Head and Neck Cystic Lesions
description
Transcript of Head and Neck Cystic Lesions
PowerPoint Presentation
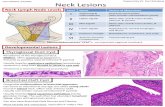
Thyroglossal Duct Cyts:Thyroglossal duct cysts are the result of a cystic dilatation of the thyroglossal duct. The normal location of a thyroglossal duct cyst is the midline of the anterior neck , in the region of the hyoid bone. The cysts are lined by columnar or squamous epithelium and may contain thyroid tissue in their walls.Embryologically, the thyroglossal duct is formed in the course of the development and descent of the thyroid gland from the foramen cecum in the tongue to its normal location in front of the trachea. Normally, the thyroglossal duct disappears. However, it may persist and may become cystic, probably as a result of secretion from the mucosal lining cells.2On very rare occasions, a papillary thyroid carcinoma may arise within a thyroglossal duct cyst. Fine needle aspiration of a benign thyroglossal duct cyst usually yields colloid material, sometimes containing a few mature squamous or columnar epithelial cells. DD: In order to correctly interpret the material present in the smear, one has to know the precise location of the mass because, by cytology alone, it may be difficult to differentiate thyroglossal duct cyst from a colloid goiter.A TDC with squamous lining and lymphoid tissue may be difficult to differentiate from a branchial cleft cyst3Branchial cleft cystsBranchial cleft cysts are congenital cysts that are located in the lateral aspect of the neck. They are the result of developmental anomalies of the branchial clefts.The cysts may remain occult until middle or older age and may appear suddenly. The branchial cysts may become inflamed and clinically painful. The cysts are usually lined by mature squamous epithelium supported by a stroma rich in lymphoid tissue, sometimes forming mature lymph follicles.Occasionally, the squamous epithelium is less mature and is composed of smaller squamous cells of parabasal type with large nuclei.On rare occasions, part of the cyst lining will be composed of mucus-producing columnar cells.
Cytology:
Aspiration usually yields thick, very turbid, white or yellow fluid. The cysts may disappear after complete aspiration of the contents, resulting in cure. may recur and the fluid can reaccumulate. Microscopically, the fluid contains a variable number of mature squamous cells and acellular squames, proteinaceous material, cellular debris, and lymphocytes. Less often, and particularly in the presence of inflammation, the squamous cells may be smaller, of a parabasal or even basal type, and may show nuclear enlargement, some hyperchromasia, or even pyknosis.The smear back ground may show evidence of acute or subacute inflammation and sometimes may contain granulation tissue, characterized by numerous capillaries, fibroblasts, and mono- and multinucleated macrophages.Branchial cleft cysts must be differentiated from metastatic squamous cell carcinoma, especially the well-differentiated, keratin-forming type that may become cystic. The degree of cellular atypia in a branchial cleft cyst may mimic carcinoma, and conversely, the cells of squamous carcinoma may be so well-differentiated that they may mimic a branchial cleft cyst.Branchiogenic carcinoma or primary cervical neoplastic cysts:1. The cervical tumour occurs along the line extending from a point just anterior to the tragus, along the anterior border of the sternocleidomastoid muscle, to the clavicle;2. The histologic appearance must be consistent with an origin from tissue known to be present in the branchial vestigial;3. No primary source of the carcinoma should be discovered during follow-up for at least 5 years;4. Cancer arising in the wall of an epithelium-lined cyst situated in the lateral aspect of the neck can be demonstrated histologicallyCervical Thymic CystFaulty development of the third and fourth pharyngeal pouches results in abnormalities of the thymus and parathyroid glands.They are found in the anterior triangle of the neck along the normal path of descent of the thymus, with or without parathyroid glands, and they have a fibrous band or a solid thymic cord connection to the pharynx or mediastinum
The thymus develops as paired structures from the third branchial pouch in the 6th week of gestation. The endodermal primordium of the thymus has a ductal or luminal connection to the pouch that is known as the thymopharyngeal duct.
9Less common overall. Males >> females. They can be found anywhere from the angle of the mandible to the sternum, paralleling the sternocleidomastoid muscle and normal descent of the thymus. 67% in less than 10 yrs.unilocular or multilocular. The epithelial lining may be cuboidal, columnar, or stratified squamous. epithelium may be replaced by fibrous or granulation tissue containing cholesterol clefts and multinucleated giant cells. To qualify a cyst as a CTC, thymic tissue must be found within the cyst wallThe differential diagnosis includes the other developmental cysts of the neck, as well as rare cystic presentations of Hodgkins disease, thymoma, and germinoma.Cervical Bronchogenic CystUncommon congenital lesions found in the skin or subcutaneous tissue in the suprasternal notch or manubrium sterni, rarely in the anterior neck or shoulder. Derived from small buds of diverticula that separate from the foregut during formation of the tracheobronchial tree. When they occur outside the thoracic cavity, the cyst presumably arises from erratic migration of sequestered primordial cells.Discovered at or soon after birth and appear as asymptomatic nodules that slowly increase in size or as draining sinuses exuding a mucoid material. They are more common in maleThe cysts range from 0.3 to 6 cm in size. They are lined by ciliated, pseudostratified columnar epitheliumIf the cyst is infected squamous epithelium is found. The cyst wall contains smooth muscle, elastic fibres and seromucous glands.A bronchogenic cyst can be distinguished from a teratoma by a complete absence of tissues other than those that can be explained on the basis of a malformation. The lack of ciliated epithelium distinguishes a lateral cervical cyst containing gastric mucosa from a cervical bronchogenic cyst. TDC can be differentiated from a bronchogenic cyst by finding thyroid folliclesDermoid CystThe term dermoid cyst should be reserved for a cystic neoplasm that originates from the ectoderm and mesoderm; endoderm is never found in these cysts. The head and neck area is a common site - located in the skin and subcutaneous tissues. The position of these dermoid cysts at the midline and along the lines of embryonic fusion of the facial processes is consistent with their origin by inclusions of ectodermal tissue along lines of closure at junctions of bone, soft tissue, and embryonic membranes. Dermoid cysts in the neck account for 22% of midline or near-midline neck lesions. May occur in upper neck, near the thyroid cartilage, and as low as the suprasternal notch. They may occur in people of almost any age. More than 50% are detected by the time a person is 6 years old, and approximately onethird are present at birth. The distribution between the sexes is approximately equal. Dermoid cysts range in size from a few millimetresto 12 cm in diameter. On microscopic examination they are lined by stratified squamous epithelium supported by a fibrous connective tissue wall. Ectodermal derivatives may be seen, including dermal adnexa such as hair follicles, sebaceous glands, and sweat glands

















![Evaluation of hepatic cystic lesions...treatment[5,6]. Currently, clinicians must also be aware of changes in the epidemiology of certain hepatic cystic lesions. Echinococcosis has](https://static.fdocuments.in/doc/165x107/5f0882797e708231d4225d6c/evaluation-of-hepatic-cystic-lesions-treatment56-currently-clinicians-must.jpg)

