IDD NEWSLETTER - ign.org · Dr Allain Parfait Nutrition Department, Ministry of Health, Burundi Dr...
Transcript of IDD NEWSLETTER - ign.org · Dr Allain Parfait Nutrition Department, Ministry of Health, Burundi Dr...
I OD INE GLOBAL NETWORK is a nongovernmental organization dedicated to sustained optimal iodine nutrition and the elimination of iodine deficiency throughout the world.
I N TH IS I SSUE
Young women in Burundi have inadequate iodine intake
IDDNEWSLETTERVOLUME 46 NUMBER 4 NOVEMBER 2018
Iodine status alarmingly low in Madagascarwomen.PAGE 6
Iodine-rich recipes now available in a UK cookbook.PAGE 11
The Iodine Global Network named a ‘standout’ charity by GiveWell for the fifth straight year! PAGE 18
© E
U C
ivil
Prot
ectio
n an
d H
uman
itaria
n Ai
d O
pera
tions
via
Flic
kr;
CC
BY
SA
Burundi is a country in the Great Lakes Region of Eastern Africa. According to a 2012 census, it has a population of more than 10 million, and a population density of more than 400/km2 (1). Burundi is landlo-cked, sharing borders with three countries – Rwanda to the north, Tanzania to the east and south, and the Democratic Republic of the Congo to the west. There is scant information regarding iodine status and salt iodization in Burundi. In 2005, a national nutrition survey reported that 87% of households had salt at home on the day of the survey, of which 98% tested positive for iodine using a qualita-tive rapid test kit (RTK). Similarly high coverage of households was confirmed in a Demographic and Health Survey (DHS) in 2010 (89% of households had salt; of these 96% had iodized salt) (2). Yet, the medi-an urinary iodine concentration (UIC) in school-age children (aged 7–12 years) was 70 µg/L, indicating that the population was iodine deficient (2,3).
A call to actionThe IGN Regional Coordinator for Eastern and Southern Africa, Dr. Vincent Assey, contacted REACH in Burundi to discuss
how to remedy the lack of recent data on iodine status and assess the effectiveness of the national strategy to combat iodine defici-ency (4). The need for a national survey was supported by key sta-keholders, including the Ministry of Health, Ministry of Education, development partners (UNICFE, WFP and WHO), and technical advisors: Director General of the Institute of Statistics (ISTEEBU), Director of Nutrition in the Ministry of Public Health and AIDS Control, and Director General of the Bureau of Business Normalization (BBN), among others. As a result of this com-mitment, a national household-based survey was carried out in February 2018 to determine the iodine content in salt consumed
at household level and the urinary iodine concentration in women of reproductive age (15–49 years) in Burundi. Secondary goals of the survey were to: (1) identify populati-on groups at high risk of iodine deficiency which may require immediate remedial measures; (2) use the updated information on iodine nutrition to strengthen advocacy at all levels, and as baseline data to assess the effectiveness of future interventions; and (3) recommend strategies to ensure that Burundi achieves and sustains optimal iodine intakes.
Survey design and subjectsMulti-stage sampling was applied to select 30 out of 119 communes, with a probability proportional to commune size. Four collines (smaller administrative units) were selected from each commune, and total of 600 households were selected from the collines, by systematic random sampling. Ten com-munes (200 households) were urban and 20 communes (400 households) were rural. Of the 600 women interviewed, 321 (53.5%) had not attained any level of edu-cation. Most of those with some education had completed only primary school (33.5%). A majority (44.5%) of the surveyed women
were breastfeeding, and 87 (14.5%) were pregnant (Table 1).
2 IDD NEWSLETTER NOVEMBER 2018 BURUNDI
Dr Sabas Kimboka, an IGN consultant, inspects salt in a wholesale shop in Bujumbura, Burundi.
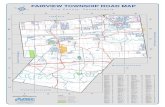
Burundi is divided into 18 provinces, which are further divided into 119 communes. 30 communes were selected to participate in the national survey.
Dr Allain Parfait Nutrition Department, Ministry of Health, Burundi Dr Sabas Kimboka, Dr Vincent Assey, Dr Festo Kavishe and Dr Jonathan Gorstein The Iodine Global Network
Sustainable prevention and control of iodine deficiency disorders in Burundi. Report of a National IDD Survey in women of reproductive age conducted in February 2018. Bujumbura: Ministry of Public Health, ISTEEBU, INSP; 2018
TABLE 1 Surveyed women by age, education level, and maternal status
Characteristic Number (%)Age (years) 15 – 19 63 (10.5)20 – 29 267 (44.5)30 – 39 190 (31.7)40 – 49 80 (1.3)Total 600 Education level No education 321 (53.5)Primary school 201 (33.5)Secondary school or above 78 (13)Total 600 Maternal status Pregnant 87 (14.5)Lactating 267 (44.5)Non-pregnant non-lactating 246 (41)Total 600
IDD NEWSLETTER NOVEMBER 2018 BURUNDI 3
Urinary iodine indicates deficiencyUrine samples from non-pregnant women (n=511) and pregnant women (n=87) were analyzed. The median UIC was 85.5 µg/L in non-pregnant non-lactating women (n=246), and 78.1 µg/L in lactating women (n=267), below the recommended cut-off of 100 µg/L, which indicates iodine defi-ciency in both groups (3). Even though a proportion of the iodine consumed by lactating women is excreted in breast milk, the difference in urinary excretion in lac-tating and non-lactating women was not significant. In pregnancy (n=87), the median UIC was 86.7 µg/L, which is also below the recommended range of 150–249 µg/L, and indicates deficiency. However, the sample size was small.
Iodine content in salt and drinking waterOn the day of the survey, 97% of househol-ds provided a salt sample for testing. Of these, 93.6% tested positive for iodine using an RTK. Out of 541 salt samples analyzed by titration, 72.3% contained more than 15 ppm of iodine, and only 6.5% were non-iodized (Table 2). The availability of iodized salt did not differ significantly between urban and rural households—an indication of a balanced distribution of iodized salt in the country. There was a positive association between
the UIC of the women in the household and the iodine concentration in household salt. All 33 salt samples collected from retail shops across the country and wholesale sellers in the city of Bujumbura contained some iodine. Analysis by titration showed that 18 samples were adequately iodized (15–40 ppm); 9 were inadequately iodized (<15 ppm) and 6 were over-iodized
(>40 ppm).Tap water samples were analyzed for iodine content, to estimate its con-tribution to iodine intake. In areas without access to tap water, samples of underground and surface water (from boreholes, springs, rivers/streams and dams) were collec-ted and analyzed (n=78). However, the iodine concen-tration in all samp-les was negligible, below 1 µg/L.
Iodization awareness and regulatory enforcementInformation about the sources of salt consumed in Burundi was solicited from households (n=582), retail shops across the country (n=24) and wholesalers in the city of Bujumbura (n=9). A majority of the samples were of the processed variety (granular or fine), but mostly were granu-lar. Only four salt samples collected from the households and only one collected from shops were unprocessed (coarse). Wholesalers in Bujumbura city reported that they did not test or verify whether the salt they purchased was iodized, instead relying on a report from Burundi Business Normalization (BBN), a government agency responsible for ensuring that all salt ente-ring the country is iodized. Neither the wholesalers nor the retailers were aware of the existence of national regulations on salt iodization. The shopkeepers also reported that their customers expressed no interest in whether the salt was iodized.
Sources of saltBurundi is a salt importing country. Most of the salt enters the country from Tanzania and Kenya, and some of it is repackaged locally (Table 3). Nyanza Mines (T) Ltd – a company based in Kigoma, Tanzania, sup-plies most of the salt consumed in Burundi.
The survey identified a number of salt brands available on the market in Burundi. Some were clearly marked with the "iodized salt" logo.
TABLE 2 Household salt samples, by iodine concentration (n = 541)
Iodine status Frequency PercentNon-iodized (iodine level <5 ppm) 35 6.5 (95% CI 5–9)
Inadequately iodized (5–14.9 ppm) 115 21.3 (95% CI 18–25)
Adequately iodized (15–40 ppm) 285 52.7 (95% CI 49–67)
Over-iodized (>40 ppm) 106 19.6 (95% CI 16–23)
TABLE 3 Top salt products identified in the survey
Brand name Company LocationChumviNzuri Nyanza Mines (T) Ltd Uvinza, Kigoma Tanzania
ChumviMawe Nyanza Mines (T) Ltd Uvinza, Kigoma Tanzania
Seasalt Sea Salt Dar es Salaam, Tanzania
Habari – Kenya
Chumvisafi International Company & Business Ngozi, Burundi
Kimonyo – Bujumbura, Burundi
– Chance Business Bujumbura, Burundi
– Inakanyana Enterprise Bujumbura, Burundi
4 IDD NEWSLETTER NOVEMBER 2018 BURUNDI
According to the company’s General Manager, Mr. Mukesh Mamlani, the iodiza-tion level of the granular salt is maintained at 45 ppm, in line with the recommenda-tions of the East African and ECSA regions, which stipulate 30–60 ppm (5). The regio-nal recommendations were adopted by the Government of Burundi through a decree dated 18th March 2015 (6). Inadequately iodized or non-iodized salt from small-scale salt producers in Tanzania could be entering Burundi through unofficial border entry points. In addition, some compa-nies from Burundi may be importing salt purchased from Nyanza Mines mixed with non-iodized salt purchased from the small salt producers. Such mixing would result in dilution of the iodine in the salt and most often would go undetected at the border.
RecommendationsThe authors of the report have made the following recommendations:• Strengthen enforcement of the national
regulations on salt iodization. Salt inspec-tors, under the guidance of the BBN, should undergo refresher training to upgrade their skills with regard to inspec-tion and the legal measures available to them to curb non-compliance.
• Monitoring of salt iodization: At pro-duction and border entry points the EA/ECSA iodization levels (30–60 ppm) should apply. The WHO categorization of inadequate concentration (<15 ppm),
adequate (15-40 ppm) and over-iodization (>40 ppm) should apply at consumption level.
• Iodine content in household salt and the median UIC in women of reproductive
age should be permanently incorporated into the national demographic and health surveys (DHS) to update the IDD situati-on every 5 years.
• Carry out public awareness campaigns, particularly in areas of low educational attainment, to create and/or raise consu-mer demand for iodized salt.
• Grassroots/local inspectors should be equipped with RTKs so that they can help households to verify the iodization status of the salt sold by village vendors.
• Form a multi-sectoral consultative group, which will guide the policy and the national program for the control of IDD. Membership of the group should be institutional and should include all relevant ministries and institutions such as those responsible for health, trade and industries, and economic planning. Other
members should be development partners and the association of salt dealers.
• In the long term, the country should esta-blish a titration laboratory to help with in-country analysis of salt iodine content. Apart from monitoring the IDD situation, the laboratory would facilitate any legal action against non-compliant entities by carrying out the necessary testing.
ConclusionsThe median UIC for both non-pregnant, non-lactating women and for lactating women indicates insufficient iodine intakes in Burundi. The low median UIC in pregnant women also suggests inadequa-te iodine intake, but the sample size was small, and a larger survey may be needed to confirm this finding. The proportion of households consuming adequately iodized salt is below the 90% threshold recommen-ded by WHO. These findings indicate that the IDD prevention program is providing inadequate amounts of iodine to young women in Burundi, and more efforts are needed to ensure that optimal iodine intakes are achieved and sustained.
References1. Burundi Population Census, 2012.2. Burundi Demographic and Health Survey Report, 2010.3. UNICEF. Guidance on the monitoring of salt iodi-zation programmes and determination of population iodine status. 2018.4. Assey V, Kimboka S. Brief report on a visit to Burundi to plan for a national IDD survey. Bujumbura, 1–7 November 2015. 5. Draft East African Standard (DEAS 35:2011). Fortified food grade salt — Specification. East African Community, Arusha Tanzania. 2011. Web: www.each.org; E-Mail: [email protected]. Republique du Burundi. Cabinet du Burundi. Decret No100/68 du 18 Mars 2015: Portant Reglementation de la Fortification des Aliments au Burundi. Bujumbura 2015.
Women in Burundi could benefit from public awareness campaigns to improve consumer demand for iodized salt.
Tony
Her
iza
CC B
Y N
D N
C
IDD NEWSLETTER NOVEMBER 2018 IODINE – UNANSWERED QUESTIONS 5
Many adverse consequences of iodine defi-ciency have long been known, but new associations are still being studied and unco-vered.
1. Mild iodine deficiency and neurocognitive outcomesObservational cohorts have demonstrated that mild iodine deficiency in pregnant women may be associated with lower child IQ and poor language development (1–3). Studies have also suggested a link between mild maternal iodine deficiency and sym-ptoms of attention-deficit hyperactivity dis-order in offspring (4). Recent data also sug-gest that iodine deficiency may be associated with decreased fertility in women (5).
2. Thyroglobulin: a new population biomarkerThyroglobulin is a thyroidal protein that is released into the circulation with thyroid hormone. Levels are elevated in populations with both inadequate and excessive iodine intakes. The use of dried blood spot (DBS) thyroglobulin measurements is of interest for population iodine assessment because samp-les can be stored at room temperature, and are simple to transport. Unlike goiter rates, thyroglobulin levels change relatively rapid-ly in response to changes in iodine intake. International standards have been developed for use of DBS thyroglobulin as an index of iodine status in populations of school-aged children (6), and studies to develop this as a biomarker in pregnancy are ongoing (7). In lactating women, it has recently been determined that UIC measures should not be used in isolation, but should be interpre-ted in conjunction with assessment of breast milk iodine concentrations (8).
3. Best interventions for IDD prevention Salt iodization programs that are able to achieve optimal UIC levels in school-aged
children frequently result in mildly low UIC in pregnant women in the same populations (9). A recent multicenter cross-sectional study aimed to determine whether USI alone can achieve optimal iodine intakes in all vulnerable population groups (10). It concluded that, as long as a high proportion of the salt that is consumed is iodized at 25 mg/kg, USI can provide sufficient dieta-ry iodine for all population groups, with the exception of borderline low intakes during pregnancy. Finally, a recent clinical trial demonstrated that in severely iodine-deficient regions it is more effective to sup-plement lactating women with iodine than to directly supplement their breastfed infants (11).
What do we need to know in the future?In many regions of the world there are currently no data regarding iodine status in pregnancy, and in most regions there are no data regarding the iodine status of lactating women. An adequately powered rando-mized clinical trial is needed to establish whether iodine supplementation for mildly/moderately iodine deficient pregnant or lactating women improves child cognitive outcomes. One such trial was previously
attempted but had to be halted when funding was withdrawn (12). Another was recently completed, but women in one of the two study sites proved to be iodine sufficient prior to the intervention (13). While there are some recent data available (14, 15), a better understanding of the effects of iodine excess is needed to inform safe upper expo-sure thresholds, especially in vulnerable groups. As
many governments work to reduce popu-lation sodium intakes, efforts are needed to understand how best to harmonize USI monitoring with salt reduction goals (16). Finally, more work is needed to establish best practices for balancing the different iodine requirements of pregnant women and school-aged children within populations.
References1. Bath SC et al. Lancet. 2013;382:331–7.2. Hynes KL et al. J Clin Endocrinol Metab. 2013;98:1954–62.3. Abel MH, et al. J Nutr. 2017;147:1314–24.4. Abel MH et al. Nutrients. 2017;13:9.5. Mills JL et al. Hum Reprod, e-pub ahead of print 2018.6. Zimmermann MB et al. J Clin Endocrinol Metab. 2013;98:1271–80.7. Stinca S et al. J Clin Endocrinol Metab. 2017;102:23–32.8. Dold S et al. J Nutr. 2017;147:528–37.9. Wong EM et al. Food Nutr Bull. 2011;32:206–12.10. Dold S et al. J Nutr. 2018; 148:587–98.11. Bouhouch RR et al. Lancet Diabetes Endocrinol. 2014;2:197–209.12. Zhou SJ et al. Trials. 2015;16:563-1–563-9.13. Gowachirapant S et al. Lancet Diabetes Endocrinol. 2017; 5:853–63.14. Chen W et al. Am J Clin Nutr. 2017;105:228–33.15. Shi X et al. J Clin Endocrinol Metab. 2015;100:1630–8.16. World Health Organization. Salt reduction and iodine fortification strategies in public health. Geneva, Switzerland: World Health Organization; 2014.
Iodine nutrition: recent research and unanswered questions
Robust data is lacking on whether iodine supplementation for non-severely iodine deficient pregnant women improves child cognition
Elizabeth N. Pearce IGN Regional Coordinator for North America
Excerpted from: European Journal of Clinical Nutrition (2018) 72:1226–1228; https://doi.org/10.1038/s41430-018-0226-7
6 IDD NEWSLETTER NOVEMBER 2018 MADAGASCAR
Universal salt iodization (USI) was adopted in Madagascar in 1995 within the frame-work of a worldwide policy to eliminate iodine deficiency disorders. To combat high rates of goiter among the Malagasy population, the legislation prescribed that crystal salt sold in bulk packaging (25–60 kg sacks) must contain a minimum of 50 ppm (or mg/kg) of iodine, and in salt sold in consumer packs (250 g), the iodine concen-tration must be at least 30 ppm. A national multi-sectoral committee for IDD was esta-blished in the 1990s under the leadership of the Ministry of Public Health and includes the ministries of Commerce, Agriculture, Scientific Research, Interior, and Justice, multilateral partners such as UNICEF, WHO, USAID, and World Bank, as well as salt producers. By 2009, about 72% of households had iodized salt, and about 56% had salt that was adequately iodized (1). In parallel, the prevalence of goiter dropped from 42.5% in 1992 to 6% in 2001, and 3.4% in 2004 (2, 3). However, the 2009–2013 political cri-sis, associated donor sanctions, government budget cuts and subsequent deterioration of public programs have led to a degradation of the salt industry and a reduction in the coverage of USI. In July 2013, the commit-tee for the elimination of iodine deficiency was reactivated under the coordination of the National Nutrition Office. In Madagascar, edible salt production is sufficient to meet the domestic demand. There are three main sources of salt: one large-scale producer in the north, producing 40–50% of the domestic salt using industrial iodization processes, about eight medium-scale enterprises in the mid-western regi-on, which supplies 30–35% of the salt in Madagascar, and over 100 small producers in the south, who supply the remaining 20–25% of the salt. Salt from the medium
and small-scale producers might not be ade-quately iodized (2), and there is no registra-tion or licensing system which would permit the monitoring of iodization levels across the country.
Assessing the impact of the saltiodization programTo assess the national salt iodization pro-gram almost two decades after the promul-gation of the salt iodization legislation in Madagascar, the first nationally representa-tive survey of iodine status was conducted from November 2015 to January 2016. The survey assessed the iodine status in women of reproductive age (WRA, 15–49 years) and the availability of iodized salt in households. This was a stratified two-stage cluster survey. Three strata were selected based on the household coverage with iodized salt reported previously (1: less than 20%; 2: from 20% to 60%; and 3: more than 60%) (Figure 1). In total, 1,721 women from 1,287 households were included in the final ana-lysis. The sample was composed of 1,131 (62.4%) non‐pregnant non-lactating women, 170 (10.7%) pregnant women, and 438 (26.9%) lactating women. Approximately 19.4% of the women surveyed never recei-ved a school education, and 29.4% were educated above elementary school level. The proportion of women having income-generating activities was 82.7%.
Young women in Madagascar have alarmingly low iodine intakes
F IGURE 1 Madagascar was divided into three survey strata according to household access to iodized salt.
<20% in stratum 1
20–60% in stratum 2
and >60% in stratum 3
Each black dot represents a village included in the survey.
TABLE 1 Household coverage with iodized salt in 2015-16 in Madagascar.
Number of samples Median (IQR) household iodine % households with adequately concentration (mg/kg) iodized salt (95% CI)
Stratum 1 420 7.9 (5.8–13.2) 15.6 (10.6, 22.0)
Stratum 2 408 35.3 (16.0–68.0) 18.0 (14.2, 23.0)
Stratum 3 312 69.0 (28.0–123.8) 38.1 (31.0, 46.0)
Excerpted from: Randremanana RV et al. First national iodine survey in Madagascar demonstrates iodine deficiency associated with low household coverage of iodized salt. Maternal & Child Nutrition. 2018 Oct:e12717.
Low iodine intakes are a public health concernThe median UIC in non-pregnant non-lactating women was 47 µg/L (IQR, 16–93 µg/L), and 53 µg/L (IQR, 9–89 µg/L) in pregnant women, denoting moderate iodine deficiency. The median UIC varied signifi-cantly with household wealth (p < 0.001), from 21 µg/L in the poorest quintile to 62 µg/L in the wealthiest quintile. The median UIC of women from households that used adequately iodized salt was 72 µg/L (IQR, 32–149 µg/L) compared with only 50 µg/L (IQR, 16–105 µg/L) in households with inadequately iodized salt. This may suggest that iodized salt is an important source of dietary iodine in Madagascar.
Low coverage with adequately iodized saltThe median iodine concentration in household salt was 10 mg/kg (IQR, 6.3–15.8 mg/kg), bellow the recommen-ded level of ≥15 mg/kg. Consequently, the proportion of households with salt that was iodized adequately was only 26.2% (95% CI, 22.1, 31.0). The availability of adequately iodized salt was lower than previously reported (1), which may reflect the low accuracy of rapid test kits (RTKs) compared with titration methods to assess iodization levels in salt. Strata 1 and 2, which are mainly supplied by
medium and small producers with low capa-city to iodize salt, had a lower proportion of households with adequately iodized salt than Stratum 3, which is supplied by the large-scale salt producer in the north (Table 1). Coarse salt was used in 87.1% of households, fine salt in 12.8% of house-holds, and rock salt in 0.1% of households. Women in most households (92.8%) reported purchasing their salt from a local market or grocery store, and the remaining 7.2% purchased their table salt from a street vendor or received it from a neighbor. More than a half of all households (59.7%) kept their salt in covered containers, 39.1% kept it in its original packaging, and 1.2% kept it wrapped in paper. Salt kept in its original packaging had on average less iodine than salt kept in covered containers.
Wealth may improve access to iodized saltThe survey data revealed that 56.8% of those who purchased their salt in grocery stores were from the two wealthiest catego-ries. A higher household wealth index score might represent more diverse food choices. Additionally, there was inequity in access to adequately iodized salt, with 41% of the wealthiest households having adequately iodized salt versus only 7% of the poorest households, which echoes the findings of other studies (4).
Conclusions and recommendationsThe new national survey shows that the population of Madagascar faces moderate iodine deficiency, which can be linked to a low proportion of households with access to adequately iodized salt. The country has not yet achieved USI, and efforts are needed to revitalize the USI program especially to red-uce the inequity and improve access to ade-quately iodized salt. To sustain effective USI in the long term, it is important to set up a system that coordinates and monitors the production of high-quality iodized salt. To this end, it is important to develop regulato-ry capacity to monitor salt production, and improve iodization capacity among small- to medium-scale salt producers. Such a strategy may include technical assistance with exper-tise in iodization best practices, building capacity in iodization technology, establish-ment of a clear quality control mechanism for salt at production point. In parallel, the monitoring and control of iodized salt during production, sale and consumption must be strengthened. Finally, a public campaign should promote the benefits of using iodized salt in schools, workplaces and the commu-nity involving the media as well as commu-nity nutrition workers and leaders.
References1. INSTAT/Madagascar and ICF Macro. 2010. Enquête Démographique et de Santé de Madagascar 2008-2009. Antananarivo, Madagascar: INSTAT and ICF Macro.2. Jooste P. 2014. Reinvigorating Madagascar's USI program. IDD Newsletter, 42(1).3. ONN. 2010. Evaluation du Plan National d’Action pour la Nutrition (PNAN 2005-2009).4. Knowles JM et al. 2017. Household coverage with adequately iodized salt varies greatly between countries and by residence type and socioeconomic status within countries: Results from 10 national coverage surveys. The Journal of Nutrition, 147(5), 1004S–1014S.
IDD NEWSLETTER NOVEMBER 2018 MADAGASCAR 7
Moderate iodine deficiency in women of childbearing age in Madagascar can negatively impact their babies.
© S
teve
Eva
ns,
via
Flic
kr;
CC
BY
NC
8 IDD NEWSLETTER NOVEMBER 2018 NORWAY
Women were recruited to the Norwegian Mother and Child Cohort Study (MoBa) in their first trimester and completed three questionnaires during their pregnancy. One was an extensive food frequency questi-onnaire asking about their habitual diet (1). The mothers also donated blood and urine samples in gestational week 18. Their children’s development has been continu-ously followed since birth through regular questionnaires and linkage to national regis-tries (e.g., the Norwegian Patient Registry for clinical diagnoses and the Norwegian Prescription Database for dispensed drugs). The cohort includes 114,000 mother-child pairs. Up until now, there have been six publications from MoBa focusing on iodine (2–7), and two more are in preparation. The detrimental effects of severe maternal iodine deficiency (ID) on child neurodevelopment are well documen-ted, but the potential impacts of maternal mild-to-moderate ID remain understu-died. Several observational studies have documented associations with poorer child cognitive functioning, but the few existing randomized controlled trials on the impact of iodine supplement use in pregnancy show conflicting results (8).
MoBa: studying the impact of mild iodine deficiency on developmentThe low iodine intake in Norwegian pregnant women came as a surprise to the researchers. Although Norway has had a long history of endemic goiter due to iodine deficiency, fortification of cow fodder in the 1950s boosted the iodine content in Norwegian milk and the goiter disappeared. However, changes in the diet, including a large decrease in milk consumption, can explain why iodine deficiency has now re-emerged. Although milk intake has decre-ased since the 1990s, milk is still the main source of maternal iodine intake together with supplement use (2,3). Neither salt nor
drinking water are important sources of iodine in the Norwegian diet. In MoBa, we calculated that the median iodine intake from food in the pregnant women was less than a half of the WHO recommended daily intake of ≥150 µg/L (Figure 1) (9). The urinary iodine concentration (UIC) was measured in a subsample of the MoBa women (n=3,000), and the result confirmed an insufficient intake (median UIC: 68 µg/L; mean UIC: 88 µg/L, SD: 80). About one-third of the MoBa women reported using iodine-con-taining supplements, and their median UIC was higher than in the women not using any supplements (98 µg/L vs. 59 µg/L).
Mild-to-moderate iodine deficiency in the world’s largest pregnancy and birth cohortMarianne Hope Abel PhD student, TINE SA/Norwegian Institute of Public Health/Oslo Metropolitan University; Helle Margrete Meltzer PhD, Research Director at the Division of Infectious Diseases and Environmental Health, Norwegian Institute of Public Health; Heidi Aase PhD, Department Director for Dept. of Child Health and Development, Norwegian Institute of Public Health; Liv Elin Torheim Professor of Public Health Nutrition, Chair of the National Nutrition Council, Oslo Metropolitan University; Anne Lise Brantsæter PhD, Norwegian Institute of Public Health, Oslo, Norway
Thousands of mother-child pairs participate in a the Norwegian Mother and Child Cohort Study (MoBa).
© K
im A
bel
In Norway, one in every four children born in the years 2002–08 is a participant of a large national pregnancy cohort. The study has revealed that the mothers were mild-to-moderately iodine deficient during pregnancy. Results have now been published that link insufficient maternal iodine intake to poorer child neurocognitive development.
IDD NEWSLETTER NOVEMBER 2018 NORWAY 9
The extensive data collection in MoBa makes it possible to examine associations between maternal iodine intake and a range of maternal and child outcomes. The pub-lished papers to date include: • A validation study of iodine intake
measured by the FFQ (2); • Determinants of suboptimal iodine intake
in MoBa (3); • Maternal iodine intake and thyroid func-
tion in pregnancy (6); • Associations between iodine intake and
measures of child neurodevelopment:o Child language, motor skills, and beha-
viour at age 3 years (4); o Child risk of attention deficit/hyperac-
tivity disorder (ADHD) (5); o Child language and learning at age 8
years (7). In addition, two papers are in preparation, one on pregnancy- and birth outcomes and the other on child risk of autism.
Iodine intake of <150 µg/day in pregnancy is associated with poorer child developmentFindings thus far indicate that maternal habi-tual iodine intake of less than about 150 µg/day is associated with changes in maternal thyroid hormone levels in pregnancy (free T4 and free T3) (6) and suboptimal child neurocognitive development at ages 3 and 8
years. Children of iodine deficient mothers had an increased risk of language delay (4,7), poorer fine motor skills (4), more behavior problems (4,7), poorer school performance in reading and writing (7), and an increased likelihood of receiving special educational services in school (7). We found no signi-ficant associations with child gross motor skills (4) or with an ADHD diagnosis in the patient registry (5). The latter might be explained by the low prevalence of ADHD diagnosis in MoBa children at the time of data collection (2%). Overall, effect sizes were small. This may indicate that mild-to-moderate iodine deficiency has only minor consequences for child neurodevelopment, but it is also likely that measurement errors of the exposure and outcomes weaken these associations.
Iodine supplement use in pregnancy may not be beneficialShort-term use of iodine-containing sup-plements may have a different impact on maternal thyroid function and child neu-rodevelopment than habitual long-term iodine intake. Thus, we explored iodine supplement use as a separate exposure. Additionally, we examined whether the time of initiation of the supplement (i.e., before pregnancy, in the first trimester, or later in pregnancy) was of importance.
Interestingly, there was no indication of beneficial effects of iodine supplement use in pregnancy. In fact, we found that initia-ting use in the first trimester was associated with more child behaviour problems (4) and ADHD symptoms, and an increased risk of an ADHD diagnosis (5). We also found that pregnant women who had initiated supplement use within the past 5 weeks had lower thyroid function (significantly lower FT4 and non-significantly lower FT3), which might indicate that an abrupt increase in iodine intake in pregnant women with mild-to-moderate ID might transiently inhi-bit thyroid function (6). The foetus is most vulnerable to changes in maternal thyroid hormone levels in the first trimester, and thus this transient inhibition might explain the negative impact on the behaviour out-comes. Importantly, these results need to be confirmed in sufficiently powered rando-mized controlled trials. It is, however, fair to conclude that knowledge to date suggests that it is important to prevent ID before conception to secure optimal fetal brain development.
F IGURE 1 Maternal iodine intake from food in the first half of pregnancy (n=82,623). The sample consists of eligible MoBa participants (singleton pregnancies, available data on iodine intake, no reported use of thyroid medication in pregnancy). The range of iodine intake from food was 9–792 µg/day.
0 50 100 150 200 250 300 350 400 450 500 550 600
Habitual iodine intake from food (µg/day)
Freq
uenc
y
0
20
00
400
0 60
00
80
00 Median (IQR): 121 (89, 161) µg/day
Nordic Nutrition Recommendations: Recommended intake in pregnancy: 175 µg/day
World Health Organization: Recommended intake in pregnancy: 250 µg/day
10 IDD NEWSLETTER NOVEMBER 2018 NORWAY
Strengths and limitationsStrengths of the MoBa study include its large sample size, extensive data collection, and the population-based prospective design. In addition, the fact that data on iodine intake is available at the individual level, that ID is highly prevalent in the MoBa mothers, and that iodine intake varied a lot between the mothers make MoBa a unique opportunity to explore the impact of ID in pregnancy. There is limited data on iodine status of the MoBa children, but based on data from other Norwegian studies, their iodine intake is likely to be adequate (7). Thus, ID is most likely to occur primarily in pregnancy and during breastfeeding. An important limitation is that MoBa is an observational study, and consequent-ly, we cannot know if the associations we study represent causal relationships. Residual confounding by other factors associated with maternal iodine intake may still exist. However, maternal iodine intake did not
differ by maternal age, marital status, or income, and varied only to a very small extent (up to ±8 µg/day) by BMI, parity, education, and smoking (3). When testing multiple associations, some associations may turn out to be significant simply due to chance. However, the associations between maternal habitual iodine intake and child neurodevelopmental outcomes were very consistent. When studying the associations between maternal iodine supplement use and the same outcome measures, the only signifi-cant associations were with behaviou-ral outcomes. Thus, we cannot rule out that this may represent a chance finding. The measures of habitual iodine intake of the mothers and of child neurocognitive development are inherently inaccurate. However, a validation study demonstrated that the MoBa FFQ provides a realistic estimate of iodine intake and is valid for ranking women from low to high intake (2,6).
ConclusionsOverall, studies from MoBa support the growing body of evidence from observatio-nal studies and animal studies that maternal mild-to-moderate ID adversely affects child neurocognitive development. The results from MoBa add to the growing body of evidence that timely prevention of maternal mild-to-moderate iodine deficiency is essen-tial to ensure that children reach their full developmental potential.
Key implications• Habitual iodine intake of below the
recommended 150 µg/day in women of childbearing age should be prevented to ensure optimal foetal brain development.
• Initiating iodine supplement use in preg-nancy to correct mild-to-moderate ID may be too late to have beneficial effects on child development. Whether supple-ment use can be harmful remains to be further explored in studies with a rando-mized controlled design.
• It is probably important to differentiate between maternal habitual iodine intake from food and short-term/recent iodine intake from supplements when studying associations with maternal and child out-comes.
• Results from observational studies indi-cate that the effects of mild-to-moderate ID and iodine supplement use on child development are small, thus randomized controlled trials need to be large and suffi-ciently powered to detect potential effects.
• When studying mild-to-moderate ID, it is important that the women are truly iodine deficient, and based on the result from MoBa, the median UIC should ideally be <100 µg/L.
References:1. Magnus P et al. Cohort profile update: The Norwegian Mother and Child Cohort Study (MoBa). Int J Epidemiol 2016;45(2):382-8. doi: 10.1093/ije/dyw029.2. Brantsaeter AL et al. Evaluation of urinary iodine excretion as a biomarker for intake of milk and dairy products in pregnant women in the Norwegian Mother and Child Cohort Study (MoBa). Eur J Clin Nutr 2009;63(3):347-54. doi: 10.1038/sj.ejcn.1602952.3. Brantsaeter AL, et al. Risk of suboptimal iodine intake in pregnant Norwegian women. Nutrients 2013;5(2):424-40. doi: 10.3390/nu5020424.4. Abel MH et al. Suboptimal maternal iodine intake is associated with impaired child neurodevelopment at 3 years of age in the Norwegian Mother and Child Cohort Study. J Nutr 2017;147(7):1314-24. doi: 10.3945/jn.117.250456.5. Abel MH et al. Maternal iodine intake and offspring attention-deficit/hyperactivity disorder: Results from a large prospective cohort study. Nutrients 2017;9(11). doi: 10.3390/nu9111239.6. Abel MH et al. Iodine Intake is Associated with Thyroid Function in Mild to Moderately Iodine Deficient Pregnant Women. Thyroid 2018;28(10):1359-71. doi: 10.1089/thy.2018.0305.7. Abel MH et al. Language delay and poorer school performance in children of mothers with inadequate iodine intake in pregnancy - results from follow up at 8 years in the Norwegian Mother and Child Cohort Study. Eur J Nutr;In review.8. Velasco I, Bath SC, Rayman MP. Iodine as essential nutrient during the first 1000 days of life. Nutrients 2018;10(3). doi: 10.3390/nu10030290.9. Andersson M et al. Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: conclusions and recom-mendations of the Technical Consultation. Public Health Nutr 2007;10(12A):1606-11. doi: 10.1017/S1368980007361004.
Short-term use of iodine-containing supplements during pregnancy may have a different impact on maternal thyroid function and child neurodevelopment than habitual long-term iodine intake.
© T
orbe
in R
onni
ng v
ie F
lickr
; C
C B
Y N
C N
D
IDD NEWSLETTER NOVEMBER 2018 IODINE COOKBOOK 11
Iodine cookbook: a recipe for improved iodine intakes in the UK
What process led to the creation of this cookbook?With the aim of increasing the iodine intake in at-risk groups, particularly prior to, and during pregnancy, we decided to create a basic cookbook of iodine-rich recipes rele-vant to the UK situation. Our intention was reinforced by our participation in the Horizon 2020 EUthyroid project which aimed to improve iodine intake across Europe. We gathered data on the iodine concentration of foods from the UK food-table database (1). Foods with an iodine concentration greater than 20 µg/100 g were defined as iodine-rich and were there-fore suitable recipe ingredients. However, clearly it is not just the iodine concentration of a food but the quantity of that food that is consumed that is important. Data from the UK National Diet and Nutrition Survey (NDNS) allowed us to identify foods that contributed more than 5% to total iodine intake. This resulted in a list of key ingredients for recipes: milk, milk products, fish/seafood and eggs. Though many countries have wide availabi-lity of iodized salt, this is not the case in the UK where it is very difficult to find. We then searched the PubMed data-base to identify additional factors that affect iodine uptake or use by the body so that we could take these into account. These factors were selenium and iron – both essential for the production of thyroid hormones (2) – and foods with goitrogenic properties, i.e., foods that can reduce iodine uptake or utili-zation.
How did you go about creating the iodine-rich recipes?Existing recipes were adapted and new reci-
pes created to give 28 easy-to-make dishes that catered for a variety of dietary requi-rements. Each recipe was analyzed using Nutritics, the online nutrient-analysis soft-ware, to provide a nutritional breakdown of iodine, iron and selenium. Nutritional con-tent per portion of recipes was rated against the European Food Safety Authority (EFSA) recommendations for adults and pregnant women. Recipes have symbols indicating their suitability for those following a gluten-free, vegetarian or vegan diet or their unsu-itability for pregnant women. As the main sources of iodine are not suitable for vegans, an iodine-fortified milk-alternative drink has been used in some recipes to optimize iodine intake for individuals who exclude the key iodine source of cows’ milk.
How would you adapt the cookbook for other countries?We already know from our EUthyroid research that the dietary factors that have the biggest contribution to iodine intake and
status (as measured by urinary iodine con-centration) vary between the UK, Spain and the Netherlands, the three countries from which we have data. Bread is an important iodine source in the Netherlands as iodized salt is used in its preparation. For Spain, fish is a very important source while for the UK, milk and dairy products are the major sour-ce. The UK has a higher concentration of iodine in milk, averaging 60 µg per 200 ml, than the other three countries. Countries such as Chile, China, Ecuador, Peru and New Zealand, where iodized salt is available to over 80% of households, could emphasize the use of adequately iodized salt in recipes as this can make a significant contribution to daily iodine intake. However, this strategy is not applicable to the UK as iodized salt is poorly available and only iodized to 11.5 mg/kg (3).
Joanne Tattersall and Declan Henderson worked on the development of the Iodine Cookbook in the course of their BSc final-year student projects. Mariana Dineva worked on the book as part of her PhD project on iodine.
References1. Public Health England. Composition of foods inte-grated dataset (CoFID) - Gov.uk. 25 March 2015. Available at: https://www.gov.uk/government/publi-cations/composition-of-foods-integrated-dataset-cofid.2. Hu S, Rayman MP. Multiple Nutritional Factors and the Risk of Hashimoto’s Thyroiditis. Thyroid 2017; 27(5):597-610.3. Bath SC, Button S, Rayman MP. Availability of iodised table salt in the UK – is it likely to influence population iodine intake? Public Health Nutr 2014; 17:450–4.
Excerpted from: Tattersall J, Henderson D, Dineva M, Bath S, Rayman M. The iodine cookbook. Department of Nutritional Sciences, Faculty of Health and Medical Sciences, University of Surrey, Guildford, UK; 2018.
In the UK, iodine deficiency has been reported in several population groups, most notably in pregnant women, young women, and those who exclude certain food groups, e.g. vegans. A new iodine-rich recipe book was developed by three students at the University of Surrey, supervised by Sarah Bath and Margaret Rayman, to help improve iodine intake, with support from the EUthyroid project.
© J
oann
e Ta
tter
sall
28 easy-to-make recipes using iodine-rich ingre-dients can be found in the new UK cookbook.
© J
oann
e Ta
tter
sall
(Inst
agra
m)
12 IDD NEWSLETTER NOVEMBER 2018 MACEDONIA
A recent publication has classified the Republic of Macedonia as one of eleven countries to achieve sustainable elimination of iodine deficiency (1). This success is a result of cross-sectoral efforts under the gui-dance of the National Committee for Iodine Deficiency, and significant involvement of the professional and academic community, including its key institutions: Institute of Pathophysiology and Nuclear Medicine, University Clinic for Child Diseases, and University Clinic for Gynecology and Obstetrics.
Universal salt iodization Prior to 2000, many reports indicated clearly that Macedonia was iodine deficient, with frequent occurrence of endemic goiter (2–4). Moderate iodine deficiency was confirmed by the first nationwide study of 11,486 schoolchildren in 1995–96, which examined the thyroid gland by palpation and ultrasonography and measured urinary iodine excretion (5, 6). The health authorities quickly recognized that iodine deficiency was an important issue which should be addressed in a timely and collaborative manner. This led to the establishment, in 1997, of a multi-sectoral National Committee for Iodine Deficiency under the auspices of the Ministry of Health. The Committee is made up of representatives of diverse sectors, including policy, professional associations, academia, international community and the salt industry. By 1999, the Committee was
ready to adopt regulation on universal salt iodization. The move met with prompt approval from all stakeholders, in particular the industry partners, who have played an instrumental role in supporting its imple-mentation and regular monitoring (5). The National Committee, in coo-peration with the Food Directorate, has implemented a series of activities to enforce and monitor salt iodization more efficiently. In addition to periodic inspection, iodiza-tion levels have been assessed in samples of household salt collected from primary schoolchildren taking part in iodine status surveys. Very quickly, the proportion of under-iodized salt dropped from 46% in 2000 to only 6% in 2001. In 2016, a survey analyzed 1,114 samples of household salt to find that only 6 were under-iodized. This success is largely the result of strict control over policy implementation. It has been
helped by the fact that Macedonia imports all salt for human consumption through a limited number of importers, and any improperly iodized salt is returned to the importer.
Continued efforts are key to sustaining iodine sufficiency in MacedoniaBorislav Karanfilski National Committee for Iodine Deficiency, Macedonia; Neda Milevska-Kostova Studiorum think-tank; Daniela Miladinova Institute of Pathophysiology and Nuclear Medicine; Viktorija Jovanovska University Clinic of Gynaecology and Obstetrics; Mirjana Kochova University Clinic of Children Diseases, Faculty of Medicine, University “Ss. Cyril and Methodius”
F IGURE 1 Urinary iodine concentration and goiter incidence in Macedonia in studies conducted from 1995 to 2007.
1995/96 2001 2002 2003 2005 2007
Urin
ary
iodi
ne c
once
ntra
tion
µg/L 300
250
200
150
100
50
0
Goi
ter
(%)
20
15
10
5
0
18.7
117
198 191
4.72.05
5
164
5.8
229 241
0.99
IDD NEWSLETTER NOVEMBER 2018 MACEDONIA 13
Achieving iodine sufficiency in school-age childrenSurveys of iodine status have shown a steady increase in the urinary iodine concentrati-on, in correlation with decreasing thyroid volumes and incidence of goiter (Figures 1 and 2). In 2003, an international team of experts nominated by WHO, UNICEF and ICCIDD declared Macedonia free of iodine deficiency.
Iodine status of pregnant womenThe first assessment of iodine status in pregnant women in Macedonia was under-taken in 2001 and included 382 women. The median urinary iodine concentrati-on (UIC) was 140.4 µg/L with 25.1% of women having a UIC below 100 µg/L, which indicates mild iodine deficiency. At the same time, the median UIC in school-children was 164.5 µg/L, within the optimal range. This result implies that iodized salt was not meeting the dietary requirement during pregnancy at the time. A survey in 2006–2007, conducted in a small sample of pregnant women, reported an improved median UIC within the optimal range (150–249 µg/L) (7,8). A new survey was com-pleted in 2017 with financial support from UNICEF. Six hundred pregnant women (200 per trimester) from across Macedonia were recruited at an ante-natal visit to the University Clinic for Gynecology and Obstetrics in Skopje, the only tertiary faci-lity for gynaecology in Macedonia. The median UIC was 167.5 µg/L, which con-firms an adequate iodine intake. In pregnant
women who were taking 150 µg iodine per day through vitamin supplements (n=300) the median UIC was 182.5 µg/L, high-er than in women who did not take any supplements (n=300, 160.2 µg/L). These results suggest that universal salt iodization alone has been effective at bringing the iodine intakes during pregnancy up to the recommended range. Given its accessibility, iodized salt offers a far more feasible way of achieving and sustaining optimal iodine intakes in this population group than sup-plementation, which is selectively available only to those who can afford it.
Neonatal TSH screening To monitor the iodine status post-partum, the University Clinic for Children's Diseases at the Medical Faculty in Skopje introduced TSH screening in 2002, covering almost 100% of newborns. The aggregate results for the period 2002–2017 in a total of 294,592 neonates report that TSH values greater than 5 mlU/L were found in 3.22% of newborns, indicative of sufficient iodine status.
ConclusionsThanks to the ongoing efforts of all stake-holders, Macedonia continues to sustain optimal iodine intakes in schoolchildren, pregnant women and newborns. However, to prevent a decline in salt iodization levels and the re-emergence of iodine deficiency, these efforts must continue, in particu-lar regular monitoring of iodine status in school-age children, women of reproductive age, and pregnant women.
AcknowledgementsThe past two decades of work on achieving and sustaining the elimination of iodine defi-ciency in the Macedonia would not have been possible without dedicated work of many institutions and individuals, inclu-ding the National Committee for Iodine Deficiency, the Association of Gynaecologists and Obstetricians of Macedonia, the civil society, and industry partners. The following experts played particularly important roles in the surveys to date: Venjamin Majstorov, Sonja Kuzmanovska, Olivija Vaskova, Daniela Pop Gjorcheva and Ana Ugrinska from the Institute of Pathophysiology and Nuclear Medicine; Goran Dimitrov, Ajla Shabani, Igor Samardziski, Goran Kocoski, Adela Stefanija and Aleksandra Atanasova Boshku from the University Clinic of Gynaecology and Obstetrics; Violeta Anastasovska and Nikolina Zdravevska from the University Clinic for Children Diseases; Vladimir Dimkovski and Jasminka Radoshevik from Studiorum think-tank, and Biljana Chuleva from the Institute of Public Health of the Republic of Macedonia.
References 1. Vitti P. 2018. Iodine deficiency disorders. UpTo-Date 15.2. Petrov S. 1954. Macedonia as a Goitrous Area. Hygiene, 7: 322-328.3. Ramzin S. 1959. The importance of Endemic Goitre, the Problems of Epidemiology and Ethology in our Country. Collection of Works of the First Yugoslavian Symposium on Goitre. Belgrade, 27- 60.4. Karanfilski B et al. 1992. Iodine Prophylaxis and Eradication of Endemic Goitre in Macedonia. Mac. Med. Review, 5-6: 140-144.5. Karanfilski B et al. 1998. Iodine deficiency in the Republic of Macedonia. University “Ss. Cyril and Methodius”, Faculty of Medicine, Institute of Pathophysiology and Nuclear Medicine, Skopje (Monograph), pp. 1-120.6. Karanfilski B et al. 2008. Iodine deficiency in preg-nancy and lactation. National Committee for iodine deficiency-Ministry of health, Skopje (Monograph) pp.1-68.7. WHO. 2013. Urinary iodine concentrations for determining iodine status in populations.8. Karanfilski, B et al. 2009. Macedonia begins to monitor IDD in pregnant and lactating women along with school-age children. IDD Newsletter, August 2009.
F IGURE 2 Thyroid volumes (median value) in schoolchildren (7–10 years of age) in Macedonia, from 1996 to 2016.
1996 2002 2003 2016
Assessment year
Volu
me
(ml)
7
6
5
4
3
2
1
0
BoysGirls
14 IDD NEWSLETTER NOVEMBER 2018 BENIN
On Saturday, October 27, Benin marked the 21st “National day of mobilization for the fight against iodine deficiency disorders” (Journée nationale de mobilisation pour la lutte contre les troubles dus à la carence en iode). Hosted at the General Education College in Agbangnizoun (Zou department) in south-western Benin, the celebrations were launched by Dr. Françoise Assogba Komlan, General Secretary of the Ministry of Agriculture, Livestock and Fisheries, and M. Venance Gandaho, Deputy General Secretary of the Ministry of Health. The theme of the day’s events: "Adequately iodized salt guarantees child development," was chosen to remind the community of the importance of iodized salt for the whole family, especially children, in the prevention of IDD. It was an opportu-nity for the authorities to educate the public on the role iodine plays in the proper func-tioning of the body. In pregnancy, iodine deficiency can be responsible for spontane-ous abortion, premature delivery, fetal death or impaired development of the fetal brain. “Iodine deficiency disorders are often irre-versible and the prevention is the only way to fight them," warned Mr. Gandaho. Dr. Assogba Komlan reminded those present that the elimination of IDD was adopted as a global goal at the World Summit for Children in 1990, including by Benin, which has since made tremendous progress thanks to collaborative efforts of many sections of the government. However, despite the efforts to promote iodized salt, pockets of low coverage still exist, particu-larly in the south. The reasons include the reluctance of local salt harvesters to iodize locally produced salt, poor involvement of local elected representatives in the promo-tion of iodized salt, and the reluctance of salt sellers to adhere to regulations and good practice, and irregular monitoring of iodiza-tion levels. This situation could be reme-died as part of the Government’s "Imple-
mentation of the food strategy to reduce malnutrition" plan, in alignment with the National Plan for Agricultural Investment and Food and Nutrition Security (Pniasan2017–2021).
The strategy foresees implementing an effec-tive food and nutrition communication plan, increasing the capacity of technical officers to implement food and nutrition advice, and promoting behaviour change in the population.
Raising awareness of iodized salt in BeninE. Jacques Hougbenou Houngla Director of Food and Applied Nutrition; Ministry of Agriculture, Livestock and Fisheries; Republic of Benin
M. Venance Gandaho, Deputy General Secretary of the Ministry of Health, speaking at the event.
A Beninese girl is testing a salt sample with a rapid test kit (RTK) to see if it turns purple, meaning it contains iodine.
IDD NEWSLETTER NOVEMBER 2018 BENIN 15
Dr. Françoise Assogba Komlan, General Secretary of the Ministry of Agriculture, handing out iodized salt.
The slogan “Adequately iodized salt guarantees child development” was printed on posters to raise the awareness of IDD.
The mayor of Agbangnizoun, Gaspard Gboli-Honon, thanked the government for launching the celebrations in his locality and committed to join in the efforts to eli-minate IDD. The Secretary General of the prefecture of Zou, Julien Ouankpo, pointed out that the indicators of iodized salt con-sumption in his department, specifically in Agbangnizoun, are not good. "It is impera-tive to change behaviour," he said.
History of iodine deficiency elimination in BeninIodine deficiency disorders were histo-rically endemic in Benin. A baseline survey of IDD in 1994 found that close to a fifth of the population had goiter, and the median UIC was only 40 µg/L. In the same year, salt iodization became mandatory, at 60–100 parts per million (ppm) of iodine at production, 50–60 ppm at importation, and 30–50 ppm at the retail level. By 2000, 76.8% of households had iodized salt, and 56% of households had salt that was iodized adequately (at least 15 ppm). At the same time, the goiter prevalence had dropped significantly and the UIC increased to 424 µg/L, indicating that iodine intakes were now excessive. In February 2009, the national legislation was amended to lower the required iodine concentration in salt to 30–40 ppm at production/retail and 15–40 ppm at the household level. A national survey in 2011 reported a median UIC in almost 800 children (6–12 yrs) to be 318 µg/L, and household coverage with adequately iodized salt of 86%. Salt har-vested by small-scale producers popular in the southern part of the country, which tends to be not iodized, has been identified as a key limiting factor in achieving universal coverage in Benin.
The event was well-attended.
16 IDD NEWSLETTER NOVEMBER 2018 NEW ZEALAND
Bread overtakes dairy to improve iodine intake in New Zealand
Are iodine intakes adequate in New Zealand?Iodization of salt was first introduced in New Zealand in 1924 which dramatically reduced the rate of goiter, from 30% of schoolchildren to less than 1% (1). In the past 20 years, several studies have indicated a re-emergence of mild iodine deficiency in New Zealand (2-4). This led to the man-datory fortification of bread with iodine through the replacement of non-iodized salt with iodized salt in New Zealand from September 2009. Representative surveys of the iodine status of New Zealand adults have shown significant improvements since the intro-duction of mandatory fortification of bread. Adults in a regional 2014/15 survey had a median urinary iodine concentration of 103 µg/L, in comparison to 53 µg/L in the 2008/09 Adult Nutrition Survey (5). This level of intake is borderline adequate, and iodine remains a priority nutrient as long as there are concerns that intake levels in the New Zealand diet are inadequate or are approaching inadequate levels.
2016 NZTDS: estimating total dietary iodine intake The 2016 New Zealand Total Diet Study (2016 NZTDS) was a large-scale food sur-vey undertaken over the 2016 calendar year. The study involved the analysis of 1,056 composite food samples, with eight samp-les taken of 132 different food types. The selected food types represent the most com-monly consumed foods for the majority of New Zealanders. All 1,056 of the collected samples were analyzed for iodine using ICP-MS. Using simulated diets developed for 10 New Zealand population cohorts, including
for the first time in the NZTDS two Pacific Island ethnicity adult cohorts, the dietary exposure/intake has been estimated.
Presence and concentrations of iodine in foodsIodine concentrations were detected in 61% (640 out of 1,056) of the sampled foods. Because the 2016 NZTDS had comparable limits of reporting (LOR) to those used in the 2009 NZTDS, the reported prevalence of iodine can be considered similar to that of 2009 NZTDS, where 66% (643 out of 982) of the food samples had detectable iodine concentrations. In 2016, iodine was widespread across the food types, however, the majority of foods (498) had concen-trations of less than 0.1 mg/kg iodine. The highest iodine concentrations were in oysters (0.8–1.8 mg/kg) and mussels (0.9–3.1 mg/kg). The impact of mandatory fortification of bread with iodine is evident in the large
increase in iodine concentrations in bread in the 2016 NZTDS, compared with previous NZTDSs (Figure 1). Of the foods newly included in the 2016 NZTDS simulated diets, sushi shows appreciable iodine concentrations (range 0.18–0.76 mg/kg). This is expected to result from the use in the sushi wraps of seaweed (nori), a natural iodine accumulator that is reported to contain 29–46 mg/kg iodine (6).
Foods contributing to iodine intakesIt is important to note that the estimates do not account for any iodine intake through the use of discretionary iodized salt, which may increase iodine intake. Iodine intakes for adult females were the lowest of the adult population cohorts, with an estimated dietary intake of 100 µg/day. For all the adult age groups, the largest contribution to iodine intakes was from cereal grain-based foods, with dairy and fish, meat and eggs
According to the latest New Zealand Total Diet Study (2016 NZTDS), the declining intake of iodine has been reversed for the first time since the mid-1990s thanks to the mandatory use of iodized salt in bread manufacture.
F IGURE 1 Iodine concentration (mid-bound mean) trends in the NZTDS (1987/88–2016)
1987/88 1990/91 1997/98 2003/04 2009 2016
NZTDS year
Iodi
ne c
once
ntra
tion
(mg/
kg)
0.45
0.4
0.35
0.3
0.25
0.2
0.15
0.1
0.05
0
Bread, wheatmeal
Bread, white
Hamburger, plain
Fish, fresh
Milk (3.25%)
Excerpted from: Pearson A et al. 2016 New Zealand Total Diet Study. Wellington: Ministry for Primary Industries; 2018. Available from: https://www.mpi.govt.nz/food-safety/food-monitoring-and-surveillance/new-zealand-total-diet-study/
IDD NEWSLETTER NOVEMBER 2018 NEW ZEALAND 17
also major contributors. Mandatory forti-fication of bread with iodine has markedly increased the contribution of cereal-based foods to total iodine intake (Figure 2). While dairy products have historically been the largest source of iodine intake in the New Zealand diet, bread was the prima-ry dietary source of iodine in the 2016 NZTDS. In the child and teenage cohorts, the estimated iodine intakes ranged from 70 µg/day for toddlers to 133 µg/day for teenage boys. The child and teenage population cohorts showed a similar high contribution from grains in the diet as the adults. For the infant and toddler age groups, dairy products were the most important source for toddlers, and dairy-based infant formula for infants. This is consistent with the 2009 NZTDS, in which dairy products contributed 66% of the iodine intake for toddlers, and infant formula 72% of the intake for infants.
Comparison with dietary requirementsThe increase in iodine intake evident since the 2009 NZTDS meant that all of the population cohorts met or exceeded the estimated average requirements (EAR) for iodine. The dietary iodine intake for infants was 76% of the adequate intake (AI), as no EAR is available in this population. The increase in dietary iodine intakes across the population cohorts is a large change from the plateau in iodine intakes since the 1997/98 NZTDS and the large decrease noted in the NZTDS studies before this (Figure 3). As a result of mandatory fortification of bread with iodine, all of the population cohorts, except infants, are now receiving dietary iodine intakes sufficient to meet nutritional requirements. This has not been achieved in most of the population cohorts since the early 1990s. Not many other national diet surveys analyze for iodine, as many nations’ soils
naturally contain iodine concentrations sufficient to contribute to dietary intakes. The Irish Total Diet Study (ITDS) reported higher dietary intakes of iodine for all of its age groups, compared with the 2016 NZTDS (7). In the ITDS, dairy products were the major contributors to dietary iodine intake.
ConclusionsDietary intake estimates for iodine have shown a remarkable improvement for all of the population cohorts, compared with previous NZTDSs, largely as a result of the mandatory fortification of bread with iodine. The daily dietary intakes for iodine for all population cohorts, apart from infants, now meet or exceed the relevant NRVs, rever-sing the decline seen since the mid-1990s.
References1. Mann, J., Aitken, E., 2003. The re-emergence of iodine deficiency in New Zealand? The New Zealand Medical Journal; 116(1170): 351–356.2. MOH (Ministry of Health), 2003. NZ Food, NZ Children: Key results of the 2002 National Children’s Nutrition Survey. MOH, Wellington.3. MOH (Ministry of Health), 2011. A focus on nutri-tion: Key findings of the 2008/09 New Zealand Adult Nutrition Survey. MOH, Wellington.4. Skeaff, S.A., Thomson, C.D., Gibson, R.S., 2002. Mild iodine deficiency in a sample of New Zealand schoolchildren. European Journal of Clinical Nutrition; 56: 1169–1175.5. MPI (Ministry for Primary Industries), 2016. Mandatory iodine fortification in New Zealand: supplement to the Australian Institute of Health and Welfare 2016 report – monitoring the health impacts of mandatory folic acid and iodine fortification. MPI, Wellington.6. Yeh, T.S., Hung, N.H, Lin, T.C., 2014. Analysis of iodine content in seaweed by GC-ECD and estimation of iodine intake. Journal of Food and Drug Analysis; 22(2): 189–196.7. FSAI (Food Safety Authority of Ireland), 2016. Report on a Total Diet Study carried out by the Food Safety Authority of Ireland in the period 2012–2014. FSAI, Dublin.
F IGURE 3 Dietary iodine intake trends in the NZTDS (1982–2016) characterized against the estimated average requirements (EARs)*
1982 1987/88 1990/91 1997/98 2003/04 2009 2016
NZTDS year
Estim
ated
dai
ly io
dine
inta
ke µ
g/da
y
350
300
250
200
150
100
50
0
Young adult male (19–24 years)
Adult female(25 years +)
Toddler (1–3 years)
EAR Adult
EAR Toddler
*Adult EAR: 100 µg/day; Toddler EAR: 65 µg/day
F IGURE 2 Major iodine contributing food group trends in the NZTDS (1997/98–2016) for young adult males (19–24 yrs) and comparison to iodine contributing food groups in the Irish adult diet (2012/14 ITDS*)
1998/99 2003/04 2009 2016 ITDSNZTDS year or overseas TDS
Cont
ribut
ion
to io
dine
inta
ke (
%)
100
90
80
70
60
50
40
30
20
10
0
*ITDS: Irish Total Diet Study (FSAI, 2016)
Other foods
Grains
Dairy products
Composite foods/takeaways
Chicken, eggs, fish and meat
18 IDD NEWSLETTER NOVEMBER 2018 MEETINGS AND ANNOUNCEMENTS
In memory of Nicté Ramírez
Nicté Yasmín Ramírez Rodríguez passed away on November 3, 2018. She was former Director of the Comprehensive Health Care System (Sistema Integral de Atención en Salud - SIAS), Ministry of Public Health and Social Assistance, Guatemala and former valued staff member of UNICEF and INCAP. She made an indelible mark as a researcher, teacher, and manager of regional and country projects in public nutrition, health and micronutrients. Nicté served as IGN National Coordinator in Guatemala for more than 15 years. In her role, she embodied tenacity, perseverance, com-mitment and cooperation, which contributed to the success of salt iodization programs and elimination of IDD across Central America. She was a dear colleague, companion and friend. Her passing is a great loss for the scientific and public health community in the Region. We extend our heartfelt condolences to her family, especially her daughter Debbi and her grandson Santi.
MEET INGS AND ANNOUNCEMENTS
GiveWell announces that IGN is a ‘standout’ charity for the fifth time
On ‘Giving Tuesday,’ which marks the ope-ning of the end-of-year season of charitable giving, the charity evaluator GiveWell posted its annual shortlist of the best and most effective organizations, to help donors make informed decisions. For the fifth year running, IGN has been named a ‘standout’ charity, which reco-gnizes the tremendous impact of iodized salt on
improving iodine intakes and eliminating the negative consequences of deficiency. Although the list of recommended charities continues to expand, GiveWell’s rigorous vetting process means that currently fewer than 20 organiza-tions globally pass muster. The GiveWell recommendation, echoed by Peter Singer’s charity The Life You Can Save,
has over the years allowed IGN to raise funds from generous and supportive donors such as Good Ventures, MaxMind, and numerous others. “The global progress towards the elimi-nation of iodine deficiency is truly a modern public health success story. Our standing with GiveWell allows us to bring this story to new audiences, and encourage them to become a part of it by supporting our work,” said Prof. Michael Zimmermann, IGN’s Chair. Salt iodization is one of the best develop-ment investments in the world: $100 invested in salt iodization programs, can protect up to 10,000 babies, children, and pregnant mothers against iodine deficiency for 1 year. Sustainable salt iodization programs can lead to higher IQ, improved child learning and development, greater national prosperity and less poverty!
To make a tax-deductible donation before 31 December, please visit our website to find out how: http://www.ign.org/Donation
Global Fortification Data Exchange (GFDx) launched in SpanishThe Spanish version of the GFDx was launched earlier in November 2018 at www.FortificacionDatos.org. The new site was showcased at the tri-annual conference of the Society for Latin American Nutrition (SLAN), in Guadalajara, Mexico. Approximately 2,300 individuals from throughout North, Central, and South America and the Caribbean participated in the conference. A live Spanish-language webi-nar entitled “How to use data visualizations to inform food forti-fication and impact nutrition with the GFDx: Global Fortification Data Exchange” will be held on December 5th at 9 am CST. Helena Pachón, Senior Nutrition Scientist at the Food Fortification Initiative (FFI), will give a demonstration of GFDx global data visualizations on topics including fortification legisla-tion, nutrient level standards, food intake and availability, and how to generate custom maps, charts, and tables, and download data for off-line analysis.
To join the webinar on December 5th, click here: https://gainhealth.zoom.us/j/243656593
Can’t make the webinar? No problem. Please visit fortificationdata.org/resources/ after December 5th to see a recording.
The GFDx booth at #SLAN2018
IDD NEWSLETTER NOVEMBER 2018 MEETINGS AND ANNOUNCEMENTS 19
On World Iodine Day, “I” goes missing in the Indian Times
In India, our partners at Tata Salt cap-tured the attention of the media and the nation with their #MissingI cam-paign. Taking the letter ‘I’ out of nati-onal headlines served to create awa-reness of the importance of iodine in the diet for Global Iodine Deficiency Disorders Prevention Day on October 21st. It was then unveiled that the #MissingI is Iodine, and consumers were asked to check whether the mis-sing ‘I’ is missing from their body too.
The campaign had a broad reach and impact. The letter ‘I’ went missing from the online portal of Times of India, and from headlines on Republic, a popular news channel, as well as tweets by major social media influencers such as cricket commenter and journalist Harsha Bhogle, and cricketer Gautam Gambhir. On Twitter, the campaign trended for about 17 hours, garnered about 20,000 conversations, and made tens of millions of impressions. IGN’s Regional Coordinator for South Asia, Chandrakant S Pandav said, “A pinch of iodized salt can give us freedom from preventable brain damage as we continue on our journey to become a healthy nation. Universal salt iodization, WHO’s preferred strategy for the elimination of IDD, results in saving 1.5 billion IQ points in children globally every year.”
IGN advocates for iodine health in the UK
Following the recent news that the UK will add folic acid to flour to prevent birth defects, IGN sent this urgent letter to the UK government via The Guardian, urging them to add iodine to salt.
“With the happy news of the impending royal birth (Harry and Meghan expecting baby in the spring, 16 October) and finally the decision to fortify flour with folate 27 years after the evidence in favour of this (All UK flour to be given folic acid additive, 15 October), surely now is the time for the government to act on its own recent evidence for the need to support the compulsory fortification of salt or bread with iodine. Iodine deficiency in pregnancy is the commo-nest treatable cause of low IQ in the world. Recent figures supplied this year by the UK National Diet and Nutrition Survey state that, in 2015-16, alt-hough iodine levels in the UK population were satisfactory, they did not meet the criterion for iodine sufficiency in pregnant and lactating women.
UK females of reproductive age are unlikely to be iodine-sufficient in pregnancy. This could to lead to a very significant drop in IQ measured in children before the age of nine. The UK is one of only 20 countries in the world that does not have a com-pulsory iodisation of a food ingredient, for example iodised salt or addition of iodised salt to bread. The royal trip to the antipodes includes Fiji, where there is iodised salt, and Australia, where there is iodine in the bread. Both these strategies ensure adequate iodine nutrition in pregnancy, unlike the situation in the UK. We urge government action before another 27 years have elapsed.
Prof John Lazarus Cardiff University; chair, UK Iodine GroupDr Sarah Bath University of SurreyDr Emilie Combet University of GlasgowProf Kate Jolly University of BirminghamJanis Hickey British Thyroid FoundationMike Marsh Kings College Hospital, LondonProf Margaret Rayman University of SurreyDr Malcolm Prentice Croydon NHS TrustDr Alex Stewart Public Health England (retd)Dr Peter Taylor Cardiff UniversityDr Mark Vanderpump Past president, British Thyroid Association”
In memory of Ma Tai
Professor Ma Tai, a pioneer and leader in the fight against IDD in China, East Asia, and worldwide, a foun-ding Board member and long-time Regional Coordinator of the Iodine Global Network, passed away on November 2, 2018 in Tianjin at the age of 97. Born in 1921, Professor Ma graduated from the School of Medicine, Nanjing Central University. In 1953 he was appointed director of the Pathophysiology Department, Tianjin Medical College. Later he became director of the Endemic Diseases Department, Tianjin Institute of Endocrinology, a role from which he retired in 1990. Professor Ma was the first Regional Coordinator for China and the Far East, and he held the role for more than 10 years. In 1998, Professor Ma received IGN’s (then ICCIDD) Distinguished Achievement Award. At the cere-mony in Beijing, Dr. Ma made the following summarizing remark: "Although I have pursued a rough and rugged path all these years, I have the comfort of seeing that the sad picture of a new endemic cretin can no lon-ger be found among the one-fifth of the world's population that lives here in China; although retired, I will not be content to be only in the audience, and hope I can still contribute to the goal of global elimination of IDD with my own hands."
20 IDD NEWSLETTER NOVEMBER 2018 ABSTRACTS
Des
ign:
ww
w.im
holz
desi
gn.c
h
Prin
t: S
pält
i D
ruck
AG
CH
–875
0 G
laru
s
T H E I D D N E W S L E T T E R is published quarterly by the Iodine Global Network and distributed free of charge in bulk by international agencies and by indi-vidual mailing. The Newsletter is also distributed to email subscribers and appears on the Iodine Global Network’s website (www.ign.org). The Newsletter welcomes comments, new information, and relevant articles on all aspects of iodine nutrition, as well as human interest stories on IDD elimination in countries.
For further details about the IDD Newsletter, please contact: Michael B. Zimmermann, M.D., the editor of the Newsletter, at the Human Nutrition Laboratory, Swiss Federal Institute of Technology Zürich, [email protected].
ABSTRACTS
The Iodine Global Network gratefully acknowledges the support of Kiwanis Children's Fund, Indianapolis, USA, and the Swiss Federal Institute of Technology Zürich for the IDD Newsletter.
© Copyright 2018 by the Iodine Global Network
Maternal iodine intake in pregnancy and child-hood neurodevelopment at 18 monthsBetween 2011 and 2015, a prospective cohort study in Australia examined the relationship between maternal iodine intake in pregnancy and childhood neurodevelop-ment, assessed using Bayley Scales of Infant and Toddler Development (Bayley-III) in 699 children at 18 months. Maternal iodine intake and urinary iodine concentration (UIC) were assessed at study entry (<20 weeks' gestation) and at 28 weeks. Maternal iodine intake in the lowest (< 220 µg/day) or highest (≥391 µg/day) quartiles was associated with lower cognitive, language and motor scores [mean difference (95% CI) ranged from 2.4 (0.01, 4.8) to 7.0 (2.8, 11.1) points lower] and a higher odds [Odds Ratio (95% CI) ranged from 2.7 (1.3, 5.6) to 2.8 (1.3, 5.7)] of cognitive developmental delay (Bayley score < 85), compared with mothers with an iodine intake in the middle quartiles. There was no association between UIC in pregnancy and Bayley-III outcomes regardless of whether UIC and the outcomes were analyzed as continuous or category variables. Both low and high iodine intakes in pregnancy were associated with poorer childhood neurodevelopment in this iodine sufficient population.Zhou SJ et al. Am J Epidemiol. 2018 Nov 19. doi: 10.1093/aje/kwy225. [Epub ahead of print]
Poverty and immigration as a barrier to iodine intake and maternal adherence to iodine supple-mentationA cross-sectional survey was conducted among immi-grant and Italian women living in poverty with limited access to the Italian National Health System to evaluate their consumption of iodized salt, iodine-rich foods, and maternal micronutrient supplements. 3483 women answered the ad hoc questionnaire between January 2017 and February 2018. The consumption of iodized salt was very low, and even lower among immigrant women. Determinants of iodized salt consumption were the peri-od spent in Italy for immigrant women and living in a family-type setting, parity and, particularly, the degree of education for Italian women. 17.5% of immigrant women and 8.6% of Italian women reported thyroid disease. 521 women (75.4% were immigrants) were pregnant or bre-astfeeding. The majority (57.3%) had no specific maternal supplementation. In conclusion, both Italian and immi-grating women with a low income or without access to the public health system have a poor adherence both to the salt iodization policy and to folic acid and iodine sup-plements in preconception and pregnancy. Magri F et al. J Endocrinol Invest. 2018 Aug 21. doi: 10.1007/s40618-018-0938-5. [Epub ahead of print]
Neonatal thyrotropin (TSH) screening as a tool for monitoring iodine nutrition in ArmeniaNeonatal thyrotropin (TSH) is influenced not only by the infant's own thyroid function, but also by maternal thyroid status, and can provide a general index of thyroid health in the community. In 2012, Armenia implemented
a program of universal neonatal hypothyroidism screening using serum TSH. The authors analyzed national scree-ning data to determine the frequency of neonatal TSH levels higher than the cut point of 5 mIU/L, indicative of sufficient iodine nutrition status. A total of 127,177 records from 2012–2016 were included. The geographic distribution of neonatal TSH records was reflective of the population of Armenia; the national percentage of records over 5 mIU/L ranged from 2.88% in 2012 to 1.71% in 2016. Minimal regional variation was noted, from a 2012–2016 cumulative high of 2.93% of records over 5 mIU/L in Shirak province to a low of 0.95% in the Vayots Dzor province. These results show no evidence of iodine deficiency and suggest that neonatal TSH may be a useful tool for monitoring iodine nutrition in Armenia.Hutchings N et al. Eur J Clin Nutr. 2018 Aug 31. doi: 10.1038/s41430-018-0298-4. [Epub ahead of print]
Severe iodine deficiency from dietary restriction and subsequent iodine excess from seaweed snack overuse in an adolescent with disordered eatingIndividuals with disordered eating commonly exclude salt and animal products from their diets, which may predispose them to iodine deficiency even without significant weight loss. Overconsumption of dietary supplements and "natural" foods are also commonly observed among eating disorder patients. This report describes an adolescent female with disordered eating presenting with growth and pubertal delay, found to have severe iodine deficiency (UIC=18 µg/L) and abnormal thyroid function resulting from strict avoidance of salt and animal products despite adequate caloric intake. To avoid having to start eating animal products, she began consuming excessive quantities of seaweed supplements to increase her iodine intake resulting in excessive iodine levels (urine iodine of >1,500 mcg/L) and worsening of thyroid function. When her parents began supervising her nutritional intake, her abnormal iodine levels, abnormal thyroid function tests, and hypogonadotropic hypogona-dism all resolved. This is the first report of both iodine deficiency and iodine excess developing from disordered eating behavior.Kumar MM. Int J Eat Disord. 2018 Sep 6. doi: 10.1002/eat.22940. [Epub ahead of print]
Data on spot-kits versus titration method for iodine determination in salt: performance and validityThe aim of this study was to compare the iodine concen-tration measured using two brands of commercial spot-kits against a titration method (using sodium thiosulfate in the presence of Lugol‐s reagent). 437 salt samples, including 20 commercial brands, were collected throug-hout Iran. A titration measurement was carried out in two laboratories using standard samples. There was no significant difference in the results between the two spot-kit brands (ICC = 0.797). The kits’ sensitivity to detect negative samples was high (more than 0.9), but increa-
sing the iodine concentration up to 15 ppm decreased their sensitivity. These findings indicate that the titration method is necessary for quantitative purposes, especially for concentrations higher than 30 ppm. However, spot-kits are suitable for qualitative and semi-quantitative measurements.Shamsollahi HR et al. Data Brief. 2018 Oct 4;21:92-96. doi: 10.1016/j.dib.2018.10.001. eCollection 2018 Dec.
Ocean acidification increases iodine accumu-lation in kelp-based coastal food websKelp is the main iodine accumulator in the ocean, and its growth and photosynthesis are likely to benefit from elevated seawater CO
2 levels due to ocean acidification.
Any change in its iodine metabolism caused by climate change may have important consequences for the global cycle of iodine, including iodine levels of coastal food webs, which underpin the nutrition of millions. Based on a short-term laboratory experiment and long-term in situ mesocosm experiment, this study found that elevated pCO
2 enhanced the growth and increased iodine accu-
mulation not only in the model kelp Saccharina japonica, but also in several other edible and ecologically significant seaweeds. Transcriptomic and proteomic analysis of S. japonica revealed that most vanadium-dependent halo-peroxidase genes involved in iodine efflux during oxi-dative stress are down-regulated under increasing pCO
2,
suggesting that ocean acidification alleviates oxidative stress in kelp, which might contribute to their enhanced growth. When consumed by marine snails (Haliotis dis-cus), elevated iodine concentrations in S. japonica caused increased iodine accumulation in the snail, accompanied by reduced synthesis of thyroid hormones. These results suggest that iodine levels in kelp-based coastal food webs are likely to increase as a result of ocean acidification, with potential impacts on the iodine cycle in coastal ecosystems.Xu D et al. Glob Chang Biol. 2018 Oct 8. doi: 10.1111/gcb.14467. [Epub ahead of print]
Knowledge and practice of iodized salt utilization among reproductive women in Addis Ababa CityA cross-sectional study was carried out on 549 househol-ds in a randomly selected district of Addis Ababa. Data were collected by a face-to-face interview and household salt was tested for iodine. Among the interviewed women, 78% (95% CI 74.9, 81.2) had a good know-ledge of iodized salt, and 76.3% (95% CI 72.7, 79.8) had iodized salt. Monthly household income (AOR = 2.97; 95% CI 1.20, 7.37) was associated with knowledge of iodized salt. Educational status (AOR = 2.45; 95% CI 2.10, 6.43) was significantly associated with the pre-sence of iodized salt. This study indicates that improving women’s education would be a highly recommended strategy for addressing iodine deficiency as a public health problem.Bazezew MM et al. BMC Res Notes. 2018 Oct 16;11(1):734. doi: 10.1186/s13104-018-3847-y