Herpes simplex infections in atopic eczema
Transcript of Herpes simplex infections in atopic eczema

Archives of Disease in Childhood, 1985, 60, 338-343
Herpes simplex infections in atopic eczema
T J DAVID AND M LONGSON
Department of Child Health and Department of Virology University of Manchester
SUMMARY One hundred and seventy nine children with atopic eczema were studied prospec-
tively for two and three quarter years; the mean period of observation being 18 months. Tenchildren had initial infections with herpes simplex. Four children, very ill with a persistently highfever despite intravenous antibiotics and rectal aspirin, continued to produce vesicles and were
given intravenous acyclovir. There were 11 recurrences among five patients. In two patients therecurrences were as severe as the initial lesions, and one of these children had IgG2 deficiency.Use of topical corticosteroids preceded the episode of herpes in only three of the 21 episodes.Symptomatic herpes simplex infections are common in children with atopic eczema, and are
suggested by the presence of vesicles or by infected eczema which does not respond to antibiotictreatment. Virological investigations are simple and rapid: electron microscopy takes minutes,and cultures are often positive within 24 hours.
Patients with atopic eczema are susceptible toparticularly severe infections with herpes simplexvirus. Most cases are probably due to type 1,1 buteczema herpeticum due to the type 2 virus has beendescribed,2 and the incidence of type 2 infectionsmay be underestimated because typing is not usuallyperformed. The source of the virus is assumed to bea close relative or friend with herpes labialis,3 butspread in hospital by nurses may occur.4 Cases ofeczema herpeticum mostly represent an initialinfection,3 though the documentation of this isscanty.5 6 Patients with eczema herpeticum maybecome seriously ill with a high fever, and death canoccur.3 The cause of death, though not always clearfrom published reports, may be due to someundetected immune deficiency state such as theWiskott-Aldrich syndrome4 7 or to secondary bac-terial infection, usually with a combination of groupA haemolytic streptococci and Staphylococcusaureus.5
Severe herpes simplex infections are known to bea complication of other dermatological disordersincluding autosomal dominant ichthyosis vulgaris,8Darier's disease,9 familial benign pemphigus,1°pemphigus foliaceous,'1 and congenital ichthyosi-form erythroderma.12 It is not known whether thesusceptibility of patients with certain skin diseases tosevere herpes simplex infections is due to anunderlying immunological abnormality or is merelyattributable to the abnormal skin.We report the incidence, clinical and laboratory
features, and treatment of herpes simplex infectionsin a group of 179 children with atopic eczema.
Patients and methods
Between January 1982 and September 1984 allchildren referred to the department of child healthwith atopic eczema were studied prospectively forevidence of infection. Patients who had been fol-lowed for less than six months were excluded. Onehundred and seventy nine patients were observedfor 3199 patient months, with a mean of 18 months.
Patients were seen routinely at least threemonthly as outpatients, but the parents were askedto attend with their child in the event of sudden orunexpected deterioration of the eczema, or if therewas new evidence of infection such as crusting,discharge, or the appearance of vesicles or pustules.The finding of intact vesicles or pustules with a smallcentral depression ('umbilicated pustules') led to thesuspicion of herpes simplex infection. Where whathad been thought to be simple bacterially infectedeczema failed to respond to treatment with appro-priate oral or parenteral antibiotics within 48 hours,infection with herpes simplex was suspected.Specimens for virology were only collected in
patients where the above criteria led to the sus-picion of herpes infection. No specimens wereobtained from patients who were well or where onlybacterial infection was suspected. Swabs for virologyin transport medium (balanced salt solution, bovine
338

serum albumen, antibiotics) were taken directly tothe regional virus laboratory. Where vesicles were
present, collection of material for electron micro-scopy was attempted. A clean dry microscope slidewas placed in contact with a vesicle that had beenpunctured with a small sterile needle. The wet slidewas allowed to dry in air. In the laboratory the driedmaterial on the slide was suspended in a drop ofdistilled water before negative staining and electronmicroscopy. Herpes virus antibodies were soughtwith a standard complement fixation test and alocally produced antigen.An initial infection was defined as the first
recognisable clinical lesion suggestive of the pres-ence of herpes simplex virus, combined with isolationof the virus in tissue culture. Seroconversion wasdefined as an initial specimen of blood with undetect-able antibody, with a titre of at least 1/20 in aconvalescent specimen, using the complementfixation test.
Results
Initial infections. During the study period initialinfections with herpes simplex virus weredocumented in 10 of the 179 patients. Tables 1 and 2
Herpes simples infections in atopic eczema 339
summarise the clinical and laboratory features.Ichthyosis was present in nine of the 10 patients anda prominent feature in three. Only three childrenhad had topical corticosteroids in the previous sixmonths. In five there was a history of a relative orfriend with herpes labialis.
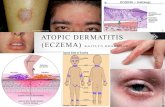
Clinical featuresIn one patient the lesions were confined to bothcheeks, and management at home simply compriseda topical antiseptic. Seven children required admis-sion to hospital, in one case as a precautionarymeasure because of poor home circumstances, andin the rest because of the severity of the lesions. Onepatient also had gingivo-stomatitis. Vesicular lesionswere seen where there was no associated bacterialinfection, but in the presence of bacterial infectionvesicles had the appearance of pustules, were
sometimes umbilicated, and contained purulentfluid (Fig. 1). In areas where vesicles were con-
fluent, raw areas of skin were seen after vesiclerupture (Fig. 2). The vesicles were usually fragileand burst easily with gentle rubbing. Once thevesicles had ruptured, and where the vesicles hadnot been confluent, the resulting lesions could bedifficult to distinguish from simple septic spots that
Table I Initial herpes simplex infections: clinical features
Case Age Sex Surface area Site of herpetic Maximum temperatureno (months) affected by eczema lesions (IC)
1 20 M 70 Legs, arms, neck, face, trunk 40-22 71 F I Both cheeks Not measured*3 21 M 8( Legs, arms, trunk, eye 40)-)4 32 M 80 Legs, left middle finger (whitlow) 40.05 94 F I Face 36-66 40 M 3 Legs 38-77 1(04 F 90 Face, neck, hands, stomatitis 37-58 5 M 15 Face, ear, eye 39 59 56 M 20 Hands, arms, heel, behind ear, face Not measured*10 54 M S Arm Not measured*
*Temperature not taken because seen in the clinic without history of fever.
Table 2 Initial herpes simplex infections: laboratory features
Case Serum IgE (IUII) Electron Herpes simplex Seroconversion*no microscopy isolation in culture
1 468 (normal <29) Positive Positive Yes2 892 (normal <63) Not done Positive Not tested3 11 700 (normal <29) Not done Positive Yes4 11 150 (normal <42) Positive Positive Yes5 129 (normal <63) Not done Positive Yes6 810 (normal <42) Not done Positive Yes7 35 (normal <80) Not done Positive Yes8 18 (normal <11) Positive Positive Yes9 1010 (normal <52) Negative Positive Yes10 5645 (normal <52) Positive Positive Yes
'Defined as initial specimen with undctectable antibody, with a titre of at least 1/20 in a convalescent specimen, using the complement fixation test.

340 David and Longson
Fig. 1 Case 3. Most vesicles have become pustular, andthere are some satellite lesions on the chest wall.
*. _i
Fig. 2 Case 4. Left ankle. A raw area is visible centrallywhere the vesicles had been confluent. Some typicalumbilicated pustules are seen above the raw area.
Fig. 3 Case 10. Right arm. Typical vesicles are only seen inthe palm. The remaining vesicles have been broken, andthe appearance ofthe wrist or ante-cubitalfossa isindistinguishablefrom that ofsimple non-herpetic infectedeczema.
had been scratched (Fig. 3). The clinical distinctionbetween bacterial and herpetic infection of thefingertip was especially difficult. One child (case 4)had a paronychia which was thought to contain pusdue to bacterial infection, but surgical explorationcombined with avulsion of the nail showed no pus.
In three children, only failure of infected eczemato respond to parenteral benzylpenicillin and fluc-loxacillin gave rise to the suspicion of herpes. In twoof these pustules were present on admission, andwith hindsight the correct diagnosis should havebeen suspected earlier. In the third, neither we northe mother had seen vesicles or pustules, and it wasthe failure of crusted infected eczema to improvewith oral antibiotics that led to the collection ofspecimens for virology.
In four children, continued production of vesicles,the persistence of high fever (greater than 39-5°C)despite parenteral benzylpenicillin and flucloxacillinin high dosage and rectal aspirin, accompanied byprostration and general debility, led to the adminis-tration of intravenous acyclovir (5 mg/kg three timesa day) for five days. In each case this was followedby a cessation of vesicle production and rapidresolution of fever. Five children were only treatedwith oral phenoxymethylpenicillin and flucloxacil-

lin, combined with a topical antiseptic ointmentcontaining povidone-iodine.
Bacteriological resultsNo bacteria were recovered from the lesions of cases
1 and 2. Staph aureus was recovered from thelesions of the other eight, accompanied byhaemolytic streptococci in seven (Lancefield groupA in six, group B in one).
Virological resultsElectron microscopy was not attempted in fivepatients, but out of the other five patients, virusparticles of the herpes group were seen in four.Herpes simplex virus was grown in tissue culture inall 10 patients. Seroconversion was found in all ninepatients from whom appropriate acute phase andconvalescent specimens had been obtained.
Immunological resultsSerum concentrations of the immunoglobulins A,G, and M were normal in nine patients. One patienthad normal serum concentrations of IgA, IgG, andIgM, but had a deficiency of the IgG subclass IgG2.She is described in detail elsewhere.13 The serumIgE values are given in Table 2.
Recurrent herpetic lesions. Recurrence of herpeticlesions occurred in five children. Clinical andlaboratory data are given in Table 3. In four (cases1, 4, 7, and 8) the initial infection had occurredduring the study period. In one (case 11) the initialinfection had occurred several years before thepatient was referred to us.
Herpes simples infections in atopic eczema 341
Clinical featuresIn cases 1 and 4 the recurrences were trivialcompared with the initial lesions. In case 11 theinitial and recurrent episodes were identical. In case
8, the recurrence comprised herpetic keratitis. Incase 7 the recurrences were only slightly lessextensive than the initial lesions, although recoverywas more rapid with the second and subsequentepisodes. In each case (apart from case 8, where therelapse was ocular) all recurrences comprised a cropof vesicles easily identified by the parents asherpetic. In none had topical corticosteroids beengiven before the recurrence. Apart from the thirdrecurrence of case 1, which coincided with arespiratory infection, the recurrences did not co-incide with intercurrent illnesses.The distribution of the recurrent lesions was most
odd. In cases 7, 8, and 11, the recurrences were all atthe precise site of the initial lesions. In case 4, thefirst recurrence affected the same single digit thathad been affected originally. The second recurrenceaffected the back of the same hand, though this hadnot been involved in the initial infection. In case 1
the first recurrence comprised herpetic whitlows(paronychia) of both middle fingers. The secondrecurrence comprised a crop of vesicles over thedorsum of the inter-phalangeal joint of boththumbs, accompanied by an herpetic whitlow (sub-ungual collection of pus from which the virus wasrecovered) of the right middle finger. This patient'sfingers had not been affected in the initial infection.He was not in the habit of sucking his thumbs orfingers. His third recurrence was again striking forthe symmetry of the lesions in both axillae, an area
Table 3 Recurrent herpetic lesions: clinical and laboratory findings
Case Age at Age at recurrence and site Electron Herpes simplexNo initial mnicroscopr isolation in
infection First recurrence Second recurrence Third recurrence culture(months)
1 2)0 26 months 27 months 30 months Pos;pos;pos Pos;pos,posBoth middle fingers Both thumbs, right Axillae, elbows, back,
(whitlows) middle finger thigh(whitlow)
4 32 34 months 51) months - Pos;pos Pos;posLeft middle finger Back of left hand
7 104 105 months 1117 months 109 months Neg;neg:neg Pos;pos;posFace, neck, hands Face, neck. hands Fiace, neck, hands
8 5 7 months - Not done PosFye
II* 96 166 months 172 months - Neg;neg Pos;posLeft pinna, left cheek l,eft pinna, left cheek
*Boy. First attack at 96 months on left pinna and left cheek. Eczema affecting 8% of skin surface area, with mild ichthyosis. IgE 61)3 IU/I(normal <70). The history suggested that there had been approximately 10 recurrences between the initial infection and his first being seen by us at the age of141) months.Pos =positive; neg =negative.

342 David and Longson
that had not been affected in the initial infection.The other areas affected in the third recurrence, theelbows, back, and thigh, had all been affected in theinitial infection.No patient was systemically ill during a herpetic
recurrence except for the respiratory infectionassociated with the third recurrence in case 1.Topical antiviral treatment (idoxuridine 0-1% eyedrops) was given for the ophthalmic relapse. Oralacyclovir (5 mg/kg three times a day for five days)was given to case 11, with topical povidone-iodineointment and oral phenoxymethylpenicillin andflucloxacillin, in the hope that it might preventfurther recurrences; it did not. Recurrences in theother three patients were treated with a topicalantiseptic and oral antibiotics.
Bacteriological resultsThere were 10 recurrences of skin lesions; Staphaureus was recovered in eight, accompanied by Pihaemolytic streptococci (Lancefield group A) in five(with group B streptococci in one).
Discussion
In this study of 179 children with atopic eczema,there were 21 symptomatic episodes of herpessimplex infection in a two and three quarter yearperiod. This may be an underestimate, for noattempt was made to look for viral infection in thosewith lesions suggestive of uncomplicated bacterialinfection or in those with no evidence of infection.Initial infections with herpes simplex are common innormal children, and there is no evidence from thisstudy or any other that the incidence is any higher inchildren with atopic eczema. Our patients were aselected group, with an excess of severe or intrac-tible cases, and it could be that the incidence orseverity of herpes infections is not as high in childrenwith less severe eczema. The fact that seven of the10 children with initial herpes infections had onlylocalhsed eczema suggests, however, that the occur-rence of eczema herpeticum is unrelated to theextent of the eczematous lesions.Why unusually severe herpes simplex infections
are associated with specific skin diseases is obscure.Presumably the explanation lies either in the abnor-mal skin itself, or in some common underlyingimmunological explanation. The fact that neutralis-ing antibodies fail to protect from recurrencessuggests that the postulated immunological defect isnot one of antibody production but of cellularimmunity. Whether the virus spreads locally in theskin or whether haematogenous spread occurs hasnot been established. Topical corticosteroids are
well known to potentiate bacterial or fungal infec-tion in the skin, but there is disagreement aboutwhether they predispose to or potentiate viralinfections.14 In only three of the 21 episodes hadthere been recent use of topical corticosteroids. Thisunusual under usage of corticosteroids partly re-flected local treatment policy and partly parentalfear (often disproportionate) of adverse affects.Clearly, in our series of patients corticosteroids werenot an important predisposing factor. A furtherunexplained problem is the curious distribution ofrecurrent lesions. While some of these were at thesite of the initial infection, as one might expect witha virus that can remain dormant, others were atdistant sites and were sometimes striking in theirbilateral symmetry. Why only some patients shouldexperience recurrent lesions is also obscure.Sudden deterioration of atopic eczema is com-
monly due to infection. Where vesicles are seen thepresence of herpes simplex should be sought.Failure of infected eczema to respond to appropriateoral antibiotics within 48 hours suggests herpes.Electron microscopy can be completed in minutes,and herpes simplex grows rapidly in sensitive cellculture, for example human embryo fibroblastswhich are commonly used in most virology labor-atories in Europe and the United States, so thatpositive results can often be obtained within 24hours. Clinical diagnosis alone is not adequate,because similar appearances may be caused byCoxsackie virus infection.15 16 Electron microscopyalone is not adequate, for it merely confirms thepresence of a virus from the herpes group.
Claims that antiviral treatment is lifesaving ineczema herpeticum are probably exaggerated, for itis doubtful whether the disease is life threateningwhen appropriate antibiotics are given. In mostcases eczema herpeticum is likely to be a highlyunpleasant disease that recovers on its own. It wouldseem unreasonable, however, to withhold a fairlysafe and effective drug such as acyclovir in severecases, particularly those with fever and systemicillness, where antiviral treatment so dramaticallyshortens the illness. Whether acyclovir is best givenintravenously17 or orally18 is unclear. Acyclovir is,however, rather insoluble and not well absorbedwhen given orally, so for ill patients we havepreferred the intravenous route. The decision totreat for five days was arbitrary-it is possible that48 hours treatment would have sufficed for theclinical response was so rapid.
We thank Dr S Richmond, Dr R W Newton, Dr R H Macdonald,Dr M R Haeney, Dr R F Williams, Professor R D H Boyd,Professor S Shuster, and the Booth Hall Children's HospitalDepartment of Medical Illustration for their help.

Herpes simples infections in atopic eczema 343
References
Leyden JJ, Baker DA. Localised herpes simplex infections inatopic dermatitis. Arch Dermatol 1979;115:311-2.
2 Hazen PG, Eppes RB. Eczema herpeticum caused by herpesvirus type 2. Arch Dermatol 1977;113:1085-6.
3 Atherton DJ, Marshall WC. Eczema herpeticum. Practitioner1982;226:971-3.
4 Clinicopathological conference. A case of recurrent Kaposi'svaricelliform eruption. Br Med J 1962;i:313-20.
5 Jackson ADM, Dudgcon JA. Kaposi's varicelliform eruption:diagnosis and treatment. Great Ormond Street Journal 1951;2:125-32.
6 Wheeler CE, Abele DC. Eczema herpeticum, primary andrecurrent. Arch Dermatol 1966;93:162-73.
7 St Geme JW, Prince JT, Burke BA, Good RA, Krivit W.Impaired cellular resistance to herpes-simplex virus in Wiskott-Aldrich syndromre. N Engl J Med 1965;273:229-34.Verbox J, Munro DD, Miller A. Recurrent eczema herpeticumassociated with ichthyosis vulgaris. Br J Dermatol 1972;86:638-40.
9 Toole JWP, Hofstader SL, Ramsay CA. Darier's disease andKaposi's varicelliform eruption. J Am Acad Dermatol 1979;1:321-4.
1 Ogilvie MM, Kesseler M, Leppard BJ, Goodwin P, White JE.Herpes simplex infections in pemphigus: an indication forurgent viral studies and specific anti-viral therapy. Br JDermatol 1983;109:611-3.
Silverstein EH, Burnett JW. Kaposi's varicelliform eruptioncomplicating pemphigus foliaceous. Arch Dermatol 1967;95:214-6.
12 Fitzgerald WC, Booker AP. Congenital ichthyosiformerythroderma. A case report of two cases in siblings, onecomplicated by Kaposi's varicelliform eruption. Arch DermSyph 1951;64:611-9.
13 David TJ, Lakhani PK, Haeney MR. Severe eczema herpe-ticum, recurrent pneumococcal meningitis and recurrent eczemaherpeticum. J Roy Soc Med 1984;77:696-7.
14 Burton JL. Side effects of topical steroid therapy. Research andClinical Forums 1983;5:61-8.
15 Higgins PG, Crow KD. Recurrent Kaposi's varicelliform erup-tion in Darier's disease. Br J Dermatol 1973;88:391-4.
16 Cushing RD, Lerner AM. Eczema herpeticum. Presenting ashand foot and mouth syndrome. Mich Med 1972;71:611-2.
7 Swart RNJ, Vermeer BJ, Van Der Meer JWH, Enschede FAJ,Versteeg J. Treatment of eczema herpeticum with acyclovir.Arch Dermatol 1983;119:13-6.
18 Woolfson H. Oral acyclovir in eczema herpeticum. Br Med J1984;288:531-2.
Correspondence to Dr T J David, Booth Hall Children's Hospital,Charlestown Road, Blackley, Manchester M9 2AA.
Received 31 December 1984