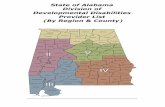
Foreign Body Ingestion in Children with Severe Developmental Disabilities: A Case Study
-
Upload
lucinda-carr -
Category
Documents
-
view
212 -
download
0
Transcript of Foreign Body Ingestion in Children with Severe Developmental Disabilities: A Case Study

Foreign Body Ingestion in Children with Severe DevelopmentalDisabilities: A Case Study
Sheena Reilly, BAppSc, PhD,1 and Lucinda Carr, MD, MBChB, DCH, MRCP, FRCPCH2
1School of Human Communication Sciences, Faculty of Health Sciences, LaTrobe University, and Royal Children’s Hospital, Melbourne,Victoria, Australia.2Neuro-disability Unit, Great Ormond Street Children’s Hospital and Institute of Child Health, London, England
Abstract. Dysphagia is common in children with severedevelopmental disabilities. The nature of these difficul-ties can predispose them to foreign body ingestion. Thisarticle presents a case that highlights the need for vigi-lance in diagnosing dysphagia in children with multipleand complex developmental disabilities where severecognitive impairment and an inability to communicatemay mask the presence of underlying problems.
Key words: Dysphagia — Foreign body ingestion —Cornelia de Lange syndrome — Developmental disabil-ity — Deglutition — Deglutition disorders.
Children with severe developmental disabilities (SDD)present a challenge to pediatric services. They are likelyto require access to specialist multidisciplinary dyspha-gia teams for management throughout infancy, child-hood, and adolescence. Although there has been increas-ing recognition of the prevalence and nature of dyspha-gia in children with complex and multiple disabilities,problems can be overlooked, particularly when they arerarely the presenting feature.
Foreign body ingestion (FBI) is a frequent and apotentially lethal occurrence in children [1]. While formany children ingested foreign bodies cause little troubleand pass through the gut uneventfully, in approximately20%–30% of children, problems may occur [2]. Symp-toms associated with FBI may include choking, cough-ing, wheezing, decrease in appetite, or refusal to eat.However, these symptoms may differ in severity and are
sometimes absent. As a result, the diagnosis of FBI maybe missed or delayed.
We report on a male with Cornelia de Langesyndrome who was referred to our multidisciplinary pe-diatric dysphagia clinic when he was 5 years 2 monthsold. The child had previously been under the care of acraniofacial team since birth and was referred by hisconsultant plastic surgeon because of concern regardingfeeding. Cornelia de Lange syndrome affects between1:40,000 and 1:100,000 children. It is associated withsevere intrauterine growth retardation, resulting in shortstature and moderate to severe cognitive impairment. Anumber of other congenital anomalies are associatedwith the syndrome including typical orofacial featuressuch as bushy eyebrows and synophrys, long curly eye-lashes, downward curving of the mouth, thin small mid-line beak of the upper lip and notch in the lower lip, higharched palate, late eruption of teeth, and micrognathia.Children tend to be hirsute with hypoplastic nipples andumbilicus present. Limb abnormalities (such as smallarms or absence of forearms) may be present. Feedingdifficulties are common and include regurgitation, pro-jectile vomiting, and chewing and swallowing difficul-ties. Speech is very slow to develop.
Background Information and History
AZ was born at 37 weeks and weighed 2.5 kg. He wasmarkedly dysmorphic, with cleft palate, micrognathia,large posterior fontanelle, small ears, webbed neck, shortlimbs, a deep sacral dimple, and other minor congenitalanomalies. A systolic murmur was detected and echo-cardiography demonstrated a large left patent arterialduct. Soon after birth he was diagnosed as having Cor-nelia de Lange syndrome.
Correspondence to:Sheena Reilly, Ph.D., School of Human Commu-nication Sciences, Faculty of Health Sciences, LaTrobe University,Melbourne, Victoria 3083, Australia. E-mail: [email protected]
Dysphagia 16:68–73 (2001)DOI: 10.1007/s004550000047
© Springer-Verlag New York Inc. 2001

Gastroesophageal reflux, with projectile vomit-ing, was diagnosed within the first year and medicalmanagement (cisapride, Gaviscon, and ranitidine) wasongoing. The cleft palate remained unrepaired; an at-tempt to repair the palate at 18 months was unsuccessfulbecause of intubation problems. He also had hip dis-placement and was under the care of an orthopedic sur-geon. No history of recurrent chest infections was re-ported but frequent eye and ear infections occurred. Heattended a special school for children with SDD.
Feeding History
Feeding was problematic from birth, resulting in naso-gastric tube feeding for the first two years of life. Bottlefeeding was commenced for a short period, although in-termittent tube feeding continued to be required over thenext 2–3 years usually in association with intercurrentillness. The nasogastric tube was removed at 3.5 yearsand the child was weaned onto liquids and purees fedfrom a soft spouted bottle. Although initially successful,he gradually began to refuse to feed orally. Parental con-cern increased as attempts at oral feeding resulted inchoking, gagging, and coughing. Around this time hesuffered a viral infection with marked changes in bowelhabit which his parents attributed to the attempted rein-troduction of particular solid feeds.
Concerns on Referral
Both parents and the referrer were concerned that therehad been deterioration in his feeding. He was almostcompletely reliant on liquid bottle feeds; these deterio-rated to the extent that feeding times were erratic and hefed little and often. Despite this, he was said to showinterest in food and liked to play “food games,” feelingthe food and taking it from other’s plates. His parentssaid they were frightened of feeding him more solidfoodstuffs because of the coughing and choking butwould like him to take a more age-appropriate diet if thiswas both advisable and possible.
Clinical Examination
On examination, he was found to be responsive and in-teractive. Classical features associated with Cornelia deLange, including short stature [weight4 18.2 kg, length4 83 cm (both well below third centile)] were present.He was noted to have a small narrow tongue and a higharched palate and was heard to grind his teeth exces-sively. A typical feeding was observed and he drank
from his bottle. No overt oral motor and/or pharyngealdysfunction was evident; lip seal was adequate, a rea-sonable volume of liquid was taken in a short period, andthere was no coughing or choking. He assisted withspoon feeding puree by taking the spoon and placing it inhis mouth. He took 3–4 spoonfuls very slowly beforebecoming agitated and refusing further food. he took thebottle-fed milk in bursts, stopping and starting through-out the feeding.
Examination revealed that his chest was clini-cally clear and his abdomen was soft. He did not have ajaw jerk, but patella and biceps reflexes were present andsymmetrical. He crawled in a reciprocal pattern aroundthe room and walked with his knees and hips flexed withsupport but not independently.
Summary of Findings
Both the history and the clinical examination suggestedthat the etiology of the presenting feeding problems werelikely to be multifactorial. First, we were aware thatfeeding difficulties (chewing and swallowing difficul-ties) were commonly associated with Cornelia de Lange.Second, gastroesophageal reflux and projectile vomitingmay have affected his appetite and desire to eat. Third, itwas not clear what effect structural anomalies, such asthe unrepaired cleft palate and shape and size of his oralcavity, might have on the ability to feed orally. Fourth,he had received prolonged periods of nasogastric tubefeeding and had subsequently missed sensitive periodsfor the introduction of different food tastes and textures.Finally, he had significant developmental delay in bothcognitive and motor functioning. His ability to managemore solid foodstuffs certainly needed to be consideredwithin the context of his overall developmental levels.
His gradual deterioration in feeding warrantedfurther investigation as a priority. A two-stage approachwas agreed upon with his parents. Initially, a bariumswallow would be performed to assess the oral, pharyn-geal, and esophageal stages of the digestive process, fol-lowed by 24-hour pH monitoring if indicated.
Results of Investigations
The barium swallow and modified barium swallow re-vealed foreign bodies in the proximal esophagus (Fig. 1).An esophageal stricture was noted below the foreignbodies (Fig. 2) and gross gastroesophageal reflux to thelevel of the stricture was noted (Fig. 3). As a result, hewas seen by the surgical team and five foreign bodies(coin, earring clasp, one other small piece of metal, and
S. Reilly and L. Carr: Foreign Body Ingestion in Children 69

two small plastic objects) were removed. Dilatation ofthe stricture was also undertaken at the same time.
In the meantime he was referred to the pediatricsurgeons about management of his ongoing reflux and tothe dietitians about nutritional needs. One month later agastrostomy and a Thal fundoplication were performedas recommended by the surgical team. He recoveredwell, although he did suffer from dumping and diarrhea(requiring hospitalization on one occasion) and somegastrostomy site granulation.
Follow up
Three months later he was admitted to the hospital witha gastrostomy site infection, severe diarrhea, fever, and a
report of blood-stained vomit and coffee-ground aspirateon one occasion. A chest x-ray showed shadows of adense object in the upper mediastinum thought to be aforeign body. An esophagoscopy was performed and asmall piece of plastic was removed from the esophagus.Approximately three months later, he presented onceagain to the surgeons with a history of increasing diffi-culty with feeding over a 4–5-week period with decreas-ing tolerance of bottle feeds and increased gagging andcoughing. He was also reported to be very irritable andthe gastrostomy site was inflamed. Esophagoscopy re-vealed the presence of foreign bodies (a piece of a sweetpacket, a piece of plastic, and some cardboard) whichwere removed from the esophagus. An esophageal stric-ture was dilated.
Fig. 1. Chest x-ray showing foreign body in the proximal oesophagus.
70 S. Reilly and L. Carr: Foreign Body Ingestion in Children

Discussion
More than three-quarters of all FBI cases in childrenoccur under the age of 6 years [3]. While the majority offoreign bodies pass through the digestive system un-eventfully in 4–7 days [4], impaction may occur in theesophagus. The ingestion of foreign bodies by SDD chil-dren carries a high morbidity and mortality rate [5].
A number of reasons have been proposed to explainwhy children with SDD might be at a higher risk of FBI:
1. Impaired or delayed fine and gross motor skills mayresult in poor control of hand-to-mouth activity andexploration of objects.
2. Children with severe developmental delay often havea prolonged oral phase involving constant mouthing
Fig. 2. Barium swallow illustrating the presence of an esophageal stricture below the foreign bodies.
S. Reilly and L. Carr: Foreign Body Ingestion in Children 71

of objects. Pica, an inability to discriminate betweenedible and nonedible substances, is also reported tooccur more frequently in children with severe cogni-tive impairment [6].
3. Oral and pharyngeal dysphagia limits control over ob-jects placed in the oral cavity [7], and reduced intraoraland pharyngeal sensation may further contribute to FBI.
4. Impaired protective mechanisms, such as frequentgagging, coughing and choking episodes, occur inchildren with SDD. A sudden episode, therefore, maynot provoke additional anxiety in the child’s caregiv-ers.
5. Communication impairment in individuals with SDDcan result in an inability to communicate even the
Fig. 3. Barium swallow showing contrast pooled in the ballooned esophagus above the stricture and gross gastroesophageal reflux to the level of thestricture.
72 S. Reilly and L. Carr: Foreign Body Ingestion in Children

most basic signals, i.e., that they had swallowedsomething unusual! Dallal et al. [2] reported examin-ing an adult patient with SDD (unable to communi-cate verbally) whose inability to open his mouth vol-untarily for an endoscopic examination was consid-ered behavioral. Subsequent examination revealedthat the patient had FBI. Alterations in state and be-havior (whether related to feeding or not) are oftenignored in people with SDD, and behavioral changesare attributed to nonorganic causes.
We believe that many, if not all, of the above factorscontributed to this patient’s repeated FBI. In addition, thepresence of an unrepaired cleft palate, a history of pro-longed nasogastric tube feeding, and the presence of se-vere gastroesophageal reflux (requiring fundoplication)were also contributory factors.
Clinicians should have a high index of suspicionin individuals with SDD who present with feeding dif-ficulties. This patient had been under the care of a cra-niofacial team since birth and had seen a number ofspecialists because of his multiple and complex disabili-ties. However, prior to referral he had not been seen bya multidisciplinary dysphagia team. The feeding difficul-ties he had were attributed to being “part of the SDD”and, therefore, other causes had not been considered.Challenging feeding behavior does coexist in peoplewith SDD; however, careful history and thorough clini-cal examination should be made before a nonorganiccause is attributed to such patients. Factors that shouldraise a high level of suspicion in individuals with SDDinclude:
• sudden refusal to eat or drink• sudden loss of appetite or weight• gradual change in eating habits or patterns• gradual exclusion of foods from the diet until the
child/adult is taking a restricted range of solids or ex-isting solely on a liquid diet
• gradual or sudden onset of “difficult” mealtime behav-ior
These factors have implications for caregivers and thestaff in schools, day care centers, and residential homesthat care for individuals with SDD. The individual’s be-havior should be monitored (a diary of events can behelpful), and referral to a multidisciplinary dysphagiateam should be expedited. Many people with SDD willnot have had a dysphagia assessment despite the fact thatmore than half are underweight and have significant co-existing feeding problems [2,8,9].
As the case we have described illustrates,regularreview of feeding status in individuals with SDD is es-sential. At the last followup visit, this patient was feedingwell; however, his parents and local team are aware ofhis tendency to ingest foreign objects despite his parentsvigilance. They recognize the warning signs that sug-gested foreign body ingestion in the past and are able toact accordingly.
References
1. Hachimi Idrissi S, Corne L, Vanenplas Y: Management of in-gested foreign bodies in childhood: our experience and review ofthe literature.Eur J Emerg Med 5:319–323, 1998
2. Dallal HJ, Odum J, Ahluwalia NK: Covert dysphagia in thementally handicapped: two case reports and a review of thepublished literature.Dysphagia 11:194–197, 1996
3. Panieri E, Bass DH: The management of ingested foreign bodiesin children—a review of 663 cases.Eur J Emerg Med 2:83–87,1995
4. Spitz L: Management of ingested foreign bodies in childhood.Br Med J 4(785):469–472, 1971 Nov 20
5. Carter G, Jancar J: Sudden deaths in the mentally handicapped.Psychol Med 14:691–695, 1984
6. Hardan A, Sahl R: Psychopathology in children and adolescentswith developmental disorders.Res Rev Disabil 18:369–382,1997
7. Smith MT, Peura DA: Foreign bodies. In: Castell DO (ed.):TheEsophagus.London: Little, Brown, 1992, pp 383–400
8. Reilly S, Skuse DH, Poblete X: Prevalence of feeding problemsand oral motor dysfunction in children with cerebral palsy: acommunity survey.J Ped 129(6):877–882, 1996
9. Kennedy M, McCombie L, Dawes P, McConnell M, DunniganMG: Nutritional support for patients with intellectual disabilityand nutrition/dysphagia disorders in community care.J Intellec-tual Dis Res 41(Part 5):430–436, 1997
S. Reilly and L. Carr: Foreign Body Ingestion in Children 73