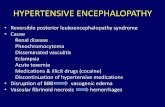
Hypertensive Encephalopathy
-
Upload
yehezkieldward -
Category
Documents
-
view
220 -
download
1
description
Transcript of Hypertensive Encephalopathy
-
4/27/2015 HypertensiveEncephalopathy
http://emedicine.medscape.com/article/166129overview#a0104 1/3
HypertensiveEncephalopathyAuthor:IrawanSusanto,MD,FACPChiefEditor:MichaelRPinsky,MD,CM,Drhc,FCCP,MCCMmore...
Updated:Apr14,2015
BackgroundThetermhypertensiveencephalopathywasintroducedin1928todescribetheencephalopathicfindingsassociatedwiththeacceleratedmalignantphaseofhypertension.Thetermsacceleratedandmalignantwereusedtodescribetheretinalfindingsassociatedwithhypertension,asfollows:
Acceleratedhypertensionisassociatedwithgroup3KeithWagenerBarkerretinopathy,whichischaracterizedbyretinalhemorrhagesandexudatesonfunduscopicexaminationMalignanthypertensionisassociatedwithgroup4KeithWagenerBarkerretinopathy,whichischaracterizedbythepresenceofpapilledema,heraldingneurologicimpairmentfromanelevatedintracranialpressure(ICP)
Withadequatecontrolofhypertension,lessthan1%ofpatientsexperienceahypertensivecrisis.Ahypertensivecrisisisclassifiedaseitherahypertensiveemergencyorahypertensiveurgency,[1]asfollows:
Acuteorongoingvitaltargetorgandamage(eg,damagetothebrain,kidney,orheart)inthesettingofseverehypertensionisconsideredahypertensiveemergencyapromptreductioninbloodpressureisrequiredwithinminutesorhoursTheabsenceoftargetorgandamageinthepresenceofasevereelevationinbloodpressure(withdiastolicbloodpressurefrequentlyexceeding120mmHg)isconsideredahypertensiveurgencyareductioninbloodpressureisrequiredwithin2448hours
Acontinuumexistsbetweentheclinicalsyndromesofhypertensiveurgencyandemergencyhence,thedistinctionbetweenthe2syndromesmaynotalwaysbeclearandpreciseinpractice.[2]
Hypertensiveencephalopathyreferstothetransientmigratoryneurologicsymptomsthatareassociatedwiththemalignanthypertensivestateinahypertensiveemergency.Theclinicalsymptomsareusuallyreversiblewithpromptinitiationoftherapy.Intheevaluationofanencephalopathicpatient,itisvitaltoexcludesystemicdisordersandvariouscerebrovasculareventsthatmaypresentwithasimilarconstellationofclinicalfindings.
PathophysiologyTheclinicalmanifestationsofhypertensiveencephalopathyareduetoincreasedcerebralperfusionfromthelossofbloodbrainbarrierintegrity,whichresultsinexudationoffluidintothebrain.Innormotensiveindividuals,anincreaseinsystemicbloodpressureoveracertainrange(ie,60125mmHg)inducescerebralarteriolarvasoconstriction,therebypreservingaconstantcerebralbloodflow(CBF)andanintactbloodbrainbarrier.
Inchronicallyhypertensiveindividuals,thecerebralautoregulatoryrangeisgraduallyshiftedtohigherpressuresasanadaptationtothechronicelevationofsystemicbloodpressure.[3]Thisadaptiveresponseisoverwhelmedduringahypertensiveemergency,inwhichtheacuteriseinsystemicbloodpressureexceedstheindividualscerebralautoregulatoryrange,resultinginhydrostaticleakageacrossthecapillarieswithinthecentralnervoussystem(CNS).BrainMRIscanshaveshownapatternoftypicallyposterior(occipitalgreaterthanfrontal)brainedemathatisreversible.Thisusuallyistermedreversibleposteriorleukoencephalopathyorposteriorreversibleencephalopathysyndrome(PRES).[4]
Withpersistentelevationofthesystemicbloodpressure,arteriolardamageandnecrosisoccur.Theprogressionofvascularpathologyleadstogeneralizedvasodilatation,cerebraledema,andpapilledema,whichareclinicallymanifestedasneurologicdeficitsandalteredmentationinhypertensiveencephalopathy.
EtiologyThemostcommoncauseofhypertensiveencephalopathyisabruptbloodpressureelevationinachronicallyhypertensivepatient.Otherconditionsthatcanpredisposeapatienttoelevatedbloodpressureandcausethesameclinicalsituationincludethefollowing:
ChronicrenalparenchymaldiseaseAcuteglomerulonephritisRenovascularhypertensionWithdrawalfromhypertensiveagents(eg,clonidine)Encephalitis,meningitisPheochromocytoma,reninsecretingtumorsSympathomimeticagents(eg,cocaine,amphetamines,phencyclidine[PCP],andlysergicaciddiethylamide[LSD])EclampsiaandpreeclampsiaHeadtrauma,cerebralinfarctionCollagenvasculardiseaseAutonomichyperactivityVasculitisIngestionoftyraminecontainingfoodsortricyclicantidepressantsincombinationwithmonoamineoxidaseinhibitors(MAOIs)
EpidemiologyandPrognosis
yehezkielHighlight
yehezkielHighlight
yehezkielHighlight
yehezkielHighlight
-
4/27/2015 HypertensiveEncephalopathy
http://emedicine.medscape.com/article/166129overview#a0104 2/3
Ofthe60millionAmericanswithhypertension,lessthan1%developahypertensiveemergency.Themorbidityandmortalityassociatedwithhypertensiveencephalopathyarerelatedtothedegreeoftargetorgandamage.Withouttreatment,the6monthmortalityforhypertensiveemergenciesis50%,andthe1yearmortalityapproaches90%.
Hypertensiveencephalopathymostlyoccursinmiddleagedindividualswhohavealongstandinghistoryofhypertension.Hypertensioningeneralismoreprevalentinmenthaninwomen.Thefrequencyofhypertensiveencephalopathyinvariousethnicgroupscorrespondstothefrequencyofhypertensioninthegeneralpopulation.Hypertensionismoreprevalentinblackpeople,exceedingthefrequencyinotherethnicminoritygroups.Theincidenceofhypertensiveencephalopathyislowestinwhitepeople.
PatientEducationReferpatientstoadietitiantoreducetheriskofvascularandhypertensivedisease.Encouragelifestylemodifications,includingsmokingcessation,increasingexercise,moderationofalcohol,andavoidanceoftobacco.
Educatepatientsaboutmedicationadherenceandcompliance,andstronglyemphasizetheneedformedicalcompliance.Explaintheeffectsofuncontrolledhypertension,includingthecomplicationsofpersistenthypertension.Informpatientsaboutsignsofacutetargetorgandamage,includingvisualchanges,persistentheadaches,andneurologicalchanges.
ContributorInformationandDisclosuresAuthorIrawanSusanto,MD,FACPClinicalProfessorofMedicine,DirectorofPulmonaryConsultationandProcedures,DivisionsofInterventionalPulmonologyandCriticalCare,UniversityofCalifornia,LosAngeles,DavidGeffenSchoolofMedicine
IrawanSusanto,MD,FACPisamemberofthefollowingmedicalsocieties:AmericanCollegeofPhysiciansAmericanSocietyofInternalMedicine
Disclosure:Nothingtodisclose.
Coauthor(s)NajiaHuda,MDAssistantProfessor,WayneStateUniversitySchoolofMedicineDirectorofMICU,DivisionofPulmonaryandCriticalCare,DetroitReceivingHospital
NajiaHuda,MDisamemberofthefollowingmedicalsocieties:AmericanCollegeofChestPhysicians,AmericanThoracicSociety,andSocietyofCriticalCareMedicine
Disclosure:Nothingtodisclose.
ChiefEditorMichaelRPinsky,MD,CM,Drhc,FCCP,MCCMProfessorofCriticalCareMedicine,Bioengineering,CardiovascularDisease,ClinicalandTranslationalScienceandAnesthesiology,ViceChairofAcademicAffairs,DepartmentofCriticalCareMedicine,UniversityofPittsburghMedicalCenter,UniversityofPittsburghSchoolofMedicine
MichaelRPinsky,MD,CM,Drhc,FCCP,MCCMisamemberofthefollowingmedicalsocieties:AmericanCollegeofChestPhysicians,AmericanCollegeofCriticalCareMedicine,AmericanHeartAssociation,AmericanThoracicSociety,AssociationofUniversityAnesthetists,EuropeanSocietyofIntensiveCareMedicine,ShockSociety,andSocietyofCriticalCareMedicine
Disclosure:LiDCOLtdHonorariaConsultingiNTELOMEDIntellectualpropertyrightsBoardmembershipEdwardsLifesciencesHonorariaConsultingMasimo,IncHonorariaBoardmembership
AdditionalContributorsRyanCChang,MDConsultingStaff,DepartmentofInternalMedicine,DivisionsofPulmonaryandCriticalCare,KaiserPermanenteSanFrancisco
RyanCChang,MDisamemberofthefollowingmedicalsocieties:AmericanCollegeofChestPhysiciansandAmericanThoracicSociety
Disclosure:Nothingtodisclose.
OlehWasylHnatiuk,MDProgramDirector,NationalCapitalConsortium,PulmonaryandCriticalCare,WalterReedArmyMedicalCenterAssociateProfessor,DepartmentofMedicine,UniformedServicesUniversityofHealthSciences
OlehWasylHnatiuk,MDisamemberofthefollowingmedicalsocieties:AmericanCollegeofChestPhysicians,AmericanCollegeofPhysicians,andAmericanThoracicSociety
Disclosure:Nothingtodisclose.
FranciscoTalavera,PharmD,PhDAdjunctAssistantProfessor,UniversityofNebraskaMedicalCenterCollegeofPharmacyEditorinChief,MedscapeDrugReference
Disclosure:MedscapeReferenceSalaryEmployment
References
1. AggarwalM.Hypertensivecrisis:hypertensiveemergenciesandurgencies.CardiolClin.200624:13546.[Medline].
2. BalesA.Hypertensivecrisis.Howtotellifit'sanemergencyoranurgency.PostgradMed.May11999105(5):11926,130.[Medline].
3. ImminkRV,vandenBornBJ,vanMontfransGA,KoopmansRP,KaremakerJM,vanLieshoutJJ.Impairedcerebralautoregulationinpatientswithmalignanthypertension.Circulation.Oct12
-
4/27/2015 HypertensiveEncephalopathy
http://emedicine.medscape.com/article/166129overview#a0104 3/3
MedscapeReference2011WebMD,LLC
2004110(15):22415.[Medline].
4. SchwartzRB,JonesKM,KalinaP,etal.Hypertensiveencephalopathy:findingsonCT,MRimaging,andSPECTimagingin14cases.AJRAmJRoentgenol.Aug1992159(2):37983.[Medline].
5. GrossmanE,MesserliFH.Highbloodpressure.Asideeffectofdrugs,poisons,andfood.ArchInternMed.Mar131995155(5):45060.[Medline].
6. FrohlichE.D.Targetorganinvolvementinhypertension:arealisticpromiseofpreventionandreversal.MedClinNorthAm.200488:19.[Medline].
7. AmraouiF,vanMontfransGA,vandenBornBJ.Valueofretinalexaminationinhypertensiveencephalopathy.JHumHypertens.Oct292009[Medline].
8. AhmedME,WalkerJM,BeeversDG,BeeversM.Lackofdifferencebetweenmalignantandacceleratedhypertension.BrMedJ(ClinResEd).Jan251986292(6515):2357.[Medline].[FullText].
9. LambertCR,HillJA,NicholsWW,FeldmanRL,PepineCJ.Coronaryandsystemichemodynamiceffectsofnicardipine.AmJCardiol.Mar1198555(6):6526.[Medline].
10. GavrasH,BrunnerHB,VaughanED,LaraghJH.Angiotensinsodiuminteractioninbloodpressuremaintenanceofrenalhypertensiveandnormotensiverats.Science.Jun291973180(4093):136971.[Medline].