Implementing Value-Based Sustainable Behavioral Health in Patient-Centered Medical Homes: Beyond the...
-
Upload
christopher-mcdonald -
Category
Documents
-
view
218 -
download
1
Transcript of Implementing Value-Based Sustainable Behavioral Health in Patient-Centered Medical Homes: Beyond the...
Implementing Value-Based Sustainable Behavioral Health in Patient-Centered Medical Homes:
Beyond the Co-Located Generalist Model
Rodger Kessler, PhDRoger Kathol, MDFrank deGruy, MD
Collaborative Family Healthcare Association 17th Annual ConferenceOctober 15-17, 2015 Portland, Oregon U.S.A.
Session # D5a October 17, 2015
Rodger Kessler has no relevant financial relationships or conflicts of interest.
Frank deGruy has no relevant financial relationships or conflicts of interest
Cartesian Solutions, Inc.™
Employment, Direct Relationship Consulting--Direct Relationship
Ownership--Direct Relationship
Case Management Society of America
Chief Medical Office/Board Advisor
Faculty Disclosure
Roger Kathol, M.D.
Learning Objectives
At the conclusion of this session, the participant will be able to:
• List three principles that lead to the successful integration of behavioral healthcare into primary care.
• Identify two common errors in created integrated practices.
• Discuss how the financing structure affects the prospects for successful integration.
Learning Assessment
• We will attempt to answer questions at the end of this presentation.
• In order for this session to qualify for CE credit, it must be evaluated. Please complete an evaluation form at the end of the session.
Introduction
• We know more than we do. There’s lots of room for improvement.
• This is an expensive problem, and addressing it will pay for itself.
• There’s mounting pressure to address this problem.
• It requires changing some long held beliefs
The Problem
• A very small minority of patients with behavioral problems are identified & effectively treated.
• Most PC practices are already overextended.• Most PC practices don’t use evidence-based care.• Most don’t have primary care trained BHC on staff.• Savings don’t accrue to the PC clinic, making this locally
expensive.• Referral out doesn’t work.• Hiring the least expensive BH also professionals doesn’t work.• Resources aren’t matched to problems.
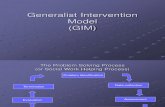
Implementing Value-Based Sustainable BH in PCMHs
(The Business Case)
Cartesian Solutions, Inc.™ ©
Roger Kathol, M.D.President, Cartesian Solutions, Inc.™
Adjunct Professor, University of Minnesota, Minneapolis, MN([email protected])
Cartesian Solutions, Inc.™ ©
Post-ACA Healthcare
3.Providers
Med Home
1.Purchasers
Triple Aim: Better Health Care, Better Outcomes, Lower Cost
--Vendors--Organizations
--Regulators--BH “Resources”
Med
Med
--adapted from Kathol & Gatteau, Healing Body AND Mind, 2007
Body
PublicPrivate
BHBH Home
2.Fund
Distributors
Accountable Care Organization
(Mind?)MindBH
3.2.
Clinically Integrated Network
Network IT System, Team Culture, Care Coordination, and Administrative Oversight
Medical Home
Specialty ClinicsHospitals
Ancillary Services
Contracted Vendors
--BH -- Pharmacy -- Lab, X-ray -- Other Cartesian Solutions, Inc.™ ©
Cartesian Solutions, Inc.™ ©
Perceived Value of Separate BH System
• Protects BH funds• Maintains BH autonomy• Retains independent decision
making power• Safeguards privacy• Provides better BH care
Cartesian Solutions, Inc.™ ©
Reality of Separate BH System
• Protects funds greater BH losses during housing bubble, state budget shortfalls, sequestration
• BH autonomy care fragmentation• Decision making insular; parochial to health• Privacy stigma; poor health outcomes• Better care 75% with BH illness receive no
treatment; 13-25 years shorter survival
Seventy-five Percent of BH Patients Are Seen in the Medical Setting
Medical Outpatients
Medical Setting
BH Patients Seen in the BH Sector (25%)
Medical Inpatients
Health Complexity
Chronic Medical Illnesses
BH Patients Seen Primarily or Only in the Medical Sector (75%)
95% BH Providers
Mental Health Sector
Cartesian Solutions, Inc.™ ©
Cartesian Solutions, Inc.™ ©
Health and Cost Impact of Comorbidity & Integrated Care
All Insured $2,920 15% Arthritis $5,220 6.6% 36% $10,710 94% Asthma $3,730 5.9% 35% $10,030 169% Cancer $11,650 4.3% 37% $18,870 62% Diabetes $5,480 8.9% 30% $12,280 124% CHF $9,770 1.3% 40% $17,200 76% Migraine $4,340 8.2% 43% $10,810 149% COPD $3,840 8.2% 38% $10,980 186%
Cartesian Solutions, Inc.™--consolidated health plan claims data
Illness Prevalence
% with Comorbid BH Condition*
Annual Cost with BH Condition
Annual Cost of Care
% Increase with BHl Condition
Patient Groups
*Approximately 10% receive evidence-based BH condition treatment
Cartesian Solutions, Inc.™ ©
Claims Expenditures for Patients With and Without BHCondition Service Use
7,5758,201
2,649
7,284
– Thomas et al, Psych Serv 56:1394-1401, 2005
7,847
5,732
BH Transition Options--The Challenge
Health Outcomes Cost Outcomes
1. Do Nothing
• Poor BH access• Retarded medical illness
improvement due to untreated BH comorbidity
• Unfavorable BH finances• Comorbid medical patients: 1 day longer
ALOS, >$6M for sitters, ~30% higher 30-day readmissions; ~$22M+ in extra service delivery costs
2. Buy Traditional
BH
• BH access• Small impact on medical sector
outcomes
• More unfavorable BH finances• Similar cost outcomes to above since
value-added BH not possible in medical setting
3. Build BH into Medical
• BH access in medical setting• Medical/BH provider
communication; patient satisfaction
• inpatient and outpatient care coordination and medical and BH outcomes
• Better payment for BH services from medical benefits
• Gap closure on ALOS, sitter use, 30-day readmissions, cost/net margin for general medical patients with BH comorbidity
Cartesian Solutions, Inc.™ ©
Cartesian Solutions, Inc.™ ©
The Transition to Non-Traditional BH Care and Care Support
3.Med/BH
Med Home
1.Purchasers
Health CareOutcome Change
--Vendors--Organizations
--Regulators
Med/BH
Body
PublicPrivate
BH
2.Fund
Distributors
Accountable Care Organization
Mind2. contracting for BH services as part of medical benefits; 3. BH clinicians part of medical provider network; Patients--integrated medical and BH services
Referral
Medical Practice
Behavioral Practice
Medical Practice
BHBehavioral
PracticeMed
Medical & Behavioral Practice
Model 1: “Cross-Referral”
Model 2: “Bidirectional”
Model 3 “Integrated”
Patient sorting
(75% of BH Patients)
(75% of BH Patients)
Specialty BH Setting(10% of BH Patients)
(90% of BH Patients)
Manderscheid & Kathol, AIM:160, 61-65, 2014 Cartesian Solutions, Inc.™ ©
The Problem
• A very small minority of patients with behavioral problems are identified & effectively treated.
• Most PC practices are already overextended.• Most PC practices don’t use evidence-based care.• Most don’t have BHC on staff.• Savings don’t accrue to the PC clinic, making this locally
expensive.• Referral out doesn’t work.• Hiring the least expensive BH also professionals doesn’t work.• Resources aren’t matched to problems.
Recommendations
• Reconsider which services for which patients.– First casefinding efforts for high-risk, high-cost
patients. Comorbidity, high utilizers, rather than universal screening.
– Deploy resources in a fully integrated fashion. More on this later.
– Employ BH clinicians with the skill and training to handle the most difficult problems.
– Stepped care.
Seven Principles of Integrated Care 1
Make BH clinicians part of medical team. Pay for them with medical benefits.
Seven Principles of Integrated Care 2
Use a common EHR, registries, and claims data. One panel. Pull complex patients from that registry.
Seven Principles of Integrated Care 3
If possible, create teams, or subteams. Construct teams with skillsets that match problems in subpopulations.
Seven Principles of Integrated Care 4
Match levels of clinicians to severity of problems, then step care up if improvement doesn’t occur.
Seven Principles of Integrated Care 5
Prospectively define desired health outcomes and treat to target, evaluating frequently.
Seven Principles of Integrated Care 6
Use evidence-based algorithms and protocols as standard of care.
Implications
• Single budget, single source of accountability for overall health.• Targeted screening, stepped care—biggest steps for efficiency.• Whole team—whole person care. Avoids mishaps of fragmented
care (ED, etc.)• Effective clinicians are less expensive in the long run.• Biggest savings with most expensive patients.• Evidence-based care best chance of improving.• Care managers heal fragmentation.
The change in care model
• Behavioral case-finding and treatment resources focus on patients with chronic medical conditions, eg, diabetes mellitus, asthma, coronary artery disease, and those patients with high health care costs, rather than conduct universal screening of all patients for behavioral problems
The change in care model
• Treatment resources should be deployed in a fully integrated fashion rather than collocated practices providing specialty mental health and substance use care
The change in clinical focus
• Behavioral clinicians involved in care and PCMH care support need training and experience to deliver evidence-based behavioral treatments proven effective at improving targeted conditions
Summary• Payment needs to be integrated or PCMH targets cannot
be met• EHR screening is used to identify high-need, high-cost,
and “complex” patients • Team care to reduce both behavioral and medical issues• Behavioral clinicians need to have expertise to provide evidence-based care• Use limited resources to focus on patients with
expensive, reversible conditions• This is not behavioral health care, it is behavioral care. • Trained cross-disciplinary care managers need to
coordinate care across the medical-behavioral continuum