Image quize
-
Upload
lm-huq -
Category
Health & Medicine
-
view
70 -
download
0
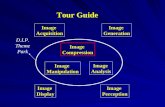
Transcript of Image quize



Welcome All

IMAGE QUIZE
Dr M Nurul Huq. BMC. Bangladesh

3y M has HGF x2d, difficult swallowing, dribbling, irritability with this sign. What is the most probable Dx?
1. Strep throat2. Diphtheria3. ITP4. Herpangina5. Herpetic stomatitis

4. Herpangina
• It is typically c/by Coxsackie A• Contagious• F subsides with appearance of ulcers (2-4mm)• Normally clears up within 7d• Supportive Rx

Inf. with which organisms is the most likely cause?
1. Coxsackie A16 2. Echovirus 16 3. G AS4. HSV type 1 5. Norwalk virus

1. Coxsackie virus type A16
The rash represents the characteristic palmar lesions of uncomplicated hand, foot, and mouth disease due to coxsackie A16 and enterovirus 71

4y M with HGF x2d, sore mouth, poor app., irritability, inability to chew, and drooling had this gum. Next day he had these ulcers. What is most probable Dx?
1. ANUG2. Herpangina3. Scurvy4. Herpes stomatitis5. Canker sores (aphthae)

4. Herpetic stomatitis
Herpetic stomatitis is c/by HSV T1or oral herpes. Young children commonly are affected. It can easily be spread from one child to another. Recovery completely within 10d without medical Rx. Aciclovir may speed up your child's recovery

13y F has halitosis, gum pain, bleed, mild F. What is the most probable Dx?
1. ANUG2. Herpes stomatitis3. Scurvy4. Ariboflavinosis5. ITP

Acute necrotizing ulcerative gingivitis (ANUG):
aka Vincent's angina. Many other names
Certain germs (including fusiform bacteria and spirochetes) have been implicated, but the full story is still not clear
Metronidazole is DoC

What is the Dx?

Aphthous stomatitis (aka recurrent aphthous stomatitis, recurring oral aphthae or recurrent aphthous ulceration or aphthae) is common (20%)
• Repeated benign and non-contagious mouth ulcers in otherwise healthy people. Called canker sores in N America
• Cause is not known: T cell-mediated immune response triggered by many factors. Different people have different factors: nutritional deficiency, trauma, stress, hormonal factors, allergy, genetic, etc.
• Periodical. Heal completely. For majority, it lasts 7–10d, attacks 3–6/y. Most appear on the non-keratinizing epith. surfaces (anywhere except the attached gum, the hard palate and the dorsum of tongue). SS: a minor nuisance with eating and drinking. The severe forms may be debilitating, even causing wt loss
• Childhood or adolescence. Usually for several years before disappearing. No cure. Rx: manage pain, reduce healing time and reduce the frequency of episodes of ulceration

What is the Dx?

Geographic tongue is irregular changing patches like map on the tongue
• Cause unknown; may be a lack of vit B or irritation from hot or spicy foods, or alcohol. Less common in smokers
• Change in pattern is due to loss of papillae: flat. Change can occur v quickly. The flat areas may stay for >1mo
• Soreness and burning pain (in some cases)
• No test. No Rx. Antihistamine gel or steroid mouth rinses may help ease discomfort. It is harmless. It may be uncomfortable and last for a long time

14mo M, immunized, had HGF ~104o x4d , a GTC fit for ~4min and gen. MPR next day on fall of F. What is the most likely Dx?1. Roseola infantum2. Measles 3. Rubella 4. Scarlet fever 5. Infectious mononucleosis

1. Roseola infantum
Roseola (aka 6th d, exanthem subitum, roseola infantum) commonly affects 6mo-2y childrenC/ by HHV 6-7
Usually several days of HGF, f/by a distinctive MPR just as the F breaks. Febrile seizure in 10-15%

5y boy had F103oF, sore throat, rash on 2nd dy. Tongue is raw bald by 4d. What is the most probable DX?1. Scarlet fever2. Measles3. Rubella4. Mucocutaneous LN syn5. Glandular fever

1.Scarlet fever
Features: Sore throat, HGF, generalized erythema, Pastia’s sign, circumoral pallor, peeling off of skin later on

5y M with F x5d, pink eyes, rash, unilateral neck swelling, sore lips, swollen hands. What is the most probable Dx?1. Kawasaki disease2. Scarlet F3. Measles4. Septicemia5. Viral hemorrhagic fever


1. Kawasaki disease
FEBRILE is used to remember the criteria• Fever• Enanthem• Bulbar conjunctivitis (nonpurulent)• Rash (polymorphic)• Internal organ involvement (not part of the criteria)• LAP• Extremity changes

Q:
What is the diagnosis?
1. Erythema chronicum migrans2. Granuloma annulare3. Pityriasis rosea. 4. Sarcoidosis. 5. Tinea circinata

5. Tinea circinata
Skin-scraping with KOH of the violaceous plaque consisting of 4 concentric rings with intervening areas of normal skin and numerous yellow-white pustules showed multiple hyphae. Dx of tinea circinata, an uncommon morphologic variant of t. corporis that is c/by the dermatophyte Trichophyton tonsurans, was made

What is the most likely Dx in a woman who presents with F, cough, rhinorrhea, and this
finding?

Measles
Serologic testing revealed elevated antirubeola IgM


What is the most likely Dx?
1. Periorbital cellulitis2. Lyme disease3. Dermatomyositis4. Periocular atopic dermatitis5. Polymorphous light eruption

Lyme disease
Erythema migrans is a common feature of early, disseminated LD. The classic rash may be varied in its presentation, as seen here

• 8y M: 10d periorbital rash, preceding knee p, F, HA• 3w ago, he was bitten by 2 ticks• He has erythema migrans periorbitally, front of R knee, R
axilla, buttocks
• B burgdorferi IgG 0.58 (<0.20), B. burgdorferi sensu lato IgG anti-VlsE 75.5 kU/L (<16.0), B. burgdorferi IgM 5.85 (<0.20). Immunoblot testing for B. garinii IgG and IgM antibodies was positive
• EM is common in early, disseminated LD. However, it may be varied in its presentation, as seen here
• He got amoxicillin 3w with full recovery

Disseminated Lyme Disease

What is the most probable Dx?

Cong. Duodenal Obstruction (Double-Bubble Sign) • A girl 1080g born at 29w did not tolerate NGT feeding 8h after birth. Her condition deteriorated, with nonbilious V and a lack of stools since birth. She had mild upper abdo. Distention• AXR: double-bubble sign, a distended stomach (arrow) and D1 (arrowhead) a pathognomonic of cong. DO
• There was no air distally. Laparoscopy: duodenal atresia , which was repaired. Oral feedings were initiated successfully on 7POD. Recovery was uneventful

What is the Dx:
1. Spina ventosa2. Sarcoidosis3. SCD4. Osteomyelitis5. Enchondroma

Spina ventosa. 17y M: 2-mo pain and swelling on dorsal L hand. No F. Visited Pakistan 6mo ago; no trauma
• PE: a hard and suppurative nodule was noted on L 3rd metacarpal. No systemic symptoms, no LAP
• Lab.: HIV -ve. XR: a slightly thinned cortex with lytic core with trabecular pieces (arrow); no periosteal reaction. CXR: normalZN staining: AFB (M tb. in CS and a pan-sensitive isolate)
• Rx: ATT 6mo
• TB dactylitis (spina ventosa) is more common in children

D 1 D 3 3 mo
What is the Dx?

Infective endocarditis
• 34y M with dim vision in the RE. Exertional dyspnea 4 mo; started 1w after a dental Rx.
• Previous extensive inv. are inconclusive• He was afebrile, had a pansystolic m and a solitary splinter
hge on R thumb• Echo.. : m-s MR, with thickening and vegetations• x4 blood CS: S viridans. IV AB. SS improved, and VA ok 8mo
later. His R fundus is shown, at admn (A), 3d later (B), and 3mo later (C). White-centered hge (Roth spots) is Dx of IE
• A comparison of A and B (3d apart) shows how quickly such spots can change. Monitoring his MR is ongoing


Linear IgA Dermatosis (LAD)is an autoimmune D in which there is a linear deposition of
IgA at the BM. It affects both children and adults. It may be drug-related. In non-drug-related category the cause is unknown. May occur following typhoid, brucella, TB, varicella, HZ, gynaecological inf, URTI. In children, it has been known historically as chr. bullous dermatosis
• LAD is characterized by the linear deposition of IgA at BM zone (BMZ). One function of the BMZ is to maintain the contiguity of the dermal-epidermal junction; antibody deposition causes complement fixation and neutrophil chemotaxis (rapid migration of neutrophils to sites of inflammation), eventually resulting in blister formation

• Antibody deposition leads to complement activation and neutrophil chemotaxis, which eventuates in loss of adhesion at the dermal-epidermal junction and in blister formation. At the molecular level, a variety of antigens have been identified, some of which are also seen in patients with bullous pemphigoid. LAD may thus be an umbrella term for a wide range of conditions, each involving a different antigen; however, further research is needed. [1]
The immune pathology appears to be identical in adults and children.
• Epidemiology[1]
• This is a rare condition.The incidence in adults in southern England has been estimated to be 1 case in 250,000 population per year. There are no figures for the incidence in children. Some studies have reported a slight preponderance of women.
The distribution of the age of onset seems to follow a bimodal pattern. In children, the age range is from 6 months to 10 years, with a mean of 3.3-4.5 years. In adults, the range is from 14-83 years with a mean of 52 years. Drug-induced disease is more prevalent in older people, probably because they are most likely to be on medication.
• Presentation[1][2][3]
• History• Before the appearance of the rash, there may be chronic
pruritus or acute itching or burning. Patients developing ocular lesions may initially note pain, grittiness or discharge.
As with any patient presenting with a rash, a detailed medication history should be taken. The rate of spread of the blisters is variable. They tend to appear quickly in drug-induced cases. In vancomycin-induced cases the onset ranges from 1-13 days after the first dose.
• Examination• Several skin presentations may occur:• Clear round or oval blisters on normal underlying skin• Small blisters (vesicles) or large ones (bullae), often target-
shaped, surmounting an erythematous area of skin which is flat or raised
• New vesicles developing in a ring around the old one (the 'string of beads' sign)
• A crop of vesicles developing close together ('cluster of jewels' sign)
• Crusts, scratch-marks, sores and ulcers• Lesions which mimic erythema multiforme, bullous
pemphigoid and dermatitis herpetiformis.• 50% of patients have blisters and ulcers around the mouth
and lips• Ophthalmological findings may include subconjunctival
fibrosis and shrinkage of the fornices• The distribution of the skin lesions varies between children
and adults. Children tend to get them on the lower abdomen, anogenital areas, perineum, hands, feet and face. In adults, lesions tend more commonly to develop on the trunk and limbs. In both age groups the distribution may be symmetrical or asymmetrical.
• Differential diagnosis• A number of skin conditions have an almost identical
appearance. These include:• Bullous pemphigoid• Dermatitis herpetiformis• Lupus erythematosus• Epidermolysis bullosa acquisita• Investigations[1][2][3]
• Histopathology of a skin biopsy shows subepidermal blistering, differentiating the condition from diseases in which blistering occurs within the epidermis (eg pemphigus).
• Direct immunofluorescence reveals IgA deposition along the basement membrane.
• Serum IgA levels may be raised but this occurs more often in the childhood version.
• Techniques to identify individual antigens within the BMZ are available but these are more research tools than diagnostic investigations.
• Associated diseases[3]
• Chronic renal failure• Immune complex glomerulonephritis• Lymphocytic colitis• Lymphoma• Other malignant tumours• Psoriasis• Rheumatoid arthritis• Sarcoidosis• Ulcerative colitis• Associated drugs• Amiodarone• Atorvastatin• Captopril• Cefamandole• Ceftriaxone• Furosemide• Glibenclamide• Interleukin-25• Lithium carbonate• Metronidazole• Non-steroidal anti-inflammatory drugs• Penicillin• Phenytoin• Somatostatin• Trimethoprim-sulfamethoxazole• Vancomycin• Management[1][2]
• Ruptured lesions and erosions may require sterile dressings. Large bullae do not require any particular treatment if intact. Infection lesions should be treated with topical mupirocin and sterile dressings twice-daily.Dapsone or sulfapyridine are the treatments of choice for non drug-related dermatitis. Sulfapyridine causes fewer adverse effects but is not as effective as dapsone in all cases.Other treatments which have been reported to help some patients include:
• Corticosteroids (prednisone or prednisolone)• Tetracycline antibiotics• Erythromycin• Colchicine• Mycophenolate mofetil• Intravenous immunoglobulins• In drug-related disease, removal of the offending drug
usually results in resolution, although this can take up to two weeks. Corticosteroids have been required to hasten resolution in severe cases.
• Hospital referral• Dermatological referral will be required for the initial
diagnosis.• An ophthalmological opinion will be required once
diagnosis has been made, irrespective of whether the patient has any eye symptoms, as changes may be detected on examination (eg subconjunctival fibrosis) before complications arise.
• Complications[1]
• Complications are usually the result of scarring. Lesions on the gums can result in desquamative gingivitis resulting to damage to the teeth. Ocular linear IgA may mimic cicatricial pemphigoid and lead to blindness. There have been reports of involvement of the pharynx, larynx, nose, rectum and oesophagus.
• Prognosis[1]
• In children, most idiopathic cases resolve within two years. In adults the disease is more protracted. Resolution does eventually occur; the mean duration is 5.6 years but it has been known to last for 15 years. The condition tends to wax and wane in severity.
One study of twelve women found that the condition was improved during pregnancy. No fetal damage was found as a result of the treatment (dapsone) or the disease

This pt would be predicted to have a higher risk for which one?
1. Cirrhosis2. Coronary artery disease 3. Gout4. Hemorrhagic stroke5. Hypothyroidism
Q:

2. Coronary artery disease
A diagonal crease in the earlobe that runs backward from the tragus at a 450 across the lobule to the rear edge of auricle may be a predictor of CADIt is thought to indicate premature aging and loss of dermal and vascular elastic fibers, has limited sensitivity, and appears to most useful in persons <60y

What is the probable Dx?

Cutaneous Leishmaniasis82y M: swollen L ear, difficulty hearing
• Topical glucocorticoids x4mo: no response
• PE: ear enlarged, indurated, red, no LAP. No
visceromegaly
• Biopsy: chr. inflam. infiltration in dermis, confluent
epithelioid granulomas, lymphocytic background. Abundant amastigotes in dermal macrophages (B)
• L infantum in culture and PCR
• Rx with amphotericin B, with complete resolution after 2mo (C) and recovery of hearing loss

What is the most likely Dx in a FT neonate with electrolyte imbalance and this exam finding?
1. CAH2. Hypospadias with cryptorchidism3. Preterm ovarian hyperstimulation syn4. Turner5. Mixed gonadal dysgenesis

Cong. adrenal hyperplasia
Evaluation of this neonate with ambiguous genitalia revealed bilateral adrenal hypertrophy, a markedly raised 17-OH progesterone, 46 XX. Salt-losing CAH due to 21-hydroxylase deficiency


• A FT infant with ambiguous genitalia (A); no FH; noted to have HR 179, no hypotension
• Lab.: K 7.4mmol/L, Na 125mmol/L, 17-OH progesterone 196μg/L ( 0.5-2.4μg/L), testosterone >15ng/ml (0.1-0.8ng/ml)
• USG: bilat. adrenal hypertrophy, no visible testes. 46 XX• Salt-losing CAH (21-OHase deficiency)
• Hypertrophy of clitoris and l. majora and presence of a urogenital sinus, may resemble hypospadias with cryptorchidism in males
• Rx of dyselectrolytemias, glucocorticoid, mineralocorticoid. At 2 y, she underwent surgical reconstruction

A 3mo F with swelling of ext. genitalia; born at 27w, stayed 75d in NICU; well at discharge. Her clitoris and vulva were swollen (A); otherwise ok. What is the most probable Dx?1. CAH2. Preterm Ovarian Hyperstimulation3. Testicular feminizing syn4. Hermaphroditism5. Bilat. Inguinal hernia

• Lab: raised S. estradiol 310pmol/L (20-40); FSH 17.2 mIU/ ml (0.5-2.4); LH 4.7mIU/ml (.01-.21)
• USG: 2 cysts on the R ovary

2. Preterm Ovarian Hyperstimulation
• Prematurity, vulvar swelling, elevated estradiol and FSHs, ovarian cysts• Self-limiting and resolves spontaneously• Serial FSH and estradiol levels were done during FU4w after, the estradiol peaked at 700 pmol/L and then declined, with both normalized. 6w later, swelling had reduced (B), complete resolution by 14w (C)Repeat US: ovarian cysts had disappeared. At 12mo: ok

What is the most likely c/of this in a man from Mexico; biopsy showing gram-negative bacilli?
1. K rhinoscleromatis2. M leprae3. Acinetobacter baumannii4. T pallidum5. M tuberculosis

Klebsiella rhinoscleromatis
Rhinoscleroma is a chr. bacterial inf. typically c/by G-ve K. rhinoscleromatis. Responds to tetracycline/ciprofloxacin.

What is the Dx in this asymptomatic M from N Africa?1. Cutaneous leishmaniasis2. Myiasis3. Paronychia4. Syphilis5. YawsQ
:


1. Cutaneous leishmaniasis
The verrucous lesion at the base of the thumb does not have the appearance of chr. paronychia; a skin smear revealed amastigote forms of the leishmania parasite

What is the Dx?

• 18y M has a 3-mo coughing, hemoptysis, wt loss, F; a small swelling on ant. chest 1w
• CT: a collar-button abs (sc abs. connected to a deeper abs. by a passage): an abs. in a LN in L mediastinum (A, red arrow) connected to sc abs (A, blue arrow); an extensive parenchymal abnormality in the LUL. A sputum: AFB, and a CS: pansusceptible M tb. HIV negative. He received 8 w standard ATD, but the infx. progressed, with increased swelling, erythema, and fluctuation (B and C). The abs was drained. Drug Rx of a tb. abs is seldom sufficient, an open drainage/excision is often needed. He has been without s/of relapse since surgery but required cosmetic surgery
TB Abscess


Sialolith

What is the most likely Dx in this 65y F with a 7d sore throat and dysphagia?1. Epiglottitis2. Foreign body aspiration3. Peritonsillar abscess4. Retropharyngeal abscess5. Thyroid nodule

1. Epiglottitis
The lateral soft-tissue XR: the “thumb sign” that indicates a swollen inflamed epiglottisDx was confirmed on subsequent imaging and laryngoscopyShe recovered with dexa- and ceftriaxone

EpiglottitisShe had muffled voice, hemodynamically stable PaO2 98% in
ambient air• PE: mild tenderness and swelling in the anterior neck, no
CxLAP or drooling. Lateral soft-tissue radiography of the neck showed the “thumb sign” (Panel A, arrow): epiglottis
• CT: substantial swelling and edema of the epiglottis (Panel B, arrow), the base of the tongue, and the lingual tonsil
• Indirect laryngoscopy: red inflamed epiglottis and the base of the tongue, with clinically significant hypertrophy of the lingual tonsil and phlegm in the throat
• Ceftriaxone and dexamethasone were initiated• She was monitored closely 48h. Blood cultures negative• SS improved, and within 3d, she was able to consume an
oral diet. She was discharged home


What is the most likely Dx?
1. Candidiasis2. Geographic tongue3. H zoster 4. Lichen planus5. Pemphigus

3. Herpes zoster
Vesicles along V3 trigeminal dermatome, including the L tongue and mandible, are most consistent with h zosterHe got 2w oral valacyclovir

What is the most likely c/of this long-standing skin finding?
1. Acromegaly2. McCune-Albright syn3. Neurofibromatosis4. Shingles5. Speckled lentiginous naevi

3. Neurofibromatosis
Biopsy was consistent with a neurofibromaDx of segmental neurofibromatosis, a variant of NF characterized by neurofibromas or café au lait macules (or both) that are confined to 1 segment. No specific Rx

What is most probable Dx in this shepherd?
1. H. whitlow2. Anthrax3. MRSA4. Contagious ecthyma5. Impetigo

• 34y M farmer: a painful pustular rash on hands (A B); worsening over 18d. He manages livestock. It began a few days after a sheep bit his L hand while being bolus-fed. He is expert in sheep care and says multiple sheep had “sore mouth.” He did not wear gloves
• PE: otherwise ok
• Swabs PCR: confirmed contagious ecthyma c/by orf virus. This is typically self-limiting
• Rx: wound care and ABT for ?bacterial superinf: recovered fully/3w. He was advised to use gloves when he handles animals or contaminated equipment

Ecthymaa skin inf. similar to impetigo; often called deep impetigoCauses: most often c/by Strep. Sometimes, Staph• may start in injured skin (scratch or insect bite). Often
develops on legsSymptoms: Main is a small blister with a red border that may
be filled with pus similar to impetigo, but much deeper• After the blister goes away, a crusty ulcer appearsExams and Tests: diagnosed simply by inspection. Rarely the
fluid is sent for exam, or a biopsy is neededRx: usually ABT oral or topical. Serious inf: IV antibiotics• Placing a warm, wet cloth over the area can help remove
ulcer crusts. Your doctor may recommend antiseptic soap or peroxide washes to speed recovery

“Sore Mouth” (contagious ecthyma, orf)• aka “scabby mouth,” or CE is a viral inf. c/by a the poxvirus
primarily of sheep and goats• common throughout the world
Sore mouth in goat kid.

What is the Dx?
1. Ac lymphangitis2. Cellulitis3. Deep VT4. Myositis5. Superficial thrombophlebitis
Q:

1. Acute lymphangitis
The erythematous and irregular linear streak extending from the hand to the axilla is most consistent with ac. LymphangitisCS: S pyogenes; he recovered with IV penicillin G

• 23y M: rapidly progressive L arm pain and erythema• He had felt well until the previous night, when his L 3rd
finger was injured during a lacrosse game. Overnight, the finger became increasingly painful, with erythema spreading to wrist. Temp: 36.7°C, HR 64/min, BP 139/85mmHg
• PE: a small blister or abscess on 3rd L finger with local heat, tenderness, erythema, linear streaking to the elbow. Within hours, the streaking progressed to the axilla
• Swab was cultured. He quickly underwent incision and drainage of the lesion, and empirical cefazolin and vancomycin. CS: S pyogenes, and AB changed to IV penicillin G; discharged with oral penicillin V

What is the Dx in this case with AP?
1. GI stromal tumor2. Obstipation3. Pancreatic phlegmon4. Subphrenic abscess5. Trichobezoar

5. Trichobezoar
The heterogeneous, meshlike mass extending from the stomach into the duodenum is most consistent with a bezoar. The patient, who had trichotillomania, recovered after laparotomy and removal of the bezoar

What is the most likely Dx in this pt. from Mauritania whose foot had developed these over several years?
1. Actinomycetoma2. Kaposi’s sarcoma3. Leishmaniasis4. Malignant melanoma5. Yaws

1. Actinomycetoma
Mycetoma, commonly aka Madura foot, is a chr., localized, slowly progressive, granulomatous infx. of deep dermis and s.c. tissue c/either by fungi (eumycetoma or implantation mycosis) or by aerobic actinomycetes (actinomycetoma)
Actinobacteria was confirmed on punch biopsyHe responded to amikacin and cotrimoxazole

A 64-year-old man from Mauritania was referred for evaluation of a multinodular tumor of the left foot. Foot lesions had been present for 38 years, starting on the left heel and gradually spreading to involve the whole foot and ankle, with walking impairment. At the time that the patient was first seen, he was in a wheelchair. The patient sought medical care because of fatigue related to anemia of chronic disease (hemoglobin level, 9 g per deciliter). He did not report problems with his foot, being accustomed to this condition. Examination revealed soft-tissue swelling; multiple painless, sometimes ulcerated, weeping tumefactions; and ipsilateral popliteal and inguinal lymphadenopathy (Panel A and Panel B show the dorsal and plantar surfaces of the foot). Magnetic resonance imaging revealed osteomyelitis of the tarsal bones. The suspected diagnosis was a mycetoma, although Kaposi's sarcoma and epithelioma cuniculatum (verrucous carcinoma) were also considered. Pathological analysis of a punch-biopsy specimen with Giemsa staining revealed an inflammatory infiltrate surrounding granules with peripheral “clubs,” identified as actinobacteria. Culture of the specimens did not grow any organism. Amikacin (for 10 days) and trimethoprim–sulfamethoxazole were given. After 1 month, the patient was discharged home and was able to walk with crutches. Ten months later, he was able to walk without assistance and had regained plantar sensitivity. Three years after beginning treatment, he was able to bend the toes and ankle (Panel C and Panel D show the dorsal and plantar surfaces of the foot). Therapy with twice-daily trimethoprim–sulfamethoxazole (160 mg and 800 mg, respectively) has been maintained at the same dose since the beginning of treatment, and improvement of the lesions is still ongoing after 5 years of antibiotic therapy.

What is the most likely Dx with eosinophilia and a diffuse erythematous rash while on hydroxychloroquine for Sjogren?1. Bullous impetigo 2. Exanthematous pustulosis3. Exfoliative dermatitis 4. Stevens-Johnson syn5. Sweet’s syn

2. Exanthematous pustulosis
Yellow hyperplastic papules on the tongue of a hydroxychloroquine-treated pt. with a diffuse erythematous rash is most consistent with hydroxychloroquine-induced ac. generalized exanthematous pustulosis. The lesions resolved following withdrawal and Rx with prednisolone

2y M: 1y refractory
eczema and a 4w Cx LAP
Growth <5th centile,
bilateral proptosis,
serous discharge from
ears, and extensive rash
on scalp, chest, upper
back, palpable defects
in the skull. No HSM or
diabetes insipidus

Langerhans'-Cell Histiocytosis

Lab.: anemia of chr d., (Hb 6.6g/dl), normal TLC, platelet, LFT
• Skeletal survey: multiple lytic lesions in skull
• LN biopsy: consistent with Langerhans'-cell histiocytosis
• He was Rx with prednisone, vinblastine, mercaptopurine
and had a complete recovery
• At 24mo FU: well
• It is a rare histiocytic d, mostly in toddlers
Suspect it in a young child with refractory eczema and chr ear
discharge

What is the Dx in this pt with axillary LAP?1. Bacterial felon2. Erysipelas3. Herpetic whitlow4. Paronychia5. Scabies

3. Herpetic whitlow
Direct fluorescence antibody testing of vesicular fluid confirmed HSV type 2The pt responded to Rx with oral acyclovir