Integrative Effects of Nitric Oxide and Endothelium-Derived Hyperpolarizing Factor Induced by...
-
Upload
yuji-harada -
Category
Documents
-
view
224 -
download
3
Transcript of Integrative Effects of Nitric Oxide and Endothelium-Derived Hyperpolarizing Factor Induced by...

rpystsp
aiaae
6
NITRIC OXIDE: Biology and ChemistryVol. 4, No. 4, pp. 354–362 (2000)doi:10.1006/niox.2000.0287, available online at http://www.idealibrary.com on
Integrative Effects of Nitric Oxide and Endothelium-DerivedHyperpolarizing Factor Induced by Acetylcholine andBradykinin in Rat Hindquarter Perfusion
Yuji Harada,*,1 Masaharu Ikeda,† Yoshinobu Murasato,* Hiroshi Suzuka,*Hiroki Nanri,† and Yoshiaki Hayashida*
*Department of Systems Physiology and †Department of Health Development, University of Occupational andEnvironmental Health, Yahatanishi, Kitakyushu 807-8555, Japan
0
Received September 28, 1999, and in revised form March 13, 200We investigated the roles of endothelium-derivedvasodilative factors in rat hindquarter perfusionusing a system for the direct measurement of nitricoxide (NO). Acetylcholine (ACh) induced the dose-dependent release of NO with a concomitant de-crease in perfusion pressure. Under the influence ofNG-monomethyl-L-arginine (L-NMMA), NO release inesponse to ACh was blocked, while the perfusionressure still decreased. In the presence of tetraeth-lammonium (TEA), the decrease in perfusion pres-ure in response to ACh was attenuated comparedo the control value. The decrease in perfusion pres-ure in response to ACh was almost abolished in theresence of both L-NMMA and TEA or with deendo-
thelialization. Bradykinin (BK) also induced NO re-lease and biphasic effects on the perfusion pres-sure. The perfusion pressure decreased with alower concentration of BK and increased with ahigher concentration. L-NMMA and TEA each abol-ished the decrease in perfusion pressure induced byBK. Furthermore, in the presence of both L-NMMA
nd TEA, the perfusion pressure actually increasedn response to BK. These results suggest that AChnd BK induce vasodilation through NO release and
potassium channel dependent mechanism viandothelium. © 2000 Academic Press
1 To whom correspondence should be addressed. Fax: 181-93-92-2684. E-mail: [email protected].
354
Key Words: acetylcholine; bradykinin; nitric ox-ide; endothelium-derived hyperpolarizing factor;direct measurement; vasodilation; perfusion.
It is generally known that acetylcholine (ACh)2 andbradykinin (BK) bind to their receptors on intact vas-cular endothelium and release vasodilative substances(1) such as nitric oxide (NO) (2, 3) and prostanoids(PGI2) (4). NO is believed to be endothelium-derivedrelaxing factor (EDRF) (2, 3). Recent reports have sug-gested that there is also an endothelium-derived hy-perpolarizing factor (EDHF), which induces the hyper-polarization and relaxation of vascular smooth musclecells in the isolated vessels (5–10). Hydrogen peroxide(11), products of lipoxygenase (12), and cytochromeP-450 (13, 14) have all been considered to be EDHF,which plays a greater role in vasodilation in smallarteries than in large arteries in experiments usingisometric force measurement (15–17). However, thecontributions of NO and EDHF to local circulation,including arterioles, are not yet clear.
Many studies have demonstrated NOS inhibitorresistant vasodilation in response to ACh (5–10). To
2 Abbreviations used: ACh, acetylcholine; BK, bradykinin; NO,nitric oxide; EDRF, endothelium-derived relaxing factor; EDHF,endothelium-derived hyperpolarizing factor; L-NMMA, NG-mono-
methyl-L-arginine; EDTA, ethylenediaminetetraacetic acid; TEA,tetraethylammonium.1089-8603/00 $35.00Copyright © 2000 by Academic Press
All rights of reproduction in any form reserved.

N
CTS
clarify the mechanisms of the vasomotor responsesto these vasoactive substances, it is necessary toanalyze NO release and physiological phenomena atthe same time. Recently, two types of direct mea-surement systems with a NO-sensitive electrodehave been developed (18, 20). These systems detectNO as a change in current induced by the electro-chemical oxidation of NO on the surface of the elec-trode. However, since the signal current for NO isquite small, it is easily affected by electrical noisearound the measurement system. Furthermore, theconcentration of endothelium-derived NO is ex-tremely low (18), and it rapidly binds to hemoglobinor oxygen in the tissue (19, 20). Therefore, it hasbeen difficult to measure NO and few reports haveshown directly the correlation between NO releaseand biological responses in perfusion systems.
In this study we developed a perfusion system forthe direct measurement of NO and analyzed (1) thecorrelation between NO release and the vascularresponse to ACh and BK in different segments ofarteries and (2) the effects of NOS inhibitor andpotassium channel blocker, which inhibits EDHF,on these vascular responses. We also discuss theinteraction of NO and EDHF in the local circulation.
METHODS
All of the protocols and surgical procedures usedin this study were performed in accordance with theguidelines specified for institutional animal careand use of the University of Occupational and En-vironmental Health, Japan.
Animal Preparation and Perfusion System
Animal preparation. Male Wistar rats (weighingbetween 300 and 350 g) were used in this experi-ment. Rats were anesthetized with pentobarbitalsodium (50 mg/kg, ip), heparinized (100 IU, iv), andthen subjected to a midline laparotomy. After re-moval of gastrointestinal tracts, bilateral renal ar-teries and veins were ligated. We prepared threetypes of perfusion systems: perfusion of the (1)aorta, (2) aorta-femoral artery, and (3) hindquarter.An 18-gauge catheter (0.95-mm i.d., 1.30-mm o.d.)
INTEGRATIVE EFFE
for inflow of the perfusion solution was inserted intothe abdominal aorta and that (0.48-mm i.d.,
Copyright © 2000 by Academic Press. All right
0.68-mm o.d.) for outflow was mounted at the caudalend of the aorta, the femoral artery or the inferiorvena cava in aorta, aorta-femoral, and hindquarterperfusion, respectively. All arterial branches fromthe trunk were ligated in aorta and aorta-femoralperfusions. The upper trunk was ligated at the cau-dal side of the ribs in hindquarter perfusion.
Perfusion solution. The perfusion solution was amodified Krebs–Henseleit solution (K–H solution)with the following composition (mM): 118 NaCl, 4.7KCl, 1.3 KH2PO4, 1.2 MgSO4, 2.5 CaCl2, 24
aHCO3, and 11 glucose. K–H solution was gassedwith 95% O and 5% CO and kept at 38°C (pH 7.4).K–H solution contained enalaprilat (1 mM) to inhibitbradykinin metabolism (22, 23), indomethacin (10mM) to inhibit the effects of prostanoids (22), andascorbic acid (100 mM) to inhibit the oxidation ofNO (24).
Perfusion system. K–H solution was perfused bya peristaltic pump (Masterflex Model No. 7553-20,Cole-Parmer Instrument Co., Vernon Hills, IL) atconstant flow in aorta (4.0 ml/min), aorta-femoral(4.0 ml/min), and hindquarter perfusion (8.0 ml/min). The perfusion pressure was measured contin-uously throughout the experiment as a real-timeindicator of vascular resistance. Phenylephrine (5 31028 to 5 3 1026 M) was added to the perfusionsolution to maintain vascular tone. In situationswhere the baseline perfusion pressure prior to ad-ministration of agonist was different, a dose of phen-ylephrine was increased or decreased in order tomake the baseline pressure similar (70–100mmHg). After the perfusion pressure reached asteady state within 20 min, vascular responses toACh or BK were investigated. These were adminis-tered by bolus injection in a volume of 50 ml into theinflow of the perfusion solution. At least 10 min wasallowed for the perfusion pressure to recover to theinitial level between applications of the reagents.
NO Measurement System
NO was measured with a NO direct-measurementsystem (Model No. 501, Inter Medical Co., Nagoya,Japan) (25). This system detects NO as a change in
355OF NO AND EDHF
current with a NO-selective electrode, composed ofPt–Ir alloy (0.2-mm diameter) coated with a three-
s of reproduction in any form reserved.

Ndaa
tls
ms
3 DA ET
layered membrane, i.e., KCl, nitrocellulose (NO-selective), and silicone. A calibration curve was pre-pared for each electrode using a NO standardsolution in the perfusion system, in which the out-flow catheter was connected to the inlet of the equip-ment with a NO-selective electrode. The equipmenthad droppers at the inlet and outlet to reduce theeffect of artificial electrical noise on the NO current.To produce a saturated NO solution (1.4 mM), pureNO gas (Iwatani Gas Co., Japan) was bubbled for 20min in deionized and deoxidized water, which hadbeen bubbled with argon (Iwatani Gas Co., Japan)for 20 min, in a sealed 5-ml vial. The electrodesdetected more than 0.06 nmol of NO, as estimatedfrom the noise range (less than 3 pA) and the NO/peak current ratio. Nitrite (up to 1021 M), nitrate (upto 1021 M), ACh (up to 1022 M), and BK (up to 1025
M) had no effect on the current.
Reagents
The following reagents were used: acetylcholine hy-drochloride (ACh), NG-monomethyl-L-arginine (L-NMMA), ethylenediaminetetraacetic acid (EDTA)–Ca2Na, ascorbic acid, tetraethylammonium (TEA)(Sigma Chemical Co., St. Louis, MO), bradykinin ace-tate (BK) (Peptide Institute, Inc., Osaka, Japan), indo-methacin (Wako Pure Chemical Industries, Ltd.,Osaka, Japan), enalaprilat (Merck & Co., Inc., Rah-way, NJ), and phenylephrine HCl (Kowa Co., Osaka,Japan). ACh (1027–1024 M), BK (5 3 1027 to 1025 M),L-NMMA, and TEA were prepared in K–H solution tokeep the pH of the perfusion solution constant (25).
Experimental Protocol
Three perfusion systems. Dose-dependent changesin perfusion pressure and NO release in response toACh (1027 to 1024 M) or BK (5 3 1027 to 1025 M) wereinvestigated in aorta, aorta-femoral, and hindquarterperfusion under the control K–H solution. Thereafter,the responses to ACh or BK were investigated underthe continuous infusion of L-NMMA (NOS inhibitor:final concentration 1.0 mM). L-NMMA was infusedinto the perfusion solution for at least 20 min beforethe administration of the reagents.
56 HARA
The responses to ACh or BK were investigated inthe hindquarter perfusion system under the pres- 2
Copyright © 2000 by Academic Press. All right
ence of L-NMMA and/or TEA (potassium channelblocker: final concentration 20 mM). To inactivatethe endothelium, sodium deoxycholate (final concen-tration 0.3%) was added to the perfusion solution for60 s. It has been reported that sodium deoxycholatedoes not interfere with the vasodilating or contract-ing properties of smooth muscle (26).
Statistical Analysis
The changes in perfusion pressure in this experi-ment were measured in terms of area (mmHg z min).
O release was estimated from a peak of the currentetected by each electrode. The data are expresseds means 6 SE and the results were evaluated by annalysis of variance (ANOVA). P values less than
0.05 were considered significant.
RESULTS
Vascular Responses to ACh in the Three PerfusionSystems
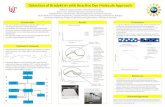
No change in NO current was observed in aorta oraorta-femoral perfusion in response to ACh or BK.Figure 1A shows typical changes in the perfusionpressure and NO release in response to ACh (1025
M) in hindquarter perfusion under the control K–Hsolution. ACh induced NO release (1.0 nmol) with aconcomitant decrease in perfusion pressure (18mmHg z min), which recovered gradually to the con-rol level in 2 min. Figure 1B summarizes NO re-ease and the change in perfusion pressure in re-ponse to ACh between 1027 and 1024 M in
hindquarter perfusion. The baseline perfusion pres-sure prior to administration of ACh was 91.1 6 2.6
mHg (n 5 27). ACh induced a decrease in perfu-ion pressure (2.5 6 1.0 to 55.0 6 6.0 mmHg z min,
n 5 6–8) with an increase in NO release (0.08 60.03 to 0.78 6 0.24 nmol, n 5 6–8) in a dose-dependent manner.
Figure 2 shows the changes in perfusion pressurein response to ACh (1027–1024 M) in different seg-ments of vessels under control perfusion or underthe continuous infusion of L-NMMA. The baselineperfusion pressure prior to administration of ACh
AL.
was 73.3 6 2.2 mmHg in aorta (n 5 24) and 67.3 6.8 mmHg in aorta-femoral perfusion (n 5 28),
s of reproduction in any form reserved.

0o
perfu6–8).
pR
respectively. ACh induced a decrease in perfusionpressure dose-dependently in aorta (0.16 6 0.16 to4.8 6 0.8 mmHg z min, n 5 6), aorta-femoral(0.018 6 0.18 to 42.8 6 9.5 mmHg z min, n 5 6), andhindquarter perfusion (2.5 6 1.0 to 55.0 6 6.0mmHg z min, n 5 6–8). In the presence of L-NMMA,the baseline perfusion pressure prior to administra-tion of ACh was 74.1 6 2.1 mmHg in aorta (n 5 24),68.0 6 2.9 mmHg in aorta-femoral (n 5 28), and94.8 6 2.5 mmHg in hindquarter perfusion (n 5
FIG. 1. (A) Typical changes in the perfusion pressure and NOperfusion under the control K–H solution. ACh induced NO releato the control level in 2 min. (B) NO release and the change in thehindquarter perfusion. Results are shown as means 6 SE (n 5
FIG. 2. Changes in perfusion pressure in response to ACh in th
INTEGRATIVE EFFE
erfusion] under the control K–H solution (open circles) or in the preesults are shown as means 6 SE (n 5 6–8). Significantly different f
Copyright © 2000 by Academic Press. All right
30), respectively. Each value was not significantlydifferent from that in control perfusion. In aorticperfusion in the presence of L-NMMA, ACh (up to1025 M) did not change the perfusion pressure and1024 M of ACh induced a decrease in perfusion pres-sure by 1.4 6 0.7 mmHg z min (n 5 6), which was amarked reduction compared to the control (P ,
.005). In aorta-femoral perfusion, in the presencef L-NMMA, ACh induced a decrease in perfusion
pressure (0 to 42.0 6 10.4 mmHg z min, n 5 7),
se in response to acetylcholine (ACh) (1025 M) in hindquartera concomitant decrease in perfusion, which recovered gradually
sion pressure in response to ACh between 1027 and 1024 M in theSignificant difference: †P , 0.05, #P , 0.001.
perfusion systems [(A) aorta, (B) aorta-femoral, (C) hindquarter
357OF NO AND EDHF
release with
CTS
e three
sence of NG-monomethyl-L-arginine (L-NMMA) (closed circles).rom control: *P , 0.0001, **P , 0.005.
s of reproduction in any form reserved.

t
t
E
as
r
i2p4ll(cmp
ts
e7
m0
sf
gmAwn
n
c
#
DA ET
which were not significantly different from the con-trol. In hindquarter perfusion, ACh (up to 1025 M)induced a decrease in perfusion pressure (4.5 6 1.5o 40.2 6 8.6 mmHg z min, n 5 7) in the presence of
L-NMMA, which were not significantly differentfrom the control, but 1024 M of ACh induced a fur-ther decrease in perfusion pressure to 141.0 6 22.1mmHg z min (n 5 7), whose magnitude was 2.5-foldhat of the control (P , 0.0001).
ffects of L-NMMA, TEA, or Deendothelializationon Baseline Pressure and Response to AChin Hindquarter Perfusion
Continuous infusion of L-NMMA (1.0 mM) inducedgradual increase in the baseline perfusion pres-
ure from 22.5 6 3.5 mmHg to a steady state of26.5 6 4.5 mmHg in 10 min without phenylephrine.With the addition of phenylephrine, the baselineperfusion pressure reached 104.3 6 5.4 mmHg (n 56). In the presence of L-NMMA and phenylephrine,ACh induced a decrease in perfusion pressure by42.8 6 9.8 mmHg z min, which was 81.5% of theesponse in control perfusion (NS, n 5 6).Continuous infusion of TEA induced a transient
ncrease in the baseline perfusion pressure from9.5 6 1.7 to 62.5 6 12.4 mmHg in 4 min. Theerfusion pressure then gradually decreased to0.7 6 3.9 mmHg in 9 min and remained at thatevel. With the addition of phenylephrine, the base-ine perfusion pressure reached 105.1 6 6.1 mmHgn 5 6). ACh was then added and induced a de-rease in the perfusion pressure to 21 6 5.7 mmHg z
in, which was 40.0% of the response in controlerfusion (P , 0.0001, n 5 6).After the addition of both L-NMMA and TEA to
he perfusion solution, the baseline perfusion pres-ure increased and reached a steady state of 61.8 6
7.5 mmHg (n 5 6). Then, the addition of phenyl-phrine increased the perfusion pressure to 102.7 6.0 mmHg (n 5 6). In the presence of both L-NMMA
and TEA, ACh induced a decrease in the perfusionpressure by 7.2 6 1.8 mmHg z min, which was a
arked reduction compared to the control (P ,.0001, n 5 6).Deendothelialization induced a rapid and tran-
358 HARA
ient increase in the baseline perfusion pressurerom 40.4 6 3.6 to 223.7 6 18.4 mmHg, which then
Copyright © 2000 by Academic Press. All right
radually decreased to a plateau level of 121.4 6 8.5mHg (n 5 6) in 8 min without phenylephrine.fter deendothelialization, the responses to AChere completely abolished (P , 0.0001 vs control,5 6). It was ascertained that papaverine (1026–
1023 M), an endothelium-independent vasodilator,induced a decrease in perfusion pressure in the pres-ence of either L-NMMA or TEA and after deendothe-lialization. Figure 3 summarizes the changes in per-fusion pressure in response to 1025 M of ACh underL-NMMA and/or TEA or after deendothelialization.
Vascular Responses to BK in the Three PerfusionSystems
Figure 4A shows typical effects of BK (5 3 1027 M)on the perfusion pressure and NO release. BK in-duced the release of NO (1.2 nmol) with a concomi-tant decrease in perfusion pressure (15 mmHg z
min). Figure 4B summarizes responses to BK (5 31027–1025 M). The baseline perfusion pressure priorto administration of BK was 91.1 6 1.9 mmHg (n 526). BK induced NO (0.39 6 0.15 to 0.62 6 0.19
mol). A low concentration of BK (5 3 1027 and 1026
M) induced a decrease in the perfusion pressure(8.7 6 1.9 and 4.5 6 1.9 mmHg z min), while a highoncentration of BK (5 3 1026 and 1025 M) induced
FIG. 3. Effects of L-NMMA, tetraethylammonium (TEA), anddeendothelialization on the response to ACh. Results are shownas means 6 SE (n 5 6). Significant difference: *P , 0.0001,
P , 0.001, †P , 0.05.
AL.
an increase in the perfusion pressure (0.59 6 2.02and 3.11 6 1.29 mmHg z min).
s of reproduction in any form reserved.

ds
6l
m
in th
(
Figure 5 shows the changes in the perfusion pres-sure in response to BK (5 3 1027 to 1025 M) in the
ifferent segments of vessels under the control K–Holution or under the continuous infusion of
L-NMMA. Under the control K–H solution, the base-line perfusion pressure prior to administration ofBK was 73.5 6 2.3 mmHg in aorta (n 5 24) and 71.3
.3.1 mmHg in aorta-femoral perfusion (n 5 28). Aow concentration of BK (5 3 1027 and 1026 M)
induced a decrease in the perfusion pressure in
FIG. 4. (A) Typical effects of bradykinin (BK) (5 3 1027 M) on peperfusion pressure in response to BK between 5 3 1027 and 1025 M6). Significant difference: #P , 0.001, **P , 0.005.
FIG. 5. Changes in perfusion pressure in response to BK (5 3 10C) hindquarter perfusion] under the control K–H solution (open
INTEGRATIVE EFFE
shown as means 6 SE (n 5 6–7). Significantly different from control:$P , 0.005, §P , 0.0001.
Copyright © 2000 by Academic Press. All right
aorta (0.63 6 0.22 and 0.13 6 0.05 mmHg z min, n 56), aorta-femoral (2.7 6 0.9 and 2.4 6 0.9 mmHg z
min, n 5 6), and hindquarter perfusion (8.7 6 1.9and 4.5 6 1.9 mmHg z min, n 5 6). A high concen-tration of BK (5 3 1026 and 1025 M) induced a smalldecrease in the perfusion pressure in aorta andaorta-femoral perfusion (0 and 0.7 6 0.5 mmHg z
min) and an increase in perfusion pressure in thehindquarter perfusion (0.59 6 2.02 and 3.11 6 1.29
mHg z min, n 5 6).
n pressure and NO release. (B) NO release and the change in thee hindquarter perfusion. Results are shown as means 6 SE (n 5
25 M) in the three perfusion systems [(A) aorta, (B) aorta-femoral,es) or in the presence of L-NMMA (closed squares). Results are
359OF NO AND EDHF
rfusio
CTS
27 to 10squar
*P , 0.0001, †P , 0.05; significantly different from zero level:
s of reproduction in any form reserved.

(m
b
mc
DA ET
In the presence of L-NMMA, the baseline perfusionpressure prior to administration of BK was 74.6 6 2.3mmHg in aorta (n 5 6), 69.7 6 2.8 mmHg in aorta-femoral (n 5 6), and 103.0 6 9.2 mmHg in hindquarterperfusion (n 5 6), respectively. Each value was notsignificantly different from that in each control perfu-sion. L-NMMA abolished or significantly attenuatedthe decrease in perfusion pressure in response to a lowconcentration of BK in the aorta (0 mmHg z min, P ,0.0001, n 5 6), in aorta-femoral (0.1 6 0.8 to 0.3 6 0.3mmHg z min, P , 0.005, n 5 6), and in hindquarterperfusion (0.8 6 0.4 to 1.5 6 1.5 mmHg z min, P ,0.0001, n 5 6–7), respectively. In the presence ofL-NMMA, a high concentration of BK did not changethe perfusion pressure in aorta or aorta-femoral per-fusion, while it induced a further increase in perfusionpressure in hindquarter perfusion (13.2 6 3.5 to15.1 6 3.6 mmHg z min, n 5 7), which were signifi-cantly different from the control (P , 0.0005, n 5 7).
Effects of L-NMMA, TEA, or Deendothelializationon the Response to BK in Hindquarter Perfusion
Changes in perfusion pressure in response to 5 31027 M of BK in the presence of L-NMMA and/or TEAare summarized in Fig. 6. The baseline perfusion pres-sure prior to administration of BK was 103.0 6 9.2
FIG. 6. Effects of L-NMMA, TEA, and deendothelialization onthe response to BK. Results are shown as means 6 SE (n 5 6).Significant difference: *P , 0.0001, **P , 0.005.
360 HARA
n 5 6), 107.7 6 7.4 (n 5 6), and 98.3 6 9.8 (n 5 6)mHg in the presence of either L-NMMA or TEA, and
Copyright © 2000 by Academic Press. All right
L-NMMA 1 TEA, respectively. Each value was notsignificantly different from that in control perfusion(108.3 6 8.3 mmHg, n 5 6). Either L-NMMA or TEAabolished the decrease in perfusion pressure in re-sponse to BK (P , 0.0001, n 5 6). In the presence ofoth L-NMMA and TEA, BK induced an increase in
perfusion pressure (27.97 6 8.97mmHg z min, P ,0.0001, n 5 6). After deendothelialization, the baselineperfusion pressure prior to administration of BK insteady state was 126.5 6 10.4 mmHg. BK induced anincrease in the perfusion pressure (5.47 6 2.24
mHg z min, P , 0.0001 vs control, n 5 6), (NS vs theombined influence of L-NMMA and TEA, n 5 6).
DISCUSSION
This study demonstrated that ACh and BK in-duced NO release and a concomitant decrease in theperfusion pressure in hindquarter perfusion. AChand BK also induced vasodilation in aorta or aorta-femoral perfusion, but no change in the NO currentwas observed in these segments. It was thought thatNO was released in response to ACh or BK in aortaand aorta-femoral perfusion, since the vasodilationwas abolished or attenuated in these segments inthe presence of L-NMMA. No change in NO currentwas observed, since the concentration of NO re-leased in the perfusate in these segments was belowthe lower limit of detection of our NO measurementsystem. NO released in the hindquarter perfusionwas detected in our system, because its vascularbeds are larger than those in aorta and aorta-femoral perfusion.
ACh produced vasodilation in the presence of a NOSinhibitor in hindquarter perfusion, but not in aortaperfusion. This result is consistent with previous re-ports that arterial size is related to the distribution ofNOS inhibitor-resistant vasodilation, which is greaterin small arteries than in large arteries (15, 17). ThisNOS inhibitor resistant vasodilation may be ascribedto vasodilative factors other than NO and prostanoids,since NO release was not observed in the NO measure-ment system and 1024 M of L-NMMA was reported tobe sufficient to completely suppress the increase intissue cGMP levels caused by a vasoactive substance(17). Furthermore, some investigators have reported
AL.
that NO attenuated the production of EDHF (30). Inthe presence of L-NMMA, NO release was inhibited
s of reproduction in any form reserved.

artiamttNsti
aB
CTS
but at the same time a much greater amount of EDHFmight be released compared to control perfusion, sothat the vasodilation might be maintained in hind-quarter perfusion.
NOS inhibitor resistant vasodilation was abol-ished after deendothelialization and significantlyattenuated in the presence of TEA in this study. Itis unlikely that TEA inhibited NOS inhibitor re-sistant vasodilation competitively with ACh forACh receptors, since TEA also attenuated the va-sodilation induced by BK, which binds to BK re-ceptors. TEA has been reported to inhibit mem-brane hyperpolarization of vascular endothelium(27, 28) and vascular smooth muscle cells (5–10,29) by blocking the large conductance calcium-activated potassium channel.
The vascular response to BK is different from thatto ACh, based on the biphasic responses in the vas-culature. BK at a low concentration induced NO andvasodilation, which was abolished in the presence ofL-NMMA, while BK at a high concentration inducedslight vasodilation or vasoconstriction, which wasfollowed by an increased NO release. This increasedNO release might be ascribed to the shear stressinduced by vasoconstriction. The change in perfu-sion pressure in response to BK at a low concentra-tion reversed to increase after deendothelializationin this study. These results suggest that BK at a lowconcentration induced endothelium-derived vasodi-lative factors and simultaneous vasoconstrictionthrough direct effects on vascular smooth musclecells. These results are consistent with those ofPersson et al. They reported that the vascular relax-tion induced by BK was mediated by nitric oxideelease through endothelial bradykinin B2 recep-ors, while vascular contraction was endothelium-ndependent and mediated through bradykinin B1nd B2 receptors located in the vascular smoothuscle layer (31, 32). In the presence of L-NMMA,
he vasodilation in response to BK was abolished inhe hindquarter perfusion as well as in aorta, andOS inhibitor-resistant vasodilation was not ob-
erved in response to BK in our study. NO is thoughto be responsible for the vasodilation induced by BKn arteries, regardless of their size.
A factor related to the potassium channel is also
INTEGRATIVE EFFE
pparently involved in the vasodilation induced byK. TEA completely abolished the vasodilation
Copyright © 2000 by Academic Press. All right
induced by BK in hindquarter perfusion. Previousstudies have reported that BK also induced thehyperpolarization and relaxation of smooth mus-cle cells (17, 22). TEA attenuated the vasodilationin response to BK, presumably through the inhi-bition of hyperpolarization in vascular smoothmuscle cells by blocking the potassium channel. Inthe presence of both TEA and NOS inhibitor orafter deendothelialization, BK induced vasocon-striction. Taken together, these results suggestthat the vascular response to BK consists of acombination of endothelium-independent vasocon-striction and endothelium-dependent vasodila-tion, via NO and a potassium channel related fac-tor, EDHF.
ACKNOWLEDGMENTS
Enalaprilat was kindly provided by Merck & Co., Inc. Thiswork was supported by a Grant-in-Aid for Scientific Research(No. 10670051) to Y.H. from the Ministry of Education, Science,Sports and Culture of Japan (1999).
REFERENCES
1. Furchgott, R. F., and Zawadzki, J. V. (1980). The obligatoryrole of endothelial cells in the relaxation of arterial smoothmuscle by acetylcholine. Nature 288, 373–376.
2. Palmer, R. M. J., Ferrige, A. G., and Moncada, S. (1987).Nitric oxide release accounts for the biological activity ofendothelium-derived relaxing factor. Nature 327, 524–526.
3. Ignarro, L. J., Buga, G. M., Wood, K. S., Byrns, R. E., andChaudhuri, G. (1987). Endothelium-derived relaxing factorproduced and released from artery and vein is nitric oxide.Proc. Natl. Acad. Sci. USA 84, 9265–9269.
4. Moncada, S., and Vane, J. (1979). Prostacyclin formation andeffects. In Chemistry and Pharmacology of Prostanoids (S. M.Roberts and F. Scheinmann, Eds.), pp. 258–273. Pergamon,Oxford.
5. Feletou, M., and Vanhoutte, P. M. (1988). Endothelium-dependent hyperpolarization of canine coronary smooth mus-cle. Br. J. Pharmacol. 93, 515–524.
6. Chen, G., Suzuki, H., and Weston, A. H. (1988). Acetylcholinereleases endothelium-derived hyperpolarizing factor andEDRF from rat blood vessels. Br. J. Pharmacol. 95, 1165–1174.
7. Taylor, S. G., and Weston, A. H. (1988). Endothelium-derivedhyperpolarizing factor: A new endogenous inhibitor from thevascular endothelium. Trends Pharmacol. Sci. 9, 272–274.
361OF NO AND EDHF
8. Komori, K., Lorenz, R. R., and Vanhoutte, P. M. (1988). Nitricoxide, ACh, and electrical and mechanical properties of ca-
s of reproduction in any form reserved.

DA ET
nine arterial smooth muscle. Am. J. Physiol. 255(1, Part 2),H207–H212.
9. Brayden, J. E. (1990). Membrane hyperpolarization is amechanism of endothelium-dependent cerebral vasodilation.Am. J. Physiol. 259(3, Part 2), H668–H673.
10. Nagao, T., and Vanhoutte, P. M. (1991). Hyperpolarizationcontributes to endothelium-dependent relaxations to acetyl-choline in femoral veins of rats. Am. J. Physiol. 261(4, Part 2),H1034–H1037.
11. Beny, J. L., and von der Weid, P. Y. (1991). Hydrogen perox-ide: An endogenous smooth muscle cell hyperpolarizing fac-tor. Biochem. Biophys. Res. Commun. 176, 378–384.
12. Hu, S., and Kim, H. S. (1993). Activation of K1 channel invascular smooth muscles by cytochrome P450 metabolites ofarachidonic acid. Eur. J. Pharmacol. 230, 215–221.
13. Komori, K., and Vanhoutte, P. M. (1990). Endothelium-derived hyperpolarizing factor. Blood Vessels 27, 238–245.
14. Campbell, W. B., Gebremedhin, D., Pratt, P. F., and Harder,D. R. (1996). Identification of epoxyeicosatrienoic acids asendothelium-derived hyperpolarizing factors. Circ. Res. 78,415–423.
15. Nagao, T., Illiano, S., and Vanhoutte, P. M. (1992). Hetero-geneous distribution of endothelium-dependent relaxationsresistant to NG-nitro-L-arginine in rats. Am. J. Physiol.263(4, Part 2), H1090–H1094.
16. Garland, J. G., and McPherson, G. A. (1992). Evidence thatnitric oxide does not mediate the hyperpolarization and re-laxation to acetylcholine in the rat small mesenteric artery.Br. J. Pharmacol. 105, 429–435.
17. Urakami-Harasawa, L., Shimokawa, H., Nakashima, M.,Egashira, K., and Takeshita, A. (1997). Importance ofendothelium-derived hyperpolarizing factor in human arter-ies. J. Clin. Invest. 100, 2793–2799.
18. Malinski, T., and Taha, Z. (1992). Nitric oxide release from asingle cell measured in situ by a porphyrinic-based microsen-sor. Nature 358(6388), 676–678.
19. Ignarro, L. J. (1990). Biosynthesis and metabolism ofendothelium-derived nitric oxide. Annu. Rev. Pharmacol.Toxicol. 30, 535–560.
20. Moncada, S., Palmer, R. M., and Higgs, E. A. (1991). Nitricoxide: Physiology, pathophysiology, and pharmacology. Phar-macol. Rev. 43, 109–142.
21. Shibuki, K. (1990). An electrochemical microprobe for detectingnitric oxide release in brain tissue. Neurosci. Res. N.Y. 9, 69–76.
362 HARA
22. Mombouli, J. V., Illiano, S., Nagao, T., Scott-Burden, T., andVanhoutte, P. M. (1992). Potentiation of endothelium-
Copyright © 2000 by Academic Press. All right
dependent relaxations to bradykinin by angiotensin I con-verting enzyme inhibitors in canine coronary artery involvesboth endothelium-derived relaxing and hyperpolarizing fac-tors. Circ. Res. 71, 137–144.
23. Blais, C., Jr., Drapeau, G., Raymond, P., Lamontagne, D.,Gervais, N., Venneman, I., and Adam, A. (1997). Contribu-tion of angiotensin-converting enzyme to the cardiac metab-olism of bradykinin: An interspecies study. Am. J. Physiol.273(5, Part 2), H2263–H2271.
24. Taddei, S., Virdis, A., Ghiadoni, L., Magagna, A., and Sal-vetti, A. (1998). Vitamin C improves endothelium-dependentvasodilation by restoring nitric oxide activity in essentialhypertension. Circulation 97, 2222–2229.
25. Ichimori, K., Ishida, H., Fukahori, M., Nakazawa, H., andMurakami, E. (1994). Practical nitric oxide measurementemploying a nitric oxide-selective electrode. Rev. Sci. In-strum. 65, 2714–2718.
26. Cusma Pelogia, N., Oliveira, S. F., Nigro, D., de Carvalho,M. H., Scivoletto, R., and Fortes, Z. B. (1993). Endotheliuminactivation in in vitro perfused vascular beds. Compari-son of methods. J. Pharmacol. Toxicol. Methods 29, 157–163.
27. Demirel, E., Rusko, J., Laskey, R. E., Adams, D. J., and vanBreemen, C. (1994). TEA inhibits ACh-induced EDRF re-lease: Endothelial Ca(21)-dependent K1 channels contributeto vascular tone. Am. J. Physiol. 267(3, Part 2), H1135–H1141.
28. Chen, G. F., and Cheung, D. W. (1992). Characterization ofacetylcholine-induced membrane hyperpolarization in endo-thelial cells. Circ. Res. 70, 257–263.
29. Chen, G., and Cheung, D. W. (1997). Effect of K(1)-channelblockers on ACh-induced hyperpolarization and relaxation inmesenteric arteries. Am. J. Physiol. 272(5, Part 2), H2306–H2312.
30. Bauersachs, J., Popp, R., Hecker, M., Sauer, E., Fleming, I.,and Busse, R. (1996). Nitric oxide attenuates the release ofendothelium-derived hyperpolarizing factor. Circulation 94,3341–3347.
31. Persson, K., and Andersson, R. G. (1998). Biphasic responseto bradykinin in isolated porcine iliac arteries is mediated bybradykinin B1 and B2 receptors. J. Cardiovasc. Pharmacol.31, 306–313
32. Yu, H., Carretero, O. A., Juncos, L. A., and Garvin, J. L.
AL.
(1998). Biphasic effect of bradykinin on rabbit afferent arte-rioles. Hypertension 32, 287–292.
s of reproduction in any form reserved.