Idiopathic Ventricular Arrhythmias Originating From the … · Heart Rhythm Disorders Idiopathic...
Transcript of Idiopathic Ventricular Arrhythmias Originating From the … · Heart Rhythm Disorders Idiopathic...
Tmpqcpdv
FUo§NS
2
Journal of the American College of Cardiology Vol. 52, No. 2, 2008© 2008 by the American College of Cardiology Foundation ISSN 0735-1097/08/$34.00P
Heart Rhythm Disorders
Idiopathic VentricularArrhythmias Originating From the Aortic RootPrevalence, Electrocardiographic and ElectrophysiologicCharacteristics, and Results of Radiofrequency Catheter Ablation
Takumi Yamada, MD,* H. Thomas McElderry, MD,* Harish Doppalapudi, MD,*Yoshimasa Murakami, MD,‡ Yukihiko Yoshida, MD,§ Naoki Yoshida, MD,‡ Taro Okada, MD,‡Naoya Tsuboi, MD,§ Yasuya Inden, MD,# Toyoaki Murohara, MD,# Andrew E. Epstein, MD,*Vance J. Plumb, MD,* Satinder P. Singh, MD,† G. Neal Kay, MD*
Birmingham, Alabama; and Ichinomiya and Nagoya, Japan
Objectives This study investigated the prevalence and electrocardiographic and electrophysiologic characteristics of aorticroot ventricular arrhythmias (VAs).
Background Idiopathic VAs originating from the ostium of the left ventricle may be ablated at the base of the aortic cusps.
Methods We studied 265 patients with idiopathic VAs with an inferior QRS-axis morphology.
Results The successful ablation site was within (or below) the aortic cusps in 44 patients (16.6%). The site of the originwas the left coronary cusp (LCC) in 24 (54.5%), the right coronary cusp (RCC) in 14 (31.8%), the noncoronarycusp (NCC) in 1 (2.3%), and at the junction between the LCC and RCC (L-RCC) in 5 (11.4%) cases. The maximumamplitude of the R-wave in the inferior leads was significantly greater with an LCC than with an RCC origin (p �
0.05). The ratio of the R-wave amplitude in leads II and III was significantly greater with an LCC than with anRCC origin (p � 0.01) and was significantly smaller in the NCC than in the other sites (p � 0.0001). The ventric-ular deflection in the His bundle electrogram was significantly later relative to the surface QRS with an LCC orL-RCC origin than with an RCC or NCC origin (p � 0.0001). The ratio of the atrial-to-ventricular deflection ampli-tude was significantly greater in the NCC than in the other sites (p � 0.0001). No other factors predicted the siteof origin.
Conclusions Idiopathic VAs are more common in the LCC than in the RCC and rarely arise from the NCC. The electrocardio-gram is useful for differentiating the site of origin. (J Am Coll Cardiol 2008;52:139–47) © 2008 by theAmerican College of Cardiology Foundation
ublished by Elsevier Inc. doi:10.1016/j.jacc.2008.03.040
tfrpouo
M
P2[t(
he myocardium around the ventricular outflow tract is aajor source of idiopathic ventricular tachycardias (VTs) or
remature ventricular contractions (PVCs) (1–8). Radiofre-uency catheter ablation is a safe and reliable technique foruring those ventricular arrhythmias (VAs) (2–8). Severalrevious reports have revealed differences in the electrocar-iographic characteristics of VAs originating from the rightentricular outflow tract (RVOT), left ventricular outflow
rom the *Division of Cardiovascular Disease and the †Department of Radiology,niversity of Alabama at Birmingham, Birmingham, Alabama; ‡Division of Cardi-logy, Aichi Prefectural Cardiovascular and Respiratory Center, Ichinomiya, Japan;Division of Cardiology, Nagoya Dai-ni Red Cross Hospital, Cardiovascular Center,agoya, Japan; and the #Department of Cardiology, Nagoya University Graduatechool of Medicine, Nagoya, Japan.
DManuscript received December 4, 2007; revised manuscript received March 3,
008, accepted March 4, 2008.
ract (LVOT), and aortic root regions (4–6,9). However,or VAs originating from the aortic root, information on theelationships between the location of their origin andrevalence and the electrocardiographic and electrophysi-logic characteristics is limited. The present study wasndertaken to examine the features that predict the site ofrigin in the aortic root.
ethods
atient characteristics. The study population consisted of65 consecutive patients (71 men, mean age 53 � 15 yearsrange 16 to 80 years]) with symptomatic idiopathic sus-ained VT (n � 34), nonsustained VT (n � 56), or PVCsn � 175) originating from the ventricular outflow tract.
uring the clinical arrhythmia, the surface electrocardio-fPobo
LwoMtiPfpsttcaadmataao1wcatw
140 Yamada et al. JACC Vol. 52, No. 2, 2008VT or PVCs Originating From the Aortic Root July 8, 2008:139–47
gram revealed a uniform QRSmorphology with an inferior axisin all patients. Echocardiographyand exercise stress testing or cor-onary angiography demonstratedno evidence of structural heartdisease in any patients. Each pa-tient gave written informed con-sent, and all antiarrhythmic drugswere discontinued for �5 half-lives before the study.Electrophysiologic study. Six-French quadripolar catheterswere introduced from the rightfemoral vein and placed acrossthe tricuspid valve to record theHis bundle (HB) activation andin the right ventricular (RV) apexfor pacing. Mapping and pacingwere performed using a 7-F4-mm-tip ablation catheter in-troduced from the right femoralvein (for the RVOT) or right
emoral artery (for the LVOT or aortic root). When fewVCs were observed at the beginning of the electrophysi-logic study, induction of the VT or PVCs was attemptedy burst pacing from the RVOT or apex with the additionf an isoproterenol infusion. During mapping of the
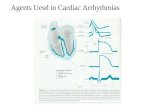
Figure 1 Successful Ablation Site of PVCs Originating From the
The first beat is a sinus beat and the second is a premature ventricular contractioatrial activations were recorded during sinus rhythm (left panel). The sequence ofceded the QRS onset by 65 ms. The aortagram showed that the ablation catheterpanels). Note that the tip of the ablation catheter was positioned at the L-RCC bymap during the PVCs revealed the earliest activation at the L-RCC (right panels). Athe ablation catheter; ABLuni � distal unipolar electrode of the ablation catheter;LL � left lateral; LVOT � left ventricular outflow tract; RAO � right anterior oblique
Abbreviationsand Acronyms
ASC � aortic sinus cusp
HB � His bundle
LCC � left coronary cusp
L-RCC � junction betweenthe left and right coronarycusps
LV � left ventricular
LVOT � left ventricularoutflow tract
NCC � noncoronary cusp
PVC � prematureventricular contraction
RCC � right coronary cusp
RV � right ventricular
RVOT � right ventricularoutflow tract
VA � ventricular arrhythmia
VT � ventriculartachycardia
VOT or aortic sinus cusps (ASCs), intravenous heparinas administered to maintain an activated clotting timef �250 s.
apping and radiofrequency catheter ablation. Activa-ion and pace mapping were performed in all cases todentify the VA origin site. In some patients, when VT orVCs were frequent, electroanatomic mapping was per-
ormed as previously reported (10–12) (Fig. 1). Pace map-ing was performed at a pacing cycle length of 500 ms andtimulus amplitude of 1 mA greater than the late-diastolichreshold. When the earliest site of activation was mappedo a site above the aortic valve, selective angiography of theoronary artery and aorta was performed before ablation tossess the anatomic relationships between those structuresnd the location of the ablation catheter. In cases where theistinction between the aortic sinuses could not be deter-ined by angiography alone, intracardiac echocardiography
lso was used to identify the site of the ablation catheter. Ifhe ablation site was close to the ostium of the coronaryrtery, radiofrequency ablation was performed with anngiographic catheter positioned within the coronary arterystium with frequent hand injections of contrast (every5 s). The wall of the ASCs as well as coronary artery flowas observed carefully by injecting an adequate volume of
ontrast to overflow into the ASC. A radiofrequencypplication was never delivered to an area within 5 mm ofhe angiographic catheter. Radiofrequency applicationsere delivered with a target temperature of 60°C and
C
). At the successful ablation site, 2 ventricular activation components and nocomponents was reversed during the PVCs. The first of the 2 components pre-cated in the junction of the left and right aortic sinus cusps (L-RCC) (center
ting the loop of the ablation catheter in the left ventricular cavity. The activationdistal electrode pair of the ablation catheter; ABLp � proximal electrode pair of
anteroposterior; LAO � left anterior oblique view; LCC � left coronary cusp;RCC � right coronary cusp; RVOT � right ventricular outflow tract.
L-RC
n (PVCthe 2was lodeflecBLd �
AP �
view;
medrddrwoddleaer
efuiIaVtFaiptStvtadtsTasccw
R
OSpoa1atd
ioao�a�Q[sPbidL3TccLwCr(sVrtnfcmr
alowpwlpptnvarcpdgvst
141JACC Vol. 52, No. 2, 2008 Yamada et al.July 8, 2008:139–47 VT or PVCs Originating From the Aortic Root
aximum power output of 50 W at sites exhibiting thearliest bipolar activity and/or a local unipolar QS patternuring the VT or PVCs. When an acceleration oreduction in the incidence of VT or PVCs was observeduring the first 10 s of the application, the radiofrequencyelivery was continued for 30 to 60 s. Otherwise, theadiofrequency delivery was terminated, and the catheteras repositioned. If the earliest ventricular activation wasbserved with an HB potential or close to the HB regionuring the VT or PVCs, radiofrequency energy waselivered at least 5 mm away from the site recording the
argest HB potential, using an initial power of 30 W. Thend point of the catheter ablation was the eliminationnd noninducibility of VT or PVCs during an isoproter-nol infusion (2 to 4 �g/min) and burst pacing from theight ventricle (to a cycle length as short as 300 ms).
When VAs were suspected to originate from thepicardial side around the LVOT, mapping was per-ormed in the great cardiac vein or anterior interventric-lar cardiac vein using a mapping or ablation catheterntroduced via the right femoral or internal jugular vein.f mapping in those cardiac veins revealed the earliestctivation preceding the onset of the QRS during theAs and an excellent pace map, the VAs were considered
o originate from the left ventricular (LV) epicardium.ollow-up. Follow-up was performed at 2 weeks, 1 month,nd every 3 months thereafter using 24-h Holter monitor-ng and 12-lead electrocardiograms. All patients who re-orted symptoms were given an event monitor to documenthe cause of the symptoms.tatistical analysis. Continuous variables are expressed as
he group mean � 1 SD. Comparisons of the continuousariables between the 2 groups were analyzed with the use ofhe Student t test. When comparisons involved �2 groups,n analysis of variance (ANOVA) was used. When groupifferences were found, a 1-way ANOVA was followed byhe Fisher least significant difference method to test theignificance of the difference among the means in all groups.he categoric variables expressed as numbers and percent-
ges in the different groups were compared with a chi-quare test and Yates correction if necessary. An overallhi-square test for a 2 � n table was constructed whenomparisons involved �2 groups. Statistical significanceas selected at a p value of �0.05.
esults
verall mapping, catheter ablation, and follow-up.uccessful ablation was acutely achieved in 260 of 265atients. In the remaining 5 patients, an LV epicardialrigin was identified that was not ablated. The successfulblation site was located in the aortic root in 44, RVOT in99, LVOT in 11, LV epicardium in 3, and pulmonaryrtery in 3 of the patients. Eventually, in 8 of 265 patients,he VA origins were deemed to be epicardial. Two proce-
ures were required to eliminate the VAs in the aortic root rn 2 patients, RVOT in 15, and LVOT in 1. The numberf radiofrequency applications required for a successfulblation was significantly larger in the VAs with an RVOTr LVOT origin than in those with an aortic root origin (4.0
1.4 or 3.8 � 0.8, respectively, vs. 2.2 � 0.9; p � 0.0001nd p � 0.0005, respectively). Over a mean follow-up of 18
12 months after the last procedure, VAs with the sameRS morphology as previously targeted recurred in 12 (11
6%] in the RVOT and 1 [9%] in the LVOT; 3 [9%] wereustained VTs, 1 [2%] nonsustained VT, and 8 [5%]VCs), and those VAs were excluded from the analysisecause their origins were not fully defined. In the remain-ng 253 patients without a VA recurrence, the origin wasetermined to be in the aortic root in 44, RVOT in 188,VOT in 10, LV epicardium in 8, and pulmonary artery in. The basic demographics of those patients are given inable 1. Three patients with an RVOT, LVOT, or left
oronary cusp (LCC) VA origin were complicated byardiomyopathy induced by frequent PVCs. In all cases, theV ejection fraction was �45% at baseline and normalizedithin 3 months after the elimination of the VAs.atheter ablation of VAs with an origin in the aortic
oot. Successful ablation was achieved in all 44 patients100%) with aortic root VAs. This represented 17.3% of theuccessfully ablated patients or 16.6% of all patients. TheA origin was determined to be in the LCC in 24 (54.5%),
ight coronary cusp (RCC) in 14 (31.8%), junction betweenhe left and right coronary cusps (L-RCC) in 5 (11.4%), andoncoronary cusp (NCC) in 1 (2.3%) patient. The distancerom the tip of the ablation catheter to the left or rightoronary artery ostia was 12.9 � 3.1 mm (range 7.5 to 17.2m) and 10.5 � 3.0 mm (range 8.3 to 18.1 mm),
espectively.In the catheter ablation of the L-RCC VAs, the tip of the
blation catheter was positioned at that site by deflecting theoop of the ablation catheter in the LV cavity in 3 patientsr on the NCC in the remaining 2 (Fig. 1). In all patientsith an RCC or NCC origin, the earliest RV activationreceding the QRS onset was recorded in the HB region,hereas in the patients with an LCC or L-RCC origin, the
ocal ventricular activation in the RV HB region neverreceded the QRS onset (Figs. 1 to 3). In 2 of our initialatients with a VA origin in the RCC or NCC contiguouso the RCC, radiofrequency applications were first deliveredear the HB region in the right ventricle, because the localentricular activation preceded the QRS onset (Fig. 2) andgood pace map (score � 10 of 12) was obtained. These
adiofrequency applications did not interrupt the VAs, butaused a slight change in the QRS morphology, with arolongation of the QRS duration and attenuation andelay of the high-amplitude near-field ventricular electro-ram in the RV HB region. The low-amplitude far-fieldentricular electrogram preceding the QRS onset was theneparated from the near-field ventricular electrogram afterhe QRS onset in the RV HB region (Fig. 2). Successful
adiofrequency ablation was achieved in the NCC, wheretwt
dtw
B
A�
p ntractit
142 Yamada et al. JACC Vol. 52, No. 2, 2008VT or PVCs Originating From the Aortic Root July 8, 2008:139–47
he local ventricular activation was recorded simultaneouslyith the activation of the far-field ventricular electrogram in
he RV HB region (Fig. 2). The amplitude of the atrial
Figure 2 Ablation Sites of a VT Originating From the NCC Near
Radiofrequency applications delivered near the His bundle (HB) region where the lslight change in the QRS morphology with the prolongation of the QRS duration anthe HB region (double arrowheads, center panel). The low-amplitude far-field ventthen separated from the near-field ventricular electrogram after the QRS onset in tcusp (NCC) where the local ventricular activation was recorded simultaneously withNote that the atrial electrogram with an amplitude greater than that of the ventricupanel). HBd � distal electrode pair of the His catheter; HBp � proximal electrode pai
asic Demographics of the Patients With Successful Ablation
Table 1 Basic Demographics of the Patients With Successful A
OriginAge(yrs)
Gender, n(M/F)
Type, n(NSVT/SVT/PVC) Hear
Ao root (n � 44) 53 � 14 26/18 9/9/26
RVOT (n � 188) 54 � 15 77/111 40/17/131
LVOT (n � 10) 59 � 6 6/4 1/2/7
LV epi (n � 8) 49 � 15 6/2 2/4/2
PA (n � 3) 54 � 14 2/1 1/1/1
F � atrial fibrillation; AFL � atrial flutter; Ao � aortic; AP � angina pectoris; Con. � conventionahyperlipidemia; HT � hypertension; LV � left ventricular; LVEF � left ventricular ejection fractio
ulmonary artery; PSVT � paroxysmal supraventricular tachycardia; PVC � premature ventricular coachycardia; VT � ventricular tachycardia.
eflection in the local electrogram was greater than that ofhe ventricular deflection only when the site of origin wasithin the NCC (Fig. 2). During 13 of 14 RCC VAs (the
B and in the NCC
ntricular activation preceded the QRS onset by 25 ms (left panel) caused attenuation and delay of the high-amplitude near-field ventricular electrogram inelectrogram (single arrowheads, center panel) preceding the QRS onset wasregion. Successful radiofrequency ablation was achieved in the noncoronaryctivation of the far-field ventricular electrogram in the HB region (center panel).ctrogram was recorded at the successful ablation site during sinus rhythm (rightHis catheter; VT � ventricular tachycardia; other abbreviations as in Figure 1.
on
ases, n Risk Factors, n LVEF (%) Mapping Technique, n
HT: 14 61 � 11 (23–81) Con.: 20
DM: 2 EA: 24
HL: 8
HT: 53 62 � 8 (41–77) Con.: 75
2
DM: 11 EA: 113
HL: 29
HT: 3 58 � 11 (43–69) Con.: 5
DM: 1 EA: 5
HL: 2
HT: 1 62 � 7 (55–76) Con.: 2
DM: 1 EA: 6
HL: 1
HT: 1 61 � 5 (55–65) Con.: 2
EA: 1
ing; DM � diabetes mellitus; EA � electro-anatomic mapping; epi � epicardium; F � female; HLT � left ventricular outflow tract; M � male; NSVT � nonsustained ventricular tachycardia; PA �
on; RVOT � right ventricular outflow tract; SSS � sick sinus syndrome; SVT � sustained ventricular
the H
ocal ved an aricularhe HB
the alar eler of the
blati
t Dise
AP: 2
AF: 1
AFL: 1
AP: 5
PSVT:
AF: 9
AFL: 4
SSS: 2
AFL: 1
AP: 2
AF: 1
AFL: 1
None
l mappn; LVO
ewfaiasj
squnpdVmiCefcVTctotb
143JACC Vol. 52, No. 2, 2008 Yamada et al.July 8, 2008:139–47 VT or PVCs Originating From the Aortic Root
xception being 1 patient in which radiofrequency ablationas first attempted at the RV HB region), a low-amplitude
ar-field ventricular electrogram preceding the high-mplitude near-field ventricular electrogram was recognizedn the RV HB region (Fig. 3). In only 3 of 14 RCC VAs,n HB electrogram was recorded at the successful ablationite (Fig. 3). During the catheter ablation of those VAs, nounctional rhythm or AH or HV delays were observed.
In none of the cases with aortic root VAs could austained VT be terminated during successful radiofre-uency applications. Even in the cases with clinically doc-mented sustained VT, the induction of sustained VT wasot always attempted if frequent PVCs with a QRS mor-hology identical to that of the sustained VT were observeduring the electrophysiologic study. In some cases, sustainedT terminated during mapping probably because of aechanical effect (Fig. 4), and thereafter only PVCs were
nduced.omparison of the clinical, electrocardiographic, and
lectrophysiologic parameters in the VAs originatingrom the aortic root. The results of the clinical, electro-ardiographic, and electrophysiologic parameters of theAs with their determined origins are given in Table 2.here were no significant differences in the clinical
haracteristics or standard electrocardiographic parame-ers (such as the morphology [in leads I and aVL as well]r precordial transition) between the origin sites withinhe aortic root (Fig. 5). However, a right bundle branchlock and right inferior axis QRS morphology was
Ventricular Tachycardia Originating From thehe Ablation Catheter at the Successful Ablation Site
ir of the right ventricular catheter; other abbreviations as in Figures 1 and 2.
Figure 3 Successful Ablation Site of a PVCOriginating From the Right Coronary Cusp
The first beat is a sinus beat and the second is a premature ventricular con-traction (PVC). At the successful ablation site, atrial and His bundle (HB)(arrows) electrograms were recorded during sinus rhythm and during the PVC;a far-field electrogram (single arrowhead) preceding the QRS onset by 18 msand the following near-field electrogram (double arrowheads) were observed inthe right ventricular HB region. Abbreviations as in Figures 1 and 2.
Figure 4 Cardiac Tracings Exhibiting the Termination of a SustainedRight Coronary Cusp by Probable Mechanical Pressure of t
RVd � distal electrode pair of the right ventricular catheter; RVp � proximal electrode pa
oRtittsfsotL6t
orvdfatgtT
gfCcRtcdCnb
D
TfNfiaT(opar
C
*
Lc rior axio
144 Yamada et al. JACC Vol. 52, No. 2, 2008VT or PVCs Originating From the Aortic Root July 8, 2008:139–47
bserved only in the VAs with an LCC origin, and an-wave in lead aVL was observed only with an origin in
he NCC. The maximal amplitude of the R-wave in thenferior leads was significantly greater in the LCC VAshan in the RCC VAs (p � 0.05) (Fig. 5). The ratio ofhe R-wave amplitude in leads II and III (III/II ratio) wasignificantly greater for the VAs with an LCC origin thanor those with an RCC origin (p � 0.01) and wasignificantly smaller for the 1 NCC origin than for thether sites (p � 0.0001) (Fig. 5). Comparing origins inhe LCC and RCC, a III/II ratio of �0.9 predicted anCC origin with a sensitivity of 100%, specificity of4.2%, positive predictive accuracy of 80.0%, and nega-ive predictive accuracy of 100%.
There were no significant differences in the electrophysi-logic parameters such as local ventricular activation timeelative to the QRS onset, amplitude of the atrial orentricular electrograms at the successful ablation site, oruration or number of radiofrequency applications neededor successful ablation between the sites of origin in theortic root. The local ventricular activation time relative tohe QRS onset at the RV HB region was significantlyreater for the VAs with LCC and L-RCC origins than forhose with RCC and individual NCC origins (p � 0.0001).
linical, Electrocardiographic, and Electrophysiologic Characteristi
Table 2 Clinical, Electrocardiographic, and Electrophysiologic C
OriginAge(yrs)
Gender, n(M/F)
Type, n(NSVT/SVT/PVC)
Duration(ms)
LCC (n � 24) 53 � 14 16/8 6/3/15 176 � 21
RCC (n � 14) 56 � 15 6/8 2/4/8 168 � 14
L-RCC (n � 5) 45 � 13 3/2 1/1/3 186 � 16
NCC (n � 1) 32 1/0 0/1/0 178
Origin
V-QRS (ms)
ABL Site HB Region A (mV)
LCC (n � 24) �29 � 10 38 � 14‡ 0.10 � 0.15
RCC (n � 14) �35 � 12 �15 � 5 0.04 � 0.08
L-RCC (n � 5) �26 � 6 34 � 3‡ 0.08 � 0.06
NCC (n � 1) �28 �25 0.22
p � 0.05; †p � 0.01 versus LCC; ‡p � 0.0001 versus each of the other sites.A � atrial electrogram; ABL � ablation; A/V � amplitude ratio in atrial and ventricular electrog
BBB � left bundle branch block; LL � left bundle branch block � left inferior axis; L-RCC � junctiousp; RCC � right coronary cusp; RF � radiofrequency; RR � right bundle branch block � right infether abbreviations as in Table 1.
he amplitude ratios in the atrial and ventricular electro- a
rams were significantly greater for the 1 NCC origin thanor the other sites (p � 0.0001).
omplications. Sinus bradycardia followed by complete AVonduction block occurred in 1 patient with PVCs with anCC origin, in whom an HB electrogram was not recorded at
he successful ablation site. Both sinus node function and AVonduction recovered soon after termination of radiofrequencyelivery in this patient. No other complications occurred.oronary arteriograms demonstrated no change in the coro-ary artery flow or diameter after the ablation compared withaseline.
iscussion
his study revealed that VAs more commonly originaterom the LCC than from the RCC and are rare in theCC. Anatomic studies may provide the rationale for thosendings (13,14). The aortic root and the mitral valve formttachments to the circular ostium of the left ventricle (Fig. 6).he aortic root consists of 3 sinuses of Valsalva, 2 of which
the right and left sinuses) make direct contact with thestium of the left ventricle. Spatially, the aortic root occu-ies a central location within the heart, with the NCCnterior and superior to the paraseptal region of the left andight atria close to the superior atrioventricular junctions. In
cteristics
QRS
logy, Transition,n
Lead I,n
LeadaVL, n
R Amplitude (mV)in Inferior Leads
III/IIRatio
V1: 7 rS: 17 QS: 15 2.1 � 0.8 1.1 � 0.1
11 V2–3: 11 R: 3 rS: 9
6 V3: 3 rsr=: 3
V3–4: 2 rSr=: 1
V4–5: 1
V1: 1 Rr=: 4 QS: 9 1.5 � 0.4* 0.9 � 0.2†
5 V1–2: 2 R: 4 rS: 5
V2: 1 rS: 4
V2–3: 7 rSr=: 1
V3–4: 3 rsr=: 1
V1–2: 1 qrS: 1 QS: 5 2.1 � 0.8 1.0 � 0.1
2 V2–3: 2 R: 2
V3: 2 rsr=: 1
rS: 1
V2–3: 1 R: 1 R: 1 0.9 0.1#
Site
RF Duration (min) No. of RF LesionsV) A/V
0.75 0.26 � 0.30‡ 2.0 � 1.0 2.3 � 0.9
0.28 0.14 � 0.24‡ 2.3 � 1.0 2.3 � 0.7
0.94 0.19 � 0.21‡ 2.6 � 0.8 3.4 � 1.0
8 2.75 1.0 1.0
B � His bundle; III/II ratio � R-wave amplitude ratio in leads II and III; LCC � left coronary cusp;and right coronary cusps; LR � left bundle branch block � right inferior axis; NCC � non-coronary
s; V � ventricular electrogram; V-QRS � local ventricular activation time relative to the QRS onset;
cs
hara
Morphon
LL: 7
LR:
RR:
LL: 9
LR:
LL: 3
LR:
LL: 1
ABL
V (m
0.67 �
0.35 �
0.90 �
0.0
rams; Hn of left
ll normally structured human hearts, the NCC is adjacent
tnrchtNaaleaait
osatlaT
aLotaLpvowaoLtotommsto
145JACC Vol. 52, No. 2, 2008 Yamada et al.July 8, 2008:139–47 VT or PVCs Originating From the Aortic Root
o the atrial myocardium on the epicardial aspect and doesot directly contact the ventricular myocardium of either theight or the left ventricle (Fig. 5). Indeed, atrial tachycardiasan be ablated within the NCC (15). Therefore, in normaluman hearts, VAs should not arise from the NCC, andhe present case of a successful ablation of the VA within theCC is quite unusual. The electrogram recorded at the
blation site demonstrated a very small ventricular potentialnd a large atrial potential, as would be expected at thisocation. It seems likely that the ablation lesion may havextended to the posterior portion of the RCC, therebyblating a portion of the ostium of the left ventricle. It islso possible that this case represented an anatomic variantn which the LV myocardium was more closely apposed tohe NCC than normally.
This study included VAs arising from the L-RCC asriginating from the aortic root because of several con-iderations. Because of the semilunar nature of thettachments of the aortic valvular cusps, there are 3riangular extensions of the aortic root that reach to theevel of the sinotubular junction of the aorta, locatedpproximately 1 cm above the base of either cusp (Fig. 6).
Figure 5 Two-Dimensional Computerized Tomography Image anElectrocardiograms of Premature Ventricular Contract
L � left coronary cusp; LA � left atrium; N � noncoronary cusp; R � right coronar
hese extensions are bound by thin fibrous walls of the t
orta between the expanded sinuses. At the base of theCC and RCC, the ventricular myocardium of thestium of the left ventricle comes in direct contact withhe aorta (Fig. 6). It is quite likely that ventricularrrhythmias that can be ablated within the base of theCC and RCC actually arise from the most superiorortion of the ostium of the left ventricle. Although theentricular myocardium at the L-RCC forms the ostiumf the left ventricle at the same level as that connectingith the LCC and RCC, it is located beneath the true
natomic junction of those cusps (Fig. 6), as confirmed byur practical findings in the catheter ablation of the-RCC VAs. Actually, the present study demonstrated
hat the clinical, electrocardiographic, and electrophysi-logic characteristics of the L-RCC VAs were similar tohose of the LCC or RCC VAs. The site of the ablationf those L-RCC VAs provides an insight into all arrhyth-ias arising from the LVOT. Although some arrhyth-ias can be ablated within the LCC or RCC, those
hould not be considered to be true ASC VAs; rather,hose VAs, whether approached by a catheter from abover below the aortic valvular annulus, should be considered
resentative 12-Leador Ventricular Tachycardia Originating From the Aortic Root
; RA � right atrium; RV � right ventricle.
d Repions
y cusp
o arise from the ostium of the left ventricle.
tpwAtNwtocftmcoa
irupgrabtLrITe
AnttfrtAet
abtapsdttlfpfhr
cprs
146 Yamada et al. JACC Vol. 52, No. 2, 2008VT or PVCs Originating From the Aortic Root July 8, 2008:139–47
Anatomic studies have revealed a close relationship be-ween the RCC or NCC and the HB (5,15). The posteriorart of the RCC is adjacent to the central fibrous body,hich carries within it the penetrating portion of the HB.nteriorly, the RCC is related to the bifurcating atrioven-
ricular bundle and the origin of the left bundle branch. TheCC lies superior to the central fibrous body throughhich the HB penetrates. The present study demonstrates
hat the local ventricular activation time relative to the QRSnset at the RV HB region might be an electrophysiologiclue for differentiating VA origins in the LCC and L-RCCrom those in the RCC and NCC. In catheter ablation ofhose arrhythmias, the HB catheter may be a useful land-ark for mapping within the RCC and NCC. During
atheter ablation within the RCC and NCC, the proximityf the RCC and NCC to the HB should be kept in mind tovoid inadvertent damage to the AV conduction system.
The electrocardiographic parameters may not be helpfuln differentiating between VAs with an origin in each aorticoot site, probably because those sites were located contig-ously to each other in the limited space. However, theresent study may provide several electrocardiographic al-orithms for differentiating VAs originating from the aorticoot. An R-wave in lead aVL during the VAs may excluden origin in the LCC, RCC, or L-RCC. A right bundleranch block QRS morphology during the VAs may suggesthat the VAs never originate from the RCC, NCC, or-RCC. For the 2 major sites of origin within the aortic
oot (LCC and RCC), the R-wave amplitude ratio in leadsI and III may be the most helpful discriminating factor.he activation time in the HB region may be helpful for
Figure 6 Two-Dimensional Computerized Tomography Images Sthe Relationships Between the Ventricular Myocardiu
Arrowheads indicate the distal edge of the ventricular myocardium connecting withpanel) indicates the ventriculoarterial junction (the ostium of the left ventricle [LV]Figure 5.
xplaining the last 2 electrocardiographic characteristics. a
lthough the activation time at successful ablation sites didot differ significantly between the LCC and RCC VAs, inhe HB region it was significantly earlier during RCC VAshan LCC VAs. These findings suggest that the activationrom the RCC may propagate to the ventricular septum andight ventricle before the LV free wall, whereas that fromhe LCC may do so after part of the LV free wall activates.lthough the LCC and the RCC are located adjacent to
ach other, the horizontal vectors of the activation fromhose sites may be in opposite directions.
Serious complications, such as chronic left main coronaryrtery occlusions (16) or aortic regurgitation, may be possi-le during catheter ablation of aortic root VAs. However,hese complications may be prevented if radiofrequencyblation is performed using the technique described in theresent study, where the only complication was transientinus bradycardia followed by transient complete AV con-uction block, which occurred during radiofrequency abla-ion in the RCC. Anatomic studies have demonstrated thathe anteriorly situated RVOT passes slightly superior to andeftward of the aortic valve and there is an anterior epicardialat pad containing parasympathetic ganglia between theulmonary infundibulum and the RCC (5,14,17). There-ore, radiofrequency energy deliveries from the RCC mayave a thermal effect on the anterior epicardial fat pad,esulting in vagal stimulation.
There are several novel findings of the present studyompared with earlier reports. First, this is the first report toropose the new concept of VAs originating from the aorticoot as a part of the ventricular ostium. This concept isupported by computerized tomography images illustrating
ngd Aortic Sinus Cusps
ft coronary cusp (L) and right coronary cusp (R), and the dotted line (rightaorta; LCA � left coronary artery; MV � mitral valve; other abbreviations as in
howim an
the le). Ao �
continuous anatomic opening into the left ventricle with
tadttrafiFpttoudteoLVSotoNa
C
Taarltw
RDBAt
R
1
1
1
1
1
1
1
1
1
1
K
147JACC Vol. 52, No. 2, 2008 Yamada et al.July 8, 2008:139–47 VT or PVCs Originating From the Aortic Root
he attachments of the aortic root anteriorly and the mitralnnulus posteriorly. The ostium of the left ventricle isivided centrally by the contiguous structures the NCC ofhe aorta and the anterior leaflet of the mitral valve. Second,his study confirms that the anatomic features of the aorticoot explain the far higher prevalence of VAs from the LCCnd RCC than from the NCC. Although there have been aew reports describing NCC VAs (18,19), none havencluded local electrograms at the successful ablation site.urthermore, the 12-lead electrocardiograms during theroposed NCC VAs exhibited very similar characteristics tohose of the RCC VAs in this study. Therefore, we believehat the NCC VAs in earlier reports might have actuallyriginated from the RCC. The careful radiographic imagingsed in the present study is likely to provide a more accurateescription of the prevalence of the aortic root VAs. Andhird, whereas most of the earlier studies contrasted thelectrocardiographic and electrophysiologic characteristicsf the aortic root VAs with those arising in the RVOT orVOT (5,6), the present study compared those features forAs confined to the aortic root.tudy limitations. The fact that there was only 1 NCCrigin precludes meaningful statistical comparisons withhe LCC and RCC origins. However, the mere fact thatnly 1 of 44 origins in the aortic root was found in theCC attests to the rarity of this location as a site for the
ortic root VA origin.
onclusions
his study revealed that the LCC is the most commonblation location of aortic root VAs, followed by the RCCnd the L-RCC. The NCC is rarely the site of origin. Theatio of the R-wave amplitude in leads II and III and theocal ventricular activation time relative to the QRS onset athe HB region were helpful for differentiating an originithin the LCC from that within the RCC.
eprint requests and correspondence: Dr. Takumi Yamada,ivision of Cardiovascular Disease, University of Alabama atirmingham, VH B147, 1670 University Boulevard, 1530 Thirdvenue South, Birmingham, Alabama 35294-0019. E-mail:
EFERENCES
1. Buxton AE, Waxman HL, Marchlinski FE, Simson MB, Cassidy D,Josephson ME. Right ventricular tachycardia: clinical and electro-physiologic characteristics. Circulation 1983;68:917–27.
2. Morady F, Kadish AH, DiCarlo L, et al. Long-term results of catheterablation of idiopathic right ventricular tachycardia. Circulation 1990;
82:2093–9. c3. Klein LS, Shih HT, Hackett FK, Zipes DP, Miles WM. Radiofre-quency catheter ablation of ventricular tachycardia in patients withoutstructural heart disease. Circulation 1992;85:1666–74.
4. Coggins DL, Lee RJ, Sweeney J, et al. Radiofrequency catheterablation as a cure for idiopathic tachycardia of both left and rightventricular origin. J Am Coll Cardiol 1994;23:1333–41.
5. Ouyang F, Fotuhi P, Ho SY, et al. Repetitive monomorphic ventric-ular tachycardia originating from the aortic sinus cusp: electrocardio-graphic characterization for guiding catheter ablation. J Am CollCardiol 2002;39:500–8.
6. Ito S, Tada H, Naito S, et al. Development and validation of an ECGalgorithm for identifying the optimal ablation site for idiopathicventricular outflow tract tachycardia. J Cardiovasc Electrophysiol2003;14:1280–6.
7. Yamada T, McElderry HT, Doppalapudi H, Kay GN. Catheterablation of ventricular arrhythmias originating from the vicinity of theHis bundle: significance of mapping of the aortic sinus cusp. HeartRhythm 2008;5:37–42.
8. Yamada T, Yoshida N, Murakami Y, et al. Electrocardiographiccharacteristics of ventricular arrhythmias originating from the junctionof the left and right coronary sinuses of valsalva in the aorta; theactivation pattern as a rationale for the electrocardiographic character-istics. Heart Rhythm 2008;5:184–92.
9. Bunch TJ, Day JD. Right meets left: a common mechanism underly-ing right and left ventricular outflow tract tachycardias. J CardiovascElectrophysiol 2006;17:1059–61.
0. Azegami K, Wilber DJ, Arruda M, Lin AC, Denman RA. Spatialresolution of pacemapping and activation mapping in patients withidiopathic right ventricular outflow tract tachycardia. J CardiovascElectrophysiol 2005;16:823–9.
1. Joshi S, Wilber DJ. Ablation of idiopathic right ventricular outflowtract tachycardia: current perspectives. J Cardiovasc Electrophysiol2005;16 Suppl 1:S52–8.
2. Yamada T, Murakami Y, Yoshida N, et al. Efficacy of electroanatomicmapping in the catheter ablation of premature ventricular contractionsoriginating from the right ventricular outflow tract. J Interv CardElectrophysiol 2007;19:187–94.
3. McAlpine WA. Heart and Coronary Arteries. New York, NY:Springer-Verlag, 1975.
4. Anderson RH. Clinical anatomy of the aortic root. Heart 2000;84:670–3.
5. Ouyang F, Ma J, Ho SY, et al. Focal atrial tachycardia originatingfrom the noncoronary aortic sinus: electrophysiological characteristicsand catheter ablation. J Am Coll Cardiol 2006;48:122–31.
6. Pons M, Beck L, Leclercq F, Ferriere M, Albat B, Davy JM. Chronicleft main coronary artery occlusion: a complication of radiofrequencyablation of idiopathic left ventricular tachycardia. Pacing Clin Elec-trophysiol 1997;20:1874–6.
7. Cummings JE, Gill I, Akhrass R, Dery M, Biblo LA, Quan KJ.Preservation of the anterior fat pad paradoxically decreases the inci-dence of postoperative atrial fibrillation in humans. J Am Coll Cardiol2004;43:994–1000.
8. Kanagaratnam L, Tomassoni G, Schweikert R, et al. Ventriculartachycardias arising from the aortic sinus of valsalva: an under-recognized variant of left outflow tract ventricular tachycardia. J AmColl Cardiol 2001;37:1408–14.
9. Chun KR, Satomi K, Kuck KH, Ouyang F, Antz M. Leftventricular outflow tract tachycardia including ventricular tachycar-dia from the aortic cusps and epicardial ventricular tachycardia.Herz 2007;32:226 –32.
ey Words: ventricular arrhythmia y aortic root y prevalence y
haracteristics y radiofrequency catheter ablation.