Hamman-rich syndrome ‘primed’ by radiation? · RESPIRATORY MEDICINE (1999) 93, 136-140 Case...
Transcript of Hamman-rich syndrome ‘primed’ by radiation? · RESPIRATORY MEDICINE (1999) 93, 136-140 Case...
RESPIRATORY MEDICINE (1999) 93, 136-140
Case Reports
Hamman-rich syndrome ‘primed’ by radiation?
S. P. WHARTON AND T. K. ROGERS
Chest Clinic, Doncastev Royal Infkmary, Doncaster DN2 5LT, U.K.
Introduction
In 1933 (1) and 1944 (2) Hamman and Rich described cases of fulminating interstitial pneumonia. Such cases are rare. There is no proven treatment although steroids and immunosuppressants are used. The prognosis is poor. Radiation-induced pulmonary fibrosis and bronchiolitis obliterans organizing pneumonia (BOOP) have been described occurring about 1 year after chest irradiation, but to our knowledge no case of Hamman-Rich syndrome has been described.
Case Report
A 53-year-old woman presented with a painful right arm. She had been generally unwell for 2 weeks with breathlessness on exertion. Three years previously she had had a left-sided mastectomy for breast carcinoma and radiotherapy to the left chest wall.
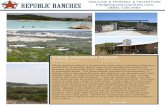
Examination revealed a tender right arm, lymphoedema of the left arm and fine inspiratory crackles at the left base. There was no pyrexia, cyanosis, clubbing, lymphadeno- pathy or dyspnoea at rest. Chest radiography revealed shadowing at the left base (Fig. 1). Venography of the right
arm and a bone scan were normal. Five days later the patient developed increasing dyspnoea and a fever of 385°C. Bilateral mid-zone crackles were present. Broncho- pneumonia was suspected and erythromycin begun. Blood gas analysis revealed a PO, of 7.6 kPa and PCO, of 3.6 kPa with a normal pH. Oxygen was administered. Two days brought no improvement. Radiographic changes were now bilateral. Lymphangitis carcinomatosa and interstitial pneumonia were considered. An autoimmune screen was negative. CT scanning was not possible due to dyspnoea. Bronchoscopy with transbronchial biopsy was performed but histology was normal. By day 16 the patient was apyrexial but deteriorating. High dose steroids were started. The decline continued with the PO, falling to 4.4 kPa despite 60% oxygen. The patient died 21 days after admission. Post-mortem examination revealed widespread changes of a Hamman-Rich type fibrosis with lesser changes of super-added infection. There was no evidence of malignant disease.
Discussion
The label ‘Hamman-Rich syndrome’ has been applied to different histological and clinical entities but we use it to
FIG. 1. Detail of chest radiograph at admission showing left basal changes. Note previous mastectomy.
Received 24 June 1998 and accepted in revised form 14 October 1998. Correspondence should be addresed to: S. P. Wharton.
0954.6111/99/020136+05 $12.00/0 0 1999 W. B. SAUNDERS COMPANY LTD
refer to a clinical picture of fulminant (sub)acute interstitial pneumonia with a histological picture dominated by interstitial elements and few acute inflammatory cells. This is similar to the ‘diffuse interstitial pneumonia’ described by Katzenstein (3). An autoimmune cause is possible. One study showed immunofluorescence in alveolar sections dis- appearing as end-stage fibrosis developed (4): but in general no convincing link has been demonstrated. We speculate that the radiotherapy given 3 years previously may have primed the lung to develop fibrosis. However, breast carci- noma is common and both diseases may have arisen by chance.
Radiation causes acute inflammation and late fibrosis in about 10% of those exposed. The delay between exposure and disease is considerable, at around 2 and 9 months respectively. Bilateral pneumontis was reported after unilateral irradiation in 1964 (5). Recent reports describe unilateral irradiation causing bilateral lymphocytic alveolitis on bronchoalveolar lavage (6,7). Additionally, cases of BOOP have been reported occurring 2-7 months after radiotherapy (8-10). BOOP has been described, con- fined entirely to the radiation field, occurring 13 yr after exposure, although causation has been disputed (11).
Radiation can cause interstitial lung disease with a con- siderable latent period. In the case described here the delay was 3 years. Latent periods can be explained by the concept of ‘priming’: ionizing radiation passing through lung tissue could damage epithelial and endothelial cells, denuding basement membranes and revealing previously hidden autoantigens. Circulating lymphocytes could be sensitized and later stimulated to produce cytopathic effects. There is thus no theoretical limit to the length of time between exposure and disease.
In presenting this case we would like to alert other clinicians to a possible association between previous radiotherapy and fulminant, late, interstitial lung disease.
References
CASE REPORTS 137
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
Il.
Hamman L, Rich A. Clinical Pathologic conference. International Clinics Forty-third Series I; 196: 1933. Hamman L, Rich A. Acute diffuse interstitial fibrosis of the lung. Bull Johns Hopkins Hasp 1944; 74: 177-212. Katzenstein ALA, Askin FB. Surgical Pathology of Nolz-Neoplastic Lung Disease. (2nd edn.), Philadelphia, PA: W.B. Saunders, 1990. Pratt DS, Schwartz MI, May JJ, et al. Rapidly fatal pulmonary fibrosis: the accelerated variant of inter- stitial pneumonitis. Thorax 1979; 34: 587-593. Smith JC. Radiation pneumonitis: case report of bilateral reaction after unilateral irradiaton. Am Rev Respiv Dis 1964; 89: 2644269. Gibson PG, Bryant DH, Morgan GW, et al. Radiation induced lung injury. Ann Intern Med 1988; 109: 288-291. Roberts CM; Foulcher E, Zaunders JJ, et al. Radiation pneumonitis: a possible lymphocyte mediated hyper- sensitivity reaction. Ann Intern Med 1993; 118: 696- 700. Kaufman J, Komorowski R. Bronchiolitis obliterans: a new clinical-pathological complication of irradiation pneumonitis. Chest 1990; 97: 1243-1244. Tobias ME, Plit M. Bronchiolitis obliterans organising pneumonia with migratory infiltrates: a late complica- tion of radiation therapy. AJR 1993; 160: 205-206. Crestani B, Kambouchner M, Soler P, et al. Migratory bronchiolitis obliterans organising pneumonia after unilateral radiation therapy for breast carcinoma. Eur Respiv J 1995; 8: 318-321. Bayle JY, Nesme P, Bejui-Thivolet F, et al. Migratory organising pneumonitis ‘primed’ by radiation therapy. Eus Respiv J 1995; 8: 322-326.