HELICAL COMPUTED TOMOGRAPHIC PORTOGRAPHY IN TEN NORMAL DOGS AND TEN DOGS WITH A PORTOSYSTEMIC SHUNT
-
Upload
paul-frank -
Category
Documents
-
view
212 -
download
0
Transcript of HELICAL COMPUTED TOMOGRAPHIC PORTOGRAPHY IN TEN NORMAL DOGS AND TEN DOGS WITH A PORTOSYSTEMIC SHUNT

HELICAL COMPUTED TOMOGRAPHIC PORTOGRAPHY IN TEN NORMAL DOGS AND TEN DOGS WITH A PORTOSYSTEMIC SHUNT
PAUL FRANK, DVM, MARY MAHAFFEY, DVM, MS, CHRISTINE EGGER, DVM, MVsc, KAREN K. CORNELL, DVM, PHD
Contrast enhanced helical computed tomography (CT) of the liver and portal system is routinely performed in human patients. The purpose of this project is to develop a practical protocol for helical CT portography in the dog. Ten clinically normal dogs were initially evaluated to develop a protocol. Using this protocol, ten dogs with confirmed portosystemic shunts (PSS) were then evaluated. Each patient was anesthetized, and a test dose of sodium iothalamate (400 mg Vml) at 0.55 mVkg was injected. Serial images were acquired at the level of T12-13 or T13-L1. The time to maximum enhancement of the portal vein was determined. This time period was used as the period between the second injection (2.2 mVkg) and the start of the helical examination of the cranial abdomen. Delay times for normal dogs ranged from 34.5 s-66.0 s (median: 43.5 s) or 1.41 skg-4.12 s k g (median: 2.09 skg). For patients with a PSS, the delay times were 16.5-70.5 s (median: 34.5 s) or 1.47-19.17 s k g (median: 3.39 skg). The aorta, caudal vena cava, portal vein, shunt vessels, and their respective branches were well visualized on the CT images. Clinical case results were surgically confirmed. The surgeons reported that the information gained from the CT portography resulted in a subjective decrease in surgical time and degree of dissection necessary compared with similar surgeries performed without angiographic infor- mation. We believe that helical CT portography in the dog will be a useful adjunct in the diagnosis of PSS. The use of helical CT portography may allow clinicians to give clients a more accurate prognosis prior to surgery and will allow patients with lesions that are not surgically correctable to avoid a costly and invasive procedure. Veterinary Radiology & Ultrasound, Vol. 44, No. 4, 2003, p p 392-400.
Key words: dogs, portosystemic shunt, computed tomography, x-ray, portography.
Introduction
ONTRAST ENHANCED HELICAL COMPUTED TOMOGRAPHY C K T ) of the liver and portal system is routinely per- formed in human patients. Indications in humans include evaluation of portal vasculature secondary to portal hyper- tension, evaluation of transjugular intrahepatic portosys- temic shunt patency, detection of portosystemic shunts (PSS), evaluation of suspected liver disease, evaluation of liver or pancreatic neoplasia, and evaluation for surgical planning.
Dual phase CT angiography of the hepatic vasculature is performed by imaging the liver immediately after intrave- nous (IV) antecubital contrast medium injection (arterial phase) and a subsequent repeat examination (portal phase).'."' ' This procedure is usually accomplished in hu- mans with a breath-hold technique to minimize motion.
From the Departments of' Anatomy and Radiology (Frank, Mahaffey) and Small Animal Medicine and Surgery (Egger, Cornell), College of Veterinary Medicine, University of Georgia, Athens, GA 30602.
Address correspondence and reprint requests to Paul Frank, DVM, at above address. P.S. Funding provided by the University of Georgia Com- panion Animal Research Fund and the Chattanooga Kennel Club, Inc.
Received April 29, 2002; accepted for publication on October 8, 2002.
This results in a short duration outpatient procedure relative to the more invasive methods of portal visualization (opera- tive mesenteric portography, percutaneous transhepatic por- tography, cranial mesenteric angiography, percutaneous splenoportography, etc).631"-12 The advantages of helical CT angiography with peripheral contrast medium injection over other methods used in humans to evaluate the portal vasculature are that helical CT angiography is noninvasive, easier to perform and interpret than Doppler ultrasonogra- phy, can be performed as an outpatient procedure, can be used in a protocol to minimize operator variation, and rapid volumetric data acquisition is Disadvantages include the fact that portal flow and pressure cannot be measured, iodinated contrast medium injection is required, artifacts caused by metallic surgical implants and motion are possible, and false positives and negatives can O C C U ~ . ~
Although anesthesia is not required for helical CT angiog- raphy in humans, any proposed use of helical CT angiog- raphy in veterinary medicine would have the additional dis- advantage of requiring anesthesia. Helical CT has the ad- vantage over traditional sequential CT in that it is faster. Acquisition speed is important for breath-hold duration and duration of maximal vascular enhancement. Helical data have the additional advantage over traditional sequential
392

VOL. 44, No. 4 HELICAL COMPUTED TOMOGRAPHIC PORTOGRAPHY 393
data in that helical data sets can be reconstructed in three dimensions with less misregistration artifact caused by respiratory motion than sequential data. ' ,14
Many sources discuss optimal imaging parameters, injec- tion parameters, and delay times for helical CT angiography in humans, with little consensus.2'6'9'12~15-18~22 Multiple pro- tocols with varying amounts and rates of contrast medium administration and delay of examination onset have been evaluated in humans. Some protocols involve computerized detection of optimal examination delay. Other protocols in- volve predetermined delay 8322 Because blood flow to the splanchnic vasculature is individually variable, some authors advocate using a test bolus of contrast me- dium or computerized bolus tracking to determine optimal delay times.2,4,12,'4~'6~'8,22 To the authors' knowledge, simi- lar studies evaluating helical computed tomographic portog- raphy in dogs have not been reported.
Purpose
The purpose of this project was to develop a practical protocol for helical CT portography in normal dogs and to determine the ability of this technique to identify shunt ves- sels in dogs with PSS. In a pilot study, it was determined that the helical CT unit* at the Veterinary Medical Teaching Hospital of the University of Georgia could not image rap- idly enough to accomplish dual phase helical CT proce- dures; therefore, only the portal phase was evaluated.
Materials and Methods
This project consisted of two phases. The first phase was to develop a protocol for helical CT portography using nor- mal dogs, and the second was to determine the utility of this procedure in dogs with PSS. For helical CT portography, it was necessary to know the time for maximum opacification of the portal vein after injection of iodinated contrast me- dium into a peripheral vein. This was determined by IV injection of iodinated contrast medium during acquisition of axial CT images at one location. The time for maximum opacification was then used to obtain the helical CT por- tography images during helical scanning of normal dogs and dogs with suspected PSS.
Normal Dogs
Ten clinically normal, random source dogs (1 2.73-3 1.82 kg, median 20.90 kg) were evaluated. All protocols were approved by the Institutional Animal Care and Use Com- mittee of the University of Georgia. Physical examination, complete blood count, serum chemistry profile (BUN, Glu, Cr, Alb, TP, ALP, ALT, T.Bili), and pre- and post-prandial bile acids were performed. Eight of the ten dogs had mildly increased pre-prandial bile acids of 6.1-12.4 FmolL; ref-
*SOMATOM AR. S t a e , Siemens AG, Munich, Germany
erence range 0-5. One dog had post-prandial bile acid val- ues of 20.3 p.mol/L; reference range 0-20. None of these values were considered to be indicative of significant liver dysfunction. Lateral abdominal radiographs were made to assess liver size. All were assessed to be within normal limits. An IV catheter? was placed in a cephalic vein, and the dogs were anesthetized. In 4 dogs, 18 gauge, 2 inch catheters were used, and in 6 dogs 20 gauge, 2 inch cath- eters were used. The anesthetic protocol consisted of atro- pine sulfate$ (0.04 mgkg IM) and acepromazine maleate# (0.1 mgkg IM) as a premedication, propofol" (4 mgkg IV) for induction, and halothane# administered via endotracheal tube as a maintenance for 7 dogs. In 3 dogs, the aceproma- zine was omitted. The patient was placed in dorsal recum- bency on the CT table, and the cephalic vein catheter was connected to a power injector** via high-pressure tubing.?? The power injector was used for all contrast medium injec- tions. Systolic blood pressure and expired CO, levels were monitored intermittently to assist in maintaining the animal at an appropriate level of anesthesia.
To insure that helical CT portography examinations were made at the time of maximal opacification of the portal vein, the time to maximal portal vein opacification was measured following a test injection of a small dose of contrast medium in each dog. After the patient was positioned in dorsal re- cumbency, a test injection of 0.55 mukg of iodinated con- trast medium (400 mg I/ml sodium iothalamatett) as made IV through the previously placed cephalic catheter at a rate of 5 ml/sec. Imaging began at the onset of the injection. Serial axial images were made at L1-2 or T12-13 every 4.5 seconds beginning at the onset of the contrast medium in- jection (Fig. 1). These images were made with incremental (non-helical) scanning mode. Intervals of 4.5 seconds were chosen because of CT machine limitations. The anatomic location of these images was L1-2 in the first 7 normal dogs. However, it was determined that this permitted only incon- sistent visualization of the portal vein. The next 3 normal dogs were imaged at T12-13 as the landmark with good visualization of the portal vein. CT numbers measured in Hounsfield units were obtained from the central portion of the portal vein for each image. This was done to determine which image contained the maximum opacification of the portal vein. The time corresponding to the image with maxi- mal portal vein opacification was used as the delay time for the second injection. Although the actual time/density chart was not produced at the time of imaging, in essence the peak
tTerumo'h', Sherwood Medical, Ireland $Phoenix Pharmaceuticals, St. Joseph, MO SBoehringer Ingelheim Vetmedica, Inc., St. Joseph, MO IIPropoFlolM, Abbott Labs, N. Chicago, IL #Halocarbon Laboratories, River Edge, NJ **Antiomat 6000rM, Liebel-Flarsheim, Cincinnati, Ohio ?-FHP30-FM, B. Braun Medical, Inc., Bethlehem, PA. (Maximum 1000
$$Conray 400LM, Mallinkrodt, Inc., St. Louis, MO p s i . )

394 FRANK ET AL. 2003
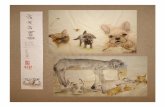
FIG. 1. Selected transverse CT images made through the abdomen at the level of the T12-13 disc space in a normal dog. Images were made every 4.5 seconds after IV injection of 0.55 mlkg of iodinated contrast medium. Dorsal is at the bottom and the patient’s right is on the left of all images. (A) Image made at 12 seconds after injection. The aorta (Ao, small curved arrow), caudal vein cava (CVC, open arrow), and portal vein (PV, large curved arrow) are not yet opacified by contrast medium. (B) Image made at 16.5 seconds after injection. The Ao is opacified, but the CVC and PV are not. The two small opacified structures are branches of the abdominal aorta. (C) Image made at 30 seconds after injection. The CVC and Ao are opacified, although the Ao is less opacified than in (B). The PV is minimally opacified. (D) Image made at 66 seconds post injection. The Ao, CVC, and PV are opacified. This is the image from which the maximum CT number was obtained from the central portion of the PV. 66 seconds was used as the delay time for the helical examination in this dog.
of the time/density curve was chosen as the optimal delay time. If the portal vein was not seen, a mesenteric vein was used as the reference vessel.
The time to maximal portal vein opacification obtained from the previous test injection was used as the time be- tween the second iiijection of contrast medium and the be- ginning of the helical examination. The second injection was at the same rate as the prior test injection, but the amount was 2.2 ml/kg. All dogs were hyperventilated be- fore the helical examination to produce apnea. This was done to minimize respiratory motion. Just before the initia- tion of the helical examination, hyperventilation was stopped. The area from the L2-3 disc space through the
dome of the diaphragm was imaged, with the first image beginning caudally. Maximum injection pressures measured by the automatic injector were recorded for each test injec- tion and helical injection.
For each dog, the imaging parameters were set for the lowest pitch and collimation that would allow for a suffi- cient time to complete the examination. The maximum con- tinuous examination time allowed by the CT machine was 42 seconds. Examination length from the L2-3 interverte- bra1 disc space through the dome of the diaphragm was chosen to allow complete visualization of the portal vein. The reconstruction interval was always one-half of the slice thickness. The dogs were imaged using a collimation 3-5

VOL. 44, No. 4 HELICAL COMPUTED TOMOGRAPHIC PORTOGRAPHY 395
mm, pitch of 1.4-1.8, and image reconstruction interval of 1.5-2.5 mm. After the procedure, the IV catheter was re- moved and visually inspected for evidence of damage.
Dog With PSS
Using the above-described technique, ten client-owned dogs (1 3-24.0 kg, median 6.75 kg) were examined after obtaining owner consent. Eight of these dogs were exam- ined by transcolonic scintigraphy prior to the helical CT portography procedure. The calculated shunt fraction ranged from 65% to 96% with a median of 80% in seven dogs. The shunt fraction was unable to be calculated for one dog because of a technical error. The helical CT portogra- phy procedure used for the patients was identical to the normal dogs with the following exceptions.
Each dog was anesthetized using a protocol approved by the hospital anesthesiologist. This protocol vaned among patients based on the unique requirements of each patient. Saphenous vein catheters were placed in 2 dogs instead of cephalic vein catheters. 20-gauge catheters were used in 4 patients, 18-gauge catheters were used in 4 patients and 22-gauge catheters were used in 2 patients (See Table 1).
TABLE 1
(4) The location of the images for the test injection was at T12-13 for 8 dogs and L1-2 for 2 dogs (See Table I).
(5) None of the patients received acepromazine. (6) Expired CO, was not monitored. (7) Maximum injection pressures during the test and helical
injections were not recorded in one dog. (8) Smaller dogs (1.8-20 kg) were imaged using a collima-
tion of 2-3 111111, a pitch of 1.33-1.67, and a reconstruc- tion interval of 1-1.5 mm. Larger dogs (16.7-24 kg) were imaged using a collimation of 5 mm, a pitch of 1.4, and a reconstruction interval of 2.5 mm.
Results
Normal Dogs
The aorta, caudal vena cava, portal vein, and their respec- tive branches were well visualized in all dogs (Fig. 2). No catheter damage was noted. Maximum injection pressures obtained during the test injection varied from 65 psi-108 psi with a median of 86. Maximum injection pressures during the helical injection varied from 65 psi-108 psi with a me- dian of 94 psi. Systolic blood pressure and expired CO, remained within normal limits at the time of imaging. The time to maximal portal vein enhancement was 34.5-66.0 sec
Group Number Delay time, Delay time Delay time/weight, Delay timelweight, in group range (sec) median (sec) range (seckg) median (seckg)
All dogs Healthy dogs Clinical cases (CC) Healthy, 20 G t Healthy, 18 G$ Healthy, T12/13§ Healthy, L1/2I1 Healthy, 20 G, T12/13 Healthy, 20 G, L1/2 Healthy, 18 G, T12/13 Healthy, 18 G, L1/2 Healthy, with ace¶ Healthy, without ace CC, 20 G CC, 18 G CC, 22 c** CC, T12/13 CC, L1/2 CC, 20 G, T12/13 CC, 20 G. L1/2 CC, 18 G, T12/13 CC, 18 G, L1/2 CC, 22 G, T 12/3 CC, 22 G, L1/2
21* 11* 10 6 5 4 7 4 2 0 5 8 3 4 4 2 8 2 3 1 4 0 1 1
16.5-66.0 34.546.0
34.5-66.0 39.0-52.5 34.5-66.0 34.5-52.5 34.5-66.0 39.0-43.5
NA 34.5-52.5 34.5-66.0 34.543.0 16.5-39.0 16.5-70.5 34.5-34.5 16.5-70.5 30.0-34.5 16.5-39.0
30.0 16.5-70.5
NA 34.5 34.5
16.5-70.5
39.0 43.5 34.5 45.75 39.0 54.75 39.0 54.75 41.25 NA
39.0 45.75 39.0 32.25 41.25 34.5 34.5 32.25 34.5 30.0 21.0 NA
34.5 34.5
1.41-19.17 1.41L4.12
1.65-3.20 1.41M.12 1.65-3.1 1 1.4 14.12
1.47-19.17
1.65-3.1 1 1.95-3.20
NA 1.414.12 1.65M.12 1.41-2.11 1.47-19.17 1.51-3.68 6.39- 15.68 1.51-19.17 1.47-15.68 3.11-19.17
1.47
NA 6.39
15.68
1.51-3.68
2.71 2.09 3.39 2.39 2.09 2.39 2.09 2.39 2.57 NA 2.09 2.40 1.65 5.26 2.77
1 I .04 3.39 8.57 7.40 1.47 2.77 NA 6.39
15.68
t = 20 gauge catheters $ = 18 gauge catheters ** = 22 gauge catheters 1 = acepromazine 9: = test scan location was at T12/13 11 = test scan location was at L ID * = Includes 10 dogs with PSS. 10 different healthy dogs, one received 2 injections.

396
A
FRANK ET AL. 2003
C
FIG. 2. Selected images made during the helical portion of the procedure in a healthy dog. Images are from caudal (A) to cranial (D). The Ao (straight solid arrow), CVC (solid arrowhead), and PV (curved solid arrow) are clearly visible in each image. The PV is seen branching within the liver parenchyma in (D) (arrow). Dorsal is at the bottom and the patient’s right is on the left of all images.
(median, 43.5 sec) or 1.41-4.12 sec/kg (median, 2.09 sec/ kg) (Table 1). All patients recovered without incident.
Dogs with PSS
The shunt vessel was identified in all dogs. The visual- ization of the aorta, caudal vena cava, portal vein, the shunt vessel(s), and their respective branches was excellent in 7 of the 10 dogs (Figs 3,4). In two dogs, prominent respiratory motion compromised image quality and made shunt identi- fication more difficult. In one dog, respiratory motion de-
creased image quality but did not inhibit identification of the shunt vessel. A total of 3 intrahepatic, 3 single extrahe- patic, 3 portal-azygous, and I multiple extrahepatic shunts were identified. In the five dogs where the procedure time was recorded, the total time from entry to the C T room to exit from the CT room was 20 to 60 minutes (median 25).
Maximum injection pressures during the test injection varied from 0 psi-1 73 psi with a median of 79. The dog with the zero reading was a very small dog and only 2 ml of contrast medium were injected. Maximum injection pres- sures during the helical injection varied from 72 psi-173 psi with a median of 94 psi. Systolic blood pressure remained

VOL. 44, No. 4 HELICAL COMPUTED TOMOGRAPHIC PORTOGRAPHY 3 97
FIG. 3. Selected images from the helical portion of the procedure in a dog with a PSS. Images are from caudal (A) to cranial (D). The Ao (straight solid ‘arrow), CVC (solid arrowhead), and PV (curved solid arrow) are clearly visible in each image. (A) The PV is enlarged and tortuous. (B) The shunt vessel (arrow) can be seen connecting the PV and CVC. (C) The PV has almost completely emptied into the CVC. (D) The PV is no longer seen and the CVC is enlarged. Diagnosis was single large extra-hepatic shunt. Dorsal is at the bottom and the patient’s right is on the left of all images.
within normal limits at the time of imaging. The time to maximum portal vein enhancement was 16.5-70.5 sec (me- dian, 34.5 sec) or 1.47-19.17 sec/kg (median, 3.39 seckg) (Table 1).
All patients underwent exploratory laparotomy after the helical CT portography procedure. Imaging data was inter- preted prior to laparotomy and included presence or absence of a shunt and an anatomical description of the shunting vessel. All shunts were confirmed at surgery and were found to be consistent with the imaging data. The surgeons re- ported that the information gained from the CT portography resulted in a subjective decrease in surgical time and degree of tissue manipulation necessary compared to similar sur- geries performed without angiographic information. Nine dogs recovered uneventfully from anesthesia. One dog with an intrahepatic shunt died in the post-operative period after attempted correction of the PSS. The helical CT portogra- phy procedure was in the same anesthetic episode as the surgery.
Discussion
The described technique of helical CT portography yielded consistently excellent visualization of the portal vein, caudal vena cava, aorta, and shunt vessels, even in very small dogs. This procedure was able to provide ana- tomically specific data that were believed to decrease the surgical time and degree of tissue manipulation that the patient endured during laparotomy.
Injection parameters, examination parameters, and delay times were based on data from studies performed in hu- mans, the results of our pilot study, and patient variables. In most CT portography procedures in humans, an injection rate of 1.5-5 mllsec of various iodine concentrations was
We chose to use the faster injection speed to maximize the bolus effect and to minimize the potential loss of small normal or abnormal vessels caused by partial volume effects. l 2 Dosage of contrast medium used in studies on adult humans varied greatly, but approxi-
used, 1,2,4,6,8-14,16-22

398 FRANK ET AL. 2003
FIG. 4. Dorsal plane reconstruction of a helical examination of the same dog as in Fig. 3. This single thin section was made with maximum intensity projection. Cranial is at the top, and the patient’s left is on the right side. The PV (straight solid arrow) is seen entering into the CVC (curved solid arrow) and the left gastric vein (solid arrowhead) is seen entering the PV. Note the slight misregistration artifact (open arrowhead) due to breathing motion. This small artifact was considered to be of no consequence in the interpretation of the helical examination in this patient.
mately 2.2 mlkg of varying concentrations of contrast me- dia was used most often. We chose a dosage of 2.2 mlkg of sodium iothalamate$$ (400 mg Uml), which resulted in a dosage of 880 mg I/kg. One study2’ in humans measuring time to peak opacification of the pancreas showed a strong correlation between time to maximum opacification of the test bolus and the larger bolus. This study also showed a large variability in the absolute values of the delay times between patients,22 similar to the current study in dogs. These facts suggest that individual test boluses will permit better results than fixed delay
Examination parameters depended on the size of the dog. The CT system in use would allow 42 seconds of continu- ous examination time before the tube capacity was reached. Thus, the spatial length of imaging was limited by the pitch (the number of slice thicknesses of table feed per rotation) and collimation (the width of a slice). A higher pitch or wider collimation would have allowed for longer examina- tion lengths; however, increasing either of these parameters would decrease resolution. Increasing the collimation in- creases the voxel size, improving the signal-to-noise ratio while sacrificing resolution. 1312,16
Patient motion is more difficult to control in dogs than in humans. Patient motion was minimized with the use of an- esthesia and hyperventilation. The patient was hyperventi- lated just before examination initiation to induce apnea for the approximately 30 to 45 seconds needed for the exami- nation. No adverse effects were noted, and all animals re- covered uneventfully except for one dog, which died in the post-operative period after attempted surgical correction of its PSS.
$$Conray 400TM, Mallinkrodt, Inc., St. Louis, MO
Expired CO, was not measured for the client-owned dogs. It was thought that adequate apnea could be induced without relying on measurements of expired CO,. Because breathing motion caused artifacts in 3 of 10 client-owned dogs, and no motion artifacts occurred in the 10 healthy dogs, CO, monitoring may be necessary to achieve CO, levels low enough to induce an adequate period of apnea. Other methods of controlling respiratory motion include the use of paralytic agents (e.g., pancuronium), manually pre- venting breathing by pressure on the rebreathing bag, or the use of a mechanical ventilator.
Spatial resolution is a concern in very small patients. Very small patients require imaging to be of sufficient reso- lution to demonstrate small shunt vessels. The smallest dog successfully imaged in this study weighed 1.8 kg, demon- strating the ability of the technique to accurately image very small dogs. Very large patients forced the use of imaging parameters that sacrificed resolution for examination length. Although most of the dogs with suspected PSS are small breed puppies, one possible routine use of helical CT por- tography may be in the evaluation of large breed puppies with suspected intrahepatic PSS. This study suggests that foreknowledge of the vascular anatomy in these cases may decrease surgical time and dissection. Although patient size could not be controlled, the smallest research dogs available were imaged to assess the ability of helical CT portography to resolve very small vessels.
There was initially some concern over the use of acepro- mazine in the normal dogs. Because acepromazine has the potential to lower the seizure threshold,23 it was suggested that acepromazine may not be a practical choice for dogs with suspected PSS. Acepromazine was chosen as a pre- anesthetic agent in the normal dogs due to its low cost and effectiveness in promoting a level plane of anesthesia. The other concern about acepromazine is its hypotensiveJ vasodilatory effects. The hypotensive effects were minimal as systolic blood pressure was maintained at physiologic levels. The authors do not believe that the vasodilatory ef- fects of acepromazine would enhance or inhibit portal vein visualization. None of the client-owned dogs received acepromazine, and portal vein visualization was excellent. Helical CT portography was successful in all of these cases, demonstrating that acepromazine is not required for visual- ization of the portal vein using helical CT portography. Regardless of specific drugs used in the anesthetic regimen, an adequate depth of anesthesia is required to maintain op- timal imaging conditions.
The proposed advantages of helical CT portography in dogs when compared with other methods used to image the portal venous system are that helical CT portography is non-invasive, provides superb anatomic specificity, and minimizes disparities caused by operator expertise. The re- sults of helical CT portography may also allow the surgeon to decrease surgical time and tissue dissection, with obvious

VOL. 44, No. 4 HELICAL COMPUTED TOMOGRAPHIC PORTOGRAPHY 399
benefits to the patient. In dogs, helcial CT portography can be performed in a relatively short period of time (20-60 min) once operators are familiar with the technique. Disad- vantages of helical CT portography include the cost of the procedure, availability of helical CT equipment, and neces- sity for general anesthesia. We estimate that helical CT portography would cost $400 to $800 in the clinical setting at our facility.
Currently, contrast portography, such as operative mes- enteric portography, splenoportography, or cranial mesen- teric angiography is considered the gold-standard for imag- ing the portal v a s ~ u l a t u r e . ~ ~ Contrast portography has the advantage of not requiring expensive helical CT equip- ment.24-26 Operative mesenteric portography and spleno- portography are also relatively simple to perform and re- quire less time to interpret than helical CT portography. The primary disadvantage of operative mesenteric portography, splenoportography, and cranial mesenteric angiography is that these procedures are invasive.
Transcolonic nuclear scintigraphy is non-invasive, and patients can be imaged without sedation or with sedatives rather than general anesthetics. Although scintigraphy pro- vides reliable data on the presence or absence of a PSS, scintigraphy provides inconsistent anatomic data of poor resolution. Scintigraphy may also not identify shunts from the cranial portion of the portal system (such as the gastric vein to cava shunt commonly seen in cats) caused by over- lap with the liver or lack of colonic blood passing through the shunt. Availability of scintigraphic equipment is also limited.24
Another method to evaluate PSS is gray scale (B-mode) andor Doppler sonography. The advantages of this method are its non-invasiveness and improved anatomic specificity compared with scintigraphy.26 Intrahepatic shunts are more reliably identified than extrahepatic.23 Although sedation andor anesthesia are not required for sonographic evalua- tion, general anesthesia and positive pressure ventilation greatly facilitates the exam.26 The primary disadvantage of ultrasonography is the disparity of accuracy between sonog- rap her^."^^ Magnetic resonance angiography for the diag- nosis of PSS in dogs has shown promise,27 but the lack of availability of this technique makes its widespread use un- likely at this time.
We believe that all dogs suspected of having a PSS may not need helical CT portography. However, helical CT por- tography may be useful in situations where an intrahepatic shunt is suspected, multiple shunts are suspected, or where some factor in the history, physical exam, or other tests is inconsistent with the diagnosis of PSS. Although no patients with confirmed microvascular dysplasia have been exam- ined with helical CT portography to this date, it may be informative to see if these patients have characteristic le- sions on helical CT portography examination. If so, this may be another reason to examine dogs with clinical signs and laboratory findings consistent with PSS but which have a normal scintigraphic or surgical examination.
This project was designed to explore the feasibility of helical CT portography in dogs. We believe that helical CT portography is not only feasible but practical. However, further studies need to be performed to refine the technique and to help establish the indications for helical CT portog- raphy in the clinical setting. Controlled comparisons of the abilities of helical CT portography, Doppler ultrasonogra- phy, non-CT portography, and transcolonic scintigraphy to detect PSS would be useful, as would studies comparing the ability of the various methods to define the vascular anatomy. Studies that compare differing imaging or injec- tion parameters such as recumbency, injection speed, con- trast medium, injection volume, power versus hand injec- tion, slice thickness, pitch, and/or two dimensional versus three dimensional reconstruction may also be useful.
In summary, we believe that this technique of helical CT portography in the dog is a useful adjunct in the diagnosis of PSS. The use of helical CT portography may allow clini- cians to give clients a more accurate prognosis before sur- gery and may allow patients with non-surgically correctable lesions to avoid a costly and invasive procedure. Due to the wide variation in optimal delay times, test injections of contrast medium should be used to determine optimal delay times for each individual patient if possible.
ACKNOWLEDGMENTS
The authors would like to thank Mr. Tim Jarrett for his technical assis- tance on this project.
REFERENCES
1. Ibukuro K, Charnsangavej C, Chase MH, et al. Helical CT angiog- raphy with multiplanar reformation: techniques and clinical applications. Radiographics 1995; 1567 1-682.
2. Freeny PC. Helical computed tomography of the liver: techniques, applications and pitfalls. Endoscopy 1997;29:5 15-523.
3. Chopra S, Ghiatas A, Encarnacion C, et al. Transjugular intrahepatic portosystemic shunts: assessment with helical CT angiography. Rddiokogy 1997;202( 1):277-280.
4. Nghiem HV, Jeffrey RB. CT angiography of the visceral vascula- ture. Semin Ultrasound CT MR. 1998; 19(5):439446.
5. Kanernatsu M, Hoshi H, Imaeda T, Mizuno S, Yokoyama R. Three-
dimensional CT demonstration of intrdhepatic portosysternic venous shunt draining into the inferior vena cava. Brit J Radio1 1997;70:418420.
6. Gryspeerdt S, Van Hoe L, Marchal G, Baert AL. Evaluation of hepatic perfusion disorders with double-phase spiral CT. Radiographics 1997; 17:337-348.
7. Pieters PC, Miller WJ, DeMeo JH. Evaluation of the portal venous system: complementary roles of invasive and noninvasive strategies. Ra- diographics 1997; 17:879-895.
8. Hortan KM, Fishman EK. Paraumbilical vein in the cirrhotic pa- tient: imaging with 3D CT angiography. Abdom Imaging 1998;23:404- 408.

400 FRANK ET AL. 2003
9. Kopka L, Rodenwaldt J, Fischer U, Mueller DW, Oestmann JW, Grahhe E. Dual-phase helical CT of the liver: effects of bolus tracking and different volumes of contrast material. Radiology 1996:201:321-326.
10. Ichikawa T, Peterson MS, Federle MP, et al. Islet cell tumor of the pancreas: biphaaic CT versus MR imaging in tumor detection. Radiology 2000;2 16: 163-1 7 1 .
1 I . Ruppert-Kohlmayr AJ, Uggowitzer MM, Kugler C, Zehedin D, Schaftler G, Ruppert GS. Focal nodular hyperplasia and hepatocellular adenoma of the liver: differentiation with multiphasic helical CT. AJR 200 I ; 1 76: 1493-1 498.
12. Ruhin GD, Dake MD, Semba CP. Current status of three- dimensional spiral CT scanning for imaging the vasculature. Radioil Clin North Am 1995;33(1):51-70.
13. Urban B, McGhie P, Fishman E. Helical CT: diagnostic pitfalls of arterial phase imaging of the upper abdomen. Am J Roentgen01 2000;174: 455a6 I.
14. Winter TC, Nghiem HV, Schmiedl UP, Freeny PC. CT angiography of the visceral vessels. Semin Ultrasound CT MR 1996; 17(4):339-351.
15. Bader TR, Prokesch RW, Grahenwoger MD. Timing of the hepatic arterial phase during contrast-enhanced computed tomography of the liver: assessment of normal values of 26 volunteers. Invest Radiol 2000;35(8): 486-492.
16. Brink JA. Spiral CT angiography of the abdomen and pelvis: inter- ventional applications. Ahdom Imaging 1997;22:365-372.
17. Herts B, Paushter D, Einstein D, Zepp R, Friedman RA, Obu- chowski N. Use of contrast material for spinal CT of the abdomen: com- parison of hepatic enhancement and vascular attenuation for three different contrast media at two different delay times. AJR 1995: 164:327-33 1.
18. Schweiger G, Chang P, Brown B. Optimizing contrast enhancement during helical CT of the liver. AJR 1998;171:1551-1558.
19. Chopra S, Dodd GD, Chintapalli KN, et al. Transjugular intrahe- patic portosystemic shunt: accuracy of helical CT angiography in the de- tection of shunt abnormalities. Radiology 2000;2 15: 1 15-1 22.
20. Chopra S, Chintapalli KN, Dodd GD. Helical CT angiography of transjugular intrahepatic shunts. Semin Ultrasound CT MR 1999;20( 1):26- 35.
21. Johnson PT, Heath DG, Kuszyk BS, Fishman EK. CT angiography with volume rendering: advantages and application in splanchnic vascular imaging. Radiology 1996:200:564-568.
22. Van Hoe L, Marchal G, Baert AL, Gryspeerdt S, Mertens L. De- termination of scan delay time in spiral CT-angiography: utility of a test bolus injection. J Comp Asst Tomography 1995:19(2):216-220.
23. Plumb DC, Veterinary Drug Handbook. Ames, 1A: Iowa State Uni- versity Press, 1999. pp. 1-2.
24. Johnson SE. Chronic hepatic disorders. In: Ettinger SJ, Feldman EC. Textbook of veterinary internal medicine: diseases of the dog and cat. Philadelphia, PA: WB Saunders, 2000. pp. 1298-1 325.
25. Schmidt S, Suter PF. Angiography of the hepatic and portal venous system in the dog and cat: an investigative method. Vet Radiol Ultrasound 1980;21(2):57-77.
26. Moon ML. Diagnostic imaging of portosystemic shunts. Semin Vet Med Surg (Small Anim) 1990;5(2):120-126.
27. Seguin B, Tobias KM, Gavin PR, Tucker RL. Use of magnetic resonance angiography for diagnosis of portosystemic shunts in dogs. Vet Radiol Ultrasound 1999;40(3):25 1-258.