INVESTIGATION INTO THE LYMPHATIC VASCULAR SPREAD ... -...
Transcript of INVESTIGATION INTO THE LYMPHATIC VASCULAR SPREAD ... -...
Thorax (1956), 11, 172.
AN INVESTIGATION INTO THE LYMPHATIC ANDVASCULAR SPREAD OF CARCINOMA
OF THE BRONCHUS *BY
H. C. NOHLFrom the London Chest Hospital
(RECEIVED FOR PUBLICATION JANUARY 28, 1956)
The present investigation was carried out be-cause little work has been done to elucidate theproblems concerning the lymphatic spread ofbronchogenic carcinoma. The question, whetherthe treatment of carcinoma of the bronchus bylobectomy rather than by pneumonectomy isbased on sound pathological principles, neededclarification. It was also felt that the establish-ment of a surgical-pathological classification forthe purpose of prognosis and assessment of variousforms of treatment, as has been donz for cancerat other sites, was long overdue. Furthermore,the anatomy of the intrapulmonary lymphaticpathways described in the past are no longertenable in the light of our present knowledge ofthe bronchial and segmental anatomy of the lungs.
Rouviere (1932), in his classic Anatomie desLymphatiques de l'Homme, gives an excellentdescription of the mediastinal lymphatic path-ways and nodes, but that of the interlobar andintrapulmonary nodes is inaccurate and his workdoes not divide the lymph flow into lobar or seg-mental distribution. Since that time few contri-butions have been made in this field; papers byMcCort and Robbins (1951), Weinberg (1951),Borrie (1952), and that by Brock and Whytehead(1955) have touched on this subject. But all ofthese authors, with the exception of Borrie,reiterate, on the whole, Rouviere's statements oneither the lymphatic anatomy or the drainage ofthe lungs.
METHOD OF INVESTIGATIONOne hundred specimens of lung resected for
bronchogenic carcinoma were examined. Of these 71were pneumonectomies and 29 were lobectomies.They constitute a continuous series, except for threecases which were not investigated, as a growth was notsuspected at the time of the operation.
* An enlarged version of a paper read to the Thoracic Societyin London in March, 1955.
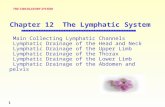
Each spezimen while still fresh and unfixed wascarefully cleared of all the visible lymph nodes, andtheir relationship to the nearest bronchus was notedand charted on a diagram (Fig. 1).
Vascular involvement was also looked for andp.eces of pulmonary vein were sent for histologicalexamination where invasion seemed most likely.Visceral or parietal pleural infiltration was noted andagain microscopic confirmation was sought. And,lastly, the situation and extent of the growth werecarefully recorded.Each lymph node was then sectioned after fixation
and two slides were made of each gland. A serialsection of each lymph node was not done, as it wouldhave entailed an insurmountable amount of work.
In all, 753 lymph nodes were histologicallyexamined, which means an average of 7.5 lymphnodes per specimen. Borrie, who undertook a similarinvestigation, found five lymph nodes per specimen.The growth itself was also examined and was de-
scribed as being one of four types (Table I).
TABLE IHISTOLOGICAL CLASSIFICATION OF CASES EXAMINED
Squamous cell carcinoma ..59Undifferentiated .28Adenocarcinoma.. 8Adeno- and squamous cell carcinoma ..
,, ,, undifferentiated cell carcinoma ..OatcelIcarcinoma. 3
Total .. .. 100
INCIDENCE OF LYMPH NODE INVOLVEMENT
The incidence of lymph node involvement wherepneumonectomies had been carried out was 88.8 %,while the incidence after lobectomy was only41.4%. The overall incidence of lymph nodeinvolvement in the 100 resected specimens wasthus 75%. This percentage is higher than theusual figures quoted (Table IL). In this series7.5 lymph nodes per specimen were found, whilein that of Brock and Whytehead, where " radical
on 21 May 2018 by guest. P
rotected by copyright.http://thorax.bm
j.com/
Thorax: first published as 10.1136/thx.11.3.172 on 1 S
eptember 1956. D
ownloaded from
LYMPHATIC AND VASCULAR SPREAD OF BRONCHIAL CARCINOMA 173
J~~~~~~~*
Name: Mr. H. L. Reg. No.. 44495
Type of growth Squamous cell carcinomaSituation of growth : Distal branch of anterior segmental bocu
TraheaPleural involvement : None
lperior Va}1 wii Trachcascular involvement: Infiltration of superior vena cava, part of which
P,tnor/ \ \- 1 \Iwas excised (perivascular). No pulmonary vein involvedi caval- l2-Oesophagus
I -Vena
Posterior'rior ]1 11 6 s ntal Lymph Nodesionary
A'bronchus I Pretracheal in superior mediastinum
2 Pretracheal attached firmly to superior vena cava, part ofwhichwasexcised. Mediallyextendingtoarchofaorta
1Apicallower32 } | ~~~lobc bronchus1lobe bronchus 4 Medial to (R) main bronchus
'ulmonary, <; 1/-5 Posterior to (R) main bronch us lower part
6 Lateral to (R) main bronchus-> t ~~Inferior pulmonairy 1diddle lobe. 1 v nvein /umnr 7 Inferior to anterior segmental bronchus of R.U.L.bronchus \f // 8 Superior to middle lobe bronchus
Pulmonary Malignant 9 Medial to lower lobe bronchus
ligament' Infiltration10 Lateral to and medial to middle lobe bronchus
Classification: A3 11 At the top of pulmonary ligarment
FIG. 1.-Chart which is used to record the site of the nodes dissected and examined histologically. It shows the nrediastiral aspect of theresected lung, with the mediastinal structures superimposed. The diagram, therefore, presents the mirror image of the orthodox view.
on 21 May 2018 by guest. P
rotected by copyright.http://thorax.bm
j.com/
Thorax: first published as 10.1136/thx.11.3.172 on 1 S
eptember 1956. D
ownloaded from
H. C. NOHL
TABLE IIINCIDENCE OF LYMPH NODE INVOLVEMENT
ACCORDING TO VARIOUS AUTHORS
Ochsner, Dixon, and DeBakey (1945) 58 resectedcases .
Rienhoff (1947) 112 pneumonectomiesWiklund (1951) 100 resected casesBorrie (1952) 200 resected casesSalzer and others (1952) 160 resected casesHigginson (1953) 62 pneumonectomiesBrock and Whytehead (1955) 109 " radical"pneumonectomies
London Chest Hospital (1954-55) 100 resectedcases
56-9%70.00%540°/48-0%;31 0%.60-6%
38-0%
75-0%
pneumonectomies" were performed, it is statedthat 30-40 lymph nodes per specimen wereexamined, and the percentage of cases showinglymph node involvement was 38% in the 109 caseswhere the state of glands is mentioned. Innecropsy series the incidence is, of course, verymuch higher and ranges from 75% (Simpson,1929) to 94% (Willis, 1953). It was often difficultto forecast from macroscopic appearances whethera lymph node was malignant or not. Often largefirm nodes were free from growth, while small,innocent-looking ones showed a secondary. Micro-scopic metastases are most likely to be foundunder the capsule of the node where the afferentlymphatic vessels open into the peripheral sinuses.
THE MACROSCOPIC ANATOMY OF THE LYMPHATICPATHWAYS OF THE LUNGS AS DEMONSTRATED BY
LYMPHATIC METASTASESAs previously stated, not much research has
been done in recent years on the lymphatic path-ways by which metastases from growths in varioussegments and lobes spread towards the hilar andmediastinal lymph nodes. For this reason the con-clusions drawn from the dissections done on the100 cases in this series are described in this sec-tion. However, in view of the fact that in themajority of cases the growth has involved morethan one segment, it is only possible to describethe lobar drainage with definite certainty.
RIGHT LUNG.-There was a total of 47 right-sided growths.Of these 19 growths were involving
18 growths 9..
2 growths ,. .
5 growths , .
2 growths , .
and 1 growth
the upper lobe,, lower lobe,, middle
lobe,, upper andlower lobesmiddle andlower lobes
,, upper andmiddle lobes
Table III shows the location of the variouslymph nodes on the right side of the chest andalso indicates the site of the growth of each par-ticular lymph node.
Figs. 2 and 3 indicate diagrammatically theanatomical position of the more important lymphnodes.Three hundred and forty-seven lymph nodes
were examined, of which 108 showed metastaticdeposits, giving an invasion rate of 31%. (Theinvasion rates for the various lobes are given inTable V.)On analysing Table III the following features
become apparent.
TABLE IIILYMPH NODES OF THE RIGHT LUNG
Site of Lymph Nodes
MediastinalPre-, para-, or retro-
trachealSubcarinal
Para-oesophageal
Pericardial or para-phrenic
In relation to upper partofright main bronchus
In relation to upper lobebronchus
In relation to upper lobeepampntal hronrhi
Not invadedInvadedNot invadedInvadedNot invadedInvadedNot invadedInvadedNot invadedInvadedNot invadedInvadedNot invadedInvaded
In relation to lower part Not invadedof right main bronchusj Invaded
In relation to middle lobe Not invadedbronchus Invaded
In relation to lower lobe Not invadedbronchus and segmen- Invadedtal branches
Pulmonary ligament .. Not invadedInvaded
Site of Growth
00
7 1 39 1 1 31310 1 2 1 16I15l li21;43 1~ 62 4
111 ~~~13
10 1 1 1 42 1 25 1 6118 10 161 2 1 1251 41 3 1 2510 1 1 11715 1 2 2 17613 1 3 131 3 7
2 1 43
Total, 347. Invaded, 108. Invasion rate, 31%.
Lower lobe growths metastasize upwards, evenoccasionally into the lymph nodes around thesegmental bronchi of the upper lobe. The sub-carinal and the para-oesophageal glands are ofteninvolved, while this seems to be a very infrequentevent with upper lobe growths.The most important lymph nodes from the sur-
gical point of view seem to be those in relation tothe lower part of the right main bronchus, i.e., thearea which lies between the upper lobe bronchusand the middle and apical lower lobe bronchi.This area was referred to by Borrie in hisHunterian Lecture as the "lymphatic sump" ofthe right lung. It is indicated in Fig. 2 by a circle,
174
,,9
on 21 May 2018 by guest. P
rotected by copyright.http://thorax.bm
j.com/
Thorax: first published as 10.1136/thx.11.3.172 on 1 S
eptember 1956. D
ownloaded from
LYMPHATIC AND VASCULAR SPREAD OF BRONCHIAL CARCINOMA
ap.s.br.= apical segmental bronchusap.s.br.l.l.=apical segmental bronchus of lower lobe.ap. s . br a.s.br. anterior segmental bronchus
o; . s.br. I.P.V.= inferior pulmonary veinM.L.B.= middle lobe bronchusP.A.= pulmonary arteryv t } >P.A.u.l.= pulmonary artery to upper lobeP.L. pulmonary ligamentPA.U.I.Vaobk ~~~~~~S.P.V.=superior pulmonary veinOes. =oesophagus
S.P.V. ~~~p.s.br. Tr.=tracheap.s.br.= posterior segmental bronchusS.V.C.-superior vena cava
Lymph Nodes:(I) Paraphrenic(2) Subcarinal
a.s.br.92t4v-1 {n) (3) Para-oesophageal(4) Paratracheal(5) Pretracheal(6) Retrotracheal
PA--~ (7) Pulmonary ligamento6p.s.br.1.1. l
one case which contradicts this observation, and
I.(Z2,t| P.V. one must assume that malignant obstruction ofM_L.B. 5 .the lymph channels caused a retrograde spread.
The lymphatic drainage with upper lobe growthsseems otherwise to be upwards, with the likelihood
Ptg.
Lof involvement of the para- and pretracheal glands.
FIG. 2.-Diagram showing the mediastinal aspect of the resectedright lung. The circle indicates the area which contains those /lymph nodesinto which both upper,rmiddle,andlowerlobes drain. J r 74Tr
shown between the two double lines in Table III. \ lThe collection of lymph nodes in this region is v/ (
frequently infiltrated from both upper and lower / ( Aorticlobe growths. This seems to have a bearing on c4I archtreatment of carcinoma by lobectomy. A car- |j /cinoma in the lower lobe, however small and peri-pheral, should, according to these observations,be treated by at least a lower and middle lob-ectomy. It is also essential to remove the tissues /most likely to contain the para-oesophageal, the \ t| 1 1subcarinal nodes, and those in the pulmonary \ .eA'/ligament. Churchill, Sweet, Soutter, and Scannell \(1950) seem to have included a middle lobectomy X | 2 L ) - A.for a growth confined to the lower lobe on \ /occasions. On the other hand obviously malignant \4 |nodes in this area will make a lobectomy techni- v - S.RV.cally impossible.
Upper lobe growths also metastasize to the St\t\
lymph nodes between the upper lobe bronchus I.P.V.and the middle and apical lower lobe bronchus.They do not, however, infiltrate the nodes below (\a line drawn from the middle lobe bronchus to the PL.\\ \\7 / RLapical lower lobe bronchus. The exception to this \rule are those upper lobe tumours which haverulearethose,upperlobetumourswhic h FIG. 3.-Diagram demonstrating the site of the most frequentlytransgressed the main fissure. However, there was found lymph nodes in the right mediastinum.
175
on 21 May 2018 by guest. P
rotected by copyright.http://thorax.bm
j.com/
Thorax: first published as 10.1136/thx.11.3.172 on 1 S
eptember 1956. D
ownloaded from
H. C. NOHL
FIG. 4a
FIG. 4b
Flo. 4c
FtG. 4.-This diagram illustrates the lymphatic drainage of the three lobes of the rightlu-ig. (4a) Upper lobe, (4b) middle lobe, (4c) lower lobe.
176
on 21 May 2018 by guest. P
rotected by copyright.http://thorax.bm
j.com/
Thorax: first published as 10.1136/thx.11.3.172 on 1 S
eptember 1956. D
ownloaded from
LYMPHATIC AND VASCULAR SPREAD OF BRONCHIAL CARCINOMA
a.p.s.br.= apico-posterior segmental bronchusap.s.br.l.l.=apical segmental bronchus lower lobe
P.a s. br. a.s.br. anterior segmental bronchus,.._*1.,.sw *ra.p. r. I.P.V.= inferior pulmonary vein
ling.br.= lingular bronchusP.A.= pulmonary artery
co.s. br. P.L. pulmonary ligamentS.P.V.= superior pulmonary veinRA.AQes.= oesophagusTr. trachea
Lymph Nodes:rspv ~~(1) Sbaia- 8gS.P.V.(2) Para-oesophageal
(3) Pulmonary ligament(4) Paraphrenic(5) Subaortic in region of recurrent laryngeal rcrve(6) Subaortic in region of ligamentum arteriosum(7) Para-aortic(8) Superior mediastinum
bronchus. This group really constitutes the bridgeof lymphatic tissue between the subcarinal and
ling.br. the right lateral or paratracheal nodes.
__I.P.V. LEFT LUNG.-Table IV and Figs. 5 and 6 repre-sent the conditions found on the left side of thechest.On this side 405 lymph nodes were found, of
___________________ __ _r__-P.L_. which 114 showed malignant invasion, which
FIG. 5.-Diagram showing the mediastinal aspect of the resectedleft lung. The circle indicates the region which contains the O\s_collection of lymph nodes to which both upper and lower lobesdrain.
/flQYSNs R \R't-ZZf-Tr.Infiltration of the subcarinal nodes by upper lobetumours, on the other hand, is very rare. Thismeans that an upper lobectomy is by itself an ( /inadequate operation where lymphatic clearanceis concerned. It should be combined with thedivision of the vena azygos and clearance of thelymph nodes around the trachea and, if technic-ally feasible, removal of all the glands around the PPA.pulmonary artery between the uppzr and apicallower lobe bronchi. Fig. 4 summarizes thesepoints. IS \ SM i1 04The anatomy of the mediastinal lymph nodes on
both sides of the chest (Figs. 3 and 6) is so well \v.described by Rouviere that no further descriptionof them need be given here. It suffices to saythat what here are described as the para-oesopha-geal glands are those of the posterior mediastnumin his nomenclature, the subcarinal nodes are theinter-tracheobronchial nodes, while the para-phrenic nodes are those which belong to the Lanterior or prevascular chain in his terminology. /Brock and Whytehead (1955) describe in additionan anterior tracheal group which lies in front of FIG. 6.-Diagram demonstrating the site of the most frequentlythe lowest part of the trachea and the right main found lymph nodes in the left mediastinum.
177
on 21 May 2018 by guest. P
rotected by copyright.http://thorax.bm
j.com/
Thorax: first published as 10.1136/thx.11.3.172 on 1 S
eptember 1956. D
ownloaded from
H. C. NOHL
TABLE IVLYMPH NODES OF THE LEFT LUNG
Site of Growth
Site of Lymph Nodes UpperUpper and LowerLobe Lower Lobe
Lobe
MediastinalIn anterior superior media- Not invaded 4
stinum or para-aortic . . Invaded 1(a) Rec. laryng.
Subaortic Lb. nerve Not invaded 30 7 13Sbotc(b) Ligamentumarteriosum Invaded 5 3 2
Subcarinal Not invaded 9 4 1Invaded 3 1 3
Para-oesophageal Not invaded 3 4Invaded 2 1
Pre- or paratracheal Not invaded 1Invaded 1
Pericardial or paraphrenic . . Not invaded 6 1Invaded 3 1
Parietal pleura .. Not invaded 3 1Invaded
In relation to upper lobe bronchus Not invaded 19 1 5Invaded 8 3 1
In relation to upper lobe segmen- Not invaded 30 2 13tal bronchi Invaded 14 7 2
Left main stem bronchus Not invaded 18 8 5Invaded 8 2 4
Between upper and lower lobe Not invadedl 32 31 11bronchus Invaded L7 1 5 14
In relation to lower lobe bronchus INot invaded 13 3 14and segmental branches Invaded 1 5 3
Pulmonary ligament Not invaded 9 6 12Invaded 1 3
Total, 405. Invaded, 114. Invasion rate, 28-1%.
means an invasion rate of 28.1 % as compared with31 % on the right side of the chest.There was a total of 53 left-sided growths.
Of these 28 growths were involving the upper lobe15 ,, ,, ,, ,, lower lobe10 ,, ,, ,, ,, upper and
lower lobesOn this side more lower lobe carcinomata in-
vaded also the upper lobe than on the right side.The nodes around the upper lobe bronchus and itssegmental branches often show metastases fromsuch neoplasms.The noteworthy features on this side were as
follows. There was only one paratracheal andone para-aortic node invaded. In both of thesecases the advanced upper lobe growth gave riseto extensive lymphatic invasion, and both patientsdied within four months of the operation. Thisseems to confirm the general opinion that on theleft side few growths drain upwards alongside thetrachea. Unlike the right side, upper lobe car-
cinomata have given rise to metastases in the sub-carinal gland. It may be that here the lymphaticdrainage crosses over to the other side to continueupwards in the right superior mediastinum.Radiological appearances in advanced cases oftenshow this contralateral spread. Warren and
Drinker (1942) demonstrated in dogs that thegreater portion of the total pulmonary lymphaticflow passes up into the right paratracheal chain,while only a small amount from the left upperlobe drains upwards in the left superior media-stinum. Weinberg (1951), who has been investi-gating the lymphatic flow by vital staining, usinga 4% solution of Pontamine sky blue at the timeof operation, noticed staining of the nodes in theopposite hemithorax in two cases in which deathoccurred 11 days after pulmonary resection. Thecross-staining had been carried through the sub-carinal and anterior mediastinal lymph nodes. Itmust also be remembered that the right para- andpretracheal nodes medial to the vena azygos doextend on occasions as far over to the left as thearch of the aorta (see Fig. 3) and are thus in closeproximity to the subaortic glands. Fig. 7 demon-strates a metastasis in a right " scalene node,"while the primary is situated in the left upper lobe.The important area from the surgical point of
view on the left side is the collection of lymphnodes lying between the upper and lower lobebronchus in the main fissure. This constitutes the" lymphatic sump," to use Borrie's phrase, on theleft side. It is indicated by a circle in Fig. 5 andlies between the bold rules in Table IV. Thelymph node situated above the apical lower lobesegmental bronchus and the node lying along theinferior border of the lingular bronchus belongto this group. These nodes frequently showedmalignant infiltration from both upper and lowerlobe growths. As on the right side, except for oneinstance, no upper lobe growth metastasized belowthis level.The nodes below the aortic arch in the region
of the recurrent laryngeal nerve and the ligamentumarteriosum were nearly always present, and in-volvement was in the majority of cases caused byupper lobe tumours. It is invasion of these nodeswhich causes recurrent laryngeal nerve paralysisin the more advanced cases.The other interesting finding was the frequent
invasion of the node situated between the anteriorsegmental bronchus and the lingular bronchus ofthe upper lobe in close proximity to the superiorpulmonary vein. It was this node which was fre-quently invading this vessel, necessitating intra-pericardial ligation at the time of operation.To sum up, the lymphatic spread on the left side
(Fig. 8): Left lower lobe growths metastasize up-wards, with frequent involvement of the nodeabove the apical lower lobe bronchus. The para-oesophageal and the nodes in the pulmonary liga-ment are liable to be invaded. The glands around
178
on 21 May 2018 by guest. P
rotected by copyright.http://thorax.bm
j.com/
Thorax: first published as 10.1136/thx.11.3.172 on 1 S
eptember 1956. D
ownloaded from
LYMPHATIC AND VASCULAR SPREAD OF BRONCHIAL CARCINOMA
the left main bronchus and the subcarinal nodesare also likely to be involved. Lower lobe tumoursoften transgress the main fissure. Such growthstend to metastasize also to the nodes in relationto the upper lobe bronchus and its segmentalbranches and the subaortic glands.
Left upper lobe growths similarly give rise tosecondaries in the node in the main fissure abovethe apical lower lobe bronchus and in the nodelying along the inferior border of the lingularbronchus. They do not, however, infiltrate nodesbelow this level. The nodes around the left mainbronchus are often involved. The subaortic nodesare liable to invasion and so are the subcarinalglands. Upward spread in the left superiormediastinum, on the other hand, seems to be rare.
In conclusion upper and lower lobectomy onthe left side, where technically feasible, shouldachieve a reasonably adequate lymphatic clearance.
COMPARISON OF INVASION RATES BETWEEN THEDIFFERENT LOBES
From Table V it will be seen that the lowerlobes carry a slightly higher invasion rate thanthe upper lobes. The cases where the middle lobe
INVASION RATES
FIG. 7.-The radiograph of a patient with a left upper lobe car-cinoma. Section of one of the lymph nodes overlying the rightscalenus anterior muscle in the same patient shows islands ofmalignant tissue (arrows).
R
TABLE VOF UPPER AND LOWER LOBESCOMPARED
Site of Growth No. of Nodes Nodes InvasionSiteofGrowth Cases Present Invaded Rate (%)
Right upper lobe 19 135 33 24-4Right upper and lowerlobe..5 32 11 33-8
Right lower lobe 18 143 47 32-8Left upper lobe 28 230 53 23Left upper and lower lobe 10 64 28 43-8Left lower lobe 15 111 33 29-7
was involved either alone or together with one ofthe adjacent lobes have been left out as the num-bers are too small.
Bignall and Moon (1955) in their large seriesof resected cases came to the conclusion that theleft lower lobe carries the worst prognosis. Thisfact could be explained by the findings of thisinvestigation. The invasion rate of the right lowerlobe is slightly higher than that of the left lowerlobe. This finding agrees with Borrie's similarinvestigation. The lower lobe growths on the leftside, however, have a frequent tendency to trans-gress the main fissure, 10 cases compared withfive on the right. When this occurs the invasionrate goes up to 43.8%. Furthermore a resectionon the left side cannot possibly deal with an un-noticed lymphatic spread to the opposite superiormediastinum.
179
on 21 May 2018 by guest. P
rotected by copyright.http://thorax.bm
j.com/
Thorax: first published as 10.1136/thx.11.3.172 on 1 S
eptember 1956. D
ownloaded from
H. C. NOHL
FIG. 8a
FIG. 8bFIG. 8.-This diagram illustrates the lymphatic drainage of the two lobes of the left lung. (8a) Upper lobe, (8b) lower lobe.
THE BRONCHIAL AND VASCULAR SPREAD OFBRONCHOGENIC CARCINOMA
PERIBRONCHIAL SPREAD.-During these dissec-tions it was observed that some very advancedgrowths had started at the periphery of the lungand were involving the parenchyma extensivelytowards the hilum. There were widespreadlymphatic metastases in these cases. The lumen ofthe bronchi showed no growth; they were
narrowed but not invaded. The pre-operativebronchoscopy was therefore negative in spite ofthe advanced state of affairs. In these cases wide-spread peribronchial lymphatic invasion hadoccurred.
INTRABRONCHIAL SPREAD.-The opposite findingwas extensive invasion of the submucous lymphchannels, so that the growth appeared to creepup the bronchus within its lumen only. In two
180
on 21 May 2018 by guest. P
rotected by copyright.http://thorax.bm
j.com/
Thorax: first published as 10.1136/thx.11.3.172 on 1 S
eptember 1956. D
ownloaded from
LYMPHATIC AND VASCULAR SPREAD OF BRONCHIAL CARCINOMA
X~~~~~~~~~~~~ ~ ~ ~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~..._q...... .
It4
FiG. 9.-Section obtained by bronchial biopsy. A submucouslymphatic vessel can.be seen containing malignant cells (arrow),while the bronchial mucosa shows normal ciliated epithelium.
cases an upper lobe growth was seen to advanceover the carina between the upper and the lowerlobe,3 down into the lower lobe bronchus,, blockingthe apical lower lobe bronchus. In these instancesthe lower lobe was otherwise free from growth.In a third patient, who did not come to operation,the growth had crept from the left main bronchusover the carina into the right main bronchus, asseen through the bronchoscope. Fig. 9 is theactual bronchial biopsy of this patient and showsthe infiltration of the submucous lymphaticvessels.The growth progresses in these cases within the
lumen by finally breaking through the mucosa.The lymphatic involvement will therefore alwaysbe more proximal than the actual growth as seenby the bronchoscopist. Any growth on the medialwall of the two main bronchi within 1 to 2 cm. ofthe carina must therefore be deemed inoperable.VASCULARSPREcAD.-It was surprising to find
how relatively infrequently the larger vessels wereinfiltrated by growth. The vessels can be traced
far into the tumour, being only cuffed, but notactually showing intimal invasion. Histologicalsections in these cases show infiltration of theperivascular lymphatics, running in the adventitiaof the vessel (Fig. 10). This makes it seem likelythat malignant emboli arise more often in thesmaller and thinner-walled vessels at the peripheryof the lung (Fig. 11).Aylwin (1951) found intimal invasion in 40%
of cases on examining the slides made fromprevious resections. But he states that a figurenearer to 60% can be reached by careful dissec-tion. The incidence of vascular involvement inthis series was only 30%.
A SURGICAL-PATHOLOGICAL CLASSIFICATIONIt was felt that a classification, such as has been
so successfully established for cancer at othersites, was urgently needed for carcinoma of thebronchus. If any form of treatment of thisdisease is to be compared with any other thera-peutic methods, it is essential to employ somescheme by which the extent of the growth andthe lymphatic and vascular involvement are re-corded. Even comparison of operative mortalityand survival figures between various published
I °.--2t ,,§.I'll
i w.#~~~~~~~~~~~~~~~" 4* .0* *: B n F.^ \
,sFi. pE - .t ?t ,w S~~~~~~~~~~~~~~~*.FIG. 1O.-Section showing malignant infiltration of the perivascular
lymphatic vessels of a small peripheral blood vessel (arrows).
181
on 21 May 2018 by guest. P
rotected by copyright.http://thorax.bm
j.com/
Thorax: first published as 10.1136/thx.11.3.172 on 1 S
eptember 1956. D
ownloaded from
H. C. NOHL
series seems meaningless without such grading.Whether with the aid of such a classification aprognosis can be given can only be ascertainedafter a lapse of time.
SALZER'S CLASSIFICATION OF CARCINOMA OF THEBRONCHUS (1951) MODIFIED
Salzer (1951) proposed such a classification:A Cases: Growth confined to the lung.B Cases: The tumour has reached the visceral
pleura, but has not infiltrated it.C Cases: The growth has infiltrated by con-
tinuity the neighbouring structures, e.g., chest wall,pericardium, oesophagus, etc.
Lymph Node InvolvementO=No lymphatic metastases.I= Infiltration of the intrapulmonary nodes has
occurred.2=The interlobar or hilar nodes are metastasized.3=The mediastinal nodes show invasion.4= Distal metastases are present, e.g., supra-
clavicular nodes, liver metastases, etc.Vascular Involvement
V=There is demonstrable invasion of the intimaof the pulmonary veins.This scheme was adopted in this series with only
slight modifications. Salzer classifies a case intothe B category when the growth encroaches on to ~~~~.
FIG. 12.-This section demons rates malignant infiltration of thesubpleural plexus of lymphatic vessels.
FIG. 11.-A malignant thrombus can be seen within the lumen of asmall blood vessel.
the visceral pleura without infiltrating it. Theremust be adhesions over this area obliterating thepleural space. He makes this latter point becauseof the likelihood of lymphatic spread across theadhesions to the chest wall. It was thought thatthe presence of adhesions was not essential toclassify a case into the B category. The risk ofinfiltration of the subpleural plexus seemed to besufficient to distinguish such a case from an A case(Fig. 12). There will then be the added risk ofpleural metastases and spread across the fissuresvia lymphatic channels which Ninfo (1950) hasbeen able to demonstrate.The other modification deemed necessary was
the introduction of an extra category indicatingconfirmed vascular involvement, as this makes theprognosis obviously worse. Such cases are desig-nated as V cases.
Fig. 13 illustrates by examples the applicationof this classification.Wurnig (1954), from the same clinic in Vienna,
recently reviewed 158 patients, who had left thehospital at least three years previously after sur-
182
on 21 May 2018 by guest. P
rotected by copyright.http://thorax.bm
j.com/
Thorax: first published as 10.1136/thx.11.3.172 on 1 S
eptember 1956. D
ownloaded from
LYMPHATIC AND VASCULAR SPREAD OF BRONCHIAL CARCINOMA
Al case B2 case
C3 case Av3 caseFIG. 13.-Illustration by exampks of the application of Salzer's modified classification.
gical resection for bronchogenic carcinoma. Theyall had been classified according to Salzer's scheme.During the first 18 months after operation therewas a rapid decline in the percentage of survivors.After this period 51 % of the A cases were deadas compared with 83% of the C cases, while theB cases took up an intermediate position. Afterthis initial drop in the percentage of survivors inthe first 18 months, th2 percentage curve levelsout, to become almost horizontal after four years.The interesting facts are that after four years 35%of survivors are found in the A category with nolymph nodes involved, while only 18% of the Acases with intrapulmonary or hilar lymph nodemetastases are alive. Among the B cases thereare only 15% of patients living and this figureapproaches the percentage of the few C survivors,of whom only 12% are alive. This seems to sug-
gest that not only is this classification valid whereprognosis is concerned, but that it also serves asa yardstick when assessing various forms of treat-ment. Furthermore, his investigation suggeststhat it is justifiable to retain the B category as aseparate entity.
ANALYSIS OF THE PRESENT MATERIAL ACCORDINGTO SALZER'S CLASSIFICATION
The 100 cases presented here have thereforebeen analysed according to the above proposedclassification (Table VI). The following facts be-come apparent on analysis. In 60% of the un-differentiated cases the mediastinal lymph nodeswere infiltrated with growth (column 3) while thishappened in only 34% of the squamous cell car-cinomata. Every one of the three oat cell car-cinomata showed mediastinal lymph node involve-
183
on 21 May 2018 by guest. P
rotected by copyright.http://thorax.bm
j.com/
Thorax: first published as 10.1136/thx.11.3.172 on 1 S
eptember 1956. D
ownloaded from
H. C. NOHL
TABLE VI100 CASES ANALYSED ACCORDING TO SUGGESTED CLASSIFICATION
Lymphatic Involvement Vascular Extent of GrowthType _____--Involvement
0 1 2 3 4 V A B C
Squamous cell carcin-oma (59 cases) . 16 (27%) 6 (10.2%) 16 (27%) 20 (34%) 1 (1-7%) 14 (23-7%) 26 (440) 20 (34%) 13 (22%)
Undifferentiated car-cinoma (28 cases) .. 5 (17%) - 6 (21-4%) 17 (607%) - 11 (40%) 8 (28 6%) 12 (42-8%) 8 (28 6%)
Adenocarcinoma(8 cases) .. .. 3 (37.5%) 1 (12-5%) - 4 (50%) - 2 (25%) 3 (3755%) 3 (37.5%) 2 (25%)
Adeno- and squamouscellcarcinoma (1 case) 1 I_ _ _ - 1 _
Adeno- and undiff. cellcarcinoma (1 case). _ 1 1 - - 1
Oat cell carcinoma (3cases) .. .. _ _ - 3(100%) - 2(666%) 2 (666%) - I (33 3%)
ment. On the other hand, 37.2% of the squamous
growths showed either no lymphatic metastases or
only infiltration of the intrapulmonary nodes(columns 0 and 1) compared with 17% of the un-
differentiated group. The difference between thetwo types is also shown in the vascular involve-ment, viz., in 40% of the undifferentiated neoplasmsvenous intimal invasion was demonstrated, whilethis was only possible in 23.7% of the squamous
growths. It was surprising to find that the differ-ence between the two types, where the extent ofthe growth was concerned, was not so striking.The number of adenocarcinomata is too small forany conclusions to be drawn.
COMPARISON BETWEEN PERIPHERAL AND CENTRALTUMOURS
It was also thought that it might be interestingto analyse these cases from the point of view ofperipheral tumours as compared with centralgrowths. Opinions still seem to be divided as towhich type carries the better prognosis. Rabinand Neuhof (1934) were the first to make a dis-tinction between the "peripheral, circumscribedtumours " and the "central non-circumscribed,infiltrating type of growths." They maintainedthat the former carried a better prognosis thanthe central type, because of moderate or latelymph node metastases. In the same issue of theJournal of Thoracic Surgery, a paper by Tuttleand Womack (1934), however, comes to the
opposite conclusion. They classed " peripheraltumours" as those situated distal to the firstbifurcation of the major bronchus, and these carrya worse prognosis than their " major bronchustumours." The definition of peripheral growthsin this investigation was: " Tumours invisible onbronchoscopy, confirmed later by dissection of thespecimen." There were, in all, 41 peripheraltumours to 59 central growths. Among the centralgrowths there were two cases where the pre-opera-tive bronchoscopy was negative, but where the dis-section later showed that the growth ought to havebeen seen.Table VII shows the relationship between the
site of the growth and the histological type. The
TABLE VIIRELATION BETWEEN SITE OF GROWTH AND HISTO-
LOGICAL TYPE
Central Peripheral
Squamous cell carcinoma (59 cases) 39 (66%) 20 (34%)Undifferentiated carcinoma (28 cases).. 15 (53%) 13 (47%)Adenocarcinoma (8 cases) 2 (25%j) 6 (75%)Other types (5 cases) . . 3 2
distribution agrees roughly with the findings ofother authors (Wiklund, 1951; Walter and Pryce,1955), especially the observation that adenocar-cinomata are more often peripheral tumours, whilethe squamous cell carcinomata tend to be more
centrally situated.
TABLE VIIIANALYSIS OF TYPES ACCORDING TO SUGGESTED CLASSIFICATION
Lymphatic Involvement Vascular Extent of GrowthType Involvement
0 1 2 3 4 V A B C
59 central tumours .. 13 (22%) 3 (5-1%/) 16 (27-1%) 27 (45-8%) - 21(35.7%) 24 (40 8%) 19 (321%) 16 (27-1%)41 peripheral tumours 12 (29-3%) 5 (12-2%) 5 (12-2%) 18 (43-9%) 1 (2-4%) 10 (24-4%) 17 (41-5%) 15 (36-6%) 9 (21-9%)
184
on 21 May 2018 by guest. P
rotected by copyright.http://thorax.bm
j.com/
Thorax: first published as 10.1136/thx.11.3.172 on 1 S
eptember 1956. D
ownloaded from
LYMPHATIC AND VASCULAR SPREAD OF BRONCHIAL CARCINOMA
Table VIII shows the analysis of the two typesaccording to the suggested classification. Accord-ing to these findings there is statistically no differ-ence between the two types where the extent ofthe growth and the lymphatic involvement areconcerned. The demonstrable vascular involve-ment is slightly higher with central growths. Thismay, however, be due to the difficulty of demon-strating vascular invasion in the small peripheralvessels.
SUMMARY
A hundred* specimens of lungs, resected forbronchogenic carcinoma, have been dissected todetermine the site and extent of the growth, andvascular and lymphatic involvement.The findings and conclusions drawn from this
investigation are:(1) The incidence of lymph node involvement
in the 100 cases was 75%.(2) There is a constant lobar lymphatic drain-
age, which is described in detail.(3) Lobectomy for bronchogenic carcinoma,
where technically feasible, is a sound procedurefrom the pathological point of view.
(4) A comparison of lymphatic invasion ratesbetween the different lobes shows that tumoursof the lower lobes on each side have a greatertendency to metastasize than those of the upperlobes, and that if the tumour transgresses thefissure the invasion rate rises significantly.
(5) A surgical-pathological classification, as hasbeen established for cancer at other sites, is pro-posed. It records the extent of growth, thelymph node infiltration, and the vascular involve-ment. The purpose of the scheme is to allowcomparisons to be made between different formsof treatment, study the different behaviour of thehistological types of growths, and assess in futurethe prognosis of each case.
(6) With the aid of this classification the 100resected cases have been analysed and the follow-ing findings ascertained:
(a) Of the squamous carcinomata 37.2% showedeither no lymphatic involvement or only infiltra-tion of the intrapulmonary nodes as comparedwith 17% of the undifferentiated carcinomata.
*Since this paper was submitted a further 75 lungs have beendissected and classified, making 175 lungs in all. The results obtainedfrom these further dissections fully substantiate the facts and state-ments set out in this paper.
(b) The mediastinal lymph node involvement ofthe two types was 34% as compared with 60.7%(squamous carcinoma to undifferentiated car-cinoma).
(c) There was also a difference in the incidenceof vascular involvement 23.7% to 40% (squamousto undifferentiated carcinomata).
(d) There was no significant difference betweenthe histological types where the extent of growthwas concerned.
(e) The peripheral tumours behave in exactlythe same way as the central tumours where theextent of the growth and the lymph node involve-ment are concerned. The vascular infiltration isonly slightly more frequent in the central growths,but this may be due to difficulty in demonstratinginvasion in the small peripheral vessels, which isthought to occur more frequently, for reasonsstated.
(7) The observation that squamous cell car-cinomata are more often centrally than peripher-ally located (66% to 34%) and the adenocarcino-mata are in the majority of cases peripheraltumours agrees with the observations by otherauthors.
In conclusion I would like to thank the surgicalstaff of the London Chest Hospital for their encourage-ment, and especially Dr. K. F. W. Hinson for muchhelp and advice. To him and his laboratory tech-nician, Mr. V. Jones, this investigation meant a con-siderable increase of work, and I am truly grateful toboth of them. My thanks are also due to Miss Y.Reeves for secretarial work.
REFERENCES
Aylwin, J. A. (1951). Thorax, 6, 250.Bignall, J. R., and Moon, A. J. (1955). Ibid., 10, 183.Borrie, J. (1952). Ann. roy. Coll. Surg., 10, 165.Brock, R., and Whytehead, L. L. (1955). Brit. J. Surg., 43, 8.Churchill, E. D., Sweet, R. H., Soutter, L., and Scannell, J. G.
(1950). J. thorac. Surg., 20, 349.Higginson, J. F. (1953). Ibid., 25, 582.McCort, J. J., and Robbins, L. L. (1951). Radiology, 57, 339.Ninfo, G. (1950). Policlinico, Sez. prat., 57, 1213.Ochsner, A., Dixon, J. L., and DeBakey, M. (1945). Clinics, 3, 1187.Rabin, C. B., and Neuhof, H. (1934). J. thorac. Surg., 4, 147.Rienhoff, W. F. (1947). Ann. Surg., 125, 541.Rouvisre, H. (1932). Anatomie des Lymphatiques de l'Homme.
Masson, Paris.Salzer, G. (1951). Wien. med. Wschr., 101, 102.- Wenzl, M., Jenny, R. H., and Stangl, A. (1952). Das
Bronchuscarcinom. Springer Verlag, Wien.Simpson, S. L. (1929). Quart. J. Med., 22, 413.Tuttle, W. C., and Womack, N. A. (1934). J. thorac. Surg., 4, 125.Walter, J. B., and Pryce, D. M. (1955). Thorax, 10, 117.Warren, M. F., and Drinker, C. K. (1942). Amer. J. Physiol., 136,
207.Weinberg, J. A. (1951). J. thorac. Surg., 22, 517.Wiklund, T. (1951). Acta chir. scand., Suppl. 162.Willis, R. A. (1953). Pathology of Tumours, 2nd ed. Butterworth,
London.Wurnig, P. (1954). Thorax-Chirurgie, 2, 281.
185
on 21 May 2018 by guest. P
rotected by copyright.http://thorax.bm
j.com/
Thorax: first published as 10.1136/thx.11.3.172 on 1 S
eptember 1956. D
ownloaded from