in People with Dementia Dr. Suzanne Timmons, Clinical Lead ...
Transcript of in People with Dementia Dr. Suzanne Timmons, Clinical Lead ...
National Clinical Guideline for the
Appropriate Prescribing of Psychotropic Medication
for non-cognitive symptoms
in People with Dementia
Dr. Suzanne Timmons, Clinical Lead
National Dementia Office
“The Health Service Executive will develop guidance
material on the appropriate management of medication for
people with dementia, and in particular on psychotropic
medication management, and make arrangements for this
material to be made available in all relevant settings,
including nursing homes”.
National Dementia Strategy Dec 2014
Background
Why was this guideline needed?
As many as 90% of people with dementia will experience distressing
non-cognitive symptoms at some stage throughout their disease
progression
Non-drug therapies (e.g. music therapy, pet therapy, environmental
measures) are generally advocated as first line treatments
Psychotropic medications have an important role to play in certain
specific situations (e.g. imminent risk of harm, severely distressing
agitation, psychosis, aggression)
However, psychotropic medications have some risks….
For every 100 people with dementia
treated with an antipsychotic:
<20 are likely to gain some benefit
>80 are likely to gain no benefit
1-2 people will have a stroke
1 person is likely to die
Risk - Benefit
Banerjee report 2009
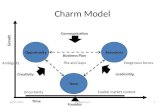
Organisational Capacity
Individual Professional
Capability
Communication and
Collaboration
Attitudes
Regulations and
Guidelines
Resources and access to services
Coping with the severity of illness /
behaviours
Skills
Knowledge
Communication and collaboration
within team and with family
Clarity of roles and responsibilities
Personal attitudes
Organisational and societal attitudes
Walsh KA, Dennehy R, Sinnott C, Browne J, Byrne S, McSharry J, Coughlan E, Timmons S.
Influences on Decision-Making Regarding Antipsychotic Prescribing in Nursing Home Residents With Dementia: A Systematic Review and Synthesis of
Qualitative Evidence. Journal of the American Medical Directors Association. 2017 Oct; 18(10):897-e1.
Walsh KA, Sinnott C, Fleming A, Mc Sharry J, Byrne S, Browne J, Timmons S.
Exploring Antipsychotic Prescribing Behaviors for Nursing Home Residents With Dementia: A Qualitative Study.
Journal of the American Medical Directors Association. 2018 Nov 1;19(11):948-58.
Scope of Guidelines
• Focus: non-cognitive symptoms • Target meds: Antipsychotics especially, but also benzodiazepines, Z
type hypnotics, antidepressants, anticonvulsants and cognitive-enhancing meds when used for non-cognitive symptoms
• Target users: Healthcare Professionals in any setting
• Goal: Appropriate prescribing (not necessarily reduced prescribing)
Process…
Expert stakeholder
group
Intellectual Disability
Sub-group
• People with Dementia
• Carers
• Advocacy groups
• Senior HSE staff
• Residential care reps
• Individual Experts
• HIQA
Development
Dec 17
Process…
Expert stakeholder
group
Literature review
Draft guidelines
Intellectual Disability
Sub-group
•People with
Dementia
•Carers
•Advocacy groups
•Senior HSE staff
•Residential care rep
• Individual Experts
•HIQA
Development
Dec 17
Process…
Expert stakeholder
group
Literature review
Draft guidelines
Expert peer review
External consultation
Guideline appraisal
Review stage Development
Dec 17 Feb-May 2019
Process…
Expert stakeholder
group
Literature review
Draft guidelines
Expert peer review
External consultation
Guideline appraisal
Dissemination
Education
Self-audit
Implementation Review stage Development
Dec 17 Late 2019 > Feb-May 2019
Prior to considering any psychotropic medication in a person with dementia, a
comprehensive assessment should be performed, by an appropriately trained
healthcare professional.
Non-pharmacological interventions should be used initially to treat non-
cognitive symptoms in a person with dementia, unless there is severe distress,
or an identifiable risk of harm to the person and/or others.
Psychotropic medication in general
If there is a positive response to treatment with antipsychotic medication, decision making about possible tapering of the medication should occur within 3 months, accompanied by a discussion with the person with dementia and/or their relevant Decision Supporter.
If a person with dementia is taking an adequate therapeutic dose of antipsychotic medication without clear clinical benefit, the medication should be tapered and stopped; where possible after discussion with the person and/or their relevant Decision Supporter.
GPP: There is little evidence that antipsychotics are effective in the treatment of certain
non-cognitive symptoms such as walking about, hoarding, fidgeting, inappropriate voiding,
verbal aggression, screaming, sexual disinhibition and repetitive actions. Therefore, any use
in the management of these symptoms needs to be particularly justified.
A full discussion with the person and/or their relevant Decision Supporter about the benefits and risks, including the increased risk of stroke, transient ischemic attack and mortality, should normally occur before antipsychotic medication is commenced.
SEVERE AGITATION PSYCHOSIS AGGRESSION
Benzodiazepines and Z type hypnotics
Due to the very limited evidence to support the use of Benzodiazepines in the management of non-cognitive symptoms in a person with dementia, and their significant adverse effects, they should be avoided for the treatment of non-cognitive symptoms, and usage strictly limited to the management of short term severe anxiety episodes. A personalised sleep management regimen may be considered for sleep disorders in a person with dementia. Melatonin should not be used for sleep disorders in people with dementia.
GPP: There are no studies of Z type hypnotics for sleep disorders in people with dementia. Due to their significant side effects, if Z type medications are considered, it should be for the shortest period possible (or as specified by medication license).
(https://www.hse.ie/eng/about/who/cspd/ncps/medicines-management/bzra-for-anxiety-insomnia/bzraguidancemmpfeb18.pdf)
•US: 33% reduction in antipsychotics in residential care from 2012 to 2017
•UK: 50% reduction from 2005 to 2015
•Hospitals: 52% reduction from 2008-2011
National initiatives elsewhere
•Training and support intervention reduced antipsychotic use by 19%, without worsening behavioural symptoms, and sustained for 12 months.
UK: Large RCT in NHs
•Reduced prn benzodiazepines from 40 to just nine residents at six weeks, maintained over many months (while recorded).
• Reduced prn hypnotics from 18 to zero, and regular from 25 to 19.
New procedure: initial trials of psychosocial interventions
•Education sessions and new tool regular antipsychotic reduced from 44% to 36%, and prn psychotropics also decreased.
Feasibility study of complex
intervention
Can we change things??
References
• National Dementia Strategy: Department of Health. (2014). The Irish National Dementia Strategy. Available at:
https://health.gov.ie/wp-content/uploads/2014/12/30115-National-Dementia-Strategy-Eng.pdf
• Prof. Sube Banerjee report 2009:The use of antipsychotic medication for people with dementia: time for action.
• Irish National Audit of Dementia: de Siún, A., O’Shea, E., Timmons, S., McArdle, D., Gibbons, P., O’Neill, D., Kennelly, S.P.
& Gallagher, P. (2014). Irish National Audit of Dementia Care in Acute Hospitals. Cork.
• Northern Ireland Audit of Dementia: O’Shea, E., Manning, E., Ross, E., McErlean, S. and Timmons, S. (2015). Northern
Ireland audit of dementia care in Acute Hospitals. Cork.
• Residential care prevalence: Bermingham, M., Leen, A., Walsh, K., O'Sullivan, D., O'Mahony, D., & Byrne, S. (2017). Use of
anti-psychotic agents in Irish long term care residents with dementia. In Pharmacoepidemiology and Drug Safety (Vol. 26,
pp. 5-5).
• Walsh KA, Dennehy R, Sinnott C, …., Timmons S. Influences on Decision-Making Regarding Antipsychotic Prescribing in
Nursing Home Residents With Dementia: A Systematic Review and Synthesis of Qualitative Evidence. Journal of the
American Medical Directors Association. 2017 Oct; 18(10):897-e1.
• Walsh KA, Sinnott C, Fleming A, Mc Sharry J, Byrne S, Browne J, Timmons S. Exploring Antipsychotic Prescribing
Behaviors for Nursing Home Residents With Dementia: A Qualitative Study. Journal of the American Medical Directors
Association. 2018 Nov 1;19(11):948-58.
• USA antipsychotic reduction: Gurwitz, J.H., Bonner, A. and Berwick, D.M. (2017). Reducing excessive use of antipsychotic
agents in nursing homes. Jama, 318(2), pp.118-119.
• UK overall antipsychotic reduction: Donegan, K., Fox, N., Black, N., Livingston, G., Banerjee, S., & Burns, A. (2017). Trends
in diagnosis and treatment for people with dementia in the UK from 2005 to 2015: a longitudinal retrospective cohort
study. The Lancet Public Health, 2(3), e149-e156.
• UK hospital antipsychotic reduction: Royal College of Psychiatrists (2013). National Audit of Dementia care in general
hospitals 2012-13: Second round audit report and update. London: HQIP.
• UK RCT in NH: Fossey, J., Ballard, C., Juszczak, E., James, I., Alder, N., Jacoby, R., et al. 2006. Effect of enhanced
psychosocial care on antipsychotic use in nursing home residents with severe dementia: cluster randomised trial. BMJ;
332:756
National Dementia Office,
Services for Older People, Social Care Division,
HSE, Unit 6, Central Business Park, Clonminch,
Tullamore, Co Offaly
Eircode: R35 TH92
Office: 057 9318451
Email: [email protected] or
UnderstandTogether.ie