Horn of Africafinalaugust06 -...
Transcript of Horn of Africafinalaugust06 -...
Health Action in Crisis Inter-regional Hub, Nairobi, Kenya P.O.BOX 45 335. Tel. +254 735339037FAX: +254 202 719 141 Email:[email protected];[email protected] 1
Heavy precipitations in late July havedeepened the humanitarian andlivelihoods crisis of the communities
already affected by the drought. Flash andriver floods have impacted upon pastoralistsand agro-pastoralists just barely recoveringfrom economic losses following consecutiveperiods of drought, causing immediate loss oflife and suffering, and aggravating theirstructural vulnerabilities.
The floods hit in varying magnitude Kenya,Somalia and Ethiopia. The toll is heavy:thousands displaced and hundreds killed(about 200,000a and 650, respectively, inEthiopia alone), destruction of housing androad infrastructure. The floods seriouslyundermined the hopes for economic recoverythat had come with the long-awaited rains.Large areas of productive land and numbers ofvital livestock were lost.
Both drought and floods disrupt livingconditions with the lack of potable water,economic distress and altogether unhygienicand unhealthy environments, that favour thedevelopment and spread of communicablediseases. The same countries that hadsuffered from the effects of drought are nowhaving to deal with outbreaks of AcuteWatery Diarrhoea in Ethiopia and measles inKenya and Somalia.
WHO, Health Action in Crisiswebsite on the HoAhttp://www.who.int/hac/crises/international/hoafrica/en/index.html
UNDP website on drought:www.Droughtnet.org
Health (http://www.droughtnet.org/health.htm)
Inter-Agency Working Groups
Home: http://www.humanitarianinfo.org/iawg-nairobi/index.asp
Thematic groups: http://www.humanitarianinfo.org/iawg-nairobi/thematic.asp
Health ReviewAugust 2006
Inter-AgencyStandingCommittee(IASC) HealthCluster
To rapidly respond to urgent needs inaffected areas it was necessary to build therequired human resources and logisticalcapacities in great demand.
Structural vulnerabilities in countries of theHorn of Africa must be addressed with andsupport to community based initiatives tomaintain coping mechanisms and forsustained livelihood development, of whichincreased access to basic social and healthservices is a key element.
Through CERF 1 and CERF 2, UN agenciessupported their respective Ministries ofHealth (MoH) and National GovernmentalOrganizations (NGOs) to provide lifesavinginterventions and to fill gaps in basic socialand health services.
CERF recipients’ main concern today is howto sustain lifesaving activities in the contextof an under- funded HoA ConsolidatedAppeal Process (CAP) 2006.
Additional funds must be mobilizedurgently to face new and additional threats,to develop comprehensive preparednessand contingency plans, to build long-termresilience capacity, and to sustain theactivities launched with CERF grants.
Links
Highlights
Horn of AfricaDrought Crisis
Editorial
Acute watery diarrheoa outbreakresponse in Ethiopia...................P.4
Health threats and vulnerabilities indrought and floods situations....P.2
Kala-azar outbreak in Wajir district,Kenya........................................... P.7
Flood interventions inEthiopia........................................P.6
Horn of Africa (HoA) synchronisepolio immuniztion campaigns.... P.9
Measles outbreak in Kenya andSomalia........................................ P.8
CERF Achievements in HoA bycountry........................................P.10
The second issue of this bulletin onlycontains information originating from theWorld Health Organization. Unfortunately, itstill does not contain any input from otherpartners. We are therefore seizing thisopportunity to request all partners in theHealth and the Nutrition clusters to send usinformation on their activities and viewsrelated to this crisis. Also kindly share withus the names and coordinates of yourorganizations’ focal points in the Horn ofAfrica countries. In future, we intendthat the Health Review speak with one voicefor the humanitarian community in the Horn.Please send comments [email protected] for inclusion inthe next issue.
DISCLAIMER
Health Action in Crisis Inter-regional Hub, Nairobi, Kenya P.O.BOX 45 335. Tel. +254 735339037FAX: +254 202 719 141 Email:[email protected];[email protected] 2
Drought versus Floods Health threats and vulnerabilities
Health threatscommon todrought and floodaffectedpopulations
Infectious diseases: malaria (amajor threat after floods but alsopresent around water point indrought situation), measles, acutediarrhoeas, acute respiratoryinfections (ARI), meningococcalmeningitis, tuberculosis,trachoma, leishmaniasis,poliomyelitis, avian flu,malnutrition, maternal risk andHIV/AIDS.
Vulnerabilitiescommon todrought and floodaffectedpopulations
Floods following long periods ofdrought increase the vulnerability
of populations already weakened.
The estimated 8.5 million hit bydrought and those recentlyaffected by floods have similarcharacteristics that increase theirvulnerability to natural disastersand reduce their access to basichealth and social services.
They are mobile populations dueto the following reasons:
Economic: drought and floodaffected areas are the poorest andthe least developed in the region.Coping and caring mechanism ofpastoralists and migrating farmersdepend heavily on livestock andlocal markets.
Insecure access to vital needssuch as water, basic health careservices, aggravated by a deeperand wider insecurity: in at leastthree of the countries , armedviolence is an important cause of
Keycharacterics ofpopulations
forced displacement: InternallyDisplaced Populations (IDPs)and Refugees.
Those who cannot move areamong the rural and the urbanpoor with urgent need ofassistance with food aid andpotable water.
The working environment inthese areas is harsh and is thusdifficult to maintain healthworkers, teachers in theirpositions. As a result access toprimary health care services isreduced as health centres areclosed in the absence of healthstaff.
Different pastoralists
Transhumant, who migrateregularly between two grazingareas along well-definedroutes every year
Pastoralists, who migratealong conventional routes, butcan move in differentdirections every year andwithin a given year(“pastoralists pursuelivelihoods dominated bylivestock rearing”(1));
Semi-nomads, who practiceother activities while retainingmigration and livestockherding as their basiceconomic activity (“Agro-pastoralist pursue a mixedlivelihood of both livestockrearing and crop farming” (1))
(1):Stephen Devereux.2006.
Vulnerable Livelihoods inSomali Region, Ethiopia, IDS Research Report 57.
Health Action in Crisis Inter-regional Hub, Nairobi, Kenya P.O.BOX 45 335. Tel. +254 735339037FAX: +254 202 719 141 Email:[email protected];[email protected] 3
Health Response to Drought
Drought versus FloodsHealth threats and vulnerabilities (Cont.P2)
Highmorbidityandmortality
-Maternal & Neonatal risks-Chronicdiseases-Current diseases
Lack of cleanwaterStagnatedwater
- ARI- Measles- Malnutrition
Environment
Socio-economic
FLOOD
Loss of assetDisplacementLoss of shelterlack of access tofood
- Health- Essentialservices
Health Response to FloodsWater bornediseases:- Cholera/Diarrhoeas- Typhoid,- Malaria- Epizoonozis
Infrastruc-ture
Health Response
1.Epid.Surveillance,Control Guidelines,
Training, Supplies and Staff
2.Nut. Surveillance,Guidelines for Nut.Supplementation&Rehabilitation,
Training, Supplies and Staff
3. Stronger programmesfor EPI, IMCI/MCH,
ED, HealthInformation,
Referral
4. Special plans, policies &procedures:outreach, etc.
OtherIllness
Loss ofcaring
capacityStressmigration,
other copingstrategies
Loss of buyingpower
DROUGHT
Loss ofLivestock
Crop Failure
Reducedfood
intake
DiarrhoeasCholera
Typhoid FeverSkin diseases
Eye diseases, etc.
WATERSHORTAGE
Under-nutritionAvitaminoses
5.Special budget
- What to do?
Assessment andSurveillanceWater qualityBreeding sitesHealth ServicesPop. movementRisk and outcomes(morbidity/mortality)
- CoordinationWho is doing whatand where?(W3)Cluster and intercluster coordination
- Filling gapsHealth servicesImmunizationWater qualityVector controlOubreak response(Malaria/AWD)Sanitation (propercamp management)
- Building capacityCommunityeducation & StafftrainingSupport Zonal andDHMT team.
The figures (1 & 2)across areapproaches to healthresponse in droughtand flood situations.They show that thesituation is mainlylinked to theshortage of potablewater and economicdistress, for loss oflivestock or othermeans of production,etc.
The erosion of theeconomic power andthe lack of access tobasic services areamong major causesof health problems.
The Health responseis along the four corefunctions of WHO inemergencies:
• Needsassessment andhealth
surveillance andInformation foraction planning
• Health actioncoordination
• Critical gapsfilling
• Capacity building
Figure 1
Figure 2
Health Action in Crisis Inter-regional Hub, Nairobi, Kenya P.O.BOX 45 335. Tel. +254 735339037FAX: +254 202 719 141 Email:[email protected];[email protected] 4
Communicable DiseasesThousands hit by Acute WateryDiarrheoa (AWD) in Ethiopia
Reportedly, the first caseof acute waterydiarrhoea (AWD9 wasregistered on 15 April2006 in Gambella region.Since then cases havespread to 4 other regions(Oromia, SNNPR, Amhara& Tigray ( figures 3 to 5)and Addis Ababa. As of 4September 16,250 casesand 123 deaths werereported with 30 districts(woredas) affected and aCase Fatality Rate (CFR)of 0.8%. The laboratorytest is still to bepublished by the FederalMinistry of Health(FMOH). A peak wasreached betweenepidemiological week 28and 32. (Figure 3).
Response tothe AWD inEthiopia
Assessmentand monitoring
The Federal Minister ofHealth (FMOH) sent arapid verification &response team toaffected areas andstrengthened theIntegrated DiseaseSurveillance System(IDSR). WHO providedtechnical assistance andparticipated in thevarious AWDassessment missions.
WHO also providedfinancial support forassessment teams.
Fig.3: Trend showing outbreak of AWD, National.
15 April 2006 - 27 August 2006
Fig.4: Trend showing outbreak of AWD, SNNPR region.
18 July 2006 - 23 August 2006
Health Action in Crisis Inter-regional Hub, Nairobi, Kenya P.O.BOX 45 335. Tel. +254 735339037FAX: +254 202 719 141 Email:[email protected];[email protected] 5
Communicable DiseasesAcute Watery Diarrheoa (AWD)response in Ethiopia
In Eritrea, no major outbreak wasreported in August 2006. The
proportionate morbidity in
populations consulting at health
Communicable DiseasesMajor causes of diseasesin Eritrea and Djibouti
facilities (countrywide by
reporting period June-July 2006)respiratory infections (42%)
shows that diarrhoeas (47%)
and are the major causes ofmorbidity.
In Djibouti, no outbreaks ofcommunicable diseases were
reported in July and August
200. Malnutrition remains aconcern as one of the
immediate and possibly long-
term effects of the drought.It is hoped that ongoingassessments will provide abaseline for planning futureinterventions.
Fig.5: Trend showing outbreak of AWD, Oromie region.
22 June 2006 - 27 August 2006
Response tothe AWD inEthiopia(cont. from P4)
Coordination
The Federal Ministry of Health(FMOH) reactivated zonal anddistrict level epidemicmanagement committees.WHO Emergency andHumanitarian Action (EHA)team provided technicalsupport at the central, regionaland district levels).
WHO worked closely with theFederal Government incoordinating the responsewith the UN system andpartners.
Resourcemobilization
The FMOH sent the resourcesmobilized from differentpartners to the affected areas.WHO facilitated theproduction of a plan of actionsubmitted to donors forfunding. WHO worked closelywith Federal Government, UNsystem and partners tomobilize resources.
Constraints
Access to the affected areas isdifficult, and even moredifficult therein. Transportand communicationinfrastructures are poor andhealth infrastructures are poortoo, lacking staff andequipment. Laboratoryconfirmation took long anddelayed the declaration of theepidemic and the mobilizationof resources. The nationalepidemic preparedness &response committees wereactivated only late in thecrisis.
Health Action in Crisis Inter-regional Hub, Nairobi, Kenya P.O.BOX 45 335. Tel. +254 735339037FAX: +254 202 719 141 Email:[email protected];[email protected] 6
Special ReportFlood interventions in Ethiopia
From mid-July 2006 to 24 August 2006 theDisaster Prevention and PreparednessAgency (DPPA) reported that 8 out of 11regions in the country have been affected.Altogether 517,400 are considered“vulnerable”; 199,900 people have beendeclared affected; 639 people reporteddead and more than 34,000 peopledisplaced.
Health sector response
Assessment and monitoring
The Ethiopian Federal Ministry of Health(FMOH) conducted assessments in all theaffected areas and fed health informationinto DPPA situation reports.WHO provided technical and financialsupport to the assessment teams.
Coordination
The FMOH participated in the DPPACommittee chaired by Deputy PrimeMinister.
WHO worked closely with the Federalgovernment in coordinating with the UNsystem and partners.
Filling gaps
Regional Health Bureaus opened clinics inthe camps hosting the people displaced bythe floods.
The FMOH deployed technical teams forsurge support and pre-positioned essentialdrugs.
WHO provided essential drugs toRegional Health Bureaus (Dire Dawa andOromiya) and supported financially theFMOH teams.
Mobilizing resources
A Joint Government and humanitarian partnersappeal of US$27,099,526 was launched.WHOworked closely with the Federal Government,the UN system and partners in mobilizingresources.
Constraints
• Difficult access to affected areas (todisplaced populations)
• Poor coordination
• Poor sharing of information, discrepancyof information –no single source,
• Poor logistics and road conditionhampered access
• Scarce capacity for programmemanagement at field level
• Instances of inappropriate non-food items
and/or gaps: e.g. shortages of tents
Surge support from WHO
Mobilization of EHA team in WCO, JointAFRO/HQ emergency planning mission forthe floods and technical support fromWHOAFRO Technical team for Cholera andmalaria Control arrived in Ethiopia.
Figure 7
Health Action in Crisis Inter-regional Hub, Nairobi, Kenya P.O.BOX 45 335. Tel. +254 735339037FAX: +254 202 719 141 Email:[email protected];[email protected] 7
Kala-azar
Kala-azar (Visceral Leishmaniasis )is a deadly disease caused byparasitic protozoa Leishmaniadonovani, transmitted to humansby the bite of infected femalesandfly, Phlebotomus argentipes. Itlowers immunity, causes persistantfever, anemia, liver and spleenenlargement, and if left untreated, itkills. The vector thrives in cracksand crevices of mud plasteredhouses, poor housing conditions,heaps of cow dung, in rat burrows,in bushes and vegetations aroundthe houses.
WHO/SEAROhttp://www.searo.who.int/en/Section10/
Section2163.htm
As of 20 August 2006, a total of 53suspected cases (last case admitted on 12th
August) have been reported in Wajir districthospital with 27 of them confirmed. There arecurrently 37 admitted kalazar patients inWajir District Hospital undergoing treatmentafter 7 patients were discharged aftercompleting their treatment schedule.
The index case was identified on 7 June 2006though the majority of the cases werereported in mid-July.
Cumulatively six deaths have so far beenreported with a case fatality rate (CFR) of11% (Figure 8). The average age of thesuspected cases is 3 years (range 6 monthsto 13 years).
Seventy percent of the cases are males. Over90% of the cases are from Isiolo district andthe remainder from Wajir.
The other related co-morbidities include:pneumonia, bleeding tendencies, anaemiaand malaria in the background of severemalnutrition.
The Isiolo hospital has enough Pentostumfor the management of these cases. There ishowever a need for additional supplies ofanti-malarial, haematinics, IV fluids andantibiotics.
Communicable DiseasesKenya: Kala-azar outbreak in Wajir andIsiolo districts
Pentostam
Pentostam (Sodium stibogluconate) isused specifically in the treatment of aprotazoal infection called leishmaniasis.It is administered by intramuscular orintravenous injection only.
Impavido
Impavido (miltefosine): Impavido is thefirst oral drug for the treatment ofvisceral and cutaneous leismaniasis.Impavido has been proven to be highlyeffective and less toxic than currenttherapies. Each capsule contains 10 or50mg of Impavido. The recommendeddose is approximately 2.5 mg per kgbodyweight per day, with a maximumdose of 150 mg pr day. Currently,Impavido is available in a 56 capsuleformat containing either 10 0r 50 mg ofImpavido.
Sourcehttp://www.searo.who.int/en/Section10/Section2163.htm
Figure 4 : Kalaazar outbreak in Wajir July- August 2006Figure 8: Kala-Azar outbreak in Wajir
July - August 2006
Health Action in Crisis Inter-regional Hub, Nairobi, Kenya P.O.BOX 45 335. Tel. +254 735339037FAX: +254 202 719 141 Email:[email protected];[email protected] 8
Communicable DiseasesMeasles outbreaks in Kenya and Somalia
Kenya
In the drought affected district ofMoyale, eight measles cases and4 deaths (CFR 50%) have beenreported since 14 July 2006. Twoof the cases are fromneighbouring Ethiopia. The agesrange from 9 months to 25 years.Five of the cases are above 5years of age. All the cases wereimmunized.
In other drought affecteddistricts, preliminary situationassessment received reported atotal of 132 suspected cases with2 deaths (3 and 21year old)inTurkana; In Kajiado, 12 caseswith no deaths and 3 cases inGarissa.
Threats of measles remain inKenya despite massiveimmunization campaignsconducted this year. Thefollowing districts from thedrought affected areas have beenaffected: West Pokot with 130cases and 3 deaths; Meru Northhas reported 116 suspectedcases of measles with 4 deaths(CFR 3%) since July 10 with 15
among them admitted. Nakurudistrict with over 100 suspectedcases reported after the measlescampaign (12 July 2006) with 43cases in August alone. Threedeaths have been reported sinceJuly 12.
Of the suspected cases (in all agegroups) reported in August only36% had been vaccinated.Overall 64% of the suspectedcases are unvaccinated (9-59months: 40% unvaccinated and43% of those over 5years areunvaccinated). This is due todifficulties in accessingpopulations during the campaignbut also because of populationmovements (including cross-border movements). MobileImmunization campaigns areongoing in affected areas.
Somalia
During the first week of August,there were rumours of measlescases associated with diarrhoeaand malnutrition coming in ElWak district of Gedo region. Ateam from Gedo Health
Consortium (GHC) visited thearea, investigated andconfirmed the cases andprovided an immediateresponse. The investigationshowed that those affectedwere mainly nomadicpastoralists who were not in thearea during the measles catch-up campaign.
The GHC team treated a total of45 children suspected ofmeasles. The team alsoidentified 35 moderatelymalnourished and 9malnourished children.
The main challenge in the areais the weak basic health care asthe number of health facilities isinsufficient to deliver essentialhealth care including ExpandedProgramme on Immunization(EPI) and other Mother andChild Health (MCH) services.
Meanwhile, the major causes ofmorbidity for children under-five in June and July 2006 werediarrhoea and malariarespectively 53% and 34%(figure 9 ).
Figure 9: Proportionate morbidity among children under 5 consulting at health facilities in Somalia
June - July 2006
Health Action in Crisis Inter-regional Hub, Nairobi, Kenya P.O.BOX 45 335. Tel. +254 735339037FAX: +254 202 719 141 Email:[email protected];[email protected] 9
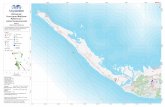
Countries in the Horn of Africa areincreasing their level of planning,coordination, and streamlining their
strategies to cut the corridor of transmissionof the poliovirus. Somalia, Ethiopia andKenya will simultaneously vaccinatemillions of children under five years of agefrom 9-12 September in the largest eversynchronized vaccination campaigns in theHorn of Africa.
In Ethiopia, the polio vaccination campaignwill administer two drops of Oral PolioVaccine (OPV) to 956,886 children, from thetwo regions of Somali and Afar that borderSomalia and parts of Kenya. On Somalia’sside of the border, vaccinators will aim toreach a total of 1.7 million children in anation-wide campaign, with exceptionalconcentration on regions bordering Ethiopiaand Kenya. In northern Kenya, a total of240,000 children will be targeted in fivedistricts bordering Somalia and Ethiopia.The Horn of Africa Technical AdvisoryGroup (TAG), which convened in Ethiopia inAugust 2006, stressed that the polioeradication drive is now at a critical stage,where most countries are strategizingtogether to pull out the best approaches tothe effective deployment of humanresources, mobilization of authorities, local
communities, households, and theparticipation of the international donorcommunity to ensure high quality surveillanceand supplemental immunization activities.Teams on the ground will ensure that eachand every child is vaccinated, by moving fromhouse to house, in cities, towns, and villages,and in hard to reach areas, using alltransportation means.
The polio eradication effort in the Horn alsoinvolves religious and community leaders,women’s groups, youth associations, schools,and governmental and non-governmentalorganizations through an immense structure ofsocial mobilization to prevent the paralysis ofmillions of children.
The complex operating and unstableenvironments, exacerbated by recurrentdrought and floods in Somalia and heavy rainsin Ethiopia, continue to have adverse effectson the implementation of immunizationcampaigns. International and national staffhave difficulties accessing conflict zone areasto regularly supervise staff working at thedistrict level. For Ethiopia, the areas wherechallenges due to insecurity are most acuteare in the Somali and Gambella Regions. This,coupled with the poor health infrastructure,and low routine immunization coverage ratesplace both countries at risk for continued
transmission or spread. In addition, Ethiopia,Somalia and northern Kenya host largepopulations of nomadic pastoralists, whopose challenges in their access forimmunization, as well as necessitating ahighly sensitive surveillance system fortracking the poliovirus.
Depending on the availability of funds, threesynchronized campaigns are planned for thisyear, in September, November and Decemberin the Horn of Africa. Globally, there is afunding gap of US$50 million for 2006, whichmust be filled urgently by October to ensurethe implementation of planned activitiesthrough the end of the year.
Horn of Africa Countries BolsterCampaign Synchronization inDrive to Eradicate Polio
Millions of children along
the borders of Ethiopia,
Kenya and Somalia will be
vaccinated in the largest
ever cross-border
immunization to cut
transmission of the
poliovirus.
Health Action in Crisis Inter-regional Hub, Nairobi, Kenya P.O.BOX 45 335. Tel. +254 735339037FAX: +254 202 719 141 Email:[email protected];[email protected] 10
CIRF AchievementsSomalia
The CERF funding facilitated thereinforcement of WHO’s technical supportto the Ministry of Health in theestablishment of mobile units, theconducting of epidemiological andnutritional surveillance programmes toincrease the coverage of primary heath carefor the vulnerable people affected bydrought in the remote areas of Djibouti.
Accomplishments
An emergency expert was contracted for 3months to strengthen the mobile unitprogram in all the districts: Dikhil, AliSabieh, Tadjourah et Obock. A referencedocument was elaborated and validatedwith the Ministry of Health. Three vehicleswere purchased to allow the extension ofthis programme in districts where there wereno vehicle available or in a poor condition.
A nutrition expert was contracted for aperiod of 2 months to implement the system.Two evaluation missions have taken place: ajoint mission with staff from WHO Genevaand WHO Cairo to evaluate the technicalsupport to the Ministry of Health andNutrition Specialist support from EMRO.
Tools and materials were prepared. Meetingshave taken place with WFP (i.e. choice ofsentinel sites) and stakeholders. A referencedocument was elaborated and validated withthe Ministry of Health
The system is in place in the Djibouti District.Hospitals, Health Centres, health posts,private care units report on a weekly basis.This system is being reinforced in otherdistricts with the purchase of a communicationsystem for the Hospital and medical centresand training sessions for staff. In May 2006,an effective response was put in placefollowing a H5N1 case.
The integrated child sickness care program(PCIME) is in place including parentaleducation on breastfeeding provided in 19health centres.
Training on technical aspects of mobile unitsactivities, nutritional surveillance and earlywarning systems started in the districts of AliSabieh, Dikhil, Arta, Tadjourah and Obock.
Fifty-seven health staff were trained in EarlyWarning System for epidemic prone diseasesand nutrition: Five Hospital Directors , Four
CERF AchievementsDjibouti
mobile clinics doctors, nurses of twenty-twohealth centres, nurses and midwifes of fiveDistrict Hospitals
Twenty-five people in charge of the mobileclinics were trained in the management andplanning of the relevant activities.
Challenges andway forward
There is a need to guarantee thecontinuation of health services in the remoteareas affected permanently by drought
In addition communication systems shouldbe improved (i.e. radio communicationsystem needed) for better communicationamong health centres, sentinel sites, andmedical and hospitals centres in each of thedistricts.
Funds must be secured to reinforce staffknowledge through continuing education,vocational training and close supervision.
Health Action in Crisis Inter-regional Hub, Nairobi, Kenya P.O.BOX 45 335. Tel. +254 735339037FAX: +254 202 719 141 Email:[email protected];[email protected] 11
With CERF funding WHO carried-out a strategy based onmanaging information,
convening consensus, joining forces andenhancing cooperation and coordination ofall humanitarian actors and filling criticalgaps. The activities were initiated with CERF1 funding and continued with CERF 2 grants.
The objective of this response strategy wasto reduce avoidable mortality and sufferingdue to life threatening health conditionsresulting from food insecurity, and tostrengthen the capacity of the system todeliver required services to these affectedpopulations.
Accomplishments
The availability of CERF funding hasassisted in providing timely information tothe health cluster. The methodology usedincluded rapid assessments, compilation ofhealth profiles and a household survey. Inaddition, the routine integrated surveillanceand response (IDSR) system wasstrengthened with the recruitment of anational officer and data manager.
An International EHA focal point wasappointed. Major successes included: Strengthening of the working relationship
among major health partners especially withthe Ministry of Health, UNICEF, UNFPA andWHO.
Raising the measles vaccination coveragefrom 63.5% to 95% among children between 12to 23 months’ old in Southern Red Sea. Vitamin A supplementation among infants
increased from 9.8% to 95%. Emergency kits were procured for rapid
responses. The kits will be distributed to treat30,000 people for a period of 3 months againstcommon diseases, manage 200 cases ofdiarrhoea including cholera, attend to 100interventions of trauma cases and conduct8,000 deliveries. The kits have been donatedto the Ministry of Health (MOH) with adistribution plan based on rapid assessmentresults.
Adapting guidelines and providing thenecessary training to the Ministry of Healthand health stakeholders to respond to life-threatening needs at district level (informationmanagement, coordination, gapsidentification, case management includingmalnutrition) was one of the main responsestrategies. In addition, monitoring of theseconditions is necessary to measure programsuccess. A total of 63 healthworkers have been trained onIntegrated Management ofChildhood Illnesses ( IMCI).
Challenges
The challenges faced included: Insufficient number of technical
expertise in the ministry of healthand of trained staff
that delayed the implementation rate. Non availability of local expertise to hire
and complement government efforts. Scarcity of supplies on the local market,
making purchase of items very complex.
Way forward
More vigorous resource mobilization isneeded. As a first step, the huge volume ofinformation generated by WHO under CERFmust be synthesized and presented todonors. Mapping the migratory route of the
population. Developing alternative health services in
the form of outreach to reach the affectedgroups. Monitoring the rainfall pattern to decide
on the mobilization of another CERF grant.
CERF AchievementsEritrea
The main causes ofmorbidity andmortality were IMCItargeted diseasesincluding diarrhoea,acute respiratoryinfections andmalnutrition.
Health assessment
team in Eritrea
Health Action in Crisis Inter-regional Hub, Nairobi, Kenya P.O.BOX 45 335. Tel. +254 735339037FAX: +254 202 719 141 Email:[email protected];[email protected] 12
WHO Ethiopia received US$350,000 from CERF grants tostrengthen emergency
preparedness and response capacities ofthe FMOH, Regional Health Offices andWoreda Health Offices, and to improvecommunication and data managementthrough technical support to RegionalHealth Offices, Woreda Health Offices andHealth Institutions.
Accomplishments
The provision of essential drugs wasnecessary due to threats of diseaseoutbreaks considering thesevere shortage of drinking water andreduced immunity due to the high level ofsevere acute malnutrition. Communicable
diseases werethe majorcauses ofmorbidity andmortality inthe districts(woredas)affected bydrought.Theinadequatesupply ofessentialdrugs in allhealthinstitutionscalled forimmediateaction as partof the lifesavinginterventions.Bothinternationaland localprocurementsalleviated thecriticalshortage ofessentialdrugs throughWHO’ssupport.
WHOsupported theFMOH in the
preparation of a response plan to the droughtaffected population. The plan helped ministryand other partners monitor the response andthe identification of gaps.
WHO conducted regular assessments todocument major developments and advisedpartners, The FMOH and health bureaus asappropriate.
Reactivating the woreda rapid response teamsand providing them with the logistics andfinancial support to conduct supportivesupervision was a priority. A total of 36 healthprofessionals from the most affected woredaswere trained on disease surveillance,management of major communicable diseaseand emergency preparedness and response.
On the spot training of the healthprofessionals was organized using theworeda focal persons, who can conduct onthe spot cascade training.
The FMOH with the support of WHO,UNICEF and other partners trained focalpersons from all regions. The focal personsare expected to conduct an assessment andfacilitate the preparation of contingencyplans for 2007.
More than 300 health professionals werereached through this on-the-spot training.
Strengthening surveillance through thetraining of health professionals, provision ofguidelines and reporting formats wasanother major area of concentration of thisproject. Sentinel surveillance sites wereselected and the pattern of majorcommunicable diseases documented.
Challenges and wayforward
Additional resource should be mobilized tosustain life saving activities started with theCERF.
Shortage of human resource at all levels wasthe major constraint in the implementation ofthis project.Strengthening health institutions andopening outreach circuits should beconsidered seriously, together with theintegration of nutrition surveillance andtreatment of severe malnutrition. This willsave unnecessary costs related to theopening of several feeding centres and willreach the community timely at reasonabledistance.
The Regional Health Bureau of SomaliRegion is planning to re-institute the Zonalstructures. There is a plan to start thetraining of Extension Health Workers inSomali region and Borena Zone of OromiyaNational Regional State. Borena Zone is alsopreparing a proposal to strengthen thehealth institutions with additional humanresources.
CERF AchievementsEthiopia
Measles vaccination
campaign
Health Action in Crisis Inter-regional Hub, Nairobi, Kenya P.O.BOX 45 335. Tel. +254 735339037FAX: +254 202 719 141 Email:[email protected];[email protected] 13
Surveillance and response activities in thedrought affected regions. WHO currentlysupports MoH directly on the field to monitorhealth threats and system’s critical capacities.
Coordination meetings were already in placebefore the inception of the project. However,health has now been brought into focus at alllevels. Coordination with health relatedsectors has also strengthened especially atthe district levels.
One of the major interventions was theimmunization of children under five yearsagainst polio and measles in the droughtaffected districts. These activities wereconducted from 29 July to 2 August 2006.
The following New Health Kits were procuredand delivered to the Ministry of Health forepidemic prone and drought affected areas: 9New Emergency Health Kits(NHEK) weredistributed in addition to reproductive healthkits, malaria drugs,13 tons of insecticides forindoor residual spraying (IRS), RapidDiagnostic kits for confirming malaria before
prescription of ACTs, Quinine ampoules fortreatment of severe malaria, 10,000Artemether ampoules for use in severemalaria when quinine is not available and63,000 tablets quinine tablets for severemalaria
The drugs and items were donated to theMinistry of Health by the WHO CountryRepresentative. WHO in collaboration withthe Kenya Red Cross facilitated thedistribution and transportation to districtsand end-users. These drugs supportedprimary health and outreach activities in theaffected districts.
To reactivate the cold chain system WHOhas placed orders for sixty (60) fridges andgas cylinders and other accessories.
WHO in collaboration with the Ministry ofHealth conducted training for healthworkers on management of severemalnutrition in Garissa.
Challenges and wayforward
Forecasts so far are that the situation maynot return to normal in the short to mediumterm.
Coordination of health sector partners wasrather weak and most of the health andnutrition sector meetings focused on eithertherapeutic feeding or foodsupplementation.
There were many actors on the fieldproviding humanitarian assistance and whoneeded technical guidance and support.
Few assessments were carried out inpockets and the overall picture in the areawas not reliable. Similarly there were noassessments conducted on the capacity ofthe health system in the affected region tocope with the situation.
To maintain the gains made so far amechanism must be found for thecontinuation of funding.
CERF AchievementsKenya
The CERF funds enabled WHO to expandits capacity to the affected region byrapidly establishing a sub-office in theregion.
Accomplishments
WHO in conjunction with MOH, UNICEFand UNFPA conducted rapid Fieldassessments in 6 districts namely Moyale,Masarbit, Samburu, Isiolo, Kajiado andTana River. The assessment resultsidentified major gaps in the health deliverysystem.
A Emergency Humanitarian Focal Pointwas transferred to the Kenya WHOCountry office. The World HealthOrganization promptly established a suboffice established in Garissa to provideeffective and readily available technicalsupport.
The arrival of the CERF fundingaccelerated the Integrated Disease
New Emergency
Health Kits (NEHK)
distributed to enblerapid response in
health facilities
Health Action in Crisis Inter-regional Hub, Nairobi, Kenya P.O.BOX 45 335. Tel. +254 735339037FAX: +254 202 719 141 Email:[email protected];[email protected] 14
CONTACT USDjiboutiDr Jihane Farah TawilahWHO [email protected] Raschida SoussiEHA Focal point
EritreaDr Andrew Michael KosiaWHO [email protected] Abdulmumini UsmanEHA Focal [email protected]
EthiopiaDr Olusegun Ayorinde BabaniyiWHO [email protected] Omar Kebbe JaitheEHA Focal [email protected]
KenyaDr Peter ErikiWHO [email protected] ;[email protected] Teprey JamesEHA Focal [email protected]
SomaliaDr Ibrahim BetelmalWHO [email protected] Juan Diaz
EHA Focal [email protected]
Accomplishments
Over 85 Somali health workers were trained(including doctors, nurses, assistant nurses,lab technicians, etc) from health facilities runby international NGOs in Somalia.
A total of 3 trainings already undertakenwith CERF 1 & 2 funds have created a pool(85) of capable response staff. Their servicesto drought affected populations will beexpanded even more when mobile outreachservices begin shortly.
Twenty eight health workers from 9 regionswere trained in communicable diseasecontrol (CDC) response
Twenty-two laboratory /health workers from9 regions were trained basic microscopy(malaria and disease surveillance)
Thirty-five nurses/assistant nurses from 7regions were trained in mobile outreachactivities to extend services to vulnerablepopulations including IDPs
At this stage from CERF 1, WHO procuredapproximately 4 New Emergency Health Kits(supplies for 10,000 persons for 3 months)and 4 diarrhoeal disease (Cholera) kits nowavailable in Somalia. These suppliesduplicated the existing number of kits thatWHO has on hand.
Immunization and laboratory supplies havebeen ordered under CERF 1 and 2 and willsoon be in-country to support the polio andmeasles mass vaccination activities as well asimprove basic laboratory responses.
Once CERF 2 funds for water qualitymonitoring become available, support for thiscrucial activity for the water/sanitation clustercan be provided.
Challenges and wayforward
Mainly security of staff in the field, specificareas and difficulty of access to populationsin certain areas with and without conflict aswell as Internally Displaces Populations(IDPs) camps/settlements.
Consideration could be given to extending thecurrent time period for usage of funding (3 – 6months), particularly for the case of Somalia,as the organization and implementation ofactivities from outside the country and dealingwith multiple health authorities (including newemerging ones) is difficult.
CERF AchievementsSomalia