Investigating TNF inhibition of IGF-1 signalling via …...Investigating TNF inhibition of IGF-1...
Transcript of Investigating TNF inhibition of IGF-1 signalling via …...Investigating TNF inhibition of IGF-1...

Investigating TNF inhibition of IGF-1
signalling via JNK in cell culture models of
skeletal muscle atrophy
Bijanka L. Gebski
This thesis is presented for the degree of Doctor of Philosophy
School of Anatomy and Human Biology
The University of Western Australia
2009

ii
Dedication
This thesis is dedicated to the wonderful women in my family, especially my mother.
You are all so very different, yet have met life’s challenges with enormous strength and
dignity. The determination to rise above any challenge, and the attitude of ‘becoming
stronger’ as a result of the journey are the most powerful qualities one may endeavour
to behold. I will be forever grateful for your guidance and inspiration.

iii
Abstract
The pro-inflammatory cytokine tumour necrosis factor (TNF) has a critical role in
skeletal muscle atrophy. The catabolic effect of TNF is partially due to abrogation of the
anabolic insulin-like growth factor 1 (IGF-1) signalling pathway. However, the precise
signalling events that lead to the loss of myofibrillar protein following activation of
TNF receptor are unknown.
The over arching aim of the study is to determine the mechanisms of by which TNF
induces atrophy in differentiated muscles cells. To achieve this aim a series of
experiments were performed to: 1) investigate the molecular events that lead to TNF
mediated myofibre atrophy, 2) determine to what extent c-Jun N-terminal Kinase (JNK)
signalling plays a part in TNF induced myotube atrophy, and in TNF-mediated
inhibition of IGF-1 induced hypertrophy, and 3) use inhibitors of JNK to block the
catabolic effects of TNF.
1) To investigate the molecular events that lead to TNF mediated myofibre atrophy, the
experiments were conducted using C2C12 mouse myotube cultures and primary
myotube cultures derived from FVB mice, and transgenic mice which over-express
Class 2 IGF-1 Ea in skeletal muscles (IGF:C2). The treatment of mature C2C12 and
FVB primary myotubes (respectively at 7 and 4 days after fusion medium) with 10
ng/mL of TNF for 3 days resulted in statistically significant myotube atrophy
(decreased mean width). The observed TNF-mediated atrophy has not previously been
demonstrated in tissue cultured myotubes. In contrast, addition of IGF-1 (20 ng/ml) to 7
day C2C12 myotubes for 3 days resulted in significant hypertrophy. Where exogenous
combinations of TNF and IGF-1 were added to the C2C12 myotubes, the atrophic effect
of TNF was prevented (and conversely the hypertrophic effect of IGF-1 was prevented).
Furthermore, when TNF was added to the IGF:C2 myotube cultures, there was no
statistically significant difference between the mean size of the TNF treated myotubes,
compared to the untreated IGF-1:C2 myotubes. These results taken into consideration
demonstrate the protective effect of IGF-1 against TNF induced atrophy.

iv
2) To assess the role of JNK signalling in TNF induced myotube atrophy, it was first
necessary to determine if TNF induced JNK phosphorylation in day 7 C2C12 myotubes.
Signalling studies confirmed that treatment with TNF (20 ng/ml) for 10 min was
sufficient to induce JNK phosphorylation in the C2C12 myotubes. Three JNK inhibitors
(2 ATP-competitive; SP600125 and AS601245 and 1 ATP-non-competitive; TAT-
TIJIP) were assessed for biological toxicity in C2C12 myotubes. The most suitable
inhibitor was TAT-TIJIP and was thus used in subsequent studies. Inhibition of JNK
activity by TAT-TIJIP was confirmed indirectly by detecting nuclear translocation of c-
Jun, which is a downstream target of phosphorylated JNK. Immunohistochemical
analyses showed nuclear localisation and phosphorylation of c-Jun in TNF treated
myotubes. Nuclear localisation and phosphorylation of c-Jun was not observed in
cultures pre-treated with TAT-TIJIP before TNF treatment, nor in the untreated control
myotubes.
3) The use of JNK inhibitors to block the catabolic effects of TNF was tested using
C2C12 and primary myotube cultures. Pre-treatment of C2C12 and primary FVB
myotubes with the JNK inhibitor TAT-TIJIP, 30 min before TNF administration (for 3
days) prevented myotube atrophy. The mean width of myotubes pre-treated with TAT-
TIJIP prior to TNF treatment closely resembled that of the control myotubes.
Administration of TNF in combination with TAT-TIJIP for 3 days to C2C12 myotubes
prevented myotube atrophy and unexpectedly resulted in hypertrophy when compared
to the mean widths of untreated and TAT-TIJIP treated myotubes. This trend was also
demonstrated in the FVB primary cultures. These combined results strongly support the
role of JNK in TNF-mediated atrophy. Preliminary studies were carried out in vivo
using the mdx mouse model of muscular dystrophy, TAT-TIJIP was administered via
intraperitoneal injection to the mice for 3 days at a dose of 10 mg/ml, however the
results form this study are inconclusive.
These novel observations are of considerable interest to the field of muscle wasting
because they demonstrate for the first time TNF-mediated myotube atrophy, the role of
JNK in situations of TNF induced muscle atrophy, and explore the use of JNK
inhibitors to prevent muscle atrophy.

v
Acknowledgments
I would like to acknowledge and thank the following people for their contributions:
Professional
I would like to thank my supervisors Professor Miranda Grounds and Dr Thea
Shavlakadze from the School of Anatomy and Human Biology, UWA for their interest
in my work and with assisting me in compiling this thesis. I also acknowledge my
external supervisor Dr Marie Bogoyevitch; formerly from the School of Biomedical,
Biomolecular & Chemical Sciences, UWA but now located at Department of
Biochemistry and Molecular Biology, University of Melbourne, Victoria.
I would also like to thank Dr Jon Whitehead (Head, Cell Signalling Group, Diamantina
Institute for Cancer, Immunology and Metabolic Medicine, Princess Alexandra
Hospital, University of Queensland) for taking the time to help me optimise IRS-1 assay
and for allowing me to undertake supervised experiments at your laboratory.
This research was made possible by generous funding from the National Health and
Medical Research Council of Australia and a Postgraduate scholarship from UWA.
Personal
Completing this thesis would not have been anywhere near possible if it was not for the
continuous support from:
My amazing (and very entertaining) family; especially Mum and Dad for believing in
me, loving me, supporting me for so very long and never giving up on the idea that B
will one day finish! Dan for your continuous, continuous and then some more support
when I needed it the most. You are an amazingly strong person, I don’t know how you
do it, and I admire you for that, thank you Frank. My grandmothers: Baba for gluten
free meals on wheels and Nanna for the stories and favoured envelopes of cash. Aunty

vi
Barb for ever and always the ‘you can do it be’ emails, Optus ‘20 minute free time’
counselling sessions, couture inspired gifts, fashion and trash mags (!) and for being my
#1 fashion spend supporter (now what can I blame when I buy that ludicrously over
priced item, PhD is done!). Uncle Alan, for as materialistic and self absorbed as it
sounds (Gen Y, Al), the ‘therapeutics’ (please never leave Bacardi Lion!!). Aunty Don
for being Aunty Don - knowing that there was always a place to go when I needed to
‘unload’ and be fed at the same time was so very important to my mental and physical
well being. Uncle Greg, thanks for getting great jobs so that I had a place to stay in
Melbourne and the home-away-from-home, Mt Lawley residence.
ALL my friends!! You guys are ‘A’! The girls (Liv, Nat, Lozza, Mallis, Donna,
Chantelle); thanks so much for sticking by and continually asking me to ‘come out b’
when you knew too well that I had ‘uni on’ of had ‘to do my thesis’. Microbio friends;
Carmel and Janie - we all (eventually) made it out onto the other side, and for that we
are tops! Chantelle, deli days made me strong, but the ability to digest more gluten than
ever is all thanks to you. Thea Shav, thank you. When I took over your seat in room
2.36 I had big shoes to fill. Thanks for sharing many laughs (and tears) with me over
numerous ‘nosh-ski’ dinners, ‘muddies’ and for good times NYC. You are so strong
shav, thanks for making me ‘get on with it’ when I really, really didn’t want to
anymore. You are a ‘tops’ friend. Girls - you are all very special to me and I am very
lucky to have wonderful friends like you.
Room 2.36; what an experience that was. I could never have dreamt that by enrolling in
a PhD I would also be sharing an office with an amazing group of hilariously funny,
intelligent, witty and determined people, with whom I would form incredibly strong
friendships. Thanks guys. The ‘ghetto’ party crew of 2008 (well wicked) and not to
forget ‘tissue couture good times’. Special thanks to Marg for getting me thru the
toughest times of my PhD, you were my ‘mum’ away from home.
Jason; thank you for providing the inspiration I so desperately needed through all things
art, music, anime, Hayao Miyazaki, Murakami and the beautiful books. If it wasn’t for
you I would not have stayed at the job for any longer than 2 months and would have had
to leave 18/33 Third Ave.

vii
My Iaido Sensei Jason Anstey, thank you for guiding me while I travel on my path of
understanding the complexity of the Japanese sword and the concept of budo.
And a big thank you to Talijancich Winery; Tali family, you are amazing! Thank you
for being such wonderful friends (and employers!) and for producing my most favourite
wine, the ‘Talijancich Viognier’. To my new colleagues at PwC; thanks so much for
understanding that I had to go home (and not Bar One) to write this thesis, and here it
is! ☺

viii
Declaration
I hereby declare that the work contained within this thesis is entirely my own.
___________________________
Bijanka Gebski
May 2009

ix
Table of Contents
Title ................................................................................................................................. i
Abstract ......................................................................................................................... ii
Acknowledgements ................................................................................................... iv
Declaration ................................................................................................................... v
Table of Contents ...................................................................................................... vi
List of Figures............................................................................................................xii
List of Tables ............................................................................................................. xv
Abbreviations ........................................................................................................... xvi
Chapter One: Introduction Overview .............................................................................................................. 1
1.1 Skeletal muscle .............................................................................................. 2
1.2 Physiological and pathological remodelling of skeletal muscle ................ 3
1.2.1 Skeletal muscle hypertrophy ............................................................ 3
1.2.2 Skeletal muscle atrophy ................................................................... 3
1.3 Duchenne Muscular Dystrophy ................................................................... 5
1.3.1 The molecular basis of Duchenne Muscular Dystrophy .................. 5
1.3.2 Mdx mouse model of DMD ............................................................. 6
1.3.2.1 Mdx mouse, muscle necrosis and voluntary exercise ....... 7
1.4 Insulin like Growth Factor -1 (IGF-1) ....................................................... 8
1.4.1 Protein analogues of IGF-1: naturally occurring and synthetic ...... 9
1.4.1.1 Naturally occurring IGF-1 isoforms ................................. 9
1.4.1.2 Naturally occurring analogue of IGF-1: Des(1-3)IGF-1... 9
1.4.1.3 Synthetic analogue of IGF-1: LONGTMR3IGF-1 ............. 9
1.4.2 IGF-1 signalling in skeletal muscle cells ....................................... 10
1.4.3 The protective benefits of IGF-1 for muscle wasting conditions:
IGF-1 over expressing animal model...................................................... 13
1.5 Tumour Necrosis Factor (TNF) ................................................................ 13
1.5.1 TNF exacerbates muscle damage................................................... 16

x
1.5.2 TNF activates c-Jun N-terminal Kinase (JNK).............................. 17
1.5.3 IGF-1 and TNF cross talk: involvement of JNK............................ 18
1.5.4 Inhibitors of JNK Kinases.............................................................. 21
1.5.4.1 ATP-competitive ............................................................. 21
1.5.4.2 ATP-non-competitive...................................................... 22
Aims and Hypothesis of the Thesis .................................................................... 23 Overall Aim ....................................................................................................... 23
Specific Aims...................................................................................................... 23
Hypothesis .......................................................................................................... 23
Chapter Two: Materials and Methods ............................................................. 24 2.1 Cell Culture ................................................................................................. 24
2.1.1 Immortalised muscle cell lines....................................................... 24
2.1.1.1 C2C12 murine myotube cultures .................................... 24
2.1.1.2 L6 rat myotubes cultures................................................. 24
2.1.2 Animal strains ................................................................................ 24
2.1.2.1 Animals used for primary muscle cell culture
preparations ................................................................................. 25
2.1.2.2 Animals used to test the effects of the JNK inhibitory
peptide TAT-TIJIP ...................................................................... 25
2.1.3 General cell culture conditions....................................................... 25
2.1.3.1 Preparation of primary cell cultures................................ 25
2.1.3.2 Resurrection of cyropreserved cell stocks....................... 26
2.1.3.3 Trypsinising and seeding sells onto plates ...................... 27
2.2 Reagents and Antibodies ............................................................................ 29
2.2.1 Treatment reagents ......................................................................... 29
2.2.2 JNK Inhibitory peptides ................................................................. 29
2.3 Antibodies .................................................................................................... 30
2.3.1 Western blotting ............................................................................. 30
2.3.2 Immunohistochemistry................................................................... 30
2.4. Myotube morphology studies .................................................................... 30
2.4.1 Treatment regime for myotube cultures......................................... 30

xi
2.4.2 Immunohistochemistry................................................................... 31
2.4.3 Image analysis: measuring myotube widths .................................. 31
2.4.4 Statistical analysis .......................................................................... 33
2.5 Western blot quantitation of JNK phosphorylation in Day 7 C2C12
myotubes ............................................................................................................ 33
2.5.1 Treatment regime for western blot analysis of phospho-JNK ....... 33
2.5.2 Extraction and sample preparation................................................. 34
2.5.3 Protein quantitation ........................................................................ 34
2.5.4 Protein Sample Preparation............................................................ 35
2.5.4.1Whole cell lysates ............................................................ 35
2.5.4.2 Immunoprecipitation of IRS-1 ........................................ 35
2.5.5 SDS Polyacrylamide Gel Electrophoresis (SDS-PAGE) .............. 35
2.5.6 Protein transfer for western blotting .............................................. 37
2.5.7 Blocking non-specific antibody binding ........................................ 37
2.5.8 Protein detection ............................................................................ 38
2.5.9 Chemiluminescent signal detection to observe protein.................. 38
2.5.10 Densitomerty for AKT signalling study....................................... 38
2.6 Animal studies to test the effects of TAT-TIJIP....................................... 38
2.6.1 Exercise induced muscle damage in adult mdx mice..................... 38
2.6.2 Animal anaesthesia and sacrifice ................................................... 39
2.6.3 Tissue sampling and processing..................................................... 39
2.6.4 Haematoxylin and eosin staining ................................................... 40
2.6.5 Image analysis: quantification of necrosis ..................................... 40
2.6.6 Statistical analysis .......................................................................... 41
Chapter Three: Validation of cell culture models of IGF-1 induced
skeletal muscle hypertrophy ................................................................................ 42
Introduction ............................................................................................................... 42
Results .......................................................................................................................... 43 3.1 Establishing optimum culture and treatment Conditions....................... 43
3.1.1 Comparing C2C12 myotube formation on different substrates ..... 43
3.1.2 Determining the optimum fusion medium and seeding density

xii
for C2C12 myotube formation ................................................................ 44 3.2 Preliminary Studies to Determine the Biological Activity and Optimum
Dosage of IGF-1 Required for Inducing Hypertrophy in C2C12 and L6
Myotube Cultures (passage > 25) .................................................................... 46
3.2.1 Effects of IGF-1 (LONGTMR3IGF-I) treatment on day 3 mouse
C2C12 muscle myotubes (passage > 25) ................................................ 46
3.2.2 Effects of Des(1-3)IGF-1 treatment on day 3 mouse C2C12
muscle myotubes (passage > 25) ............................................................ 47
3.3 Effects of IGF-1 treatment on day 3 rat L6 myotubes (passage > 25).... 49
Discussion.................................................................................................................... 52
Chapter Four: Morphological effects of IGF-1 and TNF treatment on
cultured myotubes.................................................................................................... 56
Introduction ............................................................................................................... 56
Results .......................................................................................................................... 58 4.1 Effects of IGF-1 treatment on day 7 mouse C2C12 myotubes................ 58
4.2 The effect of TNF treatment on day 7 mouse C2C12 myotubes ........... 58
4.2.1 Independent C2C12 myoblast fusion assay to test the biological
activity of TNF........................................................................................ 58
4.2.2 Effects of TNF treatment on day 7 mouse C2C12 myotubes ........ 59
4.3 Effects of combined treatment with IGF-1 and TNF on day 7 mouse
C2C12 muscle myotubes................................................................................... 61
4.4 Effects of TNF on control FVB and primary cultures of transgenic
IGF:C2 mouse myotubes .................................................................................. 62
4.4.1 Effect of TNF on day 4 FVB primary mouse myotubes................ 62
4.4.2 Testing the effect of TNF on transgenic IGF-1 class 2 primary
muscle cells ............................................................................................. 63
Discussion.................................................................................................................... 65 IGF induced myotube hypertrophy................................................................. 66
TNF induced myotube atrophy........................................................................ 66

xiii
Chapter Five: The role of TNF activated JNK in muscle wasting in
tissue cultured myotubes ....................................................................................... 71
Introduction ............................................................................................................... 71 Results .......................................................................................................................... 73
5.1 TNF activates the JNK signalling pathway in C2C12 myotubes ............ 73
5.1.1 Optimising conditions for detecting TNF activation of the JNK
signalling pathway in day 7 C2C12 myotubes........................................ 73
5.1.2 Titration study to determine if JNK phosphorylation is dependant
on dosage of TNF.................................................................................... 75
5.2 JNK inhibitors used in TNF induced myotube atrophy studies ............. 76
5.2.1 Selection of a suitable JNK inhibitor: evaluation of three
different inhibitors at two dosage levels in C2C12 myotubes ................ 76
5.2.2 Experiments to determine if TNF induced myotube atrophy
can be prevented by pre-treatment with the JNK inhibitor TAT-TIJIP 79
5.2.2.1 Analysis of the morphological effects of TAT-TIJIP
on untreated and TNF treated C2C12 myotubes......................... 79
5.2.2.2 Analysis of the morphological effects of TAT-TIJIP
on untreated and TNF treated control FVB mouse myotubes
in primary cultures ...................................................................... 80
5.2.2.3 Analysis of the morphological effects of TAT-TIJIP
on untreated and TNF treated transgenic IGF:C2 mouse
myotubes in primary cultures...................................................... 81
5.3 Confirmation of the inhibition of JNK phosphorylation by
TAT-TIJIP: immunofluorescent nuclear localisation of the
transcription factor c-Jun................................................................................. 83
5.3.1 Time course analysis of the nuclear localisation of
phosphorylated c-Jun in day 7 C2C12 myotubes.................................... 84
5.3.2 Immunofluorescent microscopy analysis of TAT-TIJIP
inhibition of c-Jun nuclear localisation (phosphorylation) in TNF
induced myotube atrophy in C2C12, FVB and IGF:C2 cultures ............ 86

xiv
5.4 Analysis of IRS-1 and AKT (downstream of IGF-1) to further
investigate TNF inhibition of IGF-1 signalling via JNK, in the model of
C2C12 myotube atrophy .................................................................................. 88
5.4.1 Optimising western blotting conditions for immunoprecipitated
IRS-1 from C2C12 Day 7 myotubes treated with IGF-1 ........................ 88
5.4.2 Western blotting analysis of AKT from C2C12 Day 7 myotubes
treated with IGF-1 or TNF ...................................................................... 90
Discussion.................................................................................................................... 92
Chapter Six: Preliminary study to investigate the effects of
TAT-TIJIP on reducing exercised induced myofibre necrosis
in vivo in mdx mice .................................................................................................. 96
Introduction ............................................................................................................... 96
Results .......................................................................................................................... 98 6.1 The effect of JNK inhibitor TAT-TIJIP on reducing myofibre necrosis
in 6 week old voluntary exercised mdx mice .................................................. 98
6.1.1 Distance run by the mdx mice........................................................ 98
6.1.2 Histological analysis of the effects of TAT-TIJIP on reducing
myofibre necrosis in voluntary exercised mdx mice .............................. 99
Discussion.................................................................................................................. 101
Chapter Seven: General Discussion ................................................................ 104
Overview.................................................................................................................... 104
7.1 Establishment of myotube culture models of IGF-1 induced
hypertrophy and TNF mediated atrophy ..................................................... 104
7.2 Combination treatments to investigate the effects of IGF-1 and
TNF................................................................................................................... 105
7.3 Involvement of JNK in TNF mediated myotube atrophy and use
of JNK inhibitors............................................................................................. 106
7.1.4 In vivo studies: preliminary findings .................................................... 108
References ................................................................................................................. 109

xv
List of Figures
Figure 1.1 Skeletal Muscle Structure .................................................................. 2
Figure 1.2 Intracellular signalling pathways initiated downstream of IGF-1
receptor............................................................................................... 12
Figure 1.3 Intracellular signalling pathways initiated downstream of the TNF
receptor 15
Figure 1.4 Schematic representation of the events occurring following
sarcolemmal damage in dystrophic myofibres................................... 16
Figure 1.5a Damaging effects of TNF in skeletal muscle is proposed to be
mediated by JNK inhibition of IGF-1 signalling ............................... 20
Figure 1.5b Potential use of JNK inhibitors for preventing JNK mediated
down regulation of IGF-1 signalling in skeletal muscle .................... 20
Figure 2.1 Neubauer haemocytometer................................................................. 28
Figure 2.2 Measuring myotube widths using Image Pro Plus software .............. 33
Figure 2.3 Illustration of the Western blotting transfer cassette.......................... 37
Figure 2.4 Exercise equipment for voluntary running......................................... 39
Figure 2.5 Typical histology of dystrophic mdx quadriceps muscle................... 41
Figure 3.1 Myotube formation on different surface coatings.............................. 44
Figure 3.2 The fusion of C2C12 myoblasts into myotubes in two media
(DMEM +/- HS) at two different initial plating densities in 35mm
collagen (type I) coated dishes........................................................... 45
Figure 3.3 Effects of IGF-1 treatment on C2C12 myotubes .............................. 48
Figure 3.4 Effects of Des(1-3) IGF-1 treatment on C2C12 myotubes ............... 49
Figure 3.5 Effects of IGF-1 treatment on L6 myotubes ..................................... 50
Figure 3.6 Immunostained L6 myotubes treated with IGF-1 ............................. 51
Figure 4.1 Fusion assay to test biological activity of TNF ................................. 59
Figure 4.2 Immunofluorescent microscopy images of Day 10 C2C12
myotubes treated with IGF-1 or TNF for 3 days ............................... 60
Figure 4.3 Quantitative analysis of mean myotube widths of untreated
(control), IGF-1 and TNF treated C2C12 cultures ............................ 61
Figure 4.4 Quantitative analysis of myotube widths of untreated (control), 62

xvi
IGF-1, TNF and combined IGF-1 and TNF treated C2C12
cultures ..............................................................................................
Figure 4.5 Quantitative analysis of myotube widths from TNF atrophy
experiments conducted on Wild type FVB and Transgenic
IGF:C2 primary skeletal muscle cell cultures ................................... 63
Figure 5.1 Optimising conditions for detecting TNF phosphorylation of JNK
in differentiated (day 7) C2C12 myotubes: preliminary
experiments ....................................................................................... 74
Figure 5.2 Time course assay of TNF phosphorylation of JNK in
differentiated (day 7) C2C12 myotubes: final protocol .................... 75
Figure 5.3 Titration study to determine the minimum effective dose of TNF
to induce phosphorylation of JNK in differentiated (day 7) C2C12
myotubes ........................................................................................... 76
Figure 5.4 Toxicity evaluation of three JNK inhibitors on day 10 C2C12
myotubes ........................................................................................... 78
Figure 5.5 Mean width of untreated control C2C12 myotubes and C2C12
myotubes treated with TNF alone, TAT-TIJIP alone, combination
of TAT-TIJIP and TNF, TAT alone and combination of TAT and
TNF ................................................................................................... 80
Figure 5.6 Mean width of untreated control primary FVB myotubes and
FVB myotubes treated with TNF alone, TAT-TIJIP alone,
combination of TAT-TIJIP and TNF, TAT alone and combination
of TAT and TNF ............................................................................... 81
Figure 5.7 Mean width of untreated control primary IGF:C2 myotubes and
IGF:C2 myotubes treated with TNF alone, TAT-TIJIP alone,
combination of TAT-TIJIP and TNF, TAT alone and combination
of TAT and TNF ............................................................................... 83
Figure 5.8 Immunofluorescence microscopy images depicting the nuclear
localisation of phosphorylated c-Jun in day 7 C2C12 myotubes
treated with TNF ............................................................................... 85
Figure 5.9 Immunofluorescent microscopy images depicting reduced nuclear
localisation of phosphorylated c-Jun in muscle cell cultures pre
treated with TAT-TIJIP inhibitor 1 hr before treatment with TNF ... 87

xvii
Figure 5.10 Comparison of tyrosine phosphorylation (pY) of IRS-1 in Insulin
stimulated C2C12 cells from two different laboratories ................... 90

xviii
Figure 5.11 Activation of AKT in differentiated (day 7) C2C12 myotubes
treated with TNF or IGF-1 ................................................................
91
Figure 6.1 Percentage of myofibre necrosis in right quadriceps muscle of
untreated and TAT-TIJIP treated voluntary exercised adult mdx
mice ................................................................................................... 100

xix
List of Tables
Table 2.1 Dimensions of various tissue culture plates and the myoblast
plating densities used in these studies .................................................. 29
Table 2.2 Concentration of BSA in the protein assay standards .......................... 34
Table 2.3a Composition of Resolving gel: 12% polyacrylamide in 1 M Tris-
HCL pH 8.8 .......................................................................................... 36
Table 2.3b Composition of Stacking gel: 6% polyacrylamide in 0.5 M Tris-
HCL pH 6.8 .......................................................................................... 36
Table 6.1 The relation between the voluntary distance ran to the amount of
exercised induce myofibre necrosis .................................................... 98

xx
Abbreviations
AKT Serine/threonine protein kinase
ANOVA Analysis of variance
ATP Adenosine triphosphate
bFGF Basic fibroblast growth factor
BSA Bovine serum albumin
CSA Cross sectional area
DEX Dexamethasome
DMD Duchenne Muscular Dystrophy
DMEM Dulbecco’s Modified Eagle’s Medium
DMSO Dimethyl sulfoxide
ERK Extra cellular signal related kinase
EDTA Ethylenediaminetetraacetic acid
FCS Foetal calf serum
FM Fusion Media
Foxo Forkhead box, sub-group O transcription factor
GH Growth hormone
GM Growth media
H&E Haematoxylin and eosin
HS Horse Serum
IFN-γ Interferon-γ
IGF-1 Insulin like growth factor-1
IGF-2 Insulin like growth factor-2
IGF-1R Insulin like growth factor-1 receptor
IGF-2R Insulin like growth factor-2 receptor
IGFBP Insulin like growth factor binding proteins
IL Interleukin
IRS-1 Insulin receptor substrate-1
JIP JNK-interacting protein
JNK c-Jun N-terminal Kinase
MAFbx Muscle atrophy F box or Atrogin-1

xxi
MAPK Mitogen-activated protein kinases
mIGF-1 Skeletal muscle-specific exon-1 Ea isoform of IGF-1
mTOR mammalian target of rapamycin
NFĸβ Nuclear factor ĸβ
PBS Phosphate buffered saline
PDL Poly-D-Lysine
PI3K Phosphatidylinositiol 3-kinase
PVA Polyvinyl alcohol mounting medium
PVDF Polyvenylidene difluoride
ROS Reactive Oxygen Species
RT Room temperature
SDS Sodium Dodecyl Sulfate
sTNF Soluble TNF
TA Tibialis anterior
TBS Tris buffered saline
TIJIP Truncated Inhibitor of JNK Interacting Protein
TIM TNF receptor associated factor-interacting motifs
TNF Tumour necrosis factor
TNF-R1 TNF receptor 1
TNF-R2 TNF receptor 2
TRAF TNF receptor associated factor
TRIS Tris(hydroxymethyl)aminomethane
UT Untreated

xxii
Publications in Referred Journals
Grounds, M. D., Radley, H. G., Gebski, B. G., Bogoyevitch, M. A. and Shavlakadze, T.
(2008). "Implications Of Cross-Talk Between Tumour Necrosis Factor And Insulin-
Like Growth Factor-1 Signalling In Skeletal Muscle." Clin Exp Pharmacol Physiol.
Manuscripts in Preparation
c-Jun N-terminal Kinases (JNKs) are critical mediators of TNF-induced myotube
atrophy
Gebski BLa, Bogoyevitch M.A.b, Grounds M.D. a, Shavlakadze T.S. a
a School of Anatomy and Human Biology, the University of Western Australia
b Department of Biochemistry and Molecular Biology, Bio21 Molecular Science and
Biotechnology Institute, The University of Melbourne, 30 Flemington Road, Victoria,
3010, AUSTRALIA.

Chapter One Introduction
1
Chapter One
Introduction
Overview
This following is a comprehensive review of the background literature pertinent to the
present study. The chapter opens with a general discussion on skeletal muscle biology
and the importance of skeletal muscle hypertrophy and atrophy is introduced. The
molecular basis of Duchenne Muscular Dystrophy (DMD) and the mdx animal model of
DMD are then discussed in relation to the prominent muscle necrosis associated with
voluntary exercise. The relationship between DMD and the c-Jun N-terminal Kinase
(JNK) is briefly discussed before an in-depth review of both the Insulin like growth
factor-1 (IGF-1) and Tumour necrosis factor (TNF) signalling pathways. The
involvement of JNK in the cross-talk between these two pathways is demonstrated and
the significant importance of this kinase in mediating the deleterious effects of TNF in
situations of muscle inflammation is discussed. Finally, various inhibitors that aim to
block the actions of activated JNK are reviewed with the advantages and disadvantages
of each presented.

Chapter One Introduction
2
1.1 Skeletal muscle
Skeletal muscles make up approximately 40% of the mass of the human body and are
composed of multinucleated muscle myofibres (or myotubes) which are formed by the
fusion of myoblasts (muscle cells). The myofibres are filled with highly organised
contractile proteins and arranged in bundles within several different layers of fibrous
connective tissue and are attached to skeletal bones by connective tissue and tendons
(Figure 1.1). Skeletal muscles are under voluntary nervous control (somatic nerve
stimulation); their primary function is movement (contraction) in addition to
maintaining normal body positioning and posture (Saladin 2004).
Figure 1.1: Skeletal Muscle Structure. (A) Skeletal muscle is arranged in bundles. The bundles are encased within three sheaths of connective tissue; epimysium covers the whole muscle, perimysium covers the bundles of the myofibre and the endomysium covers each individual myofibre (SEER, n.d) (B) Myofibres are composed of sarcoplasm filled with striated muscle cells (myofibrils) and are encased within the sarcolemma (membrane). Figure adapted from Bannister et al. (1995).
A
Sarcolemma (membrane)
Peripheral Nucleus
Mitochondria
Myofibril (muscle cell)
Sarcoplasmic Reticulum
Transverse Tubules
B

Chapter One Introduction
3
1.2 Physiological and pathological remodelling of skeletal muscle
1.2.1 Skeletal muscle hypertrophy
Skeletal muscle hypertrophy is an increase in the size, diameter (cross sectional area,
CSA) and mass of individual myofibres. In adults this develops as a compensatory
response to resistance exercise, increased physiological loading or enhanced nutritional
uptake in vivo (Grounds 2002; Jackman and Kandarian 2004). Skeletal muscle adapts to
loading changes by increasing the size and amount of contractile proteins within the
sarcomeres of each myofibre. This results in an increase in the CSA of myofibres, their
associated force production, and also an alteration in protein synthesis and degradation
rates (Goldspink 1991; Adams and Haddad 1996; Russell et al. 2000).
Numerous factors and signals also trigger hypertrophy of skeletal muscles, for example
it is well known that Insulin-like growth factor-1 (IGF-1 - which is a subject of study in
this thesis), hormones, cytokines and anabolic steroids all have a crucial role in inducing
skeletal muscle hypertrophy (Semsarian et al. 1999) (Boonyarom and Inui 2006). The
important intracellular signalling pathways responsible for skeletal muscle hypertrophy
are discussed in greater detail in Section 1.4 of this thesis.
1.2.2 Skeletal muscle atrophy and cachexia
Skeletal muscle atrophy is a reduction in the CSA and mass of individual myofibres,
accompanied by a decrease in myofibrillar protein content, decreased force production,
and lower fatigue resistance (Boonyarom and Inui 2006). The biochemical and
enzymatic responses include the reduced capacity to synthesize new protein and the up-
regulation of pathways leading to increased protein breakdown (Jackman and Kandarian
2004; Shavlakadze and Grounds 2006).
Many factors can result in muscle atrophy including neuromuscular disorders,
immobilisation/muscle disuse, denervation (Shavlakadze and Grounds 2006),
inflammatory conditions associated with cancer (Baracos et al. 1995), sepsis (Fang et al.
2000), Acquired Immune Deficiency Syndrome (AIDS) (Gonzalez-Cadavid et al. 1998),
burn injury, glucorticocoid treatment (Argiles et al. 2007), diabetes (Price et al. 1996)
and ageing and starvation (Mitch and Goldberg 1996).

Chapter One Introduction
4
As the pathological aetiology of muscle atrophy vary (Shavlakadze and Grounds 2006),
it is important to distinguish muscle atrophy resulting from disuse/denervation or
starvation, from muscle wasting induced in pathological inflammatory conditions as a
result of high levels of pro-inflammatory cytokines (also known as cachexia), such as
tumour necrosis factor (TNF) (Argiles et al. 2001). At a recent symposium, the
definition of cachexia was refined, the general consensus of the group was that
cachexia ‘is a complex metabolic syndrome’ resulting from an adaption to an
underlying illness (such as cancer) and is associated with anorexia (loss of appetite),
inflammation, insulin resistance, anaemia and increased muscle protein breakdown
(Evans et al. 2008). Due to the central role of inflammation (specifically the elevated
levels of inflammatory cytokines including TNF) in cachexia and other situations of
atrophy, therapies targeting the inflammatory pathways will continue to attract
considerable interest to reduce the severity of muscle wasting (Evans et al. 2008).
A common characteristic of atrophying muscle is induction of the ubiquitin-proteasome
protein degradation pathway (Lecker et al. 2004). Two important genes (atrogenes) up-
regulated in atrophic states are ubiquitin ligase Muscle atrophy F box (MAFbx or
Atrogin-1) and Muscle RING finger-1 (MuRF-1) (Lecker et al. 2004; Latres et al.
2005). Another important signalling pathway associated with regulation of muscle mass
is that of IGF-1; loss of IGF-1 signalling may be a key factor for skeletal muscle
atrophy (Grounds 2002).
Conversely, it is now widely understood that muscle mass can be regulated by important
growth factors (such as IGF-1) and that the loss of IGF-1 and its downstream signalling
events may be key factors in accelerating skeletal muscle atrophy (Grounds 2002).
Recent interesting reports have suggested that down-regulation of IGF-1 activated
signalling events through TNF-stimulated activation of a family of cytosolic stress-
activated kinases, known as the c-Jun N-terminal Kinase (JNKs). The action of active
JNK on key proteins involved in IGF-1 signalling pathways can inhibit IGF-1 signalling
and therefore prevent the positive effects of IGF-1 (Broussard et al. 2003; Broussard et
al. 2004; Strle et al. 2006). This is discussed in greater detail in Section 1.5 (see below).
The balance between TNF and IGF-1 signalling is also implicated in the extensive
muscle wasting associated with the lethal muscle disease Duchenne Muscular

Chapter One Introduction
5
Dystrophy (DMD). As such, and animal models of this disease (such as the mdx mouse)
are of considerable interest and importance for the development of new therapeutic
targets related to these interacting signalling pathways.
1.3 Duchenne Muscular Dystrophy
1.3.1 The molecular basis of Duchenne Muscular Dystrophy
Duchenne Muscular Dystrophy is a lethal X-linked muscle wasting disorder arising
from mutations within the dystrophin gene (Hoffman et al. 1987). These mutations
result in the absence of functional dystrophin, leading to fragility of the sarcolemma and
can result in myofibre necrosis (Blake et al. 2002). Without prenatal screening and
genetic counselling, DMD occurs at a frequency of 1 in 3500 live male births (Emery
1991). The disease is clinically evident in early childhood, usually between 3 to 5 years
of age (Emery 2002). Due to continual muscle wasting, boys with DMD are restricted to
a wheel chair by 12 years of age and 90% die in their late teens or early twenties,
usually due to cardiac or respiratory failure (Blake et al. 2002). However, the use of
mechanical assisted ventilation has increased the lifespan of DMD patients to the mid
20s (Bach et al. 1997).
Following the discovery of the molecular basis of DMD in 1987, research has been
directed towards the development of new disease treatments based on this newly
acquired and improved understanding of the underlying causes of the muscle
dysfunction. Gene replacement strategies, including myoblast and stem cell transfer,
have had limited success in the mouse and human trials (Grounds and Davies 2007;
Davies and Grounds 2007). Alternative forms of molecular therapy have also been
considered. These include the delivery of genes or minigenes via viral or non-viral
vectors (Odom et al. 2007; Wang et al. 2009), utrophin up regulation (Li et al. 2009),
gene correction (Bertoni et al. 2005; Maguire et al. 2009) and the use of antisense
oligonucleotides to mask mutations within the dystrophin gene (Wu et al. 2008;
Heemskerk et al. 2009; Yokota et al. 2009). To date, there is still no effective treatment
for DMD. The current research project thus focuses on a new strategy related to the role
of inflammation in the breakdown of dystrophic muscle.

Chapter One Introduction
6
1.3.2 Mdx mouse model of DMD
The understanding of DMD was considerably enhanced following the discovery of the
mdx mouse as a reliable animal model. Bulfield and colleagues showed that a
spontaneous X-chromosome linked mutation had arisen in their inbred C57BL/10
colony of mice; the serum of these mutant mice contained high levels of muscle-derived
pyruvate kinase and creatine kinase, which is also present in DMD (Bulfield et al.
1984). The mice also exhibited histological lesions similar to those characteristic of
early DMD, involving necrosis of muscle fibres (myofibril necrosis) (Bulfield et al.
1984; Partridge 1991). This research group named the mice ‘mdx’ (Bulfield et al. 1984).
The molecular basis of the dystrophy presented in the mdx mouse was characterised in
1989. This was achieved by cloning complementary DNA (cDNA) of mouse
dystrophin, with the sequence being used in a polymerase chain reaction (PCR) to
amplify both the normal and the mdx dystrophin transcripts (Sicinski et al. 1989).
Sicinski's group determined that the mdx mouse arose from a point mutation in exon 23
of the dystrophin gene. This single base change within exon 23 results in only 27% of
the dystrophin protein being translated prior to encountering the premature stop codon
(Sicinski et al. 1989).
One of the most significant factors of the mutation in the mdx mouse is that it does not
result in the large fibrotic lesions characteristic of human DMD. Furthermore, and most
importantly, the mice appear to be able to regenerate their skeletal muscle. Certain
muscles (such as the diaphragm) do display some of the features seen in human DMD
patients (O'Brien and Kunkel, 2001), but there has been speculation in regards to the
genetic homology of the mdx mice and that observed in human DMD (Partridge 1991;
Blake et al. 2002). In the attempt to produce an animal model that would more closely
reflect human DMD, several mouse strains mdx2Cv, mdx3Cv, mdx4Cv and mdx5Cv
were generated by the deliberate induction of ethyl-nitroso-urea at the mdx locus
(Chapman et al. 1989; O'Brien and Kunkel 2001; Blake et al. 2002). However, despite
different mutations in the dystrophin gene, these mice appeared phenotypically similar
to the naturally occurring mdx model (Partridge 1991; Blake et al. 2002) and thus the
mdx mouse is continued to be used.

Chapter One Introduction
7
1.3.2.1 Mdx mouse, muscle necrosis and voluntary exercise
Although a functional form of the dystrophin protein is absent in mdx mice (and they
are thus susceptible to muscle necrosis), the mutation does not result in the same
severity of pathology, specifically the eventual replacement of muscle by fibrous fatty
connective tissue as observed in human DMD boys (Gillis 1999). The marked
differences in the severity of the dystropathology between humans and mice may be
largely accounted for by large differences in the size and growth parameters of the 2
species (Grounds et al. 2008). However, the mdx mouse remains the most convenient
and clinically relevant mammalian model to screen drugs for the potential clinical
treatment of DMD boys (Granchelli et al. 2000; Payne et al. 2006; Grounds et al. 2008).
The age at which the mdx mice are used for muscle necrosis studies is critically
important. Histological examination of muscle sampled from mdx mice younger than 3
weeks of age bears little resemblance to that associated with the dystrophic phenotype,
but by around day 21, there is an acute onset of muscle damage in the limb and
paraspinal muscles (Coulton et al. 1988; McGeachie et al. 1993; Grounds and Torrisi
2004; Shavlakadze et al. 2004). It has been reported that the percentage of muscle
necrosis in the tibialis anterior muscle increases to approximately 20-40% in 3 week old
mdx mice (Shavlakadze et al. 2004). This rapid, acute onset of myofibre damage is then
followed by intensive muscle regeneration, which stabilises at about 6 weeks of age to a
relatively low level of around 6% (McGeachie et al. 1993).
As this reduced and ongoing low level of muscle necrosis presents a difficult model to
assess the effectiveness of drug intervention to reduce myofibre necrosis, mice have
been subjected to voluntary exercise to increase muscle damage and necrosis (Archer et
al. 2006; Hodgetts et al. 2006; Radley and Grounds 2006). This allows for potential
therapies (such as the interventions described in Chapter 6) to be more effectively tested
in adult mdx mice (Grounds et al. 2008).
The interventions to be evaluated in mdx mice that are of central interest to the present
research relate to modulating the effects of IGF-1 and TNF. The key features of IGF-1
and TNF are therefore discussed in more detail (see below).

Chapter One Introduction
8
1.4 Insulin like growth factor -1 (IGF-1)
The Insulin-like Growth Factor (IGF) system consists of three peptide hormones/ligands
(Insulin, IGF-1 and IGF-2), their receptors (insulin receptors, IGF-1 type 1 receptor;
IGF-1R and IGF-2 type 2 receptor; IGF-2R) and six IGF binding proteins (IGFBP-
1,2,3,4,5,6) (Hwa et al. 1999). The insulin receptor is a main mediator of the biological
functions of insulin, while the IGF-1 receptor mainly mediates cellular responses of
IGF-1 and IGF-2. It is considered that the IGF-2 receptor does not have a major role for
IGF-1 and IGF-2 signal transductions, but it is responsible for binding and thus
reducing IGF-2 levels during foetal development (Le Roith et al. 2001).
IGF-1 is a potent growth factor in vitro and in vivo, and its actions are regulated by
interactions with IGFBPs (Rutanen and Pekonen 1990). IGF-1 is essential for normal
muscle growth during development, stimulating proliferation and differentiation in
myoblasts (Engert et al. 1996), exerting anabolic effects such as myofibre hypertrophy
(increased size and protein content) (see below), muscle regeneration in adults and the
prevention of atrophy (muscle wasting) in ageing muscle (Musaro et al. 2001; Grounds
2002; Glass 2005). In addition IGF-1 induces satellite cell proliferation and
differentiation and interleukin 4 (IL-4); a myoblast recruitment factor for fusion with
existing myotubes (Horsley et al. 2003).
Growth hormone (GH) induces the expression of IGF-1 in many tissues, such as the
liver, pancreas, muscles, intestines, kidney, brain and adipose tissue, and therefore IGF-
1 acts as the main mediator of GH effects (Le Roith et al. 2001). IGF-1 is produced by a
range of tissues (Froesch et al. 1985), however the liver is the primary production site
(approximately 75%) of circulating IGF-1; the balance is produced locally by other
tissues. The IGF-1 gene gives rise to multiple isoforms of pre-processed IGF-1 (which
differ by termination peptides) and can exert different biological functions (Shavlakadze
et al. 2005).

Chapter One Introduction
9
1.4.1 Protein analogues of IGF-1: naturally occurring and synthetic
1.4.1.1 Naturally occurring IGF-1 isoforms
The mammalian IGF-1 gene gives rises to several isoforms of pre-processed IGF-1
which differ by termination peptides and can exert different biological functions. The
processed form is a 70-amino acid long (molecular weight 7649 Da) single IGF-1
polypeptide cross-linked by three disulfide bridges (Rinderknecht and Humbel 1978). In
mammalian species, the structure of IGF-1 is highly conserved, with mouse IGF-1 (Bell
et al. 1986) differing to human IGF-1 (Rinderknecht and Humbel 1978) by only four
amino acids. For a more detailed report on the complexity of IGF-1 isoforms and the
structure of rodent IGF-1 see (Shavlakadze et al. 2005).
1.4.1.2 Naturally occurring analogue of IGF-1: Des(1-3)IGF-1
Des(1-3)IGF-1 is a naturally occurring truncated analogue of IGF-1. Des(1-3)IGF-1 is a
67 amino acid protein that differs to human and bovine IGF-1 only by the omission of
the tripeptide Gly-Pro-Gly from the N-terminus (Ballard et al. 1987). Des(1-3)IGF-1
was discovered as the growth promoting activity of bovine colostrum on L6 myoblasts
(Francis et al. 1986). Since Des(1-3)IGF-1 has only 1% of the affinity for IGFBPs
(which normally inhibit the biological actions of naturally occurring IGF-1) (Ross et al.
1989), Des(1-3)IGF-1 has been reported to have approximately 10 times the potency of
naturally occurring IGF-1 with both cell hypertrophy and proliferation induced at
substantially lower concentration than that of IGF-1 in many cell types (Francis et al.
1988; Carlsson-Skwirut et al. 1989).
The synthesis of Des(1-3)IGF-1 is believed to occur though post-translational
modification of mature IGF-1, following the removal of the leader sequence and the C-
terminus extension (Ballard et al. 1987) It has been suggested that the N-terminus
extension sequences (encoded by exons 1 and 2) directs the specificity of a signal
peptidase to yield either IGF-1 of Des(1-3)IGF-1 (Ballard et al. 1996).
1.4.1.3 Synthetic analogue of IGF-1: LONGTMR3IGF-1
Long R3 Insulin-like Growth Factor-I (LONGTMR3IGF-1) is an 83 amino acid analogue
of IGF-I comprising the complete IGF-I sequence with the substitution of glutamic acid
(E) at position 3 with arginine (hence R3), and a 13 amino acid extension peptide at the

Chapter One Introduction
10
N-terminus. It is produced in Escherichia coli as a single, non-glycosylated, polypeptide
with a molecular weight of 9111 Da (Francis et al. 1992).
LONGTMR3IGF-1 is significantly more potent than both naturally occurring IGF-1 and
the IGF-1 analogue of Des(1-3)IGF-1 in vitro and is characterised by a reduced affinity
(greater then 1000-fold) for binding to IGFBPs (Francis et al. 1992). This significantly
reduced affinity is the result of the 13 amino acid extension. When tested in an L6
myoblast protein assay, LONGTMR3IGF-1 was the most potent peptide in stimulating
protein synthesis in the myoblasts, with Des(1-3)IGF-1 and then IGF-1 being the least
potent in that order (Francis et al. 1992). Studies performed in embryonic kidney
(HEK293) cells corroborate these finding; Voorhamme & Yandel (2006) reported that
in serum free cultures, LONGTMR3IGF-1 was a more potent growth and survival factor,
than either insulin or IGF-I .
The studies in this thesis exclusively use LONGTMR3IGF-1 to capitalise on its potency
in stimulating IGF-receptors and subsequent signalling events. Therefore, from Chapter
3, and continuing for the remainder of the thesis, whenever the term ‘IGF-1’ is used, it
refers to the LONGTMR3IGF-1 isoform.
1.4.2 IGF-1 signalling in skeletal muscle cells
It is well documented that IGF-1 plays a crucial role in mediating the anabolic
regulation of muscle mass (Florini et al. 1996) and can induce hypertrophy (Section
1.2.1) through either autocrine or paracrine mechanisms (DeVol et al. 1990). IGF-1
stimulates the proliferation and differentiation of myoblasts (Engert et al. 1996), induces
the uptake of amino acids and incorporation into proteins, regulation of glucose uptake,
and suppression of protein degradation (Florini and Magri 1989; Florini et al. 1996).
Numerous mouse muscle cell culture studies have demonstrated that treatment of
multinucleated muscle cells (myotubes) with the IGF-1 analogue LONGTMR3IGF-1
induced hypertrophy of myotubes (Florini et al. 1996; Rommel et al. 1999; Rommel et
al. 2001). Similarly, studies using the L6E9 (a subclone of the L6 cell line) show IGF-1
induced hypertrophy in myotubes via the transfection of a muscle specific IGF-1 vector
that is only activated during cell differentiation (Musaro and Rosenthal 1999; Musaro et
al. 1999; Fanzani et al. 2006). It has also been reported that the same signalling

Chapter One Introduction
11
pathways which mediate myotube hypertrophy in the C2C12 cells are also upregulated
when IGF-1 was administered to L6 myotubes (Li et al. 2005). Furthermore, the ability
of IGF-1 over-expression to reduce denervation atrophy was demonstrated in skeletal
muscle in vivo (Stitt et al. 2004; Shavlakadze et al. 2005) and appeared to be due to
suppression of the up-regulation of atrophy associated genes (Stitt et al. 2004; Latres et
al. 2005). All these functions are mediated through IGF-1 binding to its receptor (IGF-
1R) a ligand-activated receptor tyrosine kinase.
IGF-1R is a trans-membrane protein consisting of two extracellular ligand binding α-
subunits (which contain the IGF-1 binding site) and two β-subunits (Figure 1.2). When
IGF-1 binds to the extracellular α-subunits, specific tyrosine kinases in the receptor β-
subunits undergo autophosphorylation (activation) (Jacobs et al. 1983; Rubin et al.
1983; Ullrich et al. 1986). An early molecule involved in linking the receptor kinase to
the biological actions of IGF-1 is tyrosine phosphorylation of insulin receptor substrate -
1 (IRS-1) (Figure 1.2), a 135 kDa tyrosine phosphoprotein and SH2 domain containing
protein ((Keller et al. 1993; Rothenberg et al. 1991). IRS-1 serves as docking protein for
other cytoplasmic signalling molecules that contain SH2 domains, including
phosphatidylinositiol (PI) 3-kinase and Grb2 (Florini et al. 1996). Activated PI3K then
phosphorylates membrane phospholipid phosphatidylinositol 4,5-bisphosphate to
produce phosphatidylinositol 3,4,5-trisphosphate (Matsui et al. 2003) (Figure 1.2). This
modified lipid is recognised by the serine/theronine kinase AKT (Alessi et al. 1997),
which when at the membrane is phosphorylated and activated by PDK (PDK-1)
(Vivanco and Sawyers 2002) (Figure 1.2).

Chapter One Introduction
12
Figure 1.2: Intracellular signalling pathways initiated downstream of IGF-1 receptor.
In skeletal muscle cells, the pathway downstream of PI3K has been linked to
differentiation, survival, hypertrophic growth and the prevention of muscle atrophy
(Rommel et al. 1999). The activation of the defined PI3K/AKT pathway in C2C12
cultured myotubes has been described and defined a as crucial pathway for regulating
protein synthesis in skeletal muscle cells and muscle hypertrophy (Glass 2003; Rommel
et al. 2001; Latres et al. 2005). Increase phosphorylation and activation of AKT has
been demonstrated in cultured muscle cell models of IGF-1 induced hypertrophy
(Rommel et al. 2001) and in in vivo models of functional overload induced hypertrophy
(Bodine et al. 2001).
Similarly, as AKT is activated by the IGF-1 receptor, so are direct and indirect targets
of AKT; mammalian target of rapamycin (mTOR), p70S6K and 4EBP-1, all key
regulatory protein involved in protein synthesis (Rommel et al. 2001; Latres et al.
2005). The significance of the PI3KAKT/mTOR pathway in mediating hypertrophy in
skeletal muscle cells was demonstrated using the mTOR inhibitor, rapamycin. When
administered in vivo rapamycin almost completely prevented hypertrophic growth of
skeletal muscle (Bodine et al. 2001) and blocked all but 1% of the gene activated by
IGF-through the PI3K/AKT pathway (Latres et al. 2005).

Chapter One Introduction
13
Activation of the PI3K/AKT pathway can also reduce myofibre atrophy and counteract
protein degradation by inversely regulating a number of atrophy related genes such as
MAFbx (Latres et al. 2005). The down regulation of the PI3K/AKT pathway results in
the upregulation of atrophy related genes (see Section 1.2.2) via the desphohorylation of
Forkhead box, sub-group O transcription factors (Foxo) and their consequent
translocation into the nucleus (Sandri et al. 2004; Latres et al. 2005). It is Foxo3 that
directly activates transcription from MAFbx promoter (in vivo and cell culture) and
induce muscle atrophy (Sandri et al. 2004), however AKT phosphorylates Foxo
transcription factors on various sites, which results in the Foxo protein being unable to
translocate to the nucleus and thus their transcriptional functions are inhibited (Brunet et
al. 1999).
1.4.3. The protective benefits of IGF-1 for muscle wasting conditions: IGF-1 over
expressing animal model
In situations of muscle wasting, such as dystrophy, the protective benefits of IGF-1 have
been investigated and discussed in depth in various reviews (Shavlakadze et al. 2005;
Grounds et al. 2008). The over-expression of skeletal muscle specific IGF-1 (mIGF-1)
in dystrophic mdx mice can significantly reduce the severity of the dystrophic
pathology, most likely due to reduced muscle necrosis and increased protein synthesis
in the muscles (Shavlakadze et al. 2004). Over-expression of IGF-1 was generated in
transgenic mdx/mIGF-1 mice using a tissue-restricted transgene which encoded the
skeletal muscle-specific exon-1 Ea isoform of IGF-1 (called mIGF-1) (Musaro et al.
2001). At one year of age, these mice showed a 40% increase in muscle mass when
compared to mdx mice (Barton et al. 2002). Further to these observations, transgenic
mdx/mIGF-1 mice exhibited a significant reduction in the amount of fibrosis normally
observed in the diaphragms of mdx mice (Barton et al. 2002).
1.5 Tumour Necrosis Factor (TNF)
Tumour necrosis factor (TNF) is a pro-inflammatory cytokine that is elevated during
muscle wasting (cachetic) conditions such as cancer, AIDS and sepsis (Argiles et al.
2001). Initially it was thought that TNF was released by bacteria, and that TNF
mediated endotoxin induced the necrosis of certain tumours in mice, resulting in a

Chapter One Introduction
14
muscle-wasting syndrome (cachexia) in tumour-bearing mice (Carswell et al. 1975).
Later it was agreed that TNF and endotoxin were separate factors, because TNF has a
direct cytotoxic effect on various tumour cells in vitro (Hoffmann et al. 1978; Old
1981). It was also found that TNF and the protein cachetin are identical, with the latter
also involved in muscle wastage associated with cancer (Beutler et al. 1985).
It is well documented that TNF has a critical role in skeletal muscle atrophy. TNF is
also the principal cytokine mediating cachexia (muscle wasting) (Argiles et al. 1997;
Glass 2005; Arthur et al. 2008)., TNF, however also has a pivotal role in initiating a
broad range of diverse cellular responses, including inhibition of skeletal muscle
proliferation and differentiation (Miller et al. 1988; Szalay et al. 1997; Meadows et al.
2000; Foulstone et al. 2001; Coletti et al. 2002; Foulstone et al. 2004), growth arrest
(Darzynkiewicz et al. 1984), inflammatory effects (Beutler and Cerami 1988; Peterson
et al. 2006), mediation of the immune response, and apoptotic and necrotic cell death
mechanisms (Laster et al. 1988; Denecker et al. 2001; Tolosa et al. 2005). Furthermore,
it has been reported that expression levels of TNF are elevated in conditions associated
with muscle pathology such as inflammatory myopathy (Lundberg et al. 1995; Saito et
al. 2000; Efthimiou 2006), DMD (Tews 2005) and cancer cachexia (Tracey et al. 1988;
Argiles et al. 1997; Pajak et al. 2008).
TNF and the other members of the TNF ligand family stimulate a complex array of post
receptor signalling events through binding to specific receptors. The cellular signalling
response to TNF seemingly depends on the cell type and physiological conditions. Of
the approximate 29 receptors that make up the TNF receptor (TNF-R) family, two are of
significant importance to TNF exerting its biological functions, these being TNF
receptor type 1 (TNF-R1) and TNF receptor type 2 (TNF-R2). TNF-R1 is the primary
receptor for soluble TNF (sTNF) and TNF-R2 the main receptor for membrane
integrated TNF (memTNF) (Wajant et al. 2003).
TNF-R1 contains a death domain (DD) that is activated upon ligand (TNF) binding,
which then activates the caspase cascade and induces apoptosis and necrosis (Laster et
al. 1988; Denecker et al. 2001; Tolosa et al. 2005). TNF-R2 is distinct to TNF-R1
because TNF-R2 contains TRAF (TNF receptor associated factor)-interacting motifs
(TIM), which upon ligand binding, cause the recruitment of TRAF family members

Chapter One Introduction
15
(Dempsey et al. 2003). Members of the TNF-R family activate the mitogen-activted
protein kinases (MAPK) which regulate various cellular activities, such as gene
expression, mitosis, differentiation, and cell survival/apoptosis (Pearson et al. 2001),
PI3K, p38, extra cellular signal regulated kinase (ERK), nuclear factor ĸB (NF- ĸB)
(closely associated with inflammation), capsases (involved in Apotosis) and, of
considerable relevance to the present study, c-Jun-N-terminal kinase (JNK) (Karin and
Gallagher 2009). The role of TNF varies markedly according to the cell type (Shutze et
al. 1992; Wajant et al. 2003) thus in this study it will be looked at specifically from the
role it plays in skeletal muscle cells.
Figure 1.3: Intracellular signalling pathways initiated downstream of the TNF receptor. Binding of TNF to its receptor stimulates at least four distinct signal transduction pathways (Wajant et al. 2003). These are (1) apoptosis via interaction of the TNF-receptor complex and the Fas-associated protein (FA) with death domain (DD), (2) activation of JNK (associated with stress related cellular responses and atrophy), (3) activation of p44/p42MAPK (Erk 1/2) (associated with atrophy) and (4) activation of receptor-interacting protein which then activates p38 MAPK, which is responsible for activiating atrophy related genes (Li et al. 2005) and is also involved in myogenesis in skeletal muscle (Cuenda and Cohen 1999; Chen et al. 2007), and NF-κB (associated with protein loss) (Reid and Li 2001; Wajant et al. 2003). Figure modified from Sethi et al. (2008).

Chapter One Introduction
16
1.5.1 TNF exacerbates muscle damage
TNF is expressed by a wide range of inflammatory cells and elevated in inflammatory
myopathies and DMD (Kuru et al. 2003; Saito et al. 2000). TNF is also produced by
adipose tissue (Coppack 2001; Weisberg et al. 2003) which is often pronounced in
DMD muscles. In normal muscle, some small lesions of the sarcolemma may be
repaired, and myofibre necrosis does not occur (Bansal et al. 2003). However, initial
muscle lesions may also be exacerbated by pro-inflammatory cytokines (such as TNF)
and inflammatory cells (Tidball 2005) leading to necrosis and muscle breakdown
(Figure 1.3). The blockade of TNF (by either Remicade or Enbrel) in vivo has been
reported to protect dystrophic muscle from necrosis in the mdx mouse model of DMD
(Grounds and Torrisi 2004; Grounds et al. 2005). Both these drugs are currently in wide
clinical use to treat inflammatory disorders such as arthritis or Crohn’s disease.
Figure 1.4: Schematic representation of the events occurring following sarcolemmal damage in dystrophic myofibres. Lack of functional dystrophin (A) makes the myofibre membrane susceptible to damage (B). Where TNF levels are low, such tears may be rapidly resealed (C) by fusion of the membrane vesicles to the edges of damaged sarcolemma, whereby the myofibre returns to a relatively intact state (D). Alternatively (E) if TNF levels are elevated, the membrane fails to be repaired and necrosis of the sarcoplasm takes place. Inflammatory cells rapidly invade the necrotic area and start to remove damaged tissue. Necrosis is followed by regeneration (F), in which muscle precursor cells proliferate, differentiate and fuse together to form myotubes and replace the necrotic muscle segment. It is proposed that the cytokine TNF can promote necrosis in preference to resealing. Adapted from Shavlakadze et al. (2004) and Hodgetts et al. (2006).
TNF
Basement membrane Sarcolemma Satellite cell
A. Dystrophic Myofibre
B. Damage to sarcolemma
TNF
F. RegenerationE. Necrosis
C. Resealing
Sarcoplasm
D. “Intact” myofibre

Chapter One Introduction
17
1.5.2. TNF activates c-Jun N-terminal Kinase (JNK)
In major inflammatory conditions, elevated levels of the key pro-inflammatory
cytokine, TNF results in a significant increase in skeletal muscle protein degradation
(Tisdale 2005). In addition, the stress-activated c-Jun N-terminal kinases (JNKs) have
also been suggested to be involved in the pathophysiology of major inflammatory
conditions (Strle et al. 2006) such as inflammatory bowel disease (Roy et al. 2008),
mouse models of DMD (Kolodziejczyk et al. 2001; Lang et al. 2004) and in rat models
of rheumatoid arthritis (Han et al. 2001).
JNKs are a subfamily of threonine/serine (Ser/Thr) mitogen-activated protein kinases
(MAPKs) which are activated in response to a number of stimuli, including pro-
inflammatory cytokines, stress stimuli such as UV irradiation, a range of growth factors
(Kyriakis and Avruch 2001). There are three JNK encoding genes and at least 10 splice
variants (Gupta et al. 1996). The products of JNK1 and JNK2 are ubiquitously
expressed, whereas JNK3 expression is generally considered to be restricted to the
central nervous system (Yang et al. 1997; Kumagae et al. 1999).
The JNKs act within a protein kinase cascade, which when stimulated by extracellular
stimuli (stress, UV, cytokines) or intracellular stimuli (ER stress). The JNKs undergo
dual phosphorylation by the MAPK kinases MKK4 and MKK7 (Butterfield et al. 1997;
Barr and Bogoyevitch 2001). As emphasised by the name, JNKs are able to
phosphorylated and activate the transcription factor c-Jun (Cheng and Feldman 1998)
via the phosphorylation of Serine 63 (Ser63) and Serine 73 (Ser73) in the N-terminus of
c-Jun (Derijard et al. 1994; Kyriakis and Avruch 2001). The binding of JNKs to the
amino-terminal region of c-Jun results in nuclear localisation and phosphorylation of
this transcription factor (Derijard et al. 1994) leading to the activation of a number of c-
Jun gene dependent events such as apoptotic cell death (Tibbles et al. 1996; Tanaka and
Hanafusa 1998).
Activation of JNKs may contribute to progression of the disease pathogenesis of
muscular dystrophy because the mdx mouse displays muscle specific activation of
JNK1 (Kolodziejczyk et al. 2001). However, the levels of phosphorylated JNKs in
dystrophic muscle alter depending on the muscle type (Kolodziejczyk et al. 2001). In
gastroconemius muscle from both 6 week old mdx and control normal mice, low levels

Chapter One Introduction
18
of phosphorylated JNK1 were detected in both strains, whereas there was a significant
difference in levels of activated JNK2 in mdx compared to controls (Nakamura et al.
2005). Previously, JNK1 expression was studied in 12 month old mdx and the
mdx:MyoD-/- mice. It was found that there was a marginal increase in phosphorylated
JNK1 in mdx hindlimb muscle lysates compared to normal controls, with a substantial
increase in activated JNK1 in the mdx:MyoD-/- lystates, compared to both the mdx and
wild type strains (Kolodziejczyk et al. 2001). However, analysis of mdx diaphragm
muscle showed increased phosphorylated JNK 1 compared to that observed in the wild
type. It has been recently reported that increased levels of phosphorylated JNK1 were
present in the diaphragms of 7 week old mdx mice when compared to age matched
C57BL/10 controls (Hnia et al. 2007). Alterations in the expression and/or
phosphorylation levels in the different dystrophic muscles are not limited to JNK1 and
2. It has been reported that in mdx muscle, the activation levels of ERK1/2 (p44/p42
MAPK), p70 S6 kinase (p70s6k) and p38 kinase are also dependant on the muscle type
(Lang et al. 2004).
It is also important to note that there are potential benefits of TNF relevant to muscle
regeneration during physiological conditions. A study by Chen et al (2007) showed that
C2C12 that were placed in low-serum differentiation medium release low amount of
TNF. The study also reported that upon addition of a TNF neutralizing antibody to the
differentiation medium, p38 activation was blocked and differentiation suppressed,
suggesting that TNF regulates myogenesis and muscle regeneration via p38.
1.5.3 IGF-1 and TNF cross talk: involvement of JNK
While there is a general consensus that TNF plays a critical role in skeletal muscle
atrophy, the precise role of TNF activated JNK in situations of TNF mediated myofibre
atrophy is still largely unknown. There is now strong evidence that TNF can inhibit
IGF-1 expression (Frost et al. 2003) or abrogate IGF-1 receptor signalling via inhibition
of tyrosine phosphorylation of the IGF-1 docking protein, IRS-1 (Rui et al. 2001; Frost
et al. 2003; Broussard et al. 2004; Broussard et al. 2003; Strle et al. 2006; Grounds et al.
2008). It has been proposed that this inhibitory effect of TNF on IGF-1 signalling
appears to be mediated by JNK phosphorylation of IRS-1 (Broussard et al. 2003; Strle
et al. 2006) (Figure 1.4a).

Chapter One Introduction
19
Studies examining the role of JNK in signalling downstream of the insulin receptor
propose that JNK binds to, and phosphorylates, IRS-1 on Serine 307 (Ser307) (Aguirre et
al. 2000; Aguirre et al. 2002) or on Serine 318 (Ser318) (Mussig et al. 2005).
Phosphorylation of Ser307 and Ser318 induces a conformational change in the
phosphotyrosine binding domain of IRS-1, thus reducing its affinity for the insulin
receptor (Hiratani et al. 2005). IRS-1 is also considered to be a docking protein for the
IGF-1 receptor (Keller et al. 1993) (Figure 1.4a). Phosphorylation of IRS-1 on Ser307
downstream of the IGF-1 receptor results in inhibition of the PI3/AKT/mTOR pathway,
the predominant pathway downstream of IGF-1 signalling responsible for protein
synthesis (Rommel et al. 2001; Latres et al. 2005).
The role of JNK in mediating TNF induced inflammatory events and protein
degradation in skeletal muscle is only just beginning to be explored and much is still not
known. As such, the therapeutic potential of protein kinases are being increasing
targeted and investigated in the search for new therapies (Bogoyevitch et al. 2005). The
use of inhibitory peptides has allowed researchers to study the biological functions of
JNK in mammalian systems without the need for JNK gene knockout models. Of
particular interest to this study, a JIP-derived JNK inhibitor has been previously used to
establish that JNK mediates TNF suppression of IGF-1 in differentiating skeletal muscle
cells (Strle et al. 2006). Recently, the implications of TNF induced JNK activation in
skeletal muscles was also discussed, with the authors hypothesising that the inhibition
of JNK is beneficial for muscle wasting diseases such as DMD (Grounds et al. 2008).
Since it has been confirmed that JNK is a negative regulator of IGF-1 signalling in
C2C12 myoblasts (Strle et al. 2006), the next stage is to target JNK for inhibition in
C2C12 cell cultures models of TNF induced myotube atrophy (Fig .1.4b and see
Chapter 3).
Compared to other MAPKs pathways, the JNK pathway is defined by its interaction
with the JNK-interacting protein (JIP) family of scaffold proteins. Barr et al (Barr et al.
2002) demonstrated that an 11-mer peptide (TI-JIP) potentially inhibited JNK activity in
vitro. Through conjugation to the Tat peptide, it is rendered cell permeable and have
thus been used to investigate the investigate the effects of JNK in cells (Borsello et al.
2003; Kendrick et al. 2004; Kaneto et al. 2004). The specific cell permeable JNK
inhibitory peptides derived from JIP assessed in the present study (Section 1.5.4).

Chapter One Introduction
20
Figure 1.5a: Damaging effects of TNF in skeletal muscle is proposed to be mediated by JNK inhibition of IGF-1 signalling. In this image (A) TNF ligand induced activation of TNF-R results in the activation of c-Jun N Terminal kinase (JNK). (B) The damaging effects of TNF on skeletal muscle have been identified as to be mediated by JNK associating with IRS-1. Activated JNK phosphorylates IRS-1, which induces a conformational change and impairs the ability of IRS-1 to associate with IGF-1R resulting in the inhibition of IGF-1 signalling. (C) The absence of IGF-1 receptor binding to IRS-1 possibly results in a decrease in protein synthesis and an increase in protein degradation and muscle necrosis. Figure adapted from Grounds et al. (2008).
Figure 1.5b: Potential use of JNK inhibitors for preventing JNK mediated down regulation of IGF-1 signalling in skeletal muscle (A) TNF ligand induced activation of TNF-R results in the activation of c-Jun N Terminal kinase (JNK) (B) By targeting JNK for inactivation by specific JNK inhibitors, this counteracts the inhibitory action of JNK on IGF-1 signalling. (c) IGF-1 signalling is maintained which results in increase muscle protein synthesis and down regulation of muscle atrophy and necrosis. Figure adapted from Grounds et al. (2008).

Chapter One Introduction
21
1.5.4 Inhibitors of JNK kinases
The therapeutic potential of targeting protein kinases is a topic of increasing recent
interest; for comprehensive reviews see (Bogoyevitch et al. 2004; Bogoyevitch et al.
2005; Bogoyevitch and Arthur 2008). Studies involving determining the function of
JNK have largely depended on the use of blockers to inhibit JNK activity. These JNK
inhibitors have been categorised into two groups; chemical inhibitors that are ATP-
competitive (target the ATP binding site of JNK and subsequently other MAPK) and
newer peptide inhibitors that are ATP-non-competitive (directly bind to JNK)
(Bogoyevitch 2005).
1.5.4.1 ATP-competitive
ATP-competitive protein kinase inhibitors are peptides that compete for the ATP-
binding site of protein kinases and therefore inhibit protein kinase activity (Bogoyevitch
2005). Currently the most widely used inhibitor of the JNKs is SP600125
(anthra[1,9]pyrazole-6(2H)-one) (Bennett et al. 2001; Bogoyevitch 2005), although its
specificity has been questioned (Bain et al. 2003). However, when administered to
C2C12 myoblasts, SP600125 considerably attenuated the protein expression of the pro-
inflammatory cytokines TNF, IL-1 and LPS induced IL-6 (Frost et al. 2003). As it is
beyond the scope of this present study to review the structure, mode of activity and
therapeutic use of SP600125, the following reviews (Bogoyevitch 2005; Bogoyevitch
and Arthur 2008) should be consulted for a more detailed discussion.
AS601245 ((benzothiazol-2-yl) acetonitrile) is another new ATP competitive inhibitor
that is commercially available (Gaillard et al. 2005; Bogoyevitch and Arthur 2008).
AS601245 has shown to be beneficial in models of focal and global cerebral ischemia
(Carboni et al. 2004; Carboni et al. 2007). It has also been shown that treatment with
AS601245 resulted in a significant reduction on infarct size caused by myocardial
ischemia in anaesthetized rats (Ferrandi et al. 2004). Recently AS6001245 was also
successfully administered in a neonatal rat model of pneumococcal meningitis to
demonstrate that JNK may not be involved in pneumococcal meningitis-induced
hippocampal apoptosis (Sury et al. 2008).

Chapter One Introduction
22
1.5.4.2 ATP-non-competitive
ATP-non-competitive competitive protein kinases are peptides that do not compete for
the ATP-binding site of protein kinases, but through other mechanisms, such as
competing for binding to the peptide or protein binding site to inhibit protein-kinase
activity (Bogoyevitch 2005). The JIP derived peptides, such as TAT-TIJIP, TI-JIP,
JNKI-1 peptides (JIP-1-HIV-TAT, L-JNKI-1 and the protease-resistant D-amino acid
retroinverse peptide D-JNK1) have been shown to kinetically act in a substrate
competitive manner (Barr et al. 2004) and bind directly to the substrate docking domain
of JNK (Barr et al. 2004).
The cell permeable JNK inhibitors (TAT-TIJIP and D-JNKI-1) are composed of two
molecular structures. Both inhibitors contain a common cell permeable, 10 amino acid
human immunodeficiency virus-Tat cell transport sequence (TAT), that facilitates the
entry of the inhibitor into the target cells (Vives et al. 1997). The inhibitors are different
in their JNK binding sequences; TAT-TIJIP contains an 11 amino acid sequence
(Truncated Inhibitor of JNK Interacting Protein; TIJIP) (Kendrick et al. 2004) whereas
D-JNKI-1 contains a longer 20 amino acid sequence (JNK Binding Domain) (Borsello
et al. 2003).
The shorter of the two inhibitors (TAT-TIJIP) has been shown to have a beneficial
effect in preventing necrotic cell death in vitro (Arthur et al. 2007), whereas the longer
JNKI-1 peptides have been reported to be neuroprotective when tested in vivo in rat
models of cerebral ischemia (Borsello et al. 2003).
The protective effects of the ATP-competitive inhibitor SP600125, AS60125 and the
ATP-non-competitive inhibitor TAT-TIJIP in preventing TNF induced myotube atrophy
in cultured skeletal muscle cells Chapter 4 and 5 and in vivo in mdx mice models of
exercised induced skeletal muscle necrosis in Chapter 6.

Aims and Hypothesis
23
Aims and Hypothesis of the Thesis
Overall Aim
To determine the mechanisms by which TNF induces atrophy in differentiated skeletal
muscle cells.
Specific Aims
1. Validate, replicate and optimise a C2C12 muscle cell culture model of IGF-1 induced
myotube hypertrophy (Chapter 3).
2. Optimise a C2C12 cell culture model of TNF induced myotube atrophy (Chapter 4).
3. Determine to what extent TNF induced JNK signalling plays a part in mediating TNF
induced myotube atrophy and inhibiting IGF-1 induced hypertrophy (Chapter 5).
4. Test the effectiveness of the JNK inhibitor TAT-TIJIP in vivo on reducing exercised
induced myofibre necrosis (Chapter 6).
Hypothesis
The central hypothesis of the thesis is that the damaging effects of TNF on skeletal
muscles are mediated by interference, via JNK, with IGF-1 receptor signalling. It was
further proposed that:
1. Administration of TNF to myotubes in tissue culture will induce myotube atrophy
and will prevent IGF-1-mediated myotube hypertrophy.
2. Inhibition of TNF activated JNK (using JNK inhibitors) will prevent the TNF-
mediated myotube atrophy in tissue culture.
3. In vivo administration of JNK inhibitors will reduced TNF-mediated necrosis of
dystrophic muscles in mdx mice.

Chapter Two Materials and Methods
24
Chapter Two
Materials and Methods
2.1 Cell culture
In this research, immortalised and primary muscle cell cultures were used. Immortalised
cell lines were commercially purchased from the American Type Culture Collection
(ATCC; Manassas, USA). Primary muscle cell cultures were prepared from mice as
detailed below in Section 2.1.3.1. Primary cultures were included as a skeletal muscle
cell model that bears closer resemblance to muscle in vivo, compared to immortalised
cultured rodent muscle cell lines, and provided a useful additional in vitro model to
study the morphological effects of treatments on myotubes.
2.1.1 Immortalised muscle cell lines
2.1.1.1 C2C12 murine myotube cultures
The C2C12 murine skeletal myoblast (Yaffe and Saxel 1977) cell line was purchased
from the ATCC (Manassas, USA). In this study, two batches (with different passage
numbers) of C2C12 myoblast cultures were used. Initial optimisation experiments were
performed on C2C12 myoblasts that had been through at least 25 passages (actual final
passage number unknown). Due to the high passage number, these cells were not
suitable for further studies and a new batch of cells was purchased. Final hypertrophy
experiments and subsequent signalling studies were performed using these cells at
passages 4 to 6.
2.1.1.2 L6 rat myotubes cultures
The L6 rat skeletal myoblast (Yaffe 1968) cell line was provided by the Department of
Biochemistry, The University of Adelaide, Adelaide, South Australia (1992). The
passage number of these cultures is unknown.
2.1.2 Animal strains
All strains of mice were obtained from the breeding colonies established at the Animal
Resource Centre (ARC) in Murdoch, Western Australia. The mice were bred under

Chapter Two Materials and Methods
25
specific pathogen free conditions. The mice were housed in standard animal cages at the
Biological Sciences Animal Unit, at the University of Western Australia. The mice were
maintained at 12-hour day-night cycle and allowed access to standard chow and
drinking water ad libitum. All experiments were conducted in strict accordance with the
guidelines of the University of Western Australia Animal Ethics Committee and the
National Health and Medical Research Council, Australia.
2.1.2.1 Animals used for primary muscle cell culture preparations
For the preparation of primary muscle cell cultures, adult 4-5 weeks old transgenic mice
which over-express Class 2 IGF-1 Ea (IGF:C2) in skeletal muscles (Shavlakadze et al.
2005) and the background FVB strain (a wild-type control) were used.
2.1.2.2 Animals used to test the effects of the JNK inhibitory peptide TAT-TIJIP
Adult 6 week old male dystrophic mdx mice (c57BL/10ScSnmdx/mdx) were used to test
the protective effects of the JNK inhibitor TAT-TIJIP in vivo (see Chapter 6).
2.1.3 General cell culture conditions
2.1.3.1 Preparation of primary cell cultures
Myoblasts were isolated from skeletal muscles of 4 to 5 week old IGF:C2 and FVB
mice to establish the primary muscle cultures. The mice were sacrificed and dipped in
70% (v/v) ethanol. The muscles from the legs, hips and back were then excised and
placed in Dulbecco’s Modified Eagle Medium (DMEM; Invitrogen, Vic, Australia)
containing 20 µg/ml gentamycin antibiotic (Sigma-Aldrich, NSW, Australia). The
muscles were then rinsed with 3-4 changes of Phosphate Buffered Saline (PBS; 145mM
NaCl, 7.50mM Na2HPO4, 2.85mM NaH2PO4.2H20 pH 7.4) before being placed in a
sterile petri dish where special care was taken to remove tendons and nerves from the
muscle.
The muscles were then transferred to a petri dish and minced with scissors in
dissociation buffer (200U/ml collagenase type 1, and 200 U/ml dispase in 200ml
DMEM) at room temperature (RT) for 5 min. The dissociation buffer with released cells
was collected and mixed with a further 20 ml of dissociation buffer and placed in a flask
for further steps in trypsination. The tissue was digested by placing the flask on a pre-
warmed stirring plate in a 37ºC incubator for 45 min with stirring. The solution was

Chapter Two Materials and Methods
26
transferred to a 50 ml tube and centrifuged at 1500 rpm for 5 min at RT. The
supernatant was discarded and the pellet washed twice by re-suspending in PBS and re-
centrifuging at 1500 rpm, for 5 min at room temperature. The cell pellet was re-
suspended in 20 ml Trypsin/EDTA (Sigma-Aldrich), transferred to a clean flask and
placed at 37ºC with stirring for 10 min. Trypsin was inhibited by the addition of 1ml
FCS. The solution was transferred to a 50 ml tube and centrifuged for 5 min at 1500
rpm at RT. The cell pellet was resuspended in 20 ml primary cell growth medium
consisting of DMEM supplemented with 20% foetal calf serum (FCS, Sigma-Aldrich)
1% GlutaMAX-1 (Invitrogen), 1% penicillin/streptomycin Invitrogen) and 12.5 ng/ml
basic Fibroblast Growth Factor (bFGF; Sigma-Aldrich), and filtered through a 0.2 µm
sterile filter. The solution was then transferred to a 0.1% collagen coated flask and
incubated for 2 h at 37ºC in a saturated humidity atmosphere containing 5% CO2/95%
air in an incubator (Crown Scientific, WA, Australia) (This is pre-plate 1; PP1).
To remove contaminating fibroblasts, the supernatant with un-adhered cells was
transferred to another collagen coated flask with medium replenished (10 ml of primary
cell proliferation medium) at 37ºC, 5% CO2/95% air atmosphere for a further 24 h
(PP2). This process of pre-plating was continued for a further 3 days. By PP5-6,
myoblast purity was verified as > 80% through immunohistochemical staining with
monoclonal mouse anti-desmin clone DE-U-10 (D1033, Sigma-Aldrich) as described in
Section 2.4.2.
2.1.3.2 Resurrection of cyropreserved cell stocks
Immortalised skeletal muscle (C2C12 and L6) myoblasts were resurrected from
cryopreserved stocks, which had been frozen down at concentrations of approximately 1
x 105 cells/ml in 1 ml of proliferation (high serum) medium, consisting of DMEM
supplemented with 20% FCS and 1% penicillin/streptomycin, with the addition of 10%
dimethylsulphoxide (DMSO; Sigma-Aldrich). The cell stocks were stored in liquid
nitrogen until required.
Cells were thawed on ice and resuspended in 9 ml of proliferation medium under sterile
conditions in a laminar flow biological cabinet. The medium was pre-warmed in a 37ºC
water bath prior to use. Cells were then centrifuged at 1500 rpm for 3 min using an
Eppindorf Centrifuge 5702 (Crown Scientific); the supernatant was then discarded and

Chapter Two Materials and Methods
27
the cells resuspended in 10 ml of proliferation medium. The cell suspension was then
transferred to a 75cm2 flask. For proliferation, cells were grown in 10 ml proliferation
medium at 37°C in 5% CO2/95% air atmosphere.
2.1.3.3 Trypsinising and seeding cells onto plates
Myoblasts were cultured until they reached 70% confluence; the proliferation medium
was then removed and the cells were washed once with 4 ml of sterile PBS. This
ensured that all remaining media was removed, as this can interfere with the
Trypsin/EDTA reaction. PBS was discarded and 4 ml of Trypsin/EDTA solution was
added to the flask. This was gently agitated by hand for 2 to 3 min causing cell rounding
and detachment from the surface of the flask, cell detachment was confirmed by
microscopic examination. The Trypsin reaction was stopped by adding 6 ml of
proliferation medium; the cell suspension was then pelleted at 1500 rpm for 3 min in a
sterile 15 ml Falcon tube in an Eppindorf Centrifuge (model 5702). The supernatant was
then discarded and the cells resuspended in a 1 ml proliferation medium. Ten microliters
of cell suspension was removed and mixed with 90 µl of Trypan Blue solution (Sigma-
Aldrich), resulting in a 1 in 10 dilution. The extent of dilution in Trypan Blue was
dependant on the size of the pellet observed after centrifugation. Ten microliters of the
Trypan Blue/cell solution was placed on a Neubauer haemocytometer to determine the
total cell count. Cells that had a blue appearance were considered dead and not counted
(Figure 2.1). The four individual squares were counted separately and the total count
was averaged. The concentration of the cell suspension is calculated according to
Formula 1:
Formula 1: Cells/ml = sum of cells in four squares x dilution factor x 104
4
The multiplication factor (104) is derived from the volume of each of the four counted
squares, which are 0.1 mm deep and 1 x 1 mm square. This equates to a volume of 0.1
mm3 or 0.0001 ml (10-4 ml).

Chapter Two Materials and Methods
28
Figure 2.1: Neubauer haemocytometer. Cells are counted in the four large squares (A,B,C and D) which are further subdivided into 16 smaller squares. The average number of cells is taken and multiplied by 1 x 104 and the Trypan blue dilution factor. Cells are only counted on the lower and right hand lines (5 grey cells), with those falling outside, on top of left line (3 whites cells) omitted.
The amount of cell suspension required depended on the intended use of the cells and
the size and number of wells to be seeded, and was diluted to the appropriate volume in
proliferation medium (Table 2.1). Generally (except during the optimisation of plating
conditions, see Section 3.1.1) for the morphology studies, C2C12 myoblasts were plated
at a concentration of 1 x 105 cells per dish in proliferation medium, and primary muscle
cells were plated at 2.5 x 105 cells per dish in primary cell growth medium. Cells were
plated on glass cover slips (Menzel-Glaser, Germany) and coated with a 0.01% collagen
(type I) solution (Invitrogen) (diluted in PBS) in 35 mm2 plastic dishes (Falcon). In the
initial tissue culture experiments (detailed in Section 3.1.1), dishes were also coated
with 0.1 mg/ml Poly-D-Lysine (PDL) (Chemicon, Vic, Australia) diluted in PBS. For
studies requiring protein extraction (Cell signalling studies: Chapter 5), C2C12
myoblasts were plated at a concentration of 5 x 105 cells/dish in 60 mm2 uncoated
plastic dishes (Table 2.1).

Chapter Two Materials and Methods
29
Table 2.1 Dimensions of various tissue culture plates and the myoblast plating densities used in
these studies.
Usage of cells Size of well/dish Growth area (cm2)
Growth volume
Cell density (cells/well)
C2C12: 1 x 105 cells Morphology Studies
35 mm2 dish 8 2 ml Primary: 2.5 x 105 cells
Protein Extraction
60 mm2 dish 21 5 ml 5 x 105 cells
Cell fusion was induced by changing the medium from proliferation to low serum
medium (DMEM supplemented with 2% horse serum (HS)) at 48 h after plating, or
once cells had reached 70% confluence; this is termed ‘day 0’ of fusion. Fusion medium
was changed every 48 h until treatment commenced.
2.2 Reagents and Antibodies
2.2.1 Treatment reagents
Analogues of IGF-1; ‘LONGTMR3IGF-I’ and Des(1-3)IGF-1 were purchased from
GroPep (SA, Australia). Mouse recombinant Tumour necrosis factor-alpha (TNF) was
purchased from Chemicon (Vic, Australia) and both Anisomycin (A 9789), a control for
stimulating phosphorylation of c-Jun N terminal Kinase (JNK) (Cuenda and Cohen
1999) (described in detail in Section 5.1) and Insulin (15500) were purchased from
Sigma-Aldrich.
2.2.2 JNK inhibitory peptides
The ATP competitive inhibitor of JNK SP600125 was purchased from Sigma-Aldrich
and AS601245 was purchased from Sapphire Bioscience (NSW, Australia). The TAT
control peptide; a cell permeable 10 amino acid Tat cell transport sequence (TAT) and
the cell permeable JNK inhibitory peptide TAT-TIJIP; a shorter peptide inhibitor
comprising of an 11 amino acid sequence (Truncated Inhibitor region of JNK
Interacting Protein; TIJIP) linked to TAT, were all synthesised by AusPep (Parkville,
Australia). Peptide purity was at least 80% as determined by mass spectrometry. The
sequence of TAT-TIJIP was GRKKRRQRRRPPRPKRPTTLNLF, with the sequence
of TIJIP indicated in bold and underlined.

Chapter Two Materials and Methods
30
2.3 Antibodies
2.3.1 Western blotting
Primary antibodies against phospho-JNK (#4671) and total JNK protein (#9258) were
purchased from Cell Signaling Technologies (Beverly, MA, USA). Phospho-AKT (Ser
473, #4058S) and AKT (#9272) were purchased from Cell Signaling Technologies,
IRS-1 (IRS-1 c20:sc-559, Santa Cruz, CA, USA ). Monoclonal phosphotyrosine pY99
(sc-7020, Santa Cruz) and the secondary horseradish peroxidase (HRP)-conjugated anti-
rabbit antibody were purchased from Sigma-Aldrich (NSW, Australia).
2.3.2 Immunohistochemistry
Primary antibodies were obtained as follows: monoclonal mouse anti-desmin clone DE-
U-10 (D1033, Sigma-Aldrich) and mouse polyclonal phospho-c-Jun (#9165, Ser 63/73)
antibody (Cell Signaling). Secondary antibodies were goat anti-mouse IgG conjugated
to Alexa Fluor 488 (A11001, Molecular Probes, Invitrogen, Australia) and donkey anti-
rabbit IgG conjugated to Alexa Fluor 594 (A21207, Molecular Probes).
2.4. Myotube morphology studies
2.4.1 Treatment regime for myotube cultures
Due to the slow rate at which the myoblasts fused into myotubes, C2C12 cells were
treated on day 7 of fusion, whereas treatment of the primary myotube cultures began on
day 4 after fusion medium (see Chapter 4). An analogue of IGF-1 known as
‘LONGTMR3IGF-I’ (Grow-Pep, SA, Australia) was added to the myotubes at a
concentration of 10 ng/ml, and mouse recombinant TNF (Sigma-Aldrich) was added a
concentration of 20 ng/ml. For all muscle cell cultures, the medium and treatment were
replaced at 24 h intervals for 3 days.
For studies where TNF treatment was combined with the JNK inhibitors (and respective
controls), myotubes were pre-treated for 1 h with the test JNK inhibitor before TNF
treatment was administered. Both treatments were then replaced daily for 3 days.

Chapter Two Materials and Methods
31
2.4.2 Immunohistochemistry
After 3 days of treatment (C2C12 - fusion day 10; primary cultures - fusion day 7) cells
(fused on glass coverslips) were fixed for 15 min in 3% formaldehyde made up in PBS.
After 3 washes with PBS, the cells were incubated for 60min at RT in blocking buffer to
minimise non-specific antibody binding: 10% FCS diluted in PBS wash buffer (0.1%
Saponin (Sigma-Aldrich); 0.5% Bovine Serum Albumin (BSA; Sigma-Aldrich)). For
the myotube morphology studies (Chapters 3 and 4) the cells were incubated with 1:300
dilution primary monoclonal mouse anti-desmin (Sigma-Aldrich) at 4ºC overnight.
Following this, the primary antibody was then removed by washing the cells 3 times
with PBS wash buffer before the addition of the appropriate secondary antibody (used at
a dilution of 1:250). Goat anti-mouse IgG conjugated to Alexa Fluor 488 (Molecular
Probes) was applied to the cells for 60 min at RT. Cells were again washed 3 times and
the nuclei were stained for 1 min with 50 µg/ml Hoechst Nuclear Stain HO33342
(Sigma-Aldrich). The cells (on the glass coverslips) were mounted on superfrost glass
slides (Menzel-Glaser) using Polyvinyl Alcohol mounting medium (PVA; P8136-7,
Sigma-Aldrich) and stored at 4ºC. The primary antibody was omitted from one of the
coverslips to serve as a negative control.
2.4.3 Image analysis: measuring myotube widths
The slides (myotubes) were viewed under a Nikon Eclipse 90i microscope with the
filters set to 485 nm excitation and 520 nm emission for green fluorescence (to visualise
desmin staining); 544 nm excitation and 590 nm emission for red fluorescence (to
visualise phospho c-Jun stain); and 357 nm excitation and 540 nm emission for blue
fluorescence (to visualise nuclear stain). Images were captured with a Photometrics
Cool Snap ES camera and personal computer with Digital Optics V++ v.4.0 software.
For each slide (representing 1 myotube dish) the total number of fields per coverslip
was calculated using the Image Pro Plus v.4.5.1.29 software (Image Pro Plus) and
assigned a number. From each coverlslip, random fields were selected for analysis using
the random number generator function in Microsoft Office Excel 2003. From each
myotube dish a total of 10 random images were captured with a 10x objective (Figure
2.2).

Chapter Two Materials and Methods
32
To quantify myotube widths, 5-6 myotubes were selected from each of the 10 images,
resulting in a total of 50 myotubes being counted in each dish. Before each measuring
session, the system was geometrically calibrated with an image containing an object
micrometer. For each myotube, widths were sampled 50 µm apart using measuring tools
in Image Pro Plus; an example of 1 of the 10 images that were taken from each dish is
shown in Figure 2.2. Width measurements were imported into a Microsoft Office Excel
spreadsheet and averaged for each myotube (Figure 2.2). The widths that were
measured (each spaced 50 µm apart) along the entire length of the first myotube, and the
average width for that myotube is highlighted in the red box in Figure 2.2. The average
widths for each of the 6 myotubes analysed (from this particular field) is shown in red
font in Figure 2.2. Once all the myotubes from each of the 10 images/dish had been
measured, the average widths of each myotube (in red font) were summed and then
divided by the number of myotubes counted for that dish. This then resulted in 1 mean
width calculated per dish for each dish. For each treatment, a minimum of 3 myotube
culture dishes were sampled and analysed.

Chapter Two Materials and Methods
33
Figure 2.2: Measuring myotube widths using Image Pro Plus software. Representative immunofluorescent photomicrograph of day 10 C2C12 myotubes stained with anti-desmin antibodies (in green) viewed using Image Pro Plus software. Routinely, 10 random images were photographed from each treatment dish and myotube widths were recorded using the software. Each width measurement was uploaded into a Microsoft Excel spreadsheet from which statistical analyses was performed. Magnification: 10x. Scale bar: 100 µm.
2.4.4 Statistical analyses
Myotube widths are expressed as means with standard error (SE +). A one-way analysis
of variance (ANOVA) and unpaired Student’s t-tests were used to assess the level of
statistical significance of the difference between treatment and control groups for tissue
culture experiments. A ‘P’ value of < 0.05 was considered significant. All statistical
analyses were calculated using Microsoft Office Excel.
2.5 Western blot quantitation of JNK phosphorylation in day 7 C2C12 myotubes
2.5.1 Treatment regime for western blot analysis of phospho-JNK
Day 7 C2C12 myotubes were serum starved for 5 h before being treated with IGF-1 (10
ng/ml), TNF (20 ng/ml) or Anisomycin (5 nM), with protein extracted at various time
points following stimulation, except for Anisomycin treatment, where protein was

Chapter Two Materials and Methods
34
routinely extracted 15 min following stimulation to serve as positive control for JNK
phosphorylation.
2.5.2 Extraction and sample preparation
Following treatment, C2C12 myotubes were washed once with ice cold PBS and lysed
in an ice cold stress lysis buffer (20 mM HEPES pH 7.7, 2.5 mM MgCl2, 0.1 mM
EDTA, 20 mM b-glycerophosphate, 100 mM NaCl, 0.1% Triton X 100, 500 µM DTT,
100 µM Na3VO4, 100 µg/ml PMSF, 0.01% NP40, protease inhibitor cocktail tablet
(Roche 04693159001) and incubated on ice for 20 min. Cell lysates were centrifuged at
12,000 x g and the supernatant was stored in 100 µl aliquots at -80°C until used for
analyses. Protein was quantitated using the Bradford assay (see below).
2.5.3 Protein quantitation
Protein quantitation was performed using a Bio-Rad Protein Assay Kit (Bio-Rad
Laboratories, Gladesville, NSW). The kit is based on the Bradford method, using BSA
(Sigma-Aldrich) as a standard. Protein samples were quantitated with reference to a
standard absorbance curve, which was generated by measuring the OD of known
Bovine Serum Albumin (BSA) standards. The BSA standards were prepared by serial
dilutions of BSA in PBS (Table 2.2).
Table 2.2: Concentration of BSA in the protein assay standards
Standard BSA concentration
Standard 1 100 µg/ml
Standard 2 200 µg/ml
Standard 3 300 µg/ml
Standard 4 400 µg/ml
Standard 5 500 µg/ml
Each standard was aliquoted (10 µl) in duplicate glass tubes. The samples to be
analysed were then diluted 1:10 in PBS and 10 µl of each sample was aliquoted into
new tubes in duplicates. Following this, 200 µl of Bio Rad Reagent was added to each
tube, vortexed and left to stand for 10 min at RT before being analysed using a

Chapter Two Materials and Methods
35
spectrophotometer (Beckman DU Series 640, Beckman Instruments Inc, Fullerton, CA,
USA). The spectrophotometer was zeroed using PBS and the samples were measured in
the visible spectrum at 750 nm. The protein content of each homogenate was calculated
from the standard curve.
2.5.4 Protein sample preparation
2.5.4.1 Whole cell lysates
Each 100µl aliquot of homogenate was mixed with 50 µl of 3 x Protein loading buffer
(1 M Tris pH 6.8, 6% SDS, 30% Glycerol, 0.02% β-mercaptoethanol, 6% bromophenol
blue), briefly vortexed, heated at 95ºC for 5 min, and then chilled on ice until loaded
onto the gel.
To calculate the volume of the sample to be loaded, a simple formula was used. For
examples: to load 100 µg of protein from a homogenate sample (concentration of 6
µg/µl), into a well in the gel that holds a maximum of ~40 µl, 25 µl of the sample (in
protein loading buffer) was combined with 10 µl of PBS, bringing the total volume of
the sample to 35 µl. To avoid spillage all samples were made up to ~35 µl using PBS.
2.5.4.2 Immunoprecipitation of IRS-1
For the immunoprecipitation (I.P.) of IRS-1, following the appropriate treatment, the
cell lysates were prepared as previously described (see Section 2.5.2). Once protein
quantitation had been performed (see Section 2.5.3), immunoprecipitation was
performed from approximately 1mg (1000µg) of protein. Supernatants were incubated
with 2-5 µg of anti-IRS-1 antibody and protein A-Sepharose 4B Fast Flow beads (P-
9424, Sigma-Aldrich) for anywhere between 2-12 h (when attempting to optimise the
protocol) at 4ºC and with/without rotation and for 2 h (when performed in Dr John
Whitehead’s laboratory - Chapter 5) at 4ºC without rotation. Immunocomplexes were
then washed at least 5 times in an ice cold stress lysis buffer and resuspended in a
protein loading buffer. The samples were then subjected to SDS-PAGE.
2.5.5 SDS Polyacrylamide Gel Electrophoresis (SDS-PAGE)
Protein samples were resolved by SDS-PAGE under denaturing conditions on 12%
(resolving) polyacrylamide gel. The preparation and composition of this gel is described
below (Table 2.3a). After ensuring that no air bubbles formed and that the gel surface

Chapter Two Materials and Methods
36
had set flat, the resolving gel was carefully poured in the glass plate assembly and then
overlaid with ddH2O. The gel was then left to polymerize for approximately 20 min.
Following this, ddH2O was removed and the stacking gel (composition outlined in
Table 2.3b) was poured on top of the set resolving gel.
Table 2.3a: Composition of Resolving gel: 12% polyacrylamide in 1 M Tris-HCL pH 8.8
1M Tris (pH 8.8) 3.75 ml
30% Acrylamide
(37.5:1. Acrylamide/bis) 4 ml
ddH20 2.2 ml
20% SDS 50 µl
TEMED 10 µl
APS (@ 0.2 mg/µl) 75 µl
Table 2.3b: Composition of Stacking gel: 6% polyacrylamide in 0.5 M Tris-HCL pH 6.8
1M Tris (ph 6.8) 1.25 ml
30% Acrylamide
(37.5:1. Acrylamide/bis) 2 ml
ddH20 6.7 ml
20% SDS 50 µl
TEMED 10µl
APS (@ 0.2 mg/µl) 75 µl
Spacers were inserted and the gel was allowed to set. Once the stacking gel had
polymerized, the gel casting chamber was transferred to a chamber filled with 1x
Electrode Buffer (5x Electrode Buffer, pH 8.3: 15 g Trizma Base, 72 g Glycine, 5 g
SDS made up to 1 L with ddH2O). The spacers were removed and the wells were
flushed with electrode buffer to ensure that there was no unpolymerised polyacrylamide
remaining. The samples and 15 µl of the SeeBlue Plus2 Pre-stained protein standard

Chapter Two Materials and Methods
37
(Invitrogen) were loaded onto the gel, the gel was then electrophoresed for 90 min at
140 V.
2.5.6 Protein transfer for western blotting
Polyvinylidene difluoride (PVDF) membrane (Amersham) was soaked in methanol and
washed with ddH2O. The membrane, filter paper and sponge pads were pre-soaked in
cold transfer buffer (3.03 g Trizma Base, 14.4 g Glycine, 200 ml Methanol made up to 1
L with ddH2O) for 30 min at 4ºC prior to transfer.
Following electrophoresis, the gel was removed from the casting chamber. The transfer
cassette was then assembled as illustrated in Figure 2.3. The gel was then placed in the
electroblotting tank and the tank was then filled with cold transfer buffer (4ºC). The
proteins were transferred from the gel to the PVDF membrane via electrophoresis for 90
min at 100 V. A frozen cooling unit was placed into the transfer chamber immediately
prior to transfer and replaced every 45 min. Following transfer, the transfer cassette
were removed from the tank and the PVDF membrane was washed in Tris Buffered
Saline (TBS pH 7.5: 12.1 g Trizma Base, 9.0 g NaCl made up to 1 L with ddH2O and
pH with 0.5 M HCl ) with 0.1% Tween-20 (TBS-T) for 15 min.
Figure 2.3: Illustration of the Western blotting transfer cassette. The cassette is inserted into the transfer cell with the gel nearest the cathode (+).
2.5.7 Blocking non-specific antibody binding
Prior to immunoblotting the membranes were incubated with blocking solution
consisting of TBS-T supplemented with 5% non-fat milk powder for 1 h at RT with
gentle agitation. The membrane was then rinsed in TBS-T for 5 min.
Sponge pad Pre-wetted filter paper Nitrocellulose membrane PAGE gel Pre-wetted filter paper Sponge pad -
+

Chapter Two Materials and Methods
38
2.5.8 Protein detection
The membrane was incubated with diluted primary antibody (rabbit anti phospho-JNK
#4671 or rabbit anti-JNK #9258 - Cell Signaling Technology) overnight at 4ºC. All
procedures were performed according to manufacturer protocols. Primary antibodies
were diluted 1:1000 in TBS-T with 5% BSA. Following incubation in primary antibody,
the membrane was washed 3 times for 20 min in TBS-T and incubated in secondary
antibody. The secondary antibody used for detection of the primary antibodies was goat
anti-rabbit (#31460, Pierce Biotechnology, Thermo Fisher Scientific, Sydney, Australia)
at a dilution of 1:10,000 in 5% milk TBS-T. Following incubation with the secondary
antibody, the membrane was washed 3 times for 20 min in TBS-T.
2.5.9 Chemiluminescent signal detection to observe protein
The protein signal was detected by chemiluminescence using ECL detection kit (Pierce
Biotechnology). Membranes were incubated for 5 min in the SUPERSIGNAL substrate
working solution (1:1 mix of lumino/enhancer solution and stable peroxiodase solution).
Following incubation, the chemiluminescent signal was detected using Kodak Image
Station 200 mm.
2.5.10 Densitometry for AKT signalling study
Gels were scanned using a Hewlett Packard HP ScanJet 5370C and the images saved as
TIFF files at 300dpi resolution. Densitometry was performed on TIFF images using the
NIH Image freeware program ‘ImageJ: Image Processing and Analysis in Java”
(http://rsb.info.nih.gov/ij/).
2.6 Animal studies to test the effects of TAT-TIJIP
Adult 6 week old male dystrophic mdx mice (c57BL/10ScSnmdx/mdx) were obtained from
the Animal Resource Centre, Murdoch, Western Australia and maintained as previously
described (see Section 2.1.2).
2.6.1 Exercise induced muscle damage in adult mdx mice
To determine the effects of the JNK inhibitor TAT-TIJIP on exercise induced
dystrophic muscle necrosis (Chapter 6), male mdx mice (6 weeks of age) were caged
individually in 32x25x15cm rat cages and given access to a standard metal mouse

Chapter Two Materials and Methods
39
exercise wheel for 48 h. Wheels had a circumference of 30 cm and hung from the roof
of the cage to avoid possible obstruction from bedding (Figure 2.4). The amount of
voluntary exercise was calculated as distance travelled over 2 nights with a Huffy
bicycle pedometer that detected the number of wheel rotation via a small magnet
attached to the wheel (Radley and Grounds 2006).
Figure 2.4: Exercise equipment for voluntary running. Yellow arrows indicate wheel with magnet attached and white arrows indicate bike distance recorder attached to cage. Image adapted from Waters (2006).
The mice were separated into two groups; one group was treated with 10 mg/kg body
weight TAT-TIJIP while the control group received ddH20 only (diluent for TAT-TIJIP)
via intra-peritoneal injections using a 27 G x 0.5 inch needle 24 h prior to exposure to
voluntary exercise (before being placed in the cage fitted with the wheel).
2.6.2 Animal anaesthesia and sacrifice
Mice were humanely anesthetised with a gaseous mixture of 1.5% Rodia Halothane
(Merial, Paramatta NSW, Australia) N2O and O2, and killed by cervical dislocation.
2.6.3 Tissue sampling and processing
For paraffin processing, the right leg of each mouse was fixed by immersion in 4%
(w/v) paraformaldehyde (Sigma-Aldrich) (pH 7.6) diluted in PBS, for a minimum of 24
h. Quadriceps muscles were dissected (see Section 6.1) from the fixed legs, transferred
to 70% ethanol and processed in a Shandon automatic tissue processor overnight. The
muscles were bisected in the mid-region and embedded with both cut surfaces at the top
of the paraffin block for transverse sectioning.
A B

Chapter Two Materials and Methods
40
Paraffin blocks were transversely cut into 5 µm thick sections using a Leica retractable
microtome. The sections were stretched on a water bath containing 0.1% HS (1 ml HS
diluted in 1000ml H2O) at approximately 42ºC and collected on silane (3-aminopropyl-
triethoxysilane)(Sigma-Aldrich) coated glass slides (Menzel-Glaser). Slides were air
dried for approximately 30 min and placed in the oven at 37 ºC overnight to ensure
proper attachment of the section to the glass slide.
2.6.4 Haematoxylin and eosin staining
Paraffin sections were dewaxed in three changes of xylene (MERCK, Biollab, Vic.,
Australia) (2 min each) and re-hydrated by passing through graded alcohol and ddH2O:
2 changes of 100% ethanol (2 min each); 1 change of 70% ethanol (2 min); and 1
change ddH2O (1 min). Re-hydrated slides were placed in Haematoxylin (BDH
Laboratory Supplies, Biollab, Vic., Australia) (30 sec) and washed in tap water.
Haematoxylin stained slides were placed in 70% ethanol (2 min), stained in Eosin
(MERCK) (20 sec), washed, and then dehydrated in 3 changes of 100% ethanol (2 min
each) and passed through 2 changes xylene (3 min each). Slides were mounted with
PVA mountant for microscopy (BDH Laboratory Supplies) and air dried.
2.6.5 Image analysis: quantification of necrosis
Non-overlapping, bright field images of transverse mdx muscle sections were captured
with a LEICA DMBRE microscope (at 10x magnification), Nikon Digital Camera
DXM1200F and personal computer using the Image-Pro Plus v.4.5.1.29 software to
view the entire muscle cross section. Areas of muscle necrosis were identified using the
Image-Pro Plus v.4.5.1.29 software by the presence of dark blue stained inflammatory
cells (basophilic staining) and/or the fragmented sarcoplasm of necrotic myofibres (Fig
2.5). The area of necrosis was recorded as a percentage of the whole section (Radley
and Grounds 2006).

Chapter Two Materials and Methods
41
Figure 2.5: Typical histology of dystrophic mdx quadriceps muscle. (A) Unexercised mdx muscle, characterised by regenerated myofibres of different sizes with central nuclei (arrows) with a low level of necrosis (circled). (B) Exercised mdx muscle characterised by increased areas of myofibre necrosis (indicated within area outlined by broken line) identified by the infiltration of inflammatory cells (arrow) and fragmented sarcoplasm (asterisk). Scale bar, 100µm
2.6.6 Statistical analyses
All data are expressed as means + Standard Error. A two-way analysis of variance
(ANOVA) was used to assess differences between TAT-TIJIP treated and untreated
control groups for the mdx mice exercise experiment.
*
*
A B

Chapter Three Validation of cell culture models of IGF-1 induced skeletal muscle hypertrophy
42
Chapter Three
Validation of cell culture models of IGF-1 induced skeletal
muscle hypertrophy
Introduction
The purpose of this study is to validate the morphological effects of exogenous IGF-1
on skeletal muscle myotubes in tissue culture. Initial experiments focused on
establishing a skeletal muscle cell culture model that would respond to stimulation with
IGF-1. This same model was then used in TNF induced atrophy and combined with
further IGF-1 studies (see Chapter 4). The experimental design was based on published
methods reporting that addition of an analogue of IGF-1, LONGTMR3IGF-I, in tissue
culture to differentiated cells of the immortalised mouse C2C12 skeletal muscle cell line
(Yaffe and Saxel 1977) induced myotube hypertrophy (Florini et al. 1996; Rommel et
al. 1999; Rommel et al. 2001; Sultan et al. 2006). Validation of these findings is
necessary to confirm that the C2C12 cells are a suitable model to investigate the
morphological and protein changes that result from IGF-1, TNF and combined IGF-
1/TNF treatments.
Optimisation of fusion conditions was conducted on the C2C12 skeletal muscle cells
(see Section 3.1). The effect of various doses of IGF-1 treatment was tested on two
muscle cells lines; the C2C12 adult mouse, and L6 neonatal rat cell line (Yaffe 1968).
While the IGF-1 receptor is present in both cell lines, the expression of IGF-1 varies
between them; C2C12 cells express IGF-1 (Tollefsen et al. 1989), whereas L6 cells
have little or no IGF-1 expression (Engert et al. 1996). In addition those two cell lines
show altered expression of a range of myogenic factors; L6 cells have restricted
expression of myogenic factors, whereas C2C12 cell have a more normal profile of gene
expression (Engert et al. 1996).

Chapter Three Validation of cell culture models of IGF-1 induced skeletal muscle hypertrophy
43
Results
3.1 Establishing optimum culture and treatment conditions
3.1.1 Comparing C2C12 myotube formation on different substrates
Initial experiments were designed to optimise culture conditions for cell attachment,
proliferation and differentiation of mouse C2C12 muscle cells when plated in 35 mm2
plastic dishes (Falcon) and thereafter on glass cover slips. Dishes were pre-coated with a
0.01% collagen (type I) solution (Invitrogen) (diluted in PBS) or with 0.1 mg/ml Poly-
D-Lysine (PDL) (Chemicon). Myoblasts were plated at a concentration of 0.5 x 105
cells per dish in a proliferation (high serum) medium, consisting of Dulbecco’s
Modified Eagle Medium (DMEM; see Section 2.1) supplemented with 20% (v/v) foetal
calf serum (FCS). For this initial experiment, fusion was induced by changing the
medium to low serum medium (DMEM supplemented with 2% horse serum (HS) at 48
h after plating. The cells used in these preliminary experiments had been through a
minimum of 25 passages, however, as previously noted, the exact passage number of
these cells was not known.
After 3 days of culture in low serum medium, the fusion of myoblasts into myotubes
was only present when the cells were cultured in dishes that had been pre-coated with
0.01% collagen (type I) (Figure 3.1: A), but not with PDL (Figure 3.1: B) or uncoated
(plastic) dishes (Figure 3.1: C). Cells plated in the PDL and uncoated dishes did not fuse
and few cells remained attached after 3 days of culture in the low serum medium.
Compared to the numbers of cells that were plated, only half the number of cells were
attached in the PDL dishes, with less than half attached in the uncoated dishes (Figure
3:1: B and C).

Chapter Three Validation of cell culture models of IGF-1 induced skeletal muscle hypertrophy
44
Figure 3.1: Myotube formation on different surface coatings. Phase contrast images of C2C12 cells photographed at 3 days after medium was changed from proliferation (high serum) to fusion (low serum) medium. Myoblasts had aligned and fused into myotubes in the petri dish pre coated with 0.01% collagen (type I) (A), whereas cells remained unfused in the Poly-D-Lysine coated dish (B). Most cells plated in the uncoated petri dish (C) had lifted off. Magnification: 10x. Bar: 100 µm.
3.1.2 Determining the optimum fusion medium and seeding density for C2C12
myotube formation
To determine the optimum medium for inducing the fusion of C2C12 myoblasts into
myotubes, cells were plated in DMEM supplemented with, or without HS, to a final
concentration of 2%. Under these fusion conditions it was also necessary to determine
the seeding density at which overlap of C2C12 myotubes was minimised, so that
measuring individual myotubes would be possible for later morphological analysis.
Myoblasts were plated at 2 cell densities (0.5 x 105 or 1 x 105 cell per well) and cultured
in proliferation medium (DMEM + 20% FCS) for 48 h, following this the medium was
changed to fusion medium (DMEM without or with 2% HS).
At the lower cell density, the addition of horse serum to the fusion medium resulted in
the formation of slightly more myotubes (Figure 3.2: A) compared to cultures without
horse serum (Figure 3.2: C). When myotube formation was induced with the addition of
horse serum, alignment and fusion of the myoblasts into myotubes was more uniformly
spread within the culture (Figure 3.2: A and B). Cells cultured in the DMEM only
medium formed shorter and less evenly distributed myotubes compared to cells cultured
in the presence of horse serum (Figure 3.2: C and D). Furthermore, after 3 days of
culture in the DMEM only medium, the myotubes were more susceptible to lifting off
the dish with few myotubes remaining, compared to the horse serum supplemented
cultures.

Chapter Three Validation of cell culture models of IGF-1 induced skeletal muscle hypertrophy
45
The differences in the formation of myotubes in medium supplemented with or without
horse serum were subtle (Figure 3.2). However, when comparing the seeding densities
at which the cells were plated, the benefits on formation and continuity of myotubes
within dishes that were fused in the presence of horse serum was evident (Figure 3.2: B
and D). The horse serum supplemented cultures produced longer myotubes, which is
more desirable for subsequent morphological analyses. In this medium (DMEM + 2%
HS - hereafter referred to as fusion medium), the seeding density of 1 x 105 cells/well
was optimal for the formation of non-overlapping myotubes, which were able to be
cultured for up to 5 days without lifting off the dishes.
Figure 3.2: Fusion of C2C12 myoblasts into myotubes in two media (DMEM +/- HS) at two different initial plating densities in 35mm collagen (type I) coated dishes. Phase contrast images show C2C12 myotubes at day 3 of culture in Dulbecco’s Modified Eagle medium (DMEM) medium supplemented with horse serum (HS) (A and B) and without (C and D). More myoblasts fused into myotubes in horse serum supplemented medium, when plated at initial cell densities of 0.5 x 105 (A) and 1 x 105 cell/well plated (B) compared to horse serum free cultures (C and D). At an initial cell plating density of 1 x 105 cell/well, myotubes in the presence of horse serum (B) were longer and more uniformly spread than those in horse serum free medium (D). Magnification: 10x. Bar: 100 µm.

Chapter Three Validation of cell culture models of IGF-1 induced skeletal muscle hypertrophy
46
3.2. Preliminary studies to determine the biological activity and optimum
dosage of IGF-1 required for inducing hypertrophy in C2C12 and L6 myotube
cultures (passage > 25)
After optimising the seeding density and fusion media conditions, it was necessary to
determine if the C2C12 cultures were responsive to treatment with IGF-1 and, if so,
what was the optimum dosage for this to occur. This was evaluated by comparing the
phenotypic changes in myotube size in untreated and IGF-1 treated cultures. The
analysis was initially performed on C2C12 and then on L6 myotubes. Both these cell
lines had been through a minimum of 25 passages and were defined as ‘old’ cultures.
Two analogues of IGF-1 were tested; LONGTMR3IGF-I and Des(1-3)IGF-1. All studies
were conducted in triplicate.
3.2.1 Effects of IGF-1 (LONGTMR3IGF-I) treatment on day 3 mouse C2C12
muscle myotubes (passage > 25)
To compare results from this study and validate previous data by Florini et al (1996) it
was necessary to administer the same analogue and treatment dosage of IGF-1 to
differentiated C2C12 myotubes. Florini et al (1996) treated cells with an analogue of
IGF-1 known as ‘LONGTMR3IGF-I’ that has a lower affinity for IGF Binding Proteins
(IGFBPs) compared to IGF-1 (Francis et al. 1992). This is due to the addition of a 13
amino peptide at the N-terminus and the substitution of glutamic acid (E) at position 3
with arginine (R). For the remainder of the tissue culture studies this analogue is
referred to as ‘IGF-1’.
The C2C12 myoblasts used in this part of the study routinely fused to become myotubes
after 3 days of culture in low serum media (DMEM + 2% HS) when plated at an initial
seeding density of 1 x 105 cells/well (see above). This was termed day 3 of
differentiation. Myotubes were treated on day 3 for a further 3 days with IGF-1 at a
dose of 10 ng/ml, the standard dosage according to previously published hypertrophy
studies (Florini et al. 1996; Rommel et al. 1999; Rommel et al. 2001). Treatment of the
myotubes with IGF-1 at dosages of 20 ng/ml and 40 ng/ml were also included in the
study to determine if hypertrophy could be induced at a higher dosage than that
routinely administered (Florini et al. 1996; Rommel et al. 1999; Rommel et al. 2001).
Medium and treatment were replaced daily to ensure that any decrease in stability of

Chapter Three Validation of cell culture models of IGF-1 induced skeletal muscle hypertrophy
47
IGF-1, when in the culture medium, did not interfere with the interpretation of the
results for the effects of IGF-1.
Typical phase contract microscopy images of day 6 treated and untreated myotubes
(Figure 3.3) showed no noticeable change in the size of the treated myotubes, when
treated with IGF-1 at a dose of 10 ng/ml, 20 ng/ml of 40 ng/ml, compared to untreated
controls. Where myotubes had been fused in DMEM with 2% horse serum (DMEM +
HS) and treated with IGF-1 at a dose 20 ng/ml (Figure 3.3: E), small formations were
apparent which resembled ‘myosacs’; this is where the cells are branched and contain
many myonuclei (Yotov and St-Arnaud 1996; Palmer et al. 2001). These formations,
however, were only observed in one of the three myotubes culture replicates treated
with 20 ng/ml IGF-1.
Even though the optimum fusion medium for inducing fusion and propagating the
growth of C2C12 myotubes was previously determined to be DMEM + HS (see above),
in this study the myotubes were also cultured and treated in horse serum free medium to
asses whether serum starvation of the myotubes might amplify the hypertrophic effects
of IGF-1. The treated myotubes cultured in the serum free medium (DMEM only) did
not show any changes in size compared to those treated and cultured in horse serum
(Figure 3.3).
3.2.2 Effects of Des(1-3)IGF-1 treatment on day 3 mouse C2C12 muscle
myotubes (passage > 25)
As hypertrophy of C2C12 myotubes was not observed after 3 days of treatment with
IGF-1 (LONGTMR3IGF-I), a second analogue of IGF-1 (Des(1-3)IGF-1) was tested.
Des(1-3)IGF-1, as discussed previously (Section 1.4.1.2), has a sequence identical to
human or bovine IGF-1 apart from the removal of the amino tripeptide (Gly-Pro-Glu)
(Ballard et al. 1987). Des(1-3)IGF-1 is similar to the LONGTMR3IGF-I analogue as it
has a high binding affinity for the IGF-1 receptor (Ballard et al. 1987) and low binding
affinity to IGFBPs (Ross et al. 1989).
Myotubes at day 3 of differentiation were treated with either 10 ng/ml or 20 ng/ml of
Des(1-3)IGF-1 for a further 3 days. All of the treated myotubes showed no change in
size or length compared to the untreated controls (Figure 3.4). Treatment with Des(1-

Chapter Three Validation of cell culture models of IGF-1 induced skeletal muscle hypertrophy
48
3)IGF-1 at a dose of 10 ng/ml was found to induce the branching of a small number of
myotubes, irrespective of the medium conditions (Figure 3.4: B and E, indicated by
arrows).
Figure 3.3: Effects of IGF-1 treatment on C2C12 myotubes. Phase contrast microscopy images of myotubes, differentiated in both horse serum (HS) and serum free medium, and treated for 3 days with IGF-1 at a dosage of 10 ng/ml (C and D), 20 ng/ml (E and F) or 40 ng/ml (G and H) show no observable hypertrophy compared to untreated myotubes (A and B). The formation of ‘myosacs’ was depicted in one of the cultures treated with IGF-1 at a dose of 20 ng/ml (E). Magnification: 10x. Scale bar: 100 µm.

Chapter Three Validation of cell culture models of IGF-1 induced skeletal muscle hypertrophy
49
Figure 3.4: Effects of Des(1-3) IGF-1 treatment on C2C12 myotubes Phase contrast microscopy images of myotubes, differentiated in DMEM supplemented with horse serum (HS) or in serum free medium, and treated for 3 days with Des(1-3) IGF-1 at a dosage of 10 ng/ml (B and E) or 20 ng/ml (C and G) show no change in myotubes size compared to untreated myotubes (A and D). Myotube branching (indicated by arrows) was displayed in cultures treated with 10 ng/ml IGF-1 (B and E). Magnification: 10x. Scale bar: 100 µm.
3.3 Effects of IGF-1 treatment on day 3 rat L6 myotubes (passage > 25)
As the C2C12 cells (passage > 25) did not respond to treatment with either analogue of
IGF-1 (Section 3.2.1 and 3.2.1) irrespective of the dosage, the experiments with IGF-1
were repeated using the rat L6 cell line. Considering that the aim of this study was to
validate the cell models of hypertrophy detailed in publications that used the IGF-1
analogue, LONGTMR3IGF-I (Florini et al. 1996; Rommel et al. 1999; Rommel et al.
2001) experiments testing Des(1-3)IGF-1 were not pursued.
In a striking contrast with the C2C12 myotubes, the L6 cells responded to treatment
with IGF-1 (LONGTMR3IGF-I); myotube size increased over the 3 days of treatment
(Figure 3.5: B, C, E and F). Treatment with 20 ng/ml IGF-1 induced myotube
hypertrophy to cells differentiated in both media (Figure 3.5 C and F), although this
hypertrophy was more pronounced in the horse serum free cultures (Figure 3.5: F).

Chapter Three Validation of cell culture models of IGF-1 induced skeletal muscle hypertrophy
50
IGF-1 treatment at the lower dose of 10 ng/ml induced the greatest size changes to the
myotubes, regardless of the medium conditions (Figure 3.5: B and E): Many of the
myotubes appeared to have fused into myotube sheets and displayed a flat and wide
appearance, compared to the long and thin untreated myotubes controls (Figure 3.5: A
and C) .
Figure 3.5: Effects of IGF-1 treatment on L6 myotubes. Phase contrast microscopy images of L6 myotubes treated for 3 days with IGF-1 at various dosages. Untreated controls show thin myotubes after 6 days in fusion media alone (A). The formation of extremely large myotubes was seen in the cultures treated with IGF-1 at a dose of 10 ng/ml (B and E), yet fewer hypertrophic myotubes and the appearance of unfused cells are seen in 20 ng/ml treated cultures (C and F). Magnification: 10x. Scale bar: 100 µm.
The hypertrophic myotubes resulting from treatment with IGF-1 at 10 ng/ml appeared
typical of those observed when IGF-1 was added to differentiating L6 cells (Coolican et
al. 1997). The myotubes were also similar to C2C12 myosacs previously described
(Yotov and St-Arnaud 1996; Palmer et al. 2001) in that they contained large areas of
dense nuclear clustering, as visualised by immunostaining with Hoechst nuclear stain
(Figure 3.6: indicated by arrows in B and D). In the DMEM only cultures, areas of
nuclear clustering were also shown (Figure 3.6: indicated by asterisks in C). Clustering
was not observed in the myotubes cultured in DMEM + 2% HS. The areas of nuclear
clustering present in the DMEM only cultures, however, considerably smaller than
those observed after the addition of IGF-1 (Figure 3.6: C compared to D).

Chapter Three Validation of cell culture models of IGF-1 induced skeletal muscle hypertrophy
51
Figure 3.6: Immunostained L6 myotubes treated with IGF-1. Myotubes were immunostained with anti-desmin antibody (green) and counter stained with Hoechst nuclear stain (blue). Untreated controls (A and C) remain as long thin myotubes whereas in IGF-1 treated cultures (B and D) myotubes are bigger and contain large areas of mass nuclear clustering (arrows). Magnification: 20x. Scale: 100 µm.
For the L6 cells a dose of 10 ng/ml IGF-1 appeared optimal for inducing myotube
hypertrophy over 3 days; this finding accords with literature on C2C12 myotubes
(Florini et al. 1996).

Chapter Three Validation of cell culture models of IGF-1 induced skeletal muscle hypertrophy
52
Discussion
Although the morphological effects of IGF-1 on skeletal muscle in C2C12 cell cultures
has been extensively researched (and to a lesser extent in L6 cells) it was necessary to
validate these findings and determine which of these cell lines was most suitable for the
proposed research, which was to develop a skeletal muscle cell culture model that could
be used to morphologically assess and quantify the effects of exogenous IGF-1
treatment and later TNF treatment (Chapter 4). The first aim of this study was to
optimise a skeletal muscle cell culture model of hypertrophy so that increases to
myotube size could be easily measured and compared with to control cultures.
The initial experiments concentrated on optimising the plating and culture conditions
that would assist myoblast attachment and myotube formation for the C2C12 cell line
and a mouse myoblast subclone of the C2 cell line (Yaffe and Saxel 1977). This cell
line is a pure myoblast population and a well established model for skeletal muscle
differentiation (Morgan et al. 1992; Lloyd et al. 2004). It was necessary that the pre-
plating solution assisted cell attachment, but did not contain enough growth factors to
stimulate cell proliferation and differentiation, as this could interfere with results where
exogenous IGF-1 (and later TNF) is administered to the cells. On this basis, two cell
surface coatings for the plastic petri dishes, collagen (type I) and the synthetic Poly-D-
Lysine, were evaluated.
The presence of the basement membrane protein collagen (type I) allowed the formation
of C2C12 myotubes. Collagen (type I) is a heterotrimer and is commonly used to
promote cell attachment in tissue culture. On plastic surfaces, collagen (type I) has been
reported to assist differentiation of C2C12 (Lawson and Purslow 2000) and avian
skeletal myotubes (Vandenburgh et al. 1991), in addition to promoting cell adhesion for
a number of other muscle cells (Gelman and Prives 1996; Wang et al. 1996).
PDL, a positively charged molecule, is also used to enhance cell attachment to plastic
and glass surfaces. PDL has been used to promote adherence of human stem cell
derived neurons (Hayman et al. 2005) and to assist in the culture of transfected mouse
3T3 fibroblasts (Nitsch et al. 1996). However, results from this, and other studies

Chapter Three Validation of cell culture models of IGF-1 induced skeletal muscle hypertrophy
53
(Lawson and Purslow 2000) suggest that collagen (type I), and not PDL, is a more
suitable surface coating for culturing differentiated C2C12 cells in plastic petri dishes.
The differentiation of C2C12 and L6 cells in tissue culture requires a switch in medium
from a high serum (containing 10%-20% FCS) to a low serum containing medium (2%
HS) once cells have reached 75-80% confluence. The differentiation medium for
culturing C2C12 and L6 myotubes to be treated with IGF-1 needed to supply cultures
with the minimum amount of nutrients, so that differentiation and myotube attachment
(for a period of up to 10 days) was viable. As the components present in the serum are
not well characterized, and the presence of growth factors that may interfere with later
IGF-1 treatment are not known, the myotubes were differentiated and treated in both
horse serum supplemented, or serum free, medium. This allowed IGF-1 induced
hypertrophy in the myotubes to be compared between the two media conditions and
thus the determination of the extent of serum derived growth factors contribution to
changes to myotubes size.
The differentiation of C2C12 and L6 cells was induced in both horse serum and serum
free medium. The C2C12 cells routinely formed longer myotubes in horse serum
supplemented medium (Figures 3.2, 3.3 and 3.4), whereas in the L6 cell line the
myotube lengths were unaffected by the medium conditions (Figures 3.5 and 3.6). The
C2C12 myotubes routinely appeared larger than L6 myotubes, an observation also
reported in previous research (Lawson and Purslow 2000).
Lawson and Purslow colleagues (2000) published data that demonstrated that L6 cells
were unable to form myotubes when cultured in serum free medium; the fusion of L6
myotubes in horse serum free DMEM, however was observed in the present study
(Figures 3.5 and 3.6). The results from this and Lawson and Purslow (2000) however
both confirm that the optimal medium for inducing fusion, and sustaining myotube
attachment for L6 and C2C12 cells, is DMEM supplemented with 2% horse serum.
When cultured in the presence of horse serum, and on collagen (type I) coated dishes,
L6 and C2C12 cells have been reported to show very little behavioural variation based
on similar levels of creatine phosphokinase (CPK) (a measure of myoblast fusion)
activity (Lawson and Purslow 2000).

Chapter Three Validation of cell culture models of IGF-1 induced skeletal muscle hypertrophy
54
The C2C12 and L6 cell lines are routinely used for studying the growth and
differentiation of muscle because of their ability to differentiate and form myotubes
relatively quickly (within 2-3 days of culture) in low serum media. IGF-1 has widely
been reported to stimulate myotube hypertrophy in day 2-3 differentiated C2C12
myotubes at a dose of 10 ng/ml for 24 h or 48 h (Rommel et al. 1999; Rommel et al.
2001); at a dose of 100 ng/ml for 48 h (Latres et al. 2005); and at 50 nM for 72 h
(Dehoux et al. 2007). Similarly, studies using the L6E9 (a subclone of the L6 cell line)
show IGF-1 induced hypertrophy in myotubes via the transfection of a muscle specific
IGF-1 vector that is only activated during cell differentiation (Musaro and Rosenthal
1999; Musaro et al. 1999; Fanzani et al. 2006). Furthermore, the same signalling
pathways that mediate myotube hypertrophy in C2C12 cells were upregulated when
IGF-1 was administered to L6 myotubes (Li et al. 2005).
The effect of cell passage number for C2C12 cells became an area of interest in this
study when neither IGF-1 nor Des(1-3)IGF-1 induced myotube hypertrophy in C2C12
cells, whereas in the L6 cell line, treatment with IGF-1 increased myotube sizes. Hughes
et al (2007) recently discussed the critical issue of misleading results that are associated
when using high passage cultures. This appears to be the first review that highlights the
importance of passage number for studies utilising cell lines. In addition, reports
investigating the effect of both IGF-1 and TNF treatment on C2C12 myotubes
(Fernandez-Celemin et al. 2002; Dehoux et al. 2007) state in the methods that the cells
were passaged (aka split or sub-cultivated) up to a maximum of 7 times in order to
preserve cell characteristics. A review of the culturing protocols for the maintenance of
C2C12 cultures outlined by the Coriell Cell Repositories (USA; http://www.atcc.org)
raised concerns regarding the history of the C2C12 cultures used in this study. The
protocol outlined by this company makes special mention of the importance to avoid
cells becoming confluent, as this decreases the myoblastic population of the cultures.
From prior laboratory cell culture records, over many years the number of times the
C2C12 cells had been passaged and frozen down was not clearly detailed.
Due to the C2C12 cells not responding to treatment with IGF-1, whereas numerous
studies had reported IGF-1 induced hypertrophy in this cell line (Florini et al. 1996;
Rommel et al. 1999; Rommel et al. 2001; Latres et al. 2005; Dehoux et al. 2007), it was
concluded that the C2C12 cells in our laboratory may have been compromised due to

Chapter Three Validation of cell culture models of IGF-1 induced skeletal muscle hypertrophy
55
their high passage number. Therefore, a new stock of this specific cell line was
purchased from ATCC. Experiments with the L6 cells were not continued, for multiple
reasons, important among them was the observation that the administration of IGF-1 in
this cell line induced the formation of myosacs, rather than the preferred increase in
sizes of individual myotubes. Furthermore, the primary aim of this study was to validate
and replicate IGF-1 hypertrophy results that had been published using mouse C2C12
myotubes. The later point also strongly contributed to the decision to cease experiments
in the L6 line, with subsequent experiments instead concentrating on examining the
C2C12 line.
.

Chapter Four Morphological effects of IGF-1 and TNF treatment on cultured myotubes
56
Chapter Four
Morphological effects of IGF-1 and TNF treatment on
cultured myotubes
Introduction
New C2C12 cells, freshly obtained from ATCC, were used to further test the effects of
IGF-1 on myotube hypertrophy. These tests were conducted because of the lack of
response to IGF-1 of the late passage (>25 passages) C2C12 cells (Chapter 3). These
low (3-6) passage C2C12 cells were cultured for 7 days in fusion medium before the
treatment period, in contrast to only 3 days for the preliminary experiments in Chapter
3. This slight change in protocol was to reduce the complication of unfused myoblasts
in the cultures (more pronounced after only 3 days in fusion medium) and to ensure
more complete differentiation of the myotubes; this modification follows the report of
Tolosa et al. (2005).
After 7 days of culture in the optimised fusion medium, DMEM supplemented with 2%
horse serum (Section 3.1.2), IGF-1 was administered at a dose of 10 ng/ml for 3 days.
The myotubes were then analysed at day 10. This dose has been previously reported to
induce myotube hypertrophy (characterised by an increase in myotube diameter) within
2 days when added to day 2 differentiated C2C12 cells (Rommel et al. 2001; Latres et
al. 2005) and within 1 day when administered to day 3 C2C12 myotubes (Rommel et al.
1999).
After confirming that the C2C12 muscle cells served as a suitable model to detect and
quantify changes in myotubes size, the role of the pro-inflammatory cytokine tumour
necrosis factor (TNF) on inducing myotube atrophy (muscle wasting) was investigated.
TNF was administered at a dose of 20 ng/ml for 3 days, to day 7 myotubes, to determine
the morphological effect on myotube size.

Chapter Four Morphological effects of IGF-1 and TNF treatment on cultured myotubes
57
Finally, the combined effects of IGF-1 and TNF were tested in C2C12 myotubes to
determine if IGF-1: (i) induced hypertrophy; (ii) could prevent or reverse TNF induced
atrophy, (ii) or conversely, if TNF could prevent IGF-1 induced hypertrophy in this in
vitro skeletal muscle system. These hypotheses were further tested using primary
cultures of skeletal muscle cells isolated from transgenic mice which over-express Class
2 IGF-1 Ea (IGF:C2) in skeletal muscles (Shavlakadze et al. 2008 - unpublished data).
Primary cultures were included as a skeletal muscle cell model that more closely
resembles muscle in vivo, compared to cell lines, and provided a useful additional in
vitro model to study the morphological effects of combined IGF-1/TNF treatment.

Chapter Four Morphological effects of IGF-1 and TNF treatment on cultured myotubes
58
Results
4.1 Effects of IGF-1 treatment on day 7 mouse C2C12 myotubes
The new, low passage C2C12 cells clearly responded to treatment with IGF-1. IGF-1
administered to 7 day myotubes, at a dose of 10 ng/ml for 3 days, induced hypertrophy
in the new C2C12 myotube cultures. Immunofluorescence using desmin antibodies
showed wider myotubes in the IGF-1 treated cultures compared to the untreated control
cultures (Figure 4.2: B and A respectively). A detailed analysis of myofibre widths (see
Chapter 2, Section 2.4.3) confirmed that treatment with IGF-1 induced a significant
increase (P < 0.001) in myotube size (increase of approximately 25%) when compared
to untreated controls (see below; Figure 4.3).
4.2 The effect of TNF treatment on day 7 mouse C2C12 myotubes
4.2.1 Independent C2C12 myoblast fusion assay to test the biological activity of
TNF
Before testing TNF on the myotubes, an independent assay was carried out to confirm
the biological activity of TNF, based on observations that TNF inhibits myoblast
differentiation (Szalay et al. 1997). C2C12 myoblasts (passage < 5) were cultured in
growth medium for 24 h and then changed to a fusion (low serum) medium to induce
differentiation and fusion. When changing the medium, 20 ng/ml of TNF was added for
4 days and myotube formation was compared to the untreated control cultures. After 4
days it was evident that myotubes had formed in the untreated control cultures (Figure
4.1: A), whereas the addition of TNF to the myoblasts was found to inhibit myotube
formation (Figure 4.1: B).

Chapter Four Morphological effects of IGF-1 and TNF treatment on cultured myotubes
59
Figure 4.1: Fusion assay to test biological activity of TNF. Phase contrast images of myoblasts that were cultured in low serum media (A) or in the presence of TNF (20 ng/ml) (B) for 4 days. Myotubes formed in the untreated cultures (A) but not in the presence of TNF (B). Magnification: 10x. Bar: 100 µm
4.2.2 Effects of TNF treatment on day 7 mouse C2C12 myotubes
Upon verification that the TNF was biologically active, the treatment routine previously
applied in the IGF-1 hypertrophy experiments was repeated for the TNF atrophy studies
(see above Section 4.2.1). TNF, at a dose of 20 ng/ml, was administered to day 7 C2C12
myotubes for 3 days; the medium and treatment was changed daily. After 3 days of
treatment the morphological changes to the myotubes was assessed visually using
myotubes immunostained for desmin; size was quantified morphologically by the
analysis of myotube widths and the results recorded as mean myotube widths with the
standard error (SE). The significance of the difference between the untreated and treated
samples was quantified using a series of t-tests.
Immunofluorescent microscopy images (Figure 4.2) show that TNF treatment not only
reduced myotube width, but also myotube numbers. Myotubes cultures treated with
IGF-1 (Figure 4.2: B) for 3 days appear wider compared to the untreated cultures
(Figure 4.2: A). TNF treated myotubes (Figure 4.2: C) appeared thinner compared to the
untreated controls (Figure 4.2: A). There were also fewer myotubes in the TNF treated
cultures, compared to the untreated controls (Figure 4.2: C and A respectively); this
suggests that the TNF may have been toxic and killed some myotubes.

Chapter Four Morphological effects of IGF-1 and TNF treatment on cultured myotubes
60
Figure 4.2: Immunofluorescent microscopy images of day 10 C2C12 myotubes treated with IGF-1 or TNF for 3 days. Representative photomicrographs of myotubes stained with anti-desmin antibodies (in green). Myotubes treated with IGF-1 (10 ng/ml) (B) appeared wider compared to untreated controls (A). In contrast, myotubes treated with TNF (20 ng/ml) (C) show decreased width. Magnification: 10x. Bar: 100 µm.
Quantitative analysis (Figure 4.3) confirmed the various differences in myotube widths
resulting from treatment with either IGF-1 (10 ng/ml) or TNF (20 ng/ml) for 3 days
(Figure 4.3). Myotube widths were quantitated from measurements collected from 50
randomly selected myotubes per culture dish, resulting in totals of 1200, 300 and 900
myotubes being measured for the untreated controls, IGF-1, and TNF treatments
respectively. Myotube widths were taken approximately 50 µm apart throughout the
entire length of the myotube (see Methods Section 2.4.3). IGF-1 treatment induced a
significant increase (P < 0.0001) in the mean myotube width, whereas TNF treated
myotubes had significantly smaller (P < 0.0001) mean widths (decrease of
approximately 25%) compared to the untreated controls (Figure 4.3).

Chapter Four Morphological effects of IGF-1 and TNF treatment on cultured myotubes
61
Figure 4.3: Quantitative analysis of mean myotube widths of untreated (control), IGF-1 and TNF treated C2C12 cultures. C2C12 myotubes treated for 3 days with IGF-1 (10 ng/ml) show a significant increase in myotube width whereas treatment with TNF (20 ng/ml) induced a significant decrease (to mean myotube width when compared to Untreated (control) myotubes. Results are mean myotube widths + SE of independent experiments indicated for each treatment (n = 50 myotube diameters/experiment). ***P < 0.0001 vs untreated controls.
4.3 Effects of combined treatment with IGF-1 and TNF on day 7 mouse C2C12
muscle myotubes
C2C12 myotubes differentiated for 7 days in the low serum medium received various
combined treatments with IGF-1 and TNF for 3 days. To determine if IGF-1 could
prevent or reverse the atrophic effects of TNF, or if TNF could prevent IGF-1 induced
hypertrophy, the combined treatments were divided into three test groups: 1)
Simultaneous IGF-1/TNF treatment, where both IGF-1 and TNF were administered to
the myotubes at the same time; 2) IGF-1 added before TNF, where myotubes were pre-
treated with IGF-1 for 1 h before TNF treatment; and 3) TNF added before IGF-1 where
TNF was administered 24 h before IGF-1 treatment.

Chapter Four Morphological effects of IGF-1 and TNF treatment on cultured myotubes
62
Figure 4.4: Quantitative analysis of myotube widths of untreated (control), IGF-1, TNF and combined IGF-1 and TNF treated C2C12 cultures. Combined treatments resulted in no significant change to mean myotube width when compared to untreated controls. Results are mean myotube widths + SE of independent experiments indicated for each treatment (n = 50 myotube diameters/experiment).***P < 0.0001 vs untreated controls. •P < 0.05 vs TNF.
The combination treatments were found to have no significant effect on mean myotube
width when compared to the untreated control cultures (Figure 4.4). All of the combined
treated groups were significantly smaller when compared to the IGF-1 only treated
myotubes, and were larger when compared to the TNF only treated myotubes (Figure
4.4). Although myotubes treated with IGF-1 for 1 h before the administration of TNF
visually appeared to have a greater width compared with the other treatment
combinations, and with the TNF treated myotubes, the difference between them was not
statistically significant.
4.4 Effects of TNF on control FVB and primary cultures of transgenic IGF:C2
mouse myotubes
4.4.1 Effect of TNF on day 4 FVB primary mouse myotubes
The morphological effect of TNF was further tested in primary myotube cultures
derived from 4-6 week old FVB mice. FVB mice were used as the control strain, instead
of IGF:C2 transgenic negative littermates, because FVB mice are the background strain
for the transgenic IGF:C2. The isolation of muscle cells from the FVB mice minimised
the possibility of the inclusion of transgene positive cells, an error that may have

Chapter Four Morphological effects of IGF-1 and TNF treatment on cultured myotubes
63
occurred if transgenic negative littermates were used as controls. In addition, the
treatment was administered to all primary muscle cell cultures on day 4 of fusion,
compared to day 7 for the C2C12 experiments. This change in treatment time reflected
the accelerated rate at which the primary muscle cells fused into myotubes; at day 4 of
differentiation, myotubes in the primary muscle cell cultures resemble those seen in
C2C12 cultures after 7 days of differentiation. After 3 days of treatment (day 7 after
fusion medium) the myotubes were fixed and stained with desmin antibody and
myotube widths quantified as for the C2C12 experiments.
TNF treated FVB myotubes had significantly smaller (P < 0.05) mean widths
(approximately 20% decrease) when compared to untreated control cultures (Figure
4.5). This TNF induced atrophy was similar to that observed in C2C12 myotubes
(Figure 4.3).
Figure 4.5: Quantitative analysis of myotube widths from TNF atrophy experiments conducted on Wild type FVB and Transgenic IGF:C2 primary skeletal muscle cell cultures. In the control FVB wild-type myotube cultures, TNF treatment alone significantly decreased mean myotube width when compared to untreated FVB wild-type myotubes. The IGF:C2 myotubes cultures were used to test the combined treatment of TNF with IGF-1. In these IGF:C2 myotubes, the addition of TNF had no effect on mean myotube width when compared to untreated IGF:C2 myotubes. Results are mean myotubes width + SE of independent experiments indicated for each treatment (n = 50 myotube diameters/experiment). *P < 0.05 vs untreated FVB wild-type controls.
4.4.2 Testing the effect of TNF on transgenic IGF-1 class 2 primary muscle cells
The combined treatment experiment conducted on the day 7 C2C12 myotubes was
repeated using the primary skeletal muscle cells isolated from transgenic mice that over-
express Class 2 IGF-1 Ea within myotubes and myofibres. The availability of the

Chapter Four Morphological effects of IGF-1 and TNF treatment on cultured myotubes
64
IGF:C2 transgenic mice provided an opportunity to generate a muscle cell culture model
that did not require the addition of exogenous IGF-1. In this way, the preventative effect
of IGF-1 to TNF induced atrophy could be examined in a primary muscle cell culture.
The addition of TNF (20 ng/ml) to the transgenic IGF-1:C2 day 4 myotubes for 3 days
resulted in no significant change to the mean myotube size when compared to untreated
IGF-1:C2 myotubes. This trend was also observed in the C2C12 myotubes (Section
4.3). Although the myotube widths for the untreated FVB wild-type unexpectedly
appeared visually larger than for the untreated IGF:C2 transgenic myotubes, the
difference between them was not statistically significant.

Chapter Four Morphological effects of IGF-1 and TNF treatment on cultured myotubes
65
Discussion
The aim of this study was to validate if treatment with IGF-1 to well differentiated day 7
C2C12 myotubes could induce a significant increase in myotube width indicative of
hypertrophy, and if treatment with TNF could induce an atrophic response, specifically
a statistical significant decrease in myotube widths. To quantify the change in mean
myotube widths resulting from the various treatments, it was necessary to develop a
suitable model in which individual myotube widths could be measured, while
concurrently ensuring that the effects on myotube widths were the result of the
treatments acting on the well developed myotubes, and not the result of the activity of
differentiating cells.
With the optimisation of surface coating, cell plating density and fusion medium for
C2C12 myotubes previously determined (Chapter 3), it was necessary to test that the
new C2C12 cells (passage < 5) would serve as a suitable cell culture model. The
importance of maintaining C2C12 cells at low passages (passage < 7) to help preserve
the characteristics of the cell line has been recently emphasised (Fernandez-Celemin et
al. 2002; Dehoux et al. 2007; Hughes et al. 2007). Initial IGF-1 experiments outlined in
Chapter 3 were repeated in the new C2C12 cells. C2C12 cells were cultured in low
serum medium for 7 days before the experimental period. This formed the ‘model
system’ for all experiments conducted on differentiated myotubes in this study. After 7
days of culture in low serum medium, myotubes covered most of the culture and very
few myoblasts remained. This observation was also reported by Tolosa et al (Tolosa et
al. 2005) who investigated the myogenic profile of day 7 C2C12 myotubes, and
confirmed that C2C12 myotubes are more fully differentiated at day 7 (Tolosa et al.
2005). Another study that examined the expression of the structural proteins sarcomeric
actin and myosin at various stages of C2C12 differentiation, revealed that
approximately 5 days after differentiation was induced, and until 10 days when the
study was concluded, C2C12 myotubes express morphological characteristics of adult
skeletal muscle fibres (Burattini et al. 2004).

Chapter Four Morphological effects of IGF-1 and TNF treatment on cultured myotubes
66
IGF induced myotube hypertrophy
Treatment with 10 ng/ml IGF-1 induced hypertrophy in the day 7 C2C12 myotubes.
This finding confirms the hypertrophic actions of IGF-1 previously published (Rommel
et al. 1999; Rommel et al. 2001; Latres et al. 2005), however in those studies, IGF-1
was administered to cells during differentiation. The present study, however, was
concerned with the effect of IGF-1 on more fully differentiated myotubes, therefore
C2C12 cells were treated on day 7, at which point they are fully differentiated. To
determine the effect of IGF-1 on increasing myotube size (hypertrophy), compared to
increasing the number of myoblasts present (hyperplasia), the time at which IGF-1 is
administered to differentiating cells is critical. Under conditions where fusion is still
occurring at a high rate, C2C12 myoblasts divide within the first 48 h and are not fully
differentiated until day 5-7 (Burattini et al. 2004; Tolosa et al. 2005). Where IGF-1 was
added to C2C12 cells 48 h to 72 h after fusion had been induced (Rommel et al. 1999;
Rommel et al. 2001; Latres et al. 2005), the resulting change in myotube sizes observed
in these cultures after 1-2 days of treatment may have been in part due to fusion of
mononucleated cells into myotubes, in addition to an increase in protein synthesis
within the myotubes. For this reason, the present study purposely cultured C2C12
myotubes to day 7 of differentiation, before IGF-1 was administered (for 3 days), to
specifically determine if IGF-1 was inducing myotube hypertrophy (change to fused
myotube sizes), and not acting on proliferating myoblasts.
TNF induced myotube atrophy
The next series of experiments focused on the effects of the pro-inflammatory cytokine
TNF on myotube morphology, specifically any changes to myotube widths. As for IGF-
1, an independent assay was required to determine that the TNF used in the experiments
was biologically active. Results from the present TNF assay confirmed that the TNF
administered to the cells was biologically active, since C2C12 myoblasts transferred to
low serum medium in the presence of 20 ng/ml TNF did not fuse to form myotubes.
These findings support previous reports that the addition of TNF to differentiating
C2C12 myoblasts inhibits myotube formation in mouse cells (Szalay et al. 1997;
Meadows et al. 2000; Foulstone et al. 2001; Coletti et al. 2002) and also in human
primary muscle cell cultures (Miller et al. 1988; Foulstone et al. 2004).

Chapter Four Morphological effects of IGF-1 and TNF treatment on cultured myotubes
67
It has been proposed that the inhibitory effect of TNF on myotube formation is the
result of TNF acting through NF-kB activation (Guttridge et al. 2000; Li and Reid 2000)
or by TNF inhibiting the expression of myogenic transcription factors (MyoD and
myogenin) to block the synthesis of messenger RNAs of myogenic differentiation
proteins; specifically skeletal alpha-actin, myosin heavy and light chains (Szalay et al.
1997). In addition, C2C12 myoblasts transferred to low serum in 20 ng/ml TNF undergo
continual cell division compared to cells cultured in low serum alone, which prevents
the G0 cell cycle arrest required for differentiation to occur (Meadows et al. 2000).
It has been shown that TNF appears to have a critical role in skeletal muscle atrophy
and is the key cytokine mediating cachexia (muscle wasting) (Argiles et al. 1997; Glass
2005; Arthur et al. 2008). There have been few studies, however, detailing the
morphological effect of exogenous TNF treatment on cultured C2C12 myotubes, with
no studies examining the induction of myotube atrophy by TNF treatment alone.
Previous the this present study, researchers have developed an in vitro model of skeletal
muscle atrophy using the synthetic, cachectic glucocorticoid Dexamethasome (DEX);
the addition of 10-100 µM DEX for 24 h to C2C12 myotubes 2-4 days post fusion has
been reported to induce a significant decrease to myotube diameters and total protein
content (Stitt et al. 2004; Latres et al. 2005; Sacheck et al. 2004). In muscle, it is known
that DEX activates the Forkhead Box O (FoxO) class of transcription factors, resulting
in increased expression of the muscle atrophy related genes Atrogin-1 (also known as
Muscle Atrophy F-box; MAFbx) and muscle RING finger 1 (MuRF1) (Sandri et al.
2004; Stitt et al. 2004). More recently, a model of C2C12 myotube atrophy has been
reported to be developed though the combined administration of TNF with another pro-
inflammatory cytokine, interferon-γ (IFN- γ) (Dehoux et al. 2007). The present study
was the first to demonstrate that treatment with TNF (20 ng/ml) alone induces
significant changes to myotube widths in both immortalised C2C12 cells (Figure 4.3)
and primary muscle cultures (Figure 4.5).
Li et al (2005) reported that the addition of 6 ng/ml TNF to differentiated C2C12
myotubes induced activation of the Atrogin-1; this has also been shown to occur when
administered at a dose of 5 ng/ml in combination with the inflammatory cytokine,
interferon-γ (IFN- γ) (Dehoux et al. 2007). Combined treatment with TNF/ IFN-γ has

Chapter Four Morphological effects of IGF-1 and TNF treatment on cultured myotubes
68
also been reported to reduce MyoD and myosin heavy chain (MHC) protein expression
(Guttridge et al. 2000), although TNF alone had no effect on MyoD or MHC, the
authors concluded that effects of TNF on skeletal muscle cellular function could only be
demonstrated when administered in combination with another inflammatory cytokine
(Guttridge et al. 2000). A recent report by Dehoux et al (2007) showed that combined
exogenous treatment with 5 ng/ml TNF/IFN- γ was sufficient to induce myotube
atrophy in differentiated C2C12 myotubes, however the authors did not present data on
the morphological effects of TNF treatment alone. TNF induced atrophy of mature
myotubes in the present study is thus a novel observation and provides a very powerful
new in vitro model.
In the present study, the morphological effects of TNF alone was tested on day 7 C2C12
myotubes, with further confirmation sought from experiments conducted on primary
skeletal muscle cell cultures generated from 5-6 week old FVB mice. A detailed
morphological examination of mean myotube widths from C2C12 (Figure 4.3) and FVB
(Figure 4.5) myotube cultures demonstrated that 20 ng/ml TNF treatment for 3 days was
sufficient to induce a significant decrease in mean myotube width when compared to
untreated control measurements. Those data demonstrate a robust cell culture model of
TNF induced muscle atrophy utilising either well differentiated C2C12 or primary
myotubes, and provides a very useful approach for new atrophy related studies.
The inclusion of FVB primary myotubes provided an additional cell culture model to
test the morphological effects of exogenous TNF treatment, thus avoiding the need to
administer large amount of TNF in vivo to mice. Colleti et al (2005) previously studied
the morphological effects of TNF in vivo using electroporation and gene transfer of an
expression vector encoding the secreted form of murine TNF (mTNF). They compared
type IIb fibre diameters sampled from the quadriceps, tibialis anterior and
gastrocnemius muscles of mTNF and MOCK (empty construct) mice, 5 weeks after
electroporation. The study found that there was a statistically significant decrease in
myofibre cross-sectional area in the mTNF, compared to the MOCK-electroporated
mice for all of the muscles sampled. The results from the present primary FVB muscle
cell culture experiments over 3 days support Colleti et al’s results by similarly
demonstrating TNF induced myotube atrophy in vitro.

Chapter Four Morphological effects of IGF-1 and TNF treatment on cultured myotubes
69
The final experiments using the combined treatments tested if IGF-1 could prevent or
reverse the atrophic effect of TNF in the day 7 myotubes. Previously, our laboratory has
shown that muscle specific over-expression of insulin-like growth factor-1 (IGF-1) in
transgenic mdx/mIGF-1 mice significantly reduces myofibre necrosis (Shavlakadze et
al. 2004) and that this protective effect may be due to increased protein synthesis in the
muscles. Using cells isolated from the IGF:C2 mice, interactions between TNF and
IGF-1 signalling pathways were investigated, with preliminary studies focusing on
morphological changes to the IGF:C2 myotubes when treated with TNF. The data (from
C2C12 myotubes) indicate that IGF-1 prevents the myotube atrophy caused by TNF.
These results do not support previously published studies by Dehoux et al (2007), where
the combined treatment of IGF-1/TNF/IFN-γ resulted in a significant decrease in mean
myotube widths when compared to untreated controls. In contrast, the present IGF-
1/TNF experiments prevented both atrophy and hypertrophy and mean myotube widths
were the same as the controls cultures. It is particularly important to note that the results
indicate that it may be possible to reverse TNF induced atrophy, as when IGF-1 was
administered 24 h after TNF treatment was initiated, the myotubes were significantly
wider than those treated by TNF alone; there was no significant difference compared to
untreated controls (Figure 4.4)
The inclusion of muscle cell cultures isolated from transgenic mice that over-express
IGF-1 provided another model to test the combined treatments of IGF-1/TNF. IGF-1
exists as different isoforms due to different exon splicing (Shavlakadze et al. 2005);
IGF-1 isoforms that initiate from exon 2 are termed Class 2 (C2) isoforms. For
transgenic muscle cultures from mice that over-expressed IGF-1 Class 2 (IGF-1:C2),
exogenous treatment with TNF had no effect on mean myotube widths when compared
to untreated IGF-1:C2 myotubes. Importantly, this supports the findings of the C2C12
combined IGF-1/TNF treatment experiments, where IGF-1 prevented TNF-induced
myotube atrophy, and TNF prevented IGF-1 induced hypertrophy.
The collective results from these three experiments using the C2C12 myotubes
targeting; (i) IGF-1 hypertrophy, (ii) TNF atrophy and (iii) combined IGF-1/TNF,
confirm that C2C12 myotubes are a useful cell culture model to test the effects of
exogenous cytokine/growth factor treatments. The primary cell cultures further validate

Chapter Four Morphological effects of IGF-1 and TNF treatment on cultured myotubes
70
these results. A novel and very important observation was that TNF treatment induced
atrophy in both the C2C12 and FVB primary myotubes. Overall, the results gathered
from all of the experiments confirms the results of those, albeit few, previously
published and also highlights the morphological effects of TNF treatment on cultured
muscle cells.

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
71
Chapter Five
The role of TNF activated JNK in
muscle atrophy in tissue cultured myotubes
Introduction
The optimisation of the experimental conditions to study cultured C2C12 myotubes
aged 7 days, for treatment with either IGF-1 or 20 ng/ml TNF for 3 days provides a
valuable and robust system for investigating the morphological response of mouse
myotubes to IGF-1 induced hypertrophy and TNF induced atrophy (see Chapter 4). This
myotube model further elucidated the morphological response to combined treatment
with IGF-1 and TNF and thus emphasised the cross-talk between these different
pathways that can affect myotube width. Using this model, the aims of the following
experiments are to: (i) elucidate the involvement of the TNF activated mitogen-
activated protein kinase (MAPK) family, the c-Jun N-terminal kinases (JNKs), in
situations of TNF induced myotube atrophy and (ii) the impact of TNF activated JNK
on IGF-1 induced myotube hypertrophy. TNF activated JNK signalling is demonstrated
in differentiated C2C12 muscle cells in culture using morphological and phospho-
protein western analysis.
There is now strong evidence that TNF can inhibit IGF-1 expression (Frost et al. 2003)
and abrogate IGF-1 receptor signalling via inhibition of tyrosine phosphorylation of the
IGF-1 receptor docking protein insulin receptor substrate-1 (IRS-1) (Grounds et al.
2008). The inhibitory effect of TNF on IGF-1 signalling appears to be mediated by JNK
phosphorylation of IRS-1 on Serine residue 307 (Ser 307), which reduces the affinity of
IRS-1 for the IGF-1 receptor (Broussard et al. 2003; Strle et al. 2006) (see Section 1.5.3,
Figure 1.4a and b). To determine the extent to which TNF activated JNK signalling is
involved in both mediating myotube atrophy and the inhibition of IGF-1 induced
hypertrophy, JNK inhibitors were used. It was hypothesised that inhibition of TNF
activated JNK would prevent TNF-mediated atrophy and result in TNF treated myotube
sizes resembling those seen in untreated cultures.

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
72
Initial phospho-protein western blot experiments performed in this study specifically
aimed to determine if treatment with TNF could induce phosphorylation (activation) of
JNK in day 7 C2C12 myotubes. After optimising the most effective minimal dose at
which TNF induces JNK activation, and determining the appropriate time point at
which JNK activity was at a maximum after TNF stimulation, the specific role of JNK
was further investigated using JNK inhibitors. Three inhibitors were assessed for
biological toxicity in C2C12 myotubes, with only one (TAT-TIJIP) appearing to be
most suitable for use in the C2C12 myotubes when applied for 3 days at a 10 µM dose.
Using this inhibitor, the direct activity of the TNF activated JNK signalling pathway
was investigated, with the aim of determining if inhibition of the JNK pathway would
prevent TNF induced C2C12 myotube atrophy. These experiments were then further
validated in FVB and IGF-1:C2 primary myotube cultures.
The JNK inhibitor TAT-TIJIP was shown to prevent TNF induced atrophy in both the
C2C12 myotubes and primary muscle cells. Following this result, the next stage of
experiments sought to confirm that TAT-TIJIP was specifically acting on JNK. To test
this, the activity of the JNK downstream target c-Jun was assessed in TAT-TIJIP treated
cells. JNK binds to the amino-terminal region of the transcription factor c-Jun and
phosphorylates c-Jun at Ser63/73 (Cheng and Feldman 1998; Derijard et al. 1994) (see
Section 1.5.2), resulting in localisation of phosphorylated c-Jun from the cytoplasm to
the nucleus. Immunohistochemical studies with antibodies that detect phosphorylated c-
Jun confirmed the nuclear localisation of c-Jun following stimulation with 20 ng/ml
TNF in day 7 C2C12 myotubes. The nuclear localisation of c-Jun was then further
investigated in day 10 myotubes that were pre-treated with the TAT-TIJIP before
receiving TNF treatment for 3 days. In these studies, the nuclear localisation of
phosphorylated c-Jun was not detected (in contrast with controls) indicating that TAT-
TIJP was effectively inhibiting JNK activity (Cheng and Feldman 1998; Derijard et al.
1994).

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
73
Results
5.1 TNF activates the JNK signalling pathway in C2C12 myotubes
5.1.1 Optimising conditions for detecting TNF activation of the JNK signalling
pathway in day 7 C2C12 myotubes
To determine whether JNK is phosphorylated in response to TNF treatment, and at what
time point this activation is at its maximum, differentiated day 7 C2C12 myotubes were
stimulated with 20 ng/ml TNF for different time intervals, and lysates were probed for
phospho-JNK levels (Figure 5.1: A). To ensure that the solvent (sterile ddH2O) in which
TNF was dissolved had no effect on activation of JNK, an equal volume (1 µl) of
ddH2O was added to the ‘untreated’ (no TNF treatment) cultures. Following Cuenda
and Cohen's (1999) report that 10 µg/ml of anisomycin administered for 30 mins to day
6 C2C12 myotubes resulted in a four-fold activation of JNK, treatment with 10ug/ml of
the protein synthesis inhibitor Anisomycin was included as a positive control in the
study.
Initial time course experiments involved removing the cells from the incubator (which
was maintained at a constant 37ºC) and moving them to the adjacent laminar flow hood,
thereby ensuring that sterile conditions were maintained whilst treatment was
administered. By following this process, the cells were exposed to changes in
temperature, ranging from 37ºC, to room temperature (approximately 23ºC-25ºC), and
then being placed back at 37ºC for the remaining time. This also resulted in some
movement of the fluid in the culture dishes. Western blotting studies detected high
levels of JNK phosphorylation in most of the untreated control lysates, as well as in the
TNF and anisomycin (positive) control lysates. It is hypothesised that the background
phosphorylation of JNK in these controls was due to stress resulting from both
temperature change in and the mechanical disturbance of the cultures. A modified
procedure of administering TNF to undisturbed cultures within the incubator was thus
used for the final experiments (see below). The highest level of JNK phosphorylation
was detected in lysates extracted from myotubes that had been stimulated with 10 µg/ml
Anisomycin for 15 min (Figure 5.1: A). The total levels of JNK protein remained
unchanged in the untreated, TNF and the Anisomycin treated lysates (Figure 5.1: B).

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
74
It is important to note that the phosphorylated JNK (phospho-JNK) and total JNK
antibodies used in this study detect both JNK1/2, and thus two bands are shown in
Figure 5.1 A and Figure 5.2 A. Sometimes, a third band was also visible, with a
molecular weight of approximately 44kDa as shown in the phospho-JNK blots (Figures
5.2 and 5.3: A) and total JNK blots (Figures 5.1 and 5.2: B). This additional band was
also observed when the same antibodies (from the same manufacturer, Cell Signaling
Technologies) were applied to cell lysates that had been extracted from C2C12
myotubes, but did not appear in lysates that had been extracted from proliferating
C2C12 myoblasts as described in Huang et al. (2007).
Figure 5.1: Optimising conditions for detecting TNF phosphorylation of JNK in differentiated (day 7) C2C12 myotubes: preliminary experiments Myotubes cultured in fusion (low serum) medium for 7 days were treated at room temperature with 1 µl of solvent (sterile ddH2O) to serve as the untreated controls or 20 ng/ml TNF for different time intervals: 0 min (untreated control), 5 min, 10 min, 15 min and 30 min. Myotubes were stimulated with 10 µg/ml Anisomycin for 15 min to serve as a positive control for JNK phosphorylation. Cell lysates were extracted and immunoblotted with (A) anti-phospho-JNK and (B) total JNK antibodies. (A) Phosphorylation of the JNK1 and JNK2 was detected in the untreated (ddH20) controls, TNF treated and Anisomycin treated lysates. (B) Equal loading was monitored with total JNK antibody. There was no change in the level of total JNK1 and JNK2 detected between the 3 treatment groups. It was concluded that phosphorylation of JNK in the controls was a stress response to the initial treatment procedure.
This method of cell stimulation was unsuitable due to the high levels of phospho-JNK
in the untreated (sterile ddH2O control) lysates. To reduce the stress incurred on the
cells when being removed from the incubator to be treated, a change was made to the
way the treatment protocol and cells the were carefully stimulated inside the incubator,
thus avoiding the cells being exposed to sudden changes in temperature and movement
of the culture medium. This revised treatment protocol was successful negated.

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
75
Western blot analysis of the untreated control lysates from the second set of
experiments showed no detectable phospho-JNK in the untreated controls (Figure 5.2:
A). In the TNF treated myotube lysates, there was initial phosphorylation of JNK within
10 min of TNF stimulation, with the highest level of JNK phosphorylation detected
within 15 min (Figure 5.2: A). This phosphorylation of JNK then declined but persisted
for up to 30 min (Figure 5.2: A). Anisomycin stimulated a higher level of JNK2 (54
kDa) phosphorylation compared to that seen at 15 min in the TNF treated lysates.
Conversely, 15 min stimulation with TNF induced a higher level of JNK1 (46 kDa)
phosphorylation than for the Anisomycin treated lysates (Figure 5.2: A).
Figure 5.2: Time course assay of TNF phosphorylation of JNK in differentiated (day 7) C2C12 myotubes: final protocol. (A) Western blot of lysates immunoblotted with anti-phospho-JNK shows that in myotubes cultured in differentiation (low serum) medium for 7 days and treated at 37ºC with 20 ng/ml TNF, initial phosphorylation of JNK is detected within 10 min with the highest level of phosphorylation seen within 15 min. Very low levels of JNK phosphorylation are seen up until 30 min after stimulation. JNK phosphorylation was not detected in the untreated controls. Anisomycin, at a dose of 10 µg/ml, was administered for 15 min to serve as a positive control for JNK phosphorylation. (B) Equal loading was monitored with total JNK antibody. 5.1.2 Titration study to determine if JNK phosphorylation is dependant on dosage of TNF To determine whether the phosphorylation of JNK detected within 15 min of
stimulation with 20 ng/ml TNF was the highest level that could be induced in the day 7
myotubes, and additionally determine if higher dosages of TNF treatment would sustain
JNK activation, the cells were treated with varying dosages of TNF and protein was
extracted at 15 and 30 min.

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
76
In the day 7 myotubes, western blot analysis showed no detectable differences in levels
of JNK activation induced by treatment with 20 ng/ml or 50 ng/ml TNF within 15 min.
The lowest level of JNK phosphorylation was observed in the lysates extracted from
myotubes that had received 100 ng/ml TNF (Figure 5.2: A). There was a slightly higher
level of JNK phosphorylation at 30 min in the 50 ng/ml TNF treated lysates, compared
to the level observed at 30 min in the 20 ng/ml and 100 ng/ml TNF treated samples
(Figure 5.3: A). Phosphorylation of JNK was not detected in the untreated controls
(Figure 5.2: A).
Figure 5.3: Titration study to determine the minimum effective dose of TNF to induce phosphorylation of JNK in differentiated (day 7) C2C12 myotubes. (A) Western blot of lysates immunoblotted with anti-phospho-JNK shows that treatment of 7 day myotubes with 20 ng/ml, 50 ng/ml or 100 ng/ml TNF induced comparable levels of JNK phosphorylation. Phosphorylation of JNK was not detected in the untreated controls. Anisomycin, at a dose of 10 µg/ml, was administered for 15 min to serve as a positive control for JNK phosphorylation. (B) Equal loading was monitored with total JNK antibody.
5.2 JNK inhibitors used in TNF induced myotube atrophy studies
5.2.1 Selection of a suitable JNK inhibitor: evaluation of three different inhibitors
at two dosage levels in C2C12 myotubes
After confirming that exogenous treatment with 20 ng/ml TNF for 15 min was sufficient
to induce activation of the JNK signalling pathway (as demonstrated by western blot
analysis – see above), the next step in the present study was to determine which JNK
inhibitors were most suitable (i.e.; non toxic) for use in conjunction with the TNF
induced muscle cell atrophy model (as described previously - see Section 4.2).

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
77
The toxicity of three JNK inhibitors was tested (TAT-TIJIP, SP600125 and AS601245)
in conjunction with their respective controls; TAT peptide (control peptide for TAT-
TIJIP) and DMSO (diluent for TAT-TIJIP and TAT); see Section 1.5.4. Of the three
inhibitors tested, TAT-TIJIP is a novel ATP-non-competitive, JIP-derived cell
permeable peptide inhibitor of JNK, produced by Dr Marie Bogoyevich (Arthur et al.
2007). The ATP-competitive inhibitors (SP600125 and AS601245) are commercially
available. Each inhibitor was tested at two dosages (5 µM and 10 µM) for 3 days to
determine the dose at which the inhibitor did not have an adverse effect on myotube
morphology. On day 3 of treatment the myotubes were fixed and any changes to
myotube morphology were visually assessed (see Section 2.4.3).
On day 3 of treatment (day 10 after fusion) the phase contrast images of ‘control’
C2C12 myotubes (those treated with the TAT peptide or with DMSO) showed no
difference in appearance when compared to untreated myotube cultures (Figure 5.4: A,
B and C).
The myotubes that had been treated for 3 days with either 5 µM or 10 µM of the novel
JNK inhibitor peptide TAT-TIJIP had a similar appearance to the untreated and control
cultures (Figure 5.4: D1 and D2). The myotubes treated with of 5 µM of SP600125 also
appeared morphologically normal (Figure 5.4: E1), however at the higher dose (10 µM)
the myotubes appeared slightly thinner, with a noticeable increase in the number of
unfused/dying cells (Figure 5.4: E2). The myotubes that had received 5 µM AS601245
appeared thinner than the untreated cultures and were starting to detach from the culture
dish after 3 days of treatment; this suggests that the inhibitor was toxic (Figure 5.4: F1).
At the higher dose (10 µM) AS601245 was found to be highly toxic, with considerable
cell death resulting in very few myotubes remaining alive (Figure 5.4: F2).

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
78
Figure 5.4: Toxicity evaluation of three JNK inhibitors on day 10 C2C12 myotubes. Phase contrast images show untreated C2C12 myotubes at day 10 of culture in fusion medium (A1 and A2), control myotubes that had been treated for 3 days with DMSO (B1 and B2), TAT peptide treated control myotubes (C1 and C2) and test myotubes that had been treated with the JNK inhibitors TAT-TIJIP (D1,2), SP600125 (E1,2) or AS601245 (F1 and F2). Myotubes treated with 5 µM and 10 µM TAT-TIJIP (D1 and D2 respectively) showed no difference in appearance compared to untreated (A1 and A2) and TAT treated controls cultures (C1 and C2). SP600125 was non-toxic to C2C12 myotubes at a dose of 5 µM (E1) but had an adverse effect on myotubes at a dose of 10 µM (E2). Both doses of AS601245 were toxic to C2C12 myotubes (F1 and F2). Magnification: 10x. Bar: 100 µm.

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
79
5.2.2 Experiments to determine if TNF induced myotube atrophy can be prevented
by pre-treatment with the JNK inhibitor TAT-TIJIP
The following experiments were performed using C2C12 myotubes and primary
myotube cultures. It is important to note that the experiments involving the primary
FVB muscle cells were not conducted in direct parallel (at the same time) as those
experiments involving the IGF:C2 muscle cell cultures. For this reason, the results from
experiments using the control FVB muscle cells are not directly compared to those
generated from the IGF:C2 muscle cell cultures.
5.2.2.1 Analysis of the morphological effects of TAT-TIJIP on untreated and TNF
treated C2C12 myotubes
To explore the involvement of JNK in mediating TNF induced myotube atrophy, day 7
C2C12 myotubes were pre-treated with TAT-TIJIP (10 µM) for 1 h before treatment
with TNF for 3 days. Quantitative analysis (Figure 5.5) confirmed highly significant
differences in myotube widths resulting from treatment with TNF (20 ng/ml) alone
compared to combined TAT-TIJIP/TNF treatment for 3 days. Myotube widths were
quantified as previously outlined (see Section 2.4.3). Width measurements were
collected from 50 randomly selected myotubes from a number of cultures dishes; the
number of repeats is specified for each group in Figure 5.5. As a reference, the results
for the untreated and TNF treated C2C12 myotubes (shown in Figure 4.3), were
included in this study to compare pre-treated combined TAT-TIJIP/TNF treated (TAT-
TIJIP + TNF) myotubes with TNF only treated. As there were no significant differences
between new controls (n = 5) and old controls (n = 6), the results were pooled together.
Pre-treatment with TAT-TIJIP (10 µM) 1 h before the administration of TNF (20 ng/ml)
resulted in a significant increase (P < 0.0001) in mean myotube width when compared
to untreated (~20% difference) and TNF treated (~55% difference) control myotubes
(Figure 5.5). The myotubes treated with TAT-TIJIP + TNF were also significantly
wider (P < 0.01) than those that had been treated with TAT-TIJIP alone (Figure 5.5).
Both TAT-TIJIP and the TAT control peptide had no effect on myotube widths when
compared to the untreated controls (Figure 5.5). Combined treatment with the TAT
control peptide and TNF (TAT control + TNF) resulted in a significant decrease (P <
0.0001) in mean myotube widths, when compared to untreated, TAT-TIJIP and TAT

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
80
control treated myotubes; conversely, when compared to TNF treated myotubes, no
significant difference in mean myotube widths was evident (Figure 5.5).
Figure 5.5: Mean width of untreated control C2C12 myotubes and C2C12 myotubes treated with TNF alone, TAT-TIJIP alone, combination of TAT-TIJIP and TNF, TAT alone and combination of TAT and TNF. C2C12 myotubes treated for 3 days with TNF (20 ng/ml) show a significant decrease in myotube width, whereas pre-treatment with the JNK inhibitor TAT-TIJIP for 1 h before TNF treatment induced a significant increase to mean myotube width when compared to Untreated (control) myotubes. Treatment with TAT-TIJIP alone or TAT control alone or in combination with TNF had no effect on the mean myotube width when compared to untreated (control) myotubes. Results are mean myotube widths + SE of independent experiments indicated for each treatment (n = 50 myotube diameters/experiment). *P < 0.01 and *P < 0.0001. The numbers within each bar represent the number of times the experiments were repeated in separate dishes, with the results pooled.
5.2.2.2 Analysis of the morphological effects of TAT-TIJIP on untreated and TNF
treated control FVB mouse myotubes in primary cultures
To further test the preventive effects of TAT-TIJIP on TNF induced atrophy, primary
myotube cultures derived from 4-6 week old FVB mice were generated and treated with
combined TAT-TIJIP + TNF. As in the C2C12 myotubes, pre-treatment with TAT-
TIJIP 1 h before treatment with TNF (TAT-TIJIP + TNF group) for 3 days resulted in a
significant increase (P < 0.0001) in mean myotube widths when compared to TNF
treated (28% difference) control myotubes (Figure 5.6). The myotubes treated with
TAT-TIJIP + TNF were also show a significant increase in width (P < 0.005) compared
to those treated with TAT-TIJIP alone; this is similar to the results from the analysis of
C2C12 myotubes. Again, when administered alone as controls, both TAT-TIJIP and the

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
81
TAT control peptide had no effect on myotube widths, in comparison to the untreated
controls (Figure 5.6).
The combined treatment with the TAT control peptide and TNF (TAT control + TNF)
resulted in a significant decrease (P < 0.05) in the mean width of the FVB myotubes in
comparison to the untreated TAT-TIJIP and TAT control treated myotubes. Also, when
compared to the TNF treated myotubes, no significant difference in mean myotube
widths was evident (Figure 5.6). These results are again consistent with the initial study
conducted using C2C12 myotubes (Figure 5.5).
Figure 5.6: Mean width of untreated control primary FVB myotubes and FVB myotubes treated with TNF alone, TAT-TIJIP alone, combination of TAT-TIJIP and TNF, TAT alone and combination of TAT and TNF. FVB primary myotubes treated for 3 days with TNF (20 ng/ml) show a significant decrease in myotube width, whereas pre-treatment with the JNK inhibitor TAT-TIJIP for 1 h before TNF treatment induced a significant increase to mean myotube width when compared to TNF alone treated myotubes. Treatment with TAT-TIJIP alone or TAT alone had no effect on mean myotube width when compared to untreated (control) myotubes. Significant differences between the mean myotube widths are seen when myotubes treated with TAT-TIJIP alone are compared to those that had received combined TAT-TIJIP + TNF treatment, with the latter showing an increase in mean myotube widths. Results are mean myotube widths + SE of independent experiments indicated for each treatment (n = 50 myotube diameters/experiment). *P < 0.05, **P < 0.005 and *P < 0.0001. Data were pooled form three independent experiments
5.2.2.3 Analysis of the morphological effects of TAT-TIJIP on untreated and TNF
treated transgenic IGF:C2 mouse myotubes in primary cultures
The combined TAT-TIJIP + TNF treatment experiments conducted on the day 7
C2C12, myotubes and day 4 FVB, myotubes were repeated using primary cultures of
myotubes from IGF:C2 transgenic mice. The IGF:C2 myotubes provided an opportunity
to test whether the preventative effect of (endogenous) elevated IGF-1 on TNF induced

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
82
myotube atrophy (see Figure 4.5) could be further enhanced when (TNF) activated JNK
is inhibited by TAT-TIJIP.
The addition of TNF (20 ng/ml) to the IGF:C2 day 4 myotubes for 3 days resulted in no
significant change to mean myotube size in comparison to the untreated IGF:C2
myotubes (see Section 4.4.2). Pre-treatment with TAT-TIJIP (10 µM) at 1 h before the
administration of TNF (20 ng/ml) significantly increased (P < 0.05) mean myotube
widths compared to the TNF treated (~ 20% difference) and TAT control + TNF (~25%
difference) control IGF-1:C2 myotubes (Figure 5.7).
In contrast to the results using C2C12 (Figure 5.5) and FVB myotubes (Figure 5.6),
transgenic IGF:C2 myotubes treated with TAT-TIJIP + TNF presented no significant
increase in myotube widths compared to the controls treated with TAT-TIJIP alone.
Further, both the TAT-TIJIP and the TAT control peptide had no effect on myotube
widths compared to untreated controls (Figure 5.7) as was also observed for both
C2C12 and FVB cultures. Surprisingly, the IGF:C2 myotubes treated with the TAT
control alone appeared to have a larger width compared to the untreated and TAT-TIJIP
only treated myotubes, although this difference was not statistically significant. IGF:C2
myotubes treated with TAT control + TNF, were significantly smaller in width (P <
0.05; ~20%) compared with control TAT only treated myotubes and were actually the
same size as myotubes treated with only TNF.

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
83
Figure 5.7: Mean width of untreated control primary IGF:C2 myotubes and IGF:C2 myotubes treated with TNF alone, TAT-TIJIP alone, combination of TAT-TIJIP and TNF, TAT alone and combination of TAT and TNF. The transgenic IGF:C2 primary myotubes that were treated for 3 days with TNF (20 ng/ml) alone show no changes to mean myotube width when compared to untreated myotubes. Treatment with TAT-TIJIP alone or TAT alone had no effect on mean myotube width when compared to untreated (control) myotubes. Myotubes that had received combined TAT-TIJIP + TNF treatment are significantly wider when compared to those that had received TNF treatment alone. Myotubes that had been treated with TAT control alone were also significantly wider than those that had received combined TAT + TNF treatment. (n = 50 myotube diameters/experiment). *P < 0.05. Data were pooled form 3 independent experiments
5.3 Confirmation of the inhibition of JNK phosphorylation by TAT-TIJIP:
immunofluorescent nuclear localisation of the transcription factor c-Jun
The inhibitory effect of TAT-TIJIP on JNK was verified by assaying the nuclear
localisation of phosphorylated c-Jun (a downstream target of phosphorylated JNK) in
C2C12 and primary muscle cell cultures. Since the phosphorylation of JNK results in
the localisation of phosphorylated c-Jun, the inhibition of JNK phosphorylation would
be expected to prevent nuclear localisation of phosphorylated c-Jun (Melino et al.
2008).
The first immunonuclear localisation bioassay was performed to determine whether
treatment with TNF (20 ng/ml) induced the phosphorylation and nuclear localisation of
c-Jun in well differentiated day 7 C2C12 myotubes (see Section 5.3.1). Following this,
the inhibition of JNK phosphorylation by TAT-TIJIP was tested by analysing of nuclear
located phosphorylated c-Jun (see Section 5.3.2). The later study was performed in all

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
84
three skeletal muscle cell cultures, immortalised C2C12 myotubes and primary muscle
cultures generated from FVB and transgenic IGF:C2 mice.
5.3.1 Time course analysis of the nuclear localisation of phosphorylated c-Jun in
day 7 C2C12 myotubes
To determine the involvement of phosphorylated JNK in inducing the nuclear
localisation and phosphorylation of c-Jun, in mediating TNF induced myotube atrophy,
a time course of c-Jun activity was performed in day 7 C2C12 myotubes using
immunofluorescent-labelled antibodies that detect phosphorated c-Jun at Serine 73
(Ser73). It is well documented that JNK1 binds to the amino-terminal region of c-Jun
and phosphorylates c-Jun at two sites (Serine 63 and Serine 73) activating c-Jun-
dependent transcription (Derijard et al. 1994; Kyriakis and Avruch 2001). Strle et al
(2006) previously described the direct relationship between TNF phosphorylated JNK
and c-Jun in C2C12 myoblasts, reporting that phosphorylation of c-Jun was detectable
by western blot as early as 5 min after stimulation with TNF (1 µg/ml).
Day 7 C2C12 myotubes were stimulated with TNF (20 ng/ml) and fixed at various
times (15 min, 30 min, 1 h and 2 h) after treatment. The myotubes were then double
immunostained for phosphorylated c-Jun and desmin. The immunofluorescent
microscopy images shown in Figure 5.8 are representative overlays of 3 images taken at
various excitation wavelengths, depending on the detection reagent for the secondary
antibodies; anti-phosphorylated c-Jun was detected at an excitation of 593 nm
(visualised red) and anti-desmin at 495 nm (visualised green). The Hoechst nuclear stain
(Hoechst 33342) was visualised blue (at 357 nm). Therefore, when the 3 images are
overlayed, the translocation of activated c-Jun appears purple in colour.
The nuclear localisation of phosphorylated c-Jun was assessed visually in the myotubes.
Images of day 7 C2C12 myotubes that were stimulated with TNF (20 ng/ml) showed
nuclear localisation of phosphorylated c-Jun within 15 min after treatment, with the
phosphorylation persisting for up to 2 h (Figure 5.8). In the TNF treated C2C12
cultures, nuclear localisation of phosphorylated c-Jun was also detected in cells that did
not stain positive for desmin (Figure 5.8). The untreated cultures (those exposed to
ddH20 the diluent for TNF) had no detectable phosphorylated c-Jun (Figure 5.8).

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
85
Figu
re 5
.8:
Exp
osur
e to
TN
F in
crea
ses
phos
phor
ylat
ed c
-Jun
in C
2C12
myo
tube
s. M
yotu
bes
wer
e ei
ther
(A
) U
ntre
ated
(co
ntro
l) or
(B
) ex
pose
d to
20
ng/m
l TN
F (1
5 m
in -
2 h,
as i
ndic
ated
), do
uble
imm
unos
tain
ed w
ith a
ntib
odie
s rec
ogni
sing
pho
spho
-Ser
73
c-Ju
n (r
ed) a
nd d
esm
in
(gre
en),
and
then
cou
nter
stai
ned
with
Hoe
chst
nuc
lear
stai
n (b
lue)
. The
det
ectio
n of
pho
spho
ryla
ted
c-Ju
n in
the
cell
nucl
ei is
indi
cate
d by
pur
ple.
M
agni
ficat
ion:
20x
. Sca
le: 1
00µm

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
86
5.3.2 Immunofluorescent microscopy analysis of TAT-TIJIP inhibition of c-Jun
nuclear localisation (phosphorylation) in TNF induced myotube atrophy in C2C12,
FVB and IGF:C2 cultures
The nuclear localisation of phosphorylated c-Jun was also assessed visually in all
myotube cultures. Cultures were pre-treated with TAT-TIJIP for 1 h before TNF (20
ng/ml) was administered for 3 days (following the protocol for the morphological
studies in Section 2.4.2). The overlayed immunofluorescence microscopy images are
presented in Figure 5.9. In the untreated cultures (exposed to only ddH20 the diluent for
TNF) phosphorylation and nuclear localisation of c-Jun was not detected in the desmin
positive myotubes (Figure 5.9: A, B and C) but was detected in the TNF treated cultures
(Figure 5.9: A2, B2 and C2, indicated by arrows). In some cultures, the nuclear
localisation of phosphorylated c-Jun was also detected in cells that did not stain positive
for desmin (Fig 5.9: A2, B2, C2, C3 and C4, indicated by the asterisk).

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
87
Figu
re 5
.9: T
AT
-TIJ
IP p
reve
nts
c-Ju
n ph
osph
oryl
atio
n fo
llow
ing
TN
F tr
eatm
ent o
f myo
tube
s. M
yotu
bes
(C2C
12 o
r prim
ary
cultu
res
deriv
ed f
rom
FV
B (
Prim
ary
cont
rol)
or I
GF1
-ove
rexp
ress
ing
mic
e IG
F:C
2 (P
rimar
y tra
nsge
nic)
wer
e ei
ther
left
untre
ated
(c
ontro
l), e
xpos
ed to
20
ng/m
l TN
F, o
r pre
-trea
ted
for
1 h
with
eith
er 1
0 µM
TA
T-TI
JIP
pept
ide,
or
10 µ
M T
AT
pept
ide
prio
r to
TN
F tre
atm
ent.
The
myo
tube
s w
ere
then
dou
ble
imm
unos
tain
ed w
ith a
ntib
odie
s re
cogn
isin
g ph
osph
o-Se
r 73
c-J
un (
red)
, an
ti-de
smin
ant
ibod
y (g
reen
), an
d th
en c
ount
erst
aine
d w
ith H
oech
st n
ucle
ar s
tain
(bl
ue).
The
dete
ctio
n of
pho
spho
ryla
ted
c-Ju
n in
the
cell
nucl
ei is
indi
cate
d by
pur
ple.
Ast
eris
ks (*
) ind
icat
es p
hosp
hory
latio
n an
d lo
calis
atio
n of
c-J
un in
cel
ls th
at d
id n
ot s
tain
pos
itive
fo
r des
min
. Mag
nific
atio
n: 2
0x. S
cale
: 100µm
.

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
88
5.4 Analysis of IRS-1 and AKT (downstream of IGF-1) to further investigate TNF
inhibition of IGF-1 signalling via JNK, in the model of C2C12 myotube atrophy
It has been suggested that activated JNK is involved in abrogating IGF-1 signalling, via
phosphorylation of the adaptor molecule IRS-1 on serine 307 to disrupt its association
with the IGF-1 receptor (reviewed in Grounds et al. 2008), thus preventing activation
(phosphorylation) of downstream AKT (see Section 1.5.3, Figure 1.4a). To investigate
the cross-talk between TNF and IGF-1 signalling in C2C12 myotubes, a western
analysis was used to measure activation (phosphorylation) of two signalling events
downstream of the activated IGF-1 receptor, specifically the phosphorylation of IRS-1
and AKT.
5.4.1. Optimising western blotting conditions for immunoprecipitated IRS-1 from
C2C12 day 7 myotubes treated with IGF-1
As it has been previously reported that 15 min treatment with IGF-1 stimulates tyrosine
phosphorylation of IRS-1 in C2C12 myoblasts (Milasincic et al. 1996; Strle et al. 2006),
initial optimising phospho-protein experiments were performed as a time course assay
on untreated or IGF-1 (10 ng/ml) treated (5 min, 15 min, 30 min, 60 min and 1 h)
C2C12 day 7 myotubes, Immunoprecipitation of phosphorylated proteins from cell
culture or muscle samples has not been previously performed within the Grounds
laboratory, despite numerous repeated attempts over three years, which included:
trailing and testing a range of protein extraction buffers; implementation of various
modifications to the immunoprecipitation protocol (these include: incubating the protein
beads with the lysates anywhere from 2-12 hrs, with/without rocking); testing different
protein agarose beads (Protein A or Protein G) to determine if the beads were not
capturing the IRS-1 antibodies; and the purchasing and testing various IRS-1 antibodies
from various antibody companies (in an attempt to determine if the antibody was the
problem). Despite these attempts, this assay was not successful in detecting tyrosine
phosphorylated IRS-1 in C2C12 myotubes stimulated with IGF-1 or 100nM Insulin (to
act as a positive control - del Aguila et al. (1999) for 15 min. Therefore, advice was
sought from Dr Jon Whitehead, Head, Cell Signalling Group at the Diamantina Institute
for Cancer, Immunology and Metabolic Medicine, Princess Alexandra Hospital,
University of Queensland, as he has successfully used this assay in published studies on

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
89
both 3T3 adipocytes and Chinese Hamster Ovary (CHO) cells (Thomas et al. 2006).
Accordingly, I visited his laboratory for one intensive week of laboratory work in
September, 2008
At Dr Whitehead’s laboratory I had access to a number of positive controls which I
could run in parallel to test (Grounds) lysates. The positive controls were lysates
extracted from C2C12 myotube that had been stimulated with Insulin (100nM) for 15
min (del Aguila et al. 1999), in addition to lysates from untreated and Insulin treated (15
min) CHO cells over expressing the insulin receptor (IR) and IRS-1 (IRS.1) (Clark et al.
1998).
The assay was performed under Dr Whitehead’s supervision. It again, however, proved
unsuccessful with no tyrosine phosphorylation (pY) of IRS-1 detected in our C2C12
myotubes stimulated with 100nM Insulin (15 min) compared to the positive controls
from Dr Whitehead’s laboratory (15 min Insulin stimulated C2C12 myotubes and CHO-
IR-IRS-1 cells). The results from the assay thus suggest that the C2C12 cells that were
used throughout this PhD research project had very low levels of IRS-1 that could not
be detected using the current immunoprecipitation protocols.

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
90
. Figure 5.10: Comparison of tyrosine phosphorylation (pY) of IRS-1 in Insulin stimulated C2C12 cells from two different laboratories. The phosphorylation of IRS-1 was detected in lysates extracted from C2C12 myotubes that had been cultured from cell stocks at Dr Whitehead’s Laboratory, and in the positive controls; CHO-IR_IRS-1 stimulated with Insulin. There was no detectable level of pY IRS-1 in our stocks (Grounds). IRS-1 protein is present in our stocks (Grounds) and was detected in all lysates from both laboratories. In the merged image, pY IRS-1 is visualised as a yellow colour and only seen in Insulin stimulated samples form Dr Whitehead’s Laboratory (C2C12: Whitehead and CHO-IR: wt.IRS-1).
5.4.2. Western blotting analysis of AKT from C2C12 day 7 myotubes treated with
IGF-1 or TNF
Due to the problems associated with detecting phosphorylated IRS-1, the
phosphorylation of AKT was studied in C2C12 myotubes that had been treated with
IGF-1. As it has been demonstrated (in day 2 and day 4 C2C12 myotubes) that IGF-1
(10 ng/ml) induces phosphorylation of AKT (a well defined target downstream of
activated IRS-1), analysis of AKT phosphorylation is thus a logical choice to
demonstrate inhibition by TNF of IGF-1 signalling (Rommel et al. 1999; Rommel et al.
2001).
In day 7 C2C12 myotubes treated for 15 min with IGF-1 (10 ng/ml), or TNF (20 ng/ml),
phosphorylated AKT was detected and this level of activation was slightly higher than

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
91
that detected in the untreated cultures. Densitometry was performed on this one blot and
indicated that treatment with either TNF or IGF-1 induced activation of AKT
(approximately 11% and 18% increase respectively) compared to the level of activation
in the untreated control sample. Total levels of AKT protein remained relatively
unchanged in the IGF-1 and TNF treated and untreated control lysates (Figure 5.11: B).
Figure 5.11: Activation of AKT in differentiated (day 7) C2C12 myotubes treated with TNF or IGF-1. (A) Western blot of lysates immunoblotted with anti-phospho-AKT shows that in myotubes cultured in differentiation (low serum) medium for 7 days and treated at 37ºC with 1 µl of solvent (sterile ddH2O) to serve as the untreated controls, 20 ng/ml TNF or 10 ng/ml IGF-1 for 15 min. The level of AKT phosphorylation was slightly higher in the TNF and IGF-1 treated samples. (B) Equal loading was monitored with total AKT antibody.
Based on the preliminary results of this western blot, phospho-protein analysis of
activated AKT was also proved to be unsuitable assay for demonstrating the cross talk
between IGF-1 and TNF signalling pathways, because of due to the increase in
phosphorylated AKT observed in the TNF samples, compared to the untreated (sterile
ddH2O) controls.

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
92
Discussion
It has been suggested that activation of the JNK pathway is involved in the
pathophysiology of a number of inflammatory conditions, such as inflammatory bowel
disease (Roy et al. 2008), Duchenne Muscular Dystrophy ( mouse models -
Kolodziejczyk et al. 2001; Lang et al. 2004) and in rheumatoid arthritis ( rat models -
Han et al. 2001). It is also widely considered that TNF plays a critical role in skeletal
muscle atrophy (see Chapter 4), although the precise role of TNF activated JNK in
situations of TNF mediated myofibre atrophy is still largely unknown. Cell signalling
studies have suggested that the damaging effects of TNF may also be the result of JNK
interference with IGF-1 synthesis (Frost et al. 2003) or IGF-1 signalling, through the
association of JNK1 with the IGF-1 docking protein IRS-1 (Broussard et al. 2004;
Broussard et al. 2003; Strle et al. 2006; Grounds et al. 2008).
Strle et al (2006) exemplified the use of the JNK inhibitor peptide SP600125 to
establish that TNF activated JNK suppresses the biological activity of IGF-1 in
proliferating C2C12 myoblasts. The data obtained from the present study extend this
knowledge to both C2C12 myotubes and to primary cultures of mouse skeletal muscle
treated with TNF. In the present series of studies, a novel JNK inhibitor (TAT-TIJIP)
was included to test the role of activated JNK in TNF induced myotube atrophy.
With the aim of elucidating the role of JNK in TNF induced myotube atrophy, the initial
protein analysis experiments were performed to determine whether treatment with TNF
(20 ng/ml) is sufficient to induce JNK activity in well differentiated day 7 C2C12
myotubes. Previously, western blot analysis of TNF induced phospho-JNK activity has
only been shown in proliferating C2C12 myoblasts (Strle et al. 2006; Huang et al. 2007)
or by immunoprecipitation from C2C12 myotubes (at day 4 of fusion) using JNK1
antibody followed by in vitro kinase assay using GST-c-Jun as substrate (Srivastava et
al. 2007). The results presented in this study show for the first time, using western blot
analysis of total cell lysates from mature myotubes, that TNF strongly activates JNK
within 10 to 15 min after the initial TNF stimulation (Figure 5.2).
Previous research investigating the function of JNK has largely depended on the use of
inhibitors. Such JNK inhibitors have been categorised into two groups; chemical

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
93
inhibitors that are ATP-competitive (i.e. that target the ATP binding site of JNK and
subsequently other MAPK) and newer peptide inhibitors that are ATP-non-competitive
(directly bind to sites other that the ATO-binding site of JNK) (Bogoyevitch 2005 and
see Section 1.5.3, Figure 1.4a and b). To evaluate the most suitable JNK inhibitor for
use in the TNF induced models of skeletal muscle atrophy, the toxicity of two ATP-
competitive inhibitors (SP600125 and AS601245), and one novel ATP-non-competitive
JNK inhibitor (TAT-TIJIP), was tested in C2C12 myotubes.
When applied to C2C12 myotubes for 3 days, both SP600125 (10 µM) and AS601245
(at 5 µM and 10 µM concentration) were toxic in the cell cultures. The toxicity of
SP600125 in C2C12 cells has been previously demonstrated in C2C12 myoblasts when
applied for 24 h at a concentration of 10 µM (Strle et al. 2006). However, SP600125 is
still considered the most widely used of the JNK inhibitors, despite the specificity of
this inhibitor being questioned (Bain et al. 2003; Bogoyevitch and Arthur 2008).
The toxic effect of AS601245 on the C2C12 myotubes was particularly surprising
because numerous studies have reported on the protective effects of AS601245 in vivo,
in rat models of myocardial ischemia (Ferrandi et al. 2004), and cerebral ischemia
(Carboni et al. 2004). This was also demonstrated in gerbil models (Carboni et al.
2007). The first reports using the ATP-non-competitive, cell penetrable JNK inhibitor
(D-JNKI-1) demonstrated that it has some neuroprotective ability in rat models of
cerebral ischemia (Borsello et al. 2003) (See Section 1.5.4.1).
The ATP-non-competitive JNK inhibitor (TAT-TIJIP) demonstrated no adverse effects
in the present study when administered alone at a concentration of 10 µM, to day 7
C2C12 myotubes for 3 days, or when administered in combination with TNF, in both
C2C12 and primary muscle cell cultures. Similarly, a longer D-amino acid peptide (D-
JNKI-1) has been shown to be non-toxic when administered to C2C12 myoblasts for 36
h at a concentration of 10 µM (Strle et al. 2006) One advantage of using an ATP-non-
competitive JNK inhibitor, such as TAT-TIJIP or D-JNKI-1, relates to their specificity
(see Bogoyevitch et al. 2004; 2005)). Similar to D-JNKI-1, TAT-TIJIP also contains a
cell permeable 10-amino acid human immunodeficiency virus-TAT transporter
sequence which facilitates the entry of the inhibitor into cells (Vives et al. 1997).

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
94
In the present study, the use of the JNK inhibitor (TAT-TIJIP) supports the direct
involvement of activated JNK in tissue cultures models of TNF induced myotube
atrophy. One of the main mechanisms by which TNF induces myofibre atrophy and
myofibre necrosis, is TNF induced activation of NF-ĸβ (Reid and Li 2001; Eley et al.
2008). Recently, it has also been reported that treatment of C2C12 myotubes with TNF
(50 ng/ml) alone or in combination with IFNγ (10 ng/ml), depressed protein synthesis
within 2 h of administration (Eley et al. 2008; Eley et al. 2008). These findings were
suggested to be due to an increased formation of reactive oxygen species (ROS), via the
activation of p38 MAPK (Eley et al. 2008). Furthermore, it is known that ROS also
activates the JNK and p38 MAPK stress activated protein kinase pathways (Arthur et al.
2008), although the role of JNK in TNF induced muscle wasting is not well established.
A number of reports propose that JNK activation directly interacts with IGF-1
dependant events, and there is strong evidence that TNF activated JNK is involved in
the down regulation of IGF-1 mRNA synthesis in C2C12 myoblasts (Frost et al. 2003).
TNF induced JNK activity has also been suggested as being directly involved in
inhibiting the signalling pathways downstream of IGF-1, by binding to the IGF-1
docking protein IRS-1 (see Grounds et al. 2008). In the present study, repeated attempts
to demonstrate JNK interception with IGF-1 activated IRS-1 proved unsuccessful, thus
the focus was shifted onto examining the activity of AKT in the C2C12 muscle cell
cultures.
The results of the present research show a slight activation in phosphorylated AKT
when TNF was administered to the cells for 15 min compared to the level detected in
the untreated controls. In consideration of recent findings, this observation is not so
unusual, as Eley et al (2008) showed that treatment with TNF (50 ng/ml) induced
activation of mTOR in C2C12 myotubes, although this increase was apparently not
statistically significant. However, these results combined with the results of this present
study (Figure 5.11) suggest that the slight activation of mTOR and AKT induced by
TNF may be the result of autophosphorylation activated by oxidative stress (Eley et al.
2008). The involvement of oxidate stress on inducing activation of AKT is yet to be
fully defined and is an important area of potential future research.

Chapter Five The role of TNF activated JNK in muscle atrophy in tissue cultured myotubes
95
The results of the present study strongly suggest that JNK is involved in mediating TNF
induced myotube atrophy. The myotube morphology studies showed that pre-treatment
with the JNK inhibitor TAT-TIJIP prevented TNF induced myotube atrophy. Myotubes
treated with TNF alone displayed nuclear localisation and phosphorylation of c-Jun;
those pre-treated with TAT-TIJIP showed significantly fewer (if any) nuclei displaying
phosphorylated c-Jun. The preliminary signalling studies presented here require
significant further investigation, however, it was demonstrated that treatment with TNF
(as low as 20 ng/ml) is sufficient to induce phosphorylation of JNK in day 7 C2C12
myotubes. The IRS-1 and AKT studies could not be continued due to time constraints;
however the findings presented here provide a solid framework from which further
studies can and should be continued. On the basis of this study performed to this point,
it was accordingly decided that the next series of experiments would be performed in
vivo, in order to assess the protective effects of TAT-TIJIP in situations of muscle
necrosis.

Chapter Six Preliminary study to investigate the effects of TAT-TIJIP on reducing exercised induced myofibre necrosis in
vivo in mdx mice
96
Chapter Six
Preliminary study to investigate the effects of TAT-TIJIP on
reducing exercised induced myofibre necrosis in vivo
in mdx mice
Introduction
In vivo studies in dystrophic mdx mice subjected to exercise-induced muscle fibre
(myofibre) cell death (necrosis) were performed to test the effect of pharmacological
inhibition of JNK on the phenotype of dystrophic muscle, with respect to histological
quantitation of myofibre necrosis. All previous experiments have been performed using
tissue culture muscle models of TNF induced myotube atrophy. It was thus necessary to
further test the beneficial effects of the JNK inhibitory peptide TAT-TIJIP in an in vivo
situation of muscle damage and necrosis.
Animal studies were conducted on mdx mice (C57BL/10ScSnmdx/mdx), a well known
animal model for DMD (Partridge 1991). The experiments were performed using mice
6 weeks of age, selected because previous research has demonstrated that this is the
period at which muscle necrosis stabalises (to approximately 6%); three weeks after the
onset of acute muscle necrosis is seen in the limb muscles of mdx mice (Coulton et al.
1988; McGeachie et al. 1993; Grounds and Torrisi 2004; Shavlakadze et al. 2004). As
previously noted in Section 1.3.2.1, these low levels of muscle necrosis make assessing
the effectiveness of therapeutic interventions on reducing myofibre necrosis difficult,
because of this the mice were subjected to voluntary exercise.
Voluntary wheel running is a suitable exercise model for inducing a significant increase
in quadricep muscle necrosis (Archer et al. 2006; Hodgetts et al. 2006; Radley and
Grounds 2006), however for this to occur, mice from each treatment group are ideally
required to run similar distances, so that any changes to the amount of myofibre
necrosis measured in the quadriceps can be compared to the treatment, thus eliminating
the possibility that these differences are a direct result of the varying distances run.

Chapter Six Preliminary study to investigate the effects of TAT-TIJIP on reducing exercised induced myofibre necrosis in
vivo in mdx mice
97
As there is little published data on the in vivo effects of JNK inhibitors, and no
published data on the in vivo effects of TAT-TIJIP, the current experimental design was
based on methodology presented by Kaneto et al. (2004), which describes methodology
for the use of another the JNK inhibitory peptide, JIP-1-HIV-TAT (JNKI-1; similar to
TAT-TIJIP - see Section 1.5.4.2) in inhibiting JNK in vivo. The optimised protocol
described in this study involved 8 week old obese diabetic C57/BL/KsJ-db/db mice
receiving daily, intraperitoneal injections of JIP-1-HIV-TAT (at a dose of 10 mg/ml) for
2 weeks (Kaneto et al. 2004). For the present study, a similar protocol was followed; 6
week old mdx mice received daily, intraperitoneal treatments of TAT-TIJIP (10mg/kg)
for 3 days. The effects of the TAT-TIJIP treatments on exercised induced muscle
necrosis in the mdx mice are described below.

Chapter Six Preliminary study to investigate the effects of TAT-TIJIP on reducing exercised induced myofibre necrosis in
vivo in mdx mice
98
Results
6.1 The effect of JNK inhibitor TAT-TIJIP on reducing myofibre necrosis in 6
week old voluntary exercised mdx mice
6.1.1 Distance run by the mdx mice
As not all mice exercised voluntarily (Table 6.1), it was necessary to select the mice that
had run the greatest distance, as it is hypothesised that these mice would display greater
muscle damage, compared to those that ran less, and thus the effects of TAT-TIJIP
could be more effectively tested.
There was no difference in the average total distance covered over the 48 h by the
untreated mice (2.56 km), when compared to the TAT-TIJIP treated mice (2.59 km),
with (as noted above) some mice not running at all (Table 6.1). This average total
distance run by the mdx mice is significantly less than previous studies of wheel
running that reported distances between 2-6 km per 24 h (Dupont-Versteegden et al.
1994; Radley and Grounds 2006; Wineinger et al. 1998).
Mdx mice were pre-treated with TAT-TIJIP (10 mg/ml) 24 h (day 1) before being
exposed to 48 h of voluntary exercise (day 2 and 3), during which TAT-TIJIP (10
mg/kg) or sterile ddH20 (control) was administered daily until the mice were sacrificed
(day 4). From each group (Untreated and TAT-TIJIP treated), the three mice that
recorded the largest total distance run (km) (Table 6.1) were selected for further
histological analysis.

Chapter Six Preliminary study to investigate the effects of TAT-TIJIP on reducing exercised induced myofibre necrosis in
vivo in mdx mice
99
Table 6.1: The relation between the voluntary distance ran to the amount of exercised induce myofibre necrosis. From the untreated and treated groups, 3 mice with the highest distances recorded were selected for histological analysis of %necrosis in the quadriceps.
Mouse Treatment Distance (km)
Necrosis (% of quadriceps)
UT-1 Untreated 0.20 not sampled UT-2 Untreated 5.75 4.15 UT-3 Untreated 0.01 not sampled UT-4 Untreated 4.70 5.52 UT-5 Untreated 4.73 11.46 UT-6 Untreated 0.00 not sampled
Average 2.56 7.04 TAT-TIJIP -1 TAT-TI JIP 2.25 1.76 TAT-TIJIP -2 TAT-TI JIP 8.00 9.56 TAT-TIJIP -3 TAT-TI JIP 2.00 not sampled TAT-TIJIP -4 TAT-TI JIP 2.10 not sampled TAT-TIJIP -5 TAT-TI JIP 1.90 not sampled TAT-TIJIP -6 TAT-TI JIP 1.63 not sampled TAT-TIJIP -7 TAT-TI JIP 0.00 not sampled TAT-TIJIP -8 TAT-TI JIP 2.83 6.78
Average 2.59 6.03 6.1.2 Histological analysis of the effects of TAT-TIJIP on reducing myofibre
necrosis in voluntary exercised mdx mice
Of the mice that ran, the right quadriceps muscle was sampled and histologically
examined; and the percentage area of muscle necrosis was then calculated (Figure 6.1).
No difference in the amount of myofibre necrosis was observed in the quadriceps of the
TAT-TIJIP treated mice, when compared to the untreated mice (Figure 6.1).

Chapter Six Preliminary study to investigate the effects of TAT-TIJIP on reducing exercised induced myofibre necrosis in
vivo in mdx mice
100
Figure 6.1: Percentage of myofibre necrosis in right quadriceps muscle of untreated and TAT-TIJIP treated voluntary exercised adult mdx mice. Adult 6 week old mdx mice that were administered with the JNK inhibitory peptide TAT-TIJIP (10 mg/kg body weight) 24 h prior to exposure to voluntary exercise, and then treated daily for a further 2 days during the voluntary exercise period show no significant decrease in muscle damage (necrosis) when compared to voluntary exercised mice that had been treated with ddH20 (Untreated controls; diluent for TAT-TIJIP). Results are mean values + SE of independent experiments indicated for each treatment (n = 3).

Chapter Six Preliminary study to investigate the effects of TAT-TIJIP on reducing exercised induced myofibre necrosis in
vivo in mdx mice
101
Discussion
In the present study it is difficult to determine whether it is of therapeutical benefit to
inhibit JNK by way of using pharmacological inhibitions of JNK (such as TAT-TIJIP)
in in vivo situations of muscle damage. As this was the first study to evaluate the
effectiveness of TAT-TIJIP on reducing myofibre necrosis in vivo, it was extremely
difficult to determine the dosage and duration of TAT-TIJIP treatment required to have
an effect when administered to an in vivo model. For this reason, the experimental
design was based on methodology presented in a study that tested the effectiveness of
JIP-1-HIV-TAT (a JNK peptide similar to TAT-TIJIP) on inhibiting JNK activity in
vivo when administered intraperitoneally in C57BL/KsJ-db/db obese diabetic mice
(Kaneto et al. 2004).
It is important to note that Kaneto et al. (2004) treated mice daily for 2 weeks with
10mg/kg JIP-1-HIV-TAT. As time and resources were limited, in the present study this
preliminary in vivo investigation involved 8 mice, treated daily for 3 days, with
10mg/ml TAT-TIJIP. It was envisaged that the histological analyses from these mice
would then serve as preliminary data from which a new experimental design could then
be modified. However, as discussed below, further studies are required before any
conclusions can be drawn as the effectiveness of TAT-TIJIP in inhibiting the activity of
JNK in vivo, and the effect this has on reducing exercised induced muscle necrosis in
mdx mice.
There are currently no published studies detailing the stability or specificity of TAT-
TIJIP when administered in vivo. The specificity of TIJIP (the inhibitory peptide
comment of TAT-TIJIP - see Section 1.5.4.2) has been tested in vitro (Barr et al. 2002)
and in tissue culture studies. Further, there are very few published studies which
describe using the TAT-TIJIP inhibitor. TAT-TIJIP has been applied to cultured BaF3
cells as part of study aimed at evaluating the contribution of intracellular tyrosine
residues of the granulocyte colony-stimulating factor receptor (Kendrick et al. 2004); in
neuronal cultures to determine the effectiveness of TAT-TIJIP in preventing neurotic
cell death following excitotoxic insult (Arthur et al. 2007); and most recently in T
lymphocytes to ascertain the involvement on JNK in activating the transcription factor
AP-1 and mediating the production of Th1 and Th2 cytokines (Melino et al. 2008). For

Chapter Six Preliminary study to investigate the effects of TAT-TIJIP on reducing exercised induced myofibre necrosis in
vivo in mdx mice
102
these tissue culture studies, it is suggested that TAT-TIJIP is specific and has the ability
to inhibit the JNK pathway; however this is yet to be confirmed in vivo.
As this was the first study to test TAT-TIJIP in vivo, the inhibitor was administered for
3 days to voluntary exercised 6 week old mdx mice, as these animals are the most
convenient model for screening potential compounds for treating patients with severe
muscle wasting such as that seen in DMD (Granchelli et al. 2000; Payne et al. 2006).
Although a functional form of the dystrophin protein is absent in the mdx mice, the
mutation does not result in the same large fibrotic lesions seen in human DMD (Gillis
1999) and the mice appear to be able to regenerate their skeletal muscle (Grounds et al.
2005), yet certain muscles (such as the diaphragm) do, however, display some of the
features seen in human DMD patients (O'Brien and Kunkel 2001). In addition, the
serum of mdx mice has been reported to contain high levels of muscle-derived pyruvate
kinase and creatine kinase, which was also seen in DMD (Bulfield et al. 1984).
The age at which the mdx mice are selected for muscle necrosis studies is of major
importance. As discussed in Section 1.3.2.1, histological examination of muscle
sampled from mdx mice that are younger than 3 weeks of age bears little resemblance to
that associated with the dystrophic phenotype. At around day 21, however, there is an
acute onset of muscle damage in limb and paraspinal muscles (Coulton et al. 1988;
McGeachie et al. 1993; Grounds and Torrisi 2004; Shavlakadze et al. 2004). In these
mice, it has been reported that the percentage of muscle necrosis in the tibialis anterior
muscle increases to approximately 20-40% in 3 week old mdx mice (Shavlakadze et al.
2004). This percentage then decreases to around 6% at approximately 6 weeks of age as
result of muscle regeneration (McGeachie et al. 1993). For this reason, voluntary
exercise induces a significant increase in quadriceps muscle necrosis in mice (Archer et
al. 2006; Hodgetts et al. 2006; Radley and Grounds 2006). For this to occur, however,
mice from each treatment group are ideally required to run similar distance so that any
changes to the amount of myofibre necrosis measured in the quadriceps can be
compared to the treatment, thus eliminating the possibility that these differences are a
direct result of the varying distances covered.
In this study at least half of the mice failed to run and for those that did, the distances
recorded were minimal (Table 6.1). From these results, it is therefore not possible to

Chapter Six Preliminary study to investigate the effects of TAT-TIJIP on reducing exercised induced myofibre necrosis in
vivo in mdx mice
103
determine whether JNK inhibition by TAT-TIJIP would have a beneficial effect on
reducing myofibre necrosis in situations of muscle damage and wasting, as the levels of
myofibre necrosis seen in both the TAT-TIJIP treated, and more importantly the
untreated exercised mice (Figure 6.1), were relatively low and resembled normal levels
of myofibre necrosis observed at 6 weeks of age (McGeachie et al. 1993).
These results clearly demonstrate the need for further studies to be performed to
ascertain the therapeutic potential of inhibiting the JNK pathways by using TAT-TIJIP,
or other pharmacological inhibitors of JNK, in in vivo situations of myofibre necrosis.

Chapter Seven General Discussion
104
Chapter Seven
General Discussion
Overview
It is widely accepted the cytokine TNF promotes skeletal muscle atrophy and
contributes to myofibre necrosis, whereas IGF-1 has a key role in maintaining skeletal
muscle mass. The implication of cross talk between TNF and IGF-1 in skeletal muscle,
however, is not well defined (Grounds et al. 2008) and the effect of administering both
TNF and IGF-1 to skeletal muscle fibres has not yet been reported previously.
The present series of experiments comprising this research project were undertaken in
an attempt to determine the mechanisms of by which TNF induces atrophy in
differentiated muscles cells; specifically the involvement of TNF activated JNK and its
role in mediating cross-talk between IGF-1 and TNF. The initial experiments,
established that immortalised and primary mouse skeletal myotube tissue culture models
(IGF-1) induced myotube hypertrophy, and TNF induced myotube atrophy (Chapters 3
and 4). This was then followed by experiments designed to: (i) assess and
morphologically quantify the physiological effects of IGF-1, TNF and combined IGF-
1/TNF treatments (Chapter 4); (ii) confirm that TNF induces the phosphorylation of
JNK in the TNF induced skeletal muscle atrophy model developed using C2C12 cells
(Chapter 5); and (iii) use JNK inhibitors to decipher the role of JNK in mediating TNF
induced myotube atrophy, with inhibition of JNK activity confirmed by assessing c-Jun
phosphorylation (Chapter 5). Preliminary in vivo studies with JNK inhibitors were also
undertaken (Chapter 6).
7.1 Establishment of myotube culture models of IGF-1 induced hypertrophy and
TNF mediated atrophy
The present study used the C2C12 mouse skeletal muscle cell line that forms well
differentiated myotubes in tissue culture (Lloyd et al. 2004) and primary cultures of
muscles from FVB mice (to further validate the results from the C2C12 studies). The

Chapter Seven General Discussion
105
studies confirmed the use of the (LONGTMR3IGF-I) analogue of IGF-1 to induce
significant hypertrophy in C2C12 myotubes, thus confirms previous studies (Florini et
al. 1996; Rommel et al. 1999; Rommel et al. 2001; Latres et al. 2005). Refinement of
the published protocols involved treating the myotubes at day 7, after the onset of
differentiation (as opposed to day 3), in order to use more mature myotubes. This
resulted in the establishment of an improved model of IGF-1 induced myotube
hypertrophy. The refined model uses C2C12 myotubes differentiated for 7 days, the
stage at which they are reported to be fully differentiated (Tolosa et al. 2005) and thus
more closely resemble the morphology of adult myofibres (Burattini et al. 2004).
The same 7 day C2C12 myotube model was then used to test the morphological effects
of 3 days of TNF treatment. A novel observation was statistically significant myotube
atrophy within 3 days after TNF (20 ng/ml) had been administered; this atrophic effect
of TNF alone has not previously been demonstrated. It is proposed that the more mature
status of the 7 day myotubes (beyond the steep growth phase) allowed the catabolic
effects of TNF to be manifested. The results using C2C12 myotubes were supported by
experiments using primary myotube cultures generated from young FVB mice, whereas
the same 3 day treatment with TNF (20 ng/ml) induced a statistically significant
decrease in mean myotube width.
Prior to the present research, there is only one report of C2C12 myotube atrophy when
TNF was administered in combination with IFN- γ (Dehoux et al. 2007). The
establishment of a novel tissue culture model of TNF induced myotube atrophy is a
powerful tool for future studies to investigate the molecular mechanism responsible for
this TNF mediated atrophy (without the complication of additional signalling pathways
activated by IFN- γ).
7.2 Combination treatments to investigate the effects of IGF-1 and TNF
Previously, the over-expression of IGF-1 in the skeletal muscles of transgenic
mdx/mIGF-1 mice (IGF:C2 mice) has been shown to significantly reduce myofibre
necrosis (Shavlakadze et al. 2004); a protective effect suggested as being the result of
increased protein synthesis in the muscles. Based on this hypothesis, the combination of
IGF-1 and TNF treatments were tested in C2C12 myotubes, and in muscle cell cultures
generated from transgenic IGF:C2 mice.

Chapter Seven General Discussion
106
In the C2C12 myotube cultures, the simultaneous treatment of IGF-1 (10 ng/ml) and
TNF (20 ng/ml), or the addition of IGF-1 before/after TNF treatment, had no effect on
the widths of the myotubes. These finding were further supported by studies using
IGF:C2 myotubes, where the addition of TNF again had no effect on myotube widths.
The results suggest, therefore, that these cytokines cancel out the effect of each other,
and thus TNF prevented IGF-1 induced hypertrophy, and IGF-1 prevented TNF
mediated atrophy.
7.3 Involvement of JNK in TNF mediated myotube atrophy and use of JNK
inhibitors
There is now strong evidence that TNF can inhibit IGF-1 expression (Frost et al. 2003),
by abrogating IGF-1 receptor signalling through the inhibition of tyrosine
phosphorylation of IRS-1 (Grounds et al. 2008). Previous research supports that the
inhibitory effect of TNF on IGF-1 is mediated by JNK (Broussard et al. 2003; Strle et
al. 2006). Detection of phosphorylated JNK, within 10 minutes of TNF treatment of
C2C12 myotubes, confirmed that TNF rapidly activates JNK (see Section 5.1.1). This is
a new contribution to the understanding of this process which has not been previously
published. To date, detection of TNF induced phosphorylated JNK has only been
reported in proliferating C2C12 myoblasts (Strle et al. 2006; Huang et al. 2007). Other
complementary studies in the Grounds laboratory using the same C2C12 7 day myotube
model, show that transcription of the atrogenes Atrogin-1 (MAFbx) and MuRF1 is
upregulated with 2-4 hours of TNF treatment, thus confirming the rapid upregulation of
genes responsible for the catabolic effects of TNF on myotubes (Chinzou 2009).
To determine if JNK activation played a critical role in TNF mediated atrophy, JNK
inhibitors were assessed for toxicity, and one (TAT-TIJIP) selected for testing in the
C2C12 and primary FVB myotube cultures (Chapter 5). Three JNK inhibitors were
evaluated; two that were ATP-competative (SP600125 and AS601245) and one that was
ATP-non-competitive (TAT-TIJIP). Both (SP600125 and AS601245) appeared toxic
when administered to day 7 C2C12 myotubes daily for 3 days whereas TAT-TIJIP was
not. The effect of TAT-TIJIP on the widths of the myotubes was therefore quantified in
the absence and presence of TNF (along with TAT controls). A striking effect was that
the inhibition of JNK activity by TAT-TIJIP prevented TNF mediated atrophy in all

Chapter Seven General Discussion
107
three myotube models; e.g. with C2C12 and primary myotube cultures generated from
FVB and IGF:C2 mice.
A somewhat unexpected finding was that the combined treatment of TAT-TIJIP and
TNF resulted in hypertrophy in both C2C12 and primary FVB and IGF:C2 myotubes. It
was instead hypothesised that inhibition of TNF/JNK mediated atrophy would result in
myotube widths resembling those of the untreated cultures, however, TAT-TIJIP
appears to be activating pathways involved in myotube hypertrophy. This raises many
interesting questions regarding the signalling mechanism responsible for this
hypertrophy, but resolution of this lies beyond the scope of the present research project.
However, the change in phosphorylation and activation state of IGF-1-mediated
signalling, that includes the IRS-1/PI3K/AKT/mTOR pathway as well as key regulators
of protein synthesis (such as p70S6K and 4EBP-1 - Rommel et al. 2001; Latres et al.
2005) in response to TNF + TAT-TIJIP, are of significant interest for future studies.
Although the present study could not optimise an assay to detect activated IRS-1 in
C2C12 cells (probably due to low levels of such signalling in the cell line used), an
alternative indirect approach was used to confirm the inhibition of JNK activity by
TAT-TIJIP based on phosphorylation and nuclear translocation of c-Jun; a downstream
target of phosphorylated JNK. Immunohistochemical analyses showed nuclear
localisation and phosphorylation of c-Jun in TNF treated myotubes, but not in cultures
pre-treated with TAT-TIJIP before TNF treatment, nor in the untreated control
myotubes. It has been shown TNF activates Atrogin-1 when administered to
differentiated C2C12 myotubes (Li et al. 2005) and, as discussed above, the Grounds
laboratory has also demonstrated rapid TNF mediated upregulation of both Atrogin 1
(MaFbx) and MuRF1 in C2C12 myotubes (unpublished data). Based on these findings,
the specific effects of TAT-TIJIP on transcription of these atrogens could be determined
in future experiments
These combined data describe a new cell culture model for TNF mediated myotube
atrophy, with the results presented in this thesis strongly supporting a role for JNK in
TNF mediated muscle atrophy. The results identify new aspects of cross-talk in
signalling between the TNF and IGF-1 pathways in myotubes and provides a strong

Chapter Seven General Discussion
108
basis for the use of JNK inhibitors for future pre-clinical in vivo studies in mouse
models of muscle disorders
7.1.4 In vivo studies: preliminary findings
The inconclusive results from the in vivo experiments in this thesis highlighted the
importance of refining many parameters, (e.g. dosage, voluntary exercise protocol)
before in vivo testing can be thoroughly investigated
The initial in vivo study was encouraging, because there were no apparent adverse
effects after treating mice daily for 3 days with 10 mg/kg TAT-TIJIP. There is little
information available on the ideal dosage and route of delivery of such JNK inhibitors
in animals and no toxicology studies performed to assess any potential toxic side effects
when administered in vivo. Therefore, the experimental methodology was arbitrarily
based on a study, which tested in vivo, an inhibitor similar to TAT-TIJIP (Kaneto et al.
2004). Due to time limitations, the issues of toxicity, optimal dosage and ideal delivery
route could not be addressed and this needs to be taken up future research. The potential
of JNK inhibitors to reduce muscle wasting in vivo is strongly supported by the present
tissue culture studies of myotubes, and is an area of considerable interest for future
research into the possible use of such inhibitors as therapeutic interventions for muscle
wasting disorders, such as DMD and cachexia.
Based on the findings presenting in this thesis, the promising results of TAT-TIJIP in
preventing TNF-induced myotube atrophy demonstrates the potential of this JNK
inhibitor to be of therapeutic benefit for muscle wasting disorders, such as cachexia and
DMD. Through future analysis of cell signalling pathways, and eventual in vivo testing,
the specificity and possibility of using TAT-TIJIP (and other JNK inhibitors) as
therapeutic agents will begin to be understood with the optimum result being
implemented as a potential therapy for muscle wasting disorders.

References
109
References
Adams, G. R. and Haddad, F. (1996). "The relationships among IGF-1, DNA content, and protein accumulation during skeletal muscle hypertrophy." J Appl Physiol 81(6): 2509-16.
Aguirre, V., Uchida, T., Yenush, L., Davis, R. and White, M. F. (2000). "The c-Jun NH(2)-terminal kinase promotes insulin resistance during association with insulin receptor substrate-1 and phosphorylation of Ser(307)." J Biol Chem 275(12): 9047-54.
Aguirre, V., Werner, E. D., Giraud, J., Lee, Y. H., Shoelson, S. E. and White, M. F. (2002). "Phosphorylation of Ser307 in insulin receptor substrate-1 blocks interactions with the insulin receptor and inhibits insulin action." J Biol Chem 277(2): 1531-7.
Alessi, D. R., James, S. R., Downes, C. P., Holmes, A. B., Gaffney, P. R., Reese, C. B. and Cohen, P. (1997). "Characterization of a 3-phosphoinositide-dependent protein kinase which phosphorylates and activates protein kinase Balpha." Curr Biol 7(4): 261-9.
Archer, J. D., Vargas, C. C. and Anderson, J. E. (2006). "Persistent and improved functional gain in mdx dystrophic mice after treatment with L-arginine and deflazacort." Faseb J 20(6): 738-40.
Argiles, J. M., Lopez-Soriano, F. J. and Busquets, S. (2007). "Mechanisms to explain wasting of muscle and fat in cancer cachexia." Curr Opin Support Palliat Care 1(4): 293-8.
Argiles, J. M., Lopez-Soriano, J., Busquets, S. and Lopez-Soriano, F. J. (1997). "Journey from cachexia to obesity by TNF." Faseb J 11(10): 743-51.
Argiles, J. M., Meijsing, S. H., Pallares-Trujillo, J., Guirao, X. and Lopez-Soriano, F. J. (2001). "Cancer cachexia: a therapeutic approach." Med Res Rev 21(1): 83-101.
Arthur, P. G., Grounds, M. D. and Shavlakadze, T. (2008). "Oxidative stress as a therapeutic target during muscle wasting: considering the complex interactions." Curr Opin Clin Nutr Metab Care 11(4): 408-16.
Arthur, P. G., Matich, G. P., Pang, W. W., Yu, D. Y. and Bogoyevitch, M. A. (2007). "Necrotic death of neurons following an excitotoxic insult is prevented by a peptide inhibitor of c-jun N-terminal kinase." J Neurochem 102(1): 65-76.
Bach, J. R., Ishikawa, Y. and Kim, H. (1997). "Prevention of pulmonary morbidity for patients with Duchenne muscular dystrophy." Chest 112(4): 1024-1028.
Bain, J., McLauchlan, H., Elliott, M. and Cohen, P. (2003). "The specificities of protein kinase inhibitors: an update." Biochem J 371(Pt 1): 199-204.
Ballard, F. J., Francis, G. L., Ross, M., Bagley, C. J., May, B. and Wallace, J. C. (1987). "Natural and synthetic forms of insulin-like growth factor-1 (IGF-1) and the potent derivative, destripeptide IGF-1: Biological activities and receptor binding." Biochemical and Biophysical Research Communications 149(2): 398.

References
110
Ballard, F. J., Wallace, J. C., Francis, G. L., Read, L. C. and Tomas, F. M. (1996). "Des(1-3)IGF-I: a truncated form of insulin-like growth factor-I." Int J Biochem Cell Biol 28(10): 1085-7.
Bannister, L H., Williams, P. L., Berry, M. M. (eds) (1995). 'Grey's Anatomy: 38th Edition', Churchill Livingstone, New York. P 737
Bansal, D., Miyake, K., Vogel, S. S., Groh, S., Chen, C. C., Williamson, R., McNeil, P. L. and Campbell, K. P. (2003). "Defective membrane repair in dysferlin-deficient muscular dystrophy." Nature 423(6936): 168-72.
Baracos, V. E., DeVivo, C., Hoyle, D. H. and Goldberg, A. L. (1995). "Activation of the ATP-ubiquitin-proteasome pathway in skeletal muscle of cachectic rats bearing a hepatoma." Am J Physiol 268(5 Pt 1): E996-1006.
Barr, R. K., Boehm, I., Attwood, P. V., Watt, P. M. and Bogoyevitch, M. A. (2004). "The critical features and the mechanism of inhibition of a kinase interaction motif-based peptide inhibitor of JNK." J Biol Chem 279(35): 36327-38.
Barr, R. K. and Bogoyevitch, M. A. (2001). "The c-Jun N-terminal protein kinase family of mitogen-activated protein kinases (JNK MAPKs)." Int J Biochem Cell Biol 33(11): 1047-63.
Barr, R. K., Hopkins, R. M., Watt, P. M. and Bogoyevitch, M. A. (2004). "Reverse two-hybrid screening identifies residues of JNK required for interaction with the kinase interaction motif of JNK-interacting protein-1." J Biol Chem 279(41): 43178-89.
Barr, R. K., Kendrick, T. S. and Bogoyevitch, M. A. (2002). "Identification of the critical features of a small peptide inhibitor of JNK activity." J Biol Chem 277(13): 10987-97.
Barton, E. R., Morris, L., Musaro, A., Rosenthal, N. and Sweeney, H. L. (2002). "Muscle-specific expression of insulin-like growth factor I counters muscle decline in mdx mice." J Cell Biol 157(1): 137-48.
Bell, G. I., Stempien, M. M., Fong, N. M. and Rall, L. B. (1986). "Sequences of liver cDNAs encoding two different mouse insulin-like growth factor I precursors." Nucleic Acids Res 14(20): 7873-82.
Bennett, B. L., Sasaki, D. T., Murray, B. W., O'Leary, E. C., Sakata, S. T., Xu, W., Leisten, J. C., Motiwala, A., Pierce, S., Satoh, Y., Bhagwat, S. S., Manning, A. M. and Anderson, D. W. (2001). "SP600125, an anthrapyrazolone inhibitor of Jun N-terminal kinase." Proc Natl Acad Sci U S A 98(24): 13681-6.
Bertoni, C., Morris, G. E. and Rando, T. A. (2005). "Strand bias in oligonucleotide-mediated dystrophin gene editing." Hum Mol Genet 14(2): 221-33.
Beutler, B. and Cerami, A. (1988). "Tumor necrosis, cachexia, shock, and inflammation: a common mediator." Annu Rev Biochem 57: 505-18.

References
111
Beutler, B., Greenwald, D., Hulmes, J. D., Chang, M., Pan, Y. C., Mathison, J., Ulevitch, R. and Cerami, A. (1985). "Identity of tumour necrosis factor and the macrophage-secreted factor cachectin." Nature 316(6028): 552-4.
Blake, D. J., Weir, A., Newey, S. E. and Davies, K. E. (2002). "Function and genetics of dystrophin and dystrophin-related proteins in muscle." Physiol Rev 82(2): 291-329.
Bodine, S. C., Stitt, T. N., Gonzalez, M., Kline, W. O., Stover, G. L., Bauerlein, R., Zlotchenko, E., Scrimgeour, A., Lawrence, J. C., Glass, D. J. and Yancopoulos, G. D. (2001). "Akt/mTOR pathway is a crucial regulator of skeletal muscle hypertrophy and can prevent muscle atrophy in vivo." Nat Cell Biol 3(11): 1014-9.
Bogoyevitch, M. A. (2005). "Therapeutic promise of JNK ATP-noncompetitive inhibitors." Trends Mol Med 11(5): 232-9.
Bogoyevitch, M. A. and Arthur, P. G. (2008). "Inhibitors of c-Jun N-terminal kinases: JuNK no more?" Biochim Biophys Acta 1784(1): 76-93.
Bogoyevitch, M. A., Barr, R. K. and Ketterman, A. J. (2005). "Peptide inhibitors of protein kinases-discovery, characterisation and use." Biochim Biophys Acta.
Bogoyevitch, M. A., Boehm, I., Oakley, A., Ketterman, A. J. and Barr, R. K. (2004). "Targeting the JNK MAPK cascade for inhibition: basic science and therapeutic potential." Biochim Biophys Acta 1697(1-2): 89-101.
Boonyarom, O. and Inui, K. (2006). "Atrophy and hypertrophy of skeletal muscles: structural and functional aspects." Acta Physiol (Oxf) 188(2): 77-89.
Borsello, T., Clarke, P. G., Hirt, L., Vercelli, A., Repici, M., Schorderet, D. F., Bogousslavsky, J. and Bonny, C. (2003). "A peptide inhibitor of c-Jun N-terminal kinase protects against excitotoxicity and cerebral ischemia." Nat Med 9(9): 1180-6.
Broussard, S. R., McCusker, R. H., Novakofski, J. E., Strle, K., Shen, W. H., Johnson, R. W., Dantzer, R. and Kelley, K. W. (2004). "IL-1beta impairs insulin-like growth factor i-induced differentiation and downstream activation signals of the insulin-like growth factor i receptor in myoblasts." J Immunol 172(12): 7713-20.
Broussard, S. R., McCusker, R. H., Novakofski, J. E., Strle, K., Shen, W. H., Johnson, R. W., Freund, G. G., Dantzer, R. and Kelley, K. W. (2003). "Cytokine-hormone interactions: tumor necrosis factor alpha impairs biologic activity and downstream activation signals of the insulin-like growth factor I receptor in myoblasts." Endocrinology 144(7): 2988-96.
Brunet, A., Bonni, A., Zigmond, M. J., Lin, M. Z., Juo, P., Hu, L. S., Anderson, M. J., Arden, K. C., Blenis, J. and Greenberg, M. E. (1999). "Akt promotes cell survival by phosphorylating and inhibiting a Forkhead transcription factor." Cell 96(6): 857-68.
Bulfield, G., Siller, W. G., Wight, P. A. and Moore, K. J. (1984). "X chromosome-linked muscular dystrophy (mdx) in the mouse." Proc Natl Acad Sci U S A 81(4): 1189-92.

References
112
Burattini, S., Ferri, P., Battistelli, M., Curci, R., Luchetti, F. and Falcieri, E. (2004). "C2C12 murine myoblasts as a model of skeletal muscle development: morpho-functional characterization." Eur J Histochem 48(3): 223-33.
Butterfield, L., Storey, B., Maas, L. and Heasley, L. E. (1997). "c-Jun NH2-terminal kinase regulation of the apoptotic response of small cell lung cancer cells to ultraviolet radiation." J Biol Chem 272(15): 10110-6.
Carboni, S., Boschert, U., Gaillard, P., Gotteland, J. P., Gillon, J. Y. and Vitte, P. A. (2007). "AS601245, a c-Jun NH2-terminal kinase (JNK) inhibitor, reduces axon//dendrite damage and cognitive deficits after global cerebral ischaemia in gerbils." Br J Pharmacol 153(1): 157.
Carboni, S., Hiver, A., Szyndralewiez, C., Gaillard, P., Gotteland, J. P. and Vitte, P. A. (2004). "AS601245 (1,3-benzothiazol-2-yl (2-[[2-(3-pyridinyl) ethyl] amino]-4 pyrimidinyl) acetonitrile): a c-Jun NH2-terminal protein kinase inhibitor with neuroprotective properties." J Pharmacol Exp Ther 310(1): 25-32.
Carlsson-Skwirut, C., Lake, M., Hartmanis, M., Hall, K. and Sara, V. R. (1989). "A comparison of the biological activity of the recombinant intact and truncated insulin-like growth factor 1 (IGF-1)." Biochim Biophys Acta 1011(2-3): 192-7.
Carswell, E. A., Old, L. J., Kassel, R. L., Green, S., Fiore, N. and Williamson, B. (1975). "An endotoxin-induced serum factor that causes necrosis of tumors." Proc Natl Acad Sci U S A 72(9): 3666-70.
Chapman, V. M., Miller, D. R., Armstrong, D. and Caskey, C. T. (1989). "Recovery of induced mutations for X chromosome-linked muscular dystrophy in mice." Proc Natl Acad Sci U S A 86(4): 1292-6.
Chen, S., Bingwen, J and Li, Y-P. (2007). " TNF-α regulates myogenesis and muscle regeneration by activating p38 MAPK." Am J Physiol Cell Physiol 292(5): C1660-71.
Cheng, H. L. and Feldman, E. L. (1998). "Bidirectional regulation of p38 kinase and c-Jun N-terminal protein kinase by insulin-like growth factor-I." J Biol Chem 273(23): 14560-5.
Chinzou, T (2009). Role of Reactive oxygen species (ROS) and Tumor necrosis factor (TNF) in skeletal muscle atrophy [dissertation], Anatomy and Human Biology, University of Western Australia.
Clark, S. F., Martin, S., Carozzi, A. J., Hill, M. M. and James, D. E. (1998). "Intracellular localization of phosphatidylinositide 3-kinase and insulin receptor substrate-1 in adipocytes: potential involvement of a membrane skeleton." J Cell Biol 140(5): 1211-25.
Coletti, D., Yang, E., Marazzi, G. and Sassoon, D. (2002). "TNF alpha inhibits skeletal myogenesis through a PW1-dependent pathway by recruitment of caspase pathways." Embo J 21(4): 631-42.

References
113
Coolican, S. A., Samuel, D. S., Ewton, D. Z., McWade, F. J. and Florini, J. R. (1997). "The mitogenic and myogenic actions of insulin-like growth factors utilize distinct signaling pathways." J Biol Chem 272(10): 6653-62.
Coppack, S. W. (2001). "Pro-inflammatory cytokines and adipose tissue." Proc Nutr Soc 60(3): 349-56.
Coulton, G. R., Morgan, J. E., Partridge, T. A. and Sloper, J. C. (1988). "The mdx mouse skeletal muscle myopathy: I. A histological, morphometric and biochemical investigation." Neuropathol Appl Neurobiol 14(1): 53-70.
Cuenda, A. and Cohen, P. (1999). "Stress-activated protein kinase-2/p38 and a rapamycin-sensitive pathway are required for C2C12 myogenesis." J Biol Chem 274(7): 4341-6.
Darzynkiewicz, Z., Williamson, B., Carswell, E. A. and Old, L. J. (1984). "Cell cycle-specific effects of tumor necrosis factor." Cancer Res 44(1): 83-90.
Davies, K. E. and Grounds, M. D. (2007). "Modified patient stem cells as prelude to autologous treatment of muscular dystrophy." Cell Stem Cell 1(6): 595-6.
Dehoux, M., Gobier, C., Lause, P., Bertrand, L., Ketelslegers, J. M. and Thissen, J. P. (2007). "IGF-I does not prevent myotube atrophy caused by proinflammatory cytokines despite activation of Akt/Foxo and GSK-3beta pathways and inhibition of atrogin-1 mRNA." Am J Physiol Endocrinol Metab 292(1): E145-50.
del Aguila, L. F., Claffey, K. P. and Kirwan, J. P. (1999). "TNF-alpha impairs insulin signaling and insulin stimulation of glucose uptake in C2C12 muscle cells." Am J Physiol 276(5 Pt 1): E849-55.
Dempsey, P. W., Doyle, S. E., He, J. Q. and Cheng, G. (2003). "The signaling adaptors and pathways activated by TNF superfamily." Cytokine Growth Factor Rev 14(3-4): 193-209.
Denecker, G., Vercammen, D., Declercq, W. and Vandenabeele, P. (2001). "Apoptotic and necrotic cell death induced by death domain receptors." Cell Mol Life Sci 58(3): 356-70.
Derijard, B., Hibi, M., Wu, I. H., Barrett, T., Su, B., Deng, T., Karin, M. and Davis, R. J. (1994). "JNK1: a protein kinase stimulated by UV light and Ha-Ras that binds and phosphorylates the c-Jun activation domain." Cell 76(6): 1025-37.
DeVol, D. L., Rotwein, P., Sadow, J. L., Novakofski, J. and Bechtel, P. J. (1990). "Activation of insulin-like growth factor gene expression during work-induced skeletal muscle growth." Am J Physiol 259(1 Pt 1): E89-95.
Dupont-Versteegden, E. E., McCarter, R. J. and Katz, M. S. (1994). "Voluntary exercise decreases progression of muscular dystrophy in diaphragm of mdx mice." J Appl Physiol 77(4): 1736-41.
Efthimiou, P. (2006). "Tumor necrosis factor-alpha in inflammatory myopathies: pathophysiology and therapeutic implications." Semin Arthritis Rheum 36(3): 168-72.

References
114
Eley, H. L., Russell, S. T. and Tisdale, M. J. (2008). "Attenuation of depression of muscle protein synthesis induced by lipopolysaccharide, tumor necrosis factor, and angiotensin II by beta-hydroxy-beta-methylbutyrate." Am J Physiol Endocrinol Metab 295(6): E1409-16.
Eley, H. L., Russell, S. T. and Tisdale, M. J. (2008). "Mechanism of attenuation of muscle protein degradation induced by tumor necrosis factor-alpha and angiotensin II by beta-hydroxy-beta-methylbutyrate." Am J Physiol Endocrinol Metab 295(6): E1417-26.
Emery, A. E. (1991). "Population frequencies of inherited neuromuscular diseases--a world survey." Neuromuscul Disord 1(1): 19-29.
Emery, A. E. (2002). "The muscular dystrophies." Lancet 359(9307): 687-95.
Engert, J. C., Berglund, E. B. and Rosenthal, N. (1996). "Proliferation precedes differentiation in IGF-I-stimulated myogenesis." J Cell Biol 135(2): 431-40.
Evans, W. J., Morley, J. E., Argiles, J., Bales, C., Baracos, V., Guttridge, D., Jatoi, A., Kalantar-Zadeh, K., Lochs, H., Mantovani, G., Marks, D., Mitch, W. E., Muscaritoli, M., Najand, A., Ponikowski, P., Rossi Fanelli, F., Schambelan, M., Schols, A., Schuster, M., Thomas, D., Wolfe, R. and Anker, S. D. (2008). "Cachexia: a new definition." Clin Nutr 27(6): 793-9.
Fang, C. H., Li, B. G., Sun, X. and Hasselgren, P. O. (2000). "Insulin-like growth factor I reduces ubiquitin and ubiquitin-conjugating enzyme gene expression but does not inhibit muscle proteolysis in septic rats." Endocrinology 141(8): 2743-51.
Fanzani, A., Colombo, F., Giuliani, R., Preti, A. and Marchesini, S. (2006). "Insulin-like growth factor 1 signaling regulates cytosolic sialidase Neu2 expression during myoblast differentiation and hypertrophy." Febs J 273(16): 3709-21.
Fernandez-Celemin, L., Pasko, N., Blomart, V. and Thissen, J. P. (2002). "Inhibition of muscle insulin-like growth factor I expression by tumor necrosis factor-alpha." Am J Physiol Endocrinol Metab 283(6): E1279-90.
Ferrandi, C., Ballerio, R., Gaillard, P., Giachetti, C., Carboni, S., Vitte, P. A., Gotteland, J. P. and Cirillo, R. (2004). "Inhibition of c-Jun N-terminal kinase decreases cardiomyocyte apoptosis and infarct size after myocardial ischemia and reperfusion in anaesthetized rats." Br J Pharmacol 142(6): 953-60.
Florini, J. R., Ewton, D. Z. and Coolican, S. A. (1996). "Growth hormone and the insulin-like growth factor system in myogenesis." Endocr Rev 17(5): 481-517.
Florini, J. R. and Magri, K. A. (1989). "Effects of growth factors on myogenic differentiation." Am J Physiol 256(4 Pt 1): C701-11.
Foulstone, E. J., Huser, C., Crown, A. L., Holly, J. M. and Stewart, C. E. (2004). "Differential signalling mechanisms predisposing primary human skeletal muscle cells to altered proliferation and differentiation: roles of IGF-I and TNFalpha." Exp Cell Res 294(1): 223-35.

References
115
Foulstone, E. J., Meadows, K. A., Holly, J. M. and Stewart, C. E. (2001). "Insulin-like growth factors (IGF-I and IGF-II) inhibit C2 skeletal myoblast differentiation and enhance TNF alpha-induced apoptosis." J Cell Physiol 189(2): 207-15.
Francis, G. L., Read, L. C., Ballard, F. J., Bagley, C. J., Upton, F. M., Gravestock, P. M. and Wallace, J. C. (1986). "Purification and partial sequence analysis of insulin-like growth factor-1 from bovine colostrum." Biochem J 233(1): 207-13.
Francis, G. L., Ross, M., Ballard, F. J., Milner, S. J., Senn, C., McNeil, K. A., Wallace, J. C., King, R. and Wells, J. R. (1992). "Novel recombinant fusion protein analogues of insulin-like growth factor (IGF)-I indicate the relative importance of IGF-binding protein and receptor binding for enhanced biological potency." J Mol Endocrinol 8(3): 213-23.
Francis, G. L., Upton, F. M., Ballard, F. J., McNeil, K. A. and Wallace, J. C. (1988). "Insulin-like growth factors 1 and 2 in bovine colostrum. Sequences and biological activities compared with those of a potent truncated form." Biochem J 251(1): 95-103.
Froesch, E. R., Schmid, C., Schwander, J. and Zapf, J. (1985). "Actions of insulin-like growth factors." Annu Rev Physiol 47: 443-67.
Frost, R. A., Nystrom, G. J. and Lang, C. H. (2003). "Tumor necrosis factor-alpha decreases insulin-like growth factor-I messenger ribonucleic acid expression in C2C12 myoblasts via a Jun N-terminal kinase pathway." Endocrinology 144(5): 1770-9.
Gaillard, P., Jeanclaude-Etter, I., Ardissone, V., Arkinstall, S., Cambet, Y., Camps, M., Chabert, C., Church, D., Cirillo, R., Gretener, D., Halazy, S., Nichols, A., Szyndralewiez, C., Vitte, P. A. and Gotteland, J. P. (2005). "Design and synthesis of the first generation of novel potent, selective, and in vivo active (benzothiazol-2-yl)acetonitrile inhibitors of the c-Jun N-terminal kinase." J Med Chem 48(14): 4596-607.
Gelman, M. S. and Prives, J. M. (1996). "Arrest of Subunit Folding and Assembly of Nicotinic Acetylcholine Receptors in Cultured Muscle Cells by Dithiothreitol." J. Biol. Chem. 271(18): 10709-10714.
Gillis, J. M. (1999). "Understanding dystrophinopathies: an inventory of the structural and functional consequences of the absence of dystrophin in muscles of the mdx mouse." J Muscle Res Cell Motil 20(7): 605-25.
Glass, D. J. (2003). "Signalling pathways that mediate skeletal muscle hypertrophy and atrophy." Nat Cell Biol 5(2): 87-90.
Glass, D. J. (2005). "Skeletal muscle hypertrophy and atrophy signaling pathways." Int J Biochem Cell Biol 37(10): 1974-84.
Goldspink, D. F. (1991). "Exercise-related changes in protein turnover in mammalian striated muscle." J Exp Biol 160: 127-48.
Gonzalez-Cadavid, N. F., Taylor, W. E., Yarasheski, K., Sinha-Hikim, I., Ma, K., Ezzat, S., Shen, R., Lalani, R., Asa, S., Mamita, M., Nair, G., Arver, S. and Bhasin, S. (1998).

References
116
"Organization of the human myostatin gene and expression in healthy men and HIV-infected men with muscle wasting." Proc Natl Acad Sci U S A 95(25): 14938-43.
Granchelli, J. A., Pollina, C. and Hudecki, M. S. (2000). "Pre-clinical screening of drugs using the mdx mouse." Neuromuscul Disord 10(4-5): 235-9.
Grounds, M. D. (2002). "Reasons for the degeneration of ageing skeletal muscle: a central role for IGF-1 signalling." Biogerontology 3(1-2): 19-24.
Grounds, M. D. and Davies, K. E. (2007). "The allure of stem cell therapy for muscular dystrophy." Neuromuscul Disord 17(3): 206-8.
Grounds, M. D., Davies, M., Torrisi, J., Shavlakadze, T., White, J. and Hodgetts, S. (2005). "Silencing TNFalpha activity by using Remicade or Enbrel blocks inflammation in whole muscle grafts: an in vivo bioassay to assess the efficacy of anti-cytokine drugs in mice." Cell Tissue Res 320(3): 509-15.
Grounds, M. D., Radley, H. G., Gebski, B. G., Bogoyevitch, M. A. and Shavlakadze, T. (2008). "Implications Of Cross-Talk Between Tumour Necrosis Factor And Insulin-Like Growth Factor-1 Signalling In Skeletal Muscle." Clin Exp Pharmacol Physiol.
Grounds, M. D., Radley, H. G., Lynch, G. S., Nagaraju, K. and De Luca, A. (2008). "Towards developing standard operating procedures for pre-clinical testing in the mdx mouse model of Duchenne muscular dystrophy." Neurobiol Dis 31(1): 1-19.
Grounds, M. D. and Torrisi, J. (2004). "Anti-TNFalpha (Remicade) therapy protects dystrophic skeletal muscle from necrosis." Faseb J 18(6): 676-82.
Gupta, S., Barrett, T., Whitmarsh, A. J., Cavanagh, J., Sluss, H. K., Derijard, B. and Davis, R. J. (1996). "Selective interaction of JNK protein kinase isoforms with transcription factors." Embo J 15(11): 2760-70.
Guttridge, D. C., Mayo, M. W., Madrid, L. V., Wang, C. Y. and Baldwin, A. S., Jr. (2000). "NF-kappaB-induced loss of MyoD messenger RNA: possible role in muscle decay and cachexia." Science 289(5488): 2363-6.
Han, Z., Boyle, D. L., Chang, L., Bennett, B., Karin, M., Yang, L., Manning, A. M. and Firestein, G. S. (2001). "c-Jun N-terminal kinase is required for metalloproteinase expression and joint destruction in inflammatory arthritis." J Clin Invest 108(1): 73-81.
Hayman, M. W., Smith, K. H., Cameron, N. R. and Przyborski, S. A. (2005). "Growth of human stem cell-derived neurons on solid three-dimensional polymers." J Biochem Biophys Methods 62(3): 231-40.
Heemskerk, H. A., de Winter, C. L., de Kimpe, S. J., van Kuik-Romeijn, P., Heuvelmans, N., Platenburg, G. J., van Ommen, G. J., van Deutekom, J. C. and Aartsma-Rus, A. (2009). "In vivo comparison of 2'-O-methyl phosphorothioate and morpholino antisense oligonucleotides for Duchenne muscular dystrophy exon skipping." J Gene Med 11(3): 257-66.

References
117
Hiratani, K., Haruta, T., Tani, A., Kawahara, J., Usui, I. and Kobayashi, M. (2005). "Roles of mTOR and JNK in serine phosphorylation, translocation, and degradation of IRS-1." Biochem Biophys Res Commun 335(3): 836-42.
Hnia, K., Hugon, G., Rivier, F., Masmoudi, A., Mercier, J. and Mornet, D. (2007). "Modulation of p38 mitogen-activated protein kinase cascade and metalloproteinase activity in diaphragm muscle in response to free radical scavenger administration in dystrophin-deficient Mdx mice." Am J Pathol 170(2): 633-43.
Hodgetts, S., Radley, H., Davies, M. and Grounds, M. D. (2006). "Reduced necrosis of dystrophic muscle by depletion of host neutrophils, or blocking TNFalpha function with Etanercept in mdx mice." Neuromuscul Disord 16(9-10): 591-602.
Hoffman, E. P., Brown Jr, R. H. and Kunkel, L. M. (1987). "Dystrophin: The Protein Product of the Duchenne Muscular Dystrophy Locus." Cell 51: 919-928.
Hoffmann, M. K., Oettgen, H. F., Old, L. J., Mittler, R. S. and Hammerling, U. (1978). "Induction and immunological properties of tumor necrosis factor." J Reticuloendothel Soc 23(4): 307-19.
Horsley, V., Jansen, K. M., Mills, S. T. and Pavlath, G. K. (2003). "IL-4 acts as a myoblast recruitment factor during mammalian muscle growth." Cell 113(4): 483-94.
Huang, Z., Chen, D., Zhang, K., Yu, B., Chen, X. and Meng, J. (2007). "Regulation of myostatin signaling by c-Jun N-terminal kinase in C2C12 cells." Cell Signal 19(11): 2286-95.
Hughes, P., Marshall, D., Reid, Y., Parkes, H. and Gelber, C. (2007). "The costs of using unauthenticated, over-passaged cell lines: how much more data do we need?" Biotechniques 43(5): 575, 577-8, 581-2 passim.
Hwa, V., Oh, Y. and Rosenfeld, R. G. (1999). "Insulin-like growth factor binding proteins: a proposed superfamily." Acta Paediatr Suppl 88(428): 37-45.
Jackman, R. W. and Kandarian, S. C. (2004). "The molecular basis of skeletal muscle atrophy." Am J Physiol Cell Physiol 287(4): C834-43.
Jacobs, S., Kull, F. C., Jr., Earp, H. S., Svoboda, M. E., Van Wyk, J. J. and Cuatrecasas, P. (1983). "Somatomedin-C stimulates the phosphorylation of the beta-subunit of its own receptor." J Biol Chem 258(16): 9581-4.
Kaneto, H., Nakatani, Y., Miyatsuka, T., Kawamori, D., Matsuoka, T. A., Matsuhisa, M., Kajimoto, Y., Ichijo, H., Yamasaki, Y. and Hori, M. (2004). "Possible novel therapy for diabetes with cell-permeable JNK-inhibitory peptide." Nat Med 10(10): 1128-32.
Karin, M. and Gallagher, E. (2009). "TNFR signaling: ubiquitin-conjugated TRAFfic signals control stop-and-go for MAPK signaling complexes." Immunol Rev 228(1): 225-40.

References
118
Keller, S. R., Lamphere, L., Lavan, B. E., Kuhne, M. R. and Lienhard, G. E. (1993). "Insulin and IGF-I signaling through the insulin receptor substrate 1." Mol Reprod Dev 35(4): 346-51; discussion 351-2.
Kendrick, T. S., Lipscombe, R. J., Rausch, O., Nicholson, S. E., Layton, J. E., Goldie-Cregan, L. C. and Bogoyevitch, M. A. (2004). "Contribution of the membrane-distal tyrosine in intracellular signaling by the granulocyte colony-stimulating factor receptor." J Biol Chem 279(1): 326-40.
Kolodziejczyk, S. M., Walsh, G. S., Balazsi, K., Seale, P., Sandoz, J., Hierlihy, A. M., Rudnicki, M. A., Chamberlain, J. S., Miller, F. D. and Megeney, L. A. (2001). "Activation of JNK1 contributes to dystrophic muscle pathogenesis." Curr Biol 11(16): 1278-82.
Kumagae, Y., Zhang, Y., Kim, O. J. and Miller, C. A. (1999). "Human c-Jun N-terminal kinase expression and activation in the nervous system." Brain Res Mol Brain Res 67(1): 10-7.
Kuru, S., Inukai, A., Kato, T., Liang, Y., Kimura, S. and Sobue, G. (2003). "Expression of tumor necrosis factor-alpha in regenerating muscle fibers in inflammatory and non-inflammatory myopathies." Acta Neuropathol (Berl) 105(3): 217-24.
Kyriakis, J. M. and Avruch, J. (2001). "Mammalian mitogen-activated protein kinase signal transduction pathways activated by stress and inflammation." Physiol Rev 81(2): 807-69.
Lang, J. M., Esser, K. A. and Dupont-Versteegden, E. E. (2004). "Altered activity of signaling pathways in diaphragm and tibialis anterior muscle of dystrophic mice." Exp Biol Med (Maywood) 229(6): 503-11.
Laster, S. M., Wood, J. G. and Gooding, L. R. (1988). "Tumor necrosis factor can induce both apoptic and necrotic forms of cell lysis." J Immunol 141(8): 2629-34.
Latres, E., Amini, A. R., Amini, A. A., Griffiths, J., Martin, F. J., Wei, Y., Lin, H. C., Yancopoulos, G. D. and Glass, D. J. (2005). "Insulin-like growth factor-1 (IGF-1) inversely regulates atrophy-induced genes via the phosphatidylinositol 3-kinase/Akt/mammalian target of rapamycin (PI3K/Akt/mTOR) pathway." J Biol Chem 280(4): 2737-44.
Lawson, M. A. and Purslow, P. P. (2000). "Differentiation of myoblasts in serum-free media: effects of modified media are cell line-specific." Cells Tissues Organs 167(2-3): 130-7.
Le Roith, D., Bondy, C., Yakar, S., Liu, J. L. and Butler, A. (2001). "The somatomedin hypothesis: 2001." Endocr Rev 22(1): 53-74.
Lecker, S. H., Jagoe, R. T., Gilbert, A., Gomes, M., Baracos, V., Bailey, J., Price, S. R., Mitch, W. E. and Goldberg, A. L. (2004). "Multiple types of skeletal muscle atrophy involve a common program of changes in gene expression." Faseb J 18(1): 39-51.
Li, B. G., Hasselgren, P. O. and Fang, C. H. (2005). "Insulin-like growth factor-I inhibits dexamethasone-induced proteolysis in cultured L6 myotubes through

References
119
PI3K/Akt/GSK-3beta and PI3K/Akt/mTOR-dependent mechanisms." Int J Biochem Cell Biol 37(10): 2207-16.
Li, D., Long, C., Yue, Y. and Duan, D. (2009). "Sub-physiological sarcoglycan expression contributes to compensatory muscle protection in mdx mice." Hum Mol Genet 18(7): 1209-20.
Li, Y.-P., Chen, Y., John, J., Moylan, J., Jin, B., Mann, D. L. and Reid, M. B. (2005). "TNF-{alpha} acts via p38 MAPK to stimulate expression of the ubiquitin ligase atrogin1/MAFbx in skeletal muscle." FASEB J. 19(3): 362-370.
Li, Y. P. and Reid, M. B. (2000). "NF-kappaB mediates the protein loss induced by TNF-alpha in differentiated skeletal muscle myotubes." Am J Physiol Regul Integr Comp Physiol 279(4): R1165-70.
Lloyd, C. M., Berendse, M., Lloyd, D. G., Schevzov, G. and Grounds, M. D. (2004). "A novel role for non-muscle gamma-actin in skeletal muscle sarcomere assembly." Exp Cell Res 297(1): 82-96.
Lundberg, I., Brengman, J. M. and Engel, A. G. (1995). "Analysis of cytokine expression in muscle in inflammatory myopathies, Duchenne dystrophy, and non-weak controls." J Neuroimmunol 63(1): 9-16.
Maguire, K., Suzuki, T., DiMatteo, D., Parekh-Olmedo, H. and Kmiec, E. (2009). "Genetic correction of splice site mutation in purified and enriched myoblasts isolated from mdx5cv mice." BMC Mol Biol 10: 15.
Matsui, T., Nagoshi, T. and Rosenzweig, A. (2003). "Akt and PI 3-kinase signaling in cardiomyocyte hypertrophy and survival." Cell Cycle 2(3): 220-3.
McGeachie, J. K., Grounds, M. D., Partridge, T. A. and Morgan, J. E. (1993). "Age-related changes in replication of myogenic cells in mdx mice: quantitative autoradiographic studies." J Neurol Sci 119(2): 169-79.
Meadows, K. A., Holly, J. M. and Stewart, C. E. (2000). "Tumor necrosis factor-alpha-induced apoptosis is associated with suppression of insulin-like growth factor binding protein-5 secretion in differentiating murine skeletal myoblasts." J Cell Physiol 183(3): 330-7.
Melino, M., Hii, C. S., McColl, S. R. and Ferrante, A. (2008). "The effect of the JNK inhibitor, JIP peptide, on human T lymphocyte proliferation and cytokine production." J Immunol 181(10): 7300-6.
Milasincic, D. J., Calera, M. R., Farmer, S. R. and Pilch, P. F. (1996). "Stimulation of C2C12 myoblast growth by basic fibroblast growth factor and insulin-like growth factor 1 can occur via mitogen-activated protein kinase-dependent and -independent pathways." Mol Cell Biol 16(11): 5964-73.
Miller, S. C., Ito, H., Blau, H. M. and Torti, F. M. (1988). "Tumor necrosis factor inhibits human myogenesis in vitro." Mol Cell Biol 8(6): 2295-301.

References
120
Mitch, W. E. and Goldberg, A. L. (1996). "Mechanisms of muscle wasting. The role of the ubiquitin-proteasome pathway." N Engl J Med 335(25): 1897-905.
Morgan, J. E., Moore, S. E., Walsh, F. S. and Partridge, T. A. (1992). "Formation of skeletal muscle in vivo from the mouse C2 cell line." J Cell Sci 102 (Pt 4): 779-87.
Musaro, A., McCullagh, K., Paul, A., Houghton, L., Dobrowolny, G., Molinaro, M., Barton, E. R., Sweeney, H. L. and Rosenthal, N. (2001). "Localized Igf-1 transgene expression sustains hypertrophy and regeneration in senescent skeletal muscle." Nat Genet 27(2): 195-200.
Musaro, A., McCullagh, K. J., Naya, F. J., Olson, E. N. and Rosenthal, N. (1999). "IGF-1 induces skeletal myocyte hypertrophy through calcineurin in association with GATA-2 and NF-ATc1." Nature 400(6744): 581-5.
Musaro, A. and Rosenthal, N. (1999). "Maturation of the myogenic program is induced by postmitotic expression of insulin-like growth factor I." Mol Cell Biol 19(4): 3115-24.
Mussig, K., Fiedler, H., Staiger, H., Weigert, C., Lehmann, R., Schleicher, E. D. and Haring, H. U. (2005). "Insulin-induced stimulation of JNK and the PI 3-kinase/mTOR pathway leads to phosphorylation of serine 318 of IRS-1 in C2C12 myotubes." Biochem Biophys Res Commun 335(3): 819-25.
Nakamura, A., Yoshida, K., Ueda, H., Takeda, S. and Ikeda, S. (2005). "Up-regulation of mitogen activated protein kinases in mdx skeletal muscle following chronic treadmill exercise." Biochim Biophys Acta 1740(3): 326-31.
Nitsch, R. M., Deng, M., Growdon, J. H. and Wurtman, R. J. (1996). "Serotonin 5-HT2a and 5-HT2c receptors stimulate amyloid precursor protein ectodomain secretion." J Biol Chem 271(8): 4188-94.
O'Brien, K. F. and Kunkel, L. M. (2001). "Dystrophin and muscular dystrophy: past, present, and future." Mol Genet Metab 74(1-2): 75-88.
Odom, G. L., Gregorevic, P. and Chamberlain, J. S. (2007). "Viral-mediated gene therapy for the muscular dystrophies: successes, limitations and recent advances." Biochim Biophys Acta 1772(2): 243-62.
Old, L. J. (1981). "Cancer immunology: the search for specificity--G. H. A. Clowes Memorial lecture." Cancer Res 41(2): 361-75.
Pajak, B., Orzechowska, S., Pijet, B., Pijet, M., Pogorzelska, A., Gajkowska, B. and Orzechowski, A. (2008). "Crossroads of cytokine signaling--the chase to stop muscle cachexia." J Physiol Pharmacol 59 Suppl 9: 251-64.
Palmer, S., Groves, N., Schindeler, A., Yeoh, T., Biben, C., Wang, C. C., Sparrow, D. B., Barnett, L., Jenkins, N. A., Copeland, N. G., Koentgen, F., Mohun, T. and Harvey, R. P. (2001). "The small muscle-specific protein Csl modifies cell shape and promotes myocyte fusion in an insulin-like growth factor 1-dependent manner." J Cell Biol 153(5): 985-98.

References
121
Partridge, T. (1991). "Animal models of muscular dystrophy--what can they teach us?" Neuropathol Appl Neurobiol 17(5): 353-63.
Payne, E. T., Yasuda, N., Bourgeois, J. M., Devries, M. C., Rodriguez, M. C., Yousuf, J. and Tarnopolsky, M. A. (2006). "Nutritional therapy improves function and complements corticosteroid intervention in mdx mice." Muscle Nerve 33(1): 66-77.
Pearson, G., Robinson, F., Beers Gibson, T., Xu, BE., Karandikar, M., Berman, K. and Cobb, M.H. (2001). "Mitogen-activated protein (MAP) kinase pathways: regulation and physiological functions." Endocr. Rev 22(2): 153–83.
Peterson, J. M., Feeback, K. D., Baas, J. H. and Pizza, F. X. (2006). "Tumor necrosis factor-alpha promotes the accumulation of neutrophils and macrophages in skeletal muscle." J Appl Physiol 101(5): 1394-9.
Price, S. R., Bailey, J. L., Wang, X., Jurkovitz, C., England, B. K., Ding, X., Phillips, L. S. and Mitch, W. E. (1996). "Muscle wasting in insulinopenic rats results from activation of the ATP-dependent, ubiquitin-proteasome proteolytic pathway by a mechanism including gene transcription." J Clin Invest 98(8): 1703-8.
Radley, H. G., Davies, M. J. and Grounds, M. D. (2008). "Reduced muscle necrosis and long-term benefits in dystrophic mdx mice after cV1q (blockade of TNF) treatment." Neuromuscul Disord 18(3): 227-38.
Radley, H. G. and Grounds, M. D. (2006). "Cromolyn administration (to block mast cell degranulation) reduces necrosis of dystrophic muscle in mdx mice." Neurobiol Dis 23(2): 387-97.
Reid, M. B. and Li, Y. P. (2001). "Tumor necrosis factor-alpha and muscle wasting: a cellular perspective." Respir Res 2(5): 269-72.
Rinderknecht, E. and Humbel, R. E. (1978). "The amino acid sequence of human insulin-like growth factor I and its structural homology with proinsulin." J Biol Chem 253(8): 2769-76.
Rommel, C., Bodine, S. C., Clarke, B. A., Rossman, R., Nunez, L., Stitt, T. N., Yancopoulos, G. D. and Glass, D. J. (2001). "Mediation of IGF-1-induced skeletal myotube hypertrophy by PI(3)K/Akt/mTOR and PI(3)K/Akt/GSK3 pathways." Nat Cell Biol 3(11): 1009-13.
Rommel, C., Clarke, B. A., Zimmermann, S., Nunez, L., Rossman, R., Reid, K., Moelling, K., Yancopoulos, G. D. and Glass, D. J. (1999). "Differentiation stage-specific inhibition of the Raf-MEK-ERK pathway by Akt." Science 286(5445): 1738-41.
Ross, M., Francis, G. L., Szabo, L., Wallace, J. C. and Ballard, F. J. (1989). "Insulin-like growth factor (IGF)-binding proteins inhibit the biological activities of IGF-1 and IGF-2 but not des-(1-3)-IGF-1." Biochem J 258(1): 267-72.
Rothenberg, P. L., Lane, W. S., Karasik, A., Backer, J., White, M. and Kahn, C. R. (1991). "Purification and partial sequence analysis of pp185, the major cellular substrate of the insulin receptor tyrosine kinase." J Biol Chem 266(13): 8302-11.

References
122
Roy, P. K., Rashid, F., Bragg, J. and Ibdah, J. A. (2008). "Role of the JNK signal transduction pathway in inflammatory bowel disease." World J Gastroenterol 14(2): 200-2.
Rubin, J. B., Shia, M. A. and Pilch, P. F. (1983). "Stimulation of tyrosine-specific phosphorylation in vitro by insulin-like growth factor I." Nature 305(5933): 438-40.
Rui, L., Aguirre, V., Kim, J. K., Shulman, G. I., Lee, A., Corbould, A., Dunaif, A. and White, M. F. (2001). "Insulin/IGF-1 and TNF-alpha stimulate phosphorylation of IRS-1 at inhibitory Ser307 via distinct pathways." J Clin Invest 107(2): 181-9.
Russell, B., Motlagh, D. and Ashley, W. W. (2000). "Form follows function: how muscle shape is regulated by work." J Appl Physiol 88(3): 1127-32.
Rutanen, E. M. and Pekonen, F. (1990). "Insulin-like growth factors and their binding proteins." Acta Endocrinol (Copenh) 123(1): 7-13.
Sacheck, J. M., Ohtsuka, A., McLary, S. C. and Goldberg, A. L. (2004). "IGF-I stimulates muscle growth by suppressing protein breakdown and expression of atrophy-related ubiquitin ligases, atrogin-1 and MuRF1." Am J Physiol Endocrinol Metab 287(4): E591-601.
Saito, K., Kobayashi, D., Komatsu, M., Yajima, T., Yagihashi, A., Ishikawa, Y., Minami, R. and Watanabe, N. (2000). "A sensitive assay of tumor necrosis factor alpha in sera from Duchenne muscular dystrophy patients." Clin Chem 46(10): 1703-4.
Saladin, K. (2004). Anatomy & physiology: the unity of form and function. New York, McGraw-Hill.
Sandri, M., Sandri, C., Gilbert, A., Skurk, C., Calabria, E., Picard, A., Walsh, K., Schiaffino, S., Lecker, S. H. and Goldberg, A. L. (2004). "Foxo transcription factors induce the atrophy-related ubiquitin ligase atrogin-1 and cause skeletal muscle atrophy." Cell 117(3): 399-412.
SEER (n.d). Muscular System/Structure of Skeletal Muscle, [Online], available from <http://training.seer.cancer.gov/module_anatomy/unit4_2_muscle_structure.html> [April 19 2009].
Sethi, G., Sung, B. and Aggarwal, BB. (2008). " TNF: a master switch for inflammation to cancer." Front Biosci. 1 (13):5094-107.
Semsarian, C., Sutrave, P., Richmond, D. R. and Graham, R. M. (1999). "Insulin-like growth factor (IGF-I) induces myotube hypertrophy associated with an increase in anaerobic glycolysis in a clonal skeletal-muscle cell model." Biochem J 339 (Pt 2): 443-51.
Shavlakadze, T. and Grounds, M. (2006). "Of bears, frogs, meat, mice and men: complexity of factors affecting skeletal muscle mass and fat." Bioessays 28(10): 994-1009.

References
123
Shavlakadze, T., White, J., Hoh, J. F., Rosenthal, N. and Grounds, M. D. (2004). "Targeted expression of insulin-like growth factor-I reduces early myofiber necrosis in dystrophic mdx mice." Mol Ther 10(5): 829-43.
Shavlakadze, T., White, J. D., Davies, M., Hoh, J. F. and Grounds, M. D. (2005). "Insulin-like growth factor I slows the rate of denervation induced skeletal muscle atrophy." Neuromuscul Disord 15(2): 139-46.
Shavlakadze, T., Winn, N., Rosenthal, N. and Grounds, M. D. (2005). "Reconciling data from transgenic mice that overexpress IGF-I specifically in skeletal muscle." Growth Horm IGF Res 15(1): 4-18.
Schütze, S., Machleidt, T. and Krönke, M. (1992) "Mechanisms of tumor necrosis factor action." Semin. Oncol. 19(2): 16–24.
Sicinski, P., Geng, Y., Ryder-Cook, A. S., Barnard, E. A., Darlison, M. G. and Barnard, P. J. (1989). "The molecular basis of muscular dystrophy in the mdx mouse: a point mutation." Science 244(4912): 1578-80.
Srivastava, A. K., Qin, X., Wedhas, N., Arnush, M., Linkhart, T. A., Chadwick, R. B. and Kumar, A. (2007). "Tumor necrosis factor-alpha augments matrix metalloproteinase-9 production in skeletal muscle cells through the activation of transforming growth factor-beta-activated kinase 1 (TAK1)-dependent signaling pathway." J Biol Chem 282(48): 35113-24.
Stitt, T. N., Drujan, D., Clarke, B. A., Panaro, F., Timofeyva, Y., Kline, W. O., Gonzalez, M., Yancopoulos, G. D. and Glass, D. J. (2004). "The IGF-1/PI3K/Akt pathway prevents expression of muscle atrophy-induced ubiquitin ligases by inhibiting FOXO transcription factors." Mol Cell 14(3): 395-403.
Strle, K., Broussard, S. R., McCusker, R. H., Shen, W. H., LeCleir, J. M., Johnson, R. W., Freund, G. G., Dantzer, R. and Kelley, K. W. (2006). "C-jun N-terminal kinase mediates tumor necrosis factor-alpha suppression of differentiation in myoblasts." Endocrinology 147(9): 4363-73.
Sultan, K. R., Henkel, B., Terlou, M. and Haagsman, H. P. (2006). "Quantification of hormone-induced atrophy of large myotubes from C2C12 and L6 cells: atrophy-inducible and atrophy-resistant C2C12 myotubes." Am J Physiol Cell Physiol 290(2): C650-9.
Sury, M. D., Agarinis, C., Widmer, H. R., Leib, S. L. and Christen, S. (2008). "JNK is activated but does not mediate hippocampal neuronal apoptosis in experimental neonatal pneumococcal meningitis." Neurobiol Dis 32(1): 142-50.
Szalay, K., Razga, Z. and Duda, E. (1997). "TNF inhibits myogenesis and downregulates the expression of myogenic regulatory factors myoD and myogenin." Eur J Cell Biol 74(4): 391-8.
Tanaka, S. and Hanafusa, H. (1998). "Guanine-nucleotide exchange protein C3G activates JNK1 by a ras-independent mechanism. JNK1 activation inhibited by kinase

References
124
negative forms of MLK3 and DLK mixed lineage kinases." J Biol Chem 273(3): 1281-4.
Tews, D. S. (2005). "Tumour necrosis factor-mediated cell death pathways do not contribute to muscle fibre death in dystrophinopathies." Acta Neuropathol 109(2): 217-25.
Thomas, E. C., Zhe, Y., Molero, J. C., Schmitz-Peiffer, C., Ramm, G., James, D. E. and Whitehead, J. P. (2006). "The subcellular fractionation properties and function of insulin receptor substrate-1 (IRS-1) are independent of cytoskeletal integrity." Int J Biochem Cell Biol 38(10): 1686-99.
Tibbles, L. A., Ing, Y. L., Kiefer, F., Chan, J., Iscove, N., Woodgett, J. R. and Lassam, N. J. (1996). "MLK-3 activates the SAPK/JNK and p38/RK pathways via SEK1 and MKK3/6." Embo J 15(24): 7026-35.
Tidball, J. G. (2005). "Inflammatory processes in muscle injury and repair." Am J Physiol Regul Integr Comp Physiol 288(2): R345-53.
Tisdale, M. J. (2005). "Molecular pathways leading to cancer cachexia." Physiology (Bethesda) 20: 340-8.
Tollefsen, S. E., Lajara, R., McCusker, R. H., Clemmons, D. R. and Rotwein, P. (1989). "Insulin-like growth factors (IGF) in muscle development. Expression of IGF-I, the IGF-I receptor, and an IGF binding protein during myoblast differentiation." J Biol Chem 264(23): 13810-7.
Tolosa, L., Morla, M., Iglesias, A., Busquets, X., Llado, J. and Olmos, G. (2005). "IFN-gamma prevents TNF-alpha-induced apoptosis in C2C12 myotubes through down-regulation of TNF-R2 and increased NF-kappaB activity." Cell Signal 17(11): 1333-42.
Tracey, K. J., Wei, H., Manogue, K. R., Fong, Y., Hesse, D. G., Nguyen, H. T., Kuo, G. C., Beutler, B., Cotran, R. S., Cerami, A. and et al. (1988). "Cachectin/tumor necrosis factor induces cachexia, anemia, and inflammation." J Exp Med 167(3): 1211-27.
Ullrich, A., Gray, A., Tam, A. W., Yang-Feng, T., Tsubokawa, M., Collins, C., Henzel, W., Le Bon, T., Kathuria, S., Chen, E. and et al. (1986). "Insulin-like growth factor I receptor primary structure: comparison with insulin receptor suggests structural determinants that define functional specificity." Embo J 5(10): 2503-12.
Vandenburgh, H. H., Karlisch, P., Shansky, J. and Feldstein, R. (1991). "Insulin and IGF-I induce pronounced hypertrophy of skeletal myofibers in tissue culture." Am J Physiol Cell Physiol 260(3): C475-484.
Vivanco, I. and Sawyers, C. L. (2002). "The phosphatidylinositol 3-Kinase AKT pathway in human cancer." Nat Rev Cancer 2(7): 489-501.
Vives, E., Brodin, P. and Lebleu, B. (1997). "A Truncated HIV-1 Tat Protein Basic Domain Rapidly Translocates through the Plasma Membrane and Accumulates in the Cell Nucleus." J. Biol. Chem. 272(25): 16010-16017.

References
125
Voorhamme, D. and Yandell, C. A. (2006). "LONG R3IGF-I as a more potent alternative to insulin in serum-free culture of HEK293 cells." Mol Biotechnol 34(2): 201-4.
Wajant, H., Pfizenmaier, K. and Scheurich, P. (2003). "Tumor necrosis factor signaling." Cell Death Differ 10(1): 45-65.
Wang, G. F., Nikovits, W., Jr., Schleinitz, M. and Stockdale, F. E. (1996). "Atrial Chamber-specific Expression of the Slow Myosin Heavy Chain 3Gene in the Embryonic Heart." J. Biol. Chem. 271(33): 19836-19845.
Wang, Z., Chamberlain, J. S., Tapscott, S. J. and Storb, R. (2009). "Gene therapy in large animal models of muscular dystrophy." Ilar J 50(2): 187-98.
Waters, F (2006). Are the necrotic effects of Tumour Necrosis Factor-alpha (TNFα) in dystrophic muscle mediated by p53? [dissertation], Anatomy and Human Biology, University of Western Australia.
Weisberg, S. P., McCann, D., Desai, M., Rosenbaum, M., Leibel, R. L. and Ferrante, A. W., Jr. (2003). "Obesity is associated with macrophage accumulation in adipose tissue." J Clin Invest 112(12): 1796-808.
Wineinger, M. A., Abresch, R. T., Walsh, S. A. and Carter, G. T. (1998). "Effects of aging and voluntary exercise on the function of dystrophic muscle from mdx mice." Am J Phys Med Rehabil 77(1): 20-7.
Wu, B., Moulton, H. M., Iversen, P. L., Jiang, J., Li, J., Li, J., Spurney, C. F., Sali, A., Guerron, A. D., Nagaraju, K., Doran, T., Lu, P., Xiao, X. and Lu, Q. L. (2008). "Effective rescue of dystrophin improves cardiac function in dystrophin-deficient mice by a modified morpholino oligomer." Proc Natl Acad Sci U S A 105(39): 14814-9.
Yaffe, D. (1968). "Retention of differentiation potentialities during prolonged cultivation of myogenic cells." Proc Natl Acad Sci U S A 61(2): 477-83.
Yaffe, D. and Saxel, O. (1977). "Serial passaging and differentiation of myogenic cells isolated from dystrophic mouse muscle." Nature 270(5639): 725-7.
Yang, D. D., Kuan, C. Y., Whitmarsh, A. J., Rincon, M., Zheng, T. S., Davis, R. J., Rakic, P. and Flavell, R. A. (1997). "Absence of excitotoxicity-induced apoptosis in the hippocampus of mice lacking the Jnk3 gene." Nature 389(6653): 865-70.
Yokota, T., Lu, Q. L., Partridge, T., Kobayashi, M., Nakamura, A., Takeda, S. and Hoffman, E. (2009). "Efficacy of systemic morpholino exon-skipping in duchenne dystrophy dogs." Ann Neurol.
Yotov, W. V. and St-Arnaud, R. (1996). "Differential splicing-in of a proline-rich exon converts alphaNAC into a muscle-specific transcription factor." Genes Dev 10(14): 1763-72.


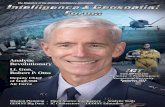
















![Overload relay - grupoimex.com térmicos.pdfTNF –20° TNF TNF –5° 750 4000 12000 1650 TNF +5° TNF +15° a b c d R [ ] i [°C] 5 47 16.5 4.7 86 60 112 Technical overview Bimetal](https://static.fdocuments.in/doc/165x107/60065006b9ae12444231e63f/overload-relay-trmicospdf-tnf-a20-tnf-tnf-a5-750-4000-12000-1650-tnf.jpg)