Fluid Therapy Basics
Transcript of Fluid Therapy Basics
-
8/8/2019 Fluid Therapy Basics
1/9
Fluid Therapy BasicsModule 1 / Dr. Elisa Mazzaferro
Welcome to the rst module of AbbottAnimal
HealthCE.coms uid therapy series, Fluid Therapy
Basics. My name is Dr. Elisa Mazzaferro, with Wheat
Ridge Animal Hospital in Wheat Ridge, Colorado.
School may seem like it was so long ago, even if
you graduated and became a veterinarian or technician
last year! Fluid therapy is not meant to be confusingor time consuming. AbbottAnimalHealthCE.coms uid
therapy series of 10 modules is meant to challenge and
augment your uid therapy knowledge.This introduc-
tory module covers the basics and will set the stage for
the future uid therapy modules, in which youll learn
practical information you can immediately use in your
practice, how to choose and administer the right type
of uid, place and care for catheters, use crystalloids
and colloids, administer uids during emergencies,
anesthesia and surgery, and monitor your patients.
Slide 1
In addition to setting the foundation for these future
uid therapy modules, this module has several objectives.
First, we will dene and then develop a full understanding
of perfusion and homeostasis. Next we will learn about
body water composition and how uid moves between
the different cell compartments. Then well review the
maintenance uid requirements for animals.Well then discuss the importance of determining both
a patients sensible and insensible uid losses. Lastly, well
wrap up by learning the importance of properly diagnosing
a patient with dehydration versus hypovolemic shock.
But before we start, youll take a short pretest to
stimulate your brain cells and help you recall some basic
concepts of uid therapy. Then, well dive in to solidify the
concepts, so that uid therapy is simple, easy, and fun!
Slide 2
Question 1: An animal presents to you in hypo-
volemic shock. All of the following are examples of
parameters to assess perfusion except for which one
listed here?
Is your answer skin tenting? Then you are abso-
lutely right! Hypovolemic shock involves decreased
uid volume within the intravascular space. As such,
decreased intravascular volume results in decreased
tissue perfusion. Perfusion parameters that can be
assessed include capillary rell time, blood pressure,
heart rate, and temperature of extremities. Conversely,
dehydration refers to decreased uid in the interstitial
and intracellular spaces. Increased skin tenting is
associated with dehydration.
Slide 3
Question 2: An intravenous catheter was placed in the
lateral saphenous vein 48 hours ago. This patient requires
aggressive uid diuresis for acute renal failure and is do-
ing well at this time. Another veterinarian in your practice
suggests that the catheter should be removed and replaced
because it has been in for too long. How should you reply?
What did you say? If you thought B and C provided
the correct reply to your colleague, youre right. Several
recent studies have documented that the length of time that
an intravenous catheter is left in place is not signicantly
associated with catheter-related problems. The catheter can
remain in place as long as it is not contributing to a fever,
and as long as it is owing without signs of pain, swelling, or
discharge at the catheter site. Large bore, shorter catheters,
such as 18 gauge, one and one-quarter inch, are the best
for administration of intravenous uid boluses. However,
large volumes of uids can also be administered through a
longer, central venous catheters, when necessary.
Slide 4
page AbbottAnimalHealthCE.com
-
8/8/2019 Fluid Therapy Basics
2/9
Question 3: A two-year-old intact female West High-
land white terrier presents to you with a four-day history of
progressive vomiting and diarrhea. Her mucous membranes
are dry, and skin tenting is markedly increased. While you
are waiting for the results of a CBC, serum chemistry, and
urinalysis, you elect to administer intravenous uids. What
uid would you choose?
The correct answer is any of the above except B. The
patient is showing signs of dehydration, with increased skin
tenting, a history of both vomiting and diarrhea, and dry mu-
cous membranes. Many intravenous crystalloid uids can be
used to replenish interstitial, intracellular, and intravascular
uid decits.
However, a 0.45% sodium chloride uid with supplemen-
tal dextrose is not a balanced electrolyte solution, and is not
appropriate for rehydration. A 0.9% sodium chloride uid is
an isotonic crystalloid that can be used, although is less bal-
anced than lactated Ringers or Normosol-R.
Slide 5
Question 4: What is an example of an acidifying iso-
tonic crystalloid solution?
The correct answer is 0.9% sodium chloride (NaCl).
This acidifying isotonic crystalloid solution contains no
buffers and can contribute to a strong ion difference when
administered. Lactated Ringers and Normosol-R both
contain buffers, and as such, are not acidifying. 5% dex-
trose in water and 0.45% sodium chloride are hypotonic
crystalloids that do not contain buffers.
Slide 6
Question 5: As you are walking out the door for lunch, your as-
sociate calls for assistance in the surgery room. He has just dropped
an ovarian pedicle and cant nd the bleeder. The abdomen is lling
with blood rapidly. As you glove up, what should you ask yourself?
You should be asking, What is the animals blood pressure? Inmany instances, the loss of blood volume can be managed simply by
relling the intravascular space with a crystalloid, unless hemorrhage
is severe. The body will regenerate red blood cells as needed.
In an emergency situation, blood pressure is the rst parameter
that you can measure to estimate organ perfusion. Titrating intra-
venous crystalloid or colloid uids to maintain normotension is the
goal to maintain vital organ perfusion in cases of hemorrhage. You
may need to change the anesthetic depth as well as add a positive
inotropic drugs, such as dopamine, or pressors, in addition to crystal-
loid and colloid uids or blood products, when necessary. In this case,
nding the ovarian pedicle and ligating the bleeder usually is a simple
task for the experienced clinician. Then, you can proceed to lunch.
Slide 7
So how did you score? No matter whether you got
all 5 right or maybe missed a few, I can guarantee that
watching this module and the future uid therapy modules
will help solidify your knowledge. So now lets jump into
Fluid Therapy Basics. Enjoy!
Slide 8
page AbbottAnimalHealthCE.com
-
8/8/2019 Fluid Therapy Basics
3/9page AbbottAnimalHealthCE.com
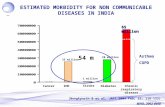
The Hungarian Biochemist Albert Szent-Gyorgyi
once said, Water is lifes mater and matrix, mother and
medium. There is no life without water. In veterinary
medicine, a variety of diseases are accompanied by
the loss of body uids. Without adequate hydration,
normal body functions become impaired and perfusion
decreases, which ultimately can lead to death if thera-
peutic interventions are not implemented.
Slide 9
Perfusion refers to the process in which blood carries
oxygen and important nutrients to body tissues. Perfusion
depends on many body compensatory responses, but
also on the administration of appropriate uid volumes to
maintain vascular volume. A discussion of intravenous
uid administration begins with an understanding of total
body water and uid balance between the various com-
partments within the body, so thats where well start.
Slide 10
Water is a major contributor to an animals body
weight. In healthy animals, approximately 60% of body
weight is water. This value can change slightly depend-
ing on age, lean body mass, degree of leanness or
obesity, and gender. For example, neonatal puppies
and kittens have a relatively higher percentage of water
in their bodies than adults. Adipose tissue contains
more water than muscle and can contribute to a larger
percentage of water in obese animals.
Water is located in separate yet intertwined com-
partments within the body. Conceptually, the body
can be divided into the intracellular and extracellular
compartments.
Slide 11
Approximately two-thirds, or 66%, of total body water is
located within the intracellular uid compartment inside of
cells. Extracellular uid is the uid that is located outside of
cells. Approximately one-third, or 33%, of total body water
is in the extracellular uid compartment. The extracellular
uid compartment can be further subdivided into the intra-
vascular and interstitial compartments. The intravascular
space contains uid within blood vessels.
It is through these blood vessels that plasma water,
cellular components, proteins, and various electrolytes ow.
The interstitial extravascular compartment is the space
located outside of the blood vessels. Intravascular uid
contributes only 8% to 10% of total body water, whereas
interstitial uid contributes 24% to total body water. A very
small amount of uid is known as transcellular uid, and is
located within the gastrointestinal tract, joints, cartilage, and
cerebrospinal space.
Slide 12
-
8/8/2019 Fluid Therapy Basics
4/9page AbbottAnimalHealthCE.com
It has been estimated that total body water is
approximately 534 to 660 ml/kg in a healthy dog.
Intravascular water volume has been estimated to be
approximately 90 ml/kg in dogs and 45 ml/kg in cats.
Slide 13
To fully understand the uid therapy needs of all
patients, we need to rst understand how uid move
throughout the body. Water in the bodys various com-
partments is in a constant state of ux and moves from
compartment to compartment. The capillary membrane
between various compartments is composed of a thin
membrane of endothelial cells that contain tight or gapjunctions through which uid and solutes can ow.
Solutes dissolved in uid can ow between compartments
by passive diffusion, where a solute moves from an area
of higher to lower concentration down its concentration
gradient. Other solutes can be moved from one compart-
ment to another by active transport mechanisms.
Slide 14
The rate of uid exchange largely depends on the
forces that favor uid retention within a compartment
versus the forces that favor uid movement or ltration
from a compartment. The colloid oncotic pressure of
a uid compartment is dictated by the concentration
of protein within that space. Albumin is a protein that
contributes approximately 80% to the colloid oncotic
pressure. The hydrostatic pressure is the pressuregenerated by the force of a uid within a compartment.
The colloid oncotic pressure inuences uid retention
within a compartment, while the hydrostatic pressure
inuences uid movement from that compartment.
Slide 15
Starling created an equation that predicts exchange of
uid between the bodys uid compartments. The equa-
tion is shown here. Kf equals the ltration coefcient that
varies from tissue to tissue within the body. Pc
and Piare the
hydrostatic pressure within the capillary (Pc) and interstitial
space (Pi). Sigma () is size of the pores in the capillary
membrane, and idescribes the effect of proteins such as
albumin that promote uid retention in the capillary (c) andthe interstitium (
i). Finally, Q
lymphdescribes the rate of lymph
ow from the interstitium.
When hydrostatic forces exceed colloid oncotic forces,
uid will leave one compartment and go to the other. Con-
versely, a relative increase in the colloid oncotic forces within
a compartment can retain uid within or may draw uid into
a compartment. So depending on whether hydrostatic forces
or colloid oncotic forces are stronger, uid will either leave
the blood vessel or enter it. This equation can have a num-
ber of important physiologic implications, especially when
disease conditions alter one or more of the variables.
Slide 16
-
8/8/2019 Fluid Therapy Basics
5/9
-
8/8/2019 Fluid Therapy Basics
6/9page AbbottAnimalHealthCE.com
Insensible losses are those which cannot directly
by measured and are lost in the form of sweat, saliva,
and excessive panting. Sensible uid loss constitutes
approximately two-thirds of an animals daily uid
requirement. Since insensible losses account for the
other one-third of a patients daily uid requirement,
their importance to the total daily uid requirement
should not be underestimated. You should be sure to
include the insensible uid loss measurement in your
patients daily uid requirement calculations so that the
volume administered is adequate. Normally, insensible
losses are estimated to be 20 to 30 ml/kg/day.
Weve talked about uid loss. Now lets talk about
uid balance, since the goal of uid therapy is to ensure
that the patient has an adequate amount of uid distrib-
uted appropriately in the body.
Slide 21
Fluid balance is largely governed by sodium concentration
within the body. Sodium and chloride concentrations in the
vascular space trigger osmoreceptors in the hypothalamus to
sense osmolality, or particle concentration. Other molecules
that contribute to osmolality include potassium, bicarbonate,
urea, and glucose. As serum sodium rises, usually due to
increased sodium intake or uid loss in excess of solute,
serum osmolality also rises. This rise in osmolality triggers the
hypothalamic release of arginine vasopressin, also known as
antidiuretic hormone, or ADH, into the peripheral circulation.
ADH stimulates the opening of water channels in the renal
collecting duct and causes the reabsorption of water. Reten-
tion of water within the vascular space dilutes the sodium
concentration and decreases osmolality. Once the animals
osmolality has been normalized and its major contributors of
osmolality have been diluted, the hypothalamus stops releas-
ing ADH, there is less re-absorption of water by the kidney,
and uid balance is normalized through this self-regulation
Slide 22
A knowledge of uid therapy would be not be complete
without a discussion of the other electrolytes and buffers
that are contained within the intracellular and extracellular
compartments. So lets take a moment to cover that next.
This is important in choosing the appropriate uid for your
compromised patients. Sodium, chloride, and bicarbonateare found in much higher concentrations in the extracellular,
intravascular compartment than in the intracellular compart-
ment. Conversely, magnesium and phosphate are found in
higher concentrations within cells, rather than within the inter-
stitial and intravascular spaces. The concentrations of these
important ions often become deranged in a variety of critical
illnesses because of gain or loss, or due to exchange second-
ary to changes in the bodys pH and buffering capacity.
It is important to understand the various electrolytes
and what can cause abnormalities so you can choose the
right uid for a dehydrated or hypovolemic animal. A more
thorough discussion of the electrolyte content of crystalloid
uids will be discussed in future uid therapy modules.
Slide 23
OK, so now its time to take this to the practical level.
Lets say this dog came into your hospital. Do you know
if she is experiencing hypovolemic shock or dehydration?
Would you be able to tell just by looking at her? Unfortu-
nately, no, you wouldnt be able to tell.
One of the most common misnomers in uid therapy is
when hypovolemia is referred to as dehydration. Dehy-
dration refers to a decrease in total body water, whereas
hypovolemia largely refers to inadequate circulating
intravascular uid volume. Dehydration refers to loss of
uid in the intracellular and interstitial uid compartments.
Since hypovolemia can be a much more serious condition
and may need to be treated much more aggressively than
dehydration, it is important that both the veterinarian and
technician be able to tell the difference between the two.
Slide 24
-
8/8/2019 Fluid Therapy Basics
7/9page AbbottAnimalHealthCE.com
To get a rough estimate of an animals degree of
dehydration, you can use subjective guidelines of skin
tenting and mucous membrane dryness. For example,
historical vomiting or diarrhea without a measurable
increase in skin tenting or mucous membrane dryness
can be categorized as less than 5% dehydration. As
the volume of uid loss increases, external evidence
of dehydration becomes more readily apparent and
become more progressive and severe. At 7% dehydra-
tion, mild tachycardia could also be present. At 10%,
the patient might also have a decreased pulse pres-
sure. Then at 12% dehydration and higher you might
see sunken eyes and dry corneas and, in severe cases,
alterations of consciousness. Evaluating these physical
parameters and determining the percent of dehydra-
tion is a component of calculating the replacement uid
volume needed for your patient.
Slide 25
To recap what weve discussed so far, weve talked
about how uid loss leads to hypovolemia, which leads
to decreased perfusion, which can lead to morbidity and
sometimes death.
So how does the body respond to uid loss? It
responds in a number of ways. First, it pulls uid into the
intravascular space from the interstitial space in order
to maintain circulating blood volume. When the intersti-
tial space can no longer replenish intravascular volume
depletion, clinical signs of hypovolemia result.
Hypovolemia refers to inadequate circulating intra-
vascular volume. Hypovolemia can result in hypovolemic
shock from excessive hemorrhage, such as that observed
with a bleeding abdominal mass, vitamin K antagonist
rodenticide intoxication, or an arterial laceration.
Slide 26
Hypovolemia also can occur due to severe uid loss
and in end-stage dehydration, such as that observed
in a puppy with parvoviral enteritis or an elderly cat in
end-stage renal failure. Parameters used to determine
an animals hydration status should not be used to
determine its intravascular volume status.Intravascular uid volume and cardiac output are
major determinants of organ perfusion. In the peripheral
tissues, parameters of perfusion include capillary rell
time, mucous membrane color, blood pressure, and
heart rate. In a normal animal, the mucous membranes
should be pink and moist, with a capillary rell time
of less than two seconds. Pale pink to whitish gray
mucous membranes with a capillary rell time thats
prolonged, tachycardia, and hypotension can be found
with either hypovolemic or cardiogenic shock.
Slide 27
So what else happens in the body with hypovolemia?
Lets take a quick look at a ow chart. Baroreceptors are
located in the carotid body and aortic arch that sense the
stretch of the vessel walls, depending on how much uid is
circulating in the intravascular space. In healthy, euvolemic
animals, stimulation of the stretch receptors triggers thevagus nerve to automatically slow heart rate. When an
animal becomes hypovolemic, the stretch receptors sense
a decrease in wall tension and decrease ring of vagal
stimuli to the brain. This allows the sympathetic nervous
system to manifest itself, and epinephrine and norepineph-
rine are released from the adrenal glands. The release
of these hormones results in vasoconstriction, improved
cardiac contractility, and an increase in heart rate. These
effects are intended to compensate for decreased intravas-
cular uid volume by improving cardiac output and, thereby,
maintaining systemic blood pressure.
Slide 28
-
8/8/2019 Fluid Therapy Basics
8/9page AbbottAnimalHealthCE.com
At the beginning of this module we dened perfusion,
and now well explore it in more depth. Oxygen delivery is
an important part of the perfusion discussion. It is depen-
dent on the animals cardiac output, which is represented in
this graph, and the amount of oxygen carried in the blood-
stream. Cardiac output is a function of heart rate and stroke
volume, or the amount of blood that the heart pumps in oneheartbeat. Factors that affect stroke volume are cardiac or
ventricular preload, ventricular afterload, and contractility.
Cardiac preload, by Starlings law of the heart, is affected
by the amount of blood that enters the ventricle and causes
the ventricular wall to stretch. The amount of wall stretch is
directly proportional to the force of contraction. If the heart
muscle is healthy, and if there is adequate circulating cardiac
preload because there is adequate intravascular circulat-
ing volume, and, thus, adequate wall stretch, the force of
contraction will be adequate. In an animal with insufcient
circulating blood volume, cardiac preload will be diminished,
thus decreasing the force of ventricular contraction. Intrave-
nous uid therapy can affect cardiac preload by replenishing
intravascular uid volume in a hypovolemic animal.
Slide 29
That brings us to another common misconception: that
uids instilled into the subcutaneous space can be used
to replenish the intravascular blood volume. In fact, uids
instilled into the subcutaneous space will be absorbed very
slowly, if at all, in a patient in hypovolemic shock.
Remember, hypovolemia refers to the intravascular
space, and dehydration refers to the interstitial and intra-cellular compartments. The only methods of accurately
replenishing intravascular uid decits are to place either
an intravenous or an intraosseous catheter. Fluids can be
administered at high rates and large volumes through these
catheters to replenish the intravascular pool.
Slide 30
There are two types of uids, crystalloids and
colloids. Which you choose depends on where you are
trying to replenish uids. Crystalloids are composed of
smaller molecules; therefore, approximately 80% of the
uid infused will leave the intravascular space within
the hour. Colloids are made of larger molecules, which
means they stay in the intravascular space longer.
There are times you might use both. An additional
module will be devoted to this discussion.
Slide 31
During compensatory shock, the heart rate and blood
pressure may be normal, or there may be tachycardia with
mild hypotension. As hypovolemic shock progresses, the
sympathetic output can become exhausted and no longer
allow an increase in cardiac output.
Slide 32
-
8/8/2019 Fluid Therapy Basics
9/9page AbbottAnimalHealthCE com
Now weve set the stage for future modules with basics
of uid therapy. Weve covered body water composition and
how uid moves between the different cell compartments.
We reviewed animals maintenance uid requirements and
discussed how important it is to determine both a patients
sensible and insensible uid losses. Then we determined the
importance of properly diagnosing a patient with dehydration
versus hypovolemic shock.
The future modules will present practical informationfor use in your practice: the various types of crystalloid and
colloid solutions, uid administration and intravenous cath-
eter techniques, strategies for uid administration as well as
potential complications of uid therapy, and uid therapy for
specic disease states. So stay tuned!
Slide 35
During late decompensatory shock, severe hypovo-
lemia coexists with dramatic worsening of the perfusion
parameters, which are manifested as bradycardia,
prolonged capillary rell time, hypotension, pale pink
to whitish gray or cyanotic mucous membranes,
hypothermia, decreased central venous pressure, and
decreased urine output.In late decompensatory shock, rapid and aggressive
intravenous uid resuscitation is necessary to save the
animals life.
Slide 33
In conclusion, youve learned that without adequate
hydration, hypovolemia results, leading to decreased
perfusion, morbidity, and possibly death. Perfusion
depends on many body compensatory responses, but
also on the administration of appropriate uid volumes to
maintain vascular volume.
Youve also learned that administration of intravenousuids requires an understanding of the type of uid loss,
the presence of underlying disease processes, the animals
acid-base and electrolyte status, the animals ability to
retain uid within the vasculature, as well as determinations
of resuscitation end-points.
Slide 34