Ganyang MCQ Endocrine
-
Upload
kirie-kozanegawa -
Category
Health & Medicine
-
view
4.964 -
download
0
Transcript of Ganyang MCQ Endocrine

ENDOCRINOLOGY
1. Causes of high prolactin level include :a) Prolactinomab) Acromegalyc) Craniopharygiomad) Pregnancye) Metoclopramide therapy
2. The following statements are true regarding a diabetic patient who is brought in drowsy :a) DKA is unlikely if focal neurological signs are presentb) CT scan of the brain is essentialc) The patient should be given a glucose drink orally if hypoglycemia is establishedd) Potassium supplement should be given if DKA is diagnosede) Bicarbonate should be given if blood pH less then 7.3
3. In thyrotoxicosisa) The diagnosis is confirmed by a lowered serum TSH levelb) Eye signs correlate poorly with the severity of the thyrotoxicosisc) Radioactive iodine is the first line treatment in acute thyrotoxicosis crisisd) Pretibial myxoedema is a recognized featuree) A non-selective beta blocker is preferred
4.The following are recognized features of hypothyroidism in adulta) Carpal tunnel syndromeb) Pericardial effusionc) Hyponatremiad) Cerebral ataxiae) Pretibial myxoedema
5. Addison’s disease is associated witha) Hypertensionb) Hyperglycemiac) Abdominal paind) Hypokalemia e) Hyperpigmentation
6. The following statement(s) is/are true regarding acromegalya) It is due to excessive growth hormone production by the posterior pituitaryb) Serum growth hormone increased after glucose administrationc) Occur in childrend) Impotence is one of the featuree) Can cause spade-like hands and feet
7. Causes of hyponatraemiaa) Addison’s diseaseb) Hyperthyroidismc) Cushing’s syndrome

d) Hypoalbuminaemiae) Diabetes insipidus
8. Hypokalemia can occur ina) Conn’s syndromeb) Diabetic ketoacidosisc) Diureticsd) Bartter’s syndromee) Addison’s disease
9.Causes of secondary hypertensiona) Conn’s syndromeb) Acromegalyc) Hyperparathyroidismd) Hyperthyroidism e) Cushing’s syndrome
10. Causes of Cushing’s syndrome includea) Small cell lung carcinomab) Pituitary tumourc) Bilateral adrenal hyperplasiad) Long term treatment of corticosteroide) Type 1 DM
11. Investigation for Cushing’s syndromea) serum Cab) serum ACTHc) dexamethasone suppression testd) serum cortisol in morning onlye) x-ray skull
12. Conn’s syndromea) Can cause muscle weaknessb) Is a secondary hyperaldosteronismc) Saline suppression test showed aldosterone not suppressed with saline and renin was
suppressed d) Patient presented with hypotensione) Bicarbonate may elevated
13. Causes of hypercalcaemiaa) Thyrotoxicosisb) Thiazides diureticsc) Chronic renal failured) DiGeorge syndromee) Addison’s disease

14. Hyperosmolar nonketotic DMa) Ketoacidosisb) Severe dehydratedc) One of the complication is CVAd) Severe hyperglycaemiae) Mortality is high (40%)
15. A 27 years old woman complained of polyuria and polydipsia. Possible diagnoses include :a) Central diabetes insipidusb) Conn’s syndromec) Hypoparathyroidismd) Psychogenic polydipsiae) Multiple myeloma
16. A 30 year-old woman presented with discharge from breast. On examination, there is evidence of galactorrhea. Which of the following contributes:
A. Chlorpromazine TB. Pregnancy TC. Cranial irradiation TD. Bromocriptine (DOPAMINE AGONIST) FE. Pituitary tumour T
17. The following statement is/ are true of eye diseasesa. microneurysms are hallmark of diabetic retinopathy T b. cotton wool spots indicate ischaemic fibres Tc. the presence of background retinopathy require urgent ophthalmology referral T
ANSWERS
1. Causes of high prolactin level include
a) T- A prolactinoma is a benign (non-cancerous) tumor of the pituitary gland that produces prolactin. A prolactinoma is the most common type of pituitary tumor. Symptoms of prolactinoma are caused by too much prolactin in the blood (hyperprolactinemia) or by pressure of the tumor on surrounding tissues. (http://endocrine-system.emedtv.com/high-prolactin-levels/causes-of-high-prolactin-levels.html)Prolactinomas are the most common cause of hyperprolactinemia (Harrison’s principle of Internal Medicine 16th Edition pg 2085)
b) T- Other tumors arising in or near the pituitary (such as those that cause acromegaly or Cushing's syndrome) may block the flow of dopamine from the brain to the prolactin-secreting cells. (http://endocrine-system.emedtv.com/high-prolactin-levels/causes-of-high-prolactin-levels.html)
c) T- Not sure. It doesn’t stated much on craniopharyngioma leading to hyperprolactinemia in Harrison’s or in the internet but does state that it may present with growth failure and endocrine dysfunction (Harrison’s principle of Internal Medicine 16th Edition pg 2457), also stated in the summary table 318-8 (Harrison’s Principle of Internal Medicine 16th Edition pg 2085) one of the cause is Rathke’s cyst which might be

the same as craniopharyngioma sbb cranio tu ialah sejenis calcified cystic tumor arising from the remnant of Rathke’s cleft in supracellar region (http://emedicine.medscape.com/article/1157758-overview) and 80% adults complain of decreased sexual drive and almost 90% of men complain of impotence, while most women complain of amenorrhea (http://emedicine.medscape.com/article/1157758-clinical) which is one of the signs of hyperprolactinemia.
d) T- Prolactin stimulates the breast to produce milk during pregnancy. After delivery of the baby, a mother's prolactin levels fall unless she breastfeeds her infant. Each time the baby nurses, prolactin levels rise to maintain milk production. (http://endocrine-system.emedtv.com/high-prolactin-levels/causes-of-high-prolactin-levels.html)Pregnancy and lactation is the most important physiologic cause of hyperprolactinemia (Harrison’s Principle of Internal Medicine 16th Edition pg 2085)
e) T- Prolactin secretion in the pituitary is normally suppressed by the brain chemical, dopamine. Drugs that block the effects of dopamine at the pituitary or that deplete dopamine stores in the brain may cause the pituitary to secrete prolactin. These medicines include:
The major tranquilizers trifluoperazine (Stelazine) and haloperidol (Haldol) Metoclopramide (Reglan), used to treat GERD and the nausea caused by certain cancer
drugs Methyldopa Reserpine. (http://endocrine-system.emedtv.com/high-prolactin-levels/causes-of-high-
prolactin-levels.html)
Additional info:*hyperprolactinemia may be caused by conditions other than prolactin-secreting pituitary adenomas, including pregnancy, high-dose estrogen therapy, renal failure, hypothyroidsm, hypothalamic lesion and dopamine-inhibiting drugs (reserpine, metoclopramide) (Robin’s Basic Pathology 8th Edition pg 755)*(table) summary of causes of hyperprolactinemia (Harrison’s Principle of Internal Medicine 16th
Edition pg 2085)
2. The following statements are true regarding a diabetic patient who is brought in drowsy :

a. False --- patient with DKA may present with CNS symptom(confusion, drowsiness, coma). Other sign and symptom include polyuria, thirst, weight loss, weakness, nausea, vomiting, leg cramps, blurred vision, abdominal pain, symptom of dehydration (hypotension, cold extremities, tachycardia), tachypnea, acetone breath and hypothermia. The pathophysiology of all the symptoms are hyperglycemia, hyperketonemia and metabolic acidosis.
b. False. Investigation that need to be done include a. Blood glucoseb. ABG --- acidosisc. RP --- hyperkalemia due to acidosis, high urea due to dehydration,d. Plasma bicarbonate --- to assess severity of acidosis, less than 12mmol/l indicate
severe acidosise. Urinalysis --- ketone in urinef. ECG --- patient may had cardiac symptom like arrhythmia and DKA may be
associated with other medical condition like acute MI.g. Screen for infection --- FBC, urine screening n culture, CRP, CXR because DKA is
usually induced by stress.
c. True --- hypoglycemia is charecterised by plasma glucose <3.5mmol/l. Patient may present with drowsiness due to less glucose to the brain. If patient able to swallow, then oral glucose should be given immediately after diagnosis is establish. If patient unable to swallow, iv glucose or glucagon should be given.
d. True --- in DKA, patient had metabolic acidosis. This will force hydrogen ion into cells, displacing potassium ion, which may be loss in urine or through vomiting. So, iv potassium chloride should be started but with caution. The dose should be sufficient to maintain plasma normal level.
e. False --- sodium bicarbonate infusion in DKA is controversial. It can be given in very severe acidosis pH<7.0 (300ml 1.26% over 30 minutes into a large vein) , together with potassium administration. But it only be considered in exceptional circumstances as complete correction of acidosis should not be attempted.
3. In thyrotoxicosisa) False. Diagnosis is confirmed with free T4 and suppressed TSH. Sebabnye, thyrotoxicosis
punye macam2 sebab. Ade yg sebabnye dari pituitary dan ade sebabnye dari thyroid gland itself. Jadi, jika dari thyroid gland itself (primary), thyroid hormone (T3 and T4) akan naik tanpa stimulation TSH. Sebagai compensatory mechanism, TSH akan suppress. Manakala, sebabnye yg masalah pada pituitary, ia akan stimulate TSH melebih2, menyebabkan thyroid hormone dihasilkan secara berlebihan. Oleh itu, TSH akan high. Jadi x sume thyrotoxicosis present with lowered TSH. Kene tgk T4 juge.
(from the page 10, Labarotory Investigation Practice Clinical Guidline for Thyroid Disorders The Malaysian Consensus 2000)
b) True. Eye sign correlate poorly of not correlate with the severity of thyrotoxicosis. Patient can be euthyroid, hypothyroid, or hyperthyroid at presentation.

(from page 203 line 2 and 3, thyroid eye disease, Oxford Handbook of Clinical Medicine 7th Edition.)
c) False. For acute thyroid crisis, the first line management, start with, rehydration, treat hyperpyrexia, beta sympathetic blocking agents (propanolol oral), iodide (sodium iodide, Lugol’s iodine,potassium iodide-SSKI), antithyroid drugs (Carbimazole, PTU), corticosteroid (IV dexamethasone, IV hydrocortisone). There is no radioactive iodine in management of acute thyrotoxicosis.
(from the page 16, Thyroid Crisis, Investigation Practice Clinical Guidline for Thyroid Disorders The Malaysian Consensus 2000)
d) True. Especially with Grave disease. Also eye disease and thyroid acropachy(clubbing) as clinical feature of Graves.
(from page 202 under Grave disease, thyrotoxicosis, Oxford Handbook of Clinical Medicine 7th Edition.)
e) True. Propanolol is non selective bête blocker. (from http://en.wikipedia.org/wiki/Propranolol ). Proponolol is suggested for treating thyrotoxicosis.
(from from the page 12, Medical management, last paragraph, Practice Clinical Guidline for Thyroid Disorders The Malaysian Consensus 2000)
4. The following are recognized features of hypothyroidism in adulta) T non-pitting edema of the hands can compress the nerve, thus causing Carpal tunnel syndrome, X’press revision in short cases, page 54b) T The myxedematous changes in the heart result in decreased contractility, cardiac enlargement, pericardial effusion, decreased pulse, and decreased cardiac output., http://webcache.googleusercontent.com/search?q=cache:GglonovGqsEJ:emedicine.medscape.com/article/122393-overview+pericardial+effusion+in+hypothyroidism&cdc) T unknown mechanism, possibly secondary to low cardiac output and glomerular filtration rate), associated with nonosmotic vasopressin(ADH) release and impaired sodium reabsorption, leading to hypotonic hyponatremia, http://webcache.googleusercontent.com/search?q=cache:lA5tUf0bg8cJ:emedicine.medscape.com/article/242166-overview+mechanism+of+hyponatremia+in+hypothyroidismd) Tunknown mechanism…huhu, http://www.nativeremedies.com/articles/ataxia-with-thyroid-problems.htmle) Fpretibial myxedema is the manifestation of hyperthyroidism i.e Graves, oxford handbook of clinical medicine, 7th edition, page 202
5. Addison’s disease is associated witha) F – Addison’s diseases one of primary renal insufficiency in regard of secretion of
cortisol (glucocorticoid insufficiency) and / or aldosterone (mineralocorticoid

insuffiency). Patient will present with severe hypotension, hyponatremia, hyperkalemia, hypoglycemia and hypercalcemia. Others such as muscle cramp, nausea, vomiting, diarrhea and unexplained fever. Vitiligo only 10-20% of patient. (Davidson,21st edition m/s 775)
b) F – Hypoglycemia. Answer same in Q7(a)c) T – muscle cramp (same in Q7(a))d) F- hyperkalemia due to low aldosterone level (Davidson,21st edition m/s 775)
(aldosterone function is increases the reabsorption of sodium and water and the release of potassium in the kidneys. (http://www.nlm.nih.gov/medlineplus/ency/article/003704.htm) So, decrease level of aldosterone will lead decrease potassium secretion from kidney.
e) T – hyperpigmentation is because of ACTH excess (Davidson,21st edition m/s 775 table 20.45)
6. The following statement(s) is/are true regarding acromegalya) It is due to excessive growth hormone production by the posterior pituitary F
Its from anterior pituitary. Posterior pituitary hanya produce ADH n oxytocin. Others hormone sume kat anterior pituitary (970 kumar n clerk)
b) Serum growth hormone increased after glucose administration FThe action of GH is to increase blood glucose. Sama mcm cortisol, epinephrine,n glucagon. 1030 kumar n clerk
c) Occur in children FKat children kite pgil gigantism. Acromegaly kat adult (979 kumar n clerk)
d) Impotence is one of the feature T(980 kumar n clerk)e) can cause spade-like hands and feet T (page 977 KUMAR N CLERK)
7. Causes of hyponatraemiaa. Addison’s disease Tb. Hyperthyroidism Fc. Cushing’s syndrome Fd. Hypoalbuminaemia Te. Diabetes insipidus T
a) Addison’s disease is a condition where there is insufficiency of adrenal hormone characterized by a deficiency of mineralocorticoids and glucocorticoids. Addison’s disease causeshyponatremiaas a result of low levels of aldosterone and causing increase excretion of sodium by kidney. (diagnose me.com & pathophysiology Elsevier)
b) It is hypothyroidism causes hyponatremia. http://www.mayoclinic.com/health/hyponatremia/DS00974/DSECTION=causes
c) Cushing's syndrome is caused by excessive activation of glucocorticoid receptors. By far the most common cause is iatrogenic, due to prolonged administration of synthetic glucocorticoids such as prednisolone. Non-iatrogenic Cushing's syndrome is rare, although it presents by many diverse routes and is often a 'spot diagnosis' made by an astute clinician. High mineralocorticoids cause retention of sodium in the body which leads hypernatremia. This condition will end up with hypertension. (Davidson’s principles and practice of medicine page 779

d) Hypoalbuminemia can also cause hypervolemichyponatremia. Hypoalbuminemia causes a shift of fluid from the plasma to the interstitial spaces and a decrease in serum volume, with release of ADH. A decrease in extracellular volume causes release of ADH and subsequent hyponatremia, as the patient will conserve fluid but excrete sodium. If the fluid is replaced without the sodium, the individual will remain hyponatremic. (http://www.medscape.com/viewarticle/714108)
e) There are four (4) fundamentally different types of Diabetes Insipidus (DI). Each has a different cause and must be treated in a different way. These four forms are:
Neurogenic, also known as central, hypothalamic, pituitary or neurohypophyseal is caused by a deficiency of the antidiuretic hormone, vasopressin.
Nephrogenic, also known as vasopressin-resistant is caused by insensitivity of the kidneys to the effect of the antidiuretic hormone, vasopressin.
Gestagenic, also known as gestational is also caused by a deficiency of the antidiuretic hormone, vasopressin that occurs only during pregnancy.
Dipsogenic, a form of primary polydipsia is caused by abnormal thirst and the excessive intake of water or other liquids.
Dipsogenic Diabetes Insipidus occurs when vasopressin is suppressed by excessive intake of fluids. The latter is usually referred to as primarypolydipsia and is most often caused by an abnormality in the part of the brain that regulates thirst. Thus, it also results in water intoxication, a condition associated with symptoms such as headache, loss of appetite, lethargy and nausea and signs such as an abnormally large decrease in the plasma sodium concentration (hyponatremia).(http://www.diabetesinsipidus.org/index.htm
8. AnswerSumber : kumar & clark 6th edition pg 704,705.
(a) Hyperaldosteronism water and sodium retention, hypokalemia, hypertension, muscle weakness.
(b) Not sure how to answer this question because as far as I concern, DKA does not cause hypokalemia, but the treatment of DKA does cause low potassium i.e. Insulin treatment will cause redistribution of potassium into cells (it cause glucose enter cell together with k+) causing hypokalemia. So,maybe the answer is false. *
(c) Thiazides and loop diuretics will increase renal excretion of k+. (exception: spironolactone a.k.a potassium sparring diuretic a.k.a aldosterone antagonist which inhibit aldosterone action thus water and sodium will be excreted and potassium is conserved
(d) Rare cause-defect in sodium and chloride reabsorption in the thick ascending limb of the loop of Henle. Consists of metabolic hypokalemia, alkalosis, hypercalciuria, normal BP, increase serum rennin and aldosteron.
(e) Syndrome of inadequate corticosteroid secretion weakness,lethargy,low BP, dark skin pigmentation.

9. Causes of secondary hypertensiona) T – Hyperaldosteronism promote water retension and cause hypertension Kumar Clark
7th edition pg.1023-4b) T - Visceral hypersomia such as heart hypersomia presents with hypertension, LVH,
cardiomyopathy, arrhythmia, etc http://emedicine.medscape.com/article/116366-overview
c) T –A growing body of evidence has demonstrated an increased incidence of hypertension http://emedicine.medscape.com/article/766906-overview
d) T – Thyroid hormone has important effects on cardiac muscle, the peripheral circulation, and the sympathetic nervous system that alter cardiovascular hemodynamic http://onlinelibrary.wiley.com/doi/10.1111/j.1524-6175.2006.05180.x/pdf
e) T – Excess cortisol has minerelocorticoid effect, attributing to hypertension http://emedicine.medscape.com/article/117365-overview
10. Causes of Cushing’s syndrome includea) T- Nonpituitary ectopic sources of ACTH, such as an oat cell carcinoma, small-cell lung
carcinoma, or carcinoid tumor, cause the balance of ACTH-dependent disease (http://emedicine.medscape.com/article/117365-overview#a0104)
b) T- They usually are due to an anterior pituitary tumor, that is, classic Cushing disease (80%) (http://emedicine.medscape.com/article/117365-overview#a0104)
c) T- In most cases the cause is bilateral adrenal hyperplasia due to hypersecretion of pituitary ACTH or ectopic production of ACTH by a nonpituitary source (Harrison’s Principle of Internal Medicine 16th Edition pg 2134). Primary bilateral hyperplasia of adrenal cortices is a rare cause of Cushing’s syndrome (Robin’s Basic Pathology 8th Edition pg 790)cause of Cushing.
d) T- In clinical practice, most cases of Cushing are caused by administration of exogenous glucocorticoids (Robin’s basic Pathology 8th Edition pg 789)
e) F-Cushing’s syndrome is a disorder caused by any condition that produces an elevation of glucocorticoid levels (Robin’s Basic Pathology 8th Edition pg 789), diabetes mellitus is a group of metabolic disorders sharing the common underlying feature of hyperglycemia (Robin’s Basic Pathology 8th Edition pg 775).
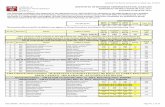
11. Investigation for Cushing’s syndromeAccording to Davidson page 780 Test for Cushing’s syndromme
a. False b. True - http://www.medscape.com/viewarticle/474901_4c. Trued. False --- kalau nak measure serum cortisol must follow the circadaian rhythume. False --- skull xray is not for diagnosis of cushing, tp nak tgk effect of high cortisol to
bone which can cause osteoporosis.
12. Conn’s syndromea) True. As Conn’s syndrome presented with hyperaldosteronism and hypokalemia.
Hypokalemia casue muscle weakness. Therefore, Conn’s syndrome cause muscle weakness.

(from page 212 under symptoms of Hyperaldosteronism, Oxford Handbook of Clinical Medicine 7th Edition)
b) False. Conn’s syndrome is primary hyperaldosteronism. Due to bilateral adrenocortical hyperplasia.
(from page 212 under causes of Hyperaldosteronism, Oxford Handbook of Clinical Medicine 7th Edition)
c) True. Saline suppression(SS) test showed failure of suppression of aldosterone and hyposecretion of renin in primary hyperaldosteronism (Conn’s syndrome). Primary aldosteronism present with rise aldosterone level while renin is reduced. Disebabkan RAAS (rennin-angiotensin-aldosterone) system. Contradict dengan secondary hyperaldosteronism, Renin would be high. Jadi, test ini menggunakan IV normal saline infusion akan menyebabkan water expension atau hypervolemic state in our body. Yg mana secara normalnya, aldosterone akan berhenti dihasilkan. Initial test should be ARR (plasma aldosterone-renin ratio) yang mane high ratio >30 suggest very high level of aldosterone, and SS is for confirmation of Conn’s
(from Harrison 17th edition, chapter 336, aldosteronism, page 2260)
d) False. Hypertension is the presentation due to mineralocorticoid effect cause sodium and water retention and potassium excretion.
(from 213 under Hypertension; a common context for hyperaldosteronism tests, Oxford Handbook of Clinical Medicine 7th Edition).
Additional 3 area of concern in Conn’s syndrome; 1-hypertension + hypokalemia, 2- refractory hypertension, 3- hypertension occurring before 40 y/o esp in women.
e) True. Bicarbonate akan elevated in the blood. Ini kerana, di proximal tubule of nephrons, acid base buffering system terjadi. Process ini bermula bersama penglibatan Na+. secara normalnya, Na+ dan bicarbonate akan di filter di glomerulus, masuk ke dalam renal tubules. Dibahagian proximal renal tubule, process, reabsorbtion of Na+ berlaku. Process ini berlaku sekali dgn excretion of H+. oleh itu, semakin banyak Na+ di reabsorb ke dalam blood, semakin banyak H+ di excreted ke dalam urine. H+ di dalam urine ini akan bergabung dgn bicarbonate yg di filter dari glomerulus tadi membentuk carbonic acid. Menggunakan enzyme carbonic anhydrase, carbonic acid di pecahkan menjadi CO2 dan H2O yang kemudiannye di bawa masuk ke dalam cells di dinding proximal tubules. Di sini, proses kimia membentuk semula bicorbanic acid dari CO2 dan H2O menggunakan enzyme carbonic anhydrase di dalam cells di proximal tubule. Bicarbonic acid ini kemudiannya terpecah menjadi bicarbonate dan H+. bicarbonate die absorb semula masuk ke dalam blood, manakala H+ di kitar semula untu di excreted out di proximal tubule (involve dalm proses pertukaran dengan Na+). Oleh itu, jika hyperaldosteronism, increase Na+ reabsorbtion which means, increase H+ excretion into the tubules. Then, increase H+ combine with bicarbonate cause more formation of carbonic acid and more carbonic acid reabsorb back from the tubules. It then change back to bicarbonate and reabsorb into the blood.

13.a. T Thyrotoxicosis can cause sufficient bone resorption to increase serum calcium in
20% of cases. http://emedicine.medscape.com/article/920955-overview .b. Tthiazide diuretics act at distal convulated tubule, by blocking Na and Cl channels at
the luminal membrane, thus decreasing the concentration of Na inside that cell. This will cause Na to enter from basal membrane thru Na-Ca countertransporter.,,thus increasing the Ca reabsorption into the blood. 2nd year lecture notes of pharmacology, tajok ‘ diuretic agent’ oleh dr chayna
c)F Hypocalcemia develops primarily from decreased intestinal calcium absorption because of low plasma calcitriol levels and possibly from calcium binding to elevated serum levels of phosphate. http://emedicine.medscape.com/article/238798-overview .
d. F DiGeorge syndrome baby have failure of third and fourth pharyngeal pouches normally during the twelfth week of pregnancy. This developmental failure results in a completely or partially absent thymus gland and parathyroid glands. The child is born with a defective immune system and an abnormally low level of calcium in the blood. http://emedicine.medscape.com/article/886526-overview.
e. TUnknown mechanism http://www.turner-white.com/pdf/hp_jan02_adrenal.pdf
14. Hyperosmolar nonketotic DMa) F - Definition HSS/HONK= the condition characterized by severe hyperglycemia
(>50mmol/L) without significant hyperketonimia or acidosis. (Davidson,21st edition m/s 812)
b) T - Hyperosmolar hyperglycemic state (HHS) most commonly occurs in patients with type 2 diabetes mellitus who have some concomitant illness that leads to reduced fluid intake. Infection is the most common cause, but many other conditions can cause altered mentation, dehydration, or both. (http://emedicine.medscape.com/article/766804-overview)
c) T – dur to viscosity increase from dehydration. http://books.google.com.my/books?id=6G86aiGXBHQC&pg=PA471&lpg=PA471&dq=hyperosmolar+hyperglycemic+state+cerebrovascular+accident&source=bl&ots=bu8XBLNRz7&sig=mk6_hJfAuuTlaeoM609JK_Gcjj8&hl=en&ei=Cm--TdurB8WIrAfns9XTDg&sa=X&oi=book_result&ct=result&resnum=10&ved=0CFMQ6AEwCQ#v=onepage&q&f=false
d) T- Same with (a). (Davidson,21st edition m/s 812)e) T – Mortality is high (40%)(Davidson,21st edition m/s 812)
15. A 27 years old woman complained of polyuria and polydipsia. Possible diagnosis include a. Central diabetes insipidus T
Page 1017 kumar n clerk
b. Conn’s syndrome FConn’s synd ialah primary hyperaldosteronism, and aldosterine causes water retention
c. Hypoparathyroidism FSpatutnyer hyperpara sb other causes of polyuria n polydipsia are hypercalcemia, hypokalemia and DM.

d. Psychogenic polydipsia T
e. Multiple myeloma TOne of the causes of hypercalcemia.
16. 21 A 30 year-old woman presented with discharge from breast. On examination, there is evidence of galactorrhea. Which of the following contributes:(List of causes - from www.endotext.org)
a. T Chlopromazine is an anti-psychotic (Neuroleptic drug) whichelevates prolactin levels; the elevation persists during chronic administration. Although disturbances such asgalactorrhoe, amenorrhea, gynecomastia, and impotence have been reported, the clinical significance of elevated serum prolactin levels is unknown for most patients.
b. T The very high levels of circulating estrogen that occur during pregnancy result in a parallel increase in the circulating levels of prolactin. The prolactin increase prepares the breasts for lactation. Prolactin levels begin to rise at 5-8 weeks into the gestation period and parallel the increase in the size and number of lactotrophs. At the end of the first trimester, serum prolactin levels are approximately 20-40 ng/mL. They increase further to 50-150 ng/mL and are 100-400 ng/mL at the end of the second and third trimesters, respectively. This is likely mediated by a direct effect on the lactotroph. A combination of factors may be responsible. Prolactin responses to normal stimuli (eg, sleep, meals, suckling) are maintained throughout pregnancy. (www.emedicine.com)
c. T Cranial irradiation is used to treat patients with primary or metastatic brain tumors and as prophylaxis for selected patients at high risk of neoplastic involvement of the nervous system. How cranial irradiation causing galactorrhoea is not well understood but based on a study done in UK, two young women developed oligomenorrhoea and galactorrhoea 4 and 7 years after whole brain irradiation for brain tumours. Both had mild hyperprolactinaemia due to irradiation-induced hypothalamic damage. In both patients, oral bromocriptine normalized prolactin levels and menstruation resumed. One patient then had a successful pregnancy. (pubmed.gov)
d. F Bromocriptine is a dopamine agonist which has inhibitory effect to the pituitary. It will inhibit the release of prolactin. Used in treatment of galactorrhoe.
e. T Both macroprolactinomas and microprolactinomas can present with galactorrhoe. Prolactinomas are the most common type of pituitary adenoma. Increase prolaction causing increase milk production in the mammary gland(from chapter 17, page 576, Fox physiology, 9th edition. )
17. The following statement is/ are true of eye disease http://www.avclinic.com/Retinal_signs.htm

(a) The earliest clinically recognizable hallmark of diabetic retinopathy is the microaneurysm. These are small round dark red dots on the retinal surface (not arising from visible vessels) that are by definition less than the diameter of the major optic veins as they cross the optic disc.
(b) Cotton wool spots are small areas of yellowish white coloration in the retina. They occur because of swelling of the surface layer of the retina, which consists of nerve fibers. This swelling almost always occurs because the blood supply to that area has been impaired and in the absence of normal blood flow through the retinal vessels the nerve fibers are injured in a particular location resulting in swelling and the appearance of a "cotton wool spot."
(c) Background (diabetic) retinopathy is the early stage of DR, need urgent ophthalmology management to prevent progression or blindness (other than good glycemic control, klau tak berjaya control DM, ada ubat untuk treat changes dlm retinopathy ni utk prevent buta).