Head & Neck Cancer Clinical Guidelines - NECN...
-
Upload
nguyenthuan -
Category
Documents
-
view
243 -
download
3
Transcript of Head & Neck Cancer Clinical Guidelines - NECN...

1
Head & Neck Cancer Clinical Guidelines
Head & Neck NSSG on behalf of NECN
Document Information
Title: NECN Head and Neck Cancer Clinical Guidelines
Author: Head and Neck NSSG Members
Circulation List: See page 2
Contact Details: Dr E Aynsley, Head and Neck NSSG Chair
Telephone: 011382 52976
Version History:
Date: 10.06.15 Version: V5.3 Review Date: May 2016
Document Control
Version Date Summary Review Date
V5.3 10.06.15 Patient pathway and 2ww referral added May 2016
V5.2 26.05.15 Oral surgery, sarcoma, salivary gland updated
May 2016
V5.1 21.05.15 Document reviewed and updated Chairs detail input.
May 2016
V 5 21.08.14 Chemotherapy update May 2015
V4.9 17.12.13 Updated primary care referral guidelines May 2014

2
Guidelines agreed by: Position: Head and Neck NSSG Chair Name: Dr E Aynsley, Organisation: South Tees NHS FT Date Agreed: 09.06.15 Position: Head and Neck NSSG ViceChair Name: Dr S Endersby Organisation: City Hospital Sunderland NHS FT Date Agreed: 17.06.15 Position: Medical Director Name: Dr M Prentice Organisation: NHS England in Cumbria and the North East Date Agreed: 17.06.15 Position: CYPCG Chair for: 14-1C-111i Pathway Pathways UAT Cancer Name: Liz Rogerson, Assistant Director of Specialised Commissioning Organisation: NHS England in Cumbria and the North East Date Agreed 17.06.15 NSSG members agreed the Guidelines on: Date Agreed: 09.06.15 Review Date: May 2016

3
CONTENTS
The Network have adopted the National Guidelines which can be located via the link below; .......................................................................................................................... 7
CONSULTATIONS ....................................................................................................... 7
CARCINOMA OF THE PHARYNX ............................................................................... 8
Anatomic Description of Site ............................................................................................ 9
Generic MDT Workup In The Pharynx ............................................................................ 10 Clinical Staging ............................................................................................................................................ 10 Imaging ......................................................................................................................................................... 10
NASOPHARYNX ........................................................................................................ 11
Anatomic Description of Site .......................................................................................... 11
Tumour Type Pathology – squamous and other ............................................................ 11
Tumour Staging UICC 6 ................................................................................................... 11
Regional Lymph Nodes Nasopharynx ............................................................................ 12
Stage Grouping: Nasopharynx ........................................................................................ 13
Additional Pre MDT Workup ............................................................................................ 13
Specifics of Treatment:.................................................................................................... 14 Radiotherapy ................................................................................................................................................ 14 Chemotherapy ............................................................................................................................................. 14 Follow-Up Schedule and Post Treatment Investigations ....................................................................... 14
Management of Recurrent Disease/Salvage .................................................................. 14
OROPHARYNX .......................................................................................................... 15
Anatomic Description of Site .......................................................................................... 15
Tumour type pathology – squamous and other ............................................................. 15
Tumour Staging ............................................................................................................... 15
Additional Pre MDT Workup Oropharynx ....................................................................... 16
Dental Assessment .......................................................................................................... 16
Treatment Modality Options In Early/Late Disease ........................................................ 16 Early (Stage I and II) ................................................................................................................................... 16 Patients with early oropharyngeal disease .............................................................................................. 16 Late (Stage III and IV) ................................................................................................................................. 16 Patients with advanced oropharyngeal disease ..................................................................................... 16
Primary Surgery ............................................................................................................... 17
Organ Preservation .......................................................................................................... 17
Specifics of Treatment:.................................................................................................... 17 Surgery .......................................................................................................................................................... 17 Radiotherapy ................................................................................................................................................ 18 Chemotherapy ............................................................................................................................................. 18 Follow-up schedule and post treatment investigations .......................................................................... 18
Management of Recurrent Disease/Salvage .................................................................. 18

4
HYPOPHARYNX ........................................................................................................ 19
Anatomic Description of Site .......................................................................................... 19
Tumour type pathology – squamous and other ............................................................. 19
Tumour Staging ............................................................................................................... 19 Primary Tumour (T) UICC 6 ....................................................................................................................... 19
Stage Grouping ................................................................................................................ 19
Additional Pre MDT Workup ............................................................................................ 19
Management of Neck ....................................................................................................... 20
Specifics Of Treatment: ................................................................................................... 21 Early Disease ............................................................................................................................................... 21 Surgery .......................................................................................................................................................... 21 Advanced disease ....................................................................................................................................... 21 Resection and reconstruction .................................................................................................................... 22 Palliation ....................................................................................................................................................... 22 Radiotherapy ................................................................................................................................................ 22 Chemotherapy ............................................................................................................................................. 22
Follow-Up Schedule and Post Treatment Investigations .............................................. 23
Management of Recurrent Disease/Salvage .................................................................. 23
CARCINOMA OF THE LARYNX ................................................................................ 24
Site .................................................................................................................................... 24
Subsites ............................................................................................................................ 24 Glottis ............................................................................................................................................................ 24 Supraglottis ................................................................................................................................................... 24 Subglottis ...................................................................................................................................................... 24 Regional Lymph Nodes. ............................................................................................................................. 24
Glottis ............................................................................................................................... 24
Anatomic Description of Site .......................................................................................... 24
Tumour Type Pathology – squamous and other ............................................................ 24
Tumour Staging UICC 6 ................................................................................................... 24
Additional Pre MDT Workup ............................................................................................ 25
Early Laryngeal Cancer ................................................................................................... 25
Advanced Glottic Cancer ................................................................................................. 26
Management of the Neck in Glottic Cancer .................................................................... 27
Specifics of Treatment:.................................................................................................... 27 Surgery .......................................................................................................................................................... 27 Radiotherapy ................................................................................................................................................ 28 Chemotherapy ............................................................................................................................................. 28
Follow-Up Schedule and Post Treatment Investigations .............................................. 28
Management of Recurrent Disease/Salvage .................................................................. 29
Supraglottis ...................................................................................................................... 29
Anatomic Description of Site .......................................................................................... 29
Stage Summary ................................................................................................................ 30

5
Additional Pre MDT workup ............................................................................................ 30
Early Supraglottic Tumours – T1-2 ................................................................................. 30
Advanced Supraglottic Tumours – T3-4 ......................................................................... 30
Management of the Neck in Supraglottic Cancer .......................................................... 31
Specifics of Treatment:.................................................................................................... 31 Surgery ........................................................................................................................................................ 31 Radiotherapy .............................................................................................................................................. 31 Chemotherapy ............................................................................................................................................ 31
Follow-up schedule and post treatment investigations ................................................ 31
Management of recurrent disease/salvage .................................................................... 32
Subglottis ......................................................................................................................... 32
Anatomic Description of Site .......................................................................................... 32
Tumour type pathology ................................................................................................... 32
Tumour Staging UICC6 .................................................................................................... 32
Stage Summary ................................................................................................................ 32
Additional Pre MDT Workup ............................................................................................ 32
Management of the Neck in Subglottic Cancer .............................................................. 32
Specifics of Treatment:.................................................................................................... 33 Surgery .......................................................................................................................................................... 33 Radiotherapy ................................................................................................................................................ 33 Chemotherapy ............................................................................................................................................. 33
Follow-Up Schedule and Post Treatment Investigations .............................................. 33
Management of Recurrent Disease/Salvage .................................................................. 33
CARCINOMA OF THE ORAL CAVITY and LIP ........................................................ 33
TNM Classification: UICC VERSION 7 ............................................................................ 33
Lip and Oral Cavity .......................................................................................................... 33
Anatomical Sites and Subsites ....................................................................................... 34
Anatomy ........................................................................................................................... 34
Rules for Classification ................................................................................................... 36 Clinical Staging .......................................................................................................................................... 36
Definition of TNM ............................................................................................................. 36
Confirmation of Diagnosis .............................................................................................. 36 Examination and biopsy .......................................................................................................................... 37 Additional imaging .................................................................................................................................... 37
Definitive Treatment ......................................................................................................... 37 Treatment of Primary Tumour ................................................................................................................ 37 Recurrence .................................................................................................................................................. 39
HEAD AND NECK SARCOMA .................................................................................. 39
MDT Management ............................................................................................................ 39
Summary .......................................................................................................................... 40

6
SALIVARY GLANDS.................................................................................................. 41
Characterisation ............................................................................................................... 41
Confirmation of Diagnosis .............................................................................................. 42
Submandibular Gland ...................................................................................................... 42 Surgery......................................................................................................................................................... 42 Radiotherapy .............................................................................................................................................. 43 Palliation ...................................................................................................................................................... 43
Parotid Gland ................................................................................................................... 43 Surgery......................................................................................................................................................... 43 Radiotherapy .............................................................................................................................................. 43 Post-operative ............................................................................................................................................ 43 Recurrent Disease ..................................................................................................................................... 44
Minor Salivary Glands ..................................................................................................... 44 Confirmation of diagnosis ...................................................................................................................... 44 Treatment .................................................................................................................................................... 44 Neck .............................................................................................................................................................. 44 Radiotherapy Indications: ....................................................................................................................... 44
CONTACTS ................................................................................................................ 44
The Policy and the Named Hospitals for Head and Neck Cancer ................................. 44
The Distribution of Neck Lump Clinics ........................................................................... 45
Referral Guidelines for Primary Care Practitioners - UAT Patients .............................. 46
Distribution Process for Referral Guidelines ................................................................. 48
Network Agreed Referral Proformas ............................................................................... 48
Internal Referral Guidelines for Non-Designated Hospital Clinicians .......................... 48
Network Agreed Named Hospital for Surgical Treatment Delivery ............................... 49
Network MDT Configuration ............................................................................................ 49
Trust .................................................................................................................................. 49
MDT linkages .................................................................................................................... 50
Trust .................................................................................................................................. 50
The Distribution of Local Support Teams in the Network ............................................. 50
Appendix 1 - Referral Guidelines for Primary Care ............................................... 51
Referral Guidelines for Primary Care Practitioners - UAT Patients ...................... 52
Appendix 2 - NSSG Guidelines for Teenage and Young Adults ........................... 60
Appendix 3– Teenage and Young Adult Pathway for initial Management ........... 61
Appendix 4 – Contact Details .................................................................................. 62
Appendix 5 – NHS Specialised Services Pathway ................................................. 63
Appendix 6 - Imaging Guidelines ............................................................................ 65
Appendix 7- Chemotherapy Protocols .................................................................... 89

7
The Network have adopted the National Guidelines which can be located via the link below; Head and Neck National Guidelines CONSULTATIONS All patients with a diagnosis of head and neck cancer must be seen in a multidisciplinary team meeting to allow adequate discussion of the case and appropriate decision-making. Team members should include:
Oncologist specialising in head & neck cancer
Appropriately trained head & neck surgeons with skills encompassing ablation and reconstruction including free tissue transfer
Specialist head and neck nurse
Additionally prosthetic support may be required both peri-operatively and in the
post operative phase: for example obturation of surgical defects. An appropriately equipped and staffed oral & maxillofacial laboratory is required to support this aspect of care
Speech and language therapists for pre-operative counselling regarding possible
post-operative speech and swallowing rehabilitation. To assess in conjunction with dietician the nutritional status and need for percutaneous gastrostomy (PEG) or radiographically inserted gastrostomy, (RIG).
Specialist anaesthetic assessment may be needed to evaluate co-morbidities that
could preclude or increase the risk of general anaesthesia.
Smoking and alcohol cessation advisors
Data collation officer; Demographic and patient journey information, regarding the cancer care spell and follow up should be collected prospectively in an appropriate electronic database.
Diagnosis and assessment services outside the MDT are required to produce sufficient information to merit referral to the MDT. Following which, the MDT will undertake further investigations as appropriate in order to produce a definitive treatment plan as per protocol. It is undesirable for investigations to proceed outside the MDT once a cancer diagnosis is reached. All nebulous neck lumps will be referred to the MDT for discussion.

8
Patient pathway

9
CARCINOMA OF THE PHARYNX MAIN AUTHOR: Richard Wight PHARYNX The division of the pharynx is summarized in the following table (including base of tongue, soft palate and uvula) (Non-epithelial tumours such as those of lymphoid tissue, soft tissue, bone, and cartilage are not included.)
Oropharynx Nasopharynx Hypopharnx
C01.9 Base of tongue, NOS
C11.0 Superior wall of nasopharynx
C13.0 Postcricoid region
C02.4 Lingual tonsil C11.1 Posterior wall of nasopharynx
C13.1 Hypopharyngeal aspect of aryepicglottic fold
C05.1 Soft palate, NOS C11.2 Lateral wall of nasopharynx
C13.2 Posterior wall of hypopharynx
C05.2 Uvula C11.3 Anterior wall of nasopharynx
C13.8 Overlapping lesion
C09.0 Tonsillar fossa C11.8 Overlapping lesion C13.9 Hypopharynx, NOS
C09.1 Tonsillar pillar
C11.9 Nasopharynx, NOS
C14.0 Pharynx, NOS
C09.9 Tonsil, NOS C14.1 Laryngopharynx
C09.8 Overlapping lesion C12.9 Pyriform sinus
C14.2 Waldeyer’s ring C14.8 Overlapping lesion of lip, oral cavity and pharynx
C10.0 Vallecula
C10.2 Lateral wall of oropharynx
C10.4 Branchial cleft
C10.8 Overlapping lesion
C10.9 Oropharynx, NOS
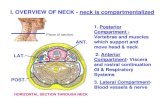
Anatomic Description of Site
Primary Sites and Sub-sites. The pharynx (including base of tongue, soft palate, and uvula) is divided into three regions: nasopharynx, oropharynx and hypopharynx. Each region is further subdivided into specific sites as summarized above. Regional Lymph Nodes. The risk of regional nodal spread from cancers of the pharynx is high. Primary nasopharyngeal tumours commonly spread to retropharyngeal, upper jugular, and spinal accessory nodes, often bilaterally. Oropharyngeal cancers involve upper and mid-jugular lymph nodes, less likely submental / submandibular nodes.

10
Hypopharyngeal cancers spread to adjacent parapharyngeal, paratracheal and midand lower jugular nodes. Bilateral lymphatic drainage is common. Metastatic Sites. The lungs are the commonest sites of distant metastases; skeletal or hepatic metastases occur less often. Mediastinal lymph node metastases are considered distant metastases. Generic MDT Workup In The Pharynx
All patients should have a chest imaging at presentation. Clinical Staging Clinical staging is employed for squamous cell carcinomas of the pharynx. Assessment is based primarily on inspection, and by indirect and direct endoscopy. Palpation of sites (when feasible) and of neck nodes is essential. Neurologic evaluation of all cranial nerves is required. Imaging studies are essential in clinical staging of pharynx tumours. Imaging Cross-sectional imaging in nasopharyngeal cancer is mandatory to complete the staging process. Computed tomography (CT) staging with axial and coronal thin section technique with contrast is the study of choice. Magnetic resonance imaging (MRI) can provide supplementary information because of its multiplanar capability, superior soft tissue contrast and its sensitivity to skull base and intracranial tumour spread. Radiologic nodal staging should be done to assess adequately the retropharyngeal and cervical nodal status. Cross-sectional imaging in oropharyngeal carcinoma is recommended when the deep tissue extent of the primary tumour is in question. CT (or MRI) may be employed. Radiologic nodal staging should also be done simultaneously. Cross-sectional imaging of hypopharyngeal carcinoma is recommended when the extent of the primary tumour is in doubt, particularly its deep extent in relationship to adjacent structures (i.e., larynx, thyroid, cervical vertebrae, and carotid sheath). CT is preferred currently because of less motion artifact than MRI. Radiologic nodal staging should be done simultaneously. PET is an emerging technology that may have a role in uncertain disease extent. The Network is gaining increased access to the modality and will continue to define its appropriate usage. Pathologic Staging Pathologic staging requires the use of all information obtained in clinical staging in addition to histological study of the surgically resected specimen. The surgeon’s evaluation of gross unresected residual tumour must also be included. The pathologic description of any lymphadenectomy specimen should describe the size, number and level of any involved nodes.

11
The general pathology services are required to provide a diagnosis sufficient to merit referral to the MDT. The MDT pathology service will produce further reports as referred to in the pathology protocol. NASOPHARYNX Anatomic Description of Site
The nasopharynx begins anteriorly at the posterior choana and extends along the plane of the airway to the level of the free border of the soft palate. It includes the vault, the lateral walls including the fossae of Rosenmuller and the mucosa covering the torus tubaris forming the eustachian tube orifice, and the posterior wall. The floor is the superior surface of the soft palate. The posterior margins of the choanal orifices and of the nasal septum are included in the nasal fossa. Parapharyngeal involvement denotes postero-lateral infiltration of tumour beyond the pharyngobasilar fascia. Involvement of the masticator space denotes extension of tumour beyond the anterior surface of the lateral pterygoid muscle, or lateral extension beyond the postero-lateral wall of the maxillary antrum, pterygo-maxillary fissure. Tumour Type Pathology – squamous and other (excludes salivary and thyroid) The predominant cancer type is squamous cell carcinoma for all pharyngeal sites. Nonepithelial tumours such as those of lymphoid tissue, soft tissue, bone and cartilage are not included in this system. For nasopharyngeal carcinomas it is recommended that the World Health Organization (WHO) Classification is used (Table 1). Histologic diagnosis is required to use this classification. Table 1. Classification of Nasopharyngeal Carcinoma WHO Classification
Former Terminology
Type 1. Squamous cell carcinoma Squamous cell carcinoma Type 2. Non-keratinizing carcinoma Transitional cell carcinoma
without lymphoid stroma Intermediate cell carcinoma with lymphoid Lymphoepithelial cell carcinoma (Regaud)
Type 3. Undifferentiated carcinoma -without lymphoid stroma
Anaplastic carcinoma, clear cell carcinoma
-with lymphoid stroma Lymphoepithelial carcinoma (Schminke)
Tumour Staging UICC 6
Primary Tumour (T)

12
TX Primary tumour cannot be assessed T0 No evidence of primary tumour Tis Carcinoma in situ
Nasopharynx
T1 Tumour confined to the nasopharynx T2 Tumour extends to soft tissues T2a Tumour extends to oropharynx +/- nasal cavity without parapharyngeal extension* T2b Any tumour with parapharyngeal extension* T3 Tumour involves bony structures and/or paranasal sinuses T4 Tumour with intracranial extension and/or involvement of cranial nerves, infra-
temporal fossa, hypopharynx, orbit, or masticator space *Note: Parapharyngeal extension denotes posterolateral infiltration of tumour beyond the pharyngobasilar fascia. Regional Lymph Nodes Nasopharynx
The distribution and the prognostic impact of regional lymph node spread from nasopharynx cancer, particularly of the undifferentiated type, is different than that of other head and neck mucosal cancers and justifies use of a different N classification scheme.
NX Regional lymph nodes cannot be assessed N0 No regional lymph node metastasis N1 Unilateral metastasis in lymph node(s). 6 cm or less in greatest dimension, above
the supraclavicular fossa* N2 Bilateral metastasis in lymph node(s), 6 cm or less in greatest dimension, above the
supraclavicular fossa* N3 Metastasis in a lymph node(s) N3a greater than 6 cm in dimension N3b extension to the supraclavicular fossa*
* Midline nodes are considered ipsilateral nodes. Supraclavicular zone or fossa is relevant to the staging of nasopharyngeal carcinoma and is the triangular region originally described by Ho. It is defined by three points: (1) the superior margin of the sternal end of the clavicle; (2) the superior margin of the lateral end of the clavicle; (3) the point where the neck meets the shoulder. Note that this would include caudal portions of Levels IV and V. All cases with lymph nodes (whole or part) in the fossa are considered N3b.

13
Stage Grouping: Nasopharynx
Stage 0 Tis N0
M0
Stage I T1 N0 M0 Stage IIA T2a N0 M0 Stage IIB T1 N1 M0
T2a N1 M0 T2b N0, N1 M0
Stage III T1 N2 M0 T2a, T2b N2 M0 T3 N0, N1, N2 M0
Stage IVA T4 N0, N1, N2 M0 Stage IVB Any T N3 M0 Stage IVC Any T Any N M1 Additional Pre MDT Workup (outside of generic or specific aspects) EBV –specific serologic tests:- IgA anti-viral capsule antigen (VCA) titres. Positive results are principally associated with WHO type 2 and type 3 NPC and more commonly associated with patients of Asian descent. Healthy teeth and surrounding soft tissue are required prior to radiotherapy. Early dental assessment is required with OPG x ray. Treatment to be delivered in hospital or primary dental care setting as appropriate. Treatment modality options in early/late disease in Network and reasons for preference (include EBM references) including multimodality if applicable. Any treatments for referral outside of Network. For management purposes patients are divided into those with type 1 squamous carcinomas (usually well differentiated in the older patient with localised disease at presentation) and those with type 2/3 carcinomas (usually poorly differentiated/ anaplastic in the younger patient presenting with bilateral neck disease). Concurrent chemoradiotherapy is the standard of care using IMRT.

14
Specifics of Treatment:
Radiotherapy See local department radiotherapy and oncology protocols. Chemotherapy See local department radiotherapy and oncology protocols. Follow-Up Schedule and Post Treatment Investigations EBV –specific serologic tests:- IgA anti-viral capsule antigen(VCA) titres. In those with a positive result at presentation (WHO type 2 and type 3 NPC) repeat titres for monitoring recurrence may be considered. Follow up schedule: YEAR 1 4 to 6 weekly YEAR 2 2 monthly YEAR 3 3 to 4 monthly YEAR 4/5 6 monthly YEAR 5 to 10 yearly Management of Recurrent Disease/Salvage
There is limited scope for salvaging patients in this situation, but local surgery may be applicable to nodal disease and chemotherapy may be an option for systemic disease.

15
OROPHARYNX Anatomic Description of Site
Oropharynx The oropharynx is the portion of the continuity of the pharynx extending from the plane of the superior surface of the soft palate to the superior surface of the hyoid bone (or floor of the vallecula) and includes the base of tongue, the inferior surface of the soft palate and the uvula, the anterior and posterior tonsillar pillars, the glossotonsillar sulci, the pharyngeal tonsils; the lateral and posteriors walls. Tumour type pathology – squamous and other (excludes salivary and thyroid) HISTOPATHOLOGIC GRADE (G): Oropharynx, Hypopharynx
GX Grade cannot be assessed G1 Well differentiated G2 Moderately differentiated G3 Poorly differentiated
Tumour Staging
Primary Tumour (T)
TX Primary tumour cannot be assessed T0 No evidence of primary tumour Tis Carcinoma in situ
Oropharynx
T1 Tumour 2cm or less in greatest dimension T2 Tumour more than 2cm but not more than 4cm in greatest dimension T3 Tumour more than 4cm in greatest dimension T4a Tumour invades the larynx, deep/extrinsic muscle of tongue, medial
pterygoid, hard palate, or mandible T4b Tumour invades lateral pterygoid muscle, pterygoid plates, lateral
nasopharynx, skull base, or carotid artery. STAGE GROUPING: Oropharynx, Hypopharynx: Identical to Larynx Stage 0 Tis N0 M0 Stage I T1 N0 M0 Stage II T2 N0 M0 Stage III T1, T2 N1 M0
T3 N0, N1 M0 T1, T2 N1 M0
Stage IVA T1, T2, T3 N1, N2 M0 T4a, N0, N1, N2 M0
Stage IVB T4b Any N M0 Any T N3 M0
Stage IVC Any T Any N M1

16
Additional Pre MDT Workup Oropharynx (outside of generic or specific aspects) Dental Assessment
Healthy teeth and surrounding soft tissue are required prior to radiotherapy. Early dental assessment is required with OPG X-ray. Treatment to be delivered in hospital or primary dental care setting as appropriate. EUA Pan- endoscopy, under general anaesthesia, is performed after completion of other staging studies, to accurately assess the surface extent of the tumour and to assess deep involvement by palpation for muscle resistance and to facilitate biopsy. A careful search for other primary tumours of the upper aero-digestive tract is indicated because of the incidence of multiple independent primary tumours occurring simultaneously. Photographs Photographs of accessible tumours. Treatment Modality Options In Early/Late Disease In the Network and reasons for preference (include EBM references) including multimodality if applicable. Any treatments for referral outside of Network Early (Stage I and II) Management of early oropharyngeal cancer should be individualised for each patient. Decisions regarding primary treatment modality should be made in consultation with the patient and should take into account the anatomical location of the tumour and availability of local expertise. Patients with early oropharyngeal disease may be treated by either primary resection with reconstruction as appropriate +/- neck dissection (selective neck dissection encompassing levels II-IV) or external beam radiotherapy encompassing the primary tumour and first echelon nodes. In well lateralised tumours prophylactic treatment of the ipsilateral neck is considered (contralateral neck left alone). Bilateral treatment of the neck is recommended when the incidence of occult disease in the contralateral neck is high (i.e. base of tongue). Postoperative radiotherapy should be considered for patients with clinical and pathological features that indicate a high risk of recurrence. Late (Stage III and IV) Management of late oropharyngeal cancer should be individualised for each patient. Decisions regarding primary treatment modality should be made in consultation with the patient and should take into account the anatomical location of the tumour and availability of local expertise. In patients where surgical resection is possible, the likelihood of obtaining adequate surgical margins with acceptable morbidity, functional outcome and quality of life must be taken into account. Patients with advanced oropharyngeal disease

17
May be treated by either primary resection (if a clear surgical margin can be obtained) or an organ preservation approach. Primary Surgery
Resection should be followed by reconstruction as appropriate. Transoral resection using either the surgical robot or laser microsurgery is now a recognised option for patients. Patients having surgery who are N+ should have a neck dissection. In well lateralised tumours prophylactic treatment of the ipsilateral neck is considered (contralateral neck left alone). Prophylactic treatment of the contralateral neck should be considered especially when tumours encroach on the midline. PET-CT is an emerging technology that may have a role in uncertain disease extent. The Network is gaining increased access to the modality and will continue to define its appropriate usage. Post-operative radiotherapy to the primary site should be considered for patients with adverse pathological features that indicate a high risk of recurrence (see below). Post-operative chemoradiotherapy is generally offered for positive margins and extracapsular spread. Patients treated with primary laser resection and neck dissection should have post-operative (chemo)radiotherapy to primary site and neck with involved nodes. Organ Preservation
Radiotherapy should be administered with chemotherapy in those with high performance status Patients treated with primary chemoradiotherapy with nodal disease should undergo and PET-CT scan at 12 weeks following completion of therapy, to assess nodal response. Non-normal scans should be discussed at the MDT and the need for neck dissection discussed. We await to results of the PET-Neck study. Specifics of Treatment:
Surgery (procedure specifics) The extensive nature of the surgery requires two surgical teams. Tonsil/Posterior pharyngeal wall For early disease trans oral laser surgery is an appropriate treatment option. For late disease, to ensure adequate exposure of the tumour ipsilateral paramedian mandibulotomy is generally the most effective and when carried out in the most appropriate site results in little morbidity. Flap reconstruction Soft palate Tumours in this area tend to appear on the free edge of the soft palate or uvula, are predominantly T1 or T2 at presentation, and can be treated effectively by either endoscopic

18
resection, with or without the CO2 laser, or by radical radiotherapy. If they are larger and radical resection is employed effective, functional reconstruction is a challenge and frequently results in significant morbidity. Base of tongue Transoral techniques are possible and the surgical robot has advanced conservative resection for this site. Due to its high morbidity total glossectomy combined with total laryngectomy is usually only applicable if other treatment avenues have been exhausted e.g. if there is recurrence in an otherwise fit and highly motivated patient. Adverse pathological features indicating post operative therapy should be considered:- - advanced T stage -close or positive surgical margins -perineural invasion -lymphovascular invasion -any positive lymph nodes, but especially if > 1 -positive nodes at level Iv or V -any node > 3 cm -extracapsular lymph node spread Radiotherapy See local department radiotherapy and oncology protocols Chemotherapy See local department radiotherapy and oncology protocols Follow-up schedule and post treatment investigations YEAR 1 4 to 6 weekly YEAR 2 2 monthly YEAR 3 3 to 4 monthly YEAR 4/5 6 monthly YEAR 5 to 10 yearly Management of Recurrent Disease/Salvage
In general, surgery is used for recurrent disease if it is resectable. Post-operative radiotherapy is used if it has not been given before. Chemotherapy may have a palliative role.

19
HYPOPHARYNX Anatomic Description of Site
The hypopharynx is that portion of the pharynx extending from the plane of the superior border of hyoid bone (or floor of vallecula) to a plane corresponding to the lower border of cricoid cartilage and includes pyriform fossae (right and left), lateral and posterior hypopharyngeal walls, and postcricoid region. Post cricoid area extends from the level of the arytenoid cartilages and connecting folds to the inferior border of cricoid cartilage and connects the two pyriform sinuses thus forming the anterior wall of the hypopharynx. The pyriform sinus extends from the pharyngoepiglottic fold to the upper end of the oesophagus at the lower border of cricoid cartilage and is bounded laterally by the lateral pharyngeal wall and medially by the lateral surface of the aryepicglottic fold, arytenoid and cricoid cartilages. The posterior pharyngeal wall extends from the level of the superior surface of the hyoid bone (or floor of the vallecula) to the inferior border of cricoid cartilage and from the apex of one pyriform sinus to the other. Tumour type pathology – squamous and other (excludes salivary and thyroid) Most are squamous carcinomas, and may include high-grade basaloid variants which have a poorer prognosis. Rarely sarcomas can arise. Tumour Staging
Primary Tumour (T) UICC 6
TX Primary tumour cannot be assessed T0 No evidence of primary tumour Tis Carcinoma in situ T1 Tumour limited to one subsite of hypopharynx and 2 cm or less in greatest
dimension T2 Tumour invades more than one subsite of hypopharynx or an adjacent site, or
measures >2 cm but < 4 cm in greatest diameter without fixation of hemilarynx T3 Tumour measures > than 4 cm in greatest dimension or with fixation of
hemilarynx T4a Tumour invades thyroid/cricoid cartilage, hyoid bone, thyroid gland,
oesophagus or central compartment soft tissue* T4b Tumour invades prevertebral fascia, encases carotid artery, or invades
mediastinal structures. *Note: Central compartment soft tissue includes prelaryngeal strap muscles and subcutaneous fat. Stage Grouping - see oropharynx above Additional Pre MDT Workup (outside of generic aspects)

20
Nutritional status - is frequently impaired in hypopharyngeal lesions and early nutritional assessment and dietetic advice is essential at the earliest opportunity Alcohol counselling - High levels of alcohol consumption are frequently found in association with hypopharyngeal carcinoma, and appropriate support should be instigated early in the care pathway. Pan-endoscopy - under general anaesthesia, is performed after completion of other staging studies, to accurately assess the surface extent of the tumour and to assess deep involvement into prevertebral muscles and to facilitate biopsy. Synchronous primaries may be found within the oesophagus and UADT, as well as submucosal spread a significant distance from the primary. Pan-endoscopy should include tracheoscopy for post cricoid/upper oesophageal lesions to exclude direct tracheal invasion. Apart from CT (see imaging) of the primary, neck and mediastinum, additional information may be provided by barium swallow, to assess distal extent. Pulmonary function tests are required for all patients considered for surgery Treatment modality options in early/late disease in Network and reasons for preference (include EBM references) including multimodality if applicable. Any treatments for referral outside of Network Management of Neck
Approximately 2/3 of patients are N+ at presentation. Occult metastases are found in about 40% of neck dissections for N0 staged disease. Pathological studies show spread in the N0 neck occurs to levels II-IV and rarely to levels I or V (25-27). Spread is bilateral in midline or bilateral tumours. Level VI involvement may occur in apical pyriform fossa or post-cricoid tumours. N0 Neck There is very little good randomised control trial or even retrospective evidence on how to manage the node negative neck most effectively. If a patient is having primary radiotherapy then first echelon nodes can be covered with the radiotherapy field. If surgical treatment is used then selective neck dissection of levels II, III, IV as a minimum is recommended, with the inclusion of level VI in those tumours that extend to the postcricoid region or apex of the pyriform fossa. If there is oropharyngeal extension then level I should be included. Bilateral dissection is required for central tumours. N1-3 Neck Comprehensive neck dissection has been the accepted standard for the N+ staged neck. The pattern of invasion of the nodes will dictate whether radical or modified radical dissection is required. This would usually mean a modified radical (functional) dissection for N1-2 disease. Pathological studies suggest that selective neck dissection of levels II - IV may be adequate for N1 disease. Although its use is controversial, there is some comparative

21
evidence of its clinical effectiveness. The available evidence on functional and quality of life outcomes suggests that selective neck dissection is superior to comprehensive dissection. Specifics Of Treatment:
Treatment planning takes the patient’s physical and mental state and wishes into consideration and recommendations may be modified according to individual circumstances. Early Disease T1 and T2 tumours are very infrequent. Single modality treatment of the primary tumour by partial pharyngolaryngectomy, radiotherapy or endoscopic resection has been reported but there is insufficient evidence to distinguish between them on the basis of local control or survival. There is a consensus that optimal treatment for all except the earliest stage tumours is combined surgery and radiotherapy, although there is little in the way of evidence. The validity of survival as a parameter to compare the effectiveness of primary treatment is hindered by the high incidence of regional and distant metastases. Local control appears to be improved by combined surgery and radiotherapy according to the little comparative data that are available. This may improve quality of survival but more data on functional outcomes of treatment is needed. Surgery T1 and T2 Conservation surgical techniques are preferable in early stage disease if feasible. Precise treatment depends on the site of the tumour. Some tumours (limited tumours upper piriform fossa and posterior pharyngeal wall) may be suitable for endoscopic resection and may offer the best functional results and lowest morbidity. The use of different modalities to treat the primary tumour and cervical nodes is appropriate in some circumstances. Resection should be wide enough to provide clear margins because positive margins are a poor prognostic factor. Submucosal tumour spread is more extensive in piriform sinus carcinoma (c.10mm) than postcricoid carcinoma (c.5mm). There appears to be a worse survival if the piriform sinus apex is involved and if disease is bulky. Radiotherapy appears to be less effective in such circumstances. Advanced disease T3-4 tumours are likely to be optimally controlled by combining radical surgery with post-operative radiotherapy. The nature of the surgery depends on the site and extent of the tumour. Some advanced tumours may be suitable for more extensive conservation or endoscopic surgery but most require total laryngectomy with partial pharyngectomy or total pharyngolaryngectomy. Studies concerning conservation surgery (near total laryngectomy and supracricoid hemilaryngopharngectomy) have reported highly selected cases but good functional results in terms of voice function have been described. Concurrent chemoradiotherapy is a very reasonable treatment for patients with a functioning larynx and serviceable swallow. There is little evidence to show a survival advantage with radical surgery over CRT – as survival is so poor generally. If a patient does not have a functioning organ, then CRT would be unwise as function would not be restored after therapy, even with a good disease response.

22
Resection and reconstruction It is difficult to be dogmatic about individual techniques in the absence of good quality data on functional outcomes. Partial pharyngectomy with or without partial laryngectomy may be used for more advanced tumours. Reconstructive options range from none (small posterior wall defects) through primary closure to flaps. Radial forearm, myofascial, myocutaneous and jejunal patch flaps have all been successfully used to reconstruct partial pharyngectomy defects. Reconstruction of total pharyngolaryngectomy by single stage techniques is the accepted standard. Free jejunal transfer is the technique that is best supported by the literature but tubed free radial forearm free flaps are an appropriate alternative with less donor site morbidity. Anterolateral thigh flaps are becoming more common. More extensive defects involving the oesophagus may require gastric transposition. Palliation Approximately one third of patients are incurable at presentation. The specialist palliative care team should be involved as early as possible in the disease process. Pain can be controlled and local protocols should be followed. Percutaneous endoscopic gastrostomies (PEGs) placed early can help maintain nutrition in an acceptable manner, though some will require open gastrostomies. Radiotherapy Primary radiotherapy with salvage surgery, although only effective in a small number of patients, is a recognised treatment in the UK. Primary radiotherapy is an appropriate treatment for small hypopharyngeal tumours. It is also indicated in those patients who are medically unfit for surgery and can obviate the need for pharyngo-laryngectomy in some circumstances. Whilst primary radiotherapy for advanced tumours does not produce as good survival figures as radical surgery, the quality of studies is impaired by selection bias in favour of surgery for fitter patients. See local department radiotherapy and oncology protocols Chemotherapy See local department radiotherapy and oncology protocols Adverse pathological features indicating post operative therapy should be considered:- - advanced T stage -close or positive surgical margins -perineural invasion -lymphovascular invasion -any positive lymph nodes, but especially if 2 or greater -any node > 3 cm -extracpasular lymph node spread

23
Follow-Up Schedule and Post Treatment Investigations
Therapeutic intervention frequently involves the thyroid and thyroid function tests should be considered for monitoring for both early and late thyroid failure. If all parathyroids have been removed calcium replacement therapy is required. YEAR 1 4 to 6 weekly YEAR 2 2 monthly YEAR 3 3 to 4 monthly YEAR 4/5 6 monthly YEAR 5 to 10 yearly
In lesions involving the postcricoid region, oesophagoscopy to be performed within 3 months of completion of radiotherapy. Neck imaging based on clinical findings. Management of Recurrent Disease/Salvage
In general, surgery is used for recurrent disease if it is resectable. Post-operative radiotherapy is used if it has not been given before. Chemotherapy may have a palliative role.

24
CARCINOMA OF THE LARYNX The division of the larynx is summarized in the following table: Site Subsites
Glottis True vocal cords including anterior and posterior commissures Supraglottis Suprahyoid epiglottis
Infrahyoid epiglottis Aryepicglottic folds (laryngeal aspect) Arytenoids Ventricular bands (false cords)
Subglottis Subglottis Regional Lymph Nodes. Incidence and distribution of cervical nodal metastases from larynx cancer varies with site of origin and the “T” category of the primary. The true cords are nearly devoid of lymphatics and rarely spread to regional nodes. The supraglottis has a rich and bilaterally interconnected lymphatic network and primary supraglottic cancers are commonly accompanied by regional lymph node spread. Glottic tumours may spread directly to adjacent soft tissue and prelaryngeal, pretracheal, paralaryngeal and paratracheal nodes as well as upper, mid and lower jugular nodes. Supraglottic tumours spread to upper/midjugular nodes, considerably less commonly to submental/submandibular nodes, but occasionally to retropharyngeal nodes. Glottis
Anatomic Description of Site
The glottis is composed of the true vocal cords, including the anterior and posterior commissures, superior and inferior surfaces of cords. It occupies a horizontal plane 1cm in thickness, extending inferiorly from the lateral margin of the ventricle. Tumour Type Pathology – squamous and other
The predominant cancer is squamous cell carcinoma. The staging guidelines are applicable to all forms of carcinoma. A number of variants of squamous carcinoma are found including –verrucous, basaloid sqaumous, sarcomatoid (spindle cell), as well as neuroendocrine carcinoma. Cartilage tumours and plasmacytomas can also rarely arise. Tumour Staging UICC 6
Glottis
Tis Carcinoma in situ T1 Tumour limited to the vocal cord(s) (may involve anterior or posterior
commissure with normal mobility. T1a Tumour limited to one vocal cord T1b Tumour involves both vocal cords T2 Tumour extends to supraglottis and/or subglottis, and/or with impaired vocal
cord mobility. T3 Tumour limited to the larynx with vocal cord fixation, and/or invades paraglottic
space, and or minor thyroid cartilage erosion (e.g. inner cortex).

25
T4a Tumour invades through the thyroid cartilage and/or invades tissues beyond the larynx (e.g., trachea, soft tissues of neck including deep extrinsic muscle of the tongue, strap muscles, thyroid or esophagus)
T4b Tumour invades prevertebral space or encases carotid artery or invades mediastinal structures
Stage 0 Tis N0 M0 Stage I T1 N0 M0 Stage II T2 N0 M0 Stage III T1, T2 N1 M0
T3 N0, N1 M0 T1, T2 N1 M0
Stage IVA T1, T2, T3 N2 M0 T4a, N0, N1, N2 M0
Stage IVB T4b Any N M0 Any T N3 M0
Stage IVC Any T Any N M1 Additional Pre MDT Workup (outside of generic or specific aspects) All patients should undergo a panendoscopy and biopsy, CXR, CT scan of larynx, neck and thorax (for T2 and above) as well as comorbidity scoring. Patients being considered for laryngeal surgery should have pulmonary function tests. Where possible, imaging of the larynx should occur. Treatment modality options in early/late disease in Network and reasons for preference (include EBM references) including multimodality if applicable. Any treatments for referral outside of Network. Early Laryngeal Cancer
The Network is currently contributing to the Easter Feasibility Trial. Tis: Evidence suggests carcinoma-in-situ can be reversible with cessation of smoking, and smoking cessation advice supports treatment Excision biopsy is the treatment of choice although excellent control rates can be achieved with both endolaryngeal microsurgery and radiotherapy. Excision with preservation of the vocal ligament if possible is probably the best option; if not then an initial biopsy followed by definitive treatment is indicated. Close follow-up where possible by the same treatment team is important. T1a – T1a: A large amount of literature, almost exclusively case series, reports that radiotherapy or endoscopic laser resection offer comparable local control rates for accessible lesions. Patient choice should be the main determinant. There is an unproven but widespread opinion that radiotherapy may offer better voice outcomes for all but mid-cord lesions..

26
Where access for endolaryngeal laser surgery is restricted radiotherapy is the treatment of choice. T1b: Treatment options here are the same as T1a (Radiotherapy, Laser surgery and Partial laryngectomy). In the UK radiotherapy remains the overall treatment of choice. Involvement of the anterior commissure in some series correlates with poorer outcome for both radiotherapy and laser therapy. This may however relate to under-staging of the disease at diagnosis. For partial laryngectomy, excellent oncological results can be obtained, but voice is likely to worse than radiotherapy. The literature supports the belief that continued smoking and alcohol consumption during and after radiotherapy worsens the outcome in terms of local control. T2: Superficial tumours without restricted cord mobility (T2a) can be treated by radiotherapy or surgery. Radiotherapy is preferable for extensive superficial tumours because of better functional results. Tumours impairing cord movement (T2b) are treated with radiotherapy (possibly considering the addition of chemotherapy) or partial laryngectomy. One recent paper reports high local control rates (93.8-95.7%) in patients undergoing induction chemotherapy and partial laryngectomy for T2 glottic carcinoma. In the absence of randomised controlled trial evidence however the impact of combined versus single modality therapy in early glottic cancer remains unclear. Advanced Glottic Cancer
T3: Large variations in tumour volume affect treatment outcome in similarly staged tumours. Treatment needs to be individualised, and volume determined based on clinical and CT findings. Bulky disease is treated surgically, while low volume disease is treated primarily with chemoradiotherapy It may be that some T3 tumours are under-staged and are really T4 due to unsuspected cartilage invasion. Treatment options are surgery or radiotherapy or combined therapy. Partial laryngectomy may be suitable for small volume tumours while radiotherapy may be the preferred option for medically unfit patients and can give better voice outcomes. Combined chemoradiotherapy gives superior survival outcomes to radiotherapy alone. In patients unfit for CRT, serious consideration should be given to surgery. A review of prognostic factors in T3 laryngeal cancers concluded that glottic lesions, female patients and N0 disease did better with primary radiotherapy and salvage surgery while patients with pre-operative tracheostomy or N+ disease did better with primary surgery. As the role of chemotherapy is changing, in otherwise fit patients with advanced disease (T3 or T4/N2+) undergoing radical radiotherapy concurrent chemotherapy is offered. T4: Primary surgery with post-operative radiotherapy is the treatment of choice since authors report higher disease-free survival compared with primary radiotherapy. Patients who are not fit for or refuse surgery may be candidates for radiotherapy. In those who are fit see above re concurrent chemotherapy.

27
A randomised controlled trial of alternating chemo-radiotherapy compared with radiotherapy alone in patients with advanced inoperable head and neck cancer (including laryngeal) reported higher disease free and overall survival in the combined treatment group. Management of the Neck in Glottic Cancer
N0 In early glottic cancer (T1-T2), there should be no need for elective neck treatment as the risk for occult neck metastases is low. There is no Level I or II evidence that elective treatment of the N0 neck in laryngeal cancer improves survival. Elective treatment of the neck inevitably carries some morbidity. Elective neck irradiation is as effective as elective neck dissection. With advanced glottic cancer (T3-T4) and transglottic, cancer there is at the present time a consensus that the neck needs to be treated electively. Treatment of the primary site will determine how the neck is treated. If the primary site is treated with radiotherapy then elective neck radiation via a wider treatment field should be performed. If the primary site is treated with surgery then an appropriate elective neck dissection should be performed. Unilateral glottic cancer would be treated with an ipsilateral selective neck dissection, and a bilateral selective neck dissection for lesions crossing the midline. Levels II, III, IV are at greatest risk. Subglottic extension of glottic cancers cancer tend to spread to the paratracheal nodes (level VI) and these should be included in the bilateral neck dissection. If the paratracheal nodes are positive then the mediastinum should be included in the post-operative radiotherapy fields. In salvage surgery treatment of the N0 neck should always be considered. N+ If radiotherapy (with or without chemotherapy) is used to treat the primary tumour both sides of the neck should be included in the irradiation fields. If post radiotherapy assessment at 6 weeks demonstrates, on clinical examination or CT scan, residual neck disease, then this should be treated with a modified or radical neck dissection. If the primary tumour is treated with surgery then a neck dissection(s) is performed with post-operative radiotherapy for multiple positive nodes (>2), or nodes demonstrating extra capsular spread or node >3cm (N2), vascular invasion or perineural spread. Histological positive paratracheal nodes indicate post-operative radiotherapy to the upper mediastinum. Specifics of Treatment:
Surgery (procedure specifics) All patients undergoing laryngeal surgery should be assessed preoperatively by a SALT and considered for surgical voice restoration in laryngectomy.

28
Radiotherapy See local department radiotherapy and oncology protocols Chemotherapy See local department radiotherapy and oncology protocols The role of chemotherapy and biologic therapy in laryngeal cancer continues to evolve. Carefully controlled trials of chemotherapy with other treatment modalities should be supported. Patients treated with chemotherapy in conjunction with other modalities outside of trials should be managed in strictly controlled situations.
Chemotherapy with radiotherapy may improve larynx preservation rates but remains under investigation.
-radiotherapy may be to increase toxicity but the
impact on survival remains unclear.
The optimal combinations of chemotherapy with differing schedules of radiotherapy have yet to be determined.
Further studies and trials for chemotherapy and biological therapy are required
and should be supported by the Network for recruitment when available. Studies of chemotherapy on laryngeal preservation have shown that the larynx could be preserved in a quarter to a third of cases without detriment to overall survival. The American VA trial, which has the longest follow-up (median follow-up over 8 years), confirms the larynx can be preserved in up to 2/3 of patients achieving complete or partial response to induction chemotherapy without jeopardising survival. The EORTC trial (of larynx preservation in patients with hypopharyngeal cancers) showed a similar effect. An interim report on a French randomised trial (GETTEC) concerning just 68 patients of a planned 300 accrual showed a worse survival outcome for those receiving induction chemotherapy. Meta-analysis of all three trials demonstrated there were no differences in overall or disease free survival, but a functional larynx was preserved in two thirds of surviving patients. A more recent authoritative meta-analysis (Meta-Analysis of Chemotherapy on Head and Neck Cancer Collaborative Group, MACHNC) confirms a significance benefit from cisplatin and fluorouracil given concurrently with radiotherapy – absolute 2 year survival benefit=7%. Such benefits however must be balanced against the side effects of the chemotherapy. Combining chemotherapy concurrently with radiotherapy may be superior to induction or neo-adjuvant chemotherapy in advanced head and neck cancers, and may improve overall survival. Two randomised trials have shown improved local control and survival in over 5 years of follow-up in patients receiving an alternating chemo-radiotherapy regime. Follow-Up Schedule and Post Treatment Investigations
YEAR 1 4 to 6 weekly YEAR 2 2 monthly

29
YEAR 3 3 to 4 monthly YEAR 4/5 6 monthly YEAR 5 to 10 Yearly YEAR 10 continue under ENT follow if continue to smoke
In lesions involving the ventricle direct laryngoscopy to be performed within 3 months of completion of radiotherapy. Neck or chest imaging based on clinical findings Management of Recurrent Disease/Salvage
Recurrent or Residual Disease The treatment will depend on whether the patient has been treated with initial irradiation or surgery. Recurrence after previous irradiation is managed with salvage surgery which generally implies total laryngectomy however some authors now report good results with salvage partial laryngectomy The surgical approach for recurrent disease is planned according to the site and extent of the original lesion. Unresectable post-surgical recurrences are treated with radiation. Stomal recurrence, particularly if arising superiorly may be resectable, requiring mediastinal resection with the cardiothoracic team and possible pharyngeal replacement. Palliative radiotherapy may be applicable for stomal recurrence if it is below the previous treatment field. Supraglottis
Anatomic Description of Site
The supraglottis is composed of the epiglottis (both its lingual and laryngeal aspects), aryepicglottic folds (laryngeal aspect), arytenoids, and ventricular bands (false cords). The epiglottis is divided for staging purposes into suprahyoid and infrahyoid portions by a plane at the level of the hyoid bone. The inferior boundary of the supraglottis is a horizontal plane passing through the lateral margin of the ventricle at its junction with the superior surface of the vocal cord.
Tumour type pathology – squamous and other (excludes salivary and thyroid) See glottis Tumour staging UICC 6
Supraglottis
T1 Tumour limited to one subsite of supraglottis with normal vocal cord mobility
T2 Tumour invades mucosa of more than one adjacent subsite of supraglottis or glottis or region outside the supraglottis (e.g. mucosa of base of tongue, vallecula, medial wall of pyriform sinus) without fixation of the larynx.

30
T3 Tumour limited to larynx with vocal cord fixation and./or invades any of the
following
Postcricoid area, pre-epiglottic tissues, paraglottic space, and/or minor thyroid cartilage erosion (e.g. inner cortex)
T4A Tumour invades through the thyroid cartilage and or invades tissues beyond
the larynx (e.g., trachea, soft tissues of neck including deep extrinsic muscle of the tongue, strap muscles, thyroid, or esophagus).
T4B Tumour invades prevertebral space or encases carotid artery or invades
mediastinal structures Stage Summary –see glottis Additional Pre MDT workup (outside of generic or specific aspects) All patients should undergo a panendoscopy and biopsy, CXR, CT scan of larynx, neck and upper thorax as well as comorbidity scoring. Patients being considered for laryngeal surgery should have pulmonary function tests. Treatment modality options in early/late disease in Network and reasons for preference (include EBM references) including multimodality if applicable. Any treatments for referral outside of Network Early Supraglottic Tumours – T1-2
Conservation surgery (including laser endolaryngeal resection) or radiotherapy are alternatives. The choice depends on the tumour distribution and co morbidity/performance status. Consideration should be given to bilateral elective neck treatment by a wider radiotherapy field. Advanced Supraglottic Tumours – T3-4
Studies have suggested there is no survival advantage for T3 laryngeal cancers in performing laryngectomy with or without post operative radiotherapy, compared to radical radiotherapy with salvage surgery, but that primary laryngectomy with post operative radiotherapy does confer a significant survival advantage in T4 laryngeal disease compared to radical radiotherapy, with if necessary, salvage surgery. The only prospective randomised trial for advanced laryngeal cancer suggests that total laryngectomy with post operative radiotherapy confers no survival advantage when compared to induction chemotherapy followed by radiotherapy, and if necessary salvage laryngectomy. This may suggest chemoradiation to be the treatment of choice in low volume T3 laryngeal disease, but that primary surgery with follow up radiotherapy should be considered for high volume T3 supraglottic disease. Primary surgery does have the advantage of allowing access to the neck nodes. Midline cancers must have both sides of the neck treated. Patients with supraglottic tumours involving the pre-epiglottic space or upper piriform fossae may be suitable for an extended supraglottic or subtotal laryngectomy rather than total laryngectomy.

31
To perform conservation laryngeal surgery the patient must have good health and pulmonary function otherwise total laryngectomy is the surgical option of choice. As the role of chemotherapy is changing, in otherwise fit patients with advanced disease (T3 or T4/N2+) undergoing radical radiotherapy concurrent chemotherapy is offered. Management of the Neck in Supraglottic Cancer
N0 In T2 and above stages of supraglottic cancer there is at the present time a consensus that the neck needs to be treated electively. Treatment of the primary site will determine how the neck is treated. If the primary site is treated with radiotherapy then elective neck radiation should be performed, usually with extended fields. If the primary site is treated with surgery then an appropriate bilateral selective neck dissection is performed. N+ If radiotherapy (with or without chemotherapy) is used to treat the primary tumour both sides of the neck should be included in the irradiation fields. If post radiotherapy assessment at 6 weeks demonstrates, on clinical examination, ultrasound +/- FNA or CT scan, residual neck disease, then this should be treated with a modified or radical neck dissection. If the primary tumour is treated with surgery then a modified radical neck dissection(s) is performed with post-operative radiotherapy for multiple positive nodes (>2), or nodes demonstrating extra capsular spread or node >3cm (N2), vascular invasion or perineural spread. Histological positive paratracheal nodes would indicate post-operative radiotherapy to the mediastinum. Bilateral dissection is arguably required for all supraglottic disease, but is essential when the disease crosses the midline. Irresectable nodal disease may be palliated by radiotherapy Specifics of Treatment:
Surgery (procedure specifics) - see glottis section and neck
Radiotherapy - see glottis section and neck
Chemotherapy - see glottic section
Follow-up schedule and post treatment investigations - see glottic section

32
Management of recurrent disease/salvage - see glottic section Subglottis
Anatomic Description of Site
The subglottis is the region extending from the lower boundary of the glottis to the lower margin of the cricoid cartilage. Tumour type pathology – squamous and other (excludes salivary and thyroid) See glottic section Tumour Staging UICC6
Subglottis
T1 Tumour limited to the subglottis
T2 Tumour extends to vocal cord(s) with normal or impaired mobility
T3 Tumour limited to larynx with vocal cord fixation
T4a Tumour invades cricoid or thyroid cartilage and/or invades tissues beyond the larynx
(e.g., trachea, soft tissues of neck including deep extrinsic muscles of the tongue, strap muscles, thyroid or esophagus)
T4b Tumour invades prevertebral space or encases carotid artery or invades
mediastinal structures Stage Summary – see glottis Additional Pre MDT Workup (outside of generic or specific aspects) See glottic section Treatment modality options in early/late disease in Network and reasons for preference (include EBM references) including multimodality if applicable. Any treatments for referral outside of Network. Most tumours are indistinguishable from glottic tumours with subglottic extension. Radiotherapy may be suitable for early tumours, but most present at a late stage often with stridor, and treatment with total laryngectomy and post-operative radiotherapy is indicated. As the role of chemotherapy is changing, in otherwise fit patients with advanced disease (T3 or T4/N2+) undergoing radical radiotherapy concurrent chemotherapy is offered. Management of the Neck in Subglottic Cancer
N0

33
In all T stages of subglottic cancer there is at the present time a consensus that the neck needs to be treated electively. Treatment of the primary site will determine how the neck is treated. If the primary site is treated with radiotherapy then elective neck radiation with extended fields should be performed. If the primary site is treated with surgery then an appropriate bilateral selective neck dissection to include level V1 nodes should be performed. N+ If radiotherapy (with or without chemotherapy) is used to treat the primary tumour both sides of the lower neck and mediastinum should be included in the irradiation fields. If post radiotherapy assessment at 6 weeks demonstrates, on clinical examination, ultrasound +/-FNA or CT scan, residual neck disease, then this should be treated with a modified or radical neck dissection. If the primary tumour is treated with surgery then a modified radical neck dissection(s) is performed with post-operative radiotherapy for multiple positive nodes (>2), or nodes demonstrating extra capsular spread or node >3cm (N2), vascular invasion or perineural spread. Histological positive paratracheal nodes would indicate post-operative radiotherapy to the mediastinum. Bilateral dissection is essential for all subglottic disease. Specifics of Treatment:
Surgery (procedure specifics) – see glottic section Radiotherapy - see glottic section Chemotherapy - see glottic section Follow-Up Schedule and Post Treatment Investigations - see glottic section Management of Recurrent Disease/Salvage - see glottic section CARCINOMA OF THE ORAL CAVITY and LIP MAIN AUTHOR: DG Bryant Update 2015: S Endersby TNM Classification: UICC VERSION 7 Lip and Oral Cavity (Non-epithelial tumours such as those of lymphoid tissue, soft tissue, bone, and cartilage are not included.)

34
Anatomical Sites and Subsites Lip
External upper lip (vermilion border ) (C00.0) External lower lip (vermilion border) (C00.1) Commissures (C00.6)
Oral cavity
Buccal mucosa - mucosa of the upper and lower lips (C00.3, 4) - cheek mucosa (C06.0) - retromolar areas (C06.2) - bucco-alveolar sulci, upper and lower (vestibule of mouth) (C06.1)
Upper alveolus and gingiva (upper gum) (C03.0) Lower alveolus and gingiva (lower gum) (C03.1) Hard palate (C05.0)
Tongue
dorsal surface and lateral borders anterior to vallate papillae (anterior two-thirds) (C02.0/1).
inferior (ventral) surface (C02.2) Floor of mouth (C04) Anatomy Primary Site. The oral cavity extends from the skin-vermilion junction of the lips to the junction of the hard and soft palate above and to the line of circumvallate papillae below and is divided into the following specific areas: Mucosal Lip. The lip begins at the junction of the vermilion border with the skin and includes only the vermilion surface or that portion of the lip that comes into contact with the opposing lip. It is well defined into an upper and lower lip joined at the commissures of the mouth. Buccal Mucosa. This includes all the membrane lining of the inner surface of the cheeks and lips from the line of contact of the opposing lips to the line of attachment of mucosa of the alveolar ridge (upper and lower) and pterygomandibular raphe. Lower Alveolar Ridge. This refers to the mucosa overlying the alveolar process of the mandible which extends from the line of attachment of mucosa in the buccal gutter to the line of free mucosa of the floor of the mouth. Posteriorly it extends to the ascending ramus of the mandible. Upper Alveolar Ridge. This refers to the mucosa overlying the alveolar process of the maxilla which extends from the line of attachment of mucosa in the upper gingival buccal gutter to the junction of the hard palate. Its posterior margin is the upper end of the pterygopalatine arch.

35
Retromolar Gingiva (Retromolar Trigone). This is the attached mucosa overlying the ascending ramus of the mandible from the level of the posterior surface of the last molar tooth to the apex superiorly, adjacent to the tuberosity of the maxilla. Floor of the Mouth. This is a semilunar space over the mylohyoid and hyoglossus muscles, extending from the inner surface of the lower alveolar ridge to the under surface of the tongue. Its posterior boundary is the base of the anterior pillar of the tonsil. It is divided into two sides by the frenulum of the tongue and contains the ostia of the submandibular and sublingual salivary glands. Hard Palate. This is the semilunar area between the upper alveolar ridge and the mucous membrane covering the palatine process of the maxillary palatine bones. It extends from the inner surface of the superior alveolar ridge to the posterior edge of the palatine bone. Anterior Two-Thirds of the Tongue (Oral Tongue). This is a freely mobile portion of the tongue that extends anteriorly from the line of circumvallate papillae to the undersurface of the tongue at the junction of the floor of the mouth. It is composed of four areas: the tip, the lateral borders, the dorsum, and the under-surface (non-villous ventral surface of the tongue). The under-surface of the tongue is considered as a separate category by the World Health Organisation (WHO). Regional Lymph Nodes . Mucosal cancer of the oral cavity may spread to regional lymph node(s). Tumours of each anatomic site have their own predictable patterns of regional spread. The risk of regional metastasis generally relates to the T category and probably more importantly to the depth of infiltration of the primary tumours. Cancer of the lip carries a low metastatic risk and initially involves adjacent submental and submandibular nodes, then jugular nodes. Cancers of the hard palate and alveolar ridge likewise have a low metastatic potential and involve buccinator, submandibular, jugular and occasionally retropharyngeal nodes. Other oral cancers will primarily spread to submandibular and jugular nodes, uncommonly posterior triangle/supraclavicular nodes. Cancer of the anterior oral tongue may spread directly to lower jugular nodes. The closer to the midline of the primary, the greater the risk of bilateral cervical nodal spread. Any previous treatment to the neck, surgical and/or radiation, may alter normal lymphatic drainage patterns resulting in unusual distribution of regional spread of disease to the cervical lymph nodes. In general, cervical lymph node involvement from oral cavity primary sites is predictable and orderly, spreading from the primary to upper, then middle, and subsequently lower cervical nodes. However, disease in the anterior oral cavity may also spread directly to the mid cervical lymph nodes. The risk of distant metastasis is more dependent upon the "N" than the "T" status of the head and neck cancer. Metastatic Sites The lungs are the commonest site of distant metastases; skeletal or hepatic metastases occur less often. Mediastinal lymph node metastases are considered distant metastases.

36
Rules for Classification Clinical Staging The assessment of the primary tumour is based upon clinical inspection and palpation of the oral cavity and neck. The assessment of the regional lymph nodes is by palpation; ultrasound is also useful in experienced practitioner’s hands. Imaging of the primary site with MRI gives good soft tissue views and will show extent of soft tissue invasion, perivascular and perineural spread, skull base involvement and intracranial tumour extension On the other hand, high resolution CT with contrast will often provide similar information if carefully done and will provide better images of bone and larynx detail and is minimally affected by motion due to much shorter acquisition times. The presence of nodal metastases should be done by CT or MRI. Ultrasonography with or without FNAC sampling may also be useful in equivocal nodes. Distant metastasis should be assessed by CT of the thorax and upper abdomen to include the lung, liver and adrenal glands. All clinical, imaging, and pathologic data should be used for accurate staging and should be available prior to first definitive treatment. Early lip tumors are often staged clinically alone. Definition of TNM Primary Tumour (T)
TX Primary tumour cannot be assessed T0 No evidence of primary tumour Tis Carcinoma in situ T1 Tumour 2 cm or less in greatest dimension T2 Tumour more than 2 cm but not more than 4 cm. in greatest dimension T3 Tumour more than 4 cm in greatest dimension T4 (lip) Tumour invades adjacent structures (e.g., through cortical bone, inferior
alveolar nerve, floor of mouth, skin of face, i.e. chin or nose) T4a (oral cavity) Tumour invades adjacent structures (e.g., through cortical bone,
into deep [extrinsic] muscle of tongue (genioglossus, hyoglossus, palatoglossus, and styloglossus), maxillary sinus, skin of face. Superficial erosion alone of bone/tooth socket by gingival primary is not sufficient to classify as T4)
T4b Tumour invades masticator space, pterygoid plates, skull base and internal carotid artery NOTE: Superficial erosion alone of bone/tooth socket by gingival primary is not sufficient to classify a tumour as T4.
Stage Grouping – Identical to Larynx Confirmation of Diagnosis

37
Examination and biopsy Careful physical examination is mandatory and has not been superseded by imaging. Examination should include either fibre-optic or direct examination of pharynx, larynx and postnasal space. Tumour site and areas of field cancerisation should be carefully documented; use of standardised tumour maps and photographs may be useful. If physical examination and biopsy is not achievable then examination under anaesthesia (EUA) is recommended. Consideration of dental extractions of poor quality teeth, re-biopsy and tonsillectomy may be indicated whilst undergoing EUA. Formal biopsy is a cornerstone of the management pathway. UK guidelines by the Royal College of Pathologists should be followed when reporting results to include degree of differentiation, tumour thickness, vascular and perineural invasion. The increased importance of high risk HPV means that testing is often desirable for certain sub-sites and should include HPV16 in situ hybridisation in addition to p16 immunohistochemistry. Additional imaging All patients need a full dental assessment and dentate patients and those with planned bone resections or osteotomies for access in open surgery should have an orthopantomagram (OPG) PET-CT is used in recurrent tumours to detect disease at primary site as well as neck and distant metastasis. It also has a role n assessing response to chemoradiotherapy. Photographs of accessible tumours is very useful. Definitive Treatment Treatment of Primary Tumour LIP Lip tumours may be treated by surgery or by radical radiotherapy. Surgical excision however is generally the preferred. Most early lesions may be excised under local anaesthesia +/- intravenous sedation. Adjacent pre-malignant tissue should also be excised. FLOOR OF MOUTH Small volume T1 and T2 tumours may be treated by surgery including trans-oral laser treatment or radiotherapy (both external beam megavoltage and interstitial techniques). In contrast, larger T2 lesions (>3 cm) usually require combination therapy with surgery and adjuvant radiotherapy. Smaller lesions may be allowed to heal following excision by a primary repair or by secondary intention. Flap reconstruction may be required for larger volume tumours For anterior tongue, buccal mucosa and floor of mouth surgery is preferred if tumour involves periosteum.

38
Large volume T2 T3 and T4 tumours require surgery with surgical excision combined with neck dissection. There will be a high probability that adjuvant radiotherapy will also be required. Tumours involving the mandible will require a rim resection or segmental mandibulotomy. Access may be facilitated by open surgery with a lip split mandibulotomy. The morbidity and potential functional impairment should be carefully discussed with patients who have massive disease. ORAL TONGUE Oral tongue tumours appear to have a different biological behaviour than other oral cavity sub-sites, metastasising more frequently to levels II and III than level I and a higher incidence of skip lesions to level IV. Therefore, excision with an elective neck dissection is usually warranted in the N0 neck. This should include levels II to IV and possibly level I. Level IIb is omitted in the N0 neck. However, in low volume T1 oral tongue tumours, without evidence of metastatic disease, laser excision of the primary tumour and a careful follow up of the neck may be considered. The N +ve neck requires an appropriate neck dissection dependent on clinical and radiographic imaging. In most of these cases, post-operative adjuvant radiotherapy should be considered. BASE OF TONGUE T1 lesions can be treated by surgery. Transoral approaches with transoral laser (TOL) surgery utilising a Steiner excision technique and more recently en-bloc resection with transoral robotic surgery (TORS) have grown in use and popularity. Advantages are rapid recovery with equivalent control rates to open surgery. Open approaches via lip and tongue split or transcervical pharyngotomy are rarely considered. They can however be treated equally well by radical radiotherapy. T2,T3 and T4 lesions require radical radiotherapy in conjunction with chemotherapy in line with an attempt at organ preservation. Surgery for residual neck disease may also be required, the diagnosis of which is aided by PET-CT follow up. If there is recurrence, or if the extent of the original tumour is deemed incurable by the above techniques, total glossectomy with laryngectomy may be considered. This has extremely high morbidity, but with careful counselling and extensive rehabilitation it can be performed in an appropriate group of patients. HARD PALATE T1 lesions may be managed by surgery with surgical excision and periosteal strip or radical radiotherapy. T2m T3 and T4 lesions require excision with a bone margin possibly amounting to a partial maxillectomy. This may require obturation or flap reconstruction. Neck involvement is unusual and a watchful waiting policy may be adopted where there is no evidence of nodal involvement. NECK

39
As base of tongue, posterior pharyngeal wall, and palatal lesions predominantly affect the midline then spread to lymph nodes bilaterally, both sides of the neck must be considered when planning treatment. In the N0 neck consideration should be given to elective treatment, either by prophylactic radiotherapy or by selective neck dissection if open resection is being employed. The N1 neck is treated by surgery either by selective or modified radical neck dissection, depending on the treatment of the primary. In early lesions radical radiotherapy may be used. In N2/N3 necks a neck dissection is indicated but may not be possible depending on the site of the disease in N2 and the extent in N3. Post operative radical radiotherapy is indicated if more than one node is involved or if extracapsular spread is present. Radiotherapy Adjuvant radiotherapy is considered in all patients with close margins, ECS and more than one positive node. Tumour size, thickness and adverse features such as differentiation, non-cohesive front and perineural or lymphovascular invasion are also considered. Chemotherapy Chemotherapy should additionally be considered in patients without contraindication who have close margins or ECS. Recurrence Best managed with aggressive surgical resection with frozen section control. Elective neck dissection advocated as 25% have occult metastases. High success rate in management of local recurrence, 75-85%. HEAD AND NECK SARCOMA MDT Management Diagnosis of sarcoma is often made late, when the tumour is already large and often unexpectedly. Optimal management and survival requires specialized care, particularly in relation to extirpative and reconstructive surgery, pathology and oncology. MDTs are the accepted form of management for conditions requiring complex care, but have to see sufficient patients annually to maintain expertise and justify resource allocation. The draft sarcoma IOG (published March 2005) recommends that “All patients with a bone or soft tissue sarcoma should be managed by a sarcoma MDT”. These would thus likely service a population of 2-3 million for soft tissue sarcoma (STS) and 7-8 million for bone sarcoma (BS)`, managing at least 100 STS and or 50 BS a year. It further recommends that all cancer centres must either:
Host a sarcoma MDT Use the facilities of a nearby sarcoma MDT Have a medical oncologist acting as an approved extended team member of
another sarcoma MDT It is accepted, however, that more than one MDT may need to be involved in the care of sarcoma patients dependent upon the site of the tumour. This is particularly so for tumours in

40
the head and neck, where all patients must have their case discussed at an MDT appropriately qualified for that site. There is recognition that the skills required for management of head and neck sarcomas are very similar to those for other tumour groups at this site. These groups, it is felt, should work in conjunction with the sarcoma MDT. Summary For patients with head and neck sarcomas to be adequately managed in the Network:
All patients with a provisional histological or radiological diagnosis of bone or soft tissue sarcoma should have their diagnosis reviewed by a specialist sarcoma pathologist or radiologist.
Patients should undergo definitive resection of their sarcoma by a surgeon who is
a member of a sarcoma MDT or by a surgeon with site specific skills in consultation with the sarcoma MDT.

41
SALIVARY GLANDS MAIN AUTHORS: - DG Bryant This section has been produced with reference to the ‘Evidence Based Conference of the Management of Salivary Gland Neoplasms’ held at the Freeman Hospital, Newcastle upon Tyne on the 19th November 1998. A full reference list from the meeting is available on the NOTO website – www.noto.org Characterisation Salivary gland malignancies are rare and present a diverse range of histology and clinical behaviour. The original 1972 WHO histological classification of salivary gland tumours insisted of four subgroups: Epithelial tumours, non-epithelial tumours, unclassified tumours and allied conditions of which the epithelial group was the larger in number. Under the new system there are seven categories:
1. Adenomas 2. Carcinomas 3. Non Epithelial tumours 4. Malignant Lymphomas 5. Secondary tumours 6. Unclassified tumours 7. Tumour-like disorders
Carcinomas are often further classified as high grade, low grade or mixed, the latter inferring a variable behaviour depending on the histological picture. Except in the case of mucoepidermoid tumours however, clinicopathological correlation has proved to be unreliable and often the clinical behaviour rather than the histology of a tumour provides a better guide for treatment. Although, overall, tumours are more common in the parotid, the incidence of malignancy is higher in the submandibular, sublingual and minor salivary glands. The more common adenomas and carcinomas are shown below: Adenomas Carcinomas
ex Pleomorphic adenoma Myoepithelial (myoepithelian adenoma) Basal cell adenoma Warthin’s tumour (adenolymphoma) Ductal Papilloma Cystadenoma Acinic cell carcinoma Mucoepidermoid carcinoma Adenoid cystic carcinoma Polymorphous low-grade (terminal duct) Papillary cystadenocarcinoma Mucinous adenocarcinoma

42
Adenocarcinoma Carcinoma in pleomorphic adenoma (malignant mixed tumour) Squamous cell carcinoma Undifferentiated carcinoma
Confirmation of Diagnosis Malignant tumours may be clinically indistinguishable from benign lesions and definitive histology is usually unavailable until after surgical resection. Diagnosis is therefore based on: Clinical presentation - pain, rapid growth, fixation, nerve involvement or neck metastasis all suggestive of malignancy. Fine Needle Aspirate Cytology is useful for major salivary gland lesions and must be examined by a cytopathologist experienced in the diagnosis of salivary gland disease. This should distinguish malignant from benign disease in 90% of cases. MRI scanning may demonstrate non-homogeneity, muscle infiltration or suspicious regional lymph node appearance suggestive of malignancy. Open biopsy should be avoided in major salivary gland lesions due to the risk of tumour spillage. It may be indicated for minor salivary gland lesions where the overlying epithelium will be excised at the time of surgery. Frozen section should be avoided, accurate diagnosis is often difficult and false negative rates are significant and therefore should not be relied upon. Submandibular Gland Surgery Primary Tumour A total excision is appropriate for most tumours confined to the gland. Some argue in favour of wider resection for adenoid cystic tumours including the lingual, hypoglossal and marginal mandibular nerve if there is any suspicion of involvement by tumour, but evidence is not strong, and the advice is counter to recommendations for the uninvolved facial nerve in parotid disease. Clinically high-grade tumours in young individuals should be treated more aggressively with excision of the gland plus a 2cm margin of apparently healthy tissue Large Tumours with bone involvement should be treated with composite resection of tumour, adjacent soft tissue cuff and segmental mandibulectomy. Neck Disease All Patients should undergo clearance of nodes in suprahyoid region. Clinically high-grade tumours or with suspicious MRI appearance should have an elective supra-omohyoid dissection.

43
Patients with clinically confirmed neck metastasis should have a neck dissection. Radiotherapy Palliation Is useful for inoperable tumours where palliation can be achieved. Post-operative radiotherapy is indicated for:
High grade or advanced stage tumours with a high risk of local recurrence
Residual disease or microscopic extra-capsular spread from lymph nodes
Surgery for recurrent disease Parotid Gland Surgery Primary Tumour Apart from lymphomas, surgery is the treatment of choice. A conservative parotidectomy should be performed with preservation of the facial nerve providing there is no tumour invasion. For deep lobe tumours this will involve a total parotidectomy plus resection of adjacent structures if necessary to achieve an en-bloc resection. Any part of the facial nerve not infiltrated by tumour should be preserved. Primary nerve grafting should be considered if microscopic clearance of the main trunk and peripheral branches can be achieved. Adenoid cystic carcinoma requires a parotidectomy with sacrifice of any part of the nerve involved by tumour. Resection of an intact nerve has been shown to improve local disease control but will not improve survival. It is unlikely that nerve grafting will compromise outcome and therefore could be considered particularly if combined with post-operative radiotherapy. Neck Neck dissection should be performed in patients with evidence of nodal disease either clinically or on MRI scanning. A prophylactic neck dissection should be considered for patients with clinically high grade tumours, i.e. adenocarcinoma, squamous and undifferentiated. Radiotherapy Post-operative As for the submandibular gland plus any patient in whom the facial nerve has been preserved despite close approximation of the tumour.

44
Recurrent Disease Requires careful evaluation of the patient with repeat imaging and a review of the histology from the initial excision. This will usually require more radical surgery with sacrifice of the nerve and overlying skin if any suspicion of involvement by tumour. Super-radical resections of skull base have not to date shown convincing evidence of improved survival. Consider chemotherapy and/or radiotherapy for palliation. Minor Salivary Glands Confirmation of diagnosis Clinical history and examination with particular reference to palate and nasal cavity. Open biopsy is permissible to confirm diagnosis. The prognosis for these patients is more closely related to stage of disease rather than histology. Treatment En-bloc resection with depth of excision equal to width to ensure adequate resection margins. Neck Therapeutic neck dissection is indicated for lymph node involvement. Elective neck dissection is indicated for adenocarcinoma, carcinoma in pleomorphic adenoma and undifferentiated carcinoma. Radiotherapy Indications:
Post-operative Microscopic residual disease Adenoid cystic tumours Aggressive undifferentiated tumours
CONTACTS The Policy and the Named Hospitals for Head and Neck Cancer
The named designated Hospitals for Head and Neck Cancer in the North of England Cancer Network are described below: Each hospital has a clinic for referral of patients with head and neck cancer in line with their locally primary care referral guidelines. In line with the manual, each designated hospital has a minimum of two designated clinicians.

45
Area Population*
Newcastle West 144 Freeman Hospital
Newcastle North & East 143 Royal Victoria Infirmary
North Tyneside 202
Northumberland 316
149 South Tyneside District Hospital
Palmer Community Hospital
Sunderland 276 Sunderland Royal Hospital Sunderland Royal
Hospital
Gateshead 200 Queen Elizabeth Hospital Queen Elizabeth
Hospital
Durham Dales, Easington &
Sedgefield
273
Darlington 105
243 University Hospital of
North Durham
Shotley Bridge
Hospital
South Tees 274
Hambleton, Richmondshire & Whitby 154
Stockton 193 University Hospital of
North Tees
Hartlepool 93 University Hospital of
Hartlepool
328 Cumberland Infirmary
West Cumberland Hospital
* - 2013 Mid Year Population Estimates
Cumbria
North Durham Sunderland Royal Hospital
Designated Hospital – Head and
Neck
Designated Hospital -
Thyroid
Freeman Hospital
Freeman Hospital
Darlington Memorial Hospital
CCG populations
North Tyneside
General Hospital
South Tyneside Palmer Community
Hospital
Darlington Memorial
Hospital
James Cook University Hospital James Cook
University Hospital
James Cook University Hospital
Cumberland Infirmary
Please note: Across NECN, Endocrine Surgeons also operate on Thyroid Cancer in addition to Head and Neck Surgeons
The Distribution of Neck Lump Clinics
The distribution of neck lump clinics for suspected Head and Neck Cancer in the North of England Cancer Network are described below in the table below, Referral Guidelines for Primary Care Practitioners – UAT patients.
Each hospital has a clinic for referral of patients with head and neck cancer in line with the locally agreed primary care referral guidelines.
Designated clinics are distributed such that the PCT’s agreed populations have sufficient access.

46
Referral Guidelines for Primary Care Practitioners - UAT Patients
The NICE Referral guidelines for suspected cancer have been agreed and adopted as the Network Referral Guidelines. These guidelines in conjunction with the Referral Forms for Patients with Suspected Cancer, Coding sheet and Cancer Services Directories provide Primary Care Practitioners with all necessary information regarding named local services and contact points. Also see Appendix 1, Primary Care Referral Guidelines.

47
Referral Guidelines for Primary Care Practitioners - UAT Patients
Area Population*
Newcastle West 144 GDP - FH Mr A Welch
Newcastle North & East 143 2 week wait central office Mr V Paleri
Northumberland 316 Fax: 0191 2231498 Mr D Meikle
North Tyneside 202 Choose & Book Mr Adams
Tel: 0345 6088888
Cumberland Infirmary Cumberland Infirmary 2 week central office Mr J Elliott
Fax: 01946 523489 Mr A Robson
West Cumberland Hospital West Cumberland
Hospital
Mr G Putnam
Mr P Counter
Sunderland 276 Appointments Office Mr R Banks
Fax: 0191 5699030 Mr C Hartley
North Durham 243 Ms H Cocks
Mr I C Martin
Mr A Burns
Mr J O’Hara
South Tyneside DH South Tyneside DH Ms H Cocks
Miss J Heaton
Palmer Community Hospital Palmer Community
Hospital
Mr T Leontsinis
Mr Pardeshi
Mr A Burns
Ms K Stone
Miss N Jones
Choose & Book Mr J Moor
Tel: 0345 6088888 Ms H Cocks S Marshall
(does not
attend clinic-
but contactable
by Bleep only)
Cancer Booking Team
(within call centre) QE
Mr P Arul
Durham Dales, Easington &
Sedgefield
273 Choose & Book Mr S Lester
Mr R Wight
Darlington 105 Tel: 0345 6088888 Mr C Edge
Col D Bryant
South Tees 274 Tel: 01642 282853 Mr C Pace
Fax: 01642 282826
Hartlepool & Stockton 286
Hambleton, Richmondshire & Whitby 154
* - 2013 Mid Year Population Estimates
200Gateshead Queen Elizabeth Hospital
Dr D Plews
(unable to
attend clinic
however they
are able to see
the patient 24-
48 hrs)
Dr A Lennard
Dr G Jackson
Dr G Jones
Dr T Menne (do
not attend
clinic-
contactable by
phone /bleep
only)
H Ob'rien
R Oakes
Locum (do not
attend clinic-
contactable by
phone/bleep
only)
South Tyneside
JCUH
Tuesday AM
MDT
Location
Freeman Hospital (FH) Freeman Hospital
Designated
Lead
Clinicians
Haemato-
oncologists
with direct
care sessions
timetabled for
the clinic
V Hervey (does
not attend
clinic- but
contactable as
liaison
haematologist)
V Hervey (does
not attend
clinic- but
contactable as
liaison
haematologist)
Freeman
Hospital
Thursday AM
SRH Friday
AM
Sunderland Royal Hospital (SRH) Sunderland Royal
Hospital (SRH)
Cumbria
CCG populations
328
149
James Cook University Hospital
(JCUH)
James Cook
University Hospital
(JCUH)
Fax: 0191 2022191
Queen Elizabeth
Hospital
Darlington Memorial Hospital
Contact Points
Darlington Memorial
Hospital
Designated Hospital Neck Lump Clinic
Location

48
Distribution Process for Referral Guidelines
Primary Care Medical Practices Primary Care referral guidelines for Head & Neck cancer, including Thyroid are sent to the Primary Care Commissioners for onward distribution to general practice and general dental practices, and also through Cancer Unit Managers for onward distribution to the relevant clinical specialities. Copies of the guidelines are available on the North of England Cancer Network’s website: http://www.necn.nhs.uk/group/head-neck-nssg/ Network Agreed Referral Proformas
All Network wide referral proformas are in line with NICE guidance for urgent referral for suspicion of cancer 2005 and comply with the following:
it is used for patients with UAT symptoms which are outside the 'urgent suspicion of cancer' definition and who have no neck lumps
it allows for the referrer to categorise a patient by presenting features, so that the hospital can direct the referral to the relevant specialty (e.g. ENT, OMFS)
the network-wide format is made locally specific by identifying a single referral point for each designated hospital to which proformas can be sent for direction to individual specialists.
Internal Referral Guidelines for Non-Designated Hospital Clinicians
The Schema below is adopted from The Manual for Cancer Services (Head & Neck 2008)

49
Network Agreed Named Hospital for Surgical Treatment Delivery
Area Population*
Newcastle West 144 Freeman Hospital
Newcastle North & East 143
Northumberland 316 Lead Clinician
North Tyneside 202 Mr D Meikle
Gateshead 200 Wards
Sunderland 276 C33
South Tyneside 149
North Durham 243
Darlington 105
South Tees 274
Hartlepool & Stockton 286
Hambleton, Richmondshire &
Whitby
154
Durham Dales, Easington &
Sedgefield
273
Cumbria 328 North Cumbria University
Hospitals NHS Trust
Ward for H&N
surgery is Beech C/D
Cumberland Infirmary
Lead Clinician
Mr G Putnam
Source - Mid-2013 Population Estimates for Clinical Commissioning Groups (CCGs) in England - ONS.gov.uk
James Cook University
Hospital
Lead Clinician
Mr S Lester
Newcastle upon Tyne Hospitals
NHS FT
Ward 10
Designated HospitalCCG populations
South Tees Hospitals NHS FT Ward 6 and Ward 35
Hospitals for Surgical
Delivery
Designated Ward
Lead Clinician Mr R
Banks
City Hospitals Sunderland NHS
FT
Sunderland Royal
Hospital
Network MDT Configuration
Trust Designated MDT Case Mix
South Tees Hospitals NHS FT North Tees & Hartlepool NHS FT Co Durham & Darlington FT (South)
James Cook University Hospital
Upper Aero-digestive Tract dealing with one or more of salivary gland tumours
Newcastle Upon Tyne Hospitals NHS FT Northumbria Healthcare NHS FT North Cumbria University Hospitals NHS FT
Freeman Hospital
Upper Aero-digestive Tract dealing with one or more of salivary gland tumours; UAT cancer involving skull base
City Hospitals Sunderland NHS FT Co Durham & Darlington NHS FT (North) Gateshead Health NHS FT South Tyneside NHS FT
Sunderland Royal Hospital
Upper Aero-digestive Tract dealing with Salivary gland tumours

50
MDT linkages
Trust Designated MDT Case Mix
South Tees Hospitals NHS FT North Tees & Hartlepool NHS FT Co Durham & Darlington NHS FT
James Cook University Hospital
Thyroid cancer
Newcastle Upon Tyne Hospitals NHS FT Northumbria Healthcare NHS FT North Cumbria University Hospitals NHS FT City Hospitals Sunderland NHS FT South Tyneside NHS FT Gateshead Health NHS FT
Royal Victoria Infirmary Thyroid Cancer
The Distribution of Local Support Teams in the Network
Designated Hospital Geographical coverage
Freeman Hospital
Northumberland, North Tyneside, Newcastle
Sunderland Royal Hospital
Sunderland, South Tyneside, North Durham, Washington, Gateshead
Cumberland Infirmary
Carlisle, Whitehaven, North Cumbria
Darlington Memorial
South Durham - Darlington, Bishop Auckland, Sedgefield (75%)
James Cook University Hospital – local support provided by Specialist MDT
Teesside – North of Tees, South of Tees, Sedgefield (25%), North Yorkshire

51
Appendix 1 - Referral Guidelines for Primary Care North of England Cancer Network Referral Guidelines for Primary Care Oral, Non Oral Lesions and Thyroid Developed by Head & Neck Site Specific group & Thyroid Sub-group May 2013 Review date: July 2015
Title: NECN Head and Neck Cancer Primary Care Referral Guidelines
Authors: Head and Neck NSSG members Thyroid Subgroup members
Circulation List: Primary care medical practices Primary dental practices Designated consultant clinicians Non-designated head and neck consultant clinicians (ENT surgeons, endocrine surgeons, OMFS surgeons, oral medicine specialists, endocrinologists, restorative dentistry consultant) – via Cancer Unit Managers Head and Neck NSSG
Contact Details: Mrs C McNeill, Peer Review Co-ordinator [email protected]
Telephone: 01138252976
Version History:
Date: 21.05.15 Version: v.05 Review Date:
July 2015
Document Control
Version
Date Summary Review Date
V0.5 21.05.15 Reviewed and no amendments require July 2015
v.05 17.12.13 Head and neck cancers (Oral Lesions)- amended
May 2015

52
Referral Guidelines for Primary Care Practitioners - UAT Patients
Area Population*
Newcastle West 144 GDP - FH Mr A Welch
Newcastle North & East 143 2 week wait central office Mr V Paleri
Northumberland 316 Fax: 0191 2231498 Mr D Meikle
North Tyneside 202 Choose & Book Mr Adams
Tel: 0345 6088888
Cumberland Infirmary Cumberland Infirmary 2 week central office Mr J Elliott
Fax: 01946 523489 Mr A Robson
West Cumberland Hospital West Cumberland
Hospital
Mr G Putnam
Mr P Counter
Sunderland 276 Appointments Office Mr R Banks
Fax: 0191 5699030 Mr C Hartley
North Durham 243 Ms H Cocks
Mr I C Martin
Mr A Burns
Mr J O’Hara
South Tyneside DH South Tyneside DH Ms H Cocks
Miss J Heaton
Palmer Community Hospital Palmer Community
Hospital
Mr T Leontsinis
Mr Pardeshi
Mr A Burns
Ms K Stone
Miss N Jones
Choose & Book Mr J Moor
Tel: 0345 6088888 Ms H Cocks S Marshall
(does not
attend clinic-
but contactable
by Bleep only)
Cancer Booking Team
(within call centre) QE
Mr P Arul
Durham Dales, Easington &
Sedgefield
273 Choose & Book Mr S Lester
Mr R Wight
Darlington 105 Tel: 0345 6088888 Mr C Edge
Col D Bryant
South Tees 274 Tel: 01642 282853 Mr C Pace
Fax: 01642 282826
Hartlepool & Stockton 286
Hambleton, Richmondshire & Whitby 154
* - 2013 Mid Year Population Estimates
200Gateshead Queen Elizabeth Hospital
Dr D Plews
(unable to
attend clinic
however they
are able to see
the patient 24-
48 hrs)
Dr A Lennard
Dr G Jackson
Dr G Jones
Dr T Menne (do
not attend
clinic-
contactable by
phone /bleep
only)
H Ob'rien
R Oakes
Locum (do not
attend clinic-
contactable by
phone/bleep
only)
South Tyneside
JCUH
Tuesday AM
MDT
Location
Freeman Hospital (FH) Freeman Hospital
Designated
Lead
Clinicians
Haemato-
oncologists
with direct
care sessions
timetabled for
the clinic
V Hervey (does
not attend
clinic- but
contactable as
liaison
haematologist)
V Hervey (does
not attend
clinic- but
contactable as
liaison
haematologist)
Freeman
Hospital
Thursday AM
SRH Friday
AM
Sunderland Royal Hospital (SRH) Sunderland Royal
Hospital (SRH)
Cumbria
CCG populations
328
149
James Cook University Hospital
(JCUH)
James Cook
University Hospital
(JCUH)
Fax: 0191 2022191
Queen Elizabeth
Hospital
Darlington Memorial Hospital
Contact Points
Darlington Memorial
Hospital
Designated Hospital Neck Lump Clinic
Location

53
Area Population*
Newcastle West 144 Freeman Hospital Freeman Hospital GDP - FH Mr A Welch
Newcastle North & East 143 Royal Victoria Infirmary Royal Victoria Infirmary 2 week wait central office Mr V Paleri
0191 2231498 Mr R Bliss
Choose & Book
Tel: 0345 608888
Northumberland 316 North Tyneside
Hospital
Mr M Carr
North Tyneside 202 Wansbeck General
Hospital
Mr S Aspinall
328 2 week central office Mr M Williams
Fax: 01946 523489 Mr L
Barthelmes
Sunderland 276 Sunderland Royal
Hospital
Appointments Office
Easington (60%) 56 Sacriston, Durham Fax: 0191 5699030 Mr T Leontsinis
Ms H Cocks
149 Ms H Cocks
Miss J Heaton
Mr T Leontsinis
Mr Pardeshi
200 Choose & Book Mr J Moor
Tel: 0345 6088888 Ms H Cocks
Cancer Booking Team
(within call centre) QE
Durham Dales, Easington &
Sedgefield (excl Easington 60%)
217 Choose & Book Mr V Shanker
Darlington 105 Tel: 0345 6088888 Mr S Lester
North Durham 243 University Hospital of North
Durham
University Hospital of
North Durham
Choose & Book Mr G Tervitt
Shotley Bridge Hospital Shotley Bridge
Hospital
Tel: 0345 6088888 Mr A Bhatti
South Tees 274 Tel: 01642 282853 Mr W M Elsaify
Fax: 01642 282826 Dr S Nag
Hambleton, Richmondshire & Whitby 154
Stockton 193 University Hospital of North Tees University Hospital of
North Tees
Mr J Kurup
Hartlepool 93 University Hospital of Hartlepool Dr S Jones
Source - Mid-2013 Population Estimates for Clinical Commissioning Groups (CCGs) in England - ONS.gov.uk
MDT
Location/MDT
Co-ordinator
Contact
Designated
Lead
Clinicians
Royal Victoria
Infirmary
Wednesday
PM
James Cook
University
Hospital Last
Friday of each
month pm
Gateshead Queen Elizabeth Hospital Queen Elizabeth
Hospital
Cumberland Infirmary
South Tyneside Palmer Community Hospital Palmer Community
Hospital
Cumbria Cumberland Infirmary
Sunderland Royal Hospital
North Tyneside Hospital
Thyroid Clinic
Location
Designated HospitalCCG populations
James Cook University Hospital James Cook
University Hospital
Tel: 01642 623292
Fax: 0191 2022191
Contact Points
Fax: 0191 2934107
Darlington Memorial Hospital Darlington Memorial
Hospital

54

55

56

57

58

59

60
Appendix 2 - NSSG Guidelines for Teenage and Young Adults Teenage and Young Adults Peer Review Measures Topic 11-1C (Functions of the Network Site Specific Groups for TYA) 1. Teenage and Young Adult Pathway for initial Management The NSSG has received the document named ‘NECN Teenage and Young Adult Cancer Pathway Guidance Paper’ and agrees to follow the generic TYA Pathway with any site specific variations to be documented. Please see Appendix 1 for pathway. 2. Teenage and Young Adult Pathway for Follow up on completion of first line treatment Patients aged 19-24 years will adopt the site specific adult follow up pathway on completion of first line treatment. It is acknowledged by both the CYPCG and NSSGs across NECN that further work is required to develop these pathways for this age group and partly in response a TYA working group has been established to take this work forward. If advice is required regarding the follow up care of a 19-24 year old patient, then the Lead TYA Clinician at the designated hospital or PTC should be contacted. Please see Appendix 2 for contact details. Patients age 16-18 years will continue to adopt the paediatric and adolescent follow up protocol of the PTC and all advice should be sought direct from the On Call Paediatric Oncologist at Royal Victoria Infirmary 0191 2336161. Paediatric Follow Up Protocols can be found on the CCLG website (2005 second edition) with the exception of trial specific protocols which can be requested via the Children’s Trial Co-ordinator based at the RVI. 3. Pathways for cases involving Specialised NHS services (Only Gynae and Sarcoma) The Gynae NSSG and SAG reviewed and agreed the Specialised NHS Service pathway for patient’s age 16-24 years. This is attached in Appendix 3.

61
Appendix 3– Teenage and Young Adult Pathway for initial Management

62
Appendix 4 – Contact Details
Name of NHS Trust and designated hospital site Name of MDT TYA Lead Clinician TYA Lead Nurse Contact Number
All MDTs:
Breast
Colorectal
Gynaeoncology (diagnostic)
Haematology
Head & Neck
Lung
Neurooncology (Brain/Spinal, Pituitary, Skull Base)
Sarcoma
Specialist Skin
Specialist pancreatic
Supra T-cell Lymphoma
Teenage and Young Adult MDT
Testicular
Thyroid
Specialist Upper GI
Specialist Urology
Gateshead Health NHS Foundation Trust - at Queen Elizabeth Hospital Specialist Gynaeoncology Ms Christine Ang
[email protected] 0191 4456148
Haematology
Specialist Urology (testicular only )
All MDTs:
Haematology
Local Urology
Thyroid
Breast
Colorectal
Lung
Local Upper GI
All MDTs:Specialist Gynaeoncology
Breast
Colorectal
Haematology
Head & Neck
Lung
Neurooncology
Specialist Skin
Thyroid
Specialist Upper GI
Specialist Urology
North Tees and Hartlepool NHS Foundation Trust - at University
Hospital of North Tees
South Tees Hospital NHS Foundation Trust - at James Cook University
HospitalDr Dianne Plews
Jill Linton
[email protected] 01642 854381
List of designated MDTs at Principal Treatment Centre and TYA Designated Hospitals (19 - 24 years)
0191 2448858 (Dect48858)Principal Treatment Centre Dr Emma Lethbridge David Short
0191 5656256Faye Laverick
[email protected] Dr Scott Marshall
City Hospitals Sunderland NHS Foundation Trust - at Sunderland Royal
Hospital
Kat Dawson
[email protected] Dr Padmaja Lokireddy 01642 617617 ext 24697

Appendix 5 – NHS Specialised Services Pathway

64

65
Appendix 6 - Imaging Guidelines HEAD & NECK NSSG IMAGING GUIDELINES
Version Control:
Title: Head & Neck Imaging Guidelines
Authors: Head & Neck NSSG members
Circulation List: Head & Neck NSSG
Contact Details: Dr E Aynsley Head and Neck NSSG Chair
Telephone: 01138252976
Version History:
Date: May 2015 Version: 0.2 Review Date: May 2016

66
CONTENTS
Introduction ............................................................................................................... 68
Head & Neck Cancers ............................................................................................... 69
Introduction ...................................................................................................................... 69
Nasopharynx ............................................................................................................. 70
Clinical background ......................................................................................................... 70
Who should be imaged? .................................................................................................. 70
Staging objectives ........................................................................................................... 70
Staging .............................................................................................................................. 71
Follow-up .......................................................................................................................... 72
Tips ................................................................................................................................... 72
Larynx ........................................................................................................................ 73
Clinical background ......................................................................................................... 73
Who should be imaged? .................................................................................................. 73
Staging objectives ........................................................................................................... 73
Staging .............................................................................................................................. 73
Follow-up .......................................................................................................................... 74
Tips ................................................................................................................................... 74
Paranasal sinuses .................................................................................................... 75
Clinical background ......................................................................................................... 75
Who should be imaged? .................................................................................................. 75
Staging objectives ........................................................................................................... 75
Staging .............................................................................................................................. 75
Follow-up .......................................................................................................................... 76
Tips ................................................................................................................................... 76
Hypopharynx ............................................................................................................. 77
Clinical background ......................................................................................................... 77
Who should be imaged? .................................................................................................. 77
Staging objectives ........................................................................................................... 77
Staging .............................................................................................................................. 77
Follow-up .......................................................................................................................... 78
Salivary Glands ......................................................................................................... 79
Clinical background ......................................................................................................... 79
Who should be imaged? .................................................................................................. 79
Staging objectives ........................................................................................................... 79

67
Staging .............................................................................................................................. 79
Follow-up .......................................................................................................................... 80
Tips ................................................................................................................................... 80
Oral cavity & oropharynx ......................................................................................... 81
Clinical background ......................................................................................................... 81
Who should be imaged? .................................................................................................. 81
Staging objectives ........................................................................................................... 81
Follow-up .......................................................................................................................... 82
Tips ................................................................................................................................... 82
Thyroid cancer .......................................................................................................... 83
Clinical background ......................................................................................................... 83
Who should be imaged? .................................................................................................. 83
Staging objectives ........................................................................................................... 83
Staging .............................................................................................................................. 84
Follow-up .......................................................................................................................... 85
Tips ................................................................................................................................... 85
Metastatic Cervical Disease With Unknown Primary ............................................. 86
Clinical Background ........................................................................................................ 86
Staging Objectives ........................................................................................................... 86
Staging .............................................................................................................................. 86
Tips ................................................................................................................................... 87
Imaging For Distant Spread ..................................................................................... 88
Clinical Background ........................................................................................................ 88
Staging Objectives ........................................................................................................... 88
Staging .............................................................................................................................. 88

68
Introduction These guidelines have been drawn up to serve the new North of England Cancer Network. They are derived from the Royal College of Radiologists document: Recommendations for Cross-Sectional Imaging in Cancer Management, 2006 and they are reproduced here with the kind permission of that college. In drawing up these guidelines we have attempted to represent the working practices of Radiologists across the network and they should serve as a guideline for developing local protocols. I would like to acknowledge the help of Dr. Simon England and Dr Ursula Schierle, Consultant Radiologists at Sunderland Royal Hospital for their help and guidance with this document. Andy Burns Chair Head and Neck NSSG (until March 2011) North of England Cancer Network

69
Head & Neck Cancers Introduction
Cancers of the head and neck mostly arise from the mucosal surfaces of the upper aero-digestive tract (most are thus squamous cell tumours). The T-staging which indicates the extent of the primary tumour is generally similar but differs in specific details related to the anatomical site of the primary tumour. In general, the N-classification is uniform for all anatomical sites except for nasopharynx and thyroid because of differing tumour biology and prognosis. The status of regional lymph nodes provides such important prognostic information that nodes should be assessed in detail in terms of location, multiplicity, size, neurovascular involvement and extra-nodal tumour spread. Not only is it important to note whether upper or lower neck lymph nodes are involved (the dividing line is the lower border of the cricoid) but it is important that specific anatomical sub-sites are included / excluded as being involved. As far as possible, neck nodal sites should be identified by nature and level to facilitate understanding between the radiologist and the clinician of sites of disease (e.g. submental [level 1A], upper deep cervical [level 2], etc.). These nodal levels conform to surgical landmarks identified at the time of surgical neck exploration. The natural history and response to therapy of metastatic nodal disease from the nasopharynx differs from tumours arising from other mucosal sites which require a different N-classification. Similarly, nodal involvement in well differentiated thyroid cancer does not significantly alter patient prognosis and thus a unique N-staging has been developed. 18FDG PET is an effective technique for imaging head and neck cancer. It has a higher sensitivity than CT for detecting lesions due to the difficulty of visualising small soft tissue tumours within the complex anatomy of the region. 18FDG PET also has a high specificity. Where available, it should be used as an adjunct to CT and MRI staging, providing more accurate information in assessing primary tumour extent as well as metastatic nodal disease in the neck. A significantly high proportion of occult primary tumours may be detected by PET-CT. The majority of these are in the region of the base of the tongue (MRI and CT not being sensitive with regard to small tongue tumours). 18FDG PET-CT has a major advantage over anatomical imaging in the assessment of the neck following surgery / radiotherapy, being able to detect and accurately re-stage disease recurrence.

70
Nasopharynx Clinical background
Cancer of the nasopharynx is peculiar in having a unique geographical distribution (Southern China) and consistently high levels of Ebstein-Barr virus antibodies. When nasopharyngeal cancers occur in Europeans, smoking and sawmill dust are additional causative factors. Squamous cell carcinoma is the commonest nasopharyngeal malignancy and most of these tumours present late, often with lymph node metastases which can be bilateral. Tumours usually arise in the Fossa of Rosenmuller and often spread submucosally and deeply. Distant metastases occur at presentation in less than 10% of cases, with lung, bone and liver being the most common sites of spread. The incidence of distant spread of disease in nasopharyngeal cancer is higher than with other head and neck tumours; rates of 30-50% are reported for N3 disease (i.e., metastasis in a lymph node greater than 6 cm in size and/or supraclavicular nodal enlargement). Many cases are detected on routine scanning for non-specific nasal or otalgic symptoms. Radiotherapy is the mainstay of treatment and imaging is designed to evaluate patients for this. Who should be imaged?
CT is often performed as the initial investigation for non-specific sino-nasal symptoms. If this demonstrates advanced disease, no further imaging is required. Consideration should be given to the use of MRI for soft tissue extension and base of skull involvement where this may alter subsequent management. The aim of imaging is to document local extent of tumour, particularly erosion into the skull base, and the presence and extent of nodal metastases. The stage of the disease can significantly alter the choice of radiotherapy technique used. The TNM staging system has been modified to take account of the additional information now available from MRI scanning, and it should be noted that CT generally over stages nasopharynx cancer compared to MRI. MRI is the imaging modality of choice for detecting perineural spread, detailed assessment of soft tissue extent. Assessment of skull base invasion will require a combination of CT and MRI. In clinically advanced disease at presentation, CT may be adequate to assess the primary tumour and extent of nodal spread. Staging objectives
To identify extent of local tumour. To identify extent and distribution of lymph node metastases. To identify organs at risk for radiotherapy damage.

71
Staging
CT CT is not as accurate as MRI for assessing the soft tissue extent of the tumour (T-staging) but is important for detecting bone involvement.
3 mm axial sections using spiral technique, following intravenous contrast enhancement through skull base and neck.
Using MDCT, slice thickness will depend on scanner capability. In general, sections are acquired at 1.25-2.5 mm and reformatted no greater than 3-5 mm for viewing.
Values of CTDIvol should normally be below the relevant national reference dose for the region of scan and patient group. MRI T-staging is best achieved with imaging in multiple planes. Contrast enhancement, with gadolinium containing chelates with or without fat suppression, is recommended for demonstration of perineural spread. A combination of axial, coronal and sagittal imaging is usually required for full assessment and treatment planning. MRI is as accurate as CT for N-staging of the neck. The area from the skull base (top of clinoids) down to suprac lavicular fossa should be included in the examination. Protocol for Imaging Nasopharynx Tumours
Sequence Plane Slice Thickness Field of View Reason
STIR T1W T2W Fat Sat T1W
Coronal Coronal Axial Axial
3mm (max) 3mm 3mm 3mm
Small Small Small Small
Identification of primary tumour and survey of neck nodes
T1W + Gad Fat Sat
Axial 3mm Small To look for perineural spread.
T1W + Gad Fat Sat
Coronal 3mm Small To look for perineural spread and intracranial extension.
T1 + Gad Sagittal 3mm Small Aid to radiotherapy planning.
PET-CT

72
18FDG PET-CT is a useful technique for the detection and re-staging of post-treatment disease recurrence. Follow-up
Reassessment imaging is often performed 3 months following completion of radiotherapy. It is advisable to use the same technique employed for initial staging at follow-up. Further imaging follow-up usually then depends on disease status and clinical symptoms. Tips
Imaging head and neck tumours in general does not determine the decision to
treat the neck nodes – this is based on the primary tumour site and the pathology.
The nasopharynx does not usually revert to normal following radiotherapy. Residual soft tissue effacement is generally seen even after successful treatment.

73
Larynx Clinical background
This is the commonest head & neck cancer site. Significant imaging developments have improved our ability to detect deep spread that may be clinically occult. Patterns of spread can alter the treatment strategy which is usually either surgery or radiotherapy. Separate primary site classification systems are used for supraglottic, glottic, and subglottic tumours. Vocal cord fixation upstages all tumours to T3 classification. Cartilage invasion is often clinically occult but upstages tumours to T4. Imaging is more accurate than clinical staging and has a major role in the asessment of potential larynx-preserving surgery techniques. Surgery or radiotherapy may be used as the primary treatment depending on the stage of disease. Cartilage invasion is generally considered an indication for more radical surgery. The lymphatic drainage of the larynx is complex. It depends on the site of the tumour and the depth of invasion. The glottis has a very sparse lymphatic network whereas the supraglottic and subglottic larynx both have very rich lymphatic networks. Contralateral nodal involvement is common but it should be noted that midline nodal disease is considered unilateral. Who should be imaged?
The diagnosis of larynx cancer is made on laryngoscopy. The contribution of imaging is to complement endoscopy by assessing the cartilages, the subglottic space and the tongue base, in particular. Cross-sectional imaging is recommended for T2 lesions or above. Lower stage tumours may not be detectable on imaging, but imaging may be indicated where clinical assessment is difficult, or early subglottic disease is suspected. CT is generally preferred as the imaging technique of choice because of speed of acquisition and patient tolerance. MRI is the best technique for assessing pre-epiglottic space and tongue base invasion. MRI is effective at demonstrating intracartilagenous tumour spread. Staging objectives
To identify extent of local tumour. To identify extent and distribution of lymph node metastases. To identify evidence of cartilage invasion.
Staging
CT
1-3 mm axial sections from hard palate, parallel to inferior border of mandible, down to thoracic inlet with intravenous contrast medium injection. Arms down by the patient’s side. Instruct patient not to swallow during data acquisition which lasts only a few seconds.

74
Using MDCT, slice thickness will depend on scanner capability. In general, sections are acquired at 0.625-1.25 mm and reformatted no greater than at 3 mm for viewing.
CT of the thorax is indicated to evaluate for metastatic disease and second primary.
Values of CTDIvol should normally be below the relevant national reference dose for the region of scan and patient group. MRI MRI is useful in specific situations such as assessing possible pre-epiglottic space and tongue base invasion, and possible early cartilage invasion. Degraded images from swallowing motion artifacts are a problem that occurs particularly in patients whose airway is compromised by tumour. A combination of axial, sagittal and coronal T1W and T2W sequences may be required to assess the region of the larynx in question. Contrast medium enhancement with spectral fat suppression is useful for evaluating the extent of soft tissue involvement. PET-CT Physiological uptake of 18FDG is observed in the larynx due to vocal cord activity. Therefore, a ‘silence’ protocol is required prior to performing PET-CT studies (i.e., the patient remaining silent for an hour prior to the study; see chapter 2 for further details). 18FDG PET-CT can be useful to detect and define the extent of submucosal spread of disease. Follow-up
Imaging 3-4 months after completion of radiotherapy is useful in documenting tumour response and serves as a baseline for future comparisons. The same imaging technique should be used as for the pre-treatment evaluation. Tips
Swallowing artefact and cord palsy can both mimic tumour. Repeating the
study immediately is possible without the need for further contrast administration if it is apparent that the images are degraded by swallowing artefact.
It is essential to scan the larynx in the correct plane to avoid misinterpretation.

75
Paranasal sinuses Clinical background
Tumours of the paranasal sinuses are the least common (3-4%) of all head and neck malignancies. They are often advanced tumours at presentation and hence have a generally poor prognosis. Early disease often presents clinically as infection and may well have co-existent inflammatory change visible on imaging. The majority (80%) are squamous cell tumours and the maxillary antra are commonest sites of involvement. Other tumour histologies suggest minor salivary gland origin. Tumour spread is by direct infiltration and by perineural extension. Bone destruction is common. In contrast to other head & neck tumours, lymph node spread is uncommon. Distant spread is also uncommon (10%) and when present involves spread to the lungs and bones. Treatment for paranasal sinus tumours is usually a combination of primary surgery and adjuvant radiotherapy. The main cause of treatment failure is local recurrence. Who should be imaged?
Imaging is indicated in all patients with biopsy proven paranasal sinus cancer. A combination of CT and MRI is generally required for complete staging prior to treatment. CT is often performed as the initial investigation for non-specific symptoms. If advanced disease is demonstrated, which is not appropriate for surgical management, no further imaging is required. The role of imaging is to help plan the surgical approach and to define the radiation fields subsequently. The anatomy is complex and interactive review of imaging in MDT meetings is recommended prior to surgery. Staging objectives
To determine extent of local tumour. To identify evidence of perineural spread. To identify evidence of skull base invasion. To identify lymph node metastases.
A combination of CT and MRI is often required for full imaging assessment. CT provides the detail regarding the bone margins of the sinus at risk, while MRI yields important information about the extent of soft tissue and perineural spread. The radiologist should be familiar with the pathways of spread and those critical areas of potential tumour spread that influence operability and the choice of surgical technique. Staging
CT
1 mm axial sections using spiral technique following injection of intravenous contrast medium through the skull base and primary tumour.
Using MDCT, slice thickness will depend on scanner capability.

76
In general sections are acquired at 1 mm and reformatted no greater than 3 mm for viewing.
3 mm axial sections through the whole neck to assess lymph nodes. Coronal reformatted images are useful for pre-surgical planning.
Values of CTDIvol should normally be below the relevant national reference dose for the region of scan and patient group. MRI MRI is best for assessing skull base invasion, soft-tissue intracranial extension and perineural spread. A selection of the following sequences should be carried out according to local protocols with or without fat saturation. Protocol for Imaging Paranasal Sinus Tumours
Sequence Plane Slice Thickness Field of View Reason
STIR T1W T2W Fat Sat T1W
Coronal Coronal Axial Axial
3mm (max) 3mm 3mm 3mm
Small Small Small Small
Identification of primary tumour and survey of neck nodes
T1W + Gad Fat Sat
Axial 3mm Small To look for perineural extension
T1W + Gad Fat Sat
Coronal 3mm Small Orbital extension (maxillary and ethmoid tumours) Intracranial and cavernous sinus extension (sphenoid and ethmoid).
T1 + Gad Sagittal 3mm Small As required
Follow-up
Routine follow-up 3-4 months after completion of treatment is useful for establishing a baseline for future comparison. MRI is more helpful than CT, and evaluating radiologists should be familiar with the expected post-surgical changes. Tips
Differentiation of tumour from retained secretions can be difficult, and is best
achieved with contrast-enhanced MRI.

77
Hypopharynx Clinical background
The hypopharynx extends from the hyoid bone superiorly down to the postcricoid region inferiorly. It includes the posterior pharyngeal wall, the piriform sinuses and the postcricoid region. Over 95% of tumours arising here are of squamous cell type. Bulky submucosal spread is typical (resulting in clinical understaging at endoscopy) and the majority have lymph node metastases to the neck at presentation. Definitive treatment may involve surgery or radiotherapy. Who should be imaged?
All patients with biopsy-proven hypopharynx cancer require cross sectional imaging for staging. Staging objectives
To determine extent of local tumour. To identify evidence of midline involvement. To identify evidence of cartilage invasion. To identify lymph node metastases. To identify involvement of apex of piriform sinus
Staging
CT
2-3 mm axial sections using spiral technique from hard palate to supraclavicular fossa following intravenous contrast medium enhancement.
Using MDCT, slice thickness will depend on scanner capability. In general sections are acquired at 1.25 – 2.5mm and are reformatted no
greater than 3 mm for viewing. Values of CTDIvol should normally be below the relevant national reference dose for the region of scan and patient group. MRI MRI is best for assessing soft tissue extent and a selection of the following sequences should be performed with or without fat saturation according to local protocols.

78
Protocol for Imaging Hypopharynx Tumours
Sequence Plane Slice Thickness Field of View Reason
STIR T1W T2W Fat Sat T1W
Coronal Coronal Axial Axial
3mm (max) 3mm 3mm 3mm
Small Small Small Small
Identification of primary tumour and survey of neck nodes
T1W + Gad Fat Sat
Axial 3mm Small
T1W + Gad Fat Sat
Coronal 3mm Small
PET-CT 18FDG PET-CT is useful for determining the extent of primary disease and also for re-staging post-treatment disease recurrence. Follow-up
Follow-up imaging 2-3 months after treatment is useful to establish a baseline for future comparison.

79
Salivary Glands Clinical background
The major salivary glands are the 3-paired parotid, submandibular and sublingual glands. Generally, the smaller the salivary gland, the more likely it is that any tumour arising within it will be malignant. Thus, benign parotid tumours are not that uncommon and are often 18FDG PET-positive. Tumours in the parotid glands arise from a variety of tissue elements, but superficial lobe tumours are more likely to be benign, while deep lobe tumours are often malignant. Malignant parotid tumours tend to be painful, rapidly growing and associated with facial nerve paralysis. The commonest benign parotid tumours are the pleomorphic adenoma (usually solitary) and Warthin’s tumour (frequently multiple and bilateral). Mucoepidermoid and adenocystic carcinomas are the most common malignant tumours. Lymph node spread is less common than with other head and neck tumours, and distant spread is usually to the lungs. The parotid has a rich network of lymphatic vessels and intra-parotid nodal involvement is often the site of metastatic disease, particularly from scalp tumours. Parotid nodal enlargement may also be seen in lymphoma. Treatment of malignant disease is usually a combination of surgery and adjuvant radiotherapy. Who should be imaged?
All patients with biopsy-proven or suspected salivary gland tumours require imaging with MRI. A definite role exists for ultra sound scanning and ultra sound guided fine needle aspiration biopsy. Staging objectives
To determine extent of local tumour. To identify lymph node metastases to the neck.
Staging
MRI MRI is the imaging modality of choice for staging salivary gland tumours. The soft tissue resolution and multiplanar imaging are necessary for surgical planning and radiation field planning. A selection of the following sequences should be performed with or without fat saturation according to local protocols.

80
Protocol for Imaging Salivary Gland Tumours
Sequence Plane Slice Thickness Field of View Reason
STIR T1W T2W Fat Sat T1W
Coronal Coronal Axial Axial
3mm (max) 3mm 3mm 3mm
Small Small Small Small
Identification of primary tumour and survey of neck nodes
T1W + Gad Fat Sat
Axial 3mm Small To look for perineural spread
T1W + Gad Fat Sat
Coronal 3mm Small To look for perineural spread and assess intracranial extension.
PET-CT The salivary glands usually demonstrate moderate physiological 18FDG uptake on PET-CT. Furthermore, salivary gland tumours can have a variable appearance on 18FDG PET-CT and some tumours do not demonstrate any significant 18FDG uptake. Therefore, the technique does not have a major role in the assessment of primary salivary tumours. Follow-up
Follow-up MRI is useful 2-3 months after completion of treatment to establish a baseline for future comparison. Tips
Intraparotid lymph nodes can mimic primary salivary tumours on imaging. Tumour characterisation is usually not required for management. Intraparotid lymph node enlargement due to other malignancies such as
lymphoma is clearly shown on 18FDG PET-CT.

81
Oral cavity & oropharynx Clinical background
Squamous cell tumours are the commonest histological subtype of tumours of the oral cavity and oropharynx and are associated with tobacco and alcohol exposure. Staging systems are based more on tumour size than on depth or extent, although it is the depth of invasion that determines the primary therapeutic approach. In the oral cavity, most tumours tend to arise along the dependent portions. Most floor of mouth tumours occur within 2 cm of the midline. Tongue tumours usually arise from the lateral aspects of the posterior two-thirds of the tongue. Buccal mucosal tumours generally arise from the inner aspects of the cheeks. Gingival tumours arise from the mucous membrane covering the floor of mouth, mandible and maxilla, and have well-defined patterns of spread that define their surgical management. The retromolar trigone is a small triangular region posterior to the last molars and tumours arising here have complex patterns of spread. Tongue base tumours are often clinically silent and often present with neck lymphadenopathy. The treatment of these tumours involves a combination of surgery and adjuvant radiotherapy. Neoadjuvant chemo-radiotherapy is under assessment. Who should be imaged?
All patients with biopsy-proven or suspected malignant oral disease should be imaged using CT or MRI depending on local protocols. Staging objectives
To determine extent of local tumour. To identify evidence of deep invasion particularly of the masticator space,
tongue and into the submandibular space. To identify evidence of bone invasion of the mandible and maxillary. To identify lymph node metastases to the neck.
Staging CT
2-3 mm axial sections using spiral technique following injection of intravenous contrast medium through the skull base and primary tumour.
Using MDCT, slice thickness will depend on scanner capability. In general, sections are acquired at 1.25-3 mm and reformatted no greater than 3 mm for viewing.
3-5 mm axial sections through the whole neck to assess lymph nodes. Values of CTDIvol should normally be below the relevant national reference dose for the region of scan and patient group.

82
MRI MRI is the preferred imaging technique and is highly dependent on the site of the primary tumour. Sequences should involve those through the neck and the primary site. A selection of the following sequences should be carried out according to local protocols with or without fat saturation. Protocol for Imaging Oral Cavity and Oral Pharynx Tumours
Sequence Plane Slice Thickness Field of View Reason
STIR T1W T2W Fat Sat T1W
Coronal Coronal Axial Axial
3mm (max) 3mm 3mm 3mm
Small Small Small Small
Identification of primary tumour and survey of neck nodes
T1W + Gad Fat Sat
Axial 3mm Small
T1W + Gad Fat Sat
Coronal 3mm Small
T1 + Gad Sagittal 3mm Small Tongue base tumours
Fat Sat Sagittal 3mm Small Epiglottic extension
PET-CT The normal palatine tonsils are almost always identified on 18FDG PET-CT, showing moderate uptake of 18FDG. There is overlap between these physiological appearances and uptake observed in primary malignancy, but asymmetrical uptake (in the absence of a tonsillectomy) in the correct clinical context should raise suspicion 18FDG PET-CT may be useful for nodal staging. Follow-up
Follow-up MRI is useful 2-3 months after completion of treatment to establish a baseline for future comparison. Tips
Superficial mucosal tumours of the tongue and buccal mucosa can be difficult
to visualise. The orthopantomogram is an important complementary imaging technique for
assessment of bone involvement of the mandible. Intense uptake of 18FDG can be observed in inflammatory conditions.

83
Thyroid cancer Clinical background
Clinical thyroid cancer is uncommon (0.5% of all cancer deaths) although there is a high frequency of occult tumours identified at post-mortem. Most thyroid cancers are relatively indolent tumours that have a chronic clinical course with infrequent metastatic disease. Papillary cancer is the most common histological type and is more frequent in iodine-rich areas. It is the main cancer induced by radiation exposure in childhood and characteristically has lowgrade malignant potential. Lymph node spread is a feature but often remains localised to the nodes without further spread. Distant spread is uncommon and the prognosis is generally excellent. Follicular cancer tends to occur in iodine-deficient areas. Unlike papillary cancer, follicular cancer rarely spreads to the nodes but can metastasise to the lungs, bones and liver. Anaplastic cancer is the most aggressive type with a poor prognosis. Medullary cancer can be sporadic or familial, and the serum calcitonin levels are usually elevated. Treatment depends on the histological type of tumour. Papillary cancers are treated surgically and radioiodine ablation can only be used post-operatively when all residual thyroid tissue has been removed. Follicular cancers are managed by total thyroidectomy and radio-ablation. Anaplastic cancers usually require radiotherapy. Medullary cancers are treated by surgery and / or radiotherapy in the early stages with chemotherapy for advanced disease. Who should be imaged?
For low volume and early stage disease pre-operative imaging is seldom required as surgery is the primary management. MRI or CT scanning is indicated when there is suspicion of tumour extension into the larynx, trachea or retrosternally into the mediastinum. MRI is the preferred imaging technique because the iodine contrast used for CT scanning may delay post-operative radio-iodine therapy. Staging objectives
To determine extent of local tumour. To identify lymph node metastases to the neck. To identify evidence of metastatic spread.
Both CT and MRI are used for thyroid cancer staging but contrast-enhanced CT may not be appropriate if management is to include diagnostic and therapeutic scanning with Iodine131.

84
Staging
USS Ultra sound scan has a definite role in the investigation of thyroid pathology and is often the first line investigation. Fine needle aspiration biopsy should be carried out with ultra sound guidance to help establish the histological diagnosis, and ultra sound can be used to stage the neck. CT The entire neck should be scanned to include the supraclavicular fossae using 3-5 mm thick sections. It should be clearly indicated by the referring clinician whether or not iodine contrast enhancement can be used. Consideration should be given to the use of gadolinium if iodine contrast is contra indicated. The thorax may be scanned without intravenous contrast to identify pulmonary metastases.
Using MDCT, slice thickness will depend on scanner capability. In general, sections are acquired at 1.25-2.5 mm and reformatted no greater than 3 mm for viewing
Values of CTDIvol should normally be below the relevant national reference dose for the region of scan and patient group. MRI MRI is the preferred imaging of choice for determining the local extent of thyroid cancer. Axial and coronal sequences with gadolinium enhancement are used as for other head and neck tumour sites. For patients who are claustrophobic and cannot tolerate MRI, CT imaging with gadolinium contrast enhancement should be performed. A selection of the following sequences should be carried out according to local protocols with or without fat saturation. Protocol for Imaging Thyroid Tumours
Sequence Plane Slice Thickness Field of View Reason
STIR T1W T2W Fat Sat T1W
Coronal Coronal Axial Axial
3mm (max) 3mm 3mm 5-6mm
Small Small Small Small
Identification of primary tumour and survey of neck nodes
T1W + Gad Fat Sat
Axial 5-6mm Small
T1W + Gad Fat Sat
Coronal 3mm Small
T1 + Gad Fat Sat
Sagittal 3mm Small Tongue base tumours and Epiglottic Extension
PET-CT

85
18FDG uptake is not usually observed in the normal thyroid gland. 18FDG uptake by well-differentiated thyroid cancer is low but increased 18FDG uptake is seen in moderately and poorly-differentiated histological types, such as Tall cell and Hurthle cell types. Poorly differentiated tumours show loss of iodine uptake and the observation of low iodine / high 18FDG uptake and vice versa is termed the “flip-flop” phenomenon. The predominant indication for the use of 18FDG PET-CT in thyroid cancer is in patients who have negative Iodine131 scans with elevated serum thyroglobulin levels because PET-CT permits the detection and localisaton of non-iodine avid metastases. Follow-up
Follow-up MRI is useful 2-3 months after completion of treatment to establish a baseline for future comparison. Tips
Most imaging is performed in the post-surgical setting to detect recurrences in
patients with rising serum thyroglobulin. Careful review of the retrotracheal and retrosternal regions is required. May need to avoid contrast-enhanced CT if radioiodine ablation is under
consideration. Diffuse increased uptake by the thyroid gland is an appearance most
frequently observed in inflammation (thyroiditis). If focal intense 18FDG uptake is seen in the thyroid gland it may either
represent uptake by a benign nodule, by an occult primary thyroid malignancy, or by an intrathyroid metastasis. When focal increased uptake is observed in the thyroid, an ultrasound with or without FNA is always indicated.

86
Metastatic Cervical Disease With Unknown Primary Clinical Background
Cervical metastasis from an unknown primary site represents 2 to 9% of all head and neck cancers. Histologically squamous cell carcinoma is the most common, with adenocarcinoma second most common. When investigating these patients every effort is made to identify the primary site both within and out with the head and neck region. There is an ever increasing role for PET-CT in this situation. If this is the cross sectional investigation of choice then this should be undertaken prior to examination under anaesthetic and biopsies. If biopsies are taken prior to performing PET-CT then false positive results occur. Alternatively, a CT scan can be performed and if this identifies a likely primary site then this should be biopsied. If however a CT scan does not identify a primary site, then PET-CT should then be performed prior to examination under anaesthetic and “blind biopsies”. Staging Objectives
To identify primary tumour within or out with the head and neck region To identify extent and distribution of neck node metastasis To identify distant metastasis
Staging
PET-CT The normal palatine tonsils are almost always identified on 18FDG PET-CT, showing moderate uptake of 18FDG. There is overlap between these physiological appearances and uptake observed in primary malignancy, but asymmetrical uptake (in the absence of a tonsillectomy) in the correct clinical context should raise suspicion. 18FDG PET-CT may be useful for nodal staging. CT
2-3 mm axial sections using spiral technique following injection of intravenous contrast medium through the skull base down to the level of the cricoid.
Using MDCT, slice thickness will depend on scanner capability. In general, sections are acquired at 1.25-3 mm and reformatted no greater than 3 mm for viewing.
3-5 mm axial sections through the whole neck to assess lymph nodes - include chest, abdomen and pelvis depending on histology of the lymph node.
Values of CTDIvol should normally be below the relevant national reference dose for the region of scan and patient group. MRI

87
MRI is best for assessing soft tissue extent if other imaging modalities identify a primary. A selection of the following sequences should be performed with or without fat saturation according to local protocols. Protocol for Imaging Metastatic Cervical Disease With Unknown Primary
Sequence Plane Slice Thickness Field of View Reason
STIR T1W T2W Fat Sat T1W
Coronal Coronal Axial Axial
3mm (max) 3mm 3mm 3mm
Small Small Small Small
Identification of primary tumour and survey of neck nodes
T1W + Gad Fat Sat
Axial 3mm Small
T1W + Gad Fat Sat
Coronal 3mm Small
Tips
Avoid any biopsies prior to PET-CT Do not allow relentless pursuit of an unknown primary to delay treatment

88
Imaging For Distant Spread Clinical Background
Approximately 4% of newly diagnosed head and neck cancer patients have thoracic malignancy (either distant metastasis or a second primary cancer). The majority of these are identified as having stage IV disease or recurrent disease prior to imaging. Investigation for distant spread in early stage disease can be limited to plain chest x-ray. However in more advanced disease and in cases of recurrence CT scan should be performed. Eye to thigh PET CT should be considered when radical treatment of the head and neck primary is planned. Staging Objectives
To identify presence of distant metastatic spread. To identify synchronous primary disease.
Staging
CT Post contrast scan with 5mm slices through thorax and upper abdomen. PET –CT Eye to thigh PET CT should be considered when radical treatment of the head and neck primary is planned.

89
Appendix 7- Chemotherapy Protocols
NECN CHEMOTHERAPY TREATMENT ALGORITHM FOR HEAD & NECK “Quality and safety for every patient every time”
Document Control
Prepared By
Issue Date
Approved By Review Date
Version Contributors Comments/ Amendment
NSSG 21.08.14 Chemotherapy group
Sept 2015
1.1 Chemotherapy Group Chair
For more information regarding this document, please contact: NSSG Chair: Dr E Aynsley

90
INTRODUCTION The 2014 Peer Review Chemotherapy Measures require each Network Site Specific group (NSSG) to agree in consultation with the Network Chemotherapy Group (NCG) a set of site specific chemotherapy treatment algorithms for the Network. Peer Review Definitions Chemotherapy treatment algorithm A guideline which specifies the acceptable ranges of regimen options for named steps on the patient pathway. Treatment algorithms are cancer site-specific. Thus, the treatment algorithm for the Head and Neck NSSG includes a statement of the range of regimens agreed as acceptable Chemotherapy The term 'chemotherapy' refers to the use of those cytotoxic agents commonly understood and accepted as being covered by this term and includes other agents such as, biological therapy and small molecule tyrosine kinase inhibitors used for the systemic treatment of cancer. In NECN Treatment Algorithms are included in each NSSG’s Clinical Guidelines which can be found under the tumour specific page of the guidelines section of the website, e.g. for Lung Cancer SUPPORTING DOCUMENTS As new regimens are approved by NICE / NHS England protocols for use of the new treatment will be uploaded to the chemotherapy site specific pages. The NSSG will be asked to update their algorithm with each new treatment approval. The availability of the Cancer Drug Fund (CDF) has increased the number of treatments potentially available to patients. CDF funded drugs may not be included in the NSSG clinical guidelines due to the dynamic nature of CDF funding (i.e. treatments can be removed as well as added). Any deviation from the algorithm should be recorded by the local Trust clinical chemotherapy service and brought to the NCG for discussion. The Area Team Policy on managing deviations from approved protocols/ algorithms is on the website:

91
HEAD & NECK ALGORITHIM Head and Neck Cancer Chemotherapy for NSSG Neoadjvuant Neoadjuvant chemotherapy is recommended for patients with bulky nodal disease. Docetaxel, cisplatin and 5FU (TPF): Docetaxel 75mg/ m2 IV day 1, Cisplatin 75-80mg / m2 IV day 1 and 5- Fluorouracil 750-1000mg/m2 IV day 1 to 4 using 48hour infusor x 2 repeated every 21 days up to 3 cycles Cisplatin and 5FU: Cisplatin 80mg / m2 IV day 1 and 5- Fluorouracil 1000mg/m2 IV day 1 to 4 every 21 days up to 3 cycles Concurrent Weekly Cisplatin 35-40mg/m2 repeated for 6 weeks with radical radiotherapy Cetuximab 400mg/m2 (Loading Dose) given one week prior to radiotherapy, weekly maintenance dose of 250mg/m2 until end of radiotherapy. For patients of good PS but contraindication to cisplatin; or as part of De-escalate trial 3 weekly Cisplatin 100mg/m2 (in trials) Palliative Cisplatin/carboplatin and 5FU (+/- cetuximab). Cetuximab is via Cancer Drugs Fund, must have PS 0/1 Docetaxel 75mg/m2 second line regimen if of good PS. Other Regimens: Epirubin/Cisplatin and 5FU (ECF) Carboplatin and etopside for small cell