ISSN: 1859-5138 Oen acce Original article · the midbrain is the ‘ ‘face of the giant panda’...
Transcript of ISSN: 1859-5138 Oen acce Original article · the midbrain is the ‘ ‘face of the giant panda’...
![Page 1: ISSN: 1859-5138 Oen acce Original article · the midbrain is the ‘ ‘face of the giant panda’ ’sign[6]. It consists of high signal intensity in the tegmentum, preservation](https://reader034.fdocuments.in/reader034/viewer/2022042405/5f1da78876bd541456289b75/html5/thumbnails/1.jpg)
Jaccr Africa 2020, Vol 4, Num 2 www.jaccrafrica.com
Journal of african clinical cases and reviews / Journal africain des cas cliniques et revues
www.jaccrafrica.com ISSN: 1859-5138 Open access
Brain MR Imaging Findings in Wilson’s disease
B Ould Cheikh Ahmed*1,2, S Azabi1,2, N Elbouardi1,2, H Abid1,2, S Bouchal1,2, B Alami1,2, M Boubbou1,2, M Maâroufi1,2, YAlaoui Lamrani Moulay1,2
AbstractObjective: The current study is an attempt to review the spectrum of intracranial MR features of Wilson disease in both children and adults.Materials and methods: Our sample in this restrospective study is sixteen patients with intracranial manifestations of Wilson disease, diagnosed on a 1.5 T MRI. We examined all the imaging and analyzed the different features according to their signal and localization.The results: Cerebral MRI confirmed the conclusion of Wilson’s disease cerebral localization. Based on the initial MR imaging findings, we were able to classify our patients into three different categories.Keywords: Wilson’s disease, Copper, MRI and panda sign.
Résumé Objectif : L’objectif de cette étude est de montrer l’intérêt de l’IRM dans le diagnostic et le suivie des atteintes cérébrales de la maladie de Wilson chez les enfants et les adultes.Matériels et méthodes : Etude rétrospective portant sur une série de 16 patients présentant des manifestations intracrâniennes de la maladie de
Wilson, nous disposons d’une IRM 1.5 T. Nous avons analysé les différents aspects caractéristiques des atteintes cérébrales de la maladie de Wilson en IRM. Les résultats : En fonction des résultats de l’IRM initiale on à diviser nos malades en groupes. Mots-clés. Maladie de Wilson, cuivre, IRM et signe du panda.
Introduction
Wilson’s disease is an autosomal recessive condition characterized by defective copper metabolism. It occurs in approximately one of every 30,000 people worldwide. It is not common before the age of 5, and Symptoms usually begin between the ages of 5 and 35 years. It affects both sexes equally [1].The cause of this condition is a deficiency in serum caeruloplasmin, which results in abnormal accumulation of copper, a heavy metal, in the liver initially, and subsequently in the brain and other organs. Excess copper attacks the brain resulting in neurological and psychiatric symptoms. Neurological manifestations are fundamentally
Résultats de l’IRM cérébrale dans la maladie de Wilson
Original article
![Page 2: ISSN: 1859-5138 Oen acce Original article · the midbrain is the ‘ ‘face of the giant panda’ ’sign[6]. It consists of high signal intensity in the tegmentum, preservation](https://reader034.fdocuments.in/reader034/viewer/2022042405/5f1da78876bd541456289b75/html5/thumbnails/2.jpg)
Jaccr Africa 2020, Vol 4, Num 2 www.jaccrafrica.com
B Ould Cheikh Ahmed and al. Jaccr Africa 2020; 4(2): 299-306
adopted protocol with a minimal sequence T2, T2 Flair, T1, the magnetic susceptibility sequence and diffusion. Some patients had gadolinium injection.
Results
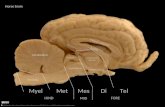
Imaging findings or procedure detailsDiagnosis of WD’s cerebral localization was confirmed by cerebral MRI. Using a 1.5 T. after the analysis of the initial brain MRI imaging, we divided our patients into 3 distinct categories: Category I: (n=3): normal MRI imaging findings (Figure 1), Category II (n=5): was characterized by T 1-weighted images with increased signal intensity in the basal ganglia (Figure 2), and Category III (n=8): demonstrated T 2-weighted images with increased signal intensity in the basal ganglia followed by the midbrain, and pons (Figures 3, 4). Among the latter group, some revealed hyperintense signals on diffusion (Figure 3).Seventy per cent of the patients with imaging abnormalities had exhibited bilateral and symmetric distribution. Sites of involvements were the globuspallidus (90%), putamen (50%), midbrain (40%), caudate nucleus (20%), thalamus (30 %), and pons (17%).
extrapyramidal syndrome consisting of resting and intention tremors, spasticity, rigidity and chorea. Dystonic signs have been described as well and comprised slowness of speech, unsteady gait, dystonic facies and posturing. In the bulk of patients, psychiatric symptoms are present and manifest by several forms of psychoses and neuroses[2].Imaging, in particular MRI, allows the diagnosis and follow-up under treatment. The precocity of both diagnosis and treatment affects the prognosis. We suggest studying Wilson’s disease’s MRI features through our series of 16 cases. Methodology
We report a retrospective study that evaluates 16 patients with clinical manifestations of Wilson disease, divided between: 06 men and 10 females with a mean age of 16 years (range from 7-32 years), seen during the period from February 2009 to September 2017. Patients were admitted with different symptoms: dysarthria, tremor, ataxia, rigidity/bradykinesia, tetra paresis, chorea/dystonia, and Hepatocellular insufficiency. All our patients underwent neurological examinations as well as magnetic resonance imaging (MRI) of the brain. Our
Fig1: WD in a 7-year-old man, normal MR imaging
![Page 3: ISSN: 1859-5138 Oen acce Original article · the midbrain is the ‘ ‘face of the giant panda’ ’sign[6]. It consists of high signal intensity in the tegmentum, preservation](https://reader034.fdocuments.in/reader034/viewer/2022042405/5f1da78876bd541456289b75/html5/thumbnails/3.jpg)
Jaccr Africa 2020, Vol 4, Num 2 www.jaccrafrica.com
B Ould Cheikh Ahmed and al. Jaccr Africa 2020; 4(2): 299-306
Fig 2 : WD in a 14-year-old female , MRI showed T1 hyper intense lesions involving bilateral thalami (black arrow) and normal T2(C).
Fig3: WD in a 10 years old female, rigidity, bradykinesia, tetra paresis. MRI revealed T2 and FLAIR hyper intense lesions involving bilateral basal ganglia (A, B), hypersignal on diffusion(C).
Fig4: WD in a 16-years-old female with dystonia, Cloning of the face and Hepatocellular insufficiency, MRI hyperintese T2(A) and flair(B) in bilateral basal ganglia (black arrow), pons and midbrain (red arrow).
![Page 4: ISSN: 1859-5138 Oen acce Original article · the midbrain is the ‘ ‘face of the giant panda’ ’sign[6]. It consists of high signal intensity in the tegmentum, preservation](https://reader034.fdocuments.in/reader034/viewer/2022042405/5f1da78876bd541456289b75/html5/thumbnails/4.jpg)
Jaccr Africa 2020, Vol 4, Num 2 www.jaccrafrica.com
B Ould Cheikh Ahmed and al. Jaccr Africa 2020; 4(2): 299-306
Figure 5: 10 years old female whose brother died because of Wilson’s disease, Hepatocellular insufficiency, MRI hyperintense T2 in the midbrain reflects the appearance of the “face of the giant panda”(high signal intensity in the tegmentum(red arrow), preservation of signal intensity of the lateral portion of the pars reticulata of the substantia nigra and red nucleus(small arrow).
Fig. 6: WD in 9 years-old female aggravation of neurological symptoms, MRI revealed hyper intense T2 in bilateral external border putamen (black arrow) and a small beach hypersintensitis T2 FLAIR of the left cortical and sub cortical frontal white matter (red arrow) (cortical and sub cortical deposits).
Fig7: 34 years-old man, suffering from WD with aggravation of neurological symptoms MRI hyper intense T2 and flair in bilateral lentiform nuclei(black arrow), with hypo intense beaches on T1 in both lenticular nuclei (red arrow) due to destructive changes.
![Page 5: ISSN: 1859-5138 Oen acce Original article · the midbrain is the ‘ ‘face of the giant panda’ ’sign[6]. It consists of high signal intensity in the tegmentum, preservation](https://reader034.fdocuments.in/reader034/viewer/2022042405/5f1da78876bd541456289b75/html5/thumbnails/5.jpg)
Jaccr Africa 2020, Vol 4, Num 2 www.jaccrafrica.com
B Ould Cheikh Ahmed and al. Jaccr Africa 2020; 4(2): 299-306
Fig 8: WD in a 15-years-old male under treatment, MRI revealed hypo intense on the magnetic susceptibility sequence. in bilateral caudate and lentiform nuclei nucleus (red arrow): hypo intensity consistent with magnetic susceptibility effect due to iron deposits.
Discussion
WD is a uncommon inborn genetic defect copper metabolism pathology which is characterized by deficiency of caeruloplasmin. The latter is the major copper-carrying protein in the blood. A variety of ATP7b genes are incriminated in the abnormally low level of caeruloplasmin. In the WD, cooper is not eliminated properly and accumulate in the liver and other organs such as the brain. The predilection site in the brain is the extrapyramidal system particularly in the putamen and globus pallidus[3]. The neurologic manifestations attributed to Wilson’s disease are understood to be secondary to nerve cells destruction. The three brains pathways affected frequently are: The dentatorubrothalamic tract, The corticospinal tract and the pontocerebellar tract. The histopathological changes that are observed in brain WD are edema, necrosis, and spongiform degeneration.Clinical presentation is non-specific and differs. Manifestations that have been described contain weakening of hands and dysarthria which are often the earliest symptoms and liver disease that is more seen in children and young adults[4].Wilson disease may present a wide spectrum
of clinical conditions, such as liver and/or neuropsychiatric disease. The diagnosis of WD requires a combination of clinical symptoms, biochemical, and detection of gene mutations, which are the foundation of a score proposed by a group of international experts. Pigmented rings in the peripheral cornea portrayed as Kayser Fleischer rings are a characteristic clinical feature. Biology test finds a low-level caeruloplasmin in the serum and an elevated urinary copper excretion. Anatomo-pathology confirms the diagnosis by liver biopsy. Radiology features in the brain are seen basically on MRI. The features depend on whether the disease is treated or untreated. The basal ganglia and midbrain are the mostly affected sites. Basal ganglia involvement comprises the putamen, globus pallidus, caudate nucleus and the ventrolateral thalamus.Brain CT does not give much information. It may reveal atrophic changes and hypodensities in the basal ganglia, cortical and cerebellar regions. Copper deposition in the brain does not increase density, and there is no particular enhancement pattern on CT[5]. MRI is the best imaging tool for the diagnosis. Not only does it offer biochemical information on copper distribution in brain tissue but it also presents an insight into the pathological and anatomical correlation of clinical signs and symptoms in WD. Interval changes seen on follow-up MR imaging have excellent correlation to clinical symptoms and can be useful in evaluating the clinical response to treatment of patients with WD.One of the characteristic feature of the WD in the midbrain is the ‘ ‘face of the giant panda’ ’sign[6]. It consists of high signal intensity in the tegmentum, preservation of signal intensity of the lateral portion of the pars reticulate, the substantia nigra, red nucleus, and hypo intensity of the superior colliculus. Furthermore, a “face of panda cub” is seen within the dorsal part of pons. “Eyes
![Page 6: ISSN: 1859-5138 Oen acce Original article · the midbrain is the ‘ ‘face of the giant panda’ ’sign[6]. It consists of high signal intensity in the tegmentum, preservation](https://reader034.fdocuments.in/reader034/viewer/2022042405/5f1da78876bd541456289b75/html5/thumbnails/6.jpg)
Jaccr Africa 2020, Vol 4, Num 2 www.jaccrafrica.com
B Ould Cheikh Ahmed and al. Jaccr Africa 2020; 4(2): 299-306
of the panda” are formed from the relative hypo intensity of the central tegmental tracts (CTT) in contrast with the hyper intensity of the aqueduct opening into the fourth ventricle (“nose and mouth of the panda”) bounded inferiorly by the superior medullary velum. The panda’s “cheeks” are formed from the superior cerebellar peduncles (Figure 5).Hyperintensity in the lentiform nuclei and mesencephalic regions on T1 has been described as the most common initial MRI abnormality (Figure 2+5) [7]. T2 hyper intensity is also seen typically involving the basal ganglia (Figure 6) [8]. There may be T2 hyper intensity in the outer rim of the deep gray matter, and/or T1 hyper intensity in cases of copper toxicosis (Figure 6), Axial T2 MR at midbrain level can show a face of giant panda sign, a characteristic finding of WD. Axial T2 MR at pons might also reveal the face of a miniature panda sign (mini giant panda). This combination is pointed out to as “double panda sign”[9].MRI of the brain is not only a useful diagnostic modality in WD but can also be used to assess disease severity and response to treatment. MRI changes are seen in almost all neurologically symptomatic patients. When patients have predominant hepatic involvement (figure7) [10] . Atrophy of the cerebrum and brainstem might be seen in long-standing cases. The exact pathogenesis of the superior colliculus hypointensity is unknown. It has been assumed that the paramagnetic effect of heavy metal deposition (e.g. iron, copper) may be responsible for this finding in WD. Iron deposition is more significant than copper for producing T2 hypointensity. Diffusion hyper intensity may be seen early in the course of the disease. It is known that such findings on diffusion MR images usually correspond to a restriction of mobility of water molecules and indicates the presence of cytotoxic edema (infarct and acute ischemia). In the case reported herein, however, such a mechanism was unlikely. As a result, bearing in mind that excess copper causes cell injury leading to inflammation and cell death, it is likely
that this finding mainly represented cell swelling associated with inflammation, hence constraint of diffusion (Figure3)[11]. The contribution of copper to the hypointensities is unknown. T1-weighted images may also show hypointensity in the most severely affected nuclei. This is probably because of destructive changes. (fig7). The Treatment can precipitate iron deposition, which translates into hypointensity in the magnetic susceptibility sequence[12] (Figure 8). The mainstay of therapy is permanent use of chelating agents (e.g. penicillamine, trientine). Surgical decompression or transjugular intrahepatic shunting (TIPS) is reserved for persistent or uncontrolled variceal bleeding unresponsive to standard conservative measures. Orthotropic liver transplantation is curative. Other treatments for WD include the following: Anticholinergics, baclofen, GABA antagonists, and levodopa to treat extrapyramidal signs. Antiepileptic’s to treat seizures. Neuroleptics to treat psychiatric symptoms. Lactulose, Protein restriction, or both to treat hepatic encephalopathy. Early diagnosis and treatment of Wilson’s disease can reduce or even prevent organ damage. People with a family history of the disease may also benefit from genetic testing that can identify one or more gene mutations [13].
Conclusion
Imaging especially the MRI plays a fundamental role in the initial positive diagnosis of Wilson’s disease as well as in the evaluation of therapeutic response. Features vary on whether the disease is treated or not. The basal ganglia and midbrain are the most frequently affected sites.
*Correspondence : Beiba Ould Cheikh Ahmed [email protected]
![Page 7: ISSN: 1859-5138 Oen acce Original article · the midbrain is the ‘ ‘face of the giant panda’ ’sign[6]. It consists of high signal intensity in the tegmentum, preservation](https://reader034.fdocuments.in/reader034/viewer/2022042405/5f1da78876bd541456289b75/html5/thumbnails/7.jpg)
Jaccr Africa 2020, Vol 4, Num 2 www.jaccrafrica.com
B Ould Cheikh Ahmed and al. Jaccr Africa 2020; 4(2): 299-306
Available online : May 06, 2020
1 Radiology Department, University Hospital Hassan II, 2 Faculty of Medicine and Pharmacy, Sidi Mohamed Ben Abdellah University, Fez, Morocco
© Journal of african clinical cases and reviews 2020 Conflict of interest : None
References
[1] T. J. Kim et al., « MR imaging of the brain in Wilson disease of childhood: findings before and after treatment with clinical correlation », AJNR Am. J. Neuroradiol., vol. 27, no 6, p. 1373-1378, juill. 2006.[2] E. A. Roberts, M. L. Schilsky, et American Association for Study of Liver Diseases (AASLD), « Diagnosis and treatment of Wilson disease: an update », Hepatol. Baltim. Md, vol. 47, no 6, p. 2089-2111, juin 2008, doi: 10.1002/hep.22261.[3] I. F. Scheiber, R. Brůha, et P. Dušek, « Chapter 5 - Pathogenesis of Wilson disease », in Handbook of Clinical Neurology, vol. 142, A. Członkowska et M. L. Schilsky, Éd. Elsevier, 2017, p. 43-55.[4] P. Ferenci, « Pathophysiology and clinical features of Wilson disease », Metab. Brain Dis., vol. 19, no 3-4, p. 229-239, déc. 2004, doi: 10.1023/b:mebr.0000043973.10494.85.[5] S. I. Harik et M. J. Post, « Computed tomography in Wilson disease », Neurology, vol. 31, no 1, p. 107-110, janv. 1981, doi: 10.1212/wnl.31.1.107.[6] J. R. Parekh et P. R. Agrawal, « Wilson’s disease: ‘face of giant panda’ and ‘trident’ signs together », Oxf. Med. Case Rep., vol. 2014, no 1, p. 16-17, avr. 2014, doi: 10.1093/omcr/omu005.[7] H. Mochizuki et al., « Atypical MRI features of Wilson’s disease: high signal in globus pallidus on T1-weighted images », Neuroradiology, vol. 39, no 3, p. 171-174, mars 1997, doi: 10.1007/s002340050386.[8] S. Kim, I. U. Song, Y. A. Chung, E. K. Choi, et J. K. Oh, « Brain MRI, Tc-99m HMPAO SPECT and F-18 FP-CIT PET/CT Findings in a Patient with Wilson Disease: A Case Report », Nucl. Med. Mol. Imaging, vol. 48, no 4, p. 303-305, déc. 2014, doi: 10.1007/s13139-014-0290-4.[9] D. A. Jacobs, C. E. Markowitz, D. S. Liebeskind, et S. L. Galetta, « The “double panda sign” in Wilson’s disease », Neurology, vol. 61, no 7, p. 969, oct. 2003, doi: 10.1212/01.wnl.0000085871.98174.4e.[10] Z.-H. Zhou et al., « Characteristics of neurological Wilson’s disease with corpus callosum abnormalities », BMC
Neurol., vol. 19, no 1, p. 85, mai 2019, doi: 10.1186/s12883-019-1313-7.[11] S. Mukherjee, B. Solanki, G. Guha, et S. P. Saha, « White matter changes in Wilson’s disease: A radiological enigma », J. Neurosci. Rural Pract., vol. 7, no 3, p. 447, sept. 2016, doi: 10.4103/0976-3147.176195.[12] X.-X. Zhou et al., « Characterizing brain mineral deposition in patients with Wilson disease using susceptibility-weighted imaging », Neurol. India, vol. 62, no 4, p. 362, janv. 2014, doi: 10.4103/0028-3886.141221.[13] S. Doganay et al., « Magnetic Susceptibility Changes in the Basal Ganglia and Brain Stem of Patients with Wilson’s Disease: Evaluation with Quantitative Susceptibility Mapping », Magn. Reson. Med. Sci., vol. 17, no 1, p. 73-79, mai 2017, doi: 10.2463/mrms.mp.2016-0145.[14] J. Yang et al., « Susceptibility-Weighted Imaging Manifestations in the Brain of Wilson’s Disease Patients », PLOS ONE, vol. 10, no 4, p. e0125100, avr. 2015, doi: 10.1371/journal.pone.0125100.[15] S. Hitoshi, M. Iwata, et K. Yoshikawa, « Mid-brain pathology of Wilson’s disease: MRI analysis of three cases », J. Neurol. Neurosurg. Psychiatry, vol. 54, no 7, p. 624-626, juill. 1991, doi: 10.1136/jnnp.54.7.624.[16] E. Masson, « Maladie de Wilson », EM-Consulte. [En ligne]. Disponible sur: https://www.em-consulte.com/article/779822/maladie-de-wilson. [Consulté le: 04-janv-2020].[17] pubmeddev et L. S. and G. E, « Normal functional imaging of the basal ganglia. - PubMed - NCBI ». [En ligne]. Disponible sur: https://www.ncbi.nlm.nih.gov/pubmed/12495872. [Consulté le: 04-janv-2020].[18] M. Grisoli, A. Piperno, L. Chiapparini, R. Mariani, et M. Savoiardo, « MR imaging of cerebral cortical involvement in aceruloplasminemia », AJNR Am. J. Neuroradiol., vol. 26, no 3, p. 657-661, mars 2005.[19] M. L. Schilsky, « Wilson disease: current status and the future », Biochimie, vol. 91, no 10, p. 1278-1281, oct. 2009, doi: 10.1016/j.biochi.2009.07.012.[20] P. J. Gow, R. A. Smallwood, P. W. Angus, A. L. Smith, A. J. Wall, et R. B. Sewell, « Diagnosis of Wilson’s disease: an experience over three decades », Gut, vol. 46, no 3, p. 415-419, mars 2000, doi: 10.1136/gut.46.3.415.[21] C. Saroli Palumbo et M. L. Schilsky, « Clinical practice guidelines in Wilson disease », Ann. Transl. Med., vol. 7, no Suppl 2, avr. 2019, doi: 10.21037/atm.2018.12.53.[22] A. Aggarwal et M. Bhatt, « Advances in Treatment of Wilson Disease », Tremor Hyperkinetic Mov., vol. 8, févr. 2018, doi: 10.7916/D841881D.
![Page 8: ISSN: 1859-5138 Oen acce Original article · the midbrain is the ‘ ‘face of the giant panda’ ’sign[6]. It consists of high signal intensity in the tegmentum, preservation](https://reader034.fdocuments.in/reader034/viewer/2022042405/5f1da78876bd541456289b75/html5/thumbnails/8.jpg)
Jaccr Africa 2020, Vol 4, Num 2 www.jaccrafrica.com
B Ould Cheikh Ahmed and al. Jaccr Africa 2020; 4(2): 299-306
To cite this article B Ould Cheikh Ahmed, S Azabi, N Elbouardi, H Abid, S
Bouchal, B Alami and al. Brain MR Imaging Findings in
Wilson’s disease. Jaccr Africa 2020; 4(2): 299-306