II. Mechanisms for Arrhythmias
Transcript of II. Mechanisms for Arrhythmias
-
8/14/2019 II. Mechanisms for Arrhythmias
1/29
1
Antiarrhyth.JDH
(MED 2/08)
30
II. MECHANISMS FORARRHYTHMIAS
Antiarrhyth.JDH
(MED 2/08)
31
A. Definition of Arrhythmias
-abnormality in rate, regularity, site oforigin, and/or sequence of activation
-they range in severity.
B. Abnormalities of Impulse Generation
1. Altered Normal Automaticity
2. Triggered Impulses (afterdepolarizations)
C. Abnormality of Conduction - Re-entryMechanisms
-
8/14/2019 II. Mechanisms for Arrhythmias
2/29
2
Antiarrhyth.JDH
(MED 2/08)
32
B. Abnormalities of Impulse Generation
1. Altered Normal Automaticity- change in spontaneous phase 4 depolarization
Affects primarily SA node and His-Purkinje fibers but in disease states, suchas from ischemia, ventricular cells can also spontaneously depolarize.
Antiarrhyth.JDH
(MED 2/08)
33
1. Altered Normal Automaticity
Favor RAPID phase 4Depolarization
Sympathetic nervous system
Catecholamines
Hypokalemia
Cell damage
ischemia
myocardial stretch
trauma
Drugsatropine
cardiac glycosides
(His-Purkinje)
Favor SLOW phase 4Depolarization
Parasympathetic nervous
system Acetycholine
Hyperkalemia
DrugsClass 1 antiarrhythmics -
quinidine
verapamil
propranolol
-
8/14/2019 II. Mechanisms for Arrhythmias
3/29
3
Antiarrhyth.JDH
(MED 2/08)
34
2. Triggered Impulses
normal action potential is interrupted orfollowed by an abnormal depolarization.Early and delayed afterdepolarizations.
a. Early afterdepolarizations (EAD)
b. Delayed afterdepolarizations (DAD)
B. Abnormalities of Impulse Generation
Antiarrhyth.JDH
(MED 2/08)
35
b. Delayed Afterdepolarizations (DAD)
- secondary depolarizations that occur after full repolarizationhas developed.
1) Phase 0 carried by sodium with fast conduction.2) Factors associated with DAD include:
- High intracellular Ca2+ load (ischemia, cardiac glycosides)- Increased SNS activity high catecholamines.- fast heart rates
-
8/14/2019 II. Mechanisms for Arrhythmias
4/29
4
Antiarrhyth.JDH
(MED 2/08)
36
a. Early afterdepolarizations (EAD)
secondary depolarizations that occur before repolarization
is complete.1) Phase 0 may be carried by Ca2+, Na+ or mixture
of the two.2) Factors associated with EAD include:
- Increased SNS activity - high catecholamines- Cell damage (hypoxia, mycocardial stretch)- slow heart rate- hypokalemia- More likely with Purkinje cells
** - Prolonged QT interval (delayed repolarization)(increased in slowed HR and prolonged AP)(drug-induced including antiarrhythmics.
antihistamines, antidepressants, others)- Markedly prolonged QT interval predisposes to
torsade de pointes (a form of ventriculartachycardia)
Antiarrhyth.JDH
(MED 2/08)
37
Electrocardiogram from a patient with the long QTsyndrome during two episodes of torsade depointes.
-
8/14/2019 II. Mechanisms for Arrhythmias
5/29
5
Antiarrhyth.JDH
(MED 2/08)
38
a. Early afterdepolarizations (EAD)
secondary depolarizations that occur before repolarization
is complete.1) Phase 0 may be carried by Ca2+, Na+ or mixture
of the two.2) Factors associated with EAD include:
- Increased SNS activity - high catecholamines- Cell damage (hypoxia, mycocardial stretch)- slow heart rate- hypokalemia- More likely with Purkinje cells
** - Prolonged QT interval (delayed repolarization)(increased in slowed HR and prolonged AP)(drug-induced including antiarrhythmics.
antihistamines, antidepressants, others)- Markedly prolonged QT interval predisposes to
torsade de pointes (a form of ventriculartachycardia)
Antiarrhyth.JDH
(MED 2/08)
39
a. Early afterdepolarizations (EAD)
secondary depolarizations that occur before repolarizationis complete.
1) Phase 0 may be carried by Ca2+, Na+ or mixtureof the two.
2) Factors associated with EAD include:
- Increased SNS activity - high catecholamines- Cell damage (hypoxia, mycocardial stretch)- slow heart rate- hypokalemia- More likely with Purkinje cells
** - Prolonged QT interval (delayed repolarization)(increased in slowed HR and prolonged AP)
(drug-induced including antiarrhythmics.antihistamines, antidepressants, others)
- Markedly prolonged QT interval predisposes totorsade de pointes (a form of ventriculartachycardia)
-
8/14/2019 II. Mechanisms for Arrhythmias
6/29
6
Antiarrhyth.JDH
(MED 2/08)
40
a. Early afterdepolarizations (EAD)
secondary depolarizations that occur before repolarization
is complete. 1) Phase 0 may be carried by Ca2+, Na+ or mixtureof the two.
2) Factors associated with EAD include:
- Increased SNS activity - high catecholamines
- Cell damage (hypoxia, mycocardial stretch)- slow heart rate- hypokalemia- More likely with Purkinje cells
** - Prolonged QT interval (delayed repolarization)(increased in slowed HR and prolonged AP)
(drug-induced including antiarrhythmics.antihistamines, antidepressants, others)- Markedly prolonged QT interval predisposes to
torsade de pointes (a form of ventriculartachycardia)
Hereditary longQT Syndromes
Acquired longEAD -> long QT
Antiarrhyth.JDH
(MED 2/08)
41
C. Abnormality of Conduction - Re-entry
II. MECHANISMS FOR ARRHYTHMIAS
A. Definition of ArrhythmiasB. Abnormalities of Impulse Generation
1. Altered Normal Automaticity2. Triggered Impulses (EAD and DAD)
-
8/14/2019 II. Mechanisms for Arrhythmias
7/29
7
Antiarrhyth.JDH
(MED 2/08)
42
C. Abnormality of Conduction - Re-entry
Requires an abnormal conduction pathway to form a
self-propagating circuit
1. Common properties of Re-entry arrhythmias
a. A divided conduction path (anatomical, pathologicalor functional) which would normally extinguish itself
b. Decremental conduction in one path with completeloss of conduction.
c. Re-activation of the extinguished pathway in thereverse direction by the remaining and unopposedpathway.
d. Correct timing of the conduction rate in the active
pathway and the refractory period of the cells in theextinguished pathway.
Responsible for many cardiac arrhythmias.
Antiarrhyth.JDH
(MED 2/08)
43
Re-entry 1
Wave fronts meet and extinguish
-
8/14/2019 II. Mechanisms for Arrhythmias
8/29
8
Antiarrhyth.JDH
(MED 2/08)
44
C. Abnormality of Conduction - Re-entry
Requires an abnormal conduction pathway to form a
self-propagating circuit
1. Common properties of Re-entry arrhythmias
a. A divided conduction path (anatomical, pathologicalor functional) which would normally extinguish itself
b. Decremental conduction in one path with completeloss of conduction.
c. Re-activation of the extinguished pathway in thereverse direction by the remaining and unopposedpathway.
d. Correct timing of the conduction rate in the active
pathway and the refractory period of the cells in theextinguished pathway.
Responsible for many cardiac arrhythmias.
Antiarrhyth.JDH
(MED 2/08)
45
Re-entry 2
(Ischemic) area with decremental conduction(i.e., an area where conduction velocityprogressively slows to zero and then dies out.)
-
8/14/2019 II. Mechanisms for Arrhythmias
9/29
9
Antiarrhyth.JDH
(MED 2/08)
46
C. Abnormality of Conduction - Re-entry
Requires an abnormal conduction pathway to form a
self-propagating circuit
1. Common properties of Re-entry arrhythmias
a. A divided conduction path (anatomical, pathologicalor functional) which would normally extinguish itself
b. Decremental conduction in one path with completeloss of conduction.
c. Re-activation of the extinguished pathway in thereverse direction by the remaining and unopposedpathway.
d. Correct timing of the conduction rate in the active
pathway and the refractory period of the cells in theextinguished pathway.
Responsible for many cardiac arrhythmias.
Antiarrhyth.JDH
(MED 2/08)
47
Re-entry 3 Re-entry current when the unopposedwavefront crosses the same area out
of the refractory period
(Ischemic) area with decremental conduction(i.e., an area where conduction velocityprogressively slows to zero and then dies out.)
-
8/14/2019 II. Mechanisms for Arrhythmias
10/29
10
Antiarrhyth.JDH
(MED 2/08)
48
C. Abnormality of Conduction - Re-entry
Requires an abnormal conduction pathway to form a
self-propagating circuit
1. Common properties of Re-entry arrhythmias
a. A divided conduction path (anatomical, pathologicalor functional) which would normally extinguish itself
b. Decremental conduction in one path with completeloss of conduction.
c. Re-activation of the extinguished pathway in thereverse direction by the remaining and unopposedpathway.
d. Correct timing of the conduction rate in the active
pathway and the refractory period of the cells in theextinguished pathway.
Responsible for many cardiac arrhythmias.
Antiarrhyth.JDH
(MED 2/08)
49
Re-entry 3 Re-entry current when the unopposedwavefront crosses the same area out
of the refractory period
(Ischemic) area with decremental conduction(i.e., an area where conduction velocityprogressively slows to zero and then dies out.)
Whydoesntthe re-entrycurrent dieout too?
-
8/14/2019 II. Mechanisms for Arrhythmias
11/29
11
Antiarrhyth.JDH
(MED 2/08)
50
Re-entry 4
Antiarrhythmic
drugs break are-entry circuitby causing abidirectionalblock.
They do thisby directly orindirectlymodifying therefractory
period of thearea ofdamaged cells
Antiarrhyth.JDH
(MED 2/08)
51
C. Abnormality of Conduction - Re-entry
Requires an abnormal conduction pathway to form aself-propagating circuit
1. Common properties of Re-entry arrhythmias
a. A divided conduction path (anatomical, pathologicalor functional) which would normally extinguish itself
b. Decremental conduction in one path with completeloss of conduction.
c. Re-activation of the extinguished pathway in thereverse direction by the remaining and unopposedpathway.
d. Correct timing of the conduction rate in the activepathway and the refractory period of the cells in the
extinguished pathway.
Responsible for many cardiac arrhythmias.
-
8/14/2019 II. Mechanisms for Arrhythmias
12/29
12
Antiarrhyth.JDH
(MED 2/08)
52
Re-entry: Common mechanism for Arrhythmias
1. Regions of anatomically-split pathways affected byischemia or other injury
2. Re-entry in AV node [paroxysmal supraventriculartachycardia (PSVT)]
3. Developmental pathologies (Wolff-Parkinson-White Syndrome, where an accessory pathwaybridges atria and ventricle in a way that can shortcircuits the AV node).
4. Areas of ischemic injury (MI)
5. Functional re-entry circuit in torsade de pointeinitiated by an EAD.
Antiarrhyth.JDH
(MED 2/08)
53
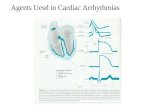
IV. ANTIARRHYTHMIC DRUGS
Class 1
Sodium Channel
Blockers
Class 2
Beta Adrenergic
Blockers
Class 3
Prolong Refractory
Period (Potassium
Channel Blockers)
Class 4
Calcium
Channel
Blockers
Other
A Quinidine
Procainamide
Disopyramide
Propranolol*
Acebutolol
Esmolol
Others
Amiodarone
Bretylium
Sotalol
Ibutilide
Verapamil
Diltiazem Adenosine
Atropine
Digoxin
B Lidocaine
Phenytoin
Mexiletine
C Flecainide
Propafenone
Moricizine
*additional mechanisms at higher concentrations (Class 1B effects)
-
8/14/2019 II. Mechanisms for Arrhythmias
13/29
13
Antiarrhyth.JDH
(MED 2/08)
54
Class 1 Antiarrhythmic Drugs
Class 1A Quinidine (Procainamide, Disopyramide)
Class 1B Lidocaine (Phenytoin, Mexiletine).
Class 1C Flecainide (Propafenone, Morcizine).
Sodium Channel Blockers
Antiarrhyth.JDH
(MED 2/08)
55
Class 1 Antiarrhythmic Drugs
Class 1A Depress phase 0 depolarization (conductionvelocity) in fast response cells and decreasesautomaticity;prolong action potential duration and increaserefractory period. Moderate effects on conduction inNORMAL cells.
Class 1B Depress phase 0 depolarization (conductionvelocity) in fast response cells and can decreaseautomaticity. No significant effect on action potentialduration. Minimal effects on conduction in NORMAL cells
Class 1C Depress phase 0 depolarization (conduction
velocity) in fast response cells and can decreaseautomaticity. Minimal effect on action potential duration.Marked effects on conduction in NORMAL cells.
-
8/14/2019 II. Mechanisms for Arrhythmias
14/29
14
Antiarrhyth.JDH
(MED 2/08)
56
Class 1 Antiarrhythmic DrugsClass 1A Depress phase 0 depolarization (conductionvelocity) in fast response cells and also can depressautomaticity; prolong action potential duration and increaserefractory period. Moderate effects on conduction inNORMAL cells.
Class 1B Depress phase 0 depolarization (conductionvelocity) in fast response cells and can decreaseautomaticity. No significant effect on action potential
duration. Minimal effects on conduction in NORMAL cells
Class 1C Depress phase 0 depolarization (conductionvelocity) in fast response cells and can decreaseautomaticity. Minimal effect on action potential duration.Marked effects on conduction in NORMAL cells.
Antiarrhyth.JDH
(MED 2/08)
57
Class 1 Antiarrhythmic Drugs
Class 1A Depress phase 0 depolarization (conductionvelocity) in fast response cells and also can depressautomaticity; prolong action potential duration and increaserefractory period. Moderate effects on conduction inNORMAL cells.
Class 1B Depress phase 0 depolarization (conductionvelocity) in fast response cells and can decreaseautomaticity. No significant effect on action potential
duration. Minimal effects on conduction in NORMAL cells
Class 1C Depress phase 0 depolarization (conductionvelocity) in fast response cells and can decreaseautomaticity. Minimal effect on action potential duration.
Marked effects on conduction in NORMAL cells.
-
8/14/2019 II. Mechanisms for Arrhythmias
15/29
-
8/14/2019 II. Mechanisms for Arrhythmias
16/29
16
Antiarrhyth.JDH
(MED 2/08)
60
A. Class 1 - Sodium Channel Blockers
2. Comparison of Lidocaine, Quinidine and Flecainide on Normal Cells
Drug State-Dependence tau Recovery (seconds)
Quinidine (1a) Open 3
Lidocaine (1b) Inactive > Open 0.1
Flecainide (1c) Open 11
The different subgroups of class 1 drugs bind to differentchannel states or have different binding kinetics.
Antiarrhyth.JDH
(MED 2/08)
61
3. Action Potentials -
Basis for conductionfrom cell to cell.
Algebraic sum ofvoltage over timeyields ECG.
PR Interval =
primarily AV nodeconduction time
QT Interval = ventricular depolarization-> repolarization time
-
8/14/2019 II. Mechanisms for Arrhythmias
17/29
17
Antiarrhyth.JDH
(MED 2/08)
62
A. Class 1 - Sodium Channel Blockers
2. Comparison of Lidocaine, Quinidine and Flecainide on Normal Cells
Antiarrhyth.JDH
(MED 2/08)
63
Class 1A - Sodium Channel Blockers
MechanismQUINIDINE
1. Predominant action
- blocks voltage gated sodium channels;
binds preferentially to open state of channel.
Selectivity for: a) cells at higher heart rate;
b) cells at less negative RMP;
Effect on cells is to:
decrease rate of phase 0increase threshold for excitability;decrease automaticity in His-Purkinjecells (but not SA cells).
-
8/14/2019 II. Mechanisms for Arrhythmias
18/29
18
Antiarrhyth.JDH
(MED 2/08)
64
Class 1A - Sodium Channel Blockers
Therapeutic Uses
QUINIDINE
1. Use has declined but is still used for -2. Variety of supraventricular and ventricular tachyarrhythmias.
2. Blocks potassium channels - prolongs refractory period.increase phase 3 and prolongs the QT interval
3. Alpha-adrenergic blockade
4. Atropine-like effect (anticholinergic)
Antiarrhyth.JDH
(MED 2/08)
65
Class 1A - Sodium Channel Blockers
Side Effects
Other Considerations
QUINIDINE
1. Prolongation of QT interval - increased risk oftorsades de pointes (2-8%; form of ventriculartachycardia which can culminate in ventricularfibrillation).
2. Hypotension due to alpha-adrenergic blockade.3. High incidence of diarrhea (30-50%)
1. Drug interaction with digoxin - increases latter'sserum level.2. Still widely used despite side effects.
-
8/14/2019 II. Mechanisms for Arrhythmias
19/29
19
Antiarrhyth.JDH
(MED 2/08)
66
Class 1A - Sodium Channel Blockers
Related Drugs(Similar to quinidine but different pharmacokinetics)
QUINIDINE
PROCAINAMIDE (Pronestyl, Procan) -
lacks vagolytic and alpha-adrenergic blockade;60-70% become ANA positive;25-50% develop a lupus-like syndrome
DISOPYRAMIDE (Norpace)
Antiarrhyth.JDH
(MED 2/08)
67
Class 1B - Sodium Channel Blockers
Mechanism LIDOCAINE (Xylocaine)
Predominant action - blocks voltage gated sodiumchannels; binds preferentially to inactivated state ofchannel. Selectivity for:
a) ventricular cells over atrial cells;b) cells with fast rate over cells with slow rate;
c) cells with less negative RMP > more negative RMP.
Sodium channel blockade leads to increased thresholdfor excitability; decreased automaticity.
-
8/14/2019 II. Mechanisms for Arrhythmias
20/29
20
Antiarrhyth.JDH
(MED 2/08)
68
Class 1B - Sodium Channel Blockers
Therapeutic Uses
Side Effects
LIDOCAINE (Xylocaine)
1. Acute suppression of ventricular arrhythmias. (nolonger the first choice for recurrent sustained V-tachor V-fib.)
2. Must be given parentally because of extensive firstpass effect - often as intravenous bolus and infusion.Latter modified with liver disease and heart failure.
1. Central nervous system symptoms - seizures (very
rapid administration) and drowsiness, dysarthriaand dysesthesia (more gradual increase in serumlevels).
2. Depression of cardiac function.
Antiarrhyth.JDH
(MED 2/08)
69
Class 1B - Sodium Channel Blockers
Other Considerations
Related Drugs(Lidocaine variants not susceptible to first-pass metabolismand can be given orally, and tend to be less selective forsick cells.)
LIDOCAINE (Xylocaine)
Also used at local anesthetic.
MEXILETINE (Mexitil)TOCAINIDE
-
8/14/2019 II. Mechanisms for Arrhythmias
21/29
21
Antiarrhyth.JDH
(MED 2/08)
70
Class 1C - Sodium Channel Blockers
Mechanism
Therapeutic Uses
FLECAINIDE (Tambocor)
1. Predominant action - blocks voltage gated sodium
channels; Selectivity for cells at high heart rate butgreater depression at normal rates than class 1A and1B.
2. Can block potassium channels (but much less ornegligible effect on QT interval ).
1. Variety of supraventricular tachycardias.
2. Life-threatening ventricular arrhythmias.
Antiarrhyth.JDH
(MED 2/08)
71
Class 1C - Sodium Channel Blockers
Side Effects
Related Drugs
FLECAINIDE (Tambocor)
1. Proarrhythmic - especially in presence ofsevere heart disease -> increase mortality
2. Depression of left ventricular function.
PROPAFENONE (Rythmol)
-
8/14/2019 II. Mechanisms for Arrhythmias
22/29
22
Antiarrhyth.JDH
(MED 2/08)
72
Class 2
Effects primarily due to blocking beta adrenergic influenceson conducting system.
(Beta - blockers)
Propranolol
AcebutololEsmolol
Others
Antiarrhyth.JDH
(MED 2/08)
73
Class 2 - Beta Adrenergic Blockers
MechanismPROPRANOLOL (Inderal)
1. Predominant action - blockade of beta adrenergicreceptors (1 in myocardium).
Therapeutic Uses
1. Beta blockers reduce mortality in early period andsubsequently after acute myocardial infarction.
2. Chronic ventricular arrhythmias.
3. Control of ventricular rate in atrial flutter or fibrillation.
4. Paroxysmal supraventricular tachycardia (PSVT).
-
8/14/2019 II. Mechanisms for Arrhythmias
23/29
23
Antiarrhyth.JDH
(MED 2/08)
74
Class 2 - Beta Adrenergic BlockersPROPRANOLOL (Inderal)
Therapeutic Uses
5. Symptomatic sinus tachycardia.
6. Catecholamine-related ventricular arrhythmias.
See lecture on "Autonomic DrugsSide Effects
Related Drugs
Esmolol Very short half-life / used i.v.
Antiarrhyth.JDH
(MED 2/08)
75
Major effect is to prolong duration of action potentialsand, thus, increase refractory period.
(Potassium Channel - blockers)Class 3
Amiodarone
Bretylium
SotalolIbutilide
-
8/14/2019 II. Mechanisms for Arrhythmias
24/29
-
8/14/2019 II. Mechanisms for Arrhythmias
25/29
25
Antiarrhyth.JDH
(MED 2/08)
78
Class 3 - Potassium Channel Blockers
2. Therapeutic Uses
AMIODARONE (Cordarone)
a. FDA recommendation - only for life-threatening ventriculararrhythmias refractory to all other available forms of therapy.
b. Powerful inhibitor of pacemaker automacitiyc. Long-term (oral) use
1. trial fibrillation and atrial flutter2. Supraventricular tachycardia3. Life-threatening (sustained) ventricular tachycardia
d. i.v. use:
1. Ventricular fibrillation2. Sustained ventricular tachycardia
Antiarrhyth.JDH
(MED 2/08)
79
Class 3 - Potassium Channel Blockers
3. Side Effects (most minimized at low doses)
AMIODARONE (Cordarone)
a. Hypotensionb. AV blockc. Arrhythmias (2%)
d. Blue-gray skin discoloratione. Pulmonary fibrosis (potentially fatal)f. Thyroid abnormalities (from iodine content)g. Corneal deposits
h. Blurred visioni. Photosensitivity
j. GI disturbances
-
8/14/2019 II. Mechanisms for Arrhythmias
26/29
26
Antiarrhyth.JDH
(MED 2/08)
80
Class 3 - Potassium Channel Blockers
Related DrugsAMIODARONE (Cordarone)
Ibutilide
Sotalol
K channel blockerNa channel activatorUses -> atrial fibrillation
K channel blockerNonselective blocker
Uses -> ventricular and atrial arrhythmiasDose-dependent torsade de pointes
Antiarrhyth.JDH
(MED 2/08)
81
Class 4Depresses slow response action potentials in AV andSA nodes where depolarization is mediated primarily bycalcium influx.
(Calcium Channel - blockers)
Verapamil
Diltiazem
-
8/14/2019 II. Mechanisms for Arrhythmias
27/29
27
Antiarrhyth.JDH
(MED 2/08)
82
Class 4 - Calcium Channel Blockers
Mechanism
Therapeutic Uses
Side Effects
Related Drugs
VERAPAMIL (Isoptin, Calan)
1. Predominant action - blocks voltage-gated L-typecalcium channels.
1. Control of ventricular rate in atrial flutter and fibrillation.2. Paroxysmal supraventricular tachycardia (PSVT) due to
reentry involving the AV node.
1. Cardiac depression.2. Hypotension.
3. Constipation (most common).
DILTIAZEM (Cardizem, Dilacor)
Antiarrhyth.JDH
(MED 2/08)
83
Other Antiarrhythmics
Mechanism ADENOSINE (Adenocard)
1. Predominant action - acts through A1 adenosinereceptors to activate potassium channels and inhibiteffects of increased cyclic AMP. This in turn leads to:
a) hyperpolarization and slowing of SA node firing;b) shortening of action potential of atrial cells;c) depression of conduction velocity through AV node.
These actions break the reentry circuit allowingresumption of normal sinus rhythm.
-
8/14/2019 II. Mechanisms for Arrhythmias
28/29
28
Antiarrhyth.JDH
(MED 2/08)
84
Other Antiarrhythmics
Therapeutic Uses
Side Effects
ADENOSINE (Adenocard)
1. Acute conversion of paroxysmal supraventriculartachycardia (PSVT) due to reentry involving the AV
node. Highly effective.
2. Given as intravenous bolus in central line. Effectstransient (maximal within 10-20 sec).
1. Transient facial flushing, dyspnea and chest pressure.
Antiarrhyth.JDH
(MED 2/08)
85
Mechanism
Therapeutic Uses
Side Effects
Other AntiarrhythmicsATROPINE
1. Predominant action - muscarinic blockade;decreases acetylcholine-induced activation ofpotassium channels through M2 receptors;increases spontaneous phase 4 depolarization of
SA node.
1. Sinus bradycardia (e.g., acute myocardial infarction)
See lecture on "Cholinergic Systems"
-
8/14/2019 II. Mechanisms for Arrhythmias
29/29
Antiarrhyth.JDH
(MED 2/08)
86
Mechanism
Therapeutic Uses
Side Effects
Other AntiarrhythmicsDIGOXIN (Lanoxin)
See lecture on "Drug Therapy of Congestive Heart FailureIncreases vagal tone and suppresses AV node activity.
Control of ventricular rate in atrial flutter and fibrillation.
See lecture on "Drug Therapy of Congestive Heart Failure"
Antiarrhyth.JDH
(MED 2/08)
87
The End