Gut Goseki histological grading gastric cancer is an ... · NodalinvolvementNO,NI,N2 1-41 4-1...
Transcript of Gut Goseki histological grading gastric cancer is an ... · NodalinvolvementNO,NI,N2 1-41 4-1...

Gut 1994; 35: 758-763
Goseki histological grading of gastric cancer is animportant predictor of outcome
I G Martin, M F Dixon, H Sue-Ling, A T R Axon, D Johnston
AbstractTNM (tumour, node, metastases) staginghas thus far been the most importantguide to prognosis in patients withgastric cancer. Histological grading, incontrast, has not provided any additionalinformation. Recently a novel gradingsystem based on tubular differentiationand mucus production has beenproposed, which was correlated withpatterns of tumour spread found atnecropsy. This study set out to assess itsvalue as a determinant of survival aftergastric resection. In a consecutive seriesof 211 patients who had potentiallycurative resection for gastric cancer, fivehistological grading systems wereassessed: the Lauren type, the WHOtype, degree of differentiation, the type oftumour border, and the lymphocyticresponse to the tumour and comparedwith the Goseki grading (I-IV). When Tand N stage were taken into account,using Cox's proportional hazards model,only the Goseki grading added further tothe ability to predict survival. Theproportional hazards ratios were: nodenegative v node positive 6 5 Ti v T3 2 45;Goseki I v Goseki IV 3- 1. Five yearsurvival of patients with mucus rich(Goseki II and IV) T3 tumours wassignificantly worse than that of patientswith mucus poor (Goseki I and III) T3tumours (18% V 53%,/ p<O0003). Gosekigrading identifies subgroups of patientswith a poorer prognosis than is predictedby TNM staging alone. It could proveuseful in the selection of patients foradjuvant therapy after potentiallycurative resection for gastric cancer.(Gut 1994; 35: 758-763)
Because of the wide variation in themorphological characteristics of gastric cancer,numerous histological classification systemshave been proposed. Jarvi2 suggested that thehistological origin of gastric cancer was withinislands of intestinal metaplasia, giving rise to theLauren classification of gastric cancers into socalled intestinal or diffuse types. Gastric cancerhas also been classified according to the degreeof differentiation exhibited by the tumour.34Ming5 proposed a classification based on thehistological appearance of the tumour border(infiltrative or expansive). Finally, the WHOproposed a morphological categorisation basedon histological appearance and type.6 Despiteinitial enthusiasm, however, for each of thesehistological classifications of gastric cancer,none has yet added to the TNM staging systemin the ability to predict outcome.
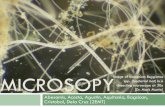
Goseki et al 7 have recently proposed a novelhistological method for classifying gastric cancerbased on intracellular mucus production andthe degree of tubular differentiation. Fourgrades of tumour were proposed (Fig 1):group I: tubules well differentiated, intracellularmucus poor; group II: tubules well differenti-ated, intracellular mucus rich; group III: tubulespoorly differentiated, intracellular mucuspoor; group IV: tubules poorly differentiated,intracellular mucus rich.The authors compared this new histological
system to the pattern of metastatic spreadfound at postmortem examination, butits relation to clinical outcome (five yearsurvival) has not yet been reported. Wedescribe here the relation between theGoseki grading system, other histologicalclassification systems, TNM staging, andclinical outcome in a consecutive series ofpatients who had received potentially curativeresection for gastric cancer.
AcademicDepartnents ofSurgery,I G MartinH Sue-LingD Johnston
Gastroenterology,A T R Axon
and Pathology, Centrefor Digestive Diseases,The General Infirmaryat Leeds, LeedsM F Dixon
Correspondence to:Mr I G Martin, AcademicDepartment of Surgery, TheGeneral Infirmary at Leeds,Great George Street, LeedsLS1 3EX.Accepted for publication13 October 1993
It has been recognised for some timethat gastric cancer exhibits wide variationin its morphology and behaviour. To date,however, the correlation between its morpho-logical characteristics and clinical behaviourhas been poor. Most clinicians have acceptedthat the morphology of gastric cancers is oflimited, if any, value in determining clinicaloutcome. The TNM (tumour, node,metastases) staging system for gastric cancerlis widely used, provides useful prognosticinformation, and is the most importantclinical method for staging adenocarcinomaof the stomach. It is widely used in manyclinical settings without reference to histo-logical morphology because the latter is felt tobe of little practical importance.
PatientsBetween 1969 and 1990, 517 patientspresented to the academic department ofsurgery with adenocarcinoma of the stomach,of whom 211 (41%) received potentiallycurative resection (defined as removal of allmacroscopic tumour, with clear resectionmargins). Most were radical (R2) resections,with extensive lymphadenectomy.8 Twentyseven of these 211 patients had intramucosalcarcinoma only. These patients wereexcluded from further analysis because thebehaviour of these lesions is well knownand any additional prognostic informationwould be marginal, and in some insufficientpathological material was available foraccurate evaluation. In three patients the
758
on Decem
ber 9, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.35.6.758 on 1 June 1994. Dow
nloaded from

Goseki histological grading ofgastnic canicer is ani important predictor of outconme
Figure 1: Haematoxylin and eosin (upper panels) and alcian blue PAS stained sections (lower panels) illustratingtypical exanmples of the four Goseki grades: (A) a tumour showing good tubulopapillary differentiationz but a poorinltracytoplasmic mucin content - grade I; (B) good tubulopapillary differentiation and plentiful intracytopasnic nmucin- grade II; (C) poor tubular differentiation and poor nmucin content - grade III; (D) poor tubular differentiation butnrch nmucini content - grade IV
pathological specimen and slides were notavailable for study. Thus 181 patients were
left for analysis. Table I shows the details ofthese 181 patients.
MethodsThe histological specimens were classifiedby one of the authors (MFD), without know-ledge of the clinical outcome, according to thefollowing systems: Goseki grade (I-IV); Laurenclassification (intestinal, mixed, diffuse); WHO
classification; Ming classification of the type ofborder (expansive, infiltrative); degree of differ-entiation (well, moderate, poor); lymphocyteinfiltration of tumour (graded 0-3; no lympho-cytes, small numbers, moderate numbers, andnumerous lymphocytes).The tumours were staged using the Unified
1987 TNM system for gastric cancer. 5
Patients were reviewed every six months at a
special gastric follow up clinic. The cause ofdeath in each case was determined from our
own records or those of the Yorkshire
759
on Decem
ber 9, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.35.6.758 on 1 June 1994. Dow
nloaded from

Martin, Dixon, Sue-Ling, Axon, J7ohnston
TABLE I Details of the 181 patients who received potentially curative resection for gastriccancer
Goseki I Goseki II Goseki III Goseki IV Total
Male:female 38:16 17:10 33:17 30:20 118:63Age (mean) 68-6 67-8 66-3 65-3 66-9Operation type
Subtotal gastrectomy: 23 15 17 29 84Total gastrectomy 27 10 29 18 84Oesophagogastrectomy 4 2 4 3 13
Tumour stageI 28 7 17 17 69II 7 8 11 10 36III 19 12 22 23 76
TABLE II The influence ofTNM staging and histologicalgrading on survival after potentially curative resection forgastric carcinoma
Five yearsurnvivalKaplan Significance
No of and Meier log rankCategory patients plot (%) test
Unified TNM staging:Ti 35 97 p<0-001T2 60 73T3 83 37T4 3 -NO 81 88 p<0-001Ni 63 56N2 37 0
Goseki grade:Goseki I 54 80Goseki II 27 44 p<0003Goseki III 50 61Goseki IV 50 46
Lauren classification:Intestinal 134 65 p<005Diffuse 36 44
WHO classification:Papillary 11 72Tubular 115 66Signet ring 9 51Mucinous 19 40Unclassified 27 42
Grade of tumour:Well differentiated 32 80 p<O 05Moderately differentiated 54 61Poorly differentiated 95 54
Ming's classification:Expansive border 42 73 NSInfiltrative border 139 56
Lymphocytic infiltration:No lymphocytes 83 56 NSLymphocytes 1 50 68Lymphocytes 2 34 60Lymphocytes 3 14 56
Regional Cancer Registry. Follow up wascomplete in all but one patient. Medianfollow up was 5-1 years. Survival was calcu-lated by the life table method of Kaplanand Meier.9 Survival curves were comparedstatistically using the log rank test.10 Thecomparative importance of various factors indetermining survival was calculated by meansof Cox's proportional hazards model.'1
Results
HISTOLOGICAL GRADING AND SURVIVALAmong the 181 patients who had potentiallycurative resection for gastric cancer, operativemortality was 6%. Cumulative survival, calcu-lated by life table analysis, after exclusion of
TABLE in Results of the application of Cox's proportional hazards model
Example ofParameter ,e hazards ratio
Nodal involvement NO, NI, N2 1-41 4-1 NOvN2 16-8Depth of tumour penetration T1, T2, T3 0-45 1-57 TI v T3 2-45Goseki grade I, II, III, IV 0-38 1-46 Goseki I v IV 3-1
operative deaths, was 60% at five years and55% at 10 years.Table II summarises the relation between
lymph node involvement (N), depth oftumour penetration (T), and survival. Fiveyear survival in patients without lymphnode metastasis was 88%; with lymph nodemetastasis, 37% (p<0001). Likewise, fiveyear survival of patients with tumour confinedto the wall of the stomach (T1 and T2) was82%, but when the tumour had penetratedthrough the serosa (T3), survival was only36% (p<0001).Table II shows the effects of the various
histological grading systems on survival,irrespective of T and N staging. The Gosekigrade, Lauren type, and grade of tumour werefound to be important predictors of outcomewhen analysed without account of T and Nstage. The WHO classification was notdesigned to predict clinical outcome and mosttumours fall in just one category (tubular); itis therefore inappropriate to apply statisticaltests across the various categories.To find out if any of these histological
grading systems added further to the T and Nstaging in predicting survival, the results wereanalysed by means of Cox's proportional haz-ards model. The histological factors thatseemed to be independently associated withsurvival after potentially curative resection forgastric cancer (see Table II) were placed inthe model together with T and N stage. Afterthe first analysis, non-contributory factors(p>005) were removed in a stepwise fashion.The final model contained only three factors:nodal involvement (N stage), depth oftumour penetration (T stage), and the Gosekigrade of the tumour. Table III shows theresults of this analysis.
Figure 2 shows the relation betweenthe Goseki histological grading system andclinical outcome. Five year survival was 80%in patients with Goseki I tumours (tubuleswell differentiated, intracellular mucuspoor) but only 46% in patients with GosekiIV tumours (tubules poorly differentiated,intracellular mucus rich) (p<0001).Of the two components of the Goseki
system, namely tubular differentiation andintracellular mucus production, mucusproduction was found to be the more impor-tant determinant of clinical outcome. Fiveyear survival of patients with tumours thatshowed good tubular differentiation (Goseki Iand II) was 69%, compared with 54% inpatients with tumours that showed poor tubu-lar differentiation (Goseki III and IV)(p<005). In contrast, five year survival ofpatients with mucus poor tumours (GosekiI and III) was 71%, but only 45% in patientswith mucus rich tumours (Goseki II and IV)(p<0 OO1). The effect of mucus productionon survival was also found to be independentofT and N staging (Figs 3 and 4).
DiscussionThe American pathologist Stout commentedin 1953 that 'histological classification was
760
on Decem
ber 9, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.35.6.758 on 1 June 1994. Dow
nloaded from

Goseki histological grading ofgastric cancer is an important predictor of outcome
08
A
A
._ d~~~~~~~~~~~~-> 0 6 <(>-A
0 04
0.
00
02
0 1 2 3 4
Survival (y)
Figure 2: Survival after potentially curative resection for gastric cancer according to theGoseki grade of the tumour.
valueless and that a knowledge of the g
appearance and spread of tumours was of nr
value in assessment of prognosis'.'2 ThiS V
has persisted for many years and there is w'spread belief among clinicians and patholo~
that histological grading of gastric cancers a
nothing fur-ther to the assessment of progn
over and above what may be derived from
T'NM stage of the tumour. This report is
first description of a histological grading sysithat shows substantial and statistically sigicant differences in survival among patients
gastric cancer, after tumour stage has btaken into account. Indeed we found that
Goseki histological grade was as importan-the depth of tumour penetration (T stage'predicting outcome using Cox's proporti(
hazards model.
1*0
08
0)
c
0.
0a0
06
04
Mucus rich, n = 3811 and IV
Mucus poor, n = 45A. I and III
,L,.A A
Q. .4
A.4~~~~~~&
A.
i ~~~~~~~~ ~~A
&Y I p<°'~~II
02
02 3 4
Survival (y)Figure 3: Survival after potentially curative resection for 83 patients with T3 gastriccancer according to mucus production.
Goseki et al based their system on twofeatures of gastric cancer: the structuralfeatures of tubular differentiation and thefunctional state of mucus production. Theystated that few would challenge the use oftubular differentiation, but believed that theuse of mucus production would be questioned
1I by others. We have shown, however, thatdegree of mucus production by the tumouris of greater importance than tubular differen-
IV tiation in the assessment of prognosis. Wetherefore support Goseki's opinion thataccumulation of mucus does not merelyrepresent the absence of a suitable tubularstructure for mucus excretion.
In Goseki's original paper the distributionof tumours among the four grades wasdifferent to that in our series with fewerpatients in Goseki grade I and proportionatelymore in Goseki grade IV. Although thereason for this is not absolutely clear there aretwo possible explanations; firstly the factthat Goseki's study was carried out onnecropsy material and hence more likely to
ross include patients with aggressive tumoursiore and secondly it is well recognised that thereniew is a higher proportion of diffuse poorlyide- differentiated tumours in Japan.gists The Lauren classification has been one ofLdds the most widely applied histological gradinglosis systems, particularly in epidemiologicalthe studies. While this system may have itsthe applications in such broad epidemiological,tem studies, there is no evidence that the Laurennifi- classification can add to the prognosticwith information that is provided by TNM staging.)een In the original description of the Laurenthe system there was an eight per cent difference in
it as survival between the intestinal and diffuse) in groups at three years (430/o v 35% respec-onal tively).13 When the Lauren classification was
applied, however, by other authors to largerseries of patients, no difference in five year sur-vival was found.'4 A further disadvantage ofthe Lauren system is that between 10 and 20%of cases remain unclassified. Ming's system,4which is based on tumour infiltration, has theadvantage over the Lauren system that all casescan be classified, but again there is no evidencethat it is of prognostic value. While the WHOclassification3 is widely used, it has severaldrawbacks; for example, it fails to classify a sig-nificant proportion of tumours and manytumours straddle two or more categories.Again, there is little evidence that the WHOclassification is important in determining clini-cal outcome, not unsurprising when it is
I<] realised that this was not the reason for theformulation of this system.
There is no evidence in published works thatany of the other histological grading systems isuseful in predicting outcome, once tumour
- spread (TNM stage) has been considered, aview that is supported by our findings. It wasdisappointing to find that the degree oflymphocyte infiltration of the tumour had
5 no apparent effect on survival. It would besatisfying if it could be shown that the body'sown immune response could be shown to havean effect on clinical outcome. This is in contrast
761
1
on Decem
ber 9, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.35.6.758 on 1 June 1994. Dow
nloaded from

762 Martin, Dixon, Sue-Ling, Axon, 3rohnston
Mucus rich, n = 2611 and IV
1-0 Mucus poor, n=37A.A land lil
~ ~ ~. .
0.8 A..
0.6'06
2 04 |-p < 0.01
CL04
0
o 1 2 3 4 5Survival (y)
Figure 4: Survival after potentially curative resection for 63 patients with Nl gastriccancer according to mucus production-
with the report of Scachenmayr, in 1979 whostated that stromal reaction had a beneficialeffect upon survival, although the evidence forthis was weak,15 and again little account wastaken ofTNM stage.Why should the differences in histological
appearance of gastric cancer emphasised byGoseki affect prognosis? The finding thatthe degree of tubular differentiation affectsprognosis should come as no surprise, butwhat is more interesting is that the amount ofmucus produced by these gastric cancersshould have such a profound effect uponclinical outcome. Mucus production has agreater impact on survival than the degree oftubular differentiation and is independent ofthe degree of tubular differentiation. We arenot the first to describe the apparently betterprognosis of tumours containing little mucus.Paile in 1971 showed a significantly poorerfive year survival in patients with tumours richin mucus. 16 In that study, however, littleaccount was taken of tumour stage and nodistinction was made between intra andextracellular mucus. Two studies have com-mented on the variable behaviour of so calledmucoid gastric carcinomas. Both Brander'7and Ishii18 showed that while signet ringcarcinomas, high in intracellular mucus,behaved in a very aggressive fashion, welldifferentiated tumours sitting in lakes ofextracellular mucus seemed to progressslowly, supporting the belief of Goseki that itis intracellular mucus that is the importantdeterminant of tumour behaviour.
It is not clear why tumours that arerich in intracellular mucus should have aworse prognosis than tumours with littleintracellular mucus. There is some evidencefrom Goseki's paper that the tumours richin mucus were associated with greaternumbers of lymph node metastasis than those
containing little mucus, although this must beinterpreted with caution given that it was apostmortem study. One research group hasshown chromosome 1 abnormalities in somepatients with gastric cancer,19 in an areaknown to code for mucus production.Whether tumours that are rich in intracellularmucus have different underlying molecularbiological abnormalities compared withtumours poor in mucus remains to bedetermined.We would propose that the Goseki classifi-
cation, if it is to be widely adopted, shouldbe changed, to transpose grades II and III,so as to reflect the greater importance ofmucus production on survival. Thus, ourproposed modification of the system wouldbe as follows: group I: intracellular mucuspoor, tubules well differentiated; group II:intracellular mucus poor, tubules poorlydifferentiated; group III: intracellular mucusrich, tubules well differentiated; group IV:intracellular mucus rich, tubules poorlydifferentiated.
It is not clear whether these findings are ofany clinical relevance. At present, we feelthat this histological grading system could notbe applied to preoperative endoscopic biopsyspecimens with any degree of accuracy,because of the small samples of tissue avail-able, although we have not formally testedthis ourselves. Nevertheless, we think thatthe Goseki classification, or our proposedmodification of it, is possibly of use in helpingto select patients for adjuvant treatment aftersurgical resection because it identifies groupsof patients in whom the prognosis is signifi-cantly worse than that predicted by TNMstaging alone. We are conscious, however,that the analysis presented here is retro-spective and based on one pathologist'sassessment of the histology. Whether thisstaging system is valid when tested prospec-tively and whether it is both repeatable andreproducible remains to be ascertained.
In summary, we have shown that the newhistological grading system proposed byGoseki provides a more accurate prognosis inpatients with gastric carcinoma when addedto the TNM staging system alone. In this, itdiffers from all other histological gradingsystems previously described. Mucus produc-tion by the tumour was found to be moreimportant in determining patients' survivalthan the degree of tubular differentiation. Ifthe Goseki system is to be widely adopted,we would propose that grades II and III betransposed to place greater emphasis on theprognostic importance of mucus production.
1 Kennedy BJ. The unified international gastric cancerstaging classification. Scanid _7 Gastroewterol 1987; 22(suppl 133): 1-13.
2 Jarvi 0, Lauren P. On the role of the heterotopias of theintestinal epithelium on the pathogenesis of gastric can-cer. Acta Pathol Microbiol Scan1d 1951; 29: 26-44.
3 Hirota T, Itabashi M, Suzuki K, Yoshida S.Clinicopathologic study of minute and small early gastriccancer. PatholAnon1 1980; 15: 1-19.
4 Ming SC. Gastric carcinoma: A pathological classification.Canlcer 1977; 39: 2475-85.
5 Kato Y, Kitigawa T, Nakamura K, Sugano H. Changes inthe histological types of gastric carcinoma in Japan.Can1cer 1981; 48: 2084-7.
on Decem
ber 9, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.35.6.758 on 1 June 1994. Dow
nloaded from

Goseki histological grading ofgastric cancer is an important predictor ofoutcome 763
6 Oota K, Sobin LH. International histological classificationof tumours No 18: histological typing of gastric andoesophageal tumours. Geneva: WHO, 1977.
7 Goseki N, Takizawa T, Koike M. Differences in the modeof extension of gastric cancer classified by histologicaltype: new histological classification of gastric carcinoma.Gut 1992; 33: 606-12.
8 Japanese Research Society for Gastric Cancer. Thegeneral rules for the gastric cancer study in surgery andpathology. 3'pn J Surg 1981; 11: 127-45.
9 Kaplan EL, Meier P. Non-parametric estimation fromincomplete observations. Jf Am Stat Assoc 1958; 53:457-81.
10 Peto R, Pike MC, Armitage P, Breslou NE, Cox DR,Howard SV, et al. Design and analysis of randomised clini-cal trials requiring prolonged observation of each patient.II Analysis and examples. BrJ' Cancer 1977; 35: 1-39.
11 Cox DR. Regression models and life tables. Jf R Statist Soc1972; 34: 187-202.
12 Stout AP. Armed forces institute ofpathology: F65 tumours ofthe stomach, fasicle 21. Washington, DC: 1953.
13 Lauren P. The two histological main types ofgastric carcinoma. Acta Pathol Micobiol Scand 1965; 64:31-49.
14 Hawley PR, Westerman P, Morson BC. BrJ_ Surg 1970;57: 877-83.
15 Schachenmayr W, Haferkamp 0. Prognostic significanceof stromal reaction in gastric carcinoma. In: HerfarthCh, Sclag P, eds. Gastric cancer. Berlin: Springer Verlag,1979: 182-92.
16 Paile A. Morphology and prognosis of carcinoma of thestomach. Ann Chir Gynaecol Fenn 1971; 60 (suppl 175):1-56.
17 Brander WL, Needham PRG, Morgan AG. Indolentmucoid carcinoma of stomach. J Clin Pathol 1974; 27:536-41.
18 Ishii T, Ikegami N, Hosada Y, Koide 0, Kanero M. Thebiological behaviour of gastric cancer. Jf Pathol 1981;134: 97-115.
19 Fey MF, Hesketh C, Wainscoat JS, Gendler S, Thein SL.Clonal allele loss in gastrointestinal cancers. Br J Cancer1989; 59: 750-4.
on Decem
ber 9, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.35.6.758 on 1 June 1994. Dow
nloaded from