Indium-111-DOTA-Lanreotide:Biodistribution ...
Transcript of Indium-111-DOTA-Lanreotide:Biodistribution ...
Indium-111-DOTA-Lanreotide: Biodistribution,Safety and Radiation Absorbed Dose in TumorPatientsIrene Virgolini, Istvan Szilvasi, Amir Kurtaran, Peter Angelberger, Markus Raderer, Ernst Havlik, Friedrich Vorbeck,Claudia Bischof, Maria Leimer, Guido Dorner, Kurt Kletter, Bruno Niederle, Werner Scheithauer and Peter Smith-JonesDepartments of Nuclear Medicine, Oncology, Biomedicai Engineering and Physics, Clinical Pharmacology', Radiology and
Surgery, and the Ludwig Boltzmann Institute for Nuclear Medicine, University of Vienna, Vienna; Department ofRadiochemistry, Research Center Seibersdorf, Austria; and Department of Nuclear Medicine, Haynal University of HealthSciences, Budapest, Hungaiy
Imaging with radiolabeled somatostatin/vasoactive intestinal peptideanalogs has recently been established for the localization diagnosis ofa variety of human tumors including neuroendocrine tumors, intestinaladenocarcinomas and lymphomas. This study reports on the biodis-tribution, safety and radiation absorbed dose of 111ln-1,4,7,10-tet-raazacyclododecane-N,N',N",N'"-tetraacetic acid (DOTA)-lanreotide,
a novel peptide tracer, which identifies hSST receptor (R)subtypes 2through 5 with high affinity, and hSSTRI with low affinity. Methods:The tumor localizing capacity of 1111n-DOTA-lanreotidewas initially
investigated in 10 patients (3 lymphomas, 5 carcinoids and 2 intestinaladenocarcinomas). lndium-111 -DOTA-lanreotide was then administered to 14 cancer patients evaluated for possible radiotherapy with90Y-DOTA-lanreotide (8 neuroendocrine tumors, 4 intestinal adeno
carcinomas, 1 Hodgkin lymphoma and 1 prostate cancer). Afterintravenous administration of1111n-DOTA-lanreotide (=150 MBq; 10nmol/patient), sequential images over one-known tumor site wererecorded during the initial 30 min after peptide application. Thereafter,whole-body images were acquired in anterior and posterior views upto 72 hr postinjection. Dosimetry calculations were performed on thebasis of scintigraphic data, urine, feces and blood activities. A comparison with 111ln-DTPA-D-Phe1-octreotide (111ln-OCT)scintigraphy
was performed in 8 of the patients. Results: After an initial rapid bloodclearance [results of biexponential fits: Teff10.4 min (fraction a., 80%)and Teff213 min (fraction a2 14%)], the radioactivity was excreted intothe urine and amounted to 42% ±3% of the injected dose (%ID)within 24 hr and 62% ±6%ID within 72 hr after injection of 111ln-DOTA-lanreotide. In all patients, tumor sites were visualized during theinitial minutes after injection of 111ln-DOTA-lanreotide. The meanradiation absorbed dose amounted to 1.2 (range 0.21-5.8) mGy/MBqfor primary tumors and/or métastases.The effective half-lives ofl11ln-DOTA-lanreotide in the tumors were Teff14.9 ±2.2 and Teff2
37.6 ±6.6 hr, and the mean residence time Twas 1.8 hr. The highestradiation absorbed doses were calculated for the spleen (0.39 ±0.13mGy/MBq), kidneys (0.34 ±0.08 mGy/MBq), urinary bladder (0.21 ±0.03 mGy/MBq) and liver (0.16 ±0.04 mGy/MBq). The effective dosewas 0.11 ±0.01 (range 0.09-0.12) mSv/MBq. During the observationperiod of 72 hr, no side effects were noted after 1111n-DGTA-lan-reotide application. The 1111n-DOTA-lanreotide radiation absorbed
tumor dose was signifcantly higher (ratio 2.25 ±0.60, p < 0.01) whendirectly compared with 111ln-OCT.Conclusion: lndium-111-DOTA-
lanreotide shows a high tumor uptake for a variety of differenthuman tumor types, has a favorable dosimetry over1111n-OCT and
is clinically safe.Key Words: 1,4,7,10-tetraazacyclododecane-N,N',N",N'"-tetraace-tic acid-lanreotide; indium-111-octreotide; somatostatin receptor;radiation absorbed dose; tumor therapyJ NucÃMed 1998; 39:1928-1936
Received Aug. 5, 1997; revision accepted Jan. 28, 1998.For correspondence or reprints contact: Irene Virgolini, MD, Department of Nuclear
Medicine, University of Vienna, WähringerGürtel18-20, Ebene 3L, A-1090 Vienna,Austria.
In the last few years increasing efforts have been undertaken tointroduce peptide receptor (R)-specific radioligands includingsomatostatin (SST) analogs (/-5) and vasoactive intestinalpeptide (VIP) (6-9) for in vivo application in tumor patients.
Based on higher amounts of SSTR/VIPR on tumor cells whencompared with normal tissues, some of these radioligands havebeen used successfully for tumor localization diagnosis innuclear medicine (1,4,7). Furthermore, initial results using highamounts of '"in-DTPA-D-Phe'-octreotide ('"in-OCT) have
indicated a significant therapeutic potential for patients withSSTR expressing tumors (10,11).
The molecular basis for the interaction of labeled SSTanalogs, or of VIP, with the cell surface is provided by receptorproteins. In recent years, at least five distinct hSSTRs have beencharacterized and have been cloned (12-18). However, the
expression of the tumor hSSTR subtypes is not yet wellunderstood (19). The current data suggest that at least one, orany combination of hSSTR subtypes, can be present in a humantumor. Whereas neuroendocrine tumors seem to predominantlyexpress hSSTR2 (20), intestinal adenocarcinomas and a varietyof other tumor types seem to overexpress mainly hSSTR3and/or hSSTR4 (19,21). A significant clinical potential hasrecently been implicated by the observation that radioiodinatedVIP, which visualizes intestinal adenocarcinomas (7), binds tohSSTR3 with high affinity (22) since hSSTR3 seems to be thesite of cross-competition between SST-14 and VIP (23).
We hypothesized that a hSSTR analog, which identifies allhSSTR subtypes would be most useful for the diagnosis andtreatment of cancer. Our approach identified a lanreotide-basedpeptide (i.e., 1,4,7,10-tetraazacyclododecane-N,N',N",N'"-tet-
raacetic acid (DOTA)-lanreotide), which, when labeled with1"In or 90Y, binds to hSSTR2 through 5 with high affinity (i.e.,
dissociation constant Kd 1-10 nM) and to hSSTRI with lowaffinity (Kd = 200 nM) (24). Furthermore, the binding behaviorof DOTA-lanreotide is distinct from its unlabeled mothersubstance "lanreotide," and is also distinct from all other
commercially known SST peptide analogs (24). In particular, incontrast to DOTA-lanreotide and lanreotide, octroetide-based
ligands do not bind with high affinity to hSSTR4, they onlybind with moderate affinity to hSSTR3 and do not bind tohSSTRI at all (19,24). Since hSSTRs are expressed by virtuallyall human tumors (19), and DOTA-lanreotide was found to bindto all transfected hSSTR subtypes, as well as to a large varietyof primary human tumors and tumor cell lines, we haveproposed this peptide to be useful to image all human tumorsexpressing hSSTR, i.e., virtually all human tumors. In thisarticle, we report on the in vivo tumor localizing capacity of' "in-DOTA-lanreotide in 24 patients, as well as its safety, and
1928 TiIKJOURNALOFNUCLEARMEDICINE•Vol. 39 •No. 11 •November 1998
the detailed radiation absorbed dose estimates for 14 patientsbefore therapy with 90Y-DOTA-lanreotide.
MATERIALS AND METHODSRadiopharmaceutical Preparation of lndium-111-DOTA-Lanreotide
DOTA-lanreotide was synthesized using the commercially available lanreotide (Somatuline*, D-ßNal-Cys-Tyr-D-Trp-Lys-Val-
Cys-Thr-NH2) and DOTA as starting materials (24). Briefly, afterconjugation, the product, [DOTA-(D)-Nal']-lanreotide, was purifiedon a CIS reverse phase, high-performance liquid cnromatography(HPLC) column using a water/acetonitrile/0.l% trifluoroacetic acidsolvent system. A second HPLC purification using water/acetoni-trile/1% acetic acid yielded the pure compound as an acetate salt[purity: 97% (RP18-HPLC), MS: MNa+: 1504 (FAB)]. The conjugate(DOTA-lanreotide) was radiolabeled with ' "lnCl3 (Nordion, Ontario,
Canada, no carrier added, >1850 MBq/ml in 0.05 M HC1). Qualitycontrol of the radiolabeled DOTA-lanreotide was performed withinstant thin-layer cnromatography (TLC), using a mobile phase of 4mM ethylenediaminetetraacetic acid (pH 4.0). In this instant TLCsystem, the peptide-bound activity remains at the origin and thepreviously uncomplexed radiometal moves with the solvent front as anEDTA complex. The radiolabeled conjugate was then formulated in0.075 MNaCl, 0.05 A/NH4OAc, 0.2 M ascorbic acid and 0.1% humanserum albumin before sterilization by filtration through a sterile MillexGV 0.2 mm membrane (Millipore, Milford, MA). A specific activityof about 20 MBq/nmol was achieved for " ' In-DOTA-lanreotide.
PatientsThe application of ulIn-DOTA-lanreotide (as well as of 90Y-
DOTA-lanreotide) to patients for tumor diagnosis and tumortherapy was approved by the Ethical Committee of the medicalfaculty of the University of Vienna. All patients gave writteninformed consent to participate. The study was performed according to the Declaration of Helsinki.
In initial applications, the feasibility of "'In-DOTA-lanreotide
to visualize human tumors was studied in 5 carcinoid tumorpatients, 3 patients with lymphomas (2 non-Hodgkin's lymphomasand 1 Hodgkin's lymphoma) and in 2 patients with intestinal
adenocarcinomas (1 pancreatic adenocarcinoma, 1 colorectal ade-nocarcinoma).
After this initial pilot series, with an additional 14 patients,whole-body biodistribution and dosimetry of '" In-DOTA-lan
reotide were evaluated (Table 1). These patients were all refracto-ry-to-conventional treatment strategies and were referred for potential treatment with 9(>Y-DOTA-lanreotide. Eight patients had
neuroendocrine tumors (6 carcinoids, 1 gastrinoma, 1 pheochro-mocytoma), 1 patient had a Hodgkin's lymphoma, 4 intestinal
adenocarcinomas (2 colorectal, 2 pancreatic), and 1 patient had anadenocarcinoma of the prostate. In all patients, diagnoses andstages of the disease were established according to World HealthOrganization criteria. The location and size of primary tumorsand/or spread of métastaseswere investigated by conventional CTor MRI, radiography, colonoscopy or surgery. All patients receiving treatment with long-acting SST analogs had to be withdrawnfor at least 7 days before the dosimetry study. In one patient,(Patient 11) treatment with octreotide was withrawn only 3 daysbefore the scintigraphic study.
Gamma Camera AcquisitionIndium-111-DOTA-lanreotide was administered as a single in
travenous bolus injection (=«150MBq; 7 nmol DOTA-lanreotide/
patient). To record potential side effects, patients were monitoredfor vital signs and were asked up to the 72 hr whole-body scan toreport any side effects.
Standard techniques were applied for recording and visualiza
tion. Planar and SPECT acquisitions were performed with a PickerPRISM 1000 (Toshiba, Japan) gamma camera equipped with amedium-energy collimator. At the time of "'In-DOTA-lanreotide
injection, the field of view covered a clinically-known tumorlocation (i.e., the collimatore were placed either over abdomen orthorax). The radiation of both energy peaks ( 173 keV and 247 keV)with settings of windows of 20% were used. Sequential imageswere recorded over 30 min (matrix 128 X 128 pixels). Serialwhole-body acquisitions were then recorded in anterior and posterior views (matrix 256 X 1024, 15 min each) at 0.5-1, 2-4, 6-8,24, 48 and 72 hr postinjection. In 4 patients, an additional 96-hrwhole-body scan was acquired. SPECT and planar acquisitions(matrix 128 X 128, 500 kcts preset) were performed usuallyfollowing the 2-4 or 24 hr whole-body scan. SPECT was performed in a 360°circle in 6°steps, 30 sec per step. Ramp filteredbackprojection and three-dimensional, low-pass postfiltering wereperformed. All scans were reconstructed in three projections andwere viewed by two independent nuclear medicine physiciansusing a simple yes- or-no evaluation system to evaluate tumors ormétastasesas visualized by gamma camera imaging.
Blood, Urine and Feces CollectionsBlood samples were collected directly before injection and after
1,5, 15, 30, 60 min and 2, 4, 8 and 24, 48 and 72 hr postinjection.Urine was collected up to 72 hr after the injection of ' " In-DOTA-
lanreotide, and the volumes and voiding time noted by the patient.In 9 patients, feces was collected over a period of 72 hr.
A sample of the blood, urine or feces was counted in acallibrated automatic gamma counter (Packard, 5000 series, Chicago, IL) and expressed as becquerels per milliliter. The countingefficiency of the system was determined by counting a calibratedsource of '"in with same geometry to that of the samples.
Radioactivity measurements were corrected for the physical decayof "'in. Radioactivity in the urine or feces was multiplied by the
uriñe/fecesvolume and the radioactivity in the samples expressedas percent of the injected '" In-DOTA-lanreotide dose. The chem
ical form of the urine radioactivity was analyzed by C18 reversephase HPLC column using a water/acetonitrile/0.1% trifluoroaceticacid solvent system.
Absorbed Dose CalculationsRegions of interest (ROls) were drawn on every whole-body
scintigram at each time point. The mean of anterior and posteriorcounts was calculated for large ROIs of the liver, spleen, kidneysand urinary bladder. In addition, ROIs were drawn for all traceraccumulations regarded as tumor sites and background regionsusing the software written for the Picker analyzing system. Allgamma camera data were background and decay corrected back tothe time of injection. Mono- or biexponential time-activity curveswere fitted. The residence times were determined by using this dataand the respective half-lives of " 'in or 90Y. The derived residence
times, as well as the data of the urinary and fecal measurements,were used for organ dose calculation on the basis of the MedicalInternal Radiation Dose (MIRD) concept (25). Absorbed organdoses were calculated by applying the MIRDOSE3 software (26).For tumor doses, the "Nodule Module" option of the program for
estimating the self-S values of spherical tumors were applied. If atumor mass was within an organ of considerable activity accumulation such as the liver, a mass-dependent background correctionwas necessary. Concerning the tumor doses for WY-DOTA-
lanreotide, the fractions of absorbed dose from beta radiation of thesurrounding tissue were estimated by using dose profile calculations. However, this contribution to the tumor dose was significantonly for small tumors < 5 g. '
The effective dose, as defined by the International Commissionon Radiological Protection, was also calculated (27).
INDIUM-111-DOTA-LANREOTIDE•Virgolini et al. 1929
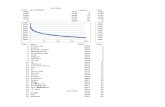
TABLE 1Patient Diagnoses and lndium-IH-DOTA-LanreotideA'ttrium-90-DOTA-Lanreotide Tumor Kinetics and Radiation Dose
Tumor dose of DOTA lanreotide
Patientno.123456SexMMFMFF,
MAge675752667136Histological
diagnosisLung
carcinoidProstateadenocarcinomaLNNmétastasesColonieadenocarcinoma"Liver
metastasisLivermétastasesRecurrent
lungcarcinoidLivermétastasesPancreaticadenocarcinomaLivermetastasisHodgkin's
lymphomaMass
(9)1616014350342PrevioustreatmentS,
E,OCTCHT,RTS,
CHTS,
OCTES,
CUTCHT,
BMT,RTal
a2 Ta,,,Tg^(%)
(%) (hr)(hr)0.21
360.34
2.44 4.5490.26
0.47 5.0384.13.2 5.0380.110.4 2.742Scintigraphy
positive,butScintigraphynegative0.31
- 37T
'broli(hr)
(hr)0.111.750.282.00.24dosimetry0.17-4.85.43.72.8111lnTbio,2 (mGy/MBq)(hr)(calculated)8220893931180.260.580.640.262.14«V(mGy/MBqO(calculated)55.59.24.134.5not
performed-870.8314
7 F
8 M
9 M
10 F
11 M
12 F
13 M
14 F
LNN métastases 22 - 1.5 - 25 0.54 - 41Bone marrow métastases 11 - 0.45 - 36 0.23 - 82
57 Colonie adenocarcinoma* S, CHT
Liver metastasis 65 E - 1.7 - 24 0.6 - 38
Liver métastases 200 0.21 8.1 6 33 3.8 6.6 6849 Recurrent gastrinoma 4.2 S 0.28 0.74 9 35 0.41 10.5 77
Uver métastases 25 0.28 0.27 7 38 0.18 7.9 9366 Jejunal carcinoid" S, OCT
Liver métastases 40 E 0.35 0.45 7 47 0.34 7.9 176Lung métastases 8 0.20 0.25 6 47 0.19 6.6 176
32 Rectal adenocarcinoma* S, CHT
Lung métastases 249 RécurrentJejunal carcinoid 25 S, OCT
Liver métastases 140Bone métastases
57 Pheochromocytoma S, MIBGBone metastasis 10Other bone and
LNN métastases62 Recurrent Jejunal carcinoid 24 S, OCT
Liver métastasesLung métastases
58 Pancreatic carcinoid*
LNN métastases 200 S, OCT - 9.4 - 37.5 5.1 - 90
Liver métastases 350 7.1 31.4 4 38 17.6 4.3 93Lung métastases 5.5 0.11 0.37 2 46 0.25 2.1 163Bone métastases 20 1.88 2.88 3 30.5 1.35 3.1 58
0.17 - 44 0.11 - 140
0.82 1.43 4.5 30 0.67 4.8 569.7 5.5 3.5 38 3.5 3.7 93Scintigraphy positive, but dosimetry not performedPrimary tumor not visualized by Scintigraphy0.75 1.13 2.0 33.5 0.57 2.1 70Scintigraphy negative or inconclusive
3.0 - 43 1.86 - 130
Scintigraphy positive, but dosimetry not performedScintigraphy positive, but dosimetry not performed
1.040.62
0.90.655.80.67
0.670.62
1.60.940.21
1.6
1.62
0.81.921.601.92
2211
159.6
5610
10.711.5
221913.6
27
26
13262132
"Primary tumor was resected.
In all patients, multiple sites of tumors were known at the time of Scintigraphy. Tumor absorbed dose calculations were performed only for those tumorswhich sizes could be accurately determined by CT/MRI. S = surgery; E = chemoembolisation; CHT = chemotherapy; RT = conventional radiotherapy;BMT = bone marrow transplantation; OCT = octreotide; LNN = lymph nodes; DOTA = 1,4,7,10-tetraazacyclododecane-N,N',N",N'"-tetraacetic acid; MIBG
= metaiodobenzylguanidine.
To estimate the activity in tumors embedded in the liver,measurements with a liver phantom in a thorax phantom tissue-equivalent were applied. The liver phantom was filled with '"in
activity in water similar to the activity found in the liver of thepatients (10 MBq/liter). Vials of different sizes were filled withwater containing the tenfold activity concentration, as comparedwith the concentration in the liver phantom, and were inserted intothe phantom to simulate activity accumulating tumors. Whole-bodyscintigraphies of the liver phantom within the thorax were performed and evaluated in the same way as of the cancer patients. Asa result, a volume-dependent function was found that could be usedfor correcting deviations in activity estimations due to the rathercomplicated differentiation of radioactivity in the liver and in thetumor by evaluating ROIs in the planar scintigrams.
lndium-111-Octreotide ScintigraphyIndium-111-OCT was prepared by reacting 10 /ug DTPA-OCT
for 10 min at 22°Cwith 100-200 MBq of '"in-Cl, according tothe manufacturer's description (Mallinckrodt, Inc., St. Louis, MO).
Comparative scintigraphies (planar and SPECT studies) wereperformed in 8 of the 14 patients listed in Table 1. The time-spanbetween both scintigraphies ranged between 4 and 12 wk.
RESULTS
SafetyAfter intravenous injection of " ' In-DOTA-lanreotide, no
side-effects were noted during the whole observation period of4 days.
1930 THEJOURNALOFNUCLEARMEDICINE•Vol. 39 •No. 11 •November 1998
10:
mo'•5cece 0,1
0,010,01 0,1 1 10
Time Postinjection (h)
100
FIGURE 1. Blood kineticsof 111ln-DOTA-lanreotide(150 MBq). Whole bloodactivity (•)and peptide activity (•)is shown (n = 12).
Whole-Body Biodistribution of lndium-111-DOTA-Lanreotide
After intravenous injection, '"in-DOTA-lanreotide was rap
idly cleared from the circulation. Radioactivity in the bloodrapidly decreased to less than 3% of the injected dose within thefirst 2 hr after injection of " ' In-DOTA-lanreotide (Fig. 1).
The cumulative radioactivity excreted into the urineamounted to 21% ±4%ID of the injected activity at 4 hr, 42%±3%ID at 24 hr, 52% ±6%ID at 48 hr and to 62% ±6%ID
at 72 hr after injection of ' " In-DOTA-lanreotide (Fig. 2). Up to
24 hr postinjection, the main excretion product was the intactpeptide, but at later time points only metabolites were seen.After 48 hr, only one major metabolite (probably DOTA-(D)ßNal)was observed (Fig. 2). Cumulative radioactivity in thefeces was 0.34% ±0.09%ID (n = 9) after 24 hr and 1.0% ±
0.7%ID after 72 hr.A biexponential function could be fitted to the whole-body
retention of radioactivity (Fig. 3A). Twenty-four percent of theactivity was eliminated with an effective half-life (Teff) of 3.3
hr, and the remaining 76% was eliminated with a Teffof 41 hr.The accumulation of "'In-DOTA-lanreotide in the major or
gans is depicted in Table 2.
Radiation Absorbed DosesThe liver, spleen, kidneys and urinary bladder were used as
the primary source organs. Individual ROIs were fitted overthese organs, as well as over tumors/metastases. The radiationabsorbed organ doses are presented in Table 3. The highestradiation-absorbed doses were calculated for the spleen (0.39mGy/MBq), kidneys (0.34 mGy/MBq), urinary bladder (0.21mGy/MBq) and liver (0.16 mGy/MBq).
The absorbed doses to the gonads and bone marrow was< 0.08 mGy/MBq. The effective dose was estimated to be0.11 ±0.01 (range 0.09-0.12) mSv/MBq.
Tumor Visualization by lndium-111-DOTA-LanreotideIn the pilot series of 10 patients, the feasibility of mln-
DOTA-lanreotide to visualize primary and/or metastatic tumorswas evidenced for carcinoid tumor patients (n = 5), lymphomapatients (n = 3) and adenocarcinoma patients (n = 2). In thecarcinoid patients, liver métastaseswere visualized in 4/4, bonemétastasesin 2/2, lung spread in 1/1 and lymph nodes in 2/2patients. In the 3 lymphomas patients, multiple tumor sites were
FIGURE 2. Cumulative urinary activityafter injection of 1"In-DOTA-lanreotide.Cumulative urinary activity is shown (n =14). Insert shows that intact peptide (•)isonly excreted during first 24 hr, and thatexcretion rate of metabolites is fairly constant over whole 48-hr period.
10 20 30 40
Time Postinjection (h)
50
20 40 60 80 100 120
Time Postinjection (h)
140r
160
INDIUM-111-DOTA-LANREOiiDE•Virgolini et al. 1931
20 40
Time Postinjection (h)
40 60 BO 100
Time Postinjection (h)
oE31
t•ea 2-
40 60 80 100
Time Postinjection (h)
20 40 60 60 100
Time Postinjection (h)
FIGURE 3. Whole-body, kidney and tumor kinetics of 111ln-DOTA-lanreotide incomparison to 111ln-OCT. (A) Whole-body kinetics of 1l1ln-DOTA-lanreotide
are given (n = 14). (B) Comparativewhole-body kinetics of 111ln-DOTA-lan-reotide (•)and 111ln-OCT (•)in Patient14 is shown. (C) Kidney uptake in carci-
noid tumor patient was significantlylower. (D) Tumor uptake was significantlyhigher for1111n-DOTA-lanreotide as compared with 111ln-OCT.
visualized in the chest, abdomen and pelvis, and bone marrowinvolvement in 2 of the 3 patients. A recurrent pancreaticadenocarcinoma and liver métastasesin a patient with colorec-tal adenocarcinoma (primary resected) were visualized as well.
A further 14 patients were referred to our department forevaluation of potential therapy with 90Y-DOTA-lanreotide (Ta
ble 1). After the dynamic study (Fig. 4), serial whole-bodyscanning (Fig. 5) for dosimetry calculations was performed.The dynamic study typically revealed the in vivo binding of
11In-DOTA-lanreotide to the tumor within the first minutes
(Fig. 4). Thereafter, tumor localization was characterized by
anterior and posterior planar imaging (Fig. 6) as well as bySPECT (Fig. 7), performed usually between the 2-4 and 6-8 hrwhole-body scan and/or after 24 hr postinjection. In all patients,at least one known tumor site was visualized by '"In-DOTA-
lanreotide scintigraphy. Several previously unknown tumorsites were seen in the carcinoid patients (Patients 11, 13 and14), the prostate cancer patient (Patient 2) and the lymphomapatient (Patient 8). A large primary pancreatic adenocarcinomain Patient 5 and multiple sites in the pheochromocytoma Patient12 were not visualized. However, in Patient 5 liver métastaseswere imaged and in Patient 12 some bone métastases.
TABLE 2Biological Clearance of Radiolabeled DOTA Lanreotide (%ID)
Time(hr)135244872LiverMean6.60
±6.41±5.84±4.21±3.10±2.57
±=
sd1.451.291.100.830.650.60Range4.23-8.224.24-7.993.96-7.042.84-5.252.21-3.971
.83-3.31Mean2.41
±2.32±2.09±1.53±1.29±0.99
±Spleen±sd0.440.460.460.470.440.42Range1.79-3.191.49-3.091.35-2.981.06-2.610.98-2.340.72-2.00Mean4.164.274.143.362.512.00Kidneys±sd±
1.09±1.21±1.10±0.89±0.75±
0.71Range2.50-5.932.52-6.392.43-5.651.79-4.211.38-3.691.03-3.25RemainderMean
±sd84.9
±2.774.4±3.068.7±4.956.9±6.248.9±6.441
.7±7.4Range80.8-89.567.4-80.458.9-76.146.5-70.240.8-65.232.9-61.5Meanclearanceratesa,
(%ID)Tb«*,(hr)a2(%ID)Tbiol2
(hr)0.651.884.880.30.664.571.7035.30.17>2004.1659.827.21.9266.4107Residencetimes111ln(hr)*>Y(hi)3.11 ±2.99
±0.860.801
.99^1.951.
93^.691.21±1.17
±0.410.400.89-2.060.87-2.012.061.97±0.54±0.551.17-2.671.14-2.5838.3±4.136.9±3.832.8-43.031.7-41.4
Based on serial l11ln-DOTA-lanreotide whole-body imaging, the residence times for "In-DOTA-lanreotide and ^-DOTA-lanreotide were calcualted.
Values refer to the data obtained in the 14 cancer patients evaluated for possible therapy (see Table 1).
1932 THEJOURNALOFNUCLEARMEDICINE•Vol. 39 •No. 11 •November 1998
TABLE 3Radiation Dose Estimates (mGy/MBq) for lndium-111 -DOTA-Lanreotide and Yttrium-90-DOTA-Lanreotide
lndium-111 -DOTA-Lanreotide Yttrium-90-DOTA-Lanreotide
Organ Mean Medium Range Mean Medium
'Based on the biodistribution of 111ln-DOTA-lanreotide. ULI = upper low intestine; LLI = lower low intestine.
Range
KidneysLiverSpleenGonadsRed
marrowUrinarybladderGastrointestinaltractSmallintestineULILUEffective
doseequivalent(mSv/MBq)Effective
dose(mSv/MBq)0.340.160.390.080.070.210.080.090.100.130.110.330.150.340.060.070.180.080.080.090.130.100.24-0.460.11-0.250.26-0.640.06-0.110.06-0.080.17-0.250.07-0.090.08-0.110.07-0.130.10-0.160.09-0.123.61.024.00.330.331.60.190.300.470.890.583.50.933.40.300.301.40.170.280.450.890.562.2-5.00.6-1.82.5-7.20.28-0.410.28-0.411.4-1.90.16-0.230.26-0.350.44
±0.520.75-1.730.46-0.69
Tumor Radiation Absorbed DoseThe tumor radiation absorbed dose for each patient is listed in
Table 1. In most of the tumors, the accumulated activity wasslightly increasing during the first hours after the injection. Atypical time-activity course showed an increase of 12% between1 and 3 hr after injection. Thus, most probably the maximumaccumulation of activity is reached between 3 and 6 hr afterinjection. Within the first 24 hr, some tumors lost a significantamount of radioactivity indicating a relatively fast component(Teffl 4.9 ±2.2 hr). The remaining activity decreased veryslowly with a Tefï2of 37.6 ± 6.6 hr. From the effectivehalf-lives, the biological half-lives were calculated to be Tbio]15.1 ±2.3 hr and Tbjol2 101 ±42 hr. The mean value of thetumor uptake was 0.085%ID/g (range 0.01%-0.24%ID/g). The
biokinetic data result in the mean residence time T, which is asuitable measure to determine the radiation absorbed doses. The
\ i '
¡ici ¿E ut?
» •FIGURE 4. Dynamic study after injection of 111ln-DOTA-lanreotide (-150
MBq) in Patient 5. This figure shows the sequential anterior images acquiredover the first 16 min after 111ln-DOTA-lanreotide injection (1 frame/min). Alarger liver metastasis (arrow) was seen by 111ln-DOTA-lanreotide immedi
ately after injection (see also Fig. 7).
mean radiation dose to the tumor was 1.2 (range 0.21-5.8)mGy/MBq.
lndium-111-DOTA-Lanreotide Versus lndium-111-
Octreotide ScintigraphyIn 8 patients, "'in-OCT scintigraphy was compared with
'"in-DOTA-lanreotide scintigraphy (Patients I, 2, 4, 8, 10, 11,13 and 14). Also by "'In-OCT scintigraphy, multiple sites of
tumor spread were visualized (Fig. 6). As compared withulIn-DOTA-lanreotide, "'in-OCT showed a faster whole-
body clearance of radioactivity (Fig. 3B). The time-activitycurve for ' " In-DOTA-lanreotide for the kidneys was lower asopposed to ' " In-OCT (Fig. 3C), whereas the tumor uptake was
remarkably higher (Fig. 3D). The ratio of the radiation absorbeddose for '"In-DOTA-lanreotide and '"In-OCT calculated for
the primary/recurrent tumors and/or métastaseswas 2.25 ±0.60 (paired Student's t-test, p < 0.01).
A clear difference was also noted for the biokinetics in theliver and the spleen (Table 4). Whereas the spleen uptakeincreased during the initial hours after injection of '"In-OCT(p < 0.01 ), it steadily decreased after injection of " ' In-DOTA-
lanreotide, starting at 1 hr postinjection. Liver uptake ofluIn-DOTA-lanreotide was about 40% higher as comparedwith '"In-OCT.
DISCUSSIONRecent studies have shown that various tumor cells express
substantial amounts of peptide receptors and, in particular, ofSSTR and VIPR (23,28). Based on these observations, we havedeveloped a novel SSTR scintigraphy by using '"In-DOTA-
lanreotide as radioligand (24). In this study, we demonstratethat this tracer is able to visualize a variety of different tumortypes in human in vivo, i.e., neuroendocrine tumors, intestinaladenocarcinomas, lymphomas and prostate cancer. Furthermore, the in vivo binding of '"In-DOTA-lanreotide to tumor
tissues was found to be remarkably higher when compared withthe accumulation and/or binding of the tracer to normal organssuch as kidneys, liver or spleen. This high tumor bindingcapacity of DOTA-lanreotide, when labeled with 90Y, provides
the basis for receptor-mediated radiotherapy in tumor patients(unpublished results).
In initial studies, the tumor localizing capacity of '"In-
DOTA-lanreotide was demonstrated in 10 patients with eithercarcinoid tumors, lymphomas or intestinal adenocarcinomas.
INDIUM-!11-DOTA-LANREOTiDE•Virgolini et al. 1933
"-
We then investigated the tumor doses and biodistribution of'"in-DOTA-lanreotide in 14 patients with advanced tumordisease evaluated for therapy with 90Y-DOTA-lanreotide. In all
patients, at least one-known tumor site was visualized byIn-DOTA-lanreotide during the first minutes after injection
of the substance. Tumor sites were still visible at 72 hrpostinjection. Indium-111-DOTA-lanreotide concentrated inmultiple sites of neuroendocrine tumors ( 11 carcinoid patients,1 gastrinoma patient and 1 pheochromocytoma patient), as wellas in lymphoma sites (4 patients), prostate cancer ( 1 patient) andliver and lung métastasesof intestinal adenocarcinomas (6patients). The few DOTA-lanreotide-negative tumor sites (aprimary pancreatic adenocarcinoma, 8 cm in diameter) inPatient 5 and multiple locations in the pheochromocytomaPatient 12) could be explained by loss of SSTR during progression of the tumors. A change in the SSTR content or cell surface
FIGURE 5. Serial whole-body scintigra-phy after injection of 111In-DOTA-lanreotide (-150 MBq) in Patient 6. Thisfigure shows anterior whole-body scans
at 0.5 (A), 4 (B), 24 (C) and 48 (D) hrpostinjection of 1111n-DOTA-lanreotide.Multiple lymph-node and bone métasta
ses were visualized in right groin, rightpelvis, distal femur, mediastinum andhead.
expression may also be the reason for the change of thescintigraphic feature in Patient 3 in whom a preceeding positive111In-DOTA-lanreotide scintigraphy (hot spot) of a larger liver
metastasis had turned after 3 mo into a cold spot showing anenhanced activity at the margin. This feature was accompaniedby largely increased size, as well as by central necrosis of themetastasis, on the CT scan. This could explain why the largertumors tended to have a slightly lower radiation absorbed dosein comparison with the small- and medium-sized tumors.
To estimate the tumor dose a patient would receive bytreatment with 90Y-DOTA-lanreotide, dosimetry studies wereperformed with "'In-DOTA-lanreotide. The assumption thatDOTA-lanreotide, when labeled either with '"in or with 90Y,
would identify the same tumor masses and would concentrateidentically in human tumors in vivo was based on our preclin-ical studies, which suggest the same stability and SSTR binding
FIGURE 6. Anterior planar scintigraphyafter injection of 111In-DOTA-lanreotide(-150 MBq, left panel) and 1l1ln-OCT
(180 MBq, right panel) in carcinoid patient(Patient 13) showing recurrent jejunal carcinoid (arrow) as well as highly metasta-sized liver.
1934 THEJOURNALOFNUCLEARMEDICINE•Vol. 39 •No. 11 •November 1998
left panel right panel
FIGURE 7. SPECT studies after injectionof1111n-DOTA-lanreotide (~150 MBq). (A)
Patient 5 showed adenocarcinoma metastasis in left liver lobe (left panel: transverse image; right panel: CT superimposed ¡mage), and in patient withrecurrent pancreatic adenocarcinoma(left panel: transverse image; right panel:CT superimposed image). left panel
behavior for both radioligands (24). Consequently, it is mostprobable that from '"in-DOTA-lanreotide scintigraphy anddosimetry results the radiation dose for 90Y-DOTA-lanreotide
can be calculated. As shown, the mean radiation absorbed dosein the tumors amounted to 18 ±11 mGy/MBq (range 4.1-56mGy/MBq) of 90Y-DOTA-lanreotide. This suggests that an
effective tumor dose of 50 Gy could be achieved after 2-4treatments with 90Y-DOTA-lanreotide using a standardized
dose of 1 GBq per treatment injection in many of our patients.As opposed to normal organs, the mean dose to a tumor is about5 times higher than to the kidneys and 4.5 times higher than thespleen (Table 2 and 3). These human data obtained for thebiodistribution of " ' In-DOTA-lanreotide are in line with previous animal biodistribution studies performed with °Y-
DOTA-lanreotide, which concentrated in organs known tocontain high densities of SSTR (24).
In terms of tumor SSTR binding, all patients in this studywere advanced cancer patients. They all had undergone treatments with chemotherapy or radiation therapy, and all hadprogressive disease at the time of admission to diagnostic
right panel
scintigaphy with "'in-DOTA-lanreotide for possible therapy
with Y-DOTA-lanreotide. Previous treatment may have effects on SSTR expression and, thus, on tumor accumulation of111In-DOTA-lanreotide. For some patients, scintigraphy and
therapy evaluation of the tumor disease may be more effectiveearlier during the course of the disease, and receptor-mediatedtherapy may thus have a greater clinical potential in smallertumors/metastases. However, the problem of visualizingsmaller tumors by gamma scintigraphy is challenging and timeconsuming, making systematic tumor dosimetry hardly efficient. The use of an 86Y-labeled DOTA-lanreotide may help to
solve this problem to some extent, but this is limited to a fewPET centers in the world with the necessary infrastructure andexpertise to produce 86Y.
Opposite to Krenning et al.'s results (29), who reported nodifference in the biodistribution of mIn-DOTA-Tyr3-OCT and1"in-OCT, a significant difference was observed for ' "in-OCTand ' ' ' In-DOTA-lanreotide in our direct comparative dosimetry
studies (in the same patients). Not only was the tumor accumulation of '"In-DOTA-lanreotide significantly higher (2.25
TABLE 4Radioactivity in Selected Organs after Intravenous Application of either lndium-111 -DOTA-Lanreotide or lndium-111 -OCT (%ID ±s.d.)
Time(hr)136244872LiverDOTA-lanreotide6.50
±1.506.18±1.315.54
±1.093.27±0.651.86
±0.391.21±0.29SpleenOCT4.72
±0.38np3.61
±1.943.22±1.741.58±
0.631.31±0.60DOTA-lanreotide2.39
±0.442.25±0.451.99
±0.441.20±0.370.79
±0.270.48±0.20OCT2.41
±0.44np2.55
±0.282.97±0.971.26
±0.560.74±0.06KidneysDOTA-lanreotide4.07
±1.124.09±1.213.84±1.052.55
±0.681.46±0.410.91
±0.32OCT4.83
±1.53np4.54
±1.773.74±1.442.20
±1.441.00±0.48RemainderDOTA-lanreotide84.1
±2.772.2±3.865.3±4.644.6±4.930.0±3.920.0±3.6OCT62.7
±6.0np39.0
±17.018.9±11.88.5±2.07.0±3.2
The time between both scintigraphies was at least 4 wk. np = not performed.
INDIUM-!11-DOTA-L.ANREOT1DK•Virgolini et al. 1935
times), but also the whole-body elimination was slower, and thekidney retention was lower when compared with ' "in-OCT. In
our cohort of patients, we obtained a higher mean tumor uptakewith '"in-DOTA-lanreotide (0.085%ID/g, n = 23) as compared with a larger study with '"In-OCT in neuroendocrine
tumors (().()123%ID/g, n = 47) (30). The spleen retention of111In-DOTA-lanreotide, compared to mIn-OCT, was low and
did not increase over the first 24 hr postinjection. This wouldseem to suggest that a large proportion of the "'In-OCT
retention by the spleen is not receptor-mediated but rather aresult of "'in being lost from "'In-OCT and being incorpo
rated into the iron cycle. Finally, the data obtained in our study(Table 4) compare well with previously reported data for"'In-OCT (29.31), which confirm our results.
Therefore, the biodistribution of " ' In-DOTA-lanreotide, asopposed to "'In-OCT, suggests that 90Y-DOTA-lanreotide
should be more efficient and cost effective for receptor-mediated tumor therapy as opposed to wY-DOTA-Tyr3-OCT.
Moreover, the universal SSTR subtype recognition profile ofDOTA-lanreotide (24), in contrast to DOTA-Tyr3-OCT, allows
the conclusion that DOTA-lanreotide is suitable for a largernumber of tumor patients including intestinal adenocarcinomasthat are also visualized by I23I-VIP through its unique selective
binding to hSSTR3 (22). In fact, the distinct in vitro bindingbehavior of DOTA-lanreotide as compared with DOTA-Tyr3-OCT (inferior binding to SSTR3-5 of DOTA-Tyr3-OCT), aswell as of other SST-14 analogs and the unmodified "mothersubstance" lanreotide itself (24), supports the notion that
DOTA-lanreotide is a novel tumor diagnostic and therapeuticagent.
Remarkably, previous results have demonstrated that severalprimary tumors such as carcinoid tumors can be imaged by both
I-VIP and '"in-OCT, while the large majority of adenocarcinomas can only be visualized by 123I-VIP. Subsequent studies
have suggested that VIP interacts at the hSSTR3 subtype (22)which is, together with SSTR4, largely expressed in intestinaladenocarcinomas (19). Most interestingly, this study demonstrates that intestinal adenocarcinomas can also be imaged by
' ' In-DOTA-lanreotide (Fig. 7), most probably on the basis of
hSSTR3 (VIP, DOTA-lanreotide) and/or hSSTR4 (DOTA-lanreotide) recognition. As '"in-OCT binds only with moder
ate affinity to hSSTR3 and does not bind to hSSTR4 at all (24),the negative scintiscans in adenocarcinomas can be explainedby lack of ligand-receptor interactions. In the light of thespecific biodistribution and its high affinity for tumor cells (24),it is suggestive that the positive in vivo images obtained afterinjection of "'In-DOTA-lanreotide are due to receptor-ligand
interactions.
CONCLUSIONDOTA-lanreotide is a novel and promising peptide tracer
with a favorable dosimetry, unique biodistribution and highaffinity to a variety of tumor cells. It promises considerableadvantages over other SST analogs for tumor therapy.
ACKNOWLEDGMENTSThis study was supported in part by the "Hochschuljubiläums-
fonds" of the University of Vienna, as well as by the Austrian
National Bank (Jubiläumsfondsproject 6950). We are indebted tothe nurses, Elfi and team, Department of Nuclear Medicine, as wellas Milla and team, Department of Surgery. Furthermore, we wouldlike to thank all technologists involved in the acquisition procedures.
REFERENCES1. Lamberts SWJ. Bakker WH. Reubi JC. Krenning EP. Somatoslatin receptor imaging
in the localization of endocrine tumors. ,V Engl J Med 1990:323:1246-1249.2. Smith-Jones PM. Stolz B. Bruns C, et al. Gallium-67/gallium-68-DFO-octreotide: a
potential radiopharmaceutical for PET imaging of somatostatin receptor-positivetumors: synthesis and radiolabeling in vitro and preliminary in vivo studies. J NucÃMed 1994:35:317-325.
3. Anderson CJ, Pajeaun TS, Edwards WB. Sherman ELC. Rogers BE. Welch MJ. Invitro and in vivo evaluation of copper-64 octreotide conjugates. J NucÃMed1995:36:2315-2325.
4. Vallabhajosula S. Moyer BR. Lister-James J, et al. Preclinical evaluation of techne-tium-99m-labeled somatostatin receptor-binding peptides. J NucÃMed 1996:37:1016-
1022.5. Virgolini I. Angelberger P. Li S. et al. In vitro and in vivo studies of three radiolabelled
somatostatin analoges: I23l-octreotide (OCT), '23I-Tyr-3-OCT and '"In-DTPA-D-
Phe-l-OCT. Ear J NucÃMed 1996:23:1388-1399.
6. Virgolini I. Raderer M. Kurtaran A. et al. Vasoactive intestinal peptide (VIP) receptorimaging for the localisation of intestinal adenocarcinomas and endocrine tumors.N Engl J Med 1994:331:1116-1121.
7. Virgolini I. Raderer M, Kurtaran A. et al. Iodine-123-vasoactive intestinal peptide
(VIP) receptor scanning: update of imaging results in patients with adenocarcinomasand endocrine tumors of the gastrointestinal tract. NucÃMed Biol 1996:23:685-692.
8. Virgolini I. Kurtaran A. Raderer M. et al. Vasoactive intestinal peptide receptorscintigraphy. J NucÃMed 1995:36:1732-1739.
9. Raderer M. Becherer A, Kurtaran A. et al. Comparison of iodine-123-vasoactiveintestinal peptide receptor scintigraphy and indium-11 l-CYT-103 immunoscintigra-phy. J NucÃMed 1996:37:1480-1487.
10. Krenning EP, Kooij PP. Bakker WH. et al. Radiotherapy with a radiolabeledsomatostatin analogue. '"In-DTPA-D-Phel-octreotide. Ann N YAcad Sci 1994:733:496-506.
11. Krenning EP, Kooij PPM, Pauwels S, et al. Somatoslatin receptor: scintigraphy andradionuclide therapy. Digestion 1996:57(suppl):57-61.
12. Yamada Y, Post SR. Wang K, Tager HS. Bell GI, Seino S. Cloning and functionalcharacterization of a family of human and mouse somatostatin receptors expressed inbrain, gastrointestinal tract and kidney. Proc Nati Acad Sci USA 1992:89:251-255.
13. Yamada Y. Reisine S, Law SE, et al. Somatostatin receptors, an expanding genefamily: cloning and functional characterization of human SSTR3. a protein coupled toadenylyl cyclase. Mol Endocrinol 1992:6:2136-2142.
14. Yamada Y, Kagimoto S, Kubota A. et al. Cloning, functional expression andpharmacological characterization of a fourth (hSSTR4) and fifth (hSSTR5) humansomatostatin receptor subtypes. Biochem Biophys Res Commun 1993:195:844-852.
15. Yasuda K, Res-Domiano S, BrederCA. et al. Cloning of a novel somatostatin receptor.SST3, coupled to adenylate cyclase. J Biol Chem 1992:267:20422-20428.
16. Demchyschyn LL. Srikant CB. Sunahara RK, et al. Cloning and expression of a humansomatostatin-14-selective receptor variant (somatostatin receptor 4) located on chromosome 20. Mol Pharmacol 1993:43:894-901.
17. Corness JD, Demchyschyn LL. Seeman P. A human somatostatin receptor (SSTR3),located on chromosome 22, displays preferential affinity for somatostatin-14 likepeptides. FEBS 1993:321:279-284.
18. Rohrer L. Raulf F. Brans C, Buetter R. Hofstaedter F, Schule R. Cloning andcharacterization of a fourth human somatostatin receptor. Proc Nail Acad Sci USA1993:90:4196-4200.
19. Virgolini 1. Pangerl T. Bischof C. Smith-Jones P, Peck-Radosavljevic M. Somatostatinreceptor subtype expression in human tissues: a prediction for diagnosis and treatmentof cancer? Ear J Clin Invest 1997:27:645-647.
20. Reubi J, Schaer JC, Waser B, Mengod G. Expression and localization of somatostatinreceptor SSTR1, SSTR2 and SSTR3 mRNAs in primary human tumors using in situhybridization. Cancer Res 1994:54:3455-3459.
21. Virgolini I. Pangerl T. Bischof C. et al. Somatostatin (SST) and vasoactive intestinalpeptide (VIP) receptor (R) subtype gene expression [Abstract]. Eur J NucÃMed1996:29:1102(A).
22. Peck-Radosavljevic M, Yang O, Leimer M, et al. The somatostatin receptor subtype 3(SSTR) acts as a VIP-acceptor [Abstract]. Gastroenlerolagy 1998:114:1172.
23. Virgolini I, Yang Q. Li S. Angelberger P. et al. Cross-competition between vasoactiveintestinal peptide and somatostatin for binding to tumor cell membrane receptors.Cancer Res 1994:54:690-700.
24. Smith-Jones P. Bischof C. Leimer M, et al. DOTA-lanreotide: a novel tumordiagnostic and therapeutic somatostatin analog [Abstract]. J Nut-l Med 1998;39:223P.
25. Loevinger R. Budinger T, Watson E. MIRD primer for absorbed dose calculations.Reston, VA: Society of Nuclear Medicine; 1988.
26. Stabin MG. MIRDOSE. Personal computer software for internal dose assessment innuclear medicine. J NucÃMed 1996:37:538-546.
27. Johansson L, Mattson S, Nosslin B, Svegbom SR. Effective dose from radiopharma-ceuticals. Eur J NucÃMed 1993:19:933-938.
28. Reubi JC. In vitro identification of vasoactive peptide receptors in human tumors:implications for tumor imaging. J NucÃMed 1995:36:1846-1853.
29. Krenning EP. Bakker WH, Kwekkeboom DJ, et al. Biodistribution of a new chelatedsomatostatin analogue, indium-11 l-DOTA-D-Phe-l-Tyr-3-octreotide. Comparisonwith indium-111-DTPA-D-Phe-1-octreotide in humans [Abstract]. J NucÃMed 1997;
38:103P.30. Krenning Ep, Kwekkeboom DJ, Bakker WH, et al. Somatostatin receptor scintigraphy
with indium-111-DTPA-D-Phe-l and iodine-123-Tyr-3-octreotide: the Rotterdamexperience with more than 1000 patients. Eur I NucÃMed 1993:20:716-731.
31. Baje M, Palmer J, Ohlsson T, Edenbrandt L. Distribution and dosimetry of '"In-
DTPA-D-Phe-1-octreotide in man assessed by whole body scintigraphy. Acta Radiology 1994;35:53-57.
1936 THEJOURNALOFNUCLEARMEDICINE•Vol. 39 •No. 11 •November 1998