Im-pancreas-procrastinotes (Edited by Jc)
-
Upload
juan-carlos-luna -
Category
Documents
-
view
213 -
download
0
Transcript of Im-pancreas-procrastinotes (Edited by Jc)

7/31/2019 Im-pancreas-procrastinotes (Edited by Jc)
http://slidepdf.com/reader/full/im-pancreas-procrastinotes-edited-by-jc 1/7
Subject: MEDICINETopic: PANCREASDate: JULY 13, 2012Lecturer: Dr. Andal-GamutanTranscriber: RSAEditor: JC LunaPages: 6
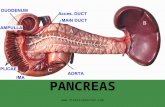
PANCREAS Pancreas is located behind the stomach Usual size is 12-15 cm length, 70 -110
grams Shape is elongated, flattened and
tapered Located at the back of the abdomen
behind the stomach
PHYSIOLOGY OF THE PANCREASThe pancreas has two types of tissues:
Exocrine tissues release enzymes that
are mainly concerned with digestionfound in the acinus and drains into ducts Endocrine tissues consist of the islet of
Langerhans and secretes hormones intothe blood stream (glucagon and insulin)that are mainly concerned with theregulation of carbohydrates
Pancreatic exocrine secretion • 1500 – 3000 ml isosmotic alkaline
(pH>8) fluid per day• 20 enzymes and zymogens• effects the major digestive activity of
GIT• provides an optimal pH for the function
of these enzymes
REGULATION OF PANCREATIC SECRETION • Gastric acid secretin p. juice rich in
H2O & elect.• Long chain FA, essential AA
(tryptophan, phenylalanine, valine,methionine) & gastric acid CCK enzyme-rich secretion (from acinar cellsin the pancreas).
• Gastrin weak stimulus for p. enzymeoutput
• Bile pancreatic secretion• Somatostatin --/pancreatic secretion
From Harrisons 18 th
editionThe exocrine pancreas is influenced by intimately interacting hormonal and neural systems. Gastric acid is the stimulus for therelease secretin from the duodenum, whichstimulates the secretion of water and electrolytes from pancreatic ductal cells.Release of Cholecystokinin (CCK) from theduodenum and proximal jejunum is triggered by long chain fatty acids, certain essential amino
acids (tryptophan, phenylalanine, valine,methionine) and gastric acid itself.
Water & electrolyte secretion
Bicarbonate – it is the ion of primary physiologicimportance within pancreatic secretion. It helpsneutralize gastric acid and creates theappropriate pH for the activity of the pancreaticenzymes.
PANCREAS Enzyme secretion - secretes amylolytic,lipolytic, and proteolytic enzymes. The acinar cell is highly compartmentalized and isconcerned with the secretion of pancreatic
enzymes.
Autoprotection - Auto digestion of thepancreas is prevented by the packaging of pancreatic proteases in precursor form and bysynthesis of protease inhibitor, which can bindand inactivate 20% of trypsin activity.
TESTS USEFUL IN THE DIAGNOSIS OFPANCREATIC DISEASES Pancreatic enzymes
amylase - elevated for 5 days lipase – obtain if more than 1 week trypsinogen pancreatic polypeptide
Pancreatic structure Radiologic and radionuclide tests Pancreatic biopsy with US or CT
guidance CT Scan is the best imaging study
From Harrisons 18
thedition
A CT Scan can confirm the clinical impression of acute pancreatitis even with less than athreefold increase in serum amylase and lipaselevels. Importantly, CT can be helpful indicating the severity of acute pancreatitis and the risk of morbidity and mortality and in evaluating the
complications of acute pancreatitis.Exocrine pancreatic function
direct stimulation – secretin indirect stimulation – nutrients followed
by assays of proteolytic, lipolytic andamylolytic enzymes
intraluminal digestion products –undigested meat, fibers, stool fat
rarely done, not available in RP measurement of fecal pancreatic
enzymes – elastase
ACUTE PANCREATITIS
Incidence: varies, depends on cause, e.g., alcohol,
gallstones, metabolic factors, drugsCommon Causes of Acute Pancreatitis
Gallstones – leading cause of AP Alcohol -2
ndmost common cause
Hypertriglyceridemia Postoperative state ERCP

7/31/2019 Im-pancreas-procrastinotes (Edited by Jc)
http://slidepdf.com/reader/full/im-pancreas-procrastinotes-edited-by-jc 2/7
Trauma Drugs Sphincter of Oddi dysfunction
CAUSES OF ACUTE PANCREATITIS Drugs for which association is definite
Azathioprine, 6-mercaptopurine Sulfonamides Thiazide diuretics Furosemide (common) Estrogen (oral contraceptives)
(common) Tetracycline (common) Valproic acid Pentamidine Dideoxyinosine
Drugs for which association is probable Acetaminophen (common) Nitrofurantoin
Methyldopa Erythromycin (common) Salicylates Metronidazole NSAIDS ACE inhibitors
UNCOMMON CAUSES OF ACUTEPANCREATITIS
Vascular causes and vasculitis Connective tissue disorders and
Thrombotic Thrombocytopenic Purpura Cancer of the pancreas
Hypercalcemia Periampullary diverticulum Pancreas divisum Hereditary pancreatitis Cystic fibrosis Renal failure
Vascular causes and Vasculitis Vascular
o Ischemic hypoperfusion state(after cardiac surgery)
o Atherosclerotic embolio
Aneurysm of celiac axis/ hepaticartery Connective tissue disorders with
Vasculitiso SLEo Necrotizing angitiso Thrombotic, thrombocytopenic
purpuraPenetrating peptic ulcer Obstruction of the ampulla of Vater
Regional enteritis Duodenal Diverticulum
RARE CAUSES OF ACUTE PANCREATITIS Infections
Mumps Viral hepatitis Other viral infections (coxsackievirus,
echovirus, cytomegalovirus) Ascariasis Mycoplasma, Campylobacter,
Mycobacterium avium complex, other bacteria
Autoimmune (e. g., Sjogren’s syndrome)
CAUSES OF ACUTE PANCREATITIS Causes to be considered in patients havingrecurrent bouts of acute pancreatitis without anobvious cause:
Occult disease of the biliary tree or pancreatic ducts, especially occultgallstones (microlithiasis, sludge)
Drugs Hypertriglyceridemia Pancreas divisum Pancreatic cancer Sphincter of Oddi dysfunction Cystic fibrosis Truly idiopathic
From Harrisons 18 th
edition
There are many causes of acute pancreatitis,but the mechanism by which these conditionstrigger pancreatic inflammation have not beenfully elucidated. Gallstones continue to be theleading cause of acute pancreatitis (30-60%) Alcohol is the second most common cause,responsible for 15-30% of cases in the US.
PATHOGENESIS Drugs: hypersensitivity reaction or generation of a toxic metabolite (in some cases it is not clear which of these mechanisms is operative)
Autodigestion theory: proteolytic enzymes areactivated in the pancreas rather than in theintestinal lumen
Autodigestion is a currently accepted pathogenic theory; according to it, pancreatitis results when proteolytic enzymes (eg. Trypsinogen,chymotrypsinogen, proelastase, and lipolytic enzymes such as phospholipase A2) areactivated in the pancreas rather than in theintestinal lumen.
Factors: endotoxins, exotoxins, viral infections,
ischemia, anoxia, direct trauma. -> Proteolyticenzyme, trypsinogen, chymotrypsinogen,protease, Phospholipase A. Once theseproteolytic enzymes are activated in thepancreas rather than in the intestinal lumen, itwill cause pancreatitis.
Activated proteloytic enzymes (trypsin) -> digestpancreatic and peripancreatic tissues -> other enzymes (elastase and phospholipase) ->digest cellular membrane -> proteolysis, edema,interstitial hemorrhage, vascular damage,coagulation necrosis, fat necrosis, parenchymalcell necrosis - > cell injury -> death- Once the proenzymes are activated it willcause a cascading catastrophic effect on thepancreas and the surrounding local and distanttissues.- Editor’s note: please read Harrison’s Principlesof Internal Medicine, 18
thEd. Chap 313, p. 2636
for a detailed discussion of “Activation of

7/31/2019 Im-pancreas-procrastinotes (Edited by Jc)
http://slidepdf.com/reader/full/im-pancreas-procrastinotes-edited-by-jc 3/7
Pancreatic Enzymes in the Pathogenesis of Acute Pancreatitis”
Cellular injury and deathLiberation of: bradykinin peptides,
vasoactive substances &histamine
- Vasodilation- Increased vascular permeability- Edema with profound effects on many organs –most notably the lung - SIRS and ARDS as well as multiorgan failure- Cascade of local as well as distant effects
Pathogenesis Activation of Pancreatic Enzymes3 Phases
1. Intrapancreatic digestive enzymeactivation and acinar cell injury -consequence of zymogen activation
2. Activation, chemoattraction andsequestration of neutrophils in thepancreas resulting in intrapancreaticinflammatory reaction of variableseverity
3. Effects of activated proteolytic enzymesand mediators, released by inflamedpancreas, on distant organs.
CLINICAL FEATURES Abdominal pain – major symptom,
steady and boring, radiating to the back
50% of the cases, lasting for severalhours, sudden in onset, severe 8/10
Nausea, vomiting, abdominal distension – due to gastric hypomotility
On physical exam patient appearsdistressed and anxious
Low-grade fever Tachycardia Hypotension Shock (uncommon): (1) retroperitoneal
burn- hypovolemia due to exudation of blood and plasma proteins into theretroperitoneal space, (2) increased
formation and release of kinin peptides – vasodilation & increased permeability,and (3) systemic effects of proteolytic &lipolytic enzymes
Jaundice – due to the edema of thehead of the pancreas with compressionof the intrapacreatic portion of thecommon bile duct.
Erythematous skin nodules –subcutaneous fat necrosis
Pulmonary findings (10-20%) – basilar rales, atelectasis, and pleural effusion(most frequently left-sided)
Cullen’s sign – faint blue discolorationaround the umbilicus, may occur as aresult of hemoperitoneum
Turner’s Sign – A blue-red-purple or green-brown discoloration of the flanks;reflects tissue catabolism of hemoglobin
LABORATORY DATA 1. Amylase and Lipase - 2 most important
2. Trypsin3. Leukocytosis (15,000 – 20,000/µL)4. Hemoconcentration – because of
exudation of plasma5. Hyperglycemia – impairment of islet cell
functioning decreased insulin andglucagon
6. Hypocalcemia – because of saponification
7. Hyperbilirubinemia8. Alk. Phos, ALT, AST9. LDH >500U/dL – poor prognosis10. Hypoalbuminemia11. Hypertriglyceridemia Lipid profile usually
more than 1,00012. Hypoxemia
DIAGNOSIS – 2 of the following: Typical abdominal pain
threefold or greater elevation in serumamylase and / or lipase level and / or
Confirmatory findings on cross-sectionalabdominal imaging
Markers of severity –hemoconcentration (hct>44%),azotemia(BUN>22mg/dL) and signs of organ failure
DIFFERENTIAL DIAGNOSIS 1. Perforated viscus2. Acute cholecystitis and biliary colic
3. Acute intestinal obstruction4. Mesenteric vascular occlusion5. Renal colic6. Myocardial infarction7. Dissecting aortic aneurysm8. Connective tissue disorders with
vasculitis9. Pneumonia10. Diabetic ketoacidosis
Factors that Adversely Affect the Survival inAcute PancreatitisRanson/Imrie criteria
- poor predictive value; many clinicians nolonger use this; very hard to apply.1. At admission or diagnosis
a. Age >55 yearsb. Leukocytosis>16,000/uLc. Hyperglycemiad. Serum LDH>400IU/Le. Serum AST>250IU/L
2. During initial 48 ha. Fall in hematocrit by >10%b. Fluid deficit of >4000mlc. Hypocalcemia(<8 mg/dLd. Hypoxemia (PO2<60mmHg)e. Increase in BUN to > 1.8mmol/L
after IV administrationf. Hypoalbunemia
>3 Ranson’s signs Acute physiology and chronic health evaluation(APACHE II) score >8 Hemorrhagic peritoneal fluidObesity(BMI>29)

7/31/2019 Im-pancreas-procrastinotes (Edited by Jc)
http://slidepdf.com/reader/full/im-pancreas-procrastinotes-edited-by-jc 4/7
Risk Factors for Severity- Age > 60 years- Obesity, BMI > 30- Comorbid disease (DM increases the
risk for severity )
Markers of Severity within 24 hrs SIRS (temp>38 or 36 C, pulse>90 PR,
tachypnea>24 RR, elevatedWBC>12,000
Hemoconcentration BISAP (bedside index of severity in
acute pancreatitis) – BUN>22mg%,Impaired mental status, SIRS:2/4present, Age>60yrs, Pleural effusion
*3 or > associated increased risk of in hospitalmortality*
Organ Failurea. Cardiovascular hypotension (BP <
90mmHg) or tachycardia>130 beats/minb. Pulmonary: PaO2<60mmHgc. Renal: oliguria(<50ml/h) or increasing BUN,
creatinine >2mg%d. Gastrointestinal bleeding>500ml/24hours
*Single organ system failure 3-10%mortality*Multisystem organ failure 47%mortality
Local complicationsa. necrosisb. pseudocystc. abscess
Markers of Severity During Hospitalization Persistent organ failure Pancreatic necrosis Hospital – acquired infection
RISK FACTORS THAT ADVERSELY AFFECTSURVIVAL IN ACUTE PANCREATITIS
CT SEVERITY INDEX IN ACUTEPANCREATITIS Points
Grade of acute pancreatitis A. Normal pancreas 0
B. Pancreatic enlargement 1C. Inflammation compared with p.&peripancreatic fat 2
D. One peripancreatic fluid collection3
E. Two or more fluid collections 4Degree of pancreatic necrosis
A. No necrosis 0B. Necrosis of one-third of pancreas
2C. Necrosis of one-half of pancreas
4D. Necrosis of more than one-half of
pancreas 6----------------------------------------------------------------3-6 scores --- negligible7-10 --- 92% morbidity rate & 17%mortality ratePresence of necrosis – morbidity >20%With out necrosis - morbidity<10%, negligiblemortality rate
Course of acute pancreatitis 2 phasesFirst phase – 1-2wks, severity is defined byclinical parameters rather than morphologicfinding persistent organ failure(>48hrs) – causeof deathSecond phase – both clinical parameters(organ failure) and morphologic criteria(necrotizing pancreatitis). Median prevalence of organ failure is 54% in necrotizing pancreatitis(10% of acute pancreatitis)
Complications of Acute Pancreatitis
1. Local
a. Necrosis
i. Sterile
ii. Infected
iii. Walled-off necrosis
b. Pancreatic fluid collectionsi. Pancreatic abscess
ii. Pancreatic pseudocyst
iii. Pain
iv. Rupture
v. Hemorrhage
vi. Infection
vii. Obstruction of
gastrointestinal tract
(stomach, duodenum,
colon)
c. Pancreatic ascites
i. Disruption of main
pancreatic duct
ii. Leaking pseudocyst
d. Involvement of contiguous organs
by necrotizing pancreatitis
i. Massive intraperitoneal
hemorrhage
ii. Thrombosis of blood
vessels (splenic vein,
portal vein)
iii. Bowel infarction
e. Obstructive jaundice
2. Systemic
a. Pulmonary
i. Pleural effusion
ii. Atelectasis
iii. Mediastinal abscess
iv. Pneumonitis
v. Acute respiratory distress
syndrome
b. Cardiovascular
i. Hypotension
ii. Hypovolemia
iii. Sudden death
iv. Nonspecific ST-T changes
in electrocardiogram
simulating myocardial
infarction
c. Pericardial effusion

7/31/2019 Im-pancreas-procrastinotes (Edited by Jc)
http://slidepdf.com/reader/full/im-pancreas-procrastinotes-edited-by-jc 5/7
d. Hematologic
i. Disseminated
intravascular coagulation
e. Gastrointestinal hemorrhage
i. Peptic ulcer disease
ii. Erosive gastritisiii. Hemorrhagic pancreatic
necrosis with erosion into
major blood vessels
iv. Portal vein thrombosis,
variceal hemorrhage
f. Renal
i. Oliguria
ii. Azotemia
iii. Renal artery and/or renal
vein thrombosis
iv. Acute tubular necrosis
g. Metabolic
i. Hyperglycemia
ii. Hypertriglyceridemia
iii. Hypocalcemia
iv. Encephalopathy
v. Sudden blindness
(Purtscher's retinopathy)
h. Central nervous system
i. Psychosis
ii. Fat emboli
i. Fat necrosis
i. Subcutaneous tissues
(erythematous nodules)
ii. Bone
iii. Miscellaneous
(mediastinum, pleura,
nervous system)
TREATMENT Conventional Measures
1. Analgesics for pain – Meperidine does
not cause spasm of the sphincter of oddi2. Intravenous fluids and colloids to
maintain normal intravascular volume3. No oral alimentation (NPO) – food can
stimulate pancreatic secretion4. Nasogastric suction to decrease gastrin
release from the stomach and preventgastric contents from enteringduodenum
*Prophylactic antibiotics for severe pancreatitis
COMPLICATIONS
Infected pancreatic necrosis Diffuse infection of an acutely inflamed,necrotic pancreas
Occurring in the first 1-2 weeks after theonset of acute pancreatitis
Should be treated by surgicaldebridement
Clinical clues that should alert theclinician to the possibility of infected
necrosis are persistent fever,leukocytosis, and organ failure in apatient with necrotizing pancreatitis
Pancreatic abscess ill-defined , liquid collection of pus that
evolves over a longer period, often 4-6weeks
Pseudocyst Collections of tissue, fluid, debris,
pancreatic enzymes and blood develop over a period of 1-4 weeks
after the onset of acute pancreatitis
Walled-off necrosis organized necrosis coalescence of the pancreatic necrosis
and peripancreatic fat necrosis intostructure that is encapsulated by fibrous
tissues contains semisolid necrotic tissue
together with a considerable amount of dark fluid representing liquifaction of devitalized pancreatic andperipancreatic tissue as well as someblood
Walled-Off necrosis and a pancreaticpseudocyst may look very similar on firstinspection of a contrast-enhanced CTscan
On closer inspection, serial imagesshow that a portion of the pancreas as
well as variable amounts of peripancreatic tissue are necrotic
Pancreatic ascites due to disruption of the main pancreatic
duct, often by an internal fistula betweenthe duct and the peritoneal cavity or aleaking Pseudocyst
Elevated serum amylase level in whomthe ascites fluid has both increased levelalbumin & markedly elevated level of amylase
ERCP/MRCP confirms the clinical
suspicion and radiologic findings andoften demonstrates passage of contrastmaterial from a disrupted major pancreatic duct or Pseudocyst into theperitoneal cavity.
Treatment: nasogastric suction &parenteral alimentation, paracentesis,long acting Somatostatin analogueoctreotide
CHRONIC PANCREATITIS Chronic inflammatory disease of the
pancreas Characterized by irreversible damage to
the pancreas as distinct from thereversible changes noted in acutepancreatitis
o presence of histologicabnormalities, including chronicinflammation, fibrosis, andprogressive destruction of both

7/31/2019 Im-pancreas-procrastinotes (Edited by Jc)
http://slidepdf.com/reader/full/im-pancreas-procrastinotes-edited-by-jc 6/7
exocrine and eventuallyendocrine tissue
Pathophysiology Alcohol-induced – precipitation of
protein (inspissated enzymes) in theducts
There is a strong association of smoking and chronic pancreatitis. Cigarettesmoking leads to an increased susceptibility to pancreatic self-digestion. Smoking is an independent,dose dependent risk factor for chronic pancreatitis.
duct dilatation, diffuse atrophy of acinar cells, fibrosis & calcification
Direct toxic effects on the pancreas
CAUSES 1. Alcohol, chronic alcoholism2. Idiopathic pancreatitis3. Cystic fibrosis4. Hypertriglyceridemia5. Severe protein-calorie malnutrition w/
hypoalbuminemia6. Pancreatic and duodenal neoplasm7. Pancreatic resection8. Gastric surgery9. Gastrinoma10. Hereditary pancreatitis11. Traumatic pancreatitis
12. Abdominal radiotherapy13. Hemochromatosis14. Enterokinase deficiency
CLINICAL FEATURES Symptoms identical to acute pancreatitis Pain may be continuous, intermittent or
absent Weight loss Abnormal stools, malabsorption
From Harrisons 18 th
edition
Patients with chronic pancreatitis seek medical attention predominantly because of twosymptoms: abdominal pain or maldigestion and weight loss.The abdominal pain may be quite variable inlocation, severity and frequency. The pain canbe constant or intermittent with frequent pain-free intervals. Eating may exacerbate pain,leading to a fear of eating with consequent weight loss. Many patients have impaired glucose tolerance with elevated fasting blood glucose levels. The diagnostic test best sensitivity and specificity is the hormonestimulation test utilizing secretin.
DIAGNOSIS 1. Amylase and lipase – not elevated2. Classic triad
pancreatic calcification – 1/3 steatorrhea diabetes mellitus
3. Intubation test – secretin stimulation test4. Cobalamin malabsorption – pancreatic
enzymes5. Marked excretion of fecal fat – p.
enzymes6. Decreased serum trypsinogen level7. Radiographic hallmark – calcification8. Sonography, CT, ERCP
Abdominal USG, CT scanning, and MRCP greatly aid in the diagnosis of pancreatic disease. In addition to excluding Pseudocyst and Pancreatic CA, CT may show calcification,dilated ducts or an atrophic pancreas. MRCP provides direct view of the pancreatic duct and isnow the diagnostic procedure of choice.
COMPLICATIONS 1. Cobalamin malabsorption2. Effusions – pleural, pericardial, or
peritoneal space
3. GI bleeding – peptic ulceration,gastiritis, pseudocyst eroding toduodenum, esophageal varices
4. Cholangitis5. Subcutaneous fat necrosis6. Bone pain7. Pancreatic cancer 8. Addiction to narcotics
TREATMENT Directed to two major problems
Pain Malabsorption
Painabstinence: alcohol & fatty mealsuse of narcoticspancreatic enzymes ,surgery
Malabsorptionpancreatic enzyme replacementsupportive measures
PANCREATIC CANCER 90% moderately differentiated mucinous
adenocarcinoma derived frompancreatic duct epithelium
5% islet cell origin
More common in men than in women Risk factors: cigarette smoking, alcoholconsumption gallstones, animal fat-richdiet, DM, chronic pancreatitis
Clinical manifestations are related tocompression or invasion the adjacentvital structures jaundice, pruritus, abd.pain, wt. loss
Diagnosiso No single laboratory testo Ultrasound and CTscano ERCP
Managemento Surgeryo Palliative management
For more info, read Harrison’s Principles of InternalMedicine, 18
thEd. Chap 313
END OF TRANSCRIPTION
“Learn as though you would never be able to master it; holdit as if you would be in fear of losing it” - Confucius

7/31/2019 Im-pancreas-procrastinotes (Edited by Jc)
http://slidepdf.com/reader/full/im-pancreas-procrastinotes-edited-by-jc 7/7