High Tibia Osteo tomy Pla e 4.5 Surgical Technique · Place an incision just above the tibial tube...
Transcript of High Tibia Osteo tomy Pla e 4.5 Surgical Technique · Place an incision just above the tibial tube...

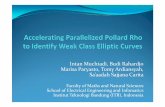
High Tibia Osteotomy Plate 4.5 Surgical Technique
Locking Compression Technology by aap


1
High Tibia Osteotomy Plate 4.5 Surgical Technique

2
Disclaimer
This surgical technique is exclusively intended for medical professionals, especially physicians, and thereforemay not be regarded as a source of information for non-medical persons. The description of this surgicaltechnique does not constitute medical advice or medical recommendations nor does it convey any diagnostic ortherapeutic information on individual cases. Therefore, the attending physician is fully responsible for providingmedical advice to the patient and obtaining the informed consent of the patient which this surgical techniquedoes not supersede.The description of this surgical technique has been compiled by medical experts and trained staff of aapImplantate AG with utmost diligence and to the best of their knowledge. However, aap Implantate AG excludesany liability for the completeness, accuracy, currentness, and quality of the information as well as for materialor immaterial damages arising from the use of this information.

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
3
Contents •
• Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .4• Material . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .4
• Description . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .4
• Indications / Contraindications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .5
• Processing (Sterilization & Cleaning) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .5
• Surgical Technique . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .6• Preoperative Planning . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .6
• Positioning . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .7
• Access . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .8
• Preparing the plate . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .9
• Placing K-wires . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .10
• Osteotomy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .12
• Opening the osteotomy gap using a Lambotte chisel . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .13
• Checking, measuring and stabilizing the osteotomy gap . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .14
• Inserting the LOQTEQ® High Tibia Osteotomy Plate . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .15
• Proximal plate fixation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .16
• Compressing the lateral cortical bone (optional) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .17
• Distal plate fixation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .18
• Replacing the spacers and securing the remaining holes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .19
• Replacing the standard screw by a locking cortical screw . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .20
• Radiological assessment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .21
• Explantation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .21
• Excursus – Artosal® (Reprobone®) wedges . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .22
• Trays . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .25• LOQTEQ® Osteotomy Set, HTO/DFO . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .25
Surgical TechniqueHigh Tibia Osteotomy Plate 4.5

Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
4
• Introduction
The LOQTEQ® High Tibia Osteotomy Plate 4.5 is part of the LOQTEQ® portfolio and unifies angular stability with modern
plate design. The corrective osteotomy of the tibial head is characteristic of joint-preserving corrections of tibial malposi-
tions. Despite its short design, the LOQTEQ® High Tibia Osteotomy Plate 4.5 ensures stable fixation of open-wedge osteo-
tomies and can therefore speed up postoperative mobilization through a smaller access and excellent angular stability.
Material
For the manufacture of angle stable plate systems materials are used which have been proven to be successful in
medical technology for decades. The anatomical plates and bone screws are made of titanium alloy.
All materials employed comply with national and international standards. They are characterized by good bio-
compatibility, a high degree of safety against allergic reactions and good mechanical properties.
Description
• High stability thanks to four locking screws in the plate head
• Fitted targeting device guarantees a safe placement of drill guides
at the preset angle
• High stability in the area of critical load thanks to an evenly rounded
transition from head to shaft
• Symmetrical plate in one length
• 4.5 mm locking screws are applied to round locking holes
• The flattened end of the plate shaft enables the tissue-conserving,
submuscular insertion of the plate

Indications/Contraindications
Indications
• Open-wedge osteotomies at the proximal medial tibia
• Treatment of bone and joint deformities
• Treatment of malpositions caused by injuries or disorders such as osteoarthritis
Contraindications
• Inflammatory or rheumatoid arthritis
• Gonarthrosis involving more than one compartment
• Poor soft tissue condition at the medial head of tibia
• Infection or inflammation (local or systemic)
• Allergies against the implant material
• High risk patients for anesthesia
• Severe soft tissue swelling impacting normal wound healing
• Fractures in children and adolescents with epiphyseal plates not yet ossified
Processing (Sterilization & Cleaning)
The implants are supplied sterile and non-sterile.
Implants and instruments that are supplied in non-sterile condition must be sterilized before use.
For this purpose, please refer to the instructions for use that are enclosed with the plates, instruments, and trays.
Do not use (sterile) implants from damaged or open inner packaging.
Implant components that have come or might have come into contact with infectious fluids (e.g. blood) must not
be resterilized and reused in another surgery. They must be returned to the manufacturer. Resterilization is prohibited
under any circumstances (see Instructions for Use).
aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
5
Introduction•
Surgical TechniqueHigh Tibia Osteotomy Plate 4.5

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
6
•Surgical Technique
Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
Preoperative Planning
• This surgical technique describes tibial head osteotomy using the example of the open-wedge method. Precise pre-
operative planning is essential for a successful procedure. This requires detailed knowledge of the anatomic and me-
chanical leg axes. For this purpose, take an image of the entire leg under load in AP view and proceed as follows:
1. Determine the mechanical
leg axis (Mikulicz line).
For this purpose, draw a
straight line from the center
of the femoral head (A) to
the middle of the talocrural
joint (B).
2. Determine the desired
weight-bearing line. From
the center of the femoral
head (A), draw the line
through the Fujisawa point
(C) lateral to the preopera-
tive center of the knee
joint (60%) to the postope-
rative talocrural joint (D).
3. Determine the center of
rotation (e) laterally, in the
proximal third of the tibio-
fibular joint but at least
15 mm below the joint line.
4. Connect the center of
rotation with the preopera-
tive endpoint (A) and the
planned endpoint of the
mechanical axis (D) and
determine the resulting
angle. This angle (α) should
correspond to the open
wedge osteotomy.
A A A A
C e
B D B D
Mikulicz lin
e
Fujisawa point
α
α

Surgical Technique•
aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
7Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
Positioning
• The patient is positioned supine on a radiolucent operating table. Ensure that the leg to receive surgery can be
placed in 90 degree flexion and complete extension.
• The surgery is performed in approx. 20° flexion to protect neurovascular structures. To facilitate access to the medial
aspect of the proximal tibia, extend the other leg and position it slightly lower. Intraoperatively, you must be able to
easily extend the leg to check the leg axis. A tourniquet may be placed.
N NOTE:
Ensure that the head of femur and the ankle can be viewed under fluoroscopy.
Start the osteotomy immediately above the pes anserinus. Ensure that there is enough space to easily place all proximal
screws and that they do not project into the osteotomy gap.
Conventional planning software can very clearly demonstrate the exact correction angles, incision depth of the osteo-
tomy and the resulting height of the osteotomy.
N NOTE:
Planning software does not replace thorough planning and in-depth surgeon training on correcting axial
malalignments.

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
8
•Surgical Technique
Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
INSTRUMENTS ART.-NO.Soft tissue retractor, radiolucent IU 7971-00
Access
• Slightly bend the leg. Place an incision just above the tibial tube-
rosity along the upper margin of the pes anserinus to the poste-
romedial edge of the medial tibial plateau.
• For access, perform the following steps:
1. Exposure of the pes anserinus and the superficial part of the
medial collateral ligament.
2. Mobilization of the medial collateral ligament and release of
the superficial part using a raspatory.
3. Insertion of the radiolucent soft tissue retractor between the
medial collateral ligament and tibia.
4. Detachment of the periosteum along the planned osteotomy.
N NOTE:
This exposure (see figure) is important to determine precisely
the course of the osteotomy.

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
9
Surgical Technique•
Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
Preparing the plate INSTRUMENTS ART.-NO.Angle Stable locking spacer LOQTEQ® 4.5 IU 7972-00Aiming device LOQTEQ® HTO plate IU 8184-01Screwdriver Duo, T25, quick coupling IU 7835-55Fixing screw aiming device LOQTEQ® LFI T25 IU 8176-04Large handle, cannulated, quick coupling IU 7706-00
• Screw the angle stable spacers (green) into the respective holes
(see figure).
• The spacers are intended to prevent irritation of the pes anserinus.
• Install the aiming device on the plate using the fixing screw.
N NOTE:
A thread holds the fixing screw in the aiming device.
For cleaning purposes, the screw must be screwed out of
the aiming device. For this purpose, apply slight pressure
onto the screw from the underside of the aiming device and
remove the screw.

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
10 Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
Placing K-wires INSTRUMENTS ART.-NO.K-wire with trocar point, ø2.5, L 200 NK 0025-20 Parallel drill guide for K-Wire, 2.5 IU 8190-25 Measuring device for K-Wire 2.5, L 200 IU 7925-20
• Place the knee in 20° flexion and adjust the fluoroscope in such a
way as to enable an AP view of the tibia.
• Under fluoroscopic monitoring, insert a K-wire ø2.5 into the
head of tibia in accordance with the planned osteotomy. For this
purpose, start over the pes anserinus, target the head of fibula
and insert to the opposite cortical bone.
N NOTE:
Under fluoroscopic monitoring, check the position of the K-wire.
If its positioning is not satisfactory, a second wire can be placed
directly next to it and compared with the first one under fluoros-
copic monitoring. Then remove the wrongly positioned K-wire.
N NOTE:
Ensure that enough space remains proximal to the osteotomy
to place the screws.
•Surgical Technique

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
11Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
• Insert the parallel drill guide (IU- 8190-25) over the K-wire to the
bone and insert a second K-wire along the planned osteotomy.
Under fluoroscopy, position the K-wires above one another.
N NOTE:
The sagittal inclination of the osteotomy should be parallel to
the tibial plateau.
• To determine the cutting depth, measure the depth of the inser-
ted K-wires using the measuring device for K-wires. Subtract
10 mm from the measured value for the opposite cortical bone.
Mark the determined value on the saw blade (e.g. with sterile pen
or Steri-Strip).
N NOTE:
In case of rotation correction or slope correction, parallel
K-wires or Steinmann pins can be inserted into the proximal
and distal fragments.
Surgical Technique•

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
12 Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
Osteotomy
• Using an oscillating saw, start below the K-wires and saw to the
marked depth along the K-wires. Ensure that the dorsal cortical
bone is completely sawed through. Do not sever the tuberosity.
• After completing the transverse cut to the planned depth, per-
form the anterior cut using a thin saw blade. This cut is perfor-
med continuously from the medial through the lateral cortical
bone. Depending on the osteotomy height and position of the
patella (Caton index), it can be performed proximally or distally.
N NOTE:
Proceed slowly. Cool the saw blade using irrigation and ensure
that the saw blade does not slip off.
Avoid abrasion at the radiolucent soft tissue retractor. Proceed
slowly when sawing. The sawing depth can be checked using
fluoroscopy.
•Surgical Technique
INSTRUMENTS ART.-NO.Soft tissue retractor, radiolucent IU 7971-00

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
13Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
Opening the osteotomy gapusing a Lambotte chisel
• Using gentle mallet taps, carefully insert the first chisel to the
lateral bridge along the transverse saw cut. The depth equals the
sawed depth.
• Slowly insert the second chisel between the first chisel and the
K-wires. The second chisel should be inserted less deep than the
first one.
N CAUTION:
It is important to open the osteotomy slowly to avoid fracture
of the lateral cortical bone.
• To further spread the osteotomy, a third chisel may be inserted
between the first two chisels. Each additional chisel is inserted
slowly and less deeply, until the desired osteotomy angle has been
achieved.
INSTRUMENTS ART.-NO.Lambotte chisel, 25mm IU 3000-25
Surgical Technique•

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
14 Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
Checking, measuring, and stabilizing the osteotomy gap
INSTRUMENTS ART.-NO.Wedge gauge IU 7960-00
• While spreading, continuously check the result on the basis of the
preoperative plan.
• After removing the chisels, carefully exert valgus stress. To deter-
mine the gap’s opening height and to maintain the opening,
place the wedge gauge into the gap. If a neutral tibial slope is
desired, the wedge gauge should be inserted dorsally.
N NOTE:
When inserting the wedge gauge, proceed carefully and if
possible do not use mallet taps to avoid damaging the cortical
bone.
• The base height of the osteotomy gap can be read off the wedge
gauge; this height should equal the preoperatively determined
height.
N NOTE:
If anterior K-wires or Steinmann pins have been used, they can
also serve to check slope correction.
N NOTE:
Use fluoroscopic monitoring to check the gap with the leg ex-
tended, in two planes. Also note the tibial slope.
•Surgical Technique

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
15Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
• The wedge gauges keep the osteotomy gap open at the desired
angle.
• Carefully remove the K-wires.
• Insert the prepared plate subcutaneously.
N NOTE:
The plate shaft should be approximately parallel to the tibial
diaphysis. Position the plate in such a way that screws can be
placed in all four proximal screw holes. The stabilizing part of
the plate (without holes) must bridge the gap.
• Screw a drill guide (blue) into the central proximal hole and in-
sert a reduction sleeve.
• Use a K-wire ø2.0 to temporarily fix in place the plate through the
reduction sleeve and use fluoroscopy to check the fit of the plate
as well as the course of the screws to be placed.
Inserting the LOQTEQ® High Tibia Osteotomy Plate
INSTRUMENTS ART.-NO.Aiming device LOQTEQ® HTO plate IU 8184-01 Drill guide for round hole LOQTEQ® 4.5, I-ø 3.9, blue IU 8167-20 Reduction sleeve for K-wire ø2.0 IU 8167-15 K-wire with trocar point, ø2.0, L 250 NK 0020-25
Surgical Technique•

• Secure the round locking holes in the proximal portion of the
plate using locking screws (blue). For this purpose, use the
previously used threaded drill guide (blue) for round holes.
The use of the screwdriver duo can facilitate the insertion and
later removal of the threaded drill guide.
• Drill to the desired depth using a drill bit ø3.8 (red-blue) for
locking screws without penetrating the opposite cortical bone.
Determine the drilling depth using the depth gauge and tighten
a locking screw (blue) of the appropriate length using the screw-
driver T25 and the handle with torque limiter.
N NOTE:
We recommend using screws of maximum possible length.
However, ensure that the lateral cortical bone is not penetrated.
N NOTE:
We recommend tightening the screws using the torque limiter.
Optimal fixation is reached once an audible click is heard.
• Secure all 3 proximal plate holes in this way.
aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
16 Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
INSTRUMENTS ART.-NO.Drill guide for round hole LOQTEQ® 4.5, I-ø 3.9, blue IU 8167-20 Twist drill ø3.8, L 180, coil 50, quick coupling IU 7438-18 Depth gauge for locking screws, large IS 7905-00 Handle with quick coupling, with torque limiter, 3.5Nm IU 7707-35Screwdriver Duo, T25, quick coupling IU 7835-55
Proximal plate fixation
•Surgical Technique

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
17Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
• In the first shaft hole below the osteotomy, the plate can be
pulled to the bone by a standard screw. For this purpose, screw
the threaded drill guide (blue) for round holes into the hole. The
use of the screwdriver duo can facilitate the insertion and later
removal of the threaded drill guide.
• Drill to the desired depth using a drill bit ø3.2 for standard screws.
Determine the drill depth using the depth gauge and tighten a
standard screw of appropriate length using the hexagonal screw-
driver.
• By tightening the screw, the plate is elastically bent. This means
that it is closer to the bone and creates a spring effect that cau-
ses compressive stress on the lateral cortical bone.
Compressing the lateral cortical bone (optional)
INSTRUMENTS ART.-NO.Drill guide for round hole LOQTEQ® 4.5, I-ø 3.9, blue IU 8167-20 Twist drill ø3.2, L 195, coil 50, quick coupling IU 7432-30 Depth gauge for locking screws, large IS 7905-00 Screwdriver, hexagonal, ø3.5 for quick coupling IU 7835-00Large handle, cannulated, quick coupling IU 7706-00
Surgical Technique•

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
18 Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
• Apply a locking screw to the penultimate hole in the distal part
of the plate. For this purpose, screw the threaded drill guide
(blue) for round holes into the hole. The use of the screwdriver
duo can facilitate the insertion and later removal of the threaded
drill guide.
• Drill bicortically to the desired depth using a drill bit ø3.8 (red-
blue) for locking screws. Determine the drilling depth using the
depth gauge and tighten a locking screw (blue) of the appro-
priate length using the screwdriver T25 and the handle with tor-
que limiter.
N NOTE:
We recommend tightening the screws using the torque limiter.
Optimal fixation is reached once an audible click is heard.
INSTRUMENTS ART.-NO.Drill guide for round hole LOQTEQ® 4.5, I-ø 3.9, blue IU 8167-20 Twist drill ø3.8, L 180, coil 50, quick coupling IU 7438-18 Depth gauge for locking screws, large IS 7905-00 Large handle, cannulated, quick coupling IU 7706-00Handle with quick coupling, with torque limiter, 3.5Nm IU 7707-35Screwdriver Duo, T25, quick coupling IU 7835-55
Distal plate fixation
•Surgical Technique

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
19Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
• Remove the spacer from the distal hole and replace it by a
locking screw. For this purpose, screw the threaded drill guide
(blue) for round holes into the hole.
• Drill to the desired depth bicortically or monocortically using a
drill bit ø3.8 (red-blue) for locking screws. Determine the drilling
depth using the depth gauge and tighten a locking screw (blue)
of appropriate length using the screwdriver T25 and the handle
with torque limiter.
N NOTE:
We recommend tightening the screws using the torque limiter.
Optimal fixation is reached once an audible click is heard.
• After removing the distal spacer, remove the proximal spacer and
replace it by a locking screw. For this purpose, screw the threaded
drill guide (blue) for round holes into the hole. Drill to the desired
depth using a drill bit ø3.8 (red-blue) for locking screws. Deter-
mine the drilling depth using the depth gauge and tighten a
locking screw (blue) of the appropriate length using the screwdri-
ver T25 and the handle with torque limiter.
N NOTE:
We recommend that you use a screw of maximum possible
length. However, ensure that the lateral cortical bone is not
penetrated.
Replacing the spacers and securing the remaining holes
INSTRUMENTS ART.-NO.Drill guide for round hole LOQTEQ® 4.5, I-ø 3.9, blue IU 8167-20 Twist drill ø3.8, L 180, coil 50, quick coupling IU 7438-18 Depth gauge for locking screws, large IS 7905-00 Screwdriver Duo, T25, quick coupling IU 7835-55Handle with quick coupling, with torque limiter, 3.5Nm IU 7707-35
Surgical Technique•

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
20 Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
• Finally, remove the previously placed standard screw from the
hole below the osteotomy gap and replace it by a locking screw.
Bicortically tighten the locking screw.
N NOTE:
You must drill again using a drill bit ø3.8 and the drill guide.
N NOTE:
We recommend tightening the screws using the torque limiter.
Optimal fixation is reached once an audible click is heard.
Replacing the standard screw by a locking cortical screw
INSTRUMENTS ART.-NO.Drill guide for round hole LOQTEQ® 4.5, I-ø 3.9, blue IU 8167-20 Twist drill ø3.8, L 180, coil 50, quick coupling IU 7438-18 Depth gauge for locking screws, large IS 7905-00 Handle with quick coupling, with torque limiter, 3.5Nm IU 7707-35 Screwdriver Duo, T25, quick coupling IU 7835-55
•Surgical Technique

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
21Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
• View the position of the plate and the correction results in two
planes under fluoroscopy.
• If the result is satisfactory, close the wound.
N NOTE:
The screwdrivers in the set (T25) are self-retaining. To achieve
maximum torque during screw removal, we recommend using
the appropriate explantation screwdriver (IU 7811-25). It al-
lows deeper penetration into the screw head and hence safe
screw removal. It can be ordered separately.
• The implant should be removed only after complete healing of the
osteotomy.
• Place an incision using the old scar.
N NOTE:
After manually loosening the screws, removal can be
performed in automated mode in a second step.
Radiological assessment
Explantation INSTRUMENTS ART.-NO.Screwdriver, T25, Round Handle IU 7811-25
Surgical Technique•

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
22 Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
• With years of experience in the development and manufacture
of biomaterials for traumatology, orthopedics and spine surgery,
aap offers optimally harmonized product combinations for
various indications.
For better and more stable fracture healing, aap recommends
complete defect filling using bone substitute in addition to the
employed osteosynthesis.
Artosal® is the optimal product for use in corrective osteotomies,
particularly thanks to its special wedge shape and its hydroxy-
apatite (HA) and β-tricalcium phosphate (β-TCP) composition.
• Artosal® is a fully synthetic osteoconductive bone substitute for
the reconstruction of aseptic bone defects and exhibits controlled
resorption.
With its ultra-porous and highly interconnected pore matrix,
Artosal® offers a similar strength as human cancellous bone and
supports the formation of the new natural bone. Artosal® can be
first coated with patient material to improve osseointegration.
Advantages
• Osteoconductive and completely biocompatible
• Very similar to the mineral component of human bone, with a
composition of 60% hydroxyapatite (HA) and 40% β-tricalcium
phosphate (β-TCP)
• Ultraporous with pore sizes of 200-800 μm
(average 250 – 400 μm)
• Interconnecting pore matrix is very similar to human cancellous
bone and particularly supports rapid and unlimited bone ingrowth
• Microporosity allows nutrient supply to the new bone
• Controlled resorbability after 1-2 years
• By products of absorption support osteoblast formation
and ingrowth
• Good adaptation to the defect size using existing surgical
instruments
Excursus - Artosal® (Reprobone®) wedges
•Surgical Technique

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
23Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
• Completely reproducible manufacture reduces or replaces the
need for autologous material
• Can be mixed with autologous material for additional enrichment
with patient growth factors
• More than 25 years of successful clinical results for material
combinations of HA and TCP
Osteoconductivity shown under fluoroscopy throughthe pores in the direction of the implant center
SIZE ANGLE ART.-NO.20 x 25 x 8 x 4 8° 24804020 x 25 x 10 x 5 10° 24804120 x 25 x 12 x 6 12° 24804220 x 25 x 14 x 7 14° 248043
30 x 35 x 8 x 4 8° 24804430 x 35 x 10 x 5 10° 24804530 x 35 x 12 x 6 12° 24804630 x 35 x 14 x 7 14° 248047
Surgical Technique•

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
24 Surgical TechniqueHigh Tibia Osteotomy Plate 4.5

Trays •
aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
25
LOQTEQ® Osteotomy Set, HTO/DFO IC 4500-00
Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
* available in 2014
ARTICLE ART.-NO.Tray for instruments, LOQTEQ® Osteotomy, empty IC 4500-01Screw rack for extension set LOQTEQ® Osteotomy, empty IC 4500-03Lid for trays, large IC 2008-00
Depth gauge for locking screws, large IS 7905-00Lambotte chisel, 25 mm IU 3000-25Twist drill ø 3.2, L 195, coil 50, quick coupling IU 7432-30Twist drill ø 3.8, L 180, coil 50, quick coupling IU 7438-18Large handle, cannulated, quick coupling IU 7706-00Handle with quick coupling, with torque limiter 3.5 Nm IU 7707-35Screwdriver, hexagonal, ø 3.5 for quick coupling IU 7835-00Screwdriver Duo, T25, quick coupling IU 7835-55Measuring device for K-Wire 2.5, L 200 IU 7925-20Wedge gauge IU 7960-00Angle gauge for closed wedge osteotomy IU 7970-00*Soft tissue retractor, radiolucent IU 7971-00Load drill guide LOQTEQ® 4.5, adjustable up to 2 mm IU 8167-03Reduction sleeve for K-wire ø 2.0 IU 8167-15Drill guide for round hole LOQTEQ® 4.5, I-ø 3.9, blue IU 8167-20Basic insert for load drill guide, LOQTEQ® 4.5, round hole IU 8167-45Fixing screw aiming device LOQTEQ® LFI T25 IU 8176-04Aiming device LOQTEQ® HTO plate IU 8184-01Aiming device LOQTEQ® DFO Plate, R IU 8185-01Aiming device LOQTEQ® DFO Plate, L IU 8185-02Parallel drill guide for K-Wire, ø 2.5 IU 8190-25K-wire with trocar point, ø 2.0, L 250 NK 0020-25K-wire with trocar point, ø 2.5, L 200 NK 0025-20
LOQTEQ® High Tibia Osteotomy Plate 4.5 PO 4560-01-2LOQTEQ® Distal Femur Osteotomy Plate 4.5, R PO 4561-01-2LOQTEQ® Distal Femur Osteotomy Plate 4.5, L PO 4562-01-2
AVALABLE ON REQUESTSrewdriver mini, SW 2.5 IU 7825-05

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
26
•Trays
Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
Standard screws with small head 4.5 Titanium
LOQTEQ® Osteotomy, Screw Rack, complete
ARTICLE ART.-NO.Cortical Screw 4.5, small head, self-tapping, L 22 SK 4512-22-2Cortical Screw 4.5, small head, self-tapping, L 24 SK 4512-24-2Cortical Screw 4.5, small head, self-tapping, L 26 SK 4512-26-2Cortical Screw 4.5, small head, self-tapping, L 28 SK 4512-28-2Cortical Screw 4.5, small head, self-tapping, L 30 SK 4512-30-2Cortical Screw 4.5, small head, self-tapping, L 32 SK 4512-32-2Cortical Screw 4.5, small head, self-tapping, L 34 SK 4512-34-2Cortical Screw 4.5, small head, self-tapping, L 36 SK 4512-36-2
ARTICLE ART.-NO.Screw rack for extension set LOQTEQ® Osteotomy, empty IC 4500-03
Angle Stable locking spacer LOQTEQ® 4.5 IU 7972-00

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
27
Trays •
Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
Screws for round locking hole 4.5 Titanium
ARTICLE ART.-NO.LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 18 SK 4526-18-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 20 SK 4526-20-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 22 SK 4526-22-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 24 SK 4526-24-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 26 SK 4526-26-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 28 SK 4526-28-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 30 SK 4526-30-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 32 SK 4526-32-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 34 SK 4526-34-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 36 SK 4526-36-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 38 SK 4526-38-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 40 SK 4526-40-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 42 SK 4526-42-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 45 SK 4526-45-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 50 SK 4526-50-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 55 SK 4526-55-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 60 SK 4526-60-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 65 SK 4526-65-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 70 SK 4526-70-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 75 SK 4526-75-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 80 SK 4526-80-2LOQTEQ® Cortical Screw 4.5, small head T25, self-tapp. L 85 SK 4526-85-2

aap Implantate AGLorenzweg 5 • 12099 Berlin • Germany
28
•Notice
Surgical TechniqueHigh Tibia Osteotomy Plate 4.5
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .

aap Implantate AGLorenzweg 5 • 12099 BerlinGermany
Phone +49 30 75019-0Fax +49 30 75019-111
Subject to technical modifications, errors and misprints.
© aap Implantate AGWP 2OP80 EN / 1405
Layout, type: deSIGN graphic - Wolfram Passlack
Illustrations: Karen Hilberg

WP
2OP0
80 E
N /
1405
aap Implantate AGLorenzweg 5 • 12099 BerlinGermany
Phone +49 30 75019-0Fax +49 30 75019-111