Interplay between Inflammation and Cell Cycle …...Central JSM Alzheimer’s Disease and Related...
Transcript of Interplay between Inflammation and Cell Cycle …...Central JSM Alzheimer’s Disease and Related...

Central JSM Alzheimer’s Disease and Related Dementia
Cite this article: Kirouac L, Mathew M, Padmanabhan J (2015) Interplay between Inflammation and Cell Cycle Deregulation in Alzheimer’s Disease. JSM Alzheimer’s Dis Related Dementia 2(2): 1018.
*Corresponding authorJaya Padmanabhan, Department of Molecular Medicine, USF Health Byrd Alzheimer’s Institute, University of South Florida, 4001 East Fletcher Avenue, Tampa, Florida, USA, Tel: 813-396-0721; Email:
Submitted: 02 December 2014
Accepted: 04 June 2015
Published: 08 June 2015
Copyright© 2015 Padmanabhan et al.
OPEN ACCESS
Keywords•Alzheimer’s disease•Inflammation•Cell cycle•Neurodegeneration
Review Article
Interplay between Inflammation and Cell Cycle Deregulation in Alzheimer’s DiseaseLisa Kirouac1,2, Mevin Mathew2 and Jaya Padmanabhan1,2*1Department of Molecular Medicine, University of South Florida, USA2USF Health Byrd Alzheimer’s Institute, University of South Florida, USA
Abstract
Alzheimer’s disease (AD) pathology is associated with neuroinflammation and the ectopic expression of cell cycle proteins, indicating that these two events may be involved in its pathogenesis. The cause and consequences of these events are still elusive. Inflammatory signaling has been shown to induce expression of the Alzheimer’s associated amyloid precursor protein (APP), whose phosphorylation and pathogenic processing are regulated in a cell cycle specific manner. The amyloid beta (Aβ) generated upon secretase-mediated processing of APP deposits in the brain parenchyma, extracellularly, to form amyloid plaques, which coincides with glial activation and chronic neuroinflammation. As reviewed in this article, interplay of the inflammatory response and cell cycle dysfunction could be underlying pathogenic processes in the neurodegeneration observed in AD. Both events are linked to neuronal abnormalities and pathological hallmarks of AD, including Tau phosphorylation and Aβ generation and deposition. Epidemiological studies have linked the use of non-steroidal anti-inflammatory drugs with a decrease in risk for developing AD, however its use in clinical trials on AD patients has largely been ineffective. It seems that an early therapeutic intervention that could target neuroinflammation and mitotic changes in compromised neurons could potentially have a great impact on the progression of AD.
ABBREVIATIONSAD:Alzheimer’s disease; Aβ: Amyloid-beta; APP: Amyloid
Precursor Protein; PS-1: Presenilin-1; PS-2: Presenelin-2; CNS: Central Nervous System; ROS: Reactive Oxygen Species; NFκB: Nuclear Factor Kappa B; IL-1: Interleukin-1; MCP-1: Monocyte Chemoattractant Protein 1; MIP: Macrophage Inflammatory Protein; CSF: Cerebral Spinal Fluid; GM-CSF: Granulocyte Macrophage-Colony Stimulating Factor; TNF-α: Tumor Necrosis Factor Alpha; TGFβ: Transforming Growth Factor α; S100β: Beta Subunit of S100; ACT: Alpha-1-Antichymotrypsin; JNK: c-Jun N-Terminal Kinase; COX-2: Cyclooxygenase-2; NSAIDs: Non-Steroidal Anti-Inflammatory Drugs; LPS: Lipopolysaccharides
INTRODUCTIONAlzheimer’s disease (AD) is the most common form of senile
dementia and is ranked 6th in leading causes of death in the United States. In its initial stages, the disease presents itself with memory loss which later progresses to impaired executive
function and ultimately, death. Pathology development precedes cognitive decline and is thought to begin in the entorhinal cortex, gradually spreading to other areas of the brain and leading to widespread synaptic loss, metabolic dysfunction and atrophy [1]. The classic lesions of the AD brain are extracellular neuritic plaques and intracellular neurofibrillary tangles [2-4]. Neuritic plaques are formed by the deposition of the insoluble amyloid-beta (Aβ) peptide, a product formed by the sequential cleavage of the amyloid precursor protein (APP) by β- and γ-secretase. Neurofibrillary tangle pathology follows plaque development and is formed by hyperphosphorylation of the microtubule-associated protein, Tau. AD can be divided into two subgroups based on genetic association and age at onset: familial and sporadic. Familial AD occurs in early age and represents only 5-10% of all AD cases. This form of early-onset AD is largely genetic and is associated with mutations in Presenilin-1 (PS1), Presenilin-2 (PS2) and APP genes. Late-onset AD, thought to be sporadic, accounts for ~90-95% of all AD cases and while its etiology is unclear, its onset occurs with advanced age.

Central
Padmanabhan et al. (2015)Email:
JSM Alzheimer’s Dis Related Dementia 2(2): 1018 (2015) 2/11
CELLULAR INFLAMMATORY MEDIATORS IN ALZHEIMER’S DISEASE
Neuroinflammation is a common feature in nearly all neurodegenerative diseases, including Alzheimer’s disease. While it is a well established hallmark to the disease, it is unclear whether this feature is causative or subsequent to AD pathogenesis. Immunohistochemical analyses reveal an inflammatory status of post-mortem human AD brains with the presence of activated glia in proximity to Aβ deposits [5-8]. Likewise, this immune response is also observed around amyloid plaques in the brains of transgenic AD mice that express human APP carrying the Swedish mutation [9-13].
The brain’s resident microglia and astrocytes are the main cellular mediators that become activated in response to injury. Astrocytes are the most abundant type of glial cells in the central nervous system (CNS), and the pathology associated with AD triggers what is called “reactive astrogliosis” [14]. This activation is defined by an increase in number, size and mobility of astrocytes, which is thought to be important for Aβ clearance and degradation [15]. Microglia comprises a marginal portion of the glial cell population in the brain and when activated, undergoes distinct morphological changes and migration to the compromised area. There, they produce a number of reactive oxygen species (ROS), cytokines, chemokines, growth factors and complement factors that are released to the surrounding tissue [16-19].
Several in vitro studies implicate the highly insoluble, fibrillar form of Aβ in inducing microglial activation and inflammatory protein expression [20-26]. This effect has also been observed with in vivo imaging of microglial migration to amyloid deposits within transgenic AD mouse brain [27, 28]. In fact, treatment of transgenic AD mice with the recombinant 5 amino acid long β-sheet breaker peptide iAβ5, has been shown to not only reduce plaque load, but also lessen inflammation-induced cerebral damage [29]. Aβ has also been shown to induce cytokine production in various ways. The nuclear factor kappa B (NFκB) pathway leads to cytokine production and this signaling pathway can be induced by the Aβ peptide [21]. Aβ is able to bind to receptors expressed on the microglial membrane and induce the MAPK pathway which subsequently leads to expression of inflammatory genes and production of chemokines and cytokines [30]. A working hypothesis for these findings is that the dense and irreversible nature of the amyloid plaque leads to stimulation of glial cells and chronic inflammation in the brain. The release of proinflammatory mediators in response to the fibrillar Aβ- along with soluble Aβ itself- results in a neurotoxic effect for healthy, adjacent neurons [31]. Additionally, these inflammatory mediators are thought to facilitate enhanced amyloidogenic processing of APP, producing more Aβ, which then feeds into the vicious cycle [22,32,33]. Conversely, others believe inflammation precedes fibrillar plaque pathology. For example, a study carried out in macaque monkeys found that glial activation is an event that occurs before deposition of fibrillar Aβ in the aging brain [34]. Several studies have also linked polymorphisms in pro-inflammatory cytokine genes, in particular Interleukin-1 (IL-1), to AD (35-40). Another example is that from a study in Down syndrome patients, who typically develop AD by middle age as
they carry an extra copy of the APP gene; this study showed that the brains of fetal and neonate Down syndrome patients (considered to be pre-amyloid plaque bearing) exhibit gliosis, and show upregulation of cytokines, further supporting the notion that inflammation and plaque development occur sequentially [41].
MOLECULAR MEDIATORS OF INFLAMMATION IN ALZHEIMER’S DISEASE
Activated microglia and astrocytes surrounding amyloid plaques secrete cytokines and chemokines that contribute to the inflammatory process. A number of cytokines and chemokines are found to be upregulated in AD brains compared to their non-demented controls [42-45].
Chemokines are a family of small proteins that recruit monocytes, macrophages, lymphocytes, neutrophils, basophils, eosinophils and dendridic cells to compromised tissues [46]. The Aβ peptide can promote the generation of chemokines such as IL-8, monocyte chemoattractant protein 1 (MCP-1), macrophage inflammatory protein (MIP)- 1α and -1β [47] from human monocytes [17]. Additionally, MIP-1β has been detected within activated astrocytes around amyloid plaques [48]. Cytokines are soluble proteins that are secreted by glia in the AD brain in response to Aβ aggregates [49]. Analysis of both AD human and transgenic mouse brain tissues and cerebral spinal fluid (CSF) show a marked increase in the levels of IL-1β, IL-1α, IL-6, IL-10, IL-12, granulocyte macrophage-colony stimulating factor (GM-CSF), tumor necrosis factor α (TNF-α) and transforming growth factor β (TGF-β) [50-57].
In the brain, TNF-α is predominantly produced by activated microglia in response to injury; however it has also been shown to be produced by neurons [58]. The role of TNF-α in AD is unclear as it has both beneficial and detrimental effects. Under non-pathological conditions, TNF-α levels are low in the brain [59] but in AD its levels are elevated in serum, CSF, cortex and glial cells [17,60,61]. The role of TNF-α is dichotomous in nature: it is able to stimulate NF-κB which in turn induces transcription of proinflammatory proteins and stimulation of survival proteins such as anti-apoptotic Bcl, manganese superoxide dismutase and calbindin [62,63]. It has been demonstrated in vitro that TNF-α is able to induce expression of APP and Aβ in glial cells [64]. Its harmful effects also include its stimulation of microglia to release glutamate, resulting in excitotoxicity [65]. TNF-α has been implicated in increased expression of both β- and γ-secretases. Furthermore, inhibition of TNF-α has been shown to mitigate disease progression in transgenic AD mice [66,67]. On the contrary, chronic TNF-α suppression can hinder the microglial response in early stages of Aβ deposition, leading to accelerated aggregation [68]. It is possible that the action that TNF-α exerts is dependent on both its levels and duration of tissue exposure in the brain.
IL-1 is an immunomodulatory cytokine, which is a key player in initiation of the immune response. IL-1 is found to be elevated immediately after brain injury [69,70] and this effect is also seen in response to amyloid plaques, as concentrations of IL-1 are increased in the AD brain [71-73]. Interestingly, IL-1 has been found to not only induce the synthesis of APP, but also mediate

Central
Padmanabhan et al. (2015)Email:
JSM Alzheimer’s Dis Related Dementia 2(2): 1018 (2015) 3/11
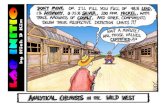
Figure 1 (A) The pathological cascade in Alzheimer’s disease. Oligomeric Aβ in AD induces activation of glia and release of inflammatory mediators. The expression of cell cycle proteins in compromised neuronal populations coincides with this neuroinflammatory response. Aberrant cell cycle activation in the AD brain has been shown to result in pathological modifications in the AD-associated proteins, APP and Tau. Hyperphosphorylation of APP results in increased production of the pathogenic Aβ peptide and its subsequent deposition in the brain. Soluble Aβ has been shown to further induce Tau hyperphosphorylation, neurofibrillary tangle formation, neurodegeneration and cell death. (B) Schematic of the inflammation and cell cycle-dependent signaling in Alzheimer’s disease: Amyloidogenic processing of APP leads to the production of the neurotoxic Aβ peptide. Reduced clearance and Aβ aggregation leads to glial activation and subsequent production of pro-inflammatory cytokines and chemokines, which can enhance expression of cell cycle regulatory proteins in the AD brain. In particular, TNF-α and COX-2 have been shown to correlate with expression of cell cycle markers. TNF-α is thought to initiate cell cycle events through the activation of the JNK pathway. Chronic exposure of neurons to inflammatory mediators thus lead to accelerated neuritic plaque and neurofibrillary tangle formation in AD brain. Inhibition of inflammation could potentially prevent aberrant cell cycle signaling and neurodegeneration associated with AD.

Central
Padmanabhan et al. (2015)Email:
JSM Alzheimer’s Dis Related Dementia 2(2): 1018 (2015) 4/11
its pathogenic processing [71,74]. This implicates a role for IL-1 in neurodegeneration, which is further highlighted by the finding that IL-1 promotes synthesis of the beta subunit of S100 protein (S100β) in astrocytes, which promotes dystrophic neurite growth [41,71,75]. Inhibition of IL-1β activity has also been shown to promote neurogenesis via the Wnt/β-catenin signaling cascade by inhibiting GSK-3β activity and subsequent Tau phosphorylation [76]. The role of IL-1β in neurodegeneration, however, is not straightforward. One study shows a protective effect of IL-1β when overexpressed in the astrocytes of transgenic AD mice; Shaftel et al. showed that sustained activation of IL-1β results in a significant decrease in the hippocampal amyloid plaque load in these mouse brains [77].
Similar to IL-1, the cytokine IL-6 is found to be increased in AD patient tissue and it also induces the expression of APP [32,78,79]. Conversely, IL-6 levels increase after treatment of cultured glial cells with the carboxy terminal fragment of APP (the last 105 amino acids) [80]. While some have found that IL-6 enhances Aβ-induced neurodegeneration in primary rat neuronal cultures [81], others have found that overexpression of IL-6 in transgenic AD mouse brain results in increased gliosis and phagocytosis, attenuating Aβ deposition [82]. The contradictory nature of these findings can be bridged by the idea that neuroinflammation is a complex and fine balanced response, capable of being both beneficial and deleterious to the brain.
Alpha-1-antichymotrypsin (ACT) is an acute phase inflammatory protein and serine protease inhibitor found to be elevated in the CSF, serum and brain of AD patients [83-85]. In the normal brain, ACT is localized to astrocytes and in the AD brain it is overexpressed in the astrocytes surrounding amyloid plaques [83,86,87]. It has been implicated in the pathophysiology of AD as transgenic AD mice carrying the human ACT gene exhibit accelerated amyloid plaque pathology development [88,89] and cognitive decline. ACT has also been shown to exert pathological effects in vitro [90]. IL-1β has been shown to increase the expression of ACT in human astrocytes, with a subsequent increase in synthesis of APP [88,91]. ACT has been shown to enhance both amyloid and Tau-associated pathologies. It has been shown to bind the toxic Aβ peptide and accelerate its fibrilization [92-95]. Studies from our lab have shown that treatment of primary mouse neurons with purified ACT protein results in Tau phosphorylation and apoptosis, implying a role for ACT in neurofibrillary tangle formation and neuronal loss associated with AD [96]. Furthermore, we determined that transgenic mice expressing human Tau and human ACT show enhanced Tau phosphorylation upon IL-1β injection, which is mediated by c-Jun N-terminal Kinase (JNK) signaling, indicating ACT and IL-1β work in collaboration to enhance Tau pathology development [97].
Another inflammatory mediator whose expression has been shown to be regulated by the cytokines IL-1β and TNF-α is Cyclooxygenase-2 (COX-2), which is responsible for the production of prostaglandin. Its function in inflammation is to induce vasodilation, thus mediating the transport of immune cells to injured tissue [98]. Interestingly, neurons are the main cell types that show increased expression of COX-2 in the AD brain [99-102], suggesting its role in the inflammatory response.
COX-2 has been shown to not only correlate with AD pathology load (neurofibrillary tangles and neuritic plaques), but also with cognitive impairment [103].
NEUROINFLAMMATION AND CELL CYCLE DYSEREGULATION IN ALZHEIMER’S DISEASE
Recent studies have explored aberrant cell cycle events in compromised neurons in the AD brain. While mature neurons are terminally differentiated and post-mitotic, neurons in the human AD brain show expression of a number of cell cycle regulatory proteins including Cyclins B, D1, D2, D3 and E [104-106]. In addition to the aberrant expression of these cell cycle markers, binucleation has been observed in the hippocampal neurons of AD patients, indicating cell cycle progression followed by defective cytokinesis [107]. Our lab has also observed ectopic expression of Cyclins D1, E and P-cdc2 (CDK1) in transgenic AD mice expressing mutant variants of APP alone or together with Presenilin 1 (PS1) [108]. We found that APP is phosphorylated at Thr668 in a mitosis-specific manner, leading to its association with centrosomes and pathogenic processing to generate enhanced Aβ peptide and C99 fragment [108]. Furthermore, the treatment of differentiated cortical neurons with oligomeric Aβ42 fragment has been shown to induce expression of cell cycle markers necessary for G1/S transition and, once entered into S phase, neurons begin to duplicate their DNA, which subsequently leads to apoptosis [109]. These findings implicate cell cycle deregulation as a possible underlying factor in neuronal loss associated with AD.
Pathogenic stimuli such as inflammation and oxidative stress have been shown to induce cell cycle events in the compromised brain [106,110-112]. In fact, there is increasing evidence for DNA synthesis and ectopic expression of cell cycle proteins such as cyclin E, cyclin B, cdc2 and CDK4 in the vulnerable neuronal populations in AD [110,111,115-117] and the aberrant cell cycle events seem to coincide with microglial activation [113]. Supporting this, one study has shown that the media from microglia treated with Aβ can induce abnormal neuronal cell cycle and subsequently, death [114]. Studies by another group showed that these cell cycle events closely correlated with secretion of TNF-α [121]. Further, preincubation of Aβ-treated microglia with TNF-α antibody significantly reduced BrdU incorporation in neurons treated with the conditioned media, implying that TNF-α secreted by the microglia is responsible for the observed cell cycle events in neurons [121]. Another study used an in vivo adoptive transfer model, where purified microglia from transgenic AD mice were injected into wild type mice that were either inoculated with IgG or anti-TNF-α antibody. Mice inoculated with anti-TNF-α antibody showed significant decrease in neuronal cyclin D1 levels [115]. This was highlighted by the fact that AD transgenic mice crossed with TNF-α null mice show basal levels of cyclin D1 in neurons [115]. Finally, the group looked at the role of JNK as it was found to be elevated in the transgenic AD mice. Using the previously described in vitro system, they discovered that treatment of neurons with SP600125, a specific JNK inhibitor, decreased BrdU incorporation upon treatment with conditioned media, suggesting that TNF-αinduces cell cycle events through JNK signaling[115]. These studies indicate that it is likely that inflammation induced glial activation could lead

Central
Padmanabhan et al. (2015)Email:
JSM Alzheimer’s Dis Related Dementia 2(2): 1018 (2015) 5/11
to the aberrant expression of cell cycle proteins and subsequent neuronal death in the AD brain.
Expression of inflammation-associated genes is associated with cell cycle dysregulation. COX-2 has been implicated in cell cycle deregulation as its enhanced expression correlates with promotion of cancer growth and its inhibition declines the growth [116]. Studies have also drawn parallels between cell cycle changes and COX-2 expression in the neurons of AD brain. In addition to its elevated levels in the AD brain, COX2 is found to be co-localized with cyclin D1, cyclin E and phosphorylated retinoblastoma (Rb) protein in the pyramidal neurons, which may be indicative of aberrant cell cycle activation in neurons[117,118]. COX-2 homozygous transgenic mice show a marked decrease in the mRNA of the cdk inhibitor p18INK4 and exhibit accelerated glutamate-induced apoptotic damage, which could be attenuated by administration of the cdk inhibitor, flavopiridol [119]. This study also showed that wild type primary hippocampal neurons treated with the COX-2 inhibitor nimesulide diminishes glutamate-mediated apoptotic damage and inhibits subsequent phosphorylation of Rb [119].
TARGETING INFLAMMATION FOR TREATMENT OF ALZHEIMER’S DISEASE
In prospective case-cohort epidemiological studies, elevated serum levels of specific acute phase proteins have shown a positive correlation with development of AD [120-123]. Other studies have shown the beneficial effects of chronic use of non-steroidal anti-inflammatory drugs (NSAIDs) in slowing, or even preventing AD [124-127], and post mortem analysis of brain tissue from AD patients on NSAIDs has also revealed a consistent reduction in inflammation [128]. In vivo studies using transgenic AD mice show that long-term administration of the NSAID Ibuprofen both decreases neuroinflammation and improves cognition [113]. An early treatment regimen with Ibuprofen given to transgenic AD mice improved spatial learning and hippocampal-dependent memory function [129]. Early Ibuprofen administration also resulted in reduced amyloid plaque load, glial activation and expression of inflammatory mediators in the transgenic AD mouse brain [129-131]. Epidemiologists have been interested in studying patients with rheumatoid arthritis and osteoarthritis as these individuals exposed to NSAIDs for long periods of time show an inverse relationship between AD and treated arthritis [132].
It is debated how NSAIDs might exert these effects. Some studies find that NSAIDs act as modulators of γ-secrestase by interacting with APP itself and shifting the pathogenic cleavage site to yield a shorter Aβ fragment [133-136]. Others have suggested that NSAIDs are capable of lowering β-secretase levels [137]. Finally, an in vitro study by Hirohata et al. found that NSAIDs have a direct inhibitory effect on formation of Aβ fibrils [138]. These observations however, have not held up in clinical trials. Individuals with clinical AD symptoms that were treated with NSAIDs showed no beneficial effects [139-141]. It is possible that the inverse relationship between rheumatoid arthritis and AD could be due to the intrinsic factors underlying the autoimmune disorder. Injection of transgenic AD mice with granulocyte macrophage-colony stimulating factor (GM-CSF),
an inflammatory cytokine involved in leukocyte stimulation in rheumatoid arthritis, has been shown to reduce amyloid plaque burden, improve cognitive deficits and increase hippocampal synaptic area [142].
Many studies, however, maintain that there is a direct link in NSAID usage and reduced AD risk. A recent study modeled inflammation in AD through the activation of microglia by injecting lipopolysaccharide (LPS) into young AD mice, which were then aged. Tellingly, the administration of NSAIDs to young mice prevented AD pathology [113]. As a culmination of the reviewed relationship between inflammation, cell cycle dysregulation and Alzheimer’s disease, this study also indicated that early treatment leads to blockade of microglial activation and neuronal cell cycle events [113]. Late NSAID treatment in aged mice, while halting new neuronal cell cycle events, could not reverse existing ones [113]. This study underscores the close relationship between neuroinflammation and cell cycle in compromised neurons of the AD brain and suggests that early therapeutic intervention may lead to the best outcome.
CONCLUSIONIn Alzheimer’s disease, pathologically vulnerable neurons
undergo ectopic cell cycle events that are thought to result in neuronal apoptosis. Expression of cell cycle markers in these susceptible neuronal populations could be an improper attempt of regeneration of an injured nerve cell, unable to properly proceed through mitosis. Interestingly, ectopic cell cycle protein expression has been found to be induced by neuroinflammatory mediators. In addition to the histopathological hallmarks of AD, namely neuritic plaques and neurofibrillary tangles, AD brains also show neuroinflammation and neuronal loss. Gliosis and inflammatory mediators coexist with amyloid plaques and neurofibrillary tangles. It appears that neuroinflammation, while initially beneficial in protecting neurons from injury, can induce neurodegeneration upon chronic exposure. Furthermore, there is strong evidence for collaboration between expression of cell cycle regulators and inflammatory mediators within these pathologies. Epidemiological studies indicate that long-term use of NSAIDs positively correlate with a decreased risk in developing AD, however clinical trials using NSAIDs to treat patients with AD have been unsuccessful. Current research shows that preventative NSAID treatment could prove to be a beneficial strategy for treating AD. Studies in transgenic AD mice show that early NSAID treatment inhibits chronic inflammation within the brain and halts mitotic events in compromised neurons. It is unclear whether the downstream effects of cell cycle dysregulation triggers an inflammatory response or if neuroinflammation precedes these cell cycle events. In any case, it is likely that there is interplay between these complex biological events and timing is important in targeting these events for prevention of neurodegeneration associated with AD.
ACKNOWLEDGEMENTSThe work in JP’s lab was supported by grants from
Alzheimer’s Association (IIRG-08-90842), the National Institute on Aging (1R21AG031429-01A2) and the Byrd Institute Small Grant Program.

Central
Padmanabhan et al. (2015)Email:
JSM Alzheimer’s Dis Related Dementia 2(2): 1018 (2015) 6/11
REFERENCES1. Khan UA, Liu L, Provenzano FA, Berman DE, Profaci CP, Sloan R, et
al. Molecular drivers and cortical spread of lateral entorhinal cortex dysfunction in preclinical Alzheimer’s disease. Nat Neurosci. 2014; 17: 304-311.
2. Selkoe DJ. The molecular pathology of Alzheimer’s disease. Neuron. 1991; 6: 487-498.
3. Alzheimer A, Stelzmann RA, Schnitzlein HN, Murtagh FR. An English translation of Alzheimer’s 1907 paper, “Uber eine eigenartige Erkankung der Hirnrinde”. Clin Anat. 1995; 8: 429-431.
4. Kosik KS, Joachim CL, Selkoe DJ. Microtubule-associated protein tau (tau) is a major antigenic component of paired helical filaments in Alzheimer disease. Proceedings of the National Academy of Sciences of the United States of America. 1986; 83: 4044-4048.
5. Haga S, Akai K, Ishii T. Demonstration of microglial cells in and around senile (neuritic) plaques in the Alzheimer brain. An immunohistochemical study using a novel monoclonal antibody. Acta Neuropathol. 1989; 77: 569-575.
6. Itagaki S, McGeer PL, Akiyama H, Zhu S, Selkoe D. Relationship of microglia and astrocytes to amyloid deposits of Alzheimer disease. J Neuroimmunol. 1989; 24: 173-182.
7. Akiyama H, Mori H, Saido T, Kondo H, Ikeda K, McGeer PL. Occurrence of the diffuse amyloid beta-protein (Abeta) deposits with numerous Abeta-containing glial cells in the cerebral cortex of patients with Alzheimer’s disease. Glia. 1999; 25: 324-331.
8. Heneka MT, O’Banion MK. Inflammatory processes in Alzheimer’s disease. J Neuroimmunol. 2007; 184: 69-91.
9. Sasaki A, Shoji M, Harigaya Y, Kawarabayashi T, Ikeda M, Naito M, et al. Amyloid cored plaques in Tg2576 transgenic mice are characterized by giant plaques, slightly activated microglia, and the lack of paired helical filament-typed, dystrophic neurites. Virchows Archiv : an international journal of pathology. 2002; 441: 358-367.
10. Stalder M, Phinney A, Probst A, Sommer B, Staufenbiel M, Jucker M. Association of microglia with amyloid plaques in brains of APP23 transgenic mice. Am J Pathol. 1999; 154: 1673-1684.
11. Wegiel J, Imaki H, Wang KC, Wegiel J, Wronska A, Osuchowski M, et al. Origin and turnover of microglial cells in fibrillar plaques of APPsw transgenic mice. Acta Neuropathol. 2003; 105: 393-402.
12. Wegiel J, Wang KC, Imaki H, Rubenstein R, Wronska A, Osuchowski M, et al. The role of microglial cells and astrocytes in fibrillar plaque evolution in transgenic APP(SW) mice. Neurobiol Aging. 2001; 22: 49-61.
13. Gordon MN, Holcomb LA, Jantzen PT, DiCarlo G, Wilcock D, Boyett KW, et al. Time course of the development of Alzheimer-like pathology in the doubly transgenic PS1+APP mouse. Exp Neurol. 2002; 173: 183-195.
14. DeWitt DA, Perry G, Cohen M, Doller C, Silver J. Astrocytes regulate microglial phagocytosis of senile plaque cores of Alzheimer’s disease. Exp Neurol. 1998; 149: 329-340.
15. Meraz-Ríos MA, Toral-Rios D, Franco-Bocanegra D, Villeda-Hernández J, Campos-Peña V. Inflammatory process in Alzheimer’s Disease. Front Integr Neurosci. 2013; 7: 59.
16. Lawson LJ, Perry VH, Gordon S. Turnover of resident microglia in the normal adult mouse brain. Neuroscience. 1992; 48: 405-415.
17. Lue LF, Rydel R, Brigham EF, Yang LB, Hampel H, Murphy GM Jr, et al. Inflammatory repertoire of Alzheimer’s disease and nondemented elderly microglia in vitro. Glia. 2001; 35: 72-79.
18. Walker DG, Kim SU, McGeer PL. Complement and cytokine gene expression in cultured microglial derived from postmortem human brains. J Neurosci Res. 1995; 40: 478-493.
19. Kettenmann H, Hanisch UK, Noda M, Verkhratsky A. Physiology of microglia. Physiol Rev. 2011; 91: 461-553.
20. Combs CK, Johnson DE, Karlo JC, Cannady SB, Landreth GE. Inflammatory mechanisms in Alzheimer’s disease: inhibition of beta-amyloid-stimulated proinflammatory responses and neurotoxicity by PPARgamma agonists. J Neurosci. 2000; 20: 558-567.
21. Combs CK, Karlo JC, Kao SC, Landreth GE. beta-Amyloid stimulation of microglia and monocytes results in TNFalpha-dependent expression of inducible nitric oxide synthase and neuronal apoptosis. J Neurosci. 2001; 21: 1179-1788.
22. Del Bo R, Angeretti N, Lucca E, De Simoni MG, Forloni G. Reciprocal control of inflammatory cytokines, IL-1 and IL-6, and beta-amyloid production in cultures. Neurosci Lett. 1995; 188: 70-74.
23. Giulian D, Haverkamp LJ, Li J, Karshin WL, Yu J, Tom D, et al. Senile plaques stimulate microglia to release a neurotoxin found in Alzheimer brain. Neurochem Int. 1995; 27: 119-137.
24. Klegeris A, Walker DG, McGeer PL. Interaction of Alzheimer beta-amyloid peptide with the human monocytic cell line THP-1 results in a protein kinase C-dependent secretion of tumor necrosis factor-alpha. Brain Res. 1997; 747:114-121.
25. Sondag CM, Dhawan G, Combs CK. Beta amyloid oligomers and fibrils stimulate differential activation of primary microglia. J Neuroinflammation. 2009; 6: 1.
26. Dhawan G, Floden AM, Combs CK. Amyloid-β oligomers stimulate microglia through a tyrosine kinase dependent mechanism. Neurobiol Aging. 2012; 33: 2247-2261.
27. Bolmont T, Haiss F, Eicke D, Radde R, Mathis CA, Klunk WE, et al. Dynamics of the microglial/amyloid interaction indicate a role in plaque maintenance. J Neurosci. 2008; 28: 4283-4292.
28. Meyer-Luehmann M, Spires-Jones TL, Prada C, Garcia-Alloza M, de Calignon A, Rozkalne A, et al. Rapid appearance and local toxicity of amyloid-beta plaques in a mouse model of Alzheimer’s disease. Nature. 2008; 451: 720-724.
29. Permanne B, Adessi C, Saborio GP, Fraga S, Frossard MJ, Van Dorpe J, et al. Reduction of amyloid load and cerebral damage in a transgenic mouse model of Alzheimer’s disease by treatment with a beta-sheet breaker peptide. FASEB J. 2002; 16: 860-862.
30. Ho GJ, Drego R, Hakimian E, Masliah E. Mechanisms of cell signaling and inflammation in Alzheimer’s disease. Curr Drug Targets Inflamm Allergy. 2005; 4: 247-256.
31. Halliday G, Robinson SR, Shepherd C, Kril J. Alzheimer’s disease and inflammation: a review of cellular and therapeutic mechanisms. Clin Exp Pharmacol Physiol. 2000; 27: 1-8.
32. Ringheim GE, Szczepanik AM, Petko W, Burgher KL, Zhu SZ, Chao CC. Enhancement of beta-amyloid precursor protein transcription and expression by the soluble interleukin-6 receptor/interleukin-6 complex. Brain Res Mol Brain Res. 1998; 55: 35-44.
33. Misonou H, Morishima-Kawashima M, Ihara Y. Oxidative stress induces intracellular accumulation of amyloid beta-protein (Abeta) in human neuroblastoma cells. Biochemistry. 2000; 39: 6951-6959.
34. Martin LJ, Pardo CA, Cork LC, Price DL. Synaptic pathology and glial responses to neuronal injury precede the formation of senile plaques and amyloid deposits in the aging cerebral cortex. Am J Pathol. 1994; 145: 1358-1381.
35. Rainero I, Bo M, Ferrero M, Valfrè W, Vaula G, Pinessi L. Association

Central
Padmanabhan et al. (2015)Email:
JSM Alzheimer’s Dis Related Dementia 2(2): 1018 (2015) 7/11
between the interleukin-1alpha gene and Alzheimer’s disease: a meta-analysis. Neurobiol Aging. 2004; 25: 1293-1298.
36. Griffin WS, Nicoll JA, Grimaldi LM, Sheng JG, Mrak RE. The pervasiveness of interleukin-1 in alzheimer pathogenesis: a role for specific polymorphisms in disease risk. Exp Gerontol. 2000; 35: 481-487.
37. Nicoll JA, Mrak RE, Graham DI, Stewart J, Wilcock G, MacGowan S, et al. Association of interleukin-1 gene polymorphisms with Alzheimer’s disease. Ann Neurol. 2000; 47: 365-368.
38. Du Y, Dodel RC, Eastwood BJ, Bales KR, Gao F, Lohmüller F, et al. Association of an interleukin 1 alpha polymorphism with Alzheimer’s disease. Neurology. 2000; 55: 480-483.
39. Grimaldi LM, Casadei VM, Ferri C, Veglia F, Licastro F, Annoni G, et al. Association of early-onset Alzheimer’s disease with an interleukin-1alpha gene polymorphism. Ann Neurol. 2000; 47: 361-365.
40. Hedley R, Hallmayer J, Groth DM, Brooks WS, Gandy SE, Martins RN. Association of interleukin-1 polymorphisms with Alzheimer’s disease in Australia. Ann Neurol. 2002; 51: 795-797.
41. Griffin WS, Stanley LC, Ling C, White L, MacLeod V, Perrot LJ, et al. Brain interleukin 1 and S-100 immunoreactivity are elevated in Down syndrome and Alzheimer disease. Proc Natl Acad Sci U S A. 1989; 86: 7611-7615.
42. Griffin WS, Mrak RE. Interleukin-1 in the genesis and progression of and risk for development of neuronal degeneration in Alzheimer’s disease. J Leukoc Biol. 2002; 72: 233-238.
43. Finch CE, Morgan TE. Systemic inflammation, infection, ApoE alleles, and Alzheimer disease: a position paper. Curr Alzheimer Res. 2007; 4: 185-189.
44. Mrak RE, Griffin WS. Glia and their cytokines in progression of neurodegeneration. Neurobiol Aging. 2005; 26: 349-354.
45. Cacquevel M, Lebeurrier N, Chéenne S, Vivien D. Cytokines in neuroinflammation and Alzheimer’s disease. Curr Drug Targets. 2004; 5: 529-534.
46. Luster AD. Chemokines--chemotactic cytokines that mediate inflammation. N Engl J Med. 1998; 338: 436-445.
47. Fiala M, Zhang L, Gan X, Sherry B, Taub D, Graves MC, et al. Amyloid-beta induces chemokine secretion and monocyte migration across a human blood--brain barrier model. Mol Med. 1998; 4: 480-489.
48. Xia MQ, Qin SX, Wu LJ, Mackay CR, Hyman BT. Immunohistochemical study of the beta-chemokine receptors CCR3 and CCR5 and their ligands in normal and Alzheimer’s disease brains. Am J Pathol. 1998; 153: 31-37.
49. Meda L, Baron P, Prat E, Scarpini E, Scarlato G, Cassatella MA, et al. Proinflammatory profile of cytokine production by human monocytes and murine microglia stimulated with beta-amyloid[25-35]. J Neuroimmunol. 1999; 93: 45-52.
50. Blum-Degen D, Müller T, Kuhn W, Gerlach M, Przuntek H, Riederer P. Interleukin-1 beta and interleukin-6 are elevated in the cerebrospinal fluid of Alzheimer’s and de novo Parkinson’s disease patients. Neurosci Lett. 1995; 202: 17-20.
51. Jiang H, Hampel H, Prvulovic D, Wallin A, Blennow K, Li R, et al. Elevated CSF levels of TACE activity and soluble TNF receptors in subjects with mild cognitive impairment and patients with Alzheimer’s disease. Mol Neurodegener. 2011; 6: 69.
52. Mrak RE, Griffin WS. Potential inflammatory biomarkers in Alzheimer’s disease. J Alzheimers Dis. 2005; 8: 369-375.
53. Patel NS, Paris D, Mathura V, Quadros AN, Crawford FC, Mullan MJ.
Inflammatory cytokine levels correlate with amyloid load in transgenic mouse models of Alzheimer’s disease. J Neuroinflammation. 2005; 2: 9.
54. Tarkowski E, Issa R, Sjögren M, Wallin A, Blennow K, Tarkowski A, et al. Increased intrathecal levels of the angiogenic factors VEGF and TGF-beta in Alzheimer’s disease and vascular dementia. Neurobiol Aging. 2002; 23: 237-243.
55. Meager A. Seventh WHO informal consultation on standards for cytokines, growth factors and endocrinological substances. Biologicals: J Int Association Biological Standardization. 2004; 32: 105-111.
56. Meager A, Visvalingam K, Dilger P, Bryan D, Wadhwa M. Biological activity of interleukins-28 and -29: comparison with type I interferons. Cytokine. 2005; 31: 109-118.
57. Swardfager W, Lanctôt K, Rothenburg L, Wong A, Cappell J, Herrmann N. A meta-analysis of cytokines in Alzheimer’s disease. Biol Psychiatry. 2010; 68: 930-941.
58. Breder CD, Tsujimoto M, Terano Y, Scott DW, Saper CB. Distribution and characterization of tumor necrosis factor-alpha-like immunoreactivity in the murine central nervous system. J Comp Neurol. 1993; 337: 543-567.
59. Rubio-Perez JM, Morillas-Ruiz JM. A review: inflammatory process in Alzheimer’s disease, role of cytokines. ScientificWorldJournal. 2012; 2012: 756357.
60. Fillit H, Ding WH, Buee L, Kalman J, Altstiel L, Lawlor B, et al. Elevated circulating tumor necrosis factor levels in Alzheimer’s disease. Neurosci Lett. 1991; 129: 318-320.
61. Tarkowski E, Blennow K, Wallin A, Tarkowski A. Intracerebral production of tumor necrosis factor-alpha, a local neuroprotective agent, in Alzheimer disease and vascular dementia.J Clin Immunol. 1999; 19: 223-230.
62. Kamata H, Honda S, Maeda S, Chang L, Hirata H, Karin M. Reactive oxygen species promote TNFalpha-induced death and sustained JNK activation by inhibiting MAP kinase phosphatases. Cell. 2005; 120: 649-661.
63. Wajant H, Pfizenmaier K, Scheurich P. Tumor necrosis factor signaling. Cell Death Differ. 2003; 10: 45-65.
64. Lahiri DK, Chen D, Vivien D, Ge YW, Greig NH, Rogers JT. Role of cytokines in the gene expression of amyloid beta-protein precursor: identification of a 5’-UTR-binding nuclear factor and its implications in Alzheimer’s disease. J Alzheimers Dis. 2003; 5: 81-90.
65. Takeuchi H, Jin S, Wang J, Zhang G, Kawanokuchi J, Kuno R, et al. Tumor necrosis factor-alpha induces neurotoxicity via glutamate release from hemichannels of activated microglia in an autocrine manner. The Journal of biological chemistry. 2006; 281: 21362-21368.
66. McAlpine FE, Lee JK, Harms AS, Ruhn KA, Blurton-Jones M, Hong J, et al. Inhibition of soluble TNF signaling in a mouse model of Alzheimer’s disease prevents pre-plaque amyloid-associated neuropathology. Neurobiol Dis. 2009; 34: 163-177.
67. Tweedie D, Ferguson RA, Fishman K, Frankola KA, Van Praag H, Holloway HW, et al. Tumor necrosis factor-alpha synthesis inhibitor 3,6’-dithiothalidomide attenuates markers of inflammation, Alzheimer pathology and behavioral deficits in animal models of neuroinflammation and Alzheimer’s disease. Journal of neuroinflammation. 2012; 9: 106.
68. Montgomery SL, Mastrangelo MA, Habib D, Narrow WC, Knowlden SA, Wright TW, et al. Ablation of TNF-RI/RII expression in Alzheimer’s disease mice leads to an unexpected enhancement of pathology:

Central
Padmanabhan et al. (2015)Email:
JSM Alzheimer’s Dis Related Dementia 2(2): 1018 (2015) 8/11
implications for chronic pan-TNF-α suppressive therapeutic strategies in the brain. Am J Pathol. 2011; 179: 2053-2070.
69. Winter CD, Iannotti F, Pringle AK, Trikkas C, Clough GF, Church MK. A microdialysis method for the recovery of IL-1beta, IL-6 and nerve growth factor from human brain in vivo. J Neurosci Methods. 2002; 119: 45-50.
70. Woodroofe MN, Sarna GS, Wadhwa M, Hayes GM, Loughlin AJ, Tinker A, et al. Detection of interleukin-1 and interleukin-6 in adult rat brain, following mechanical injury, by in vivo microdialysis: evidence of a role for microglia in cytokine production. J Neuroimmunol. 1991; 33: 227-236.
71. Griffin WS, Sheng JG, Roberts GW, Mrak RE. Interleukin-1 expression in different plaque types in Alzheimer’s disease: significance in plaque evolution. J Neuropathol Exp Neurol. 1995; 54: 276-281.
72. Griffin WS, Sheng JG, Royston MC, Gentleman SM, McKenzie JE, Graham DI, et al. Glial-neuronal interactions in Alzheimer’s disease: the potential role of a ‘cytokine cycle’ in disease progression. Brain Pathol. 1998; 8: 65-72.
73. Prehn JH, Bindokas VP, Jordán J, Galindo MF, Ghadge GD, Roos RP, et al. Protective effect of transforming growth factor-beta 1 on beta-amyloid neurotoxicity in rat hippocampal neurons. Mol Pharmacol. 1996; 49: 319-328.
74. Goldgaber D, Harris HW, Hla T, Maciag T, Donnelly RJ, Jacobsen JS, et al. Interleukin 1 regulates synthesis of amyloid beta-protein precursor mRNA in human endothelial cells. Proc Natl Acad Sci U S A. 1989; 86: 7606-7610.
75. Li Y, Wang J, Sheng JG, Liu L, Barger SW, Jones RA, et al. S100 beta increases levels of beta-amyloid precursor protein and its encoding mRNA in rat neuronal cultures. J Neurochem. 1998; 71: 1421-1428.
76. Kitazawa M, Cheng D, Tsukamoto MR, Koike MA, Wes PD, Vasilevko V, et al. Blocking IL-1 signaling rescues cognition, attenuates tau pathology, and restores neuronal β-catenin pathway function in an Alzheimer’s disease model. J Immunol. 2011; 187: 6539-6549.
77. Shaftel SS, Kyrkanides S, Olschowka JA, Miller JN, Johnson RE, O’Banion MK. Sustained hippocampal IL-1 beta overexpression mediates chronic neuroinflammation and ameliorates Alzheimer plaque pathology. J Clin Invest. 2007; 117: 1595-1604.
78. Hüll M, Berger M, Volk B, Bauer J. Occurrence of interleukin-6 in cortical plaques of Alzheimer’s disease patients may precede transformation of diffuse into neuritic plaques. Ann N Y Acad Sci. 1996; 777: 205-212.
79. Altstiel LD, Sperber K. Cytokines in Alzheimer’s disease. Prog Neuropsychopharmacol Biol Psychiatry. 1991; 15: 481-495.
80. Chong Y. Effect of a carboxy-terminal fragment of the Alzheimer’s amyloid precursor protein on expression of proinflammatory cytokines in rat glial cells. Life Sci. 1997; 61: 2323-2333.
81. Qiu Z, Gruol DL. Interleukin-6, beta-amyloid peptide and NMDA interactions in rat cortical neurons. J Neuroimmunol. 2003; 139: 51-57.
82. Chakrabarty P, Jansen-West K, Beccard A, Ceballos-Diaz C, Levites Y, Verbeeck C, et al. Massive gliosis induced by interleukin-6 suppresses Abeta deposition in vivo: evidence against inflammation as a driving force for amyloid deposition. FASEB J. 2010; 24: 548-559.
83. Abraham CR, Selkoe DJ, Potter H. Immunochemical identification of the serine protease inhibitor alpha 1-antichymotrypsin in the brain amyloid deposits of Alzheimer’s disease. Cell. 1988; 52: 487-501.
84. Licastro F, Parnetti L, Morini MC, Davis LJ, Cucinotta D, Gaiti A, et al. Acute phase reactant alpha 1-antichymotrypsin is increased in
cerebrospinal fluid and serum of patients with probable Alzheimer disease. Alzheimer Dis Assoc Disord. 1995; 9: 112-128.
85. Licastro F, Mallory M, Hansen LA, Masliah E. Increased levels of alpha-1-antichymotrypsin in brains of patients with Alzheimer’s disease correlate with activated astrocytes and are affected by APOE 4 genotype. J Neuroimmunol. 1998; 88: 105-110.
86. Abraham CR, Shirahama T, Potter H. Alpha 1-antichymotrypsin is associated solely with amyloid deposits containing the beta-protein. Amyloid and cell localization of alpha 1-antichymotrypsin. Neurobiol Aging. 1990; 11: 123-129.
87. Pasternack JM, Abraham CR, Van Dyke BJ, Potter H, Younkin SG. Astrocytes in Alzheimer’s disease gray matter express alpha 1-antichymotrypsin mRNA. Am J Pathol. 1989; 135: 827-834.
88. Nilsson LN, Bales KR, DiCarlo G, Gordon MN, Morgan D, Paul SM, et al. Alpha-1-antichymotrypsin promotes beta-sheet amyloid plaque deposition in a transgenic mouse model of Alzheimer’s disease. J Neurosci. 2001; 21: 1444-1451.
89. Mucke L, Yu GQ, McConlogue L, Rockenstein EM, Abraham CR, Masliah E. Astroglial expression of human alpha(1)-antichymotrypsin enhances alzheimer-like pathology in amyloid protein precursor transgenic mice. Am J Pathol. 2000; 157: 2003-2010.
90. Nilsson LN, Arendash GW, Leighty RE, Costa DA, Low MA, Garcia MF, et al. Cognitive impairment in PDAPP mice depends on ApoE and ACT-catalyzed amyloid formation. Neurobiol Aging. 2004; 25: 1153-1167.
91. Das S, Potter H. Expression of the Alzheimer amyloid-promoting factor antichymotrypsin is induced in human astrocytes by IL-1. Neuron. 1995; 14: 447-456.
92. Ma J, Brewer HB Jr, Potter H. Alzheimer A beta neurotoxicity: promotion by antichymotrypsin, ApoE4; inhibition by A beta-related peptides. Neurobiol Aging. 1996; 17: 773-780.
93. Eriksson S, Janciauskiene S, Lannfelt L. Alpha 1-antichymotrypsin regulates Alzheimer beta-amyloid peptide fibril formation. Proc Natl Acad Sci U S A. 1995; 92: 2313-2317.
94. Fraser PE, Nguyen JT, McLachlan DR, Abraham CR, Kirschner DA. Alpha 1-antichymotrypsin binding to Alzheimer A beta peptides is sequence specific and induces fibril disaggregation in vitro. J Neurochem. 1993; 61: 298-305.
95. Abraham CR, McGraw WT, Slot F, Yamin R. Alpha 1-antichymotrypsin inhibits A beta degradation in vitro and in vivo. Ann N Y Acad Sci. 2000; 920: 245-248.
96. Padmanabhan J1, Levy M, Dickson DW, Potter H. Alpha1-antichymotrypsin, an inflammatory protein overexpressed in Alzheimer’s disease brain, induces tau phosphorylation in neurons. Brain. 2006; 129: 3020-3034.
97. Tyagi E, Fiorelli T, Norden M, Padmanabhan J. Alpha 1-Antichymotrypsin, an Inflammatory Protein Overexpressed in the Brains of Patients with Alzheimer’s Disease, Induces Tau Hyperphosphorylation through c-Jun N-Terminal Kinase Activation. Int J Alzheimers Dis. 2013; 2013: 606083.
98. Williams TJ. The role of prostaglandins in inflammation. Ann R Coll Surg Engl. 1978; 60: 198-201.
99. Hoozemans JJ, Rozemuller AJ, Janssen I, De Groot CJ, Veerhuis R, Eikelenboom P,. Cyclooxygenase expression in microglia and neurons in Alzheimer’s disease and control brain. Acta Neuropathol. 2001; 101: 2-8.
100. Pasinetti GM, Aisen PS. Cyclooxygenase-2 expression is increased in frontal cortex of Alzheimer’s disease brain. Neuroscience. 1998; 87: 319-324.

Central
Padmanabhan et al. (2015)Email:
JSM Alzheimer’s Dis Related Dementia 2(2): 1018 (2015) 9/11
101. Yermakova AV, Rollins J, Callahan LM, Rogers J, O’Banion MK. Cyclooxygenase-1 in human Alzheimer and control brain: quantitative analysis of expression by microglia and CA3 hippocampal neurons. J Neuropathol Exp Neurol. 1999; 58: 1135-1146.
102. Oka A, Takashima S. Induction of cyclo-oxygenase 2 in brains of patients with Down’s syndrome and dementia of Alzheimer type: specific localization in affected neurones and axons. Neuroreport. 1997; 8: 1161-1164.
103. Ho L, Purohit D, Haroutunian V, Luterman JD, Willis F, Naslund J, et al. Neuronal cyclooxygenase 2 expression in the hippocampal formation as a function of the clinical progression of Alzheimer disease. Arch Neurol. 2001; 58: 487-492.
104. Raina AK, Monteiro MJ, McShea A, Smith MA. The role of cell cycle-mediated events in Alzheimer’s disease. Int J Exp Pathol. 1999; 80: 71-76.
105. Busser J, Geldmacher DS, Herrup K. Ectopic cell cycle proteins predict the sites of neuronal cell death in Alzheimer’s disease brain. J Neurosci. 1998; 18: 2801-2807.
106. Vincent I, Jicha G, Rosado M, Dickson DW. Aberrant expression of mitotic cdc2/cyclin B1 kinase in degenerating neurons of Alzheimer’s disease brain. J Neurosci. 1997; 17: 3588-3598.
107. Zhu X, Siedlak SL, Wang Y, Perry G, Castellani RJ, Cohen ML, Smith MA. Neuronal binucleation in Alzheimer disease hippocampus. Neuropathol Appl Neurobiol. 2008; 34: 457-465.
108. Judge M, Hornbeck L, Potter H, Padmanabhan J. Mitosis-specific phosphorylation of amyloid precursor protein at threonine 668 leads to its altered processing and association with centrosomes. Mol Neurodegener. 2011; 6: 80.
109. Copani A, Condorelli F, Caruso A, Vancheri C, Sala A, Giuffrida Stella AM, et al. Mitotic signaling by beta-amyloid causes neuronal death. FASEB J. 1999; 13: 2225-2234.
110. Arendt T, Rödel L, Gärtner U, Holzer M. Expression of the cyclin-dependent kinase inhibitor p16 in Alzheimer’s disease. Neuroreport. 1996; 7: 3047-3049.
111. McShea A, Harris PL, Webster KR, Wahl AF, Smith MA. Abnormal expression of the cell cycle regulators P16 and CDK4 in Alzheimer’s disease. Am J Pathol. 1997; 150: 1933-1939.
112. Bonda DJ, Bajić VP, Spremo-Potparevic B, Casadesus G, Zhu X, Smith MA, et al. Review: cell cycle aberrations and neurodegeneration. Neuropathol Appl Neurobiol. 2010; 36: 157-163.
113. Varvel NH, Bhaskar K, Kounnas MZ, Wagner SL, Yang Y, Lamb BT, et al. NSAIDs prevent, but do not reverse, neuronal cell cycle reentry in a mouse model of Alzheimer disease. J Clin Invest. 2009; 119: 3692-3702.
114. Wu Q, Combs C, Cannady SB, Geldmacher DS, Herrup K. Beta-amyloid activated microglia induce cell cycling and cell death in cultured cortical neurons. Neurobiol Aging. 2000; 21: 797-806.
115. Bhaskar K, Maphis N, Xu G, Varvel NH, Kokiko-Cochran ON, Weick JP, et al. Microglial derived tumor necrosis factor-α drives Alzheimer’s disease-related neuronal cell cycle events. Neurobiol Dis. 2014; 62: 273-285.
116. Harris RE. Cyclooxygenase-2 (cox-2) and the inflammogenesis of cancer. Subcell Biochem. 2007; 42: 93-126.
117. Hoozemans JJ, Brückner MK, Rozemuller AJ, Veerhuis R, Eikelenboom P, Arendt T. Cyclin D1 and cyclin E are co-localized with cyclo-oxygenase 2 (COX-2) in pyramidal neurons in Alzheimer disease temporal cortex. J Neuropathol Exp Neurol. 2002; 61: 678-688.
118. Hoozemans JJ, Veerhuis R, Rozemuller AJ, Arendt T, Eikelenboom P. Neuronal COX-2 expression and phosphorylation of pRb precede p38 MAPK activation and neurofibrillary changes in AD temporal cortex. Neurobiol Dis. 2004; 15: 492-499.
119. Mirjany M, Ho L, Pasinetti GM. Role of cyclooxygenase-2 in neuronal cell cycle activity and glutamate-mediated excitotoxicity. J Pharmacol Exp Ther. 2002; 301: 494-500.
120. Dik MG, Jonker C, Hack CE, Smit JH, Comijs HC, Eikelenboom P. Serum inflammatory proteins and cognitive decline in older persons. Neurology. 2005; 64: 1371-1377.
121. Engelhart MJ, Geerlings MI, Meijer J, Kiliaan A, Ruitenberg A, van Swieten JC, et al. Inflammatory proteins in plasma and the risk of dementia: the rotterdam study. Arch Neurol. 2004; 61: 668-672.
122. Schmidt R, Schmidt H, Curb JD, Masaki K, White LR, Launer LJ. Early inflammation and dementia: a 25-year follow-up of the Honolulu-Asia Aging Study. Ann Neurol. 2002; 52: 168-174.
123. Yaffe K, Lindquist K, Penninx BW, Simonsick EM, Pahor M, Kritchevsky S, et al. Inflammatory markers and cognition in well-functioning African-American and white elders. Neurology. 2003; 61: 76-80.
124. McGeer PL, Schulzer M, McGeer EG. Arthritis and anti-inflammatory agents as possible protective factors for Alzheimer’s disease: a review of 17 epidemiologic studies. Neurology. 1996; 47: 425-432.
125. Stewart WF, Kawas C, Corrada M, Metter EJ. Risk of Alzheimer’s disease and duration of NSAID use. Neurology. 1997; 48: 626-632.
126. Vlad SC, Miller DR, Kowall NW, Felson DT. Protective effects of NSAIDs on the development of Alzheimer disease. Neurology. 2008; 70: 1672-1677.
127. in t’ Veld BA, Ruitenberg A, Hofman A, Launer LJ, van Duijn CM, Stijnen T, et al. Nonsteroidal antiinflammatory drugs and the risk of Alzheimer’s disease. N Engl J Med. 2001; 345: 1515-1521.
128. Mackenzie IR. Postmortem studies of the effect of anti-inflammatory drugs on Alzheimer-type pathology and associated inflammation. Neurobiol Aging. 2001; 22: 819-822.
129. Kukar T, Prescott S, Eriksen JL, Holloway V, Murphy MP, Koo EH, et al. Chronic administration of R-flurbiprofen attenuates learning impairments in transgenic amyloid precursor protein mice. BMC Neurosci. 2007; 8: 54.
130. Lim GP, Yang F, Chu T, Gahtan E, Ubeda O, Beech W, et al. Ibuprofen effects on Alzheimer pathology and open field activity in APPsw transgenic mice. Neurobiol Aging. 2001; 22: 983-991.
131. Lim GP, Yang F, Chu T, Chen P, Beech W, Teter B, et al. Ibuprofen suppresses plaque pathology and inflammation in a mouse model for Alzheimer’s disease. J Neurosci. 2000; 20: 5709-5714.
132. Zandi PP, Breitner JC. Do NSAIDs prevent Alzheimer’s disease? And, if so, why? The epidemiological evidence. Neurobiol Aging. 2001; 22: 811-817.
133. Avramovich Y, Amit T, Youdim MB. Non-steroidal anti-inflammatory drugs stimulate secretion of non-amyloidogenic precursor protein. J Biol Chem. 2002; 277: 31466-31473.
134. Eriksen JL, Sagi SA, Smith TE, Weggen S, Das P, McLendon DC, et al. NSAIDs and enantiomers of flurbiprofen target gamma-secretase and lower Abeta 42 in vivo. J Clin Invest. 2003; 112: 440-449.
135. Weggen S, Eriksen JL, Das P, Sagi SA, Wang R, Pietrzik CU, et al. A subset of NSAIDs lower amyloidogenic Abeta42 independently of cyclooxygenase activity. Nature. 2001; 414: 212-216.
136. Kukar TL, Ladd TB, Bann MA, Fraering PC, Narlawar R, Maharvi GM,

Central
Padmanabhan et al. (2015)Email:
JSM Alzheimer’s Dis Related Dementia 2(2): 1018 (2015) 10/11
et al. Substrate-targeting gamma-secretase modulators. Nature. 2008; 453: 925-929.
137. Sastre M, Dewachter I, Rossner S, Bogdanovic N, Rosen E, Borghgraef P, et al. Nonsteroidal anti-inflammatory drugs repress beta-secretase gene promoter activity by the activation of PPARgamma. Proc Natl Acad Sci U S A. 2006; 103: 443-448.
138. Hirohata M, Ono K, Naiki H, Yamada M. Non-steroidal anti-inflammatory drugs have anti-amyloidogenic effects for Alzheimer’s beta-amyloid fibrils in vitro. Neuropharmacology. 2005; 49: 1088-1099.
139. ADAPT Research Group, Martin BK, Szekely C, Brandt J, Piantadosi S, Breitner JC, et al. Cognitive function over time in the Alzheimer’s
Disease Anti-inflammatory Prevention Trial (ADAPT): results of a randomized, controlled trial of naproxen and celecoxib. Arch Neurol. 2008; 65: 896-905.
140. Aisen PS. The potential of anti-inflammatory drugs for the treatment of Alzheimer’s disease. Lancet Neurol. 2002; 1: 279-284.
141. van Gool WA, Aisen PS, Eikelenboom P. Anti-inflammatory therapy in Alzheimer’s disease: is hope still alive? J Neurol. 2003; 250: 788-792.
142. Boyd TD, Bennett SP, Mori T, Governatori N, Runfeldt M, Norden M, et al. GM-CSF upregulated in rheumatoid arthritis reverses cognitive impairment and amyloidosis in Alzheimer mice. J Alzheimers Dis. 2010; 21: 507-518.

Central
Padmanabhan et al. (2015)Email:
JSM Alzheimer’s Dis Related Dementia 2(2): 1018 (2015) 11/11
Kirouac L, Mathew M, Padmanabhan J (2015) Interplay between Inflammation and Cell Cycle Deregulation in Alzheimer’s Disease. JSM Alzheimer’s Dis Related Dementia 2(2): 1018.
Cite this article