Implant News
-
Upload
maxisurgeon -
Category
Documents
-
view
191 -
download
0
Transcript of Implant News
Why CT Scans Are Already the Standard of CareDr. Alan A. Winter
“It is a dentist’s responsibility to provide reasonable and ordinary care, skill, and
diligence as other dentists in good standing in the same neighborhood provide, and
deviations from these standards that produce untoward results constitutes malpractice.”
These words were cobbled together from multiple definitions on standard of care. They
are not to be construed as legal “gospel” but to provoke discussion regarding which
treatment options we choose to present to patients and those we avoid without even
presenting them for consideration.
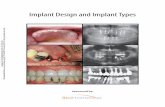
Fig. 1 - 60-year old patient
with existing bridge desires
implants.
Fig. 2 - Bicortical ridge.
For instance, what is the standard of care when replacing a singlemissing tooth? What if a dentist has never inserted an implant or prefers(and likes) fabricating three-unit bridges? Does an implant still have to bepresented as an option to the patient (regardless if the adjacent teeth arepristine or already have been restored)?
Sinus GraftsDo we avoid sinus grafts as a treatment option which are predictable
and would solve the patient’s need for posterior maxillary implants or do werecommend some alternative restoration or surgery because we do not per-form sinus grafts? Do we use only one type or length/width of dental implantfor all clinical situations while knowing that a larger inventory or anotherimplant system would produce better results?
Do we eyeball every implant insertion when a surgical guide may aid inthe placement? Do we choose to limit decision making to conventional two-dimensional dental/digital X-rays and/or panoramic images knowing that thereis a 3-D CT scanner around the corner or miles away (but still in reasonabletraveling distance) that would enable a better treatment plan, and a moreprecise and safer implant placement?
“In-House”Lumped together, each practitioner needs to ask and answer the
following question, “Do we always do what is best for the patient even if itmeans referring the patient elsewhere for a part or all of the service, or dowe base all treatment options on keeping treatment ‘in house’?” And is thetreatment “in house” equivalent to what the patient could reasonably receiveelsewhere in the local dental community?
LegalityThe trouble is, and the law says, that we have a greater responsibility
than providing the best dental care we can possibly give our patients. Weneed to make them aware of the best possible care that exists in the localcommunity when compared to services provided in our offices. That is notanything most of us are comfortable doing, yet that’s what “standard ofcare” is all about.
Case 1A sixty-year old female [Fig. 1] patient presents to her dentist in
good heath with the chief complaint that she would like an anterior bridge
removed and implants inserted so she could have “individual teeth.” Her hygiene was impeccable, and she nolonger wanted to use a floss threader now that she was aware of dental implants and their proven success.From a practice management perspective, is it best to remove the existing bridge before referring the patientto the surgeon for implant placement? Or, should the dentist (who does not insert implants) refer the patient
July/August 2007
Vol. 9 No. 4
Implant News & Views“Keeping you up-to-date on implant dentistry”
Page 2 Implant News & Views
for an implant consult before proceeding with treatment? What would be the standard of care in this case?And what radiographic information is needed to make a decision? Is the dental X-ray in Fig. 1 adequate todetermine the best course of treatment?
In this case, the dentist referred the patient to a dental CT lab, in order to make certain implantscould be inserted before he removed the existing prosthesis. Fig. 2 reveals that the edentulous ridge wasbi-cortical and without cancellous bone. The surgeon felt this site was not a good candidate for implantplacement and used the CT images to explain why to the patient. Furthermore, the surgeon felt that anysort of ridge augmentation would be compromised and the chance existed that the resulting esthetics wouldbe unsatisfactory. Here, the CT scan provided the opportunity “not” to attempt a case that could haveyielded disastrous results.
Consider, for a moment, the dilemma if the dentist had already removed the bridge and fabricated anacrylic provisional restoration. Who would pay for final prosthesis after the surgeon declined to performsurgery?
Case 2 - Panoramic ViewsIn the next case, let’s explore how panoramic images skew treatment decisions. Fig. 3 demonstrates
a panoramic view in SimPlant™. The treatment plan was to insert two implants where #s 14 and 15 weremissing. Options included inserting the appropriate-sized implants into the available bone, using an os-teotome technique to insert longer implants, perform a sinus graft and wait for healing, or insert implants atthe time of surgery.
Fig. 3 - Panoramic image appears to indicate an adequate amount
of bone under the left maxillary sinus.
Since enough bone appears un-der the sinus to use osteototmes, let’sexplore what would happen if only thistwo-dimensional panoramic image wasused as opposed to a 3-D CT scan. Fig.4 reveals more information that wouldhelp the surgeon insert the implant.What appeared on the panoramic viewin site #15 to be at least 10mm of bone,measures only 4mm from the center ofthe crest, and a polyp is noted on themedial wall of the sinus that was hiddenfrom view. In actuality, thick buccal bonegave the impression that enough bonewas available to (easily) insert an im-plant without the need for more infor-mation. It is not in the scope of thispaper to discuss treatment, but whatsurgeon wouldn’t want this informationin order to provide the best possible care?
Going the extra mile for more in-formation can no longer be considered a“standard of excellence” that separatesone clinician from another. Getting allthe information necessary – in this case,3-D imaging - to make an informed deci-sion should not be glossed over by themask of “judgment” or leaving the “op-tion” up to the patient. There are nooptions to standard of care.
Post-SurgicalWhat about using 3-D imaging as
a post-surgical tool? In Fig. 5, we note
Fig. 4 - Cross-section reveals a different perspective indicating
the panoramic view was an illusion of a thick buccal wall of bone.The reality is that only about 4mm of bone exists under the floor
of the sinus.
that a graft had been performed in the maxillary left sinus. The height from the alveolar crest measuresalmost 20 millimeters. Does a panoramic view provide enough information to proceed with implant place-ment? Consider a 3-D transaxial image of the same site [Fig. 6].
Imagine how quickly the bur would perforate the thin alveolar crest, puncture the sinus membrane,and either embed into the graft or dislodge it from the lateral sinus wall. How would it be explained that the
Page 3Implant News & Views
of the mandibular nerve that was not viewable on the panoramic image but was easily visible on the cross-sectional view.
loose bone graft “rattling” around in the sinus could have been avoided had the surgeon prescribed that thepatient get a post-op CT scan prior to surgery? All too often, dentists feel obligated - especially when itcomes to radiographic imaging - to make decisions based on the patients funds, insurance reimbursements,or simply thinking that 2-D X-rays are adequate for the intended treatment. What is the radiographicstandard of care for any augmented site after bone grafts have been performed?
Fig. 5 - A panoramic image reveals an adequate amount of bone
in the maxillary left after sinus graft surgery.
Fig. 6
Case 3As a
last case, con-sider the fol-lowing. A den-tist inserts animplant in the#30 site. Pre-op analysis in-dicated thatenough boneexisted abovethe nerve so
that a 3-D CT scan was not recommended [fig. 7]. The surgery was unevent-ful, yet when the local anesthetic wore off, the patient complained of continuedparesthesia. Since there was no apparent reason for the lingering paresthesia,the dentist sent the patient for a post-op CT scan.
Figure 8 demonstrates that the implant was touching an aberrant branch
Fig. 7 - A panoramic view indicates adequate bone between the
apex of the implant and the mandibular nerve.
Fig. 8 - Sagittal image of implant #30 site indicates the nerve
touching an aberrant branch of the mandibular nerve.
SummaryIt is difficult to identify when a
procedure or technique transforms froma standard of excellence into the stan-dard of care. And while it may be equallydifficult to know when a new technology,technique, product, or therapy emergesas a part of many of the local dental opin-ion makers’ armamentarium, there is a timewhen a dentist can no longer say, “I knowabout this or that, but I choose not torecommend it for my patients.”
Furthermore, one of the reasonsfor taking a 3-D CT scan is not becausesomething is suspected that may inter-fere or alter the patient’s treatment.Rather, CT scans should be recommendedfor the unexpected, to make certain we’renot missing anything even though for allappearances, the 2-D X-rays look “nor-mal.”
At the time of this writing, a promi-nent California lawyer is consulting withmajor dental insurance companies to cre-ate a new “Informed Refusal” document.This document suggests that dentists notonly recommend 3-D imaging for complexcases, but have the patient sign a docu-ment should they refuse to do so. The converse may also exist: will it be malpractice not to make therecommendation and subsequently not need to provide the “Informed Refusal” for the patient’s signature.You be the judge.
Page 4Implant News & Views
Alan A. Winter, DDS is a board certified periodontist and Associate Professor of
Clinical Dentistry in the Department of Periodontics and Implantology at NYU. He
practices periodontics in Manhattan, NY. Dr. Winter and his partner Dr. Alan S. Pollack
founded APW Dental Imaging, now called I-dontics, LLC that owns/operates eleven
dental CT scan centers in four states - NY, NJ, GA, and FL. He can be contacted at 212-
838-0940, cell: 201-213-4438 or [email protected].
Subscribe to
Implant News & Views1.888.385.1535
or visitwww.implantnewsandviews.com
call us about quantity discounts