Intracerebral Hemorrhage Andrew Asimos, MD Associate Director Stroke Care Program Carolinas Medical...
-
Upload
cory-welch -
Category
Documents
-
view
214 -
download
1
Transcript of Intracerebral Hemorrhage Andrew Asimos, MD Associate Director Stroke Care Program Carolinas Medical...
Intracerebral Hemorrhage Intracerebral Hemorrhage
Andrew Asimos, MDAndrew Asimos, MD
Associate DirectorAssociate DirectorStroke Care ProgramStroke Care Program
Carolinas Medical CenterCarolinas Medical CenterCharlotte, NCCharlotte, NC
Clinical Assistant Professor of Emergency MedicineClinical Assistant Professor of Emergency MedicineUniversity of North CarolinaUniversity of North Carolina
Chapel Hill, NCChapel Hill, NC
Andrew Asimos, MD
Case PresentationCase Presentation
• ED setting– Community ED– On-call neurologist– Neurosurgical services not available– CT scanner (not located in or adjacent to the
ED)– No MRI– ICU beds available, on-call intensivist
Andrew Asimos, MD
Case PresentationCase Presentation
• 39 yo black male transported via paramedics with complaint of headache and right sided facial droop & paralysis starting 20 minutes PTA
• Reported SBP of 220 mm Hg in the field
• 16 g IV left anticubital fossa at KVO
• Not following commands
Andrew Asimos, MD
Initial ED EvaluationInitial ED Evaluation
• Obese black male• Drowsy, but arousable with verbal stimuli• Dysarthric with unintelligible speech,
adequately handling secretions• No respiratory difficulty or abnormal breathing
pattern• Diaphoretic with normal heart sounds,
bounding pulses
Andrew Asimos, MD
Initial Vital SignsInitial Vital Signs
• BP– 220/125 mm Hg right arm– 212/116 mm Hg left arm
• Pulse– 64 regular
• Temperature– 99.9° F rectally
• Respiratory rate– 18 regular
Andrew Asimos, MD
Neurologic ExamNeurologic Exam
• NIHSS Score = 23– Obtunded LOC– Unable to perform simple commands on left– Partial gaze palsy to the left– Complete right sided facial paralysis– No movement of right arm or leg– Severe sensory loss on the right– Global aphasia– Unintelligible speech– Profound neglect of right hemispace
Andrew Asimos, MD
Major ED ICH Management IssuesMajor ED ICH Management Issues
• Scientific evidence for recommended treatment
• Ability to diagnose based on clinical presentation
• BP management guidelines
• ICP treatment recommendations
• Who needs a neurosurgeon
Andrew Asimos, MD
Spontaneous Spontaneous Intracerebral Hemorrhage (ICH)Intracerebral Hemorrhage (ICH)
• ICH over twice as common as SAH– 8 - 13% of all strokes
• Greater chance of death or major disability than with ischemic stroke or SAH
• More common in males, blacks, and the elderly• 50% cases due to the effects of chronic
hypertension on intracranial perforating arteries
Broderick J et al. J Neurosurg. 1993;78:188-191.
Andrew Asimos, MD
Evidence Based Treatment for ICHEvidence Based Treatment for ICH
• Lack of RCT on ICH– As of 1995
• 4 small randomized surgical trials (353 total pts)• 4 small medical trials (513 total pts)
• Broad variability in treatment• No proven benefit of surgical or medical
treatment for ICH based on RCT– 7000 operations/year in US to remove ICH
Broderick JP et al. Stroke. 1999;30:905-915
Andrew Asimos, MD
Classic Presentation of ICHClassic Presentation of ICH
• Sudden onset of a focal deficit progressing over minutes to hours
• Headache (40%)*
• Nausea & Vomiting
• Early decreased LOC (50%)**
• Elevated blood pressure (90%)
• Early symptom progression
* Gorelick PB et al. Neurology. 1986;36:1445-1450.** Caplan L. General symptoms and signs. In: Kase CS, Caplan LR, eds. Intracerebral hemorrhage. Stroke. 1997;28:1-5.
Andrew Asimos, MD
Distinguishing ICH from Distinguishing ICH from Ischemic StrokeIschemic Stroke
• No collection of clinical features sufficiently predictive
Andrew Asimos, MD
Distinguishing ICH from Distinguishing ICH from Ischemic StrokeIschemic Stroke
• No collection of clinical features sufficiently predictive
Andrew Asimos, MD
Distinguishing ICH from Distinguishing ICH from Ischemic StrokeIschemic Stroke
• No collection of clinical features sufficiently predictive
Andrew Asimos, MD
Outcome from ICHOutcome from ICH
• Of the estimated 37,000 Americans who experienced an ICH in 1997– 35-50% dead at one month
• Half of all deaths within the first 2 days
– Only 10% living independently at one month– 20% independent at 6 months– Volume of intraventricular hemorrhage is an
important determinant of outcome in supratentorial ICH
Broderick J et al. J Neurosurg. 1993;78:188-191.Anderson et al. J Neurol Neurosurg Psychiatry. 1994;57:936-940.Counsell C et al. Cerebrovasc Dis. 1995;5:26-34.Tuhrim S et al. Critical Care Medicine. 1999;27(3):617-21.
Andrew Asimos, MD
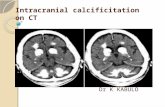
Initial Diagnostic EvaluationInitial Diagnostic Evaluation
• Non-contrast head CT is key– Readily identifies blood– Size and location of
hemorrhage– May expose contributing
structural abnormalities• Tumor• AVM
– Reveals structural complications
• Herniation• Intraventricular hemorrhage• Hydrocephalus
Andrew Asimos, MD
Returning to Our CaseReturning to Our Case
• Upon return from CT– BP remains 220/125 mm Hg– Increasingly obtunded– Drooling– Pulse ox 91% on 2 liters O2 nasal cannula– Deficits essentially unchanged
Andrew Asimos, MD
Airway and OxygenationAirway and Oxygenation
• Airway protection and adequate ventilation critical
• Aggressive airway management if decreasing LOC or signs of brainstem dysfunction
• RSI with drugs to avoid reflex arrhythmias and/or hemodynamic derangement
Andrew Asimos, MD
Aggressive Airway Aggressive Airway Management CriticalManagement Critical
performed in = Bad Idea
Prophylactic intubation may prevent the necessity of intubating the patient while in CT
Andrew Asimos, MD
Returning to Our CaseReturning to Our Case
• Patient successfully RSI’d– Lidocaine– Etomidate– Succinylcholine
Andrew Asimos, MD
Medical Management of ICH: Medical Management of ICH: Randomized TrialsRandomized Trials
• Four small trials– Steroid versus placebo (2 trials)– Hemodilution versus best medical therapy– Glycerol versus placebo
• No demonstrated benefit
• Infectious complications worse with steroid treatment
Italian Acute Stroke Study Group. Lancet. 1988;1:318-321.Yu YL et al. Stroke. 1992;23:967-971.Poungvarian N et al. N Eng J Med. 1987;316:1229-1233.Tellez H, Bauer R. Stroke. 1972;4: 541-546.
Andrew Asimos, MD
Blood Pressure Management in ICHBlood Pressure Management in ICH
• Optimal BP level should be somewhat individualized
• Treatment recommendations for elevated BP in ICH more aggressive than for ischemic stroke
Broderick JP et al. Stroke. 1999;30:905-915Adams HP Jr et al. Circulation. 1996;94:1167–1174.
Andrew Asimos, MD
Blood Pressure Management in ICHBlood Pressure Management in ICH
• Theoretical rationale for lowering BP is to decrease risk of ongoing bleeding from ruptured small arteries and arterioles
Brott T et al. Stroke. 1997;28:1–5.
Andrew Asimos, MD
Blood Pressure Management in ICHBlood Pressure Management in ICH
• Theoretical rationale for lowering BP is to decrease risk of ongoing bleeding from ruptured small arteries and arterioles
Brott T et al. Stroke. 1997;28:1–5.
Andrew Asimos, MD
Blood Pressure Management in ICHBlood Pressure Management in ICH
• Overaggressive BP treatment may decrease CPP and theoretically worsen brain injury, particularly in the setting of increased intracranial pressure
CPP = MAP - ICPCPP = MAP - ICP
Andrew Asimos, MD
Blood Pressure Management in ICHBlood Pressure Management in ICHScenario Treatment Recommendation
SBP >230 mm Hg or DBP > 140 mm Hg
nitroprusside
SBP 180-230 mm Hg, DBP 105-140 mm Hg, or MAP 130 mm Hg
labetalol, esmolol, enalapril, or other easily titratable medication
If SBP <180 mm Hg and DBP < 105 mm Hg
Defer antihypertensive therapy
If ICP monitoring available
CPP Maintained > 70 mm Hg
Adapted from Brott T, Reed RL. Stroke. 1989;20:694–697.
Andrew Asimos, MD
Returning to Our CaseReturning to Our Case
• Blood pressure lowered to 170/100 mm Hg after 3 doses of labetalol
• 600 cc’s of 0.9 NS intravenously infused thus far
• No witnessed seizure activity
• Repeat rectal temperature 100.6° F
Andrew Asimos, MD
Returning to Our CaseReturning to Our Case
• IVF rate reduced to KVO
• 650 mg tylenol suppository administered
• Blood pressure begins rising again
• Pulse decreases to 50’s
Andrew Asimos, MD
Management Options for Management Options for Increased ICP After ICHIncreased ICP After ICH
• Elevate HOB
• Osmotherapy
• Controlled hyperventilation
• Barbituate coma
• Ventricular drains
Broderick JP et al. Stroke. 1999;30:905-915
Andrew Asimos, MD
Causes of Increased ICP After ICHCauses of Increased ICP After ICH
• Mass effect of the hematoma
• Secondary Hydrocephalus
• Edema
Andrew Asimos, MD
Stepwise Recommended Stepwise Recommended Treatment to Control ICPTreatment to Control ICP
• Osmotherapy– Mannitol 20% (0.25-0.5 g/kg every 4 hrs)
• In the ED, reserved for pts with clinical deterioration associated with mass effect
• Furosemide (10 mg every 2-8 hrs) may be added to maintain an osmotic gradient
Broderick JP et al. Stroke. 1999;30:905-915
Andrew Asimos, MD
Stepwise Recommended Stepwise Recommended Treatment to Control ICPTreatment to Control ICP
• Hyperventilation– Hypocarbia causes cerebral vasoconstriction– Reduction in CBF almost immediate– Peak ICP reduction about 30 minutes after pCO2
change– Reduction of pCO2 to 35-30 mmHg
• Best achieved by raising ventilation rate at constant tidal volume (12-14 mL/kg)
• Lowers ICP 25-30% in most pts
Broderick JP et al. Stroke. 1999;30:905-915
Andrew Asimos, MD
Stepwise Recommended Stepwise Recommended Treatment to Control ICPTreatment to Control ICP
• Neuromuscular paralysis– In combination with adequate sedation
reduces elevated ICP by preventing increases in intrathoracic and venous pressure
– Nondepolarizing agents preferred
Broderick JP et al. Stroke. 1999;30:905-915
Andrew Asimos, MD
Returning to Our CaseReturning to Our Case
• Patient bolused with 50 gm mannitol• ABG after 20 minutes on the ventilator
reveals pCO2 to 32 mmHg• Patient bolused with 8 mg midazolam
and 10 mg vecuronium• Charge nurse in the ICU wants to know if
you’ll need a bed or will be transferring the patient
Andrew Asimos, MD
Recommendations for Surgical Recommendations for Surgical Treatment for ICHTreatment for ICH
• Nonsurgical Candidates– Small hemorrhages (<10 cm3)– Minimal neurologic deficits– GCS score 4
• If cerebellar hemorrhage with brainstem compression, may be a candidate for lifesaving surgery
Andrew Asimos, MD
Recommendations for Recommendations for Surgical Treatment for ICHSurgical Treatment for ICH
• Surgical Candidates– Cerebellar hemorrhage >3 cm with neurological
deterioration or brainstem compression and hydrocephalus from ventricular obstruction
– Associated structural lesion with chance for good outcome and surgical accessibility
– Young with moderate to large hemorrhage and clinical deterioration
Andrew Asimos, MD
Returning to Our CaseReturning to Our Case
• Patient transferred to tertiary care center with neurosurgical expertise
ED Presentation
Andrew Asimos, MD
Returning to Our CaseReturning to Our Case
• Undergoes craniotomy and evacuation of hemorrhage with ventriculostomy placement
ED Presentation 24 hrs after ED Presentation
Andrew Asimos, MD
Returning to Our CaseReturning to Our Case
• Followup CT shows excellent resolution of hemorrhage
ED Presentation 24 hrs after ED Presentation 5 days after ED Presentation
Andrew Asimos, MD
Patient Status at DischargePatient Status at Discharge
• Discharged to extended care facility 24 days after admission
• Intermittently following commands with left arm, right sided hemiparesis, apraxia, and aphasia
• Antihypertensive regimen– Clonidine– Minoxidil– Atenolol
Andrew Asimos, MD
Value of Value of Neurosurgical Intervention?Neurosurgical Intervention?
• A meta-analysis suggests that for patients with intraventricular extension of ICH, treatment with ventricular drainage combined with fibrinolytics may improve outcome
• Data support a RCT of surgical evacuation versus conservative treatment– Patients < 60-65 years of age– Admission GCS of 6-11– Hematoma not mainly located in the thalamus– Volume in the range of 30-100 ml– Midline shift < 10 mm
Nieuwkamp DJ et al. J Neurology. 2000;247(2):117-21.Hardemark HG et al. Cerebrovascular Diseases. 9(1):10-21, 1999 Jan-Feb.
Andrew Asimos, MD
Future Trends for ICHFuture Trends for ICH
• Large prospective, randomized, placebo controlled trials to examine– Judicious application of current therapeutic
modalities• Ventricular drainage combined with fibrinolytics• Stereotactic CT-guided aspiration and thrombolysis of
intracerebral hematoma
– Potential benefit of proposed new treatment modalities
• Neuroprotectives
Nieuwkamp DJ et al. J Neurology. 2000;247(2):117-21.Hardemark HG et al. Cerebrovascular Diseases. 9(1):10-21, 1999 Jan-Feb.
Andrew Asimos, MD
Summary Points: ICHSummary Points: ICH
• No large supporting specific medical or surgical therapies
• Distinction between ICH and ischemic stroke cannot be based on H&P
• Consensus based BP management guidelines• Stepwise treatment for ICP when indicated• Neurosurgical intervention not indicated for all
patients