Final Pocahontas Memorial Hospital Clinic Report
-
Upload
chelsey-bertram-mha -
Category
Documents
-
view
754 -
download
15
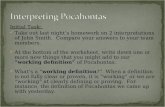
Transcript of Final Pocahontas Memorial Hospital Clinic Report

Running head: POCAHONTAS MEMORIAL HOSPITAL CLINIC REPORT 1
Pocahontas Memorial Hospital Clinic Report
Chelsey Bertram
HCM 580 – Organizational Management Strategy and Execution
Colorado State University – Global Campus
April 19, 2016
Dr. Bradley Beavais

POCAHONTAS MEMORIAL HOSPITAL CLINIC REPORT 2
Pocahontas Memorial Hospital Clinic Report
Pocahontas Memorial Hospital (PMH) in Pocahontas County, West Virginia, has decided
to look into the feasibility of building a satellite clinic as part of the annual strategic planning
process. The clinic would be to help expand care to the over 9,000 residents of this over 900
square mile rural county (Capstone Project Case Study Information, n.d.). This report was
conducted to asses if this was a possible along with any recommendations for this project’s
feasibility.
PMH is a hospital with core values and a mission statement focused on improving
healthcare through education, compassion, best practices, and a positive culture within the
organization (Pocahontas Memorial Hospital, n.d.). The hospital already runs a clinic within the
hospital that provides laboratory services, vaccinations, and monthly clinic focused on different
diseases. The rural population of Pocahontas County faces many challenges in obtaining much
needed healthcare. There are financial challenges; many people live in poverty, making it
difficult to pay for healthcare or have no health insurance. They also face transportation
challenges, little to no public transportation and challenging roadways, making it difficult to get
to appointments or get to care when needed (US Department of Health and Human Services,
2013). The mission of PMH is to provide care and a satellite clinic would provide healthcare to
residents not living in close enough proximity of the hospital.
Assessment of Satellite Clinic
To determine if this satellite clinic is possible there needs to be an assessment looking at
various parts. The internal and external stakeholders will need to be identified, as well as,
foreseeable challenges. A market analysis and a SWOT (Strengths, Weaknesses, Opportunities,

POCAHONTAS MEMORIAL HOSPITAL CLINIC REPORT 3
and Threats) analysis will be conducted to look at other important areas that will influence this
project.
Stakeholders: Internal and External
Stakeholders are people who have an interest in the organization. They can be within the
organization or people outside the organization, the important detail is that these people are those
that care about the organization and are affected by any changes. The stakeholders are those that
should be involved with any strategic changes, perhaps not each individual person in large
organizations, but their opinion should be registered (Ginter, Duncan, & Swayne, 2013).
Internal Stakeholders. Internal stakeholders are those people that work or are affected
by changes directly within the hospital. For PMH there are four groups of internal stakeholders:
employees, patients, families of patients, and the Executive Board or Board of Directors.
Employees for PMH will be the one of the first affected by the satellite clinic. Some employees
may be able to work closer to home if they are able to transfer. Others will notice the anticipated
workload change, becoming lighter. But all level of employees from orderlies and cafeteria staff
to physicians will notice the change (Ginter, et all, 2013).
The current patients will see changes as well. These patients may be able to receive care
closer to their home, making it more encouraging to receive the care they need. Others that are
closer to the hospital and the current clinic could see less of a wait time, since there would be
fewer patients using the same facility. This could encourage patients to seek care, as it doesn’t
take as long to receive care.
The families of patients are also stakeholders. This is because the families assist with care
at home in many cases, thus if a person can receive care easier and quicker than before, the care

POCAHONTAS MEMORIAL HOSPITAL CLINIC REPORT 4
at home can be supported. Also since many families in rural American communities share or
have limited vehicles for transportation, there would be less drive time with the satellite clinic,
thus limiting interference with other family member’s work and school schedules (Cook & Hoas,
2008).
The Executive Board or Board of Directors has a vested interest in the potential satellite
clinic since they make most of the decisions regarding strategic planning. The Board would want
to know and be assured that this change would continue to support the mission statement of the
organization and fund the hospital. For many healthcare organizations funding is a large concern
(Healthcare Financial Management, 2013).
External Stakeholders. Stakeholders outside the organization also need
acknowledgment since the change influences them and they can influence the change. For an
organization like PMH the community of the whole county is a stakeholders, as well as, potential
donors or investors for the clinic. The community will more than likely be full of patients or
potential patients, but as a whole they can influence the decision. Research supports the idea that
the community be involved in the decisions about clinics and healthcare support, especially in
rural communities. Town hall type meetings or other open forums allow the members to speak
up on either side of the decision (Farmer & Nimegeer, 2014).
The potential donors or investors are the people who ultimately make the clinic happen,
since without funds the clinic couldn’t happen. They want to be assured that they would get a
return on their investment or the donation will be used in a way they approve. Thus proposals
would need to be presented and potentially adjusted to suite all involved with the clinic (Ginter,
et all, 2013).

POCAHONTAS MEMORIAL HOSPITAL CLINIC REPORT 5
Environmental Challenges
For a project like this proposed satellite clinic for PMH, there needs to be a realization
about the challenges that are currently being faced and those that can be face at this new clinic.
Staffing challenges such as work load and equipment that is out of date, funding challenge and
community involvement are the biggest challenges. These will impact the already struggling
staffing problem.
Staffing Challenges. Many people who work in healthcare do report that since there is a
shortage of staff, the work load is extremely difficult to handle. PMH has a patient to doctor
tratio of 8,508 to 1, meaning there are about two physicians in the county. This ratio is higher
than the overall nationwide ratio (Capstone Project Case Study Information, n.d.). There is no
current data for PMH on the ratio of nursing staff and other members of a healthcare team to
make a full assessment of workload. But to follow the trend nationwide, there is shortage is all
levels of healthcare staff. The lack of employees creates more work for those that are employed
at the hospital. This overload leads to low retention rates, mental health illnesses including
depression and anxiety for staff, and poor work habits (Darkwa, Newman, Kawakab, &
Chowdhury, 2015).
The staff many times deals with old equipment or inadequate equipment, this too affect
workload. If the machines designed to help with testing don’t work properly or isn’t available in
the center, then staff may wait for the machinery to be fixed or develop another test that may not
be as accurate. This increases workload. Many healthcare personal who work in rural
environments report that having inadequate equipment is one of the hardest parts of working in
the environment because it adds to their already large workloads (Darkwa, et all, 2015).

POCAHONTAS MEMORIAL HOSPITAL CLINIC REPORT 6
Funding. Many rural healthcare organizations do not typically acquire large enough
revenue to support expansion or updating much of the equipment. The organizations support a
smaller population that usually has government funded healthcare, verse counterparts in urban
areas that have a larger population that can be insured through a private insurance company thus
larger revenues. This is especially challenging as healthcare has been moving towards the focus
of better quality care for lower costs (Solving the rural healthcare revenue conundrum, 2013).
Community Involvement. The typical rural community is very close and doesn’t like
change; they also have fear about healthcare because of the cost associated with it. The satellite
clinic will need community members to use it, to make it worthwhile. The community may be
more aware of what exactly the clinic should provide, since the community members may be
more in tune with challenges that they themselves or neighbors deal with in regards to healthcare
such as substance abuse or diabetes (Farmer & Nimegeer, 2014).
Market Analysis
As Pocahontas Memorial Hospital is looking at creating a new rural healthcare clinic in
the county it is important to look at the market and create a full analysis to make a decision. A
market analysis is made up of five different parts: an overview of the industry, target market,
competition, projections, and any regulations related to the market.
Overview of Industry. The healthcare industry has been going through many changes
due to new laws or acts and increased public interest. But it continues to be an industry of
growth. That is because the United States continues to increase spending on healthcare while
underperforming when compared to other developed countries. The United States fails to achieve
better health outcomes than countries like the United Kingdom, Switzerland, and Australia. In

POCAHONTAS MEMORIAL HOSPITAL CLINIC REPORT 7
four editions of a report by The Commonwealth Fund, the Untitled States finished last or near
last in many categories like access to care, efficiency and equity of healthcare (2014). The
United States spends $4,197 per capita on healthcare, more than double for the Organization for
Economic Co-Operation Development (OECD) average (OECD, 2015). The passing of the
Patient Protection and Affordable Care Act (PPACA) is expected in decrease cost for both
individuals and the government overall, while increasing quality of care, leading to an increase in
quality of life (The Commonwealth Fund, 2014). That can be part of the motivation of
Pocahontas Memorial Hospital’s interest in creating a clinic.
Target Market. For PMH is the only hospital in the whole county for 9,131 residents,
according to the 2010 Census. Thus the market is the residents of this small rural county in West
Virginia. The population is majority Caucasian with limited/lower income levels – the median
income is $26,401 per household (Capstone Project Case Study Information, n.d).
Analysis of Competition. PMH is the only hospital in the county, but it does not mean
there is no competition. The six counties surrounding Pocahontas County all have county
hospitals, which many be more convenient for the residents living at the opposite end of the
county to travel to. A cursory look at the hospitals it appears that the other hospitals are all of
similar (small) size with similar challenges regarding market. There also appears to be no private
practices in the county for additional competition (County Health Roadmaps & Rankings, n.d.).
But that does not mean that the hospital needs to become lax about care or competition, a
hospital still needs to strive to improve health while overcoming their challenges.
Projections. Healthcare is in a period of change, especially with the PPACA requiring
residents to have health insurance or face stiff penalties from the federal government, thus

POCAHONTAS MEMORIAL HOSPITAL CLINIC REPORT 8
meaning healthcare organizations will see an increase in patients (The Commonwealth Fund,
2014). The idea of reaching Pocahontas County residents, who do not live in the direct area of
Pocahontas Memorial Hospital, would increase the number of patients seen. The healthcare
industry is expected to continue to grow in the future, even with the projections of staffing
shortages in most areas, including the United States (The Commonwealth Fund, 2014).
Regulations. The healthcare industry has many regulations protecting patients in many
aspects of their care, but the operation of a rural clinic has its own regulations. The Centers for
Medicare and Medicaid Services (CMS) has a long list of regulations that must be followed in
order to receive payment from Medicare and/or Medicaid. The regulations require compliance
with any and all federal, state, and local laws that affect healthcare, the location, the building, the
responsibilities of staff, even how the clinic is evaluated. In recent edits the staff of a rural clinic
or center needs to be compromised of at least on physician and one physician’s assistant or nurse
practitioner, plus the option to have a social worker and a certified mid-wife (Centers for
Medicare and Medicaid Services, 2015).
SWOT Analysis
A SWOT analysis looks at various aspects both within an organization and the external
environment. SWOT breaks down to: Strengths, Weaknesses, Opportunities, and Threats to the
Organization. This is one of many analyses an organization can conduct on themselves when
preparing for a strategic change (Ginter, et all 2013).
Strengths. For PMH there are three strengths for the hospital, they are all points coming
from within the organization. The first is the focus the organization has on creating a healthy
lifestyle. It is a part of the mission statement for PMH (Pocahontas Memorial Hospital, n.d.).

POCAHONTAS MEMORIAL HOSPITAL CLINIC REPORT 9
Another strength is how the hospital already has the clinic within the hospital providing many
different items such as laboratory services, rotating clinics, and immunizations (Capstone Project
Case Study Information, n.d.). This shows how, the proposed satellite clinic would have an
example to follow. The final strength is how the ratio of physicians to patients is higher than the
national average, showing that the hospital has a positive reputation within a medical community
and the Pocahontas County (Capstone Case Study Information, n.d.)
Weaknesses. Even with the great strengths, there are weaknesses there too. The first is
the small size of the hospital; it is only 25 bed and low trauma level – level 4 (Capstone Case
Study Information, n.d.). If there was any form of large scale tragedy the hospital may not be
able to handle the situation. The next two are weaknesses from the environment that directly
weaken the hospital. The rural environment makes transportation a challenge for residents to
attend appointments (U.S. Department of Health & Human Services, 2013). This makes it
difficult for the hospital to maintain full schedules, supporting the revenue (Capstone Case Study
Information, n.d.). The last is the already apparent national shortage of healthcare professionals,
which is even more challenged in a rural environment. (U.S. Department of Health & Human
Services, 2013).
Opportunity. PMH does also have areas that can be beneficial. The first being how
PPACA is expanding Medicaid benefits to more people, which would increase the number of
potential patients to the hospital, even with the low reimbursement rate, could increase revenue
(U.S. Department of Health & Human Services, 2013). There are also federally based
organizations that provide funds for rural communities to help focus on healthcare which can
help with the expansion of the satellite clinic (U.S. Department of Health & Human Services,
2013).

POCAHONTAS MEMORIAL HOSPITAL CLINIC REPORT 10
Threats to the Organization. All organizations can be threatened by external forces.
PMH is not without threats. The first is the average income for Pocahontas County of $26,401 a
year (Capstone Case Study Information, n.d.). The lack of means to cover the cost of healthcare
threatens the organizations ability to have a sufficient budget. There are many times that
hospitals have to absorb the cost of care when insurance or an individual cannot pay for it, there
is a higher risk of this when the average population is of a lower socioeconomic status. The other
threat is the strictness of the CMS regulations for rural healthcare clinics. It is highly important
for any healthcare organization to follow these rules to be reimbursed by Medicare and/or
Medicaid (Centers of Medicare and Medicaid Service, 2015).
Recommendations and Implementation
In order to decide if this clinic will work, there needs to be solutions created to overcome
challenges such as those discussed above, as wells as recommendations for value adding
support, plans for implementation – both short and long term, and suggested evaluations and
benchmarks for this project.
Strategies for Potential Weaknesses or Threats. The first weakness is the small size of
the PMH. The current size of the hospital is 25 beds (Capstone Case Study Information, n.d.).
One way that the hospital is looking at overcoming that weakness is the proposed satellite clinic,
which would increase the number of patients the hospital system can care for. The second
location would help patients located in other regions of the county; PMH is located in the
southeast region (Capstone Case Study Information, n.d.). But with the current plan of expanding
via the satellite clinic there is little chance of expanding the current hospital’s capacity.

POCAHONTAS MEMORIAL HOSPITAL CLINIC REPORT 11
The second threat is the strict regulation from the CMS on rural health clinics. The
document on describing all details of the clinic must be followed in order to receive
reimbursement for care of patients with Medicare and/or Medicaid (Centers of Medicare and
Medicaid Services, 2015). The best way to overcome this challenge is to review the most current
version of the document and follow the regulations step by step.
The third weakness or challenge is the rural environment of Pocahontas County. The
rural area compromises patients ability to receive any form of care (emergency or regular care)
(U.S. Department of Health & Human Services, 2013). The proposed satellite clinic would help
those patients living in areas far away from PMH, as long as this clinic becomes a reality. If the
clinic doesn’t happen, one way to assist with this challenge would be to provide phone or email
appointments for questions or care that doesn’t require physical testing or examination.
One more threat or weakness is the lower socioeconomic statues of the county. This lack
of funds of the population affects the budget of the hospital. If the hospital overall budget does
not provide funds to build a clinic that will be a challenge. But there are some ways to assist the
organization reach its goal. The key is to work with the community to make it be a part of the
new clinic. Some hospitals have reach out to local banks to process the loan with success. Others
reach out to large volunteer organizations (like Rotary Club) that have chapters nerby, with the
ability to donate a larger sum of money from the organization as a whole (Nayak, 2013). It may
take a combination of these and other tools to help raise the funds needed to start on this
endeavor.
The last treat or weakness is the shortage of healthcare employees, even though PMH’s
physician to patient ratio is above that of the nation, there is no statement of the number of other

POCAHONTAS MEMORIAL HOSPITAL CLINIC REPORT 12
healthcare providers like nurses, technicians, and therapists (Capstone Case Study Information,
n.d.). The rural environment of Pocahontas County adds to the challenge; there is a lower rate of
retention for rural environments for healthcare professions. The biggest complaints from
healthcare workers in rural environments steam from higher workloads, inadequate equipment,
and culture. Some ways of encouraging employees to stay include pay and/or benefits package
and having equipment that is of good quality that would be higher or in line with those seen in an
urban area. The equipment at bare minimum must pass the same level of quality assurance and
control when tested by an outside facility (Olusegn, 2012).
Financially based incentives aren’t the only items that work and do not always work,
especially since many rural environments have limited budgets. One of the best ways to attract or
retain employees is to recruit employees from a similar rural background. The employees that
come from a similar background have an understanding of the culture and the challenges that are
a part of a rural community, thus there will be less of a “culture shock” (Darkwa, Newman,
Kawkab, & Chowdhry, 2015).
Feasibility for Development of the Satellite Clinic. The feasibility of this project is
very dependent on two large details: funding and staffing. The research supports the various
ways presented to reach this goal, so yes the hospital could happen, if those two details are
completed. There are of course other important details like following the CMS regulations that
need to be followed, but following regulations is an easier challenge then finding staff and initial
sources of money for the clinic.
Value-Adding Strategies. Value-adding strategies are a way of going “above and
beyond” the requirements or standard practices. They can be done pre-appointment, at the

POCAHONTAS MEMORIAL HOSPITAL CLINIC REPORT 13
appointment, and post-appointment (Ginter, Duncan, & Swyane, 2013). Pre-appointment
strategies should include the option to make appointments through an online calendar, slots of
time saved for patients who need an appointment the next day or walk it, and the ability to
collect basic information before the appointment to easy traffic and make it more convenient.
During the appointment using a timing or computer system that minimizes wait times for patients
in either the waiting room or in the actual office, comfortable and sanitary wait rooms, and space
for parents, spouses or family members to be in the appointment room if the patient needs or
wants someone there with them, all would add value to the clinic. Finally, after the appointment
staff can call after a set number of days to remind of any follow up appointments and schedule,
answer any questions the patient may have, or follow up about taking medications either
currently being used or recently taken. There can even be an email account for the clinic or
individual providers so patients can email regarding small questions after the appointment.
Strategic Initiatives. The strategic initiative of PMH is to help increase the availability
of care to the members of the county through the proposed satellite clinic. This strategic decision
allows the organization to focus on strengths such as high ratio of physicians to patient and the
desire to help create health lifestyles for their patients. Then use that edge and continue forward
to help overcome the previous mentioned weaknesses or threats. The clinic supports all
stakeholders by providing care to community members, provides job security to employees, and
helps the community overcome the health challenges the community faces.
Short-term plans for implementation. In order for the plan to be successful, there are
some items that need to be addressed. Funding needs to be secured from any and all sources that
have already been discussed. The community needs to be informed and allowed to speak, town
hall meetings have been suggested as a way to do both items at once (Farmer & Nimgeer, 2015).

POCAHONTAS MEMORIAL HOSPITAL CLINIC REPORT 14
There needs to be a decision about location and type of clinic: mobile versus stationary, done by
the board or the team selected for this project. This decision would affect the number of
employees, type of employees, and equipment needed. If the decision is for the clinic to be
freestanding, then a contractor would be needed for the building or the renovation of location.
These are all items that are needed to be successful for the satellite clinic.
Long-term plans for implementation. Once the short term plans have been
implemented and decisions made, the success of the organization and project depends on other
items. The first will be a plan on how to recruit employees for the clinic; this will probably be a
plan that needs to be constantly running to avoid shortages in staffing. Another plan needs to be
the marketing plan, showing the county that the clinic is open and the various options available
like the other clinic. There also need to be contracts with insurance companies, even though the
population is low-income, qualifying for Medicaid, with ACA there are other insurance
companies available to residents.
Evaluations and benchmarks. Every project needs places and ways to make sure the
project is preforming to standards and allow for changes to reach those marks. For the satellite
clinic there needs to be a timeline established keeping the team(s) on track with the end result of
opening. Items to be included would be funding, purchasing land, securing equipment, hiring
employees, and a timeline just for building the clinic. Once the clinic is running there needs to
ways to make sure this project is up to PMH standards of care by comparing it to the current
standards of hospital and its clinic. One would be patient satisfaction ratings through mailed
surveys. This option is low cost, but allows for the organization to receive feedback. An
important detail is the need to write the questions so they are easy to understand by majority of
the patients (Berkowitz, 2011). Another benchmark would be to prove the clinic is being used.

POCAHONTAS MEMORIAL HOSPITAL CLINIC REPORT 15
This can be done with a computer system marking out appointments and rooms (Joshi, Ransom,
Nash, & Ransom, 2014). Finally, a comparison of lab testing needs to be done, by comparing
turnaround time to the other clinic, other clinics in the area. There also needs to be a quality
assurance that the test results are correct, by using an outside party to verity results regularly
(Olusegun, 2012).
Conclusion
After conducting research on PMH, the business environment, and potential challenges
there were some items that needed to be addressed in order for the satellite clinic to be feasible.
The challenges can be overcome with work, which makes this projected clinic feasible. There do
need to be plans set in place for both short and long term implementation as well as benchmarks
to prove the benefits of the satellite clinic in Pocahontas County.

POCAHONTAS MEMORIAL HOSPITAL CLINIC REPORT 16
References
Berkowitz, E.N. (2011). Essentials of health care marketing. Jones and Bartlett Learning.
Cook, A.F. Hoas, H. (2008). Ethics and rural healthcare: What really happens? What might help?
American Journal of Bioethics, 8(4), 52-56. Doi:10.1080/15265160802166009
Capstone Project Case Study Information [Word]. (n.d.).
Centers of Medicare and Medicaid Services (2015). Retrieved from
https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/
GuidanceforLawsAndRegulations/RHC.html
County Health Roadmaps & Rankings. (n.d.) Retrieved from
http://www.countyhealthrankings.org/
Darkwa, E., Newman, M.S., Kawkab, M., & Chowdhury, M.E. (2015). A qualitative study of
factors influencing retention of doctors and nurses at rural healthcare facilities in
Bangladesh. BMC Health Services Research. 15(1), 1-12.
Farmer, J. & Nimgeer, A. (2015). Community participation to design healthcare services. BMC
Health Services Research, 14(1), 130-139. Doi:10.1186/1472-16963-14-130
Ginter, P. M. (2013). The Strategic Management of Health Care Organizations (7th Ed.). San
Francisco, CA: Jossey-Bass.
Joshi, M., Ransom, R., Nash., Ransom, S.,(2014) The Healthcare Quality Book: Vision, Strategy,
and Tools (3rd ed.). Chicago, Illinois: Health Administration Press

POCAHONTAS MEMORIAL HOSPITAL CLINIC REPORT 17
No Author (2015) Compare your country. OECD. Retrieved from
http://www.compareyourcountry.org/health?cr=oecd&lg=en
No Author. (2014). Mirror, Mirror on the Wall, 2014 Update: how the U.S. healthcare system
compares internationally. The Commonwealth Fund. Retrieved from
http://www.commonwealthfund.org/publications/fund-reports/2014/jun/mirror-mirror
Olusegun, A.P. (2012). Improving lab services and workforce in rural health facilities. Journal of
Pakistan Medical Students 2(3), 103-108
Pocahontas Memorial Hospital (no date). Retrieved from www.pmhwv.org
Solving the rural healthcare revenue conundrum. (2013). Healthcare Financial Management,
67(1), 132-3. Retrieved from https://csuglobal.idm.oclc.org/login?
url=http:search.proquest.com.csuglobal.idm.oclc.org/docview/1282582598?
accountid=38569
U.S. Department of Health & Human Services. (2013). The affordable care act: What it means
for rural America. Retrieved from
http://www.hhs.gov/healthcare/facts/factsheets/2013/09/rural09202013.html