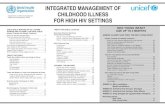
IMCI SEssion 4 - Main Symptoms
Transcript of IMCI SEssion 4 - Main Symptoms

1
Main Symptoms- cough or difficult breathing- diarrhea- fever- ear problems
Session 4

2
Learning Objectives
By the end of this session, the students will be able to:(1) recall the anatomy and pathophysiology;
(2) recognize the symptoms and signs;
(3) assess and classify symptoms and signs;
(4) identify the correct treatment and when to refer;
(5) provide counseling; and
(6) specify necessary follow-up care

3
Cough or Difficult Breathing
Session 4-a

4
•Nasal passages •Windpipe or trachea •Lungs
Parts of the Respiratory System

5
Inside the alveolus

6
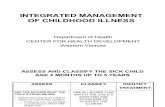
ASK: Does the child have cough or difficult breathing?
If YES
IF YES, ASK:•For how long?
LOOK, LISTEN, FEEL:•Count the breaths in one minute•Look for chest indrawing•Look and listen for stridor
Child must be calm
If the child is: Fast breathing is: 2 mos – 12 mos. 50 breaths/min or more 12 mos – 5 yrs 40 breaths/min or more
Classify child’s illness using the color-coded classification table for cough or difficult breathing
If NO
Ask about next main
symptoms:diarrhea, fever, ear problems
Cough or Difficult Breathing

7
Video of child with chest indrawing

8
Video of child with stridor

9
Cough or Difficult Breathing
•Any general danger sign or•Chest indrawing or•Stridor in a calm child
SEVERE PNEUMONIA OR VERY SEVERE DISEASE
Give first dose of an appropriate antibioticRefer URGENTLY to hospital
•Fast breathing PNEUMONIA
Give an appropriate oral antibiotic for 5 daysSoothe the throat and relieve the cough with a safe remedyAdvise mother when to return immediatelyFollow-up in 2 days
No signs of pneumonia or very severe disease
NO PNEUMONIA: COUGH OR COLD
If coughing > 30 days, refer for assessmentSoothe the throat and relieve the cough with a safe remedyAdvise mother when to return immediatelyFollow-up in 5 days if not improving
SIGNS CLASSIFY AS IDENTIFY TREATMENT

10
Treatment
Soothe the Throat, Relieve the Cough with a Safe RemedySafe remedies to recommend:
Breastmilk for exclusively breastfed infant
tamarind, calamansi, ginger
Harmful remedies to discourage:Codeine cough syrupOther cough syrupsOral and nasal decongestants

11
Treatment for Pneumonia or Very Severe Disease
CotrimoxazoleGive 2 times daily
for 5 days
AmoxycillinGive 3 times daily
for 5 days
Age orWeight
Adulttab.
80mgTMP
400 mgSMX
Syrup40 mgTMP
200 mgSMX
Tablet
250 mg
Syrup
125mg/ 5 ml
2 -12 mos 1/2 5.0 ml. 1/2 5.0 ml
12mos-5yrs 1 7.5 ml 1 10 ml.

12
Vitamin A Supplementationfor Severe Pneumonia or Very Severe Disease
Vitamin A CapsuleAge
100,000 IU 200,000 IU
6 to 12 mos. 1 capsule ½ capsule
12 mos-5 yrs 2 capsules 1 capsule

13
DIARRHEA
Session 4-b

14
Anatomy of the Gastrointestinal System

15
DiarrheaFor ALL sick children ask the mother about the child’s problem, check for general danger signs,ask about cough or difficult breathing and then
ASK: DOES THE CHILD HAVE DIARRHOEA?
If NO If YES
Does the child have diarrhoea?
IF YES, ASK: LOOK, LISTEN, FEEL:œFor how long? œLook at the child’s general condition. Is the child:œIs there blood in thestool Lethargic or unconscious? Restless or irritable?œLook for sunken eyes.
œOffer the child fluid. Is the child: Not able to drink or drinking poorly? Drinking eagerly, thirsty?
œPinch the skin of the abdomen. Does it go back: Very slowly (longer than 2 seconds)? Slowly?
CLASSIFY the child’s illness using the colour-coded classification tables for diarrhoea.
Then ASK about the next main symptoms: fever, ear problem, and CHECK for malnutrition andanaemia, immunization status and for other problems.
Classify DIARRHOEA

16
DIARRHEA
Does the child have diarrhea?IF YES, ASK:For how long?Is there blood in the stool?
LOOK, LISTEN, FEEL: Look at the child’s general
condition, is the child: Lethargic or unconscious? Restless or irritable? Look for sunken eyes Offer the child fluid. Is the
child: Not able to drink or drinking
poorly? Drinking eagerly, thirsty?
Pinch the skin of the abdomenDoes it go back: Very slowly (> than 2 secs)?Slowly?

17
Video of a child with sunken eyes

18
Video of Skin Pinching

19
Two of the following signs:Lethargic or unconsciousSunken eyesNot able to drink or drinking poorlySkin pinch goes back very slowly
SEVERE
DEHYDRATION
If child has no other severe classification:
— Give fluid for severe dehydration (Plan C).
OR
If child also has another severe classification:
— Refer URGENTLY to hospital with mother giving frequent sips of ORS on the way.
Advise the mother to continue breastfeeding
If child is 2 years or older and there is cholera in your area, give antibiotic for cholera.
Two of the following signs:Restless, irritableSunken eyesDrinks eagerly, thirstySkin pinch goes back slowly
SOME
DEHYDRATION
Give fluid and food for some dehydration (Plan B).If child also has a severe classification:
— Refer URGENTLY to hospital with mother
giving frequent sips of ORS on the way.
Advise the mother to continue breastfeedingAdvise mother when to return immediately.Follow-up in 5 days if not improving.
Not enough signs to
classify as some or
severe dehydration. NO DEHYDRATION
Give fluid and food to treat diarrhoea at home (Plan A).
Advise mother when to return immediately.
Follow-up in 5 days if not improving.
CLASSIFICATION TABLE FOR DEHYDRATION
SIGNS CLASSIFY ASIDENTIFY TREATMENT
(Urgent pre-referral treatments are in bold print.)

20
No Dehydration

21
Some Dehydration

22
Severe Dehydration

23
Tell the Mother:
(a) Breastfeed frequently and longer for each feed.
(b) If the child is exclusively breastfed, give ORS or clean water in addition to breastmilk.
(c) If the child is NOT exclusively breastfed, give 1 or more of the following:ORSFood-based fluidsClean Water
No Dehydration

24
Treatment Plan A
Age Amount of Fluid Type of Fluid
< 2 yrs 50-100 ml (¼-½ cup) after each loose stool2-10 yrs 100-200 ml (½-1 cup) after each loose stool
ORS, rice water, yogurt, soup with salt
No Dehydration
• Give frequent small sips from a cup.
• If the child vomits, wait 10 minutes. Then continue, but more slowly.
• Continue giving extra fluids until the diarrhea stops.

25
Give frequent small sips from a cup. If the child vomits, wait 10 minutes. Then
continue, but more slowly. Continue giving extra fluids until the
diarrhea stops. Reassess after 4 hours and classify the
child for dehydration.
Some Dehydration

26
If the mother must leave before completing treatment:show her how to prepare the ORS solution at home.show her how much to give to finish the 4 hour treatment at homegive her enough ORS packets to complete rehydration.
Some Dehydration

27
Treatment Plan B (Determine amount of ORS to be given in 4 hours)
Age Up to 4 mos 4mos - 12mos 12mos – 2years 2 years – 5years
Some Dehydration
< 6kg 6 - < 10kg 10 - <12kg 12-19kg 200-400 400-700 700-900 900-1400
• The approximate amount of ORS can also be calculated by multiplying the child’s weight (in kg) by 75.
WEIGHT In ml

28
Severe Dehydration
Can you give Intravenous fluids (IV) immediately?

29
Severe Dehydration
Treatment Plan CTo treat severe dehydration (IV fluid: pLRS)
Age Initial Phase Subsequent Phase (30 ml/kg) (70 ml/kg)
Infants (<12 mos) 1 hour *5 hours
Older children 30 minutes* 2½ hours
*Repeat once if radial pulse is still very weak or imperceptible.

30
Reassess the child every 1-2 hours. If hydration status is not improving, give the IV drip more rapidly.
Also give ORS (5ml/kg/hr) as soon as the child can drink.
Reassess the infant after 6 hours & a child after 3 hours. Classify dehydration.
Severe Dehydration

31
If trained to use a nasogastric tube for
rehydration?
Severe Dehydration

32
Start hydration by tube (or mouth) with ORS solution. Give (20ml/kg/hr) for 6 hours. (Total of 120ml/kg)
Reassess the child every 2 hours.– If there is repeated vomiting or increasing abdominal
distention, give the fluid more slowly.– If hydration status is not improving after 3 hours, send
the child for IV therapy.
After 6 hours, reassess the child. Classify dehydration.
Severe Dehydration

33
Dehydration present SEVERE
PERSISTENT
DIARRHOEA
Treat dehydration before referral unless the child has another severe classification.Refer to hospital.
No dehydration PERSISTENT
DIARRHOEA
Advise the mother on feeding a child who has PERSISTENT DIARRHOEA.Follow-up in 5 days.
SIGNS CLASSIFY ASIDENTIFY TREATMENT
(Urgent pre-referral treatments are in bold print.)
CLASSIFICATION TABLE FOR PERSISTENT DIARRHEA

34
After 5 days: Ask: If the diarrhoea has NOT stopped (3 or more
stools) do a full reassessment, give the treatment, then refer to hospital.
If the diarrhoea has stopped (< 3 stools per day) Tell the mother to follow the usual feeding recommendations for the child’s age.
Persistent Diarrhea

35
Blood in the stool
DYSENTERY
Treat for 5 days with an oral antibiotic recommended for Shigella in your area.Follow-up in 2 days.
CLASSIFICATION TABLE FOR DYSENTERY
SIGNS CLASSIFY ASIDENTIFY TREATMENT
(Urgent pre-referral treatments are in bold print.)

36
After 2 days:Ask: if the child is dehydrated, treat hydration.
if the number of stools, amount of stools, fever, abdominal pain or eating is same or worse: Change to 2nd line antibiotics & give for 5 days. Advise to return in 2 days.
Dysentery

37
EXCEPTIONS:
If the child is less than 12 months old or was dehydrated on the 1st visit or had measles within the last 3 months. REFER TO HOSPITAL.
If fewer stools, less blood in stools, less fever, less abdominal pain & eating better, continue antibiotics.
Dysentery

38
Session 4-c
Fever

39
Assess FEVER
A child has the main symptom of fever if:
– the child has history of fever– the child feels hot– the child has an axillary temperature of
37.5 or above

40
Does the child have fever?(by history, or feels hot or temperature 37.5C and above)
Decide Malaria RiskAsk: Does the child live in a malaria area?
Has the child visited malaria area in the past 4 weeks?
If yes to either, obtain a blood smear.
Then Ask: For how long does the child has fever?
If >7 days, has the fever been present everyday?
Has the child had measles within the last 3 months?
Look and Feel: Look and feel for stiff neck. Look for runny nose
Look for signs of Measles:• Generalized rash.• One of these: cough, runny nose or
red eyes

41
Does the child have fever?(by history, or feels hot or temperature 37.5C and above)
If the child has measles now or within the last three months:
Look for mouth ulcers.– Are they deep and extensive?
Look for pus draining from the eye.
Look for clouding of the cornea.

42
Does the child have fever?(by history, or feels hot or temperature 37.5C and above)
Then Ask: Has the child had any bleeding
from the nose or gums or in the vomitus or stools?
Has the child had black vomitus or stools?
Has the child had abdominal pain?
Has the child been vomiting?
Look and Feel: Look for bleeding from nose or
gums.
Look for skin petechiae Feel for cold clammy extremities.
If none of the above ASK or LOOK and FEEL signs are present and the child is 6 months or older and fever present for more than 3 days.
Perform Torniquet Test.
Decide Dengue Risk: Yes or NoIf Dengue Risk:

43
Does the child have fever?(by history, or feels hot or temperature 37.5C and above)
Decide Malaria Risk:
If the child has measles now or within the last three months:
Decide Dengue Risk: Yes or No
If Dengue Risk:
Classify FEVER
Malaria Risk (including travel to malaria area)
No Malaria Risk

44
Deciding Malaria Risk
Malaria is caused by parasites in the blood called “plasmodia”– “Plasmodium falciparum”
Transmitted by Anopheles mosquito
Know the malaria risk in your areas.

45
Malaria Risk Areas
1. Palawan
2. Davao Oriental
3. Davao del Norte
4. Compostela Valley
5. Tawi-tawi
6. Sulu
7. Agusan del Sur
8. Mindoro Occidental
9. Kalinga Apayao
10. Agusan del Norte
11. Isabela
12. Cagayan
13. Quezon
14. Ifugao
15. Zamboanga del Sur
16. Bukidnon
17. Misamis Oriental
18. Quirino
19. Mountain Province
20. Basilan

46
Classify FEVER
Classify FEVER
Malaria Risk (including travel to malaria area)
No Malaria Risk
Malaria Risk Any general danger sign or Stiff Neck
VERY SEVERE FEBRILE DISEASE/MALARIA
Blood smear (+)If blood smear not done:NO runny nose and, NO measles, and NO other
causes of fever
MALARIA
Blood smear (-), orRunny nose, orMeasles orOther causes of fever.
FEVER:
MALARIA UNLIKELY
No Malaria Risk Any general danger sign or Stiff Neck
VERY SEVERE
FEBRILE DISEASE
No sign of very severe
febrile disease
FEVER:
NO MALARIA

47
Malaria Risk
Any general danger
sign or Stiff Neck
VERY SEVERE FEBRILE DISEASE
/MALARIA
Give first dose of Quinine (under medical supervision or if a hospital is not accessible withing 4 hours)Give first dose of appropriate antibiotics.Treat the child to prevent low blood sugar.Give one dose of Paracetamol in health center for
high fever (38.5C or above.)Send a blood smear with the patient.
Refer URGENTLY to a hospital.
Blood smear (+)If blood smear not
done:NO runny nose and, NO measles, and NO other causes of fever
MALARIA
Treat the child with an oral antimalarial.Give one dose of Paracetamol in health center for
high fever (38.5C or above.)Advise mother when to return immediately.Follow up in 2 days if fever persists.If the fever is present every day for more than 7 days, refer for assessment.

48
Malaria Risk
Blood smear
(-), or Runny nose,
or Measles or Other causes
of fever.
FEVER:
MALARIA UNLIKELY
Give one dose of Paracetamol in
health center for high fever (38.5C
or above.) Advise mother when to return
immediately. Follow up in 2 days if fever persists. If the fever is present every day for
more than 7 days, refer for
assessment.Treat other causes of fever.

49
TREAT THE CHILD: Antimalarial Agents
Give an Oral Antimalarial1st line Antibiotics: Chloroquine and Primaquine2nd line Antibiotics: Sulfadoxine and Pyrimethamine
If Chloroquine:The child should be watched closely for 30 minutes. If the child vomits, give another dose.
Itching is a possible side effect of the drug.
If Sulfadoxine and Pyrimethamine:Give single dose in health center.

50
Antimalarial AgentsCHLOROQUINE
Give for 3 days
PRIMAQUINE
Single dose for P.
falciparum
PRIMAQUINE
Daily for 14 days for P.
vivax
SULFADOXINE + PYRIMETHAMINE
Single dose
AGE Tablet (150mg base)
Tablet(15mg base)
Tablet(15mg base)
Tablet(500mg Sulfadoxine 25mg
Pyrimethamine)Day 1 Day 2 Day 3
2 months up to 5 months (4 - <7kg) ½ ½ ½ 1/4
5 months up to 12 months (7 - <10kg) ½ ½ ½ 1/2
12 months up to 3 years (10 - <14kg) 1 1 ½ 1/2 1/4 3/4
3 years up to 5 years (14 – 19kg) 1½ 1½ 1 3/4 1/2 1

51
TREAT THE CHILD: Antimalarial Agents
Chloroquine is given for 3 days.
Explain to the mother that itching is a possible side effect. It is NOT dangerous. The mother should continue to give the drug.

52
TREAT THE CHILD: Antimalarial Agents
If the species of malaria is identified through blood smear, give the following:
– P. falciparum – single dose Primaquine with the first dose of Chloroquine
– P. vivax – first dose of Primaquine with Chloroquine and give mother enough for one dose each day for the next 13 days.

53
TREAT THE CHILD: Antimalarial Agents
If you do not have the blood smear or you do not know which species of malaria is present, treat as P. falciparum.
Do not give Primaquine to children under 12 months of age.

54
TECHNICAL UPDATES: Antimalarial Agents
TECHNICAL BASIS: Artemisinin Based Combination TherapiesBased on available safety and efficacy data, the following therapeutic options are available and have potential for deployment (in prioritized order) if costs are not an issue: Arthemether – lumefantrine (Coarthem TM) Artesunate (3 days) + amodiaquine Artesunate (3 days) + SP in areas where SP remains high SP + Amodiaquine in areas where both SP and Amodiaquine remain high. This mainly limited to West Africa.

55
TECHNICAL UPDATES: Antimalarial Agents
Administer intramuscular antibiotic if the child cannot take an oral antibiotic
Quinine for severe malaria
Breastmilk or sugar to prevent low blood sugar.

56
Give an Intramuscular Antibiotic
A child may need an antibiotic before he leaves for the hospital, if he/she:– is not able to drink or breastfeed– vomits everything– has convulsions– is abnormally sleepy or difficult to awaken

57
Give an Intramuscular Antibiotic
Age or Weight CHLORAMPHENICOLDose: 40 mg/kg
Add 5 ml sterile water to vial containing 1000mg = 5.6 ml at 180mg/ml
2 – 4 months (4 - <6kg) 1 ml = 180 mg
4 – 9 months (6 - <8kg) 1.5 ml = 270 mg
9 – 12 months (8 -10 kg) 2 ml = 360 mg
1 – 3 years (10 - <14kg) 2.5 ml = 450 mg
3 – 5 years (14 – 19 kg) 3.5 ml = 630 mg

58
Give Quinine for Severe Malaria
Quinine is the preferred because it is rapidly effective.
Quinine is more safe and effective than intramuscular Chloroquine.
Possible side effects of Quinine injections are: sudden drop in blood pressure, dizziness, ringing in the ears and a sterile abscess.

59
Give Quinine for Severe Malaria
For children being referred with very severe febrile disease/Malaria:
– Give the 1st dose of IM Quinine and refer the child urgently to the hospital
If referral is not possible:– Give the 1st dose of IM Quinine– The child should remain lying down for 1 hour– Repeat the Quinine injection 4 to 8 hours later, and then every 12
hours until the child is able to take an oral antimalarial.– Do not continue Quinine injection for more than 1 week.– DO NOT GIVE QUININE TO A CHILD LESS THAN 4 MONTHS
OF AGE.

60
Give Quinine for Severe Malaria
Age or WeightINTRAMUSCULAR QUININE
300 mg/ml (In 2 ml ampules)
4 months – 12 months
(6 - <10kg)0.3 ml
12 months – 2 years
(10 - <12kg)0.4 ml
2 – 3 years
(12 - <14kg)0.5 ml
3 – 5 years (14 – 19kg) 0.6 ml

61
TREAT THE CHILD: To Prevent Low Blood Sugar
If the child is able to breastfeed:– Ask the mother to breastfeed the child.
If the child is not able to breastfeed but is able to swallow:– Give expressed breastmilk or breastmilk
substitute. If neither is available, give sugar water. Give 30 – 50 ml of milk or sugar water before departure.

62
TREAT THE CHILD: To Prevent Low Blood Sugar
To make Sugar Water:
Dissolve 4 level teaspoons of sugar (20 grams)
in a 200 ml cup of clean water.
If the child is not able to swallow:– Give 50 ml of sugar water by nasogastric tube.

63
TREAT THE CHILD: Paracetamol for High Fever
PARACETAMOL
Age or WeightTablet
(500mg)
Syrup
(120mg/5ml)
2 months up to 3 years (4 - <14kg)
1/4 5ml (1 tsp)
3 years up to 5 years (14 – 19 kg)
1/2 10 ml (2 tsp)

64
No Malaria Risk
Any general danger sign or Stiff Neck
VERY SEVERE
FEBRILE DISEASE
Give first dose of appropriate antibiotics.Treat the child to prevent low blood sugar.Give one dose of Paracetamol in health center for high fever (38.5C or above.)Refer URGENTLY to a hospital.
No sign of very severe febrile disease
FEVER:
NO MALARIA
Give one dose of Paracetamol in health center for high fever (38.5C or above.)Advise mother when to return immediately.Follow up in 2 days if fever persists.If the fever is present every day for more than 7 days, refer for assessment.

65
Does the child have fever?(by history, or feels hot or temperature 37.5C and above)
Decide Malaria Risk:If the child has measles now or within the last threemonths:
Decide Dengue Risk: Yes or No
If Dengue Risk:
Classify FEVER
Severe Complicated Measles
Measles with Eye or Mouth Complications
Measles
If dengue Risk, classify page 77 of the module Assess and Classify the Sick Child Age 2 months up to 5 years

66
If the child has measles now or within the last three months:
Look for mouth ulcers: are they deep and extensiveLook for pus draining from the eyeLook for clouding of the cornea
Does the child have fever?(by history, or feels hot or temperature 37.5C and above)
If measles now or within last three months, classify

67
Measles
Fever and generalized rash are the main signs of measles.
Highly infectious. Over crowding and poor housing increases
the risk of developing measles. Caused by a virus that infects the layers of
cells that line the lung, gut, eye, mouth and throat.

68
Measles
Complications of measles occur in about 30% of all cases– diarrhea (including dysentery and persistent
diarrhea)– pneumonia and stridor– mouth ulcers– ear infection– severe eye infection (which may lead to corneal
ulceration and blindness) Encephalitis occurs in about 1/1000 cases. (look for
danger signs such as convulsions, abnormally sleepy or difficult to awaken)

69
Classify MEASLESClouding of the corneaDeep extensive mouth ulcers
SEVERE COMPLICATED
MEASLES
Give Vitamin AGive first dose of an appropriate
antibioticsIf clouding of the cornea or pus draining
from the eye, apply Tetracycline eye
ointmentRefer URGENTLY to the hospital
Pus draining from the eyeMouth ulcers
MEASLES WITH EYE OR MOUTH
COMPLICATIONS
Give Vitamin AGive first dose of an appropriate
antibioticsIf pus draining from the eye, apply
Tetracycline eye ointmentIf mouth ulcers, teach the mother to treat
with gentian violetFollow up in two days
Measles now or within the last 3 months
MEASLES Give Vitamin A

70
Children with Measles

71 Koplik’s spots

72
TREAT THE CHILD: Give Vitamin A
TREATMENT Give one dose of Vitamin A in the Health Center
SUPPLEMENTATION Give one dose of Vitamin A in the Health Center
if:– Child is 6 months of age or older– Child has not received a dose of Vitamin A in
the past 6 months

73
TREAT THE CHILD: Give Vitamin A
AGEVitamin A Capsule
100,000 IU 200,000 IU
2 – 6 months 50,000 IU
6 – 12 months 1 cap 1/2 cap
1 – 5 years 2 caps 1 cap
200,000 IU = 6 drops 100,000 IU = 3 drops

74
Does the child have fever?(by history, or feels hot or temperature 37.5C and above)
Decide Malaria Risk:
If the child has measles now or within the last threemonths:
Classify FEVER
Severe DHF
Fever; DHF Unlikely
Torniquet Test 1.3gp
Torniquet Test 2.3gp
Decide Dengue Risk: Yes or No
If Dengue Risk:

75
Tourniquet Test
Inflate blood pressure cuff to a point midway between systolic and diastolic pressure for 5 minutes
Positive test: 20 or more petechiae per 1 inch² (6.25 cm²)

76
Classify DENGUE HEMORRHAGIC FEVER
bleeding from the nose or gums Bleeding in the vomitus or stoolsSkin petechiaeCold clammy extremitiesCapillary refill more than 3 secondsabdominal pain or Vomiting orPositive torniquet test
SEVERE DENGUE HEMORRHAGIC
FEVER
If skin petechiae or abdominal pain or vomiting or positive torniquet test are the only positive signs, give ORSIf any other signs of bleeding are present, give fluids rapidly as in Plan CTreat the child to prevent low blood sugarRefer all chioldren URGENTLY to the hospitalDO NOT GIVE ASPIRIN
No signs of severe dengue hemorrhagic fever
FEVER; DENGUE HEMORRHAIC FEVER
UNLIKELY
Advise mother when to return immediatelyFollow up in 2 days if fever persists or child shows signs of bleeding.DO NOT GIVE ASPIRIN

77
Dengue Hemorrhagic Fever
A child with dengue hemorrhagic fever or dengue shock syndrome may present severely hypotensive with disseminated intravascular coagulation (DIC), as this severely ill PICU patient did. Crystalloid fluid resuscitation and standard DIC treatment are critical to the child's survival.

78
Delayed capillary refill may be the first sign of intravascular volume depletion. Hypotension usually is a late sign in children. This child's capillary refill at 6 seconds was delayed well beyond a normal duration of 2 seconds.

79
Session 4-d
Ear Problem

80
Assess EAR PROBLEM
A child with ear problem is assessed for:
– Ear pain– Ear discharge
If present, how long has the child has had ear discharge
– Tender swelling behind the ear, a sign of mastoiditis

81
Assess EAR PROBLEM
Then Ask: Does the child have an ear problem?
If YES, ASK: Is there ear pain? Is there ear discharge? If yes, for how long?
LOOK and FEEL: Look for pus draining from the ear. Feel for tender swelling behind the ear.
Ask about ear problem in ALL sick children.

82
Classify EAR PROBLEM
Tender swelling behind the ear
MASTOIDITIS Give the first dose of an appropriate antibioticsGive first dose of Paracetamol for painRefer URGENTLY to hospital
Pus is seen draining from the ear and discharge is reported for less than 14 days, orEar pain
ACUTE EAR INFECTION
Give an antibiotic for 5 days. (Amoxicillin)*Give Paracetamol for pain.Dry the ear by wicking.Follow up in 5 days.
Pus is seen draining from the ear and discharge is reported for 14 days or more.
CHRONIC EAR INFECTION
topical quinolone ear drops for at least two weeks Dry the ear by wicking.Follow up in 5 days.
No ear pain and no pus is seen draining from the ear.
NO EAR INFECTION No additional treatment.
*Oral amoxicillin is a better choice for the management of suppurative otitis media in countries where antimicrobial resistance to cotrimoxazole is high.

83
TECHNICAL UPDATES: Chronic Suppurative Otitis Media
TECHNICAL BASIS: aural toilet combined with antimicrobial
treatment is more effective than aural toilet alone
topical antibiotics were found to be better than systemic antibiotics in resolving otorrhea and eradicating middle ear bacteria
topical quinolones were found to be better than topical non-quinolones
– topical ofloxacin or ciprofloxacin vs intramuscular gentamicin, topical gentamicin, tobramycin or neomycin-polymyxin

84
TECHNICAL UPDATES: Acute Otitis Media
TECHNICAL BASIS: oral amoxicillin as the better choice for the
management of acute ear infection in countries where antimicrobial resistance to cotrimoxazole is high.
reduces the risk of mastoiditis in populations where it is more common

85
TREAT THE CHILD: Dry the Ear by Wicking
Dry the ear at least 3 times daily.– Roll a clean absorbent cotton or soft tissue
paper into a wick.– Place the wick in the child’s ear.– Remove the wick when wet.– Replace the wick with a clean one and
repeat these steps until the ear is dry. Do not use a cotton-tipped applicator, a stick
or a flimsy paper that will fall apart in the ear.

86
TREAT THE CHILD: Dry the Ear by Wicking
Wick the ear 3 times daily. Use this treatment for as many days as it
takes until the wick no longer gets wet when put in the ear and no pus drains from the ear.
Do not place anything (oil, foil or other substances) in the ear between wicking treatments.
Do not allow the child to go into swimming.