 75patients with 566 brain metastases showed greater tu-mor lesion response at 6 months from SRS for patientsreceiving ipilimumab nivolumab or pembrolizumabwithin 4 weeks of their SRS27 Those receiving concurrenttherapy had by 6 months a decrease of 949 in compar-ison to 662 for those not receiving checkpoint inhibi-tors within 4 weeks Prospective clinical trials areinvestigating different combinations of RT with immunecheckpoint blockers in this setting For instance new tri-als are currently evaluating intracranial tumor control at 6months and the timing of immune therapy or immunecheckpoint inhibitors in relation to SRS28
Vaccines are also being developed for primary braintumors showing some evidence for their use Vaccinesdeveloped from dendritic cells and tumor lysate with tu-mor antigens such as the epidermal growth factor recep-tor variant III vaccine have shown promise29 Forinstance in a placebo controlled phase II trial of ICT-107a vaccine composed on autologous dendritic cells andtumor antigens progression-free survival was increasedby 2 months for those receiving the vaccine30 Radiationmay assist in serving as a primer for the immunogeniceffects by facilitating tumor antigen uptake by dendriticcells and cross presentation on major histocompatibilitycomplex I Thus RT may assist in the tumor-specific cy-totoxic T lymphocytes associated with the immunemechanism
In conclusion although there may be challenges to com-bining and sequencing brain tumors radiosensitizersand immunotherapy the opportunities and potential fornovel applications are promising For brain tumors brainmetastases are typically underrepresented in trials
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
113
despite being among the most common intracraniallesions Despite their large population patients with brainmetastases are often excluded from clinical trials withnovel agents due to concerns regarding confounding out-comes and tolerability12 Primary gliomas also offer anovel frontier for the use of immunotherapy to standardadjuvant chemotherapy and radiation particularly forpatients with GBM less likely to respond to TMZ such aswith unmethylated MGMT As studies work to define therole of RT and radiosensitizers and immunotherapy fur-ther analysis is needed to assess the timing of RT andthese treatments
References
1 Stupp R Hegi ME Mason WP et al Effects of radiotherapy withconcomitant and adjuvant temozolomide versus radiotherapy aloneon survival in glioblastoma in a randomised phase III study 5-yearanalysis of the EORTC-NCIC trial Lancet Oncol 2009 10459ndash466
2 Lawrence TS Blackstock AW McGinn C The mechanism of actionof radiosensitization of conventional chemotherapeutic agentsSemin Radiat Oncol 2003 1313ndash21
3 Lesueur P Chevalier F Austry JB et al Poly-(ADP-ribose)-polymer-ase inhibitors as radiosensitizers a systematic review of pre-clinicaland clinical human studies Oncotarget 2017 8(40)69105ndash69124
4 Lester A Rapkins R Nixdorf S Khasraw M McDonald KCombining PARP inhibitors with radiation therapy for the treatmentof glioblastoma is PTEN predictive of response Clin Transl Oncol2017 19273ndash278
5 Gupta SK Kizilbash SH Carlson BL et al Delineation of MGMT hyper-methylation as a biomarker for veliparib-mediated temozolomide-sensi-tizing therapy of glioblastoma J Natl Cancer Inst 2016 108
6 Kleinberg LR Blakeley J Mikkelsen T et al An American BrainTumor Consortium (ABTC) phase 1 trial of veliparib (ABT-888)temozolomide (TMZ) and concurrent radiation therapy (RT) fornewly diagnosed glioblastoma multiforme (GBM) need for modifica-tion to approach for combining these therapies InternationalJ Radiat Oncol Biol Phys 2012 84S7ndashS8
7 Oronsky BT A Review of two promising radiosensitizers in brainmetastases Rrx-001 and 2-deoxyglucose In NC Oronsky edJ Cancer Sci Ther 2015 pp 137ndash141
8 Kim MM Parmar H Cao Y et al Concurrent whole brain radiother-apy and RRx-001 for melanoma brain metastases Neuro Onc2016 18455ndash456
9 Mehta MP Wang D Wang F et al Veliparib in combination withwhole brain radiation therapy in patients with brain metastasesresults of a phase 1 study J Neurooncol 2015 122409ndash417
10 Chabot P Hsia TC Ryu JS et al Veliparib in combination withwhole-brain radiation therapy for patients with brain metastasesfrom non-small cell lung cancer results of a randomized globalplacebo-controlled study J Neurooncol 2017 131105ndash115
11 Ochiai S Nomoto Y Yamashita Y et al Roles of valproic acid inimproving radiation therapy for glioblastoma a review of literaturefocusing on clinical evidence Asian Pac J Cancer Prev 201617463ndash466
12 Tan AC Heimberger AB Menzies AM Pavlakis N Khasraw MImmune checkpoint inhibitors for brain metastases Curr Oncol Rep2017 1938
13 DrsquoSouza NM Fang P Logan J Yang J Jiang W Li JCombining radiation therapy with immune checkpoint blockade
for central nervous system malignancies Frontiers Oncol 20166212
14 Parsa AT Waldron JS Panner A et al Loss of tumor suppressorPTEN function increases B7-H1 expression and immunoresistancein glioma Nat Med 2007 1384ndash88
15 Binder DC Davis AA Wainwright DA Immunotherapy for cancer inthe central nervous system current and future directionsOncoimmunology 2016 5e1082027
16 Newcomb EW Demaria S Lukyanov Y et al The combination ofionizing radiation and peripheral vaccination produces long-termsurvival of mice bearing established invasive GL261 gliomas ClinCancer Res 2006 124730ndash4737
17 Zeng J See AP Phallen J et al Anti-PD-1 blockade and stereotac-tic radiation produce long-term survival in mice with intracranial glio-mas Int J Radiat Oncol Biol Phys 2013 86343ndash349
18 Chow KK Hara W Lim M Li G Combining immunotherapy withradiation for the treatment of glioblastoma J Neurooncol2015123459ndash464
19 Belcaid Z Phallen JA Zeng J et al Focal radiation therapy com-bined with 4-1BB activation and CTLA-4 blockade yields long-termsurvival and a protective antigen-specific memory response in amurine glioma model PLoS One 2014 9e101764
20 Topalian SL Hodi FS Brahmer JR et al Safety activity and im-mune correlates of anti-PD-1 antibody in cancer N Engl J Med2012 3662443ndash2454
21 Bienkowski M Preusser M Prognostic role of tumour-infiltrating in-flammatory cells in brain tumours literature review Curr OpinNeurol 2015 28647ndash658
22 Harter PN Bernatz S Scholz A et al Distribution and prognostic rel-evance of tumor-infiltrating lymphocytes (TILs) and PD-1PD-L1 im-mune checkpoints in human brain metastases Oncotarget 2015640836ndash40849
23 Berghoff AS Ricken G Widhalm G et al Tumour-infiltrating lym-phocytes and expression of programmed death ligand 1 (PD-L1) inmelanoma brain metastases Histopathology 2015 66289ndash299
24 Silk AW Bassetti MF West BT Tsien CI Lao CD Ipilimumab and ra-diation therapy for melanoma brain metastases Cancer Med 20132899ndash906
25 Knisely JP Yu JB Flanigan J Sznol M Kluger HM Chiang VLRadiosurgery for melanoma brain metastases in the ipilimumab eraand the possibility of longer survival J Neurosurg 2012117227ndash233
26 Kiess AP Wolchok JD Barker CA et al Stereotactic radiosurgeryfor melanoma brain metastases in patients receiving ipilimumabsafety profile and efficacy of combined treatment Int J Radiat OncolBiol Phys 2015 92368ndash375
27 Qian JM Yu JB Kluger HM Chiang VL Timing and type of immunecheckpoint therapy affect the early radiographic response of mela-noma brain metastases to stereotactic radiosurgery Cancer 20161223051ndash3058
28 Silk AW Cao Y Gomez-Hassan D et al A randomized phase IIstudy of ipilimumab induction in patients with melanoma brain me-tastases receiving stereotactic radiosurgery J Clin Oncol 2015 33TPS9079ndashTPS9079
29 Neagu MR Reardon DA An Update on the role of immunotherapyand vaccine strategies for primary brain tumors Curr TreatOptions Oncol 2015 1654
30 Wen PY Reardon DA Phuphanich S et al A randomized double-blind placebo-controlled phase 2 trial of dendritic cell (DC) vaccina-tion with ICT-107 in newly diagnosed glioblastoma (GBM) patientsJ Clin Oncol 2014 322005ndash2005
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
114
British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

Malignant gliomas are among the most difficult oncologi-cal entities to treat Despite aggressive treatment prog-nosis remains poor and recurrence and treatmentfailures seem inevitable The current standard-of-caretherapy includes maximal safe surgical resection fol-lowed by concurrent and adjuvant chemoradiotherapyHistorically surgical resection has conferred greater sur-vival benefit to these patients than adjuvant therapiespresumably through the cornerstone principle of cytore-duction However the extent of surgical resection is fre-quently limited by nearby eloquent tissue and risks to keyneurological functions In addition the value of such ag-gressive approaches has been questioned in light of thewidespread infiltration of glioma cells Meanwhile our un-derstanding of glioma biology continues to advance rap-idly fueled in large part by the acquisition of tumor tissueduring surgery Thus the exact role and value of surgeryparticularly in comparing the clinical benefits of maximalextent of resection (EOR) with the biomedical benefits oftissue provision has been a topic of great interest anddebate in both the neuro-oncological and neurosurgicalcommunities
EOR patient age tumor histology performance statusand molecular markers have been widely accepted assignificant predictors of patient outcomes in malignantglioma9 In the past 2 decades many large retrospectivecohort studies have demonstrated improvements in sur-vival with increasing EOR5917 Due to ethical considera-tions evidence from a randomized prospective studysupporting the clinical benefit of aggressive resectionsdoes not exist and likely never will Instead the closestthing to such evidence in malignant glioma comes fromthe randomized phase III trial comparing surgical resec-tions with or without the use of 5-aminolevulinic acid(5-ALA) The use of 5-ALA serving as a means to and aproxy for greater EOR resulted in extended overall sur-vival for patients with newly diagnosed glioblastoma19 Arecent meta-analysis of 41 117 unique patients by Brownet al adherent to the guidelines of PRISMA (PreferredReporting Items for Systematic Reviews and Meta-Analyses) also demonstrated a clear survival benefit forgross total resection over subtotal resection or biopsy atupfront surgery for glioblastoma1 The body of literatureas a whole clearly favored aggressive resections andthere seemed to be little disagreement for a strategytoward maximal resection when clinically feasibleHowever the challenge still remains when such strategiescome at the risk of neurological morbidity A recent reportby Rahman et al illustrates that the survival benefits fromaggressive resection are lost if the patient develops anew postoperative neurologic deficit as a result15
All the while our understanding of glioma genetics mo-lecular biology and mechanisms of resistance has con-tinued to deepen and evolve borne of thoughtful andsystematic studies using patient-acquired tumor sam-ples Molecular profiles and tumor genetics have proventhemselves to be the best predictors of clinical behaviorand now represent crucial components of the diagnostic
classification scheme of infiltrating gliomas12 With tumortissue at the molecular and genetic level being able to ro-bustly predict patient outcomes accurate tissue diagno-sis has become paramount in the management ofgliomas The role and value of open surgical resection to-ward this end have become clearer as concerns of sam-pling error with biopsy alone led to a number of studiesevaluating the ldquoaccuracyrdquo of stereotactic biopsy proce-dures Jackson et al reported a series of 81 patients whounderwent stereotactic biopsy followed by open surgicalresection The tissue diagnosis was concordant betweenbiopsy and open resection samples in only 51 ofpatients6 Other studies have also demonstrated diagnos-tic concordance between stereotactic biopsy and surgi-cal resection samples in only 57 to 79 ofcases131428 The major limitation of stereotactic biopsyfor infiltrating gliomas likely stems from the significantintratumoral heterogeneity and collectively these studieshighlight the value of open surgical resection in providinga more global representation and understanding of thetumor tissue
The value of extensive resection is perhaps even moreprofound when considering the therapeutic implicationsof such heterogeneity Multiple-site and serial-samplinganalyses have revealed a high degree of both spatial andtemporal heterogeneity within these tumors a conse-quence of serial evolutionary events during tumor growthand progression23 These studies have also led to theconcept of therapy-driven clonal selection and preferen-tial regrowth of resistant cell populations as a potentialmechanism of treatment failure Efforts to expand our un-derstanding of the tremendously complex network ofmutations and biological consequences of chronologicalhierarchy would be greatly facilitated by carefullyplanned thoughtful acquisition of tumor samples duringsurgery
Despite the recent paradigm shift in glioma diagnosticclassification little gains have been made in improvingthe overall prognosis for patients with malignant gliomassince the introduction of concurrent and adjuvant temo-zolomide in 200521 The strategies more recently tested inlarge randomized phase III trials by and large have yieldeddisappointing results while the reasons and mechanismsof treatment failures remain unclear Even so encourag-ing responses have occasionally been seen in varioussubsets of patients and studies exploring the presenceof potential biomarkers have generated intriguing andpromising results in these populations The developmentof the antindashvascular endothelial growth factor monoclonalantibody bevacizumab is one such example Two initialphase II trials showed prolonged progression-free sur-vival in recurrent glioblastoma relative to historical con-trols prompting the US Food and Drug Administration togrant accelerated approval to bevacizumab for recurrentglioblastoma in 2009825 However 2 large randomized tri-als evaluating the addition of bevacizumab to radiationand temozolomide in the newly diagnosed setting failedto show a benefit in overall survival24 and its utility in the
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
106
recurrent setting is now a topic of debate in light of sub-sequent phase III trial results However a post hoc analy-sis of patients enrolled in the AVAglio trial recentlydemonstrated that bevacizumab improved overall sur-vival for those with a proneural subtype tumor18 Just asO6-methylguanine-DNA-methyltransferase (MGMT) pro-moter methylation does for temozolomide the geneticprofile of the tumor could serve as a potential biomarkerof clinical response for bevacizumab as well and valida-tion studies are currently ongoing Such analyses al-though performed post hoc require targeted prospectivecollection of tumor tissue at initial surgery In addition ge-netic profiling of newly diagnosed malignant gliomas willneed to become routine if this approach is to be utilizedwidely Similarly cilengitide an inhibitor of aVb3 andaVb5 integrins with anti-angiogenic properties showedinitial promise in recurrent glioblastoma studies but failedto show any additional benefit in the newly diagnosedsetting20 A subsequent post hoc analysis of the phase IItrial revealed improved progression-free and overall sur-vival in patients with high aVb3 levels in the tumor cells26
However tumor tissues were not systematically collectedand less than half of the patientsrsquo tumor tissues wereavailable for analysis from the phase III trialUnfortunately this drug will most likely not undergo fur-ther development and one cannot help wonder if the out-come would have been different if the enrollment in thephase III trial had been enriched for or restricted to tumorswith high expression of the aVb3 integrin The only trueldquosuccess storyrdquo since the adaptation of radiation andtemozolomide has come from the novel approach of tu-mor treating fields (TTFields) a transcutaneous deliveryof low-intensity intermediate frequency alternating elec-tric fields The multicenter phase III trial EF-14 random-ized patients with supratentorial glioblastoma withoutevidence of tumor progression following standard che-moradiation to receive maintenance treatment withTTFields plus temozolomide or temozolomide alone22
The study was terminated early based on results of aplanned interim analysis demonstrating benefit inprogression-free survival overall survival a secondaryendpoint was also significantly enhanced at this timeDespite the trialrsquos success TTFields has not been univer-sally adopted by the neuro-oncology community andenthusiasm among clinicians and patients remains low27
Experts have raised concerns regarding the study designsuch as its open-label design lacking a sham-treatmentcontrol arm as well as the generalizability of the resultsbased on the unique randomization point occurring afterconcurrent chemoradiation16 Perhaps most significantlya lack of widely understood mechanism of action hasalso been raised as a factor with comparison to othertreatments the preclinical data for TTFields is relativelylacking particularly when applied in conjunction with che-moradiation27 Even during the early phase stages theuse of robust tissue-based analyses exploring the mech-anism of action such as dose response modeling andmultisite tissue biopsies may have mitigated some of
these concerns and led to wider acceptance by the com-munity Bevacizumab and cilengitide clearly benefitedfrom retrospective analyses of human tumor tissue toidentify susceptible treatment populations while the en-thusiasm for TTFields is perhaps in part tempered by thelack thereof Collectively the evolution of these treat-ments underscores the value of extensive targeted tissuesampling in furthering development of new adjunctivetherapies
Open surgical resection of tumors with such targeted tis-sue acquisition for analysis will continue to play a key rolein prospective clinical trial designs Comparison ofpretreatment and posttreatment tissue profiles representsa valuable line of investigation by delving into mecha-nisms of therapeutic action as well as mechanisms oftreatment failures1011 It also provides an opportunity toinvestigate a number of key fundamental steps along anagentrsquos path to clinical success such as does the agentsuccessfully traffic to the tumor if so how much anddoes the agent then actually have its hypothesizedeffects at the biochemical or cellular level Thusearly-phase trials can and should include posttreatmentmolecular endpoints when possible in addition to safetyendpoints Immunotherapy and immune checkpoint inhi-bition represent exciting novel therapeutic approachesfor neuro-oncology particularly based on their success inmetastatic cancers Large phase III trials studying block-ade of the programmed cell death protein (PD)1PDligand 1 axis with monoclonal antibodies for newlydiagnosed and recurrent glioblastoma are under way butinitial reports have been concerning for negative resultsAs in the development of many previous novel agentstissue-based mechanism studies have been largely lack-ing in the preclinical phases However an Alliance-supported trial currently enrolling focuses on a biomarkeras a primary endpoint patients with recurrent glioblas-toma indicated for surgery are randomized to receivepembrolizumab a PD1 inhibitor either before or aftersurgery (NCT02852655) The resected tumor tissue willthen be analyzed for the profile of tumor-infiltratingT cells and comparison will be made between the 2groups This study represents a tremendously valuableopportunity to explore the impact and the potential chal-lenges of checkpoint inhibition for malignant gliomas inthe clinical setting and should the large phase III trialsend up negative this pilot study will be very informative
Advances in imaging biomarkers and molecular charac-terization of gliomas in conjunction with new targetedtherapies will continue to improve and transform themanagement of these tumors Multimodality imaging cannow more accurately reflect ongoing biological processeswithin these tumors such as the presence of oncogenicmutations or cells undergoing malignant transformationNovel biomarkers such as circulating tumor DNA showpromise in detecting early recurrence or monitoring treat-ment response3724 Lastly the new classification schemerevolving around molecular characterization will provide a
Volume 2 Issue 3 The Value of Surgical Resection for Malignant Gliomas in the Modern Era
107
necessary corollary to these novel diagnostic tools Itremains indisputable however that clinical validation ofthese novel diagnostic tools will also require systematiccorrelation with human tumor tissue obtained throughsurgery These samples ideally gathered prospectivelywill provide a pivot upon which we can expand our under-standing of the complex network of oncological pro-cesses driving these tumors
Malignant gliomas are incredibly challenging disease en-tities in many ways due to the inter- and intratumoral het-erogeneity that is a hallmark of them Experience to datehints that future successes in malignant gliomas rest inneuro-oncology entering the era of precision medicinewhere validated biomarkers and targeted personalizedtherapies are seamlessly integrated into the managementparadigm Accordingly systems supporting surgical re-section and patient-specific tumor tissue analysis mustbe built and organized to guide the decision making fortherapy As our overall approach to the management ofmalignant gliomas evolves so should the framework ofsurgical management The clinical benefits of maximalsafe resection are well founded and well reportedHowever the oncological neurosurgeon must now lookbeyond maximal cytoreduction itself and recognize thevalue of thoughtful acquisition and analysis of tumor tis-sue Modern neurosurgeons must consider themselvessurgical neuro-oncologists and engagement and partici-pation of surgeons into clinical trials particularly early-phase trials should be encouraged and valued In turnwe should provide our surgical trainees with the trainingand tools in neuro-oncology to help them participate andcontribute in multidisciplinary collaborative efforts aimingto advance the understanding of brain tumor biology andultimately improve the outlook of our patients
References
1 Lacroix M Abi-Said D Fourney DR Gokaslan ZL et al A multivariateanalysis of 416 patients with glioblastoma multiforme prognosisextent of resection and survival J Neurosurg 2001 95190ndash198
2 Hervey-Jumper SL Berger MS Maximizing safe resection of low-and high-grade glioma J Neurooncol 2016 130269ndash282
3 Sanai N Polley MY McDermott MW Parsa AT Berger MS An ex-tent of resection threshold for newly diagnosed glioblastomas JNeurosurg 2011 1153ndash8
4 Stummer W Pichlmeier U Meinel T et al Fluorescence-guided sur-gery with 5-aminolevulinic acid for resection of malignant glioma arandomised controlled multicentre phase III trial Lancet Oncol2006 7392ndash401
5 Brown TJ Brennan MC Li M et al Association of the extent ofresection with survival in glioblastoma a systematic review andmeta-analysis JAMA Oncol 2016 21460ndash1469
6 Rahman M Abbatematteo J De Leo EK et al The effects of new orworsened postoperative neurological deficits on survival of patientswith glioblastoma J Neurosurg 2017 127123ndash131
7 Louis DN Perry A Reifenberger G et al The 2016 World HealthOrganization Classification of Tumors of the Central NervousSystem a summary Acta Neuropathol 2016 131803ndash820
8 McGirt MJ Bulsara KR Cummings TJ et al Prognostic value ofmagnetic resonance imaging-guided stereotactic biopsy in the
evaluation of recurrent malignant astrocytoma compared with a le-sion due to radiation effect J Neurosurg 2003 9814ndash20
9 Muragaki Y Chernov M Maruyama T et al Low-grade glioma onstereotactic biopsy how often is the diagnosis accurate MinimInvasive Neurosurg 2008 51275ndash279
10 Woodworth G McGirt MJ Samdani A Garonzik I Olivi AWeingart JD Accuracy of frameless and frame-based image-guided stereotactic brain biopsy in the diagnosis of glioma com-parison of biopsy and open resection specimen Neurol Res 200527358ndash362
11 Suzuki H Aoki K Chiba K et al Mutational landscape and clonal ar-chitecture in grade II and III gliomas Nat Genet 2015 47458ndash468
12 Stupp R Mason WP van den Bent MJ et al Radiotherapy plus con-comitant and adjuvant temozolomide for glioblastoma N Engl JMed 2005 352987ndash996
13 Kreisl TN Kim L Moore K et al Phase II trial of single-agent bevaci-zumab followed by bevacizumab plus irinotecan at tumor progres-sion in recurrent glioblastoma J Clin Oncol 2009 27740ndash745
14 Vredenburgh JJ Desjardins A Herndon 2nd JE et al Phase II trial ofbevacizumab and irinotecan in recurrent malignant glioma ClinCancer Res 2007 131253ndash1259
15 Chinot OL Wick W Mason W et al Bevacizumab plusradiotherapy-temozolomide for newly diagnosed glioblastomaN Engl J Med 2014 370709ndash722
16 Gilbert MR Dignam JJ Armstrong TS et al A randomized trial ofbevacizumab for newly diagnosed glioblastoma N Engl J Med2014 370699ndash708
17 Sandmann T Bourgon R Garcia J et al Patients with proneural glio-blastoma may derive overall survival benefit from the addition of bev-acizumab to first-line radiotherapy and temozolomide retrospectiveanalysis of the AVAglio trial J Clin Oncol 2015 332735ndash2744
18 Jackson RJ Fuller GN Abi-Said D et al Limitations of stereotacticbiopsy in the initial management of gliomas Neuro Oncol 20013193ndash200
19 Stupp R Hegi ME Gorlia T et al Cilengitide combined with stan-dard treatment for patients with newly diagnosed glioblastoma withmethylated MGMT promoter (CENTRIC EORTC 26071-22072study) a multicentre randomised open-label phase 3 trial LancetOncol 2014 151100ndash1108
20 Weller M Nabors LB Gorlia T et al Cilengitide in newly diagnosedglioblastoma biomarker expression and outcome Oncotarget2016 715018ndash15032
21 Stupp R Taillibert S Kanner AA et al Maintenance therapy withtumor-treating fields plus temozolomide vs temozolomide alone forglioblastoma a randomized clinical trial JAMA 20153142535ndash2543
22 Wick W TTFields where does all the skepticism come from NeuroOncol 2016 18303ndash305
23 Sampson JH Alternating electric fields for the treatment of glioblas-toma JAMA 2015 3142511ndash2513
24 Lang FF Asher A Prospective clinical trials of brain tumor therapy thecritical role of neurosurgeons J Neurooncol 2004 69151ndash167
25 Lang FF Gilbert MR Puduvalli VK et al Toward better early-phasebrain tumor clinical trials a reappraisal of current methods and pro-posals for future strategies Neuro Oncol 2002 4268ndash277
26 Elkhaled A Jalbert L Constantin A et al Characterization of metab-olites in infiltrating gliomas using ex vivo (1)H high-resolution magicangle spinning spectroscopy NMR Biomed 2014 27578ndash593
27 Jalbert LE Neill E Phillips JJ et al Magnetic resonance analysis ofmalignant transformation in recurrent glioma Neuro Oncol 2016181169ndash1179
28 Touat M Duran-Pena A Alentorn A Lacroix L Massard C Idbaih AEmerging circulating biomarkers in glioblastoma promises andchallenges Expert Rev Mol Diagn 2015 151311ndash1323
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
108
Update on RadiationCombinations in theTreatment of Patientswith Malignant BrainTumors FromRadiosensitizers toImmunotherapy
Debra Nana Yeboa MD1
Erik P Sulman MD PhD123
Departments of 1Radiation Oncology2Translational Molecular Pathology and3Genomic Medicine The University of Texas MDAnderson Cancer Center 1515 Holcombe BlvdUnit 97 Houston Texas USA Tel 713-563-2300dnyeboamdandersonorg andepsulmanmdandersonorg
109
AbstractAdvances in radiosensitizers and immunotherapyhave ushered in a new frontier in brain tumortreatment The brain has often been viewed as asanctuary site due to the bloodndashbrain barrier andthus the 2 primary modalities of therapy includedsurgery and radiation therapy (RT) More recentlysystemic therapies have played a greater role aseither combination therapy radiosensitizers or im-munotherapy Two novel radiosensitizers are beingdeveloped for the treatment of brain metastasesRRx-001 for example is a small molecule thataccelerates the NO2 to NO conversion of deoxyhe-moglobin and the agent 2-dexoyglucose (2-DG) is anonmetabolized glucose analogue that interfereswith ATP formation Poly(ADP-ribose) DNA polymer-ase inhibitors are promising due to their distinctradiobiological effects Veliparib and olaparib areamong the most studied with randomized trialsexploring their use in gliomas and brain metastasesImmunotherapy including immune checkpoint inhib-itors may play a role for both primary gliomas andbrain metastases RT has been shown to enhancethe function of cytotoxic T lymphocytes induce infil-tration of cytotoxic T lymphocytes and enhancefunction Trials are presently exploring use of bothprogrammed cell death protein (PD)1 and PD ligand1 blockade in glioblastoma patients with radiationSimilarly several immunotherapies are being investi-gated with either stereotactic radiosurgery or wholebrain radiation therapy for brain metastases In thisreview the use of radiosensitizers and immunother-apy agents with RT will be discussed broadly
Keywords brain metastases brain tumors gliomasimmunotherapy radiation therapy radiosensitizers
Radiosensitizers andImmunotherapy inBrain TumorsAdvances in radiosensitizers and immunotherapy haveushered in a new frontier to brain tumor treatment Braintumors however are a diverse class sharing only similaranatomic location Both primary brain malignancies andbrain metastasis have widely diverse histologies and mo-lecular phenotypes With the bloodndashbrain barrier thebrain has often been viewed as a sanctuary site and thusthe 2 primary modalities of therapy included surgery andradiation with decreased benefit from systemic agentsdue to lack of brain penetration However more recentlysystemic therapies have played a greater role as eithercombination therapy radiosensitizers or immunother-apy While temozolomide (TMZ) has played a pivotal rolefor glioblastoma (GBM) only a subset of patients benefitfrom the treatment1 The use of alternative systemicagents that may potentiate the effects of radiation ther-apy (RT) is becoming increasingly appealing Similarly forbrain metastases a variety of systemic agents are beingexplored primarily based on histology and immune pro-file In this review the use of radiosensitizers and immu-notherapy agents currently under investigation with RTwill be discussed
RadiosensitizersThe guiding concept of radiation sensitization is to in-crease the biologic effect of radiation such as increasedDNA damage decreased DNA repair decreased hypoxiaor increased G2M cell cycle blockade leading to im-proved tumor control and increased patient survival2
Poly(adenosine diphosphate-ribose) DNA polymerase(PARP) inhibitors are promising radiosensitizers due totheir roles in DNA repair3 PARP inhibitors work againstPARP1 a nuclear enzyme involved in the recruitment ofrepair proteins used in base excision repair and single-strand break repair PARP1 may also play a role in nonho-mologous end-joining4 The primary investigation ofPARP inhibitors has been in potentiating radiation andchemotherapy effects the latter in the context of homolo-gous repair deficient tumors For radiation the primarymechanism of action is inducing damage to nucleotidesleading to single-strand and double-strand breaks ThusPARP inhibitors in combination with radiation have an ap-pealing mechanism to inhibit or delay DNA repair andlikely convert more single-strand breaks to double-strandbreaks4
While several PARP inhibitors are currently being evalu-ated in a variety of tumors including talazoparib and nira-parib veliparib and olaparib are among the most studiedand there are randomized trials exploring their use in
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
110
gliomas The US National Cancer Institute (NCI)ndashfundedAlliance for Clinical Trials in Oncology (Alliance) A071102is a randomized phase IIIII trial evaluating the use ofveliparib in combination with TMZ in the adjuvant settingin patients with GBM tumors exhibiting hypermethylationof the O6 methylguanine DNA methyltransferase (MGMT)gene promoter Preclinical data supporting this trial sug-gested that only patients with MGMT methylated tumorswould benefit from the combination a group of patientsfor whom TMZ concurrent with radiation might be mostbeneficial5 A phase I trial performed by the NCI-fundedAmerican Brain Tumor Consortium attempted to combineveliparib with radiation and TMZ but failed to identify asuitable recommended phase II dose due to significanthemotoxicity6 Thus attempts to combine radiation withveliparib have focused on patients least likely to benefitfrom TMZ namely with MGMT unmethylated tumors forwhom TMZ could be withheld The Australian VeliparibRT and TMZ trial in newly diagnosed unmethylatedMGMT glioblastoma (VERTU) is a single-arm study inwhich patients receive RT with veliparib followed by adju-vant TMZ and veliparib4
An ongoing novel approach to radiosensitize gliomasinvolves a combination with an agent that interferes withan essential metabolic process 2-Dexoyglucose (2-DG)is a nonmetabolized glucose analogue that acts as acompetitive inhibitor of glycolysis It is transported acrossthe bloodndashbrain barrier by the glucose transporter GLUT-1 and thus has good penetration into the CNSIntracellularly it is trapped and accumulates in cells simi-lar to the mechanism of 18-fluorodeoxyglucose 2-DG isphosphorylated by glycolytic enzymes and the
phosphorylated 2-DG (2-deoxyglucose-P) is trapped in-tracellularly Inhibition of hexokinase activity by 2-DGinterferes with ATP formation and results in tumor celldeath7 While it has positive attributes by selectively tar-geting metabolically active tumor cells 2-DG has alsobeen associated with Q-T prolongation The currentphase III trial in gliomas is assessing the toxicity and tol-erability of 2-DG with hypofractionated radiation of 5 Gyas a radiosensitizer7
Two novel radiosensitizers are being developed for thetreatment of brain metastases First RRx-001 is a smallmolecule initially designed by the aerospace industry Itworks in part as a radiosensitizer by increasing blood flowand thus oxygenation of tumors through nitric oxideRRx-001 which binds to hemoglobin accelerates theNO2 to NO conversion of deoxyhemoglobin It workslocally under hypoxic conditions and subsequentlythe radiosensitive effects through nitric oxide are invasodilation and inhibiting DNA repair enzymes8 Nitricoxide is relatively benign The higher levels of oxidativestress with H2O2 and superoxide in tumors in comparisonto normal tissues result in the preferential generation ofreactive peroxynitrite in the presence of higher nitric oxidelevels7 This accounts for the increased specificity anddecreased toxicity with RRx-001 The dose limiting toxic-ity in a phase I trial of 25 patients treated with eitherweekly or biweekly infusions was infusional pain relatedto the release of NO at the site of injection7 Outside ofpreclinical models 2 clinical reports examining wholebrain radiation therapy (WBRT) with RRx-001 reported anintracranial response A patient with melanoma and 2hemorrhagic edematous lesions of 26 cm and 33 cm
Table 1 Clinical trials involving immunotherapy and radiation therapy1213
Clinical Trials Number Phase Disease Type Treatment Groups
NCT02667587 II Newly diagnosed GBMMGMT-methylated
Nivolumabthorn TMZthorn RT vs placebothornTMZ thorn RT
NCT02617589 III Newly diagnosed GBM Nivolumabthorn RT vs TMZthorn RTNCT02336165 II Newly diagnosed unmethylated
MGMT recurrent glioblastomaMEDI4736thorn standard RT vs MEDI4736 thorn
bevacizumabNCT02530502 III Newly diagnosed GBM RTthorn TMZthorn pembrolizumab TMZthorn
pembrolizumabNCT02313272 I Recurrent glioma Hypofractionated stereotactic radiationthorn
pembrolizumab thorn bevacizumabNCT02696993 III Brain metastases Nivolumabthorn SRS nivolumabthornWBRT
nivolumabthorn ipilimumab thorn SRS nivolu-mabthorn ipilimumab thornWBRT
NCT02115139 II Melanoma brain metastases Ipilimumab thornWBRTNCT02097732 II Melanoma brain metastases Ipilimumab SRS ipilimumab vs SRS
ipilimumabNCT01703507 I Melanoma brain metastases Ipilimumab thornWBRT vs ipilimumab thorn SRSNCT02107755 II Melanoma brain metastases Ipilimumab thorn SRSNCT02858869 pilot Melanoma and NSCLC Pembrolizumabthorn SRSNCT01950195 I Melanoma brain metastases Ipilimumab thorn SRSNCT02662725 II Melanoma brain metastases Ipilimumab thorn SRS
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
111
after a single intravenous dose of RRx-001 of 5 mgm2 4days before WBRT resulted in symptomatic improvementwithin 48 hours By 4 months after radiation there was areduction in size in the largest dimension down to 10 cmand 23 cm of the respective lesions A second report of amelanoma patient with at least 18 lesions after receivingRRx-001 of 5 mgm2 4 days before WBRT as well astwice weekly doses during the 2 weeks of radiation alsoshowed response The patient at 4 months had disap-pearance of 13 of 18 lesions with shrinkage of theremaining 5 lesions8 Presently BRAINSTORM is a phaseIII dose escalation trial of RRx-001 designed to be ad-ministered twice weekly for 2 weeks with WBRT (30 Gy in10 fractions) with the option for weekly maintenance8
Veliparib has also been evaluated in the setting of brainmetastases It was tested in a global randomized con-trolled trial with WBRT Veliparib is orally bioavailable andcrosses the bloodndashbrain barrier It was first examined in amultihistology phase I trial in patients with nonndashsmall celllung cancer (NSCLC) breast cancer melanoma and re-nal and colorectal cancers among others The study of81 patients tested dose tolerance of veliparib from 10 to300 mg orally twice a day with WBRT to 30 Gy in 10 frac-tions or 375 Gy in 15 fractions9 The phase I trial dose es-calation portion did not reach the predefined criteria forthe maximum tolerated dose but there was amplificationof the adverse effects of nausea and vomiting among thehighest dose cohort of 300 mg bid9 The adverse eventprofile at 200 mg bid was similar to that of WBRT aloneDoses of veliparib from 20 to 200 mg bid demonstratesimilar antitumor activity and other studies in preclinicalmodels found that 50 mg daily demonstrated significantreduction in poly(ADP-ribose) in peripheral blood mono-nuclear cells and tumor tissue while also effectivelycrossing the bloodndashbrain barrier Thus the subsequentphase II trial examined 50 mg with WBRT9 In order to as-sess a more homogeneous cohort the phase III globalrandomized trial studied only NSCLC at the 2 doses of50 mg and 200 mg twice daily versus placebo twice a daywith WBRT10 The primary endpoint was overall survivalIn 307 patients in a 111 randomization of 50 mg bid200 mg bid or placebo twice daily the study found nosignificant differences in overall survival among the differ-ent groups10 The majority of patients across the treat-ment groups had a graded prognostic assessment (GPA)score of25 and a Karnofsky performance status ofgt80 The median overall survival was 185 days forpatients receiving placebo and 209 days for those receiv-ing veliparib without any statistically significant differ-ence These results were similar to the disease-specificestimate of median survival for the disease-specific GPAof NSCLC patients with brain metastases10
Several other radiosensitizers have failed to improve overradiation alone in a number of trials These have includedtrials with WBRT including motexafin gadolinium efap-roxyn bortozemib thalidomide teniposide topotecanpaclitaxel and cisplatin7 Of note other PARP inhibitorsalso being assessed include talazoparib and niraparib4
which may yield positive results The use of valproic acid(VPA) as a histone deacetylase inhibitor has also beenconsidered to have radiosensitizing potential in additionto its anti-epileptic drug properties11 While studies havereported that patients with GBM receiving an anti-epilep-tic agent may have higher overall survival than those re-ceiving standard chemoradiation therapy alone thebenefit remains controversial Retrospective analysissuggested that patients taking VPA specifically had bettersurvival in comparison to other anti-epileptic drugs Alsoa recent prospective phase II trial was performed in 37patients with GBM receiving VPA 25 mgkg concurrentlywith TMZ chemoradiation and reported a median survivalof 296 months While controversial further data andinvestigation are needed into this and other agents thatmay potentiate RT
Immunotherapy and radiationImmune checkpoint inhibitors lead to activation of T cellswhich may traffic across the bloodndashbrain barrier to inter-act with tumor Primary brain tumors may evade the im-mune system through upregulation of immunecheckpoints and possible immunosuppression12
Monoclonal antibodies promote immune-mediated anti-tumor activity by inhibiting the immune functionndashmediated cytotoxic T-lymphocyte associated protein 4(CTLA-4) and programmed cell death protein 1 (PD-1)receptors PD protein ligand (PD-L1) is upregulated inGBM through oncogenic signaling possibly throughphosphatase and tensin homolog loss and interleukin-10signaling1314 RT has also been shown to enhance thefunction of cytotoxic T lymphocytes RT may induce aninfiltration of cytotoxic T lymphocytes and enhance theirfunction It may also induce antindashCTLA-4 agents inhibitingT-cell function and increasing the CD8thorn T cellregulatoryT cell ratio in cases of melanoma15 Thus PD-1 and PD-L1 blockers may have a further role in CNS managementwith the use of radiation
In preclinical models radiation has been examined withimmunotherapy that included among other mechanismsvaccination PD-1 blockade and CTLA-4 blockade Inmice radiation plus a vaccination of irradiated gliomacells was associated with increased survival of 40 to80 compared with 0 to 10 for other groups stud-ied16 A benefit of PD-1 blockade with stereotactic radio-surgery (SRS) specifically has also been shown in amouse model In comparison to mice treated with radia-tion antindashPD-1 therapy or a combination only those re-ceiving combination therapy had a higher percentagesurvival alive beyond 180 days after treatment17 Othermouse carcinoma models have identified response withanti-CTLA antibody and fractionated radiation therapy18
CD137 activation CTLA-4 blockade and focal radiationtherapy have been examined in an immunocompetent in-tracranial GBM model Mice treated with triple combina-tion therapy had 50 greater survival19 In other murine
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
112
models the use of antindashPD-1 and antindashCTLA-4 agentsshowed improved survival and increased tumor infiltratingleukocyte populations compared with single modalitywith concurrent radiation16 There are conflicting data re-garding timing or sequencing of therapy with some ani-mal models showing no difference in tumor response inrelation to timing of RT and delivery of immunotherapy18
For instance in one animal model CTLA-4 blockade de-livered simultaneously with radiation or delivered a coupleof days after showed no difference in survival among themice19
Increased PD-1 expression in circulating monocytes hasbeen identified as a biomarker for tumor-induced immu-nosuppression and may serve as a prognostic factor forpotentially worse survival outcomes in clinic13 In onestudy GBM patients with lower PD-L1 expression hadhigher median overall survival than those with higher PD-L1 expression suggesting that lower expression may beassociated with less immunosuppression and more im-mune activity against the tumor glioma20 RT with immunecheckpoint blockade is being investigated to assess if theaddition of PD-1 and PD-L1 inhibitors may improve theoutcomes or toxicity profile of standard therapy For in-stance a multi-institutional trial opened as a phase III willevaluate outcomes in GBM receiving radiation and pem-brolizumab with TMZ (NCT02530502) Next durvalumabor MEDI4736 a PD-L1 inhibitor is being examined forunmethylated MGMT GBMs with standard radiotherapy(NCT02336165)12 The impact of checkpoint inhibitorsduring adjuvant treatment of GBM is currently beingevaluated in the NCI-funded NRG-BN002 trial(NCT02311920) which will evaluate the antindashCTLA-4antibody ipilimumab alone or in combination with theantindashPD-1 antibody nivolumab for patients with newlydiagnosed GBM
Brain metastases have clonal populations of cells differ-ent from the rest of the brain and a unique microenviron-ment that may influence immunotherapy There may bemore immune infiltrates in metastases than in primarybrain tumors21 PD-L1 expression in brain metastasesvaries by histology In a series evaluating PD-L1 expres-sion in various tumors including melanoma NSCLCbreast renal colorectal and small cell less than 10showed significant expression22 There was greatest ex-pression among NSCLC and melanoma with a correla-tion between PD-L1 expression and tumor infiltratinglymphocytes22 Institutional series have examined thecombination of radiation and immune checkpoint block-ade In another study specific to melanoma brain metas-tases PD-L1 expression was found in over 50 of thecases and among those cases over 40 expressedPD-L1 in more than 5 of tumor cells23 The largest bodyof data for use of PD-L1 with radiation is for melanomaand NSCLC
Ipilimumab is a human monoclonal antibody that blocksCTLA-4 and allows for T-cell activation and proliferationto enhance the immune response to cancer In a
retrospective review of 70 patients with brain metastasestreated with SRS or WBRT the 33 patients receiving im-munotherapy had a median survival of 183 months incomparison to the 37 patients who did not receive ipili-mumab with a median survival of 53 months While therewere limited data among the cohort to evaluate sequenc-ing of therapy among 10 evaluable patients 40 whoreceived ipilimumab prior to RT had a partial response incomparison to only 10 among the cohort of 22 evalu-able patients who did not receive ipilimumab therapy atall with radiation24 Another retrospective institutionalstudy of 77 patients in which 37 received ipilimumabfound that patients treated with SRS and ipilimumab hada median survival of 213 months versus 49 months forthose not receiving ipilimumab Most interestingly theyidentified that the correlation remained significant evenafter adjusting for additional factors such as performancestatus Secondly there was not an increased need for useof salvage WBRT25
The sequencing of radiotherapy and immune checkpointinhibitors is of interest In a study of patients with brainmetastases the one-year survival for patients receivingSRS before ipilimumab was greater at 65 in contrast to56 for those receiving it concurrently and 40 for thosereceiving it after SRS26 Similarly another study of 75patients with 566 brain metastases showed greater tu-mor lesion response at 6 months from SRS for patientsreceiving ipilimumab nivolumab or pembrolizumabwithin 4 weeks of their SRS27 Those receiving concurrenttherapy had by 6 months a decrease of 949 in compar-ison to 662 for those not receiving checkpoint inhibi-tors within 4 weeks Prospective clinical trials areinvestigating different combinations of RT with immunecheckpoint blockers in this setting For instance new tri-als are currently evaluating intracranial tumor control at 6months and the timing of immune therapy or immunecheckpoint inhibitors in relation to SRS28
Vaccines are also being developed for primary braintumors showing some evidence for their use Vaccinesdeveloped from dendritic cells and tumor lysate with tu-mor antigens such as the epidermal growth factor recep-tor variant III vaccine have shown promise29 Forinstance in a placebo controlled phase II trial of ICT-107a vaccine composed on autologous dendritic cells andtumor antigens progression-free survival was increasedby 2 months for those receiving the vaccine30 Radiationmay assist in serving as a primer for the immunogeniceffects by facilitating tumor antigen uptake by dendriticcells and cross presentation on major histocompatibilitycomplex I Thus RT may assist in the tumor-specific cy-totoxic T lymphocytes associated with the immunemechanism
In conclusion although there may be challenges to com-bining and sequencing brain tumors radiosensitizersand immunotherapy the opportunities and potential fornovel applications are promising For brain tumors brainmetastases are typically underrepresented in trials
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
113
despite being among the most common intracraniallesions Despite their large population patients with brainmetastases are often excluded from clinical trials withnovel agents due to concerns regarding confounding out-comes and tolerability12 Primary gliomas also offer anovel frontier for the use of immunotherapy to standardadjuvant chemotherapy and radiation particularly forpatients with GBM less likely to respond to TMZ such aswith unmethylated MGMT As studies work to define therole of RT and radiosensitizers and immunotherapy fur-ther analysis is needed to assess the timing of RT andthese treatments
References
1 Stupp R Hegi ME Mason WP et al Effects of radiotherapy withconcomitant and adjuvant temozolomide versus radiotherapy aloneon survival in glioblastoma in a randomised phase III study 5-yearanalysis of the EORTC-NCIC trial Lancet Oncol 2009 10459ndash466
2 Lawrence TS Blackstock AW McGinn C The mechanism of actionof radiosensitization of conventional chemotherapeutic agentsSemin Radiat Oncol 2003 1313ndash21
3 Lesueur P Chevalier F Austry JB et al Poly-(ADP-ribose)-polymer-ase inhibitors as radiosensitizers a systematic review of pre-clinicaland clinical human studies Oncotarget 2017 8(40)69105ndash69124
4 Lester A Rapkins R Nixdorf S Khasraw M McDonald KCombining PARP inhibitors with radiation therapy for the treatmentof glioblastoma is PTEN predictive of response Clin Transl Oncol2017 19273ndash278
5 Gupta SK Kizilbash SH Carlson BL et al Delineation of MGMT hyper-methylation as a biomarker for veliparib-mediated temozolomide-sensi-tizing therapy of glioblastoma J Natl Cancer Inst 2016 108
6 Kleinberg LR Blakeley J Mikkelsen T et al An American BrainTumor Consortium (ABTC) phase 1 trial of veliparib (ABT-888)temozolomide (TMZ) and concurrent radiation therapy (RT) fornewly diagnosed glioblastoma multiforme (GBM) need for modifica-tion to approach for combining these therapies InternationalJ Radiat Oncol Biol Phys 2012 84S7ndashS8
7 Oronsky BT A Review of two promising radiosensitizers in brainmetastases Rrx-001 and 2-deoxyglucose In NC Oronsky edJ Cancer Sci Ther 2015 pp 137ndash141
8 Kim MM Parmar H Cao Y et al Concurrent whole brain radiother-apy and RRx-001 for melanoma brain metastases Neuro Onc2016 18455ndash456
9 Mehta MP Wang D Wang F et al Veliparib in combination withwhole brain radiation therapy in patients with brain metastasesresults of a phase 1 study J Neurooncol 2015 122409ndash417
10 Chabot P Hsia TC Ryu JS et al Veliparib in combination withwhole-brain radiation therapy for patients with brain metastasesfrom non-small cell lung cancer results of a randomized globalplacebo-controlled study J Neurooncol 2017 131105ndash115
11 Ochiai S Nomoto Y Yamashita Y et al Roles of valproic acid inimproving radiation therapy for glioblastoma a review of literaturefocusing on clinical evidence Asian Pac J Cancer Prev 201617463ndash466
12 Tan AC Heimberger AB Menzies AM Pavlakis N Khasraw MImmune checkpoint inhibitors for brain metastases Curr Oncol Rep2017 1938
13 DrsquoSouza NM Fang P Logan J Yang J Jiang W Li JCombining radiation therapy with immune checkpoint blockade
for central nervous system malignancies Frontiers Oncol 20166212
14 Parsa AT Waldron JS Panner A et al Loss of tumor suppressorPTEN function increases B7-H1 expression and immunoresistancein glioma Nat Med 2007 1384ndash88
15 Binder DC Davis AA Wainwright DA Immunotherapy for cancer inthe central nervous system current and future directionsOncoimmunology 2016 5e1082027
16 Newcomb EW Demaria S Lukyanov Y et al The combination ofionizing radiation and peripheral vaccination produces long-termsurvival of mice bearing established invasive GL261 gliomas ClinCancer Res 2006 124730ndash4737
17 Zeng J See AP Phallen J et al Anti-PD-1 blockade and stereotac-tic radiation produce long-term survival in mice with intracranial glio-mas Int J Radiat Oncol Biol Phys 2013 86343ndash349
18 Chow KK Hara W Lim M Li G Combining immunotherapy withradiation for the treatment of glioblastoma J Neurooncol2015123459ndash464
19 Belcaid Z Phallen JA Zeng J et al Focal radiation therapy com-bined with 4-1BB activation and CTLA-4 blockade yields long-termsurvival and a protective antigen-specific memory response in amurine glioma model PLoS One 2014 9e101764
20 Topalian SL Hodi FS Brahmer JR et al Safety activity and im-mune correlates of anti-PD-1 antibody in cancer N Engl J Med2012 3662443ndash2454
21 Bienkowski M Preusser M Prognostic role of tumour-infiltrating in-flammatory cells in brain tumours literature review Curr OpinNeurol 2015 28647ndash658
22 Harter PN Bernatz S Scholz A et al Distribution and prognostic rel-evance of tumor-infiltrating lymphocytes (TILs) and PD-1PD-L1 im-mune checkpoints in human brain metastases Oncotarget 2015640836ndash40849
23 Berghoff AS Ricken G Widhalm G et al Tumour-infiltrating lym-phocytes and expression of programmed death ligand 1 (PD-L1) inmelanoma brain metastases Histopathology 2015 66289ndash299
24 Silk AW Bassetti MF West BT Tsien CI Lao CD Ipilimumab and ra-diation therapy for melanoma brain metastases Cancer Med 20132899ndash906
25 Knisely JP Yu JB Flanigan J Sznol M Kluger HM Chiang VLRadiosurgery for melanoma brain metastases in the ipilimumab eraand the possibility of longer survival J Neurosurg 2012117227ndash233
26 Kiess AP Wolchok JD Barker CA et al Stereotactic radiosurgeryfor melanoma brain metastases in patients receiving ipilimumabsafety profile and efficacy of combined treatment Int J Radiat OncolBiol Phys 2015 92368ndash375
27 Qian JM Yu JB Kluger HM Chiang VL Timing and type of immunecheckpoint therapy affect the early radiographic response of mela-noma brain metastases to stereotactic radiosurgery Cancer 20161223051ndash3058
28 Silk AW Cao Y Gomez-Hassan D et al A randomized phase IIstudy of ipilimumab induction in patients with melanoma brain me-tastases receiving stereotactic radiosurgery J Clin Oncol 2015 33TPS9079ndashTPS9079
29 Neagu MR Reardon DA An Update on the role of immunotherapyand vaccine strategies for primary brain tumors Curr TreatOptions Oncol 2015 1654
30 Wen PY Reardon DA Phuphanich S et al A randomized double-blind placebo-controlled phase 2 trial of dendritic cell (DC) vaccina-tion with ICT-107 in newly diagnosed glioblastoma (GBM) patientsJ Clin Oncol 2014 322005ndash2005
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
114
British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

recurrent setting is now a topic of debate in light of sub-sequent phase III trial results However a post hoc analy-sis of patients enrolled in the AVAglio trial recentlydemonstrated that bevacizumab improved overall sur-vival for those with a proneural subtype tumor18 Just asO6-methylguanine-DNA-methyltransferase (MGMT) pro-moter methylation does for temozolomide the geneticprofile of the tumor could serve as a potential biomarkerof clinical response for bevacizumab as well and valida-tion studies are currently ongoing Such analyses al-though performed post hoc require targeted prospectivecollection of tumor tissue at initial surgery In addition ge-netic profiling of newly diagnosed malignant gliomas willneed to become routine if this approach is to be utilizedwidely Similarly cilengitide an inhibitor of aVb3 andaVb5 integrins with anti-angiogenic properties showedinitial promise in recurrent glioblastoma studies but failedto show any additional benefit in the newly diagnosedsetting20 A subsequent post hoc analysis of the phase IItrial revealed improved progression-free and overall sur-vival in patients with high aVb3 levels in the tumor cells26
However tumor tissues were not systematically collectedand less than half of the patientsrsquo tumor tissues wereavailable for analysis from the phase III trialUnfortunately this drug will most likely not undergo fur-ther development and one cannot help wonder if the out-come would have been different if the enrollment in thephase III trial had been enriched for or restricted to tumorswith high expression of the aVb3 integrin The only trueldquosuccess storyrdquo since the adaptation of radiation andtemozolomide has come from the novel approach of tu-mor treating fields (TTFields) a transcutaneous deliveryof low-intensity intermediate frequency alternating elec-tric fields The multicenter phase III trial EF-14 random-ized patients with supratentorial glioblastoma withoutevidence of tumor progression following standard che-moradiation to receive maintenance treatment withTTFields plus temozolomide or temozolomide alone22
The study was terminated early based on results of aplanned interim analysis demonstrating benefit inprogression-free survival overall survival a secondaryendpoint was also significantly enhanced at this timeDespite the trialrsquos success TTFields has not been univer-sally adopted by the neuro-oncology community andenthusiasm among clinicians and patients remains low27
Experts have raised concerns regarding the study designsuch as its open-label design lacking a sham-treatmentcontrol arm as well as the generalizability of the resultsbased on the unique randomization point occurring afterconcurrent chemoradiation16 Perhaps most significantlya lack of widely understood mechanism of action hasalso been raised as a factor with comparison to othertreatments the preclinical data for TTFields is relativelylacking particularly when applied in conjunction with che-moradiation27 Even during the early phase stages theuse of robust tissue-based analyses exploring the mech-anism of action such as dose response modeling andmultisite tissue biopsies may have mitigated some of
these concerns and led to wider acceptance by the com-munity Bevacizumab and cilengitide clearly benefitedfrom retrospective analyses of human tumor tissue toidentify susceptible treatment populations while the en-thusiasm for TTFields is perhaps in part tempered by thelack thereof Collectively the evolution of these treat-ments underscores the value of extensive targeted tissuesampling in furthering development of new adjunctivetherapies
Open surgical resection of tumors with such targeted tis-sue acquisition for analysis will continue to play a key rolein prospective clinical trial designs Comparison ofpretreatment and posttreatment tissue profiles representsa valuable line of investigation by delving into mecha-nisms of therapeutic action as well as mechanisms oftreatment failures1011 It also provides an opportunity toinvestigate a number of key fundamental steps along anagentrsquos path to clinical success such as does the agentsuccessfully traffic to the tumor if so how much anddoes the agent then actually have its hypothesizedeffects at the biochemical or cellular level Thusearly-phase trials can and should include posttreatmentmolecular endpoints when possible in addition to safetyendpoints Immunotherapy and immune checkpoint inhi-bition represent exciting novel therapeutic approachesfor neuro-oncology particularly based on their success inmetastatic cancers Large phase III trials studying block-ade of the programmed cell death protein (PD)1PDligand 1 axis with monoclonal antibodies for newlydiagnosed and recurrent glioblastoma are under way butinitial reports have been concerning for negative resultsAs in the development of many previous novel agentstissue-based mechanism studies have been largely lack-ing in the preclinical phases However an Alliance-supported trial currently enrolling focuses on a biomarkeras a primary endpoint patients with recurrent glioblas-toma indicated for surgery are randomized to receivepembrolizumab a PD1 inhibitor either before or aftersurgery (NCT02852655) The resected tumor tissue willthen be analyzed for the profile of tumor-infiltratingT cells and comparison will be made between the 2groups This study represents a tremendously valuableopportunity to explore the impact and the potential chal-lenges of checkpoint inhibition for malignant gliomas inthe clinical setting and should the large phase III trialsend up negative this pilot study will be very informative
Advances in imaging biomarkers and molecular charac-terization of gliomas in conjunction with new targetedtherapies will continue to improve and transform themanagement of these tumors Multimodality imaging cannow more accurately reflect ongoing biological processeswithin these tumors such as the presence of oncogenicmutations or cells undergoing malignant transformationNovel biomarkers such as circulating tumor DNA showpromise in detecting early recurrence or monitoring treat-ment response3724 Lastly the new classification schemerevolving around molecular characterization will provide a
Volume 2 Issue 3 The Value of Surgical Resection for Malignant Gliomas in the Modern Era
107
necessary corollary to these novel diagnostic tools Itremains indisputable however that clinical validation ofthese novel diagnostic tools will also require systematiccorrelation with human tumor tissue obtained throughsurgery These samples ideally gathered prospectivelywill provide a pivot upon which we can expand our under-standing of the complex network of oncological pro-cesses driving these tumors
Malignant gliomas are incredibly challenging disease en-tities in many ways due to the inter- and intratumoral het-erogeneity that is a hallmark of them Experience to datehints that future successes in malignant gliomas rest inneuro-oncology entering the era of precision medicinewhere validated biomarkers and targeted personalizedtherapies are seamlessly integrated into the managementparadigm Accordingly systems supporting surgical re-section and patient-specific tumor tissue analysis mustbe built and organized to guide the decision making fortherapy As our overall approach to the management ofmalignant gliomas evolves so should the framework ofsurgical management The clinical benefits of maximalsafe resection are well founded and well reportedHowever the oncological neurosurgeon must now lookbeyond maximal cytoreduction itself and recognize thevalue of thoughtful acquisition and analysis of tumor tis-sue Modern neurosurgeons must consider themselvessurgical neuro-oncologists and engagement and partici-pation of surgeons into clinical trials particularly early-phase trials should be encouraged and valued In turnwe should provide our surgical trainees with the trainingand tools in neuro-oncology to help them participate andcontribute in multidisciplinary collaborative efforts aimingto advance the understanding of brain tumor biology andultimately improve the outlook of our patients
References
1 Lacroix M Abi-Said D Fourney DR Gokaslan ZL et al A multivariateanalysis of 416 patients with glioblastoma multiforme prognosisextent of resection and survival J Neurosurg 2001 95190ndash198
2 Hervey-Jumper SL Berger MS Maximizing safe resection of low-and high-grade glioma J Neurooncol 2016 130269ndash282
3 Sanai N Polley MY McDermott MW Parsa AT Berger MS An ex-tent of resection threshold for newly diagnosed glioblastomas JNeurosurg 2011 1153ndash8
4 Stummer W Pichlmeier U Meinel T et al Fluorescence-guided sur-gery with 5-aminolevulinic acid for resection of malignant glioma arandomised controlled multicentre phase III trial Lancet Oncol2006 7392ndash401
5 Brown TJ Brennan MC Li M et al Association of the extent ofresection with survival in glioblastoma a systematic review andmeta-analysis JAMA Oncol 2016 21460ndash1469
6 Rahman M Abbatematteo J De Leo EK et al The effects of new orworsened postoperative neurological deficits on survival of patientswith glioblastoma J Neurosurg 2017 127123ndash131
7 Louis DN Perry A Reifenberger G et al The 2016 World HealthOrganization Classification of Tumors of the Central NervousSystem a summary Acta Neuropathol 2016 131803ndash820
8 McGirt MJ Bulsara KR Cummings TJ et al Prognostic value ofmagnetic resonance imaging-guided stereotactic biopsy in the
evaluation of recurrent malignant astrocytoma compared with a le-sion due to radiation effect J Neurosurg 2003 9814ndash20
9 Muragaki Y Chernov M Maruyama T et al Low-grade glioma onstereotactic biopsy how often is the diagnosis accurate MinimInvasive Neurosurg 2008 51275ndash279
10 Woodworth G McGirt MJ Samdani A Garonzik I Olivi AWeingart JD Accuracy of frameless and frame-based image-guided stereotactic brain biopsy in the diagnosis of glioma com-parison of biopsy and open resection specimen Neurol Res 200527358ndash362
11 Suzuki H Aoki K Chiba K et al Mutational landscape and clonal ar-chitecture in grade II and III gliomas Nat Genet 2015 47458ndash468
12 Stupp R Mason WP van den Bent MJ et al Radiotherapy plus con-comitant and adjuvant temozolomide for glioblastoma N Engl JMed 2005 352987ndash996
13 Kreisl TN Kim L Moore K et al Phase II trial of single-agent bevaci-zumab followed by bevacizumab plus irinotecan at tumor progres-sion in recurrent glioblastoma J Clin Oncol 2009 27740ndash745
14 Vredenburgh JJ Desjardins A Herndon 2nd JE et al Phase II trial ofbevacizumab and irinotecan in recurrent malignant glioma ClinCancer Res 2007 131253ndash1259
15 Chinot OL Wick W Mason W et al Bevacizumab plusradiotherapy-temozolomide for newly diagnosed glioblastomaN Engl J Med 2014 370709ndash722
16 Gilbert MR Dignam JJ Armstrong TS et al A randomized trial ofbevacizumab for newly diagnosed glioblastoma N Engl J Med2014 370699ndash708
17 Sandmann T Bourgon R Garcia J et al Patients with proneural glio-blastoma may derive overall survival benefit from the addition of bev-acizumab to first-line radiotherapy and temozolomide retrospectiveanalysis of the AVAglio trial J Clin Oncol 2015 332735ndash2744
18 Jackson RJ Fuller GN Abi-Said D et al Limitations of stereotacticbiopsy in the initial management of gliomas Neuro Oncol 20013193ndash200
19 Stupp R Hegi ME Gorlia T et al Cilengitide combined with stan-dard treatment for patients with newly diagnosed glioblastoma withmethylated MGMT promoter (CENTRIC EORTC 26071-22072study) a multicentre randomised open-label phase 3 trial LancetOncol 2014 151100ndash1108
20 Weller M Nabors LB Gorlia T et al Cilengitide in newly diagnosedglioblastoma biomarker expression and outcome Oncotarget2016 715018ndash15032
21 Stupp R Taillibert S Kanner AA et al Maintenance therapy withtumor-treating fields plus temozolomide vs temozolomide alone forglioblastoma a randomized clinical trial JAMA 20153142535ndash2543
22 Wick W TTFields where does all the skepticism come from NeuroOncol 2016 18303ndash305
23 Sampson JH Alternating electric fields for the treatment of glioblas-toma JAMA 2015 3142511ndash2513
24 Lang FF Asher A Prospective clinical trials of brain tumor therapy thecritical role of neurosurgeons J Neurooncol 2004 69151ndash167
25 Lang FF Gilbert MR Puduvalli VK et al Toward better early-phasebrain tumor clinical trials a reappraisal of current methods and pro-posals for future strategies Neuro Oncol 2002 4268ndash277
26 Elkhaled A Jalbert L Constantin A et al Characterization of metab-olites in infiltrating gliomas using ex vivo (1)H high-resolution magicangle spinning spectroscopy NMR Biomed 2014 27578ndash593
27 Jalbert LE Neill E Phillips JJ et al Magnetic resonance analysis ofmalignant transformation in recurrent glioma Neuro Oncol 2016181169ndash1179
28 Touat M Duran-Pena A Alentorn A Lacroix L Massard C Idbaih AEmerging circulating biomarkers in glioblastoma promises andchallenges Expert Rev Mol Diagn 2015 151311ndash1323
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
108
Update on RadiationCombinations in theTreatment of Patientswith Malignant BrainTumors FromRadiosensitizers toImmunotherapy
Debra Nana Yeboa MD1
Erik P Sulman MD PhD123
Departments of 1Radiation Oncology2Translational Molecular Pathology and3Genomic Medicine The University of Texas MDAnderson Cancer Center 1515 Holcombe BlvdUnit 97 Houston Texas USA Tel 713-563-2300dnyeboamdandersonorg andepsulmanmdandersonorg
109
AbstractAdvances in radiosensitizers and immunotherapyhave ushered in a new frontier in brain tumortreatment The brain has often been viewed as asanctuary site due to the bloodndashbrain barrier andthus the 2 primary modalities of therapy includedsurgery and radiation therapy (RT) More recentlysystemic therapies have played a greater role aseither combination therapy radiosensitizers or im-munotherapy Two novel radiosensitizers are beingdeveloped for the treatment of brain metastasesRRx-001 for example is a small molecule thataccelerates the NO2 to NO conversion of deoxyhe-moglobin and the agent 2-dexoyglucose (2-DG) is anonmetabolized glucose analogue that interfereswith ATP formation Poly(ADP-ribose) DNA polymer-ase inhibitors are promising due to their distinctradiobiological effects Veliparib and olaparib areamong the most studied with randomized trialsexploring their use in gliomas and brain metastasesImmunotherapy including immune checkpoint inhib-itors may play a role for both primary gliomas andbrain metastases RT has been shown to enhancethe function of cytotoxic T lymphocytes induce infil-tration of cytotoxic T lymphocytes and enhancefunction Trials are presently exploring use of bothprogrammed cell death protein (PD)1 and PD ligand1 blockade in glioblastoma patients with radiationSimilarly several immunotherapies are being investi-gated with either stereotactic radiosurgery or wholebrain radiation therapy for brain metastases In thisreview the use of radiosensitizers and immunother-apy agents with RT will be discussed broadly
Keywords brain metastases brain tumors gliomasimmunotherapy radiation therapy radiosensitizers
Radiosensitizers andImmunotherapy inBrain TumorsAdvances in radiosensitizers and immunotherapy haveushered in a new frontier to brain tumor treatment Braintumors however are a diverse class sharing only similaranatomic location Both primary brain malignancies andbrain metastasis have widely diverse histologies and mo-lecular phenotypes With the bloodndashbrain barrier thebrain has often been viewed as a sanctuary site and thusthe 2 primary modalities of therapy included surgery andradiation with decreased benefit from systemic agentsdue to lack of brain penetration However more recentlysystemic therapies have played a greater role as eithercombination therapy radiosensitizers or immunother-apy While temozolomide (TMZ) has played a pivotal rolefor glioblastoma (GBM) only a subset of patients benefitfrom the treatment1 The use of alternative systemicagents that may potentiate the effects of radiation ther-apy (RT) is becoming increasingly appealing Similarly forbrain metastases a variety of systemic agents are beingexplored primarily based on histology and immune pro-file In this review the use of radiosensitizers and immu-notherapy agents currently under investigation with RTwill be discussed
RadiosensitizersThe guiding concept of radiation sensitization is to in-crease the biologic effect of radiation such as increasedDNA damage decreased DNA repair decreased hypoxiaor increased G2M cell cycle blockade leading to im-proved tumor control and increased patient survival2
Poly(adenosine diphosphate-ribose) DNA polymerase(PARP) inhibitors are promising radiosensitizers due totheir roles in DNA repair3 PARP inhibitors work againstPARP1 a nuclear enzyme involved in the recruitment ofrepair proteins used in base excision repair and single-strand break repair PARP1 may also play a role in nonho-mologous end-joining4 The primary investigation ofPARP inhibitors has been in potentiating radiation andchemotherapy effects the latter in the context of homolo-gous repair deficient tumors For radiation the primarymechanism of action is inducing damage to nucleotidesleading to single-strand and double-strand breaks ThusPARP inhibitors in combination with radiation have an ap-pealing mechanism to inhibit or delay DNA repair andlikely convert more single-strand breaks to double-strandbreaks4
While several PARP inhibitors are currently being evalu-ated in a variety of tumors including talazoparib and nira-parib veliparib and olaparib are among the most studiedand there are randomized trials exploring their use in
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
110
gliomas The US National Cancer Institute (NCI)ndashfundedAlliance for Clinical Trials in Oncology (Alliance) A071102is a randomized phase IIIII trial evaluating the use ofveliparib in combination with TMZ in the adjuvant settingin patients with GBM tumors exhibiting hypermethylationof the O6 methylguanine DNA methyltransferase (MGMT)gene promoter Preclinical data supporting this trial sug-gested that only patients with MGMT methylated tumorswould benefit from the combination a group of patientsfor whom TMZ concurrent with radiation might be mostbeneficial5 A phase I trial performed by the NCI-fundedAmerican Brain Tumor Consortium attempted to combineveliparib with radiation and TMZ but failed to identify asuitable recommended phase II dose due to significanthemotoxicity6 Thus attempts to combine radiation withveliparib have focused on patients least likely to benefitfrom TMZ namely with MGMT unmethylated tumors forwhom TMZ could be withheld The Australian VeliparibRT and TMZ trial in newly diagnosed unmethylatedMGMT glioblastoma (VERTU) is a single-arm study inwhich patients receive RT with veliparib followed by adju-vant TMZ and veliparib4
An ongoing novel approach to radiosensitize gliomasinvolves a combination with an agent that interferes withan essential metabolic process 2-Dexoyglucose (2-DG)is a nonmetabolized glucose analogue that acts as acompetitive inhibitor of glycolysis It is transported acrossthe bloodndashbrain barrier by the glucose transporter GLUT-1 and thus has good penetration into the CNSIntracellularly it is trapped and accumulates in cells simi-lar to the mechanism of 18-fluorodeoxyglucose 2-DG isphosphorylated by glycolytic enzymes and the
phosphorylated 2-DG (2-deoxyglucose-P) is trapped in-tracellularly Inhibition of hexokinase activity by 2-DGinterferes with ATP formation and results in tumor celldeath7 While it has positive attributes by selectively tar-geting metabolically active tumor cells 2-DG has alsobeen associated with Q-T prolongation The currentphase III trial in gliomas is assessing the toxicity and tol-erability of 2-DG with hypofractionated radiation of 5 Gyas a radiosensitizer7
Two novel radiosensitizers are being developed for thetreatment of brain metastases First RRx-001 is a smallmolecule initially designed by the aerospace industry Itworks in part as a radiosensitizer by increasing blood flowand thus oxygenation of tumors through nitric oxideRRx-001 which binds to hemoglobin accelerates theNO2 to NO conversion of deoxyhemoglobin It workslocally under hypoxic conditions and subsequentlythe radiosensitive effects through nitric oxide are invasodilation and inhibiting DNA repair enzymes8 Nitricoxide is relatively benign The higher levels of oxidativestress with H2O2 and superoxide in tumors in comparisonto normal tissues result in the preferential generation ofreactive peroxynitrite in the presence of higher nitric oxidelevels7 This accounts for the increased specificity anddecreased toxicity with RRx-001 The dose limiting toxic-ity in a phase I trial of 25 patients treated with eitherweekly or biweekly infusions was infusional pain relatedto the release of NO at the site of injection7 Outside ofpreclinical models 2 clinical reports examining wholebrain radiation therapy (WBRT) with RRx-001 reported anintracranial response A patient with melanoma and 2hemorrhagic edematous lesions of 26 cm and 33 cm
Table 1 Clinical trials involving immunotherapy and radiation therapy1213
Clinical Trials Number Phase Disease Type Treatment Groups
NCT02667587 II Newly diagnosed GBMMGMT-methylated
Nivolumabthorn TMZthorn RT vs placebothornTMZ thorn RT
NCT02617589 III Newly diagnosed GBM Nivolumabthorn RT vs TMZthorn RTNCT02336165 II Newly diagnosed unmethylated
MGMT recurrent glioblastomaMEDI4736thorn standard RT vs MEDI4736 thorn
bevacizumabNCT02530502 III Newly diagnosed GBM RTthorn TMZthorn pembrolizumab TMZthorn
pembrolizumabNCT02313272 I Recurrent glioma Hypofractionated stereotactic radiationthorn
pembrolizumab thorn bevacizumabNCT02696993 III Brain metastases Nivolumabthorn SRS nivolumabthornWBRT
nivolumabthorn ipilimumab thorn SRS nivolu-mabthorn ipilimumab thornWBRT
NCT02115139 II Melanoma brain metastases Ipilimumab thornWBRTNCT02097732 II Melanoma brain metastases Ipilimumab SRS ipilimumab vs SRS
ipilimumabNCT01703507 I Melanoma brain metastases Ipilimumab thornWBRT vs ipilimumab thorn SRSNCT02107755 II Melanoma brain metastases Ipilimumab thorn SRSNCT02858869 pilot Melanoma and NSCLC Pembrolizumabthorn SRSNCT01950195 I Melanoma brain metastases Ipilimumab thorn SRSNCT02662725 II Melanoma brain metastases Ipilimumab thorn SRS
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
111
after a single intravenous dose of RRx-001 of 5 mgm2 4days before WBRT resulted in symptomatic improvementwithin 48 hours By 4 months after radiation there was areduction in size in the largest dimension down to 10 cmand 23 cm of the respective lesions A second report of amelanoma patient with at least 18 lesions after receivingRRx-001 of 5 mgm2 4 days before WBRT as well astwice weekly doses during the 2 weeks of radiation alsoshowed response The patient at 4 months had disap-pearance of 13 of 18 lesions with shrinkage of theremaining 5 lesions8 Presently BRAINSTORM is a phaseIII dose escalation trial of RRx-001 designed to be ad-ministered twice weekly for 2 weeks with WBRT (30 Gy in10 fractions) with the option for weekly maintenance8
Veliparib has also been evaluated in the setting of brainmetastases It was tested in a global randomized con-trolled trial with WBRT Veliparib is orally bioavailable andcrosses the bloodndashbrain barrier It was first examined in amultihistology phase I trial in patients with nonndashsmall celllung cancer (NSCLC) breast cancer melanoma and re-nal and colorectal cancers among others The study of81 patients tested dose tolerance of veliparib from 10 to300 mg orally twice a day with WBRT to 30 Gy in 10 frac-tions or 375 Gy in 15 fractions9 The phase I trial dose es-calation portion did not reach the predefined criteria forthe maximum tolerated dose but there was amplificationof the adverse effects of nausea and vomiting among thehighest dose cohort of 300 mg bid9 The adverse eventprofile at 200 mg bid was similar to that of WBRT aloneDoses of veliparib from 20 to 200 mg bid demonstratesimilar antitumor activity and other studies in preclinicalmodels found that 50 mg daily demonstrated significantreduction in poly(ADP-ribose) in peripheral blood mono-nuclear cells and tumor tissue while also effectivelycrossing the bloodndashbrain barrier Thus the subsequentphase II trial examined 50 mg with WBRT9 In order to as-sess a more homogeneous cohort the phase III globalrandomized trial studied only NSCLC at the 2 doses of50 mg and 200 mg twice daily versus placebo twice a daywith WBRT10 The primary endpoint was overall survivalIn 307 patients in a 111 randomization of 50 mg bid200 mg bid or placebo twice daily the study found nosignificant differences in overall survival among the differ-ent groups10 The majority of patients across the treat-ment groups had a graded prognostic assessment (GPA)score of25 and a Karnofsky performance status ofgt80 The median overall survival was 185 days forpatients receiving placebo and 209 days for those receiv-ing veliparib without any statistically significant differ-ence These results were similar to the disease-specificestimate of median survival for the disease-specific GPAof NSCLC patients with brain metastases10
Several other radiosensitizers have failed to improve overradiation alone in a number of trials These have includedtrials with WBRT including motexafin gadolinium efap-roxyn bortozemib thalidomide teniposide topotecanpaclitaxel and cisplatin7 Of note other PARP inhibitorsalso being assessed include talazoparib and niraparib4
which may yield positive results The use of valproic acid(VPA) as a histone deacetylase inhibitor has also beenconsidered to have radiosensitizing potential in additionto its anti-epileptic drug properties11 While studies havereported that patients with GBM receiving an anti-epilep-tic agent may have higher overall survival than those re-ceiving standard chemoradiation therapy alone thebenefit remains controversial Retrospective analysissuggested that patients taking VPA specifically had bettersurvival in comparison to other anti-epileptic drugs Alsoa recent prospective phase II trial was performed in 37patients with GBM receiving VPA 25 mgkg concurrentlywith TMZ chemoradiation and reported a median survivalof 296 months While controversial further data andinvestigation are needed into this and other agents thatmay potentiate RT
Immunotherapy and radiationImmune checkpoint inhibitors lead to activation of T cellswhich may traffic across the bloodndashbrain barrier to inter-act with tumor Primary brain tumors may evade the im-mune system through upregulation of immunecheckpoints and possible immunosuppression12
Monoclonal antibodies promote immune-mediated anti-tumor activity by inhibiting the immune functionndashmediated cytotoxic T-lymphocyte associated protein 4(CTLA-4) and programmed cell death protein 1 (PD-1)receptors PD protein ligand (PD-L1) is upregulated inGBM through oncogenic signaling possibly throughphosphatase and tensin homolog loss and interleukin-10signaling1314 RT has also been shown to enhance thefunction of cytotoxic T lymphocytes RT may induce aninfiltration of cytotoxic T lymphocytes and enhance theirfunction It may also induce antindashCTLA-4 agents inhibitingT-cell function and increasing the CD8thorn T cellregulatoryT cell ratio in cases of melanoma15 Thus PD-1 and PD-L1 blockers may have a further role in CNS managementwith the use of radiation
In preclinical models radiation has been examined withimmunotherapy that included among other mechanismsvaccination PD-1 blockade and CTLA-4 blockade Inmice radiation plus a vaccination of irradiated gliomacells was associated with increased survival of 40 to80 compared with 0 to 10 for other groups stud-ied16 A benefit of PD-1 blockade with stereotactic radio-surgery (SRS) specifically has also been shown in amouse model In comparison to mice treated with radia-tion antindashPD-1 therapy or a combination only those re-ceiving combination therapy had a higher percentagesurvival alive beyond 180 days after treatment17 Othermouse carcinoma models have identified response withanti-CTLA antibody and fractionated radiation therapy18
CD137 activation CTLA-4 blockade and focal radiationtherapy have been examined in an immunocompetent in-tracranial GBM model Mice treated with triple combina-tion therapy had 50 greater survival19 In other murine
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
112
models the use of antindashPD-1 and antindashCTLA-4 agentsshowed improved survival and increased tumor infiltratingleukocyte populations compared with single modalitywith concurrent radiation16 There are conflicting data re-garding timing or sequencing of therapy with some ani-mal models showing no difference in tumor response inrelation to timing of RT and delivery of immunotherapy18
For instance in one animal model CTLA-4 blockade de-livered simultaneously with radiation or delivered a coupleof days after showed no difference in survival among themice19
Increased PD-1 expression in circulating monocytes hasbeen identified as a biomarker for tumor-induced immu-nosuppression and may serve as a prognostic factor forpotentially worse survival outcomes in clinic13 In onestudy GBM patients with lower PD-L1 expression hadhigher median overall survival than those with higher PD-L1 expression suggesting that lower expression may beassociated with less immunosuppression and more im-mune activity against the tumor glioma20 RT with immunecheckpoint blockade is being investigated to assess if theaddition of PD-1 and PD-L1 inhibitors may improve theoutcomes or toxicity profile of standard therapy For in-stance a multi-institutional trial opened as a phase III willevaluate outcomes in GBM receiving radiation and pem-brolizumab with TMZ (NCT02530502) Next durvalumabor MEDI4736 a PD-L1 inhibitor is being examined forunmethylated MGMT GBMs with standard radiotherapy(NCT02336165)12 The impact of checkpoint inhibitorsduring adjuvant treatment of GBM is currently beingevaluated in the NCI-funded NRG-BN002 trial(NCT02311920) which will evaluate the antindashCTLA-4antibody ipilimumab alone or in combination with theantindashPD-1 antibody nivolumab for patients with newlydiagnosed GBM
Brain metastases have clonal populations of cells differ-ent from the rest of the brain and a unique microenviron-ment that may influence immunotherapy There may bemore immune infiltrates in metastases than in primarybrain tumors21 PD-L1 expression in brain metastasesvaries by histology In a series evaluating PD-L1 expres-sion in various tumors including melanoma NSCLCbreast renal colorectal and small cell less than 10showed significant expression22 There was greatest ex-pression among NSCLC and melanoma with a correla-tion between PD-L1 expression and tumor infiltratinglymphocytes22 Institutional series have examined thecombination of radiation and immune checkpoint block-ade In another study specific to melanoma brain metas-tases PD-L1 expression was found in over 50 of thecases and among those cases over 40 expressedPD-L1 in more than 5 of tumor cells23 The largest bodyof data for use of PD-L1 with radiation is for melanomaand NSCLC
Ipilimumab is a human monoclonal antibody that blocksCTLA-4 and allows for T-cell activation and proliferationto enhance the immune response to cancer In a
retrospective review of 70 patients with brain metastasestreated with SRS or WBRT the 33 patients receiving im-munotherapy had a median survival of 183 months incomparison to the 37 patients who did not receive ipili-mumab with a median survival of 53 months While therewere limited data among the cohort to evaluate sequenc-ing of therapy among 10 evaluable patients 40 whoreceived ipilimumab prior to RT had a partial response incomparison to only 10 among the cohort of 22 evalu-able patients who did not receive ipilimumab therapy atall with radiation24 Another retrospective institutionalstudy of 77 patients in which 37 received ipilimumabfound that patients treated with SRS and ipilimumab hada median survival of 213 months versus 49 months forthose not receiving ipilimumab Most interestingly theyidentified that the correlation remained significant evenafter adjusting for additional factors such as performancestatus Secondly there was not an increased need for useof salvage WBRT25
The sequencing of radiotherapy and immune checkpointinhibitors is of interest In a study of patients with brainmetastases the one-year survival for patients receivingSRS before ipilimumab was greater at 65 in contrast to56 for those receiving it concurrently and 40 for thosereceiving it after SRS26 Similarly another study of 75patients with 566 brain metastases showed greater tu-mor lesion response at 6 months from SRS for patientsreceiving ipilimumab nivolumab or pembrolizumabwithin 4 weeks of their SRS27 Those receiving concurrenttherapy had by 6 months a decrease of 949 in compar-ison to 662 for those not receiving checkpoint inhibi-tors within 4 weeks Prospective clinical trials areinvestigating different combinations of RT with immunecheckpoint blockers in this setting For instance new tri-als are currently evaluating intracranial tumor control at 6months and the timing of immune therapy or immunecheckpoint inhibitors in relation to SRS28
Vaccines are also being developed for primary braintumors showing some evidence for their use Vaccinesdeveloped from dendritic cells and tumor lysate with tu-mor antigens such as the epidermal growth factor recep-tor variant III vaccine have shown promise29 Forinstance in a placebo controlled phase II trial of ICT-107a vaccine composed on autologous dendritic cells andtumor antigens progression-free survival was increasedby 2 months for those receiving the vaccine30 Radiationmay assist in serving as a primer for the immunogeniceffects by facilitating tumor antigen uptake by dendriticcells and cross presentation on major histocompatibilitycomplex I Thus RT may assist in the tumor-specific cy-totoxic T lymphocytes associated with the immunemechanism
In conclusion although there may be challenges to com-bining and sequencing brain tumors radiosensitizersand immunotherapy the opportunities and potential fornovel applications are promising For brain tumors brainmetastases are typically underrepresented in trials
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
113
despite being among the most common intracraniallesions Despite their large population patients with brainmetastases are often excluded from clinical trials withnovel agents due to concerns regarding confounding out-comes and tolerability12 Primary gliomas also offer anovel frontier for the use of immunotherapy to standardadjuvant chemotherapy and radiation particularly forpatients with GBM less likely to respond to TMZ such aswith unmethylated MGMT As studies work to define therole of RT and radiosensitizers and immunotherapy fur-ther analysis is needed to assess the timing of RT andthese treatments
References
1 Stupp R Hegi ME Mason WP et al Effects of radiotherapy withconcomitant and adjuvant temozolomide versus radiotherapy aloneon survival in glioblastoma in a randomised phase III study 5-yearanalysis of the EORTC-NCIC trial Lancet Oncol 2009 10459ndash466
2 Lawrence TS Blackstock AW McGinn C The mechanism of actionof radiosensitization of conventional chemotherapeutic agentsSemin Radiat Oncol 2003 1313ndash21
3 Lesueur P Chevalier F Austry JB et al Poly-(ADP-ribose)-polymer-ase inhibitors as radiosensitizers a systematic review of pre-clinicaland clinical human studies Oncotarget 2017 8(40)69105ndash69124
4 Lester A Rapkins R Nixdorf S Khasraw M McDonald KCombining PARP inhibitors with radiation therapy for the treatmentof glioblastoma is PTEN predictive of response Clin Transl Oncol2017 19273ndash278
5 Gupta SK Kizilbash SH Carlson BL et al Delineation of MGMT hyper-methylation as a biomarker for veliparib-mediated temozolomide-sensi-tizing therapy of glioblastoma J Natl Cancer Inst 2016 108
6 Kleinberg LR Blakeley J Mikkelsen T et al An American BrainTumor Consortium (ABTC) phase 1 trial of veliparib (ABT-888)temozolomide (TMZ) and concurrent radiation therapy (RT) fornewly diagnosed glioblastoma multiforme (GBM) need for modifica-tion to approach for combining these therapies InternationalJ Radiat Oncol Biol Phys 2012 84S7ndashS8
7 Oronsky BT A Review of two promising radiosensitizers in brainmetastases Rrx-001 and 2-deoxyglucose In NC Oronsky edJ Cancer Sci Ther 2015 pp 137ndash141
8 Kim MM Parmar H Cao Y et al Concurrent whole brain radiother-apy and RRx-001 for melanoma brain metastases Neuro Onc2016 18455ndash456
9 Mehta MP Wang D Wang F et al Veliparib in combination withwhole brain radiation therapy in patients with brain metastasesresults of a phase 1 study J Neurooncol 2015 122409ndash417
10 Chabot P Hsia TC Ryu JS et al Veliparib in combination withwhole-brain radiation therapy for patients with brain metastasesfrom non-small cell lung cancer results of a randomized globalplacebo-controlled study J Neurooncol 2017 131105ndash115
11 Ochiai S Nomoto Y Yamashita Y et al Roles of valproic acid inimproving radiation therapy for glioblastoma a review of literaturefocusing on clinical evidence Asian Pac J Cancer Prev 201617463ndash466
12 Tan AC Heimberger AB Menzies AM Pavlakis N Khasraw MImmune checkpoint inhibitors for brain metastases Curr Oncol Rep2017 1938
13 DrsquoSouza NM Fang P Logan J Yang J Jiang W Li JCombining radiation therapy with immune checkpoint blockade
for central nervous system malignancies Frontiers Oncol 20166212
14 Parsa AT Waldron JS Panner A et al Loss of tumor suppressorPTEN function increases B7-H1 expression and immunoresistancein glioma Nat Med 2007 1384ndash88
15 Binder DC Davis AA Wainwright DA Immunotherapy for cancer inthe central nervous system current and future directionsOncoimmunology 2016 5e1082027
16 Newcomb EW Demaria S Lukyanov Y et al The combination ofionizing radiation and peripheral vaccination produces long-termsurvival of mice bearing established invasive GL261 gliomas ClinCancer Res 2006 124730ndash4737
17 Zeng J See AP Phallen J et al Anti-PD-1 blockade and stereotac-tic radiation produce long-term survival in mice with intracranial glio-mas Int J Radiat Oncol Biol Phys 2013 86343ndash349
18 Chow KK Hara W Lim M Li G Combining immunotherapy withradiation for the treatment of glioblastoma J Neurooncol2015123459ndash464
19 Belcaid Z Phallen JA Zeng J et al Focal radiation therapy com-bined with 4-1BB activation and CTLA-4 blockade yields long-termsurvival and a protective antigen-specific memory response in amurine glioma model PLoS One 2014 9e101764
20 Topalian SL Hodi FS Brahmer JR et al Safety activity and im-mune correlates of anti-PD-1 antibody in cancer N Engl J Med2012 3662443ndash2454
21 Bienkowski M Preusser M Prognostic role of tumour-infiltrating in-flammatory cells in brain tumours literature review Curr OpinNeurol 2015 28647ndash658
22 Harter PN Bernatz S Scholz A et al Distribution and prognostic rel-evance of tumor-infiltrating lymphocytes (TILs) and PD-1PD-L1 im-mune checkpoints in human brain metastases Oncotarget 2015640836ndash40849
23 Berghoff AS Ricken G Widhalm G et al Tumour-infiltrating lym-phocytes and expression of programmed death ligand 1 (PD-L1) inmelanoma brain metastases Histopathology 2015 66289ndash299
24 Silk AW Bassetti MF West BT Tsien CI Lao CD Ipilimumab and ra-diation therapy for melanoma brain metastases Cancer Med 20132899ndash906
25 Knisely JP Yu JB Flanigan J Sznol M Kluger HM Chiang VLRadiosurgery for melanoma brain metastases in the ipilimumab eraand the possibility of longer survival J Neurosurg 2012117227ndash233
26 Kiess AP Wolchok JD Barker CA et al Stereotactic radiosurgeryfor melanoma brain metastases in patients receiving ipilimumabsafety profile and efficacy of combined treatment Int J Radiat OncolBiol Phys 2015 92368ndash375
27 Qian JM Yu JB Kluger HM Chiang VL Timing and type of immunecheckpoint therapy affect the early radiographic response of mela-noma brain metastases to stereotactic radiosurgery Cancer 20161223051ndash3058
28 Silk AW Cao Y Gomez-Hassan D et al A randomized phase IIstudy of ipilimumab induction in patients with melanoma brain me-tastases receiving stereotactic radiosurgery J Clin Oncol 2015 33TPS9079ndashTPS9079
29 Neagu MR Reardon DA An Update on the role of immunotherapyand vaccine strategies for primary brain tumors Curr TreatOptions Oncol 2015 1654
30 Wen PY Reardon DA Phuphanich S et al A randomized double-blind placebo-controlled phase 2 trial of dendritic cell (DC) vaccina-tion with ICT-107 in newly diagnosed glioblastoma (GBM) patientsJ Clin Oncol 2014 322005ndash2005
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
114
British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

necessary corollary to these novel diagnostic tools Itremains indisputable however that clinical validation ofthese novel diagnostic tools will also require systematiccorrelation with human tumor tissue obtained throughsurgery These samples ideally gathered prospectivelywill provide a pivot upon which we can expand our under-standing of the complex network of oncological pro-cesses driving these tumors
Malignant gliomas are incredibly challenging disease en-tities in many ways due to the inter- and intratumoral het-erogeneity that is a hallmark of them Experience to datehints that future successes in malignant gliomas rest inneuro-oncology entering the era of precision medicinewhere validated biomarkers and targeted personalizedtherapies are seamlessly integrated into the managementparadigm Accordingly systems supporting surgical re-section and patient-specific tumor tissue analysis mustbe built and organized to guide the decision making fortherapy As our overall approach to the management ofmalignant gliomas evolves so should the framework ofsurgical management The clinical benefits of maximalsafe resection are well founded and well reportedHowever the oncological neurosurgeon must now lookbeyond maximal cytoreduction itself and recognize thevalue of thoughtful acquisition and analysis of tumor tis-sue Modern neurosurgeons must consider themselvessurgical neuro-oncologists and engagement and partici-pation of surgeons into clinical trials particularly early-phase trials should be encouraged and valued In turnwe should provide our surgical trainees with the trainingand tools in neuro-oncology to help them participate andcontribute in multidisciplinary collaborative efforts aimingto advance the understanding of brain tumor biology andultimately improve the outlook of our patients
References
1 Lacroix M Abi-Said D Fourney DR Gokaslan ZL et al A multivariateanalysis of 416 patients with glioblastoma multiforme prognosisextent of resection and survival J Neurosurg 2001 95190ndash198
2 Hervey-Jumper SL Berger MS Maximizing safe resection of low-and high-grade glioma J Neurooncol 2016 130269ndash282
3 Sanai N Polley MY McDermott MW Parsa AT Berger MS An ex-tent of resection threshold for newly diagnosed glioblastomas JNeurosurg 2011 1153ndash8
4 Stummer W Pichlmeier U Meinel T et al Fluorescence-guided sur-gery with 5-aminolevulinic acid for resection of malignant glioma arandomised controlled multicentre phase III trial Lancet Oncol2006 7392ndash401
5 Brown TJ Brennan MC Li M et al Association of the extent ofresection with survival in glioblastoma a systematic review andmeta-analysis JAMA Oncol 2016 21460ndash1469
6 Rahman M Abbatematteo J De Leo EK et al The effects of new orworsened postoperative neurological deficits on survival of patientswith glioblastoma J Neurosurg 2017 127123ndash131
7 Louis DN Perry A Reifenberger G et al The 2016 World HealthOrganization Classification of Tumors of the Central NervousSystem a summary Acta Neuropathol 2016 131803ndash820
8 McGirt MJ Bulsara KR Cummings TJ et al Prognostic value ofmagnetic resonance imaging-guided stereotactic biopsy in the
evaluation of recurrent malignant astrocytoma compared with a le-sion due to radiation effect J Neurosurg 2003 9814ndash20
9 Muragaki Y Chernov M Maruyama T et al Low-grade glioma onstereotactic biopsy how often is the diagnosis accurate MinimInvasive Neurosurg 2008 51275ndash279
10 Woodworth G McGirt MJ Samdani A Garonzik I Olivi AWeingart JD Accuracy of frameless and frame-based image-guided stereotactic brain biopsy in the diagnosis of glioma com-parison of biopsy and open resection specimen Neurol Res 200527358ndash362
11 Suzuki H Aoki K Chiba K et al Mutational landscape and clonal ar-chitecture in grade II and III gliomas Nat Genet 2015 47458ndash468
12 Stupp R Mason WP van den Bent MJ et al Radiotherapy plus con-comitant and adjuvant temozolomide for glioblastoma N Engl JMed 2005 352987ndash996
13 Kreisl TN Kim L Moore K et al Phase II trial of single-agent bevaci-zumab followed by bevacizumab plus irinotecan at tumor progres-sion in recurrent glioblastoma J Clin Oncol 2009 27740ndash745
14 Vredenburgh JJ Desjardins A Herndon 2nd JE et al Phase II trial ofbevacizumab and irinotecan in recurrent malignant glioma ClinCancer Res 2007 131253ndash1259
15 Chinot OL Wick W Mason W et al Bevacizumab plusradiotherapy-temozolomide for newly diagnosed glioblastomaN Engl J Med 2014 370709ndash722
16 Gilbert MR Dignam JJ Armstrong TS et al A randomized trial ofbevacizumab for newly diagnosed glioblastoma N Engl J Med2014 370699ndash708
17 Sandmann T Bourgon R Garcia J et al Patients with proneural glio-blastoma may derive overall survival benefit from the addition of bev-acizumab to first-line radiotherapy and temozolomide retrospectiveanalysis of the AVAglio trial J Clin Oncol 2015 332735ndash2744
18 Jackson RJ Fuller GN Abi-Said D et al Limitations of stereotacticbiopsy in the initial management of gliomas Neuro Oncol 20013193ndash200
19 Stupp R Hegi ME Gorlia T et al Cilengitide combined with stan-dard treatment for patients with newly diagnosed glioblastoma withmethylated MGMT promoter (CENTRIC EORTC 26071-22072study) a multicentre randomised open-label phase 3 trial LancetOncol 2014 151100ndash1108
20 Weller M Nabors LB Gorlia T et al Cilengitide in newly diagnosedglioblastoma biomarker expression and outcome Oncotarget2016 715018ndash15032
21 Stupp R Taillibert S Kanner AA et al Maintenance therapy withtumor-treating fields plus temozolomide vs temozolomide alone forglioblastoma a randomized clinical trial JAMA 20153142535ndash2543
22 Wick W TTFields where does all the skepticism come from NeuroOncol 2016 18303ndash305
23 Sampson JH Alternating electric fields for the treatment of glioblas-toma JAMA 2015 3142511ndash2513
24 Lang FF Asher A Prospective clinical trials of brain tumor therapy thecritical role of neurosurgeons J Neurooncol 2004 69151ndash167
25 Lang FF Gilbert MR Puduvalli VK et al Toward better early-phasebrain tumor clinical trials a reappraisal of current methods and pro-posals for future strategies Neuro Oncol 2002 4268ndash277
26 Elkhaled A Jalbert L Constantin A et al Characterization of metab-olites in infiltrating gliomas using ex vivo (1)H high-resolution magicangle spinning spectroscopy NMR Biomed 2014 27578ndash593
27 Jalbert LE Neill E Phillips JJ et al Magnetic resonance analysis ofmalignant transformation in recurrent glioma Neuro Oncol 2016181169ndash1179
28 Touat M Duran-Pena A Alentorn A Lacroix L Massard C Idbaih AEmerging circulating biomarkers in glioblastoma promises andchallenges Expert Rev Mol Diagn 2015 151311ndash1323
The Value of Surgical Resection for Malignant Gliomas in the Modern Era Volume 2 Issue 3
108
Update on RadiationCombinations in theTreatment of Patientswith Malignant BrainTumors FromRadiosensitizers toImmunotherapy
Debra Nana Yeboa MD1
Erik P Sulman MD PhD123
Departments of 1Radiation Oncology2Translational Molecular Pathology and3Genomic Medicine The University of Texas MDAnderson Cancer Center 1515 Holcombe BlvdUnit 97 Houston Texas USA Tel 713-563-2300dnyeboamdandersonorg andepsulmanmdandersonorg
109
AbstractAdvances in radiosensitizers and immunotherapyhave ushered in a new frontier in brain tumortreatment The brain has often been viewed as asanctuary site due to the bloodndashbrain barrier andthus the 2 primary modalities of therapy includedsurgery and radiation therapy (RT) More recentlysystemic therapies have played a greater role aseither combination therapy radiosensitizers or im-munotherapy Two novel radiosensitizers are beingdeveloped for the treatment of brain metastasesRRx-001 for example is a small molecule thataccelerates the NO2 to NO conversion of deoxyhe-moglobin and the agent 2-dexoyglucose (2-DG) is anonmetabolized glucose analogue that interfereswith ATP formation Poly(ADP-ribose) DNA polymer-ase inhibitors are promising due to their distinctradiobiological effects Veliparib and olaparib areamong the most studied with randomized trialsexploring their use in gliomas and brain metastasesImmunotherapy including immune checkpoint inhib-itors may play a role for both primary gliomas andbrain metastases RT has been shown to enhancethe function of cytotoxic T lymphocytes induce infil-tration of cytotoxic T lymphocytes and enhancefunction Trials are presently exploring use of bothprogrammed cell death protein (PD)1 and PD ligand1 blockade in glioblastoma patients with radiationSimilarly several immunotherapies are being investi-gated with either stereotactic radiosurgery or wholebrain radiation therapy for brain metastases In thisreview the use of radiosensitizers and immunother-apy agents with RT will be discussed broadly
Keywords brain metastases brain tumors gliomasimmunotherapy radiation therapy radiosensitizers
Radiosensitizers andImmunotherapy inBrain TumorsAdvances in radiosensitizers and immunotherapy haveushered in a new frontier to brain tumor treatment Braintumors however are a diverse class sharing only similaranatomic location Both primary brain malignancies andbrain metastasis have widely diverse histologies and mo-lecular phenotypes With the bloodndashbrain barrier thebrain has often been viewed as a sanctuary site and thusthe 2 primary modalities of therapy included surgery andradiation with decreased benefit from systemic agentsdue to lack of brain penetration However more recentlysystemic therapies have played a greater role as eithercombination therapy radiosensitizers or immunother-apy While temozolomide (TMZ) has played a pivotal rolefor glioblastoma (GBM) only a subset of patients benefitfrom the treatment1 The use of alternative systemicagents that may potentiate the effects of radiation ther-apy (RT) is becoming increasingly appealing Similarly forbrain metastases a variety of systemic agents are beingexplored primarily based on histology and immune pro-file In this review the use of radiosensitizers and immu-notherapy agents currently under investigation with RTwill be discussed
RadiosensitizersThe guiding concept of radiation sensitization is to in-crease the biologic effect of radiation such as increasedDNA damage decreased DNA repair decreased hypoxiaor increased G2M cell cycle blockade leading to im-proved tumor control and increased patient survival2
Poly(adenosine diphosphate-ribose) DNA polymerase(PARP) inhibitors are promising radiosensitizers due totheir roles in DNA repair3 PARP inhibitors work againstPARP1 a nuclear enzyme involved in the recruitment ofrepair proteins used in base excision repair and single-strand break repair PARP1 may also play a role in nonho-mologous end-joining4 The primary investigation ofPARP inhibitors has been in potentiating radiation andchemotherapy effects the latter in the context of homolo-gous repair deficient tumors For radiation the primarymechanism of action is inducing damage to nucleotidesleading to single-strand and double-strand breaks ThusPARP inhibitors in combination with radiation have an ap-pealing mechanism to inhibit or delay DNA repair andlikely convert more single-strand breaks to double-strandbreaks4
While several PARP inhibitors are currently being evalu-ated in a variety of tumors including talazoparib and nira-parib veliparib and olaparib are among the most studiedand there are randomized trials exploring their use in
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
110
gliomas The US National Cancer Institute (NCI)ndashfundedAlliance for Clinical Trials in Oncology (Alliance) A071102is a randomized phase IIIII trial evaluating the use ofveliparib in combination with TMZ in the adjuvant settingin patients with GBM tumors exhibiting hypermethylationof the O6 methylguanine DNA methyltransferase (MGMT)gene promoter Preclinical data supporting this trial sug-gested that only patients with MGMT methylated tumorswould benefit from the combination a group of patientsfor whom TMZ concurrent with radiation might be mostbeneficial5 A phase I trial performed by the NCI-fundedAmerican Brain Tumor Consortium attempted to combineveliparib with radiation and TMZ but failed to identify asuitable recommended phase II dose due to significanthemotoxicity6 Thus attempts to combine radiation withveliparib have focused on patients least likely to benefitfrom TMZ namely with MGMT unmethylated tumors forwhom TMZ could be withheld The Australian VeliparibRT and TMZ trial in newly diagnosed unmethylatedMGMT glioblastoma (VERTU) is a single-arm study inwhich patients receive RT with veliparib followed by adju-vant TMZ and veliparib4
An ongoing novel approach to radiosensitize gliomasinvolves a combination with an agent that interferes withan essential metabolic process 2-Dexoyglucose (2-DG)is a nonmetabolized glucose analogue that acts as acompetitive inhibitor of glycolysis It is transported acrossthe bloodndashbrain barrier by the glucose transporter GLUT-1 and thus has good penetration into the CNSIntracellularly it is trapped and accumulates in cells simi-lar to the mechanism of 18-fluorodeoxyglucose 2-DG isphosphorylated by glycolytic enzymes and the
phosphorylated 2-DG (2-deoxyglucose-P) is trapped in-tracellularly Inhibition of hexokinase activity by 2-DGinterferes with ATP formation and results in tumor celldeath7 While it has positive attributes by selectively tar-geting metabolically active tumor cells 2-DG has alsobeen associated with Q-T prolongation The currentphase III trial in gliomas is assessing the toxicity and tol-erability of 2-DG with hypofractionated radiation of 5 Gyas a radiosensitizer7
Two novel radiosensitizers are being developed for thetreatment of brain metastases First RRx-001 is a smallmolecule initially designed by the aerospace industry Itworks in part as a radiosensitizer by increasing blood flowand thus oxygenation of tumors through nitric oxideRRx-001 which binds to hemoglobin accelerates theNO2 to NO conversion of deoxyhemoglobin It workslocally under hypoxic conditions and subsequentlythe radiosensitive effects through nitric oxide are invasodilation and inhibiting DNA repair enzymes8 Nitricoxide is relatively benign The higher levels of oxidativestress with H2O2 and superoxide in tumors in comparisonto normal tissues result in the preferential generation ofreactive peroxynitrite in the presence of higher nitric oxidelevels7 This accounts for the increased specificity anddecreased toxicity with RRx-001 The dose limiting toxic-ity in a phase I trial of 25 patients treated with eitherweekly or biweekly infusions was infusional pain relatedto the release of NO at the site of injection7 Outside ofpreclinical models 2 clinical reports examining wholebrain radiation therapy (WBRT) with RRx-001 reported anintracranial response A patient with melanoma and 2hemorrhagic edematous lesions of 26 cm and 33 cm
Table 1 Clinical trials involving immunotherapy and radiation therapy1213
Clinical Trials Number Phase Disease Type Treatment Groups
NCT02667587 II Newly diagnosed GBMMGMT-methylated
Nivolumabthorn TMZthorn RT vs placebothornTMZ thorn RT
NCT02617589 III Newly diagnosed GBM Nivolumabthorn RT vs TMZthorn RTNCT02336165 II Newly diagnosed unmethylated
MGMT recurrent glioblastomaMEDI4736thorn standard RT vs MEDI4736 thorn
bevacizumabNCT02530502 III Newly diagnosed GBM RTthorn TMZthorn pembrolizumab TMZthorn
pembrolizumabNCT02313272 I Recurrent glioma Hypofractionated stereotactic radiationthorn
pembrolizumab thorn bevacizumabNCT02696993 III Brain metastases Nivolumabthorn SRS nivolumabthornWBRT
nivolumabthorn ipilimumab thorn SRS nivolu-mabthorn ipilimumab thornWBRT
NCT02115139 II Melanoma brain metastases Ipilimumab thornWBRTNCT02097732 II Melanoma brain metastases Ipilimumab SRS ipilimumab vs SRS
ipilimumabNCT01703507 I Melanoma brain metastases Ipilimumab thornWBRT vs ipilimumab thorn SRSNCT02107755 II Melanoma brain metastases Ipilimumab thorn SRSNCT02858869 pilot Melanoma and NSCLC Pembrolizumabthorn SRSNCT01950195 I Melanoma brain metastases Ipilimumab thorn SRSNCT02662725 II Melanoma brain metastases Ipilimumab thorn SRS
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
111
after a single intravenous dose of RRx-001 of 5 mgm2 4days before WBRT resulted in symptomatic improvementwithin 48 hours By 4 months after radiation there was areduction in size in the largest dimension down to 10 cmand 23 cm of the respective lesions A second report of amelanoma patient with at least 18 lesions after receivingRRx-001 of 5 mgm2 4 days before WBRT as well astwice weekly doses during the 2 weeks of radiation alsoshowed response The patient at 4 months had disap-pearance of 13 of 18 lesions with shrinkage of theremaining 5 lesions8 Presently BRAINSTORM is a phaseIII dose escalation trial of RRx-001 designed to be ad-ministered twice weekly for 2 weeks with WBRT (30 Gy in10 fractions) with the option for weekly maintenance8
Veliparib has also been evaluated in the setting of brainmetastases It was tested in a global randomized con-trolled trial with WBRT Veliparib is orally bioavailable andcrosses the bloodndashbrain barrier It was first examined in amultihistology phase I trial in patients with nonndashsmall celllung cancer (NSCLC) breast cancer melanoma and re-nal and colorectal cancers among others The study of81 patients tested dose tolerance of veliparib from 10 to300 mg orally twice a day with WBRT to 30 Gy in 10 frac-tions or 375 Gy in 15 fractions9 The phase I trial dose es-calation portion did not reach the predefined criteria forthe maximum tolerated dose but there was amplificationof the adverse effects of nausea and vomiting among thehighest dose cohort of 300 mg bid9 The adverse eventprofile at 200 mg bid was similar to that of WBRT aloneDoses of veliparib from 20 to 200 mg bid demonstratesimilar antitumor activity and other studies in preclinicalmodels found that 50 mg daily demonstrated significantreduction in poly(ADP-ribose) in peripheral blood mono-nuclear cells and tumor tissue while also effectivelycrossing the bloodndashbrain barrier Thus the subsequentphase II trial examined 50 mg with WBRT9 In order to as-sess a more homogeneous cohort the phase III globalrandomized trial studied only NSCLC at the 2 doses of50 mg and 200 mg twice daily versus placebo twice a daywith WBRT10 The primary endpoint was overall survivalIn 307 patients in a 111 randomization of 50 mg bid200 mg bid or placebo twice daily the study found nosignificant differences in overall survival among the differ-ent groups10 The majority of patients across the treat-ment groups had a graded prognostic assessment (GPA)score of25 and a Karnofsky performance status ofgt80 The median overall survival was 185 days forpatients receiving placebo and 209 days for those receiv-ing veliparib without any statistically significant differ-ence These results were similar to the disease-specificestimate of median survival for the disease-specific GPAof NSCLC patients with brain metastases10
Several other radiosensitizers have failed to improve overradiation alone in a number of trials These have includedtrials with WBRT including motexafin gadolinium efap-roxyn bortozemib thalidomide teniposide topotecanpaclitaxel and cisplatin7 Of note other PARP inhibitorsalso being assessed include talazoparib and niraparib4
which may yield positive results The use of valproic acid(VPA) as a histone deacetylase inhibitor has also beenconsidered to have radiosensitizing potential in additionto its anti-epileptic drug properties11 While studies havereported that patients with GBM receiving an anti-epilep-tic agent may have higher overall survival than those re-ceiving standard chemoradiation therapy alone thebenefit remains controversial Retrospective analysissuggested that patients taking VPA specifically had bettersurvival in comparison to other anti-epileptic drugs Alsoa recent prospective phase II trial was performed in 37patients with GBM receiving VPA 25 mgkg concurrentlywith TMZ chemoradiation and reported a median survivalof 296 months While controversial further data andinvestigation are needed into this and other agents thatmay potentiate RT
Immunotherapy and radiationImmune checkpoint inhibitors lead to activation of T cellswhich may traffic across the bloodndashbrain barrier to inter-act with tumor Primary brain tumors may evade the im-mune system through upregulation of immunecheckpoints and possible immunosuppression12
Monoclonal antibodies promote immune-mediated anti-tumor activity by inhibiting the immune functionndashmediated cytotoxic T-lymphocyte associated protein 4(CTLA-4) and programmed cell death protein 1 (PD-1)receptors PD protein ligand (PD-L1) is upregulated inGBM through oncogenic signaling possibly throughphosphatase and tensin homolog loss and interleukin-10signaling1314 RT has also been shown to enhance thefunction of cytotoxic T lymphocytes RT may induce aninfiltration of cytotoxic T lymphocytes and enhance theirfunction It may also induce antindashCTLA-4 agents inhibitingT-cell function and increasing the CD8thorn T cellregulatoryT cell ratio in cases of melanoma15 Thus PD-1 and PD-L1 blockers may have a further role in CNS managementwith the use of radiation
In preclinical models radiation has been examined withimmunotherapy that included among other mechanismsvaccination PD-1 blockade and CTLA-4 blockade Inmice radiation plus a vaccination of irradiated gliomacells was associated with increased survival of 40 to80 compared with 0 to 10 for other groups stud-ied16 A benefit of PD-1 blockade with stereotactic radio-surgery (SRS) specifically has also been shown in amouse model In comparison to mice treated with radia-tion antindashPD-1 therapy or a combination only those re-ceiving combination therapy had a higher percentagesurvival alive beyond 180 days after treatment17 Othermouse carcinoma models have identified response withanti-CTLA antibody and fractionated radiation therapy18
CD137 activation CTLA-4 blockade and focal radiationtherapy have been examined in an immunocompetent in-tracranial GBM model Mice treated with triple combina-tion therapy had 50 greater survival19 In other murine
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
112
models the use of antindashPD-1 and antindashCTLA-4 agentsshowed improved survival and increased tumor infiltratingleukocyte populations compared with single modalitywith concurrent radiation16 There are conflicting data re-garding timing or sequencing of therapy with some ani-mal models showing no difference in tumor response inrelation to timing of RT and delivery of immunotherapy18
For instance in one animal model CTLA-4 blockade de-livered simultaneously with radiation or delivered a coupleof days after showed no difference in survival among themice19
Increased PD-1 expression in circulating monocytes hasbeen identified as a biomarker for tumor-induced immu-nosuppression and may serve as a prognostic factor forpotentially worse survival outcomes in clinic13 In onestudy GBM patients with lower PD-L1 expression hadhigher median overall survival than those with higher PD-L1 expression suggesting that lower expression may beassociated with less immunosuppression and more im-mune activity against the tumor glioma20 RT with immunecheckpoint blockade is being investigated to assess if theaddition of PD-1 and PD-L1 inhibitors may improve theoutcomes or toxicity profile of standard therapy For in-stance a multi-institutional trial opened as a phase III willevaluate outcomes in GBM receiving radiation and pem-brolizumab with TMZ (NCT02530502) Next durvalumabor MEDI4736 a PD-L1 inhibitor is being examined forunmethylated MGMT GBMs with standard radiotherapy(NCT02336165)12 The impact of checkpoint inhibitorsduring adjuvant treatment of GBM is currently beingevaluated in the NCI-funded NRG-BN002 trial(NCT02311920) which will evaluate the antindashCTLA-4antibody ipilimumab alone or in combination with theantindashPD-1 antibody nivolumab for patients with newlydiagnosed GBM
Brain metastases have clonal populations of cells differ-ent from the rest of the brain and a unique microenviron-ment that may influence immunotherapy There may bemore immune infiltrates in metastases than in primarybrain tumors21 PD-L1 expression in brain metastasesvaries by histology In a series evaluating PD-L1 expres-sion in various tumors including melanoma NSCLCbreast renal colorectal and small cell less than 10showed significant expression22 There was greatest ex-pression among NSCLC and melanoma with a correla-tion between PD-L1 expression and tumor infiltratinglymphocytes22 Institutional series have examined thecombination of radiation and immune checkpoint block-ade In another study specific to melanoma brain metas-tases PD-L1 expression was found in over 50 of thecases and among those cases over 40 expressedPD-L1 in more than 5 of tumor cells23 The largest bodyof data for use of PD-L1 with radiation is for melanomaand NSCLC
Ipilimumab is a human monoclonal antibody that blocksCTLA-4 and allows for T-cell activation and proliferationto enhance the immune response to cancer In a
retrospective review of 70 patients with brain metastasestreated with SRS or WBRT the 33 patients receiving im-munotherapy had a median survival of 183 months incomparison to the 37 patients who did not receive ipili-mumab with a median survival of 53 months While therewere limited data among the cohort to evaluate sequenc-ing of therapy among 10 evaluable patients 40 whoreceived ipilimumab prior to RT had a partial response incomparison to only 10 among the cohort of 22 evalu-able patients who did not receive ipilimumab therapy atall with radiation24 Another retrospective institutionalstudy of 77 patients in which 37 received ipilimumabfound that patients treated with SRS and ipilimumab hada median survival of 213 months versus 49 months forthose not receiving ipilimumab Most interestingly theyidentified that the correlation remained significant evenafter adjusting for additional factors such as performancestatus Secondly there was not an increased need for useof salvage WBRT25
The sequencing of radiotherapy and immune checkpointinhibitors is of interest In a study of patients with brainmetastases the one-year survival for patients receivingSRS before ipilimumab was greater at 65 in contrast to56 for those receiving it concurrently and 40 for thosereceiving it after SRS26 Similarly another study of 75patients with 566 brain metastases showed greater tu-mor lesion response at 6 months from SRS for patientsreceiving ipilimumab nivolumab or pembrolizumabwithin 4 weeks of their SRS27 Those receiving concurrenttherapy had by 6 months a decrease of 949 in compar-ison to 662 for those not receiving checkpoint inhibi-tors within 4 weeks Prospective clinical trials areinvestigating different combinations of RT with immunecheckpoint blockers in this setting For instance new tri-als are currently evaluating intracranial tumor control at 6months and the timing of immune therapy or immunecheckpoint inhibitors in relation to SRS28
Vaccines are also being developed for primary braintumors showing some evidence for their use Vaccinesdeveloped from dendritic cells and tumor lysate with tu-mor antigens such as the epidermal growth factor recep-tor variant III vaccine have shown promise29 Forinstance in a placebo controlled phase II trial of ICT-107a vaccine composed on autologous dendritic cells andtumor antigens progression-free survival was increasedby 2 months for those receiving the vaccine30 Radiationmay assist in serving as a primer for the immunogeniceffects by facilitating tumor antigen uptake by dendriticcells and cross presentation on major histocompatibilitycomplex I Thus RT may assist in the tumor-specific cy-totoxic T lymphocytes associated with the immunemechanism
In conclusion although there may be challenges to com-bining and sequencing brain tumors radiosensitizersand immunotherapy the opportunities and potential fornovel applications are promising For brain tumors brainmetastases are typically underrepresented in trials
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
113
despite being among the most common intracraniallesions Despite their large population patients with brainmetastases are often excluded from clinical trials withnovel agents due to concerns regarding confounding out-comes and tolerability12 Primary gliomas also offer anovel frontier for the use of immunotherapy to standardadjuvant chemotherapy and radiation particularly forpatients with GBM less likely to respond to TMZ such aswith unmethylated MGMT As studies work to define therole of RT and radiosensitizers and immunotherapy fur-ther analysis is needed to assess the timing of RT andthese treatments
References
1 Stupp R Hegi ME Mason WP et al Effects of radiotherapy withconcomitant and adjuvant temozolomide versus radiotherapy aloneon survival in glioblastoma in a randomised phase III study 5-yearanalysis of the EORTC-NCIC trial Lancet Oncol 2009 10459ndash466
2 Lawrence TS Blackstock AW McGinn C The mechanism of actionof radiosensitization of conventional chemotherapeutic agentsSemin Radiat Oncol 2003 1313ndash21
3 Lesueur P Chevalier F Austry JB et al Poly-(ADP-ribose)-polymer-ase inhibitors as radiosensitizers a systematic review of pre-clinicaland clinical human studies Oncotarget 2017 8(40)69105ndash69124
4 Lester A Rapkins R Nixdorf S Khasraw M McDonald KCombining PARP inhibitors with radiation therapy for the treatmentof glioblastoma is PTEN predictive of response Clin Transl Oncol2017 19273ndash278
5 Gupta SK Kizilbash SH Carlson BL et al Delineation of MGMT hyper-methylation as a biomarker for veliparib-mediated temozolomide-sensi-tizing therapy of glioblastoma J Natl Cancer Inst 2016 108
6 Kleinberg LR Blakeley J Mikkelsen T et al An American BrainTumor Consortium (ABTC) phase 1 trial of veliparib (ABT-888)temozolomide (TMZ) and concurrent radiation therapy (RT) fornewly diagnosed glioblastoma multiforme (GBM) need for modifica-tion to approach for combining these therapies InternationalJ Radiat Oncol Biol Phys 2012 84S7ndashS8
7 Oronsky BT A Review of two promising radiosensitizers in brainmetastases Rrx-001 and 2-deoxyglucose In NC Oronsky edJ Cancer Sci Ther 2015 pp 137ndash141
8 Kim MM Parmar H Cao Y et al Concurrent whole brain radiother-apy and RRx-001 for melanoma brain metastases Neuro Onc2016 18455ndash456
9 Mehta MP Wang D Wang F et al Veliparib in combination withwhole brain radiation therapy in patients with brain metastasesresults of a phase 1 study J Neurooncol 2015 122409ndash417
10 Chabot P Hsia TC Ryu JS et al Veliparib in combination withwhole-brain radiation therapy for patients with brain metastasesfrom non-small cell lung cancer results of a randomized globalplacebo-controlled study J Neurooncol 2017 131105ndash115
11 Ochiai S Nomoto Y Yamashita Y et al Roles of valproic acid inimproving radiation therapy for glioblastoma a review of literaturefocusing on clinical evidence Asian Pac J Cancer Prev 201617463ndash466
12 Tan AC Heimberger AB Menzies AM Pavlakis N Khasraw MImmune checkpoint inhibitors for brain metastases Curr Oncol Rep2017 1938
13 DrsquoSouza NM Fang P Logan J Yang J Jiang W Li JCombining radiation therapy with immune checkpoint blockade
for central nervous system malignancies Frontiers Oncol 20166212
14 Parsa AT Waldron JS Panner A et al Loss of tumor suppressorPTEN function increases B7-H1 expression and immunoresistancein glioma Nat Med 2007 1384ndash88
15 Binder DC Davis AA Wainwright DA Immunotherapy for cancer inthe central nervous system current and future directionsOncoimmunology 2016 5e1082027
16 Newcomb EW Demaria S Lukyanov Y et al The combination ofionizing radiation and peripheral vaccination produces long-termsurvival of mice bearing established invasive GL261 gliomas ClinCancer Res 2006 124730ndash4737
17 Zeng J See AP Phallen J et al Anti-PD-1 blockade and stereotac-tic radiation produce long-term survival in mice with intracranial glio-mas Int J Radiat Oncol Biol Phys 2013 86343ndash349
18 Chow KK Hara W Lim M Li G Combining immunotherapy withradiation for the treatment of glioblastoma J Neurooncol2015123459ndash464
19 Belcaid Z Phallen JA Zeng J et al Focal radiation therapy com-bined with 4-1BB activation and CTLA-4 blockade yields long-termsurvival and a protective antigen-specific memory response in amurine glioma model PLoS One 2014 9e101764
20 Topalian SL Hodi FS Brahmer JR et al Safety activity and im-mune correlates of anti-PD-1 antibody in cancer N Engl J Med2012 3662443ndash2454
21 Bienkowski M Preusser M Prognostic role of tumour-infiltrating in-flammatory cells in brain tumours literature review Curr OpinNeurol 2015 28647ndash658
22 Harter PN Bernatz S Scholz A et al Distribution and prognostic rel-evance of tumor-infiltrating lymphocytes (TILs) and PD-1PD-L1 im-mune checkpoints in human brain metastases Oncotarget 2015640836ndash40849
23 Berghoff AS Ricken G Widhalm G et al Tumour-infiltrating lym-phocytes and expression of programmed death ligand 1 (PD-L1) inmelanoma brain metastases Histopathology 2015 66289ndash299
24 Silk AW Bassetti MF West BT Tsien CI Lao CD Ipilimumab and ra-diation therapy for melanoma brain metastases Cancer Med 20132899ndash906
25 Knisely JP Yu JB Flanigan J Sznol M Kluger HM Chiang VLRadiosurgery for melanoma brain metastases in the ipilimumab eraand the possibility of longer survival J Neurosurg 2012117227ndash233
26 Kiess AP Wolchok JD Barker CA et al Stereotactic radiosurgeryfor melanoma brain metastases in patients receiving ipilimumabsafety profile and efficacy of combined treatment Int J Radiat OncolBiol Phys 2015 92368ndash375
27 Qian JM Yu JB Kluger HM Chiang VL Timing and type of immunecheckpoint therapy affect the early radiographic response of mela-noma brain metastases to stereotactic radiosurgery Cancer 20161223051ndash3058
28 Silk AW Cao Y Gomez-Hassan D et al A randomized phase IIstudy of ipilimumab induction in patients with melanoma brain me-tastases receiving stereotactic radiosurgery J Clin Oncol 2015 33TPS9079ndashTPS9079
29 Neagu MR Reardon DA An Update on the role of immunotherapyand vaccine strategies for primary brain tumors Curr TreatOptions Oncol 2015 1654
30 Wen PY Reardon DA Phuphanich S et al A randomized double-blind placebo-controlled phase 2 trial of dendritic cell (DC) vaccina-tion with ICT-107 in newly diagnosed glioblastoma (GBM) patientsJ Clin Oncol 2014 322005ndash2005
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
114
British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

Update on RadiationCombinations in theTreatment of Patientswith Malignant BrainTumors FromRadiosensitizers toImmunotherapy
Debra Nana Yeboa MD1
Erik P Sulman MD PhD123
Departments of 1Radiation Oncology2Translational Molecular Pathology and3Genomic Medicine The University of Texas MDAnderson Cancer Center 1515 Holcombe BlvdUnit 97 Houston Texas USA Tel 713-563-2300dnyeboamdandersonorg andepsulmanmdandersonorg
109
AbstractAdvances in radiosensitizers and immunotherapyhave ushered in a new frontier in brain tumortreatment The brain has often been viewed as asanctuary site due to the bloodndashbrain barrier andthus the 2 primary modalities of therapy includedsurgery and radiation therapy (RT) More recentlysystemic therapies have played a greater role aseither combination therapy radiosensitizers or im-munotherapy Two novel radiosensitizers are beingdeveloped for the treatment of brain metastasesRRx-001 for example is a small molecule thataccelerates the NO2 to NO conversion of deoxyhe-moglobin and the agent 2-dexoyglucose (2-DG) is anonmetabolized glucose analogue that interfereswith ATP formation Poly(ADP-ribose) DNA polymer-ase inhibitors are promising due to their distinctradiobiological effects Veliparib and olaparib areamong the most studied with randomized trialsexploring their use in gliomas and brain metastasesImmunotherapy including immune checkpoint inhib-itors may play a role for both primary gliomas andbrain metastases RT has been shown to enhancethe function of cytotoxic T lymphocytes induce infil-tration of cytotoxic T lymphocytes and enhancefunction Trials are presently exploring use of bothprogrammed cell death protein (PD)1 and PD ligand1 blockade in glioblastoma patients with radiationSimilarly several immunotherapies are being investi-gated with either stereotactic radiosurgery or wholebrain radiation therapy for brain metastases In thisreview the use of radiosensitizers and immunother-apy agents with RT will be discussed broadly
Keywords brain metastases brain tumors gliomasimmunotherapy radiation therapy radiosensitizers
Radiosensitizers andImmunotherapy inBrain TumorsAdvances in radiosensitizers and immunotherapy haveushered in a new frontier to brain tumor treatment Braintumors however are a diverse class sharing only similaranatomic location Both primary brain malignancies andbrain metastasis have widely diverse histologies and mo-lecular phenotypes With the bloodndashbrain barrier thebrain has often been viewed as a sanctuary site and thusthe 2 primary modalities of therapy included surgery andradiation with decreased benefit from systemic agentsdue to lack of brain penetration However more recentlysystemic therapies have played a greater role as eithercombination therapy radiosensitizers or immunother-apy While temozolomide (TMZ) has played a pivotal rolefor glioblastoma (GBM) only a subset of patients benefitfrom the treatment1 The use of alternative systemicagents that may potentiate the effects of radiation ther-apy (RT) is becoming increasingly appealing Similarly forbrain metastases a variety of systemic agents are beingexplored primarily based on histology and immune pro-file In this review the use of radiosensitizers and immu-notherapy agents currently under investigation with RTwill be discussed
RadiosensitizersThe guiding concept of radiation sensitization is to in-crease the biologic effect of radiation such as increasedDNA damage decreased DNA repair decreased hypoxiaor increased G2M cell cycle blockade leading to im-proved tumor control and increased patient survival2
Poly(adenosine diphosphate-ribose) DNA polymerase(PARP) inhibitors are promising radiosensitizers due totheir roles in DNA repair3 PARP inhibitors work againstPARP1 a nuclear enzyme involved in the recruitment ofrepair proteins used in base excision repair and single-strand break repair PARP1 may also play a role in nonho-mologous end-joining4 The primary investigation ofPARP inhibitors has been in potentiating radiation andchemotherapy effects the latter in the context of homolo-gous repair deficient tumors For radiation the primarymechanism of action is inducing damage to nucleotidesleading to single-strand and double-strand breaks ThusPARP inhibitors in combination with radiation have an ap-pealing mechanism to inhibit or delay DNA repair andlikely convert more single-strand breaks to double-strandbreaks4
While several PARP inhibitors are currently being evalu-ated in a variety of tumors including talazoparib and nira-parib veliparib and olaparib are among the most studiedand there are randomized trials exploring their use in
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
110
gliomas The US National Cancer Institute (NCI)ndashfundedAlliance for Clinical Trials in Oncology (Alliance) A071102is a randomized phase IIIII trial evaluating the use ofveliparib in combination with TMZ in the adjuvant settingin patients with GBM tumors exhibiting hypermethylationof the O6 methylguanine DNA methyltransferase (MGMT)gene promoter Preclinical data supporting this trial sug-gested that only patients with MGMT methylated tumorswould benefit from the combination a group of patientsfor whom TMZ concurrent with radiation might be mostbeneficial5 A phase I trial performed by the NCI-fundedAmerican Brain Tumor Consortium attempted to combineveliparib with radiation and TMZ but failed to identify asuitable recommended phase II dose due to significanthemotoxicity6 Thus attempts to combine radiation withveliparib have focused on patients least likely to benefitfrom TMZ namely with MGMT unmethylated tumors forwhom TMZ could be withheld The Australian VeliparibRT and TMZ trial in newly diagnosed unmethylatedMGMT glioblastoma (VERTU) is a single-arm study inwhich patients receive RT with veliparib followed by adju-vant TMZ and veliparib4
An ongoing novel approach to radiosensitize gliomasinvolves a combination with an agent that interferes withan essential metabolic process 2-Dexoyglucose (2-DG)is a nonmetabolized glucose analogue that acts as acompetitive inhibitor of glycolysis It is transported acrossthe bloodndashbrain barrier by the glucose transporter GLUT-1 and thus has good penetration into the CNSIntracellularly it is trapped and accumulates in cells simi-lar to the mechanism of 18-fluorodeoxyglucose 2-DG isphosphorylated by glycolytic enzymes and the
phosphorylated 2-DG (2-deoxyglucose-P) is trapped in-tracellularly Inhibition of hexokinase activity by 2-DGinterferes with ATP formation and results in tumor celldeath7 While it has positive attributes by selectively tar-geting metabolically active tumor cells 2-DG has alsobeen associated with Q-T prolongation The currentphase III trial in gliomas is assessing the toxicity and tol-erability of 2-DG with hypofractionated radiation of 5 Gyas a radiosensitizer7
Two novel radiosensitizers are being developed for thetreatment of brain metastases First RRx-001 is a smallmolecule initially designed by the aerospace industry Itworks in part as a radiosensitizer by increasing blood flowand thus oxygenation of tumors through nitric oxideRRx-001 which binds to hemoglobin accelerates theNO2 to NO conversion of deoxyhemoglobin It workslocally under hypoxic conditions and subsequentlythe radiosensitive effects through nitric oxide are invasodilation and inhibiting DNA repair enzymes8 Nitricoxide is relatively benign The higher levels of oxidativestress with H2O2 and superoxide in tumors in comparisonto normal tissues result in the preferential generation ofreactive peroxynitrite in the presence of higher nitric oxidelevels7 This accounts for the increased specificity anddecreased toxicity with RRx-001 The dose limiting toxic-ity in a phase I trial of 25 patients treated with eitherweekly or biweekly infusions was infusional pain relatedto the release of NO at the site of injection7 Outside ofpreclinical models 2 clinical reports examining wholebrain radiation therapy (WBRT) with RRx-001 reported anintracranial response A patient with melanoma and 2hemorrhagic edematous lesions of 26 cm and 33 cm
Table 1 Clinical trials involving immunotherapy and radiation therapy1213
Clinical Trials Number Phase Disease Type Treatment Groups
NCT02667587 II Newly diagnosed GBMMGMT-methylated
Nivolumabthorn TMZthorn RT vs placebothornTMZ thorn RT
NCT02617589 III Newly diagnosed GBM Nivolumabthorn RT vs TMZthorn RTNCT02336165 II Newly diagnosed unmethylated
MGMT recurrent glioblastomaMEDI4736thorn standard RT vs MEDI4736 thorn
bevacizumabNCT02530502 III Newly diagnosed GBM RTthorn TMZthorn pembrolizumab TMZthorn
pembrolizumabNCT02313272 I Recurrent glioma Hypofractionated stereotactic radiationthorn
pembrolizumab thorn bevacizumabNCT02696993 III Brain metastases Nivolumabthorn SRS nivolumabthornWBRT
nivolumabthorn ipilimumab thorn SRS nivolu-mabthorn ipilimumab thornWBRT
NCT02115139 II Melanoma brain metastases Ipilimumab thornWBRTNCT02097732 II Melanoma brain metastases Ipilimumab SRS ipilimumab vs SRS
ipilimumabNCT01703507 I Melanoma brain metastases Ipilimumab thornWBRT vs ipilimumab thorn SRSNCT02107755 II Melanoma brain metastases Ipilimumab thorn SRSNCT02858869 pilot Melanoma and NSCLC Pembrolizumabthorn SRSNCT01950195 I Melanoma brain metastases Ipilimumab thorn SRSNCT02662725 II Melanoma brain metastases Ipilimumab thorn SRS
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
111
after a single intravenous dose of RRx-001 of 5 mgm2 4days before WBRT resulted in symptomatic improvementwithin 48 hours By 4 months after radiation there was areduction in size in the largest dimension down to 10 cmand 23 cm of the respective lesions A second report of amelanoma patient with at least 18 lesions after receivingRRx-001 of 5 mgm2 4 days before WBRT as well astwice weekly doses during the 2 weeks of radiation alsoshowed response The patient at 4 months had disap-pearance of 13 of 18 lesions with shrinkage of theremaining 5 lesions8 Presently BRAINSTORM is a phaseIII dose escalation trial of RRx-001 designed to be ad-ministered twice weekly for 2 weeks with WBRT (30 Gy in10 fractions) with the option for weekly maintenance8
Veliparib has also been evaluated in the setting of brainmetastases It was tested in a global randomized con-trolled trial with WBRT Veliparib is orally bioavailable andcrosses the bloodndashbrain barrier It was first examined in amultihistology phase I trial in patients with nonndashsmall celllung cancer (NSCLC) breast cancer melanoma and re-nal and colorectal cancers among others The study of81 patients tested dose tolerance of veliparib from 10 to300 mg orally twice a day with WBRT to 30 Gy in 10 frac-tions or 375 Gy in 15 fractions9 The phase I trial dose es-calation portion did not reach the predefined criteria forthe maximum tolerated dose but there was amplificationof the adverse effects of nausea and vomiting among thehighest dose cohort of 300 mg bid9 The adverse eventprofile at 200 mg bid was similar to that of WBRT aloneDoses of veliparib from 20 to 200 mg bid demonstratesimilar antitumor activity and other studies in preclinicalmodels found that 50 mg daily demonstrated significantreduction in poly(ADP-ribose) in peripheral blood mono-nuclear cells and tumor tissue while also effectivelycrossing the bloodndashbrain barrier Thus the subsequentphase II trial examined 50 mg with WBRT9 In order to as-sess a more homogeneous cohort the phase III globalrandomized trial studied only NSCLC at the 2 doses of50 mg and 200 mg twice daily versus placebo twice a daywith WBRT10 The primary endpoint was overall survivalIn 307 patients in a 111 randomization of 50 mg bid200 mg bid or placebo twice daily the study found nosignificant differences in overall survival among the differ-ent groups10 The majority of patients across the treat-ment groups had a graded prognostic assessment (GPA)score of25 and a Karnofsky performance status ofgt80 The median overall survival was 185 days forpatients receiving placebo and 209 days for those receiv-ing veliparib without any statistically significant differ-ence These results were similar to the disease-specificestimate of median survival for the disease-specific GPAof NSCLC patients with brain metastases10
Several other radiosensitizers have failed to improve overradiation alone in a number of trials These have includedtrials with WBRT including motexafin gadolinium efap-roxyn bortozemib thalidomide teniposide topotecanpaclitaxel and cisplatin7 Of note other PARP inhibitorsalso being assessed include talazoparib and niraparib4
which may yield positive results The use of valproic acid(VPA) as a histone deacetylase inhibitor has also beenconsidered to have radiosensitizing potential in additionto its anti-epileptic drug properties11 While studies havereported that patients with GBM receiving an anti-epilep-tic agent may have higher overall survival than those re-ceiving standard chemoradiation therapy alone thebenefit remains controversial Retrospective analysissuggested that patients taking VPA specifically had bettersurvival in comparison to other anti-epileptic drugs Alsoa recent prospective phase II trial was performed in 37patients with GBM receiving VPA 25 mgkg concurrentlywith TMZ chemoradiation and reported a median survivalof 296 months While controversial further data andinvestigation are needed into this and other agents thatmay potentiate RT
Immunotherapy and radiationImmune checkpoint inhibitors lead to activation of T cellswhich may traffic across the bloodndashbrain barrier to inter-act with tumor Primary brain tumors may evade the im-mune system through upregulation of immunecheckpoints and possible immunosuppression12
Monoclonal antibodies promote immune-mediated anti-tumor activity by inhibiting the immune functionndashmediated cytotoxic T-lymphocyte associated protein 4(CTLA-4) and programmed cell death protein 1 (PD-1)receptors PD protein ligand (PD-L1) is upregulated inGBM through oncogenic signaling possibly throughphosphatase and tensin homolog loss and interleukin-10signaling1314 RT has also been shown to enhance thefunction of cytotoxic T lymphocytes RT may induce aninfiltration of cytotoxic T lymphocytes and enhance theirfunction It may also induce antindashCTLA-4 agents inhibitingT-cell function and increasing the CD8thorn T cellregulatoryT cell ratio in cases of melanoma15 Thus PD-1 and PD-L1 blockers may have a further role in CNS managementwith the use of radiation
In preclinical models radiation has been examined withimmunotherapy that included among other mechanismsvaccination PD-1 blockade and CTLA-4 blockade Inmice radiation plus a vaccination of irradiated gliomacells was associated with increased survival of 40 to80 compared with 0 to 10 for other groups stud-ied16 A benefit of PD-1 blockade with stereotactic radio-surgery (SRS) specifically has also been shown in amouse model In comparison to mice treated with radia-tion antindashPD-1 therapy or a combination only those re-ceiving combination therapy had a higher percentagesurvival alive beyond 180 days after treatment17 Othermouse carcinoma models have identified response withanti-CTLA antibody and fractionated radiation therapy18
CD137 activation CTLA-4 blockade and focal radiationtherapy have been examined in an immunocompetent in-tracranial GBM model Mice treated with triple combina-tion therapy had 50 greater survival19 In other murine
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
112
models the use of antindashPD-1 and antindashCTLA-4 agentsshowed improved survival and increased tumor infiltratingleukocyte populations compared with single modalitywith concurrent radiation16 There are conflicting data re-garding timing or sequencing of therapy with some ani-mal models showing no difference in tumor response inrelation to timing of RT and delivery of immunotherapy18
For instance in one animal model CTLA-4 blockade de-livered simultaneously with radiation or delivered a coupleof days after showed no difference in survival among themice19
Increased PD-1 expression in circulating monocytes hasbeen identified as a biomarker for tumor-induced immu-nosuppression and may serve as a prognostic factor forpotentially worse survival outcomes in clinic13 In onestudy GBM patients with lower PD-L1 expression hadhigher median overall survival than those with higher PD-L1 expression suggesting that lower expression may beassociated with less immunosuppression and more im-mune activity against the tumor glioma20 RT with immunecheckpoint blockade is being investigated to assess if theaddition of PD-1 and PD-L1 inhibitors may improve theoutcomes or toxicity profile of standard therapy For in-stance a multi-institutional trial opened as a phase III willevaluate outcomes in GBM receiving radiation and pem-brolizumab with TMZ (NCT02530502) Next durvalumabor MEDI4736 a PD-L1 inhibitor is being examined forunmethylated MGMT GBMs with standard radiotherapy(NCT02336165)12 The impact of checkpoint inhibitorsduring adjuvant treatment of GBM is currently beingevaluated in the NCI-funded NRG-BN002 trial(NCT02311920) which will evaluate the antindashCTLA-4antibody ipilimumab alone or in combination with theantindashPD-1 antibody nivolumab for patients with newlydiagnosed GBM
Brain metastases have clonal populations of cells differ-ent from the rest of the brain and a unique microenviron-ment that may influence immunotherapy There may bemore immune infiltrates in metastases than in primarybrain tumors21 PD-L1 expression in brain metastasesvaries by histology In a series evaluating PD-L1 expres-sion in various tumors including melanoma NSCLCbreast renal colorectal and small cell less than 10showed significant expression22 There was greatest ex-pression among NSCLC and melanoma with a correla-tion between PD-L1 expression and tumor infiltratinglymphocytes22 Institutional series have examined thecombination of radiation and immune checkpoint block-ade In another study specific to melanoma brain metas-tases PD-L1 expression was found in over 50 of thecases and among those cases over 40 expressedPD-L1 in more than 5 of tumor cells23 The largest bodyof data for use of PD-L1 with radiation is for melanomaand NSCLC
Ipilimumab is a human monoclonal antibody that blocksCTLA-4 and allows for T-cell activation and proliferationto enhance the immune response to cancer In a
retrospective review of 70 patients with brain metastasestreated with SRS or WBRT the 33 patients receiving im-munotherapy had a median survival of 183 months incomparison to the 37 patients who did not receive ipili-mumab with a median survival of 53 months While therewere limited data among the cohort to evaluate sequenc-ing of therapy among 10 evaluable patients 40 whoreceived ipilimumab prior to RT had a partial response incomparison to only 10 among the cohort of 22 evalu-able patients who did not receive ipilimumab therapy atall with radiation24 Another retrospective institutionalstudy of 77 patients in which 37 received ipilimumabfound that patients treated with SRS and ipilimumab hada median survival of 213 months versus 49 months forthose not receiving ipilimumab Most interestingly theyidentified that the correlation remained significant evenafter adjusting for additional factors such as performancestatus Secondly there was not an increased need for useof salvage WBRT25
The sequencing of radiotherapy and immune checkpointinhibitors is of interest In a study of patients with brainmetastases the one-year survival for patients receivingSRS before ipilimumab was greater at 65 in contrast to56 for those receiving it concurrently and 40 for thosereceiving it after SRS26 Similarly another study of 75patients with 566 brain metastases showed greater tu-mor lesion response at 6 months from SRS for patientsreceiving ipilimumab nivolumab or pembrolizumabwithin 4 weeks of their SRS27 Those receiving concurrenttherapy had by 6 months a decrease of 949 in compar-ison to 662 for those not receiving checkpoint inhibi-tors within 4 weeks Prospective clinical trials areinvestigating different combinations of RT with immunecheckpoint blockers in this setting For instance new tri-als are currently evaluating intracranial tumor control at 6months and the timing of immune therapy or immunecheckpoint inhibitors in relation to SRS28
Vaccines are also being developed for primary braintumors showing some evidence for their use Vaccinesdeveloped from dendritic cells and tumor lysate with tu-mor antigens such as the epidermal growth factor recep-tor variant III vaccine have shown promise29 Forinstance in a placebo controlled phase II trial of ICT-107a vaccine composed on autologous dendritic cells andtumor antigens progression-free survival was increasedby 2 months for those receiving the vaccine30 Radiationmay assist in serving as a primer for the immunogeniceffects by facilitating tumor antigen uptake by dendriticcells and cross presentation on major histocompatibilitycomplex I Thus RT may assist in the tumor-specific cy-totoxic T lymphocytes associated with the immunemechanism
In conclusion although there may be challenges to com-bining and sequencing brain tumors radiosensitizersand immunotherapy the opportunities and potential fornovel applications are promising For brain tumors brainmetastases are typically underrepresented in trials
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
113
despite being among the most common intracraniallesions Despite their large population patients with brainmetastases are often excluded from clinical trials withnovel agents due to concerns regarding confounding out-comes and tolerability12 Primary gliomas also offer anovel frontier for the use of immunotherapy to standardadjuvant chemotherapy and radiation particularly forpatients with GBM less likely to respond to TMZ such aswith unmethylated MGMT As studies work to define therole of RT and radiosensitizers and immunotherapy fur-ther analysis is needed to assess the timing of RT andthese treatments
References
1 Stupp R Hegi ME Mason WP et al Effects of radiotherapy withconcomitant and adjuvant temozolomide versus radiotherapy aloneon survival in glioblastoma in a randomised phase III study 5-yearanalysis of the EORTC-NCIC trial Lancet Oncol 2009 10459ndash466
2 Lawrence TS Blackstock AW McGinn C The mechanism of actionof radiosensitization of conventional chemotherapeutic agentsSemin Radiat Oncol 2003 1313ndash21
3 Lesueur P Chevalier F Austry JB et al Poly-(ADP-ribose)-polymer-ase inhibitors as radiosensitizers a systematic review of pre-clinicaland clinical human studies Oncotarget 2017 8(40)69105ndash69124
4 Lester A Rapkins R Nixdorf S Khasraw M McDonald KCombining PARP inhibitors with radiation therapy for the treatmentof glioblastoma is PTEN predictive of response Clin Transl Oncol2017 19273ndash278
5 Gupta SK Kizilbash SH Carlson BL et al Delineation of MGMT hyper-methylation as a biomarker for veliparib-mediated temozolomide-sensi-tizing therapy of glioblastoma J Natl Cancer Inst 2016 108
6 Kleinberg LR Blakeley J Mikkelsen T et al An American BrainTumor Consortium (ABTC) phase 1 trial of veliparib (ABT-888)temozolomide (TMZ) and concurrent radiation therapy (RT) fornewly diagnosed glioblastoma multiforme (GBM) need for modifica-tion to approach for combining these therapies InternationalJ Radiat Oncol Biol Phys 2012 84S7ndashS8
7 Oronsky BT A Review of two promising radiosensitizers in brainmetastases Rrx-001 and 2-deoxyglucose In NC Oronsky edJ Cancer Sci Ther 2015 pp 137ndash141
8 Kim MM Parmar H Cao Y et al Concurrent whole brain radiother-apy and RRx-001 for melanoma brain metastases Neuro Onc2016 18455ndash456
9 Mehta MP Wang D Wang F et al Veliparib in combination withwhole brain radiation therapy in patients with brain metastasesresults of a phase 1 study J Neurooncol 2015 122409ndash417
10 Chabot P Hsia TC Ryu JS et al Veliparib in combination withwhole-brain radiation therapy for patients with brain metastasesfrom non-small cell lung cancer results of a randomized globalplacebo-controlled study J Neurooncol 2017 131105ndash115
11 Ochiai S Nomoto Y Yamashita Y et al Roles of valproic acid inimproving radiation therapy for glioblastoma a review of literaturefocusing on clinical evidence Asian Pac J Cancer Prev 201617463ndash466
12 Tan AC Heimberger AB Menzies AM Pavlakis N Khasraw MImmune checkpoint inhibitors for brain metastases Curr Oncol Rep2017 1938
13 DrsquoSouza NM Fang P Logan J Yang J Jiang W Li JCombining radiation therapy with immune checkpoint blockade
for central nervous system malignancies Frontiers Oncol 20166212
14 Parsa AT Waldron JS Panner A et al Loss of tumor suppressorPTEN function increases B7-H1 expression and immunoresistancein glioma Nat Med 2007 1384ndash88
15 Binder DC Davis AA Wainwright DA Immunotherapy for cancer inthe central nervous system current and future directionsOncoimmunology 2016 5e1082027
16 Newcomb EW Demaria S Lukyanov Y et al The combination ofionizing radiation and peripheral vaccination produces long-termsurvival of mice bearing established invasive GL261 gliomas ClinCancer Res 2006 124730ndash4737
17 Zeng J See AP Phallen J et al Anti-PD-1 blockade and stereotac-tic radiation produce long-term survival in mice with intracranial glio-mas Int J Radiat Oncol Biol Phys 2013 86343ndash349
18 Chow KK Hara W Lim M Li G Combining immunotherapy withradiation for the treatment of glioblastoma J Neurooncol2015123459ndash464
19 Belcaid Z Phallen JA Zeng J et al Focal radiation therapy com-bined with 4-1BB activation and CTLA-4 blockade yields long-termsurvival and a protective antigen-specific memory response in amurine glioma model PLoS One 2014 9e101764
20 Topalian SL Hodi FS Brahmer JR et al Safety activity and im-mune correlates of anti-PD-1 antibody in cancer N Engl J Med2012 3662443ndash2454
21 Bienkowski M Preusser M Prognostic role of tumour-infiltrating in-flammatory cells in brain tumours literature review Curr OpinNeurol 2015 28647ndash658
22 Harter PN Bernatz S Scholz A et al Distribution and prognostic rel-evance of tumor-infiltrating lymphocytes (TILs) and PD-1PD-L1 im-mune checkpoints in human brain metastases Oncotarget 2015640836ndash40849
23 Berghoff AS Ricken G Widhalm G et al Tumour-infiltrating lym-phocytes and expression of programmed death ligand 1 (PD-L1) inmelanoma brain metastases Histopathology 2015 66289ndash299
24 Silk AW Bassetti MF West BT Tsien CI Lao CD Ipilimumab and ra-diation therapy for melanoma brain metastases Cancer Med 20132899ndash906
25 Knisely JP Yu JB Flanigan J Sznol M Kluger HM Chiang VLRadiosurgery for melanoma brain metastases in the ipilimumab eraand the possibility of longer survival J Neurosurg 2012117227ndash233
26 Kiess AP Wolchok JD Barker CA et al Stereotactic radiosurgeryfor melanoma brain metastases in patients receiving ipilimumabsafety profile and efficacy of combined treatment Int J Radiat OncolBiol Phys 2015 92368ndash375
27 Qian JM Yu JB Kluger HM Chiang VL Timing and type of immunecheckpoint therapy affect the early radiographic response of mela-noma brain metastases to stereotactic radiosurgery Cancer 20161223051ndash3058
28 Silk AW Cao Y Gomez-Hassan D et al A randomized phase IIstudy of ipilimumab induction in patients with melanoma brain me-tastases receiving stereotactic radiosurgery J Clin Oncol 2015 33TPS9079ndashTPS9079
29 Neagu MR Reardon DA An Update on the role of immunotherapyand vaccine strategies for primary brain tumors Curr TreatOptions Oncol 2015 1654
30 Wen PY Reardon DA Phuphanich S et al A randomized double-blind placebo-controlled phase 2 trial of dendritic cell (DC) vaccina-tion with ICT-107 in newly diagnosed glioblastoma (GBM) patientsJ Clin Oncol 2014 322005ndash2005
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
114
British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

AbstractAdvances in radiosensitizers and immunotherapyhave ushered in a new frontier in brain tumortreatment The brain has often been viewed as asanctuary site due to the bloodndashbrain barrier andthus the 2 primary modalities of therapy includedsurgery and radiation therapy (RT) More recentlysystemic therapies have played a greater role aseither combination therapy radiosensitizers or im-munotherapy Two novel radiosensitizers are beingdeveloped for the treatment of brain metastasesRRx-001 for example is a small molecule thataccelerates the NO2 to NO conversion of deoxyhe-moglobin and the agent 2-dexoyglucose (2-DG) is anonmetabolized glucose analogue that interfereswith ATP formation Poly(ADP-ribose) DNA polymer-ase inhibitors are promising due to their distinctradiobiological effects Veliparib and olaparib areamong the most studied with randomized trialsexploring their use in gliomas and brain metastasesImmunotherapy including immune checkpoint inhib-itors may play a role for both primary gliomas andbrain metastases RT has been shown to enhancethe function of cytotoxic T lymphocytes induce infil-tration of cytotoxic T lymphocytes and enhancefunction Trials are presently exploring use of bothprogrammed cell death protein (PD)1 and PD ligand1 blockade in glioblastoma patients with radiationSimilarly several immunotherapies are being investi-gated with either stereotactic radiosurgery or wholebrain radiation therapy for brain metastases In thisreview the use of radiosensitizers and immunother-apy agents with RT will be discussed broadly
Keywords brain metastases brain tumors gliomasimmunotherapy radiation therapy radiosensitizers
Radiosensitizers andImmunotherapy inBrain TumorsAdvances in radiosensitizers and immunotherapy haveushered in a new frontier to brain tumor treatment Braintumors however are a diverse class sharing only similaranatomic location Both primary brain malignancies andbrain metastasis have widely diverse histologies and mo-lecular phenotypes With the bloodndashbrain barrier thebrain has often been viewed as a sanctuary site and thusthe 2 primary modalities of therapy included surgery andradiation with decreased benefit from systemic agentsdue to lack of brain penetration However more recentlysystemic therapies have played a greater role as eithercombination therapy radiosensitizers or immunother-apy While temozolomide (TMZ) has played a pivotal rolefor glioblastoma (GBM) only a subset of patients benefitfrom the treatment1 The use of alternative systemicagents that may potentiate the effects of radiation ther-apy (RT) is becoming increasingly appealing Similarly forbrain metastases a variety of systemic agents are beingexplored primarily based on histology and immune pro-file In this review the use of radiosensitizers and immu-notherapy agents currently under investigation with RTwill be discussed
RadiosensitizersThe guiding concept of radiation sensitization is to in-crease the biologic effect of radiation such as increasedDNA damage decreased DNA repair decreased hypoxiaor increased G2M cell cycle blockade leading to im-proved tumor control and increased patient survival2
Poly(adenosine diphosphate-ribose) DNA polymerase(PARP) inhibitors are promising radiosensitizers due totheir roles in DNA repair3 PARP inhibitors work againstPARP1 a nuclear enzyme involved in the recruitment ofrepair proteins used in base excision repair and single-strand break repair PARP1 may also play a role in nonho-mologous end-joining4 The primary investigation ofPARP inhibitors has been in potentiating radiation andchemotherapy effects the latter in the context of homolo-gous repair deficient tumors For radiation the primarymechanism of action is inducing damage to nucleotidesleading to single-strand and double-strand breaks ThusPARP inhibitors in combination with radiation have an ap-pealing mechanism to inhibit or delay DNA repair andlikely convert more single-strand breaks to double-strandbreaks4
While several PARP inhibitors are currently being evalu-ated in a variety of tumors including talazoparib and nira-parib veliparib and olaparib are among the most studiedand there are randomized trials exploring their use in
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
110
gliomas The US National Cancer Institute (NCI)ndashfundedAlliance for Clinical Trials in Oncology (Alliance) A071102is a randomized phase IIIII trial evaluating the use ofveliparib in combination with TMZ in the adjuvant settingin patients with GBM tumors exhibiting hypermethylationof the O6 methylguanine DNA methyltransferase (MGMT)gene promoter Preclinical data supporting this trial sug-gested that only patients with MGMT methylated tumorswould benefit from the combination a group of patientsfor whom TMZ concurrent with radiation might be mostbeneficial5 A phase I trial performed by the NCI-fundedAmerican Brain Tumor Consortium attempted to combineveliparib with radiation and TMZ but failed to identify asuitable recommended phase II dose due to significanthemotoxicity6 Thus attempts to combine radiation withveliparib have focused on patients least likely to benefitfrom TMZ namely with MGMT unmethylated tumors forwhom TMZ could be withheld The Australian VeliparibRT and TMZ trial in newly diagnosed unmethylatedMGMT glioblastoma (VERTU) is a single-arm study inwhich patients receive RT with veliparib followed by adju-vant TMZ and veliparib4
An ongoing novel approach to radiosensitize gliomasinvolves a combination with an agent that interferes withan essential metabolic process 2-Dexoyglucose (2-DG)is a nonmetabolized glucose analogue that acts as acompetitive inhibitor of glycolysis It is transported acrossthe bloodndashbrain barrier by the glucose transporter GLUT-1 and thus has good penetration into the CNSIntracellularly it is trapped and accumulates in cells simi-lar to the mechanism of 18-fluorodeoxyglucose 2-DG isphosphorylated by glycolytic enzymes and the
phosphorylated 2-DG (2-deoxyglucose-P) is trapped in-tracellularly Inhibition of hexokinase activity by 2-DGinterferes with ATP formation and results in tumor celldeath7 While it has positive attributes by selectively tar-geting metabolically active tumor cells 2-DG has alsobeen associated with Q-T prolongation The currentphase III trial in gliomas is assessing the toxicity and tol-erability of 2-DG with hypofractionated radiation of 5 Gyas a radiosensitizer7
Two novel radiosensitizers are being developed for thetreatment of brain metastases First RRx-001 is a smallmolecule initially designed by the aerospace industry Itworks in part as a radiosensitizer by increasing blood flowand thus oxygenation of tumors through nitric oxideRRx-001 which binds to hemoglobin accelerates theNO2 to NO conversion of deoxyhemoglobin It workslocally under hypoxic conditions and subsequentlythe radiosensitive effects through nitric oxide are invasodilation and inhibiting DNA repair enzymes8 Nitricoxide is relatively benign The higher levels of oxidativestress with H2O2 and superoxide in tumors in comparisonto normal tissues result in the preferential generation ofreactive peroxynitrite in the presence of higher nitric oxidelevels7 This accounts for the increased specificity anddecreased toxicity with RRx-001 The dose limiting toxic-ity in a phase I trial of 25 patients treated with eitherweekly or biweekly infusions was infusional pain relatedto the release of NO at the site of injection7 Outside ofpreclinical models 2 clinical reports examining wholebrain radiation therapy (WBRT) with RRx-001 reported anintracranial response A patient with melanoma and 2hemorrhagic edematous lesions of 26 cm and 33 cm
Table 1 Clinical trials involving immunotherapy and radiation therapy1213
Clinical Trials Number Phase Disease Type Treatment Groups
NCT02667587 II Newly diagnosed GBMMGMT-methylated
Nivolumabthorn TMZthorn RT vs placebothornTMZ thorn RT
NCT02617589 III Newly diagnosed GBM Nivolumabthorn RT vs TMZthorn RTNCT02336165 II Newly diagnosed unmethylated
MGMT recurrent glioblastomaMEDI4736thorn standard RT vs MEDI4736 thorn
bevacizumabNCT02530502 III Newly diagnosed GBM RTthorn TMZthorn pembrolizumab TMZthorn
pembrolizumabNCT02313272 I Recurrent glioma Hypofractionated stereotactic radiationthorn
pembrolizumab thorn bevacizumabNCT02696993 III Brain metastases Nivolumabthorn SRS nivolumabthornWBRT
nivolumabthorn ipilimumab thorn SRS nivolu-mabthorn ipilimumab thornWBRT
NCT02115139 II Melanoma brain metastases Ipilimumab thornWBRTNCT02097732 II Melanoma brain metastases Ipilimumab SRS ipilimumab vs SRS
ipilimumabNCT01703507 I Melanoma brain metastases Ipilimumab thornWBRT vs ipilimumab thorn SRSNCT02107755 II Melanoma brain metastases Ipilimumab thorn SRSNCT02858869 pilot Melanoma and NSCLC Pembrolizumabthorn SRSNCT01950195 I Melanoma brain metastases Ipilimumab thorn SRSNCT02662725 II Melanoma brain metastases Ipilimumab thorn SRS
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
111
after a single intravenous dose of RRx-001 of 5 mgm2 4days before WBRT resulted in symptomatic improvementwithin 48 hours By 4 months after radiation there was areduction in size in the largest dimension down to 10 cmand 23 cm of the respective lesions A second report of amelanoma patient with at least 18 lesions after receivingRRx-001 of 5 mgm2 4 days before WBRT as well astwice weekly doses during the 2 weeks of radiation alsoshowed response The patient at 4 months had disap-pearance of 13 of 18 lesions with shrinkage of theremaining 5 lesions8 Presently BRAINSTORM is a phaseIII dose escalation trial of RRx-001 designed to be ad-ministered twice weekly for 2 weeks with WBRT (30 Gy in10 fractions) with the option for weekly maintenance8
Veliparib has also been evaluated in the setting of brainmetastases It was tested in a global randomized con-trolled trial with WBRT Veliparib is orally bioavailable andcrosses the bloodndashbrain barrier It was first examined in amultihistology phase I trial in patients with nonndashsmall celllung cancer (NSCLC) breast cancer melanoma and re-nal and colorectal cancers among others The study of81 patients tested dose tolerance of veliparib from 10 to300 mg orally twice a day with WBRT to 30 Gy in 10 frac-tions or 375 Gy in 15 fractions9 The phase I trial dose es-calation portion did not reach the predefined criteria forthe maximum tolerated dose but there was amplificationof the adverse effects of nausea and vomiting among thehighest dose cohort of 300 mg bid9 The adverse eventprofile at 200 mg bid was similar to that of WBRT aloneDoses of veliparib from 20 to 200 mg bid demonstratesimilar antitumor activity and other studies in preclinicalmodels found that 50 mg daily demonstrated significantreduction in poly(ADP-ribose) in peripheral blood mono-nuclear cells and tumor tissue while also effectivelycrossing the bloodndashbrain barrier Thus the subsequentphase II trial examined 50 mg with WBRT9 In order to as-sess a more homogeneous cohort the phase III globalrandomized trial studied only NSCLC at the 2 doses of50 mg and 200 mg twice daily versus placebo twice a daywith WBRT10 The primary endpoint was overall survivalIn 307 patients in a 111 randomization of 50 mg bid200 mg bid or placebo twice daily the study found nosignificant differences in overall survival among the differ-ent groups10 The majority of patients across the treat-ment groups had a graded prognostic assessment (GPA)score of25 and a Karnofsky performance status ofgt80 The median overall survival was 185 days forpatients receiving placebo and 209 days for those receiv-ing veliparib without any statistically significant differ-ence These results were similar to the disease-specificestimate of median survival for the disease-specific GPAof NSCLC patients with brain metastases10
Several other radiosensitizers have failed to improve overradiation alone in a number of trials These have includedtrials with WBRT including motexafin gadolinium efap-roxyn bortozemib thalidomide teniposide topotecanpaclitaxel and cisplatin7 Of note other PARP inhibitorsalso being assessed include talazoparib and niraparib4
which may yield positive results The use of valproic acid(VPA) as a histone deacetylase inhibitor has also beenconsidered to have radiosensitizing potential in additionto its anti-epileptic drug properties11 While studies havereported that patients with GBM receiving an anti-epilep-tic agent may have higher overall survival than those re-ceiving standard chemoradiation therapy alone thebenefit remains controversial Retrospective analysissuggested that patients taking VPA specifically had bettersurvival in comparison to other anti-epileptic drugs Alsoa recent prospective phase II trial was performed in 37patients with GBM receiving VPA 25 mgkg concurrentlywith TMZ chemoradiation and reported a median survivalof 296 months While controversial further data andinvestigation are needed into this and other agents thatmay potentiate RT
Immunotherapy and radiationImmune checkpoint inhibitors lead to activation of T cellswhich may traffic across the bloodndashbrain barrier to inter-act with tumor Primary brain tumors may evade the im-mune system through upregulation of immunecheckpoints and possible immunosuppression12
Monoclonal antibodies promote immune-mediated anti-tumor activity by inhibiting the immune functionndashmediated cytotoxic T-lymphocyte associated protein 4(CTLA-4) and programmed cell death protein 1 (PD-1)receptors PD protein ligand (PD-L1) is upregulated inGBM through oncogenic signaling possibly throughphosphatase and tensin homolog loss and interleukin-10signaling1314 RT has also been shown to enhance thefunction of cytotoxic T lymphocytes RT may induce aninfiltration of cytotoxic T lymphocytes and enhance theirfunction It may also induce antindashCTLA-4 agents inhibitingT-cell function and increasing the CD8thorn T cellregulatoryT cell ratio in cases of melanoma15 Thus PD-1 and PD-L1 blockers may have a further role in CNS managementwith the use of radiation
In preclinical models radiation has been examined withimmunotherapy that included among other mechanismsvaccination PD-1 blockade and CTLA-4 blockade Inmice radiation plus a vaccination of irradiated gliomacells was associated with increased survival of 40 to80 compared with 0 to 10 for other groups stud-ied16 A benefit of PD-1 blockade with stereotactic radio-surgery (SRS) specifically has also been shown in amouse model In comparison to mice treated with radia-tion antindashPD-1 therapy or a combination only those re-ceiving combination therapy had a higher percentagesurvival alive beyond 180 days after treatment17 Othermouse carcinoma models have identified response withanti-CTLA antibody and fractionated radiation therapy18
CD137 activation CTLA-4 blockade and focal radiationtherapy have been examined in an immunocompetent in-tracranial GBM model Mice treated with triple combina-tion therapy had 50 greater survival19 In other murine
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
112
models the use of antindashPD-1 and antindashCTLA-4 agentsshowed improved survival and increased tumor infiltratingleukocyte populations compared with single modalitywith concurrent radiation16 There are conflicting data re-garding timing or sequencing of therapy with some ani-mal models showing no difference in tumor response inrelation to timing of RT and delivery of immunotherapy18
For instance in one animal model CTLA-4 blockade de-livered simultaneously with radiation or delivered a coupleof days after showed no difference in survival among themice19
Increased PD-1 expression in circulating monocytes hasbeen identified as a biomarker for tumor-induced immu-nosuppression and may serve as a prognostic factor forpotentially worse survival outcomes in clinic13 In onestudy GBM patients with lower PD-L1 expression hadhigher median overall survival than those with higher PD-L1 expression suggesting that lower expression may beassociated with less immunosuppression and more im-mune activity against the tumor glioma20 RT with immunecheckpoint blockade is being investigated to assess if theaddition of PD-1 and PD-L1 inhibitors may improve theoutcomes or toxicity profile of standard therapy For in-stance a multi-institutional trial opened as a phase III willevaluate outcomes in GBM receiving radiation and pem-brolizumab with TMZ (NCT02530502) Next durvalumabor MEDI4736 a PD-L1 inhibitor is being examined forunmethylated MGMT GBMs with standard radiotherapy(NCT02336165)12 The impact of checkpoint inhibitorsduring adjuvant treatment of GBM is currently beingevaluated in the NCI-funded NRG-BN002 trial(NCT02311920) which will evaluate the antindashCTLA-4antibody ipilimumab alone or in combination with theantindashPD-1 antibody nivolumab for patients with newlydiagnosed GBM
Brain metastases have clonal populations of cells differ-ent from the rest of the brain and a unique microenviron-ment that may influence immunotherapy There may bemore immune infiltrates in metastases than in primarybrain tumors21 PD-L1 expression in brain metastasesvaries by histology In a series evaluating PD-L1 expres-sion in various tumors including melanoma NSCLCbreast renal colorectal and small cell less than 10showed significant expression22 There was greatest ex-pression among NSCLC and melanoma with a correla-tion between PD-L1 expression and tumor infiltratinglymphocytes22 Institutional series have examined thecombination of radiation and immune checkpoint block-ade In another study specific to melanoma brain metas-tases PD-L1 expression was found in over 50 of thecases and among those cases over 40 expressedPD-L1 in more than 5 of tumor cells23 The largest bodyof data for use of PD-L1 with radiation is for melanomaand NSCLC
Ipilimumab is a human monoclonal antibody that blocksCTLA-4 and allows for T-cell activation and proliferationto enhance the immune response to cancer In a
retrospective review of 70 patients with brain metastasestreated with SRS or WBRT the 33 patients receiving im-munotherapy had a median survival of 183 months incomparison to the 37 patients who did not receive ipili-mumab with a median survival of 53 months While therewere limited data among the cohort to evaluate sequenc-ing of therapy among 10 evaluable patients 40 whoreceived ipilimumab prior to RT had a partial response incomparison to only 10 among the cohort of 22 evalu-able patients who did not receive ipilimumab therapy atall with radiation24 Another retrospective institutionalstudy of 77 patients in which 37 received ipilimumabfound that patients treated with SRS and ipilimumab hada median survival of 213 months versus 49 months forthose not receiving ipilimumab Most interestingly theyidentified that the correlation remained significant evenafter adjusting for additional factors such as performancestatus Secondly there was not an increased need for useof salvage WBRT25
The sequencing of radiotherapy and immune checkpointinhibitors is of interest In a study of patients with brainmetastases the one-year survival for patients receivingSRS before ipilimumab was greater at 65 in contrast to56 for those receiving it concurrently and 40 for thosereceiving it after SRS26 Similarly another study of 75patients with 566 brain metastases showed greater tu-mor lesion response at 6 months from SRS for patientsreceiving ipilimumab nivolumab or pembrolizumabwithin 4 weeks of their SRS27 Those receiving concurrenttherapy had by 6 months a decrease of 949 in compar-ison to 662 for those not receiving checkpoint inhibi-tors within 4 weeks Prospective clinical trials areinvestigating different combinations of RT with immunecheckpoint blockers in this setting For instance new tri-als are currently evaluating intracranial tumor control at 6months and the timing of immune therapy or immunecheckpoint inhibitors in relation to SRS28
Vaccines are also being developed for primary braintumors showing some evidence for their use Vaccinesdeveloped from dendritic cells and tumor lysate with tu-mor antigens such as the epidermal growth factor recep-tor variant III vaccine have shown promise29 Forinstance in a placebo controlled phase II trial of ICT-107a vaccine composed on autologous dendritic cells andtumor antigens progression-free survival was increasedby 2 months for those receiving the vaccine30 Radiationmay assist in serving as a primer for the immunogeniceffects by facilitating tumor antigen uptake by dendriticcells and cross presentation on major histocompatibilitycomplex I Thus RT may assist in the tumor-specific cy-totoxic T lymphocytes associated with the immunemechanism
In conclusion although there may be challenges to com-bining and sequencing brain tumors radiosensitizersand immunotherapy the opportunities and potential fornovel applications are promising For brain tumors brainmetastases are typically underrepresented in trials
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
113
despite being among the most common intracraniallesions Despite their large population patients with brainmetastases are often excluded from clinical trials withnovel agents due to concerns regarding confounding out-comes and tolerability12 Primary gliomas also offer anovel frontier for the use of immunotherapy to standardadjuvant chemotherapy and radiation particularly forpatients with GBM less likely to respond to TMZ such aswith unmethylated MGMT As studies work to define therole of RT and radiosensitizers and immunotherapy fur-ther analysis is needed to assess the timing of RT andthese treatments
References
1 Stupp R Hegi ME Mason WP et al Effects of radiotherapy withconcomitant and adjuvant temozolomide versus radiotherapy aloneon survival in glioblastoma in a randomised phase III study 5-yearanalysis of the EORTC-NCIC trial Lancet Oncol 2009 10459ndash466
2 Lawrence TS Blackstock AW McGinn C The mechanism of actionof radiosensitization of conventional chemotherapeutic agentsSemin Radiat Oncol 2003 1313ndash21
3 Lesueur P Chevalier F Austry JB et al Poly-(ADP-ribose)-polymer-ase inhibitors as radiosensitizers a systematic review of pre-clinicaland clinical human studies Oncotarget 2017 8(40)69105ndash69124
4 Lester A Rapkins R Nixdorf S Khasraw M McDonald KCombining PARP inhibitors with radiation therapy for the treatmentof glioblastoma is PTEN predictive of response Clin Transl Oncol2017 19273ndash278
5 Gupta SK Kizilbash SH Carlson BL et al Delineation of MGMT hyper-methylation as a biomarker for veliparib-mediated temozolomide-sensi-tizing therapy of glioblastoma J Natl Cancer Inst 2016 108
6 Kleinberg LR Blakeley J Mikkelsen T et al An American BrainTumor Consortium (ABTC) phase 1 trial of veliparib (ABT-888)temozolomide (TMZ) and concurrent radiation therapy (RT) fornewly diagnosed glioblastoma multiforme (GBM) need for modifica-tion to approach for combining these therapies InternationalJ Radiat Oncol Biol Phys 2012 84S7ndashS8
7 Oronsky BT A Review of two promising radiosensitizers in brainmetastases Rrx-001 and 2-deoxyglucose In NC Oronsky edJ Cancer Sci Ther 2015 pp 137ndash141
8 Kim MM Parmar H Cao Y et al Concurrent whole brain radiother-apy and RRx-001 for melanoma brain metastases Neuro Onc2016 18455ndash456
9 Mehta MP Wang D Wang F et al Veliparib in combination withwhole brain radiation therapy in patients with brain metastasesresults of a phase 1 study J Neurooncol 2015 122409ndash417
10 Chabot P Hsia TC Ryu JS et al Veliparib in combination withwhole-brain radiation therapy for patients with brain metastasesfrom non-small cell lung cancer results of a randomized globalplacebo-controlled study J Neurooncol 2017 131105ndash115
11 Ochiai S Nomoto Y Yamashita Y et al Roles of valproic acid inimproving radiation therapy for glioblastoma a review of literaturefocusing on clinical evidence Asian Pac J Cancer Prev 201617463ndash466
12 Tan AC Heimberger AB Menzies AM Pavlakis N Khasraw MImmune checkpoint inhibitors for brain metastases Curr Oncol Rep2017 1938
13 DrsquoSouza NM Fang P Logan J Yang J Jiang W Li JCombining radiation therapy with immune checkpoint blockade
for central nervous system malignancies Frontiers Oncol 20166212
14 Parsa AT Waldron JS Panner A et al Loss of tumor suppressorPTEN function increases B7-H1 expression and immunoresistancein glioma Nat Med 2007 1384ndash88
15 Binder DC Davis AA Wainwright DA Immunotherapy for cancer inthe central nervous system current and future directionsOncoimmunology 2016 5e1082027
16 Newcomb EW Demaria S Lukyanov Y et al The combination ofionizing radiation and peripheral vaccination produces long-termsurvival of mice bearing established invasive GL261 gliomas ClinCancer Res 2006 124730ndash4737
17 Zeng J See AP Phallen J et al Anti-PD-1 blockade and stereotac-tic radiation produce long-term survival in mice with intracranial glio-mas Int J Radiat Oncol Biol Phys 2013 86343ndash349
18 Chow KK Hara W Lim M Li G Combining immunotherapy withradiation for the treatment of glioblastoma J Neurooncol2015123459ndash464
19 Belcaid Z Phallen JA Zeng J et al Focal radiation therapy com-bined with 4-1BB activation and CTLA-4 blockade yields long-termsurvival and a protective antigen-specific memory response in amurine glioma model PLoS One 2014 9e101764
20 Topalian SL Hodi FS Brahmer JR et al Safety activity and im-mune correlates of anti-PD-1 antibody in cancer N Engl J Med2012 3662443ndash2454
21 Bienkowski M Preusser M Prognostic role of tumour-infiltrating in-flammatory cells in brain tumours literature review Curr OpinNeurol 2015 28647ndash658
22 Harter PN Bernatz S Scholz A et al Distribution and prognostic rel-evance of tumor-infiltrating lymphocytes (TILs) and PD-1PD-L1 im-mune checkpoints in human brain metastases Oncotarget 2015640836ndash40849
23 Berghoff AS Ricken G Widhalm G et al Tumour-infiltrating lym-phocytes and expression of programmed death ligand 1 (PD-L1) inmelanoma brain metastases Histopathology 2015 66289ndash299
24 Silk AW Bassetti MF West BT Tsien CI Lao CD Ipilimumab and ra-diation therapy for melanoma brain metastases Cancer Med 20132899ndash906
25 Knisely JP Yu JB Flanigan J Sznol M Kluger HM Chiang VLRadiosurgery for melanoma brain metastases in the ipilimumab eraand the possibility of longer survival J Neurosurg 2012117227ndash233
26 Kiess AP Wolchok JD Barker CA et al Stereotactic radiosurgeryfor melanoma brain metastases in patients receiving ipilimumabsafety profile and efficacy of combined treatment Int J Radiat OncolBiol Phys 2015 92368ndash375
27 Qian JM Yu JB Kluger HM Chiang VL Timing and type of immunecheckpoint therapy affect the early radiographic response of mela-noma brain metastases to stereotactic radiosurgery Cancer 20161223051ndash3058
28 Silk AW Cao Y Gomez-Hassan D et al A randomized phase IIstudy of ipilimumab induction in patients with melanoma brain me-tastases receiving stereotactic radiosurgery J Clin Oncol 2015 33TPS9079ndashTPS9079
29 Neagu MR Reardon DA An Update on the role of immunotherapyand vaccine strategies for primary brain tumors Curr TreatOptions Oncol 2015 1654
30 Wen PY Reardon DA Phuphanich S et al A randomized double-blind placebo-controlled phase 2 trial of dendritic cell (DC) vaccina-tion with ICT-107 in newly diagnosed glioblastoma (GBM) patientsJ Clin Oncol 2014 322005ndash2005
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
114
British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

gliomas The US National Cancer Institute (NCI)ndashfundedAlliance for Clinical Trials in Oncology (Alliance) A071102is a randomized phase IIIII trial evaluating the use ofveliparib in combination with TMZ in the adjuvant settingin patients with GBM tumors exhibiting hypermethylationof the O6 methylguanine DNA methyltransferase (MGMT)gene promoter Preclinical data supporting this trial sug-gested that only patients with MGMT methylated tumorswould benefit from the combination a group of patientsfor whom TMZ concurrent with radiation might be mostbeneficial5 A phase I trial performed by the NCI-fundedAmerican Brain Tumor Consortium attempted to combineveliparib with radiation and TMZ but failed to identify asuitable recommended phase II dose due to significanthemotoxicity6 Thus attempts to combine radiation withveliparib have focused on patients least likely to benefitfrom TMZ namely with MGMT unmethylated tumors forwhom TMZ could be withheld The Australian VeliparibRT and TMZ trial in newly diagnosed unmethylatedMGMT glioblastoma (VERTU) is a single-arm study inwhich patients receive RT with veliparib followed by adju-vant TMZ and veliparib4
An ongoing novel approach to radiosensitize gliomasinvolves a combination with an agent that interferes withan essential metabolic process 2-Dexoyglucose (2-DG)is a nonmetabolized glucose analogue that acts as acompetitive inhibitor of glycolysis It is transported acrossthe bloodndashbrain barrier by the glucose transporter GLUT-1 and thus has good penetration into the CNSIntracellularly it is trapped and accumulates in cells simi-lar to the mechanism of 18-fluorodeoxyglucose 2-DG isphosphorylated by glycolytic enzymes and the
phosphorylated 2-DG (2-deoxyglucose-P) is trapped in-tracellularly Inhibition of hexokinase activity by 2-DGinterferes with ATP formation and results in tumor celldeath7 While it has positive attributes by selectively tar-geting metabolically active tumor cells 2-DG has alsobeen associated with Q-T prolongation The currentphase III trial in gliomas is assessing the toxicity and tol-erability of 2-DG with hypofractionated radiation of 5 Gyas a radiosensitizer7
Two novel radiosensitizers are being developed for thetreatment of brain metastases First RRx-001 is a smallmolecule initially designed by the aerospace industry Itworks in part as a radiosensitizer by increasing blood flowand thus oxygenation of tumors through nitric oxideRRx-001 which binds to hemoglobin accelerates theNO2 to NO conversion of deoxyhemoglobin It workslocally under hypoxic conditions and subsequentlythe radiosensitive effects through nitric oxide are invasodilation and inhibiting DNA repair enzymes8 Nitricoxide is relatively benign The higher levels of oxidativestress with H2O2 and superoxide in tumors in comparisonto normal tissues result in the preferential generation ofreactive peroxynitrite in the presence of higher nitric oxidelevels7 This accounts for the increased specificity anddecreased toxicity with RRx-001 The dose limiting toxic-ity in a phase I trial of 25 patients treated with eitherweekly or biweekly infusions was infusional pain relatedto the release of NO at the site of injection7 Outside ofpreclinical models 2 clinical reports examining wholebrain radiation therapy (WBRT) with RRx-001 reported anintracranial response A patient with melanoma and 2hemorrhagic edematous lesions of 26 cm and 33 cm
Table 1 Clinical trials involving immunotherapy and radiation therapy1213
Clinical Trials Number Phase Disease Type Treatment Groups
NCT02667587 II Newly diagnosed GBMMGMT-methylated
Nivolumabthorn TMZthorn RT vs placebothornTMZ thorn RT
NCT02617589 III Newly diagnosed GBM Nivolumabthorn RT vs TMZthorn RTNCT02336165 II Newly diagnosed unmethylated
MGMT recurrent glioblastomaMEDI4736thorn standard RT vs MEDI4736 thorn
bevacizumabNCT02530502 III Newly diagnosed GBM RTthorn TMZthorn pembrolizumab TMZthorn
pembrolizumabNCT02313272 I Recurrent glioma Hypofractionated stereotactic radiationthorn
pembrolizumab thorn bevacizumabNCT02696993 III Brain metastases Nivolumabthorn SRS nivolumabthornWBRT
nivolumabthorn ipilimumab thorn SRS nivolu-mabthorn ipilimumab thornWBRT
NCT02115139 II Melanoma brain metastases Ipilimumab thornWBRTNCT02097732 II Melanoma brain metastases Ipilimumab SRS ipilimumab vs SRS
ipilimumabNCT01703507 I Melanoma brain metastases Ipilimumab thornWBRT vs ipilimumab thorn SRSNCT02107755 II Melanoma brain metastases Ipilimumab thorn SRSNCT02858869 pilot Melanoma and NSCLC Pembrolizumabthorn SRSNCT01950195 I Melanoma brain metastases Ipilimumab thorn SRSNCT02662725 II Melanoma brain metastases Ipilimumab thorn SRS
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
111
after a single intravenous dose of RRx-001 of 5 mgm2 4days before WBRT resulted in symptomatic improvementwithin 48 hours By 4 months after radiation there was areduction in size in the largest dimension down to 10 cmand 23 cm of the respective lesions A second report of amelanoma patient with at least 18 lesions after receivingRRx-001 of 5 mgm2 4 days before WBRT as well astwice weekly doses during the 2 weeks of radiation alsoshowed response The patient at 4 months had disap-pearance of 13 of 18 lesions with shrinkage of theremaining 5 lesions8 Presently BRAINSTORM is a phaseIII dose escalation trial of RRx-001 designed to be ad-ministered twice weekly for 2 weeks with WBRT (30 Gy in10 fractions) with the option for weekly maintenance8
Veliparib has also been evaluated in the setting of brainmetastases It was tested in a global randomized con-trolled trial with WBRT Veliparib is orally bioavailable andcrosses the bloodndashbrain barrier It was first examined in amultihistology phase I trial in patients with nonndashsmall celllung cancer (NSCLC) breast cancer melanoma and re-nal and colorectal cancers among others The study of81 patients tested dose tolerance of veliparib from 10 to300 mg orally twice a day with WBRT to 30 Gy in 10 frac-tions or 375 Gy in 15 fractions9 The phase I trial dose es-calation portion did not reach the predefined criteria forthe maximum tolerated dose but there was amplificationof the adverse effects of nausea and vomiting among thehighest dose cohort of 300 mg bid9 The adverse eventprofile at 200 mg bid was similar to that of WBRT aloneDoses of veliparib from 20 to 200 mg bid demonstratesimilar antitumor activity and other studies in preclinicalmodels found that 50 mg daily demonstrated significantreduction in poly(ADP-ribose) in peripheral blood mono-nuclear cells and tumor tissue while also effectivelycrossing the bloodndashbrain barrier Thus the subsequentphase II trial examined 50 mg with WBRT9 In order to as-sess a more homogeneous cohort the phase III globalrandomized trial studied only NSCLC at the 2 doses of50 mg and 200 mg twice daily versus placebo twice a daywith WBRT10 The primary endpoint was overall survivalIn 307 patients in a 111 randomization of 50 mg bid200 mg bid or placebo twice daily the study found nosignificant differences in overall survival among the differ-ent groups10 The majority of patients across the treat-ment groups had a graded prognostic assessment (GPA)score of25 and a Karnofsky performance status ofgt80 The median overall survival was 185 days forpatients receiving placebo and 209 days for those receiv-ing veliparib without any statistically significant differ-ence These results were similar to the disease-specificestimate of median survival for the disease-specific GPAof NSCLC patients with brain metastases10
Several other radiosensitizers have failed to improve overradiation alone in a number of trials These have includedtrials with WBRT including motexafin gadolinium efap-roxyn bortozemib thalidomide teniposide topotecanpaclitaxel and cisplatin7 Of note other PARP inhibitorsalso being assessed include talazoparib and niraparib4
which may yield positive results The use of valproic acid(VPA) as a histone deacetylase inhibitor has also beenconsidered to have radiosensitizing potential in additionto its anti-epileptic drug properties11 While studies havereported that patients with GBM receiving an anti-epilep-tic agent may have higher overall survival than those re-ceiving standard chemoradiation therapy alone thebenefit remains controversial Retrospective analysissuggested that patients taking VPA specifically had bettersurvival in comparison to other anti-epileptic drugs Alsoa recent prospective phase II trial was performed in 37patients with GBM receiving VPA 25 mgkg concurrentlywith TMZ chemoradiation and reported a median survivalof 296 months While controversial further data andinvestigation are needed into this and other agents thatmay potentiate RT
Immunotherapy and radiationImmune checkpoint inhibitors lead to activation of T cellswhich may traffic across the bloodndashbrain barrier to inter-act with tumor Primary brain tumors may evade the im-mune system through upregulation of immunecheckpoints and possible immunosuppression12
Monoclonal antibodies promote immune-mediated anti-tumor activity by inhibiting the immune functionndashmediated cytotoxic T-lymphocyte associated protein 4(CTLA-4) and programmed cell death protein 1 (PD-1)receptors PD protein ligand (PD-L1) is upregulated inGBM through oncogenic signaling possibly throughphosphatase and tensin homolog loss and interleukin-10signaling1314 RT has also been shown to enhance thefunction of cytotoxic T lymphocytes RT may induce aninfiltration of cytotoxic T lymphocytes and enhance theirfunction It may also induce antindashCTLA-4 agents inhibitingT-cell function and increasing the CD8thorn T cellregulatoryT cell ratio in cases of melanoma15 Thus PD-1 and PD-L1 blockers may have a further role in CNS managementwith the use of radiation
In preclinical models radiation has been examined withimmunotherapy that included among other mechanismsvaccination PD-1 blockade and CTLA-4 blockade Inmice radiation plus a vaccination of irradiated gliomacells was associated with increased survival of 40 to80 compared with 0 to 10 for other groups stud-ied16 A benefit of PD-1 blockade with stereotactic radio-surgery (SRS) specifically has also been shown in amouse model In comparison to mice treated with radia-tion antindashPD-1 therapy or a combination only those re-ceiving combination therapy had a higher percentagesurvival alive beyond 180 days after treatment17 Othermouse carcinoma models have identified response withanti-CTLA antibody and fractionated radiation therapy18
CD137 activation CTLA-4 blockade and focal radiationtherapy have been examined in an immunocompetent in-tracranial GBM model Mice treated with triple combina-tion therapy had 50 greater survival19 In other murine
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
112
models the use of antindashPD-1 and antindashCTLA-4 agentsshowed improved survival and increased tumor infiltratingleukocyte populations compared with single modalitywith concurrent radiation16 There are conflicting data re-garding timing or sequencing of therapy with some ani-mal models showing no difference in tumor response inrelation to timing of RT and delivery of immunotherapy18
For instance in one animal model CTLA-4 blockade de-livered simultaneously with radiation or delivered a coupleof days after showed no difference in survival among themice19
Increased PD-1 expression in circulating monocytes hasbeen identified as a biomarker for tumor-induced immu-nosuppression and may serve as a prognostic factor forpotentially worse survival outcomes in clinic13 In onestudy GBM patients with lower PD-L1 expression hadhigher median overall survival than those with higher PD-L1 expression suggesting that lower expression may beassociated with less immunosuppression and more im-mune activity against the tumor glioma20 RT with immunecheckpoint blockade is being investigated to assess if theaddition of PD-1 and PD-L1 inhibitors may improve theoutcomes or toxicity profile of standard therapy For in-stance a multi-institutional trial opened as a phase III willevaluate outcomes in GBM receiving radiation and pem-brolizumab with TMZ (NCT02530502) Next durvalumabor MEDI4736 a PD-L1 inhibitor is being examined forunmethylated MGMT GBMs with standard radiotherapy(NCT02336165)12 The impact of checkpoint inhibitorsduring adjuvant treatment of GBM is currently beingevaluated in the NCI-funded NRG-BN002 trial(NCT02311920) which will evaluate the antindashCTLA-4antibody ipilimumab alone or in combination with theantindashPD-1 antibody nivolumab for patients with newlydiagnosed GBM
Brain metastases have clonal populations of cells differ-ent from the rest of the brain and a unique microenviron-ment that may influence immunotherapy There may bemore immune infiltrates in metastases than in primarybrain tumors21 PD-L1 expression in brain metastasesvaries by histology In a series evaluating PD-L1 expres-sion in various tumors including melanoma NSCLCbreast renal colorectal and small cell less than 10showed significant expression22 There was greatest ex-pression among NSCLC and melanoma with a correla-tion between PD-L1 expression and tumor infiltratinglymphocytes22 Institutional series have examined thecombination of radiation and immune checkpoint block-ade In another study specific to melanoma brain metas-tases PD-L1 expression was found in over 50 of thecases and among those cases over 40 expressedPD-L1 in more than 5 of tumor cells23 The largest bodyof data for use of PD-L1 with radiation is for melanomaand NSCLC
Ipilimumab is a human monoclonal antibody that blocksCTLA-4 and allows for T-cell activation and proliferationto enhance the immune response to cancer In a
retrospective review of 70 patients with brain metastasestreated with SRS or WBRT the 33 patients receiving im-munotherapy had a median survival of 183 months incomparison to the 37 patients who did not receive ipili-mumab with a median survival of 53 months While therewere limited data among the cohort to evaluate sequenc-ing of therapy among 10 evaluable patients 40 whoreceived ipilimumab prior to RT had a partial response incomparison to only 10 among the cohort of 22 evalu-able patients who did not receive ipilimumab therapy atall with radiation24 Another retrospective institutionalstudy of 77 patients in which 37 received ipilimumabfound that patients treated with SRS and ipilimumab hada median survival of 213 months versus 49 months forthose not receiving ipilimumab Most interestingly theyidentified that the correlation remained significant evenafter adjusting for additional factors such as performancestatus Secondly there was not an increased need for useof salvage WBRT25
The sequencing of radiotherapy and immune checkpointinhibitors is of interest In a study of patients with brainmetastases the one-year survival for patients receivingSRS before ipilimumab was greater at 65 in contrast to56 for those receiving it concurrently and 40 for thosereceiving it after SRS26 Similarly another study of 75patients with 566 brain metastases showed greater tu-mor lesion response at 6 months from SRS for patientsreceiving ipilimumab nivolumab or pembrolizumabwithin 4 weeks of their SRS27 Those receiving concurrenttherapy had by 6 months a decrease of 949 in compar-ison to 662 for those not receiving checkpoint inhibi-tors within 4 weeks Prospective clinical trials areinvestigating different combinations of RT with immunecheckpoint blockers in this setting For instance new tri-als are currently evaluating intracranial tumor control at 6months and the timing of immune therapy or immunecheckpoint inhibitors in relation to SRS28
Vaccines are also being developed for primary braintumors showing some evidence for their use Vaccinesdeveloped from dendritic cells and tumor lysate with tu-mor antigens such as the epidermal growth factor recep-tor variant III vaccine have shown promise29 Forinstance in a placebo controlled phase II trial of ICT-107a vaccine composed on autologous dendritic cells andtumor antigens progression-free survival was increasedby 2 months for those receiving the vaccine30 Radiationmay assist in serving as a primer for the immunogeniceffects by facilitating tumor antigen uptake by dendriticcells and cross presentation on major histocompatibilitycomplex I Thus RT may assist in the tumor-specific cy-totoxic T lymphocytes associated with the immunemechanism
In conclusion although there may be challenges to com-bining and sequencing brain tumors radiosensitizersand immunotherapy the opportunities and potential fornovel applications are promising For brain tumors brainmetastases are typically underrepresented in trials
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
113
despite being among the most common intracraniallesions Despite their large population patients with brainmetastases are often excluded from clinical trials withnovel agents due to concerns regarding confounding out-comes and tolerability12 Primary gliomas also offer anovel frontier for the use of immunotherapy to standardadjuvant chemotherapy and radiation particularly forpatients with GBM less likely to respond to TMZ such aswith unmethylated MGMT As studies work to define therole of RT and radiosensitizers and immunotherapy fur-ther analysis is needed to assess the timing of RT andthese treatments
References
1 Stupp R Hegi ME Mason WP et al Effects of radiotherapy withconcomitant and adjuvant temozolomide versus radiotherapy aloneon survival in glioblastoma in a randomised phase III study 5-yearanalysis of the EORTC-NCIC trial Lancet Oncol 2009 10459ndash466
2 Lawrence TS Blackstock AW McGinn C The mechanism of actionof radiosensitization of conventional chemotherapeutic agentsSemin Radiat Oncol 2003 1313ndash21
3 Lesueur P Chevalier F Austry JB et al Poly-(ADP-ribose)-polymer-ase inhibitors as radiosensitizers a systematic review of pre-clinicaland clinical human studies Oncotarget 2017 8(40)69105ndash69124
4 Lester A Rapkins R Nixdorf S Khasraw M McDonald KCombining PARP inhibitors with radiation therapy for the treatmentof glioblastoma is PTEN predictive of response Clin Transl Oncol2017 19273ndash278
5 Gupta SK Kizilbash SH Carlson BL et al Delineation of MGMT hyper-methylation as a biomarker for veliparib-mediated temozolomide-sensi-tizing therapy of glioblastoma J Natl Cancer Inst 2016 108
6 Kleinberg LR Blakeley J Mikkelsen T et al An American BrainTumor Consortium (ABTC) phase 1 trial of veliparib (ABT-888)temozolomide (TMZ) and concurrent radiation therapy (RT) fornewly diagnosed glioblastoma multiforme (GBM) need for modifica-tion to approach for combining these therapies InternationalJ Radiat Oncol Biol Phys 2012 84S7ndashS8
7 Oronsky BT A Review of two promising radiosensitizers in brainmetastases Rrx-001 and 2-deoxyglucose In NC Oronsky edJ Cancer Sci Ther 2015 pp 137ndash141
8 Kim MM Parmar H Cao Y et al Concurrent whole brain radiother-apy and RRx-001 for melanoma brain metastases Neuro Onc2016 18455ndash456
9 Mehta MP Wang D Wang F et al Veliparib in combination withwhole brain radiation therapy in patients with brain metastasesresults of a phase 1 study J Neurooncol 2015 122409ndash417
10 Chabot P Hsia TC Ryu JS et al Veliparib in combination withwhole-brain radiation therapy for patients with brain metastasesfrom non-small cell lung cancer results of a randomized globalplacebo-controlled study J Neurooncol 2017 131105ndash115
11 Ochiai S Nomoto Y Yamashita Y et al Roles of valproic acid inimproving radiation therapy for glioblastoma a review of literaturefocusing on clinical evidence Asian Pac J Cancer Prev 201617463ndash466
12 Tan AC Heimberger AB Menzies AM Pavlakis N Khasraw MImmune checkpoint inhibitors for brain metastases Curr Oncol Rep2017 1938
13 DrsquoSouza NM Fang P Logan J Yang J Jiang W Li JCombining radiation therapy with immune checkpoint blockade
for central nervous system malignancies Frontiers Oncol 20166212
14 Parsa AT Waldron JS Panner A et al Loss of tumor suppressorPTEN function increases B7-H1 expression and immunoresistancein glioma Nat Med 2007 1384ndash88
15 Binder DC Davis AA Wainwright DA Immunotherapy for cancer inthe central nervous system current and future directionsOncoimmunology 2016 5e1082027
16 Newcomb EW Demaria S Lukyanov Y et al The combination ofionizing radiation and peripheral vaccination produces long-termsurvival of mice bearing established invasive GL261 gliomas ClinCancer Res 2006 124730ndash4737
17 Zeng J See AP Phallen J et al Anti-PD-1 blockade and stereotac-tic radiation produce long-term survival in mice with intracranial glio-mas Int J Radiat Oncol Biol Phys 2013 86343ndash349
18 Chow KK Hara W Lim M Li G Combining immunotherapy withradiation for the treatment of glioblastoma J Neurooncol2015123459ndash464
19 Belcaid Z Phallen JA Zeng J et al Focal radiation therapy com-bined with 4-1BB activation and CTLA-4 blockade yields long-termsurvival and a protective antigen-specific memory response in amurine glioma model PLoS One 2014 9e101764
20 Topalian SL Hodi FS Brahmer JR et al Safety activity and im-mune correlates of anti-PD-1 antibody in cancer N Engl J Med2012 3662443ndash2454
21 Bienkowski M Preusser M Prognostic role of tumour-infiltrating in-flammatory cells in brain tumours literature review Curr OpinNeurol 2015 28647ndash658
22 Harter PN Bernatz S Scholz A et al Distribution and prognostic rel-evance of tumor-infiltrating lymphocytes (TILs) and PD-1PD-L1 im-mune checkpoints in human brain metastases Oncotarget 2015640836ndash40849
23 Berghoff AS Ricken G Widhalm G et al Tumour-infiltrating lym-phocytes and expression of programmed death ligand 1 (PD-L1) inmelanoma brain metastases Histopathology 2015 66289ndash299
24 Silk AW Bassetti MF West BT Tsien CI Lao CD Ipilimumab and ra-diation therapy for melanoma brain metastases Cancer Med 20132899ndash906
25 Knisely JP Yu JB Flanigan J Sznol M Kluger HM Chiang VLRadiosurgery for melanoma brain metastases in the ipilimumab eraand the possibility of longer survival J Neurosurg 2012117227ndash233
26 Kiess AP Wolchok JD Barker CA et al Stereotactic radiosurgeryfor melanoma brain metastases in patients receiving ipilimumabsafety profile and efficacy of combined treatment Int J Radiat OncolBiol Phys 2015 92368ndash375
27 Qian JM Yu JB Kluger HM Chiang VL Timing and type of immunecheckpoint therapy affect the early radiographic response of mela-noma brain metastases to stereotactic radiosurgery Cancer 20161223051ndash3058
28 Silk AW Cao Y Gomez-Hassan D et al A randomized phase IIstudy of ipilimumab induction in patients with melanoma brain me-tastases receiving stereotactic radiosurgery J Clin Oncol 2015 33TPS9079ndashTPS9079
29 Neagu MR Reardon DA An Update on the role of immunotherapyand vaccine strategies for primary brain tumors Curr TreatOptions Oncol 2015 1654
30 Wen PY Reardon DA Phuphanich S et al A randomized double-blind placebo-controlled phase 2 trial of dendritic cell (DC) vaccina-tion with ICT-107 in newly diagnosed glioblastoma (GBM) patientsJ Clin Oncol 2014 322005ndash2005
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
114
British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

after a single intravenous dose of RRx-001 of 5 mgm2 4days before WBRT resulted in symptomatic improvementwithin 48 hours By 4 months after radiation there was areduction in size in the largest dimension down to 10 cmand 23 cm of the respective lesions A second report of amelanoma patient with at least 18 lesions after receivingRRx-001 of 5 mgm2 4 days before WBRT as well astwice weekly doses during the 2 weeks of radiation alsoshowed response The patient at 4 months had disap-pearance of 13 of 18 lesions with shrinkage of theremaining 5 lesions8 Presently BRAINSTORM is a phaseIII dose escalation trial of RRx-001 designed to be ad-ministered twice weekly for 2 weeks with WBRT (30 Gy in10 fractions) with the option for weekly maintenance8
Veliparib has also been evaluated in the setting of brainmetastases It was tested in a global randomized con-trolled trial with WBRT Veliparib is orally bioavailable andcrosses the bloodndashbrain barrier It was first examined in amultihistology phase I trial in patients with nonndashsmall celllung cancer (NSCLC) breast cancer melanoma and re-nal and colorectal cancers among others The study of81 patients tested dose tolerance of veliparib from 10 to300 mg orally twice a day with WBRT to 30 Gy in 10 frac-tions or 375 Gy in 15 fractions9 The phase I trial dose es-calation portion did not reach the predefined criteria forthe maximum tolerated dose but there was amplificationof the adverse effects of nausea and vomiting among thehighest dose cohort of 300 mg bid9 The adverse eventprofile at 200 mg bid was similar to that of WBRT aloneDoses of veliparib from 20 to 200 mg bid demonstratesimilar antitumor activity and other studies in preclinicalmodels found that 50 mg daily demonstrated significantreduction in poly(ADP-ribose) in peripheral blood mono-nuclear cells and tumor tissue while also effectivelycrossing the bloodndashbrain barrier Thus the subsequentphase II trial examined 50 mg with WBRT9 In order to as-sess a more homogeneous cohort the phase III globalrandomized trial studied only NSCLC at the 2 doses of50 mg and 200 mg twice daily versus placebo twice a daywith WBRT10 The primary endpoint was overall survivalIn 307 patients in a 111 randomization of 50 mg bid200 mg bid or placebo twice daily the study found nosignificant differences in overall survival among the differ-ent groups10 The majority of patients across the treat-ment groups had a graded prognostic assessment (GPA)score of25 and a Karnofsky performance status ofgt80 The median overall survival was 185 days forpatients receiving placebo and 209 days for those receiv-ing veliparib without any statistically significant differ-ence These results were similar to the disease-specificestimate of median survival for the disease-specific GPAof NSCLC patients with brain metastases10
Several other radiosensitizers have failed to improve overradiation alone in a number of trials These have includedtrials with WBRT including motexafin gadolinium efap-roxyn bortozemib thalidomide teniposide topotecanpaclitaxel and cisplatin7 Of note other PARP inhibitorsalso being assessed include talazoparib and niraparib4
which may yield positive results The use of valproic acid(VPA) as a histone deacetylase inhibitor has also beenconsidered to have radiosensitizing potential in additionto its anti-epileptic drug properties11 While studies havereported that patients with GBM receiving an anti-epilep-tic agent may have higher overall survival than those re-ceiving standard chemoradiation therapy alone thebenefit remains controversial Retrospective analysissuggested that patients taking VPA specifically had bettersurvival in comparison to other anti-epileptic drugs Alsoa recent prospective phase II trial was performed in 37patients with GBM receiving VPA 25 mgkg concurrentlywith TMZ chemoradiation and reported a median survivalof 296 months While controversial further data andinvestigation are needed into this and other agents thatmay potentiate RT
Immunotherapy and radiationImmune checkpoint inhibitors lead to activation of T cellswhich may traffic across the bloodndashbrain barrier to inter-act with tumor Primary brain tumors may evade the im-mune system through upregulation of immunecheckpoints and possible immunosuppression12
Monoclonal antibodies promote immune-mediated anti-tumor activity by inhibiting the immune functionndashmediated cytotoxic T-lymphocyte associated protein 4(CTLA-4) and programmed cell death protein 1 (PD-1)receptors PD protein ligand (PD-L1) is upregulated inGBM through oncogenic signaling possibly throughphosphatase and tensin homolog loss and interleukin-10signaling1314 RT has also been shown to enhance thefunction of cytotoxic T lymphocytes RT may induce aninfiltration of cytotoxic T lymphocytes and enhance theirfunction It may also induce antindashCTLA-4 agents inhibitingT-cell function and increasing the CD8thorn T cellregulatoryT cell ratio in cases of melanoma15 Thus PD-1 and PD-L1 blockers may have a further role in CNS managementwith the use of radiation
In preclinical models radiation has been examined withimmunotherapy that included among other mechanismsvaccination PD-1 blockade and CTLA-4 blockade Inmice radiation plus a vaccination of irradiated gliomacells was associated with increased survival of 40 to80 compared with 0 to 10 for other groups stud-ied16 A benefit of PD-1 blockade with stereotactic radio-surgery (SRS) specifically has also been shown in amouse model In comparison to mice treated with radia-tion antindashPD-1 therapy or a combination only those re-ceiving combination therapy had a higher percentagesurvival alive beyond 180 days after treatment17 Othermouse carcinoma models have identified response withanti-CTLA antibody and fractionated radiation therapy18
CD137 activation CTLA-4 blockade and focal radiationtherapy have been examined in an immunocompetent in-tracranial GBM model Mice treated with triple combina-tion therapy had 50 greater survival19 In other murine
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
112
models the use of antindashPD-1 and antindashCTLA-4 agentsshowed improved survival and increased tumor infiltratingleukocyte populations compared with single modalitywith concurrent radiation16 There are conflicting data re-garding timing or sequencing of therapy with some ani-mal models showing no difference in tumor response inrelation to timing of RT and delivery of immunotherapy18
For instance in one animal model CTLA-4 blockade de-livered simultaneously with radiation or delivered a coupleof days after showed no difference in survival among themice19
Increased PD-1 expression in circulating monocytes hasbeen identified as a biomarker for tumor-induced immu-nosuppression and may serve as a prognostic factor forpotentially worse survival outcomes in clinic13 In onestudy GBM patients with lower PD-L1 expression hadhigher median overall survival than those with higher PD-L1 expression suggesting that lower expression may beassociated with less immunosuppression and more im-mune activity against the tumor glioma20 RT with immunecheckpoint blockade is being investigated to assess if theaddition of PD-1 and PD-L1 inhibitors may improve theoutcomes or toxicity profile of standard therapy For in-stance a multi-institutional trial opened as a phase III willevaluate outcomes in GBM receiving radiation and pem-brolizumab with TMZ (NCT02530502) Next durvalumabor MEDI4736 a PD-L1 inhibitor is being examined forunmethylated MGMT GBMs with standard radiotherapy(NCT02336165)12 The impact of checkpoint inhibitorsduring adjuvant treatment of GBM is currently beingevaluated in the NCI-funded NRG-BN002 trial(NCT02311920) which will evaluate the antindashCTLA-4antibody ipilimumab alone or in combination with theantindashPD-1 antibody nivolumab for patients with newlydiagnosed GBM
Brain metastases have clonal populations of cells differ-ent from the rest of the brain and a unique microenviron-ment that may influence immunotherapy There may bemore immune infiltrates in metastases than in primarybrain tumors21 PD-L1 expression in brain metastasesvaries by histology In a series evaluating PD-L1 expres-sion in various tumors including melanoma NSCLCbreast renal colorectal and small cell less than 10showed significant expression22 There was greatest ex-pression among NSCLC and melanoma with a correla-tion between PD-L1 expression and tumor infiltratinglymphocytes22 Institutional series have examined thecombination of radiation and immune checkpoint block-ade In another study specific to melanoma brain metas-tases PD-L1 expression was found in over 50 of thecases and among those cases over 40 expressedPD-L1 in more than 5 of tumor cells23 The largest bodyof data for use of PD-L1 with radiation is for melanomaand NSCLC
Ipilimumab is a human monoclonal antibody that blocksCTLA-4 and allows for T-cell activation and proliferationto enhance the immune response to cancer In a
retrospective review of 70 patients with brain metastasestreated with SRS or WBRT the 33 patients receiving im-munotherapy had a median survival of 183 months incomparison to the 37 patients who did not receive ipili-mumab with a median survival of 53 months While therewere limited data among the cohort to evaluate sequenc-ing of therapy among 10 evaluable patients 40 whoreceived ipilimumab prior to RT had a partial response incomparison to only 10 among the cohort of 22 evalu-able patients who did not receive ipilimumab therapy atall with radiation24 Another retrospective institutionalstudy of 77 patients in which 37 received ipilimumabfound that patients treated with SRS and ipilimumab hada median survival of 213 months versus 49 months forthose not receiving ipilimumab Most interestingly theyidentified that the correlation remained significant evenafter adjusting for additional factors such as performancestatus Secondly there was not an increased need for useof salvage WBRT25
The sequencing of radiotherapy and immune checkpointinhibitors is of interest In a study of patients with brainmetastases the one-year survival for patients receivingSRS before ipilimumab was greater at 65 in contrast to56 for those receiving it concurrently and 40 for thosereceiving it after SRS26 Similarly another study of 75patients with 566 brain metastases showed greater tu-mor lesion response at 6 months from SRS for patientsreceiving ipilimumab nivolumab or pembrolizumabwithin 4 weeks of their SRS27 Those receiving concurrenttherapy had by 6 months a decrease of 949 in compar-ison to 662 for those not receiving checkpoint inhibi-tors within 4 weeks Prospective clinical trials areinvestigating different combinations of RT with immunecheckpoint blockers in this setting For instance new tri-als are currently evaluating intracranial tumor control at 6months and the timing of immune therapy or immunecheckpoint inhibitors in relation to SRS28
Vaccines are also being developed for primary braintumors showing some evidence for their use Vaccinesdeveloped from dendritic cells and tumor lysate with tu-mor antigens such as the epidermal growth factor recep-tor variant III vaccine have shown promise29 Forinstance in a placebo controlled phase II trial of ICT-107a vaccine composed on autologous dendritic cells andtumor antigens progression-free survival was increasedby 2 months for those receiving the vaccine30 Radiationmay assist in serving as a primer for the immunogeniceffects by facilitating tumor antigen uptake by dendriticcells and cross presentation on major histocompatibilitycomplex I Thus RT may assist in the tumor-specific cy-totoxic T lymphocytes associated with the immunemechanism
In conclusion although there may be challenges to com-bining and sequencing brain tumors radiosensitizersand immunotherapy the opportunities and potential fornovel applications are promising For brain tumors brainmetastases are typically underrepresented in trials
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
113
despite being among the most common intracraniallesions Despite their large population patients with brainmetastases are often excluded from clinical trials withnovel agents due to concerns regarding confounding out-comes and tolerability12 Primary gliomas also offer anovel frontier for the use of immunotherapy to standardadjuvant chemotherapy and radiation particularly forpatients with GBM less likely to respond to TMZ such aswith unmethylated MGMT As studies work to define therole of RT and radiosensitizers and immunotherapy fur-ther analysis is needed to assess the timing of RT andthese treatments
References
1 Stupp R Hegi ME Mason WP et al Effects of radiotherapy withconcomitant and adjuvant temozolomide versus radiotherapy aloneon survival in glioblastoma in a randomised phase III study 5-yearanalysis of the EORTC-NCIC trial Lancet Oncol 2009 10459ndash466
2 Lawrence TS Blackstock AW McGinn C The mechanism of actionof radiosensitization of conventional chemotherapeutic agentsSemin Radiat Oncol 2003 1313ndash21
3 Lesueur P Chevalier F Austry JB et al Poly-(ADP-ribose)-polymer-ase inhibitors as radiosensitizers a systematic review of pre-clinicaland clinical human studies Oncotarget 2017 8(40)69105ndash69124
4 Lester A Rapkins R Nixdorf S Khasraw M McDonald KCombining PARP inhibitors with radiation therapy for the treatmentof glioblastoma is PTEN predictive of response Clin Transl Oncol2017 19273ndash278
5 Gupta SK Kizilbash SH Carlson BL et al Delineation of MGMT hyper-methylation as a biomarker for veliparib-mediated temozolomide-sensi-tizing therapy of glioblastoma J Natl Cancer Inst 2016 108
6 Kleinberg LR Blakeley J Mikkelsen T et al An American BrainTumor Consortium (ABTC) phase 1 trial of veliparib (ABT-888)temozolomide (TMZ) and concurrent radiation therapy (RT) fornewly diagnosed glioblastoma multiforme (GBM) need for modifica-tion to approach for combining these therapies InternationalJ Radiat Oncol Biol Phys 2012 84S7ndashS8
7 Oronsky BT A Review of two promising radiosensitizers in brainmetastases Rrx-001 and 2-deoxyglucose In NC Oronsky edJ Cancer Sci Ther 2015 pp 137ndash141
8 Kim MM Parmar H Cao Y et al Concurrent whole brain radiother-apy and RRx-001 for melanoma brain metastases Neuro Onc2016 18455ndash456
9 Mehta MP Wang D Wang F et al Veliparib in combination withwhole brain radiation therapy in patients with brain metastasesresults of a phase 1 study J Neurooncol 2015 122409ndash417
10 Chabot P Hsia TC Ryu JS et al Veliparib in combination withwhole-brain radiation therapy for patients with brain metastasesfrom non-small cell lung cancer results of a randomized globalplacebo-controlled study J Neurooncol 2017 131105ndash115
11 Ochiai S Nomoto Y Yamashita Y et al Roles of valproic acid inimproving radiation therapy for glioblastoma a review of literaturefocusing on clinical evidence Asian Pac J Cancer Prev 201617463ndash466
12 Tan AC Heimberger AB Menzies AM Pavlakis N Khasraw MImmune checkpoint inhibitors for brain metastases Curr Oncol Rep2017 1938
13 DrsquoSouza NM Fang P Logan J Yang J Jiang W Li JCombining radiation therapy with immune checkpoint blockade
for central nervous system malignancies Frontiers Oncol 20166212
14 Parsa AT Waldron JS Panner A et al Loss of tumor suppressorPTEN function increases B7-H1 expression and immunoresistancein glioma Nat Med 2007 1384ndash88
15 Binder DC Davis AA Wainwright DA Immunotherapy for cancer inthe central nervous system current and future directionsOncoimmunology 2016 5e1082027
16 Newcomb EW Demaria S Lukyanov Y et al The combination ofionizing radiation and peripheral vaccination produces long-termsurvival of mice bearing established invasive GL261 gliomas ClinCancer Res 2006 124730ndash4737
17 Zeng J See AP Phallen J et al Anti-PD-1 blockade and stereotac-tic radiation produce long-term survival in mice with intracranial glio-mas Int J Radiat Oncol Biol Phys 2013 86343ndash349
18 Chow KK Hara W Lim M Li G Combining immunotherapy withradiation for the treatment of glioblastoma J Neurooncol2015123459ndash464
19 Belcaid Z Phallen JA Zeng J et al Focal radiation therapy com-bined with 4-1BB activation and CTLA-4 blockade yields long-termsurvival and a protective antigen-specific memory response in amurine glioma model PLoS One 2014 9e101764
20 Topalian SL Hodi FS Brahmer JR et al Safety activity and im-mune correlates of anti-PD-1 antibody in cancer N Engl J Med2012 3662443ndash2454
21 Bienkowski M Preusser M Prognostic role of tumour-infiltrating in-flammatory cells in brain tumours literature review Curr OpinNeurol 2015 28647ndash658
22 Harter PN Bernatz S Scholz A et al Distribution and prognostic rel-evance of tumor-infiltrating lymphocytes (TILs) and PD-1PD-L1 im-mune checkpoints in human brain metastases Oncotarget 2015640836ndash40849
23 Berghoff AS Ricken G Widhalm G et al Tumour-infiltrating lym-phocytes and expression of programmed death ligand 1 (PD-L1) inmelanoma brain metastases Histopathology 2015 66289ndash299
24 Silk AW Bassetti MF West BT Tsien CI Lao CD Ipilimumab and ra-diation therapy for melanoma brain metastases Cancer Med 20132899ndash906
25 Knisely JP Yu JB Flanigan J Sznol M Kluger HM Chiang VLRadiosurgery for melanoma brain metastases in the ipilimumab eraand the possibility of longer survival J Neurosurg 2012117227ndash233
26 Kiess AP Wolchok JD Barker CA et al Stereotactic radiosurgeryfor melanoma brain metastases in patients receiving ipilimumabsafety profile and efficacy of combined treatment Int J Radiat OncolBiol Phys 2015 92368ndash375
27 Qian JM Yu JB Kluger HM Chiang VL Timing and type of immunecheckpoint therapy affect the early radiographic response of mela-noma brain metastases to stereotactic radiosurgery Cancer 20161223051ndash3058
28 Silk AW Cao Y Gomez-Hassan D et al A randomized phase IIstudy of ipilimumab induction in patients with melanoma brain me-tastases receiving stereotactic radiosurgery J Clin Oncol 2015 33TPS9079ndashTPS9079
29 Neagu MR Reardon DA An Update on the role of immunotherapyand vaccine strategies for primary brain tumors Curr TreatOptions Oncol 2015 1654
30 Wen PY Reardon DA Phuphanich S et al A randomized double-blind placebo-controlled phase 2 trial of dendritic cell (DC) vaccina-tion with ICT-107 in newly diagnosed glioblastoma (GBM) patientsJ Clin Oncol 2014 322005ndash2005
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
114
British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

models the use of antindashPD-1 and antindashCTLA-4 agentsshowed improved survival and increased tumor infiltratingleukocyte populations compared with single modalitywith concurrent radiation16 There are conflicting data re-garding timing or sequencing of therapy with some ani-mal models showing no difference in tumor response inrelation to timing of RT and delivery of immunotherapy18
For instance in one animal model CTLA-4 blockade de-livered simultaneously with radiation or delivered a coupleof days after showed no difference in survival among themice19
Increased PD-1 expression in circulating monocytes hasbeen identified as a biomarker for tumor-induced immu-nosuppression and may serve as a prognostic factor forpotentially worse survival outcomes in clinic13 In onestudy GBM patients with lower PD-L1 expression hadhigher median overall survival than those with higher PD-L1 expression suggesting that lower expression may beassociated with less immunosuppression and more im-mune activity against the tumor glioma20 RT with immunecheckpoint blockade is being investigated to assess if theaddition of PD-1 and PD-L1 inhibitors may improve theoutcomes or toxicity profile of standard therapy For in-stance a multi-institutional trial opened as a phase III willevaluate outcomes in GBM receiving radiation and pem-brolizumab with TMZ (NCT02530502) Next durvalumabor MEDI4736 a PD-L1 inhibitor is being examined forunmethylated MGMT GBMs with standard radiotherapy(NCT02336165)12 The impact of checkpoint inhibitorsduring adjuvant treatment of GBM is currently beingevaluated in the NCI-funded NRG-BN002 trial(NCT02311920) which will evaluate the antindashCTLA-4antibody ipilimumab alone or in combination with theantindashPD-1 antibody nivolumab for patients with newlydiagnosed GBM
Brain metastases have clonal populations of cells differ-ent from the rest of the brain and a unique microenviron-ment that may influence immunotherapy There may bemore immune infiltrates in metastases than in primarybrain tumors21 PD-L1 expression in brain metastasesvaries by histology In a series evaluating PD-L1 expres-sion in various tumors including melanoma NSCLCbreast renal colorectal and small cell less than 10showed significant expression22 There was greatest ex-pression among NSCLC and melanoma with a correla-tion between PD-L1 expression and tumor infiltratinglymphocytes22 Institutional series have examined thecombination of radiation and immune checkpoint block-ade In another study specific to melanoma brain metas-tases PD-L1 expression was found in over 50 of thecases and among those cases over 40 expressedPD-L1 in more than 5 of tumor cells23 The largest bodyof data for use of PD-L1 with radiation is for melanomaand NSCLC
Ipilimumab is a human monoclonal antibody that blocksCTLA-4 and allows for T-cell activation and proliferationto enhance the immune response to cancer In a
retrospective review of 70 patients with brain metastasestreated with SRS or WBRT the 33 patients receiving im-munotherapy had a median survival of 183 months incomparison to the 37 patients who did not receive ipili-mumab with a median survival of 53 months While therewere limited data among the cohort to evaluate sequenc-ing of therapy among 10 evaluable patients 40 whoreceived ipilimumab prior to RT had a partial response incomparison to only 10 among the cohort of 22 evalu-able patients who did not receive ipilimumab therapy atall with radiation24 Another retrospective institutionalstudy of 77 patients in which 37 received ipilimumabfound that patients treated with SRS and ipilimumab hada median survival of 213 months versus 49 months forthose not receiving ipilimumab Most interestingly theyidentified that the correlation remained significant evenafter adjusting for additional factors such as performancestatus Secondly there was not an increased need for useof salvage WBRT25
The sequencing of radiotherapy and immune checkpointinhibitors is of interest In a study of patients with brainmetastases the one-year survival for patients receivingSRS before ipilimumab was greater at 65 in contrast to56 for those receiving it concurrently and 40 for thosereceiving it after SRS26 Similarly another study of 75patients with 566 brain metastases showed greater tu-mor lesion response at 6 months from SRS for patientsreceiving ipilimumab nivolumab or pembrolizumabwithin 4 weeks of their SRS27 Those receiving concurrenttherapy had by 6 months a decrease of 949 in compar-ison to 662 for those not receiving checkpoint inhibi-tors within 4 weeks Prospective clinical trials areinvestigating different combinations of RT with immunecheckpoint blockers in this setting For instance new tri-als are currently evaluating intracranial tumor control at 6months and the timing of immune therapy or immunecheckpoint inhibitors in relation to SRS28
Vaccines are also being developed for primary braintumors showing some evidence for their use Vaccinesdeveloped from dendritic cells and tumor lysate with tu-mor antigens such as the epidermal growth factor recep-tor variant III vaccine have shown promise29 Forinstance in a placebo controlled phase II trial of ICT-107a vaccine composed on autologous dendritic cells andtumor antigens progression-free survival was increasedby 2 months for those receiving the vaccine30 Radiationmay assist in serving as a primer for the immunogeniceffects by facilitating tumor antigen uptake by dendriticcells and cross presentation on major histocompatibilitycomplex I Thus RT may assist in the tumor-specific cy-totoxic T lymphocytes associated with the immunemechanism
In conclusion although there may be challenges to com-bining and sequencing brain tumors radiosensitizersand immunotherapy the opportunities and potential fornovel applications are promising For brain tumors brainmetastases are typically underrepresented in trials
Volume 2 Issue 3 Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors
113
despite being among the most common intracraniallesions Despite their large population patients with brainmetastases are often excluded from clinical trials withnovel agents due to concerns regarding confounding out-comes and tolerability12 Primary gliomas also offer anovel frontier for the use of immunotherapy to standardadjuvant chemotherapy and radiation particularly forpatients with GBM less likely to respond to TMZ such aswith unmethylated MGMT As studies work to define therole of RT and radiosensitizers and immunotherapy fur-ther analysis is needed to assess the timing of RT andthese treatments
References
1 Stupp R Hegi ME Mason WP et al Effects of radiotherapy withconcomitant and adjuvant temozolomide versus radiotherapy aloneon survival in glioblastoma in a randomised phase III study 5-yearanalysis of the EORTC-NCIC trial Lancet Oncol 2009 10459ndash466
2 Lawrence TS Blackstock AW McGinn C The mechanism of actionof radiosensitization of conventional chemotherapeutic agentsSemin Radiat Oncol 2003 1313ndash21
3 Lesueur P Chevalier F Austry JB et al Poly-(ADP-ribose)-polymer-ase inhibitors as radiosensitizers a systematic review of pre-clinicaland clinical human studies Oncotarget 2017 8(40)69105ndash69124
4 Lester A Rapkins R Nixdorf S Khasraw M McDonald KCombining PARP inhibitors with radiation therapy for the treatmentof glioblastoma is PTEN predictive of response Clin Transl Oncol2017 19273ndash278
5 Gupta SK Kizilbash SH Carlson BL et al Delineation of MGMT hyper-methylation as a biomarker for veliparib-mediated temozolomide-sensi-tizing therapy of glioblastoma J Natl Cancer Inst 2016 108
6 Kleinberg LR Blakeley J Mikkelsen T et al An American BrainTumor Consortium (ABTC) phase 1 trial of veliparib (ABT-888)temozolomide (TMZ) and concurrent radiation therapy (RT) fornewly diagnosed glioblastoma multiforme (GBM) need for modifica-tion to approach for combining these therapies InternationalJ Radiat Oncol Biol Phys 2012 84S7ndashS8
7 Oronsky BT A Review of two promising radiosensitizers in brainmetastases Rrx-001 and 2-deoxyglucose In NC Oronsky edJ Cancer Sci Ther 2015 pp 137ndash141
8 Kim MM Parmar H Cao Y et al Concurrent whole brain radiother-apy and RRx-001 for melanoma brain metastases Neuro Onc2016 18455ndash456
9 Mehta MP Wang D Wang F et al Veliparib in combination withwhole brain radiation therapy in patients with brain metastasesresults of a phase 1 study J Neurooncol 2015 122409ndash417
10 Chabot P Hsia TC Ryu JS et al Veliparib in combination withwhole-brain radiation therapy for patients with brain metastasesfrom non-small cell lung cancer results of a randomized globalplacebo-controlled study J Neurooncol 2017 131105ndash115
11 Ochiai S Nomoto Y Yamashita Y et al Roles of valproic acid inimproving radiation therapy for glioblastoma a review of literaturefocusing on clinical evidence Asian Pac J Cancer Prev 201617463ndash466
12 Tan AC Heimberger AB Menzies AM Pavlakis N Khasraw MImmune checkpoint inhibitors for brain metastases Curr Oncol Rep2017 1938
13 DrsquoSouza NM Fang P Logan J Yang J Jiang W Li JCombining radiation therapy with immune checkpoint blockade
for central nervous system malignancies Frontiers Oncol 20166212
14 Parsa AT Waldron JS Panner A et al Loss of tumor suppressorPTEN function increases B7-H1 expression and immunoresistancein glioma Nat Med 2007 1384ndash88
15 Binder DC Davis AA Wainwright DA Immunotherapy for cancer inthe central nervous system current and future directionsOncoimmunology 2016 5e1082027
16 Newcomb EW Demaria S Lukyanov Y et al The combination ofionizing radiation and peripheral vaccination produces long-termsurvival of mice bearing established invasive GL261 gliomas ClinCancer Res 2006 124730ndash4737
17 Zeng J See AP Phallen J et al Anti-PD-1 blockade and stereotac-tic radiation produce long-term survival in mice with intracranial glio-mas Int J Radiat Oncol Biol Phys 2013 86343ndash349
18 Chow KK Hara W Lim M Li G Combining immunotherapy withradiation for the treatment of glioblastoma J Neurooncol2015123459ndash464
19 Belcaid Z Phallen JA Zeng J et al Focal radiation therapy com-bined with 4-1BB activation and CTLA-4 blockade yields long-termsurvival and a protective antigen-specific memory response in amurine glioma model PLoS One 2014 9e101764
20 Topalian SL Hodi FS Brahmer JR et al Safety activity and im-mune correlates of anti-PD-1 antibody in cancer N Engl J Med2012 3662443ndash2454
21 Bienkowski M Preusser M Prognostic role of tumour-infiltrating in-flammatory cells in brain tumours literature review Curr OpinNeurol 2015 28647ndash658
22 Harter PN Bernatz S Scholz A et al Distribution and prognostic rel-evance of tumor-infiltrating lymphocytes (TILs) and PD-1PD-L1 im-mune checkpoints in human brain metastases Oncotarget 2015640836ndash40849
23 Berghoff AS Ricken G Widhalm G et al Tumour-infiltrating lym-phocytes and expression of programmed death ligand 1 (PD-L1) inmelanoma brain metastases Histopathology 2015 66289ndash299
24 Silk AW Bassetti MF West BT Tsien CI Lao CD Ipilimumab and ra-diation therapy for melanoma brain metastases Cancer Med 20132899ndash906
25 Knisely JP Yu JB Flanigan J Sznol M Kluger HM Chiang VLRadiosurgery for melanoma brain metastases in the ipilimumab eraand the possibility of longer survival J Neurosurg 2012117227ndash233
26 Kiess AP Wolchok JD Barker CA et al Stereotactic radiosurgeryfor melanoma brain metastases in patients receiving ipilimumabsafety profile and efficacy of combined treatment Int J Radiat OncolBiol Phys 2015 92368ndash375
27 Qian JM Yu JB Kluger HM Chiang VL Timing and type of immunecheckpoint therapy affect the early radiographic response of mela-noma brain metastases to stereotactic radiosurgery Cancer 20161223051ndash3058
28 Silk AW Cao Y Gomez-Hassan D et al A randomized phase IIstudy of ipilimumab induction in patients with melanoma brain me-tastases receiving stereotactic radiosurgery J Clin Oncol 2015 33TPS9079ndashTPS9079
29 Neagu MR Reardon DA An Update on the role of immunotherapyand vaccine strategies for primary brain tumors Curr TreatOptions Oncol 2015 1654
30 Wen PY Reardon DA Phuphanich S et al A randomized double-blind placebo-controlled phase 2 trial of dendritic cell (DC) vaccina-tion with ICT-107 in newly diagnosed glioblastoma (GBM) patientsJ Clin Oncol 2014 322005ndash2005
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
114
British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

despite being among the most common intracraniallesions Despite their large population patients with brainmetastases are often excluded from clinical trials withnovel agents due to concerns regarding confounding out-comes and tolerability12 Primary gliomas also offer anovel frontier for the use of immunotherapy to standardadjuvant chemotherapy and radiation particularly forpatients with GBM less likely to respond to TMZ such aswith unmethylated MGMT As studies work to define therole of RT and radiosensitizers and immunotherapy fur-ther analysis is needed to assess the timing of RT andthese treatments
References
1 Stupp R Hegi ME Mason WP et al Effects of radiotherapy withconcomitant and adjuvant temozolomide versus radiotherapy aloneon survival in glioblastoma in a randomised phase III study 5-yearanalysis of the EORTC-NCIC trial Lancet Oncol 2009 10459ndash466
2 Lawrence TS Blackstock AW McGinn C The mechanism of actionof radiosensitization of conventional chemotherapeutic agentsSemin Radiat Oncol 2003 1313ndash21
3 Lesueur P Chevalier F Austry JB et al Poly-(ADP-ribose)-polymer-ase inhibitors as radiosensitizers a systematic review of pre-clinicaland clinical human studies Oncotarget 2017 8(40)69105ndash69124
4 Lester A Rapkins R Nixdorf S Khasraw M McDonald KCombining PARP inhibitors with radiation therapy for the treatmentof glioblastoma is PTEN predictive of response Clin Transl Oncol2017 19273ndash278
5 Gupta SK Kizilbash SH Carlson BL et al Delineation of MGMT hyper-methylation as a biomarker for veliparib-mediated temozolomide-sensi-tizing therapy of glioblastoma J Natl Cancer Inst 2016 108
6 Kleinberg LR Blakeley J Mikkelsen T et al An American BrainTumor Consortium (ABTC) phase 1 trial of veliparib (ABT-888)temozolomide (TMZ) and concurrent radiation therapy (RT) fornewly diagnosed glioblastoma multiforme (GBM) need for modifica-tion to approach for combining these therapies InternationalJ Radiat Oncol Biol Phys 2012 84S7ndashS8
7 Oronsky BT A Review of two promising radiosensitizers in brainmetastases Rrx-001 and 2-deoxyglucose In NC Oronsky edJ Cancer Sci Ther 2015 pp 137ndash141
8 Kim MM Parmar H Cao Y et al Concurrent whole brain radiother-apy and RRx-001 for melanoma brain metastases Neuro Onc2016 18455ndash456
9 Mehta MP Wang D Wang F et al Veliparib in combination withwhole brain radiation therapy in patients with brain metastasesresults of a phase 1 study J Neurooncol 2015 122409ndash417
10 Chabot P Hsia TC Ryu JS et al Veliparib in combination withwhole-brain radiation therapy for patients with brain metastasesfrom non-small cell lung cancer results of a randomized globalplacebo-controlled study J Neurooncol 2017 131105ndash115
11 Ochiai S Nomoto Y Yamashita Y et al Roles of valproic acid inimproving radiation therapy for glioblastoma a review of literaturefocusing on clinical evidence Asian Pac J Cancer Prev 201617463ndash466
12 Tan AC Heimberger AB Menzies AM Pavlakis N Khasraw MImmune checkpoint inhibitors for brain metastases Curr Oncol Rep2017 1938
13 DrsquoSouza NM Fang P Logan J Yang J Jiang W Li JCombining radiation therapy with immune checkpoint blockade
for central nervous system malignancies Frontiers Oncol 20166212
14 Parsa AT Waldron JS Panner A et al Loss of tumor suppressorPTEN function increases B7-H1 expression and immunoresistancein glioma Nat Med 2007 1384ndash88
15 Binder DC Davis AA Wainwright DA Immunotherapy for cancer inthe central nervous system current and future directionsOncoimmunology 2016 5e1082027
16 Newcomb EW Demaria S Lukyanov Y et al The combination ofionizing radiation and peripheral vaccination produces long-termsurvival of mice bearing established invasive GL261 gliomas ClinCancer Res 2006 124730ndash4737
17 Zeng J See AP Phallen J et al Anti-PD-1 blockade and stereotac-tic radiation produce long-term survival in mice with intracranial glio-mas Int J Radiat Oncol Biol Phys 2013 86343ndash349
18 Chow KK Hara W Lim M Li G Combining immunotherapy withradiation for the treatment of glioblastoma J Neurooncol2015123459ndash464
19 Belcaid Z Phallen JA Zeng J et al Focal radiation therapy com-bined with 4-1BB activation and CTLA-4 blockade yields long-termsurvival and a protective antigen-specific memory response in amurine glioma model PLoS One 2014 9e101764
20 Topalian SL Hodi FS Brahmer JR et al Safety activity and im-mune correlates of anti-PD-1 antibody in cancer N Engl J Med2012 3662443ndash2454
21 Bienkowski M Preusser M Prognostic role of tumour-infiltrating in-flammatory cells in brain tumours literature review Curr OpinNeurol 2015 28647ndash658
22 Harter PN Bernatz S Scholz A et al Distribution and prognostic rel-evance of tumor-infiltrating lymphocytes (TILs) and PD-1PD-L1 im-mune checkpoints in human brain metastases Oncotarget 2015640836ndash40849
23 Berghoff AS Ricken G Widhalm G et al Tumour-infiltrating lym-phocytes and expression of programmed death ligand 1 (PD-L1) inmelanoma brain metastases Histopathology 2015 66289ndash299
24 Silk AW Bassetti MF West BT Tsien CI Lao CD Ipilimumab and ra-diation therapy for melanoma brain metastases Cancer Med 20132899ndash906
25 Knisely JP Yu JB Flanigan J Sznol M Kluger HM Chiang VLRadiosurgery for melanoma brain metastases in the ipilimumab eraand the possibility of longer survival J Neurosurg 2012117227ndash233
26 Kiess AP Wolchok JD Barker CA et al Stereotactic radiosurgeryfor melanoma brain metastases in patients receiving ipilimumabsafety profile and efficacy of combined treatment Int J Radiat OncolBiol Phys 2015 92368ndash375
27 Qian JM Yu JB Kluger HM Chiang VL Timing and type of immunecheckpoint therapy affect the early radiographic response of mela-noma brain metastases to stereotactic radiosurgery Cancer 20161223051ndash3058
28 Silk AW Cao Y Gomez-Hassan D et al A randomized phase IIstudy of ipilimumab induction in patients with melanoma brain me-tastases receiving stereotactic radiosurgery J Clin Oncol 2015 33TPS9079ndashTPS9079
29 Neagu MR Reardon DA An Update on the role of immunotherapyand vaccine strategies for primary brain tumors Curr TreatOptions Oncol 2015 1654
30 Wen PY Reardon DA Phuphanich S et al A randomized double-blind placebo-controlled phase 2 trial of dendritic cell (DC) vaccina-tion with ICT-107 in newly diagnosed glioblastoma (GBM) patientsJ Clin Oncol 2014 322005ndash2005
Radiation Combinations in the Treatment of Patients with Malignant Brain Tumors Volume 2 Issue 3
114
British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

British Neuro Oncology Society Conference 2017
Approximately 250 people with an in-terest in neuro-oncology attended partor all of ldquoEngaging Science EnhancingSurvivalrdquo in Edinburgh June 21ndash232017 In addition to our guest speak-ers including a number from NorthAmerica Denmark and Italy and widerepresentation from throughout theUK there were also proffered papersfrom Greece Hong Kong and India
As well as the plenary sessions in-cluding the Clerk Maxwell CancerLecture and the Stephen BakerMemorial Lecture there were prof-fered papers posters and lunchtimeseminars and exhibitions by spon-sors There were often parallel ses-sions so that attendees could choosebetween science clinical and alliedpatient care topics such as quality oflife and palliative care Bursaries wereavailable to ensure that those startingout in the field could attend Ofcourse the social and networkingopportunities were not ignored witha Welcome Reception at DynamicEarth and the Conference Dinnertaking place at the Playfair Library
BNOS would like to thank the variousorganizations and charities whosesponsorship made this meetingpossible AbbVie BrainLab MedacBrainstrust Brain Tumour ResearchB Braun Bristol-Myers SquibbCancer Research UK CodmanIntegra International Brain TumourAlliance Medtronic MercianNovartis Renishaw Severn StorzThe Brain Tumour CharityTrusteDoctor and Vitaflo
Council would also like to acknowl-edge the hard work of the Edinburghteam led by Imran Liaquat Sessionswere filmed and will be made avail-able on the BNOS website and theabstracts of the proffered papers andposters are available to all via theconference website This report isintended to provide a flavor of the
conference via some of the themesthat stood out amongst the sessionsthat I attended
Glioma StemCellsGlioma stem cells underpin malig-nancy and recurrence via their angio-genic and invasive nature andresistance to chemoradiation Thevascular microenvironments of neuraland glioma stem cells differ with twotypes of signaling maintaining quies-cence amongst the former and theperivascular invasion characteristicsof the latter New insights into the ge-nomic and epigenomic landscapes ofglioma were discussed frequentlyWhilst the former of course contin-ues to be studied eg helping under-standing of how IDH mutation confersbetter prognosis via a significantenrichment of genes involved in apo-ptosis and endoplasmic reticulumstress response inhibitors of epige-netic regulatory proteins are now alsoa focus Hence there were papersdescribing development of animalmodels to replicate both aspects andnot just single nucleotide variationsInsights into neuronal differentiationas a potential therapeutic avenue forGBM were also presented Preclinicaldata were presented demonstratingthat a subset of Ascl1-expressingpatient-derived glioma stem cell linescan be induced to differentiate intoneurons leading to pronouncedtumor suppression and extendedsurvival
The FOXG1 and SOX2 transcriptionalfactors found in high levels in gliomadrive unconstrained self-renewal ofneural stem cells This is effected bypreventing premature differentiation
via control of the core cell cycle appa-ratus and epigenetic machinery AsSOX2 and OLIG2 progenitors areabsent in adult brain but cycling rap-idly in the fetal brain work is now pro-gressing to investigate whether theZika virus (which is known to result incongenital birth defects while havinglittle effect when nonpregnant adultsare infected) penetrates and targetsglioma stem cells
Early DiagnosisIt can be argued that there is no advan-tage to be gained from earlier diagnosisof adult brain tumors as there is no evi-dence that this would positively affectoutcome but just increases the periodof anxiety for patients and their familiesHowever the contrary view was madestrongly that a long symptomatic periodprior to diagnosis (particularly in thosewith more subtle symptoms than seiz-ures) leads to poor quality of life frustra-tion and psychological damage Earlydiagnosis therefore should be a priorityand a better triage procedure is requiredto help GPs know whom to refer forurgent imaging Analysis of open-access computed tomography refer-rals for possible CNS malignancy byLothian-based GPs for 2010ndash2015showed a rate of only 16 of scanspositive for brain tumormdashheadache(either alone or in combination withother symptoms) being the mostcommon complaint among patientswith positive scans
A potential infrared spectroscopicmethod based on a serum sample isbeing developed as a cancerno can-cer test (95 sensitivity and 88specificity) It takes 10 minutes andcould be utilized in a GP practice Thiswas thought to be economically via-ble the incremental cost-effectivenessratio per quality-adjusted life year
115
Volume 2 Issue 3 Conference Report
(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

(QALY) being far below the NationalInstitute for Health and ClinicalExcellence (NICE) threshold ofpound20000ndashpound30000 (although the costof additional secondary care if acase were diagnosed earlier was notincluded) However there are alsoother factors to be consideredsuch as would a GP feel able towithhold referral after a negativetest even though symptoms hadjustified invoking the test in the firstplace
BiomarkersIt was encouraging to hear that theWHO 2016 biomarker-based classi-fications appear to be well estab-lished Indeed it was suggested thatthe next classification will be signifi-cantly different again and that the re-view time span of 9 years may betoo long In particular IDH wild-typeastrocytoma is considered only aprovisional entity within the newclassification as these can havevery variable prognoses There is agrowing view that they can be fur-ther classified into molecularly highgrade (harboring EGFR H3F3A orTERTp mutations) and lower gradeThe former are a distinct rapidlyprogressive subgroup without histo-pathological grade 4 characteristicsbut suspected to represent earlyglioblastomas (ldquobaby GBMsrdquo)whereas the latter lack all of thesebiomarkers the most favourablesurvival being noted in those withMYB amplification
It was thought that adult gliomapatients should be informed as totheir IDH mutation and MGMT pro-moter status and their implications asthey have such a dramatic effect ontreatment response and outcomes
The role of biomarkers in the sub-classification of medulloblastoma(first to 4 and now to 7 or possibly12 subgroups) is now evident in im-pact on treatment most notably thepossibility of reducing aggressivetreatment in the better-prognosissubgroups so as to limit the signifi-cant long-term toxicity
ImagingOne might be forgiven for thinkingthat biomarker assays could nowdrive all diagnosis and treatment de-cision making however tumors arenotoriously heterogeneous and plas-tic over time and it is not always pos-sible to obtain the repeated tissuesamples required to conduct assaysHence while identification of bio-markers is now vital there is definitelystill a role for (ever more) sophisti-cated imaging techniques and inte-grated diagnostic phenotypic-genotypic methods For exampleMR perfusion imaging may replaceconventional MRI techniques that failto detect the regions of low tumor celldensity remaining after resection butwhich are responsible for subsequenttumor recurrence diffusion-weightedMRI may identify non-enhancing IDHwild-type tumors despite an initiallyinnocuous imaging appearance andPETCT can differentiate tumor phe-notypes and between disease pro-gression and radionecrosis
Despite the significant engineeringchallenge a multimodality imagingtool for concurrent spectroscopy andMRI has been built via the EU-fundedINSERT project (INtegrated SPECTMRI for Enhanced stratification inRadio-chemo Therapy) A prototypeis now available providing simulta-neous biological readouts alignedwith high quality anatomical informa-tion which should enhance stratifica-tion and early treatment responseassessment without the confoundingproblem of pseudoprogression seenwhen MRI alone is utilized
SurgeryFormal surgical trials are rare For ex-ample although a systematic reviewof studies investigating efficacy andsafety of 5-aminolevulinic acid (5-ALA)ndashguided resection has identified46 formal surgical trials they aremostly only deemed Level 2ndash3 evi-dence Although use of 5-ALA cor-rectly identifies tumor tissue thereare sensitivity and specificity
limitations Hence it was encourag-ing to hear of proposals for 2 pro-spective multicenter trials tocompare intraoperative imagingtechniques (MRI and ultrasound) and5-ALA with white light microscopy
The Bristol team reported howeverthat although awake surgery and intra-operative MRI are the most effectiveindividual aids in preventing damageto functional brain while maximizingthe extent of resection and despitehigh levels of patient satisfactionusing them together is demanding forthe anesthetic and nursing teams andfor the patient at 10 hours thetheater times being about 2 hours lon-ger than for a standard craniotomyHence the combination is mostly onlyused for grade 2 tumor resections andthose grade 3ndash4 tumors possibly im-plicating eloquent areas
It was depressing to hear of the veryslow uptake of use of 5-ALA acrossthe UK an audit of neuro-surgicalcenters and their catchment areasshows that even though only oneunit has no interest in using it andall others have surgeons trained inits use only 43 of centers havefully implemented its use with a fur-ther 23 using it to a limited extentThe only 2 (foreign) studies whichcalculated cost-effectiveness pro-vide a cost per QALY of pound6500ndashpound7400 (although only one takes intoconsideration all medical costs)mdashbut even so the barrier remains oneof funding As all efforts to obtain fullNHS approval for its use have failed(and the recent approval of 5-ALA inthe USA is not expected to have anysignificant impact on UK usage)surgeons should perhaps be crea-tive in finding savings elsewhere inorder to fund its use For example inSouthampton measures have beenintroduced to ensure high rates ofelective admissions and reducedlength of stay (LOS) Their medianLOS for intrinsic tumors is 1 day(versus 6 days nationally) MeanLOS (vs national) is 25 (64) days forhigh-grade glioma 29 (65) days formetastases and 47 (92) days forbenign tumorsmdashall the lowest in theUKmdashwithout compromising read-mission reoperation or mortality
Conference Report Volume 2 Issue 3
116
rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

rates (The use of the NationalNeurosurgical Audit Program[NNAP] and Get It Right First Time[GIRFT] data for benchmarkingwas recommended) Not only hasthis proven popular with patientsbut it has improved efficiencyreduced cost cancellations andwaiting times and has morewidespread implications acrossthe NHS
Local DrugDeliveryWe know that residual cancer cellsremain at the margin even aftergross total resection and that target-ing this invasive region is vital in thedevelopment of new therapiesHence there is significant interest inlocally delivered chemotherapy
The Nottingham team is deliveringcombined temozolomide and etopo-side directly into the resection cavityin a thermo-setting biodegradablepaste and this has achieved signifi-cant extension to overall survival inan orthotopic rat model Similarlyencapsulated disulfiram nanopar-ticles have been developed inWolverhampton to protect the drugfrom degradation thereby extendingits half-life and this in combinationwith copper significantly inhibits gli-oma in orthotopic xenograft mousemodels at a very low dose
In Bristol convection-enhanced de-livery of panobinostat-loaded nano-micelles allows administration of thewater insoluble histone deacetylaseinhibitor in a high-grade glioma ratmodel An added sophistication be-ing studied in Edinburgh is that ofcoupling a prodrug with the use of anontoxic and catalytic implant totrigger local release of cytotoxicagents The prodrug is initially ren-dered nontoxic by masking the func-tional groups key to its mode ofaction which are then unmasked bypalladium in the implant As the pal-ladium device catalytically unmasksthe prodrug the treatment coursewould not be limited by the lifetime
of the implant and could be readilyrepeated in cases of recurrence
An example of local delivery whichhas reached man is that of irinotecanincorporated into biodegradable hy-drogel microspheres for injectioninto the postsurgical cavity wall Aphase I study in Birmingham hasshown less local swelling and woundhealing issues than have been dem-onstrated for carmustine wafers de-spite early offloading However thisshorter period of exposure is com-pensated for by a much higher thanexpected activation of irinotecan toits active metabolite
RadiationTherapyEven with stereotactic radiosurgeryalone (without whole brain irradia-tion) recent studies have demon-strated that around half of patientssuffer memory impairment Hencehaving identified that a considerableproportion of patients receiving ra-diosurgery for isolated metastasesreceive significant radiation to thehippocampus a proposed new pro-spective study in Wales will correlatedetailed radiation dosimetry neuro-cognitive function and functionalMRI measurements of organs at risk
It was interesting to hear thatTTField treatment is now being con-sidered in the UK In Nottingham anearly study has shown antiprolifera-tive effects on pediatric brain tumorcell lines at clinically deliverable fieldsettings and implantable multipledeep brain stimulation electrodesmay address the compliance issuesassociated with the Optune system
There is also a focus on identifyingnovel therapeutics to overcome in-herent radioresistance Irradiation ofglioblastoma cells can for examplepromote enhanced motility and inva-siveness both in vitro and in vivothrough activation of myotonic dys-trophy kinasendashrelated CDC42-binding kinase thought to offer apotential new targetRadiosensitization can also be
engendered in glioma stem cells bypoly(ADP-ribose) polymerase(PARP) inhibitors the most devel-oped being olaparib which is beingstudied in the PARADIGM clinical tri-als and an ataxiandashtelangiectasiamutated kinase (ATM) inhibitor soonto enter man A UK consortium isdeveloping a multi-armmultistagetrial in collaboration withAstraZeneca to test their portfolio ofDNA damage response candidates
Proton BeamTherapyIn 2016 the NHS sent 210 patients tothe USA and Switzerland for protonbeam therapy at a cost of pound114000each (compared with 136 in 2015 and104 in 2014) Two proton beam instal-lations in the UK both considered na-tional centers are being built withManchester due to start clinical prac-tice in summer 2018 (their cyclotronwas delivered on June 22) via 3 gan-tries (plus a fourth research facility)University College London Hospitals(UCLH) will follow in 2021 The firstpriority is to repatriate patients whowould otherwise have gone abroadbefore commissioning more ldquocorerdquoindications in pediatrics (particularlymedulloblastoma) and adults (sar-coma head and neck selected casesof meningioma orbital cancer chor-doma and other base-of-skull can-cers) and then eventually addingevaluative trials for further indicationsOnce both centers are fully functionalit is anticipated that 1500 patients willbe treated per year (1 of currentpatients treated with photon radio-therapy a far lower proportion thanplanned in Holland for example) A14-hour clinical day and total opera-tion from 6 am until 11 pm each daywill be in place with implications re-garding contracts and many other lo-gistical aspects All patients will beconsented and planned for both pho-ton and proton therapy as a contin-gency and outcomes data will becollected for all patients Specific clin-ical requirements such as exclusionof metal from the treatment area and
Volume 2 Issue 3 Conference Report
117
how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

how to maintain clear separation ofthe target site from neighboring struc-tures were discussed
There are of course other single gan-try commercial proton beam facilitiescoming onstream throughout the UKimminently While these are unlikelyto be able to handle more complexcases they are likely to create pres-sure on NHS commissioners to in-clude a broader range of indications
ClinicalManagementThe recently available relative wealthof clinical trial data in low-grade glio-mas still leaves many unansweredquestions For example
bull Which subset of patients do notbenefit from chemoradiation
bull How should one treat IDH wild-type patients
bull What is the optimal timing for ini-tiating treatment for particularlyindolent tumors
bull Can one delay treatment in orderto reduce the cognitive deficitwithout loss in efficacy
bull Why does it take about 4 years be-fore the survival curves of the bestand poorer prognosis patientsseparate
bull Can one reduce or fractionate ra-diotherapy or ensure hippocam-pal sparing
bull Is proton beam therapy superiorto traditional photon therapy
bull What is the impact of using che-motherapy alone on survival
bull Are temozolomide PCV andnitrosoureas equivalent
bull What is the impact of a neoadju-vant tumor lysate vaccine
bull Are IDH or checkpoint inhibitorseffective
A number of other studies are in prog-ress or opening imminently but thedifficulty caused by long survivaltimes means that valid surrogate end-points are required Those suggestedwere progression-free survival (butonly if treatment does not alter vascu-lar permeability) change in the rate of
progression (if in addition to exclud-ing anti-angiogenic agents one canmeasure this prior to initiating ther-apy) and response rate
Of course one also has to consideradditional management factorsand not just survival advantagemdashfor example the psychological ef-fect of providing patients with anestimate of projected survival pos-sible if biopsy and hence bio-marker assay has beenconducted or the reduction in seiz-ures resulting from surgery and ir-radiation even if not associatedwith radiological or clinical re-sponse (although there is a sug-gestion that seizure response maybe an early indicator of response tochemoradiation)
Seizures are of course a commonpresenting symptom or may de-velop later meaning that anti-epileptic agents are often givenprophylactically with significant ad-verse effects Hence if as sug-gested by a study in meningiomasexistence of preoperative seizuresmay be a significant predictor ofpostoperative seizures it may bepossible to withhold anti-epilepticdrugs in some patients While seiz-ures are less common in high-grade gliomas it has been foundthat secondary transformationalhigh-grade gliomas (as opposed toprimary de novo ones) and thepresence of IDH mutation are asso-ciated with increased likelihood ofseizure at presentation
Increased survival in childhood can-cer also comes with difficulties infollow-up whether of survival or ofthe many potentially significantlong-term side effects (neurocogni-tive psychosocial growth and de-velopment organ dysfunctionfertility and reproduction carcinoge-nicity) which may only become evi-dent years after treatment In theface of the current very limited evi-dence of their value in restoring sub-sequent fertility a research study isunder way in Edinburgh to carry outtissue and oocyte preservation inprepubertal children prior to theirtreatment
The ElderlyThe vast majority of the increasedincidence of brain tumors is due togliomas occurring in patients over70 years in whom there is poorerprognosis due to more aggressivebiology (for example IDH mutationis rare and EGFR amplificationcommon) frailty comorbiditiesand issues with access to careFitness to treat is difficult to defineand often evident only after theevent A number of studies in thisage group have now been pub-lished and it was recommendedthat up to age 69 the aim should bemaximum resection andchemoradiation and likewise inolder patients who are MGMTpromoter positive (or temozolo-mide alone if they canrsquot tolerateradiotherapy) There was a call for anew study of chemoradiationversus temozolomide alone aftergross resection in MGMT promoterpositive patients over age 70although concern was raised in theaudience as to the dramatic declinein performance status that canaccompany craniotomy in suchelderly patients
DietIn answer to the considerable inter-est shown in diet (the impact of life-style factors on survival wasnumber 1 on the list of priorities forresearch identified by the JamesLind Alliance) 2 parallel multicenteropen-label phase II randomized tri-als of the modified ketogenic dietare due to open in patients withhigh-grade gliomas receiving che-moradiotherapy (the primary end-point will be overall survival) and inpatients with low-grade gliomas(primary endpoint symptomlevels) Many factors have had tobe taken into consideration duringtrial design including how to en-sure that patients acceptrandomization and do not ldquoself-prescriberdquo and the amount of die-tetic support available
Conference Report Volume 2 Issue 3
118
Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

Immuno-therapeuticsOnce it was realized that the CNS isnot totally immune privileged that leu-kocytes can traffic to the CNS andthat there are lymphatics in the brainit was natural to try to emulate the dra-matic results achieved with immuno-therapy (vaccines and antindashCTLA-4PD1 and PDL-1 checkpoint inhibitors)for metastatic CNS disease in mela-noma and lung in primary glioma
Prospective randomized double-blind trials are now in place to studythe dendritic cell vaccines in gliomawith results from the DCVax trialexpected in 12ndash18 months The out-come of the other study (ICT-107utilizing ldquooff the shelfrdquo rather thanpersonalised antigens) may how-ever be compromised or delayedas it has been reported that recruit-ment has been suspended while thecompany explores strategic optionsfor further financing
Unfortunately the single peptidevaccine rindopepimut was shown tobe inferior to the control arm butresults from a phase II study with themultipeptide vaccine IMA950 areawaited The REO-Glio trialmdashwhichadds reovirus an oncolytic virusand granulocyte-macrophagecolony-stimulating factorpretreatment to standard-of-carechemoradiation in adult gliomamdashwillopen summer 2017 at 4 sites
DrugDiscoveryUnderstandably perhaps there wascompetition between speakers as towhether it is surgery or radiationtreatment that plays the central rolein the management of patients withbrain tumors Current methods ofdrug discovery via genomics andidentification of molecular targetsare proving of no real success whilebeing very long and costly andhence phenotypic screening viahigh-throughput microscopy and
stem cell technology with targetdeconvolution only at a late stage isnow coming to the fore
Clinical TrialDesignMedulloblastoma provides a masterclass in international collaboration toconduct effective trials despite therebeing only 650 cases per year in theEU (and 150 high-risk cases)However achieving consensusmeans that time from concept to atrial starting is too long especially asthe design must be flexible enough toallow additional new therapies to beslotted in as they become available
Unfortunately the picture is not thesame in adult brain tumors Datafrom the National Cancer ResearchInstitute Clinical Studies Groupshow huge inequality across thecountry regarding access to braintumor trials Recruitment is challeng-ing with barriers being amongstothers resources differing patientpathways and lack of trials The ma-jority of patients donrsquot remembertheir physicians speaking to themabout possible trial participationand it was admitted that when undertime pressure in clinic this may notoccur Twenty-six percent ofpatients wanted to take part in astudy but were unable to due to thelack of an appropriate trial or inclu-sionexclusion criteria Twenty-fivepercent of potential patients are lostfor preventable reasons such asdistance from a participating hospi-tal In order to address this and re-cruit all brain tumor patients in theUK all centers should take part intrials whereas currently many feelthat the setup effort is not worth-while if they are only likely to have ahandful of appropriate patients
QualitativeResearchA rather different (but again quiteworrying) topic listed all the different
types of biases that can affect physi-cian and surgeon decision makingand the advice these practitionersgive to patients It was recom-mended that best practice tumorboards and not just multidisciplinarymeetings be used to ensure thatviews of other similar specialists aretaken into consideration
Attendees were also introduced tothe role of qualitative research viasemi-structured face-to-face inter-views Examples largely focused onpatient satisfaction with awake crani-otomy gamma knife radiosurgeryldquowait and seerdquo management in low-grade glioma end-of-life care or in-formation provision prior to surgerybut this technique can also be usedto elicit physiciansrsquo views such ashow do they feel about elective surgi-cal resampling of malignant tumorsto guide treatment or do they (andthe family) experience the loss of therelationship after their patient dies
ConclusionsIt is interesting to look back at thereports I have written after this con-ference in previous years and toidentify trends This year the scien-tific papers were thoroughly sprin-kled with epigenetics andeveryonemdashscientists surgeons andoncologists alikemdashwere talkingabout the tumor margin andinvasiveness
While we still have a long way to goto improve outcomes (the latestldquogreat white hoperdquo immunotherapyis still a long way from proving fruit-ful) there is a staggering amount ofinformation available from ever moresophisticated imaging techniquesand biomarker classification and ad-vanced radiotherapy modalities areallowing less aggressive regimes toreduce side effects
Internationally neuro-oncologymust be congratulated on reusingclinical trial data to extract every lastdrop of information One frequentlyheard results from repeated sub-group analyses of completed trialsand there were more and more
Volume 2 Issue 3 Conference Report
119
demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

demands for new stratification fac-tors to be built into trial designHowever much more needs to bedone in the UK before recruitment ofadult patients into trials emulatesthat achieved in pediatrics
Management information (for exam-ple benchmarking data and qualita-tive research) long the domain ofbusiness is now finding its place inmedicine and there is obviouslyroom for thinking creatively as far asNHS cost constraints are concerned
AppendixThe Young Investigator of the YearAward jointly funded by BNOS and
Brain Tumour Research was madeto Harry Bulstrode University ofCambridge
The best poster prize was awardedfor ldquo18F-methylcholine PETCTin vivo magnetic resonance spec-troscopy imaging and tissue enzymebiomarkers of choline metabolism inprimary brain gliomasrdquo by MatthewGrech-Sollars (Imperial CollegeLondon)
The best scientific oral presentationwas ldquoA human iPS cell-based modelof medulloblastoma demonstratesco-operativity between SHH signal-ling and mutation in an epigeneticmodifierrdquo by Jignesh Tailor (StGeorgersquos University HospitalLondon)
The best clinical oral presentationwas ldquoThe impact of visual impair-ment on Health-Related Quality ofLife (HRQoL) scores in brain tumourpatientsrdquo by Sana Sharrack(University of Cambridge)
BNOS 2018 will be held July 4ndash6 inWinchester
Abstracted from a report pre-pared by Maryanne Roach onbehalf of the BNOS Council andBNOS 2017 organizing committeeFull version on BNOS websitehttpwwwbnosorguk
Maryanneroachbnosorguk
Conference Report Volume 2 Issue 3
120
Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

Indian Society of Neuro-Oncology Annual ConferenceReport 2017
The 9th Annual Conference of the Indian Society ofNeuro-Oncology (ISNO) was successfully organized byKidwai Memorial Institute of Oncology (KMIO) and hostedby the National Institute of Mental Health and Neuro-Sciences (NIMHANS) at the NIMHANS Convention Centerin Bangalore from March 10th to 12th 2017
The ISNO Executive Committee (EC) acknowledges andappreciates the hard work of all members of the organiz-ing team led admirably by Dr Lokesh (KMIO) and Dr VaniSantosh (NIMHANS) and executed through the untiringefforts utmost sincerity and dedication of Dr UdayKrishna as the Organizing Secretary of ISNOCON 2017
The conference had more than 300 registrations includingover 100 top-notch faculty from several leading nationaland international academic institutions who presentedand discussed the various aspects of clinical and basicneuro-oncology The international faculty list comprisedluminaries such as Dr Minesh Mehta (RadiationOncologist Miami Florida USA) Dr Vinay Puduvalli(Neuro-Oncologist Ohio USA) Dr Felice Giangespero
(Neuro-Pathologist Italy) Dr Santosh Kesari (Neuro-Oncologist Santa Monica USA) Dr Eng Siew-Koh(Radiation Oncologist Australia) Dr Zarnie Lwin (MedicalOncologist Australia) Dr Girish Dhall (PediatricOncologist UCLA USA) Dr Garnie Burkhoudarian(Neurosurgeon Santa Monica USA) and Dr VenkataYenugonda (Clinical Pharmacologist Santa Monica USA)
The 2 main themes of the meeting were ldquo2016 Update ofWHO Classification of Central Nervous System (CNS)Tumors and Impact on Managementrdquo and ldquoNovel Therapiesin Neuro-Oncology and Impact on Managementrdquo The meet-ing started with the ISNO Educational Session in the form of3 parallel Workshops on Radiation Oncology BasicTranslational Neuro-Oncology and Neurosurgery under thedynamic leadership of Dr Rakesh Jalali Dr Vani Santosh andDr Arivazhagan respectively
The formal scientific session started on Day 1 with thetheme ldquo2016 Update of WHO Classificationrdquo and ldquoImpacton Management in Clinical Practicerdquo A focused sessionon recent updates in ldquoPediatric Neuro-Oncologyrdquo followed
121
Volume 2 Issue 3 Conference Report
the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

the WHO update This was followed by the ISNO AwardSession and the prestigious ISNO Presidentrsquos Oration byDr Rakesh Jalali The first day ended with formal inaugu-ration of the meeting by distinguished guests and lumi-naries (see photograph)
Day 2 of the conference was themed ldquoNovel Therapies inNeuro-Oncologyrdquo and ldquoImpact on Managementrdquo in vari-ous fields such as skull-base tumors adult diffuse glio-mas molecular mechanisms of resistance retreatmentand immunotherapy This was followed by the much-awaited Ab Guha Oration Dr Minesh Mehta world-renowned Radiation Oncologist and presently the DeputyDirector of the Miami Cancer Institute Florida USA deliv-ered the prestigious Ab Guha Oration tracing the journey inthe management of ldquoLow Grade Gliomasrdquo This was fol-lowed by the very exciting ldquoDo Not Miss Itrdquo session on 6landmark papers in various fields of neuro-oncology withpotential to shapechange practice The day ended with amultidisciplinary discussion on interesting and challengingcase capsules (Tumor Board)
Day 3 of the conference started with parallel ldquoMeet theExpertrdquo sessions on ldquoImmunotherapyrdquo and ldquoGerm CellTumorsrdquo followed by scientific presentations onldquoNanotechnology in Neuro-Oncologyrdquo and ldquoBasicBiology of Glioblastomardquo This was followed by theProffered Paper session a lively debate on ldquoIntegration ofMolecular Techniques in Routine Neuro-oncologicPracticerdquo and the ldquoIndian CNS Tumor Registryrdquo initiative
A number of cash prizes grants and awards were givenduring ISNOCON 2017 as follows
ldquoISNO Presidentrsquos Award for Best Clinical Researcherrdquofor 2017 was awarded to Dr Tejpal Gupta RadiationOncologist Tata Memorial Centre Mumbai for his re-search work on medulloblastoma
ldquoISNO Annual Award for Outstanding Work in Neuro-Oncologyrdquo for 2017 was awarded to Dr Shilpee DuttPrincipal Investigator and Scientist ACTREC TataMemorial Centre Mumbai for her innovative biological re-search on glioblastoma resistance models
ISNO Studentsrsquo Awards for 2017 Two awards were givenin this category
(1) Clinical Neuro-Oncology Dr Archya DasguptaClinical Research Fellow Radiation OncologyACTREC Tata Memorial Centre Mumbai for hisoriginal research on the radiogenomics ofmedulloblastoma
(2) BasicTranslational Neuro-Oncology Dr JyothiNair Research Fellow Shilpee Dutt Lab ACTRECTata Memorial Centre Mumbai for her PhD-relatedwork on resistance mechanisms in glioblastoma
ISNO 2017 Travel Grants Twenty-eight top-scoringabstracts of a total of 80 abstracts (8 abstracts in theISNO Award Session and 20 abstracts selected forOral Presentation in the Proferred Papers Session)were given ISNO Travel Grants to attend ISNOCON2017 consisting of a cash prize of Rs 5000 and acitation
ISNO 2017 Poster Awards Four best posters of the 52abstracts selected for Poster Presentation one eachfrom Neurosurgery Radiation OncologyNeuropathology and Basic Neuro-Oncology were se-lected for Poster Awards consisting of a cash prize of Rs3000 and a citation
ISNO 2017 Training Fellowship Dr Vibhay Pareek pursu-ing DNB in radiation oncology at Jupiter HospitalMumbai was awarded the ldquoISNO Training Fellowshiprdquo for2017 He is entitled to complete a 4- to 6-week trainingcourse on ldquoRadiosurgery in Neuro-Oncologyrdquo under thetutelage and mentorship of Dr Rakesh Jalali at TataMemorial Centre Mumbai
The 10th Annual Conference of the Society (ISNOCON2018) is being organized and hosted by the All IndiaInstitute of Medical Sciences (AIIMS) New Delhi fromMarch 10th to 12th 2018 under the able leadership ofDr Ashish Suri (Organizing Secretary) and Dr ChitraSarkar (Organizing Chairperson) You can e-mail atisnocon2018gmailcom or visit our website atwwwisnoin for more details
Dr Tejpal Gupta Professor Radiation Oncology TataMemorial Centre
Joint Secretary Indian Society of Neuro-Oncology
Conference Report Volume 2 Issue 3
122
SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

SupportingFamilyCaregivers asPart of Neuro-OncologyPatient Care
Cristina Cruz MPHMargaretta S Page RN MS
123
The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

The needs of the neuro-oncology patient are significantlydifferent compared with those of patients affected byother cancers Though the treatment of radiation andchemotherapy is one commonality to other cancer treat-ments high-grade glioma patients can suffer from physi-cal decline as well as significant changes in moodbehavior and cognition causing distress for bothpatients and their caregivers1 These neurologic-specificsymptoms can be overwhelming to caregivers particu-larly cognitive decline and personality changes that occurin a patient who may outwardly appear to be fine Thesecaregivers are known to experience ldquopoorer social func-tioning more mental health concerns and higher carerburden than carers of patients with other cancersrdquo2
In a recent publication of the European Association ofNeuro-Oncologyrsquos palliative care guidelines EANOacknowledges the role of the family caregiver in patientcare and the psychosocial effects of the illness on thesecaregivers3 The guidelines recognize the benefits ofaddressing this caregiver strain through psychoeduca-tional interventions employing specialized neuro-oncology staff who can assess needs and by encourag-ing providers to treat family members as part of the careteam More research is needed to understand the bestsustainable practices to support family caregivers sincethey serve as a strong component of the neuro-oncologypatientrsquos care team This article presents one approach tosupporting the loved ones caring for a brain tumor pa-tientmdasha caregiverfamily support program embeddedwithin the neuro-oncology clinic at the University ofCalifornia San Francisco (UCSF)
Creating a CaregiverProgramThe Gordon Murray Neuro-Oncology Caregiver Programat the UCSFrsquos Division of Adult Neuro-Oncology was cre-ated in response to a need identified by a former neuro-oncology caregiver The programrsquos goal is to increasecaregiver preparedness across the trajectory of the ill-ness with hopes to sustain or improve quality of lifeamong patientsrsquo caregivers and subsequently improvepatientsrsquo quality of life and health outcomes
In 2011 Randi Murray collaborated with other formercancer caregivers and cancer survivors to initiate theBrain Tumor Initiative4 which would raise funds to furtherdevelop the neuro-oncology care and research offered atUCSF At its inception the caregiver program was taskedwith allocating staff to provide guidance and informa-tional resources to prepare neuro-oncology caregivers forthe different symptoms and side effects brain tumorpatients can experience The Gordon Murray CaregiverProgram was the most novel component of the initiativersquoscharge and it remains the only clinic-based caregiversupport program in neuro-oncology practice today
The programrsquos multidisciplinary team aims to preparecaregivers for their roles by offering resources healthcare navigation and emotional support through proactiveoutreach one-on-one consultations peer support oppor-tunities and educational offerings The staff includes amedical director nurse coordinator social worker andprogram analyst who are an active part of the adultneuro-oncology clinic team (see Table 1 for further detailson staff job descriptions)5
Offering SupportAcross the DiseaseTrajectoryThe Caregiver Programrsquos theory for its programming andoutreach is based on Paula Sherwoodrsquos stress responsemodel 6 for family caregivers of patients with a primarymalignant brain tumor In Sherwoodrsquos model which isrooted in Lazarus and Folkmanrsquos work on stress and cop-ing caregivers have both internal and external resourcesthat are accessed to address the patientrsquos evolving careneeds Sherwood models neuro-oncology caregiversrsquoemotional and physical stress responses to be a result ofthe caregiversrsquo primary appraisal of the patientrsquos healthstatus and care needs (ie assistance with activities ofdaily living and independent activities of daily livingchanges in cognitive functioning low KPS score7 and asecondary appraisal of the internal and external resour-ces that he or she has available to address those needsA caregiverrsquos internal resources are their physical andemotional traits or characteristics These resources caninclude the caregiverrsquos sense of mastery self-efficacyphysical health and emotional health External resourcesinclude more tangible forms of support such as financialmeans health information hired caregivers peer supportor respite care The number and quality of these resour-ces moderate the caregiverrsquos stress responses whichcan present in many ways affecting both physical andemotional health
There are several touch points in the Caregiver Programwhere caregivers are supported across the disease tra-jectory (see Table 2 for further details on each programcomponent) Staff connect with caregivers to assessneeds for support at each of these time points When theprogram was first created an internal assessment formwas created as part of the intake process Currently pro-gram staff use a framework that guides conversationswith caregivers to assess needs for support or resourcesthat may fall under informational practical social oremotional concerns
The program is designed to both supplement andstrengthen a caregiverrsquos internal and external resourcesDedicated caregiver support staff serve as an extra line ofsupport that is consistently available to family members
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
124
above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

above the assistance provided by the clinicrsquos staffProgram staff help caregivers cope with the psychoso-cial effects of the disease through connecting care-givers to peer support local counseling services andmonthly support groups Caregivers are also encour-aged to contact the program staff to discuss strategiesto manage the stress of caregiving Caregivers canmeet with staff in the caregiver program room a sepa-rate space decorated with soft lighting and calming col-ors for more extensive conversations to discussconcerns that may not always be shared in front of thepatient Additionally the program offers several resour-ces to educate caregivers about what to expect at dif-ferent stages of the disease trajectory8 and parentingresources9 to talk about the effects of the disease onthe patientrsquos children
To fortify the caregiverrsquos external resources the programconnects family members to existing caregiver supportservices and materials that can increase family membersrsquoability to provide care for patients This includes informa-tional resources regarding organizing care understand-ing the disease and managing symptoms financialassistance programs respite programs assistance withnavigating home health care and other cancer supportservices For example the program collaborated with fel-lows in UCSFrsquos Palliative Care program to create a man-ual that educates caregivers about what to expect duringa patientrsquos transition to hospice10 Recently more resour-ces have been curated for patients accessing different
types of care such as clinical trials or palliative care tobe shared by providers in the clinic A caregiver lending li-brary was also recently created to offer self-help andstress management books that caregivers can review ontheir own time
Educating Providers onSupporting theNeuro-OncologyCaregiverSince the program began there have been more op-portunities to offer education to other providers aboutsupporting the neuro-oncology caregiver as part of abrain tumor patientrsquos care In addition to serving asguest faculty in the UCSF Palliative Care FellowshipTraining program the programrsquos nurse coordinatortravels to hospices throughout the Bay Area to providein-service education to hospice nurses social work-ers and chaplains about the disease-specific needs ofbrain tumor patients and their families at end of life11
The goal of this outreach is to not only shed light onthe patientrsquos symptoms at end of life but also to ex-plore how the neurologic deficits that these patients
Table 1 Gordon Murray Caregiver Program Team Job Descriptions
Team Member Role
Medical Director Leadership vision oversight of development of the program Offers prioritization of pro-gram elements and progress Develops national and international agendas by creatingpolicy initiatives for long term goals to improve caregiver outcomes Leads caregiver re-search initiatives and evaluates program and caregiver outcome data Financial over-sight and fiscal support
NurseCoordinatorwith expertise inneuro-oncology
Operational development and day-to-day management of the Caregiver programProvides clinical expertise and direct care to caregivers and families of neuro-oncology
patients Offers education about the disease and needs of the neuro-oncology caregiverto caregivers and other health professionals involved with caring for brain tumor patientsalong the disease trajectory Serves as consultant to others in the department medicalleft and community at large Participates in application of and evaluation of evidence-based solutions in the care of the caregiver Participates in clinical research
Neuro-oncologysocial worker
Provides psychosocial assessments crisis intervention consultation education and link-age to supportive services and community resources that are specifically offered andintended for the neuro-oncology caregiver Participates in program goal setting and out-come evaluations
Facilitates monthly neuro-oncology caregiver support groupProgram Analyst Provides administrative and operational support to the Caregiver Program Develops docu-
mentation for program implementation toolkit needs assessment tools and programevaluation procedures Manages all program internal and external communications andmarketing Collaborates with clinic team to triage caregiver concerns Meets all care-givers of newly diagnosed patients at first visit to the Neuro Oncology clinic
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
125
experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

experience can impact the family during the final stageof the illness
Evaluating theProgramrsquos ImpactResearch is still developing to fully understand how sup-porting caregivers can impact their mastery and self-efficacy to care for patients with brain tumors The pro-gram has been able to develop services and outreach inresponse to the most common caregiver needs identifiedthrough the literature and interactions with family mem-bers In a 2011 study conducted among patientndashcaregiverdyads within UCSF Neuro-Oncologyrsquos clinic caregiversidentified the following areas as being of high importanceand in need of improvement in the clinicrsquos practice
emotional support to manage their anxiety and stress andgetting connected with caregivers who have experiencedsimilar situations12 Other areas that caregivers identifiedas very important included understanding how to managesymptoms knowing the side effects from treatment andmanaging the uncertainty of the patientrsquos prognosisToday some of the most common referrals the CaregiverProgram team receives from the providers in the clinic arein regard to guidance with accessing disability benefitsmanaging challenging patient behaviors hiring in-homehealth support and providing emotional support whentransitioning the patient to hospice care
Thus far the program has relied on distributing annualfeedback surveys that have asked broad questions aboutthe support received from the Caregiver Program to guideprogramming decisions Now that the program has estab-lished itself within the clinic and among fellow UCSF part-ners in care the programrsquos next goals are to measureoutcomes and analyze the programrsquos impact to identify
Table 2 Gordon Murray Caregiver Program Caregiver Outreach
Outreach Target Population Time Point of Service Objectives of Outreach
Inpatient EducationOutreach
Families of postoperativepatients with newly diag-nosed glioma
Prior to discharge fromhospital
Prepare caregivers for caringfor patient postopregarding
bull Medication managementbull Addressing seizuresbull Health care navigation
New to ClinicIntroductions
Patientscaregivers who arevisiting the clinic for theirfirst appointment and arereceiving their diagnosisprognosis and treatmentplan
At conclusion of consult withneuro-oncologist
Provide initial caregiverresources
bull Introductory healthinformation
bull Caregiver handbookbull ABTA resourcesbull Peer caregiver support info
GBM Outreach CallsProactive outreachacross 3 phone callsto address commonconcerns during firststage of standard ofcare treatment
Caregivers of newly diag-nosed glioblastomapatients
Two weeks and 4 weeks afterfirst clinic appointmentAfter post-radiation MRI fol-low-up appointment
See Table 3 for more details
Hospice TransitionCounseling
Families of patients who haverecently been recom-mended to hospice
Upon MD referral or upon re-quest from caregiver
bull Educate family members onservices available throughhospice
bull Explain symptoms at end oflife to prepare families onwhat to expect
Bereavement Outreach Caregivers of patients whohave died
One month or later afterpatientrsquos death
bull Assess for bereavementsupport needs
bull Connect caregivers to griefsupport groups or othergrief counseling
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
126
other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

other ways to best meet caregiver needs Over time the in-formation from these outcome measures will be used to re-fine the programrsquos resources and standard operatingprocedures for caregiver outreach
The first step in this next phase of the program is to con-cretely measure the effect of the support provided tocaregivers The program team will use the CaregiverPreparedness score13 as the primary outcome measurefor caregivers of newly diagnosed glioblastoma (GBM)patients who are offered proactive outreach ThePreparedness Scale is a self-assessment tool that askscaregivers questions about how prepared they feel tomanage aspects of the patientrsquos care such as emergentcare needs navigating health care services and thestress of caregiving This measure most closely alignswith the support currently provided to caregivers assess-ing the social emotional practical and informationaldomains The goal is to measure caregiversrsquo prepared-ness prior to the first GBM outreach call for a pre-measurement and then after the post-radiation MRIfollow-up appointment to collect a post-measurement(see Table 3 for more details on the GBM outreach proto-col for caregivers of newly diagnosed GBM patients)
Most recently the program has decided to build a data-base to collect and store these caregiver outcomes datahosted through the REDCap14 electronic data capturetool This tool will allow staff to electronically distributeneeds assessments and surveys to caregivers in a securemanner Caregivers will be able to privately and objec-tively state where they need assistance as they reviewlists of some of neuro-oncology caregiversrsquo most com-mon concerns Pre- and post- outcome measures will becollected more consistently with this systematized distri-bution of assessments This database will also store de-mographic data about caregivers to identify trendsamong the programrsquos high utilizers allowing the team tofurther understand caregiver needs
Strategies forSupporting Caregiverswith CurrentInfrastructureThe Caregiver Program as it exists today within the UCSFadult neuro-oncology clinic would not be possible with-out the generosity of the donors involved in the BrainTumor Initiative Philanthropic dollars provided for theprogramrsquos staffing costs allowing for the developmentand launch of the program in its first 3 years Now that theprogram staffrsquos salaries have been allocated to thedepartmentrsquos budget the program relies on donationsonly to finance ongoing programming evaluation and re-source development
The chief goal of the program is to serve as a model forcaregiver support so that in time these services can bemade available in all neuro-oncology practices Untilthis support service can be made available everywherethere are a few strategies that can be utilized amongproviders in the clinic to prepare family members fortheir new caregiving roles To successfully implementthese strategies clinics should work with all providersto establish buy-in and create consistent sustainablepractices so that patients and their families receive eq-uitable care
One of the first steps to effectively supporting caregiversis to recognize their role in the patientrsquos care and to regu-larly assess their needs to effectively care for the patientat home Caregiver needs should be assessed at eachappointment to offer timely effective interventions Thisis especially relevant for caregivers of high-grade tumorpatients who tend to have rapid decline
Secondly resources should be readily available to ad-dress common caregiver concerns Most often care-givers are not aware of what they will need until they arewell into managing the logistics of treatment This makesanticipating needs somewhat difficult At UCSF Neuro-Oncology caregivers of newly diagnosed patients areprovided a manual that provides a comprehensive over-view on symptoms and side effects throughout differentstages of treatment along with a review of helpful resour-ces and tools for these different stages Families are alsooffered disease-specific resources from the AmericanBrain Tumor Association (ABTA) ABTA (abtaorg) pro-vides concise resources designed for both patients15 andcaregivers16 and has a listing of brain tumorndashspecific sup-port groups available in each state
Lastly a listing of cancer support services available inthe areas where patients live should be curated andshared among providers Patients travel from severaldifferent counties within California to have an appoint-ment at UCSF Neuro-Oncology such that the programrsquossocial worker has become very familiar with many of theresources available to patients throughout the stateOver time the social worker has curated a county-specific list of caregiver support services and other fre-quently requested providers where patients and care-givers can be referred The team often references theseresources as clinicians inquire about referrals forpatients and families receiving treatment locally Similarresources can be organized and stored on a shareddrive within the clinic where providers can access themas needed
Currently there is no reimbursement process for caregiversupport services and funding for dedicated staff to pro-vide these services as part of patient care is not widelyavailable Advocacy efforts for federal policy changes toinclude and reimburse caregiver services must continueas family caregivers have increasingly become an exten-sion of the health care team The profile of the unpaidfamily caregiver is more visible as patients live longer with
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
127
improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

improved treatment For brain tumor patients how-ever small steps to support their family caregiversmay lead to long strides in better patient care and bet-ter coping among patients and families so that every-one impacted by the disease can have a better qualityof life
References
1 Trad W Koh E-S Daher M et al Screening for psychological dis-tress in adult primary brain tumor patients and caregivers consider-ations for cancer care coordination Frontiers Oncol 20155203
2 Halkett G Lobb E Shaw T et al Distress and psychological morbid-ity do not reduce over time in carers of patients with high-grade gli-oma Support Cancer Care 201525887ndash893
Table 3 Gordon Murray Caregiver ProgrammdashGBM Outreach Protocol
GBM OutreachTime Point
Outreach Objectives Performance Objectives Talking Points
Call 1Two weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Orient caregiver toworking with healthcare team at Neuro-Oncology
2 Assess caregiverrsquos abil-itylimitations to fulfillcaregiver duties
1 Caregiver will learnresources available tohimher during treat-ment at Neuro-Oncology
2 Caregiver to identifytheir informal supportteam amongfriendsfamily
3 Caregiver will identifyprogress towardstarting treatment retransportation findingproviders etc
1 How has it been organizingappointmentscare for the nextsteps in treatment plan Haveyou been able to communicatewith the team
2 Do you know who to contact inNeuro-Onc
3 Who else is helping you take careof the patient
4 Normalize common concernsduring XRT treatment (ie fatiguegetting to appointments etc)
Call 2Four weeks af-ter first appoint-ment at UCSFNeuro-Oncology
1 Prepare caregiver forsupporting patientmak-ing arrangements dur-ing radiation
2 Health care navigation3 Arranging for disability
work leave4 Address financial
concerns offernavigation
1 Caregiver will learnskills to navigatediscussions with familychildren patient recaregiving duties ordisease
2 Caregiver will navigateconcerns about arrang-ing time off for or payingfor treatment (insurancenavigation)
1 How have you and your familybeen managing the new changesin routine
2 Now that your loved one has be-gun treatment have you had anyconcerns about paying for treat-ment or accessing insurancecoverage
3 Are you able to navigate any ofthese concerns with your radia-tion-oncology team
4 Have you had any issues makingarrangements with your em-ployer or the patientrsquos employerfor time-off during treatmentDisability benefits
Call 3After post-radi-ation MRI fol-low-up appoint-ment at UCSFNeuro-Oncology
1 Confirm caregiverrsquos un-derstanding of nextsteps in treatment andaddress informationneeds
2 Transitioning back toworkdeveloping a newroutine after radiationtreatments
3 What to expect next4 Staying in touch with
Neuro-Oncology teambetween MRI scan
1 Help caregiver adapt tonew stage in treatment
2 Help caregiver problemsolve outreachresourceidentification to navi-gate new transition
3 Discuss resourcescop-ing strategies for livingwith uncertainty of ill-ness and diseasetrajectory
1 How will you need to support thepatient after your last visit withthe neuro-oncologist Do youfeel prepared to manage the nextstage of treatment
2 Will you be going back to yourold routine in any way
3 Do you have other support tohelp take care of your loved oneduring this transition back towork etc
4 Do you think yoursquoll be able tomake time for self-care in newroutine
Supporting Family Caregivers as Part of Neuro-Oncology Patient Care Volume 2 Issue 3
128
3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

3 Pace A Dirven L Koekkoek J et al European Association forNeuro-Oncology (EANO) guidelines for palliative care in adults withglioma Lancet Oncol 201718e330ndashe340
4 Bardi J ( 2011) Three Women Lead UCSFrsquos 25 Million FundraisingInitiative to Fight Brain Cancer Retrieved from httpswwwucsfedunews20111010834three-women-lead-ucsfs-25-million-fundraising-initiative-fight-brain-cancer
5 Page M Chang S Creating a caregiver program in neuro-oncologyNeuro-Oncol Prac 20174(2)116ndash122
6 Sherwood P Given B Given C et al Caregivers of persons with abrain tumor a conceptual model Nurs Inquiry 200411(1)43ndash53
7 Sherwood P Given B Given C et al Predictors of stress in care-givers of person with a primary malignant brain tumor ResearchNurs Health 200629105ndash120
8 Goodman S Rabow M Folkman S Orientation to Caregiving AHandbook for Family Caregivers of Patients with Brain Tumors 2nd edSan Francisco CA The Regents of the University of California 2013
9 Smith I A Tiny Boat at Sea Portland OR Grief Watch 2000
10 Cohn M Calton B et al Transitions in Care for Patients with BrainTumors Palliative and Hospice Care San Francisco CA TheRegents of the University of California 2014
11 Chang S Dunbar E et al End-of-Life Care for Brain Tumor PatientsSan Francisco CA The Regents of the University of California2015
12 Parvataneni R Polley M Freeman T et al Identifying the needs ofbrain tumor patients and their caregivers J Neurooncol2011104737ndash744
13 Archbold P Stewart B Greenlick M et al Mutuality and prepared-ness as predictors of caregiver role strain Research Nurs Health199013375ndash384
14 Harris P Taylor R et al Research electronic data capture (REDCap)A metadata-driven methodology and workflow process for providingtranslational research informatics support J Biomed Inform200942(2)377ndash381
15 Brain Tumors A Handbook for the Newly-Diagnosed Chicago ILAmerican Brain Tumor Association Retrieved from httpwwwabtaorgsecurenewly-diagnosed-1pdf
16 Caregiver Handbook Managing Brain Tumor Side Effects ampSymptoms Chicago IL American Brain Tumor AssociationRetrieved from httpwwwabtaorgsecurecaregiver-handbookpdfvfrac142
Volume 2 Issue 3 Supporting Family Caregivers as Part of Neuro-Oncology Patient Care
129
REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

REPORT FROM ASCO 2017
With regard to CNS tumors the 2017annual meeting of the AmericanSociety of Clinical Oncology (ASCO)included 9 oral presentations thatfocused on primary brain tumors andbrain metastases There was a clini-cal science symposium on maximiz-ing the approach to central nervoussystem tumors
Martin van den Bent presented thefinal results of the TAVAREC trialwhich was a randomized phase II ofpatients with recurrent grade IIIII gli-oma without 1p19q codeletion Onehundred and fifty-five patients wererandomized to receive temozolomidewith or without bevacizumab in firstrecurrence Overall survival (OS) rateat 12 months (primary endpoint) wassimilar in both of the arms 61 inthe temozolomide arm and 55 inthe temozolomide with bevacizumabarm Neurocognitive function wassimilar in both groups Overallsurvival was longer in tumors withisocitrate dehydrogenase 1 or 2(IDH12) mutations compared withIDH wild-type tumors (15 mo vs 107mo Pfrac14 0001) The study demon-strated that addition of bevacizumabto temozolomide failed to improveprogression-free survival (PFS) or OSin this patient population
Mizuhiko Terasaki discussed theresults of the randomized double-blind phase III trial of 88 humanleukocyte antigen A24ndashpositiveglioblastoma patients refractory totemozolomide from 20 Japanesehospitals Patients in the experimen-tal group received a personalizedpeptide vaccination (4 peptideschosen from 12 peptide candidates)Median OS in the vaccine group at84 months was similar to the OS of80 months in the best supportivecare group (control arm)
Fred Lang presented the results ofthe phase Ib randomized study of theoncolytic adenovirus DNX-2401 withor without interferon gamma for re-current glioblastoma OS-12 and OS-18 rates for all patients enrolled were33 and 22 respectively regard-less of treatment assignment andsupport an ongoing phase II study ofDNX-2401 for recurrentglioblastoma
Andrew B Lassman presented theefficacy analysis of ABT-414 with orwithout temozolomide in patientswith epidermal growth factor recep-tor (EGFR)ndashamplified recurrentglioblastoma He reported an objec-tive response rate (ORR) of 10(2 complete response [CR] and 9 par-tial response [PR] in 115 patients anddisease control rate of 52 [CRthornPRthorn stable disease] and PFS6 rateof 26 Report of the phase IIEuropean Organisation for Researchand Treatment of Cancer study ofABT-414 is expected to be presentedat the 2017 Annual Society of Neuro-Oncology Meeting in San Francisco
Thomas Graillon presented theCEVOREM study a phase II trial ofeverolimus and octreotide in 20patients with refractory and progres-sive meningioma The combinationresulted in a PFS6 of 58 andPFS12 of 38 and may warrant fur-ther evaluation in this patient popula-tion with limited medical therapyoptions
Oral presentations in brain metasta-ses in the CNS section included aphase I study of AZD3759 the firstEGFR inhibitor primarily designed tocross the bloodndashbrain barrier to treatpatients with EGFR-mutant non-small-cell lung carcinoma with CNSmetastases The use of AZD3759
was associated with the intracranialORR of 63 by investigatorsrsquo as-sessment in 19 evaluable patientsand extracranial ORR of 50 (10 of20 evaluable patients) CambridgeBrain Mets Trial 1 (CamBMT1) aphase Ib proof-of-principle study ofafatinib penetration into cerebralmetastases was presented Thestudy showed that it is feasible toconduct a window-of-opportunitystudy of targeted agents in patientswith operable brain metastases
Three oral presentations focused ontherapeutic options for patients withbrain metastases from melanomaMichael Davis presented a phase IIstudy of dabrafenib and trametinibin 4 cohorts of patients with BRAFmutant melanoma brain metastasesThe cohorts A B and C enrolledasymptomatic patients while cohortD included symptomatic brain me-tastases The patients in cohorts A(radiation naıve) and B (priortreatment) had good performancestatus and harbored BRAF V600Emutations Cohort C includedpatients with BRAF V600DKR-positive asymptomatic melanomabrain metastases with or withoutprevious local brain therapy andcohort D included BRAF V600DEKR-positive patients Theinvestigator-assessed intracranialresponses by Response EvaluationCriteria in Solid Tumors v11 criteriawere 58 44 56 and 59 incohorts A B C and D respectivelyA phase II study of a combination ofipilimumab and nivolumab inpatients with brain metastases frommelanoma was presented byHussein Tawbi Response rates of55 and an intracranial PFS6 of67 were reported among 75patients enrolled in the study
130
Volume 2 Issue 3 Meeting Report
Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

Georgina Long from the MelanomaInstitute Australia presented pre-liminary results of a randomizedphase II study of nivolumab ornivolumab plus ipilimumab in mela-noma patients with brain metasta-ses The median intracranial PFSwas 48 months in the nivolumaband ipilimumab arm and 27 monthsin the nivolumab alone armResponse rates of 50 were seenin the combination arm of nivolumaband ipilimumab in 20 patients whowere treatment naıve
A phase II trial of bevacizumab andtemozolomide for upfront treatmentof elderly patients with newly
diagnosed glioblastoma was part ofthe poster discussion LeiaNghiemphu reported that use of bev-acizumab and temozolomide as anupfront treatment resulted in a me-dian OS of 123 months (148 mo forthose with methylation of O6-methyl-guanine-DNA methyltransferase[MGMT] 100 mo for unmethylatedMGMT) in patients with newly diag-nosed glioblastoma age70 andKarnofsky performance status60The poster session covered almostall subfields of neuro-oncologyThere was an educational session onbrain metastases and different thera-pies in gliomas
Manmeet Ahluwalia MD FACP
Miller Family Endowed Chair inNeuroOncology
Director Brain Metastasis ResearchProgram Program DirectorNeuroOncology Fellowship Headof Operations
Burkhardt Brain Tumor andNeuro-Oncology Center ClevelandClinic
Professor Cleveland Clinic LernerCollege of Medicine Of the CaseWestern Reserve University
email ahluwamccforgPhone 216-444-6145Fax 216-444-0924
Volume 2 Issue 3 Meeting Report
131
InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

InterviewHoward Colman MD PhDDirector of Medical Neuro-Oncology Professor ofNeurosurgery Neurology and Internal Medicine(Oncology) Huntsman Cancer Institute Universityof Utah
132
1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

1 How do you currently use NGS technology in yourcurrent practice Eg whole-genome sequencing(WGS) whole-exome sequencing (WES) transcrip-tome sequencing targeted gene panels and whyAll patients trial patients For diagnosis ortreatment
At Huntsman Cancer Institute at the University ofUtah we currently perform NGS sequencing onmost patients with primary brain tumors when thereis sufficient tissue In terms of NGS technology wehave used various commercial and local variationsincluding mutation hotspot panels targeted exome(and promoter) panels whole exome sequencingand for selected cases combined DNA and RNA se-quencing Our experience indicates that both wholeexome sequencing and larger targeted panels thatprovide adequate coverage of important brain tumorgenes (including fusions) are sufficient for most diag-nostic and treatment information in gliomas andother primary brain tumors Good coverage of can-cer predisposition mutations and more recently infor-mation on mutational load and microsatelliteinstability status are also important for identificationof patients with unsuspected germline mutationsand those that may be candidates for treatment withcheckpoint inhibitors or other immunotherapies Theone technology we have found insufficient are so-called hotspot panels that are mainly aimed at identi-fying specific point mutations These panels are of-ten optimized for targeted therapies in other solidtumors and fail to identify many of the key alterations(larger mutations deletions and gene fusions) im-portant in brain tumors While not currently part ofour clinical practice RNA sequencing in combinationwith DNA sequencing provides the potential for evenmore sensitivity for detection of some alterationsparticularly gene fusions As technology improvesand costs go down this approach may becomemore common in routine practice
Results of NGS are used in our clinical practice inseveral ways including clarifying diagnosis deter-mining clinical trial eligibility and identifying patientswho may be candidates for targeted or checkpointtherapies In terms of diagnosis NGS is most usefulin situations where current WHO criteria still leavesome ambiguity regarding diagnosis or prognosisThis is particularly relevant in gliomas that are wildtype for IDH1 by initial immunohistochemical testingWhile many of these tumors harbor alterations similarto GBM in genes such as EGFR PTEN NF1 andorTERT promoter there is a distinct subset of tumorsin which the NGS results can influence diagnosis orprognosis Some of these tumors harbor alterationsin BRAF or other genes suggestive of a different di-agnosis (eg ganglioglioma pilocytic astrocytoma)and some turn out to be IDH mutated by sequencingeven when initial IHC results are negative NGSresults are also necessary for enrollment in an
increasing number of clinical trials that include spe-cific molecular alterations as inclusion criteria Whilestill a minority of patients there are also a select setof gliomas meningiomas craniopharyngiomas andothers that are candidates for targeted therapiesbased on alterations in specific genes includingBRAF mutations and fusions ROS1 and TRKfusions SMO mutations etc The recent FDA ap-proval of checkpoint inhibitors for all solid tumorswith microsatellite instability also raises the potentialto treat brain tumors with this alteration or high muta-tional burden with immunologic agents
2 What are you most interested in learning with NGSEg identification of driver mutations detection ofresistance mechanisms quantification of muta-tional burden evaluation of tumor gene expressiondiagnosis of germline mutations
While the utility and information needed from NGSvaries by patient and tumor type we are generallymost interested in the pattern of driver mutationsand alterations quantification of mutational burdenand microsatellite status and diagnosis of germlinemutations As described above the pattern of spe-cific driver gene mutations and alterations can bevery informative for clarifying diagnosis (and progno-sis) in certain WHO diagnostic categories that can in-clude a more heterogeneous molecular group oftumors (eg IDH wild type gliomas) Within diagnosticcategories the specific driver alterations can be im-portant to identify rare subsets of patients who mayderive benefit from targeted therapies although de-finitive data for efficacy of these alterations and as-sociated treatments are often lacking for braintumors relative to other solid tumors Mutational bur-den and microsatellite status are used to identifythose patients who may benefit from use of check-point inhibitors or other immune modulators Thiscan be important for enrollment in clinical trials butnow also potentially for ldquoon-labelrdquo use with the re-cent FDA approval for MSI-high tumors
We have also successfully identified a number ofpatients with previously unsuspected germline alter-ations based on NGS results that demonstrate alter-ations that are not typically found in particular braintumor types Specific germline mutations that wehave identified include RET SDH BRCA TP53 andbiallelic mismatch repair mutations Appropriateidentification of these unsuspected alterations andreferral of these patients and their families to cancergenetics can have important implicationsImplementation of appropriate testing and screeningfor the patient and extended family members can po-tentially prevent or facilitate early diagnosis of addi-tional cancers
3 What is the long-term utility of NGS in neuro-oncology Eg to predict responders to immuno-therapy either through RNA-Seq based gene
Volume 2 Issue 3 Interview
133
expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

expression or mutational burden could also drivesignificant clinical uptake of clinical NGS testing Isthere applicability to ctDNA for early diagnosismore representative view of tumor heterogeneity
There are several potential ways NGS testing andtechnologies may evolve in terms of long-term utilityin neuro-oncology First while the success of tar-geted therapies in general have been disappointingin brain tumors relative to other solid tumor typesthere are a number of potential situations where ac-cumulating data suggest promising efficacy such asBRAF alterations These alterations can be seencommonly (but not universally) in some histologic di-agnoses (eg ganglioglioma pilocytic astrocytoma)but rarely in others (eg IDH wild-type astrocytoma)There are also very promising data in other solidtumors for specific targeted therapies for alterationsthat occur very rarely in brain tumors such as ROS1and TRK fusions If developing data show clearly forefficacy of individual agents for specific alterationsthen NGS is potentially necessary for all patientswith these diagnoses in order to make sure that all ofthe rare patients with these alterations get the appro-priate therapies Second there is promise based onrecent data and FDA approvals that checkpointinhibitors may have efficacy for brain tumors with mi-crosatellite instability (and possibly high mutationalburden) but specific data for brain tumors are still indevelopment Thus importance and uptake of NGSin routine practice will depend in some degree on ob-servation of clear benefit of targeted immunother-apy or other treatments in selected brain tumor
populations Lastly as technologies improve thereis the potential for comprehensive NGS testing to re-place several of the individual molecular tests thatare done as part of the standard evaluation of manybrain tumors For example NGS and related technol-ogies can potentially be used to quantify copy num-ber alterations and gene methylation So one canimagine that in the future we could perform one testas part of initial evaluation of a tumor sample thatresults in all the relevant diagnostic data (IDH 1p19q) prognosticpredictive data (eg MGMT methyl-ation) and alterations relevant to targeted and immu-notherapies and germline information
Circulating tumor DNA (ctDNA) analysis and so-called liquid biopsies from blood or CSF are showingsome promising data for specific applications suchas diagnosis of IDH mutant gliomas If additionaldata indicate good sensitivity and specificity of thesetechnologies for IDH and other brain tumor altera-tions this approach may be particularly useful for ini-tial diagnosis of patients with non-enhancing MRIabnormalities In these situations additional informa-tion from ctDNA testing may be used to suggest like-lihood of diagnosis of infiltrating glioma or otherbrain tumor which would be useful for making the de-cision for early surgical intervention or initial closeobservation While these technologies also have thepotential to be used for monitoring disease statusand perhaps indicate evidence of disease responseor recurrence or resistance to specific therapeuticagents the data for this application in brain tumorsto date are currently lacking
Interview Volume 2 Issue 3
134
InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

InterviewJohn de Groot MDProfessor Department of Neuro-OncologyUniversity of Texas MD Anderson Cancer Center1515 Holcombe Blvd Houston TX 77030
135
1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

1 How do you currently use NGS technology in your-clinical practice
Our overall goal is to utilize patient- and tumor-specific information to optimize treatment forpatients with primary brain tumors We currently usethe Clinical Laboratory Improvement Amendments(CLIA) MD Andersonndashdeveloped NGS targeted se-quencing panel called Oncomine for most of ournewly diagnosed and recurrent glioma patients whoare trial eligible and have undergone surgery at MDAnderson This panel includes over 120 of the mostcommonly mutated genes in cancer as well as copynumber alterations (CNAs) Patients operated on out-side of our institution may already have NGS resultscommonly from Foundation Medicine The mutationand CNA information is primarily used to identify pa-tient eligibility for clinical trials using molecularly tar-geted therapies Mutational burden derived fromNGS may also be an eligibility requirement for enroll-ment on some immunotherapy clinical trials
The new World Health Organization 2016 guidelinesintegrate histologic diagnosis with tumor molecularmarkers Although the majority of information can beobtained from immunohistochemistry (IDH1 R132H)and fluorescence in situ hybridization (1p19q) thewidespread availability of NGS testing complementsthe integrated pathologic diagnosis The informationused from CLIA-based testing may also be useful inthe management of patients with rare mutational var-iants (eg low-grade glioma harboring noncanonicalmutations in IDH1 [R132C R132G etc] or IDH2)Additionally the diagnosis of rare tumors maybenefit from NGS testing For example an IDH12negative lower-grade glioma with a BRAF V600E mu-tation may be consistent with a pleomorphic xan-thoastrocytoma (PXA) and not an IDH wild-typeanaplastic astrocytoma
Additionally we consent patients who are treated atMD Anderson to our prospective longitudinal tumorprofiling protocol which is the foundation of our re-search database that collects demographic clinicaltherapeutic radiographic and biospecimen (tumorcirculating tumor [ct]DNA etc) NGS sequencingdata Currently tumor tissue is subjected to a 200
gene targeted gene panel whole exome sequencingand RNA sequencing platforms Although tumor andliquid biopsy data are obtained using non-CLIA NGSpanels this information can be used to identify andretrospectively analyze molecular cohorts and clini-cal outcomes data
2 What are you most interested in learning fromNGS
We are most interested in learning gene mutationsCNAs (deletions and amplifications) mutational bur-den and fusions Although the latter is not yet avail-able in our in-house panel there are several clinicaltrials that enroll patients based on gene fusions(fibroblast growth factor receptor neurotrophic tyro-sine kinase receptor etc) In circumstances where apatient treated with a targeted therapy develops pro-gression and undergoes resection the tumor isresequenced to identify resistance mechanismsThis may enable the patient to be treated with com-bination therapies to target resistance pathways
3 What is the long-term utility of NGS in neuro-oncology
Many challenges remain before the value of NGScan be fully realized in neuro-oncology Tumor het-erogeneity is a formidable challenge to developingeffective targeted therapies for brain tumor patientsThe information from NGS may provide an overallpicture of target expression within the tumor butthere are also a few examples of targeted therapythat leads to clinical benefit in patients Next-genera-tion sequencing using single cell methodologies isbeing developed and may enhance the ability to opti-mally tailor therapies to each patientrsquos tumorAdditionally there are gene amplification events thatoccur in extrachromosomal DNA that are not beingdetected with NGS platforms Another major issue inneuro-oncology relates to the difficulty in repeatedlyaccessing the tumor for analysis There is a criticalneed to optimize blood-based ctDNA and exosomalanalyses to evaluate tumor biology over time and tointegrate this information with imaging neurologicfunction and clinical outcomes
Interview Volume 2 Issue 3
136
InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

InterviewPatrick Y Wen MDDirector Center For Neuro-oncologyDana-Farber Cancer InstituteProfessor of Neurology Harvard Medical School
137
1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

1 How do you currently use NGS technology in yourpractice Eg whole-genome sequencing (WGS)whole-exome sequencing (WES) transcriptomesequencing and targeted gene panels and why Allpatients trial patients For diagnosis or treatment
For almost all patients with adequate tumor tissue atDana-Farber Cancer Institute we perform a targetedNGS panel called Oncopanel that surveys exonicDNA sequences of 447 cancer genes and 191regions across 60 genes for rearrangement detec-tion as well as providing information on copy num-ber alterations and mutational burden In additionwe usually conduct whole-genome array compara-tive genomic hybridization or more recentlyOncoscan for additional copy number informationThis information is used to select patients for trialswith specific targeted therapies or in the case oftumors with high mutational load for trials withcheckpoint inhibitors
In collaboration with Accelerated Brain Cancer Cure(ABC2) our Chief of Neuropathology Keith Ligon isleading a multicenter study called ALLELE usingWES for patients with newly diagnosed glioblastoma(GBM) We are using this especially for one of ourmulticenter trials called INdividualized Screening trialof Innovative Glioblastoma Therapy (INSIGhT) fornewly diagnosed GBM with unmethylated MGMTThis is a biomarker-driven Bayesian adaptive designtrial which utilizes the information generated by theWES from the ALLELE study for randomization ofpatients into specific treatment arms with targetedmolecular agents
2 What are you most interested in learning withNGSEg identification of driver mutations detec-tion of resistance mechanisms quantification ofmutational burden evaluation of tumor gene ex-pression diagnosis of germline mutations
We are interested in driver mutations copy numberalterations gene fusions and mutational burdenprimarily
3 What is the long-term utility of NGS in neuro-oncol-ogy Eg to predict responders to immunotherapyeither through RNA-Seq based gene expression ormutational burden could also drive significantclinical uptake of clinical NGS testing Is thereapplicability to ctDNA for early diagnosismorerepresentative view of tumor heterogeneity
In the long term it is likely that as the cost of testingcontinues to decrease and the turnaround timeimproves most brain tumor patients will undergoNGS testing of some form This will allow patients tobe selected for specific targeted molecular therapiesand immunotherapy trials There is also growing in-terest in developing personalized vaccines based onthe presence of neoantigens and if theseapproaches are successful the need for WES willexpand
Ideally technology will eventually improve suffi-ciently to allow ctDNA to be readily detected Thiswill provide valuable information on the molecularalterations in the tumor and potentially allow early di-agnosis as well as early detection of the develop-ment resistance
Interview Volume 2 Issue 3
138
Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

Hotspots inNeuro-Oncology 2017
Riccardo SoffiettiProfessor Neurology and Neuro-OncologySchool of Medicine University of Turin ItalyHead Dept Neuro-OncologyUniversity Hospital Turin
139
Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

Chemotherapy for adult low-grade gliomas clinicaloutcomes by molecular subtype in a phase II study ofadjuvant temozolomide
Wahl M et al Neuro Oncol 201719(2)242ndash251
Optimal adjuvant management of adult low-grade glio-mas is controversial The recent update of the WorldHealth Organization classification of brain tumors 2016based on molecular subtype definitions has the potentialto individualize adjuvant therapy but has not yet beenevaluated as part of a prospective trial
In the February issue of Neuro-Oncology Wahl and col-leagues from the University of California San Franciscohave published the results of a single-arm mono-institu-tional phase II trial on upfront chemotherapy with temozo-lomide for grade II gliomas after incomplete resectionPatients received monthly cycles of standard temozolo-mide for up to 1 year or until disease progression Forpatients with available tissue molecular subtype wasassessed based upon 1p19q codeletion and isocitratedehydrogenase 1 R132H mutation status The primaryoutcome was radiographic response rate secondary out-comes included progression-free survival (PFS) and over-all survival (OS) One hundred twenty patients wereenrolled with median follow-up of 75 years Overall re-sponse rate was 6 with median PFS and OS of 42 and97 years respectively Molecular subtype was associ-ated with rate of disease progression during treatment(Plt 0001) PFS (Pfrac14 0007) and OS (Plt 0001)Patients with 1p19q codeletion demonstrated a 0 riskof progression during treatment In an exploratory analy-sis pretreatment lesion volume was associated with bothPFS (Plt 0001) and OS (Plt 0001)
In conclusion this study suggests that patients with high-risk low-grade glioma receiving adjuvant temozolomidemay display a high rate of radiographic stability and favor-able survival outcomes while meaningfully delaying radio-therapy Patients with 1p19q codeletion are potentialcandidates for omission of adjuvant radiotherapy butfurther work is needed to directly compare chemotherapywith combined modality therapy This important studyhas shown 2 main limitations First the response evalua-tion was based on Macdonald criteria with measurementof the enhancing tumor only and not on the more modernResponse Assessment in Neuro-Oncology criteria whichinclude measurement of the non-enhancing tumor aswell Second the predictive capacity of methylation ofO6-methylguanine-DNA methyltransferase for responseto temozolomide was not analyzed
Phase III randomized study of radiation and temozolo-mide versus radiation and nitrosourea therapy foranaplastic astrocytoma results of NRG OncologyRTOG 9813
Chang S et al Neuro Oncol 201719(2)252ndash258
The primary objective of this multi-institutional random-ized phase III study was to compare the overall survival(OS) of patients with newly diagnosed anaplastic
astrocytoma (AA) receiving radiotherapy (RT) and eithertemozolomide (TMZ) or a nitrosourea (NU) Secondaryendpoints were time to tumor progression (TTP) toxicityand the effect of isocitrate dehydrogenase 1 (IDH1) muta-tion status on clinical outcome
In the February issue of Neuro-Oncology Chang and col-leagues have reported the final results Eligible patientswith centrally reviewed histologically confirmed newlydiagnosed AA were randomized to receive eitherRTthornTMZ (nfrac1497) or RTthornNU (nfrac1499) The study closedearly because the target accrual rate was not met
Median follow-up time for patients still alive was101 years (19ndash126 y) and 66 of the patients diedMedian survival time was 39 years in the RTthornTMZ arm(95 CI 30ndash70) and 38 years in the RTthornNU arm (95CI 22ndash70) corresponding to a hazard ratio (HR) of 094(Pfrac14036 95 CI 067ndash132) The differences inprogression-free survival (PFS) and TTP between the 2arms were not statistically significant Patients in theRTthornNU arm experienced more grade3 toxicity (758vs 479 Plt 0001) mainly related to myelosuppres-sion Of the 196 patients 111 were tested forIDH1-R132H status (60 RTthornTMZ and 51 RTthornNU)Fifty-four patients were IDH negative and 49 were IDHpositive with a better OS in IDH-positive patients (mediansurvival time 79 vs 28 y Pfrac140004 HRfrac14 050 95 CI031ndash081)
In conclusion RTthornTMZ did not appear to significantlyimprove OS or TTP for AA compared with RTthorn NURTthornTMZ was better tolerated IDH1-R132H mutationwas associated with longer survival
This study is important as it suggests that for treatment ofnewly diagnosed AA the choice of the alkylating agentsto be associated with radiotherapy does not impact theoutcome
Pointcounterpoint randomized versus single-armphase II clinical trials for patients with newly diag-nosed glioblastoma
Grossman SA et al Neuro Oncol 201719(4)469ndash474
In this article which appeared in the April issue of Neuro-Oncology Grossman and colleagues discussed the prosand cons of single-arm versus randomized phase II stud-ies in patients with newly diagnosed glioblastoma (GBM)taking into account such factors as (i) the availability ofappropriate controls (ii) the interpretability of the resultingdata (iii) the goal of rapidly screening many novel agentsusing as few patients as necessary (iv) utilization of lim-ited financial and patient resources and (v) maximizationof patient participation in these studies
In conclusion phase II trials are critically important in thedevelopment of novel therapies for patients with newlydiagnosed GBMs These trials represent the initialevaluation of activity in this disease and are specificallydesigned to triage novel compounds and approachesinto those that do and do not deserve further study Whileit often appears that there is a conflict between
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
140
randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

randomized and single-arm phase II trial designs in real-ity each has its place in furthering effective drug develop-ment Since the vast majority of experimental drugstested in patients with newly diagnosed GBM have beenclinically ineffective designing small single-arm phase IIstudies to eliminate ineffective therapies early is reason-able However larger randomized phase II trials are im-portant to reduce confounders and false positivesInvestigators should carefully consider the trial endpointthe availability of appropriate controls and how trialresults will be used to inform further development of theexperimental therapy when choosing a designUltimately single-arm and randomized phase II trials (aswell as adaptive and integrated designs) provide usefultools for evaluating the efficacy of novel therapeutics innewly diagnosed GBM when applied in an appropriatefashion
Leptomeningeal metastases a RANO proposal forresponse criteria
Chamberlain M et al Neuro Oncol 201719(4)484ndash492
Leptomeningeal metastases (LM) currently lack standard-ization with respect to response assessment AResponse Assessment in Neuro-Oncology (RANO) work-ing group with expertise in LM developed a consensusproposal for evaluating patients treated for this diseaseIn the April issue of Neuro-Oncology Chamberlain andcolleagues proposed 3 basic elements for assessing re-sponse in LM a standardized neurological examinationcerebrospinal fluid (CSF) cytology or flow cytometry andradiographic evaluation The group recommends that allpatients enrolling in clinical trials undergo CSF analysis(cytology in all cancers flow cytometry in hematologiccancers) complete contrast-enhanced neuraxis MRI andin instances of planned intra-CSF therapy radioisotopeCSF flow studies In conjunction with the RANONeurological Assessment working group a standardizedinstrument was created for assessing the neurologicalexam in patients with LM Considering that most lesionsin LM are nonmeasurable and that assessment of neuro-imaging in LM is subjective neuroimaging is graded asstable progressive or improved using a novel radiologi-cal LM response scorecard Radiographic disease pro-gression in isolation (ie negative CSF cytologyflowcytometry and stable neurological assessment) would bedefined as LM disease progression
This is the first attempt to standardize the criteria for eval-uating response in clinical trials on leptomeningeal dis-eases and now they are being validated in several USand European prospective studies Moreover such astandardization may serve as a guide also in the dailyclinical practice to optimize the management of thisdifficult category of patients
The Neurologic Assessment in Neuro-Oncology(NANO) scale a tool to assess neurologic functionfor integration into the Response Assessment inNeuro-Oncology (RANO) criteria
Nayak L et al Neuro Oncol 201719(5)625ndash635
The Macdonald criteria and the Response Assessment inNeuro-Oncology (RANO) criteria define radiologic param-eters to classify therapeutic outcome among patientswith malignant glioma and specify that clinical statusmust be incorporated and prioritized for overall assess-ment But neither provides specific parameters to do soA standardized metric to measure neurologic functionwould permit more effective overall response assessmentin neuro-oncology
An international group of physicians including neurolo-gists medical oncologists radiation oncologists andneurosurgeons with expertise in neuro-oncology draftedthe Neurologic Assessment in Neuro-Oncology (NANO)scale as an objective and quantifiable metric of neuro-logic function evaluable during a routine office examina-tion Nayak and colleagues reported in the May issue ofNeuro-Oncology the proposal for a NANO scale whichwas tested in a multicenter study to determine its overallreliability interobserver variability and feasibility
Overall the NANO scale is a quantifiable evaluation of 9relevant neurologic domains based on direct observationand testing conducted during routine office visits Thescore defines overall response criteria A prospectivemultinational study noted agt90 interobserver agree-ment rate with kappa statistic ranging from 035 to 083(fair to almost perfect agreement) and a median assess-ment time of 4 minutes (interquartile range 3ndash5) This newscale should be validated in prospective clinical trials inthe different brain tumor subtypes
Natural course and prognosis of anaplastic ganglio-gliomas a multicenter retrospective study of 43 casesfrom the French Brain Tumor Database
Terrier LM et al Neuro Oncol 201719(5)678ndash688
Anaplastic gangliogliomas (GGGs) are rare tumors whosenatural history is poorly documented In the May issue ofNeuro-Oncology Terrier and colleagues on behalf ofANOCEF tried to define their clinical and imaging featuresand to identify prognostic factors by analyzing all casesof GGGs in the adult prospectively entered into theFrench Brain Tumor Database between March 2004 andApril 2014 After diagnosis was confirmed by pathologicalcentral review clinical imaging therapeutic andoutcome data were collected retrospectively
Forty-three patients with anaplastic GGG (median age494 y) from 18 centers were included Presenting symp-toms were neurological deficit (372) epileptic seizure(372) and increased intracranial pressure (256)Typical imaging findings were unifocal location (947)contrast enhancement (881) central necrosis (432)and mass effect (476) Therapeutic strategy includedsurgical resection (953) adjuvant radiochemotherapy(488) or radiotherapy alone (279) Medianprogression-free survival (PFS) and overall survival (OS)were 80 and 247 months respectively Three- and5-year tumor recurrence rates were 69 and 100
Volume 2 Issue 3 Hotspots in Neuro-Oncology 2017
141
respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

respectively The 5-year survival rate was 249Considering unadjusted significant prognostic factors tu-mor midline crossing and frontal location were associatedwith shorter OS Temporal and parietal locations were as-sociated with longer and shorter PFS respectively Noneof these factors remained statistically significant in multi-variate analysis
In conclusion this is a large series providing clinicalimaging therapeutic and prognostic features of adult
patients treated for an intracerebral anaplastic GGGOur results show that pathological diagnosis is diffi-cult that survivals are only slightly better than for glio-blastomas and that complete surgical resectionfollowed by adjuvant chemoradiotherapy offers longersurvival It will be important in future studies toinvestigate new molecular markers (such as BRAFmutations) that could serve as targets for moleculardrugs
Hotspots in Neuro-Oncology 2017 Volume 2 Issue 3
142
Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

Hotspots inNeuro-OncologyPractice 2017
Susan Marina Chang MD
Director Division of Neuro-Oncology Departmentof Neurological Surgery University of CaliforniaSan Francisco 505 Parnassus Ave M779 SanFrancisco CA 94143 USA
143
(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

(1) Sabel M et al Effects of physically active videogaming on cognition and activities of daily living inchildhood brain tumor survivors a randomized pilotstudy Neuro-Oncology Practice 20174(2)98ndash110
Carlson-Green B et al Feasibility and efficacy of anextended trial of home-based working memory train-ing for pediatric brain tumor survivors a pilot studyNeuro-Oncology Practice 20174(2)111ndash120
In recent years there has been a significant research effortfocused on developing effective interventions aimed atcognitive rehabilitation for children with brain tumors Thearticle by Sabel et al describes a pilot study on a physicalexercise regimen that can be done at home using a videoconsole While the small study did not show difference incognitive function before and after intervention activitiesof daily living scores were significantly improved provid-ing a rationale for further exploration of physical exerciseas a component of overall rehabilitation The authors sug-gest that it may be combined with other active tasks tochallenge cognitive ability possibly for an extended pe-riod of time with modulated intensities and tested in anadequate patient sample
The article by Carlson-Green et al provides results of afeasibility study using the platform CogmedVR to improveneurocognitive function in children who have beentreated for a brain tumor They found that participantslargely enjoyed performing the tasks and that there wassignificant improvement in working memory verbal tasksand visuo-spatial tasks between baseline and 6-monthpost-intervention scores Parents also reported improve-ment in participantsrsquo academic and social skills As withthe physical exercise regimen reported by Sabel et alCogmed is a home-based intervention and the inherentflexibility and convenience that it provides has beenfound to improve compliance
(2) Hovey EJ et al Continuing or ceasing bevacizumabbeyond progression in recurrent glioblastoma an ex-ploratory randomized phase II trial Neuro-OncologyPractice 20174(3)171ndash181
Patients with high-grade glioma are often prescribedbevacizumab at recurrence as part of standard careHowever the question of whether to continue with thetherapy (possibly combined with another drug) after fur-ther relapse has been a subject of debate among clini-cians with little data to guide practical decisions TheCabaraet study investigated this important clinical ques-tion and the investigators came to the conclusion thatpatients who continued bevacizumab beyond diseaseprogression did not have clear survival benefits This is ahighly relevant study for any provider treating patientswith glioma
(3) Likar R Nahler G The use of cannabis in support-ive care and treatment of brain tumor Neuro-Oncology Practice 20174(3)151ndash160
Cannabis has a long history as an intervention for cancerpain and in controlling common negative effects of both
treatment and tumor It has been widely used to treat avariety of symptoms including nausea and vomiting lossof appetite mood disorders and sleep disorders In thiscomprehensive review the authors delve into this historyand provide a specific discussion of the different types ofcannabinoids and how they may best be used in neuro-palliative care A shift in cultural attitudes towards psy-chotropic drugs in medicine has led to a resurgence instudies on these compounds and it is critical for pro-viders to have accurate information when guidingpatients who are interested in exploring these therapies
(4) Dirven L et al Development of an item bank forcomputerized adaptive testing of self-reported cogni-tive difficulty in cancer patients Neuro-OncologyPractice 20174(3)189ndash196
A common theme in papers examining quality of life is alack of standardized definitions and assessments whichare essential for making useful comparisons across stud-ies The professional societies in neuro-oncology are inthe best position to make improvements in this area bycreating validated tools that can be widely adopted in theneuro-oncology community This article by Dirven et almdashon behalf of the European Organisation for Research andTreatment of Cancer (EORTC) Quality of Life Groupmdashdescribes development of a computerized adaptive test-ing version of each scale of the EORTC Quality of LifeQuestionnaire (EORTC QLQ-C30) Cognitive deficits arean especially important problem for patients with brain tu-mor and having an easy-to-use tool facilitates acquisitionof data elements that can be used for analysis
(5) Page MS Chang SM Creating a caregiver programin neuro-oncology Neuro-Oncology Practice20174(2)116ndash122
This article describes the building and implementation ofa dedicated neuro-oncology caregiver program at theUniversity of California San Francisco The program hasa structure of providing general information to all ldquonew tothe clinicrdquo newcomers proactive extra interventions tocaregivers of ldquonewly diagnosed glioblastomardquo patientsadditional support to a ldquohigh-risk transitionrdquo groupmdashparticularly with reference to their needs of possible palli-ative and hospice caremdashand finally a ldquobereavementrdquogroup for counseling and emotional support An initialevaluation of the program demonstrated that the newlydiagnosed glioblastoma and high-risk transition groupshad the highest needs primarily in emotional support andadvocacy issues Overall the program received positivefeedback from caregivers and the authors intend tostrengthen their services with more staff including a dedi-cated neuropsychologist and more in-depth interven-tions in several key areas identified in their preliminaryfindings
(6) Pugh S Essence of survival analysis Neuro-Oncology Practice 20174(2)77ndash81
One of the most popular features of Neuro-OncologyPractice is ldquoStatistics for the Practicing Clinicianrdquomdasha series
Hotspots in Neuro-Oncology Practice 2017 Volume 2 Issue 3
144
of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

of articles covering statistical methods used in neuro-oncology studies and how to interpret statistical results inorder to appropriately counsel patients In this article stat-istician Stephanie Pugh focuses on survival analysesexplaining calculations for both progression-free and
overall survival analyses and how to interpret estimates ofthese critical endpoints that are used in a majority of clinicaltrials It also includes the rationale for censoring data frompatients lost to follow-up and a detailed explanation ofhazard models with illustrative case examples
Volume 2 Issue 3 Hotspots in Neuro-Oncology Practice 2017
145
The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

The EANOYoungsterInitiative WhatDoes MentoringMean to You
Anna Sophie Berghoff MD PhD
Department of Medicine I Comprehensive CancerCenter- CNS Tumours Unit (CCC-CNS) MedicalUniversity of Vienna Weuroahringer Gurtel 18-20 1090Vienna Austria
146
Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

Career development for neuro-oncology youngsters is amain focus of the recently founded EANO youngsterscommittee With mentoring being an essential part ofevery youngsterrsquos personal career development we aimto put a special focus on this topic
ldquoHow to find a good mentorrdquo as well as ldquohow to get mostout of your mentoringrdquo are questions every youngsteraddresses frequently Therefore we aim to focus on thisessential topic during the EANO youngster track of theupcoming EANO congress 2018 To get started we askedourselves as well as our mentors ldquoWhat does mentoringmean to yourdquo Find enclosed our answers and ourmentorsrsquo
Carina Thome biologist currently holding a postdoc-toral fellow position at the German Cancer ResearchCenter (Heidelberg Germany)
bull Transfer skills and knowledge in science but also innon-science related issues
bull Regular meetings and constructive feedbackbull Establish and helping with contacts and networks in
and outside the communitybull Opportunity to present and discuss results and data in
the communitybull Open minded for new input however take handle
and tolerate criticisms
Wolfgang Wick (mentor of Carina Thome) head of theneurology department University of HeidelbergGermany
bull Time for interaction outside the daily working routinebull Time for discussion on conference topics while being
at a conferencebull Activating an international network for the menteebull Training of specific skills for presentation etcbull Finding role modelsbull Supporting activity in the neuro-oncology community
Alessia Pellerino neurology from the University ofTurin and her mentors Riccardo Soffietti (head DeptNeuro-Oncology University and City of Health andScience University Hospital of Turin Italy) andRoberta Ruda (head of the Outpatient Service andMultidisciplinary Brain Tumor Board City of Healthand Science HospitalUniversity of Turin)
bull Since I was a young resident in neurology my mentorstaught me a method in clinical and research practicethey taught me to lead the clinical trials with ethicsand intellectual honesty They remind me to respectpatients and their families Their examples and theircareers inspire me and make me love my daily work
bull My mentors gave me the theoretical and practicalknowledge to reach a progressive independence as aneurologist through the years In case of difficult situa-tions they always stay available for advice and helpThey never leave me in troubles and help me to facecomplications
bull My mentors require hard work and dedication fromtheir team and gave to all collaborators the opportu-nity to participate in national and internationalmeetings and develop several projects and write orig-inal papers and reviews
bull My mentors know that there are other greatneurologists and neuro-oncologists in Europe and theUS in this regard they stimulate and support youngresearchers to go abroad in order to share knowledgeand gain new stimulating experiences
bull My mentors continuously tell me that an excellent clin-ical activity needs to be fed and supported by basicand translational knowledge and research
bull My mentors always tell me that a good daily practiceshould be guided by an adherence to validated inter-national guidelines
Aleksandar Stanimirovic neurosurgery resident at theclinical center of Serbia
bull Giving time and attention to the mentee A goodmentor should always find time to give somethingback
bull Teaching the mentees to keep an open mind to allprogress in modern medicine
bull Give hope and hold the fear of the mentee showinghimher to trust in the decisions that are being madeand not to be afraid of failure The mentee must neverbe paralyzed by the fear of failure or heor she willnever push in the direction of the right vision
bull Mustnrsquot be a naysayerbull At the end of the day a good mentor leaves behind
outstanding people and doctors and the field of in-terest in a better state than it was when heshebegan
Dr Danica Grujicic (mentor of AleksandarStanimirovic) head of the neuro-oncology depart-ment of the Clinic of Neurosurgery at the ClinicalCenter of Serbia
bull Transfer of knowledge in a sense of continuous andnon-stop patient observation and patient controls
bull Training junior colleagues and teaching them differentsurgical techniques
bull Teaching mentees the principles of radio and chemo-therapy for brain tumors
bull Stimulating younger doctors to better organize themedical care for neuro-oncology patients
bull Insisting upon making and publishing scientific papersbased on personal and recent experiences
Amelie Darlix neuro-oncologist at the MontpellierCancer Institute (France)
bull Encourage me to think by myself rather than imposehisher views
bull Share hisher clinical experiencebull Define short-term and long-term goals with me in
terms of research scientific publications and career
Volume 2 Issue 3 The EANO Youngster Initiative What Does Mentoring Mean to You
147
bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

bull Brainstorm with me in order to make new ideas andprojects emerge
bull And celebrate successes
Emilie le Rhun (mentor of Amelie Darlix) neuro-oncol-ogist at Centre Hospitalier Regional et Universitaire(CHRU) de Lille France
bull To help to develop new ideas and translational re-search projects
bull To help to develop a clinical specialty profilebull To define career plans with milestonesbull To discuss emerging areas of basic and translational
researchbull To re-evaluate progress annually
Anna Berghoff medical oncology trainee at theMedical University of Vienna Austria
bull Show possibilities and guide career developmentbull Mentoring in a ldquosee one do one teach onerdquo manner
and encourage mentee to also mentee himherselfyounger students (MD students)
bull Help with practical question like scholarships or grantapplications
bull Be patient (especially in the early steps)
Matthias Preusser (mentor of Anna Berghoff) neuro-oncologist at the Medical University Vienna Austria
bull To guide and help develop skills and a personal styleThe goal is not to produce a clone of the mentor butpersons with their own ideas and ways of thinking andworking
bull To give advice that is in the best interest of the men-tee even if it is not in the mentorrsquos best interest
bull To change the way of mentoring over time to allow agradual development of the mentee At some pointthe mentee should become a mentor on hisher own
bull To be open to learn from the menteebull Let the mentee make hisher own experiences includ-
ing mistakes but in a positive way
Asgeir Jakola neurosurgeon and associate professorat the Sahlgrenska University Hospital GothenburgSweden
bull Improves the studentrsquos learning and a great opportu-nity to impact the organization
bull Teaches the student how to speak up and be heard frac14improved communication skills
bull Educates the student how to receive constructivefeedback in important areas
bull Improves the studentrsquos interpersonal relationshipskills
bull Helps the student better understand the organiza-tionrsquos culture and unspoken rules both of which canbe critical for success
Roger Henriksson (mentor of Asgeir Jakola) head ofthe Regional Cancer Centre StockholmGotland
bull Listen actively not only to whatrsquos been said but alsoto whatrsquos not said
bull Trust the student in finding the best solution for solv-ing problems but be supportive
bull Be curious ask questions rather than give answersbull Help the student to see things from the positive side
point out the strengthsbull Be generous with yourself your feelings and your
experiences
Tobias Weiss neurology resident at the UniversityHospital in Zurich Switzerland
bull Strategically guidesupport the mentee to reach hisher short- or long-term goals
bull Availability and responsivenessbull Bridge contacts and help to establish new networks
or integrate into existing structuresbull Help to find judge role modelsbull Open-minded to continuously improve
Michael Weller chairman of the Department ofNeurology University Hospital in Zurich Switzerland
bull Promoting focused research of high qualitybull Supporting innovative research ideasbull Promoting international cooperation and networkingbull Developing excellence in specialized areas of patient
carebull Promoting educational and presentation skills
The EANO Youngster Initiative What Does Mentoring Mean to You Volume 2 Issue 3
148
- 01_OP-WFNO170041
- 02_OP-WFNO170042
- 03_OP-WFNO170037
- 04_OP-WFNO170032
- 05_OP-WFNO170030
- 06_OP-WFNO170033
- 07_OP-WFNO170034
- 08_OP-WFNO170035
- 09_OP-WFNO170031
- 10_OP-WFNO170039
- 11_OP-WFNO170040
- 12_OP-WFNO170038
- 13_OP-WFNO170028
- 14_OP-WFNO170029
- 15_OP-WFNO170036
-

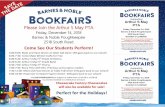






![[Armor] 6507 the GI in Combat - NW Europe 1944-45 [Concord]](https://static.fdocuments.in/doc/165x107/55cf98c3550346d0339987bf/armor-6507-the-gi-in-combat-nw-europe-1944-45-concord.jpg)










