Herpes simplex keratitis & herpes zoster opthalmicus
-
Upload
laxmi-eye-institute -
Category
Healthcare
-
view
10.011 -
download
1
Transcript of Herpes simplex keratitis & herpes zoster opthalmicus

HSV Keratitis and Herpes Zoster Ophthalmicus
Presenter : Dr.Rasika Thakur Moderator : Dr. Vishram Sangit

Case presentationHSV keratitis
Introduction Pathology and Clinical featuresTreatment
Herpes zoster ophthalmicusIntroduction Pathology and Clinical featuresTreatment
Clinical pattern of Herpes simplex keratitis: A case series

Case scenario 1
Mr X, 24/MCame to us on 29/12/2011 with c/o redness
and watering of RE since 2 monthsBCVA-RE:FC1/2 m,N36,LE:6/6,N6Patient had taken treatment elsewhere ,but
found no relief with Eye drop tobramycinEye drop moxifloxacin and ketorolac Eye ointment neosporin
• Recurrent attack of HSV keratitis

29/12/2011

2/1/2012

5/1/2012 13/1/2012

27/1/2012 1/3/2012

13/9/2012

26/10/2012

30/11/2012

Case scenario ii
Patient Mr.XYZ, 65/MC/o redness and watering since 7 days

18/3/2014
Fortified cefazolin half hourly
Ciplox eyedrop half hourlyAtropin eyedrop TDS

21/3/2014

28/3/2014

2/4/2014
Impression -HSV keratitis with bacterial keratitis

21/4/2014

Mixed corneal ulcer

Introduction
Herpes simplex is the leading cause of infectious corneal blindness*
While not all humans manifest herpes infection, more than 90% carry the latent virus
HSV keratitis is Herpes simplex viral infection of the cornea
*Liedtke W., Opalka B., Zimmermann C.W., Lignitz E.: Age distribution of latent herpes simplex virus 1 and varicella-zoster virus genome in human nervous tissue. J Neurol Sci 1993; 116:6-11

Herpes simplex virus

Life cycle of HSV

Primary HSV infection
Blepharoconjunctivitis Follicular conjunctivitis Lid vesicles and conjunctival dendrites Kaposi’s varicelliform eruption Severe morbidity -multi-system failure or
bacterial superinfection
Darougar S., Hunter P.A., Viswalingam M., et al: Acute follicular conjunctivitis and keratoconjunctivitis due to herpes simplex virus in London. Br J Ophthalmol 1978; 62:843-849

Clinical Importance
Human herpesviruses have in common a state called “latency” where the virus remains dormant in cells and periodically reactivates
Herpes simplex viruses 1 and 2 (HSV-1 and HSV-2) have an affinity for the sensory ganglion cells and are therefore called neurotrophic viruses

Recurrent HSV Infections
Multiple factors are thought to cause recurrence including fever, sunlight, irradiation, menses, and emotional stress
Recurrent disease most commonly causes keratitis
HSVK is broadly classified into epithelial and stromal/endothelial keratitis

Epithelial Keratitis
SymptomsFB sensationphotophobiaRednessBlurred vision
Clinical featuresPunctate epithelial keratitisClassic arborizing dendritic epithelial ulcers with
terminal bulbsGeographic epithelial ulcerCiliary flush & conjunctival injection

Epithelial Keratitis
Dendritic ulcerGeographic ulcerMarginal keratitisMetaherpetic (trophic) ulcer

Dendritic ulcerClassic herpetic lesionThe borders are slightly raised,grayish, and stain
with rose bengal as they consist of infected cells that have undergone acantholysis
On resolution, a dendrite-shaped scar, called a ghost dendrite, may remain in the superficial stroma

Geographic ulcer
Immunocompromised, on topical steroids, or have longstanding, untreated ulcers*
Dichotomous branching and terminal bulbs are seen at the periphery
*Wilhelmus K.R., Coster D.J., Donovan H.C., et al: Prognosis indicators of herpetic keratitis. Analysis of a five-year observation period after corneal ulceration. Arch Ophthalmol 1981; 99:1578-1582

Marginal keratitis
Located near the limbus The presence of an epithelial defect and lack of
corneal sensation can aid in diagnosisSignificant stromal inflammationThey are more resistant to treatment and
frequently become trophic ulcers*
*Thygeson P.: Marginal herpes simplex keratitis simulating marginal catarrhal ulcer. Invest Ophthalmol 1971; 10:1006

Treatment
Indications- ulcers larger than 4 mm, marginal ulcers, and ulcers with underlying stromal inflammation
Topical antivirals
Gentle wiping débridement is a very good adjunct therapy as infected cells are acantholytic and are poorly adherent
Wilhelmus K.R.: The treatment of herpes simplex virus epithelial keratitis. Trans Am Ophthalmol Soc 2000; 98:505-532

Metaherpetic (trophic) ulcerTrophic ulcer,if it arises de novo or a
metaherpetic ulcer if it follows a dendrite or geographic ulcer
Causes-Toxicity from antiviral medicationsLack of neural-derived growth factorsPoor tear surfacingLow-grade stromal inflammation
Neurotrophic ulcers start as roughened epithelium, which then breaks down to produce an epithelial defect with smooth margins

Treatment
Stop toxic medicationsTear film supplementationBandage contact lenses Amniotic membraneThe cautious use of topical steroids may be
necessary if there is significant underlying inflammation

Stromal/Endothelial Keratitis
It is an immune-mediated response to nonreplicating viral particles
All layers of the cornea are affected and may involve the trabecular meshwork and iris
It is classified based on the predominant site and type of involvement

Stromal/Endothelial Keratitis
EndotheliitisNecrotizing keratitisImmune stromal keratitisKeratouveitis

Endotheliitis
Manifests as overlying stromal edema from endothelial dysfunction
Longstanding stromal edema leads to permanent scarring and is the major cause of decreased vision associated with HSVK

Endotheliitis
Localized endotheliitis Disc-shaped area of
corneal edema so called disciform keratitis
There is minimal stromal inflammation and no epithelial involvement
Diffuse and linear endotheliitis Accompanied by
trabeculitis with a resulting elevated intraocular pressure
Pseudo-guttae and Descemet’s folds

Necrotizing keratitis
Inflammation in the cornea is due to a reaction to live viral particles in the corneal stroma
Corneal melting and perforationAssociated with uveitis and trabeculitis that may
lead to recalcitrant glaucoma

Necrotizing keratitis

Immune stromal keratitis
Manifests as focal, multifocal, or diffuse stromal opacities or an immune ring
Stromal edema and a mild anterior chamber reaction
It is called interstitial keratitis (IK) if accompanied by vascularization

Keratouveitis
Uveitis is usually granulomatous with large “mutton-fat” keratic precipitates on the endothelium
It can lead to significant morbidity from synechiae, cataracts, and glaucoma
Unilateral uveitis associated with high intraocular pressure is almost always caused by HSV

Treatment
The mainstay of treatment is topical steroids as they decrease inflammation and therefore scarring
Oral antivirals Topical antivirals Aggressive topical and systemic antivirals along
with steroids are necessary in necrotizing keratitis and focal serous iritis

Diagnosis
Diagnostic testing is seldom needed in epithelial HSVK because of its classic clinical features and is not useful in stromal keratitis as there is usually no live virus present

Diagnosis
Culture DNA Testing Fluorescent Antibody TestingTzanck Smear Serum Antibody Testing

HERPETIC EYE DISEASE STUDY (HEDS)
To assess the effect of adding steroids and acyclovir to conventional therapy with trifluridine (TFT)
It was a prospective RandomizedDouble-maskedPlacebo-controlledMulti-center study Divided into six trials: three therapeutic, two
preventive, and one cohort

HEDS
Herpes Stromal Keratitis, Not on Steroids Trial
Compared with the placebo group, patients who received prednisolone phosphate drops had faster resolution and fewer treatment failures
Wilhelmus K.R., Gee L., Hauck W.W., et al: Herpetic Eye Disease Study. A controlled trial of topical corticosteroids for herpes simplex stromal keratitis. Ophthalmology 1994; 101:1883-1895

HEDS
Herpes Stromal Keratitis, on Steroid Treatment There was no apparent benefit to adding oral
acyclovir to topical corticosteroids and TFT. However, visual acuity improved over 6 months in more patients in the acyclovir group than in the placebo group
Barron B.A., Gee L., Hauck W.W., et al: Herpetic Eye Disease Study. A controlled trial of oral acyclovir for herpes simplex stromal keratitis. Ophthalmology 1994; 101:1871-1882

HEDS
Herpes Simplex Virus Iridocyclitis, Receiving Topical Steroids
The trial was stopped because of slow recruitment, but treatment failures occurred at a higher rate in the placebo group than in the acyclovir group, indicating a potential benefit to adding oral acyclovir to the regimen of a topical steroid and an antiviral
A controlled trial of oral acyclovir for iridocyclitis caused by herpes simplex virus. The Herpetic Eye Disease Study Group. Arch Ophthalmol 1996; 114:1065-1072

HEDS
Herpes Simplex Virus Epithelial Keratitis Trial
In the treatment of acute HSV epithelial keratitis with TFT, the addition of oral acyclovir offered no additional benefit in preventing subsequent stromal keratitis or iritis

HEDS
Acyclovir Prevention Trial
Oral acyclovir reduced the risk of any form of recurrent ocular herpes by 41% and stromal keratitis by 50%. The risk of multiple recurrences decreased from 9% to 4%
Although there was no rebound increase in keratitis after discontinuation of the acyclovir, the protection did not persist once the acyclovir was discontinued
Oral acyclovir for herpes simplex virus eye disease: effect on prevention of epithelial keratitis and stromal keratitis. Herpetic Eye Disease Study Group. Arch Ophthalmol 2000; 118:1030-1036

HEDS
Ocular HSV Recurrence Factor Study
No association was found between psychological or other forms of stress and HSV recurrences
Previous episodes of epithelial keratitis were not a predictor for future occurrences while previous, especially multiple, episodes of stromal keratitis markedly increased the probability of subsequent stromal keratitis
Oral acyclovir for herpes simplex virus eye disease: effect on prevention of epithelial keratitis and stromal keratitis. Herpetic Eye Disease Study Group. Arch Ophthalmol 2000; 118:1030-1036

Limitations: Many of the trials had inadequate recruitment or high
dropout rate
Oral acyclovir in the prevention trials was only used for 3 weeks
The steroid regimen was standardized and not tailored to inflammation
TFT was used in both the study and placebo groups in all the therapeutic trials

Current antivirals

Treatment
Steroids1% prednisolone acetate or 0.1%
dexamethasone is usedSurgery
Penetrating keratoplasty (PKP) Conjunctival flap Amniotic membrane (AMT)

FUTURE DIRECTIONS
Heat shock and glycoprotein subunit vaccines have shown some promise in clinical trials in decreasing the number and severity of recurrences of HSVK
while newer medications such as topical ganciclovir and cidofovir may prove to be more effective and cause less toxicity compared to current therapy*
Although monotherapy with interferon has not been found to be effective, it increases the efficacy of acyclovir and ganciclovir when given in combination**
*Colin J., Hoh H.B., Easty D.L., et al: Ganciclovir ophthalmic gel (Virgan; 0.15%) in the treatment of herpes simplex keratitis. Cornea 1997; 16:393-399**Wilhelmus K.R.: The treatment of herpes simplex virus epithelial keratitis. Trans Am Ophthalmol Soc 2000; 98:505-532

Herpes zoster ophthalmicus

Introduction
Recurrent infection of varicella (chickenpox) in the ophthalmic division of the trigeminal dermatome most frequently affecting the nasociliary branch

Epidemiology and clinical Importance
Herpes zoster is a neurocutaneous disease caused by the human herpes virus 3
Member of the herpes virus family (Herpesviridae) and exclusively infects human or simian cells
The lifetime risk is 20–30%, and 50% of those living until 85 years of age will be affected*
Physical trauma and surgery have been correlated with the development of zoster**
*Donahue J.G., Choo P.W., Manson J.E., Platt R.: The incidence of herpes zoster. Arch Intern Med 1995; 155:1605-1609**Evans R.W., Lee A.G.: Herpes zoster ophthalmicus, ophthalmoplegia and trauma. Headache 2004; 44:286-288

Pathogenesis
In temperate climates,primary infection occurs before the age of 10, manifests as chickenpox (varicella)
The virus then establishes a latent state in the sensory ganglia
When there is diminished virus-specific and cell-mediated immunity, the virus may reactivate and spread to the corresponding dermatome along a spinal or cranial nerve to generate the characteristic unilateral vesicular exanthema

Pathogenesis
Begins with a prodrome of influenza-like illness -fatigue, malaise, nausea and mild fever accompanied by progressive pain and skin hyperesthesia
A diffuse erythematous or maculopapular rash then appears over a single dermatome 3–5 days later
These eruptions progress to form clusters of papules and clear vesicles, which then evolve through stages of pustulation and crusting

Clinical manifestations

Clinical manifestations
Eyelids Periorbital edema, pain, and hyperesthesia of
the eyelid skinSecondary bacterial infection may occur
following dermal involvement*Complications- scarring, cicatricial ectropion
or entropion, trichiasis, madarosis, poliosis, or even frank loss of eyelid tissue
*Weiss R.: Herpes zoster following spinal surgery. Clin Exp Dermatol 1989; 14:56-57

Clinical manifestations
Conjunctiva papillary, pseudomembranous, membranous, or follicular reaction
Episclera/Sclera HZV episcleritis and scleritis may be either
localized or diffuse

Clinical manifestations
Cornea Herpes zoster corneal disease can result in
significant vision loss. Five basic clinical forms:
Epithelial keratitis (acute or chronic)Nummular stromal keratitisDisciform keratitisLimbal vascular keratitisNeurotrophic keratitis, with or without corneal perforation

Clinical manifestations
Uveitis- Nongranulomatous or granulomatous
iridocyclitis (anterior uveitis) with keratic precipitates and posterior synechiae
Lens -Posterior subcapsular cataracts

Clinical manifestations
Anterior Chamber Angle and Glaucoma Plugging of the trabecular meshwork due to
the presence of cellular debris, iris pigment, or hyphema
Pupillary-block glaucoma secondary to posterior synechiae, with resultant iris bombe
Peripheral anterior synechiaeChronic open-angle glaucoma-due to damage
to the trabecular meshwork
Chang S.D., De Luise V.P.: In: Tasman W., Jaeger E.A., ed. Duane’s ophthalmology, Vol, 4. Philadelphia, PA: Lippincott Williams & Wilkins; 2001.ch 20 (CD-ROM)

Clinical manifestations
Pupil Horner’s syndrome A tonic pupil secondary to herpes zoster ciliary
ganglionitisOptic Nerve
Neuroretinitis, retrobulbar neuritis, or an ischemic optic neuropathy
Herpes zoster optic neuritis may result from local transmission of the virus within the orbit from the fifth to the second cranial nerve

Clinical manifestations
Vitreous-Vitreous opacities, vitritis, and vitreous hemorrhage
Retina –Retinal hemorrhagesRetinal thrombophlebitisBranch or central retinal artery occlusionRetinal arteritisNecrotizing retinopathy, necrotizing retinitisExudative or rhegmatogenous retinal detachment Ischemic perivasculitis

Clinical manifestations
Extraocular Muscles Ophthalmoplegia 11–31%Affect cranial nerves three, four, and sixCan also manifest as a myositis that may also
lead to ophthalmoplegia

Clinical manifestations
Postherpetic Neuralgia Pain that continues following rash healing Pain has three phases:
Acute pain occurring within 30 days after rash onset
Subacute herpetic neuralgia that persists beyond the acute phase but resolves before 120 days
Chronic PHN that persists 120 days or more after rash onset

Herpes zoster ophthalmicus in acquired
imune deficiency syndrone (AIDS) HZO is an important early clinical marker for
AIDS, especially in high-risk younger patientsHigher incidence, greater severity, and
prolonged course of corneal and uveitic involvement, as well as postherpetic neuralgia
Treatment -prolonged treatment course of intravenous acyclovir

Herpes zoster ophthalmicus in acquired imune deficiency syndrome(AIDS)
Progressive outer retinal necrosis a distinct form of necrotizing herpetic retinopathy
Characterized by multifocal, deep retinal lesions that rapidly progress to confluence with minimal or no intraocular inflammation, an absence of vascular inflammation, and perivenular clearing of retinal opacification

Diagnosis
The diagnosis of herpes zoster disease is based on clinical findings
Direct detection of the virus and indirect serological detection of specific antibodies
Cytologic examination of cutaneous vesicular scrapings reveals multiple eosinophilic intranuclear inclusions (Lipschutz bodies) and multinucleated giant cells (Tzanck preparation)
Electron microscopy VZV-DNA can also be directly detected in clinical
specimens using real-time PCR

Management
Systemic medication-Oral acyclovir (800 mg, five times daily) for 7–
10 daysFamciclovir (500 mg three times daily for 7
days)Valacyclovir (1000 mg three times daily)
Cobo L.M., Foulks G.N., Liesegang T., et al: Oral acyclovir in the treatment of acute herpes zoster ophthalmicus. Ophthalmology 1986; 9

Management of Ocular Manifestation
Palliative therapy including Burow’s solution, cool compresses, mechanical cleansing of the involved skin, and topical antibiotic ointment without steroid are helpful in treating skin lesions
Débridement may also be helpfulNeurotrophic keratitis or the epithelial defects -
nonpreserved artificial tears, eye ointments, pressure patching, or therapeutic soft contact lenses

Management of Ocular Manifestation
Tarsorrhaphy, conjunctival flap, or autologous conjunctival transplantation
Steroids should not be used in cases of exposure or neurotrophic keratitis because of the possibility of keratolysis*
Topical cycloplegicsAqueous suppressants and topical corticosteroids
should be used to treat HZO glaucoma
*Liesegang T.: Corneal complications from herpes zoster ophthalmicus. Ophthalmology 1985; 92:316.

Management of Ocular Manifestation
Herpes zoster retinitis, optic neuritis, chorioretinitis, acute retinal necrosis syndrome, and progressive outer retinal necrosis are best treated with a combination of systemic steroids and acyclovir i.v

Postherpetic Neuralgia treatment
AnalgesicsAntidepressants (amitriptyline, desipramine,
clomipramine), carbamazepine, and phenytoinFamciclovir and valacyclovir significantly reduce
the duration but not incidenceSteroids have no effect on PHN

Postherpetic Neuralgia treatment
Amitriptyline for 90 days reduced the incidence of pain at 6 months.
Trial of percutaneous electrical nerve stimulation (PENS) in 50 patients suggested a decrease in pain incidence at 3 and 6 months when compared with famciclovir

Clinical pattern of Herpes simplex keratitis: A case series
Dr Vishram Sangit1
Dr Suhas Haldipurkar1,Dr Maninder Setia1,
Mr Anirban Paik1
1 Laxmi Eye Institute, Panvel, Maharashtra
FP-799; Electronic Poster no. 11

Purpose
To study the clinicoepidemiological pattern of Herpes
simplex keratitis in a tertiary eye hospital in western
Maharashtra

Results41 eyes of 40 patients identifiedAll diagnoses – clinicalMean age - 44.4 +/- 18.54 yearsM:F – 27:13Past history of similar episode- 20 patientsHistory of trauma in 7 patientsOnly 2 out of 40 patients reported pain as the presenting complaintRedness and blurring of vision was the most common symptom
reported by 38 patientsMean duration of symptoms before presentation was 17.67 days ( range 2 to 90 days)

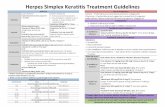
Clinical form of HSV Keratitis

Treatment protocols
Epithelial disease- Acyclovir ointment 5 times a day for 3 weeks
Stromal disease- Acyclovir ointment 5 times a day with 1% prednisolone acetate in tapering doses
Endothelitis- Intensive prednisolone acetate 1% with systemic Acyclovir 400 mg 5 times a day

Treatment outcomes
All cases resolved on medical therapy
Mean duration to resolution for entire group was 34.18 +/- 15.85 days
Clinical form
Epithelial Stromal Endothelitis Kerato-uveitis Mixed
Duration (days)
18.6 39.06 29.66 35 35.91
Time to resolution in various forms of HSV keratitis

Mean time to resolution in various forms of HSV keratitis ( days)

Recurrence patternPrimary clinical form developing recurrence during treatment
Clinical form of recurrence in HSV keratitis (%)

ConclusionsStromal form of HSV keratitis is the commonest
presentation in our series followed by mixed variety
HSV keratitis affects people in young and productive age group
Good response to medical therapy achieved in all forms
Resolution of stromal keratitis takes longest while epithelial keratitis takes shortest time
Recurrences are common and clinical form of disease in recurrences can be different from the original disease form

Thank you