Interim Analysis of ACE-011-REN-001: The First 28-Day Dose...
Transcript of Interim Analysis of ACE-011-REN-001: The First 28-Day Dose...

Interim Analysis of ACE-011-REN-001: The First 28-Day Dose Cycle of Low and Medium Starting Doses of Sotatercept Compared to Placebo for Correction of Anemia in Hemodialysis Subjects
Mohamed El-Shahawy1; James Cotton2; Jeffrey Kaupke3; Thomas D. Wooldridge4; Hem N. Singh5; William T. Smith51Academic Medical Research Institute, Los Angeles, CA, USA; 2Tyler Nephrology Associates PC, Tyler, TX, USA; 3Nephrology Specialist Medical Group, Orange, CA, USA; 4Nephrology & Hypertension Associates LTD, Tupelo, MS, USA; 5Celgene Corporation, Warren, NJ, USA
INTRODUCTION• The anemia seen in patients with end-stage kidney disease (ESKD) is largely due to decreased biosynthesis of erythropoietin from the kidneys.1-3
• A number of erythropoiesis-stimulating agents (ESAs) have demonstrated efficacy in increasing hemoglobin (Hb) levels in patients with ESKD,4,5 but pose significant safety risks, including persistent hypertension, serious cardiovascular events, and increased risk of death.4,5
• Multiple observational studies have linked low Hb levels to poor cardiovascular outcomes.6 However, recent clinical studies have demonstrated that ESAs are unable to modify this risk when targeting a normal Hb level.5,7-9
• Sotatercept (ACE-011) is an ActRIIA-IgG1 fusion protein trap that binds with high affinity to activin A and other members of the TGFb superfamily and acts on late-stage erythropoiesis to increase the production of mature erythrocytes into the circulation.10-12
• This 2-part, phase IIA, randomized, placebo-controlled trial is the first to evaluate the pharmacokinetics (PK), safety, tolerability, and Hb effect of sotatercept in ESKD subjects with renal anemia receiving hemodialysis.
• In part 1, after a single subcutaneous dose (0.1 mg/kg) of sotatercept13:
– PK parameters were similar to a phase I study in healthy postmenopausal women, with a long half-life (21 days).
– Sotatercept was not dialyzable.
– There was no evidence of a pharmacodynamic effect on Hb concentrations at the single, 0.1 mg/kg dose.
– Sotatercept was well tolerated with no observed changes in blood pressure (BP), and no consistent changes in safety laboratory or electrocardiographic parameters.
• Part 2 is an ongoing, randomized, single-blind, placebo-controlled, sequential dose-escalation study in subjects with ESKD on hemodialysis evaluating the PK, safety, tolerability, and Hb effects of sotatercept for the correction of ESKD-related anemia.
• We report the preliminary, interim analysis of the sotatercept 0.3 mg/kg (low dose) and 0.5 mg/kg (medium dose) treatment groups.
• Pending acceptable interim analysis results, additional patients may be randomized in a staggered parallel fashion to sotatercept 0.7 mg/kg once every 28 days (high dose) and sotatercept 0.7 mg/kg once every 14 days for 28 days followed by 0.4 mg/kg every 14 days for the remainder of the treatment period (Figure 1).
METHODSKey Inclusion Criteria• Adults receiving at least 3 hours of high-flux hemodialysis at each session for at least 12 weeks before screening and no planned changes to the hemodialysis regimen
during the study period
• Adequate Hb response (Hb ≥10 to ≤12 g/dL predialysis mean of 3 consecutive Hb concentrations) to stable doses of ESA (epoetin alfa, darbepoetin) for at least 6 weeks before and during screening, excluding dose holds for high Hb (maximum dose: epoetin alfa ≤500 IU/kg/week; darbepoetin ≤95 μg/week)
• ESKD-related anemia: Hb ≥8 to ≤10 g/dL predialysis after ESA washout
• Adequate iron status (transferrin saturation ≥20%)
• Kt/V ≥1.2 or urea reduction ratio ≥65%
• Parathyroid hormone concentration ≤1,000 pg/mL; phosphorous ≤7 mg/dL; and total albumin-corrected calcium ≥8.0 to ≤10.5 mg/dL
Key Exclusion Criteria• Anemia due to non-renal causes
• ESKD due to malignancy or history of malignancy (excluding excised and cured non-melanoma skin cancer and cervical carcinoma in situ)
• Systemic hematologic disease
• Peritoneal dialysis or compromised venous access
• Uncontrolled diabetes mellitus (HbA1C >9%), hypertension (home systolic BP [SBP] >160 mm Hg, home diastolic BP [DBP] >90 mm Hg), or heart failure (New York Heart Association class ≥3)
• Alanine transaminase and/or aspartate transaminase values >2× the upper limit of normal; C-reactive protein >50 mg/L
• Red blood cell transfusion <8 weeks before screening
• Anticipated or scheduled living donor renal transplant
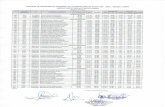
Study Design• This was a randomized, single-blind, placebo-controlled, sequential dose-escalation study in subjects with ESKD on hemodialysis (Figure 1).
• Eligible subjects were randomized to 2 arms (sotatercept or placebo in a 3:1 ratio) in 4 sequential dose groups (sotatercept 0.3 mg/kg, 0.5 mg/kg, 0.7 mg/kg, or 0.7 mg/kg loading dose followed by 0.4 mg/kg).
– This interim analysis informed the data monitoring committee’s decision to open enrollment for the high-dose group (sotatercept 0.7 mg/kg).
– At the time of abstract submission:
§ Enrollment in the sotatercept 0.3 mg/kg and 0.5 mg/kg dose groups was completed.
§ Enrollment in the sotatercept 0.7 mg/kg dose group was ongoing.
• Sotatercept doses could have been delayed, reduced, or discontinued based on the subject’s absolute predialysis Hb level or change in Hb level observed after dosing, or discontinued based on change in home BP measurements.
– Delayed: Hb ≥11 to <13 g/dL on Dose Cycle Day 36 (0.3, 0.5, and 0.7 mg/kg dose groups) or Dose Cycle Day 19 (0.7/0.4 mg/kg dose group)
– Reduced: If a dose was delayed, OR if Hb <11 g/dL AND rate of rise of >2 g/dL (0.3, 0.5, and 0.7 mg/kg dose groups) or >1 g/dL (0.7/0.4 mg/kg dose group)
– Discontinued:
§ Persistent hypertension recorded by home BP monitor mean of 4 days of home SBP >160 mm Hg AND increase in SBP from baseline of >20 mm Hg, or mean increase from baseline DBP of >10 mm Hg
§ Hb ≥13 g/dL at any time after randomization
§ Hb ≥12 to <13 g/dL for 2 consecutive weeks at any time after randomization
• Rescue treatment was recommended for subjects with Hb <9 g/dL after the first dose cycle, and those required to discontinue sotatercept could receive ESA treatment or red blood cell transfusion.
• All randomized subjects, including those who were rescued or discontinued early, continued to follow the visit schedule and home BP monitoring throughout the 200-day treatment phase and 112-day follow-up phase.
• The current report describes interim analysis of the sotatercept 0.3 mg/kg and 0.5 mg/kg dose groups for the purpose of determining safety of proceeding to the next dose group.
Figure 1. Study Design
Follow-up phase for 112 days for PK
and safety
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.3 mg/kgSC (n ~9) q28d,up to 8 doses
Placebo (n ~3)q28d, up to 8 doses
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.5 mg/kgSC (n ~9) q28d,up to 8 doses
Placebo (n ~3)q28d, up to 8 doses
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.7 mg/kgSC (n ~9) q28d,
up to 8 doses
Placebo (n ~3)q28d, up to 8 doses
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.7 mg/kg SC q14d(2 doses), then 0.4 mg/kg SC q14d
up to 13 doses (n ~9)
Placebo (n ~3)q14d, up to 15 doses
Note: All randomized subjects will continue treatment with sotatercept 0.3, 0.5, or 0.7 mg/kg or placebo for up to 8 doses* unless rescued or discontinued early. *At 0.7/0.4 mg/kg, all randomized subjects will continue treatment for up to 15 doses unless rescued or discontinued early.28 days after the 6th subject is dosed with sotatercept in each dose group (0.3, 0.5, and 0.7 mg/kg), an interim analysis will occur to evaluate PK and safety before opening the next dose group.
Table 3. Sotatercept PK in ESKD Subjects on Hemodialysis (Dose 1, Cycle 1)
Sotatercept
Parameter0.3 mg/kg
n=90.5 mg/kg
n=6
tmax, mean (min–max), day 12 (2–14) 7 (2–14)
Cmax, mean (SD), μg/mL 2.4 (0.96) 3.5 (0.73)
AUC28d, mean (SD), day•μg/mL 50.5 (17.4) 73.2 (11.5)
t1/2,z, mean (SD), day 22.3 (3.0)* 24.5 (8.9)*†
CL/F, mean (SD), mL/day/kg 3.65 (1.60)* 3.83 (1.19)*†
Vz/F, mean (SD), mL/kg 117 (54)* 124 (27.9)*†
AUC28d=area under the concentration-vs.-time curve up to 28 days; CL/F=oral clearance; Vz/F=apparent volume of distribution.*Estimated according to a 1-compartment model.†The 28-day data may not be sufficient for accurate estimation in some subjects.
Figure 2. Sotatercept Serum Concentration Over Time
Seru
m S
otat
erce
pt (µ
g/m
L)
5
4
3
2
1
0
Days After the First Dose
0 7 14 21 28
Sotatercept 0.3 mg/kg
Sotatercept 0.5 mg/kg
Safety• An overview of AEs is provided in Table 4.
• A decrease in serum calcium levels during follow-up in subjects who had received sotatercept 0.3 mg/kg was noted, without AEs of hypocalcemia.
• There were no other observed trends in laboratory, electrocardiogram, or vital sign parameters, including study visit and intra-dialytic BP, in either dose group of sotatercept during long-term follow-up.
• No anti-drug antibodies, injection site reactions, or hypersensitivity reactions were observed.
Table 4. Overview of AEs (Safety Population, N=20)
Placebo Sotatercept
n=50.3 mg/kg
n=90.5 mg/kg
n=6
Subjects, n (%)
Cumulative days on study 864 2046 634
Any AE 3 (60.0) 8 (88.8) 3 (50.0)
≥1 severe AE 2 (40.0) 2 (22.2) 2 (33.3)
≥1 serious AE 2 (40.0) 2 (22.2) 1 (16.7)
Death 1 (20.0) 0 (0.0) 0 (0.0)
AEs in ≥2 subjects in a treatment group, n (%)
Fatigue 1 (20.0) 2 (22.2) 0 (0.0)
Pain 0 (0.0) 2 (22.2) 0 (0.0)
Constipation 1 (20.0) 2 (22.2) 0 (0.0)
Hypertension 0 (0.0) 3 (33.3)* 0 (0.0)
*A total of 3 subjects randomized to sotatercept 0.3 mg/kg reported 4 AEs of hypertension; 3 of the 4 events occurred after rescue with erythropoietin.
EfficacyTarget Hb Increase (≥1 g/dL), and Target Hb Range (10–12 g/dL) During the First 28 Days
• Baseline Hb levels were 9.7 g/dL in subjects receiving placebo, 9.3 g/dL in subjects receiving sotatercept 0.3 mg/kg, and 8.9 g/dL in subjects receiving sotatercept 0.5 mg/kg.
• Hb increase ≥1.0 g/dL was achieved by 20% (placebo), 37.5% (sotatercept 0.3 mg/kg), and 40% (sotatercept 0.5 mg/kg) of subjects (Figure 3).
• The desired Hb range (10–12 g/dL) was achieved in 60% (placebo), 25% (sotatercept 0.3 mg/kg), and 60% (sotatercept 0.5 mg/kg) during the first dose cycle.
• Mean peak Hb increase in the first 28-day dose cycle was 0.1 g/dL in subjects receiving placebo, 0.5 g/dL in subjects receiving sotatercept 0.3 mg/kg, and 0.8 g/dL in subjects receiving sotatercept 0.5 mg/kg (Figure 4).
• Rescue therapy was required (Hb <9 g/dL) in 2 of 5 subjects after administration of placebo and 1 of 8 subjects after administration of sotatercept 0.3 mg/kg, while none required rescue after sotatercept 0.5 mg/kg (Figure 3).
Figure 3. Hb Increase During the First 28-Day Dose Cycle (Per-Protocol Population)*
0
30
20
10
40
60
50
70
80
90
100
Subj
ects
(%)
Placebo(n=5)
40
40
20
Sotatercept 0.3 mg/kg(n=8)
13
50
37
Sotatercept 0.5 mg/kg
(n=5)
60
40
0.1-0.9 g/dL
Required Rescue (Hb <9 g/dL)
≥1.0 g/dL
*Two subjects with a major protocol violation were excluded from efficacy analyses.
PK Assessment• Blood samples for analysis of sotatercept PK were collected at each study visit and on each sotatercept or placebo dosing day. Additional samples were obtained after
dose 1 at 4 hours post-dose on Day 1 and at 48 hours post-dose on Day 3.
• A validated, competitive enzyme-linked immunosorbent assay using anti‐human ActRIIA antibodies (R&D Systems, Minneapolis, MN) was used to measure the sotatercept serum concentration.
Hb Assessments• Blood samples for Hb assessment were obtained at all scheduled study visits, including before dosing.
Home BP Monitoring• Because of the burden of hypertension in the hemodialysis population, and the inherent variability in hemodialysis-related BP measurement, home BP monitoring was
used to provide a BP profile more reflective of the subject’s steady state.
• Subjects obtained their BP at home 2×/day (3 measurements each upon waking and at bedtime) for 4 consecutive days within 7 days of a scheduled dosing day. Each subject was trained to use a sponsor-provided BP monitor.
• At least 3 waking and 3 bedtime values downloaded from the device by study personnel were used to calculate mean BP values before screening, randomization, and re-dosing.
• Home BP monitoring continued for subjects requiring rescue.
Safety Assessments• Safety assessments included collection of adverse events (AEs), hematology testing, and vital signs at each visit and physical examination and 12-lead
electrocardiogram at selected scheduled time points.
– Safety assessments were done in the event of early termination/withdrawal.
• Proportions of subjects with Hb >12 g/dL at any time and rise in Hb >2 g/dL over 4 weeks were also determined.
• At each interim analysis, blood samples were analyzed for the presence of anti-sotatercept antibodies.
Statistical Analysis• Sotatercept multidose PK was examined among all subjects who received at least 1 dose of study medication and who had evaluable PK data.
• Sotatercept efficacy was evaluated in the full analysis set (FAS), which comprised all randomized subjects who received at least 1 dose of study medication and had at least 1 post-dose follow-up visit, and a baseline value (for analyses that require baseline comparison). Subjects assigned to placebo in both dose groups were combined to form a single placebo group for analysis purposes.
• Efficacy end points included:
– Proportion of subjects achieving target Hb increase (≥1 g/dL increase from baseline).
– Proportion of subjects achieving target Hb concentration >10 g/dL to <12 g/dL.
– Proportion of subjects requiring rescue therapy.
– Change from baseline Hb during the first 28-day dosing cycle, including peak Hb response.
• Proportional and continuous end points were summarized descriptively.
• The final mean home BP value was calculated by first determining the mean of 3 waking and 3 bedtime sets of BP measures. Next, the mean waking and mean bedtime values from a single day were both used to calculate the day mean. Finally, the mean of the day means was calculated, and this comprised the final mean home BP.
• Home BP measures and safety measures were summarized descriptively.
RESULTSSubjects• A total of 21 subjects were randomized and received study medication. One subject was randomized to sotatercept 0.5 mg/kg and received 1 dose of study medication;
however, this subject did not have the first follow-up visit at the time of the interim database cutoff point and was not included in either the safety or efficacy population. A total of 20 subjects comprise the FAS and safety population:
– 5 who received placebo.
– 9 who received sotatercept 0.3 mg/kg.
– 6 who received sotatercept 0.5 mg/kg.
• Interim subject disposition is illustrated in Table 1.
• Baseline subject demographics and disease characteristics were generally similar across treatment groups (Table 2).
• Major protocol violations were noted for 2 subjects randomized to sotatercept. One subject (0.3 mg/kg) received erythropoietin prior to randomization and through the first dose cycle, and was discontinued from the study; 1 subject (0.5 mg/kg) had an incomplete baseline home BP evaluation, which showed a non-qualifying elevation in BP prior to randomization, and was discontinued from study medication early. These subjects were excluded from efficacy analyses, as a per-protocol analysis defined in the protocol. Included in the efficacy analysis population were:
– 5 who received placebo.
– 8 who received sotatercept 0.3 mg/kg.
– 5 who received sotatercept 0.5 mg/kg.
Table 1. Subject Disposition (FAS, N=20)
GroupOngoing on Study Drug
D/C Study Drug (Being Followed)
Completers on Study Drug (≥200 Days)
Completers After D/C Study Drug Early Termination Total Rescued
D/C Study Drug Due to Stopping Rule
Placebo, n=5 0 2 1 1 1 3 0
Sotatercept 0.3 mg/kg, n=9 0 0 2 5 2 7 0
Sotatercept 0.5 mg/kg, n=6 3 2 0 0 1 2 1
D/C=discontinued.
Table 2. Demographic Characteristics of Subjects (FAS, N=20)
Placebo Sotatercept
n=50.3 mg/kg
n=90.5 mg/kg
n=6
Age, mean, years 58.4 59.9 60.7
Female, n (%) 1 (20.0) 6 (66.7) 1 (16.7)
Race, n (%)
White 1 (20.0) 3 (33.3) 4 (66.7)
Black 3 (60.0) 6 (66.7) 2 (33.3)
Asian 1 (20.0) 0 (0.0) 0 (0.0)
Ethnicity
Hispanic 0 (0.0) 2 (22.2) 4 (66.7)
Non-Hispanic 5 (100.0) 7 (77.8) 2 (33.3)
Weight, postdialysis mean, kg 75.8 79.4 81.0
Body mass index, mean, kg/m2 25.4 27.8 27.3
Sotatercept PK• Preliminary, interim PK data, based on analysis of all subjects randomized to sotatercept 0.3 mg/kg and the first 6 subjects randomized to sotatercept 0.5 mg/kg, are
presented in Table 3.
• Sotatercept exhibited dose-dependent increases in the serum drug exposure (Cmax and AUC), with a mean elimination half-life (t1/2,z) of 22 to 25 days.
• Sotatercept mean concentration-vs.-time profiles for the 0.3 mg/kg and 0.5 mg/kg dose groups are shown in Figure 2.
Figure 4. Mean Peak Hemoglobin Increase During the First 28-Day Dose Cycle (Per-Protocol Population)*
Sotatercept 0.3 mg/kg (n=8)
Sotatercept 0.5 mg/kg (n=5)
Placebo (n=5)
0.1
0.5
0.8
0
0.3
0.2
0.1
0.4
0.5
0.6
0.7
0.8
0.9
Hb (g
/dL)
Cha
nge
From
Bas
elin
e
Mean Peak Hemoglobin Response
*Two subjects with a major protocol violation were excluded from efficacy analyses.
Change From Baseline in Hb Concentration• Mean Hb concentration in subjects who received sotatercept 0.3 mg/kg and 0.5 mg/kg exhibited a greater increase from baseline in the first 15 days post-dose
(vs. placebo); however, the increases were not sustained through the entire dose cycle.
• Hb levels throughout multiple dose cycles among subjects who did not require rescue were generally highest among subjects receiving sotatercept 0.5 mg/kg (Figure 5).
Figure 5. Hb Change From Baseline During Long-term Sotatercept Treatment Censored for Rescue
−3
−2
−1
0
1
2
3
4
50 100 150 200 250
Days After the First Dose
Hem
oglo
bin
(g/d
L)
Sotatercept 0.3 mg/kg (n=8)Sotatercept 0.5 mg/kg (n=5)
Placebo (n=5)
Home BP Measurements• Home BP measures in the first dose cycle revealed that all 3 groups had increases in group mean SBP, with the largest change in subjects receiving sotatercept
0.3 mg/kg, while the largest change in DBP was in subjects receiving placebo. All the group mean changes were <10 mm Hg (Figure 6A and B).
– Findings were similar when analyzed for both the per-protocol population (Figure 6A) and FAS (Figure 6B).
• With long-term treatment, home BP measures showed no consistent change from baseline among subjects in any of the treatment groups (Figure 7).
Figure 6. Change From Baseline in Home BP at the End of Dose Cycle 1 in the (A) Per-Protocol Population* and (B) FAS
Sotatercept 0.3 mg/kg (n=7)
Sotatercept 0.5 mg/kg (n=4)
Placebo (n=3)
Sotatercept 0.3 mg/kg (n=9)
Sotatercept 0.5 mg/kg (n=5)
Placebo (n=4)
Chan
ge F
rom
Bas
elin
e BP
(mm
Hg)
0.0
2.0
6.0
3.3 3.3
–0.3 –1.0
0.0
1.0
2.0
3.0
4.0
5.0
6.0
7.0
SBP DBP
A
B
Chan
ge F
rom
Bas
elin
e BP
(mm
Hg)
2.3
7.5
3.0 2.5
7.6
0.4
0.0
1.0
2.0
3.0
4.0
5.0
6.0
7.0
8.0
SBP DBP
*Data exclude subjects with protocol violations and are censored for those who required rescue in the first dose cycle.
Figure 7. Change From Baseline Home BP Measurements (FAS) of (A) SBP and (B) DBP During Long-term Sotatercept Treatment, Censored for Rescue
A SBP
B DBP
–20
–15
–10
–5
0
5
10
15
20
25
50 100 150 200 250
Sotatercept 0.3 mg/kg (n=9)Sotatercept 0.5 mg/kg (n=5)
Placebo (n=4)
Hom
e DB
P (m
m H
g)
–50
–40
–30
–20
–10
0
10
20
30
40
50 100 150 200 250
Sotatercept 0.3 mg/kg (n=9)Sotatercept 0.5 mg/kg (n=5)
Placebo (n=4)
Hom
e SB
P (m
m H
g)
CONCLUSIONS• Sotatercept exhibited linear PK characteristics, and a long half-life of 22 to 25 days.
• Sotatercept was well tolerated, with AEs similar to those observed with placebo and no trends toward increased BP.
• Exposure to sotatercept was not associated with the development of anti-drug antibodies, injection site reactions, or hypersensitivity reactions.
• In the first 28 days of treatment, the proportion of subjects achieving the target Hb increase of ≥1 g/dL was greater in the treatment groups than in the placebo group, and the proportion requiring rescue therapy in the first 28 days was dose-related, with no subjects in the sotatercept 0.5 mg/kg group requiring rescue.
• In this initial 28-day analysis, in which the placebo and sotatercept 0.3 mg/kg groups had higher baseline Hb, no differences between groups achieving the target Hb range (10-12 g/dL) were observed. Dose escalation continues per protocol.
• Mean peak Hb response in the first 28 days was dose-related, with the sotatercept 0.5 mg/kg dose having the highest mean peak Hb response.
• Hb improvements were generally sustained for multiple dosing cycles in the sotatercept 0.5 mg/kg dose group.
• This preliminary interim analysis indicates adequate Hb responses and safety of sotatercept at 0.3 and 0.5 mg/kg and provides evidence to continue the evaluation of sotatercept at 0.7 mg/kg in patients with ESKD on hemodialysis.
REFERENCES1. Babitt JL, Lin HY. Mechanisms of anemia in CKD. J Am Soc Nephrol. 2012;23:1631-1634.
2. Jacobson LO, Goldwasser E, Fried W, et al. Role of the kidney in erythropoiesis. Nature. 1957;179:633-634.
3. McGonigle RJ, Wallin JD, Shadduck RK, et al. Erythropoietin deficiency and inhibition of erythropoiesis in renal insufficiency. Kidney Int. 1984;25:437-444.
4. Eschbach JW, Egrie JC, Downing MR, et al. Correction of the anemia of end-stage renal disease with recombinant human erythropoietin. Results of a combined phase I and II clinical trial. N Engl J Med. 1987;316:73-78.
5. Singh AK, Szczech L, Tang KL, et al. Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med. 2006;355: 2085-2098.
6. Fishbane S. Anemia and cardiovascular risk in the patient with kidney disease. Heart Fail Clin. 2008;4:401-410.
7. Besarab A, Bolton WK, Browne JK, et al. The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. N Engl J Med. 1998;339:584-590.
8. Drueke TB, Locatelli F, Clyne N, et al. Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med. 2006;355:2071-2084.
9. Pfeffer MA, Burdmann EA, Chen CY, et al. A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. N Engl J Med. 2009;361:2019-2032.
10. Pearsall RS, Canalis E, Cornwall-Brady M, et al. A soluble activin type IIA receptor induces bone formation and improves skeletal integrity. Proc Natl Acad Sci U S A. 2008;105:7082-7087.
11. Iancu-Rubin C, Mosoyan G, Wang J, et al. Stromal cell-mediated inhibition of erythropoiesis can be attenuated by sotatercept (ACE-011), an activin receptor type II ligand trap. Exp Hematol. 2013;41:155-166.
12. Sherman ML, Borgstein NG, Mook L, et al. Multiple-dose, safety, pharmacokinetic, and pharmacodynamic study of sotatercept (ActRIIA-IgG1), a novel erythropoietic agent, in healthy postmenopausal women. J Clin Pharmacol. 2013;53:1121-1130.
13. Wooldridge T, Kaplan M, Alcorn H Jr, et al. The pharmacokinetics and safety of a single-dose of sotatercept (ACE-011) in subjects on hemodialysis and the effects of its murine analog (RAP-011) on anemia and in preventing bone loss in C57BL/6 mice with 5/6 nephrectomy [oral presentation]. Presented at: American Society of Nephrology Kidney Week 2012; October 30-November 4, 2012; San Diego, CA.
This study was sponsored by Celgene Corporation.
Presented at: the National Kidney Foundation (NKF) 2014 Spring Clinical Meeting; April 22–26, 2014; Las Vegas, NV.Scan this QR code to receive
the PDF of the poster

Inte
rim A
naly
sis
of A
CE-0
11-R
EN-0
01: T
he F
irst 2
8-Da
y Do
se C
ycle
of L
ow a
nd M
ediu
m S
tart
ing
Dose
s
of S
otat
erce
pt C
ompa
red
to P
lace
bo fo
r Cor
rect
ion
of A
nem
ia in
Hem
odia
lysi
s Su
bjec
tsM
oham
ed E
l-Sha
haw
y1 ; Ja
mes
Cot
ton2 ;
Jeffr
ey K
aupk
e3 ; Th
omas
D. W
oold
ridge
4 ; He
m N
. Sin
gh5 ;
Will
iam
T. S
mith
51 A
cade
mic
Med
ical
Res
earc
h In
stitu
te, L
os A
ngel
es, C
A, U
SA; 2 T
yler
Nep
hrol
ogy
Asso
ciat
es P
C, Ty
ler,
TX, U
SA; 3 N
ephr
olog
y Sp
ecia
list M
edic
al G
roup
, Ora
nge,
CA,
USA
; 4 Nep
hrol
ogy
& Hy
perte
nsio
n As
soci
ates
LTD,
Tupe
lo, M
S, U
SA; 5 C
elge
ne C
orpo
ratio
n, W
arre
n, N
J, US
A
INTR
ODUC
TION
• Th
e an
emia
see
n in
pat
ient
s w
ith e
nd-s
tage
kid
ney
dise
ase
(ESK
D) is
larg
ely
due
to d
ecre
ased
bio
synt
hesi
s of
ery
thro
poie
tin fr
om th
e ki
dney
s.1-
3
• A
num
ber o
f ery
thro
poie
sis-
stim
ulat
ing
agen
ts (E
SAs)
hav
e de
mon
stra
ted
effic
acy
in in
crea
sing
hem
oglo
bin
(Hb)
leve
ls in
pat
ient
s w
ith E
SKD,
4,5 b
ut p
ose
sign
ifica
nt
safe
ty ri
sks,
incl
udin
g pe
rsis
tent
hyp
erte
nsio
n, s
erio
us c
ardi
ovas
cula
r eve
nts,
and
incr
ease
d ris
k of
dea
th.4,
5
• M
ultip
le o
bser
vatio
nal s
tudi
es h
ave
linke
d lo
w H
b le
vels
to p
oor c
ardi
ovas
cula
r out
com
es.6 H
owev
er, r
ecen
t clin
ical
stu
dies
hav
e de
mon
stra
ted
that
ESA
s ar
e un
able
to
mod
ify th
is ri
sk w
hen
targ
etin
g a
norm
al H
b le
vel.5,
7-9
• So
tate
rcep
t (AC
E-01
1) is
an
ActR
IIA-Ig
G1 fu
sion
pro
tein
trap
that
bin
ds w
ith h
igh
affin
ity to
act
ivin
A a
nd o
ther
mem
bers
of t
he T
GFb
supe
rfam
ily a
nd a
cts
on la
te-s
tage
er
ythr
opoi
esis
to in
crea
se th
e pr
oduc
tion
of m
atur
e er
ythr
ocyt
es in
to th
e ci
rcul
atio
n.10
-12
• Th
is 2
-par
t, ph
ase
IIA, r
ando
miz
ed, p
lace
bo-c
ontro
lled
trial
is th
e fir
st to
eva
luat
e th
e ph
arm
acok
inet
ics
(PK)
, saf
ety,
tole
rabi
lity,
and
Hb e
ffect
of s
otat
erce
pt in
ESK
D su
bjec
ts w
ith re
nal a
nem
ia re
ceiv
ing
hem
odia
lysi
s.
• In
par
t 1, a
fter a
sin
gle
subc
utan
eous
dos
e (0
.1 m
g/kg
) of s
otat
erce
pt13
:
–PK
par
amet
ers
wer
e si
mila
r to
a ph
ase
I stu
dy in
hea
lthy
post
men
opau
sal w
omen
, with
a lo
ng h
alf-
life
(21
days
).
–So
tate
rcep
t was
not
dia
lyza
ble.
–Th
ere
was
no
evid
ence
of a
pha
rmac
odyn
amic
effe
ct o
n Hb
con
cent
ratio
ns a
t the
sin
gle,
0.1
mg/
kg d
ose.
–So
tate
rcep
t was
wel
l tol
erat
ed w
ith n
o ob
serv
ed c
hang
es in
blo
od p
ress
ure
(BP)
, and
no
cons
iste
nt c
hang
es in
saf
ety
labo
rato
ry o
r ele
ctro
card
iogr
aphi
c pa
ram
eter
s.
• Pa
rt 2
is a
n on
goin
g, ra
ndom
ized
, sin
gle-
blin
d, p
lace
bo-c
ontro
lled,
seq
uent
ial d
ose-
esca
latio
n st
udy
in s
ubje
cts
with
ESK
D on
hem
odia
lysi
s ev
alua
ting
the
PK, s
afet
y, to
lera
bilit
y, an
d Hb
effe
cts
of s
otat
erce
pt fo
r the
cor
rect
ion
of E
SKD-
rela
ted
anem
ia.
• W
e re
port
the
prel
imin
ary,
inte
rim a
naly
sis
of th
e so
tate
rcep
t 0.3
mg/
kg (l
ow d
ose)
and
0.5
mg/
kg (m
ediu
m d
ose)
trea
tmen
t gro
ups.
• Pe
ndin
g ac
cept
able
inte
rim a
naly
sis
resu
lts, a
dditi
onal
pat
ient
s m
ay b
e ra
ndom
ized
in a
sta
gger
ed p
aral
lel f
ashi
on to
sot
ater
cept
0.7
mg/
kg o
nce
ever
y 28
day
s (h
igh
dose
) and
sot
ater
cept
0.7
mg/
kg o
nce
ever
y 14
day
s fo
r 28
days
follo
wed
by
0.4
mg/
kg e
very
14
days
for t
he re
mai
nder
of t
he tr
eatm
ent p
erio
d (F
igur
e 1)
.
MET
HODS
Key
Incl
usio
n Cr
iteria
• Ad
ults
rece
ivin
g at
leas
t 3 h
ours
of h
igh-
flux
hem
odia
lysi
s at
eac
h se
ssio
n fo
r at l
east
12
wee
ks b
efor
e sc
reen
ing
and
no p
lann
ed c
hang
es to
the
hem
odia
lysi
s re
gim
en
durin
g th
e st
udy
perio
d
• Ad
equa
te H
b re
spon
se (H
b ≥1
0 to
≤12
g/d
L pr
edia
lysi
s m
ean
of 3
con
secu
tive
Hb c
once
ntra
tions
) to
stab
le d
oses
of E
SA (e
poet
in a
lfa, d
arbe
poet
in) f
or a
t lea
st 6
wee
ks
befo
re a
nd d
urin
g sc
reen
ing,
exc
ludi
ng d
ose
hold
s fo
r hig
h Hb
(max
imum
dos
e: e
poet
in a
lfa ≤
500
IU/k
g/w
eek;
dar
bepo
etin
≤95
μg/
wee
k)
• ES
KD-r
elat
ed a
nem
ia: H
b ≥8
to ≤
10 g
/dL
pred
ialy
sis
afte
r ESA
was
hout
• Ad
equa
te ir
on s
tatu
s (tr
ansf
errin
sat
urat
ion
≥20%
)
• Kt
/V ≥
1.2
or u
rea
redu
ctio
n ra
tio ≥
65%
• Pa
rath
yroi
d ho
rmon
e co
ncen
tratio
n ≤1
,000
pg/
mL;
pho
spho
rous
≤7
mg/
dL; a
nd to
tal a
lbum
in-c
orre
cted
cal
cium
≥8.
0 to
≤10
.5 m
g/dL
Key
Excl
usio
n Cr
iteria
• An
emia
due
to n
on-r
enal
cau
ses
• ES
KD d
ue to
mal
igna
ncy
or h
isto
ry o
f mal
igna
ncy
(exc
ludi
ng e
xcis
ed a
nd c
ured
non
-mel
anom
a sk
in c
ance
r and
cer
vica
l car
cino
ma
in s
itu)
• Sy
stem
ic h
emat
olog
ic d
isea
se
• Pe
riton
eal d
ialy
sis
or c
ompr
omis
ed v
enou
s ac
cess
• Un
cont
rolle
d di
abet
es m
ellit
us (H
bA1C
>9%
), hy
perte
nsio
n (h
ome
syst
olic
BP
[SBP
] >16
0 m
m H
g, h
ome
dias
tolic
BP
[DBP
] >90
mm
Hg)
, or h
eart
failu
re (N
ew Y
ork
Hear
t As
soci
atio
n cl
ass
≥3)
• Al
anin
e tra
nsam
inas
e an
d/or
asp
arta
te tr
ansa
min
ase
valu
es >
2× th
e up
per l
imit
of n
orm
al; C
-rea
ctiv
e pr
otei
n >
50 m
g/L
• Re
d bl
ood
cell
trans
fusi
on <
8 w
eeks
bef
ore
scre
enin
g
• An
ticip
ated
or s
ched
uled
livi
ng d
onor
rena
l tra
nspl
ant
Stud
y De
sign
• Th
is w
as a
rand
omiz
ed, s
ingl
e-bl
ind,
pla
cebo
-con
trolle
d, s
eque
ntia
l dos
e-es
cala
tion
stud
y in
sub
ject
s w
ith E
SKD
on h
emod
ialy
sis
(Fig
ure
1).
• El
igib
le s
ubje
cts
wer
e ra
ndom
ized
to 2
arm
s (s
otat
erce
pt o
r pla
cebo
in a
3:1
ratio
) in
4 se
quen
tial d
ose
grou
ps (s
otat
erce
pt 0
.3 m
g/kg
, 0.5
mg/
kg, 0
.7 m
g/kg
, or
0.7
mg/
kg lo
adin
g do
se fo
llow
ed b
y 0.
4 m
g/kg
).
–Th
is in
terim
ana
lysi
s in
form
ed th
e da
ta m
onito
ring
com
mitt
ee’s
dec
isio
n to
ope
n en
rollm
ent f
or th
e hi
gh-d
ose
grou
p (s
otat
erce
pt 0
.7 m
g/kg
).
–At
the
time
of a
bstra
ct s
ubm
issi
on:
§En
rollm
ent i
n th
e so
tate
rcep
t 0.3
mg/
kg a
nd 0
.5 m
g/kg
dos
e gr
oups
was
com
plet
ed.
§En
rollm
ent i
n th
e so
tate
rcep
t 0.7
mg/
kg d
ose
grou
p w
as o
ngoi
ng.
• So
tate
rcep
t dos
es c
ould
hav
e be
en d
elay
ed, r
educ
ed, o
r dis
cont
inue
d ba
sed
on th
e su
bjec
t’s a
bsol
ute
pred
ialy
sis
Hb le
vel o
r cha
nge
in H
b le
vel o
bser
ved
afte
r dos
ing,
or
dis
cont
inue
d ba
sed
on c
hang
e in
hom
e BP
mea
sure
men
ts.
–De
laye
d: H
b ≥1
1 to
<13
g/d
L on
Dos
e Cy
cle
Day
36 (0
.3, 0
.5, a
nd 0
.7 m
g/kg
dos
e gr
oups
) or D
ose
Cycl
e Da
y 19
(0.7
/0.4
mg/
kg d
ose
grou
p)
–Re
duce
d: If
a d
ose
was
del
ayed
, OR
if Hb
<11
g/d
L AN
D ra
te o
f ris
e of
>2
g/dL
(0.3
, 0.5
, and
0.7
mg/
kg d
ose
grou
ps) o
r >1
g/dL
(0.7
/0.4
mg/
kg d
ose
grou
p)
–Di
scon
tinue
d:
§Pe
rsis
tent
hyp
erte
nsio
n re
cord
ed b
y ho
me
BP m
onito
r mea
n of
4 d
ays
of h
ome
SBP
>16
0 m
m H
g AN
D in
crea
se in
SBP
from
bas
elin
e of
>20
mm
Hg,
or m
ean
incr
ease
from
bas
elin
e DB
P of
>10
mm
Hg
§Hb
≥13
g/d
L at
any
tim
e af
ter r
ando
miz
atio
n
§Hb
≥12
to <
13 g
/dL
for 2
con
secu
tive
wee
ks a
t any
tim
e af
ter r
ando
miz
atio
n
• Re
scue
trea
tmen
t was
reco
mm
ende
d fo
r sub
ject
s w
ith H
b <
9 g/
dL a
fter t
he fi
rst d
ose
cycl
e, a
nd th
ose
requ
ired
to d
isco
ntin
ue s
otat
erce
pt c
ould
rece
ive
ESA
treat
men
t or
red
bloo
d ce
ll tra
nsfu
sion
.
• Al
l ran
dom
ized
sub
ject
s, in
clud
ing
thos
e w
ho w
ere
resc
ued
or d
isco
ntin
ued
early
, con
tinue
d to
follo
w th
e vi
sit s
ched
ule
and
hom
e BP
mon
itorin
g th
roug
hout
the
200-
day
treat
men
t pha
se a
nd 1
12-d
ay fo
llow
-up
phas
e.
• Th
e cu
rren
t rep
ort d
escr
ibes
inte
rim a
naly
sis
of th
e so
tate
rcep
t 0.3
mg/
kg a
nd 0
.5 m
g/kg
dos
e gr
oups
for t
he p
urpo
se o
f det
erm
inin
g sa
fety
of p
roce
edin
g to
the
next
do
se g
roup
.
Figu
re 1
. Stu
dy D
esig
n
Follo
w-u
p ph
ase
for
112
days
for P
K a
nd s
afet
y
Scre
enin
g an
dES
A w
asho
ut(D
ay –
90 to
Day
–1)
Sota
terc
ept 0
.3 m
g/kg
SC (n
~9)
q28
d,up
to 8
dos
es
Plac
ebo
(n ~
3)q2
8d, u
p to
8 d
oses
Scre
enin
g an
dES
A w
asho
ut(D
ay –
90 to
Day
–1)
Sota
terc
ept 0
.5 m
g/kg
SC (n
~9)
q28
d,up
to 8
dos
es
Plac
ebo
(n ~
3)q2
8d, u
p to
8 d
oses
Scre
enin
g an
dES
A w
asho
ut(D
ay –
90 to
Day
–1)
Sota
terc
ept 0
.7 m
g/kg
SC (n
~9)
q28
d,
up to
8 d
oses
Plac
ebo
(n ~
3)q2
8d, u
p to
8 d
oses
Scre
enin
g an
dES
A w
asho
ut(D
ay –
90 to
Day
–1)
Sota
terc
ept 0
.7 m
g/kg
SC
q14d
(2 d
oses
), th
en 0
.4 m
g/kg
SC
q14d
up to
13
dose
s (n
~9)
Plac
ebo
(n ~
3)q1
4d, u
p to
15
dose
s
Note
: All
rand
omiz
ed s
ubje
cts
will
con
tinue
trea
tmen
t with
sot
ater
cept
0.3
, 0.5
, or 0
.7 m
g/kg
or p
lace
bo fo
r up
to 8
dos
es*
unle
ss re
scue
d or
dis
cont
inue
d ea
rly.
*At 0
.7/0
.4 m
g/kg
, all
rand
omiz
ed s
ubje
cts
will
con
tinue
trea
tmen
t for
up
to 1
5 do
ses
unle
ss re
scue
d or
dis
cont
inue
d ea
rly.
28 d
ays
afte
r the
6th
sub
ject
is d
osed
with
sot
ater
cept
in e
ach
dose
gro
up (0
.3, 0
.5, a
nd 0
.7 m
g/kg
), an
inte
rim a
naly
sis
will
occ
ur to
eva
luat
e PK
and
saf
ety
befo
re o
peni
ng th
e ne
xt d
ose
grou
p.
Tabl
e 3.
Sot
ater
cept
PK
in E
SKD
Subj
ects
on
Hem
odia
lysi
s (D
ose
1, C
ycle
1)
Sota
terc
ept
Para
met
er0.
3 m
g/kg
n=9
0.5
mg/
kg
n=6
t max
, mea
n (m
in–m
ax),
day
12 (2
–14)
7 (2
–14)
C max
, mea
n (S
D), μ
g/m
L2.
4 (0
.96)
3.5
(0.7
3)
AUC 28
d, m
ean
(SD)
, day
•μg/
mL
50.5
(17.
4)73
.2 (1
1.5)
t 1/2,
z, m
ean
(SD)
, day
22.3
(3.0
)*24
.5 (8
.9)*
†
CL/F
, mea
n (S
D), m
L/da
y/kg
3.65
(1.6
0)*
3.83
(1.1
9)*†
V z/F, m
ean
(SD)
, mL/
kg11
7 (5
4)*
124
(27.
9)*†
AUC 28
d=ar
ea u
nder
the
conc
entra
tion-
vs.-
time
curv
e up
to 2
8 da
ys; C
L/F=
oral
cle
aran
ce; V
z/F=
appa
rent
vol
ume
of d
istri
butio
n.*E
stim
ated
acc
ordi
ng to
a 1
-com
partm
ent m
odel
.† T
he 2
8-da
y da
ta m
ay n
ot b
e su
ffici
ent f
or a
ccur
ate
estim
atio
n in
som
e su
bjec
ts.
Figu
re 2
. Sot
ater
cept
Ser
um C
once
ntra
tion
Over
Tim
e
Serum Sotatercept (µg/mL)
5 4 3 2 1 0
Days
Afte
r the
Firs
t Dos
e
07
1421
28
Sota
terc
ept 0
.3 m
g/kg
Sota
terc
ept 0
.5 m
g/kg
Safe
ty•
An o
verv
iew
of A
Es is
pro
vide
d in
Tab
le 4
.
• A
decr
ease
in s
erum
cal
cium
leve
ls d
urin
g fo
llow
-up
in s
ubje
cts
who
had
rece
ived
sot
ater
cept
0.3
mg/
kg w
as n
oted
, with
out A
Es o
f hyp
ocal
cem
ia.
• Th
ere
wer
e no
oth
er o
bser
ved
trend
s in
labo
rato
ry, e
lect
roca
rdio
gram
, or v
ital s
ign
para
met
ers,
incl
udin
g st
udy
visi
t and
intra
-dia
lytic
BP,
in e
ither
dos
e gr
oup
of
sota
terc
ept d
urin
g lo
ng-t
erm
follo
w-u
p.
• No
ant
i-dru
g an
tibod
ies,
inje
ctio
n si
te re
actio
ns, o
r hyp
erse
nsiti
vity
reac
tions
wer
e ob
serv
ed.
Tabl
e 4.
Ove
rvie
w o
f AEs
(Saf
ety
Popu
latio
n, N
=20
)
Plac
ebo
Sota
terc
ept
n=5
0.3
mg/
kg
n=9
0.5
mg/
kg
n=6
Subj
ects
, n (%
)
Cum
ulat
ive
days
on
stud
y86
420
4663
4
Any
AE3
(60.
0)8
(88.
8)3
(50.
0)
≥1 s
ever
e AE
2 (4
0.0)
2 (2
2.2)
2 (3
3.3)
≥1 s
erio
us A
E2
(40.
0)2
(22.
2)1
(16.
7)
Deat
h1
(20.
0)0
(0.0
)0
(0.0
)
AEs
in ≥
2 su
bjec
ts in
a tr
eatm
ent g
roup
, n (%
)
Fatig
ue1
(20.
0)2
(22.
2)0
(0.0
)
Pain
0 (0
.0)
2 (2
2.2)
0 (0
.0)
Cons
tipat
ion
1 (2
0.0)
2 (2
2.2)
0 (0
.0)
Hype
rtens
ion
0 (0
.0)
3 (3
3.3)
*0
(0.0
)
*A to
tal o
f 3 s
ubje
cts
rand
omiz
ed to
sot
ater
cept
0.3
mg/
kg re
porte
d 4
AEs
of h
yper
tens
ion;
3 o
f the
4 e
vent
s oc
curr
ed a
fter r
escu
e w
ith e
ryth
ropo
ietin
.
Effic
acy
Targ
et H
b In
crea
se (≥
1 g/
dL),
and
Targ
et H
b Ra
nge
(10–
12 g
/dL)
Dur
ing
the
Firs
t 28
Days
• Ba
selin
e Hb
leve
ls w
ere
9.7
g/dL
in s
ubje
cts
rece
ivin
g pl
aceb
o, 9
.3 g
/dL
in s
ubje
cts
rece
ivin
g so
tate
rcep
t 0.3
mg/
kg, a
nd 8
.9 g
/dL
in s
ubje
cts
rece
ivin
g so
tate
rcep
t 0.
5 m
g/kg
.
• Hb
incr
ease
≥1.
0 g/
dL w
as a
chie
ved
by 2
0% (p
lace
bo),
37.5
% (s
otat
erce
pt 0
.3 m
g/kg
), an
d 40
% (s
otat
erce
pt 0
.5 m
g/kg
) of s
ubje
cts
(Fig
ure
3).
• Th
e de
sire
d Hb
rang
e (1
0–12
g/d
L) w
as a
chie
ved
in 6
0% (p
lace
bo),
25%
(sot
ater
cept
0.3
mg/
kg),
and
60%
(sot
ater
cept
0.5
mg/
kg) d
urin
g th
e fir
st d
ose
cycl
e.
• M
ean
peak
Hb
incr
ease
in th
e fir
st 2
8-da
y do
se c
ycle
was
0.1
g/d
L in
sub
ject
s re
ceiv
ing
plac
ebo,
0.5
g/d
L in
sub
ject
s re
ceiv
ing
sota
terc
ept 0
.3 m
g/kg
, and
0.8
g/d
L
in s
ubje
cts
rece
ivin
g so
tate
rcep
t 0.5
mg/
kg (F
igur
e 4)
.
• Re
scue
ther
apy
was
requ
ired
(Hb
<9
g/dL
) in
2 of
5 s
ubje
cts
afte
r adm
inis
tratio
n of
pla
cebo
and
1 o
f 8 s
ubje
cts
afte
r adm
inis
tratio
n of
sot
ater
cept
0.3
mg/
kg, w
hile
no
ne re
quire
d re
scue
afte
r sot
ater
cept
0.5
mg/
kg (F
igur
e 3)
.
Figu
re 3
. Hb
Incr
ease
Dur
ing
the
Firs
t 28-
Day
Dose
Cyc
le (P
er-P
roto
col P
opul
atio
n)*
030 20 104060 50708090100
Subjects (%)
Plac
ebo
(n=
5)
404020
Sota
terc
ept 0
.3 m
g/kg
(n=
8)
135037
So
tate
rcep
t 0.5
mg/
kg(n
=5)
6040
0.1-
0.9
g/dL
Requ
ired
Resc
ue (H
b <
9 g/
dL)
≥1.0
g/d
L
*Tw
o su
bjec
ts w
ith a
maj
or p
roto
col v
iola
tion
wer
e ex
clud
ed fr
om e
ffica
cy a
naly
ses.
PK A
sses
smen
t•
Bloo
d sa
mpl
es fo
r ana
lysi
s of
sot
ater
cept
PK
wer
e co
llect
ed a
t eac
h st
udy
visi
t and
on
each
sot
ater
cept
or p
lace
bo d
osin
g da
y. Ad
ditio
nal s
ampl
es w
ere
obta
ined
afte
r do
se 1
at 4
hou
rs p
ost-
dose
on
Day
1 an
d at
48
hour
s po
st-d
ose
on D
ay 3
.
• A
valid
ated
, com
petit
ive
enzy
me-
linke
d im
mun
osor
bent
ass
ay u
sing
ant
i‐hum
an A
ctRI
IA a
ntib
odie
s (R
&D S
yste
ms,
Min
neap
olis
, MN)
was
use
d to
mea
sure
the
sota
terc
ept s
erum
con
cent
ratio
n.
Hb A
sses
smen
ts•
Bloo
d sa
mpl
es fo
r Hb
asse
ssm
ent w
ere
obta
ined
at a
ll sc
hedu
led
stud
y vi
sits
, inc
ludi
ng b
efor
e do
sing
.
Hom
e BP
Mon
itorin
g•
Beca
use
of th
e bu
rden
of h
yper
tens
ion
in th
e he
mod
ialy
sis
popu
latio
n, a
nd th
e in
here
nt v
aria
bilit
y in
hem
odia
lysi
s-re
late
d BP
mea
sure
men
t, ho
me
BP m
onito
ring
was
us
ed to
pro
vide
a B
P pr
ofile
mor
e re
flect
ive
of th
e su
bjec
t’s s
tead
y st
ate.
• Su
bjec
ts o
btai
ned
thei
r BP
at h
ome
2×/d
ay (3
mea
sure
men
ts e
ach
upon
wak
ing
and
at b
edtim
e) fo
r 4 c
onse
cutiv
e da
ys w
ithin
7 d
ays
of a
sch
edul
ed d
osin
g da
y.
Each
sub
ject
was
trai
ned
to u
se a
spo
nsor
-pro
vide
d BP
mon
itor.
• At
leas
t 3 w
akin
g an
d 3
bedt
ime
valu
es d
ownl
oade
d fro
m th
e de
vice
by
stud
y pe
rson
nel w
ere
used
to c
alcu
late
mea
n BP
val
ues
befo
re s
cree
ning
, ran
dom
izat
ion,
an
d re
-dos
ing.
• Ho
me
BP m
onito
ring
cont
inue
d fo
r sub
ject
s re
quiri
ng re
scue
.
Safe
ty A
sses
smen
ts•
Safe
ty a
sses
smen
ts in
clud
ed c
olle
ctio
n of
adv
erse
eve
nts
(AEs
), he
mat
olog
y te
stin
g, a
nd v
ital s
igns
at e
ach
visi
t and
phy
sica
l exa
min
atio
n an
d 12
-lead
el
ectro
card
iogr
am a
t sel
ecte
d sc
hedu
led
time
poin
ts.
–Sa
fety
ass
essm
ents
wer
e do
ne in
the
even
t of e
arly
term
inat
ion/
with
draw
al.
• Pr
opor
tions
of s
ubje
cts
with
Hb
>12
g/d
L at
any
tim
e an
d ris
e in
Hb
>2
g/dL
ove
r 4 w
eeks
wer
e al
so d
eter
min
ed.
• At
eac
h in
terim
ana
lysi
s, b
lood
sam
ples
wer
e an
alyz
ed fo
r the
pre
senc
e of
ant
i-sot
ater
cept
ant
ibod
ies.
Stat
istic
al A
naly
sis
• So
tate
rcep
t mul
tidos
e PK
was
exa
min
ed a
mon
g al
l sub
ject
s w
ho re
ceiv
ed a
t lea
st 1
dos
e of
stu
dy m
edic
atio
n an
d w
ho h
ad e
valu
able
PK
data
.
• So
tate
rcep
t effi
cacy
was
eva
luat
ed in
the
full
anal
ysis
set
(FAS
), w
hich
com
pris
ed a
ll ra
ndom
ized
sub
ject
s w
ho re
ceiv
ed a
t lea
st 1
dos
e of
stu
dy m
edic
atio
n an
d ha
d at
le
ast 1
pos
t-do
se fo
llow
-up
visi
t, an
d a
base
line
valu
e (fo
r ana
lyse
s th
at re
quire
bas
elin
e co
mpa
rison
). Su
bjec
ts a
ssig
ned
to p
lace
bo in
bot
h do
se g
roup
s w
ere
com
bine
d to
form
a s
ingl
e pl
aceb
o gr
oup
for a
naly
sis
purp
oses
.
• Ef
ficac
y en
d po
ints
incl
uded
:
–Pr
opor
tion
of s
ubje
cts
achi
evin
g ta
rget
Hb
incr
ease
(≥1
g/dL
incr
ease
from
bas
elin
e).
–Pr
opor
tion
of s
ubje
cts
achi
evin
g ta
rget
Hb
conc
entra
tion
>10
g/d
L to
<12
g/d
L.
–Pr
opor
tion
of s
ubje
cts
requ
iring
resc
ue th
erap
y.
–Ch
ange
from
bas
elin
e Hb
dur
ing
the
first
28-
day
dosi
ng c
ycle
, inc
ludi
ng p
eak
Hb re
spon
se.
• Pr
opor
tiona
l and
con
tinuo
us e
nd p
oint
s w
ere
sum
mar
ized
des
crip
tivel
y.
• Th
e fin
al m
ean
hom
e BP
val
ue w
as c
alcu
late
d by
firs
t det
erm
inin
g th
e m
ean
of 3
wak
ing
and
3 be
dtim
e se
ts o
f BP
mea
sure
s. N
ext,
the
mea
n w
akin
g an
d m
ean
bedt
ime
valu
es fr
om a
sin
gle
day
wer
e bo
th u
sed
to c
alcu
late
the
day
mea
n. F
inal
ly, th
e m
ean
of th
e da
y m
eans
was
cal
cula
ted,
and
this
com
pris
ed th
e fin
al m
ean
hom
e BP
.
• Ho
me
BP m
easu
res
and
safe
ty m
easu
res
wer
e su
mm
ariz
ed d
escr
iptiv
ely. RE
SULT
SSu
bjec
ts•
A to
tal o
f 21
subj
ects
wer
e ra
ndom
ized
and
rece
ived
stu
dy m
edic
atio
n. O
ne s
ubje
ct w
as ra
ndom
ized
to s
otat
erce
pt 0
.5 m
g/kg
and
rece
ived
1 d
ose
of s
tudy
med
icat
ion;
ho
wev
er, t
his
subj
ect d
id n
ot h
ave
the
first
follo
w-u
p vi
sit a
t the
tim
e of
the
inte
rim d
atab
ase
cuto
ff po
int a
nd w
as n
ot in
clud
ed in
eith
er th
e sa
fety
or e
ffica
cy p
opul
atio
n.
A to
tal o
f 20
subj
ects
com
pris
e th
e FA
S an
d sa
fety
pop
ulat
ion:
–5
who
rece
ived
pla
cebo
.
–9
who
rece
ived
sot
ater
cept
0.3
mg/
kg.
–6
who
rece
ived
sot
ater
cept
0.5
mg/
kg.
• In
terim
sub
ject
dis
posi
tion
is il
lust
rate
d in
Tab
le 1
.
• Ba
selin
e su
bjec
t dem
ogra
phic
s an
d di
seas
e ch
arac
teris
tics
wer
e ge
nera
lly s
imila
r acr
oss
treat
men
t gro
ups
(Tab
le 2
).
• M
ajor
pro
toco
l vio
latio
ns w
ere
note
d fo
r 2 s
ubje
cts
rand
omiz
ed to
sot
ater
cept
. One
sub
ject
(0.3
mg/
kg) r
ecei
ved
eryt
hrop
oiet
in p
rior t
o ra
ndom
izat
ion
and
thro
ugh
the
first
dos
e cy
cle,
and
was
dis
cont
inue
d fro
m th
e st
udy;
1 s
ubje
ct (0
.5 m
g/kg
) had
an
inco
mpl
ete
base
line
hom
e BP
eva
luat
ion,
whi
ch s
how
ed a
non
-qua
lifyi
ng e
leva
tion
in B
P pr
ior t
o ra
ndom
izat
ion,
and
was
dis
cont
inue
d fro
m s
tudy
med
icat
ion
early
. The
se s
ubje
cts
wer
e ex
clud
ed fr
om e
ffica
cy a
naly
ses,
as
a pe
r-pr
otoc
ol a
naly
sis
defin
ed
in th
e pr
otoc
ol. I
nclu
ded
in th
e ef
ficac
y an
alys
is p
opul
atio
n w
ere:
–5
who
rece
ived
pla
cebo
.
–8
who
rece
ived
sot
ater
cept
0.3
mg/
kg.
–5
who
rece
ived
sot
ater
cept
0.5
mg/
kg.
Tabl
e 1.
Sub
ject
Dis
posi
tion
(FAS
, N=
20)
Grou
pOn
goin
g on
St
udy
Drug
D/C
Stud
y Dr
ug
(Bei
ng F
ollo
wed
)Co
mpl
eter
s on
Stu
dy D
rug
(≥20
0 Da
ys)
Com
plet
ers
Afte
r D/C
St
udy
Drug
Early
Ter
min
atio
nTo
tal R
escu
edD/
C St
udy
Drug
Du
e to
Sto
ppin
g Ru
le
Plac
ebo,
n=
50
21
11
30
Sota
terc
ept 0
.3 m
g/kg
, n=
90
02
52
70
Sota
terc
ept 0
.5 m
g/kg
, n=
63
20
01
21
D/C=
disc
ontin
ued.
Tabl
e 2.
Dem
ogra
phic
Cha
ract
eris
tics
of S
ubje
cts
(FAS
, N=
20)
Plac
ebo
Sota
terc
ept
n=5
0.3
mg/
kg
n=9
0.5
mg/
kg
n=6
Age,
mea
n, y
ears
58.4
59.9
60.7
Fem
ale,
n (%
)1
(20.
0)6
(66.
7)1
(16.
7)
Race
, n (%
)
Whi
te1
(20.
0)3
(33.
3)4
(66.
7)
Blac
k3
(60.
0)6
(66.
7)2
(33.
3)
Asia
n1
(20.
0)0
(0.0
)0
(0.0
)
Ethn
icity
Hisp
anic
0 (0
.0)
2 (2
2.2)
4 (6
6.7)
Non-
Hisp
anic
5 (1
00.0
)7
(77.
8)2
(33.
3)
Wei
ght,
post
dial
ysis
mea
n, k
g75
.879
.481
.0
Body
mas
s in
dex,
mea
n, k
g/m
225
.427
.827
.3
Sota
terc
ept P
K•
Prel
imin
ary,
inte
rim P
K da
ta, b
ased
on
anal
ysis
of a
ll su
bjec
ts ra
ndom
ized
to s
otat
erce
pt 0
.3 m
g/kg
and
the
first
6 s
ubje
cts
rand
omiz
ed to
sot
ater
cept
0.5
mg/
kg, a
re
pres
ente
d in
Tab
le 3
.
• So
tate
rcep
t exh
ibite
d do
se-d
epen
dent
incr
ease
s in
the
seru
m d
rug
expo
sure
(Cm
ax a
nd A
UC),
with
a m
ean
elim
inat
ion
half-
life
(t 1/2,
z) of
22
to 2
5 da
ys.
• So
tate
rcep
t mea
n co
ncen
tratio
n-vs
.-tim
e pr
ofile
s fo
r the
0.3
mg/
kg a
nd 0
.5 m
g/kg
dos
e gr
oups
are
sho
wn
in F
igur
e 2.
Figu
re 4
. Mea
n Pe
ak H
emog
lobi
n In
crea
se D
urin
g th
e Fi
rst 2
8-Da
y Do
se C
ycle
(Per
-Pro
toco
l Pop
ulat
ion)
*
Sota
terc
ept 0
.3 m
g/kg
(n=
8)
Sota
terc
ept 0
.5 m
g/kg
(n=
5)
Plac
ebo
(n=
5)
0.1
0.5
0.8
0
0.3
0.2
0.1
0.4
0.5
0.6
0.7
0.8
0.9
Hb (g/dL) Change From Baseline
Mea
n Pe
ak H
emog
lobi
n Re
spon
se
*Tw
o su
bjec
ts w
ith a
maj
or p
roto
col v
iola
tion
wer
e ex
clud
ed fr
om e
ffica
cy a
naly
ses.
Chan
ge F
rom
Bas
elin
e in
Hb
Conc
entra
tion
• M
ean
Hb c
once
ntra
tion
in s
ubje
cts
who
rece
ived
sot
ater
cept
0.3
mg/
kg a
nd 0
.5 m
g/kg
exh
ibite
d a
grea
ter i
ncre
ase
from
bas
elin
e in
the
first
15
days
pos
t-do
se
(vs.
pla
cebo
); ho
wev
er, t
he in
crea
ses
wer
e no
t sus
tain
ed th
roug
h th
e en
tire
dose
cyc
le.
• Hb
leve
ls th
roug
hout
mul
tiple
dos
e cy
cles
am
ong
subj
ects
who
did
not
requ
ire re
scue
wer
e ge
nera
lly h
ighe
st a
mon
g su
bjec
ts re
ceiv
ing
sota
terc
ept 0
.5 m
g/kg
(F
igur
e 5)
.
Figu
re 5
. Hb
Chan
ge F
rom
Bas
elin
e Du
ring
Long
-ter
m S
otat
erce
pt T
reat
men
t Cen
sore
d fo
r Res
cue
−3
−2
−101234
5010
015
020
025
0
Days
Afte
r the
Firs
t Dos
e
Hemoglobin (g/dL)
Sota
terc
ept 0
.3 m
g/kg
(n=
8)So
tate
rcep
t 0.5
mg/
kg (n
=5)
Plac
ebo
(n=
5)
Hom
e BP
Mea
sure
men
ts•
Hom
e BP
mea
sure
s in
the
first
dos
e cy
cle
reve
aled
that
all
3 gr
oups
had
incr
ease
s in
gro
up m
ean
SBP,
with
the
larg
est c
hang
e in
sub
ject
s re
ceiv
ing
sota
terc
ept
0.3
mg/
kg, w
hile
the
larg
est c
hang
e in
DBP
was
in s
ubje
cts
rece
ivin
g pl
aceb
o. A
ll th
e gr
oup
mea
n ch
ange
s w
ere
<10
mm
Hg
(Fig
ure
6A a
nd B
).
–Fi
ndin
gs w
ere
sim
ilar w
hen
anal
yzed
for b
oth
the
per-
prot
ocol
pop
ulat
ion
(Fig
ure
6A) a
nd F
AS (F
igur
e 6B
).
• W
ith lo
ng-t
erm
trea
tmen
t, ho
me
BP m
easu
res
show
ed n
o co
nsis
tent
cha
nge
from
bas
elin
e am
ong
subj
ects
in a
ny o
f the
trea
tmen
t gro
ups
(Fig
ure
7).
Figu
re 6
. Cha
nge
From
Bas
elin
e in
Hom
e BP
at t
he E
nd o
f Dos
e Cy
cle
1 in
the
(A) P
er-P
roto
col P
opul
atio
n*
and
(B) F
AS
Sota
terc
ept 0
.3 m
g/kg
(n=
7)
Sota
terc
ept 0
.5 m
g/kg
(n=
4)
Plac
ebo
(n=
3)
Sota
terc
ept 0
.3 m
g/kg
(n=
9)
Sota
terc
ept 0
.5 m
g/kg
(n=
5)
Plac
ebo
(n=
4)
Change From Baseline BP (mm Hg)
0.0
2.0
6.0
3.3
3.3
–0.3
–1
.0
0.0
1.0
2.0
3.0
4.0
5.0
6.0
7.0
SBP
DBP
A B
Change From Baseline BP (mm Hg)
2.3
7.5
3.0
2.5
7.6
0.4
0.0
1.0
2.0
3.0
4.0
5.0
6.0
7.0
8.0
SBP
DBP
*Dat
a ex
clud
e su
bjec
ts w
ith p
roto
col v
iola
tions
and
are
cen
sore
d fo
r tho
se w
ho re
quire
d re
scue
in th
e fir
st d
ose
cycl
e.
Figu
re 7
. Cha
nge
From
Bas
elin
e Ho
me
BP M
easu
rem
ents
(FAS
) of (
A) S
BP a
nd (B
) DBP
Dur
ing
Long
-ter
m
Sota
terc
ept T
reat
men
t, Ce
nsor
ed fo
r Res
cue
ASB
P
BDB
P
–20
–15
–10–50510152025
5010
015
020
025
0
Sota
terc
ept 0
.3 m
g/kg
(n=
9)So
tate
rcep
t 0.5
mg/
kg (n
=5)
Plac
ebo
(n=
4)
Home DBP (mm Hg)
–50
–40
–30
–20
–10010203040
5010
015
020
025
0
Sota
terc
ept 0
.3 m
g/kg
(n=
9)So
tate
rcep
t 0.5
mg/
kg (n
=5)
Plac
ebo
(n=
4)
Home SBP (mm Hg)
CONC
LUSI
ONS
• So
tate
rcep
t exh
ibite
d lin
ear P
K ch
arac
teris
tics,
and
a lo
ng h
alf-
life
of 2
2 to
25
days
.
• So
tate
rcep
t was
wel
l tol
erat
ed, w
ith A
Es s
imila
r to
thos
e ob
serv
ed w
ith p
lace
bo a
nd n
o tre
nds
tow
ard
incr
ease
d BP
.
• Ex
posu
re to
sot
ater
cept
was
not
ass
ocia
ted
with
the
deve
lopm
ent o
f ant
i-dru
g an
tibod
ies,
inje
ctio
n si
te re
actio
ns, o
r hyp
erse
nsiti
vity
reac
tions
.
• In
the
first
28
days
of t
reat
men
t, th
e pr
opor
tion
of s
ubje
cts
achi
evin
g th
e ta
rget
Hb
incr
ease
of ≥
1 g/
dL w
as g
reat
er in
the
treat
men
t gro
ups
than
in th
e pl
aceb
o gr
oup,
and
the
prop
ortio
n re
quiri
ng re
scue
ther
apy
in th
e fir
st 2
8 da
ys w
as d
ose-
rela
ted,
with
no
subj
ects
in th
e so
tate
rcep
t 0.5
mg/
kg g
roup
requ
iring
resc
ue.
• In
this
initi
al 2
8-da
y an
alys
is, i
n w
hich
the
plac
ebo
and
sota
terc
ept 0
.3 m
g/kg
gro
ups
had
high
er b
asel
ine
Hb, n
o di
ffere
nces
bet
wee
n gr
oups
ach
ievi
ng th
e ta
rget
Hb
rang
e (1
0-12
g/d
L) w
ere
obse
rved
. Dos
e es
cala
tion
cont
inue
s pe
r pro
toco
l.
• M
ean
peak
Hb
resp
onse
in th
e fir
st 2
8 da
ys w
as d
ose-
rela
ted,
with
the
sota
terc
ept 0
.5 m
g/kg
dos
e ha
ving
the
high
est m
ean
peak
Hb
resp
onse
.
• Hb
impr
ovem
ents
wer
e ge
nera
lly s
usta
ined
for m
ultip
le d
osin
g cy
cles
in th
e so
tate
rcep
t 0.5
mg/
kg d
ose
grou
p.
• Th
is p
relim
inar
y in
terim
ana
lysi
s in
dica
tes
adeq
uate
Hb
resp
onse
s an
d sa
fety
of s
otat
erce
pt a
t 0.3
and
0.5
mg/
kg a
nd p
rovi
des
evid
ence
to c
ontin
ue th
e ev
alua
tion
of s
otat
erce
pt a
t 0.7
mg/
kg in
pat
ient
s w
ith E
SKD
on h
emod
ialy
sis.
REFE
RENC
ES1.
Ba
bitt
JL, L
in H
Y. M
echa
nism
s of
ane
mia
in C
KD. J
Am
Soc
Nep
hrol
. 201
2;23
:163
1-16
34.
2.
Jaco
bson
LO,
Gol
dwas
ser E
, Frie
d W
, et a
l. Ro
le o
f the
kid
ney
in e
ryth
ropo
iesi
s. N
atur
e. 1
957;
179:
633-
634.
3.
McG
onig
le R
J, W
allin
JD,
Sha
dduc
k RK
, et a
l. Er
ythr
opoi
etin
defi
cien
cy a
nd in
hibi
tion
of e
ryth
ropo
iesi
s in
rena
l ins
uffic
ienc
y. Ki
dney
Int.
1984
;25:
437-
444.
4.
Esch
bach
JW
, Egr
ie J
C, D
owni
ng M
R, e
t al.
Corr
ectio
n of
the
anem
ia o
f end
-sta
ge re
nal d
isea
se w
ith re
com
bina
nt h
uman
ery
thro
poie
tin. R
esul
ts o
f a c
ombi
ned
phas
e I
and
II cl
inic
al tr
ial.
N En
gl J
Med
. 198
7;31
6:73
-78.
5.
Sing
h AK
, Szc
zech
L, T
ang
KL, e
t al.
Corr
ectio
n of
ane
mia
with
epo
etin
alfa
in c
hron
ic k
idne
y di
seas
e. N
Eng
l J M
ed. 2
006;
355:
208
5-20
98.
6.
Fish
bane
S. A
nem
ia a
nd c
ardi
ovas
cula
r ris
k in
the
patie
nt w
ith k
idne
y di
seas
e. H
eart
Fail
Clin
. 200
8;4:
401-
410.
7.
Besa
rab
A, B
olto
n W
K, B
row
ne J
K, e
t al.
The
effe
cts
of n
orm
al a
s co
mpa
red
with
low
hem
atoc
rit v
alue
s in
pat
ient
s w
ith c
ardi
ac d
isea
se w
ho a
re re
ceiv
ing
hem
odia
lysi
s an
d ep
oetin
. N E
ngl J
Med
. 199
8;33
9:58
4-59
0.
8.
Drue
ke T
B, L
ocat
elli
F, Cl
yne
N, e
t al.
Norm
aliz
atio
n of
hem
oglo
bin
leve
l in
patie
nts
with
chr
onic
kid
ney
dise
ase
and
anem
ia. N
Eng
l J M
ed. 2
006;
355:
2071
-208
4.
9.
Pfef
fer M
A, B
urdm
ann
EA, C
hen
CY, e
t al.
A tri
al o
f dar
bepo
etin
alfa
in ty
pe 2
dia
bete
s an
d ch
roni
c ki
dney
dis
ease
. N E
ngl J
Med
. 200
9;36
1:20
19-2
032.
10. P
ears
all R
S, C
anal
is E
, Cor
nwal
l-Bra
dy M
, et a
l. A
solu
ble
activ
in ty
pe II
A re
cept
or in
duce
s bo
ne fo
rmat
ion
and
impr
oves
ske
leta
l int
egrit
y. Pr
oc N
atl A
cad
Sci U
S A
. 20
08;1
05:7
082-
7087
.
11. I
ancu
-Rub
in C
, Mos
oyan
G, W
ang
J, e
t al.
Stro
mal
cel
l-med
iate
d in
hibi
tion
of e
ryth
ropo
iesi
s ca
n be
atte
nuat
ed b
y so
tate
rcep
t (AC
E-01
1), a
n ac
tivin
rece
ptor
type
II
ligan
d tra
p. E
xp H
emat
ol. 2
013;
41:1
55-1
66.
12. S
herm
an M
L, B
orgs
tein
NG,
Moo
k L,
et a
l. M
ultip
le-d
ose,
saf
ety,
phar
mac
okin
etic
, and
pha
rmac
odyn
amic
stu
dy o
f sot
ater
cept
(Act
RIIA
-IgG1
), a
nove
l ery
thro
poie
tic
agen
t, in
hea
lthy
post
men
opau
sal w
omen
. J C
lin P
harm
acol
. 201
3;53
:112
1-11
30.
13. W
oold
ridge
T, K
apla
n M
, Alc
orn
H Jr
, et a
l. Th
e ph
arm
acok
inet
ics
and
safe
ty o
f a s
ingl
e-do
se o
f sot
ater
cept
(ACE
-011
) in
subj
ects
on
hem
odia
lysi
s an
d th
e ef
fect
s of
its
mur
ine
anal
og (R
AP-0
11) o
n an
emia
and
in p
reve
ntin
g bo
ne lo
ss in
C57
BL/6
mic
e w
ith 5
/6 n
ephr
ecto
my
[ora
l pre
sent
atio
n]. P
rese
nted
at:
Amer
ican
Soc
iety
of
Neph
rolo
gy K
idne
y W
eek
2012
; Oct
ober
30-
Nove
mbe
r 4, 2
012;
San
Die
go, C
A.
This
stu
dy w
as s
pons
ored
by
Celg
ene
Corp
orat
ion.
Pres
ente
d at
: the
Nat
iona
l Kid
ney
Foun
datio
n (N
KF) 2
014
Sprin
g Cl
inic
al M
eetin
g; A
pril
22–2
6, 2
014;
Las
Veg
as, N
V.Sc
an th
is Q
R co
de to
rece
ive
the
of th
e po
ster

Interim Analysis of ACE-011-REN-001: The First 28-Day Dose Cycle of Low and Medium Starting Doses of Sotatercept Compared to Placebo for Correction of Anemia in Hemodialysis Subjects
Mohamed El-Shahawy1; James Cotton2; Jeffrey Kaupke3; Thomas D. Wooldridge4; Hem N. Singh5; William T. Smith51Academic Medical Research Institute, Los Angeles, CA, USA; 2Tyler Nephrology Associates PC, Tyler, TX, USA; 3Nephrology Specialist Medical Group, Orange, CA, USA; 4Nephrology & Hypertension Associates LTD, Tupelo, MS, USA; 5Celgene Corporation, Warren, NJ, USA
INTRODUCTION• The anemia seen in patients with end-stage kidney disease (ESKD) is largely due to decreased biosynthesis of erythropoietin from the kidneys.1-3
• A number of erythropoiesis-stimulating agents (ESAs) have demonstrated efficacy in increasing hemoglobin (Hb) levels in patients with ESKD,4,5 but pose significant safety risks, including persistent hypertension, serious cardiovascular events, and increased risk of death.4,5
• Multiple observational studies have linked low Hb levels to poor cardiovascular outcomes.6 However, recent clinical studies have demonstrated that ESAs are unable to modify this risk when targeting a normal Hb level.5,7-9
• Sotatercept (ACE-011) is an ActRIIA-IgG1 fusion protein trap that binds with high affinity to activin A and other members of the TGFb superfamily and acts on late-stage erythropoiesis to increase the production of mature erythrocytes into the circulation.10-12
• This 2-part, phase IIA, randomized, placebo-controlled trial is the first to evaluate the pharmacokinetics (PK), safety, tolerability, and Hb effect of sotatercept in ESKD subjects with renal anemia receiving hemodialysis.
• In part 1, after a single subcutaneous dose (0.1 mg/kg) of sotatercept13:
– PK parameters were similar to a phase I study in healthy postmenopausal women, with a long half-life (21 days).
– Sotatercept was not dialyzable.
– There was no evidence of a pharmacodynamic effect on Hb concentrations at the single, 0.1 mg/kg dose.
– Sotatercept was well tolerated with no observed changes in blood pressure (BP), and no consistent changes in safety laboratory or electrocardiographic parameters.
• Part 2 is an ongoing, randomized, single-blind, placebo-controlled, sequential dose-escalation study in subjects with ESKD on hemodialysis evaluating the PK, safety, tolerability, and Hb effects of sotatercept for the correction of ESKD-related anemia.
• We report the preliminary, interim analysis of the sotatercept 0.3 mg/kg (low dose) and 0.5 mg/kg (medium dose) treatment groups.
• Pending acceptable interim analysis results, additional patients may be randomized in a staggered parallel fashion to sotatercept 0.7 mg/kg once every 28 days (high dose) and sotatercept 0.7 mg/kg once every 14 days for 28 days followed by 0.4 mg/kg every 14 days for the remainder of the treatment period (Figure 1).
METHODSKey Inclusion Criteria• Adults receiving at least 3 hours of high-flux hemodialysis at each session for at least 12 weeks before screening and no planned changes to the hemodialysis regimen
during the study period
• Adequate Hb response (Hb ≥10 to ≤12 g/dL predialysis mean of 3 consecutive Hb concentrations) to stable doses of ESA (epoetin alfa, darbepoetin) for at least 6 weeks before and during screening, excluding dose holds for high Hb (maximum dose: epoetin alfa ≤500 IU/kg/week; darbepoetin ≤95 μg/week)
• ESKD-related anemia: Hb ≥8 to ≤10 g/dL predialysis after ESA washout
• Adequate iron status (transferrin saturation ≥20%)
• Kt/V ≥1.2 or urea reduction ratio ≥65%
• Parathyroid hormone concentration ≤1,000 pg/mL; phosphorous ≤7 mg/dL; and total albumin-corrected calcium ≥8.0 to ≤10.5 mg/dL
Key Exclusion Criteria• Anemia due to non-renal causes
• ESKD due to malignancy or history of malignancy (excluding excised and cured non-melanoma skin cancer and cervical carcinoma in situ)
• Systemic hematologic disease
• Peritoneal dialysis or compromised venous access
• Uncontrolled diabetes mellitus (HbA1C >9%), hypertension (home systolic BP [SBP] >160 mm Hg, home diastolic BP [DBP] >90 mm Hg), or heart failure (New York Heart Association class ≥3)
• Alanine transaminase and/or aspartate transaminase values >2× the upper limit of normal; C-reactive protein >50 mg/L
• Red blood cell transfusion <8 weeks before screening
• Anticipated or scheduled living donor renal transplant
Study Design• This was a randomized, single-blind, placebo-controlled, sequential dose-escalation study in subjects with ESKD on hemodialysis (Figure 1).
• Eligible subjects were randomized to 2 arms (sotatercept or placebo in a 3:1 ratio) in 4 sequential dose groups (sotatercept 0.3 mg/kg, 0.5 mg/kg, 0.7 mg/kg, or 0.7 mg/kg loading dose followed by 0.4 mg/kg).
– This interim analysis informed the data monitoring committee’s decision to open enrollment for the high-dose group (sotatercept 0.7 mg/kg).
– At the time of abstract submission:
§ Enrollment in the sotatercept 0.3 mg/kg and 0.5 mg/kg dose groups was completed.
§ Enrollment in the sotatercept 0.7 mg/kg dose group was ongoing.
• Sotatercept doses could have been delayed, reduced, or discontinued based on the subject’s absolute predialysis Hb level or change in Hb level observed after dosing, or discontinued based on change in home BP measurements.
– Delayed: Hb ≥11 to <13 g/dL on Dose Cycle Day 36 (0.3, 0.5, and 0.7 mg/kg dose groups) or Dose Cycle Day 19 (0.7/0.4 mg/kg dose group)
– Reduced: If a dose was delayed, OR if Hb <11 g/dL AND rate of rise of >2 g/dL (0.3, 0.5, and 0.7 mg/kg dose groups) or >1 g/dL (0.7/0.4 mg/kg dose group)
– Discontinued:
§ Persistent hypertension recorded by home BP monitor mean of 4 days of home SBP >160 mm Hg AND increase in SBP from baseline of >20 mm Hg, or mean increase from baseline DBP of >10 mm Hg
§ Hb ≥13 g/dL at any time after randomization
§ Hb ≥12 to <13 g/dL for 2 consecutive weeks at any time after randomization
• Rescue treatment was recommended for subjects with Hb <9 g/dL after the first dose cycle, and those required to discontinue sotatercept could receive ESA treatment or red blood cell transfusion.
• All randomized subjects, including those who were rescued or discontinued early, continued to follow the visit schedule and home BP monitoring throughout the 200-day treatment phase and 112-day follow-up phase.
• The current report describes interim analysis of the sotatercept 0.3 mg/kg and 0.5 mg/kg dose groups for the purpose of determining safety of proceeding to the next dose group.
Figure 1. Study Design
Follow-up phase for 112 days for PK
and safety
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.3 mg/kgSC (n ~9) q28d,up to 8 doses
Placebo (n ~3)q28d, up to 8 doses
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.5 mg/kgSC (n ~9) q28d,up to 8 doses
Placebo (n ~3)q28d, up to 8 doses
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.7 mg/kgSC (n ~9) q28d,
up to 8 doses
Placebo (n ~3)q28d, up to 8 doses
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.7 mg/kg SC q14d(2 doses), then 0.4 mg/kg SC q14d
up to 13 doses (n ~9)
Placebo (n ~3)q14d, up to 15 doses
Note: All randomized subjects will continue treatment with sotatercept 0.3, 0.5, or 0.7 mg/kg or placebo for up to 8 doses* unless rescued or discontinued early. *At 0.7/0.4 mg/kg, all randomized subjects will continue treatment for up to 15 doses unless rescued or discontinued early.28 days after the 6th subject is dosed with sotatercept in each dose group (0.3, 0.5, and 0.7 mg/kg), an interim analysis will occur to evaluate PK and safety before opening the next dose group.
Table 3. Sotatercept PK in ESKD Subjects on Hemodialysis (Dose 1, Cycle 1)
Sotatercept
Parameter0.3 mg/kg
n=90.5 mg/kg
n=6
tmax, mean (min–max), day 12 (2–14) 7 (2–14)
Cmax, mean (SD), μg/mL 2.4 (0.96) 3.5 (0.73)
AUC28d, mean (SD), day•μg/mL 50.5 (17.4) 73.2 (11.5)
t1/2,z, mean (SD), day 22.3 (3.0)* 24.5 (8.9)*†
CL/F, mean (SD), mL/day/kg 3.65 (1.60)* 3.83 (1.19)*†
Vz/F, mean (SD), mL/kg 117 (54)* 124 (27.9)*†
AUC28d=area under the concentration-vs.-time curve up to 28 days; CL/F=oral clearance; Vz/F=apparent volume of distribution.*Estimated according to a 1-compartment model.†The 28-day data may not be sufficient for accurate estimation in some subjects.
Figure 2. Sotatercept Serum Concentration Over Time
Seru
m S
otat
erce
pt (µ
g/m
L)
5
4
3
2
1
0
Days After the First Dose
0 7 14 21 28
Sotatercept 0.3 mg/kg
Sotatercept 0.5 mg/kg
Safety• An overview of AEs is provided in Table 4.
• A decrease in serum calcium levels during follow-up in subjects who had received sotatercept 0.3 mg/kg was noted, without AEs of hypocalcemia.
• There were no other observed trends in laboratory, electrocardiogram, or vital sign parameters, including study visit and intra-dialytic BP, in either dose group of sotatercept during long-term follow-up.
• No anti-drug antibodies, injection site reactions, or hypersensitivity reactions were observed.
Table 4. Overview of AEs (Safety Population, N=20)
Placebo Sotatercept
n=50.3 mg/kg
n=90.5 mg/kg
n=6
Subjects, n (%)
Cumulative days on study 864 2046 634
Any AE 3 (60.0) 8 (88.8) 3 (50.0)
≥1 severe AE 2 (40.0) 2 (22.2) 2 (33.3)
≥1 serious AE 2 (40.0) 2 (22.2) 1 (16.7)
Death 1 (20.0) 0 (0.0) 0 (0.0)
AEs in ≥2 subjects in a treatment group, n (%)
Fatigue 1 (20.0) 2 (22.2) 0 (0.0)
Pain 0 (0.0) 2 (22.2) 0 (0.0)
Constipation 1 (20.0) 2 (22.2) 0 (0.0)
Hypertension 0 (0.0) 3 (33.3)* 0 (0.0)
*A total of 3 subjects randomized to sotatercept 0.3 mg/kg reported 4 AEs of hypertension; 3 of the 4 events occurred after rescue with erythropoietin.
EfficacyTarget Hb Increase (≥1 g/dL), and Target Hb Range (10–12 g/dL) During the First 28 Days
• Baseline Hb levels were 9.7 g/dL in subjects receiving placebo, 9.3 g/dL in subjects receiving sotatercept 0.3 mg/kg, and 8.9 g/dL in subjects receiving sotatercept 0.5 mg/kg.
• Hb increase ≥1.0 g/dL was achieved by 20% (placebo), 37.5% (sotatercept 0.3 mg/kg), and 40% (sotatercept 0.5 mg/kg) of subjects (Figure 3).
• The desired Hb range (10–12 g/dL) was achieved in 60% (placebo), 25% (sotatercept 0.3 mg/kg), and 60% (sotatercept 0.5 mg/kg) during the first dose cycle.
• Mean peak Hb increase in the first 28-day dose cycle was 0.1 g/dL in subjects receiving placebo, 0.5 g/dL in subjects receiving sotatercept 0.3 mg/kg, and 0.8 g/dL in subjects receiving sotatercept 0.5 mg/kg (Figure 4).
• Rescue therapy was required (Hb <9 g/dL) in 2 of 5 subjects after administration of placebo and 1 of 8 subjects after administration of sotatercept 0.3 mg/kg, while none required rescue after sotatercept 0.5 mg/kg (Figure 3).
Figure 3. Hb Increase During the First 28-Day Dose Cycle (Per-Protocol Population)*
0
30
20
10
40
60
50
70
80
90
100
Subj
ects
(%)
Placebo(n=5)
40
40
20
Sotatercept 0.3 mg/kg(n=8)
13
50
37
Sotatercept 0.5 mg/kg
(n=5)
60
40
0.1-0.9 g/dL
Required Rescue (Hb <9 g/dL)
≥1.0 g/dL
*Two subjects with a major protocol violation were excluded from efficacy analyses.
PK Assessment• Blood samples for analysis of sotatercept PK were collected at each study visit and on each sotatercept or placebo dosing day. Additional samples were obtained after
dose 1 at 4 hours post-dose on Day 1 and at 48 hours post-dose on Day 3.
• A validated, competitive enzyme-linked immunosorbent assay using anti‐human ActRIIA antibodies (R&D Systems, Minneapolis, MN) was used to measure the sotatercept serum concentration.
Hb Assessments• Blood samples for Hb assessment were obtained at all scheduled study visits, including before dosing.
Home BP Monitoring• Because of the burden of hypertension in the hemodialysis population, and the inherent variability in hemodialysis-related BP measurement, home BP monitoring was
used to provide a BP profile more reflective of the subject’s steady state.
• Subjects obtained their BP at home 2×/day (3 measurements each upon waking and at bedtime) for 4 consecutive days within 7 days of a scheduled dosing day. Each subject was trained to use a sponsor-provided BP monitor.
• At least 3 waking and 3 bedtime values downloaded from the device by study personnel were used to calculate mean BP values before screening, randomization, and re-dosing.
• Home BP monitoring continued for subjects requiring rescue.
Safety Assessments• Safety assessments included collection of adverse events (AEs), hematology testing, and vital signs at each visit and physical examination and 12-lead
electrocardiogram at selected scheduled time points.
– Safety assessments were done in the event of early termination/withdrawal.
• Proportions of subjects with Hb >12 g/dL at any time and rise in Hb >2 g/dL over 4 weeks were also determined.
• At each interim analysis, blood samples were analyzed for the presence of anti-sotatercept antibodies.
Statistical Analysis• Sotatercept multidose PK was examined among all subjects who received at least 1 dose of study medication and who had evaluable PK data.
• Sotatercept efficacy was evaluated in the full analysis set (FAS), which comprised all randomized subjects who received at least 1 dose of study medication and had at least 1 post-dose follow-up visit, and a baseline value (for analyses that require baseline comparison). Subjects assigned to placebo in both dose groups were combined to form a single placebo group for analysis purposes.
• Efficacy end points included:
– Proportion of subjects achieving target Hb increase (≥1 g/dL increase from baseline).
– Proportion of subjects achieving target Hb concentration >10 g/dL to <12 g/dL.
– Proportion of subjects requiring rescue therapy.
– Change from baseline Hb during the first 28-day dosing cycle, including peak Hb response.
• Proportional and continuous end points were summarized descriptively.
• The final mean home BP value was calculated by first determining the mean of 3 waking and 3 bedtime sets of BP measures. Next, the mean waking and mean bedtime values from a single day were both used to calculate the day mean. Finally, the mean of the day means was calculated, and this comprised the final mean home BP.
• Home BP measures and safety measures were summarized descriptively.
RESULTSSubjects• A total of 21 subjects were randomized and received study medication. One subject was randomized to sotatercept 0.5 mg/kg and received 1 dose of study medication;
however, this subject did not have the first follow-up visit at the time of the interim database cutoff point and was not included in either the safety or efficacy population. A total of 20 subjects comprise the FAS and safety population:
– 5 who received placebo.
– 9 who received sotatercept 0.3 mg/kg.
– 6 who received sotatercept 0.5 mg/kg.
• Interim subject disposition is illustrated in Table 1.
• Baseline subject demographics and disease characteristics were generally similar across treatment groups (Table 2).
• Major protocol violations were noted for 2 subjects randomized to sotatercept. One subject (0.3 mg/kg) received erythropoietin prior to randomization and through the first dose cycle, and was discontinued from the study; 1 subject (0.5 mg/kg) had an incomplete baseline home BP evaluation, which showed a non-qualifying elevation in BP prior to randomization, and was discontinued from study medication early. These subjects were excluded from efficacy analyses, as a per-protocol analysis defined in the protocol. Included in the efficacy analysis population were:
– 5 who received placebo.
– 8 who received sotatercept 0.3 mg/kg.
– 5 who received sotatercept 0.5 mg/kg.
Table 1. Subject Disposition (FAS, N=20)
GroupOngoing on Study Drug
D/C Study Drug (Being Followed)
Completers on Study Drug (≥200 Days)
Completers After D/C Study Drug Early Termination Total Rescued
D/C Study Drug Due to Stopping Rule
Placebo, n=5 0 2 1 1 1 3 0
Sotatercept 0.3 mg/kg, n=9 0 0 2 5 2 7 0
Sotatercept 0.5 mg/kg, n=6 3 2 0 0 1 2 1
D/C=discontinued.
Table 2. Demographic Characteristics of Subjects (FAS, N=20)
Placebo Sotatercept
n=50.3 mg/kg
n=90.5 mg/kg
n=6
Age, mean, years 58.4 59.9 60.7
Female, n (%) 1 (20.0) 6 (66.7) 1 (16.7)
Race, n (%)
White 1 (20.0) 3 (33.3) 4 (66.7)
Black 3 (60.0) 6 (66.7) 2 (33.3)
Asian 1 (20.0) 0 (0.0) 0 (0.0)
Ethnicity
Hispanic 0 (0.0) 2 (22.2) 4 (66.7)
Non-Hispanic 5 (100.0) 7 (77.8) 2 (33.3)
Weight, postdialysis mean, kg 75.8 79.4 81.0
Body mass index, mean, kg/m2 25.4 27.8 27.3
Sotatercept PK• Preliminary, interim PK data, based on analysis of all subjects randomized to sotatercept 0.3 mg/kg and the first 6 subjects randomized to sotatercept 0.5 mg/kg, are
presented in Table 3.
• Sotatercept exhibited dose-dependent increases in the serum drug exposure (Cmax and AUC), with a mean elimination half-life (t1/2,z) of 22 to 25 days.
• Sotatercept mean concentration-vs.-time profiles for the 0.3 mg/kg and 0.5 mg/kg dose groups are shown in Figure 2.
Figure 4. Mean Peak Hemoglobin Increase During the First 28-Day Dose Cycle (Per-Protocol Population)*
Sotatercept 0.3 mg/kg (n=8)
Sotatercept 0.5 mg/kg (n=5)
Placebo (n=5)
0.1
0.5
0.8
0
0.3
0.2
0.1
0.4
0.5
0.6
0.7
0.8
0.9
Hb (g
/dL)
Cha
nge
From
Bas
elin
e
Mean Peak Hemoglobin Response
*Two subjects with a major protocol violation were excluded from efficacy analyses.
Change From Baseline in Hb Concentration• Mean Hb concentration in subjects who received sotatercept 0.3 mg/kg and 0.5 mg/kg exhibited a greater increase from baseline in the first 15 days post-dose
(vs. placebo); however, the increases were not sustained through the entire dose cycle.
• Hb levels throughout multiple dose cycles among subjects who did not require rescue were generally highest among subjects receiving sotatercept 0.5 mg/kg (Figure 5).
Figure 5. Hb Change From Baseline During Long-term Sotatercept Treatment Censored for Rescue
−3
−2
−1
0
1
2
3
4
50 100 150 200 250
Days After the First Dose
Hem
oglo
bin
(g/d
L)
Sotatercept 0.3 mg/kg (n=8)Sotatercept 0.5 mg/kg (n=5)
Placebo (n=5)
Home BP Measurements• Home BP measures in the first dose cycle revealed that all 3 groups had increases in group mean SBP, with the largest change in subjects receiving sotatercept
0.3 mg/kg, while the largest change in DBP was in subjects receiving placebo. All the group mean changes were <10 mm Hg (Figure 6A and B).
– Findings were similar when analyzed for both the per-protocol population (Figure 6A) and FAS (Figure 6B).
• With long-term treatment, home BP measures showed no consistent change from baseline among subjects in any of the treatment groups (Figure 7).
Figure 6. Change From Baseline in Home BP at the End of Dose Cycle 1 in the (A) Per-Protocol Population* and (B) FAS
Sotatercept 0.3 mg/kg (n=7)
Sotatercept 0.5 mg/kg (n=4)
Placebo (n=3)
Sotatercept 0.3 mg/kg (n=9)
Sotatercept 0.5 mg/kg (n=5)
Placebo (n=4)
Chan
ge F
rom
Bas
elin
e BP
(mm
Hg)
0.0
2.0
6.0
3.3 3.3
–0.3 –1.0
0.0
1.0
2.0
3.0
4.0
5.0
6.0
7.0
SBP DBP
A
B
Chan
ge F
rom
Bas
elin
e BP
(mm
Hg)
2.3
7.5
3.0 2.5
7.6
0.4
0.0
1.0
2.0
3.0
4.0
5.0
6.0
7.0
8.0
SBP DBP
*Data exclude subjects with protocol violations and are censored for those who required rescue in the first dose cycle.
Figure 7. Change From Baseline Home BP Measurements (FAS) of (A) SBP and (B) DBP During Long-term Sotatercept Treatment, Censored for Rescue
A SBP
B DBP
–20
–15
–10
–5
0
5
10
15
20
25
50 100 150 200 250
Sotatercept 0.3 mg/kg (n=9)Sotatercept 0.5 mg/kg (n=5)
Placebo (n=4)
Hom
e DB
P (m
m H
g)
–50
–40
–30
–20
–10
0
10
20
30
40
50 100 150 200 250
Sotatercept 0.3 mg/kg (n=9)Sotatercept 0.5 mg/kg (n=5)
Placebo (n=4)
Hom
e SB
P (m
m H
g)
CONCLUSIONS• Sotatercept exhibited linear PK characteristics, and a long half-life of 22 to 25 days.
• Sotatercept was well tolerated, with AEs similar to those observed with placebo and no trends toward increased BP.
• Exposure to sotatercept was not associated with the development of anti-drug antibodies, injection site reactions, or hypersensitivity reactions.
• In the first 28 days of treatment, the proportion of subjects achieving the target Hb increase of ≥1 g/dL was greater in the treatment groups than in the placebo group, and the proportion requiring rescue therapy in the first 28 days was dose-related, with no subjects in the sotatercept 0.5 mg/kg group requiring rescue.
• In this initial 28-day analysis, in which the placebo and sotatercept 0.3 mg/kg groups had higher baseline Hb, no differences between groups achieving the target Hb range (10-12 g/dL) were observed. Dose escalation continues per protocol.
• Mean peak Hb response in the first 28 days was dose-related, with the sotatercept 0.5 mg/kg dose having the highest mean peak Hb response.
• Hb improvements were generally sustained for multiple dosing cycles in the sotatercept 0.5 mg/kg dose group.
• This preliminary interim analysis indicates adequate Hb responses and safety of sotatercept at 0.3 and 0.5 mg/kg and provides evidence to continue the evaluation of sotatercept at 0.7 mg/kg in patients with ESKD on hemodialysis.
REFERENCES1. Babitt JL, Lin HY. Mechanisms of anemia in CKD. J Am Soc Nephrol. 2012;23:1631-1634.
2. Jacobson LO, Goldwasser E, Fried W, et al. Role of the kidney in erythropoiesis. Nature. 1957;179:633-634.
3. McGonigle RJ, Wallin JD, Shadduck RK, et al. Erythropoietin deficiency and inhibition of erythropoiesis in renal insufficiency. Kidney Int. 1984;25:437-444.
4. Eschbach JW, Egrie JC, Downing MR, et al. Correction of the anemia of end-stage renal disease with recombinant human erythropoietin. Results of a combined phase I and II clinical trial. N Engl J Med. 1987;316:73-78.
5. Singh AK, Szczech L, Tang KL, et al. Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med. 2006;355: 2085-2098.
6. Fishbane S. Anemia and cardiovascular risk in the patient with kidney disease. Heart Fail Clin. 2008;4:401-410.
7. Besarab A, Bolton WK, Browne JK, et al. The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. N Engl J Med. 1998;339:584-590.
8. Drueke TB, Locatelli F, Clyne N, et al. Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med. 2006;355:2071-2084.
9. Pfeffer MA, Burdmann EA, Chen CY, et al. A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. N Engl J Med. 2009;361:2019-2032.
10. Pearsall RS, Canalis E, Cornwall-Brady M, et al. A soluble activin type IIA receptor induces bone formation and improves skeletal integrity. Proc Natl Acad Sci U S A. 2008;105:7082-7087.
11. Iancu-Rubin C, Mosoyan G, Wang J, et al. Stromal cell-mediated inhibition of erythropoiesis can be attenuated by sotatercept (ACE-011), an activin receptor type II ligand trap. Exp Hematol. 2013;41:155-166.
12. Sherman ML, Borgstein NG, Mook L, et al. Multiple-dose, safety, pharmacokinetic, and pharmacodynamic study of sotatercept (ActRIIA-IgG1), a novel erythropoietic agent, in healthy postmenopausal women. J Clin Pharmacol. 2013;53:1121-1130.
13. Wooldridge T, Kaplan M, Alcorn H Jr, et al. The pharmacokinetics and safety of a single-dose of sotatercept (ACE-011) in subjects on hemodialysis and the effects of its murine analog (RAP-011) on anemia and in preventing bone loss in C57BL/6 mice with 5/6 nephrectomy [oral presentation]. Presented at: American Society of Nephrology Kidney Week 2012; October 30-November 4, 2012; San Diego, CA.
This study was sponsored by Celgene Corporation.
Presented at: the National Kidney Foundation (NKF) 2014 Spring Clinical Meeting; April 22–26, 2014; Las Vegas, NV.Scan this QR code to receive
the PDF of the poster

Interim Analysis of ACE-011-REN-001: The First 28-Day Dose Cycle of Low and Medium Starting Doses of Sotatercept Compared to Placebo for Correction of Anemia in Hemodialysis Subjects
Mohamed El-Shahawy1; James Cotton2; Jeffrey Kaupke3; Thomas D. Wooldridge4; Hem N. Singh5; William T. Smith51Academic Medical Research Institute, Los Angeles, CA, USA; 2Tyler Nephrology Associates PC, Tyler, TX, USA; 3Nephrology Specialist Medical Group, Orange, CA, USA; 4Nephrology & Hypertension Associates LTD, Tupelo, MS, USA; 5Celgene Corporation, Warren, NJ, USA
INTRODUCTION• The anemia seen in patients with end-stage kidney disease (ESKD) is largely due to decreased biosynthesis of erythropoietin from the kidneys.1-3
• A number of erythropoiesis-stimulating agents (ESAs) have demonstrated efficacy in increasing hemoglobin (Hb) levels in patients with ESKD,4,5 but pose significant safety risks, including persistent hypertension, serious cardiovascular events, and increased risk of death.4,5
• Multiple observational studies have linked low Hb levels to poor cardiovascular outcomes.6 However, recent clinical studies have demonstrated that ESAs are unable to modify this risk when targeting a normal Hb level.5,7-9
• Sotatercept (ACE-011) is an ActRIIA-IgG1 fusion protein trap that binds with high affinity to activin A and other members of the TGFb superfamily and acts on late-stage erythropoiesis to increase the production of mature erythrocytes into the circulation.10-12
• This 2-part, phase IIA, randomized, placebo-controlled trial is the first to evaluate the pharmacokinetics (PK), safety, tolerability, and Hb effect of sotatercept in ESKD subjects with renal anemia receiving hemodialysis.
• In part 1, after a single subcutaneous dose (0.1 mg/kg) of sotatercept13:
– PK parameters were similar to a phase I study in healthy postmenopausal women, with a long half-life (21 days).
– Sotatercept was not dialyzable.
– There was no evidence of a pharmacodynamic effect on Hb concentrations at the single, 0.1 mg/kg dose.
– Sotatercept was well tolerated with no observed changes in blood pressure (BP), and no consistent changes in safety laboratory or electrocardiographic parameters.
• Part 2 is an ongoing, randomized, single-blind, placebo-controlled, sequential dose-escalation study in subjects with ESKD on hemodialysis evaluating the PK, safety, tolerability, and Hb effects of sotatercept for the correction of ESKD-related anemia.
• We report the preliminary, interim analysis of the sotatercept 0.3 mg/kg (low dose) and 0.5 mg/kg (medium dose) treatment groups.
• Pending acceptable interim analysis results, additional patients may be randomized in a staggered parallel fashion to sotatercept 0.7 mg/kg once every 28 days (high dose) and sotatercept 0.7 mg/kg once every 14 days for 28 days followed by 0.4 mg/kg every 14 days for the remainder of the treatment period (Figure 1).
METHODSKey Inclusion Criteria• Adults receiving at least 3 hours of high-flux hemodialysis at each session for at least 12 weeks before screening and no planned changes to the hemodialysis regimen
during the study period
• Adequate Hb response (Hb ≥10 to ≤12 g/dL predialysis mean of 3 consecutive Hb concentrations) to stable doses of ESA (epoetin alfa, darbepoetin) for at least 6 weeks before and during screening, excluding dose holds for high Hb (maximum dose: epoetin alfa ≤500 IU/kg/week; darbepoetin ≤95 μg/week)
• ESKD-related anemia: Hb ≥8 to ≤10 g/dL predialysis after ESA washout
• Adequate iron status (transferrin saturation ≥20%)
• Kt/V ≥1.2 or urea reduction ratio ≥65%
• Parathyroid hormone concentration ≤1,000 pg/mL; phosphorous ≤7 mg/dL; and total albumin-corrected calcium ≥8.0 to ≤10.5 mg/dL
Key Exclusion Criteria• Anemia due to non-renal causes
• ESKD due to malignancy or history of malignancy (excluding excised and cured non-melanoma skin cancer and cervical carcinoma in situ)
• Systemic hematologic disease
• Peritoneal dialysis or compromised venous access
• Uncontrolled diabetes mellitus (HbA1C >9%), hypertension (home systolic BP [SBP] >160 mm Hg, home diastolic BP [DBP] >90 mm Hg), or heart failure (New York Heart Association class ≥3)
• Alanine transaminase and/or aspartate transaminase values >2× the upper limit of normal; C-reactive protein >50 mg/L
• Red blood cell transfusion <8 weeks before screening
• Anticipated or scheduled living donor renal transplant
Study Design• This was a randomized, single-blind, placebo-controlled, sequential dose-escalation study in subjects with ESKD on hemodialysis (Figure 1).
• Eligible subjects were randomized to 2 arms (sotatercept or placebo in a 3:1 ratio) in 4 sequential dose groups (sotatercept 0.3 mg/kg, 0.5 mg/kg, 0.7 mg/kg, or 0.7 mg/kg loading dose followed by 0.4 mg/kg).
– This interim analysis informed the data monitoring committee’s decision to open enrollment for the high-dose group (sotatercept 0.7 mg/kg).
– At the time of abstract submission:
§ Enrollment in the sotatercept 0.3 mg/kg and 0.5 mg/kg dose groups was completed.
§ Enrollment in the sotatercept 0.7 mg/kg dose group was ongoing.
• Sotatercept doses could have been delayed, reduced, or discontinued based on the subject’s absolute predialysis Hb level or change in Hb level observed after dosing, or discontinued based on change in home BP measurements.
– Delayed: Hb ≥11 to <13 g/dL on Dose Cycle Day 36 (0.3, 0.5, and 0.7 mg/kg dose groups) or Dose Cycle Day 19 (0.7/0.4 mg/kg dose group)
– Reduced: If a dose was delayed, OR if Hb <11 g/dL AND rate of rise of >2 g/dL (0.3, 0.5, and 0.7 mg/kg dose groups) or >1 g/dL (0.7/0.4 mg/kg dose group)
– Discontinued:
§ Persistent hypertension recorded by home BP monitor mean of 4 days of home SBP >160 mm Hg AND increase in SBP from baseline of >20 mm Hg, or mean increase from baseline DBP of >10 mm Hg
§ Hb ≥13 g/dL at any time after randomization
§ Hb ≥12 to <13 g/dL for 2 consecutive weeks at any time after randomization
• Rescue treatment was recommended for subjects with Hb <9 g/dL after the first dose cycle, and those required to discontinue sotatercept could receive ESA treatment or red blood cell transfusion.
• All randomized subjects, including those who were rescued or discontinued early, continued to follow the visit schedule and home BP monitoring throughout the 200-day treatment phase and 112-day follow-up phase.
• The current report describes interim analysis of the sotatercept 0.3 mg/kg and 0.5 mg/kg dose groups for the purpose of determining safety of proceeding to the next dose group.
Figure 1. Study Design
Follow-up phase for 112 days for PK
and safety
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.3 mg/kgSC (n ~9) q28d,up to 8 doses
Placebo (n ~3)q28d, up to 8 doses
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.5 mg/kgSC (n ~9) q28d,up to 8 doses
Placebo (n ~3)q28d, up to 8 doses
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.7 mg/kgSC (n ~9) q28d,
up to 8 doses
Placebo (n ~3)q28d, up to 8 doses
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.7 mg/kg SC q14d(2 doses), then 0.4 mg/kg SC q14d
up to 13 doses (n ~9)
Placebo (n ~3)q14d, up to 15 doses
Note: All randomized subjects will continue treatment with sotatercept 0.3, 0.5, or 0.7 mg/kg or placebo for up to 8 doses* unless rescued or discontinued early. *At 0.7/0.4 mg/kg, all randomized subjects will continue treatment for up to 15 doses unless rescued or discontinued early.28 days after the 6th subject is dosed with sotatercept in each dose group (0.3, 0.5, and 0.7 mg/kg), an interim analysis will occur to evaluate PK and safety before opening the next dose group.
Table 3. Sotatercept PK in ESKD Subjects on Hemodialysis (Dose 1, Cycle 1)
Sotatercept
Parameter0.3 mg/kg
n=90.5 mg/kg
n=6
tmax, mean (min–max), day 12 (2–14) 7 (2–14)
Cmax, mean (SD), μg/mL 2.4 (0.96) 3.5 (0.73)
AUC28d, mean (SD), day•μg/mL 50.5 (17.4) 73.2 (11.5)
t1/2,z, mean (SD), day 22.3 (3.0)* 24.5 (8.9)*†
CL/F, mean (SD), mL/day/kg 3.65 (1.60)* 3.83 (1.19)*†
Vz/F, mean (SD), mL/kg 117 (54)* 124 (27.9)*†
AUC28d=area under the concentration-vs.-time curve up to 28 days; CL/F=oral clearance; Vz/F=apparent volume of distribution.*Estimated according to a 1-compartment model.†The 28-day data may not be sufficient for accurate estimation in some subjects.
Figure 2. Sotatercept Serum Concentration Over Time
Seru
m S
otat
erce
pt (µ
g/m
L)
5
4
3
2
1
0
Days After the First Dose
0 7 14 21 28
Sotatercept 0.3 mg/kg
Sotatercept 0.5 mg/kg
Safety• An overview of AEs is provided in Table 4.
• A decrease in serum calcium levels during follow-up in subjects who had received sotatercept 0.3 mg/kg was noted, without AEs of hypocalcemia.
• There were no other observed trends in laboratory, electrocardiogram, or vital sign parameters, including study visit and intra-dialytic BP, in either dose group of sotatercept during long-term follow-up.
• No anti-drug antibodies, injection site reactions, or hypersensitivity reactions were observed.
Table 4. Overview of AEs (Safety Population, N=20)
Placebo Sotatercept
n=50.3 mg/kg
n=90.5 mg/kg
n=6
Subjects, n (%)
Cumulative days on study 864 2046 634
Any AE 3 (60.0) 8 (88.8) 3 (50.0)
≥1 severe AE 2 (40.0) 2 (22.2) 2 (33.3)
≥1 serious AE 2 (40.0) 2 (22.2) 1 (16.7)
Death 1 (20.0) 0 (0.0) 0 (0.0)
AEs in ≥2 subjects in a treatment group, n (%)
Fatigue 1 (20.0) 2 (22.2) 0 (0.0)
Pain 0 (0.0) 2 (22.2) 0 (0.0)
Constipation 1 (20.0) 2 (22.2) 0 (0.0)
Hypertension 0 (0.0) 3 (33.3)* 0 (0.0)
*A total of 3 subjects randomized to sotatercept 0.3 mg/kg reported 4 AEs of hypertension; 3 of the 4 events occurred after rescue with erythropoietin.
EfficacyTarget Hb Increase (≥1 g/dL), and Target Hb Range (10–12 g/dL) During the First 28 Days
• Baseline Hb levels were 9.7 g/dL in subjects receiving placebo, 9.3 g/dL in subjects receiving sotatercept 0.3 mg/kg, and 8.9 g/dL in subjects receiving sotatercept 0.5 mg/kg.
• Hb increase ≥1.0 g/dL was achieved by 20% (placebo), 37.5% (sotatercept 0.3 mg/kg), and 40% (sotatercept 0.5 mg/kg) of subjects (Figure 3).
• The desired Hb range (10–12 g/dL) was achieved in 60% (placebo), 25% (sotatercept 0.3 mg/kg), and 60% (sotatercept 0.5 mg/kg) during the first dose cycle.
• Mean peak Hb increase in the first 28-day dose cycle was 0.1 g/dL in subjects receiving placebo, 0.5 g/dL in subjects receiving sotatercept 0.3 mg/kg, and 0.8 g/dL in subjects receiving sotatercept 0.5 mg/kg (Figure 4).
• Rescue therapy was required (Hb <9 g/dL) in 2 of 5 subjects after administration of placebo and 1 of 8 subjects after administration of sotatercept 0.3 mg/kg, while none required rescue after sotatercept 0.5 mg/kg (Figure 3).
Figure 3. Hb Increase During the First 28-Day Dose Cycle (Per-Protocol Population)*
0
30
20
10
40
60
50
70
80
90
100
Subj
ects
(%)
Placebo(n=5)
40
40
20
Sotatercept 0.3 mg/kg(n=8)
13
50
37
Sotatercept 0.5 mg/kg
(n=5)
60
40
0.1-0.9 g/dL
Required Rescue (Hb <9 g/dL)
≥1.0 g/dL
*Two subjects with a major protocol violation were excluded from efficacy analyses.
PK Assessment• Blood samples for analysis of sotatercept PK were collected at each study visit and on each sotatercept or placebo dosing day. Additional samples were obtained after
dose 1 at 4 hours post-dose on Day 1 and at 48 hours post-dose on Day 3.
• A validated, competitive enzyme-linked immunosorbent assay using anti‐human ActRIIA antibodies (R&D Systems, Minneapolis, MN) was used to measure the sotatercept serum concentration.
Hb Assessments• Blood samples for Hb assessment were obtained at all scheduled study visits, including before dosing.
Home BP Monitoring• Because of the burden of hypertension in the hemodialysis population, and the inherent variability in hemodialysis-related BP measurement, home BP monitoring was
used to provide a BP profile more reflective of the subject’s steady state.
• Subjects obtained their BP at home 2×/day (3 measurements each upon waking and at bedtime) for 4 consecutive days within 7 days of a scheduled dosing day. Each subject was trained to use a sponsor-provided BP monitor.
• At least 3 waking and 3 bedtime values downloaded from the device by study personnel were used to calculate mean BP values before screening, randomization, and re-dosing.
• Home BP monitoring continued for subjects requiring rescue.
Safety Assessments• Safety assessments included collection of adverse events (AEs), hematology testing, and vital signs at each visit and physical examination and 12-lead
electrocardiogram at selected scheduled time points.
– Safety assessments were done in the event of early termination/withdrawal.
• Proportions of subjects with Hb >12 g/dL at any time and rise in Hb >2 g/dL over 4 weeks were also determined.
• At each interim analysis, blood samples were analyzed for the presence of anti-sotatercept antibodies.
Statistical Analysis• Sotatercept multidose PK was examined among all subjects who received at least 1 dose of study medication and who had evaluable PK data.
• Sotatercept efficacy was evaluated in the full analysis set (FAS), which comprised all randomized subjects who received at least 1 dose of study medication and had at least 1 post-dose follow-up visit, and a baseline value (for analyses that require baseline comparison). Subjects assigned to placebo in both dose groups were combined to form a single placebo group for analysis purposes.
• Efficacy end points included:
– Proportion of subjects achieving target Hb increase (≥1 g/dL increase from baseline).
– Proportion of subjects achieving target Hb concentration >10 g/dL to <12 g/dL.
– Proportion of subjects requiring rescue therapy.
– Change from baseline Hb during the first 28-day dosing cycle, including peak Hb response.
• Proportional and continuous end points were summarized descriptively.
• The final mean home BP value was calculated by first determining the mean of 3 waking and 3 bedtime sets of BP measures. Next, the mean waking and mean bedtime values from a single day were both used to calculate the day mean. Finally, the mean of the day means was calculated, and this comprised the final mean home BP.
• Home BP measures and safety measures were summarized descriptively.
RESULTSSubjects• A total of 21 subjects were randomized and received study medication. One subject was randomized to sotatercept 0.5 mg/kg and received 1 dose of study medication;
however, this subject did not have the first follow-up visit at the time of the interim database cutoff point and was not included in either the safety or efficacy population. A total of 20 subjects comprise the FAS and safety population:
– 5 who received placebo.
– 9 who received sotatercept 0.3 mg/kg.
– 6 who received sotatercept 0.5 mg/kg.
• Interim subject disposition is illustrated in Table 1.
• Baseline subject demographics and disease characteristics were generally similar across treatment groups (Table 2).
• Major protocol violations were noted for 2 subjects randomized to sotatercept. One subject (0.3 mg/kg) received erythropoietin prior to randomization and through the first dose cycle, and was discontinued from the study; 1 subject (0.5 mg/kg) had an incomplete baseline home BP evaluation, which showed a non-qualifying elevation in BP prior to randomization, and was discontinued from study medication early. These subjects were excluded from efficacy analyses, as a per-protocol analysis defined in the protocol. Included in the efficacy analysis population were:
– 5 who received placebo.
– 8 who received sotatercept 0.3 mg/kg.
– 5 who received sotatercept 0.5 mg/kg.
Table 1. Subject Disposition (FAS, N=20)
GroupOngoing on Study Drug
D/C Study Drug (Being Followed)
Completers on Study Drug (≥200 Days)
Completers After D/C Study Drug Early Termination Total Rescued
D/C Study Drug Due to Stopping Rule
Placebo, n=5 0 2 1 1 1 3 0
Sotatercept 0.3 mg/kg, n=9 0 0 2 5 2 7 0
Sotatercept 0.5 mg/kg, n=6 3 2 0 0 1 2 1
D/C=discontinued.
Table 2. Demographic Characteristics of Subjects (FAS, N=20)
Placebo Sotatercept
n=50.3 mg/kg
n=90.5 mg/kg
n=6
Age, mean, years 58.4 59.9 60.7
Female, n (%) 1 (20.0) 6 (66.7) 1 (16.7)
Race, n (%)
White 1 (20.0) 3 (33.3) 4 (66.7)
Black 3 (60.0) 6 (66.7) 2 (33.3)
Asian 1 (20.0) 0 (0.0) 0 (0.0)
Ethnicity
Hispanic 0 (0.0) 2 (22.2) 4 (66.7)
Non-Hispanic 5 (100.0) 7 (77.8) 2 (33.3)
Weight, postdialysis mean, kg 75.8 79.4 81.0
Body mass index, mean, kg/m2 25.4 27.8 27.3
Sotatercept PK• Preliminary, interim PK data, based on analysis of all subjects randomized to sotatercept 0.3 mg/kg and the first 6 subjects randomized to sotatercept 0.5 mg/kg, are
presented in Table 3.
• Sotatercept exhibited dose-dependent increases in the serum drug exposure (Cmax and AUC), with a mean elimination half-life (t1/2,z) of 22 to 25 days.
• Sotatercept mean concentration-vs.-time profiles for the 0.3 mg/kg and 0.5 mg/kg dose groups are shown in Figure 2.
Figure 4. Mean Peak Hemoglobin Increase During the First 28-Day Dose Cycle (Per-Protocol Population)*
Sotatercept 0.3 mg/kg (n=8)
Sotatercept 0.5 mg/kg (n=5)
Placebo (n=5)
0.1
0.5
0.8
0
0.3
0.2
0.1
0.4
0.5
0.6
0.7
0.8
0.9
Hb (g
/dL)
Cha
nge
From
Bas
elin
e
Mean Peak Hemoglobin Response
*Two subjects with a major protocol violation were excluded from efficacy analyses.
Change From Baseline in Hb Concentration• Mean Hb concentration in subjects who received sotatercept 0.3 mg/kg and 0.5 mg/kg exhibited a greater increase from baseline in the first 15 days post-dose
(vs. placebo); however, the increases were not sustained through the entire dose cycle.
• Hb levels throughout multiple dose cycles among subjects who did not require rescue were generally highest among subjects receiving sotatercept 0.5 mg/kg (Figure 5).
Figure 5. Hb Change From Baseline During Long-term Sotatercept Treatment Censored for Rescue
−3
−2
−1
0
1
2
3
4
50 100 150 200 250
Days After the First Dose
Hem
oglo
bin
(g/d
L)
Sotatercept 0.3 mg/kg (n=8)Sotatercept 0.5 mg/kg (n=5)
Placebo (n=5)
Home BP Measurements• Home BP measures in the first dose cycle revealed that all 3 groups had increases in group mean SBP, with the largest change in subjects receiving sotatercept
0.3 mg/kg, while the largest change in DBP was in subjects receiving placebo. All the group mean changes were <10 mm Hg (Figure 6A and B).
– Findings were similar when analyzed for both the per-protocol population (Figure 6A) and FAS (Figure 6B).
• With long-term treatment, home BP measures showed no consistent change from baseline among subjects in any of the treatment groups (Figure 7).
Figure 6. Change From Baseline in Home BP at the End of Dose Cycle 1 in the (A) Per-Protocol Population* and (B) FAS
Sotatercept 0.3 mg/kg (n=7)
Sotatercept 0.5 mg/kg (n=4)
Placebo (n=3)
Sotatercept 0.3 mg/kg (n=9)
Sotatercept 0.5 mg/kg (n=5)
Placebo (n=4)
Chan
ge F
rom
Bas
elin
e BP
(mm
Hg)
0.0
2.0
6.0
3.3 3.3
–0.3 –1.0
0.0
1.0
2.0
3.0
4.0
5.0
6.0
7.0
SBP DBP
A
B
Chan
ge F
rom
Bas
elin
e BP
(mm
Hg)
2.3
7.5
3.0 2.5
7.6
0.4
0.0
1.0
2.0
3.0
4.0
5.0
6.0
7.0
8.0
SBP DBP
*Data exclude subjects with protocol violations and are censored for those who required rescue in the first dose cycle.
Figure 7. Change From Baseline Home BP Measurements (FAS) of (A) SBP and (B) DBP During Long-term Sotatercept Treatment, Censored for Rescue
A SBP
B DBP
–20
–15
–10
–5
0
5
10
15
20
25
50 100 150 200 250
Sotatercept 0.3 mg/kg (n=9)Sotatercept 0.5 mg/kg (n=5)
Placebo (n=4)
Hom
e DB
P (m
m H
g)
–50
–40
–30
–20
–10
0
10
20
30
40
50 100 150 200 250
Sotatercept 0.3 mg/kg (n=9)Sotatercept 0.5 mg/kg (n=5)
Placebo (n=4)
Hom
e SB
P (m
m H
g)
CONCLUSIONS• Sotatercept exhibited linear PK characteristics, and a long half-life of 22 to 25 days.
• Sotatercept was well tolerated, with AEs similar to those observed with placebo and no trends toward increased BP.
• Exposure to sotatercept was not associated with the development of anti-drug antibodies, injection site reactions, or hypersensitivity reactions.
• In the first 28 days of treatment, the proportion of subjects achieving the target Hb increase of ≥1 g/dL was greater in the treatment groups than in the placebo group, and the proportion requiring rescue therapy in the first 28 days was dose-related, with no subjects in the sotatercept 0.5 mg/kg group requiring rescue.
• In this initial 28-day analysis, in which the placebo and sotatercept 0.3 mg/kg groups had higher baseline Hb, no differences between groups achieving the target Hb range (10-12 g/dL) were observed. Dose escalation continues per protocol.
• Mean peak Hb response in the first 28 days was dose-related, with the sotatercept 0.5 mg/kg dose having the highest mean peak Hb response.
• Hb improvements were generally sustained for multiple dosing cycles in the sotatercept 0.5 mg/kg dose group.
• This preliminary interim analysis indicates adequate Hb responses and safety of sotatercept at 0.3 and 0.5 mg/kg and provides evidence to continue the evaluation of sotatercept at 0.7 mg/kg in patients with ESKD on hemodialysis.
REFERENCES1. Babitt JL, Lin HY. Mechanisms of anemia in CKD. J Am Soc Nephrol. 2012;23:1631-1634.
2. Jacobson LO, Goldwasser E, Fried W, et al. Role of the kidney in erythropoiesis. Nature. 1957;179:633-634.
3. McGonigle RJ, Wallin JD, Shadduck RK, et al. Erythropoietin deficiency and inhibition of erythropoiesis in renal insufficiency. Kidney Int. 1984;25:437-444.
4. Eschbach JW, Egrie JC, Downing MR, et al. Correction of the anemia of end-stage renal disease with recombinant human erythropoietin. Results of a combined phase I and II clinical trial. N Engl J Med. 1987;316:73-78.
5. Singh AK, Szczech L, Tang KL, et al. Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med. 2006;355: 2085-2098.
6. Fishbane S. Anemia and cardiovascular risk in the patient with kidney disease. Heart Fail Clin. 2008;4:401-410.
7. Besarab A, Bolton WK, Browne JK, et al. The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. N Engl J Med. 1998;339:584-590.
8. Drueke TB, Locatelli F, Clyne N, et al. Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med. 2006;355:2071-2084.
9. Pfeffer MA, Burdmann EA, Chen CY, et al. A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. N Engl J Med. 2009;361:2019-2032.
10. Pearsall RS, Canalis E, Cornwall-Brady M, et al. A soluble activin type IIA receptor induces bone formation and improves skeletal integrity. Proc Natl Acad Sci U S A. 2008;105:7082-7087.
11. Iancu-Rubin C, Mosoyan G, Wang J, et al. Stromal cell-mediated inhibition of erythropoiesis can be attenuated by sotatercept (ACE-011), an activin receptor type II ligand trap. Exp Hematol. 2013;41:155-166.
12. Sherman ML, Borgstein NG, Mook L, et al. Multiple-dose, safety, pharmacokinetic, and pharmacodynamic study of sotatercept (ActRIIA-IgG1), a novel erythropoietic agent, in healthy postmenopausal women. J Clin Pharmacol. 2013;53:1121-1130.
13. Wooldridge T, Kaplan M, Alcorn H Jr, et al. The pharmacokinetics and safety of a single-dose of sotatercept (ACE-011) in subjects on hemodialysis and the effects of its murine analog (RAP-011) on anemia and in preventing bone loss in C57BL/6 mice with 5/6 nephrectomy [oral presentation]. Presented at: American Society of Nephrology Kidney Week 2012; October 30-November 4, 2012; San Diego, CA.
This study was sponsored by Celgene Corporation.
Presented at: the National Kidney Foundation (NKF) 2014 Spring Clinical Meeting; April 22–26, 2014; Las Vegas, NV.Scan this QR code to receive
the PDF of the poster

Interim Analysis of ACE-011-REN-001: The First 28-Day Dose Cycle of Low and Medium Starting Doses of Sotatercept Compared to Placebo for Correction of Anemia in Hemodialysis Subjects
Mohamed El-Shahawy1; James Cotton2; Jeffrey Kaupke3; Thomas D. Wooldridge4; Hem N. Singh5; William T. Smith51Academic Medical Research Institute, Los Angeles, CA, USA; 2Tyler Nephrology Associates PC, Tyler, TX, USA; 3Nephrology Specialist Medical Group, Orange, CA, USA; 4Nephrology & Hypertension Associates LTD, Tupelo, MS, USA; 5Celgene Corporation, Warren, NJ, USA
INTRODUCTION• The anemia seen in patients with end-stage kidney disease (ESKD) is largely due to decreased biosynthesis of erythropoietin from the kidneys.1-3
• A number of erythropoiesis-stimulating agents (ESAs) have demonstrated efficacy in increasing hemoglobin (Hb) levels in patients with ESKD,4,5 but pose significant safety risks, including persistent hypertension, serious cardiovascular events, and increased risk of death.4,5
• Multiple observational studies have linked low Hb levels to poor cardiovascular outcomes.6 However, recent clinical studies have demonstrated that ESAs are unable to modify this risk when targeting a normal Hb level.5,7-9
• Sotatercept (ACE-011) is an ActRIIA-IgG1 fusion protein trap that binds with high affinity to activin A and other members of the TGFb superfamily and acts on late-stage erythropoiesis to increase the production of mature erythrocytes into the circulation.10-12
• This 2-part, phase IIA, randomized, placebo-controlled trial is the first to evaluate the pharmacokinetics (PK), safety, tolerability, and Hb effect of sotatercept in ESKD subjects with renal anemia receiving hemodialysis.
• In part 1, after a single subcutaneous dose (0.1 mg/kg) of sotatercept13:
– PK parameters were similar to a phase I study in healthy postmenopausal women, with a long half-life (21 days).
– Sotatercept was not dialyzable.
– There was no evidence of a pharmacodynamic effect on Hb concentrations at the single, 0.1 mg/kg dose.
– Sotatercept was well tolerated with no observed changes in blood pressure (BP), and no consistent changes in safety laboratory or electrocardiographic parameters.
• Part 2 is an ongoing, randomized, single-blind, placebo-controlled, sequential dose-escalation study in subjects with ESKD on hemodialysis evaluating the PK, safety, tolerability, and Hb effects of sotatercept for the correction of ESKD-related anemia.
• We report the preliminary, interim analysis of the sotatercept 0.3 mg/kg (low dose) and 0.5 mg/kg (medium dose) treatment groups.
• Pending acceptable interim analysis results, additional patients may be randomized in a staggered parallel fashion to sotatercept 0.7 mg/kg once every 28 days (high dose) and sotatercept 0.7 mg/kg once every 14 days for 28 days followed by 0.4 mg/kg every 14 days for the remainder of the treatment period (Figure 1).
METHODSKey Inclusion Criteria• Adults receiving at least 3 hours of high-flux hemodialysis at each session for at least 12 weeks before screening and no planned changes to the hemodialysis regimen
during the study period
• Adequate Hb response (Hb ≥10 to ≤12 g/dL predialysis mean of 3 consecutive Hb concentrations) to stable doses of ESA (epoetin alfa, darbepoetin) for at least 6 weeks before and during screening, excluding dose holds for high Hb (maximum dose: epoetin alfa ≤500 IU/kg/week; darbepoetin ≤95 μg/week)
• ESKD-related anemia: Hb ≥8 to ≤10 g/dL predialysis after ESA washout
• Adequate iron status (transferrin saturation ≥20%)
• Kt/V ≥1.2 or urea reduction ratio ≥65%
• Parathyroid hormone concentration ≤1,000 pg/mL; phosphorous ≤7 mg/dL; and total albumin-corrected calcium ≥8.0 to ≤10.5 mg/dL
Key Exclusion Criteria• Anemia due to non-renal causes
• ESKD due to malignancy or history of malignancy (excluding excised and cured non-melanoma skin cancer and cervical carcinoma in situ)
• Systemic hematologic disease
• Peritoneal dialysis or compromised venous access
• Uncontrolled diabetes mellitus (HbA1C >9%), hypertension (home systolic BP [SBP] >160 mm Hg, home diastolic BP [DBP] >90 mm Hg), or heart failure (New York Heart Association class ≥3)
• Alanine transaminase and/or aspartate transaminase values >2× the upper limit of normal; C-reactive protein >50 mg/L
• Red blood cell transfusion <8 weeks before screening
• Anticipated or scheduled living donor renal transplant
Study Design• This was a randomized, single-blind, placebo-controlled, sequential dose-escalation study in subjects with ESKD on hemodialysis (Figure 1).
• Eligible subjects were randomized to 2 arms (sotatercept or placebo in a 3:1 ratio) in 4 sequential dose groups (sotatercept 0.3 mg/kg, 0.5 mg/kg, 0.7 mg/kg, or 0.7 mg/kg loading dose followed by 0.4 mg/kg).
– This interim analysis informed the data monitoring committee’s decision to open enrollment for the high-dose group (sotatercept 0.7 mg/kg).
– At the time of abstract submission:
§ Enrollment in the sotatercept 0.3 mg/kg and 0.5 mg/kg dose groups was completed.
§ Enrollment in the sotatercept 0.7 mg/kg dose group was ongoing.
• Sotatercept doses could have been delayed, reduced, or discontinued based on the subject’s absolute predialysis Hb level or change in Hb level observed after dosing, or discontinued based on change in home BP measurements.
– Delayed: Hb ≥11 to <13 g/dL on Dose Cycle Day 36 (0.3, 0.5, and 0.7 mg/kg dose groups) or Dose Cycle Day 19 (0.7/0.4 mg/kg dose group)
– Reduced: If a dose was delayed, OR if Hb <11 g/dL AND rate of rise of >2 g/dL (0.3, 0.5, and 0.7 mg/kg dose groups) or >1 g/dL (0.7/0.4 mg/kg dose group)
– Discontinued:
§ Persistent hypertension recorded by home BP monitor mean of 4 days of home SBP >160 mm Hg AND increase in SBP from baseline of >20 mm Hg, or mean increase from baseline DBP of >10 mm Hg
§ Hb ≥13 g/dL at any time after randomization
§ Hb ≥12 to <13 g/dL for 2 consecutive weeks at any time after randomization
• Rescue treatment was recommended for subjects with Hb <9 g/dL after the first dose cycle, and those required to discontinue sotatercept could receive ESA treatment or red blood cell transfusion.
• All randomized subjects, including those who were rescued or discontinued early, continued to follow the visit schedule and home BP monitoring throughout the 200-day treatment phase and 112-day follow-up phase.
• The current report describes interim analysis of the sotatercept 0.3 mg/kg and 0.5 mg/kg dose groups for the purpose of determining safety of proceeding to the next dose group.
Figure 1. Study Design
Follow-up phase for 112 days for PK
and safety
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.3 mg/kgSC (n ~9) q28d,up to 8 doses
Placebo (n ~3)q28d, up to 8 doses
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.5 mg/kgSC (n ~9) q28d,up to 8 doses
Placebo (n ~3)q28d, up to 8 doses
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.7 mg/kgSC (n ~9) q28d,
up to 8 doses
Placebo (n ~3)q28d, up to 8 doses
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.7 mg/kg SC q14d(2 doses), then 0.4 mg/kg SC q14d
up to 13 doses (n ~9)
Placebo (n ~3)q14d, up to 15 doses
Note: All randomized subjects will continue treatment with sotatercept 0.3, 0.5, or 0.7 mg/kg or placebo for up to 8 doses* unless rescued or discontinued early. *At 0.7/0.4 mg/kg, all randomized subjects will continue treatment for up to 15 doses unless rescued or discontinued early.28 days after the 6th subject is dosed with sotatercept in each dose group (0.3, 0.5, and 0.7 mg/kg), an interim analysis will occur to evaluate PK and safety before opening the next dose group.
Table 3. Sotatercept PK in ESKD Subjects on Hemodialysis (Dose 1, Cycle 1)
Sotatercept
Parameter0.3 mg/kg
n=90.5 mg/kg
n=6
tmax, mean (min–max), day 12 (2–14) 7 (2–14)
Cmax, mean (SD), μg/mL 2.4 (0.96) 3.5 (0.73)
AUC28d, mean (SD), day•μg/mL 50.5 (17.4) 73.2 (11.5)
t1/2,z, mean (SD), day 22.3 (3.0)* 24.5 (8.9)*†
CL/F, mean (SD), mL/day/kg 3.65 (1.60)* 3.83 (1.19)*†
Vz/F, mean (SD), mL/kg 117 (54)* 124 (27.9)*†
AUC28d=area under the concentration-vs.-time curve up to 28 days; CL/F=oral clearance; Vz/F=apparent volume of distribution.*Estimated according to a 1-compartment model.†The 28-day data may not be sufficient for accurate estimation in some subjects.
Figure 2. Sotatercept Serum Concentration Over Time
Seru
m S
otat
erce
pt (µ
g/m
L)
5
4
3
2
1
0
Days After the First Dose
0 7 14 21 28
Sotatercept 0.3 mg/kg
Sotatercept 0.5 mg/kg
Safety• An overview of AEs is provided in Table 4.
• A decrease in serum calcium levels during follow-up in subjects who had received sotatercept 0.3 mg/kg was noted, without AEs of hypocalcemia.
• There were no other observed trends in laboratory, electrocardiogram, or vital sign parameters, including study visit and intra-dialytic BP, in either dose group of sotatercept during long-term follow-up.
• No anti-drug antibodies, injection site reactions, or hypersensitivity reactions were observed.
Table 4. Overview of AEs (Safety Population, N=20)
Placebo Sotatercept
n=50.3 mg/kg
n=90.5 mg/kg
n=6
Subjects, n (%)
Cumulative days on study 864 2046 634
Any AE 3 (60.0) 8 (88.8) 3 (50.0)
≥1 severe AE 2 (40.0) 2 (22.2) 2 (33.3)
≥1 serious AE 2 (40.0) 2 (22.2) 1 (16.7)
Death 1 (20.0) 0 (0.0) 0 (0.0)
AEs in ≥2 subjects in a treatment group, n (%)
Fatigue 1 (20.0) 2 (22.2) 0 (0.0)
Pain 0 (0.0) 2 (22.2) 0 (0.0)
Constipation 1 (20.0) 2 (22.2) 0 (0.0)
Hypertension 0 (0.0) 3 (33.3)* 0 (0.0)
*A total of 3 subjects randomized to sotatercept 0.3 mg/kg reported 4 AEs of hypertension; 3 of the 4 events occurred after rescue with erythropoietin.
EfficacyTarget Hb Increase (≥1 g/dL), and Target Hb Range (10–12 g/dL) During the First 28 Days
• Baseline Hb levels were 9.7 g/dL in subjects receiving placebo, 9.3 g/dL in subjects receiving sotatercept 0.3 mg/kg, and 8.9 g/dL in subjects receiving sotatercept 0.5 mg/kg.
• Hb increase ≥1.0 g/dL was achieved by 20% (placebo), 37.5% (sotatercept 0.3 mg/kg), and 40% (sotatercept 0.5 mg/kg) of subjects (Figure 3).
• The desired Hb range (10–12 g/dL) was achieved in 60% (placebo), 25% (sotatercept 0.3 mg/kg), and 60% (sotatercept 0.5 mg/kg) during the first dose cycle.
• Mean peak Hb increase in the first 28-day dose cycle was 0.1 g/dL in subjects receiving placebo, 0.5 g/dL in subjects receiving sotatercept 0.3 mg/kg, and 0.8 g/dL in subjects receiving sotatercept 0.5 mg/kg (Figure 4).
• Rescue therapy was required (Hb <9 g/dL) in 2 of 5 subjects after administration of placebo and 1 of 8 subjects after administration of sotatercept 0.3 mg/kg, while none required rescue after sotatercept 0.5 mg/kg (Figure 3).
Figure 3. Hb Increase During the First 28-Day Dose Cycle (Per-Protocol Population)*
0
30
20
10
40
60
50
70
80
90
100
Subj
ects
(%)
Placebo(n=5)
40
40
20
Sotatercept 0.3 mg/kg(n=8)
13
50
37
Sotatercept 0.5 mg/kg
(n=5)
60
40
0.1-0.9 g/dL
Required Rescue (Hb <9 g/dL)
≥1.0 g/dL
*Two subjects with a major protocol violation were excluded from efficacy analyses.
PK Assessment• Blood samples for analysis of sotatercept PK were collected at each study visit and on each sotatercept or placebo dosing day. Additional samples were obtained after
dose 1 at 4 hours post-dose on Day 1 and at 48 hours post-dose on Day 3.
• A validated, competitive enzyme-linked immunosorbent assay using anti‐human ActRIIA antibodies (R&D Systems, Minneapolis, MN) was used to measure the sotatercept serum concentration.
Hb Assessments• Blood samples for Hb assessment were obtained at all scheduled study visits, including before dosing.
Home BP Monitoring• Because of the burden of hypertension in the hemodialysis population, and the inherent variability in hemodialysis-related BP measurement, home BP monitoring was
used to provide a BP profile more reflective of the subject’s steady state.
• Subjects obtained their BP at home 2×/day (3 measurements each upon waking and at bedtime) for 4 consecutive days within 7 days of a scheduled dosing day. Each subject was trained to use a sponsor-provided BP monitor.
• At least 3 waking and 3 bedtime values downloaded from the device by study personnel were used to calculate mean BP values before screening, randomization, and re-dosing.
• Home BP monitoring continued for subjects requiring rescue.
Safety Assessments• Safety assessments included collection of adverse events (AEs), hematology testing, and vital signs at each visit and physical examination and 12-lead
electrocardiogram at selected scheduled time points.
– Safety assessments were done in the event of early termination/withdrawal.
• Proportions of subjects with Hb >12 g/dL at any time and rise in Hb >2 g/dL over 4 weeks were also determined.
• At each interim analysis, blood samples were analyzed for the presence of anti-sotatercept antibodies.
Statistical Analysis• Sotatercept multidose PK was examined among all subjects who received at least 1 dose of study medication and who had evaluable PK data.
• Sotatercept efficacy was evaluated in the full analysis set (FAS), which comprised all randomized subjects who received at least 1 dose of study medication and had at least 1 post-dose follow-up visit, and a baseline value (for analyses that require baseline comparison). Subjects assigned to placebo in both dose groups were combined to form a single placebo group for analysis purposes.
• Efficacy end points included:
– Proportion of subjects achieving target Hb increase (≥1 g/dL increase from baseline).
– Proportion of subjects achieving target Hb concentration >10 g/dL to <12 g/dL.
– Proportion of subjects requiring rescue therapy.
– Change from baseline Hb during the first 28-day dosing cycle, including peak Hb response.
• Proportional and continuous end points were summarized descriptively.
• The final mean home BP value was calculated by first determining the mean of 3 waking and 3 bedtime sets of BP measures. Next, the mean waking and mean bedtime values from a single day were both used to calculate the day mean. Finally, the mean of the day means was calculated, and this comprised the final mean home BP.
• Home BP measures and safety measures were summarized descriptively.
RESULTSSubjects• A total of 21 subjects were randomized and received study medication. One subject was randomized to sotatercept 0.5 mg/kg and received 1 dose of study medication;
however, this subject did not have the first follow-up visit at the time of the interim database cutoff point and was not included in either the safety or efficacy population. A total of 20 subjects comprise the FAS and safety population:
– 5 who received placebo.
– 9 who received sotatercept 0.3 mg/kg.
– 6 who received sotatercept 0.5 mg/kg.
• Interim subject disposition is illustrated in Table 1.
• Baseline subject demographics and disease characteristics were generally similar across treatment groups (Table 2).
• Major protocol violations were noted for 2 subjects randomized to sotatercept. One subject (0.3 mg/kg) received erythropoietin prior to randomization and through the first dose cycle, and was discontinued from the study; 1 subject (0.5 mg/kg) had an incomplete baseline home BP evaluation, which showed a non-qualifying elevation in BP prior to randomization, and was discontinued from study medication early. These subjects were excluded from efficacy analyses, as a per-protocol analysis defined in the protocol. Included in the efficacy analysis population were:
– 5 who received placebo.
– 8 who received sotatercept 0.3 mg/kg.
– 5 who received sotatercept 0.5 mg/kg.
Table 1. Subject Disposition (FAS, N=20)
GroupOngoing on Study Drug
D/C Study Drug (Being Followed)
Completers on Study Drug (≥200 Days)
Completers After D/C Study Drug Early Termination Total Rescued
D/C Study Drug Due to Stopping Rule
Placebo, n=5 0 2 1 1 1 3 0
Sotatercept 0.3 mg/kg, n=9 0 0 2 5 2 7 0
Sotatercept 0.5 mg/kg, n=6 3 2 0 0 1 2 1
D/C=discontinued.
Table 2. Demographic Characteristics of Subjects (FAS, N=20)
Placebo Sotatercept
n=50.3 mg/kg
n=90.5 mg/kg
n=6
Age, mean, years 58.4 59.9 60.7
Female, n (%) 1 (20.0) 6 (66.7) 1 (16.7)
Race, n (%)
White 1 (20.0) 3 (33.3) 4 (66.7)
Black 3 (60.0) 6 (66.7) 2 (33.3)
Asian 1 (20.0) 0 (0.0) 0 (0.0)
Ethnicity
Hispanic 0 (0.0) 2 (22.2) 4 (66.7)
Non-Hispanic 5 (100.0) 7 (77.8) 2 (33.3)
Weight, postdialysis mean, kg 75.8 79.4 81.0
Body mass index, mean, kg/m2 25.4 27.8 27.3
Sotatercept PK• Preliminary, interim PK data, based on analysis of all subjects randomized to sotatercept 0.3 mg/kg and the first 6 subjects randomized to sotatercept 0.5 mg/kg, are
presented in Table 3.
• Sotatercept exhibited dose-dependent increases in the serum drug exposure (Cmax and AUC), with a mean elimination half-life (t1/2,z) of 22 to 25 days.
• Sotatercept mean concentration-vs.-time profiles for the 0.3 mg/kg and 0.5 mg/kg dose groups are shown in Figure 2.
Figure 4. Mean Peak Hemoglobin Increase During the First 28-Day Dose Cycle (Per-Protocol Population)*
Sotatercept 0.3 mg/kg (n=8)
Sotatercept 0.5 mg/kg (n=5)
Placebo (n=5)
0.1
0.5
0.8
0
0.3
0.2
0.1
0.4
0.5
0.6
0.7
0.8
0.9
Hb (g
/dL)
Cha
nge
From
Bas
elin
e
Mean Peak Hemoglobin Response
*Two subjects with a major protocol violation were excluded from efficacy analyses.
Change From Baseline in Hb Concentration• Mean Hb concentration in subjects who received sotatercept 0.3 mg/kg and 0.5 mg/kg exhibited a greater increase from baseline in the first 15 days post-dose
(vs. placebo); however, the increases were not sustained through the entire dose cycle.
• Hb levels throughout multiple dose cycles among subjects who did not require rescue were generally highest among subjects receiving sotatercept 0.5 mg/kg (Figure 5).
Figure 5. Hb Change From Baseline During Long-term Sotatercept Treatment Censored for Rescue
−3
−2
−1
0
1
2
3
4
50 100 150 200 250
Days After the First Dose
Hem
oglo
bin
(g/d
L)
Sotatercept 0.3 mg/kg (n=8)Sotatercept 0.5 mg/kg (n=5)
Placebo (n=5)
Home BP Measurements• Home BP measures in the first dose cycle revealed that all 3 groups had increases in group mean SBP, with the largest change in subjects receiving sotatercept
0.3 mg/kg, while the largest change in DBP was in subjects receiving placebo. All the group mean changes were <10 mm Hg (Figure 6A and B).
– Findings were similar when analyzed for both the per-protocol population (Figure 6A) and FAS (Figure 6B).
• With long-term treatment, home BP measures showed no consistent change from baseline among subjects in any of the treatment groups (Figure 7).
Figure 6. Change From Baseline in Home BP at the End of Dose Cycle 1 in the (A) Per-Protocol Population* and (B) FAS
Sotatercept 0.3 mg/kg (n=7)
Sotatercept 0.5 mg/kg (n=4)
Placebo (n=3)
Sotatercept 0.3 mg/kg (n=9)
Sotatercept 0.5 mg/kg (n=5)
Placebo (n=4)
Chan
ge F
rom
Bas
elin
e BP
(mm
Hg)
0.0
2.0
6.0
3.3 3.3
–0.3 –1.0
0.0
1.0
2.0
3.0
4.0
5.0
6.0
7.0
SBP DBP
A
B
Chan
ge F
rom
Bas
elin
e BP
(mm
Hg)
2.3
7.5
3.0 2.5
7.6
0.4
0.0
1.0
2.0
3.0
4.0
5.0
6.0
7.0
8.0
SBP DBP
*Data exclude subjects with protocol violations and are censored for those who required rescue in the first dose cycle.
Figure 7. Change From Baseline Home BP Measurements (FAS) of (A) SBP and (B) DBP During Long-term Sotatercept Treatment, Censored for Rescue
A SBP
B DBP
–20
–15
–10
–5
0
5
10
15
20
25
50 100 150 200 250
Sotatercept 0.3 mg/kg (n=9)Sotatercept 0.5 mg/kg (n=5)
Placebo (n=4)
Hom
e DB
P (m
m H
g)
–50
–40
–30
–20
–10
0
10
20
30
40
50 100 150 200 250
Sotatercept 0.3 mg/kg (n=9)Sotatercept 0.5 mg/kg (n=5)
Placebo (n=4)
Hom
e SB
P (m
m H
g)
CONCLUSIONS• Sotatercept exhibited linear PK characteristics, and a long half-life of 22 to 25 days.
• Sotatercept was well tolerated, with AEs similar to those observed with placebo and no trends toward increased BP.
• Exposure to sotatercept was not associated with the development of anti-drug antibodies, injection site reactions, or hypersensitivity reactions.
• In the first 28 days of treatment, the proportion of subjects achieving the target Hb increase of ≥1 g/dL was greater in the treatment groups than in the placebo group, and the proportion requiring rescue therapy in the first 28 days was dose-related, with no subjects in the sotatercept 0.5 mg/kg group requiring rescue.
• In this initial 28-day analysis, in which the placebo and sotatercept 0.3 mg/kg groups had higher baseline Hb, no differences between groups achieving the target Hb range (10-12 g/dL) were observed. Dose escalation continues per protocol.
• Mean peak Hb response in the first 28 days was dose-related, with the sotatercept 0.5 mg/kg dose having the highest mean peak Hb response.
• Hb improvements were generally sustained for multiple dosing cycles in the sotatercept 0.5 mg/kg dose group.
• This preliminary interim analysis indicates adequate Hb responses and safety of sotatercept at 0.3 and 0.5 mg/kg and provides evidence to continue the evaluation of sotatercept at 0.7 mg/kg in patients with ESKD on hemodialysis.
REFERENCES1. Babitt JL, Lin HY. Mechanisms of anemia in CKD. J Am Soc Nephrol. 2012;23:1631-1634.
2. Jacobson LO, Goldwasser E, Fried W, et al. Role of the kidney in erythropoiesis. Nature. 1957;179:633-634.
3. McGonigle RJ, Wallin JD, Shadduck RK, et al. Erythropoietin deficiency and inhibition of erythropoiesis in renal insufficiency. Kidney Int. 1984;25:437-444.
4. Eschbach JW, Egrie JC, Downing MR, et al. Correction of the anemia of end-stage renal disease with recombinant human erythropoietin. Results of a combined phase I and II clinical trial. N Engl J Med. 1987;316:73-78.
5. Singh AK, Szczech L, Tang KL, et al. Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med. 2006;355: 2085-2098.
6. Fishbane S. Anemia and cardiovascular risk in the patient with kidney disease. Heart Fail Clin. 2008;4:401-410.
7. Besarab A, Bolton WK, Browne JK, et al. The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. N Engl J Med. 1998;339:584-590.
8. Drueke TB, Locatelli F, Clyne N, et al. Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med. 2006;355:2071-2084.
9. Pfeffer MA, Burdmann EA, Chen CY, et al. A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. N Engl J Med. 2009;361:2019-2032.
10. Pearsall RS, Canalis E, Cornwall-Brady M, et al. A soluble activin type IIA receptor induces bone formation and improves skeletal integrity. Proc Natl Acad Sci U S A. 2008;105:7082-7087.
11. Iancu-Rubin C, Mosoyan G, Wang J, et al. Stromal cell-mediated inhibition of erythropoiesis can be attenuated by sotatercept (ACE-011), an activin receptor type II ligand trap. Exp Hematol. 2013;41:155-166.
12. Sherman ML, Borgstein NG, Mook L, et al. Multiple-dose, safety, pharmacokinetic, and pharmacodynamic study of sotatercept (ActRIIA-IgG1), a novel erythropoietic agent, in healthy postmenopausal women. J Clin Pharmacol. 2013;53:1121-1130.
13. Wooldridge T, Kaplan M, Alcorn H Jr, et al. The pharmacokinetics and safety of a single-dose of sotatercept (ACE-011) in subjects on hemodialysis and the effects of its murine analog (RAP-011) on anemia and in preventing bone loss in C57BL/6 mice with 5/6 nephrectomy [oral presentation]. Presented at: American Society of Nephrology Kidney Week 2012; October 30-November 4, 2012; San Diego, CA.
This study was sponsored by Celgene Corporation.
Presented at: the National Kidney Foundation (NKF) 2014 Spring Clinical Meeting; April 22–26, 2014; Las Vegas, NV.Scan this QR code to receive
the PDF of the poster

Interim Analysis of ACE-011-REN-001: The First 28-Day Dose Cycle of Low and Medium Starting Doses of Sotatercept Compared to Placebo for Correction of Anemia in Hemodialysis Subjects
Mohamed El-Shahawy1; James Cotton2; Jeffrey Kaupke3; Thomas D. Wooldridge4; Hem N. Singh5; William T. Smith51Academic Medical Research Institute, Los Angeles, CA, USA; 2Tyler Nephrology Associates PC, Tyler, TX, USA; 3Nephrology Specialist Medical Group, Orange, CA, USA; 4Nephrology & Hypertension Associates LTD, Tupelo, MS, USA; 5Celgene Corporation, Warren, NJ, USA
INTRODUCTION• The anemia seen in patients with end-stage kidney disease (ESKD) is largely due to decreased biosynthesis of erythropoietin from the kidneys.1-3
• A number of erythropoiesis-stimulating agents (ESAs) have demonstrated efficacy in increasing hemoglobin (Hb) levels in patients with ESKD,4,5 but pose significant safety risks, including persistent hypertension, serious cardiovascular events, and increased risk of death.4,5
• Multiple observational studies have linked low Hb levels to poor cardiovascular outcomes.6 However, recent clinical studies have demonstrated that ESAs are unable to modify this risk when targeting a normal Hb level.5,7-9
• Sotatercept (ACE-011) is an ActRIIA-IgG1 fusion protein trap that binds with high affinity to activin A and other members of the TGFb superfamily and acts on late-stage erythropoiesis to increase the production of mature erythrocytes into the circulation.10-12
• This 2-part, phase IIA, randomized, placebo-controlled trial is the first to evaluate the pharmacokinetics (PK), safety, tolerability, and Hb effect of sotatercept in ESKD subjects with renal anemia receiving hemodialysis.
• In part 1, after a single subcutaneous dose (0.1 mg/kg) of sotatercept13:
– PK parameters were similar to a phase I study in healthy postmenopausal women, with a long half-life (21 days).
– Sotatercept was not dialyzable.
– There was no evidence of a pharmacodynamic effect on Hb concentrations at the single, 0.1 mg/kg dose.
– Sotatercept was well tolerated with no observed changes in blood pressure (BP), and no consistent changes in safety laboratory or electrocardiographic parameters.
• Part 2 is an ongoing, randomized, single-blind, placebo-controlled, sequential dose-escalation study in subjects with ESKD on hemodialysis evaluating the PK, safety, tolerability, and Hb effects of sotatercept for the correction of ESKD-related anemia.
• We report the preliminary, interim analysis of the sotatercept 0.3 mg/kg (low dose) and 0.5 mg/kg (medium dose) treatment groups.
• Pending acceptable interim analysis results, additional patients may be randomized in a staggered parallel fashion to sotatercept 0.7 mg/kg once every 28 days (high dose) and sotatercept 0.7 mg/kg once every 14 days for 28 days followed by 0.4 mg/kg every 14 days for the remainder of the treatment period (Figure 1).
METHODSKey Inclusion Criteria• Adults receiving at least 3 hours of high-flux hemodialysis at each session for at least 12 weeks before screening and no planned changes to the hemodialysis regimen
during the study period
• Adequate Hb response (Hb ≥10 to ≤12 g/dL predialysis mean of 3 consecutive Hb concentrations) to stable doses of ESA (epoetin alfa, darbepoetin) for at least 6 weeks before and during screening, excluding dose holds for high Hb (maximum dose: epoetin alfa ≤500 IU/kg/week; darbepoetin ≤95 μg/week)
• ESKD-related anemia: Hb ≥8 to ≤10 g/dL predialysis after ESA washout
• Adequate iron status (transferrin saturation ≥20%)
• Kt/V ≥1.2 or urea reduction ratio ≥65%
• Parathyroid hormone concentration ≤1,000 pg/mL; phosphorous ≤7 mg/dL; and total albumin-corrected calcium ≥8.0 to ≤10.5 mg/dL
Key Exclusion Criteria• Anemia due to non-renal causes
• ESKD due to malignancy or history of malignancy (excluding excised and cured non-melanoma skin cancer and cervical carcinoma in situ)
• Systemic hematologic disease
• Peritoneal dialysis or compromised venous access
• Uncontrolled diabetes mellitus (HbA1C >9%), hypertension (home systolic BP [SBP] >160 mm Hg, home diastolic BP [DBP] >90 mm Hg), or heart failure (New York Heart Association class ≥3)
• Alanine transaminase and/or aspartate transaminase values >2× the upper limit of normal; C-reactive protein >50 mg/L
• Red blood cell transfusion <8 weeks before screening
• Anticipated or scheduled living donor renal transplant
Study Design• This was a randomized, single-blind, placebo-controlled, sequential dose-escalation study in subjects with ESKD on hemodialysis (Figure 1).
• Eligible subjects were randomized to 2 arms (sotatercept or placebo in a 3:1 ratio) in 4 sequential dose groups (sotatercept 0.3 mg/kg, 0.5 mg/kg, 0.7 mg/kg, or 0.7 mg/kg loading dose followed by 0.4 mg/kg).
– This interim analysis informed the data monitoring committee’s decision to open enrollment for the high-dose group (sotatercept 0.7 mg/kg).
– At the time of abstract submission:
§ Enrollment in the sotatercept 0.3 mg/kg and 0.5 mg/kg dose groups was completed.
§ Enrollment in the sotatercept 0.7 mg/kg dose group was ongoing.
• Sotatercept doses could have been delayed, reduced, or discontinued based on the subject’s absolute predialysis Hb level or change in Hb level observed after dosing, or discontinued based on change in home BP measurements.
– Delayed: Hb ≥11 to <13 g/dL on Dose Cycle Day 36 (0.3, 0.5, and 0.7 mg/kg dose groups) or Dose Cycle Day 19 (0.7/0.4 mg/kg dose group)
– Reduced: If a dose was delayed, OR if Hb <11 g/dL AND rate of rise of >2 g/dL (0.3, 0.5, and 0.7 mg/kg dose groups) or >1 g/dL (0.7/0.4 mg/kg dose group)
– Discontinued:
§ Persistent hypertension recorded by home BP monitor mean of 4 days of home SBP >160 mm Hg AND increase in SBP from baseline of >20 mm Hg, or mean increase from baseline DBP of >10 mm Hg
§ Hb ≥13 g/dL at any time after randomization
§ Hb ≥12 to <13 g/dL for 2 consecutive weeks at any time after randomization
• Rescue treatment was recommended for subjects with Hb <9 g/dL after the first dose cycle, and those required to discontinue sotatercept could receive ESA treatment or red blood cell transfusion.
• All randomized subjects, including those who were rescued or discontinued early, continued to follow the visit schedule and home BP monitoring throughout the 200-day treatment phase and 112-day follow-up phase.
• The current report describes interim analysis of the sotatercept 0.3 mg/kg and 0.5 mg/kg dose groups for the purpose of determining safety of proceeding to the next dose group.
Figure 1. Study Design
Follow-up phase for 112 days for PK
and safety
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.3 mg/kgSC (n ~9) q28d,up to 8 doses
Placebo (n ~3)q28d, up to 8 doses
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.5 mg/kgSC (n ~9) q28d,up to 8 doses
Placebo (n ~3)q28d, up to 8 doses
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.7 mg/kgSC (n ~9) q28d,
up to 8 doses
Placebo (n ~3)q28d, up to 8 doses
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.7 mg/kg SC q14d(2 doses), then 0.4 mg/kg SC q14d
up to 13 doses (n ~9)
Placebo (n ~3)q14d, up to 15 doses
Note: All randomized subjects will continue treatment with sotatercept 0.3, 0.5, or 0.7 mg/kg or placebo for up to 8 doses* unless rescued or discontinued early. *At 0.7/0.4 mg/kg, all randomized subjects will continue treatment for up to 15 doses unless rescued or discontinued early.28 days after the 6th subject is dosed with sotatercept in each dose group (0.3, 0.5, and 0.7 mg/kg), an interim analysis will occur to evaluate PK and safety before opening the next dose group.
Table 3. Sotatercept PK in ESKD Subjects on Hemodialysis (Dose 1, Cycle 1)
Sotatercept
Parameter0.3 mg/kg
n=90.5 mg/kg
n=6
tmax, mean (min–max), day 12 (2–14) 7 (2–14)
Cmax, mean (SD), μg/mL 2.4 (0.96) 3.5 (0.73)
AUC28d, mean (SD), day•μg/mL 50.5 (17.4) 73.2 (11.5)
t1/2,z, mean (SD), day 22.3 (3.0)* 24.5 (8.9)*†
CL/F, mean (SD), mL/day/kg 3.65 (1.60)* 3.83 (1.19)*†
Vz/F, mean (SD), mL/kg 117 (54)* 124 (27.9)*†
AUC28d=area under the concentration-vs.-time curve up to 28 days; CL/F=oral clearance; Vz/F=apparent volume of distribution.*Estimated according to a 1-compartment model.†The 28-day data may not be sufficient for accurate estimation in some subjects.
Figure 2. Sotatercept Serum Concentration Over Time
Seru
m S
otat
erce
pt (µ
g/m
L)
5
4
3
2
1
0
Days After the First Dose
0 7 14 21 28
Sotatercept 0.3 mg/kg
Sotatercept 0.5 mg/kg
Safety• An overview of AEs is provided in Table 4.
• A decrease in serum calcium levels during follow-up in subjects who had received sotatercept 0.3 mg/kg was noted, without AEs of hypocalcemia.
• There were no other observed trends in laboratory, electrocardiogram, or vital sign parameters, including study visit and intra-dialytic BP, in either dose group of sotatercept during long-term follow-up.
• No anti-drug antibodies, injection site reactions, or hypersensitivity reactions were observed.
Table 4. Overview of AEs (Safety Population, N=20)
Placebo Sotatercept
n=50.3 mg/kg
n=90.5 mg/kg
n=6
Subjects, n (%)
Cumulative days on study 864 2046 634
Any AE 3 (60.0) 8 (88.8) 3 (50.0)
≥1 severe AE 2 (40.0) 2 (22.2) 2 (33.3)
≥1 serious AE 2 (40.0) 2 (22.2) 1 (16.7)
Death 1 (20.0) 0 (0.0) 0 (0.0)
AEs in ≥2 subjects in a treatment group, n (%)
Fatigue 1 (20.0) 2 (22.2) 0 (0.0)
Pain 0 (0.0) 2 (22.2) 0 (0.0)
Constipation 1 (20.0) 2 (22.2) 0 (0.0)
Hypertension 0 (0.0) 3 (33.3)* 0 (0.0)
*A total of 3 subjects randomized to sotatercept 0.3 mg/kg reported 4 AEs of hypertension; 3 of the 4 events occurred after rescue with erythropoietin.
EfficacyTarget Hb Increase (≥1 g/dL), and Target Hb Range (10–12 g/dL) During the First 28 Days
• Baseline Hb levels were 9.7 g/dL in subjects receiving placebo, 9.3 g/dL in subjects receiving sotatercept 0.3 mg/kg, and 8.9 g/dL in subjects receiving sotatercept 0.5 mg/kg.
• Hb increase ≥1.0 g/dL was achieved by 20% (placebo), 37.5% (sotatercept 0.3 mg/kg), and 40% (sotatercept 0.5 mg/kg) of subjects (Figure 3).
• The desired Hb range (10–12 g/dL) was achieved in 60% (placebo), 25% (sotatercept 0.3 mg/kg), and 60% (sotatercept 0.5 mg/kg) during the first dose cycle.
• Mean peak Hb increase in the first 28-day dose cycle was 0.1 g/dL in subjects receiving placebo, 0.5 g/dL in subjects receiving sotatercept 0.3 mg/kg, and 0.8 g/dL in subjects receiving sotatercept 0.5 mg/kg (Figure 4).
• Rescue therapy was required (Hb <9 g/dL) in 2 of 5 subjects after administration of placebo and 1 of 8 subjects after administration of sotatercept 0.3 mg/kg, while none required rescue after sotatercept 0.5 mg/kg (Figure 3).
Figure 3. Hb Increase During the First 28-Day Dose Cycle (Per-Protocol Population)*
0
30
20
10
40
60
50
70
80
90
100
Subj
ects
(%)
Placebo(n=5)
40
40
20
Sotatercept 0.3 mg/kg(n=8)
13
50
37
Sotatercept 0.5 mg/kg
(n=5)
60
40
0.1-0.9 g/dL
Required Rescue (Hb <9 g/dL)
≥1.0 g/dL
*Two subjects with a major protocol violation were excluded from efficacy analyses.
PK Assessment• Blood samples for analysis of sotatercept PK were collected at each study visit and on each sotatercept or placebo dosing day. Additional samples were obtained after
dose 1 at 4 hours post-dose on Day 1 and at 48 hours post-dose on Day 3.
• A validated, competitive enzyme-linked immunosorbent assay using anti‐human ActRIIA antibodies (R&D Systems, Minneapolis, MN) was used to measure the sotatercept serum concentration.
Hb Assessments• Blood samples for Hb assessment were obtained at all scheduled study visits, including before dosing.
Home BP Monitoring• Because of the burden of hypertension in the hemodialysis population, and the inherent variability in hemodialysis-related BP measurement, home BP monitoring was
used to provide a BP profile more reflective of the subject’s steady state.
• Subjects obtained their BP at home 2×/day (3 measurements each upon waking and at bedtime) for 4 consecutive days within 7 days of a scheduled dosing day. Each subject was trained to use a sponsor-provided BP monitor.
• At least 3 waking and 3 bedtime values downloaded from the device by study personnel were used to calculate mean BP values before screening, randomization, and re-dosing.
• Home BP monitoring continued for subjects requiring rescue.
Safety Assessments• Safety assessments included collection of adverse events (AEs), hematology testing, and vital signs at each visit and physical examination and 12-lead
electrocardiogram at selected scheduled time points.
– Safety assessments were done in the event of early termination/withdrawal.
• Proportions of subjects with Hb >12 g/dL at any time and rise in Hb >2 g/dL over 4 weeks were also determined.
• At each interim analysis, blood samples were analyzed for the presence of anti-sotatercept antibodies.
Statistical Analysis• Sotatercept multidose PK was examined among all subjects who received at least 1 dose of study medication and who had evaluable PK data.
• Sotatercept efficacy was evaluated in the full analysis set (FAS), which comprised all randomized subjects who received at least 1 dose of study medication and had at least 1 post-dose follow-up visit, and a baseline value (for analyses that require baseline comparison). Subjects assigned to placebo in both dose groups were combined to form a single placebo group for analysis purposes.
• Efficacy end points included:
– Proportion of subjects achieving target Hb increase (≥1 g/dL increase from baseline).
– Proportion of subjects achieving target Hb concentration >10 g/dL to <12 g/dL.
– Proportion of subjects requiring rescue therapy.
– Change from baseline Hb during the first 28-day dosing cycle, including peak Hb response.
• Proportional and continuous end points were summarized descriptively.
• The final mean home BP value was calculated by first determining the mean of 3 waking and 3 bedtime sets of BP measures. Next, the mean waking and mean bedtime values from a single day were both used to calculate the day mean. Finally, the mean of the day means was calculated, and this comprised the final mean home BP.
• Home BP measures and safety measures were summarized descriptively.
RESULTSSubjects• A total of 21 subjects were randomized and received study medication. One subject was randomized to sotatercept 0.5 mg/kg and received 1 dose of study medication;
however, this subject did not have the first follow-up visit at the time of the interim database cutoff point and was not included in either the safety or efficacy population. A total of 20 subjects comprise the FAS and safety population:
– 5 who received placebo.
– 9 who received sotatercept 0.3 mg/kg.
– 6 who received sotatercept 0.5 mg/kg.
• Interim subject disposition is illustrated in Table 1.
• Baseline subject demographics and disease characteristics were generally similar across treatment groups (Table 2).
• Major protocol violations were noted for 2 subjects randomized to sotatercept. One subject (0.3 mg/kg) received erythropoietin prior to randomization and through the first dose cycle, and was discontinued from the study; 1 subject (0.5 mg/kg) had an incomplete baseline home BP evaluation, which showed a non-qualifying elevation in BP prior to randomization, and was discontinued from study medication early. These subjects were excluded from efficacy analyses, as a per-protocol analysis defined in the protocol. Included in the efficacy analysis population were:
– 5 who received placebo.
– 8 who received sotatercept 0.3 mg/kg.
– 5 who received sotatercept 0.5 mg/kg.
Table 1. Subject Disposition (FAS, N=20)
GroupOngoing on Study Drug
D/C Study Drug (Being Followed)
Completers on Study Drug (≥200 Days)
Completers After D/C Study Drug Early Termination Total Rescued
D/C Study Drug Due to Stopping Rule
Placebo, n=5 0 2 1 1 1 3 0
Sotatercept 0.3 mg/kg, n=9 0 0 2 5 2 7 0
Sotatercept 0.5 mg/kg, n=6 3 2 0 0 1 2 1
D/C=discontinued.
Table 2. Demographic Characteristics of Subjects (FAS, N=20)
Placebo Sotatercept
n=50.3 mg/kg
n=90.5 mg/kg
n=6
Age, mean, years 58.4 59.9 60.7
Female, n (%) 1 (20.0) 6 (66.7) 1 (16.7)
Race, n (%)
White 1 (20.0) 3 (33.3) 4 (66.7)
Black 3 (60.0) 6 (66.7) 2 (33.3)
Asian 1 (20.0) 0 (0.0) 0 (0.0)
Ethnicity
Hispanic 0 (0.0) 2 (22.2) 4 (66.7)
Non-Hispanic 5 (100.0) 7 (77.8) 2 (33.3)
Weight, postdialysis mean, kg 75.8 79.4 81.0
Body mass index, mean, kg/m2 25.4 27.8 27.3
Sotatercept PK• Preliminary, interim PK data, based on analysis of all subjects randomized to sotatercept 0.3 mg/kg and the first 6 subjects randomized to sotatercept 0.5 mg/kg, are
presented in Table 3.
• Sotatercept exhibited dose-dependent increases in the serum drug exposure (Cmax and AUC), with a mean elimination half-life (t1/2,z) of 22 to 25 days.
• Sotatercept mean concentration-vs.-time profiles for the 0.3 mg/kg and 0.5 mg/kg dose groups are shown in Figure 2.
Figure 4. Mean Peak Hemoglobin Increase During the First 28-Day Dose Cycle (Per-Protocol Population)*
Sotatercept 0.3 mg/kg (n=8)
Sotatercept 0.5 mg/kg (n=5)
Placebo (n=5)
0.1
0.5
0.8
0
0.3
0.2
0.1
0.4
0.5
0.6
0.7
0.8
0.9
Hb (g
/dL)
Cha
nge
From
Bas
elin
eMean Peak Hemoglobin Response
*Two subjects with a major protocol violation were excluded from efficacy analyses.
Change From Baseline in Hb Concentration• Mean Hb concentration in subjects who received sotatercept 0.3 mg/kg and 0.5 mg/kg exhibited a greater increase from baseline in the first 15 days post-dose
(vs. placebo); however, the increases were not sustained through the entire dose cycle.
• Hb levels throughout multiple dose cycles among subjects who did not require rescue were generally highest among subjects receiving sotatercept 0.5 mg/kg (Figure 5).
Figure 5. Hb Change From Baseline During Long-term Sotatercept Treatment Censored for Rescue
−3
−2
−1
0
1
2
3
4
50 100 150 200 250
Days After the First Dose
Hem
oglo
bin
(g/d
L)
Sotatercept 0.3 mg/kg (n=8)Sotatercept 0.5 mg/kg (n=5)
Placebo (n=5)
Home BP Measurements• Home BP measures in the first dose cycle revealed that all 3 groups had increases in group mean SBP, with the largest change in subjects receiving sotatercept
0.3 mg/kg, while the largest change in DBP was in subjects receiving placebo. All the group mean changes were <10 mm Hg (Figure 6A and B).
– Findings were similar when analyzed for both the per-protocol population (Figure 6A) and FAS (Figure 6B).
• With long-term treatment, home BP measures showed no consistent change from baseline among subjects in any of the treatment groups (Figure 7).
Figure 6. Change From Baseline in Home BP at the End of Dose Cycle 1 in the (A) Per-Protocol Population* and (B) FAS
Sotatercept 0.3 mg/kg (n=7)
Sotatercept 0.5 mg/kg (n=4)
Placebo (n=3)
Sotatercept 0.3 mg/kg (n=9)
Sotatercept 0.5 mg/kg (n=5)
Placebo (n=4)
Chan
ge F
rom
Bas
elin
e BP
(mm
Hg)
0.0
2.0
6.0
3.3 3.3
–0.3 –1.0
0.0
1.0
2.0
3.0
4.0
5.0
6.0
7.0
SBP DBP
A
B
Chan
ge F
rom
Bas
elin
e BP
(mm
Hg)
2.3
7.5
3.0 2.5
7.6
0.4
0.0
1.0
2.0
3.0
4.0
5.0
6.0
7.0
8.0
SBP DBP
*Data exclude subjects with protocol violations and are censored for those who required rescue in the first dose cycle.
Figure 7. Change From Baseline Home BP Measurements (FAS) of (A) SBP and (B) DBP During Long-term Sotatercept Treatment, Censored for Rescue
A SBP
B DBP
–20
–15
–10
–5
0
5
10
15
20
25
50 100 150 200 250
Sotatercept 0.3 mg/kg (n=9)Sotatercept 0.5 mg/kg (n=5)
Placebo (n=4)
Hom
e DB
P (m
m H
g)
–50
–40
–30
–20
–10
0
10
20
30
40
50 100 150 200 250
Sotatercept 0.3 mg/kg (n=9)Sotatercept 0.5 mg/kg (n=5)
Placebo (n=4)
Hom
e SB
P (m
m H
g)
CONCLUSIONS• Sotatercept exhibited linear PK characteristics, and a long half-life of 22 to 25 days.
• Sotatercept was well tolerated, with AEs similar to those observed with placebo and no trends toward increased BP.
• Exposure to sotatercept was not associated with the development of anti-drug antibodies, injection site reactions, or hypersensitivity reactions.
• In the first 28 days of treatment, the proportion of subjects achieving the target Hb increase of ≥1 g/dL was greater in the treatment groups than in the placebo group, and the proportion requiring rescue therapy in the first 28 days was dose-related, with no subjects in the sotatercept 0.5 mg/kg group requiring rescue.
• In this initial 28-day analysis, in which the placebo and sotatercept 0.3 mg/kg groups had higher baseline Hb, no differences between groups achieving the target Hb range (10-12 g/dL) were observed. Dose escalation continues per protocol.
• Mean peak Hb response in the first 28 days was dose-related, with the sotatercept 0.5 mg/kg dose having the highest mean peak Hb response.
• Hb improvements were generally sustained for multiple dosing cycles in the sotatercept 0.5 mg/kg dose group.
• This preliminary interim analysis indicates adequate Hb responses and safety of sotatercept at 0.3 and 0.5 mg/kg and provides evidence to continue the evaluation of sotatercept at 0.7 mg/kg in patients with ESKD on hemodialysis.
REFERENCES1. Babitt JL, Lin HY. Mechanisms of anemia in CKD. J Am Soc Nephrol. 2012;23:1631-1634.
2. Jacobson LO, Goldwasser E, Fried W, et al. Role of the kidney in erythropoiesis. Nature. 1957;179:633-634.
3. McGonigle RJ, Wallin JD, Shadduck RK, et al. Erythropoietin deficiency and inhibition of erythropoiesis in renal insufficiency. Kidney Int. 1984;25:437-444.
4. Eschbach JW, Egrie JC, Downing MR, et al. Correction of the anemia of end-stage renal disease with recombinant human erythropoietin. Results of a combined phase I and II clinical trial. N Engl J Med. 1987;316:73-78.
5. Singh AK, Szczech L, Tang KL, et al. Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med. 2006;355: 2085-2098.
6. Fishbane S. Anemia and cardiovascular risk in the patient with kidney disease. Heart Fail Clin. 2008;4:401-410.
7. Besarab A, Bolton WK, Browne JK, et al. The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. N Engl J Med. 1998;339:584-590.
8. Drueke TB, Locatelli F, Clyne N, et al. Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med. 2006;355:2071-2084.
9. Pfeffer MA, Burdmann EA, Chen CY, et al. A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. N Engl J Med. 2009;361:2019-2032.
10. Pearsall RS, Canalis E, Cornwall-Brady M, et al. A soluble activin type IIA receptor induces bone formation and improves skeletal integrity. Proc Natl Acad Sci U S A. 2008;105:7082-7087.
11. Iancu-Rubin C, Mosoyan G, Wang J, et al. Stromal cell-mediated inhibition of erythropoiesis can be attenuated by sotatercept (ACE-011), an activin receptor type II ligand trap. Exp Hematol. 2013;41:155-166.
12. Sherman ML, Borgstein NG, Mook L, et al. Multiple-dose, safety, pharmacokinetic, and pharmacodynamic study of sotatercept (ActRIIA-IgG1), a novel erythropoietic agent, in healthy postmenopausal women. J Clin Pharmacol. 2013;53:1121-1130.
13. Wooldridge T, Kaplan M, Alcorn H Jr, et al. The pharmacokinetics and safety of a single-dose of sotatercept (ACE-011) in subjects on hemodialysis and the effects of its murine analog (RAP-011) on anemia and in preventing bone loss in C57BL/6 mice with 5/6 nephrectomy [oral presentation]. Presented at: American Society of Nephrology Kidney Week 2012; October 30-November 4, 2012; San Diego, CA.
This study was sponsored by Celgene Corporation.
Presented at: the National Kidney Foundation (NKF) 2014 Spring Clinical Meeting; April 22–26, 2014; Las Vegas, NV.Scan this QR code to receive
the PDF of the poster

Interim Analysis of ACE-011-REN-001: The First 28-Day Dose Cycle of Low and Medium Starting Doses of Sotatercept Compared to Placebo for Correction of Anemia in Hemodialysis Subjects
Mohamed El-Shahawy1; James Cotton2; Jeffrey Kaupke3; Thomas D. Wooldridge4; Hem N. Singh5; William T. Smith51Academic Medical Research Institute, Los Angeles, CA, USA; 2Tyler Nephrology Associates PC, Tyler, TX, USA; 3Nephrology Specialist Medical Group, Orange, CA, USA; 4Nephrology & Hypertension Associates LTD, Tupelo, MS, USA; 5Celgene Corporation, Warren, NJ, USA
INTRODUCTION• The anemia seen in patients with end-stage kidney disease (ESKD) is largely due to decreased biosynthesis of erythropoietin from the kidneys.1-3
• A number of erythropoiesis-stimulating agents (ESAs) have demonstrated efficacy in increasing hemoglobin (Hb) levels in patients with ESKD,4,5 but pose significant safety risks, including persistent hypertension, serious cardiovascular events, and increased risk of death.4,5
• Multiple observational studies have linked low Hb levels to poor cardiovascular outcomes.6 However, recent clinical studies have demonstrated that ESAs are unable to modify this risk when targeting a normal Hb level.5,7-9
• Sotatercept (ACE-011) is an ActRIIA-IgG1 fusion protein trap that binds with high affinity to activin A and other members of the TGFb superfamily and acts on late-stage erythropoiesis to increase the production of mature erythrocytes into the circulation.10-12
• This 2-part, phase IIA, randomized, placebo-controlled trial is the first to evaluate the pharmacokinetics (PK), safety, tolerability, and Hb effect of sotatercept in ESKD subjects with renal anemia receiving hemodialysis.
• In part 1, after a single subcutaneous dose (0.1 mg/kg) of sotatercept13:
– PK parameters were similar to a phase I study in healthy postmenopausal women, with a long half-life (21 days).
– Sotatercept was not dialyzable.
– There was no evidence of a pharmacodynamic effect on Hb concentrations at the single, 0.1 mg/kg dose.
– Sotatercept was well tolerated with no observed changes in blood pressure (BP), and no consistent changes in safety laboratory or electrocardiographic parameters.
• Part 2 is an ongoing, randomized, single-blind, placebo-controlled, sequential dose-escalation study in subjects with ESKD on hemodialysis evaluating the PK, safety, tolerability, and Hb effects of sotatercept for the correction of ESKD-related anemia.
• We report the preliminary, interim analysis of the sotatercept 0.3 mg/kg (low dose) and 0.5 mg/kg (medium dose) treatment groups.
• Pending acceptable interim analysis results, additional patients may be randomized in a staggered parallel fashion to sotatercept 0.7 mg/kg once every 28 days (high dose) and sotatercept 0.7 mg/kg once every 14 days for 28 days followed by 0.4 mg/kg every 14 days for the remainder of the treatment period (Figure 1).
METHODSKey Inclusion Criteria• Adults receiving at least 3 hours of high-flux hemodialysis at each session for at least 12 weeks before screening and no planned changes to the hemodialysis regimen
during the study period
• Adequate Hb response (Hb ≥10 to ≤12 g/dL predialysis mean of 3 consecutive Hb concentrations) to stable doses of ESA (epoetin alfa, darbepoetin) for at least 6 weeks before and during screening, excluding dose holds for high Hb (maximum dose: epoetin alfa ≤500 IU/kg/week; darbepoetin ≤95 μg/week)
• ESKD-related anemia: Hb ≥8 to ≤10 g/dL predialysis after ESA washout
• Adequate iron status (transferrin saturation ≥20%)
• Kt/V ≥1.2 or urea reduction ratio ≥65%
• Parathyroid hormone concentration ≤1,000 pg/mL; phosphorous ≤7 mg/dL; and total albumin-corrected calcium ≥8.0 to ≤10.5 mg/dL
Key Exclusion Criteria• Anemia due to non-renal causes
• ESKD due to malignancy or history of malignancy (excluding excised and cured non-melanoma skin cancer and cervical carcinoma in situ)
• Systemic hematologic disease
• Peritoneal dialysis or compromised venous access
• Uncontrolled diabetes mellitus (HbA1C >9%), hypertension (home systolic BP [SBP] >160 mm Hg, home diastolic BP [DBP] >90 mm Hg), or heart failure (New York Heart Association class ≥3)
• Alanine transaminase and/or aspartate transaminase values >2× the upper limit of normal; C-reactive protein >50 mg/L
• Red blood cell transfusion <8 weeks before screening
• Anticipated or scheduled living donor renal transplant
Study Design• This was a randomized, single-blind, placebo-controlled, sequential dose-escalation study in subjects with ESKD on hemodialysis (Figure 1).
• Eligible subjects were randomized to 2 arms (sotatercept or placebo in a 3:1 ratio) in 4 sequential dose groups (sotatercept 0.3 mg/kg, 0.5 mg/kg, 0.7 mg/kg, or 0.7 mg/kg loading dose followed by 0.4 mg/kg).
– This interim analysis informed the data monitoring committee’s decision to open enrollment for the high-dose group (sotatercept 0.7 mg/kg).
– At the time of abstract submission:
§ Enrollment in the sotatercept 0.3 mg/kg and 0.5 mg/kg dose groups was completed.
§ Enrollment in the sotatercept 0.7 mg/kg dose group was ongoing.
• Sotatercept doses could have been delayed, reduced, or discontinued based on the subject’s absolute predialysis Hb level or change in Hb level observed after dosing, or discontinued based on change in home BP measurements.
– Delayed: Hb ≥11 to <13 g/dL on Dose Cycle Day 36 (0.3, 0.5, and 0.7 mg/kg dose groups) or Dose Cycle Day 19 (0.7/0.4 mg/kg dose group)
– Reduced: If a dose was delayed, OR if Hb <11 g/dL AND rate of rise of >2 g/dL (0.3, 0.5, and 0.7 mg/kg dose groups) or >1 g/dL (0.7/0.4 mg/kg dose group)
– Discontinued:
§ Persistent hypertension recorded by home BP monitor mean of 4 days of home SBP >160 mm Hg AND increase in SBP from baseline of >20 mm Hg, or mean increase from baseline DBP of >10 mm Hg
§ Hb ≥13 g/dL at any time after randomization
§ Hb ≥12 to <13 g/dL for 2 consecutive weeks at any time after randomization
• Rescue treatment was recommended for subjects with Hb <9 g/dL after the first dose cycle, and those required to discontinue sotatercept could receive ESA treatment or red blood cell transfusion.
• All randomized subjects, including those who were rescued or discontinued early, continued to follow the visit schedule and home BP monitoring throughout the 200-day treatment phase and 112-day follow-up phase.
• The current report describes interim analysis of the sotatercept 0.3 mg/kg and 0.5 mg/kg dose groups for the purpose of determining safety of proceeding to the next dose group.
Figure 1. Study Design
Follow-up phase for 112 days for PK
and safety
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.3 mg/kgSC (n ~9) q28d,up to 8 doses
Placebo (n ~3)q28d, up to 8 doses
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.5 mg/kgSC (n ~9) q28d,up to 8 doses
Placebo (n ~3)q28d, up to 8 doses
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.7 mg/kgSC (n ~9) q28d,
up to 8 doses
Placebo (n ~3)q28d, up to 8 doses
Screening andESA washout
(Day –90 to Day –1)
Sotatercept 0.7 mg/kg SC q14d(2 doses), then 0.4 mg/kg SC q14d
up to 13 doses (n ~9)
Placebo (n ~3)q14d, up to 15 doses
Note: All randomized subjects will continue treatment with sotatercept 0.3, 0.5, or 0.7 mg/kg or placebo for up to 8 doses* unless rescued or discontinued early. *At 0.7/0.4 mg/kg, all randomized subjects will continue treatment for up to 15 doses unless rescued or discontinued early.28 days after the 6th subject is dosed with sotatercept in each dose group (0.3, 0.5, and 0.7 mg/kg), an interim analysis will occur to evaluate PK and safety before opening the next dose group.
Table 3. Sotatercept PK in ESKD Subjects on Hemodialysis (Dose 1, Cycle 1)
Sotatercept
Parameter0.3 mg/kg
n=90.5 mg/kg
n=6
tmax, mean (min–max), day 12 (2–14) 7 (2–14)
Cmax, mean (SD), μg/mL 2.4 (0.96) 3.5 (0.73)
AUC28d, mean (SD), day•μg/mL 50.5 (17.4) 73.2 (11.5)
t1/2,z, mean (SD), day 22.3 (3.0)* 24.5 (8.9)*†
CL/F, mean (SD), mL/day/kg 3.65 (1.60)* 3.83 (1.19)*†
Vz/F, mean (SD), mL/kg 117 (54)* 124 (27.9)*†
AUC28d=area under the concentration-vs.-time curve up to 28 days; CL/F=oral clearance; Vz/F=apparent volume of distribution.*Estimated according to a 1-compartment model.†The 28-day data may not be sufficient for accurate estimation in some subjects.
Figure 2. Sotatercept Serum Concentration Over Time
Seru
m S
otat
erce
pt (µ
g/m
L)
5
4
3
2
1
0
Days After the First Dose
0 7 14 21 28
Sotatercept 0.3 mg/kg
Sotatercept 0.5 mg/kg
Safety• An overview of AEs is provided in Table 4.
• A decrease in serum calcium levels during follow-up in subjects who had received sotatercept 0.3 mg/kg was noted, without AEs of hypocalcemia.
• There were no other observed trends in laboratory, electrocardiogram, or vital sign parameters, including study visit and intra-dialytic BP, in either dose group of sotatercept during long-term follow-up.
• No anti-drug antibodies, injection site reactions, or hypersensitivity reactions were observed.
Table 4. Overview of AEs (Safety Population, N=20)
Placebo Sotatercept
n=50.3 mg/kg
n=90.5 mg/kg
n=6
Subjects, n (%)
Cumulative days on study 864 2046 634
Any AE 3 (60.0) 8 (88.8) 3 (50.0)
≥1 severe AE 2 (40.0) 2 (22.2) 2 (33.3)
≥1 serious AE 2 (40.0) 2 (22.2) 1 (16.7)
Death 1 (20.0) 0 (0.0) 0 (0.0)
AEs in ≥2 subjects in a treatment group, n (%)
Fatigue 1 (20.0) 2 (22.2) 0 (0.0)
Pain 0 (0.0) 2 (22.2) 0 (0.0)
Constipation 1 (20.0) 2 (22.2) 0 (0.0)
Hypertension 0 (0.0) 3 (33.3)* 0 (0.0)
*A total of 3 subjects randomized to sotatercept 0.3 mg/kg reported 4 AEs of hypertension; 3 of the 4 events occurred after rescue with erythropoietin.
EfficacyTarget Hb Increase (≥1 g/dL), and Target Hb Range (10–12 g/dL) During the First 28 Days
• Baseline Hb levels were 9.7 g/dL in subjects receiving placebo, 9.3 g/dL in subjects receiving sotatercept 0.3 mg/kg, and 8.9 g/dL in subjects receiving sotatercept 0.5 mg/kg.
• Hb increase ≥1.0 g/dL was achieved by 20% (placebo), 37.5% (sotatercept 0.3 mg/kg), and 40% (sotatercept 0.5 mg/kg) of subjects (Figure 3).
• The desired Hb range (10–12 g/dL) was achieved in 60% (placebo), 25% (sotatercept 0.3 mg/kg), and 60% (sotatercept 0.5 mg/kg) during the first dose cycle.
• Mean peak Hb increase in the first 28-day dose cycle was 0.1 g/dL in subjects receiving placebo, 0.5 g/dL in subjects receiving sotatercept 0.3 mg/kg, and 0.8 g/dL in subjects receiving sotatercept 0.5 mg/kg (Figure 4).
• Rescue therapy was required (Hb <9 g/dL) in 2 of 5 subjects after administration of placebo and 1 of 8 subjects after administration of sotatercept 0.3 mg/kg, while none required rescue after sotatercept 0.5 mg/kg (Figure 3).
Figure 3. Hb Increase During the First 28-Day Dose Cycle (Per-Protocol Population)*
0
30
20
10
40
60
50
70
80
90
100
Subj
ects
(%)
Placebo(n=5)
40
40
20
Sotatercept 0.3 mg/kg(n=8)
13
50
37
Sotatercept 0.5 mg/kg
(n=5)
60
40
0.1-0.9 g/dL
Required Rescue (Hb <9 g/dL)
≥1.0 g/dL
*Two subjects with a major protocol violation were excluded from efficacy analyses.
PK Assessment• Blood samples for analysis of sotatercept PK were collected at each study visit and on each sotatercept or placebo dosing day. Additional samples were obtained after
dose 1 at 4 hours post-dose on Day 1 and at 48 hours post-dose on Day 3.
• A validated, competitive enzyme-linked immunosorbent assay using anti‐human ActRIIA antibodies (R&D Systems, Minneapolis, MN) was used to measure the sotatercept serum concentration.
Hb Assessments• Blood samples for Hb assessment were obtained at all scheduled study visits, including before dosing.
Home BP Monitoring• Because of the burden of hypertension in the hemodialysis population, and the inherent variability in hemodialysis-related BP measurement, home BP monitoring was
used to provide a BP profile more reflective of the subject’s steady state.
• Subjects obtained their BP at home 2×/day (3 measurements each upon waking and at bedtime) for 4 consecutive days within 7 days of a scheduled dosing day. Each subject was trained to use a sponsor-provided BP monitor.
• At least 3 waking and 3 bedtime values downloaded from the device by study personnel were used to calculate mean BP values before screening, randomization, and re-dosing.
• Home BP monitoring continued for subjects requiring rescue.
Safety Assessments• Safety assessments included collection of adverse events (AEs), hematology testing, and vital signs at each visit and physical examination and 12-lead
electrocardiogram at selected scheduled time points.
– Safety assessments were done in the event of early termination/withdrawal.
• Proportions of subjects with Hb >12 g/dL at any time and rise in Hb >2 g/dL over 4 weeks were also determined.
• At each interim analysis, blood samples were analyzed for the presence of anti-sotatercept antibodies.
Statistical Analysis• Sotatercept multidose PK was examined among all subjects who received at least 1 dose of study medication and who had evaluable PK data.
• Sotatercept efficacy was evaluated in the full analysis set (FAS), which comprised all randomized subjects who received at least 1 dose of study medication and had at least 1 post-dose follow-up visit, and a baseline value (for analyses that require baseline comparison). Subjects assigned to placebo in both dose groups were combined to form a single placebo group for analysis purposes.
• Efficacy end points included:
– Proportion of subjects achieving target Hb increase (≥1 g/dL increase from baseline).
– Proportion of subjects achieving target Hb concentration >10 g/dL to <12 g/dL.
– Proportion of subjects requiring rescue therapy.
– Change from baseline Hb during the first 28-day dosing cycle, including peak Hb response.
• Proportional and continuous end points were summarized descriptively.
• The final mean home BP value was calculated by first determining the mean of 3 waking and 3 bedtime sets of BP measures. Next, the mean waking and mean bedtime values from a single day were both used to calculate the day mean. Finally, the mean of the day means was calculated, and this comprised the final mean home BP.
• Home BP measures and safety measures were summarized descriptively.
RESULTSSubjects• A total of 21 subjects were randomized and received study medication. One subject was randomized to sotatercept 0.5 mg/kg and received 1 dose of study medication;
however, this subject did not have the first follow-up visit at the time of the interim database cutoff point and was not included in either the safety or efficacy population. A total of 20 subjects comprise the FAS and safety population:
– 5 who received placebo.
– 9 who received sotatercept 0.3 mg/kg.
– 6 who received sotatercept 0.5 mg/kg.
• Interim subject disposition is illustrated in Table 1.
• Baseline subject demographics and disease characteristics were generally similar across treatment groups (Table 2).
• Major protocol violations were noted for 2 subjects randomized to sotatercept. One subject (0.3 mg/kg) received erythropoietin prior to randomization and through the first dose cycle, and was discontinued from the study; 1 subject (0.5 mg/kg) had an incomplete baseline home BP evaluation, which showed a non-qualifying elevation in BP prior to randomization, and was discontinued from study medication early. These subjects were excluded from efficacy analyses, as a per-protocol analysis defined in the protocol. Included in the efficacy analysis population were:
– 5 who received placebo.
– 8 who received sotatercept 0.3 mg/kg.
– 5 who received sotatercept 0.5 mg/kg.
Table 1. Subject Disposition (FAS, N=20)
GroupOngoing on Study Drug
D/C Study Drug (Being Followed)
Completers on Study Drug (≥200 Days)
Completers After D/C Study Drug Early Termination Total Rescued
D/C Study Drug Due to Stopping Rule
Placebo, n=5 0 2 1 1 1 3 0
Sotatercept 0.3 mg/kg, n=9 0 0 2 5 2 7 0
Sotatercept 0.5 mg/kg, n=6 3 2 0 0 1 2 1
D/C=discontinued.
Table 2. Demographic Characteristics of Subjects (FAS, N=20)
Placebo Sotatercept
n=50.3 mg/kg
n=90.5 mg/kg
n=6
Age, mean, years 58.4 59.9 60.7
Female, n (%) 1 (20.0) 6 (66.7) 1 (16.7)
Race, n (%)
White 1 (20.0) 3 (33.3) 4 (66.7)
Black 3 (60.0) 6 (66.7) 2 (33.3)
Asian 1 (20.0) 0 (0.0) 0 (0.0)
Ethnicity
Hispanic 0 (0.0) 2 (22.2) 4 (66.7)
Non-Hispanic 5 (100.0) 7 (77.8) 2 (33.3)
Weight, postdialysis mean, kg 75.8 79.4 81.0
Body mass index, mean, kg/m2 25.4 27.8 27.3
Sotatercept PK• Preliminary, interim PK data, based on analysis of all subjects randomized to sotatercept 0.3 mg/kg and the first 6 subjects randomized to sotatercept 0.5 mg/kg, are
presented in Table 3.
• Sotatercept exhibited dose-dependent increases in the serum drug exposure (Cmax and AUC), with a mean elimination half-life (t1/2,z) of 22 to 25 days.
• Sotatercept mean concentration-vs.-time profiles for the 0.3 mg/kg and 0.5 mg/kg dose groups are shown in Figure 2.
Figure 4. Mean Peak Hemoglobin Increase During the First 28-Day Dose Cycle (Per-Protocol Population)*
Sotatercept 0.3 mg/kg (n=8)
Sotatercept 0.5 mg/kg (n=5)
Placebo (n=5)
0.1
0.5
0.8
0
0.3
0.2
0.1
0.4
0.5
0.6
0.7
0.8
0.9
Hb (g
/dL)
Cha
nge
From
Bas
elin
e
Mean Peak Hemoglobin Response
*Two subjects with a major protocol violation were excluded from efficacy analyses.
Change From Baseline in Hb Concentration• Mean Hb concentration in subjects who received sotatercept 0.3 mg/kg and 0.5 mg/kg exhibited a greater increase from baseline in the first 15 days post-dose
(vs. placebo); however, the increases were not sustained through the entire dose cycle.
• Hb levels throughout multiple dose cycles among subjects who did not require rescue were generally highest among subjects receiving sotatercept 0.5 mg/kg (Figure 5).
Figure 5. Hb Change From Baseline During Long-term Sotatercept Treatment Censored for Rescue
−3
−2
−1
0
1
2
3
4
50 100 150 200 250
Days After the First Dose
Hem
oglo
bin
(g/d
L)
Sotatercept 0.3 mg/kg (n=8)Sotatercept 0.5 mg/kg (n=5)
Placebo (n=5)
Home BP Measurements• Home BP measures in the first dose cycle revealed that all 3 groups had increases in group mean SBP, with the largest change in subjects receiving sotatercept
0.3 mg/kg, while the largest change in DBP was in subjects receiving placebo. All the group mean changes were <10 mm Hg (Figure 6A and B).
– Findings were similar when analyzed for both the per-protocol population (Figure 6A) and FAS (Figure 6B).
• With long-term treatment, home BP measures showed no consistent change from baseline among subjects in any of the treatment groups (Figure 7).
Figure 6. Change From Baseline in Home BP at the End of Dose Cycle 1 in the (A) Per-Protocol Population* and (B) FAS
Sotatercept 0.3 mg/kg (n=7)
Sotatercept 0.5 mg/kg (n=4)
Placebo (n=3)
Sotatercept 0.3 mg/kg (n=9)
Sotatercept 0.5 mg/kg (n=5)
Placebo (n=4)
Chan
ge F
rom
Bas
elin
e BP
(mm
Hg)
0.0
2.0
6.0
3.3 3.3
–0.3 –1.0
0.0
1.0
2.0
3.0
4.0
5.0
6.0
7.0
SBP DBP
A
B
Chan
ge F
rom
Bas
elin
e BP
(mm
Hg)
2.3
7.5
3.0 2.5
7.6
0.4
0.0
1.0
2.0
3.0
4.0
5.0
6.0
7.0
8.0
SBP DBP
*Data exclude subjects with protocol violations and are censored for those who required rescue in the first dose cycle.
Figure 7. Change From Baseline Home BP Measurements (FAS) of (A) SBP and (B) DBP During Long-term Sotatercept Treatment, Censored for Rescue
A SBP
B DBP
–20
–15
–10
–5
0
5
10
15
20
25
50 100 150 200 250
Sotatercept 0.3 mg/kg (n=9)Sotatercept 0.5 mg/kg (n=5)
Placebo (n=4)
Hom
e DB
P (m
m H
g)
–50
–40
–30
–20
–10
0
10
20
30
40
50 100 150 200 250
Sotatercept 0.3 mg/kg (n=9)Sotatercept 0.5 mg/kg (n=5)
Placebo (n=4)
Hom
e SB
P (m
m H
g)
CONCLUSIONS• Sotatercept exhibited linear PK characteristics, and a long half-life of 22 to 25 days.
• Sotatercept was well tolerated, with AEs similar to those observed with placebo and no trends toward increased BP.
• Exposure to sotatercept was not associated with the development of anti-drug antibodies, injection site reactions, or hypersensitivity reactions.
• In the first 28 days of treatment, the proportion of subjects achieving the target Hb increase of ≥1 g/dL was greater in the treatment groups than in the placebo group, and the proportion requiring rescue therapy in the first 28 days was dose-related, with no subjects in the sotatercept 0.5 mg/kg group requiring rescue.
• In this initial 28-day analysis, in which the placebo and sotatercept 0.3 mg/kg groups had higher baseline Hb, no differences between groups achieving the target Hb range (10-12 g/dL) were observed. Dose escalation continues per protocol.
• Mean peak Hb response in the first 28 days was dose-related, with the sotatercept 0.5 mg/kg dose having the highest mean peak Hb response.
• Hb improvements were generally sustained for multiple dosing cycles in the sotatercept 0.5 mg/kg dose group.
• This preliminary interim analysis indicates adequate Hb responses and safety of sotatercept at 0.3 and 0.5 mg/kg and provides evidence to continue the evaluation of sotatercept at 0.7 mg/kg in patients with ESKD on hemodialysis.
REFERENCES1. Babitt JL, Lin HY. Mechanisms of anemia in CKD. J Am Soc Nephrol. 2012;23:1631-1634.
2. Jacobson LO, Goldwasser E, Fried W, et al. Role of the kidney in erythropoiesis. Nature. 1957;179:633-634.
3. McGonigle RJ, Wallin JD, Shadduck RK, et al. Erythropoietin deficiency and inhibition of erythropoiesis in renal insufficiency. Kidney Int. 1984;25:437-444.
4. Eschbach JW, Egrie JC, Downing MR, et al. Correction of the anemia of end-stage renal disease with recombinant human erythropoietin. Results of a combined phase I and II clinical trial. N Engl J Med. 1987;316:73-78.
5. Singh AK, Szczech L, Tang KL, et al. Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med. 2006;355: 2085-2098.
6. Fishbane S. Anemia and cardiovascular risk in the patient with kidney disease. Heart Fail Clin. 2008;4:401-410.
7. Besarab A, Bolton WK, Browne JK, et al. The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. N Engl J Med. 1998;339:584-590.
8. Drueke TB, Locatelli F, Clyne N, et al. Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med. 2006;355:2071-2084.
9. Pfeffer MA, Burdmann EA, Chen CY, et al. A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. N Engl J Med. 2009;361:2019-2032.
10. Pearsall RS, Canalis E, Cornwall-Brady M, et al. A soluble activin type IIA receptor induces bone formation and improves skeletal integrity. Proc Natl Acad Sci U S A. 2008;105:7082-7087.
11. Iancu-Rubin C, Mosoyan G, Wang J, et al. Stromal cell-mediated inhibition of erythropoiesis can be attenuated by sotatercept (ACE-011), an activin receptor type II ligand trap. Exp Hematol. 2013;41:155-166.
12. Sherman ML, Borgstein NG, Mook L, et al. Multiple-dose, safety, pharmacokinetic, and pharmacodynamic study of sotatercept (ActRIIA-IgG1), a novel erythropoietic agent, in healthy postmenopausal women. J Clin Pharmacol. 2013;53:1121-1130.
13. Wooldridge T, Kaplan M, Alcorn H Jr, et al. The pharmacokinetics and safety of a single-dose of sotatercept (ACE-011) in subjects on hemodialysis and the effects of its murine analog (RAP-011) on anemia and in preventing bone loss in C57BL/6 mice with 5/6 nephrectomy [oral presentation]. Presented at: American Society of Nephrology Kidney Week 2012; October 30-November 4, 2012; San Diego, CA.
This study was sponsored by Celgene Corporation.
Presented at: the National Kidney Foundation (NKF) 2014 Spring Clinical Meeting; April 22–26, 2014; Las Vegas, NV.Scan this QR code to receive
the PDF of the poster