Imci Lecture.1 Ppt
-
Upload
alyssandra-faye-carsula -
Category
Documents
-
view
550 -
download
39
description
Transcript of Imci Lecture.1 Ppt

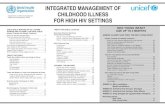
Integrated Integrated
Management of Management of Childhood IllnessesChildhood Illnesses

DefinitionDefinitionThis is an innovative approach which was This is an innovative approach which was started in 1995 by WHO and UNICEF with started in 1995 by WHO and UNICEF with the aim of introducing a comprehensive the aim of introducing a comprehensive and timely management of the 5 most and timely management of the 5 most common causes of ill health and death common causes of ill health and death among under-fives.among under-fives.These illnesses are:These illnesses are:Pneumonia MeaslesPneumonia MeaslesDiarrhea MalnutritionDiarrhea MalnutritionMalariaMalaria

Reasons for Developing IMCI Reasons for Developing IMCI Strategy:Strategy:
1.1. Curative CareCurative Care2.2. Aspect of NutritionAspect of Nutrition3.3. ImmunizationImmunization4.4. Disease preventionDisease prevention5.5. Health promotionHealth promotion

Objectives:Objectives:
To reduce death, frequency and To reduce death, frequency and severity of illness and disability.severity of illness and disability.Contribute to improved growth and Contribute to improved growth and developmentdevelopment

Components of IMCIComponents of IMCI1.1. Improvement of Improvement of
health worker skills.health worker skills. This takes the form of This takes the form of
training in the case training in the case management of sick management of sick children. In the children. In the Philippines, the DOH Philippines, the DOH has trained facilitators has trained facilitators and provincial Health and provincial Health management teams management teams on the case on the case management training management training for health workersfor health workers..

Components of IMCIComponents of IMCI
2.2. Improvement of Improvement of Health Systems- Health Systems- The IMCI strategy The IMCI strategy requires that the requires that the health system is health system is strengthened to strengthened to support the support the strategy in the strategy in the following ways.following ways.

Ensuring the Ensuring the availability of availability of essential drugs & essential drugs & suppliessupplies

Organization Organization of the hospital of the hospital emergency emergency area to area to support rapid support rapid evaluation & evaluation & management management of sick childrenof sick children

Training of Training of health workers health workers in Emergency in Emergency Triage Triage Assessment and Assessment and Treatment Treatment (ETAT)(ETAT)

Adherence to Adherence to National policies National policies for standard of for standard of care.care.Availing job Availing job aides in critical aides in critical areaarea

Components of IMCIComponents of IMCI
3. Improvement 3. Improvement of Family and of Family and Community Community PracticesPractices

Family & Community Family & Community PracticesPractices
A. Growth Promotion A. Growth Promotion & Development& Development
Exclusive Exclusive breastfeeding for 6 breastfeeding for 6 monthsmonths
Appropriate Appropriate complementary complementary feeding from 6 feeding from 6 mos. While mos. While continuing BF up to continuing BF up to 2 years 2 years

A. Growth A. Growth Promotion & Promotion & DevelopmentDevelopment
Adequate Adequate micronutrients micronutrients through diet or through diet or supplementation.supplementation.Promote mental Promote mental and psychosocial and psychosocial development.development.

B. Disease PreventionB. Disease PreventionProper disposal of Proper disposal of feces, hand washing feces, hand washing etc.etc.Adequate rest and Adequate rest and sleep under treated sleep under treated mosquito netsmosquito netsPrevention of HIV/AIDSPrevention of HIV/AIDSPrevent child Prevent child Abuse/neglect & taking Abuse/neglect & taking appropriate action.appropriate action.

C. Home C. Home ManagementManagementContinue to feed & Continue to feed & offer more food & offer more food & fluids when child is fluids when child is sick.sick.Give child appropriate Give child appropriate home treatment for home treatment for infections.infections.Take appropriate Take appropriate actions to prevent actions to prevent and manage child and manage child injuries & accidents.injuries & accidents.

D. Care Seeking and D. Care Seeking and ComplianceCompliance
Take child to Take child to complete full course complete full course of immunization of immunization before 1before 1stst birthday. birthday.Recognize when child Recognize when child needs treatment needs treatment outside home and outside home and take to H.C.take to H.C.

D. Care Seeking & D. Care Seeking & ComplianceCompliance
Follow Health Follow Health Worker’s advice Worker’s advice about treatment, about treatment, follow-up & referral.follow-up & referral.
Mother’s class Mother’s class attendance & attendance & Tetanus Toxoid Tetanus Toxoid vaccination during vaccination during pregnancy.pregnancy.
Active participation Active participation of men in childcare of men in childcare & reproductive & reproductive health activitieshealth activities

Principles of Integrated CarePrinciples of Integrated Care1.1. All sick children must be examined for All sick children must be examined for
“general danger signs”“general danger signs”2.2. All sick children must be routinely All sick children must be routinely
assessed for major symptomsassessed for major symptoms3.3. Only a limited number of carefully Only a limited number of carefully
selected clinical signs are used.selected clinical signs are used.4.4. A combination of individual signs lead A combination of individual signs lead
to a child’s classification(s) rather than to a child’s classification(s) rather than diagnosis.diagnosis.

Principles of Integrated CarePrinciples of Integrated Care5. IMCI guidelines address most but not 5. IMCI guidelines address most but not
all of the major reasons a sick child is all of the major reasons a sick child is brought to a clinic.brought to a clinic.
6. IMCI management procedures use a 6. IMCI management procedures use a limited number of essential drugs and limited number of essential drugs and encourage active participation of encourage active participation of caretakers in the treatment of caretakers in the treatment of children.children.
7. An essential component of the IMCI 7. An essential component of the IMCI guidelines is the counseling about guidelines is the counseling about feeding, fluids and when to return to a feeding, fluids and when to return to a health facility.health facility.

Assessment Using IMCI Assessment Using IMCI StrategyStrategy
In IMCI we assess In IMCI we assess children for a number children for a number of things:of things:Assessment Checklist Assessment Checklist divided into four:divided into four:First PartFirst Part
History takingHistory taking Second PartSecond Part General Danger SignsGeneral Danger Signs

Assessment Using IMCI Assessment Using IMCI StrategyStrategy
Assessment Assessment Checklist divided Checklist divided into four:into four:
Third Part Third Part Main symptomsMain symptoms Cough or Difficult Cough or Difficult
breathingbreathing DiarrheaDiarrhea FeverFever Ear problemsEar problems

Assessment ChecklistAssessment Checklist
Fourth Part:Fourth Part:Nutritional Nutritional StatusStatusImmunization Immunization StatusStatusOther Other ProblemsProblems

History TakingHistory TakingBasically the asking part we cannot ask Basically the asking part we cannot ask the child so we will ask the mother, the child so we will ask the mother, significant other, or primary caregiver. significant other, or primary caregiver.
Basic communication that you have to Basic communication that you have to consider:consider:
Listen carefully to what the primary Listen carefully to what the primary caregiver says.caregiver says.
Use words the primary caregiver Use words the primary caregiver understandsunderstands
Give the primary caregiver time to answer Give the primary caregiver time to answer the questions.the questions.
Ask additional questions when the Ask additional questions when the primary caregiver is not sure about the primary caregiver is not sure about the answer.answer.

Things to ask the Mother or Things to ask the Mother or the Primary Caregiverthe Primary Caregiver
Asking for General Danger Signs:Asking for General Danger Signs:1. Is the child not able to drink or breastfeed1. Is the child not able to drink or breastfeed2. Does the child vomits everything?2. Does the child vomits everything?3. Has the child had convulsions?3. Has the child had convulsions?Then ask about Main Symptoms:Then ask about Main Symptoms:For Pneumonia:For Pneumonia:1.1. Does the child have cough or difficult Does the child have cough or difficult
breathing? If yes for how long?breathing? If yes for how long?For Diarrheal diseases:For Diarrheal diseases:1. Does the child have diarrhea? If yes, for 1. Does the child have diarrhea? If yes, for
how long? And is there blood in the stool?how long? And is there blood in the stool?

For diseases with fever:For diseases with fever:1.1. Does the child have fever? If yes since Does the child have fever? If yes since
when?when?2.2. For how long does the child had fever?For how long does the child had fever?3.3. If more than seven days, has fever been If more than seven days, has fever been
present everyday?present everyday? For Malarial risk:For Malarial risk:1.1. Does the child live in malaria area?Does the child live in malaria area?2.2. Has the child visited a malaria in past 4 Has the child visited a malaria in past 4
weeks? If yes to either, obtain a blood weeks? If yes to either, obtain a blood smear. smear.
For Measles:For Measles:1. Has the child had measles within the last 3 1. Has the child had measles within the last 3
months?months?

For Ear For Ear problems:problems:
1. Does the child 1. Does the child have an Ear have an Ear problem?problem?
2. Is there ear 2. Is there ear pain?pain?
3. Is there ear 3. Is there ear discharge? If discharge? If yes, for how yes, for how long?long?

General Danger SignsGeneral Danger SignsLethargic or unconscious – An Lethargic or unconscious – An unconscious child is likely to be unconscious child is likely to be seriously ill. A lethargic child, seriously ill. A lethargic child, who is awake but does not take who is awake but does not take any notice of his or her any notice of his or her surroundings or does not surroundings or does not respond normally to sounds or respond normally to sounds or movement, may also be very movement, may also be very sick.sick.

General Danger SignsGeneral Danger Signs
History of Convulsions or convulsing History of Convulsions or convulsing now- The child has had convulsions now- The child has had convulsions during the present illness. during the present illness. Convulsions may be the result of Convulsions may be the result of fever. In this instance, they do little fever. In this instance, they do little harm beyond frightening the mother.harm beyond frightening the mother.

General Danger SignsGeneral Danger Signs
Vomiting everything – The child Vomiting everything – The child vomits everything. The vomiting vomits everything. The vomiting itself may be a sign of serious illness, itself may be a sign of serious illness, but it is also important to note but it is also important to note because such a child will not be able because such a child will not be able to take medication or fluids for to take medication or fluids for rehydrationrehydration

General Danger SignsGeneral Danger Signs
Not able to drink or breastfeed – The Not able to drink or breastfeed – The child is unable to drink or breastfeed. child is unable to drink or breastfeed. A child may be unable to drink either A child may be unable to drink either because he is too weak or because because he is too weak or because he cannot swallow. Do not rely he cannot swallow. Do not rely completely on the mother’s evidence completely on the mother’s evidence for this, but observe while she tries for this, but observe while she tries to breastfeed or to give the child to breastfeed or to give the child something to drinksomething to drink

If a child has one or more of these If a child has one or more of these signs, he/she must be considered signs, he/she must be considered seriously ill and will almost always need seriously ill and will almost always need referral. In order to start treatment for referral. In order to start treatment for severe illnesses without delay, the child severe illnesses without delay, the child should be quickly assessed for the should be quickly assessed for the most important causes of serious most important causes of serious illness and death- acute respiratory illness and death- acute respiratory infection (ARI), diarrhea, and fever infection (ARI), diarrhea, and fever (especially associated with malaria and (especially associated with malaria and measles). A rapid assessment of measles). A rapid assessment of nutritional status is also essential, as nutritional status is also essential, as malnutrition is another main cause of malnutrition is another main cause of death.death.

Assessment of Main SymptomsAssessment of Main SymptomsGeneral Physical ExaminationGeneral Physical ExaminationFor danger signs:For danger signs:
1.See if the child is abnormally sleepy or difficult 1.See if the child is abnormally sleepy or difficult to awaken.to awaken.
For Pneumonia:For Pneumonia:Count the breath in one minute. (calm child)Count the breath in one minute. (calm child) RR of 60 bpm for 0-2 months is normalRR of 60 bpm for 0-2 months is normal RR of 50 bpm for 2 months-1 year is normalRR of 50 bpm for 2 months-1 year is normal RR of 40bpm for 1-5 years is normalRR of 40bpm for 1-5 years is normal Look for chest indrawing (calm Child)Look for chest indrawing (calm Child) Look and listen for stridor or wheezingLook and listen for stridor or wheezing Check the respiratory rate of the childCheck the respiratory rate of the child

Assessment of Main SymptomsAssessment of Main SymptomsFor Diarrheal diseases: Offer the child For Diarrheal diseases: Offer the child Abnormally sleepy or difficult to awaken?Abnormally sleepy or difficult to awaken? Restless and irritable?Restless and irritable?Look for sunken eyes.Look for sunken eyes.Offer the child fluid. Is the child:Offer the child fluid. Is the child:Not able to drink or drinking poorlyNot able to drink or drinking poorlyDrinking eagerly, thirsty?Drinking eagerly, thirsty?Pinch the skin of the abdomen. Does it Pinch the skin of the abdomen. Does it go back:go back:Very slowly (longer than 2 seconds)Very slowly (longer than 2 seconds)SlowlySlowly

Assessment of Main SymptomsAssessment of Main SymptomsFor diseases with fever:For diseases with fever:Feels hotFeels hotTemperature (37.5°C or above)Temperature (37.5°C or above)For Malarial risk:For Malarial risk:Look or feel for stiff neckLook or feel for stiff neckLook for runny noseLook for runny noseChillsChills

Assessment of Main SymptomsAssessment of Main SymptomsFor Measles:For Measles: Generalized rashGeneralized rashOne of these: cough, runny nose, or One of these: cough, runny nose, or red eyesred eyesLook for mouth ulcers.Look for mouth ulcers.
Are they deep and extensive?Are they deep and extensive?Look for pus draining from the eye.Look for pus draining from the eye.Look for clouding of the corneaLook for clouding of the cornea

Assessment of Main SymptomsAssessment of Main SymptomsFor Ear problems:For Ear problems:Look for pus draining from the earLook for pus draining from the earFeel for tender swelling behind the ear.Feel for tender swelling behind the ear.For Malnutrition:For Malnutrition:Look for visible severe wasting.Look for visible severe wasting.Look for edema of both feet.Look for edema of both feet.Look for palmar pallor?Look for palmar pallor?Severe palmar pallorSevere palmar pallorSome palmar pallorSome palmar pallorDetermine weight for age.Determine weight for age.Very lowVery low

Main Symptom: CoughMain Symptom: CoughCount the breath in one minute. (calm Count the breath in one minute. (calm
child)child) RR of 60 bpm for 0-2 months is normalRR of 60 bpm for 0-2 months is normal RR of 50 bpm for 2 months-1 year is RR of 50 bpm for 2 months-1 year is
normalnormal RR of 40bpm for 1-5 years is normalRR of 40bpm for 1-5 years is normal Look for chest indrawing (calm Child)Look for chest indrawing (calm Child) Look and listen for stridor or wheezingLook and listen for stridor or wheezing

Child with Chest IndrawingChild with Chest Indrawing

Main Symptom: DiarrheaMain Symptom: DiarrheaAbnormally sleepy or difficult to awaken.Abnormally sleepy or difficult to awaken.Restless and irritableRestless and irritableLook for sunken eyesLook for sunken eyesOffer the child fluid. Is the child:Offer the child fluid. Is the child:Not able to drink or drinking poorly?Not able to drink or drinking poorly?Drinking eagerly, thirsty?Drinking eagerly, thirsty?Pinch the skin of the abdomen. Does it Pinch the skin of the abdomen. Does it go back:go back:Very slowly (longer than two seconds)Very slowly (longer than two seconds)Slowly?Slowly?

Dehydrated ChildDehydrated Child

For Diseases with FeverFor Diseases with FeverFeels hotFeels hotTemperature 37.5 and aboveTemperature 37.5 and aboveFor Malarial RiskFor Malarial RiskLook or feel for stiff neckLook or feel for stiff neckLook for runny nose.Look for runny nose.ChillsChills

For Measles:For Measles:Generalized Rash and Generalized Rash and One of these: cough, runny nose, or red One of these: cough, runny nose, or red eyeseyesLook for mouth ulcers.Look for mouth ulcers.
Are they deep and extensive?Are they deep and extensive?Look for pus draining from the eye.Look for pus draining from the eye.Look for clouding of the cornea.Look for clouding of the cornea.For Ear problems:For Ear problems:Look for pus draining from the ear.Look for pus draining from the ear.Feel for tender swelling behind the earFeel for tender swelling behind the ear

For Malnutrition:For Malnutrition:Look for visible wastingLook for visible wastingLook for edema of both feetLook for edema of both feetLook for palmar pallorLook for palmar pallor
Severe palmar pallor?Severe palmar pallor? Some palmar pallor?Some palmar pallor?
Determine weight for age.Determine weight for age. Very low?Very low?

Main Symptom: CoughMain Symptom: Cough
Count the breath in one minute. (calm Count the breath in one minute. (calm child)child)
RR of 60 bpm for 0-2 months is RR of 60 bpm for 0-2 months is normalnormal
RR of 50 bpm for 2 months-1 year is RR of 50 bpm for 2 months-1 year is normalnormal
RR of 40bpm for 1-5 years is normalRR of 40bpm for 1-5 years is normal Look for chest indrawing (calm Child)Look for chest indrawing (calm Child) Look and listen for stridor or Look and listen for stridor or
wheezingwheezing

Those who simply have a cough or cold Those who simply have a cough or cold and do not require antibiotics. A child and do not require antibiotics. A child with cough and cold normally improves with cough and cold normally improves in one or two weeks. However, a child in one or two weeks. However, a child with chronic cough (more than 30 with chronic cough (more than 30 days) needs to be further assessed days) needs to be further assessed ( and if needed, referred) to exclude ( and if needed, referred) to exclude primary complex, asthma, whooping primary complex, asthma, whooping cough or another problem.cough or another problem.Breastmilk is a good soothing remedy, Breastmilk is a good soothing remedy, you can also increase fluid intake for you can also increase fluid intake for children above 6 months you can children above 6 months you can introduce sampalok, kalamansi and introduce sampalok, kalamansi and luya.luya.

No signs of No signs of Pneumonia or very Pneumonia or very severe diseasesevere disease
No Pneumonia cough No Pneumonia cough or coldor cold

3 Key Clinical Signs are used to Assess 3 Key Clinical Signs are used to Assess a Sick Child with Cough or Difficult a Sick Child with Cough or Difficult Breathing:Breathing:Respiratory Rate-distinguishes children Respiratory Rate-distinguishes children who have pneumonia from those who who have pneumonia from those who do not have. Those who require do not have. Those who require antibiotics are likely to have bacterial antibiotics are likely to have bacterial pneumonia. This group includes all pneumonia. This group includes all children with fast respiratory rate. Fast children with fast respiratory rate. Fast breathing , as defined by WHO detects breathing , as defined by WHO detects 80% of children with pneumonia who 80% of children with pneumonia who need antibiotic treatment. Treatment need antibiotic treatment. Treatment based on this classification has been based on this classification has been shown to reduce mortality.shown to reduce mortality.

Fast BreathingFast Breathing PneumoniaPneumonia

Lower chest wall indrawing, which Lower chest wall indrawing, which indicates severe pneumonia- defined indicates severe pneumonia- defined as the inward movement of the bony as the inward movement of the bony structure of the chest wall with structure of the chest wall with inspiration, is a useful indicator of inspiration, is a useful indicator of severe pneumonia. Chest indrawing severe pneumonia. Chest indrawing should only be considered present if should only be considered present if it is consistently present in a calm it is consistently present in a calm child. Agitation, a blocked nose or child. Agitation, a blocked nose or breastfeeding can all cause breastfeeding can all cause temporary chest indrawing.temporary chest indrawing.

Stridor and wheezing, which indicates Stridor and wheezing, which indicates those with severe pneumonia who those with severe pneumonia who require hospital admission. Stridor is a require hospital admission. Stridor is a harsh noise made when the child harsh noise made when the child inhales (breathes in). Children who inhales (breathes in). Children who have stridor when calm have a have stridor when calm have a substantial risk of obstruction and substantial risk of obstruction and should be referred. Sometimes a should be referred. Sometimes a wheezing noise noise is heard when the wheezing noise noise is heard when the child exhales (breathes out). This is not child exhales (breathes out). This is not stridor. A wheezing sound is most often stridor. A wheezing sound is most often associated with asthma.associated with asthma.

Any general danger Any general danger signsignChest indrawingChest indrawingStridor in calm Stridor in calm childchild
Severe PneumoniaSevere Pneumonia ororVery severe diseaseVery severe disease

Main Symptom: DiarrheaMain Symptom: DiarrheaAbnormally sleepy or difficult to Abnormally sleepy or difficult to awaken?awaken?Restless and irritable?Restless and irritable?Look for sunken eyes.Look for sunken eyes.Offer the child fluid. Is the child:Offer the child fluid. Is the child:
Not able to drink or drinking poorly?Not able to drink or drinking poorly? Drinking eagerly, thirsty?Drinking eagerly, thirsty?
Pinch the skin of the abdomen. Does it Pinch the skin of the abdomen. Does it go back: Very slowly (longer than 2 go back: Very slowly (longer than 2 seconds)seconds)
SlowlySlowly

All children with Diarrhea should be All children with Diarrhea should be checked to determine the duration of checked to determine the duration of diarrhea, if blood is present in the diarrhea, if blood is present in the stool and if dehydration is present. A stool and if dehydration is present. A number of clinical signs are used to number of clinical signs are used to determine the level of dehydration: determine the level of dehydration: Depending on the degree of Depending on the degree of dehydration, a child with diarrhea dehydration, a child with diarrhea may be lethargic or unconscious or may be lethargic or unconscious or look restless/irritable. The eyes of a look restless/irritable. The eyes of a dehydrated child may look sunken. In dehydrated child may look sunken. In a severely malnourished child who is a severely malnourished child who is visibly wasted the eyes may always visibly wasted the eyes may always look sunkenlook sunken

Not enough signs Not enough signs to classify as some to classify as some or severe or severe dehydrationdehydration
No DehydrationNo Dehydration

Two of the following Two of the following signs:signs:Restless, irritableRestless, irritableSunken eyesSunken eyesDrinks eagerly, Drinks eagerly, thirstythirstySkin pinch goes back Skin pinch goes back slowlyslowly
Some DehydrationSome Dehydration

Two of the Two of the following signs:following signs:Lethargic or Lethargic or unconsciousunconsciousSunken eyesSunken eyesNot able to drink or Not able to drink or drinking poorlydrinking poorlySkin pinch goes Skin pinch goes back very slowlyback very slowly
Severe Severe DehydrationDehydration

Main Symptom: FeverMain Symptom: Fever
For diseases with feverFor diseases with fever Feels hotFeels hot Temperature (37.5°C or above)Temperature (37.5°C or above)For Malarial risk:For Malarial risk:Look or feel for stiff neckLook or feel for stiff neckLook for runny noseLook for runny noseChillsChills

All sick children should be checked All sick children should be checked for fever. Fever is a very common for fever. Fever is a very common condition and is often the main condition and is often the main reason for bringing children to the reason for bringing children to the health center. It may be caused by health center. It may be caused by minor infections, but may also be the minor infections, but may also be the most obvious sign of a life most obvious sign of a life threatening illness, particularly threatening illness, particularly Malaria(esp. lethal malaria) or other Malaria(esp. lethal malaria) or other severe infections, including severe infections, including meningitis, typhoid fever, or meningitis, typhoid fever, or measles.measles.

A child presenting with fever should A child presenting with fever should be assessed for:be assessed for:Stiff neck – this may be a sign of Stiff neck – this may be a sign of meningitis, cerebral malaria or meningitis, cerebral malaria or another severe febrile disease. If the another severe febrile disease. If the child is conscious and alert, check child is conscious and alert, check stuffiness by tickling the feet, asking stuffiness by tickling the feet, asking the child to bend his /her neck to the child to bend his /her neck to look down or be very gently bending look down or be very gently bending the child’s head forward to assess the child’s head forward to assess pain or stiffness.pain or stiffness.

Any danger sign Any danger sign ororStiff neckStiff neck
Very severe Very severe febrile diseasefebrile disease

Risk of Malaria and other endemic Risk of Malaria and other endemic infections. A high malaria risk setting infections. A high malaria risk setting is defined as a situation in which is defined as a situation in which more than 5% of cases of febrile more than 5% of cases of febrile disease in children age 2 to 59 disease in children age 2 to 59 months are malarial disease. months are malarial disease.
Fever (by history Fever (by history Or feels hot or MalariaOr feels hot or Malariatemperaturetemperature37.5°C or above)37.5°C or above)

Runny nose Runny nose presentpresentMeasles Measles present present Other causes Other causes of fever of fever presentpresent
Fever-Malaria Fever-Malaria unlikelyunlikely

For Measles:For Measles:Generalized rash Generalized rash One of these: cough,runnynose, red One of these: cough,runnynose, red eyes.eyes.Look for mouth ulcersLook for mouth ulcers Are they deep and extensiveAre they deep and extensiveLook for pus draining from the eye.Look for pus draining from the eye.Look for clouding of the corneaLook for clouding of the cornea

Any danger Any danger sign orsign orClouding of Clouding of cornea orcornea orDeep or Deep or extensive extensive mouth ulcersmouth ulcers
Severe Severe complicated complicated MeaslesMeasles

Treatment with this case includes Treatment with this case includes vitamin A, tetracycline ointment for vitamin A, tetracycline ointment for children with pus draining from the children with pus draining from the eye, and gentian violet for children eye, and gentian violet for children with mouth ulcers. Measles with mouth ulcers. Measles depresses the immune system, these depresses the immune system, these children may be also referred to children may be also referred to hospital for treatment.hospital for treatment.

Pus draining Pus draining from the eye from the eye or or Mouth ulcersMouth ulcers
Measles with Measles with Eye or Mouth Eye or Mouth complicationscomplications

If no signs of measles complications If no signs of measles complications have been found after a complete have been found after a complete examination, a child is classified as examination, a child is classified as having measles. These children can having measles. These children can be effectively and safely managed at be effectively and safely managed at home with vitamin A treatment.home with vitamin A treatment.
Measles now or MeaslesMeasles now or Measles Within the last threeWithin the last three monthsmonths

Main Symptom: Ear ProblemsMain Symptom: Ear Problems
For Ear problemsFor Ear problemsLook for pus draining from the ear.Look for pus draining from the ear.Feel for tender swelling behind the ear.Feel for tender swelling behind the ear.The most serious complications of an The most serious complications of an ear infection is a deep infection in the ear infection is a deep infection in the mastoid bone. It usually manifests with mastoid bone. It usually manifests with tender swelling behind one of the tender swelling behind one of the child’s ears. In infants, this tender child’s ears. In infants, this tender swelling also maybe above the ear. swelling also maybe above the ear.

Tender Tender swelling swelling behind the earbehind the ear
MastoiditisMastoiditis

Children presenting with tenderness Children presenting with tenderness and swelling of the mastoid bone are and swelling of the mastoid bone are classified as having Mastoiditis and classified as having Mastoiditis and should be referred to the hospital for should be referred to the hospital for treatment. Before referral, these treatment. Before referral, these children first should receive a dose of children first should receive a dose of antibiotic and a single dose of antibiotic and a single dose of paracetamol for pain. paracetamol for pain.

Ear discharge for Ear discharge for fewer than 14 days fewer than 14 days or or Ear painEar pain
Acute Ear InfectionAcute Ear Infection

Main symptom: Low weight per AgeMain symptom: Low weight per Age
For MalnutritionFor MalnutritionLook for visible wastingLook for visible wastingBaggy pantsBaggy pantsLook for edema of both feetLook for edema of both feetLook for palmar pallorLook for palmar pallor
Severe palmar pallorSevere palmar pallor Some palmar pallorSome palmar pallor
Determine weight for ageDetermine weight for age Very lowVery low

Visible severe wasting – This is Visible severe wasting – This is defined as severe wasting of the defined as severe wasting of the shoulders, arms, buttocks, and legs, shoulders, arms, buttocks, and legs, with ribs easily seen, and indicators with ribs easily seen, and indicators presence of marasmus. Edema of presence of marasmus. Edema of both feet.both feet.Presence of edema – (accumulation Presence of edema – (accumulation of fluid) in both feet may signal of fluid) in both feet may signal kwashiorkor. Children with edema of kwashiorkor. Children with edema of both feet may have other diseases both feet may have other diseases like nephrotic syndrome.like nephrotic syndrome.

Palmar pallor – Children with severe Palmar pallor – Children with severe malnutrition or severe anemia malnutrition or severe anemia (exhibiting visible severe wasting, or (exhibiting visible severe wasting, or severe palmar pallor or edema of severe palmar pallor or edema of both feet) are at high risk of death both feet) are at high risk of death from various severe diseases and from various severe diseases and need urgent referral to a hospital need urgent referral to a hospital where their treatment can be where their treatment can be carefully monitored.carefully monitored.

Visible severe Visible severe wastingwastingSevere palmar Severe palmar pallorpallorEdema of both feetEdema of both feet
Severe Malnutrition Severe Malnutrition or Severe Anemiaor Severe Anemia

Some Palmar Some Palmar pallorpallor(Very) low (Very) low weight for ageweight for age
Anemia or Anemia or (very) Low (very) Low WeightWeight