Introduction to Medical ICU: Part II David Oxman, MD Assistant Professor of Medicine Pulmonary &...
-
Upload
mauricio-lister -
Category
Documents
-
view
218 -
download
4
Transcript of Introduction to Medical ICU: Part II David Oxman, MD Assistant Professor of Medicine Pulmonary &...
Introduction to Medical ICU: Part II
David Oxman, MDAssistant Professor of Medicine
Pulmonary & Critical CareThomas Jefferson University Hospital
July 19, 2013
• One day cross-sectional study of ICU clinicians• Conflicts perceived by 72% of respondents• Physician-nurse conflict most common at 32%.• Most common conflict causing behaviors
– Personal animosity– Mistrust– Communication gaps
Azoulay AJRCCM 2009
Interdisciplinary Communication in ICU
•Bad Communication associated with:– Job dissatisfaction– Burnout– Misperception of patient care goals– Medical errors
•Tools to improve interdisciplinary communication in ICU
– Creating safe atmosphere to speak up – Willingness to listen– Leveling Hierarchy (Interdisciplinary rounds)
Role of the MICU Fellow in Promoting Good ICU
Communication•At center of daily activities of ICU•Can foster good communication between disciplines
•Often aware conflicts first.•Set an example for the residents
Why an Integrated approach?We Need Coordinated Care
• Many tasks and demands on critical care staff
• About aligning the people, processes, and technology already existing in ICUs
• ABCDE bundle is interdisciplinary, and designed to:
• Improve collaboration among clinical team members • Standardize care processes• Break the cycle of oversedation and prolonged ventilation
What are the components of the ABCDE Bundle?
Awakening and Breathing Coordination
Choice of Analgesics and Sedatives
Delirium Identification and Management
Early Exercise and Mobility
AB
D
E
C
Daily Awakening TrialsWhy Is Interruption of Sedation Effective?
•Less accumulation of sedative drug and metabolites
•Less sedative medication used overall
•Opportunity for more effective weaning from mechanical ventilation
Sessler CN. Crit Care Med 2004
Kress et al. NEJM. 2000
•Shorter duration of mechanical ventilation
•Shorter ICU LOS
• Fewer tests for altered mental status
Kress et al. N Engl J Med 2000; 342:1471-7
Results
“SAT + SBT” Was Superior to Conventional Sedation + SBT
Girard et al. Lancet 2008; 371:126-34
P = 0.02
P = 0.01
Extubated faster Discharged from ICU sooner
Using the Right Drugs is Important –It’s a Balancing Act
Calm Alert
Free of pain and anxiety
Lightly
sedated
Deeply
sedated
Pain,
anxiety
Agitation, vent
dyssynchrony
Spectrum of Distress/Comfort/Sedation
Dangerous
agitation
Unresponsive
LOS
Dost
Delirium
VAP
Self-harm
Caregiver assault
Stress
MI
Over sedation
Patient Comfort and
Venti latory Optimization
Consequences of Suboptimal Sedation
Inadequate sedation/analgesia
• Anxiety• Pain• Patient-ventilator
dyssynchrony • Agitation
– Self-removal of tubes/catheters
• Care provider assault• Myocardial ischemia• Family dissatisfaction
Excessive sedation
• Prolonged mechanical ventilation, ICU LOS
– Tracheostomy– DVT, VAP
• Additional testing• Added cost• Inability to communicate• Cannot evaluate for
delirium
The Ideal ICU Sedative•Rapid onset of action and rapidly cleared.
•Predictable dose response
•Easy to administer
•Minimal drug accumulation
•Few adverse effects
•Minimal drug interaction
•Cheap 1. Ostermann ME, et al. JAMA. 2000;283:1451-1459.
2. Jacobi J, et al. Crit Care Med. 2002;30:119-141.
3. Dasta JF, et al. Pharmacother. 2006;26:798-805.
4. Nelson LE, et al. Anesthesiol. 2003;98:428-436.
Does not exist
CChoice of
Analgesics and Sedatives
Assessing and Targeting Sedation
Richmond Agitation Sedation Scale
Score RAAS Description
+4 Combative, violent, danger to staff
+3 Pulls or removes tube(s) or catheters; aggressive
+2 Frequent non-purposeful movement, fights ventilator
+1 Anxious, apprehensive, but not aggressive
0 Alert and calm
-1 Awakens to voice (eye opening/contact) >10 sec
-2 Light sedation, briefly awakens to voice (eye opening/contact) <10 sec
-3 Moderate sedation, movement or eye opening. No eye contact
-4 Deep sedation, no response to voice, but movement or eye opening to physical stimulation
-5 Unarousable, no response to voice or physical stimulation
Choice of Analgesics and Sedatives
The choice driven by:
Goals for each patient
Clinical pharmacology
Costs
C
Key Points on Sedation
• Assess and target.
• Bolus first and
then consider
continuous
infusion.
• Daily interruption
Delirium KillsDuration and Mortality
Pisani MA. Am J Respir Crit Care Med. 2009;180:1092-1097.
Kaplan-Meier
Survival Curve
Each day of delirium in the ICU increases the hazard of mortality by 10%
P < 0.001
Patient Factors
Increased age
Alcohol use
Male gender
Living alone
Smoking
Renal disease
Environment
Admission via ED or
through transfer
Isolation
No clock
No daylight
No visitors
Noise
Use of physical restraints
Predisposing Disease
Cardiac disease
Cognitive impairment
(eg, dementia)
Pulmonary disease
Acute Illness
Length of stay
Fever
Medicine service
Lack of nutrition
Hypotension
Sepsis
Metabolic disorders
Tubes/catheters
Medications:
- Anticholinergics
- Corticosteroids
- Benzodiazepines
Less Modifiable
More Modifiable
DELIRIUM
Van Rompaey B, et al. Crit Care. 2009;13:R77.
Inouye SK, et al. JAMA.1996;275:852-857.
Skrobik Y. Crit Care Clin. 2009;25:585-591.
Delirium: What Can We Do?
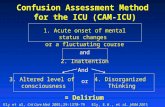
Diagnosis is Key !!Confusion Assessment Method for the ICU (CAM-ICU)
Feature 1: Acute change or fluctuating
course of mental status
And
Feature 2: Inattention
And
Feature 3: Altered level of
consciousnessFeature 4: Disorganized thinking
Or
Inouye, et. al. Ann Intern Med 1990; 113:941-948.1
Ely, et. al. CCM 2001; 29:1370-1379.4
Ely, et. al. JAMA 2001; 286:2703-2710.5
Letter A test• “SAVEAHAART”•Say above 10 Letters & instruct patient to squeeze hand every time you say letter “A”
• Inattention PRESENT if > 2 errors
Diagnosing Delirium in Patient on
Mechanical Ventilation
Early Progressive Exercise and Mobility
Early progressive mobility programs result in:
Better patient outcomes Shorter hospital stays Decreased development of
hospital acquired complications
The level of exercise and mobility is individualized and incrementally progressed
E
Early Mobility“Move It Or Lose It”
Immobility not beneficial and associated with harm
–Myopathy/neuropathy–Delayed weaning from
ventilator–Delirium– Infections–Pressure ulcers
E
Early Exercise in the ICU
• Early exercise = progressive mobility• Study design: paired SAT/SBT protocol with PT/OT from
earliest days of mechanical ventilation
Schweickert WD, et al. Lancet. 2009;373:1874-1882.
Wake Up, Breathe, and Move
Early Exercise Study Results
OutcomeIntervention
(n=49)Control(n=50) P
Functionally independent at discharge 29 (59%) 19 (35%) 0.02
ICU delirium (days) 2.0 (0.0-6.0) 4.0 (2.0-7.0) 0.03
Time in ICU with delirium (%) 33 (0-58) 57 (33-69) 0.02
Hospital delirium (days) 2.0 (0.0-6.0) 4.0 (2.0-8.0) 0.02
Hospital days with delirium (%) 28 (26) 41 (27) 0.01
Barthel index score at discharge 75 (7.5-95) 55 (0-85) 0.05
ICU-acquired paresis at discharge 15 (31%) 27 (49%) 0.09
Ventilator-free days 23.5 (7.4-25.6) 21.1 (0.0-23.8) 0.05
Length of stay in ICU (days) 5.9 (4.5-13.2) 7.9 (6.1-12.9) 0.08
Length of stay in hospital (days) 13.5 (8.0-23.1) 12.9 (8.9-19.8) 0.93
Hospital mortality 9 (18%) 14 (25%) 0.53
Schweickert WD, et al. Lancet. 2009;373:1874-1882.
Early Progressive Exercise and Mobility
•All patients are candidates for mobilization if:– No clinical contraindications to physical
activity– Pass a safety screen for participation
• Patients initially not eligible mobilization or who have had interruptions in exercise will continually reassessed for participation
• The level of exercise and mobility is individualized and incrementally progressed
Just Count Something
“No matter what you ultimately do in medicine a doctor should be a scientist in his or her world. In the simplest terms, this means that we should count something…It doesn’t really matter what you count. You don’t need a research grant. The only requirement is that what you count should be interesting to you.”
Atul Gawande
ICU Database
•Let’s us look above the daily grind.•Illuminates random experiences.•Concrete uses:• Measuring utilization• Measuring performance• Platform for clinical research
MICU Database
• 95% of data entered by nursing/clerical staff• Fellows responsible for:
– Primary MICU diagnosis– Select comorbidities (yes or no)– APACHE scores
• Coming to Methodist• Regular feedback of data
ICU Infection Control
• Key Performance Measure for ICU• Hospital Compensation from Payors at Risk• Intensivist’s Bonuses at Risk!!!
Infections with Surveillance Programs1. Central Line Associated Bloodstream Infections
(CLASBI)2. Ventilator-Associated Pneumonia (VAP)3. Catheter-Associated Urinary Tract Infection (CAUTI)4. Clostridium Difficile Colitis
Reducing ICU-Acquired Infections• CLASBI
– Insertion bundle– Avoid femoral site– No blood draws through catheter– Good catheter maintenance– Remove when not needed
• VAP– Shorten duration of mechanical ventilation: Daily SAT/SBT– VAP Bundle
• CAUTI: – Don’t place foley if not necessary– Get Foley’s out when not needed
• Clostridium Difficile: Limit unnecessary antibiotics















































![Theories of the digital in architecture€¦ · Theories of the digital in architecture / [edited by] Rivka Oxman and Robert Oxman, Routledge, Taylor & Francis Group. THE IMPORTANCE](https://static.fdocuments.in/doc/165x107/5f0b1e277e708231d42eef8d/theories-of-the-digital-in-architecture-theories-of-the-digital-in-architecture.jpg)



![OXMAN E. G. Images Without Metaphor - Reviewing French Film Theory [Th]](https://static.fdocuments.in/doc/165x107/577cc00a1a28aba7118ea90a/oxman-e-g-images-without-metaphor-reviewing-french-film-theory-th.jpg)