Infectious diseases of liver 16 6-2016
-
Upload
mahatma-gandhi-medical-college-hospital -
Category
Health & Medicine
-
view
40 -
download
0
Transcript of Infectious diseases of liver 16 6-2016
VIRAL HEPATITIS• Hepatotropic viruses (A, B, C, D, E,G)
• Unless otherwise specified, the term “viral hepatitis” refers to the diseases caused by this group of hepatotropic viruses
• Yellow fever virus• Herpes simplex virus and CMV• Epstein-Barr virus
Hepatitis virusesHAV HBV HCV HDV HEV
Agent ss RNA ds DNA ss RNA ss RNA ss RNA
Route Fecal-oral
Paren-teral
Parenteral
Paren-teral
Water
Incuba-tion
2-6 weeks
4-26 weeks
2-26 weeks
4-7Weeks
2-8Weeks
Carrier state
none 01-1% donors
0.2-1% donors
1-10%
chronic None 5-10% >50% <5% NoneCancer No Yes Yes - -
HEPATITIS A
• “Infectious hepatitis” – in countries with substandard hygiene; 25% of clinically evident acute hepatitis worldwide; Rare after childhood
• Fecal – oral route; virus is shed in feces 2-3 weeks before & I week after onset of jaundice
• Incubation 2-6 weeks; No carrier state or chronicity
• Mild or asymptomatic in most cases; Rarely fulminant hepatitis; fatality ~0.1%
• IgM antibody in serum is reliable marker for infection; IgG antibody provides lifelong immunity
Specific antibody against HAV of the immunoglobulin (Ig) M type appears in blood at the onset of symptoms, constituting a reliable marker of acute infection
Fecal shedding of the virus ends as the IgM titer rises. IgM response decline in a few months and is followed by the
appearance of IgG anti-HAV. IgG anti-HAV- persists for years, perhaps for life, providing
protective immunity against reinfection by all strains of HAV. Hence, the HAV vaccine is effective.
HEPATITIS B VIRUS• Causes “Serum hepatitis”• Clinical spectrum caused by HBV
• Acute hepatitis• Chronic non-progressive hepatitis• Progressive chronic hepatitis ending in cirrhosis• Asymptomatic carrier state• Backdrop for hepatitis D
HEPATITIS B VIRUS• Hepadnavirus• Mature virus particle is called Dane particle• Has
• Core protein (HBcAg & HBeAg)• Envelope glycoprotein (HBsAg)• DNA polymerase • HBX protein is necessary for viral replication &
causation of hepatocellular carcinoma.• It disrupts normal growth control of infected liver cells by
transcriptional activation of several growth-promoting genes, such as insulin-like growth factor II and receptors for insulin-like growth factor I.
• HBx binds to p53 and appears to interfere with its growth-suppressing activities
HEPATITIS B VIRUS INFECTION-Pathogenesis• Proliferative phase
• Episomal DNA with formation of complete virions & all antigens
• Cell surface expression of HBsAg & HBcAg lead to activation of CD8+ T cells
• Integrative phase• Virus DNA is incorporated into the host cell
DNA. With the cessation of viral replication, infectivity ends & liver damage subsides.
HEPATITIS B• World wide carrier rate – 300 million• 300,000 new cases each year in US• Endemic in Africa & SE Asia • It is present in all the fluids of the body• Transmitted by transfusion, IV drug use, dialysis,
homosexual activity, needle stick accidents, trans-placental
HEPATITIS B• HBsAg – appears before onset of symptoms, peaks
during overt disease & declines in 3-6 months• HBeAg, HBV DNA, DNA polymerase appear after
HBsAg & indicate replication• IgM ahti-HBc becomes detectable after onset of
symptoms• IgG anti-HBs appears after the disappearance of
HBsAg and provides lifelong protection
HEPATITIS B• Disappearance of HBeAg with appearance of anti-
HBeAg is indicative of subsiding disease• Loss of HBeAg with failure to form Anti-HBeAg is
associated with fulminant course• Persistence of circulating HBsAg, HBeAg & HBV
DNA usually with anti-Hbc (occasionally with anti-HBs) is associated with progressive disease
Immunoperoxidase stain for HBsAg from the same case,
showing cytoplasmic inclusions of viral particles.
HEPATITIS C • The most important transfusion associated
hepatitis • 90-95% of all transfusion associated hepatitis• Also common in homosexuals, hemophiliacs, IV
drug users & hemodialysis patients• Seroprevalence in US - <0.2% • In patients with unexplained cirrhosis & liver
cancer – prevalence of anti-HCV =>50%• Progression to chronic disease - >50%
HEPATITIS C • Incubation – 2 to 26 weeks• HCV RNA is detectable for 1-3 weeks• Circulating RNA persists even in the presence of
antibodies• Clinical course is milder than Hepatitis B• Persistent infection & chronic hepatitis are
hallmarks; cirrhosis in 5-10 years• Persistent transaminasemia in chronic cases
Chronic viral hepatitis due to hepatitis C virus, showing portal tract expansion with inflammatory cells and fibrous tissue and interface hepatitis with spillover of inflammation into the adjacent parenchyma. A lymphoid aggregate is present.
HEPATITIS D• Delta agent• Absolutely dependent on HBV for multiplication
and causes hepatitis only in the presence of HBV• Two types of infection
• Co-infection• Superinfection
• Simultaneous infection leads to more fulminant course
• IgM anti-HDV is a good marker for HDV exposure
Differing clinical consequences of two patterns of combined
hepatitis D virus and hepatitis B virus infection.
HEPATITIS E• Epidemics in Asia, (Indian subcontinent) sub-
Saharan Africa & Mexico• Primarily in young to middle aged• In most cases self-limited disease• But in pregnant women, high mortality rate (20%)• No chronicity
CLINICAL SYNDROMES WITH HEPATITIS VIRUSES• Carrier state – without clinically apparent disease
or chronic hepatitis (healthy or chronic)• Asymptomatic infection – serologic evidence of
infection only (transaminasemia or antibodies)• Acute hepatitis – icteric or unicteric• Chronic hepatitis – without or with progression to
cirrhosis• Fulminant hepatitis – massive or sub-massive
necrosis
ACUTE VIRAL HEPATITIS• Incubation period• Symptomatic pre-icteric phase – non-specific
constitutional symptoms including fatigue, nausea, anorexia, weight loss, low fever, serum-sickness like symptoms
• Symptomatic icteric phase – conjugated hyperbilirubinemia
• convalescence
CHRONIC HEPATITIS• Symptomatic biochemical or serologic evidence of
continuing or relapsing hepatic disease for more than 6 months with histologically documented inflammation & necrosis
• Causes • Hepatitis viruses (particularly HCV)• Wilson’s disease• Alpha-1 antitrypsin disease• Chronic alcoholism• Drugs (isoniazid, methyl dopa, methotrexate)• autoimmunity
Acute viral hepatitis showing disruption of lobular architecture, inflammatory cells in the sinusoids, and hepatocellular apoptosis
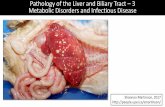
BACTERIAL INFECTIONS OF THE LIVER• Abscess – cholangitic (ascending)
• pylephlebitic (e.g. diverticulitis, appendicitis)• arterial (sepsis)
• Granulomas• TB, tularemia, brucellosis
• Diffuse inflammation• sepsis
• Amoebiasis - abscess• Malaria - hepatomegaly (congestion and uptake of
RBC)• Ascaris - biliary obstruction• Clonorchis sinensis - periductal fibrosis• Schistosomiasis - periductal fibrosis• Echinococcus - cystic hydatid disease
PROTOZOAL AND HELMINTHIC DISEASES