Herpes simplex keratitis
-
Upload
vichhey -
Category
Healthcare
-
view
398 -
download
5
Transcript of Herpes simplex keratitis
Outline
• Introduction
• Epithelial keratitis
• Disciform keratitis
• Necrotizing stromal keratitis
• Neurotrophic ulceration
• Prophylaxis
• Complication
I-Introduction
• Herpetic eye disease is the most common infectious cause of corneal blindness in developed countries
• 60% of corneal ulcers in developing countries
• 10 million people worldwide may have herpetic eye disease
I-Introduction
• Herpes simplex virus (HSV)• Two subtypes are HSV-1 and HSV-2 => neuronal ganglia
• HSV-1 causes infection above the waist (principally the face, lips and eyes)
• HSV-2 causes acquired infection (genital herpes). Rarely HSV-2 transmitted to the eye
• HSV transmission is facilitated in conditions of crowding and poor hygiene
I-Introduction
• Primary infection• Usually occurs in childhood
• Spread by droplet transmission, or less frequently by direct inoculation
• It is uncommon during the first 6 months of life (maternal antibodies)
• Symptom• Mild fever, malaise and upper respiratory tract symptoms
• Blepharitis and follicular conjunctivitis (usually mild and self-limited)
• Treatment• If necessary, involves topical acyclovir ointment
I-Introduction
• Recurrent infection• After primary infection: the virus is carried to the sensory for dermatome
• Subclinical reactivation• Can periodically occur
• Are contagious
• Clinical reactivation• A variety of stressors such as fever, hormonal change, ultraviolet radiation, trauma, or
trigeminal injury
• The pattern of disease• Depend on the site of reactivation
I-Introduction
• Recurrent infection• The rate for ocular recurrence
• After one episode is about 10% at 1 year and 50% at 10 year
• The higher the number of previous attacks the greater the risk of recurrence
• Risk factors for severe disease• Which may be frequently recurrent, include atopic eye disease, childhood,
immunodeficiency or suppression, malnutrition, measles and malaria
II-Epithelial keratitis
1. Clinical features
Epithelial (dendritic or geographic) keratitis is associated with active virus replication
• Presentation• May be at any age with
• Mild discomfort
• Redness
• Photophobia
• Watering
• Blurred vision
II-Epithelial keratitis
1. Clinical features
• Signs in chronological order• Swollen opaque epithelial cells arranged in a coarse punctate or stellate
pattern• Central desquamation results in a linear-branching (dendritic) ulcer• The ends of the ulcer have characteristic terminal buds and the bed of the
ulcer stains well with fluorescein• Margin of the ulcer stain with rose Bengal• Corneal sensation is reduced• Mild associated subepithelial haze is typical• Elevated IOP may occur• Following healing• Mild subepithelial scarring may develop after healing
II-Epithelial keratitis
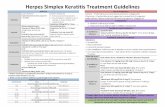
2. Treatment• Topical
• Aciclovir 3% ointment or ganciclovir 0.15% gel (5 times daily)• Trifluridine (up to nine times a day)
• Debridement• Protect adjacent healthy epithelium from infection• Eliminated the antigenic stimulus to stromal inflammation
• Oral antiviral• Probably indicated in most immunodeficient patients, poorly tolerated, or in resistant cases
• Interferon• Combination => speed healing
• Skin lesions• Treated with acyclovir cream five times daily
II-Epithelial keratitis
2. Treatment
• IOP control• If glaucoma treatment is necessary, prostaglandin derivatives should probably be avoided
• Tropical steroids• Are not used unless significant disciform keratitis is also present
• Slow healing or frequent recurrence• Combination of two topical agents with oral valaciclovir or famiciclovir
III-Disciform keratitis
• The exact aetiology: controversial
• It may be active HSV infection of keratocytes or endothelium, or a hypersensitivity reaction to viral antigen in the cornea
III-Disciform keratitis
1. Clinical features
• Presentation• Gradual onset of blurred vision which may be associated with haloes around lights
• Discomfort and redness are common but tend to be milder than in purely epithelial disease
III-Disciform keratitis
1. Clinical features
• Signs• A central zone of stromal oedema often with overlying epithelial oedema
• Keratic precipitates underlying the oedema
• Folds in Descement membrane in severe cases
• A surrounding immune ring of stromal haze
• IOP may be elevated
• Reduced corneal sensation
• Healed lesions • Faint ring of stromal or subepithelial opacification and thinning,
• Superficial or deep vascularization
III-Disciform keratitis
2. Treatment• Initial treatment
• Topical steroids (prednisolone 1% or dexamethasone 0.1%) with antiviral cover, both q.i.d
• Subsequently prednisolone 0.5% once daily is usually a safe dose at which to stop topical antiviral cover
• With active epithelial ulceration• Try to keep the steroid intensity as low as possible for adequate effect (b.d or t.i.d)
• With a more intensive antiviral (5 times daily)
• Topical cyclosporine 0.05%• Particularly in presence of epithelial ulceration
• To facilitate tapering of topical steroids
IV-Necrotizing stroma keratitis
• This rare condition is • Result from active viral replication within the stromal, though immune-
mediated inflammation
1. Signs• Stromal necrosis and melting, often with profound interstitial opacification
• Anterior uveitis with keratic precipitates underlying the area of active stromal infiltration
• An epithelial defect may be present
• Progression to scarring, vascularization and lipid deposition is common
2. Treatment• Similar to that of aggressive disciform keratitis
• But oral antiviral supplementation
V-Neurotrophic ulceration
• Neurotrophic ulceration • Caused by failure of re-epithelialization resulting from corneal anaesthesia
• Often exacerbated by other factors such as drug toxicity
1. Signs• A non-healing epithelial defect, sometimes after prolonged topical treatment
• The stromal beneath the defect is grey and opaque and may become thin
• Secondary bacterial or fungal infection may occur
2. Treatment• Topical steroid to control any inflammatory component should be kept to a minimum
VI-Prophylaxis
• Long-term daily aciclovir reduces the rate of recurrence of epithelial and stromal keratitis by about 50% and is usually well tolerated
• Considered in patients with frequent debilitating recurrence, particularly if bilateral or involving an only eye
• The standard dose of aciclovir is 400 mg b.d
• Oral valaciclovir 500 mg once daily or famiciclovir are alternatives
• The prophylactic effect decrease or disappear when the drug is stopped






























![Immunology of Herpes Simplex Virus Infection: …...[CANCER RESEARCH 36, 836-844, February 1976] Immunology of Herpes Simplex Virus Infection: Relevance to Herpes Simplex Virus Vaccines](https://static.fdocuments.in/doc/165x107/5e3c207dedbcb80872726a41/immunology-of-herpes-simplex-virus-infection-cancer-research-36-836-844.jpg)