Infectious Diseases MERS- CoV Plans for Hajj 1436...Should be supplemented with other important...
Transcript of Infectious Diseases MERS- CoV Plans for Hajj 1436...Should be supplemented with other important...
-
Infectious Diseases MERS-
CoV Plans for Hajj 1436
Last updated: 19/9/2015
-
MERS-CoV Diversion Plans for Hajj
Purpose of this document
▪ Document clinical operations protocols that must be followed for MERS–CoV cases diversions to
appropriate facilities during the 1436 Hajj season
1
-
Disclaimer for use of this document
This document:
▪ Focuses on protocols to follow during the 1436 Hajj season▪ Focuses on Hajj related locations (Makkah, Madinah, Holy Sites, and
Jeddah) and does NOT cover protocols to follow in other regions in KSA
▪ Is NOT intended as a comprehensive MERS-CoV response guideline▪ Should be supplemented with other important guidelines such as Haj plan
1436 and infection prevention and control and isolation guidelines which are
found on the MOH website:
– MERS-CoV guideline : http://www.moh.gov.sa/en/CCC/StaffRegulations/Corona/
Documents/IPC%20Guidelines%20for%20MERS-
coV%20Infection.pdf
– Is subject to change as guidelines are updated
2
http://www.moh.gov.sa/en/CCC/StaffRegulations/Corona/Documents/IPC Guidelines for MERS-coV Infection.pdf
-
▪ Dr Abdullah Assiri, the Assistant Deputy Minister for preventive Health
▪ Dr. Tariq Al-Arnous, The General Director of General Directorate of Medical Emergency
▪ Dr. Abdulhafiz Turkustani, General Director Assistant for Public Health, Makkah Region
▪ Dr Ali Albarrak, Saudi Centers for Disease Control
▪ Dr Hail Al-Abdely , General Director of the General Directorate of Infection Prevention and Control
▪ Dr. Raafat Al-Hakeem, The Director-General of Communicable Diseases Control
▪ Nasser Abutaleb, 937 Callcenter Director
This document was modified and updated by
Acknowledgments
For any comments, clarifications, or recommendations pertaining to this
document please email Dr. Wail Tashkandi at
For any comments, clarifications, or recommendations pertaining to this document please email Mr.Nasserabutaleb at [email protected]
-
Contents
▪ Guiding principles
▪ Case definitions
▪ MERS-CoV dedicated teams
▪ MERS-CoV diversion plans
▪ Transfer protocols
▪ Home isolation protocols
3
-
General guiding principles to follow in handling MERS-CoV cases (1 of 2)
1 Case definitions available on MoH websites: MERS-CoV
http://www.moh.gov.sa/en/CCC/StaffRegulations/Corona/Documents/IPC%20Guidelines%20for%20MERS-coV%20Infection.pdf
2 Transfer protocols available in this document
General
▪ All hospital staff should be aware of latest MERS-CoV case definitions1
▪ At all times, handle suspect patients with appropriate protectionequipment (i.e. PPEs applied on patients and by health
professionals) and follow all recommended IPC guidelines2
▪ When transferring patients to other locations, transfer protocols2 should be followed
▪ For other infectious diseases not covered in this guideline, please follow standard MoH guidelines
The following principles were followed to create the referral pathways. They should be
followed in case of doubt or when handling cases not specifically addressed in this guide:
4
http://www.moh.gov.sa/en/CCC/StaffRegulations/Corona/Documents/IPC Guidelines for MERS-coV Infection.pdf
-
General guiding principles to follow in handling MERS-CoV cases (2 of 2)
1 Transfer protocols available in this document
Suspected
cases
▪ MERS-CoV: When possible (i.e. isolation room and adequate personal available), preference is to admitting suspect MERS-CoV patients in same facility that
received patient rather than transferring patient to other ERs or MERS-CoV
Designated Hospitals (MDH) or (CoE)
▪ MERS-CoV: Confirmed MERS-CoV patients should be transferred to MERS-CoVDesignated Hospitals (MDH) or Center of Excellence (CoE) following appropriate
transfer protocols1
Confirmed
cases
5
-
Contents
▪ Guiding principles
▪ Case definitions
▪ MERS-CoV dedicated teams
▪ MERS-CoV diversion plans
▪ Transfer protocols
▪ Home isolation protocols
7
-
Suspect case (patients who should be tested for MERS-CoV)
Adults (> 14 years)
I. Acute respiratory illness with clinical and/or radiological,
evidence of pulmonary parenchymal disease (pneumonia or
Acute Respiratory Distress Syndrome .
OR
II. A hospitalized patient with healthcare associated pneumonia
based on clinical and radiological evidence.
OR
III. Upper or lower respiratory illness within 2 weeks after
exposure to a confirmed or probable case of MERS-CoV
infection.
OR
IV. Unexplained acute febrile (≥38°C) illness, AND body aches,
headache, diarrhea, or nausea/vomiting, with or without
respiratory symptoms, AND leucopenia (WBC)
Pediatrics (≤ 14 years)
I. Meets the above case definitions and has at least one of the
following
a. History of exposure to a confirmed or suspected
MERS CoV in the 14 days prior to onset of symptoms
b. History of contact with camels or camel products in
the 14 days prior to onset of symptoms
II. Unexplained severe pneumonia
▪ A probable case is a patient in category I or
II above (Adults and
pediatrics) with
inconclusive laboratory
results for MERS-CoV
and other possible
pathogens who is a
close contact of a
laboratory-confirmed
MERS-CoV case or who
works in a hospital
where MERS-CoV cases
are cared for or had
recent contact with
camels or camel’s
products. Confirmed
case
▪ confirmed case is a person with laboratory
confirmation of
MERS-CoV infection
MERS-CoV case definition
8
-
Contents
▪ Guiding principles
▪ Case definitions
▪ MERS-CoV dedicated teams
▪ MERS-CoV diversion plans
▪ Transfer protocols
▪ Home isolation protocols
9
-
Dedicated teams, reachable through the 937 hotline, will be in place to
assist in managing MERS-CoV
MERS-CoV
▪ MERS-CoV Team: Infectious Diseases consultant on call that can help indiagnosing cases over the phone and advising on appropriate course of action
to take
▪ ECMO team: Emergency team that responds when there is an ECMO need to insert ECMO and transfer the patient
Teams, reachable through the 937 hotline, who can help in diagnosing, handling, or
transferring cases
10
-
12
ECMO Leads in Center of Excellence will be in place to assist in managing
MERS-CoV cases, through the 937 hotline
▪ Age < 60 years old with potential reversible lung pathology.
▪ PF ratio (PaO2:FiO2) < 80 mmHg with FiO2 at 100%.
▪ Respiratory acidosis (PH < 7.2).
▪ PEEP > 15 cm H2O with Pplat > 35 cm H2O.
▪ Murray score 3 - 4 .
▪ No absolute contradiction for ECMO
Indication for V-V ECMO
11
-
Contents
▪ Guiding principles
▪ Case definitions
▪ MERS-CoV teams
▪ MERS-CoV diversion plans
▪ Transfer protocols
▪ Home isolation protocols
12
-
14
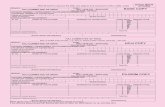
Identification of suspected MERS-CoV cases at Hospitals and PHCs at
Makkah, Holy Sites, Madinah, and Jeddah
History of contact with a known MERS-CoV case
in the last month OR
History of direct or indirect contact with camels in
the last month
YES
Put regular mask on
patient and companions.
Separate physically from
other patients.
Inform IPC and PH
CXR, CBC and swab for
MERS-CoV and Influenza
NO
Treat symptomatically
Educate on respiratory
and hand hygiene
Supply with medical
mask,Discharge if
medically fit
NO
YES
In PHC, if a patient is suspected, transfer
patient to nearest hospital. If patient is
clinically stable and it’s difficult to transfer
due to logistical challenges, apply mask and
direct him/her to the nearest hospital
Acute respiratory symptoms (cough, SOB,
runny nose, sore throat)
Clinical signs
of pneumonia?
-
Diversion plan for a suspect MERS-CoV (ICU and non-ICU) patient in
Makkah, Madinah or Jeddah Hospitals
Suspected1
patient
Immediately give
patient a mask
Admit to
isolation
room
Is isolation
room
available?
Yes No
Test MERS-CoV
and influenza
MERS-
CoV
Team
decision
Initiate
transfer to MDH or CoE2,3 or
Notify
hospital
IPC team
Call 937
(MERS-
CoV Team) if
support or
consultation
needed
Transfer to
MDH
Admit: Hospital IPC team to ensure
appropriate measures are taken (beds
are separated by 1-1.5 meters
1 Refer to MERS-CoV case definition as per MoH’s MERS-CoV online guideline : http://www.moh.gov.sa/en/CCC/StaffRegulations/Corona/Documents/IPC%20Guidelines%20for%20MERS-coV%20Infection.pdf
2 Follow transfer from hospital protocol presented in this guide
3 List of MDHs presented in this guide
4 937 has latest list of MDH hospitals
Keep in hospital
14
http://www.moh.gov.sa/en/CCC/StaffRegulations/Corona/Documents/IPC Guidelines for MERS-coV Infection.pdf
-
Diversion plan for a confirmed MERS-CoV (ICU and non-ICU) patient in
Makkah, Madinah, Holy Sites, or Jeddah Hospitals
1 Refer to MERS-CoV case definition as per MoH’s MERS-CoV online guideline : http://www.moh.gov.sa/en/CCC/StaffRegulations/Corona/Documents/IPC%20Guidelines%20for%20MERS-coV%20Infection.pdf
2 Follow protocol for confirming +ve MERS-CoV case
3 Follow transfer from hospital protocol
4 937 has latest list of MDH hospitals
Confirmed MERS-
CoV ICU patient1,2
Initiate transfer to
MDH through
MERS-CoV team
(937)3,4
Notify hospital IPC
team
15
http://www.moh.gov.sa/en/CCC/StaffRegulations/Corona/Documents/IPC Guidelines for MERS-coV Infection.pdf
-
Special note regarding allowing suspect or confirmed MERS-CoV cases to
participate in the Hajj caravan on the day of Arafa
On the day of Arafa, confirmed/suspect MERS-CoV patients can join
the Hajj Caravan bus (if they are fit to do so). The following
precautions are to be followed:
Patients are to be seated 1 to 1.5 meters apart
Patients are to wear surgical masks, keep on changing the masks
when they get wet
Patients are not allowed to leave the bus
16
-
Contents
▪ Guiding principles
▪ Case definitions
▪ MERS-CoV dedicated teams
▪ MERS-CoV diversion plans
▪ Transfer protocols
▪ Home isolation protocols
17
-
Transfer protocol of a MERS-CoV case from a Hospital to an MDH
Patient needs
ECMO
Is patient
transferable?
Initiate ground transport
ICU patient
Confirmed MERS-CoV
patient in Laboratory
Laboratory
Communicates with
Public Health and
Hospital
Hospital (MD) calls
MERS-CoV team (937)
Continue ICU
management
ECMO team reaches
patient in same hospital
communication with Dr.
Tariq Al-Arnous or his
designee
937 Will connect the MD
with receiving MDH; and
connct with ID /ICU if per
consultation regarding
management … etc
YesYes
No
No
Yes
Is ground
transfer faster
than air?
Yes
No
Initiate air transport
No
18
-
Air transport execution protocol for MERS-CoV cases
Air transport
request
Call Dr. Tariq Al-
Arnous or his
designee1
Saudi Red
Crescent team
Confirmed
MERS-CoV
patient
Air transport
Air transport
YesNo
1 Through the radio network
or phone or his disgnee
19
-
Transfer protocol for ECMO
Hospital calls hotline (937)
and connects to ID
consultant on call
Situation Room
will follow up till
the transfer has
been completed
On call consultant
1. Assesses patient eligibility
For ECMO with
the Intensivist in
the respective
CoE
2. Understands patient
details and transfer
locations
3. Receive contact
information of intenvsist
physician at the receiving
CoE and treating
physician
Dispatch ECMO team
▪ Level 3 ambulance to transport surgeon,
perfusionist and ECMO
machine to referring
hospital for insertion,
stabilization of patient
and transport back to
MERS-CoV Designated
Hospital
CallAlpha Star to initiate
air ambulance with ECMO
team
No
Yes
Is helipad
available?
20
-
Contents
▪ Guiding principles
▪ Case definitions
▪ MERS-CoV teams
▪ MERS-CoV diversion plans
▪ Transfer protocols
▪ Home isolation protocols
21
-
Home isolation in Makkah protocol
If rooms not available or not meeting required
standard, isolation at (Almutahasneen Sections)
at Noor hospital
Follow diversion plans
Provide room in mission
housing according to
isolation standards.
(There are rooms that
have been reserved for
isolation)
Case needs
admission
Case does not
need admission – asymptomatic
or suspected contact
Local
residentsPilgrims
Isolate citizens
in their home
after assurance
of suitability by
the preventive
team
MERS-CoV Patient
22
-
Home isolation in Madinah
Follow diversion plans
Case needs
admission
MERS-CoV Patient
Cases that don’t need
admission shall be quarantined
in their hotel if suitable
If hotel is not suitable, cases
shall be quarantined in Ohoud
Hospital
If ohoud Hospital is full, cases
shall be quarantined in Miqat
Hospital
If is full, cases shall be
quarantined In Rehabilitation
Hospital
If Al Miqat Hospital is full, cases
shall be quarantined at Pilgrim
City hospital
If Pligrim city is full, cases shall
be quarantined at primary
healthcare centers
23
-
25
Specific Madinah & Jeddah hospitals have been designated to handle
confirmed MERS-CoV cases
Jeddah▪ KAMC-Jeddah
Madinah ▪ Ohoud
Surge plansMERS-CoV
Designated Hospital
a) If surge reached at KAMC-Jeddah, transfer Non-
MERS patients to MOH governmental hospital and
private hospitals, if needed.
b) If KAMC-Jeddah is full, transfer to East Jeddah.
c) If surge reached at East Jeddah, transfer to King Faisal
hospital in Taif. If ECMO is needed transfer to PMAH-
Riyadh/ Dammam Medical Complex through 937
a) If surge reached at Ohoud, transfer to King Faisal
hospital Taif.
25
a) if surge reach KAMC, transfer to East Jeddah
b) If surge reached East Jeddah, transfer to King Faisal
hospital in taif. If ECMO is needed transfer to PMAH-
Riyadh/ Dammam Medical Complex through 937
▪ Any Confirmed MERS-CoV
case among
pilgrims or citizens
or
residents: (KAMC).
Makkah
&
Holy
Sites
(pilgrims
or
resident)
-
26
Suspected MERS-
CoV1
Using approved swabs2
Trained nurse or physician
collect samples3 in a
designated area4
Report to public health
officer and infection
control at your hospital
Send samples to your
hospital lab
Get a notification number
from PH officer and add
this number to lab request
plus HESN Code.
Hospital lab call
(5504518 or 5572593)
landline for pickup
Sending a MERS-CoV specimen from Mashaer hospitals to the lab
(valid from 8 to 15 Thul hejjah 1436)
1- See definition in
page 8
2- Swabs with transport
media are available at
hospitals labs,
additional swabs will
be provided by public
health officer at your
hospital
3- Preferred samples
are sputum or tracheal
aspirate, if not feasible,
then nasopharyngeal
swab
4- In a single room with
HEPA filter, HCW to
wear fitted N95, eye
protection, gloves and
gown